Abstract
PURPOSE
Worldwide, more than 80% of people diagnosed with cancer will require surgery during their disease course, but only 5% to 20% of low- and middle-income countries have access to safe, affordable, and timely surgery. Developing surgical oncology skills requires significant time and mentoring. Virtual reality (VR) simulators can reduce the time required to master surgical procedures but are prohibitively expensive. We sought to determine whether a VR simulator using low-cost computer gaming equipment could train novice surgeons in Africa to perform a virtual radical abdominal (open) hysterectomy (RAH).
METHODS
Our RAH VR simulator used the Oculus Rift (Oculus VR, Menlo Park, CA), a VR headset with hand controllers that costs less than $1,500. Surgical novices learned to perform five key steps of a virtual RAH. We measured and identified predictors of movement and time efficiency for the simulation.
RESULTS
Ten novice surgeons in Lusaka, Zambia, enrolled in the study. Movement and time efficiency greatly improved over time. Independent predictors of movement efficiency were number of simulations, surgical experience, and time since college graduation. Independent predictors of time efficiency were number of simulations, surgical experience, days between simulation sessions, age, sex, and an interaction between number of simulations and surgical experience.
CONCLUSION
Low-cost VR may be an effective tool to help surgical novices learn complex surgical oncology procedures. If learning to perform VR surgical procedures with low-cost hardware leads to faster mastery of surgical procedures in the operating room, low-cost VR may represent one of the solutions to increasing access to surgical cancer care globally.
INTRODUCTION
Cancer is the second leading cause of death in the world and is projected to increase at a staggering rate.1 Of the 15.2 million new patients diagnosed with cancer each year, more than 80% will require surgery at least once during the course of their disease.2,3 Less than 5% of low-income countries and only 20% of middle-income countries are able to provide basic cancer surgery as a result of human resource deficiencies and other health care infrastructure weaknesses.3
Context
Key Objective
Can low-cost virtual reality (VR) simulators help train surgeons in low-resource settings perform cancer surgery?
Knowledge Generated
We created a VR simulator using the Oculus Rift (Oculus VR, Menlo Park, CA), a VR headset with hand controllers that are commercially available and cost less than $1,500. Surgical trainees in Zambia learning to perform a virtual radical hysterectomy showed significant improvement in movement and time efficiency over time. The system was robust and worked effectively under local conditions in a Zambian teaching hospital.
Relevance
Low-cost VR may be an effective tool to help surgical novices learn complex surgical oncology procedures, regardless of setting. If learning to perform surgical procedures using low-cost VR hardware leads to faster mastery of surgical procedures in the operating room, low-cost VR may represent one of the solutions to increasing access to surgical cancer care globally.
Radical abdominal hysterectomy (RAH) is a surgical procedure central to the treatment of early-stage invasive cancer of the cervix, a disease whose burden is greatest in the world’s poorest countries.2,4 Few surgeons in these settings have formal training to perform this procedure. Two of the major challenges in developing surgical oncology capacity is the time required to train surgeons and the availability of mentors.
Virtual reality (VR) simulators hold promise in helping to ameliorate the shortage of surgeons. Research on simulator-based training conducted in developed countries has found that VR simulators can reduce the time required to develop surgical proficiency in the operating room.5-8 The VR simulator aims to create pretrained novices by helping them acquire the psychomotor skills, sensory acuity, and cognitive planning required to achieve the surgical dexterity necessary to perform complex surgical tasks.9,10 VR simulations may accelerate the development of surgical skills.
Surgical trainees randomly assigned to VR training before performing laparoscopic cholecystectomy made fewer errors, performed the procedure faster, and required only half the time to reach the skill level of intermediately skilled surgeons as those randomly assigned to standard training.6,11 In addition, some studies have shown that skills acquired during VR surgical simulations may successfully transfer to the operating room.5,12
The adoption of VR to train surgeons in lower-resource settings is limited as a result of the cost of the technology and the availability of surgical simulations relevant to lower-resource countries. The hardware and software to run these simulations can cost hundreds of thousands of dollars and require skilled technicians to maintain them in working order.10 The high cost makes these simulations infeasible to support surgical training in lower-resource settings. In addition, most VR surgical simulators have been developed and rigorously evaluated to train surgeons on laparoscopic or robotic procedures rather than on the open surgical producers commonly performed in lower-resource countries. We sought to determine whether a VR surgical simulator using inexpensive computer gaming equipment would be effective in enhancing the skills of surgical trainees learning to perform a virtual open RAH.
