Abstract
Objective
Although nutrition-specific interventions are designed based on maternal, household and community-level correlates, no attempt has been made to project stunting and wasting and identify intervention priorities in India. The objective of this paper is to model the stunting and wasting in the state of Odisha, India by scaling up maternal and child health interventions under alternative scenarios.
Design
This study primarily used data from National Family Health Survey 4, 2015–2016.
Measures
The LiST (Lives Saved Tool) software is used to model the nutritional outcomes and prioritise interventions. The projections were carried out under four alternative scenarios: scenario 1—if the coverage indicators continued based on past trends; scenario 2—scaled up to the level of the richest quintile; scenario 3—scaled up to that of Tamil Nadu; and scenario 4—scaled up to an aspirational coverage level.
Results
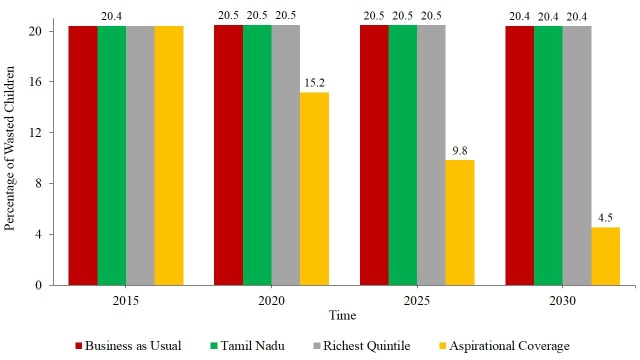
In 2015, out of 3.52 million under-5 children in Odisha, around 1.20 million were stunted. By 2030, the numbers of stunted children will be 1.11 million under scenario 1, 1.07 million under scenario 2, 1.09 million under scenario 3 and 0.89 million under scenario 4. The projected stunting level will be 25% under scenario 4 and around 31% under all other scenarios. By 2030, the level of wasting will remain unchanged at 20% under the first three scenarios and 4.3% under scenario 4. Appropriate complementary feeding would avert about half of the total stunting cases under all four scenarios, followed by zinc supplementation. Water connection at home, washing hands with soap and improved sanitation are other effective interventions.
Conclusion
Sustaining the maternal and child health interventions, promoting evidence-based stunting and wasting reduction interventions, and a multisectoral approach can achieve the World Health Assembly targets and Sustainable Development Goals of undernutrition in Odisha.
Keywords: stunting, list, odisha, India
Strengths and limitations of this study.
This is the first study that used the Lives Saved Tool (LiST) to project stunting and wasting up to 2030 under four alternative scenarios in Odisha, India.
LiST modelling takes into account coverage of interventions and population risk factors.
The study has identified priority interventions to reduce stunting in Odisha.
Due to data limitations, some default values (national estimates) have been used.
LiST modelling does not include the effects of agriculture, kitchen garden, deworming and salt iodisation on reduction of stunting.
Introduction
Reduction of malnutrition among children has been accorded high priority in global, national and local development agenda. The World Health Assembly (WHA) set six commendable targets for stunting, wasting, overweight, anaemia, low birth weight and exclusive breast feeding to improve the state of maternal and child health. It recommended that stunting be reduced by 40% from its current level and wasting to 5% among under-5 children by 2025.1 Twelve of the 17 targets of the Sustainable Development Goals (SDGs) are directly or indirectly related to malnutrition. Target 2 aims at reducing malnutrition in all forms by 2030, and target 2.2 reiterates achieving the WHA target.2 Globally, 156 million children under 5 years of age are stunted, 93 million are underweight and 50 million are wasted.3 Majority of undernourished children reside in South Asia, and India accounts for 40% of stunted children globally.4 Despite intense global, national and regional efforts, the progress on reduction of malnutrition continues to be slow and uneven across and within countries.5–8
Malnutrition among children is commonly measured using height and weight, and quantified using stunting, wasting, underweight, overweight and obesity. Stunting is a form of chronic energy deficiency and defined as the height-for-age below 2 SD of the median of the WHO reference population. Wasting is a form of acute chronic deficiency and measured as the weight-for-height below 2 SD of the median of the WHO reference population. Stunting and wasting are the outcomes of poor nutrition and healthcare during pregnancy and early childhood. The UNICEF framework distinguished the immediate cause, underlying cause and basic cause of undernutrition among children.4 Numerous studies have identified the individual, maternal, household and community correlates of stunting and wasting in low-income and middle-income countries. Maternal characteristics such as underweight, low body mass index, low educational attainment and early age at marriage are consistently associated with a high chance of stunting and wasting of under-5 children.4 9–11 Household poverty, unimproved sanitation and unhygienic practices are the key household correlates of stunting and wasting.12
A number of studies have documented the magnitude, cause and consequences of malnutrition.13–16 Malnutrition among children is associated with a number of adverse outcomes—high risk of infant and child mortality,17 18 childhood morbidity,19 20 disability and low cognitive development.21 22 The long-term economic and health consequences of nutritional deficiency are severe—low productivity, low adult height and high risk of cardiovascular diseases.23 Poverty is positively associated with the level of malnutrition at both the micro and macro levels.21 24 25
Many national and state governments of low-income and middle-income countries are implementing nutrition-specific and nutrition-sensitive intervention programmes to reduce stunting, wasting and underweight among children. Nutrition-specific interventions include increasing coverage of breast feeding, complementary foods, micronutrient supplementation, promotion of dietary diversity and feeding and maternal nutrition. Nutrition-sensitive programmes include improving access to improved water, sanitation and agricultural intervention. In India, a number of centrally and state-sponsored programmes that have a direct or an indirect effect on nutrition are operational. Notable centrally sponsored programmes implemented across the country are the National Health Mission, Swachh Bharat Abhiyan and Integrated Child Development Services (ICDS). The recently launched National Nutrition Mission (NNM) in India has a multisectoral approach across various departments that aims to reduce malnutrition. The state of Odisha has been identified as a positive deviant in implementing maternal health and nutrition.26 Evidence from many low-income and middle-income countries suggests that effective health and nutrition interventions and multisectoral coordination can reduce malnutrition in low-resource settings.5 10 21 27
Investment decisions in a low-resource setting require current levels of malnutrition, future trends and the likely effect of interventions. Recently, Lives Saved Tool (LiST)-based studies are being increasingly used among national and local governments, international organisations, bilateral donors, researchers, project planners, healthcare practitioners, non-governmental organisations (NGOs) and academia for programme evaluation, strategic planning and evidence-based decision making, setting national and global targets on nutritional and health outcomes.28 LiST is a nutrition modelling tool developed by the Institute for International Programs at Johns Hopkins Bloomberg School of Public Health, Baltimore, USA, and is available for public use (http://livessavedtool.org). LiST was initially developed in 2003 to estimate the impact of community-based interventions on reduction of under-5 mortality.29 Over the last 15 years, LiST has been updated and extended to estimate the impact of interventions on stunting, wasting, anaemia, low birth weight, birth outcome, stillbirth, maternal mortality, pneumonia and diarrhoea.21 30–34 Stunting and wasting were integrated in LiST in 2008. The default data inbuilt in LiST were taken from various reliable sources—Demographic and Health Surveys (DHS), Multiple Indicator Cluster Surveys(MICS) and WHO/UNICEF Joint Monitoring Programme, and the assumptions and methods have been drawn from a large number of empirical studies.35 The default effectiveness values are drawn from systematic reviews and meta-analyses, which allows users to use their own data at the subnational or national level. There are a number of scientific publications based on LiST in different geographical settings.29 36–40 The missed opportunity tool within LiST has been used for prioritising interventions.41 A detailed description, utility, assumptions, application and update of LiST have been published in leading health and nutrition journals.30 33 42–45
Studies from 48 Sub-Saharan African countries based on LiST analyses suggest that a modest increase in outreach intervention and addressing missed opportunities for birth can save lives.46 The LiST-based predicted neonatal mortality was close to the observed mortality rate in South Asian countries. LiST modelling was used to understand the effect of scaling up of interventions on reduction of diarrhoeal death in 68 high-priority countries.31 The estimates using LiST suggest that about 280 000 lives were saved due to different interventions in Malawi over a period of 13 years.47 Recently, LiST was used to estimate the impact of Oral Rehydration Solution (ORS) and zinc supplementation on reduction of child mortality in Bihar, India.27 LiST projection accurately modelled reduction of mortality in Ghana and underestimated in Mali due to data constraints.48 LiST modelling has also been used to examine the effect of inequality in coverage distribution by wealth quintile and place of residence on under-5 mortalities in Peru.49
Despite rising income, reduction in poverty level, increase in educational attainment, and increase in maternal and child care utilisation, stunting, wasting and underweight among children remain high in India. While the level of stunting in children under 5 years has declined from 48% in 2005–2006 to 38% in 2015–2016, the level of wasting has increased from 20% to 21% during this period.50 The national average in malnutrition conceals large variations across the states of India; the level of undernutrition is persistently high in the poorer states of India. The state-level correlation coefficient of poverty with stunting was 0.72 and with underweight 0.71, respectively.
