Abstract
Background: Pain is a marker of bodily status, that despite being aversive under most conditions, may also be perceived as a positive experience. However, how bodily states represent, define, and interpret pain signals, and how these processes might be reflected in common language, remains unclear.
Methods: Qualitative and quantitative methods were used to explore the relationship between bodily awareness, pain reactions, and descriptions. A list of pain-related terms was generated from open-ended interviews with persons with spinal cord injury (SCI), and 138 participants (persons with SCI, health professionals, and a healthy control group) rated each descriptor as representative of pain on a gradated scale. A lexical decision task was used to test the strength of the automatic association of the word “pain” with positive and negative concepts. The behavioral results were related to body awareness, experience of pain, and exposure to pain, by comparing the three groups.
Results: Higher positive and lower negative pain descriptors, as well as slower response times when categorizing pain as an unpleasant experience were found in the SCI group. The effect was not modulated by either the time since the injury or the present pain intensity, but it was linked to the level of subjective bodily awareness. Compared with the SCI group, health experts and non-experts both associated more quickly the word “pain” and unpleasant in the lexical decision task. However, while health professionals attributed positive linguistic qualities to pain, pain was exclusively associated with negative descriptors in healthy controls group.
Conclusions: These findings are discussed in terms of their theoretical and clinical implications. An awareness of bodily signals prominently affects both the sensory and linguistic responses in persons with SCI. Pain should be evaluated more broadly to understand and, by extension, to manage, experiences beyond its adverse side.
Keywords: spinal cord injury, chronic pain, lexical pain descriptors, positive representations of pain
Introduction
Pain is one of the most common and constant symptoms following spinal cord injury (SCI). Over a third of persons experience severe and disabling pain, which often becomes chronic.1–7 Persons with SCI might feel the effects of their pain mentally,8 emotionally,9 or socially,10 with a devastating impact on quality of life.11 The International Spinal Cord Injury Pain Classification indicates several distinct types of pain: neuropathic, nociceptive, other, and unknown pain.12 Often, such pain—especially if chronic––is associated with changes in the bodily self.13–15 Neuropathic pain is most frequently reported and is defined as “pain caused by a lesion of the somatosensory nervous system,”16 with rates reported between 65% and 96%.1 This sort of pain is reported “at level” of the lesion, where there is normal sensation, as well as “below level” of the injury in areas that are insensible and immobile. Nociceptive pain refers to pain that is commonly musculoskeletal and/or visceral and is the result of physical damage, or potential damage, to the body. This type of pain is located in areas where the person has at least some preserved sensation. Despite knowledge of the pathophysiologic changes that occur after SCI, the mechanisms that produce chronic pain are not completely understood.17,18
Although pain is considered essentially private19 and is often difficult to verbalize,20 it is usually described, following SCI, with negative terms: sharp, stabbing, burning, or dull. However, these terms barely touch on the manifold facets of chronic pain experienced after SCI. Despite its unpleasantness, persons also report pain to be important in re-establishing a connection with their affected body parts and restoring their sense of bodily self: “My physical pain is in my hands and down in the legs and feet. I cannot do anything to get a connection with my body. If I pinch my leg, it is numb, so having the pain puts me in touch with my body. The pain is the connection—my friend, the pain.”21 This quote from a person with SCI suggests that pain is intrinsically linked to the body and can also be perceived as a positive experience that is even reflected in the language.22
Pain is therefore a complex, subjective, and multifaceted experience that depends on a mutual interaction of sensory input and cognitive processes. Alterations in bodily states might modulate pain perception, and suffering from chronic pain might alter a broad range of cognitive processes and behaviors23–25 that are highly dependent on communication. Despite the fact that pain is typically a marker of a negative body state, positive aspects of pain can be associated with increased body awareness and facilitation of cognitive control.26,27 Overriding such compelling stimuli with cognitive strategies could therefore be effective in reducing pain.28
The aim of the present study was to investigate the language used by persons with SCI to describe the bodily pain. The terms commonly used in pain questionnaires29–31 are the same terms that persons with but also without SCI use to describe the pain. A limited pool of terms is commonly used when describing pain, and many pain-related words remain unknown to people with SCI. Therefore, the applicability of these terms for pain questionnaires in SCI remains controversial.32 Studying individuals with SCI would potentially enhance the understanding of the interplay of bodily self and one’s sensory experiences, as well as describe the linguistic and cognitive aspects of pain. Improving health professionals’ ability to interpret a patient’s description of pain would impact on pain-related assessment and treatment.
Three groups of people with different levels of exposure to and experiences of bodily pain were used to compare descriptions of pain: people with SCI, who experience chronic pain of varying intensities, qualities, and constancies; health professionals with specific knowledge of and experience in treating pain in persons with SCI; and healthy individuals who have no specific knowledge of pain beyond their typical experience. Since pain is generally considered to indicate a negative state of a person’s body, it was expected that individuals with SCI would express more hostility directed toward pain when compared to healthy subjects. However, it was also expected that individuals with SCI would use broader descriptors and the association of pain words with negative concepts would be weaker due to their altered body representation. Development of a clearly defined, broader range of pain descriptors could facilitate communication between patients and professionals, as well as expand patients’ interpretations of the meaning of pain.
Methods
To examine the relationship between body, pain, and language, we conducted a study collecting qualitative (Phase I), subjective (Phase II), and objective (Phase III) data. In Phase I, we gathered qualitative data to identify potential negative and neutral-positive verbal descriptors of pain from open-ended interviews in people with SCI. Then, in Phase II, these selected descriptors were rated subjectively by three groups with different levels of exposure to pain and experiences of their body in pain. In the third phase, using a quantitative objective measure, we tested the strength of the automatic associations of the word “pain” as positive or negative for the three different groups.
