Abstract
Evidence suggests that early pubertal timing may operate as a transdiagnostic risk factor (i.e., shared across syndromes of psychopathology) for both genders. The current study examined associations between pubertal timing and dimensional psychopathology, structured across different levels of three organizational models: 1) DSM-based syndrome model, 2) traditional model of internalizing and externalizing factors, and 3) bifactor (p-factor) model, which includes a general psychopathology factor as well as internalizing- and externalizing- specific factors. For study analyses, 567 youth–parent pairs completed psychopathology measures when youth (55.5% female) were 13.58 (SD = 2.37, range = 9–17). Findings across all models revealed that early pubertal timing served as a transdiagnostic risk factor and also displayed some syndrome specific associations. Gender did not moderate any relationships between pubertal timing and psychopathology. Study findings reinforce the importance of examining risk across different levels of psychopathology conceptualization and analysis.
Pre-pubertal children have relatively low rates of psychiatric disorders; however, with the onset of puberty, rates of psychopathology climb sharply. A large body of evidence indicates that entering puberty earlier than one’s peers (i.e., early pubertal timing) increases risk for psychopathology (e.g., Dimler & Natsuaki, 2015; Mendle & Ferrero, 2012; Mendle, Turkheimer, & Emery, 2007). A recent meta-analysis found that early pubertal timing was equally associated with internalizing and externalizing syndromes (Ullsperger & Nikolas, 2017). Additionally, earlier age at menarche has been associated with internalizing (distress and fear) and externalizing disorders (Platt et al., 2017). This evidence suggests early pubertal timing may serve as a transdiagnostic risk factor consistent with the stage termination or maturational disparity hypothesis (Benoit, Lacourse, & Claes, 2013; Brooks-Gunn, Petersen, & Eichorn, 1985; Compas et al., 1995) of the association between pubertal timing and psychopathology, as early-maturing youth were found to be at higher risk of internalizing and externalizing syndromes. As much of the extant research has included and investigated only one specific DSM-defined disorder/syndrome at a time, whether early pubertal timing operates as a transdiagnostic risk (i.e., shared across syndromes) needs to be directly empirically examined.
Given recent critiques of the DSM nosology (e.g., Berenbaum, 2012; Frances & Widiger, 2012; Kotov et al., 2017; Kozak & Cuthbert, 2016; Uher & Rutter, 2012), there has been strong, renewed debate about the optimal approach to define, conceptualize, and assess psychopathology. Alternative approaches to the DSM have been proposed, including latent dimensional psychopathology models (e.g., Kotov et al., 2017; Sanislow, 2016). Presently, three organizational models are frequently used to represent and measure psychopathology across different granularity levels: 1) separate DSM-based syndromes (e.g., social anxiety, depression, ADHD), 2) a model of an internalizing and an externalizing factor (e.g., Achenbach, 1966), and 3) a bifactor model that includes a higher-order common psychology factor (the “p-factor”, Caspi et al., 2014) and two unique internalizing- and externalizing- specific factors representing variance independent of the p factor. In the current study, we evaluated how early pubertal timing relates to dimensionally assessed psychopathology across these organizational models.
Just as a microscope may be the most informative instrument for examining unicellular organisms and a telescope may be the most informative instrument for examining celestial bodies, the levels of the three models of psychopathology may be each useful for varying research objectives. Kotov and colleagues (2017) discuss the problem of selecting an appropriate “grain size” in the structure and conceptualization of psychopathology. They cogently argue that there is not necessarily a single correct grain size in psychopathology research; rather, the right choice of grain size may depend on the specific question being investigated. As pubertal timing has yet to be investigated as a predictor across the “grain sizes” or structural levels of these models of psychopathology, it is unknown how early pubertal timing will map onto each level, from the lower-order (e.g., discrete syndromes) to the higher order (e.g., p-factor) levels. Assessing only one level of a model, as is the current practice, may lead to incomplete inferences as researchers may conceptualize pubertal timing as a specific risk factor for particular disorders or syndromes, when it might better be characterized as a broader transdiagnostic risk factor (e.g., for all internalizing syndromes or for general psychopathology).
Pubertal timing in relation to different structural models of psychopathology
Much of the extant research on pubertal timing has been conducted with dimensional assessments based on diagnostic criteria of DSM disorders (Table 1). This research demonstrates robust and reliable evidence for early pubertal timing as a risk factor independently for depression as well as externalizing symptoms more broadly (Dimler & Natsuaki, 2015; Graber, 2013; Ullsperger & Nikolas, 2017). However, as Table 1 reveals, there have been few studies of some DSM-based syndromes (e.g., ADHD) during the pubertal transition, so the field lacks knowledge on how pubertal timing relates to some forms of psychopathology. In addition, many studies have examined the association between pubertal timing and one specific syndrome or set of symptoms at a time; as a result, multivariate relations between pubertal timing and multiple manifestations of psychopathology have not been systematically investigated, especially across different grain sizes.
Table 1.
Early pubertal timing as a risk factor for forms of psychopathology.
