Abstract
Background: Pain is one of the most common symptoms experienced by patients with end-stage renal disease. Although NSAIDs may lead to adverse events, NSAID use appears to be considerably high in patients with end-stage renal disease. However, whether NSAID use is associated with an increased risk of mortality in this population remains unknown.
Aim: This study aimed to investigate the association between the use of NSAIDs and the risk of mortality in patients with end-stage renal disease.
Patients and methods: We used the population-based Taiwan National Health Insurance Research Database to investigate the association between the use of NSAIDs and the risk of mortality in patients with end-stage renal disease receiving dialysis. A total of 3,383 patients with newly diagnosed end-stage renal disease requiring long-term dialysis between 1998 and 2012 were included in the current study, and the study outcome was evaluated until December 31, 2013. Time-dependent Cox regression models were applied to examine the association between NSAID use and mortality risk.
Results: In the study cohort, 2,623 (78%) patients used NSAIDs during the follow-up period. The median follow-up period was 4.0 years, during which 1,515 patients died. The results of multivariable analysis demonstrated that compared with NSAID nonuse, the use of any NSAIDs, nonselective NSAIDs, and selective cyclooxygenase-2 inhibitors was associated with a significantly increased risk of all-cause mortality with an adjusted HR (95% CI) of 1.39 (1.21–1.60), 1.36 (1.19–1.55), and 1.61 (1.42–1.83), respectively.
Conclusion: The results suggest that NSAID use was associated with an increased risk of mortality in the patients with end-stage renal disease. Future randomized controlled trials are needed to validate these observational findings.
Keywords: end-stage renal disease, NSAIDs, mortality
Introduction
The prevalence and incidence of end-stage renal disease have been rapidly increasing worldwide. The number of patients with end-stage renal disease receiving renal replacement therapy was estimated to be 2.6 million in 2010, and it is expected to rise to 5.4 million by 2030.1 Patients with end-stage renal disease experience multiple symptoms, of which pain is one of the most common symptoms.2 Studies have reported that pain affected >50% of patients with end-stage renal disease and that a large number of patients were not being effectively treated.3,4
Pain may result in some deteriorative consequences in patients with end-stage renal disease including anxiety, depression, sleep disturbance, decreased physical activity, likeliness of withdrawal from dialysis, and cardiovascular complications.5 To relieve pain and improve the quality of life, analgesic therapy is commonly used in patients with end-stage renal disease.6 However, various conditions may cause pain in these patients including musculoskeletal disease, peripheral neuropathy, peripheral vascular disease, chronic infections, kidney disorders, and dialysis procedure.3,5 In addition, patients with end-stage renal disease can have complex medication regimens that may lead to medication-related problems.7 The aforementioned reasons can cause difficulties in pain management. When selecting pain medications, the type and severity of pain, potential side effects, alterations in pharmacokinetics, comorbid disease states, and drug–drug interactions should be considered.8
The WHO analgesic ladder is a generally accepted guideline for pain management.9 According to WHO’s pain relief recommendations, NSAIDs are first-line analgesics for relieving mild to moderate pain. However, the available data suggest that NSAIDs should be used with caution in patients with end-stage renal disease because they are associated with increased risks of cardiovascular complications, gastrointestinal bleeding, and compromise of renal function.5,6,10 Although NSAIDs may lead to adverse events, the use of NSAIDs appears to be inappropriately high in patients with end-stage renal disease despite recommendations against their use.11–13 This may partly be due to the lack of clinicians’ and patients’ awareness regarding the possible adverse effects of NSAIDs in patients with end-stage renal disease.14
Although there is a general consensus that the use of NSAIDs should be avoided in patients with end-stage renal disease, limited evidence is available regarding adverse clinical outcomes associated with NSAID use in this population.14,15 The present study investigated the association between the use of NSAIDs and the risk of mortality in patients with end-stage renal disease receiving dialysis by using the population-based Taiwan National Health Insurance Research Database.
Material and methods
Data source
The Taiwan National Health Insurance Research Database was used as the data source in the present study. Taiwan’s National Health Insurance is a compulsory and single-payer program that provides health-care coverage to nearly all 23 million residents of Taiwan.16,17 This program enables the public to receive comprehensive medical care including inpatient and outpatient care, dental care, and prescription drugs. The Taiwan National Health Insurance Research Database contains encrypted registration files and original claims data of beneficiaries enrolled in the National Health Insurance program. The Taiwan National Health Insurance Research Database is maintained by the National Health Research Institutes and provided to scientists for research purposes. In this study, we analyzed the medical records of 1 million representative individuals randomly selected from 23 million beneficiaries in the Taiwan National Health Insurance Research Database between 1997 and 2013. This study was approved by the Joint Institutional Review Board of Taipei Medical University, and the requirement of patient-informed consent was waived (TMU-JIRB No. N201506025).
Study population
The study population consisted of patients with end-stage renal disease receiving dialysis, and these patients were identified on the basis of their catastrophic illness certificate. In Taiwan, individuals who require extended treatment because of severe and chronic diseases, such as those with end-stage renal disease requiring long-term dialysis treatment, may apply for the catastrophic illness certificate. Patients are not required to make copayments for medical services if they have catastrophic illness certificates. To receive the catastrophic illness certificate, patients must fulfill the following two requirements: (1) a diagnosis of end-stage renal disease and (2) necessity of receiving long-term dialysis treatment. Once the aforementioned conditions are confirmed by nephrologists and verified by the National Health Insurance Administration, patients can obtain the catastrophic illness certificate. Therefore, we used the catastrophic illness registration file to identify patients with end-stage renal disease who required long-term dialysis therapy. The present study comprised patients aged ≥20 years who had catastrophic illness certificates with the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code of 585.x between 1998 and 2012.