METHODS
Study Design
The study used an iterative user-centered design process to develop a virtual RAH simulation. The construct validity of the simulator was then rigorously evaluated with surgical trainees in Lusaka, Zambia. All research was performed after review and approval by the relevant human participants review boards.
Participants
Participants in the VR design process were gynecologic oncologists and gynecologic trainees in the United States and Zambia. Participants in the simulation evaluation were senior medical students and resident trainees in obstetrics and gynecology and a fellow in gynecologic oncology at University Teaching Hospital–Women and Newborn Hospital in Lusaka, Zambia.
VR Platform
We designed the VR platform to work efficiently with standard, affordable, and commercially available VR hardware (Oculus Rift; Oculus VR, Menlo Park, CA) and software (Unreal Engine; Epic Games, Cary, NC) to provide high-quality visuals and believable surgeon hand interactions. We created near identical VR reproduction of an operating room using 1:1 scale matching the elements of an actual surgical theater in a typical large district hospital in Lusaka, Zambia, including the equipment, instruments, supplies, and sounds.
We constructed the human female pelvic internal anatomy in three dimensions, with particular attention to realism to simulate organs, peritoneum, connective tissue, and vascular structures. The artwork contained appropriate rigging to allow surgeons to manipulate, clamp, cut, and suture. We designed the scene lighting to simulate visibility in a standard operating room environment. To make the simulation as visually realistic as possible as well as efficient, we designed the main surgical field to run at a frame rate of 120 frames per second and all else at greater than 60 frames per second.12a
Multiple hand positions were simulated using Oculus Touch hardware. Left and right hands were modeled for the user to interact within the environment in a realistic way. Surgical instruments were modeled for each of the instruments commonly used in the RAH procedure in Zambia.
The five sequential steps in the simulated RAH procedure were as follows: exposing the lateral pelvic retroperitoneal spaces; mobilizing the uterine artery over the ureter; mobilizing the ureter from the medial leaf of the broad ligament; unroofing the ureter; and dividing the uterosacral, cardinal, and vesicouterine ligaments. The procedure required a minimum of 39 actions that required the appropriate selection and use of six surgical instruments or materials and the appropriate use of hands. The simulation was designed and built by an interdisciplinary team consisting of an instructional designer, gynecologic oncologist, an artist, an interactions designer, and a health systems researcher working on the project part time for 9 months.
Training Intervention
Participants received standard didactic training on the RAH procedure currently available in the institution, which was augmented by RAH VR training. Standard RAH didactic training consisted of a 1-hour lecture by a senior gynecologic oncologist on the RAH surgical procedure. The lecture covered cervical cancer pathology and staging, pelvic anatomy, steps in the RAH procedure, and common intra- and postoperative complications. Participants also received individualized training on how to use the VR simulator. Finally, participants received copies of the didactic and VR training material in electronic written and video formats to refresh their memory as needed.
Within the virtual environment, participants could see and hear the sounds contained in a standard surgical suite. On a monitor above the patient in the virtual world, participants could read instructions on the step of the procedure they were to complete. Surgical instruments for each step of the simulated operation were automatically populated in random order on a tray within reach. Participants were required to know which instrument to select for each substep of the procedure they were about to commence because the simulator did not contain another virtual surgeon or nurse for assistance. If an incorrect surgical instrument was selected for a surgical step, the required action could not be performed. To continue, the participant had to recognize that he or she was using an incorrect instrument, place the incorrect instrument in an empty tray, and then select the correct instrument to proceed. The simulation did not simulate intraoperative complications caused by surgical errors, variations in anatomy or disease severity, or bleeding.
Throughout the simulation, participants received feedback on their progress and performance. At the completion of each successful substep, participants heard a distinctive chime, saw the visual field change to the next step, and received praise (“Yes,” “Good,” “That’s right”) from an audio file of the voice of the senior surgeon.