| Internalizing | Depression | Social Anxiety | Phy. Sx. | Externalizing | Aggression | ODD/CD | ADHD | Any Dx | |
| CATEGORICAL (diagnoses) | 9* 14*# | 18* | 9* 14*# | 9* 18** | |||||
| DIMENSIONAL (symptoms) | 1## 10*# 13* 21*# 22*# 26** 28* |
3** 6# 8* 11** 15* 16** 19* 23** 25** 27** 30** 31* 32## |
4** 5*# 11#* 16## |
1** 12** 6* 13* 21*# |
7** 15# 20** 28* 29* |
2** 17* 20** 24* 29* |
11** |
| 1. Arim & Shapka (2008) | 93 boys and 167 girls | ASEBA (Achenbach & Rescorla, 2001) | boys and girls, more externalizing (and not internalizing). |
| 2. Bakker et al. (2011) | 1,004 boys and 1,060 girls | parent-report on conflict with authorities | boys and girls, more conflict with authorities. |
| 3. Benoit et al. (2013) | 653 boys and 778 girls | CES-D (Radloff, 1977) | boys and girls, more depressive symptoms. |
| 4. Blumenthal et al. (2009) | 87 boys and 80 girls | RCADS-SP (Chorpita et al., 2000) | boys and girls, more social anxiety symptoms. |
| 5. Blumenthal et al. (2011) | 70 boys and 68 girls | RCADS-SP | girls, more social anxiety symptoms. no effects for boys. |
| 6. Carter et al. (2011) | 607 girls | CES-D; ODD as defined in CIDI (Kessler et al. 1998) | girls, more externalizing (and not depressive symptoms). |
| 7. Chen & Raine (2018) | 411 (51% boys) | CBCL; YSR ( Achenbach, 1991; Achenbach & Edelbrock, 1981) | boys and girls, more aggression. |
| 8. Conley et al. (2012) | 78 girls and 71 boys | KSADS-E (symptoms) (Orvaschel, 1995) | girls, more depressive symptoms. |
| 9. Copeland et al. (2010) | 630 girls | CAPA (Angold & Costello, 2007) | girls, greater risk of depression dx, conduct dx, any dx. |
| 10. Crockett et al. (2013) | 512 boys and 513 girls | CBCL; CDI; (Kovacs, 1992) | girls, more internalizing. boys, no effects. |
| 11. Ge et al. (2006) | 400 boys and 467 girls | DISC-IV (symptoms) (Shaffer et al. 2000) | boys and girls, higher depressive and ADHD symptoms. for boys (and not girls), higher social anxiety symptoms. |
| 12. Ge et al. (2002) | 400 boys and 476 girls | DISC-IV (symptoms) | boys and girls, more externalizing. |
| 13. Ge et al. (2001) | 202 boys | SCL-90-R (Derogatis, 1983) | boys, more internalizing and externalizing. |
| 14. Graber et al. (2004) | 92 boys, 539 girls | KSADS | girls, greater risk of MDD, ODD/CD dx. no effects for boys. |
| 15. Graber et al. (2006) | 100 girls | YSR | girls, more depressive symptoms. no effects for aggression. |
| 16. Hamlat et al. (2014) | 120 girls and 113 boys | CDI, MASC (March et al., 1997) | boys and girls, more depressive symptoms. no effects for social anxiety. |
| 17. Haynie (2003) | 5,477 girls | self-report on delinquency | girls, more delinquency. |
| 18. Jin et al. (2008) | 424 boys, 472 girls | DISC-IV | boys and girls, greater risk of any dx. |
| 19. Keenan et al. (2014) | 2450 girls | Childhood/Adolescent Symptom Inventory-Fourth Edition (Gadow & Sprafkin, 1997, 2008) | girls, more depressive symptoms. |
| 20. Lynne et al. (2007) | 629 boys and 737 girls | YSR; self-report of delinquency | boys and girls, more aggression and delinquency. |
| 21. Marceau et al. (2011) | 364 boys and 373 girls | CBCL; YSR | girls, more internalizing and externalizing. boys, no effects. |
| 22. Marceau et al. (2012) | 706 same-sex twin pairs (50% girls) and 687 same-sex twin/ sibling pairs (47% girls) | CBCL; YSR; CDI; CES-D | girls, more internalizing. boys, no effects. |
| 23. Mendle et al (2010) | 128 boys and 138 girls | CDI | boys and girls, more depressive symptoms. |
| 24. Mrug et al. (2008) | 330 girls | Problem Behavior Frequency Scale (Farrell et al. 1992) | girls, more delinquency. |
| 25. Nadeem & Graham (2005) | 534 boys and 676 girls | CDI | boys and girls, more depressive symptoms. |
| 26. Natsuaki et al. (2009) | 110 boys and 106 girls | symptom counts on DISC-IV | boys and girls, more internalizing symptoms. |
| 27. Rudolph & Troop- Gordon (2010) | 81 boys and 86 girls | KSADS-E (symptoms) | boys and girls, more depressive symptoms. |
| 28. Sontag et al. (2008) | 111 girls | YSR | girls, more internalizing and aggression. |
| 29. Susman et al. (2007) | 56 boys, 55 girls | DISC-IV; CBCL; Crick and Grotpeter’s (1995) Children’s Social Behavior Scale | boys, more conduct disorder symptoms. girls, more aggression. |
| 30. Teunissen et al. (2011) | 294 boys and 319 girls | CDI | boys and girls, more depressive symptoms. |
| 31. White et al. (2012) | 344 girls | DISC-IV (symptoms) | girls, more depressive symptoms. |
| 32. Winer et al. (2016) | 412, 45.4% girls | RCADS (Chorpita &Ebesutani, 2014) | boys and girls, no effects for depressive symptoms. |
Note: * = evidence for girls, * = evidence for boys, # = null evidence for girls, # = null evidence for boys.
Several studies have found early pubertal timing to be significantly associated with the broader constructs of internalizing or externalizing problems (Table 1). Structuring syndromes into two higher-order factors of internalizing and externalizing has been used to effectively model psychological symptoms in children and adolescents (e.g., Achenbach, 1966, Achenbach & Edelbrock, 1978). This “internalizing and externalizing” model allows each syndrome to load onto either the internalizing or externalizing factor and has been found to be stable across ages and populations (Krueger, 1999; Krueger, Caspi, Moffitt, & Silva, 1998, Krueger, Chentsova-Dutton, Markon, Goldberg, & Ormel, 2003). As DSM-based syndromes exhibit a high degree of comorbidity (Castellanos-Ryan et al., 2016), the “internalizing and externalizing” model may provide a more parsimonious and informative way to model the relationships between syndromes.
Internalizing and externalizing factors are usually found to be correlated and thus share common variance (meta-analysis found the correlation to be r = .50, Krueger & Markon, 2006); their covariance is directly accounted for in the bifactor model of psychopathology. In the bifactor model, all syndromes load onto a common latent factor (p factor) representing covariance among all syndrome factors, and each syndrome loads onto either an internalizing-specific or externalizing-specific factor. The bifactor model has been found to fit well with both diagnostic and symptom level data across many samples and age groups (e.g., Lahey et al., 2011; Snyder et al., 2017; Tackett et al., 2013; for reviews see Hankin et al., 2016; Lahey et al., 2017). Pubertal timing has yet to be examined as a risk factor in relation to the p-factor or the internalizing- and externalizing- specific dimensions of the bifactor model of psychopathology.
In addition, it is important to determine if the effects of timing at each structural level of psychopathology are moderated by gender. Early pubertal timing has been conceptualized as a risk factor primarily for girls and has been studied less often in boys (Graber, 2013; Negriff, Susman, & Trickett, 2011). Girls enter puberty earlier than boys (Dorn, Dahl, & Woodward, 2006) and may therefore experience the largest “developmental mismatch” between biological maturation and cognitive maturation (Graber, 2013). Girls who mature early may be unprepared to cope with the social and emotional pressures associated with pubertal development (e.g., dating, sexual attention from older boys), and this may lead to increases in psychopathology (Natsuaki, Samuels, & Leve, 2015). However, a recent meta-analysis found that early pubertal timing increases the risk of internalizing and externalizing problems similarly for both girls and boys (Ullsperger & Nikolas, 2017). Thus, further research is needed to clarify whether early pubertal timing confers risk similarly for boys and girls.