The baseline demographics of the study population were obtained from the registry for beneficiaries. The age of patients was determined at the beginning of dialysis treatment. Baseline comorbidities were determined using the Charlson Comorbidity Index according to the medical records 1 year before the beginning of dialysis treatment.18,19
Study outcome
The study outcome was all-cause mortality during the follow-up period. The date of death was determined according to records in the Registry of Catastrophic Illness Database of the Taiwan National Health Insurance Research Database. The observation period began from when patients started to receive dialysis and ended at their death, withdrawal from the National Health Insurance program, or the end of 2013, whichever occurred first.
Exposure to NSAIDs
The detailed prescription information, including drug name, dosage, frequency, method of administration, start date, and duration of use, are recorded in the Taiwan National Health Insurance Research Database. All NSAID dispensations received by individual patients during the study period were obtained from the Taiwan National Health Insurance Research Database. All analyzed NSAIDs are shown in Table S1 of the electronic supplementary material including 25 traditional NSAIDs and 3 selective cyclooxygenase-2 (COX-2) inhibitors. The defined daily dose (DDD) recommended by the WHO was used as a measuring unit to compare the drug consumption of different NSAIDs.20
Table S1.
All analyzed nonsteroidal anti-inflammatory drugs (NSAIDs) in this study
| Classification of NSAIDs | ATC code | Drug name |
|---|---|---|
| Traditional NSAIDs | M01AB01 | Indometacin |
| M01AB02 | Sulindac | |
| M01AB03 | Tolmetin | |
| M01AB05 | Diclofenac | |
| M01AB06 | Alclofenac | |
| M01AB08 | Etodolac | |
| M01AB11 | Acemetacin | |
| M01AB15 | Ketorolac | |
| M01AB16 | Aceclofenac | |
| M01AC01 | Piroxicam | |
| M01AC02 | Tenoxicam | |
| M01AC06 | Meloxicam | |
| M01AE01 | Ibuprofen | |
| M01AE02 | Naproxen | |
| M01AE03 | Ketoprofen | |
| M01AE04 | Fenoprofen | |
| M01AE05 | Fenbufen | |
| M01AE09 | Flurbiprofen | |
| M01AE11 | Tiaprofenic acid | |
| M01AG01 | Mefenamic acid | |
| M01AG02 | Tolfenamic acid | |
| M01AG03 | Flufenamic acid | |
| M01AX01 | Nabumetone | |
| M01AX02 | Niflumic acid | |
| M01AX17 | Nimesulide | |
| Selective COX-2 inhibitors | M01AH01 | Celecoxib |
| M01AH02 | Rofecoxib | |
| M01AH05 | Etoricoxib |
Abbreviations: ATC, Anatomical Therapeutic Chemical; COX, cyclooxygenase.
Statistical analysis
Baseline characteristics were summarized using counts and percentages. The categorical variables of baseline characteristics between NSAID users and nonusers were compared using the chi-square test. To prevent immortal time bias, we used time-dependent Cox regression models to examine the association between NSAID use and all-cause mortality.21,22 We treated NSAID use as a time-varying covariate to calculate HRs and 95% CIs for NSAID users compared with nonusers. To reduce the potential residual effect of NSAID use before dialysis, new user design was used in the current study. Patients who received NSAID treatment before follow-up period were excluded. Therefore, study subjects were initially classified as nonusers until they received NSAID treatment, from which time they were then reclassified as NSAID users until the end of follow-up. To observe a dose–response relationship, we further grouped the cumulative NSAID use of NSAID users into three groups: ≤30 DDDs, 31 to 90 DDDs, and >90 DDDs. To verify the dose–response relationship between NSAID use and the risk of mortality, the cumulative NSAID use category was treated as a continuous variable to test for linear trend. A test for linear trend was applied across dose categories. In addition to overall NSAID use, we conducted analyses for the use of nonselective NSAIDs and selective COX-2 inhibitors. Adjusted HRs were computed after adjustment for age, sex, residence area, types of dialysis, opioid use, and baseline comorbidities, including myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease, liver disease, dementia, rheumatoid disease, peptic ulcer, hypertension, and diabetes mellitus. Because age, sex, residence area, cardiovascular disease, and opioid use are predictors of mortality in patients with end-stage renal disease, we conducted subgroup analyses to examine whether the mortality risk differed in the presence or absence of these characteristics.23–26
All analyses were performed using the SAS System for Windows 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
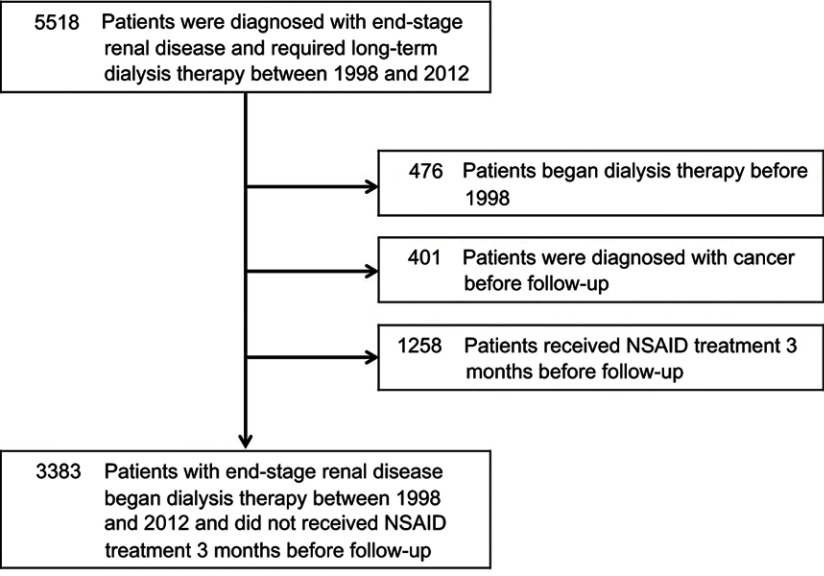
Of the 1 million representative individuals randomly selected from the Taiwan National Health Insurance Research Database, 5,518 patients aged ≥20 years were diagnosed with end-stage renal disease and required long-term dialysis therapy between 1998 and 2012. After excluding 476 patients who began dialysis therapy before 1998, 401 patients who were diagnosed with cancer before follow-up, and 1258 patients who received NSAID treatment 3 months before follow-up, a total of 3,383 patients were included (Figure 1).
