Abstract
PURPOSE:
Patients report strong preferences regarding which provider—oncologist or primary care provider (PCP)—handles their primary care after initial cancer treatment (eg, other cancer screenings, preventive care, comorbidity management). Little is known about associations between provider involvement during initial cancer treatment and patient preferences for provider roles after initial treatment.
METHODS:
Women who received a diagnosis of early-stage breast cancer in 2014 to 2015 were identified from the Georgia and Los Angeles County SEER registries and surveyed (N = 2,502; 68% response rate). Women reported the level of their providers’ involvement in their care during initial cancer treatment. Associations between level of medical oncologist’s participation and PCP’s engagement during initial cancer treatment and patient preferences for oncologist led (v PCP led) other cancer screenings after initial treatment were examined using multivariable logistic regression models.
Results:
During their initial cancer treatment, 20% of women reported medical oncologists participated substantially in delivering primary care and 66% reported PCPs were highly engaged in their cancer care. Two-thirds (66%) of women preferred medical oncologists to handle other cancer screenings after initial treatment. Women who reported substantial medical oncologist participation in primary care were more likely (adjusted odds ratio, 1.42; 95% CI, 1.05 to 1.91) and those who reported high PCP engagement in cancer care were less likely (adjusted odds ratio, 0.41; 95% CI, 0.31 to 0.53) to prefer oncologist-led other cancer screenings after initial treatment.
Conclusions:
Providers’ involvement during initial cancer treatment may affect patient preferences regarding provision of follow-up primary care. Clarifying provider roles as early as during cancer treatment may help to better delineate their roles throughout survivorship.
INTRODUCTION
Improving the quality of survivorship care for the rapidly growing population of cancer survivors in the United States has been identified as a national priority.1,2 The services encompassing survivorship care are broad, ranging from cancer-related follow-up such as recurrence surveillance and monitoring for treatment late effects to providing more traditional primary care such as screening for other cancers, managing comorbidities, and performing routine health maintenance.2 National organizations have recommended team-based care models whereby oncologists (ie, cancer specialists) work together with primary care providers (PCPs) to provide this care.2,3 Although this model may help address the diverse health needs of cancer survivors, its implementation is challenging because of the lack of clarity around which provider—oncologist or PCP—should direct specific aspects of survivorship care.
In traditional models of survivorship care, oncologists routinely manage many aspects of their patient’s care. Though PCPs are well positioned to comanage care with oncologists, they remain underused during survivorship, and how to best incorporate them remains unclear. In fact, many patients prefer their oncologist to direct their primary care services after completion of their initial treatment.4,5 Several provider-level barriers exist to increasing PCP involvement during survivorship, including PCPs endorsing knowledge gaps about what survivorship entails and discordance in provider role preferences across PCPs and oncologists.6,7 The lack of structured care models to guide which provider should direct various aspects of survivorship care may contribute to physicians providing services outside the normal scope of their specialty and hinder the adoption of team-based cancer care models.
To support the successful adoption of team-based care models, however, patient preferences for which provider should manage aspects of their survivorship need to be considered. Therefore, the goal of this study was to examine factors associated with patients’ preferences for medical oncologists delivering primary care (ie, screening for other cancers, general preventive care, and comorbidity management) during survivorship. Using a large, population-based sample of women with early-stage breast cancer, we examined the association between medical oncologist and PCP involvement in care during initial cancer treatment and patients’ preferences for oncologist-led primary care in the first year after completing initial treatment (ie, during survivorship).
METHODS
Study Population
The Individualized Cancer Care Study (iCanCare) is a large, diverse, population-based survey study of women from 20 to 79 years old who received a new diagnosis of early-stage breast cancer in 2014 to 2015 and their providers.4,8 We performed secondary data analyses from the patient survey. Women were identified from the Georgia and Los Angeles County SEER registries (N = 3,930) and surveyed approximately 2 months after definitive surgery (n = 2,502; 68% response rate). We excluded women who did not have a PCP (n = 176) or medical oncologist (n = 313), because these are the providers who are primarily involved in the survivorship care of patients with early-stage breast cancer. Therefore, included in this analysis are data from the 2,053 women who identified having a medical oncologist and PCP at the time of survey. We provided a $20 cash incentive and used a modified Dillman approach to patient recruitment, including reminders to nonrespondents.9 The study was approved by the University of Michigan institutional review board.