The present study
Recent reviews suggest that early pubertal timing may be best characterized as a transdiagnostic risk factor, yet this hypothesis has not been directly examined. By exploring how pubertal timing relates to alternative models of psychopathology, we can clarify which dimensions are significantly linked to early pubertal timing and so illuminate potential mechanisms of risk for early maturing youth. The current study examined the effects of pubertal timing on psychopathology, operationalized and structured across three models: 1) DSM-based syndrome model, 2) traditional model of internalizing and externalizing factors, and 3) bi- (p-) factor model, which includes the p-factor as well as internalizing- and externalizing- specific factors. In addition, we explored whether gender moderated each association between pubertal timing and psychopathology, as instantiated across these three models.
Method
Participants
Youth and a parent from the general community were recruited from the third, sixth, and ninth grades of public schools in the Denver and central New Jersey metro areas (for additional details on study, see Hankin et al., 2015). Inclusion criteria for participants included English fluency and that children did not have an autism spectrum disorder, psychosis, or intellectual/developmental disabilities. For the current analyses, 567 youth–parent pairs completed psychopathology measures at the second timepoint (18 months after study baseline) when youth were 13.58 (SD = 2.37, range = 9–17). The sample (55.5% female) was generally comparable to the ethnic and racial characteristics of the overall population of the United States, although there were relatively fewer Latina/o (12%) participants. Youth were 70% Caucasian, 12% African-American, 9% Asian/ Pacific Islander, and 9% other/multiracial. Median annual family income was $86,500, and 18.3% of participants received free/reduced lunch.
Measure of pubertal timing
The Pubertal Development Scale (PDS).
The PDS (Petersen, Crockett, Richards, & Boxer, 1988) is a six-item self-report questionnaire that assesses current pubertal development. The PDS has good psychometric properties and convergent validity based on self- and physician-rated Tanner stages (Petersen et al., 1988; Siegel, Yancey, Aneshensel, & Schuler, 1999). Each characteristic (except menstruation, which is coded 1 = has not begun, 4 = has begun) is rated on a 4-point scale (1 = no development, 2 = development has barely begun, 3 = development is definitely underway, 4 = development is complete). In the total sample, the average PDS score was 2.46 (SD = 0.64) and 2.4% of individuals reported scores of 4 indicating that development was complete. In the third grade, sixth grade, and ninth grade cohorts, average PDS scores were 1.94 (SD = 0.56), 2.43 (SD = 0.48), and 3.00 (SD = 0.37), respectively. Prior to conducting analyses, the PDS total score from child report was regressed on age separately for girls and boys, and the residual obtained was used as a continuous measure of pubertal timing (Dorn et al., 2006; Dorn, Susman, & Ponirakis, 2003; Hamlat et al., 2014). Larger values of the timing variable indicate more advanced pubertal status relative to (same-sex) others of the same age (i.e., earlier pubertal timing).
Syndrome-based measures
The Children’s Depression Inventory (CDI).
The CDI (Kovacs, 1992) is a 27-item measure designed to assess affective, behavioral, and cognitive symptoms of depression in youth ages 7 to 17, which demonstrates good reliability and validity (Klein, Dougherty, & Olino, 2005). Both parent and child report of the CDI were used in the current project. Internal consistency for child report and parent report were both 0.88.
The Multidimensional Anxiety Scale for Children (MASC).
The MASC (March, Parker, Sullivan, Stallings, & Conners, 1997) is a 39-item questionnaire assessing anxiety symptoms in youth. In current analyses, we used both parent and child report of MASC subscales of physical symptoms, social anxiety, and separation anxiety as these subscales have excellent retest and internal reliability and good convergent and discriminant validity (Baldwin & Dadds, 2007; Grills-Taquechel, Ollendick, & Fisak, 2008). Internal consistency for physical symptoms was 0.85 for child report and 0.84 for parent report, for social anxiety was 0.87 for child report and 0.88 for parent report, and for separation anxiety was 0.76 for child report and 0.79 for parent report.
Child Behavior Checklist (CBCL)/ Youth Self Report (YSR).
Subscales of the CBCL (parent report) and YSR (child report) from the Achenbach System of Empirically Based Assessment were used to assess symptoms of oppositional defiance disorder (ODD) and conduct disorder (CD). These DSM-based subscales have demonstrated good reliability and validity (Achenbach & Rescorla, 2001). Internal consistency for ODD was 0.66 for child report and 0.78 for parent report and for CD was 0.70 for child report and 0.78 for parent report.
Early Adolescent Temperament Questionnaire Revised (EATQ-R).
Both parent and child reports of the aggression scale of the EATQ-R (Ellis & Rothbart, 2001) were used to assess aggressive physical and verbal actions. This scale demonstrates good reliability and validity (Snyder et al., 2015). Internal consistency was 0.78 for child report and 0.74 for parent report.
Swanson, Nolan and Pelham Questionnaire (SNAP-IV).
To assess symptoms of inattention and hyperactivity, we used parent report of the NIMH Collaborative Multisite Multimodal Treatment Study of Children with Attention Deficit Hyperactivity Disorder (ADHD) version of the SNAP-IV, which has good reliability and validity (Swanson et al., 2001). Internal consistency for parent report was .94 for inattention and .90 for hyperactivity.
Statistical Analysis Plan
Structural equation modeling was conducted in Mplus v7.4 (Muthén and Muthén, 2012) using full information maximum likelihood (FIML) estimation to handle missing data. For all models, “good fit” was defined as RMSEA less than or equal to .06, confirmatory fit index (CFI) greater than or equal to .95, and SRMR less than or equal to .08. “Acceptable fit” was defined as RMSEA greater than or equal to .08 and CFI greater than or equal to .90 (Hu & Bentler, 1998, 1999). Akaike information criterion (AIC) and Bayesian information criterion (BIC) were used to determine the best fitting model (lower = better fit). With the exception of ADHD (parent only), both parent and child report of psychopathology were used in all models.
Structural models of psychopathology.
All models used identical measures as indicators; however, each model organized the structure of psychopathology differently. For example, in the bifactor model, the ADHD variables loaded onto the p-factor but not onto the externalizing-specific factor; similarly, in the two-factor model, the ADHD variables did not load onto the externalizing factor. In both of these models, all psychopathology measures (including ADHD) loaded onto the appropriate reporter factor and random intercept factor (which were orthogonal to all other factors). In all models, to account for variance related to reporter, parent reports and child reports of psychopathology were loaded onto parent and child reporter factors, respectively, and parent and child reports were also loaded onto a random intercept factor in all models.