Figure 1.
Flowchart of study sample selection.
Among these 3,383 patients with newly diagnosed end-stage renal disease, 2623 (78%) used NSAIDs during the follow-up period. Compared with the NSAID nonusers, the NSAID users were younger, more likely to use opioids, and less likely to have myocardial infarction, congestive heart failure, cerebrovascular disease, dementia, hypertension, and diabetes mellitus (Table 1). Other characteristics, such as sex, residence area, types of dialysis, peripheral vascular disease, chronic pulmonary disease, liver disease, rheumatoid disease, and peptic ulcer, did not appear to differ significantly between the NSAID users and nonusers.
Table 1.
Characteristics of patients with end-stage renal disease according to NSAID use
| Characteristics | Total | Any NSAID use | P-value | ||||
|---|---|---|---|---|---|---|---|
| (N=3,383) | Yes (N=2,623) | No (N=760) | |||||
| N (%) | N (%) | N (%) | |||||
| Age, years | <0.001 | ||||||
| <55 | 1,088 | (32.2) | 926 | (35.3) | 162 | (21.3) | |
| 55–64 | 816 | (24.1) | 654 | (24.9) | 162 | (21.3) | |
| 65–74 | 809 | (23.9) | 625 | (23.8) | 184 | (24.2) | |
| ≥75 | 670 | (19.8) | 418 | (15.9) | 252 | (33.2) | |
| Sex | 0.91 | ||||||
| Male | 1,720 | (50.8) | 1335 | (50.9) | 385 | (50.7) | |
| Female | 1,663 | (49.2) | 1288 | (49.1) | 375 | (49.3) | |
| Residence area | 0.18 | ||||||
| Central city | 1,893 | (56.0) | 1486 | (56.7) | 407 | (53.6) | |
| Suburban | 1,091 | (32.3) | 840 | (32.0) | 251 | (33.0) | |
| Countryside | 399 | (11.8) | 297 | (11.3) | 102 | (13.4) | |
| Dialysis | 0.60 | ||||||
| Hemodialysis | 3,082 | (91.1) | 2386 | (91.0) | 696 | (91.6) | |
| Peritoneal dialysis | 301 | (8.9) | 237 | (9.0) | 64 | (8.4) | |
| Comorbidity | |||||||
| Myocardial infarction | 151 | (4.5) | 96 | (3.7) | 55 | (7.2) | <0.001 |
| Congestive heart failure | 842 | (24.9) | 583 | (22.2) | 259 | (34.1) | <0.001 |
| Peripheral vascular disease | 66 | (2.0) | 48 | (1.8) | 18 | (2.4) | 0.35 |
| Cerebrovascular disease | 495 | (14.6) | 314 | (12.0) | 181 | (23.8) | <0.001 |
| Chronic pulmonary disease | 381 | (11.3) | 283 | (10.8) | 98 | (1.9) | 0.11 |
| Liver disease | 210 | (6.2) | 161 | (6.1) | 49 | (6.5) | 0.76 |
| Dementia | 88 | (2.6) | 43 | (1.6) | 45 | (5.9) | <0.001 |
| Rheumatoid disease | 50 | (1.5) | 40 | (1.5) | 10 | (1.3) | 0.67 |
| Peptic ulcer | 704 | (20.8) | 529 | (20.2) | 175 | (23.0) | 0.09 |
| Hypertension | 2,906 | (85.9) | 2236 | (85.3) | 670 | (88.2) | 0.04 |
| Diabetes mellitus | 1,824 | (53.9) | 1357 | (51.7) | 467 | (61.5) | <0.001 |
| Opioid use | 1,385 | (40.9) | 1240 | (47.3) | 145 | (19.1) | <0.001 |
The mean follow-up period of the study cohort was 4.0 years (interquartile range, 1.9–7.2 years), and 1515 patients from this cohort died. In the time-varying multivariable analysis, NSAID use was found to be associated with an increased risk of mortality (adjusted HR, 1.39; 95% CI, 1.21–1.60; Table 2). We also analyzed the relationship between the use of two types of NSAIDs, selective COX-2 inhibitors and nonselective NSAIDs, and the risk of mortality. Likewise, the use of nonselective NSAIDs and selective COX-2 inhibitors was associated with a higher risk of mortality (adjusted HR, 1.36; 95% CI, 1.19–1.55 and adjusted HR, 1.61; 95% CI, 1.42–1.83, respectively; Table 2).
Table 2.