Phase I: the opposing dimensions of pain descriptors
The pain descriptors used in this study were generated by the analysis of transcripts of open clinical interviews (prior, unpublished results) with 17 persons with SCI experiencing chronic pain who reported feelings related to bodily pain. The persons with SCI were asked about their interactions and challenges concerning bodily pain, the role it plays in their lives and daily experiences (if any), and what aspects of their lives it has changed, or is in the process of changing. Since these open interviews featured spontaneous and natural language, they provided greater ecological validity than studies using sample terms that were previously selected from a pool of canonical descriptors.29–31 The use of stimuli to activate participants’ personal pain schemata is considered essential to effectively measure and manipulate pain processing.33 Although the majority of terms described the negative aspects of pain, some reported positive experience about their pain. Through an analysis of the interview transcripts, a pool of words was generated, thus covering a broad range of gradated positive and negative dimensions of the phenomenological spectrum of bodily pain. The descriptors with a negative valence regarding physical pain (eg, hurting, damaging, burning, crushing, stabbing, lancinating, or vicious sensations), there is an obvious link between the psychological experience of pain (ie, compressive, afflicting, distressing, exhausting, intolerable, oppressive, annoying, and unpleasant) and an awareness of the resulting restrictions when performing daily activities (ie, disadvantage, obstacle, impediment, and barrier). The descriptors tend to have a neutral-positive valence treat pain as an important aspect of being alive or as an indicator of sensation or damage to spatial and bodily awareness. Physical wellness (eg, health, well-being, good, fine) and awareness of pain as a crucial element of a complete body (eg, integrity, intact, whole, undamaged) are viewed as necessary (eg, essential, indispensable, fundamental, and crucial). Through an analysis of a collection of words and their synonyms, a pool of terms were selected and organized around the “reference” descriptors, thus covering a broad range of gradated positive and negative dimensions of the phenomenological spectrum of bodily pain. Terms (translated from Italian) that tend to be representative of an implicit negative (suffering and discomfort, hurt and damage, disadvantage and restriction) and positive (essential and useful, well-being and health, integrity and completeness) valence of the bodily pain experience were used as stimulus words in the subsequent phase.
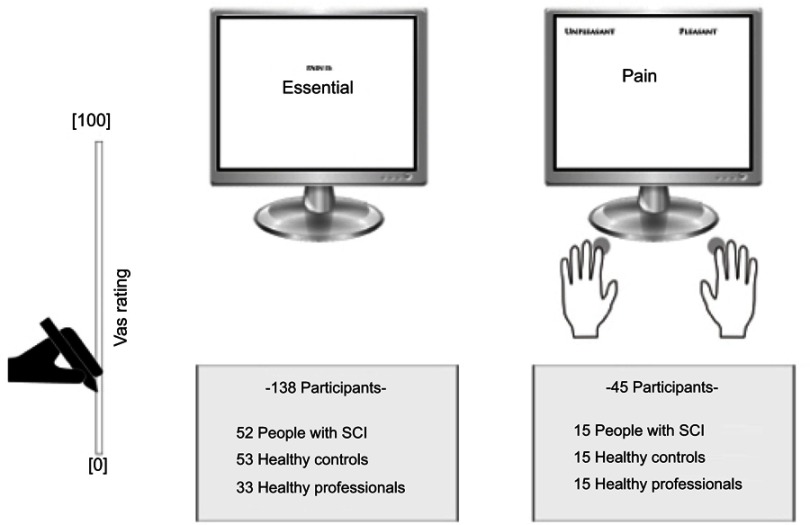
A schematic representation of the stimuli and procedures is displayed on the left side of Figure 1.
Figure 1.
Schematic representation of the stimuli and procedure. Phase II (left side): a series of randomly presented positive and negative labels were numerically rated from 0 (not at all) to 100 (completely) on a visual analog scale (left panel). Phase III (right side): a series of words randomly coupled with the words “pleasant” and “unpleasant” were used in a lexical decision task (right panel). The number of three groups of participants engaged in the two procedures is reported.
Abbreviation: SCI, spinal cord injury.
Phase II: subjective rating of pain descriptors
Participants
A total of 138 participants took part in this study. Specifically, we recruited 52 persons with diagnosed SCI (5 women; mean [±SD] age: 37.8 years ±11.1; range: 19–64 years), 33 physical therapists working with people with SCI (19 women; mean age: 40 years ±10.7; range: 22–64 years), and 53 healthy controls (19 women; mean age: 40.2 years ±9.6; range: 20–63 years).
All persons with SCI were in the chronic injury phase (at least 6 months post-injury) and had lesions ranging from C4 to L1. Their neurological injury level was determined using the International Standards for Neurological Classification of SCI.34 The diversity of pain localization was broad, ranging from chronic pain in specific body part to pain in the entire body. Their subjective ratings of the pain in terms of “intensity” and “unpleasantness” were determined using a numeric rating scale ranging from 0 (no pain/not at all unpleasant) to 10 (worst pain imaginable/most unpleasant imaginable).35 The demographic and clinical data are summarized in Table 1.
Table 1.