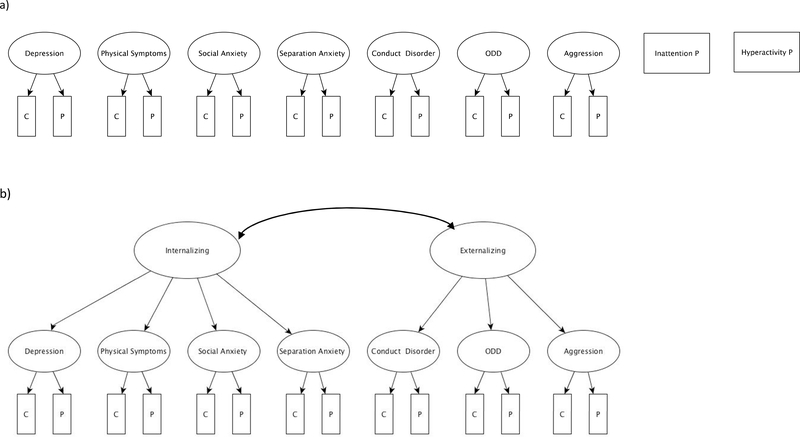
1). Syndrome-based dimensional model (Figure 1a).
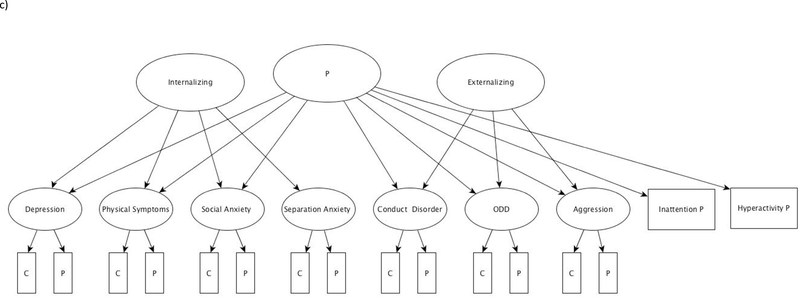
Figure 1.
a) Syndrome-based model without controls. All syndrome factors (and the two manifest variables of inattention and hyperactivity) were separately regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender. b) Internalizing and Externalizing model. In this model, internalizing and externalizing factors were regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender. c) P-factor model. In this model, the p-factor as well as the internalizing and externalizing factors were each regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender. Note: reporter and random intercept factors omitted for clarity in all models. ODD = Oppositional Defiant Disorder; C = child report; P= parent report.
Separate syndrome factors were constructed for depression, physical symptoms, social anxiety, separation anxiety, ODD, CD, and aggression, with both child and parent report of each syndrome constrained to load equally on its associated factor. Parent report of ADHD was measured by two separate manifest variables, representing the domains of inattention and hyperactivity. Two versions of the model were created: in the first version of the model, all syndrome factors and the two manifest variables of inattention and hyperactivity were regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender. In this version, all correlations between factors were constrained to zero and so did not allow any covariance between syndromes. In the second version of the model, we regressed each syndrome on our predictors (pubertal timing, gender, and their interaction) while controlling for the other syndromes in the regressions. This was done for the latent syndrome factors as well as the manifest variables of hyperactivity and inattention.
2). “Internalizing and Externalizing” model (Figure 1b).
Syndrome factors (as described in syndrome model above), were loaded onto factors that represent either the internalizing (i.e., depression, physical symptoms, social anxiety, separation anxiety) or externalizing factor (i.e., ODD, CD, aggression). As in Snyder et al., 2017, manifest variables of inattention and hyperactivity were not loaded onto the externalizing factor due to non-significant loadings. All correlations between syndrome factors were constrained to zero but internalizing and externalizing factors were allowed to covary with one another. Internalizing and externalizing factors were regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender.
3). P-factor model (Figure 1c).
The model had identical measures and specifications as the T1 model in Snyder et al., 2017. In addition to loading on either the internalizing or externalizing factor, all syndrome factors (except separation anxiety) were loaded onto a common factor, the p-factor. As in Snyder et al., 2017, the separation anxiety factor was not loaded onto the p-factor due to non-significant loading. Hyperactivity and inattention loaded only onto the p factor as neither loaded significantly on the externalizing-specific factor (as in the “internalizing and externalizing” model). ADHD variables loading significantly onto the p-factor but not onto the externalizing specific factor has been found in prior work (e.g., Martel et al., 2017; Snyder et al., 2017). All correlations between factors were constrained to zero so the p-factor as well as the internalizing- and externalizing- specific factors were all constrained to be orthogonal to each other (i.e., did not correlate with each other). The p-factor as well as the internalizing and externalizing factors were regressed upon pubertal timing, gender, and the interaction of pubertal timing and gender.
Results
The hypotheses, design, and analysis plan were preregistered at the Open Science Framework and can be accessed at https://osf.io/qgea2/. Psychopathology levels for the sample matched epidemiological studies (e.g., Kessler et al., 2012) as 24% of youth had experienced a depressive episode, 16.3% had a history of an anxiety disorder, 5.2% had clinical levels of ADHD symptoms, and 5.6% had clinical levels of conduct problems (Hankin et al., 2015; Snyder et al., 2017). Girls had higher levels of depression (β = .15, p =.03), physical symptoms (β = .24, p =.001), social anxiety (β = .35, p <.001), and separation anxiety (β = .22, p <.001), and boys had higher levels of inattention (β = .13, p <.001). See Table 2 for descriptive statistics and manifest correlations. Correlations showed expected magnitudes and directions of effect sizes across forms of psychopathology and informant/reporter.
Table 2.