Association between the use of NSAIDs and the risk of all-cause mortality in patients with end-stage renal disease
| NSAID use | Number of mortality | Person-years | Incidence rate (95% CI) (per 100 person-years) | Crude HR(95% CI) | Adjusted HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Any NSAIDs | ||||||||
| No | 372 | 4,994 | 7.4 | (6.7–8.2) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 1,143 | 11,711 | 9.8 | (9.2–10.3) | 1.40 | (1.22–1.60) | 1.39 | (1.21–1.60) |
| Nonselective NSAIDs | ||||||||
| No | 400 | 5,241 | 7.6 | (6.9–8.4) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 1,115 | 11,464 | 9.7 | (9.2–10.3) | 1.34 | (1.18–1.54) | 1.36 | (1.19–1.55) |
| Selective COX-2 inhibitors | ||||||||
| No | 1,111 | 13,835 | 8.0 | (7.6–8.5) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 404 | 2,870 | 14.1 | (12.8–15.5) | 1.81 | (1.61–2.04) | 1.61 | (1.42–1.83) |
Notes: Adjusted HRs were computed after adjustment of age, sex, residence area, types of dialysis, baseline comorbidities, and opioid use.
Abbreviation: COX, cyclooxygenase.
A significant dose–response association was observed between the cumulative use of any NSAID and mortality. Adjusted HRs for mortality were 1.32 (95% CI, 1.15–1.53), 1.57 (95% CI, 1.31–1.88), and 1.65 (95% CI, 1.35–2.01) for cumulative NSAID use of 1–30 DDDs, 31–90 DDDs, and >90 DDDs, respectively (Table 3). The higher the cumulative use of NSAIDs, the higher was the risk of mortality (P for trend <0.001). A similar dose–response association was observed in nonselective NSAID use. Adjusted HRs for mortality were 1.32 (95% CI, 1.15–1.51), 1.47 (95% CI, 1.23–1.76), and 1.62 (95% CI, 1.31–2.01) for the cumulative nonselective NSAID use of 1–30 DDDs, 31–90 DDDs, and >90 DDDs, respectively (P for trend <0.001). The aforementioned dose–response relationship between cumulative NSAID use and mortality was not observed for selective COX-2 inhibitors (Table 3).
Table 3.
Dose–response associations between the use of NSAIDs and the risk of all-cause mortality in patients with end-stage renal disease
| Cumulative NSAID use (DDDs) |
Number of mortality | Person-years | Incidence rate (95% CI) (per 100 person-years) | Crude HR (95% CI) | Adjusted HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Any NSAIDs | ||||||||
| 0 | 372 | 4,994 | 7.4 | (6.7–8.2) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 | 620 | 6,767 | 9.2 | (8.5–9.9) | 1.33 | (1.15–1.53) | 1.32 | (1.15–1.53) |
| 31−90 | 283 | 2,849 | 9.9 | (8.8–11.2) | 1.49 | (1.25–1.78) | 1.57 | (1.31–1.88) |
| >90 | 240 | 2,095 | 11.5 | (10.1–13.0) | 1.78 | (1.47–2.16) | 1.65 | (1.35–2.01) |
| Non-selective NSAIDs | ||||||||
| 0 | 400 | 5,241 | 7.6 | (6.9–8.4) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 | 676 | 7,103 | 9.5 | (8.8–10.3) | 1.32 | (1.15–1.51) | 1.32 | (1.15–1.51) |
| 31−90 | 268 | 2,766 | 9.7 | (8.6–10.9) | 1.37 | (1.15–1.64) | 1.47 | (1.23–1.76) |
| >90 | 171 | 1,595 | 10.7 | (9.2–12.5) | 1.57 | (1.27–1.93) | 1.62 | (1.31–2.01) |
| Selective COX-2 inhibitors | ||||||||
| 0 | 1,111 | 13,835 | 8.0 | (7.6–8.5) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 | 245 | 1,748 | 14.0 | (12.4–15.9) | 1.80 | (1.56–2.07) | 1.70 | (1.47–1.96) |
| 31−90 | 98 | 599 | 16.4 | (13.4–19.9) | 2.09 | (1.69–2.58) | 1.61 | (1.29–1.99) |
| >90 | 61 | 523 | 11.7 | (9.1–15.0) | 1.53 | (1.17–1.99) | 1.31 | (1.00–1.71) |
Notes: Adjusted HRs were computed after adjustment of age, sex, residence area, types of dialysis, baseline comorbidities, and opioid use.
Abbreviations: DDD, defined daily dose; COX, cyclooxygenase.
The most commonly used nonselective NSAIDs were diclofenac, mefenamic acid, and ibuprofen, which were used by 1675 (50%), 1252 (37%), and 701 (21%) study subjects, respectively. The most frequently used selective COX-2 inhibitors were celecoxib, etoricoxib, and rofecoxib, which were used by 710 (21%), 226 (7%), and 96 (3%) patients, respectively. We further analyzed the relationship between the use of these six individual NSAIDs and the risk of mortality. The results showed that the use of diclofenac, celecoxib, and etoricoxib were associated with a higher risk of mortality. Adjusted HRs for mortality were 1.44 (95% CI, 1.28–1.61), 1.57 (95% CI, 1.38–1.79), and 1.69 (95% CI, 1.33–2.16) for diclofenac, celecoxib, and etoricoxib, respectively (Table 4). A significant dose–response association between individual NSAID use and mortality was observed for diclofenac, but not for celecoxib and etoricoxib. Adjusted HRs for mortality were 1.44 (95% CI, 1.29–1.62), 1.28 (95% CI, 1.00–1.64), and 1.95 (95% CI, 1.33–2.86) for cumulative diclofenac use of 1–30 DDDs, 31–90 DDDs, and >90 DDDs, respectively (P for trend <0.001; Table S2).