The clinical and demographic characteristics of people with SCI
| Case | Time since injury (days) | NLI | ASIA IS grade | Pain intensity | Pain unpleasantness |
|---|---|---|---|---|---|
| P1 | 1,440 | T9 | A | 5.5 | 6.6 |
| P2 | 1,650 | T3 | A | 7.5 | 10 |
| P3 | 700 | T12 | A | 5 | 6 |
| P4 | 1,650 | T9 | A | 2 | 0 |
| P5 | 2,537 | T12 | A | 7 | 6 |
| P6 | 1,070 | T10 | A | 10 | 10 |
| P7 | 10,700 | T4 | A | 6.5 | 6.5 |
| P8 | 6,520 | T5 | A | 5.5 | 8 |
| P9 | 1,270 | T10 | A | 6 | 6 |
| P10 | 4,330 | T5 | A | 5 | 0 |
| P11 | 1,885 | T4 | A | 7 | 8 |
| P12 | 7,250 | T7 | A | 3 | 0 |
| P13 | 6,320 | T8 | A | 4 | 0 |
| P14 | 1,580 | T4 | A | 4 | 4 |
| P15 | 4,860 | T9 | A | 4 | 6 |
| P16 | 970 | T8 | A | 5 | 5 |
| P17 | 390 | T7 | A | 6 | 5 |
| P18 | 9,425 | T7 | A | 7 | 8 |
| P19 | 845 | T12 | D | 7.5 | 9 |
| P20 | 750 | T12 | A | 0 | 0 |
| P21 | 1,335 | T7 | A | 5 | 6 |
| P22 | 2,580 | T4 | A | 10 | 10 |
| P23 | 2,520 | T3 | A | 6 | 8 |
| P24 | 2,670 | L1 | A | 6 | 8 |
| P25 | 4,495 | T11 | A | 10 | 8.5 |
| P26 | 790 | T12 | B | 4 | 8 |
| P27 | 930 | T7 | A | 8 | 7 |
| P28 | 570 | T4 | A | 0 | 0 |
| P29 | 1,335 | T10 | A | 0 | 0 |
| P30 | 2,305 | T8 | A | 2 | 8 |
| P31 | 2,920 | T3 | A | 9 | 10 |
| P32 | 1,730 | T5 | A | 10 | 10 |
| P33 | 2,155 | T3 | B | 8 | 8 |
| P34 | 3,495 | L2 | B | 7.5 | 7.5 |
| P35 | 575 | T11 | B | 4 | 5 |
| P36 | 9,125 | T10 | B | 7 | 5 |
| P37 | 1,490 | C7 | A | 2 | 2 |
| P38 | 1,185 | C6 | A | 4 | 3 |
| P39 | 1,975 | C7 | B | 7 | 10 |
| P40 | 2,920 | C4 | B | 0 | 0 |
| P41 | 5,475 | T8 | A | 7 | 5 |
| P42 | 4,380 | C7 | A | 8 | 10 |
| P43 | 2,190 | C6 | B | 7 | 8 |
| P44 | 9,490 | C6 | A | 5 | 10 |
| P45 | 6,205 | C6 | A | 5 | 10 |
| P46 | 9,125 | C6 | B | 0 | 0 |
| P47 | 4,380 | C5 | A | 0 | 0 |
| P48 | 2,190 | C6 | B | 8 | 8 |
| P49 | 1,095 | C6 | B | 8 | 10 |
| P50 | 14,235 | C6 | B | 0 | 0 |
| P51 | 1,825 | C7 | B | 8 | 10 |
| P52 | 13,870 | C7 | A | 7 | 4 |
| Mean | 3,610 | 5.4 | 5.8 |
Notes: The neurological levels of lesions and injury, as determined by ISNCSCI are indicated. In bold, the subsample (Nos. 1–15) of participants who took part in the lexical decision task (Phase III).
Abbreviations: ISNCSCI, International Standards for Neurological Classification of SCI; SCI, spinal cord injury; NLI, neurological level of injury; ASIA, American Spinal Injury Association; IS, impairment scale.
All the therapists were employed full time and had, on average, 5 years of experience (range: 1–20 years) in treating individuals with SCI.
No participant had a history of psychiatric disorders or substance abuse. The study was performed in accordance with the relevant guidelines and regulations of the 1964 Declaration of Helsinki and the ethics committee of the Istituto di Ricovero e Cura a Carattere Scientifico Fondazione Santa Lucia in Rome approved all procedures. Written informed consent was obtained from all participants.
Materials and procedure
Each participant was presented with each selected descriptor related to a specific aspect of pain. The descriptors were presented serially and in a random order across participants to remove any possible effects of the presentation order. The participants were instructed to numerically rate each descriptor in terms of how well it captured their experience of pain using a continuous vertical 100-cm VAS that ranged from 0 (not at all) to 100 (completely).
Phase III: Objective measures of the word “pain”
Lexical reaction time (RT) for the word “pain”
Data generated in Phase II can be considered as only subjective and should be associated to other more objective measures of the word “pain” to generate conclusive results. To obtain a complete picture of the nature of pain and language in persons with SCI, we analyzed accuracy and RTs using an implicit association test (IAT) when presenting the word “pain”, and other control words. A subsample of volunteers from Phase II participated in Phase III.
Participants
A subsample of the right-handed participants36 in the sample of Phase II performed the IAT:37 15 individuals with SCI (12 men; mean age: 37.8 years; range: 19–56 years) and an equivalent number of age- and gender-matched individuals from the two other groups: 15 able-bodied physical therapists who worked with people with SCI (11 men; mean age: 37.8 years; range: 25–58 years) and 15 healthy controls (11 men; mean age: 37.3 years; range: 23–50 years).
According to ASIA’s International Standards for Neurologic Classification of Spinal Cord Injury, people with SCI had complete thoracic lesions ranging from T3 to T12 and were in the chronic stage of injury (which varied between 700 and 10,700 days). All the individuals with SCI had impaired tactile sensitivity and experienced chronic pain at or below the level of injury, as defined by a prior clinical assessment.
All the therapists were employed full time and had, on average, five years of experience (range: 1–20 years) in treating individuals with SCI and some form of pain.
Materials and procedure
The performance on the lexical decision-making task was measured by analysis of the previous study’s findings regarding RT and accuracy using an IAT.37 Generally, in IAT blocks, stimulus items can be presented as pictures (block 1), words (block 2), or a combination of pictures and words (blocks 3 and 4). In block 2, single words (without pictures) were presented to participants on the screen for the first time. Participants were required to categorize each word as “pleasant” or “unpleasant.”
Block 2 comprised 10 negative words (eg, pain, agony, evil, failure) and 10 positive words (eg, glory, happiness, wonderful). Participants were tasked with classifying each word as quickly and accurately as possible by pressing either the left or right key on a keyboard. The words were presented in the center of a 17-inch monitor (resolution: 1,024×768 pixels; refresh frequency: 60 Hz) on a gray background and subtended to a 10.6”×10.6” square region around the fovea. The category cues (pleasant and unpleasant) were presented in the top left/right corner of the screen. Answers were given pressing the appropriate left-hand (Q) or right-hand (P) key, which was not a problem in people with thoracic lesions that caused paralysis of the lower limbs while sparing upper limbs function. Presentation of the stimuli and registration of the answers were controlled using E-Prime software (Psychology Software Tools, Inc., Sharpsburg, PA, USA). The order in which the words were presented was randomized. Each word was presented four times in total, twice for each of the two different versions of block 2 of the IAT. Based on our study objectives, we analyzed the RTs related to the word “pain” and two control words (agony=agonia, glory=gloria), which were matched in terms of length to “pain” (dolore) in Italian, which appeared in block 2 of the IAT. One control word had a positive valence (glory=gloria), and the other had a negative valence (agony=agonia).38 A schematic representation of the stimuli and procedures is displayed on the right side of Figure 1.