Correlations between manifest indicator variables.
| Child Report | Parent Report | Mean | SD | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |||||
| Child Report | 1 | Depression | -- | .51 | .43 | .08 | .48 | .57 | .43 | .36 | .23 | .16 | −.04 | .14 | .14 | .21 | .13 | .17 | 5.27 | 5.86 |
| 2 | Physical Symptoms | -- | .52 | .39 | .32 | .34 | .31 | .18 | .28 | .10 | .13 | .08 | .05 | .07 | .05 | .09 | 6.44 | 5.73 | ||
| 3 | Social Anxiety | -- | .38 | .25 | .23 | .26 | .13 | .10 | .24 | .05 | −.01 | −.03 | .00 | −.10 | .00 | 7.53 | 5.79 | |||
| 4 | Separation Anxiety | -- | −.01 | −.07 | .03 | .01 | .12 | .17 | .46 | −.01 | −.03 | −.01 | .08 | .00 | 5.23 | 4.40 | ||||
| 5 | Oppositional Defiant Disorder | -- | .62 | .55 | .29 | .20 | .09 | −.06 | .30 | .25 | .20 | .15 | .21 | 2.12 | 1.89 | |||||
| 6 | Conduct Disorder | -- | .63 | .23 | .16 | .08 | −.09 | .24 | .30 | .19 | .08 | .25 | 2.71 | 2.59 | ||||||
| 7 | Aggression | -- | .20 | .15 | .08 | −.03 | .21 | .20 | .13 | .09 | .26 | 11.24 | 4.08 | |||||||
| Parent Report | 8 | Depression | -- | .53 | .48 | .26 | .52 | .54 | .53 | .44 | .47 | 3.99 | 5.16 | |||||||
| 9 | Physical Symptoms | -- | .43 | .42 | .40 | .36 | .32 | .41 | .39 | 4.78 | 4.63 | |||||||||
| 10 | Social Anxiety | -- | .39 | .37 | .32 | .35 | .29 | .39 | 9.56 | 5.44 | ||||||||||
| 11 | Separation Anxiety | -- | .21 | .13 | .15 | .27 | .19 | 5.97 | 4.81 | |||||||||||
| 12 | Oppositional Defiant Disorder | -- | .72 | .49 | .48 | .62 | 1.80 | 2.04 | ||||||||||||
| 13 | Conduct Disorder | -- | .46 | .45 | .64 | 1.85 | 2.53 | |||||||||||||
| 14 | Inattention | -- | .61 | .43 | 15.14 | 4.89 | ||||||||||||||
| 15 | Hyperactivity | -- | .47 | 8.12 | 6.65 | |||||||||||||||
| 16 | Aggression | -- | ||||||||||||||||||
Syndrome-based model.
The first version of the syndrome-based model (Table 3, S1-9) constrained all syndrome factors to be orthogonal with one another. The model fit of this first version was acceptable (e.g., CFI = .90, RMSEA= .080 [.073, .087], SRMR = .085). In this model, earlier pubertal timing was significantly associated with higher symptoms of depression (β = .51, p =.002), CD (β = .95, p <.001), ODD (β = .80, p <.001), and aggression (β = .72, p =.003). Later pubertal timing was associated with higher symptoms of separation anxiety (β = −.42, p =.003). Gender did not moderate any associations between pubertal timing and psychopathology.
Table 3.
Model fit statistics and correlations for syndrome, internalizing and externalizing, and p-factor models
| Syndrome Model w/o Covariance | Depression, Controlling for Others | Physical Sx, Controlling for Others | Social Anx, Controlling for Others | Separation Anx, Controlling for Others | Conduct Disorder, Controlling for Others | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fit Stats | |||||||||||||||||||||||||
| χ2 (df) | 512.742 (110) | 581.19 (126) | 596.45 (126) | 589.28 (126) | 584.76 (126) | 654.94 (127)* | |||||||||||||||||||
| AIC | 36,052.47 | 36,088.92 | 36,104.18 | 36,097.01 | 36,092.49 | 36,160.67 | |||||||||||||||||||
| BIC | 36,166.58 | 36,184.20 | 36,199.46 | 36,192.29 | 36,187.77 | 36,254.78 | |||||||||||||||||||
| CFI | .90 | .89 | .89 | .89 | .89 | .87 | |||||||||||||||||||
|
RMSEA
[95% CI] |
.080 [.073, .087] |
.079 [.073, .086] |
081 [.074, .087] |
080 [.074, .087] |
080 [.073, .086] |
085 [.079, .092] |
|||||||||||||||||||
| SRMR | .085 | .093 | .092 | .095 | .095 | .093 | |||||||||||||||||||
| Predictor | Factor |
St
Est |
SE |
Est/
SE |
p |
St
Est |
SE |
Est/
SE |
p |
St
Est |
SE |
Est/
SE |
p |
St
Est |
SE |
Est/
SE |
p |
St
Est |
SE |
Est/
SE |
p |
St
Est |
SE |
Est/
SE |
p |
| Pubertal Timing | Depress | .51 | .16 | 3.12 | <.01 | .06 | .10 | 0.66 | .51 | ||||||||||||||||
| Phy Sx | .28 | .19 | 1.45 | .15 | .20 | .08 | 2.42 | .02 | |||||||||||||||||
| Social Anx |
.25 | .16 | 1.54 | .12 | .13 | .09 | 1.47 | .14 | |||||||||||||||||
| Sep Anx | -.42 | .14 | −2.93 | <.01 | −.40 | .08 | −5.06 | <.001 | |||||||||||||||||
| CD | .95 | .17 | 5.56 | <.01 | .18 | .09 | 2.05 | .04 | |||||||||||||||||
| ODD | .80 | .21 | 3.81 | <.01 | |||||||||||||||||||||
| Agg | .72 | .25 | 2.92 | <.01 | |||||||||||||||||||||
| Inatt | .08 | .08 | 0.95 | .35 | |||||||||||||||||||||
| Hyp | .04 | .09 | 0.46 | .65 | |||||||||||||||||||||
|
Gender (0=male, 1=female) |
Depress | .15 | .07 | 2.13 | .03 | .11 | .06 | 1.79 | .07 | ||||||||||||||||
| Phy Sx | .24 | .07 | 3.18 | <.01 | .02 | .06 | 0.40 | .69 | |||||||||||||||||
|
Social Anx |
.35 | .07 | 5.47 | <.01 | .19 | .06 | 3.35 | .001 | |||||||||||||||||
| Sep Anx | .22 | .05 | 4.14 | <.01 | .09 | .05 | 1.85 | .06 | |||||||||||||||||
| CD | −.06 | .08 | 0.82 | .41 | −.04 | .06 | −0.74 | .46 | |||||||||||||||||
| ODD | .08 | .10 | 0.67 | .50 | |||||||||||||||||||||
| Agg | −.06 | .11 | −0.54 | .59 | |||||||||||||||||||||
| Inatt | −.13 | .04 | −3.57 | <.01 | |||||||||||||||||||||
| Hyp | −.05 | .04 | −1.32 | .19 | |||||||||||||||||||||
| Timing x Gender | Depress | −.10 | .18 | −0.57 | .57 | .05 | .09 | 0.50 | .62 | ||||||||||||||||
| Phy Sx | .04 | .20 | 0.18 | .86 | .10 | .08 | 1.25 | .21 | |||||||||||||||||