State of child health in Odisha
Odisha, with a population of 41.9 million in 2011, is one of the poorer states in India. Demographically, the state is a paradox with a relatively low fertility rate and a high infant mortality rate. About 45.9% of the population in the state was living below the long-term poverty line compared with 29.5% at the national average.51 In 2005, the Infant Mortality Rate (IMR) of Odisha was the highest in the country—75 per 1000 live births, which reduced to 46 by 2015.52 During the last decade, the state has made commendable progress in maternal care indicators. The share of institutional births has increased from 36% in 2005–2006 to 85% in 2015–2016, but the nutritional indicators remained poor in the state. The coverage of early initiation of breast feeding increased from 54% in 2005–2006 to 69% in 2015–2016. By 2015–2016, about 34% of children under 5 were stunted, 34% were underweight and 20% were wasted.53 The level of stunting, wasting and underweight was higher than that in many states in India.
Need for the study
Political commitment, efforts of the development partner and increased allocation of national and state resources for improving the nutritional outcome in India are intense. The recently launched NNM has an estimated budget of US$1389 million (US$1=65.11 rupees) for the initial 3 years. It aimed at creating awareness about nutrition and promoting healthy feeding practices to reduce undernutrition in 200 high burden districts of India. NNM plans to reduce the level of stunting, undernutrition, anaemia and low birth weight in a time-bound manner through a multisectoral nutrition programme.54 Although studies have identified the individual, household, maternal and community determinants of stunting and wasting in India, there is no study that has projected the nutritional outcome and provided a comprehensive assessment of various nutrition and health interventions in India.7 55–59 To our knowledge, this is the first ever comprehensive study based on LiST that projects stunting and wasting trends and the effect of various interventions on reducing stunting and wasting in the state of Odisha, thus providing evidence on trends and on likely outcomes to guide investment decisions. The study is important in the state of Odisha, which has a high incidence of poverty and malnutrition. The Government of Odisha, the central government and the Azim Premji Philanthropic Initiatives are working extensively to reduce stunting and wasting in the state. In this context, it is helpful to provide the numerical estimates of stunting and wasting and assess the ability of the state to meet the SDG target by 2030. This paper examines the impact of health and nutrition interventions on the reduction of stunting and wasting in Odisha using LiST. It also estimates the number of stunting cases averted by intervention (missed opportunities).
Data and methods
Data
Data from multiple sources have been used in the study. These include Census of India, 2011, Sample Registration System (SRS) and the National Family Health Survey (NFHS). Data on single year age distribution were collected from the Census of India, 2011 and that of fertility and life expectancy at birth were taken from the SRS. The SRS is a statistical unit in the Office of the Registrar General and Census Commissioner, Ministry of Home Affairs, Government of India. It has been providing annual fertility and mortality estimates for the states of India since 1971 (www.censusindia.gov.in). The SRS used a dual recording system in data collection process, and the estimates are used extensively in research and planning. Data on Total Fertility Rate (TFR) and life expectancy at birth for the state of Odisha were taken from the SRS report and used for population projection. The population projection for the state has been carried out from 2011 to 2030. To project nutritional outcome, data from NFHS-4, 2015–2016 and projected population have been used. The NFHS-4 is the fourth in the series of DHS in India that provides comprehensive information on fertility, mortality, contraception, nutrition and health of the population. The NFHS-4 was conducted in 2015–2016 across all the states and union territories of India. A total of 190 indicators have been used for projection. Out of 190 indicators, 34 have been estimated from the unit data of NFHS-4 (files on households, women, persons and kids of Odisha and Tamil Nadu have been used), 51 were taken directly from the published NFHS-4 state report (Odisha) and 105 were the default value for India. The NFHS-4 state report provides estimates of selected indicators (http://rchiips.org/nfhs/NFHS-4Reports/Odisha.pdf). The coverage indicators (maternal care, vitamin A supplement, breast feeding, measles and pneumonia and treatment, and management of serious neonatal illness) were primarily used to understand the effect of maternal and child health intervention on the reduction of stunting and wasting. A total of 66 coverage indicators were used in estimation, and we provide the baseline value and scale-up value under each scenario as supporting documents/evidence. The variables, dimensions and indicators that have been used for nutritional projection have been grouped into 17 subgroups (supplementary appendix 1). The unit data from NFHS-4 were tabulated using STATA V.15. The nutritional outcomes are projected from 2015 to 2030 using SPECTRUM V.5.71.
bmjopen-2018-028681supp001.pdf (517KB, pdf)
Methods
The nutritional modelling in LiST requires inputs on demographic, epidemiological and maternal and child health parameters. The projection is based on a linear, mathematical and deterministic model with a fixed relationship of coverage intervention (input) and health and nutritional outcome (output).60 LiST is designed to capture the reduction in current mortality/nutrition through increase in coverage indicators and interventions. In the context of nutrition, the effectiveness of interventions is measured in terms of reduction of the number of stunting and wasting cases. The projection exercise involves two steps—projection of demographic output using the DemProj and projecting stunting and wasting using LiST. The DemProj and LiST are two important modules of SPECTRUM V.5.71. The DemProj estimates population by age group along with other demographic parameters. In the first step, we have projected the population from 2011 to 2030 as the last Census of India was available for 2011. We have used the projected population of 2015 in 5-year age groups and projected stunting and wasting from 2015 to 2030. The demographic projections of Odisha were based on the following assumptions of fertility, mortality and migration.