Sensitivity to pain and body awareness
To assess pain sensation and body awareness, all the persons with SCI were asked to rate the intensity of perceived pain and their ability to identify sensations arising from affected body parts on a VAS compared to their normal facial sensation. With respect to perceived pain, the lower and upper extremes of the VAS scale were identified by “no pain” and “the worst possible pain,” respectively. For perceived body sensations, the lower and upper extremes were identified by “I cannot perceive” and “I have complete sensation, as on the face.”
Other measures
To assess the acceptance of pain and coping, we employed: 1) a 20-item chronic pain acceptance questionnaire (CPAQ-R)39 which showed satisfactory statistics of internal consistency (Cronbach’s alpha >0.80);40 and 2) a 27-item measure of strategies for coping with pain (CSQ-R)41 which showed excellent internal consistency (Cronbach’s alpha >0.90) and good intraclass correlation coefficients (>0.80).41 We also tested the degree of mood disturbance using the Beck Depression Inventory42 which showed excellent internal consistency (Cronbach’s alpha >0.89).43
Statistical analyses
Phase II
The mean ratings of each word in the questionnaire were collapsed into a single score for the negative dimension and neutral-positive dimension. This was entered into a 2 (Descriptor)×3 (Group) mixed-measures ANOVA, with Descriptor (Neutral-Positive/Negative) as a within-subjects factor and Group (People with SCI/Physical Therapists/Healthy Controls) as a between-subjects factor.
Phase III
In line with previous studies,44–46 the individual RTs and correct answer rates during the lexical decision task were computed, from which we derived an index of inverse efficiency (IE) score (IE=[RT]/[1 - proportion of errors]). The IE score allows us to combine RTs and the correct answer rate into a single measure.47 During the IAT, the correct associations were considered to be “glory” with pleasant and “pain”/“agony” with unpleasant. In trials with the word “pain,” a higher IE score indicated less association between pain and “unpleasant.” The IE data were examined via an ANOVA with Word (pain=dolore, agony=agonia, glory=gloria) as a within-subjects factor and Group (People with SCI/Physical Therapists/Healthy Controls) as a between-subjects factor. Moreover, Spearman’s correlation coefficients were calculated between the IE data and the time since injury, subjective ratings of body awareness, and intensity of pain among people with SCI.
All pairwise comparisons were performed using the Newman–Keuls post hoc test. A significance threshold of p<0.05 was set for all statistical analyses. All data are reported as the mean±the standard error of the mean (SEM).
Results
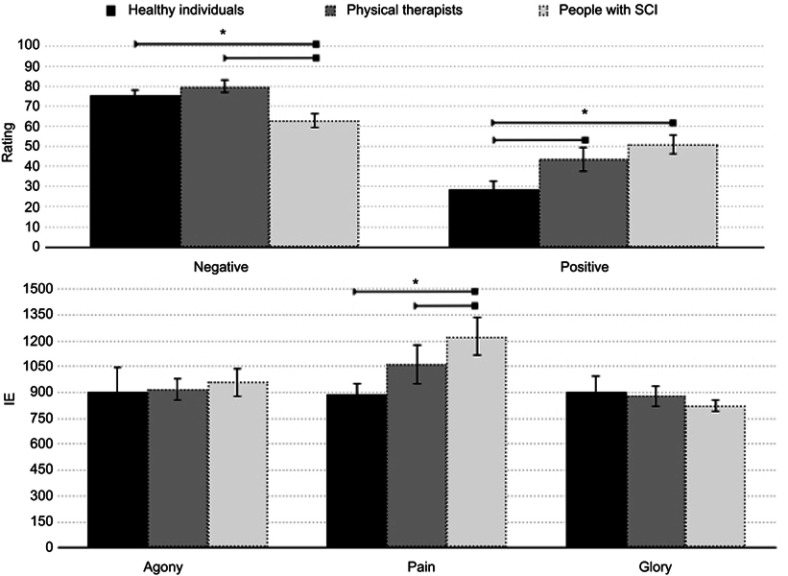
Phase II: the effect of the positive and negative dimensions on lexical pain
The mixed-model ANOVA with Descriptor (Positive/Negative)×Group (People with SCI, Physical Therapists, Healthy Controls) revealed a significant main effect of Descriptor (F(1,135)=90.52; p<0.001, η2=0.40), which was explained, unsurprisingly, by the higher ratings for Negative Descriptors (M=71.84, SEM=2.11) compared to those for Positive Descriptors (M=40.68, SEM=2.90, p<0.001). No main effect of Group was observed (F(2,135)=2.13; p=0.13, η2=0.03). Importantly, we did observe a significant interaction between Descriptor and Group (F(2,135)=11.33; p<0.001, η2=0.14). The Newman–Keuls post hoc test revealed that People with SCI had a significantly lower rating for Negative Descriptors (M=62.98, SEM=3.82) compared to both Physical Therapists (M=79.96, SEM=3.29, p=0.01) and Healthy Controls (M=75.47, SEM=3.16, p=0.04), who did not differ in their ratings (p=0.46).
Conversely, People with SCI had significantly higher ratings for Positive Descriptors (M=51.05, SEM=4.67) compared to Healthy Controls (M=28.67, SEM=3.97, p<0.001), but not compared to Physical Therapists (M=43.63, SEM=6.46, p=0.23), who did differ from each other (p=0.01). All of the results are reported in the top panel of Figure 2.
Figure 2.
Results obtained from the three groups of participants. Phase II (top panel): the y-axis reflects the ratings of positive and negative descriptors of pain obtained from the three groups of participants (healthy controls, people with SCI, and physical therapists), which are shown on the x-axis. Higher ratings indicate a stronger association of the word “pain” with negative or positive lexical dimensions. Phase III (bottom panel): the y-axis depicts the IE score obtained from the three groups of participants, shown on the x-axis, for the words “pain,” “agony,” and “glory.” Higher IE scores indicate greater response latency and less accuracy when the word “pain” is paired with a negative trait than when the word is paired with a positive trait. The error bars in both panels indicate the SEM, and asterisks (*) indicate significant results.
Abbreviations: SCI, spinal cord injury; IE, inverse efficiency.