| Social Anx | −.19 | .16 | −1.16 | .25 | −.15 | .08 | 1.25 | .08 | |||||||||||||||||
| Sep Anx | .03 | .15 | 0.22 | .83 | .04 | .08 | 0.50 | .62 | |||||||||||||||||
| CD | −.30 | .23 | −1.33 | .18 | −.06 | .09 | −0.69 | .49 | |||||||||||||||||
| ODD | −.27 | .26 | −1.04 | .30 | |||||||||||||||||||||
| Agg | −.39 | .27 | −1.45 | .15 | |||||||||||||||||||||
| Inatt | −.03 | .08 | −0.36 | .72 | |||||||||||||||||||||
| ODD, Controlling for Others | Aggression, Controlling for Others | Hyperactivity, Controlling for Others | Inattention, Controlling for Others | Internalizing and Externalizing Model | P-factor Model | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fit Stats | |||||||||||||||||||||||||||
| χ2 (df) | 667.88 (126) |
663.44 (126) | 559.80 (124) | 532.81 (124) | 398.21 (119) | 266.65 (109) | |||||||||||||||||||||
| AIC | 36,175.61 | 36,171.17 | 36,071.53 | 36,044.54 | 35,91 9.95 |
35,808.39 | |||||||||||||||||||||
| BIC | 36,270.89 | 36,266.45 | 36,169.17 | 36,142.18 | 36,02 3.46 |
35,923.66 | |||||||||||||||||||||
| CFI | .87 | .87 | .89 | .90 | .93 | .96 | |||||||||||||||||||||
|
RMSEA [95% CI] |
087 [.080, .093] |
086 [.080, .093] |
078 [.072, .085] |
076 [.069, .083 |
.064 [.057, .071] |
050 [.043, .058] |
|||||||||||||||||||||
| SRMR | .094 | .096 | .098 | .095 | .066 | .046 | |||||||||||||||||||||
|
St Est |
SE | Est/ SE | p |
St Est |
SE |
Est/ SE |
P |
St Est |
SE |
Est/ SE |
p |
St Est |
SE |
Est/ SE |
p |
St Est |
SE |
Est/ SE |
p |
St Est |
SE |
Est/ SE |
p | ||||
| Pubertal Timing | ODD | .06 | .11 | 0.58 | .56 | Int | .51 | .11 | 4.79 | <.01 | Int | .53 | .11 | 4.78 | <.01 | ||||||||||||
| Agg | −.14 | .11 | −1.31 | .19 | Ex | .33 | .10 | 3.45 | <.01 | Ex | .42 | .11 | 4.04 | <.01 | |||||||||||||
| Inatt | −.08 | .06 | −1.28 | .20 | p | .69 | .12 | 5.52 | <.01 | ||||||||||||||||||
| Hyp | −.12 | .06 | −2.15 | .03 | |||||||||||||||||||||||
|
Gender 0=male, 1=female |
ODD | .11 | .07 | 1.58 | .11 | Int | .33 | .06 | 5.54 | <.01 | Int | .40 | .06 | 6.77 | .01 | ||||||||||||
| Agg | −.11 | .07 | −1.54 | .12 | Ex | .06 | .06 | 1.13 | .26 | Ex | .16 | .06 | 2.56 | .01 | |||||||||||||
| Inatt | −.01 | .03 | −0.29 | .77 | p | −.17 | .06 | −3.09 | <.01 | ||||||||||||||||||
| Hyp | −.13 | .03 | −4.22 | <.01 | |||||||||||||||||||||||
| Timing x Gender | ODD | −.01 | .10 | −0.10 | .92 | Int | −.06 | .12 | −0.49 | .63 | Int | −.05 | .10 | −0.52 | .60 | ||||||||||||
| Agg | −.08 | .10 | −0.72 | .47 | Ex | −.16 | .10 | −1.67 | .09 | Ex | −.08 | .12 | −0.70 | .48 | |||||||||||||
| Inatt | −.05 | .06 | −0.88 | .38 | p | −.05 | .10 | −0.52 | .60 | ||||||||||||||||||
| Hyp | .02 .05 0.31 .76 | ||||||||||||||||||||||||||
Note: AIC = Akaike information criterion; BIC = Bayesian information criterion (sample size adjusted); CFI = comparative fit index; CI = confidence interval; RMSEA = root mean square error of approximation; SRMR = Standardized Root Mean Square Residual; Depress = Depression; Phy Sx = Physical Symptoms; Social Anx = Anxiety; Sep Anx = Separation Anxiety, CD = Conduct Disorder; ODD = Oppositional Defiant Disorder; Agg = Aggression; Inatt = Inattention; Hyp = Hyperactivity; Int = Internalizing; Ext = Externalizing.
MASC-SP (child report) variance constrained to zero due to negative variance.
Note: reporter and random intercept factors omitted for clarity in all models. ODD = Oppositional Defiant Disorder; C = child report; P= parent report.
When we regressed each syndrome on our predictors (pubertal timing, gender, and their interaction) while controlling for the other syndromes in the regressions, fit across these models (Table 3, S2-S10) was close to acceptable (e.g., CFI ranged from .87 to .90, RMSEA = ranged from .076 [.069, .083] to. 087 [.080, .093], SRMR ranged from .092 to .098. In the syndrome models controlling for other syndromes, earlier pubertal timing was no longer significantly associated with depression, ODD, or aggression but was still significantly associated with higher symptoms of CD (β = .18, p =.04). Earlier pubertal timing was now also associated with physical symptoms (β = .20, p =.02). Later pubertal timing was still associated with higher symptoms of separation anxiety (β = −.40, p <.001) and was now associated with inattention (β = −.12, p =.03). Again, there were no significant interactions between pubertal timing and gender.
“Internalizing and Externalizing” model.
The internalizing and externalizing model (Table 3, S11) demonstrated acceptable fit (e.g., CFI = .93, RMSEA = .064 [.057, .071], SRMR = .066) and better (lower AIC/BIC) than all syndrome models. Internalizing and externalizing factors were significantly correlated (β = .35, p <.001). Earlier pubertal timing was significantly correlated with both internalizing (β = .51, p <.001) and externalizing (β = .33, p =.001) factors. Gender did not moderate associations between pubertal timing and either the internalizing or externalizing factors. Girls were higher than boys on the internalizing factor (β = .33, p <.001), but there was no gender difference for the externalizing factor.
P-factor model.