Assumptions on demographic projection
The trends of TFR from the SRS for the state of Odisha and the current level of TFR of Kerala are used to project the TFR by 2030. The TFR of Odisha has declined from 2.6 in 2001 to 2.2 in 2011, and to 2.0 in 2016. We kept the actual values of TFR until 2016 as these are available from the SRS and assumed to reach 1.8 by 2030. The minimum level of TFR has been kept at 1.8, currently observed for the state of Kerala. It may be mentioned that Kerala was the first Indian state to achieve the replacement level of fertility (TFR of 2.1) about two decades ago and the TFR remained around 1.8 for a long time. Thus, based on the trends of fertility decline in Odisha, it is logical to assume that the TFR of Odisha will decline from 2.0 in 2016 to 1.8 in 2030. The TFR of Odisha in 2030 is assumed to be similar to the current TFR level of Kerala. The age-specific fertility rate of Odisha in 2030 is assumed to follow Kerala’s Age Specific Fertility Rate (ASFR) pattern of 2016.
The life expectancy at birth for males was assumed to increase from 63.8 years in 2011 to 72.2 years in 2030. The life expectancy at birth for females is expected to increase from 65.9 years in 2011 to 77.9 years in 2030. The average annual increase in life expectancy is assumed to increase at 0.6 years for males and 0.65 years for females based on observed changes in recent years. The upper limit of life expectancy has been fixed at the observed level of Kerala. The state of Kerala leads the country in many maternal and child health outcomes. The IMR of Kerala was lowest in the country and the healthcare system in the state is comparatively advanced. The mortality pattern of Odisha is assumed to follow the UN South Asian model.
The population is assumed to be closed to migration.
Projection of stunting and wasting under alternative scenarios
We have projected the stunting and wasting levels of Odisha from 2015 to 2030 under four alternative scenarios. Each scenario is projected based on input in the base year and assumptions for the final year. The details of the assumptions under each scenario are given below.
Scenario 1 (business as usual)
The health coverage of 2030 is based on the past trends, known as business as usual (BAU). The changes in indicators observed during 2005–2006 and 2015–2016, the two points for which estimates of many indicators are available, form the basis of assumption under BAU. In case the estimates for the final year (2030) exceed 90%, the indicator has been fixed at 90%.
Scenario 2 (wealthiest quintile)
The current coverage is raised to the level of the richest quintile of Odisha by 2030. In case the coverage of an indicator for the wealthiest quintile is lower than that of the state average, the base year value of Odisha is used. The NFHS data do not collect data on income or consumption expenditure, but collect data on household assets, household amenities and housing structure that are used to construct a wealth index. Based on the wealth index, a wealth quintile is computed and used as a proxy for the economic well-being of the household. The wealthiest quintile refers to the population in the 80%–100% range of the wealth index and available in the data set.
Scenario 3 (best practices state—Tamil Nadu)
Tamil Nadu was selected as a comparator and the best performing state (where the stunting level is lower and health coverage is higher) from 18 major states of India. In case the coverage indicator of the best practices state is lower than that of Odisha, the base year value of Odisha is used.
Scenario 4 (aspirational coverage)
The coverage of selected indicators has been kept at 90% by 2030. If the current level of an indicator exceeds 90% in the base year, the current level is assumed to remain the same in 2030.
We have used the missed opportunity analyses to compare the relative impact of different interventions on reducing stunting and wasting. The missed opportunity analyses are based on the assumption that each individual intervention is scaled up from the current coverage to 90% during the subsequent year. In the absence of universal access to the stipulated interventions, potential undernutrition and death are termed ‘missed opportunities’.41
Patient and public involvement
Patients and the public were not involved. The paper uses secondary data available for public use.
Results
Table 1 presents a set of demographic, social, economic and health indicators of Odisha and Tamil Nadu for recent years. Demographically and economically, Tamil Nadu is an advanced state, while Odisha is a poor performing state in India. The infant mortality rate in Tamil Nadu was 19 per 1000 live births compared with 46 in Odisha.52 The life expectancy at birth for both male and female in Tamil Nadu was higher than that in Odisha.61 The socioeconomic indicators of Tamil Nadu are also better than those of Odisha. About half of the population in Odisha is living below the poverty line compared with one-fifth in Tamil Nadu.51 The per capita income of Odisha is about half of Tamil Nadu’s.62 With respect to stunting, wasting and underweight, the current levels in Tamil Nadu are lower than those in Odisha.50 The coverage of maternal care suggests that institutional delivery, antenatal and natal care are higher in Tamil Nadu than in Odisha.50
Table 1.
Key demographic, social, economic and health indicators of Odisha and Tamil Nadu
| Variable | Sources & Year | Odisha | Tamil Nadu |
| Demographic | |||
| Total population | Census of India 2011 | 41 974 218 | 72 147 030 |
| Sex ratio | Census of India 2011 | 978 | 995 |
| Total fertility rate | SRS 2015 | 2.0 | 1.6 |
| Infant mortality rate | SRS 2015 | 46.0 | 19.0 |
| Life expectancy (male) | SRS 2012–2016 | 66.2 | 69.5 |
| Life expectancy (female) | SRS 2012–2016 | 69.1 | 73.4 |
| Life expectancy (person) | SRS 2012–2016 | 67.6 | 71.4 |
| Social | |||
| Female literacy rate | Census of India 2011 | 64.4 | 73.9 |
| Percentage of population below poverty line | Rangarajan Committee, 2011–2012 | 45.9 | 22.4 |
| Economic | |||
| Per capita state domestic product (rupees) | RBI, 2014–2015 | 64 869.0 | 128 385.0 |
| Health | |||
| Stunting | NFHS-4, 2015–2016 | 34.1 | 27.1 |
| Wasting | NFHS-4, 2015–2016 | 20.4 | 19.7 |
| Underweight | NFHS-4, 2015–2016 | 34.4 | 23.8 |
| Institutional delivery | NFHS-4, 2015–2016 | 85.4 | 98.9 |
| Antenatal care* | NFHS-4, 2015–2016 | 82.9 | 91.7 |
| Postnatal care† | NFHS-4, 2015–2016 | 78.6 | 74.2 |
*Receiving antenatal care from a skilled provider.
†Postnatal check within 2 days of birth.
NFHS-4, National Family and Health Survey 4; RBI, Reserve Bank of India; SRS, Sample Registration System.
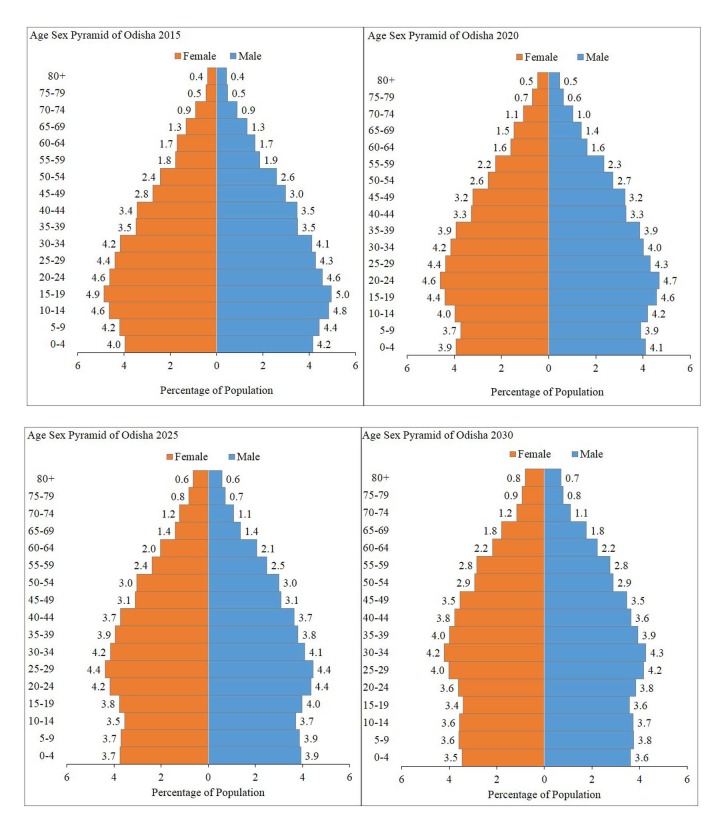
Figure 1 presents the age–sex pyramid of Odisha for four time periods—2015, 2020, 2025 and 2030. The population of Odisha was projected to be 43.8 million in 2015, 46.2 million in 2020, 48.4 million in 2025 and 50.3 million in 2030. The shape of the pyramid, depicting the age and sex structure, is expected to be narrower by 2030, largely due to falling fertility and increasing longevity. In 2015, the age structure of the population was similar to that of a population which had experienced declining mortality and fertility in recent years. About 26.2% of the population in 2015 were under 15 years of age and 9.6% were 60 years and above. By 2030, about 21.7% of the population in the state will be less than 15 years of age and 13.5% will be 60 years and above.