Phase III: effect of the word “pain” on lexical RT
The speed at which individuals categorized a word as pleasant or unpleasant is an index of the strength of the association between that word and category cue. For example, if the word “pain” was strongly associated with the “unpleasant” category, then there was less response latency and more accuracy than when the word was paired with the “pleasant” category. Participants’ performance is shown in Figure 2. High IE scores reflect slower and less accurate responses to the word “pain” paired with “unpleasant.” An ANOVA with Group (People with SCI, Physical Therapists, Healthy Controls) as the between-subjects factor and Word (Pain, Agony, Glory) as the within-subjects factor revealed a significant main effect of Word (F(2,84)=8.54; p<0.0001 np2>0.17). The Newman–Keuls post hoc test for multiple comparisons showed significant differences in IE score between the word “Pain” (1058.9) and the words “Agony” (928) and “Glory” (869) (for all, p<0.02). No main effect of Group was observed (F(2,42)=0.63; p=0.53, η2=0.02). Importantly, we observed a significant interaction between Word and Group (F(4,84)=3.5; p<0.01, η2=0.14). The Newman–Keuls post hoc test revealed that People with SCI had a significantly higher IE score for the word “Pain” (1,226) than did both Healthy Controls (887, p=0.001) and Physical Therapists (1,063, p=0.048), who slightly differed (but not significantly) from each other (p=0.079). These results indicate that people with SCI, and to some degree therapists, are generally slower and less accurate in associating the word “pain” with unpleasantness compared to healthy individuals without any specific knowledge of pain beyond occasional personal experiences. The IE scores for “Agony” (960, 919, and 907 for People with SCI, Physical Therapists, and Healthy Controls, respectively) and “Glory” (825, 878, and 905, respectively) were similar among the groups, thus ruling out the effect of unspecific performance. All the results are reported in the bottom panel of Figure 2.
Associations between perceived pain and body awareness
We observed an interesting significant inverse correlation coefficient between body sensitivity and the IE score for the word “pain.” In particular, body awareness was rated as lower among persons with a higher IE score (r=−0.63; t=−2.96; p<0.016). No correlation was found between intensity of perceived pain or body sensitivity and the other two words (for all, p>0.1). Neither time since injury, nor intensity of pain at time of testing, were observed to have an effect (for all, p>0.1). Furthermore, no significant correlation was found between IE and the acceptance of pain or strategies for coping or between IE and the degree of mood disturbance (depression) (for all, p>0.1). Therefore, our results demonstrate that only body awareness evokes pain-related linguistic differences.
Discussion
Influential theoretical models have emphasized the multidimensional nature and the positive—in addition to the more obvious negative—aspects of pain perception.26,48 However, the vast majority of empirical studies on pain still focus on its adverse consequences. In the current study, we investigated linguistic descriptions of pain and reactions to pain-related words in three groups with different experiences of body alterations and chronic pain sensations: individuals with SCI, health professionals who work with spinal cord injuries, and a healthy control group. The subjective and objective data revealed three main findings:
The selection of pain descriptors showed that, in all three groups, the negative terms were judged to better fit the description of pain than the positive ones.
Compared to the control group, the group of persons with SCI provided more positive, and less negative, verbal descriptions of pain. Similarly, the persons with SCI demonstrated longer response times when categorizing pain as unpleasant in the lexical decision task. An effect of the level of body awareness was also found.
Health professionals, who observe patients’ pain on a daily basis, also provided more positive pain descriptors, though the RTs in the lexical decision task were similar to the control group.
Positive lexical pain descriptors in individuals with SCI
Individuals with SCI judged positive terms as also being representative of their pain experience, when compared to the control group. This suggests that a complete loss of somatosensory and motor processes for body parts below the level of the lesion might weaken the genuine association of pain as a negative experience, despite the often devastating effects.49 Importantly, these findings were mirrored by their behavior in a lexical decision task: individuals with SCI took longer to categorize the word “pain” as an unpleasant word. This effect was specific for the word “pain” and did not hold for other negative words, such as “agony,” thus ruling out non-specific effects unrelated to pain responses, such as reduced attention or generally slowed RTs.
With the aim of understanding what mechanisms underlie such an effect, we correlated the increase in RT with clinical measures, such as time since injury, chronic pain perception, and (lack of) body awareness. The only predictor of the difference in RT was body awareness, suggesting that decreased body awareness is associated with less negative evaluations of the word “pain.” A plausible interpretation for this effect is that chronic pain might help to overcome the partial disconnection from the body, which has shown to lead to disorders of the bodily self.13,14 Some individuals might prefer to experience a connection to their body over feeling nothing at all,50 even if it takes the form of pain15 (see also “Ian”—the case presented in21). The body–brain disconnection might make people more vigilant in relation to their disembodied body,51–53 thus leading people with SCI to take advantage of any residual sensation, including pain. In some instances, pain may be the only way to create body awareness and a protective body space,54 which might help to define the space in which the body is located55 a major neuroscientific constraint of body self-consciousness.56,57
An alternative explanation may be that the brain–body disconnection makes the extreme unpleasantness and intensity of acute pain, as a signal of bodily harm, more tolerable for people with SCI, even in terms of their pain-related vocabulary. Moreover, given the continuous presence of pain, constant awareness may gradually attenuate, and people with SCI may develop a more graduated, refined, and specific selection of words or pain descriptors, as well as a broader vocabulary. The participants with SCI more consciously, and more commonly, associated pain with positive words regarding the body (eg, “completeness,” “functional,” “useful”) than healthy participants. This suggests that subjective information may flow and integrate at different levels, moving from the body to the pain-processing system before being lexically elaborated in the language system. Embodied cognition accounts suggest that bodily states, and even compound aspects of language, can be “grounded” in both cognitive states and their outcomes.58
Theoretically, the different behaviors in individuals with SCI could also indicate more general coping strategies, such as viewing pain as something positive to foster acceptance of their condition.26,59 However, no significant correlation was found between the differences in RTs (IE score) and measures of mood disorder, acceptance, coping score, or daily functioning. While previous studies have found an association between the severity of pain and degree of mood disturbance and pain acceptance,60,61 these studies were conducted in the sub-acute phase and not in the chronic phase as ours was. Although more research will be needed, this suggests that the reaction to, and the interpretation of, pain might change over time in individuals with SCI.62
Positive lexical pain descriptors in health experts and non-experts
Our results showed that, for the control group of healthy non-expert participants, pain is an exclusively unpleasant experience, as evidenced both by the lack of association between “pain” and positive descriptors and by faster RTs in categorizing the word “pain” as negative. This suggests that the relative lack of pain exposure in this group precludes both an understanding of the complex effects of pain and the view of pain as potentially positive, or even healthy. This is congruent with the culturally dominant idea of pain as a malevolent attack on the body and for survival.63
However, our data show that this idea may change through learned knowledge, even without the subjective experience of pain. While the group of therapists did not have more experience with subjective perception of pain than the control group of healthy individuals, they were, due to their profession, more conscious of the potential positive effects of pain. Implicitly, the group of therapists did not show any difference in the response time for classifying “pain” words as a negative concept compared with the control group, but they did associate positive terms with pain comparably with the persons with SCI. This effect may be derived either from trained knowledge on pain mechanisms or from daily observations of pain experiences and management of persons with SCI, which in turn might enhance awareness of the positive role of pain in clinical settings.
