Abstract
PURPOSE:
We examined associations between caregiving intensity and mental health among cancer caregivers at the population level and potential moderation by an actionable intervention target, support service needs.
METHODS:
Behavioral Risk Factors Surveillance System survey data (2015) from caregivers of adult patients with cancer was analyzed. Caregiving intensity included hours per week caregiving (high, > 20; low, ≤ 20) and caregiving duration (long, > 2 years; short, ≤ 2 years). Mental health was reported as number of mentally unhealthy days (MUDs) in the past 30. Support service needs comprised caregiving classes, service access, support groups, counseling, and respite care. Multivariable linear regression models were performed adjusting for sociodemographics and sampling weights.
RESULTS:
A total of 1,831 caregivers were included in the study, representing approximately 1.1 million cancer caregivers in the 18 US states, distributed with the following intensity: 122 (8.3%) caregivers reported care at high hours/long duration, 213 (13.1%) high hours/short duration, 329 (18.4%) low hours/long duration, and 910 (60.2%) low hours/short duration. Mean MUDs was 6 (SE, 0.5). The highest reported unmet service need was help with service access (48.4%). Higher caregiving intensity and support service need were associated with more MUDs (P < .05), with a significant interaction (P = .02) between caregiving intensity and unmet support service needs. High hour/long duration caregivers reporting any unmet needs had a mean of 15 versus 8 MUDs for those with no unmet needs.
CONCLUSION:
High-intensity cancer caregiving was associated with poor mental health, especially for those reporting support service needs. Developing strategies to optimize support service provision for high-intensity cancer caregivers is warranted.
INTRODUCTION
Caring for a relative or friend with cancer is both ubiquitous and taxing, but precise estimates of the prevalence of family/informal (unpaid) caregivers and characteristics of caregiving burden are largely unknown and untracked by health care systems.1,2 As highlighted by the National Academy of Medicine3 and the National Institutes of Health,4 this is a major public health issue for oncology clinicians, cancer centers, health systems, and policy makers, because these cancer family caregivers provide daily assistance and care to patients in the home, oftentimes over a period of several years. Evidence suggests that caregivers experience marked distress5,6 that threatens health and, by consequence, their ability to manage care for their care recipients.7-9 Clarifying the intensity of family caregiving and its health impact is a critical step toward building the case for increasing public health surveillance and enhanced formal support for this hidden workforce.
There are few population-based reports of individuals actively caregiving for an individual with cancer. Most studies rely on small convenience samples.4 The most widely cited prevalence statistic—that 2.8 million Americans are currently caring for a relative or friend with a primary cancer diagnosis—comes from a 2016 National Alliance for Caregiving report. However, this estimate was derived from a probability sample accessed via the internet and from a small subsample of 111 cancer caregivers (out of 1,275 caregivers of all disease types).10 Few other population-based data sources exist to corroborate these estimates. However, in 2015, the Behavioral Risk Factor Surveillance System (BRFSS), a national state-based telephone survey on health and health-related risk behaviors run by the Centers for Disease Control and Prevention, included an optional caregiving module fielded by some states. The availability of these data now makes additional population-based estimates of cancer caregiving possible.
Using this national BRFSS data set, the purpose of this study was to characterize cancer caregiving in the United States, and the relationship between caregiving intensity and its impact on mental health, to help identify caregivers in strongest need of intervention. We hypothesized that higher-intensity cancer caregiving would be associated with worse caregiver mental health. A secondary objective was to examine whether having unmet support service needs moderates the relationship between caregiving intensity on mental health, predicting that caregivers who had support service needs met would report better mental health.
METHODS
Data
Data were drawn from the 2015 Caregiving Module of the BRFSS, an annual, nationally representative telephone survey of US adults conducted by the Centers for Disease Control and Prevention on health from probability-sampled households in US states.11 Deidentified data are publicly available; hence, this study was exempt from institutional review board approval.