Table 4.
Association between the usage of frequently used individual NSAIDs and the risk of all-cause mortality in patients with end-stage renal disease
| NSAID use | Number of mortality | Person-years | Incidence rate (95% CI) (per 100 person-years) | Crude HR (95% CI) | Adjusted HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Non-selective NSAIDs | ||||||||
| Diclofenac | ||||||||
| No | 810 | 9,967 | 8.1 | (7.6–8.7) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 705 | 6,738 | 10.5 | (9.7–11.3) | 1.33 | (1.19–1.49) | 1.44 | (1.28–1.61) |
| Mefenamic acid | ||||||||
| No | 1,017 | 1,1004 | 9.2 | (8.7–9.8) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 498 | 5,701 | 8.7 | (8.0–9.5) | 0.91 | (0.81–1.03) | 1.00 | (0.89–1.13) |
| Ibuprofen | ||||||||
| No | 1,255 | 13,718 | 9.1 | (8.7–9.7) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 260 | 2,987 | 8.7 | (7.7–9.8) | 0.93 | (0.81–1.07) | 1.13 | (0.98–1.30) |
| Selective COX-2 inhibitors | ||||||||
| Celecoxib | ||||||||
| No | 1,170 | 14,267 | 8.2 | (7.7–8.7) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 345 | 2,438 | 14.2 | (12.7–15.7) | 1.77 | (1.56–2.01) | 1.57 | (1.38–1.79) |
| Etoricoxib | ||||||||
| No | 1,442 | 16,321 | 8.8 | (8.4–9.3) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 73 | 384 | 19.0 | (15.1–23.9) | 2.17 | (1.71–2.75) | 1.69 | (1.33–2.16) |
| Rofecoxib | ||||||||
| No | 1,453 | 16,103 | 9.0 | (8.6–9.5) | 1.00 | (reference) | 1.00 | (reference) |
| Yes | 62 | 602 | 10.3 | (8.0–13.2) | 1.13 | (0.87–1.46) | 1.17 | (0.91–1.52) |
Notes: Adjusted HRs were computed after adjustment of age, sex, residence area, types of dialysis, baseline comorbidities, and opioid use.
Abbreviation: COX, cyclooxygenase.
Table S2.
Dose–response associations between the use of individual NSAIDs and the risk of all-cause mortality in patients with end-stage renal disease
| Cumulative NSAID use | Number of mortality | Person-years | Incidence rate (95% CI) (per 100 person-years) | Crude HR(95% CI) | Adjusted HR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| Diclofenac | ||||||||
| 0 DDDs (0 g) | 810 | 9967 | 8.1 | (7.6–8.7) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 DDDs (0.1−3 g) | 599 | 5656 | 10.6 | (9.8–11.5) | 1.34 | (1.19–1.50) | 1.44 | (1.29–1.62) |
| 31−90 DDDs (3.1−9 g) | 77 | 851 | 9.1 | (7.2–11.3) | 1.17 | (0.92–1.50) | 1.28 | (1.00–1.64) |
| >90 DDDs (>9 g) | 29 | 231 | 12.6 | (8.7–18.1) | 1.68 | (1.15–2.45) | 1.95 | (1.33–2.86) |
| Celecoxib | ||||||||
| 0 DDDs (0 g) | 1170 | 14267 | 8.2 | (7.7–8.7) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 DDDs (0.2−6 g) | 222 | 1565 | 14.2 | (12.4–16.2) | 1.77 | (1.53–2.05) | 1.68 | (1.44–1.95) |
| 31−90 DDDs (6.1−18 g) | 76 | 474 | 16.0 | (12.8–20.1) | 1.99 | (1.58–2.52) | 1.56 | (1.22–1.98) |
| >90 DDDs (>18 g) | 47 | 399 | 11.8 | (8.9–15.7) | 1.50 | (1.11–2.02) | 1.18 | (0.88–1.60) |
| Etoricoxib | ||||||||
| 0 DDDs (0 g) | 1442 | 16321 | 8.8 | (8.4–9.3) | 1.00 | (reference) | 1.00 | (reference) |
| 1−30 DDDs (0.06−1.8 g) | 53 | 237 | 22.4 | (17.1–29.3) | 2.53 | (1.92–3.34) | 1.95 | (1.47–2.57) |
| 31−90 DDDs (1.9−5.4 g) | 13 | 93 | 14.0 | (8.1–24.1) | 1.60 | (0.93–2.78) | 1.19 | (0.69–2.07) |
| >90 DDDs (>5.4 g) | 7 | 54 | 13.0 | (6.2–27.2) | 1.48 | (0.70–3.11) | 1.40 | (0.66–2.96) |
Notes: Adjusted HRs were computed after adjustment of age, sex, residence area, types of dialysis, baseline comorbidities, and opioid use.
Abbreviations: DDD, defined daily dose.