Measures
As previously described, questionnaire content was developed on the basis of a conceptual framework, research questions and hypotheses, reported literature, and our prior work.8,10
Independent variables: provider involvement in care during initial cancer treatment.
Provider involvement during initial cancer treatment encompassed two distinct measures: (1) oncologist participation in primary care unrelated to the patient’s breast cancer, and (2) PCP engagement in cancer care.
Oncologist participation in primary care unrelated to the patient’s breast cancer.
To report the extent of their oncologist’s participation in primary care unrelated to their breast cancer during initial treatment, respondents were asked to answer how frequently (on a 5-point Likert scale from “never” to “a lot”) their cancer physicians had done any of the following: written a prescription for a problem other than breast cancer, given a referral to another specialist for something unrelated to breast cancer, and ordered a test for something other than breast cancer. We averaged responses from each of the three items and dichotomized scores to reflect oncologists’ '“never” or “rarely” (little participation, score < 3) versus “sometimes,” “often,” or “a lot” (ie, substantial participation, score ≥ 3) participating in primary care during initial treatment.
PCP engagement in cancer care.
Respondents were asked to report their perception of the extent of their PCP’s engagement in cancer care during initial treatment.11 Respondents were asked, “In the past 6 months, how often did your PCP seem informed and up-to-date about the care you got from your breast cancer doctors?” Responses were reported on a 5-point Likert scale (ranging from “never” to “always”) and dichotomized into low (ie, “never,” “rarely”; score < 3) versus high (ie, “sometimes,” “almost always,” and “always”; score ≥ 3) engagement for analyses.8
Dependent variable: patient preferences for oncologist-led primary care after initial treatment.
Respondents indicated their preferences for the role of oncologists and PCPs in delivering three aspects of their primary care after initial treatment, chosen to reflect care that is routinely managed by PCPs: (1) screening for other cancers, (2) general preventive care (eg. vaccinations, check-ups), and (3) management of comorbidities (eg, diabetes, heart disease). For each of the three aspects, respondents were asked, “After your initial cancer treatment is finished, which doctor would you prefer to see for each of the following?” The response categories included “Prefer primary care provider,” “Prefer cancer doctor” (ie, oncologist), “Either one is fine,” or “Prefer to see both.”
Given our interest in understanding patients’ preferences for oncologists managing care routinely provided by PCPs, responses were categorized as oncologist led versus PCP led (PCP/either/both). We then created a summary score to reflect patients’ overall preference for oncologist-led primary care after initial treatment; the score was based on if the patient preferred oncologist-led care for any one of the three primary care services. However, because the distribution of this summary score was mostly driven by patient preference for oncologist-led other cancer screenings, we focused on this aspect of primary care only as our primary outcome for analysis.
Covariables.
Covariables included patient-reported demographic characteristics, including age at diagnosis, race/ethnicity, education, insurance status, and SEER study site. Patient-reported clinical characteristics included number of comorbidities (including heart disease, chronic obstructive pulmonary disease, diabetes, blood clots, connective tissue disease, stroke, and depression) and receipt of breast cancer treatment (including surgery, chemotherapy and endocrine therapy).
We included three additional measures obtained from the survey that, on the basis of our conceptual framework, likely influence provider-role preferences during survivorship. Continuity with their PCP was determined by asking respondents, “How long have you been seeing your primary care provider?” Frequency of visits to their PCP was determined by asking respondents “How many times have you seen your PCP since your cancer diagnosis?” Worry about recurrence was determined by asking respondents to indicate how often they worried about their cancer coming back in the past month (on a 5-point Likert scale, ranging from “almost never” to “almost always”), with responses dichotomized to frequent (corresponding to “sometimes,” “often,” and “almost always”; score ≥ 3) versus less worry (corresponding to “almost never” and “rarely”; score < 3).
Statistical Analysis
Patient demographic and clinical characteristics were summarized using basic descriptive statistics. The distribution of patient preference for oncologist-led other cancer screenings after initial treatment was estimated using weighted proportions. Using Rao-Scott χ2 tests, we compared patient preference for oncologist-led other cancer screenings after initial treatment by provider involvement (ie, oncologist participation in primary care unrelated to their breast cancer and PCP engagement in cancer care) during initial cancer treatment. We then used multivariable logistic regression models to examine the association between patient preference for oncologist-led other cancer screening after initial treatment and provider involvement in care during initial cancer treatment, adjusting for age, race, insurance, education, SEER site, comorbidity, type of treatment, PCP continuity, PCP frequency, and recurrence worry.