Figure 1.
Per cent distribution of population by age and sex (age–sex pyramid) of Odisha, 2015, 2020, 2025 and 2030.
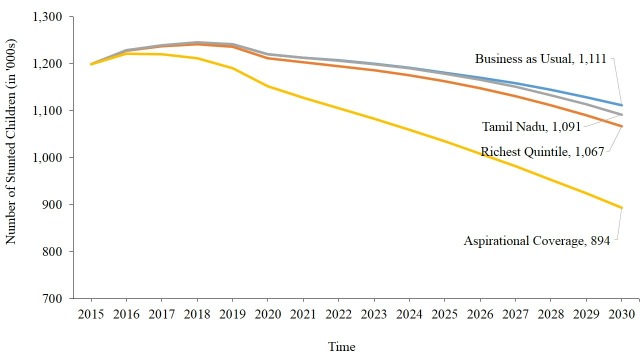
Figure 2 presents the number of stunted children under 5 in Odisha under alternative scenarios. Under ‘Business as Usual’, the total number of stunted children in Odisha was projected at 1.2 million in 2015, 1.22 million in 2020 and 1.11 million in 2030. If the coverage indicators of Odisha are scaled up to the level prevailing in Tamil Nadu by 2030, the number of stunted children will be 1.09 million by 2030. It will be 1.07 million if the health coverage is scaled up to the richest quintile of Odisha by 2030. The number of stunting cases under aspirational coverage would be minimum for all time periods (0.89 million in 2030) in the state. Under all three scenarios except aspirational coverage, the number of stunted children is likely to start declining from 2019 onwards. Under aspirational coverage, the number of stunted cases is likely to decline continuously from 2017.
Figure 2.
Projected number of stunting children under 5 in alternative scenarios in Odisha, 2015–2030.
Online supplementary appendix 1 presents the projected level of stunting by age group under alternative scenarios in Odisha. Under all four scenarios, the level of stunting in age groups 6–11 months, 12–23 months and 24–59 months is expected to decrease during the coming decade. Among all four scenarios, the aspirational coverage has a faster rate of decrease in the level of stunted children across all age groups. The least decline would be for children under 1 month.
Online supplementary appendix 2 presents the projected number of stunted children under alternative scenarios in Odisha by different age groups. The age group 24–59 months has the largest number of stunted children. About 0.77 million children in the age group 24–59 months were stunted in 2015 and were likely to reduce to 0.73 million by 2030 under ‘Business as Usual’. The number of stunting cases in each age group will be smaller under aspirational coverage.
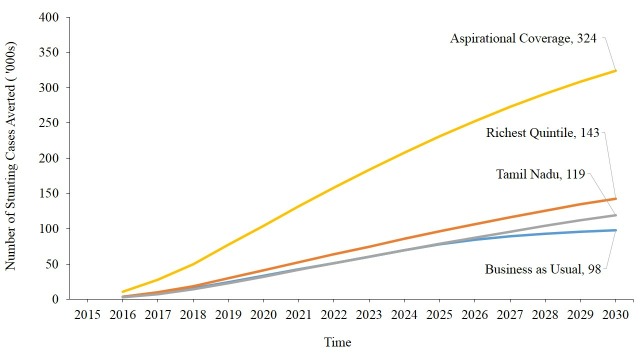
Figure 3 presents the cumulative number of stunting cases that would be avoided under alternative scenarios during 2015–2030. Under BAU, about 97 559 child stunting cases would be avoided by 2030. If the health coverage is scaled up to the level prevailing in the best practices state (Tamil Nadu), about 118 905 stunting cases can be avoided. The number of stunting cases averted will be higher if the coverage is scaled up to the health coverage of the richest quintile by 2030. Under aspirational coverage, about 323 533 child stunting cases are likely to be avoided by 2030.
Figure 3.
Projected number of stunting cases averted among children under 5 under alternative scenarios in Odisha, 2016–2030.
Online supplementary appendix 3 presents the projected number of stunting cases averted under alternative scenarios in Odisha by age groups. The pace of decrease in the number of stunting cases averted is faster under the aspirational coverage scenario as compared with other scenarios.
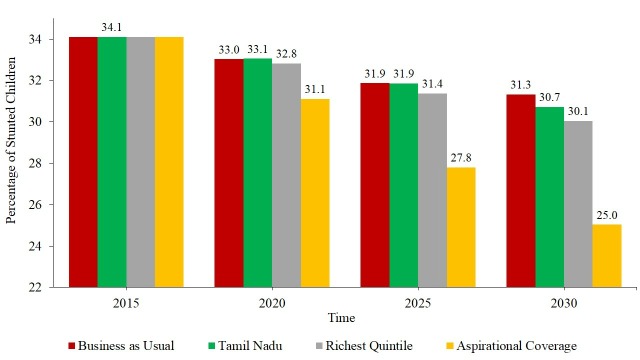
Figure 4 presents the projected level of stunting in children under alternative scenarios. Under BAU, the level of child stunting in Odisha is expected to decline from 34.1% in 2015 to 31.3% in 2030. The current level of health coverage in the state is relatively high, and the state has made considerable progress in increasing health coverage over the last decade. If the current health coverage is scaled up to the health practices of the richest quintile, the level of child stunting is projected to decline to 30.1% in 2030. And if the extent of health practices reaches that of Tamil Nadu in 2030, the stunting level is expected to reach 30.7%. But if health coverage is scaled up to aspirational coverage, the child stunting level is expected to be 25.0% in 2030.
Figure 4.
Projected level of stunting among under-5 children under alternative scenarios in Odisha, 2015–2030.
Figure 5 presents the level of wasting among children under 5 projected under alternative scenarios in Odisha. Under BAU, the level of wasting is likely to remain unchanged in 2030 (20.4%). The levels of wasting projected under the richest quintile scenario and that prevailing in Tamil Nadu yield similar estimates. If the health coverage is scaled up to the aspirational 90% coverage, wasting in children may reduce to 4.5% in 2030. Like stunting, wasting in children may be reduced significantly under aspirational coverage.
Figure 5.
Projected level of wasting among under-5 children under alternative scenarios in Odisha, 2015–2030.
Online supplementary appendix 4 presents the estimates of wasting level projected under alternative scenarios in Odisha by different age groups. In all five age groups in all three scenarios except that of aspirational coverage, the level of wasting is expected to be similar over time.