The p-factor model (Table 3, S12) demonstrated good fit (e.g., CFI = .96, RMSEA = .050 [.043, .058], SRMR = .046) and the best (lowest) AIC/BIC of all models. Earlier pubertal timing was significantly correlated with the p-factor (β = .42, p <.001) and (after accounting for the p-factor), both internalizing- (β = .53, p <.001) and externalizing- (β = .69, p <.001) specific factors. There were no significant interactions between pubertal timing and gender for the p-factor or the internalizing-specific and externalizing-specific factors. Boys were higher than girls on levels of the p-factor (β = .17, p =.002); however, girls were higher on levels of both internalizing- (β = .20, p =.01) and externalizing- (β = .16, p =.01) specific factors (after accounting for the p-factor).
Discussion
The current study examined how pubertal timing was associated with dimensionally assessed psychopathology in youth represented and analyzed across three organizational models: DSM-based syndromes, internalizing and externalizing factors, and a bifactor model that included the common psychopathology (p)-factor. Findings across all models suggested early pubertal timing acted as a transdiagnostic risk factor as well as demonstrated some unique links to specific forms of psychopathology. First, in the DSM-based syndrome model, early pubertal timing was associated with syndromes with relatively equal effect sizes; however, most of these associations were nonsignificant when the other syndromes were used as covariates. Next, in the “internalizing and externalizing” model, early pubertal timing demonstrated moderate associations with both the internalizing factor and externalizing factor. Last, early pubertal timing was associated with the p-factor and also displayed unique relationships with the internalizing-specific and externalizing-specific factors in the p-factor model. Across all models, gender did not moderate the relationship between pubertal timing and psychopathology. Study findings reinforce the importance of examining risk factors across different grain sizes in psychopathology measurement, conceptualization, and analysis.
Taken together, the results of the current study suggest that early pubertal timing serves as a transdiagnostic risk factor and also demonstrates some specificity to particular forms of psychopathology. The transdiagnostic effect found for pubertal timing is in line with a recent meta-analysis (Ullsperger & Nikolas, 2017), in which early pubertal timing had relatively equivalent effects on internalizing and externalizing problems. Current study results also support some syndrome specificity for pubertal timing. In the syndrome model, when other syndromes were controlled for, early pubertal timing displayed unique individual relationships with physical symptoms and conduct disorder (CD). In addition, late pubertal timing was associated with separation anxiety as well as inattention. Our finding that some syndromes (e.g., depression, oppositional defiant disorder (ODD), aggression) showed univariate associations with early pubertal timing that were not obtained in models in which other syndromes were controlled for is consistent with the perspective that early pubertal timing confers transdiagnostic risk for psychopathology. At the same time, the presence of unique relationships with CD and physical symptoms suggests that early pubertal timing demonstrates some specific effects that transcend transdiagnostic influence. These patterns further reinforce the importance of considering different grain sizes in conceptualizing and analyzing psychopathological outcomes and of including multiple forms of psychopathology in measurement and analysis.
Further, the current study suggests that if pubertal timing is structured as a transdiagnostic risk factor that includes various forms of psychopathology, similar effects are found for both genders. In the past, boys were thought to benefit from early maturation; however, recent research has found that boys with early pubertal timing demonstrate higher levels of psychopathology (Mendle & Ferrero, 2012). For girls, it is widely accepted that early maturers experience higher levels of internalizing problems; on the other hand, evidence of the association between early timing and externalizing problems in girls has been mixed (Dimler & Natsuaki, 2015). A meta-analysis examining the effects of early pubertal timing found significant effects for externalizing syndromes among both boys and girls (Dimler & Natsuaki, 2015). These meta-analytic results are consistent with the present study, which showed that gender did not modify the effect of pubertal timing on psychopathology.
It is useful to consider the current study’s findings in the context of the main explanatory theories of pubertal timing and psychopathology. The most widely accepted hypothesis for the association between early pubertal timing and psychopathology is the stage termination or maturational disparity hypothesis (Benoit, Lacourse, & Claes, 2013; Brooks-Gunn, Petersen, & Eichorn, 1985; Compas et al., 1995). The disparity hypothesis posits that children who physically mature earlier than their peers lack the cognitive or emotional maturity to successfully navigate the psychosocial consequences (e.g., becoming sexually active) of early pubertal maturation, which may ultimately lead to psychopathology (Ge & Natsuaki, 2009). The current findings provide some support for the disparity hypothesis as both early-maturing boys and girls were at higher risk for psychopathology. The disparity hypothesis is thought to apply similarly to both externalizing and internalizing disorders and does not make specific syndrome-level predictions. A secondary explanatory model of pubertal timing and psychopathology is the social or maturational deviance hypothesis, which holds that children who mature “off-time” (i.e., either earlier or later than their same-sex peers) will experience higher levels of psychopathology (Petersen, Crockett, Richards, & Boxer, 1988). Gendered interpretations of the deviance hypothesis predict that earlier maturing girls and later maturing boys (i.e., those most deviant from their peer group) have the highest risk of psychopathology; however, we did not find significant gender differences in the effects of pubertal timing on psychopathology in any of our models.
A third framework is the vulnerability-stress model (or contextual amplification hypothesis; Ge and Natsuaki, 2009), which suggests that early pubertal timing may interact with certain stressors or contexts to lead to psychopathology. If so, early pubertal timing may serve as a non-specific risk factor and the specific resulting psychopathology could be largely determined by contextual factors, whose effects may differ by gender. For instance, early maturers demonstrated higher levels of externalizing behaviors if they affiliated with older peers or peers who engaged in delinquent behaviors (Halpern et al., 2007, Lynne et al., 2007) and a higher risk of depression if they experienced recent family stress (Rudolph & Troop-Gordon, 2010). One model to test the hypothesis that early pubertal timing experienced in various contexts leads to specific forms of psychopathology would be the contextual amplification of the maturational disparity hypothesis. Future research should seek to evaluate if certain contexts experienced by early maturers are more likely to lead to specific syndromes or presentations (e.g., internalizing vs. externalizing).