Two objectives outlined in Healthy People 202011a-11b are associated with the development of the Caregiver Module: Objective OA-9, reducing the proportion of unpaid caregivers of older adults who report an unmet need for a caregiver support service, and Objective DH-2.2, increasing the number of state health departments that conduct health surveillance of caregivers for people with disabilities. The Caregiver Module was originally fielded in 2006 to 2009, then updated for fielding in 2008 to 2012, and updated again and fielded in 2015 to an eight-item module fielded in 24 states: Alabama, Florida, Hawaii, Idaho, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Mississippi, Nebraska, New Jersey, New York, Oregon, Pennsylvania, South Carolina, Tennessee, Utah, Virginia, West Virginia, Wisconsin, and Wyoming. Items assess the care recipient’s relationship to the caregiver, duration spent and hours per week caregiving, care recipient major health problem/reason for caregiving, whether the caregiver manages personal care and/or household tasks, unmet support service needs, and whether a person expects to serve as a caregiver in the next 2 years. A report on caregiving for patients with Alzheimer’s/dementia combining BRFSS data from 2009 and 2010 from selected states reported that cancer was the second most common care recipient major health problem, with a 13.9% prevalence.12 The year 2015 was chosen for the current study, given that it was the year in which the largest number of states fielded the caregiving module at the time of this analysis. Data from the Caregiving, Healthy Days, and Demographics sections and Caregiving Module were used for the current study.
Individuals were eligible for sample selection from the 24 states that fielded the caregiving module if they endorsed the following question: “During the past 30 days, did you provide regular care or assistance to a friend or family member who has a health problem or disability?”13 A total of 24,034 (21.77% weighted) endorsed this question. Of those who indicated they were caregivers, 1,910 (9.1% weighted) from 18 states indicated that cancer was the major health problem in the care recipient. Participants were asked to name the relationship between caregiver and care recipient. Those who responded that the care recipient was a child (n = 76) were excluded from the current analysis, given the focus of the article of caregiving for adults with cancer, leaving 1,831 (96.6% weighted) caregivers of adult patients with cancer.
Measures
Our data included the following demographic characteristics for cancer family caregivers in the BRFSS survey: caregiver age at survey (18 to 34, 35 to 54, 55 to 64, and older than 65 years of age), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic), sex (male, female), income groups (< $25K, $25 to $50K, > $50K), educational attainment (high school, some college or technical school, college or technical school graduate or higher), employment (working, not working, retired), region of the country (Northeast: Pennsylvania, New Jersey; Midwest: Illinois, Indiana, Iowa, Wisconsin; South: Alabama, Kentucky, Louisiana, Mississippi, South Carolina, Tennessee, Virginia, West Virginia; West: Hawaii, Idaho, Oregon, Wyoming), marital status (married, not married) living with any children in the house (none, one or more), and the relationship of caregivers to care recipient (spouse v nonspouse). Urban/rural status was moderately correlated with region (r = 0.30), and preliminary analyses demonstrated it not to be associated with caregiver mental health; thus, it was not included as a covariate. Of the 1,831 used to estimate prevalence, 48 caregivers were excluded for missing demographics and 209 for missing caregiving intensity data (caregiving duration and/or hours per week), resulting in a final analytic data set of 1,574 caregivers.
Caregiving intensity was operationalized as according to two dimensions: hours per week caregiving and duration in months. Hours per week caregiving was dichotomized as 20 or more or less than 20 hours, and caregiving duration was dichotomized at 2 or more or less than 2 years, on the basis of previous work.10 Caregiving for patients with cancer, in comparison with other health conditions, has been shown to be more intense but episodic.10 Thus, given the possible concurrent experiences of becoming accustomed to caregiving and experiencing burnout, a four-level caregiving intensity variable was constructed from both dimensions: high hours/long duration, high hours/short duration, low hours/long duration, and low hours/short duration.