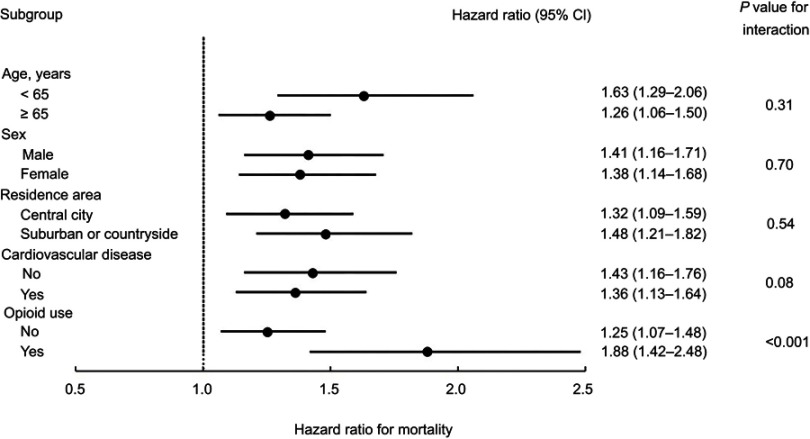
The results of subgroup analyses revealed that the association between NSAID use and mortality risk across different subgroups remained consistent with entire cohort. After adjusting for baseline characteristics, the use of NSAIDs was associated with a higher risk of mortality in different age, sex, residence area, cardiovascular disease, and opioid use subgroups (Figure 2). However, the effect of NSAID use on mortality risk was higher for opioid users than opioid nonusers (P for interaction <0.001).
Figure 2.
Subgroup analysis of association between NSAID use and all-cause mortality. The reference group was NSAID nonusers. Cardiovascular disease included myocardial infarction, congestive heart failure, peripheral vascular disease, and cerebrovascular disease.
Discussion
Although there is a general consensus that the use of NSAIDs should be avoided in patients with end-stage renal disease because of the potential deleterious effects of NSAIDs, clinical studies on the detrimental effects of NSAIDs on patients with end-stage renal disease remain scant.6,10,14 To the best of our knowledge, this is the first nationwide population-based cohort study investigating the association between the use of NSAIDs and the risk of mortality in patients with end-stage renal disease. Our findings suggest that NSAID use was associated with an increased risk of mortality in the patients with end-stage renal disease. In addition, significant dose–response relationships between NSAID use and mortality were observed in the current study. A single-center cohort study found that baseline NSAID use was not associated with mortality risk in patients with chronic kidney disease.27 However, due to lacking information about NSAID use during the 6 years follow-up, the study cannot conclude the association between NSAID use and the risk of mortality. The relationship between the use of NSAIDs and an increased risk of mortality has been reported in previous studies for patients with chronic heart failure and myocardial infarction.28,29 Although clinical guidelines discourage the use of NSAIDs in patients with cardiovascular disease, the results of these two studies have shown that NSAIDs were used in 34% of patients with chronic heart failure and 42% of patients with myocardial infarction, and their use was associated with an increased risk of death and cardiovascular morbidity. Similarly, although Taiwan chronic kidney disease clinical guidelines recommend that NSAIDs should be used with caution and in reduced doses in patients with chronic kidney disease,30 our results showed that NSAIDs were used in 78% of the patients with end-stage renal disease receiving dialysis, and their use was associated with an increased risk of mortality. These results suggest that clinicians and patients lack the awareness that NSAIDs can be harmful to patients with end-stage renal disease.
The cardiovascular and gastrointestinal safety of NSAIDs, including selective COX-2 inhibitors and nonselective NSAIDs, have attracted increasing attention in the past years.31–33 The results of a large meta-analysis of 280 placebo-controlled trials and 474 active-controlled trials showed that both nonselective NSAIDs and selective COX-2 inhibitors increased the risks of heart failure and upper gastrointestinal complications.31 This meta-analysis also reported that diclofenac, ibuprofen, and selective COX-2 inhibitors significantly increased fatal coronary events. Another meta-analysis of 31 large-scale randomized controlled trials found that individual NSAIDs increased cardiovascular risks by varying degrees.32 The results of this meta-analysis showed that etoricoxib and diclofenac significantly increased the risk of cardiovascular death by approximately four times compared with placebo. These findings indicate NSAID use is associated with increased risks of gastrointestinal complications, cardiovascular adverse events, and mortality. Our findings regarding the relationship between the use of both nonselective NSAIDs and selective COX-2 inhibitors and the risk of mortality are consistent with those of the aforementioned previous studies. In addition, a significant dose–response relationship was observed between cumulative NSAID use and mortality risk in the current study.
NSAIDs exhibit their analgesic, anti-inflammatory, and antipyretic effects by inhibiting COX-1 and COX-2.33 However, the inhibition of these two types of COXs may disturb normal physiological functions throughout the body, including gastric cytoprotection, kidney function, platelet aggregation, and thrombosis, and subsequently may lead to adverse effects, including gastrointestinal ulcers and bleeding, renal dysfunction, myocardial infarction, heart failure, venous thrombosis, hypertension, and stroke.33–35 Studies have indicated that NSAIDs are frequently used in patients with end-stage renal disease who are susceptible to cardiovascular and gastrointestinal complications.11,13,36,37 However, few studies have investigated the safety of NSAID use in this population. A case-control study reported that the use of nonselective NSAIDs was associated with an increased risk of gastrointestinal bleeding in patients receiving hemodialysis.36 The results of another case–crossover study indicated that NSAID use resulted in a 1.31-fold increased risk of stroke in patients receiving dialysis.37 The results of these two studies indicate that NSAID use is harmful to patients with end-stage renal disease. Advances in renal replacement therapy provide the opportunity for patients with end-stage renal disease to prolong their lives; however, mortality in patients with end-stage renal disease remains far in excess of that in the general population.38,39 To improve the prognosis of patients with end-stage renal disease, we need to pay attention to the harmful effects of NSAID use.