We performed multiple sensitivity analyses to confirm the robustness of our results. We examined the outcome as the original four-level response variable and recategorized it in different ways from that described in the previous paragraphs (eg, oncologist-led v PCP-led care or care by both, excluding those with preference for either to lead care). Our results were largely similar (four-level response: oncologist-led odds ratio [OR] [95% CI] for cancer screening: 1.82 [1.01 to 3.28]; general preventive care OR, 2.47 [1.48 to 4.12]; comorbidity management OR, 5.28 [2.82 to 9.87]). Although we focused on preferences for oncologist-led other cancer screenings as the main primary outcome for our models for reasons described earlier in Methods, we also assessed associations between provider involvement (ie, oncologist participation in primary care and PCP engagement in cancer care) and patients’ preferences for overall primary care, general preventive care, and comorbidity management. Results from these sensitivity analyses all yielded similar results.
All statistical analyses incorporated weights to allow our statistical inference to be more representative of the target population and to reduce potential bias as a result of nonresponse.12-14 All analyses were performed by using SAS, version 9.4 (SAS Institute, Cary, NC).
RESULTS
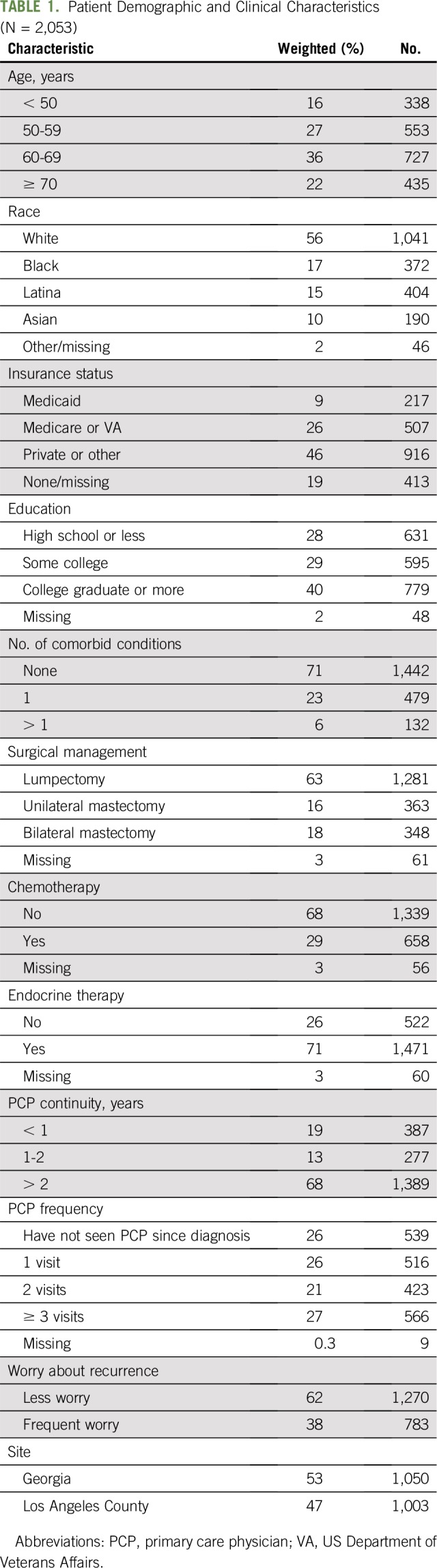
Table 1 describes our sample characteristics. Twenty percent of patients reported their oncologist substantially participated in primary care unrelated to their breast cancer during initial treatment: 26% of patients reported their oncologists wrote prescriptions for conditions unrelated to breast cancer, 18% reported their oncologists ordered tests for conditions other than their breast cancer, and 16% reported their oncologist referred them to other specialists for conditions other than their breast cancer. Two-thirds of patients (66%) reported their PCPs were highly engaged in their cancer care during treatment.
TABLE 1.