Each substep had movement and time targets to enable participants to gauge their performance and progress to a gold standard and to identify steps in the procedure they may wish to focus particular attention on in subsequent simulations. At the end of each simulation, participants received a summary screen with step-specific summary scores of their movements and time as well as a proficiency score, which was a composite of their movement and time scores.
The simulator was located in the hospital near the clinical wards for ease of access and was accessible from 9:00 am to 5:00 pm, Monday through Friday. Participants were encouraged to schedule as many simulation sessions as their time allowed and to complete up to six simulations each session. Participants were instructed to continue training on the simulator until they reached a proficiency score of 85 or higher five times in a row.
Measures
Demographic characteristics.
Before the standard training, all participants received a baseline interview administered by a trained research assistant. The baseline interview collected basic demographic data (age, sex, and educational history) and previous general surgical, gynecologic, and gynecologic oncology training received. Also collected from participants was information on the number of simple and radical hysterectomies in which they participated over the past year and over their lifetime, previous experience with surgical simulations and VR, and level of comfort with computers in general.
Procedural efficiency.
The VR simulator tracked all hand movements made by the participant during the simulation. The time of the beginning and end of each movement was also tracked. Procedural efficiency was evaluated by the two independent measures (movement and time) and one composite measure (a measure that incorporated both movement and time).
Movement efficiency score.
Each procedural step had a minimum number of hand movements with which the step could effectively be completed. On the basis of feedback received during beta testing, we adjusted the procedural accuracy goals to make them achievable over time by novices. For each step of the simulated procedure, participants received a movement efficiency score [(Goal number of hand movements/Actual number of hand movements) × 100].
Time efficiency score.
Time efficiency goals were based on the minimum amount of time needed to complete the simulation subsets by the developers who were experts in video gaming. For each step of the simulated procedure, participants received a time efficiency score [(Goal time to complete step/Actual time to complete step) × 100].
Self-assessment.
After each session, participants could view their efficiency subscores and were asked to identify the areas where improvement was needed and to reflect in writing on how they could improve in those areas.
Analyses
The data were cleaned and managed using R version 3.5.1.13 All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC). Time and movement values at each VR step that were extreme outliers (standardized residuals in the top 0.1%) were adjusted by multiple imputation of scores adjusted on the basis of the participant’s previous simulator performances.
To determine predictors of VR simulation performance, we considered the following two dependent measures of VR skill: movement efficiency and time efficiency. We performed generalized estimating equation modeling on each dependent variable to determine the independent effects of level of surgical experience, sex, years of medical training, previous knowledge, self-efficacy scores, number of previous VR simulations, and number of days since the last simulation session. Each participant’s skill scores were considered as a series of repeated measures. Because of the limited sample size, we assumed the covariance structure to be AR(1), in which only one parameter would be estimated.
RESULTS
Ten participants enrolled in the study, of whom eight were senior medical students, one was an obstetrics and gynecology resident, and one was a gynecologic oncology fellow. The average age of participants was 35.8 years (standard deviation, 5.8 years), 60% were men, and 40% were women. On average, participants had been in medical training for 6.7 years (standard deviation, 2.7 years). None of the senior medical students had ever completed or assisted in a simple or radical hysterectomy. The fellow had assisted with a radical hysterectomy.
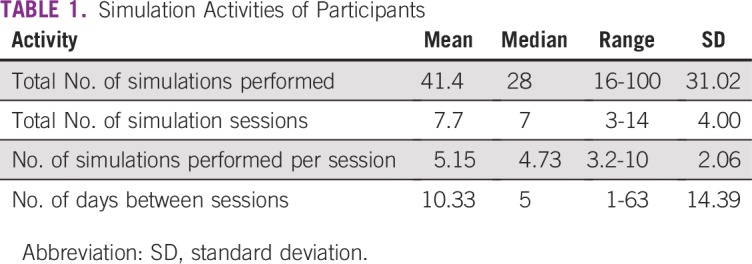
The participants used the simulator 7.7 times on average and performed an average of 5.15 simulations at each session. Table 1 lists the simulation activities of participants.