Table 2 presents the number of stunting cases averted by each of the interventions under four alternative scenarios at four points of time. Under each scenario, appropriate complementary feeding practices will avert the largest number of stunting cases in each time period. In the case of BAU, appropriate feeding practices will avert 56 148 child stunting cases, accounting for 53% of stunting cases by 2030. The estimated number of stunting cases averted due to complementary feeding under the richest quintile was 70.523, about 50% of the stunting cases averted. The pattern was similar with respect to aspirational coverage. The second next effective intervention for reducing stunting in children was zinc supplement in all three scenarios except that of Tamil Nadu. Water connection at home, washing hands with soap and improved sanitation also have a considerable impact on the reduction of stunting in all these scenarios.
Table 2.
Projected number of stunting cases averted among children under 5 by type of interventions and alternative scenarios in Odisha, 2015–2030
| Stunting cases averted (Number) | Percentage of stunting cases averted by 2030 due to | ||||
| 2016 | 2020 | 2025 | 2030 | ||
| Business as usual | |||||
| Appropriate complementary feeding | 1164 | 15 053 | 37 457 | 56 148 | 53.04 |
| Zinc supplementation | 1434 | 10 922 | 24 173 | 25 812 | 24.38 |
| Improved sanitation—utilisation of latrines or toilets | 279 | 2957 | 6884 | 7845 | 7.41 |
| Water connection at home | 267 | 2827 | 6582 | 7500 | 7.08 |
| Hand washing with soap | 196 | 2076 | 4834 | 5509 | 5.20 |
| Vitamin A supplementation | 83 | 816 | 1876 | 2126 | 2.01 |
| ITN/IRS—households protected from malaria | 13 | 256 | 644 | 745 | 0.70 |
| Rotavirus vaccine | 11 | 72 | 150 | 181 | 0.17 |
| Total | 3447 | 34 979 | 82 600 | 105 866 | 100.00 |
| Richest quintile | |||||
| Appropriate complementary feeding | 1446 | 18 693 | 46 472 | 70 523 | 49.52 |
| Zinc supplementation | 957 | 7355 | 16 253 | 23 871 | 16.76 |
| Improved sanitation—utilisation of latrines or toilets | 674 | 6928 | 15 695 | 22 414 | 15.74 |
| Water connection at home | 540 | 5547 | 12 566 | 17 945 | 12.60 |
| Hand washing with soap | 135 | 1385 | 3138 | 4481 | 3.15 |
| Age-appropriate breastfeeding practices | 16 | 258 | 611 | 878 | 0.62 |
| Birth intervals | 12 | 196 | 512 | 819 | 0.58 |
| Vitamin A supplementation | 22 | 210 | 473 | 675 | 0.47 |
| ITN/IRS—households protected from malaria | 12 | 178 | 438 | 655 | 0.46 |
| Rotavirus vaccine | 11 | 56 | 106 | 144 | 0.10 |
| Total | 3825 | 40 806 | 96 264 | 142 405 | 100.00 |
| Best practices—Tamil Nadu | |||||
| Appropriate complementary feeding | 1774 | 22 984 | 57 113 | 87 059 | 72.68 |
| Water connection at home | 595 | 6467 | 15 012 | 22 077 | 18.43 |
| Improved sanitation—utilisation of latrines or toilets | 283 | 3075 | 7138 | 10 497 | 8.76 |
| Rotavirus vaccine | 11 | 56 | 110 | 153 | 0.13 |
| Total | 2663 | 32 582 | 79 373 | 119 786 | 100.00 |
| Aspirational coverage | |||||
| Appropriate complementary feeding | 3167 | 41 293 | 99 725 | 147 267 | 45.63 |
| Zinc supplementation | 3916 | 28 091 | 60 116 | 85 790 | 26.58 |
| Water connection at home | 1899 | 16 983 | 33 891 | 42 837 | 13.27 |
| Hand washing with soap | 727 | 6507 | 12 986 | 16 414 | 5.09 |
| Improved sanitation—utilisation of latrines or toilets | 637 | 5700 | 11 375 | 14 378 | 4.46 |
| Age-appropriate breastfeeding practices | 229 | 2593 | 5335 | 6747 | 2.09 |
| ITN/IRS—households protected from malaria | 171 | 1991 | 4571 | 6537 | 2.03 |
| Vitamin A supplementation | 105 | 897 | 1782 | 2254 | 0.70 |
| Rotavirus vaccine | 11 | 156 | 372 | 497 | 0.15 |
| Total | 10 862 | 104 211 | 230 153 | 322 721 | 100.00 |
ITN, Insecticide-Treated Nets; IRS, Indore Residual Spraying.
Table 3 presents the number of childhood stunting cases averted by type of interventions in Odisha during 2015–2030, using missed opportunity analyses. The missed opportunity is estimated by increasing the coverage to 90% in the following year. Although the outcome of missed opportunity is unrealistic, it gives an idea about how to prioritise intervention strategies to reduce the stunting and wasting in the state. Appropriate complementary feeding, zinc supplementation, water connection at home, washing hands with soap, improved sanitation and hygienic disposal of children’s stools are the top 6 interventions for averting stunting in Odisha. These interventions are identified in table 2. A total of 123 254 cases of stunting are expected to be averted by appropriate complementary feeding. Zinc supplementation is expected to avert stunting of around 97 003 cases, while water connection at home is estimated to avert 76 178 cases of stunting, and washing hands with soap is expected to avert stunting of 30 555 cases. Improved sanitation is expected to avert nearly 26 402 cases of stunting in the state.
Table 3.
Number of stunting cases averted by type of interventions under missed opportunity analysis in Odisha, 2015–2030
| Stunting cases averted (Number) | Percentage of stunting cases averted by intervention | Baseline coverage | Scale-up coverage | |
| Appropriate complementary feeding | 123 254 | 31.20 | 22.2 | 90 |
| Zinc supplementation | 97 003 | 24.56 | 17.0 | 90 |
| Water connection at home | 76 178 | 19.28 | 9.6 | 90 |
| Hand washing with soap | 30 555 | 7.74 | 17.0 | 90 |
| Improved sanitation—utilisation of latrines or toilets | 26 402 | 6.68 | 33.7 | 90 |
| Intermittent preventive treatment of malaria during pregnancy | 10 051 | 2.54 | 0 | 90 |
| ITN/IRS—households protected from malaria | 9039 | 2.29 | 56.78 | 90 |
| Balanced energy supplementation | 8877 | 2.25 | 0 | 90 |
| Breastfeeding promotion | 4994 | 1.26 | 48.1 | 90 |
| Vitamin A supplementation | 4856 | 1.23 | 69.7 | 90 |
| Calcium supplementation | 2475 | 0.63 | 0 | 90 |
| Rotavirus vaccine | 1338 | 0.34 | 5.0 | 90 |
| Total | 395 022 | 100.00 |
Discussion and conclusion
Global progress in the reduction of malnutrition and realising the WHA/SDG targets at the national level is contingent on reduction of stunting and wasting in the poorer states of India. Although the Government of India, the Government of Odisha, international organisations and NGOs are working on multiple nutrition-specific and nutrition-sensitive interventions, no comprehensive study has examined the impact of various intervention on the reduction of stunting and wasting in India. This is the first ever comprehensive study that examines the impact of various interventions on the reduction of stunting and wasting under four alternative scenarios in the state of Odisha. Reduction in infant and under-5 mortality in the post-National Health Mission period was faster in Odisha than in many other states in India. Maternal and child health has improved significantly. However, the level of stunting and wasting was higher in Odisha than that in many states in India, including Tamil Nadu and Kerala. We have projected stunting and wasting under four alternative scenarios and identified priority interventions for reducing malnutrition in the state.