Limitations and implications for clinical practice
The limitations of this study cannot be ignored. First, this preliminary study was conducted in the context of bodily pain and the complexity of somatic awareness in SCI. The clinical relevance to other pain conditions should be explicitly addressed.
Second, the list of descriptors was somewhat lacking in a standardized and validated approach. The word classification should be validated by psycholinguistic indexes (ie, frequency, familiarity, imageability, and context availability).
Third, this study is far from definitive, as only a limited number of possible pain descriptors were considered. Although standardized pain data sets are used to identify and treat the pain, we hope that additional positive aspects of pain, as pointed out by our study, will further enhance the comprehension of the complex experience of pain.
Overall, our results highlight the dynamic link between body representation, pain, and lexical pain descriptors. The data suggest that pain might be associated with positive, in addition to negative, concepts through alterations in body and pain perception and, to some degree, through professional training. A large natural-language sample of descriptive terms used was suggested by people with SCI who have tried to make sense of their bodily pain rather than linking it to exclusively adverse concepts. Such an open-response approach overcomes an important limitation of previous lexical studies on pain—that classically used pain-related terms are associated with negative bodily states,29-31,64 as they are when typically referred to as lexical descriptors of pain in a healthy sample. As observed, healthy participants might attribute only negative aspects to “pain” and, thus, reduce or disregard the multifaceted aspects of pain.
Our results suggest that pain, especially if used to access body awareness, might also have positive connotations. This preliminary finding has several implications for pain management, especially in the clinical context. In particular, the idea of pain as exclusively restricting one’s potential self may need to be reconceptualized65 to accommodate the ways in which pain increases sensitivity to physical experiences and heightens one’s corporeal self-awareness. Catastrophic thinking and the amplification of pain are associated with higher pain ratings of negative words in clinical assessments.66 It may be possible to alter negative and adverse verbal experiences of pain, thereby generating new lines of inquiry and novel assessment tools to explore how individuals experience pain. The new generation of practitioner–clinicians and care teams could take advantage of this approach and consider not only a broader and qualitative assessment of pain, but also specific educational sessions, in order to reduce negative bias toward pain.67 For those trying to understand and manage pain experiences, the adoption of a broader pain perspective may also lead to changes in the strategies used to choose descriptors in lexical pain questionnaires.
Acknowledgments
This work was supported by the Italian Ministry of Health (RF-2018-12365682) and Ania Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103(3):249–257. [DOI] [PubMed] [Google Scholar]
- 2.Bonica JJ. History of pain concepts and pain therapy. Mt Sinai J Med. 1991;58(3):191–202. [PubMed] [Google Scholar]
- 3.Finnerup NB. Pain in patients with spinal cord injury. Pain. 2013;154(Suppl 1):S71–S76. doi: 10.1016/j.pain.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 4.Siddall PJ, Loeser JD. Pain following spinal cord injury. Spinal Cord. 2001;39(2):63–73. [DOI] [PubMed] [Google Scholar]
- 5.Dijkers M, Bryce T, Zanca J. Prevalence of chronic pain after traumatic spinal cord injury: a systematic review. J Rehabil Res Dev. 2009;46(1):13–29. [PubMed] [Google Scholar]
- 6.Werhagen L, Budh CN, Hultling C, Molander C. Neuropathic pain after traumatic spinal cord injury–relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord. 2004;42(12):665–673. doi: 10.1038/sj.sc.3101641 [DOI] [PubMed] [Google Scholar]
- 7.Cruz-Almeida Y, Martinez-Arizala A, Widerstrom-Noga EG. Chronicity of pain associated with spinal cord injury: a longitudinal analysis. J Rehabil Res Dev. 2005;42(5):585–594. [DOI] [PubMed] [Google Scholar]
- 8.Molton IR, Stoelb BL, Jensen MP, Ehde DM, Raichle KA, Cardenas DD. Psychosocial factors and adjustment to chronic pain in spinal cord injury: replication and cross-validation. J Rehabil Res Dev. 2009;46(1):31–42. doi: 10.1682/JRRD.2008.03.0044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Summers JD, Rapoff MA, Varghese G, Porter K, Palmer RE. Psychosocial factors in chronic spinal cord injury pain. Pain. 1991;47(2):183–189. [DOI] [PubMed] [Google Scholar]
- 10.Richards JS, Meredith RL, Nepomuceno C, Fine PR, Bennett G. Psycho-social aspects of chronic pain in spinal cord injury. Pain. 1980;8(3):355–366. doi: 10.1016/0304-3959(80)90079-2 [DOI] [PubMed] [Google Scholar]
- 11.van Leeuwen CM, Post MW, van Asbeck FW, et al. Life satisfaction in people with spinal cord injury during the first five years after discharge from inpatient rehabilitation. Disabil Rehabil. 2012;34(1):76–83. doi: 10.3109/09638288.2011.587089 [DOI] [PubMed] [Google Scholar]
- 12.Bryce TN, Biering-Sorensen F, Finnerup NB, et al. International spinal cord injury pain classification: part I. Background and description. March 6–7,2009. Spinal Cord. 2012;50(6):413–417. doi: 10.1038/sc.2011.156 [DOI] [PubMed] [Google Scholar]