TABLE 1.
Simulation Activities of Participants
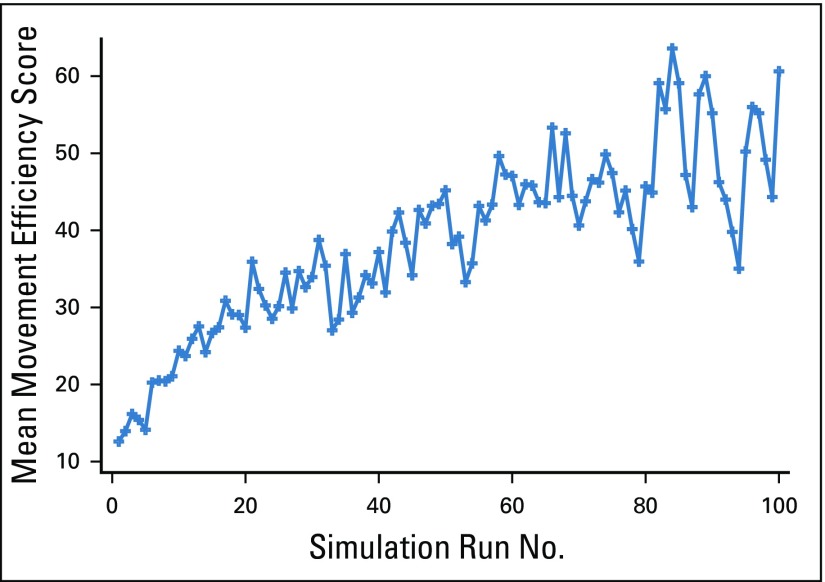
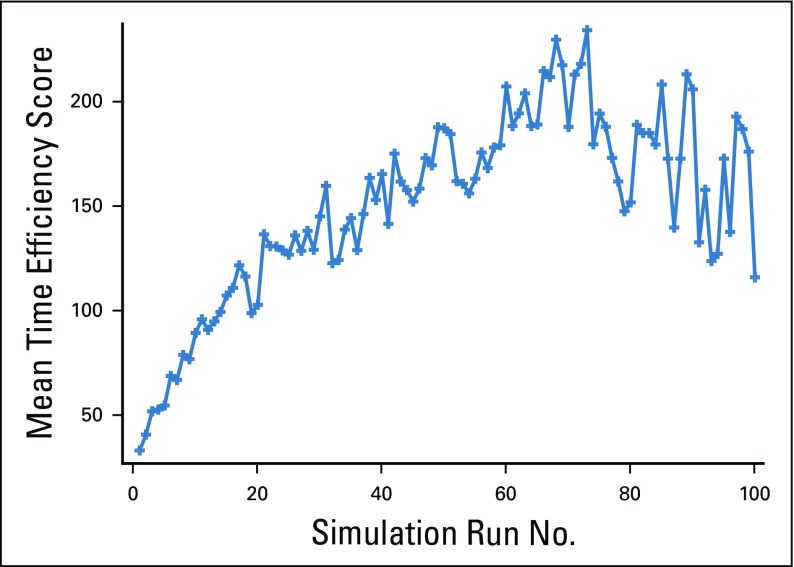
Movement efficiency (Fig 1) and time efficiency (Fig 2) of the participants increased over successive simulations and began to plateau at approximately 60 simulations. Fewer participants completed high numbers of simulations, and as result, there was greater variability at higher levels of simulations performed.
FIG 1.
Movement efficiency scores by simulation run number.
FIG 2.
Time efficiency scores by simulation run number.