Our salient findings are as follows:
The population of Odisha is expected to increase from 43.8 million in 2015 to 50.3 million in 2030. The number of under-5 children was 3.55 million in 2015 and likely to remain stable at 3.56 million over the next 15 years. By 2030, the projected level of stunted children is likely to be the lowest under aspirational coverage (25%), similar to that under the richest quintile and Tamil Nadu coverage (30.1% and 30.7%, respectively) and highest under BAU (31.3%). The number of stunting cases averted under aspirational coverage would be more than three times higher than that under BAU and twice that of the richest quintile. The projected level of stunting is not expected to reach the WHA/SDG target under any of the scenarios.
The reduction in wasting is likely to decline to 4.5% under the aspirational coverage level but remains similar to the base level under all the other three scenarios. The projected level of wasting is expected to reach the WHA target of less than 5% by 2025 if the aspirational coverage is reached.
Results from these four scenarios are consistent in identifying the intervention priority. Appropriate complementary feeding followed by zinc supplementation, washing hands with soap and improved sanitation are four interventions that are expected to reduce a large number of stunting cases in the state. By 2030, appropriate complementary feeding practice is likely to reduce about half of the stunting cases under each of the scenarios. Zinc supplementation is also a priority intervention for the reduction of stunting in the state.
The Government of Odisha is committed to implementing several innovative state-specific schemes to improve the health and nutrition outcome. In 2011, the Department of Women and Child Development, Government of Odisha launched "Mamata", a hundred per cent, state-sponsored conditional cash transfer maternal benefit scheme to increase utilisation of maternal and child healthcare services and infant and young child feeding practices in the state. It entitles a sum of 6000 rupees to pregnant and lactating mothers over a period of about 18 months in instalments. It covered all pregnant and lactating mothers of 19 years and above for the first two births and not working in government/public sector undertaking. Evaluative studies suggest that the scheme was successful in improving at least seven maternal care variables such as pregnancy registration, antenatal care, exclusive breast feeding, full immunisation and so on, and household food security.60 A total number of 547 000 mothers were beneficiaries for the financial year 2017–2018 with a budget allocation of 378.37 cores rupees. The state has been identified as a positive deviant in implementing the maternal health and nutrition programmes.27 Besides, the Odisha Multi-Sector Nutrition Action Plan, in partnership with Azim Premji Philanthropic Initiatives, was launched to increase the coverage of nutrition-specific and nutrition-sensitive interventions through a multisectoral convergence model to realise the WHA and SDG targets. It aims at increasing demand and improved delivery of nutrition-related services, increased state capacity and commitment to nutrition, improved multisectoral planning and coordination, and improved political commitment and leadership for nutrition.61 Over the years, the programme has built partnerships, piloted projects and mainstreamed the interventions with the help of existing platforms and through convergence with schemes/programmes of government departments.
Our findings on prioritising interventions are consistent across literature. Literature suggests the positive effect of complementary feeding on the reduction of malnutrition in low-income and middle-income countries,62 and our findings also suggest that complementary feeding is the most nutrition-specific intervention. The current level of complementary feeding practices is extremely low, and scaling up the coverage to 90% would reduce stunting significantly. With a reversing trend on timely introduction of complementary foods and the extremely low proportion of children with adequate diet, the current level of stunting and wasting cannot be reduced without complementary feeding practices. While exclusive breast feeding is recommended until 6 months of life, complementary feeding from 6 to 23 months is essential to reduce stunting among children under 2 years, which contributes significantly to under-5 stunting. The state needs to invest to promote and support optimal complementary feeding practices. This can be effected through information, education and communication activities, and educating mothers on complementary feeding practices. Second, our results also highlight the role of zinc supplementation in the reduction of stunting in the state. Zinc supplementation helps in cellular growth and cellular metabolism, and has a proven effect on reducing stunting of children until prepuberty.63–65 Currently zinc supplementation is less than 20%, and increasing the level to 90% level will avert about 97 000 stunting cases. Third, we recommend sustaining the current level of health and nutrition schemes in the state and extend "Mamata" to cover the initial 1000 days of life, which may have a significant effect on improving nutritional outcomes among under-2 children. During conception and 1000 days of life, the development of the brain is enormous, and therefore the intake of vitamins, minerals and other nutrients is essential for healthy development to help achieve nutritional outcomes for under-5 children. The cash incentives may be enhanced depending on resources and budget. Fourth, besides nutrition-specific interventions, nutrition-sensitive interventions can help the state bridge the gap for nutrition outcomes. Recently the Government of Odisha has taken the initiative of reducing malnutrition through increased millet production across 30 blocks, spreading across seven tribal-dominated districts of Odisha. One of the main objectives of the programme is inclusion of millets in state nutrition programmes such as the ICDS, Mid-Day Meal Scheme, Integrated Tribal Development Agency, Welfare Hostels and eventually in the Public Distribution System. Increased production and consumption of millets are given priority to address both increased crop failures and nutritional deficiency. Millets are rich in calories, protein, fibre, vitamins and minerals. Depending on the success of the existing programme, it may be scaled up to the remaining geography of the state. Fifth, we suggest that studies on the effect of early initiation and exclusive breast feeding, dietary diversity, and management of severe and acute malnutrition be undertaken in the state, although they were not captured in the modelling exercise. Similarly, LiST modelling does not account for the effect of deworming and salt iodisation. Zinc supplementation for 12–59 months of children is currently a non-existent programme and needs to be initiated in the state of Odisha. Also, water connection at home is both a community-level and household-level intervention. According to the NFHS-4, only 10% of the households had piped water connection at home and such provisioning in remote rural areas was very low. Provision of water facilities at home required larger public investment. Similarly, improving sanitation was given priority under the Swachh Bharat Abhiyan, and the coverage of improved sanitation in 2015 was 61% in urban and 23% in rural Odisha. An increase in the use of improved sanitation coverage to 90% will avert stunting cases. Last, the management of severe and moderate acute malnutrition plays an important role in the reduction of wasting among under-5 children. Odisha has only facility-based management of severely acutely malnourished children and refers the children to nutrition rehabilitation centres for infection control and restoring appetite. Currently, there is no existing programme in the state to take care of moderately or acutely malnourished children.
We mention the following limitations of the study. Despite its comprehensive coverage, the study does not include estimates of intervention effects of deworming and salt iodisation in projection. The nutrition-sensitive intervention programmes in agriculture, education and child development are proven to reduce stunting and wasting. Second, owing to lack of data at the state level, a number of default values at the national/global level were considered in estimation. Perhaps, more precise estimates could have been derived using data at the state level. Third, LiST is based on a set of assumptions and constant relationship of input and output. Despite this limitation, the estimates serve as a guiding block in designing nutrition-sensitive and nutrition-specific programmes in the state.
To conclude, efforts to sustain high coverage of maternal (antenatal, natal and postnatal care), child health and nutrition interventions (early initiation of breast feeding, exclusive breast feeding and so on) and increase the coverage of low coverage interventions (paediatric Iron Folic Acid(IFA), zinc supplementation during diarrhoea and supplementary feeding) must be stepped up to meet the WHA and SDG targets in Odisha and in the country.