Caregiver mental health was indicated by a single item asking respondents about mentally unhealthy days: “Thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?”15 The Mentally Unhealthy Days (MUD) measure has been shown to explain 64% of the variation in a widely known legacy measure, the Short Form (SF)-36 Mental Component Summary score.15 In addition, MUD showed ten-fold lower missing data rates than the Patient Health Questionnaire and Kessler-6 in another BRFSS study of adults experiencing frequent mental distress.16 MUD has also been found to be correlated with (r = 0.40) but distinct from depressive symptoms in a study of older adults using data from the Chicago Health and Aging Project.17 Unmet support service needs were elicited by asking respondents: “Of the following support services, which one do you most need, that you are not currently getting?” Responses included: “Classes about giving care, such as giving medications,” “Help in getting access to services,” “Support groups,” “Individual counseling to help cope with giving care,” “Respite care,” and “You don’t need any of these support services.”
Statistical Analysis
Descriptive statistics included distributions and prevalence estimates of the characteristics of cancer caregivers and their unmet support service needs (any v no need). Multivariable linear regression modeled MUDs and unmet support service needs regressed on caregiving intensity. Unmet supportive care needs were examined as a moderator to determine if the association between intensity and MUDs was stronger in those with unmet supportive care needs. Sampling weights were applied to generate population-based estimates. Analyses were conducted using the Statistical Analysis Software (SAS Institute, Cary, NC) callable version of SUDAAN (RTI International, Research Triangle Park, NC) to account for complex sampling design and incorporate sampling weights. Results were interpreted as significant for two-sided P values < .05.
RESULTS
Of 24,034 BRFSS respondents who reported serving as a caregiver in 2015, 1,831 endorsed caring for an adult with cancer, representative of an estimated 1.1 million people (95% CI, 1.0 to 1.2 million people) in these 18 US states (Data Supplement). Estimates range from 5,652 (95% CI, 3,508 to 7,796) cancer caregivers in Wyoming to 176,581 (95% CI, 119,267 to 233,896) caregivers in Pennsylvania.
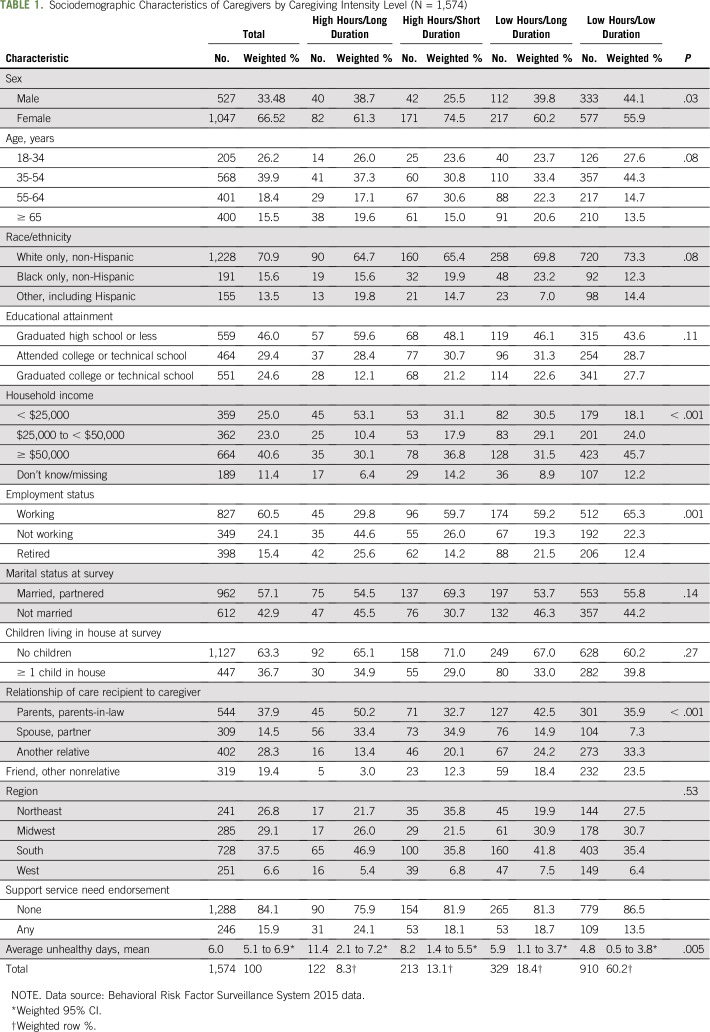
Out of 1,574 cancer caregiver respondents, 66.5% caregivers were female, 57.1% were married, and 46.0% reported high school education or less (n = 559; 46.0%; Table 1). Almost half the sample (48%) reported incomes less than $50,000. A total of 544 (37.9%) indicated they were providing care to a parent or parent-in-law, followed by another relative (n = 402; 28.3%).