Patient Demographic and Clinical Characteristics (N = 2,053)
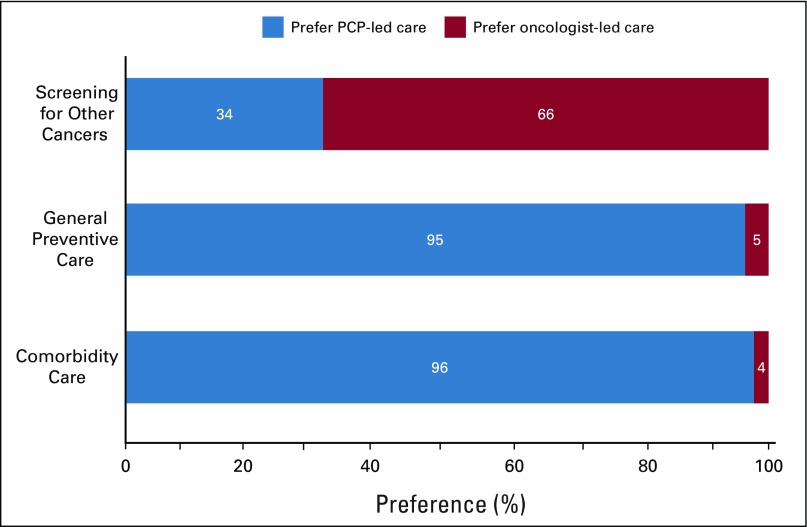
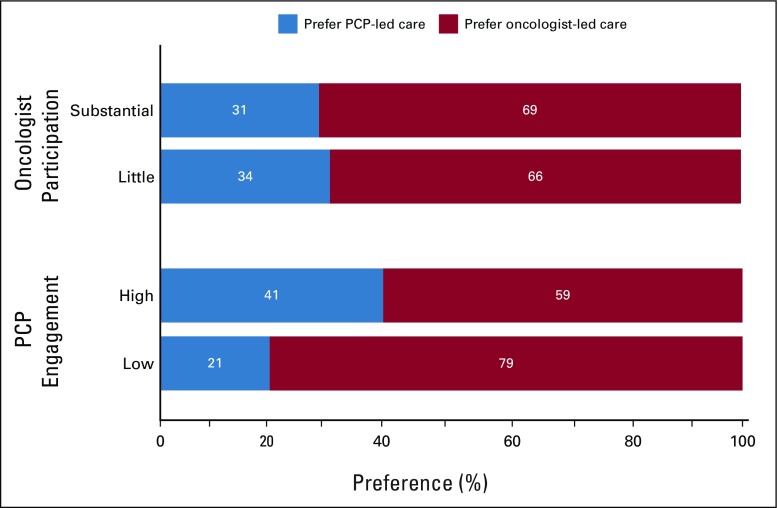
Most women (66%) preferred their oncologist to screen for other cancers after initial treatment, whereas only a very small minority preferred their oncologist to provide general preventive care (5%) and manage their comorbidities (4%; Fig 1). Oncologist participation in primary care unrelated to the patient’s breast cancer during initial treatment was not significantly associated with patient preferences for oncologist-led other cancer screenings after initial treatment (Fig 2). However, patients who reported high PCP engagement in cancer care during initial treatment were less likely to prefer oncologist-led other cancer screenings after initial treatment (59% v 79% low PCP engagement). Associations between provider involvement during initial cancer treatment and patient preferences for oncologist-led primary care after initial treatment using other the categories overall primary care and general preventive and comorbidity management are presented in Appendix Fig A1 (online only).
Fig 1.
Patient preferences for provider roles in delivering primary care after initial treatment. PCP, primary care provider.
Fig 2.
Patient preferences for oncologist-led other cancer screening after initial treatment by level of oncologist participation in primary care and PCP engagement in cancer care during initial cancer treatment. PCP, primary care provider.