The major strengths of this study are its nationwide coverage, large study population, complete follow-up, and comprehensive diagnoses and prescription information. The data used in the current study were medical records of 1 million representative beneficiaries who were randomly selected from 23 million insured individuals with minimal selection bias. In addition, we identified NSAID prescriptions by using a nationwide administrative database; this enabled us to obtain detailed NSAID prescription records and prevent recall bias. Furthermore, study patients were verified based on their catastrophic illness certificate to ensure high case validity. Finally, we used the new user design to reduce the potential residual effect of NSAID use before dialysis.
This study has several limitations that should be addressed. First, patients can obtain over-the-counter NSAIDs that are not covered by the Taiwan National Health Insurance. Therefore, the use of NSAIDs may be underestimated. Second, it is likely that patients were not fully compliant with NSAID prescriptions. Third, data used in this study are from a claim-based database; accordingly, no detailed clinical information regarding biochemical data, physical activity, body mass index, smoking, and alcohol consumption was available. Fourth, patients’ comorbidities were defined according to ICD-9-CM codes in claims data. Only few of these diagnoses were proved to have high positive predict value.40 Finally, because the Registry of Catastrophic Illness Database of the Taiwan National Health Insurance Research Database provides only the date of death, information regarding the exact cause of death is not available.
Conclusion
In conclusion, a considerable number of the patients with end-stage renal disease experienced acute or chronic pain. However, the results of the current observational study suggested that NSAID use was associated with an increased risk of mortality in the patients with end-stage renal disease and the risk of mortality is proportional to the cumulative use of NSAIDs. Future randomized controlled trials are needed to validate these observational findings.
Acknowledgments
This study was based in part on data from the Taiwan National Health Insurance Research Database provided by the National Health Insurance Administration, Ministry of Health and Welfare and managed by National Health Research Institutes. The interpretations and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare or National Health Research Institutes. This study was supported by grants from the Taiwan Ministry of Health and Welfare (CCMP102-RD-015). This manuscript was edited by Wallace Academic Editing.
Disclosure
Dr Yuan-Wen Lee reports grants from the Taiwan Ministry of Health and Welfare, during the conduct of the study. The authors report no other conflicts of interest in this work.
Supplementary materials
References
- 1.Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9 [DOI] [PubMed] [Google Scholar]
- 2.Murtagh FE, Addington-Hall J, Higginson IJ. The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis. 2007;14:82–99. doi: 10.1053/j.ackd.2006.10.001 [DOI] [PubMed] [Google Scholar]
- 3.Davison SN. Pain in hemodialysis patients: prevalence, cause, severity, and management. Am J Kidney Dis. 2003;42:1239–1247. doi: 10.1053/j.ajkd.2003.08.025 [DOI] [PubMed] [Google Scholar]
- 4.Brkovic T, Burilovic E, Puljak L. Prevalence and severity of pain in adult end-stage renal disease patients on chronic intermittent hemodialysis: a systematic review. Patient Prefer Adherence. 2016;10:1131–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santoro D, Satta E, Messina S, Costantino G, Savica V, Bellinghieri G. Pain in end-stage renal disease: a frequent and neglected clinical problem. Clin Nephrol. 2013;79(Suppl 1):S2–S11. [PubMed] [Google Scholar]
- 6.Kurella M, Bennett WM, Chertow GM. Analgesia in patients with ESRD: a review of available evidence. Am J Kidney Dis. 2003;42:217–228. doi: 10.1016/S0272-6386(03)00645-0 [DOI] [PubMed] [Google Scholar]
- 7.Pai AB, Cardone KE, Manley HJ, et al. Medication reconciliation and therapy management in dialysis-dependent patients: need for a systematic approach. Clin J Am Soc Nephrol. 2013;8:1988–1999. doi: 10.2215/CJN.01420213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathew RO, Bettinger JJ, Wegrzyn EL, Fudin J. Pharmacotherapeutic considerations for chronic pain in chronic kidney and end-stage renal disease. J Pain Res. 2016;9:1191–1195. doi: 10.2147/JPR.S125270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barakzoy AS, Moss AH. Efficacy of the World Health Organization analgesic ladder to treat pain in end-stage renal disease. J Am Soc Nephrol. 2006;17:3198–3203. doi: 10.1681/ASN.2006050477 [DOI] [PubMed] [Google Scholar]
- 10.Williams AW, Dwyer AC, Eddy AA, et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012;7:1664–1672. doi: 10.2215/CJN.10251011 [DOI] [PubMed] [Google Scholar]
- 11.Davison SN, Koncicki H, Brennan F. Pain in chronic kidney disease: a scoping review. Semin Dial. 2014;27:188–204. doi: 10.1111/sdi.2014.27.issue-2 [DOI] [PubMed] [Google Scholar]
- 12.Wu J, Ginsberg JS, Zhan M, et al. Chronic pain and analgesic use in CKD: implications for patient safety. Clin J Am Soc Nephrol. 2015;10:435–442. doi: 10.2215/CJN.06520714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heleniak Z, Cieplińska M, Szychliński T, et al. Nonsteroidal anti-inflammatory drug use in patients with chronic kidney disease. J Nephrol. 2017;30:781–786. doi: 10.1007/s40620-016-0352-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plantinga L, Grubbs V, Sarkar U, et al. Nonsteroidal anti-inflammatory drug use among persons with chronic kidney disease in the United States. Ann Fam Med. 2011;9:423–430. doi: 10.1370/afm.1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davison SN. Pain, analgesics, and safety in patients with CKD. Clin J Am Soc Nephrol. 2015;10:350–352. doi: 10.2215/CJN.00600115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Health Insurance Administration, Ministry of Health and Welfare. Universal Health Coverage in Taiwan. 2018. Available from: https://www.nhi.gov.tw/English/Content_List.aspx?n=8FC0974BBFEFA56D&topn=ED4A30E51A609E49. Accessed January7, 2019.