- 13.Lenggenhager B, Scivoletto G, Molinari M, Pazzaglia M. Restoring tactile awareness through the rubber hand illusion in cervical spinal cord injury. Neurorehabil Neural Repair. 2013;27(8):704–708. doi: 10.1177/1545968313491009 [DOI] [PubMed] [Google Scholar]
- 14.Lenggenhager B, Pazzaglia M, Scivoletto G, Molinari M, Aglioti SM. The sense of the body in individuals with spinal cord injury. PLoS One. 2012;7(11):e50757. doi: 10.1371/journal.pone.0050757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pazzaglia M, Haggard P, Scivoletto G, Molinari M, Lenggenhager B. Pain and somatic sensation are transiently normalized by illusory body ownership in a patient with spinal cord injury. Restor Neurol Neurosci. 2016;34(4):603–613. doi: 10.3233/RNN-150611 [DOI] [PubMed] [Google Scholar]
- 16.Jensen TS, Baron R, Haanpaa M, et al. A new definition of neuropathic pain. Pain. 2011;152(10):2204–2205. doi: 10.1016/j.pain.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 17.D’Angelo R, Morreale A, Donadio V, et al. Neuropathic pain following spinal cord injury: what we know about mechanisms, assessment and management. Eur Rev Med Pharmacol Sci. 2013;17(23):3257–3261. [PubMed] [Google Scholar]
- 18.Finnerup NB, Baastrup C. Spinal cord injury pain: mechanisms and management. Curr Pain Headache Rep. 2012;16(3):207–216. doi: 10.1007/s11916-012-0259-x [DOI] [PubMed] [Google Scholar]
- 19.Wittgeinstein L. Remarks on the Philosophy of Psychology. Oxford: Blackweel; 1980. [Google Scholar]
- 20.Wagstaff S, Smith OV, Wood PH. Verbal pain descriptors used by patients with arthritis. Ann Rheum Dis. 1985;44(4):262–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cole J. Still Lives. Cambridge:: MIT press; 2004. [Google Scholar]
- 22.Biro D. The Language of Pain: Finding Words, Compassion and Relief. New York:: WW Norton & Company; 2010. [Google Scholar]
- 23.Baliki MN, Chialvo DR, Geha PY, et al. Chronic pain and the emotional brain: specific brain activity associated with spontaneous fluctuations of intensity of chronic back pain. J Neurosci. 2006;26(47):12165–12173. doi: 10.1523/JNEUROSCI.3576-06.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dworkin RH. An overview of neuropathic pain: syndromes, symptoms, signs, and several mechanisms. Clin J Pain. 2002;18(6):343–349. [DOI] [PubMed] [Google Scholar]
- 25.Pazzaglia M. Body and odors: not just molecules, after all. Curr Dir Psychol Sci. 2015;24(4):329–333. doi: 10.1177/0963721415575329 [DOI] [Google Scholar]
- 26.Bastian B, Jetten J, Hornsey MJ, Leknes S. The positive consequences of pain: a biopsychosocial approach. Pers Soci Psychol Rev. 2014;18(3):256–279. doi: 10.1177/1088868314527831 [DOI] [PubMed] [Google Scholar]
- 27.Pazzaglia M, Galli G, Lewis JW, Scivoletto G, Giannini AM, Molinari M. Embodying functionally relevant action sounds in patients with spinal cord injury. Sci Rep. 2018;8(1):15641. doi: 10.1038/s41598-018-34133-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weisenberg M. Cognitive aspects of pain and pain control. Int J Clin Exp Hypn. 1998;46(1):44–61. doi: 10.1080/00207149808409989 [DOI] [PubMed] [Google Scholar]
- 29.Fernandez E, Towery S. A parsimonious set of verbal descriptors of pain sensation derived from the McGill Pain Questionnaire. Pain. 1996;66(1):31–37. [DOI] [PubMed] [Google Scholar]
- 30.Fernandez E, Krusz JC, Hall S. Parsimonious collection of pain descriptors: classification and calibration by pain patients. J Pain. 2011;12(4):444–450. doi: 10.1016/j.jpain.2010.10.011 [DOI] [PubMed] [Google Scholar]
- 31.Fernandez E, Vargas R, Mahometa M, Ramamurthy S, Boyle GJ. Descriptors of pain sensation: a dual hierarchical model of latent structure. J Pain. 2012;13(6):532–536. doi: 10.1016/j.jpain.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 32.Siddall PJ. Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord. 2009;47(5):352–359. doi: 10.1038/sc.2008.136 [DOI] [PubMed] [Google Scholar]
- 33.Crombez G, Van Ryckeghem DM, Eccleston C, Van Damme S. Attentional bias to pain-related information: a meta-analysis. Pain. 2013;154(4):497–510. doi: 10.1016/j.pain.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 34.Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–S56. doi: 10.1080/10790268.2003.11754575 [DOI] [PubMed] [Google Scholar]
- 35.Galer BS, Jensen MP. Development and preliminary validation of a pain measure specific to neuropathic pain: the Neuropathic Pain Scale. Neurology. 1997;48(2):332–338. [DOI] [PubMed] [Google Scholar]
- 36.Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9(1):97–113. [DOI] [PubMed] [Google Scholar]
- 37.Galli G, Lenggenhager B, Scivoletto G, Molinari M, Pazzaglia M. Don‘t look at my wheelchair! The plasticity of longlasting prejudice. Med Educ. 2015;49(12):1239–1247. doi: 10.1111/medu.12834 [DOI] [PubMed] [Google Scholar]
- 38.Montefinese M, Ambrosini E, Fairfield B, Mammarella N. The adaptation of the Affective Norms for English Words (ANEW) for Italian. Behav Res Methods. 2014;46(3):887–903. doi: 10.3758/s13428-013-0405-3 [DOI] [PubMed] [Google Scholar]
- 39.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107(1–2):159–166. [DOI] [PubMed] [Google Scholar]
- 40.Bernini O, Pennato T, Cosci F, Berrocal C. The psychometric properties of the chronic pain acceptance questionnaire in Italian patients with chronic pain. J Health Psychol. 2010;15(8):1236–1245. doi: 10.1177/1359105310365576 [DOI] [PubMed] [Google Scholar]
- 41.Monticone M, Ferrante S, Giorgi I, Galandra C, Rocca B, Foti C. The 27-item coping strategies questionnaire-revised: confirmatory factor analysis, reliability and validity in Italian-speaking subjects with chronic pain. Pain Res Manag. 2014;19(3):153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. [DOI] [PubMed] [Google Scholar]