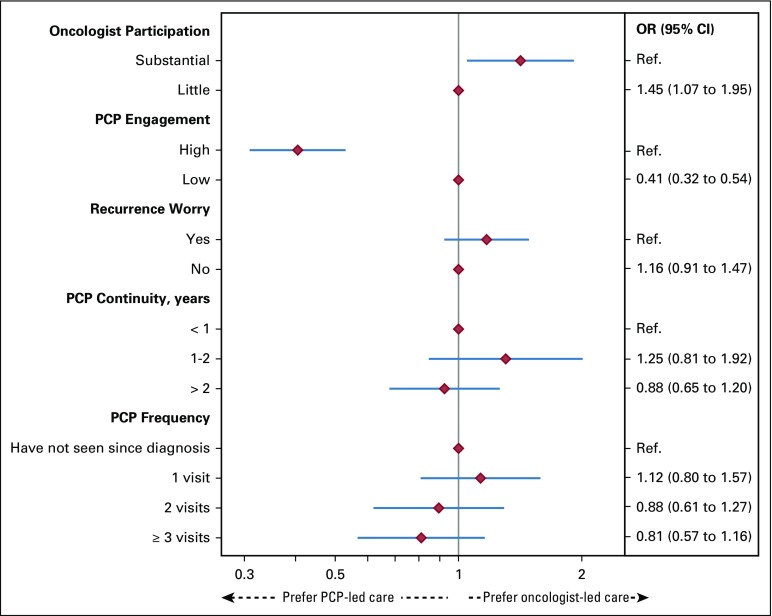
Figure 3 displays multivariable-adjusted associations between provider involvement in care during initial cancer treatment and patient preferences for oncologist-led other cancer screenings after initial treatment. Substantial oncologist participation in primary care unrelated to patients’ breast cancer during initial treatment was significantly associated with increased odds of women preferring oncologist-led other cancer screenings after initial treatment (adjusted OR, 1.45; 95% CI, 1.07 to 1.95). In contrast, high PCP engagement in cancer care during initial treatment was significantly associated with decreased odds of women preferring oncologist-led other cancer screenings after initial treatment (adjusted OR, 0.41; 95% CI, 0.32 to 0.54). Models examining overall primary care, general preventive care, and comorbidity care yielded similar results (data not shown).
Fig 3.
Adjusted odds ratio (95% CI) of patient preference for oncologist-led other cancer screenings after initial treatment associated with provider involvement in care during initial cancer treatment. PCP, primary care provider; Ref., referent.
DISCUSSION
In our large, population-based cohort of women with early-stage breast cancer, the majority of women preferred their oncologist to lead their screening for other cancers after initial cancer treatment. This finding was notable given that cancer screening is a service typically managed by PCPs. We also found that preferences for oncologist-led other cancer screenings after initial treatment were strongly associated with how involved providers were during initial cancer treatment; patients reporting substantial oncologist participation in primary care unrelated to their breast cancer during initial treatment were more likely to prefer their oncologists to lead screening for other cancers after initial treatment, whereas those reporting high PCP engagement in cancer care during initial treatment were less likely to do so. Our results suggest that clarity in provider roles for delivering various aspects of follow-up care after initial cancer treatment is needed; however, discussions among providers and patients may need to be initiated during primary treatment itself.
Research from our group has demonstrated significant variation across patient race and education for preferences for oncologists to lead certain aspects of breast cancer survivorship care.4 Our current findings extend this work by examining the influence of provider involvement during initial treatment on patient preferences for which provider delivers their primary care after initial treatment. Similar to prior research, a notable minority of women in our study reported their oncologists were substantially participating in their primary care unrelated to their breast cancer during their cancer treatment.15 It may be that increased frequency of visits with oncologists during treatment facilitates both discussion and follow-up of any of the patient’s needs and concerns. This may lead patients to expect their oncologist, not their PCP, to continue providing these types of primary care services after their initial treatment is finished. The overlap in provider roles during treatment—such as when oncologists are delivering primary care services—may make it difficult for patients to perceive transitioning this care back to their PCP after treatment. As increasing efforts in cancer care delivery focus on how to optimize models of team-based survivorship care, interventions that promote effective and coordinated shared care between oncologists and PCPs, such that patients receive noncancer care (ie, primary care) services from their PCP during treatment, are increasingly necessary.
Women in our study who perceived high PCP engagement in cancer care during initial treatment were less likely to prefer oncologists lead screening for other cancers after initial treatment. However, it is notable that greater than 33% of women in our sample perceived their PCPs had low engagement during treatment, a result complementary to studies of PCPs who report limited involvement during treatment.16 Our models accounted for duration of the patient’s relationship with their PCP and frequency of their visits, suggesting that a patient’s perceptions of PCP “engagement” may extend beyond office visits and rather be defined by the quality of the PCP’s involvement in cancer care. In a randomized controlled trial of shared care between general practitioners and cancer specialists, patients who visited their PCP during treatment did not have differences in their psychosocial outcomes, such as anxiety and depression.17 Taken together, these results suggest that to support PCP involvement in follow-up care after initial cancer treatment, efforts to promote high-quality and effective PCP engagement, and not just merely visiting their PCP, are needed early and often during treatment.