Supplementary Material
Acknowledgments
Authors thank the Azim Premji Philanthropic Initiative, Bengaluru for providing the Publication fees of this article
Footnotes
Contributors: NRM, SKM and MS conceptualised and designed the study. DM and SKM reviewed the literature for relevant data and documentation. WBM and SKM compiled the data and performed the analysis. NRM, SKM and MS prepared the first draft of the manuscript. SKM provided the overall supervision in preparation of the manuscript. All authors read and approved the final manuscript.
Competing interests: None declared.
Ethics approval: This study is a projection exercise and the input is based on publicly available data (National Family Health Survey, 2015–2016) and with no access to personal identifiers.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data used in this study for analysis are publicly available and can be obtained from http://rchiips.org/NFHS/index.shtml. The unit-level data are also available from the Demographic and Health Survey (DHS) data repository and could be accessed upon data request subject to non-profit and academic interest only. In another case, the corresponding author of the paper should be contacted.
Patient consent for publication: Not required.
References
- 1. World Health Organization. Global Nutrition Monitoring Framework: Operational Guidance for tracking progress in meeting targets for 2025, 2017. [Google Scholar]
- 2. United Nations. Report of the Inter-Agency and Expert Group on Sustainable Development Goal Indicators. E/CN.3/2016/2/Rev.1, 2016. [Google Scholar]
- 3. World Health Organization. Health in 2015: From MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals, 2015. [Google Scholar]
- 4. Nutrition IC. The achievable imperative for global progress New York. New York, NY, USA: NY United Nations Children’s Fund, 2013. [Google Scholar]
- 5. International Food Policy Research Institute. Global Nutrition report 2016: from promise to impact: ending malnutrition by 2030. Washington, DC, 2016. [Google Scholar]
- 6. Van de Poel E, Hosseinpoor AR, Speybroeck N, et al. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Organ 2008;86:282–91. 10.2471/BLT.07.044800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Bank. Socioeconomic inequalities in child malnutrition in the developing world policy research working paper 2434, 2000. [Google Scholar]
- 8. Panda BK, Mohanty SK. Progress and prospects of health-related sustainable development goals in india. J Biosoc Sci 2019;51:335–52. 10.1017/S0021932018000202 [DOI] [PubMed] [Google Scholar]
- 9. Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. The Lancet 2008;371:417–40. 10.1016/S0140-6736(07)61693-6 [DOI] [PubMed] [Google Scholar]
- 10. Black RE, Alderman H, Bhutta ZA, et al. Maternal and child nutrition: building momentum for impact. Lancet 2013;382:372–5. 10.1016/S0140-6736(13)60988-5 [DOI] [PubMed] [Google Scholar]
- 11. Vollmer S, Bommer C, Krishna A, et al. The association of parental education with childhood undernutrition in low- and middle-income countries: comparing the role of paternal and maternal education. Int J Epidemiol 2017;46:dyw133–23. 10.1093/ije/dyw133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cumming O, Cairncross S, Water C. Can water, sanitation and hygiene help eliminate stunting? Current evidence and policy implications. Matern Child Nutr 2016;12 Suppl 1:91–105. 10.1111/mcn.12258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008;371:243–60. 10.1016/S0140-6736(07)61690-0 [DOI] [PubMed] [Google Scholar]
- 14. Bryce J, Coitinho D, Darnton-Hill I, et al. Maternal and child undernutrition: effective action at national level. Lancet 2008;371:510–26. 10.1016/S0140-6736(07)61694-8 [DOI] [PubMed] [Google Scholar]
- 15. Morris SS, Cogill B, Uauy R. Effective international action against undernutrition: why has it proven so difficult and what can be done to accelerate progress? Lancet 2008;371:608–21. 10.1016/S0140-6736(07)61695-X [DOI] [PubMed] [Google Scholar]
- 16. Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340–57. 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Van Lerberghe W. The world health report 2008: primary health care: now more than ever: World Health Organization, 2008. [Google Scholar]
- 18. UNICEF. The State of the world’s children 1998: executive summary, 1998. [Google Scholar]
- 19. Torlesse H, Kiess L, Bloem MW. Association of household rice expenditure with child nutritional status indicates a role for macroeconomic food policy in combating malnutrition. J Nutr 2003;133:1320–5. 10.1093/jn/133.5.1320 [DOI] [PubMed] [Google Scholar]
- 20. Sari M, de Pee S, Bloem MW, et al. Higher household expenditure on animal-source and nongrain foods lowers the risk of stunting among children 0-59 months old in Indonesia: implications of rising food prices. J Nutr 2010;140:195S–200. 10.3945/jn.109.110858 [DOI] [PubMed] [Google Scholar]
- 21. Bhutta ZA, Das JK, Rizvi A, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 2013;382:452–77. 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- 22. Horton S, Steckel RH. Malnutrition: global economic losses attributable to malnutrition 1900–2000 and projections to 2050. how much have global problems cost the earth? A Scorecard from 1900 to. 2013 Oct 10, 2050:247–72. [Google Scholar]
- 23. Subramanian SV, Kawachi I, Inequality I. and Health: What have we Learned so far? Epidemiologic Reviews 2004;26:78–91. [DOI] [PubMed] [Google Scholar]
- 24. Svedberg P. Poverty and undernutrition: theory, measurement, and policy: Clarendon Press, 2000. [Google Scholar]
- 25. Vollmer S, Harttgen K, Kupka R, et al. Levels and trends of childhood undernutrition by wealth and education according to a Composite Index of Anthropometric Failure: evidence from 146 Demographic and Health Surveys from 39 countries. BMJ Glob Health 2017;2:e000206 10.1136/bmjgh-2016-000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kohli N, Avula R, van den Bold M, et al. What will it take to accelerate improvements in nutrition outcomes in Odisha? Learning from the past. Glob Food Sec 2017;12:38–48. 10.1016/j.gfs.2017.01.007 [DOI] [Google Scholar]
- 27. Ayyanat JA, Harbour C, Kumar S, et al. LiST modelling with monitoring data to estimate impact on child mortality of an ORS and zinc programme with public sector providers in Bihar, India. BMC Public Health 2018;18:103 10.1186/s12889-017-5008-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stegmuller AR, Self A, Litvin K, et al. How is the Lives Saved Tool (LiST) used in the global health community? Results of a mixed-methods LiST user study. BMC Public Health 2017;17:773 10.1186/s12889-017-4750-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? The Lancet 2003;362:65–71. 10.1016/S0140-6736(03)13811-1 [DOI] [PubMed] [Google Scholar]
- 30. Walker N, Tam Y, Friberg IK. Overview of The Lives Saved Tool (LiST). 13, 2013:S1 10.1186/1471-2458-13-S3-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fischer Walker CL, Friberg IK, Binkin N, et al. Scaling up diarrhea prevention and treatment interventions: a Lives Saved Tool analysis. PLoS Med 2011;8:e1000428 10.1371/journal.pmed.1000428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blencowe H, Cousens S, Kamb M, et al. Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health 2011;11 Suppl 3:S9 10.1186/1471-2458-11-S3-S9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kozuki N, Katz J, Clermont A, et al. New Option in the Lives Saved Tool (LiST) Allows for the Conversion of Prevalence of Small-for-Gestational-Age and Preterm Births to Prevalence of Low Birth Weight. J Nutr 2017;147:2141S–6. 10.3945/jn.117.247767 [DOI] [PubMed] [Google Scholar]