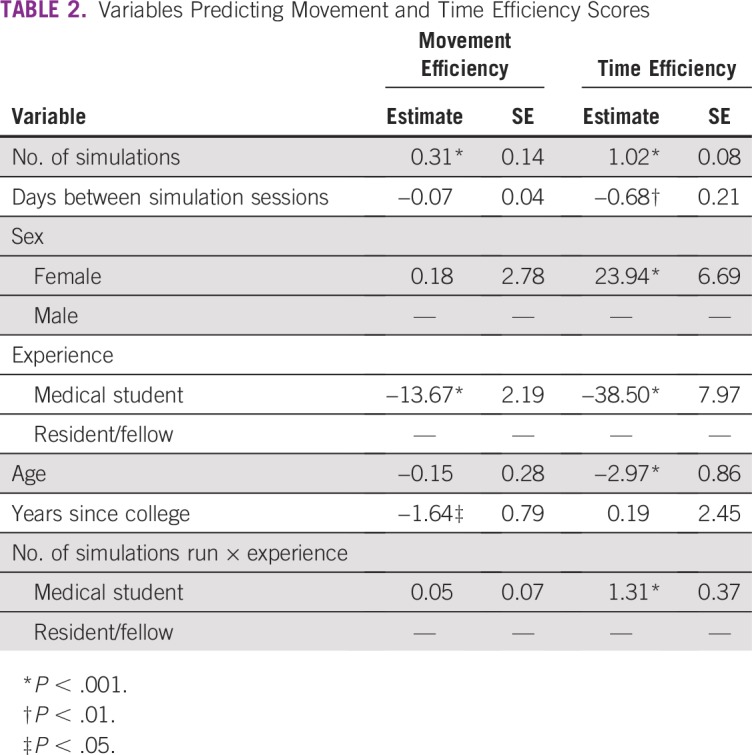
Movement efficiency was strongly and independently associated with the number of simulations performed, level of experience, and years since graduation (Table 2). Higher number of simulations completed, being a resident or fellow as opposed to a senior medical student, and recent graduation from college were all associated with higher levels of movement efficiency. Time efficiency showed a similar pattern; however, more variables were independently related to time efficiency. The more frequently the simulation was practiced and the fewer days that elapsed between sessions, the faster the participants performed the simulation. In addition, sex, previous surgical experience, and age were independently associated with greater time efficiency. Women, participants with a higher level of surgical experience, and younger participants were more time efficient than men, participants with less experience, and older participants, respectively. Furthermore, there was an interaction between number of simulations performed and experience level. Participants with less surgical experience became more time efficient with successive simulations than those with more surgical experience.
TABLE 2.
Variables Predicting Movement and Time Efficiency Scores
DISCUSSION
We have shown that a surgical simulator, using simple low-cost computer gaming equipment, can help surgical trainees in a lower-resource setting learn to perform a complex VR surgical oncology procedure. We designed the simulation to work using commercially available VR hardware and software that require minimal maintenance and support. The VR simulation runs offline, so it does not require high-speed Internet connections other than for installation and periodic maintenance. The research team in Zambia became self-sufficient after their initial training session on the VR equipment and simulations. During the study, we experienced few technical issues that required support because of the stability of the VR software and ease of operability and low maintenance of commercial VR technology.
As expected, movement and time efficiency were strongly associated with the number of simulations performed and the level of surgical experience. Time efficiency was also associated with age. We also found an unexpected interaction between number of simulations performed and surgical experience, with medical students showing more rapid improvement with successive simulations than residents or fellows. At least two interpretations might explain this finding—exposure to video games and deliberate practice.
Young people in developing countries, like those in developed countries, may have significant experience with video games and new media. Although there was no difference in reported number of years of experience with computers between medical students and residents or fellows, it is possible that the medical students had more experience with computer games. Such a finding would be consistent with a previous VR study that found that computer game users made fewer errors than nonusers on a VR laparoscopic surgery simulator.14 An alternative explanation relates to a modification that was made to the self-assessment portion of the study after the medical students had started practicing on the simulator but before the residents or fellows were recruited. At the end of each simulation session, participants were asked to complete a performance self-assessment. In the original self-assessment, participants were asked to reflect in writing on their overall performance during the session and to identify aspects they would like to remember and to improve upon during the next session. The self-assessment was revised to be more specific. In the revised self-assessment, participants were asked to review their performance on each of the five subsets in the procedure, to identify the specific substep where improvement was most needed, and to reflect in writing on how they might improve their performance during subsequent simulations. When the self-assessment form was changed, participant reflections for improvement tended to focus more on their need to carefully study pelvic anatomy and instrument placement before their next simulation session.