Common barriers PCPs report to their involvement in cancer survivorship care include lack of expertise or formal training and poor communication from oncologists regarding future management of patients’ cancers and goals of follow-up care.6,18,19 In addition, previous research suggests that PCPs perceive that patients lack trust in their ability to provide survivorship care and prefer, instead, specialist-led care.20,21 This perception is further supported by prior findings that suggest survivors who saw their oncologist for follow-up care reported lower stress and cancer-related worry compared with those who saw their PCP.5 Our findings also support this notion: More than two-thirds of women preferred their oncologist to screen for other cancers. Ramsay et al22 found that patients preferred to stay with their oncologists during survivorship; this may reflect patients having greater trust in their oncologist because of their repeated interactions while receiving treatment and perception that the oncologist is the expert in all aspects of cancer care, including screening. Though our survey questions did specifically differentiate between provider preferences for “screening for other cancers” and “follow-up for breast cancer (mammograms),” patients may not have discerned the difference in screening for other cancers from surveillance of their primary breast cancer and repeated education is needed regarding which services their oncologist and PCP can and should provide.
Implementing a team-based model of survivorship care that leverages both the strengths of oncologists and PCPs in delivering high-quality care, within the limitations of the time and workforce constraints of both specialties, remains a challenge. Our results suggest that efforts to clarify provider roles, as early as during initial treatment, may help bring clarity in provider responsibilities during survivorship. Supporting greater PCP engagement earlier in the cancer continuum may help facilitate communication between specialties and with patients about roles going forward and mitigate difficulties with coordination during survivorship. Likewise, efforts should target improving communication among providers and between providers and their patients about who will be managing the specific aspects of their cancer- and noncancer-related follow-up care. Oncologists should consider encouraging their patients to return to their PCP for care unrelated to their cancer diagnosis and/or treatment. Most women in our study did not have any comorbid conditions, and PCP engagement may be even more salient for women who have multiple medical comorbidities. Last, improving PCP knowledge about the specifics of follow-up care after cancer treatment will be critically important to promoting their involvement in survivorship care delivery going forward. This includes offering educational materials (eg, continuing medical education, journal clubs) and developing clinical practice guidelines particularly for PCPs.23,24
There are potential limitations that warrant comment. First, though we assessed patient preferences for provider roles after initial treatment, we do not yet know whether or how preferences will actually drive the use of services during this period. However, to the extent that preferences influence use, clarifying provider roles and which provider patients should see for aspects for their care after initial treatment is important. Second, we asked patients to report their preferences for provider roles within a year of their cancer diagnosis. It is possible that patient preferences for provider roles may evolve the longer it has been since their primary treatment. Third, we relied on patient self-report of their oncologist’s and PCP’s involvement during initial treatment. However, our questions targeted specific aspects of care and only asked about providers’ behaviors since diagnosis to facilitate more accurate recall by patients. Finally, as our population only includes patients with breast cancer in Los Angeles County and Georgia, generalizability to other populations may be limited.
In conclusion, the lack of clarity about provider roles in delivering follow-up care after initial cancer treatment has been a barrier to the implementation of team-based survivorship care. Our results underscore the importance of “upstream” factors (ie, provider involvement during cancer treatment) influencing patient preferences for provider roles during survivorship. Engaging PCPs earlier in the cancer continuum may help promote the transition of primary care services back to PCPs, resulting in optimal team-based models of care during survivorship.
ACKNOWLEDGMENT
Supported by Grant No. P01CA163233 to the University of Michigan from the National Cancer Institute (NCI) and Michigan Medicine Rogel Cancer Center Research Grant. L.P.W. is also supported by a career development grant from the NCI (Grant No. K07 CA201052). Cancer incidence data collection was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 5NU58DP003862-04/DP003862; the NCI’s SEER Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute. Cancer incidence data collection in Georgia was supported by contract HHSN261201300015I, Task Order HHSN26100006 from the NCI and cooperative agreement 5NU58DP003875-04-00 from the CDC.