- 34. Fischer Walker CL, Walker N, Walker N. The Lives Saved Tool (LiST) as a model for diarrhea mortality reduction. BMC Med 2014;12:70 10.1186/1741-7015-12-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fox MJ, Martorell R, van den Broek N, et al. Assumptions and Methods in The Lives Saved Tool (LiST). 11, 2011:I1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Boschi-Pinto C, Young M, Black RE. The Child Health Epidemiology Reference Group reviews of the effectiveness of interventions to reduce maternal, neonatal and child mortality. Int J Epidemiol 2010;39(suppl_1):i3–i6. 10.1093/ije/dyq018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Steinglass R, Cherian T, Vandelaer J, et al. Development and use of the Lives Saved Tool (LiST): a model to estimate the impact of scaling up proven interventions on maternal, neonatal and child mortality. Int J Epidemiol 2011;40:519–20. 10.1093/ije/dyq173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Winfrey W, McKinnon R, Stover J. Methods used in the Lives Saved Tool (LiST). BMC Public Health 2011;11 Suppl 3:S32 10.1186/1471-2458-11-S3-S32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Darmstadt GL, Bhutta ZA, Cousens S, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 2005;365:977–88. 10.1016/S0140-6736(05)71088-6 [DOI] [PubMed] [Google Scholar]
- 40. George CM, Vignola E, Ricca J, et al. Evaluation of the effectiveness of care groups in expanding population coverage of Key child survival interventions and reducing under-5 mortality: a comparative analysis using the lives saved tool (LiST). BMC Public Health 2015;15:835 10.1186/s12889-015-2187-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tam Y, Pearson L. Using the missed opportunity tool as an application of the Lives Saved Tool (LiST) for intervention prioritization. BMC Public Health 2017;17:735 10.1186/s12889-017-4736-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mayberry A, Morris S. Introduction to Nutrition Modeling in the Lives Saved Tool (LiST). J Nutr 2017;147:2129S–31S. 10.3945/jn.116.245746 [DOI] [PubMed] [Google Scholar]
- 43. Clermont A, Walker N. Nutrition Interventions in the Lives Saved Tool (LiST). J Nutr 2017;147:jn243766–40S. 10.3945/jn.116.243766 [DOI] [PubMed] [Google Scholar]
- 44. Boschi-Pinto C, Black RE. Development and use of the Lives Saved Tool: a model to estimate the impact of scaling up proven interventions on maternal, neonatal and child mortality. Int J Epidemiol 2011;40:520–1. 10.1093/ije/dyq171 [DOI] [PubMed] [Google Scholar]
- 45. Friberg IK, Bhutta ZA, Darmstadt GL, et al. Comparing modelled predictions of neonatal mortality impacts using LiST with observed results of community-based intervention trials in South Asia. Int J Epidemiol 2010;39 Suppl 1(suppl_1):i11–i20. 10.1093/ije/dyq017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Friberg IK, Kinney MV, Lawn JE, et al. Sub-Saharan Africa’s mothers, newborns, and children: how many lives could be saved with targeted health interventions? PLoS Med 2010;7:e1000295 10.1371/journal.pmed.1000295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kanyuka M, Ndawala J, Mleme T, et al. Malawi and Millennium Development Goal 4: a Countdown to 2015 country case study. Lancet Glob Health 2016;4:e201–14. 10.1016/S2214-109X(15)00294-6 [DOI] [PubMed] [Google Scholar]
- 48. Hazel E, Gilroy K, Friberg I, et al. Comparing modelled to measured mortality reductions: applying the Lives Saved Tool to evaluation data from the Accelerated Child Survival Programme in West Africa. Int J Epidemiol 2010;39(suppl_1):i32–i39. 10.1093/ije/dyq019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tam Y, Huicho L, Huayanay-Espinoza CA, et al. Remaining missed opportunities of child survival in Peru: modelling mortality impact of universal and equitable coverage of proven interventions. BMC Public Health 2016;16:1048 10.1186/s12889-016-3668-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS. 2017a. http://rchiips.org/NFHS/NFHS-4Reports/India.pdf (Accessed on 20 Apr 2018).
- 51. NITI Aayog. Nourishing India. National Nutrition Strategy, Government of India. 2018. http://niti.gov.in/writereaddata/files/document_publication/Nutrition_Strategy_Booklet.pdf (Accessed on 22 Apr 2018).
- 52. Joe W, Mishra US, Navaneetham K. Health Inequality in India: Evidence from NFHS 3. Economic and Political Weekly 2008;2:41–7. [Google Scholar]
- 53. Mazumdar S. Determinants of Inequality in Child Malnutrition in India: The Poverty-Undernutrition Linkage. Asian Population Studies 2010;6:307–33. [Google Scholar]
- 54. Kumar A, Kumari D, Singh A. Increasing socioeconomic inequality in childhood undernutrition in urban India: trends between 1992-93, 1998-99 and 2005-06. Health Policy Plan 2015;30:1003–16. 10.1093/heapol/czu104 [DOI] [PubMed] [Google Scholar]
- 55. Khan J, Mohanty SK. Spatial heterogeneity and correlates of child malnutrition in districts of India. BMC Public Health 2018;18:1027 10.1186/s12889-018-5873-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fenske N, Burns J, Hothorn T, et al. Understanding child stunting in India: a comprehensive analysis of socio-economic, nutritional and environmental determinants using additive quantile regression. PLoS One 2013;8:e78692 10.1371/journal.pone.0078692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Raghunathan K, Chakrabarti S, Avula R, et al. Can conditional cash transfers improve the uptake of nutrition interventions and household food security? Evidence from Odisha’s Mamata scheme. PLoS One 2017;12:e0188952 10.1371/journal.pone.0188952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Garnett GP, Cousens S, Hallett TB, et al. Mathematical models in the evaluation of health programmes. Lancet 2011;378:515–25. 10.1016/S0140-6736(10)61505-X [DOI] [PubMed] [Google Scholar]
- 59. Office of the Register General. Sample Registration System, Abridged Life Tables 2012-16. New Delhi: Office of the Registrar General, India. 2018. http://www.censusindia.gov.in/Vital_Statistics/SRS_Life_Table/SRS-12-16/3.Lftb%202012-16_85.pdf (Accessed on 31 may 2018).
- 60. RBI. Handbook of Statistics on the Indian Economy 2016-17: RBI Bulletin, Mumbai. 2017. https://rbidocs.rbi.org.in/rdocs/Publications/PDFs/0HANDBOOK2017C9CF31D4B78241C9843272E441CD7010.PDF (Accessed on 31 May 2018).
- 61. Government of Odisha. Odisha multi-sectoral nutrition action plan, 2017-20. [Google Scholar]
- 62. Lassi ZS, Das JK, Zahid G, et al. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: a systematic review. BMC Public Health 2013;13:S13 10.1186/1471-2458-13-S3-S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Prasad AS. Discovery of human zinc deficiency and studies in an experimental human model. Am J Clin Nutr 1991;53:403–12. 10.1093/ajcn/53.2.403 [DOI] [PubMed] [Google Scholar]
- 64. Imdad A, Bhutta ZA. Effect of preventive zinc supplementation on linear growth in children under 5 years of age in developing countries: a meta-analysis of studies for input to the lives saved tool. BMC Public Health 2011;11 Suppl 3:S22 10.1186/1471-2458-11-S3-S22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Brown KH, Peerson JM, Rivera J, et al. Effect of supplemental zinc on the growth and serum zinc concentrations of prepubertal children: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2002;75:1062–71. 10.1093/ajcn/75.6.1062 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-028681supp001.pdf (517KB, pdf)