The self-assessment form modification was designed to strengthen motivation and engagement and allow participants to see the direct effect of focused effort on performance improvement. By having participants review objective performance feedback, identify substeps needing improvement, and finally, develop a performance improvement plan, we intended to stimulate deliberate practice. Deliberate practice techniques have been shown to reduce errors and the time to mastery for a wide range of surgical and medical procedures.15-20
The simulation was designed to be run with low-cost standard computer gaming equipment so that it may be more easily scaled in surgical training programs in lower-resource settings. Although a low-cost VR surgical simulation training platform may strengthen training in lower-resource settings, it may also have application in higher-resource settings. In a recent survey of US obstetrics and gynecology residency program directors, less than 50% felt that graduates entering subspecialty training programs had the surgical skills to independently perform a simple hysterectomy.21 Given the rapid adoption of minimally invasive surgical procedures (eg, laparoscopy, robotic surgery) in high-income countries, surgeons in these settings may have less experience performing open surgical procedures. This could have unintended adverse outcomes. A recent randomized clinical trial revealed that disease-free survival was superior for patients with cervical cancer who underwent open rather than minimally invasive radical hysterectomy.22,23 Our simulation may provide an efficient way to enhance learning and relearning of the open approach to this surgical procedure.
Future versions of the simulation could incorporate variations in disease severity, complications caused by surgical errors, and bleeding to strengthen procedural and surgical skills further. If learning to perform VR surgical procedures using low-cost hardware reduces time to master actual cancer surgery procedures, then low-cost VR simulation could be used to train cancer surgeons, could increase access to surgical cancer care globally, and could have wide application in medical and surgical education.
ACKNOWLEDGMENT
We gratefully acknowledge many people for their assistance in various aspects of the development and execution of this study, including Benjamin Chi; Kaitlyn Contreras Castro; George Hickey; Akihito Kamata, PhD; Afshan Kamrudin; Price Morgan; Lei Shi; and Lauren Shook at Southern Methodist University; Namakau Nyambe and Solomon Simalumba at University Teaching Hospital–Women and Newborn Hospital; and Jayanthi Lea, MD, at the University of Texas Southwestern Medical Center. In addition, we thank the many students and trainees at the University of Zambia, Southern Methodist University, and the University of Texas Southwestern Medical Center for their time, enthusiasm, and helpful feedback.
Footnotes
Supported by UK Research and Innovation Global Challenges Research Fund (GCRF) Grant No. ES/P010962/1, Medical Research Grant No. GCRF_Zambia_UK MR/P025420/1 (comparison of traditional v virtual simulation–enhanced training for scaling the cervical cancer surgery workforce in Zambia), and the Dedman College Interdisciplinary Institute and Center for Global Health Impact at Southern Methodist University.
Presented, in part, at the Toronto Global Cancer Control Conference, Toronto, Ontario, Canada, March 1-3, 2018, and the Union for International Cancer Control World Cancer Congress, Kuala Lumpur, Malaysia, October 1-4, 2018.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Administrative support: Eric G. Bing, Groesbeck P. Parham
Provision of study materials or patients: Eric G. Bing, Groesbeck P. Parham, Mulindi Mwanahamuntu
Collection and assembly of data: Eric G. Bing, Jonathan Skinner, Richard Sullivan
Data analysis and interpretation: Eric G. Bing, Jonathan Skinner, Richard Sullivan
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jgo/site/misc/authors.html.