Appendix
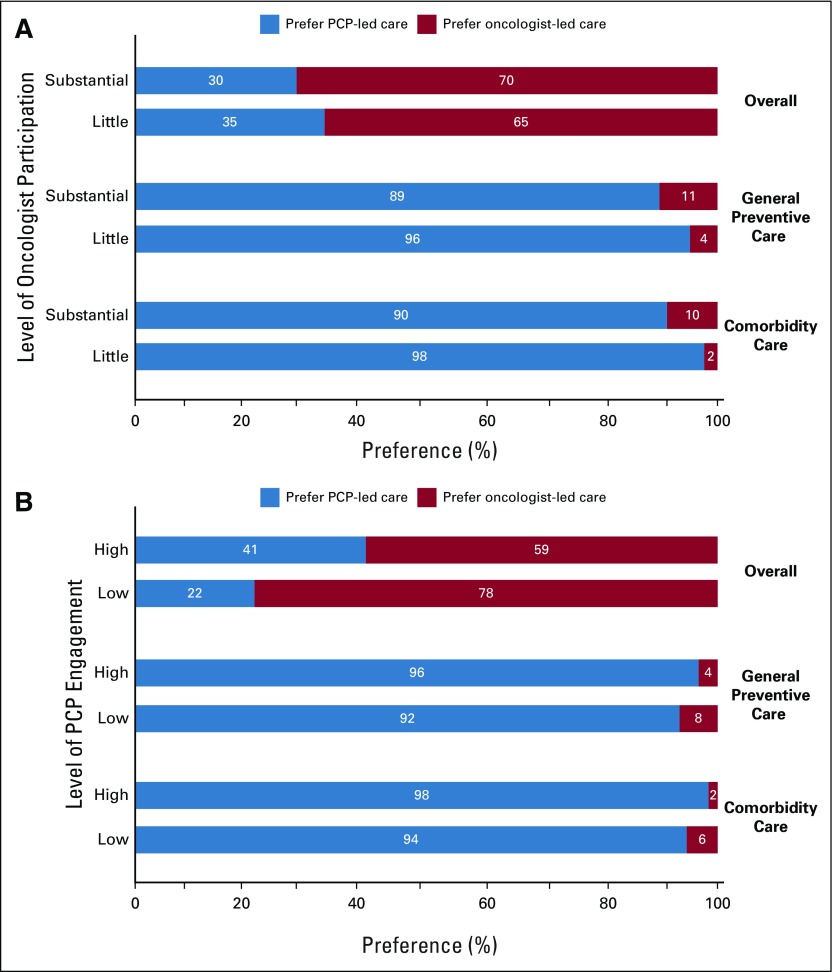
Fig A1.
Patient preferences for oncologist-led primary care services after initial treatment by level of (A) oncologist participation in primary care and (B) PCP engagement in cancer care during initial cancer treatment. PCP, primary care provider.
AUTHOR CONTRIBUTIONS
Conception and design: Archana Radhakrishnan, Steven J. Katz, Sarah T. Hawley, Lauren P. Wallner
Financial support: Steven J. Katz, Sarah T. Hawley
Administrative support: Steven J. Katz, Sarah T. Hawley, Lauren P. Wallner
Provision of study materials or patients: Ann S. Hamilton, Kevin C. Ward, Steven J. Katz, Sarah T. Hawley
Collection and assembly of data: Yun Li, Ann S. Hamilton, Kevin C. Ward
Data analysis and interpretation: Archana Radhakrishnan, Sarah T. Hawley, Lauren P. Wallner, Yun Li, Allison K.C. Furgal, Reshma Jagsi
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Provider Involvement in Care During Initial Cancer Treatment and Patient Preferences for Provider Roles After Initial Treatment
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Reshma Jagsi
Employment: University of Michigan
Stock and Other Ownership Interests: Equity Quotient
Consulting or Advisory Role: Amgen, Vizient
Research Funding: AbbVie (Inst)
Travel, Accommodations, Expenses: Amgen
Lauren P. Wallner
Research Funding: GlaxoSmithKline (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Centers for Disease Control and Prevention . A National Action Plan for Cancer Survivorship: Advancing Public Health Strategies. Atlanta: US Department of Health and Human Services; 2004. [Google Scholar]
- 2.Institute of Medicine, National Research Council . From Cancer Patient to Cancer Survivor. Washington, DC: National Academies Press; 2005. [Google Scholar]
- 3.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallner LP, Li Y, Furgal AKC, et al. Patient preferences for primary care provider roles in breast cancer survivorship care. J Clin Oncol. 2017;35:2942–2948. doi: 10.1200/JCO.2017.73.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayer EL, Gropper AB, Neville BA, et al. Breast cancer survivors’ perceptions of survivorship care options. J Clin Oncol. 2012;30:158–163. doi: 10.1200/JCO.2011.36.9264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dossett LA, Hudson JN, Morris AM, et al. The primary care provider (PCP)-cancer specialist relationship: A systematic review and mixed-methods meta-synthesis. CA Cancer J Clin. 2017;67:156–169. doi: 10.3322/caac.21385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung WY, Aziz N, Noone A-M, et al. Physician preferences and attitudes regarding different models of cancer survivorship care: A comparison of primary care providers and oncologists. J Cancer Surviv. 2013;7:343–354. doi: 10.1007/s11764-013-0281-y. [DOI] [PubMed] [Google Scholar]
- 8.Wallner LP, Abrahamse P, Uppal JK, et al. Involvement of primary care physicians in the decision making and care of patients with breast cancer. J Clin Oncol. 2016;34:3969–3975. doi: 10.1200/JCO.2016.67.8896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dillman DA, Smyth JD, Christian LM. Internet, Phone, Mail, and Mixed-Mode Surveys: the Tailored Design Method. Hoboken, NJ: John Wiley & Sons; 2014. [Google Scholar]