TABLE 1.
Sociodemographic Characteristics of Caregivers by Caregiving Intensity Level (N = 1,574)
Caregiving Intensity and Mental Health
The distribution of caregiving intensity was as follows: 122 (8.3%) reported caregiving for high hours/long duration, 213 (13.1%) high hours/short duration, 329 (18.4%) low hours/long duration, and 910 (60.2%) low hours/short duration. Distribution of caregiving intensity varied significantly by the following variables: sex, household income, employment status, and relationship of care recipient to caregiver (all P < .05). The average number of MUDs in the past 30 was 6.0 (95% CI, 5.1 to 6.9). MUDs varied significantly by caregiving intensity (P = .005; Table 2).
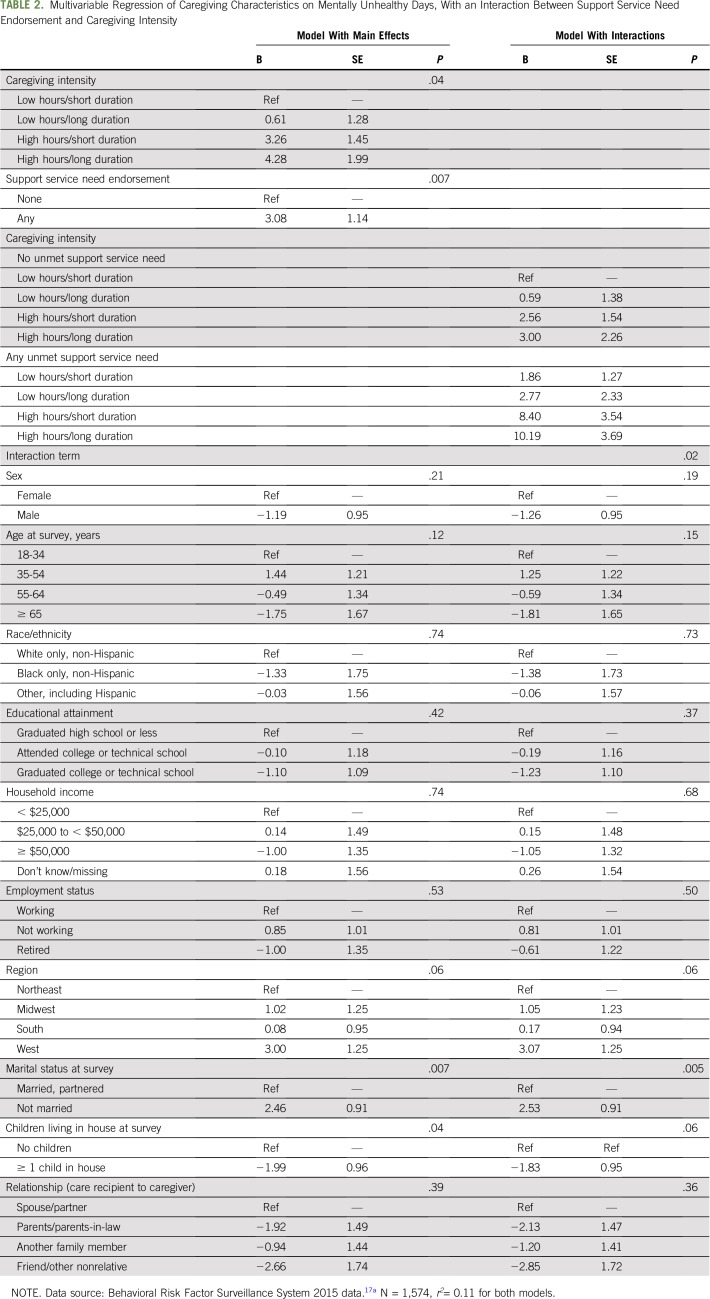
TABLE 2.