- 17.Lee YW, Chen TL, Shih YR, et al. Adjunctive traditional Chinese medicine therapy improves survival in patients with advanced breast cancer: a population-based study. Cancer. 2014;120:1338–1344. doi: 10.1002/cncr.28579 [DOI] [PubMed] [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 19.Tonelli M, Wiebe N, Guthrie B, et al. Comorbidity as a driver of adverse outcomes in people with chronic kidney disease. Kidney Int. 2015;88:859–866. doi: 10.1038/ki.2015.29 [DOI] [PubMed] [Google Scholar]
- 20.WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment 2019. Oslo, Norway: WHO Collaborating Centre; 2018. Available from: https://www.whocc.no/filearchive/publications/2019_guidelines_web.pdf. Accessed January 7, 2019. [Google Scholar]
- 21.Lévesque LE, Hanley JA, Kezouh A, Suissa S. Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. BMJ. 2010;340:b5087. doi: 10.1136/bmj.c293 [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Weinhandl ED, Gilbertson DT, Collins AJ, St Peter WL. Issues regarding ‘immortal time’ in the analysis of the treatment effects in observational studies. Kidney Int. 2012;81:341–350. [DOI] [PubMed] [Google Scholar]
- 23.Robinson BM, Zhang J, Morgenstern H, et al. Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney Int. 2014;85:158–165. doi: 10.1038/ki.2013.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tong J, Liu M, Li H, et al. Mortality and associated risk factors in dialysis patients with cardiovascular disease. Kidney Blood Press Res. 2016;41:479–487. doi: 10.1159/000443449 [DOI] [PubMed] [Google Scholar]
- 25.McQuillan R, Trpeski L, Fenton S, Lok CE. Modifiable risk factors for early mortality on hemodialysis. Int J Nephrol. 2012;2012:435736. doi: 10.1155/2012/435736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimmel PL, Fwu CW, Abbott KC, Eggers AW, Kline PP, Eggers PW. Opioid prescription, morbidity, and mortality in United States dialysis patients. J Am Soc Nephrol. 2017;28:3658–3670. doi: 10.1681/ASN.2016080886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu HJ, Wu IW, Hsu KH, et al. The association between chronic musculoskeletal pain and clinical outcome in chronic kidney disease patients: a prospective cohort study. Ren Fail. 2019;41:257–266. doi: 10.1080/0886022X.2019.1596817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gislason GH, Rasmussen JN, Abildstrom SZ, et al. Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure. Arch Intern Med. 2009;169:141–149. doi: 10.1001/archinternmed.2008.525 [DOI] [PubMed] [Google Scholar]
- 29.Schjerning Olsen AM, Fosbøl EL, Lindhardsen J, et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011;123:2226–2235. doi: 10.1161/CIRCULATIONAHA.110.004671 [DOI] [PubMed] [Google Scholar]
- 30.Taiwan Society of Nephrology. Taiwan chronic kidney disease clinical guidelines. 2015. Available from: https://www.tsn.org.tw/. Accessed April26, 2019.
- 31.Bhala N, Emberson J, Merhi A, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 382;2013:769–779. doi: 10.1016/S0140-6736(13)60900-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammaroty drugs: network meta-analysis. BMJ. 2011;342:c7086. doi: 10.1136/bmj.c7086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt M, Lamberts M, Olsen AM, et al. Cardiovascular safety of non-aspirin non-steroidal anti-inflammatory drugs: review and position paper by working group for Cardiovascular Pharmacotherapy of the European Society of Cardiology. Eur Heart J. 2016;37:1015–1023. doi: 10.1093/eurheartj/ehv505 [DOI] [PubMed] [Google Scholar]
- 34.Day RO, Graham GG. Non-steroidal anti-inflammatory drugs (NSAIDs). BMJ. 2013;346:f3195. doi: 10.1136/bmj.f1164 [DOI] [PubMed] [Google Scholar]
- 35.Grosser T, Fries S, FitzGerald GA. Biological basis for the cardiovascular consequences of COX-2 inhibition: therapeutic challenges and opportunities. J Clin Invest. 2006;116:4–15. doi: 10.1172/JCI27291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jankovic SM, Aleksic J, Rakovic S, et al. Nonsteroidal anti-inflammatory drugs and risk of gastrointestinal bleeding among patients on hemodialysis. J Nephrol. 2009;22:502–507. [PubMed] [Google Scholar]
- 37.Hsu CC, Chang YK, Hsu YH, et al. Association of nonsteroidal anti-inflammatory drug use with stroke among dialysis patients. Kidney Int Rep. 2017;2:400–409. doi: 10.1016/j.ekir.2017.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prichard SS. Comorbidities and their impact on outcome in patients with end-stage renal disease. Kidney Int. 2000;57(suppl 74):S100–S104. doi: 10.1046/j.1523-1755.2000.07417.x [DOI] [Google Scholar]
- 39.Storey BC, Staplin N, Harper CH, et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney Int. 2018;93:1165–1174. doi: 10.1016/j.kint.2017.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 2015;114:254–259. doi: 10.1016/j.jfma.2013.09.009 [DOI] [PubMed] [Google Scholar]