- 10.Friese CR, Martinez KA, Abrahamse P, et al. Providers of follow-up care in a population-based sample of breast cancer survivors. Breast Cancer Res Treat. 2014;144:179–184. doi: 10.1007/s10549-014-2851-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services, Agency for Healthcare Research and Quality: CAHPS patient-centered medical home (PCMH) item set.http://www.ahrq.gov/cahps/Surveys-Guidance/Item-Sets/PCMH/index.htmlAccessed December 19, 2017
- 12.Kish L. Survey Sampling. Hoboken, NJ: Wiley Classics Library; 1995. [Google Scholar]
- 13.Groves RM, Fowler FJ, Jr, Couper MP, et al. Survey Methodology. 2nd ed. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- 14.Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software. Ann Arbor, MI, University of Michigan, 2002:1-73.
- 15.Klabunde CN, Haggstrom D, Kahn KL, et al. Oncologists’ perspectives on post-cancer treatment communication and care coordination with primary care physicians. Eur J Cancer Care (Engl) 2017;26:e12628. doi: 10.1111/ecc.12628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lawrence RA, McLoone JK, Wakefield CE, et al. Primary care physicians’ perspectives of their role in cancer care: A systematic review. J Gen Intern Med. 2016;31:1222–1236. doi: 10.1007/s11606-016-3746-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson CE, Saunders CM, Phillips M, et al. Randomized controlled trial of shared care for patients with cancer involving general practitioners and cancer specialists. J Oncol Pract. 2015;11:349–355. doi: 10.1200/JOP.2014.001569. [DOI] [PubMed] [Google Scholar]
- 18.Rubinstein EB, Miller WL, Hudson SV, et al. Cancer survivorship care in advanced primary care practices: A qualitative study of challenges and opportunities. JAMA Intern Med. 2017;177:1726–1732. doi: 10.1001/jamainternmed.2017.4747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis RA, Neal RD, Hendry M, et al. Patients’ and healthcare professionals’ views of cancer follow-up: Systematic review. Br J Gen Pract. 2009;59:e248–e259. doi: 10.3399/bjgp09X453576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roorda C, Berendsen AJ, Haverkamp M, et al. Discharge of breast cancer patients to primary care at the end of hospital follow-up: A cross-sectional survey. Eur J Cancer. 2013;49:1836–1844. doi: 10.1016/j.ejca.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 21.Del Giudice ME, Grunfeld E, Harvey BJ, et al. Primary care physicians’ views of routine follow-up care of cancer survivors. J Clin Oncol. 2009;27:3338–3345. doi: 10.1200/JCO.2008.20.4883. [DOI] [PubMed] [Google Scholar]
- 22.Ramsay JM, Mann K, Kaul S, et al. Follow-up care provider preferences of adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol. 2018;7:204–209. doi: 10.1089/jayao.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nekhlyudov L, O’Malley DM, Hudson SV. Integrating primary care providers in the care of cancer survivors: Gaps in evidence and future opportunities. Lancet Oncol. 2017;18:e30–e38. doi: 10.1016/S1470-2045(16)30570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skolarus TA, Wolf AMD, Erb NL, et al. American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J Clin. 2014;64:225–249. doi: 10.3322/caac.21234. [DOI] [PubMed] [Google Scholar]