Multivariable Regression of Caregiving Characteristics on Mentally Unhealthy Days, With an Interaction Between Support Service Need Endorsement and Caregiving Intensity
Moderating Effect of Caregiver Support Service Needs
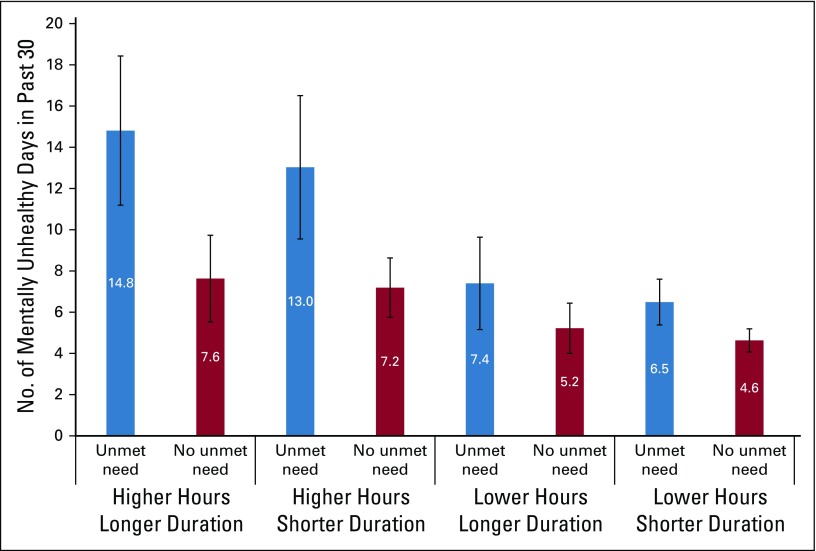
A total of 246 (15.9% weighted) cancer caregivers reported having any support service needs (Table 1). Those who endorsed any needs selected their primary need, which yielded the following distribution: help getting access to services was the most commonly endorsed (48.4%), followed by individual counseling to help cope with giving care (15.6%); classes about giving care, such as giving medications (13.6%); support groups (13.1%); and respite care (9.3%). Multivariable regression modeling on MUDs with adjustment revealed that caregiving burden and support service need endorsement were significantly associated with MUDs (P = .04; Table 2). Individuals reporting high hours/long duration caregiving on average reported 4 additional MUDs over low hours/low duration caregivers (SE, 1.99 MUDs). Those reporting high hours/short duration reported 3 additional MUDs (SE, 1.45 MUDs), and those reporting low hours/long duration caregiving reported 0.6 additional MUDs (SE, 1.28). Those reporting any support service need were more likely to report more MUDs (average 3 [SE, 1.14] more MUDs) compared with those with none. There was a significant interaction (P = .02) between caregiving intensity and unmet support service need, with more MUDs highest among those with high hours/long duration caregiving and any support service needs (Table 2; Fig 1). Cancer caregivers reporting high hours/long duration caregiving and any unmet support service need reported 15 unhealthy days on average per month, followed by those caregiving for low hours/long duration (13 MUDs; Fig 1). The number of MUDs was lowest for those without unmet support service needs and who were caregiving low hours/short duration (5 MUDs).
Fig 1.
Number of mentally unhealthy days by caregiving intensity and unmet support service, adjusted for other covariates in the full model.
DISCUSSION
On the basis of a sample of 1,831 family caregivers from 18 states representing all US regions, we estimate approximately 1.1 million family caregivers of adults with cancer living in these states. More than one in five cancer family caregivers were performing in the role more than 20 hours per week, and one in four were providing care over a span of 2 or more years. On average, cancer caregivers felt mentally unhealthy nearly 1 week each month, and high-intensity caregivers experienced more than double that time. However, the number of MUDs was lower for caregivers reporting that their support service needs were being met. To our knowledge, this is the first US-based nationally representative study to describe the intensity, mental health, and support service use of cancer family caregivers, which is a critical step to rally support from the oncology community for enhanced public health surveillance and support service development for this vulnerable yet invaluable hidden frontline workforce.