- 43.Sacco R, Santangelo G, Stamenova S, et al. Psychometric properties and validity of Beck Depression Inventory II in multiple sclerosis. Eur J Neurol. 2016;23(4):744–750. doi: 10.1111/ene.12932 [DOI] [PubMed] [Google Scholar]
- 44.Kitagawa N, Spence C. Investigating the effect of a transparent barrier on the crossmodal congruency effect. Exp Brain Res. 2005;161(1):62–71. doi: 10.1007/s00221-004-2046-3 [DOI] [PubMed] [Google Scholar]
- 45.Murphy FC, Klein RM. The effects of nicotine on spatial and non-spatial expectancies in a covert orienting task. Neuropsychologia. 1998;36(11):1103–1114. [DOI] [PubMed] [Google Scholar]
- 46.Kennett S, Eimer M, Spence C, Driver J. Tactile-visual links in exogenous spatial attention under different postures: convergent evidence from psychophysics and ERPs. J Cogn Neurosci. 2001;13(4):462–478. [DOI] [PubMed] [Google Scholar]
- 47.Townsend JT, Ashby FG. Stochastic Modeling of Elementary Psychological Processes. Cambridge: Cambridge University Press; 1983. [Google Scholar]
- 48.Borelli E, Crepaldi D, Porro CA, Cacciari C. The psycholinguistic and affective structure of words conveying pain. PLoS One. 2018;13(6):e0199658. doi: 10.1371/journal.pone.0199658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saulino M, Averna JF. Evaluation and management of SCI-associated pain. Curr Pain Headache Rep. 2016;20(9):53. doi: 10.1007/s11916-016-0587-3 [DOI] [PubMed] [Google Scholar]
- 50.Bruehlmeier M, Dietz V, Leenders KL, Roelcke U, Missimer J, Curt A. How does the human brain deal with a spinal cord injury? Eur J Neurosci. 1998;10(12):3918–3922. doi: 10.1046/j.1460-9568.1998.00454.x [DOI] [PubMed] [Google Scholar]
- 51.Cole J. Perspectives on embodiment and prosthetic incorporation in those with spinal cord injury: comment on “The embodiment of assistive devices-from wheelchair to exoskeleton” by M. Pazzaglia and M. Molinari. Phys Life Rev. 2016;16:176–177. doi: 10.1016/j.plrev.2016.01.018 [DOI] [PubMed] [Google Scholar]
- 52.Zantedeschi M, Pazzaglia M. Commentary: non-invasive brain stimulation, a tool to revert maladaptive plasticity in neuropathic pain. Front Hum Neurosci. 2016;10:544. doi: 10.3389/fnhum.2016.00544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pazzaglia M, Zantedeschi M. Plasticity and Awareness of Bodily Distortion. Neural Plast. 2016;2016:9834340. doi: 10.1155/2016/5260671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aldrich S, Eccleston C. Making sense of everyday pain. Soc Sci Med. 2000;50(11):1631–1641. [DOI] [PubMed] [Google Scholar]
- 55.Moseley GL, Gallace A, Spence C. Bodily illusions in health and disease: physiological and clinical perspectives and the concept of a cortical ‘body matrix‘. Neurosci Biobehav Rev. 2012;36(1):34–46. doi: 10.1016/j.neubiorev.2011.03.013 [DOI] [PubMed] [Google Scholar]
- 56.Blanke O, Metzinger T. Full-body illusions and minimal phenomenal selfhood. Trends Cogn Sci. 2009;13(1):7–13. doi: 10.1016/j.tics.2008.10.003 [DOI] [PubMed] [Google Scholar]
- 57.Pazzaglia M, Scivoletto G, Giannini AM, Leemhuis E. My hand in my ear: a phantom limb re-induced by the illusion of body ownership in a patient with a brachial plexus lesion. Psychol Res. 2018;83:196–204. [DOI] [PubMed] [Google Scholar]
- 58.Barsalou LW. Grounded cognition. Annu Rev Psychol. 2008;59:617–645. doi: 10.1146/annurev.psych.59.103006.093639 [DOI] [PubMed] [Google Scholar]
- 59.Harris MH. Pain barriers revisited: ten myths and misconceptions about pain management. S D J Med. 2003;56(7):257–258. [PubMed] [Google Scholar]
- 60.Nicholson Perry K, Nicholas MK, Middleton J. Spinal cord injury-related pain in rehabilitation: a cross-sectional study of relationships with cognitions, mood and physical function. Eur J Pain. 2009;13(5):511–517. doi: 10.1016/j.ejpain.2008.06.003 [DOI] [PubMed] [Google Scholar]
- 61.Craig A, Tran Y, Siddall P, et al. Developing a model of associations between chronic pain, depressive mood, chronic fatigue, and self-efficacy in people with spinal cord injury. J Pain. 2013;14(9):911–920. doi: 10.1016/j.jpain.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 62.Taylor J, Huelbes S, Albu S, Gomez-Soriano J, Penacoba C, Poole HM. Neuropathic pain intensity, unpleasantness, coping strategies, and psychosocial factors after spinal cord injury: an exploratory longitudinal study during the first year. Pain Med. 2012;13(11):1457–1468. doi: 10.1111/j.1526-4637.2012.01483.x [DOI] [PubMed] [Google Scholar]
- 63.Kern E. Cultural-historical aspects of pain. Acta Neurochir (Wien). 1987;38:165–181. [DOI] [PubMed] [Google Scholar]
- 64.Pazzaglia M, Leemhuis E, Giannini AM, Haggard P. The homuncular jigsaw: investigations of phantom limb and body awareness following brachial plexus block or avulsion. J Clin Med. 2018;8:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Galli G, Pazzaglia M. Commentary on: “The body social: an enactive approach to the self“. A tool for merging bodily and social self in immobile individuals. Front Psychol. 2015;6:305. doi: 10.3389/fpsyg.2015.00305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hearn JH, Finlay KA, Fine PA. The devil in the corner: a mixed-methods study of metaphor use by those with spinal cord injury-specific neuropathic pain. Br J Health Psychol. 2016;21(4):973–988. doi: 10.1111/bjhp.12211 [DOI] [PubMed] [Google Scholar]
- 67.Galli G, Pazzaglia M. Novel perspectives on health professionals‘ attitudes to disability. Med Educ. 2016;50(8):804–806. doi: 10.1111/medu.13111 [DOI] [PubMed] [Google Scholar]