Richard Sullivan
Honoraria: Pfizer
Consulting or Advisory Role: Pfizer (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: Delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16:1193–1224. doi: 10.1016/S1470-2045(15)00223-5. [DOI] [PubMed] [Google Scholar]
- 4.Torre LA, Islami F, Siegel RL, et al. Global cancer in women: Burden and trends. Cancer Epidemiol Biomarkers Prev. 2017;26:444–457. doi: 10.1158/1055-9965.EPI-16-0858. [DOI] [PubMed] [Google Scholar]
- 5.Banks EH, Chudnoff S, Karmin I, et al. Does a surgical simulator improve resident operative performance of laparoscopic tubal ligation? Am J Obstet Gynecol. 2007;197:541.e1–541.e5. doi: 10.1016/j.ajog.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 6.Coleman RL, Muller CY. Effects of a laboratory-based skills curriculum on laparoscopic proficiency: A randomized trial. Am J Obstet Gynecol. 2002;186:836–842. doi: 10.1067/mob.2002.121254. [DOI] [PubMed] [Google Scholar]
- 7.Grantcharov TP, Kristiansen VB, Bendix J, et al. Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg. 2004;91:146–150. doi: 10.1002/bjs.4407. [DOI] [PubMed] [Google Scholar]
- 8.Larsen CR, Grantcharov T, Aggarwal R, et al. Objective assessment of gynecologic laparoscopic skills using the LapSimGyn virtual reality simulator. Surg Endosc. 2006;20:1460–1466. doi: 10.1007/s00464-005-0745-x. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher A. 2018 Proficiency-based progression simulation training for more than an interesting educational experience. Musculoskelet Surg Res 2:139-141, [Google Scholar]
- 10.Gallagher AG, Ritter EM, Champion H, et al. Virtual reality simulation for the operating room: Proficiency-based training as a paradigm shift in surgical skills training. Ann Surg. 2005;241:364–372. doi: 10.1097/01.sla.0000151982.85062.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larsen CR, Soerensen JL, Grantcharov TP, et al. Effect of virtual reality training on laparoscopic surgery: Randomised controlled trial. BMJ. 2009;338:b1802. doi: 10.1136/bmj.b1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance: Results of a randomized, double-blinded study. Ann Surg. 2002;236:458–464. doi: 10.1097/00000658-200210000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12a.Parham G, Bing EG, Cuevas A, et al. Creating a low-cost virtual reality surgical simulation to increase surgical oncology capacity and capability. ecancer. 2019;13:910. doi: 10.3332/ecancer.2019.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.R Core Team R: A Language and Environment for Statistical Computing. https://cran.r-project.org/doc/manuals/r-release/fullrefman.pdf
- 14.Grantcharov TP, Bardram L, Funch-Jensen P, et al. Impact of hand dominance, gender, and experience with computer games on performance in virtual reality laparoscopy. Surg Endosc. 2003;17:1082–1085. doi: 10.1007/s00464-002-9176-0. [DOI] [PubMed] [Google Scholar]
- 15.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(suppl 10):S70–S81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 16.Kessler DO, Auerbach M, Pusic M, et al. A randomized trial of simulation-based deliberate practice for infant lumbar puncture skills. Simul Healthc. 2011;6:197–203. doi: 10.1097/SIH.0b013e318216bfc1. [DOI] [PubMed] [Google Scholar]
- 17.Nesbitt JC, St Julien J, Absi TS, et al. Tissue-based coronary surgery simulation: Medical student deliberate practice can achieve equivalency to senior surgery residents. J Thorac Cardiovasc Surg. 2013;145:1453–1459. doi: 10.1016/j.jtcvs.2013.02.048. [DOI] [PubMed] [Google Scholar]
- 18.Hsu JL, Korndorffer JR, Jr, Brown KM. Design of vessel ligation simulator for deliberate practice. J Surg Res. 2015;197:231–235. doi: 10.1016/j.jss.2015.02.068. [DOI] [PubMed] [Google Scholar]
- 19.Pukenas EW, Dodson G, Deal ER, et al. Simulation-based education with deliberate practice may improve intraoperative handoff skills: A pilot study. J Clin Anesth. 2014;26:530–538. doi: 10.1016/j.jclinane.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Palter VN, Grantcharov TP. 2014 Individualized deliberate practice on a virtual reality simulator improves technical performance of surgical novices in the operating room: A randomized controlled trial. Ann Surg 259:443-448, [Google Scholar]
- 21.Guntupalli SR, Doo DW, Guy M, et al. Preparedness of obstetrics and gynecology residents for fellowship training. Obstet Gynecol. 2015;126:559–568. doi: 10.1097/AOG.0000000000000999. [DOI] [PubMed] [Google Scholar]
- 22.Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- 23.Melamed A, Margul DJ, Chen L, et al. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905–1914. doi: 10.1056/NEJMoa1804923. [DOI] [PMC free article] [PubMed] [Google Scholar]