Because this study was based on a large national sample, these findings greatly reinforce and corroborate reports by other cancer caregiving research,7,8,10,18,19 namely that providing support to a relative with cancer can worsen one’s mental health. On average, caregivers in our study who were providing 20 or more hours of care per week over a duration of 2 or more years had 11.4 MUDs per month compared with 4.8 MUDs for those caregivers reporting less than 20 hours per week and who had been in the role less than 2 years. Caregiving intensity can increase as cancer progresses and requires more intense home symptom management and more support for care recipients’ activities of daily living.20 The accumulation of caregiving tasks in combination with witnessing someone struggle with cancer can exceed a caregivers’ coping strategies used to counterbalance stresses on day-to-day mental health. The BRFSS survey did not contain data on cancer staging or on what caregivers perceived their greatest source of stress to be. Thus, future surveillance efforts, both at the national level and locally in cancer centers, should include data on the care recipients’ cancer stage and on sources of caregivers’ distress. Of note, additional findings in our study include the additional demands that some caregivers reported, including caring for children in the home and employment, suggesting the need to identify the sociodemographic group who may be at high risk of poor mental health and/or poor support service access.
Another strength of the BRFSS data for this analysis was the collection of support service needs by cancer caregivers. Approximately 16% of all cancer caregivers and nearly one in four (24.1%) high-intensity caregivers reported at least one unmet support service need, consistent with other studies.10,21-24 Almost half of those with unmet needs indicated needing help with service access. This suggests that a good starting point for ameliorating distress may be the provision of navigation services to enhance family access to services that may already exist in their local communities and cancer centers.25,26 Cancer centers participating in payment models that include patient navigation, such as the Centers for Medicaid and Medicare Services Oncology Care Model,27 might also consider enhancing their navigation programs to also screen, assess, and provide direct services to family caregivers.
Few cancer caregivers in this study expressed a desire for formal psychological support. A cross-sectional study of cancer caregivers in Belgium found that only one in five caregivers indicated a desire for support, despite one in two reporting significant levels of distress,22 which might suggest that some caregivers may not recognize the need for and value of psychosocial support. In addition, unmet needs can persist into cancer survivorship. One longitudinal study found one third of cancer caregivers reporting unmet needs at 24 months postdiagnosis, including concerns about cancer recurrence.28 In addition, there may be cultural norms that suppress help seeking from distressed caregivers if providing care to a relative is viewed as an expected part of the familial relationship.29 Together, these previous findings in conjunction with the current study suggest a need for health systems and oncology clinicians to more proactively assess caregiver distress and support service needs.
Encouragingly, those caregivers in this analysis who did have their support services needs met had significantly fewer MUDs. High-intensity cancer caregivers with at least one unmet support service need experienced 15 MUDs per month, versus 8 for those who reported none. First, this suggests that when support services are accessed, they seem to be successful in addressing these caregivers’ needs and alleviating their mental distress. Second, it indicates that support services seem to already exist in many communities; hence, cancer centers may only need to develop mechanisms to screen and refer families to already existing support services in their catchment areas. It is important to note the data for the current study came from a population-based sample; thus, findings on support service needs might differ from studies conducted with caregivers sourced from clinical settings. The inclusion of items on supportive service utilization in future national surveys of caregivers would inform better understanding of what caregivers find most helpful.
The findings of this study should be interpreted with certain caveats. Overall, the BRFSS study is designed to assess population-based prevalence of health experiences, behaviors, and outcomes; thus, specific and detailed information on the needs and preferences, such as specific caregiving support service needs, must be followed up with additional study. Only one major component of burden, time intensity, was captured by the current study, because of availability of data. Caregiver burden is clearly subjective, multidimensional, and challenging to quantify, however. It might also include impact of caregiving on health, finances, and family functioning.30 Additional limitations of the study include respondent recall bias, lack of verification, and specific information about the care recipient’s cancer diagnosis, and that the caregiving module was only fielded in about half the states in the United States. The caregiving module asked respondents to indicate the support service need they most needed, rather than allowing respondents to select more than one option, which may underestimate cumulative need. Caregiver mental health was captured by a single item, MUD, which is designed to give a prevalence estimate of perceived mental health and distress but not intended to substitute as a screener for depression or other serious mental health problems.31 Notably, MUD is correlated with depressive symptoms but considered unique.17 The current study made use of this increasingly recognized measure to capture a broader spectrum of distress among family caregivers. Finally, these data are cross-sectional, and, hence, we are unable to affirm beyond speculation the causal mechanisms that may be affecting the relationship between caregiving intensity, mental health, and support service need. Major strengths of the study, however, include use of a population-based sample, large sample size, and direct assessment of caregiving conditions and burden from caregivers themselves.
In conclusion, high-intensity cancer caregiving was associated with poor mental health, especially for those reporting support service needs. Having supportive service needs met may result in greatly reducing the impact of this intensity on caregivers’ mental health. Prioritizing the development of national strategies to optimize assessment and provision of support services for high-intensity cancer caregivers is strongly warranted.
Footnotes
Supported by the National Institute of Nursing Research Grant No. 1K99NR015903 (J.N.D.-O.).
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Provision of study material or patients: Erin E. Kent
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Population-Based Profile of Mental Health and Support Service Need Among Family Caregivers of Adults With Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
No potential conflicts of interest were reported.
REFERENCES
- 1.Kelly K, Wolfe N, Gibson MJ, et al. : Listening to Family Caregivers: The Need to Include Family Caregiver Assessment in Medicaid Home- and Community-Based Service Waiver Programs. Washington, DC, AARP Public Policy Institute, 2013 [Google Scholar]
- 2.Schulz R: Research priorities in geriatric palliative care: Informal caregiving. J Palliat Med 16:1008-1012, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Academies of Sciences, Engineering, and Medicine: Families caring for an aging America. Washington, DC, National Academies Press, 2016. [PubMed]
- 4.Kent EE, Rowland JH, Northouse L, et al. : Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer 122:1987-1995, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Applebaum AJ, Breitbart W: Care for the cancer caregiver: A systematic review. Palliat Support Care 11:231-252, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stenberg U, Ruland CM, Miaskowski C: Review of the literature on the effects of caring for a patient with cancer. Psychooncology 19:1013-1025, 2010 [DOI] [PubMed] [Google Scholar]
- 7.Dionne-Odom JN, Demark-Wahnefried W, Taylor RA, et al. : The self-care practices of family caregivers of persons with poor prognosis cancer: Differences by varying levels of caregiver well-being and preparedness. Support Care Cancer 25:2437-2444, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadhwa D, Burman D, Swami N, et al. : Quality of life and mental health in caregivers of outpatients with advanced cancer. Psychooncology 22:403-410, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Litzelman K, Kent EE, Mollica M, et al. : How does caregiver well-being relate to perceived quality of care in patients with cancer? Exploring associations and pathways. J Clin Oncol 34:3554-3561, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Alliance for Caregiving, National Cancer Institute, Cancer Support Community: Cancer Caregiving in the U.S.: An Intense. Episodic, and Challenging Experience. Washington, DC, National Alliance for Caregiving, 2016. [Google Scholar]
- 11.Mokdad AH: The Behavioral Risk Factors Surveillance System: Past, present, and future. Annu Rev Public Health 30:43-54, 2009 [DOI] [PubMed] [Google Scholar]
- 11a. Department of Health and Human Services Office of Disease Prevention and Health Promotion: Healthy people 2020 DH-2.2: Increase the number of state and the District of Columbia health departments that conduct health surveillance of caregivers for people with disabilities, 2011, https://www.healthypeople.gov/2020/topics-objectives/topic/disability-and-health/objectives. [Google Scholar]
- 11b. Department of Health and Human Services Office of Disease Prevention and Health Promotion: Healthy people 2020 OA-9: Reduce the proportion of unpaid caregivers of older adults who report an unmet need for caregiver support services, 2011, https://www.healthypeople.gov/2020/topics-objectives/topic/older-adults/objectives. [Google Scholar]
- 12. Caregiving Across the United States: Caregivers of persons with Alzheimer's disease or dementia in 8 states and the District of Columbia, 2010. https://www.alz.org/documents_custom/public-health/2009-2010-combined-caregiving.pdf. [Google Scholar]
- 13. Centers for Disease Control and Prevention: Behavioral Risk Factor Surveillance System (BRFSS). Caregiver Module. 2017. https://www.cdc.gov/aging/healthybrain/brfss-faq-caregiver.htm.
- 14. Reference deleted.
- 15. Centers for Disease Control and Prevention. Measuring Healthy Days. Atlanta, GA. 2000. [Google Scholar]
- 16.Liu J, Jiang N, Fan AZ, et al. : Alternatives in assessing mental healthcare disparities using the behavioral risk factor surveillance system. Health Equity 2:199-206, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skarupski KA, Zack MM, Bienias JL, et al. : The relationship between mentally unhealthy days and depressive symptoms among older adults over time. J Appl Gerontol 30:241-253, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17a.Centers for Disease Control and Prevention (CDC): Behavioral risk factor surveillance system survey data, Department of Health and Human Services, Atlanta, GA. 2015 [Google Scholar]
- 18.Goren A, Gilloteau I, Lees M, et al. : Quantifying the burden of informal caregiving for patients with cancer in Europe. Support Care Cancer 22:1637-1646, 2014 [DOI] [PubMed] [Google Scholar]
- 19.Jones SB, Whitford HS, Bond MJ: Burden on informal caregivers of elderly cancer survivors: Risk versus resilience. J Psychosoc Oncol 33:178-198, 2015 [DOI] [PubMed] [Google Scholar]
- 20.Ornstein KA, Kelley AS, Bollens-Lund E, et al. : A national profile of end-of-life caregiving in the United States. Health Aff (Millwood) 36:1184-1192, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dionne-Odom JN, Applebaum AJ, Ornstein KA, et al. : Participation and interest in support services among family caregivers of older adults with cancer. Psychooncology 27:969-976, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merckaert I, Libert Y, Lieutenant F, et al. : Desire for formal psychological support among caregivers of patients with cancer: Prevalence and implications for screening their needs. Psychooncology 22:1389-1395, 2013 [DOI] [PubMed] [Google Scholar]
- 23.Mosher CE, Champion VL, Hanna N, et al. : Support service use and interest in support services among distressed family caregivers of lung cancer patients. Psychooncology 22:1549-1556, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanderwerker LC, Laff RE, Kadan-Lottick NS, et al. : Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol 23:6899-6907, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dionne-Odom JN, Azuero A, Lyons KD, et al. : Benefits of early versus delayed palliative care to informal family caregivers of patients with advanced cancer: Outcomes from the ENABLE III randomized controlled trial. J Clin Oncol 33:1446-1452, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rocque GB, Pisu M, Jackson BE, et al. : Resource use and Medicare costs during lay navigation for geriatric patients with cancer. JAMA Oncol 3:817-825, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clough JD, Kamal AH: Oncology care model: Short- and long-term considerations in the context of broader payment reform. J Oncol Pract 11:319-321, 2015 [DOI] [PubMed] [Google Scholar]
- 28.Girgis A, Lambert SD, McElduff P, et al. : Some things change, some things stay the same: A longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psychooncology 22:1557-1564, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Mosher CE, Given BA, Ostroff JS: Barriers to mental health service use among distressed family caregivers of lung cancer patients. Eur J Cancer Care (Engl) 24:50-59, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sautter JM, Tulsky JA, Johnson KS, et al. : Caregiver experience during advanced chronic illness and last year of life. J Am Geriatr Soc 62:1082-1090, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moriarty DG, Zack MM, Kobau R: The Centers for Disease Control and Prevention’s Healthy Days Measures: Population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 1:37, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]