Most studies have found a robust relationship between early pubertal timing and externalizing problems and have largely conducted their investigation from a broadband standpoint and not examined specific syndromes. Our results suggest that the risk for externalizing problems associated with early pubertal timing might be primarily explained by CD ODD, and aggression, rather than ADHD. Moreover, current study findings highlight the need for additional theoretical work to account for the unique relationships found between early pubertal timing and antisocial/ rule breaking behavior (CD). For instance, early pubertal maturation has been found to have a robust association with delinquency (Mendle & Ferrero, 2012), and pubertal development has been correlated with genetic risk for (non-aggressive) antisocial and rule breaking behavior (Harden et al., 2015). Additional work is also needed on the unique relationship between early pubertal timing and physical symptoms. Physical symptoms of anxiety have been rarely examined in relation to pubertal timing; however, one study reported null results for the association between pubertal status and physical symptoms (Deardorff et al., 2007). In addition, the current study found significant associations with later pubertal timing and separation anxiety and with later pubertal timing and inattention. Separation anxiety is thought to decrease across adolescence (Van Oort et al., 2009); however, to our knowledge, ours is the first study to investigate and find a relationship between pubertal timing and separation anxiety. Work on the relationship between pubertal timing and inattention is also limited but retrospective work has found associations between early pubertal timing and attention difficulties (Ostojic & Miller, 2016). The limited research concerning pubertal timing and social anxiety has also yielded mixed results. Early pubertal timing has been associated with social anxiety symptoms for only girls (and not boys; Blumenthal et al., 2011), for only boys (and not girls; Ge et al., 2006), and for neither gender (Hamlat et al., 2014). Associations between pubertal timing and social anxiety may be dependent upon contextual factors (Reardon et al., 2009), such as peer difficulties (Blumenthal et al., 2009), and omitted moderators may be responsible for some of the discrepancies noted in extant research.
The current study contains the first evidence of early pubertal timing as a transdiagnostic risk factor by demonstrating a relationship between early pubertal timing and the common psychopathology factor. One strength of the present study is that by investigating pubertal timing across structural levels of three alternative models, we were able to able to portion out both common and specific associations of pubertal timing with psychopathology. This allowed us to consider different “grain sizes” of psychopathology structure in associations with pubertal timing. A second strength is that the study included both youth and parent report of psychopathology (with the exception of ADHD) as well as reporter factors in all models to remove variance due to reporter. Finally, conducting analyses within a large, community sample spanning childhood to adolescence allowed us to optimally evaluate relationships of interest between timing of pubertal maturation and psychopathology.
There were several limitations of the current study. One limitation is that the study sample did not contain enough non-Caucasian participants to examine race or ethnicity as moderators of timing effects. As there may be racial and/or ethnic differences in rates of physical maturation (Herman-Giddens et al., 1997) as well as in the effects of pubertal timing on psychopathology (e.g., Hamlat et al., 2014), future research should examine if early pubertal timing functions as a transdiagnostic risk factor for children of different racial and ethnic backgrounds. A second limitation is that the current study consisted of cross-sectional data. Cross-sectional data was sufficient for a first investigation of pubertal timing as a transdiagnostic risk factor as the literature has often found a more proximal association between pubertal timing and psychopathology (Table 1). The p-factor demonstrates a high degree of stability during adolescence (Snyder et al., 2017); however, prospective studies are needed to evaluate the longitudinal effects of pubertal timing at both lower-order (e.g., discrete syndromes) and higher-order (e.g., internalizing, p-factor) dimensions of psychopathology as some evidence suggests effects do not persist past adolescence (e.g., Graber, 2013). A third limitation is the use of solely the PDS as a metric of pubertal development; although we found sufficient variability in development using the PDS in our sample, self-report measures of puberty necessarily conflate biological and psychological changes. Future research on this topic may want to supplement selfreport with more objective measures (e.g., gonadal and adrenal hormonal signals) of pubertal maturation (Shirtcliff, Dahl, & Pollak, 2009).
Further, mechanisms mediating the relationship between pubertal timing and psychopathology dimensions were not investigated in the current study. Future research may want to examine potential transdiagnostic mediators of the association between pubertal timing and general psychopathology, such as emotional regulation or shared genetic liability. Evidence suggests that hormonal changes during puberty may regulate cortical plasticity during this sensitive period, and also affect neurotransmitter function, so these are additional possible mediating mechanisms (Piekarski et al., 2017). Examinations of the mechanisms by which early pubertal timing confers transdiagnostic risk may help target common processes across syndromes. Additionally, the presence of independent associations for early pubertal timing with p, internalizing-specific and externalizing-specific factors suggests that there may be multiple mechanisms at work, which may function specifically for particular factors.
Supplementary Material
Footnotes
The authors declare that they have no conflicts of interest.
Contributor Information
Elissa J. Hamlat, University of Illinois at Urbana-Champaign
Hannah R. Snyder, Brandeis University
Jami F. Young, Children’s Hospital of Philadelphia University of Pennsylvania Perelman School of Medicine
Benjamin L. Hankin, University of Illinois at Urbana-Champaign
References
- Achenbach TM (1966). The Classification of Children’s Psychiatric Symptoms: A Factor-Analytic Study. Psychological Monographs: General and Applied, 80(7), 1–37. [DOI] [PubMed] [Google Scholar]
- Achenbach TM (1991). Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry. [Google Scholar]
- Achenbach TM, & Edelbrock S (1978). The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin, 85(6), 1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, & Edelbrock CS (1981). Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monographs of the Society for Research in Child Development, 46(1), 1–82. [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla L (2001). Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Angold A, & Costello EJ (2006). Puberty and depression. Child and Adolescent Psychiatric Clinics, 15(4), 919–937. [DOI] [PubMed] [Google Scholar]
- Arim RG, & Shapka JD (2008). The impact of pubertal timing and parental control on adolescent problem behaviors. Journal of Youth and Adolescence, 37, 445–455. [Google Scholar]
- Bakker MP, Ormel J, Lindenberg S, Verhulst FC, & Oldehinkel AJ (2011). Generation of interpersonal stressful events: The role of poor social skills and early physical maturation in young adolescents--The TRAILS study. The Journal of Early Adolescence, 31(5), 633–655. [Google Scholar]
- Baldwin JS, & Dadds MR (2007). Reliability and validity of parent and child versions of the Multidimensional Anxiety Scale for children in community samples. Journal of the American Academy of Child & Adolescent Psychiatry, 46(2), 252–260. [DOI] [PubMed] [Google Scholar]
- Benoit A, Lacourse E, & Claes M (2013). Pubertal timing and depressive symptoms in late adolescence: The moderating role of individual, peer, and parental factors. Development and Psychopathology, 25(2), 455–471. [DOI] [PubMed] [Google Scholar]
- Berenbaum SA, Beltz AM, & Corley R (2015). The Importance of Puberty for Adolescent Development: Conceptualization and Measurement. Advances in Child Development and Behavior, 48, 53–92. [DOI] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Babson KA, Gahr JL, Trainor CD, & Frala JL (2011). Elevated social anxiety among early maturing girls. Developmental Psychology, 47(4), 1133–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Trainor CD, Babson KA, & Bunaciu L (2009). Interactive roles of pubertal timing and peer relations in predicting social anxiety symptoms among youth. Journal of Adolescent Health, 44(4), 401–403. [DOI] [PubMed] [Google Scholar]
- Brooks-Gunn J, Petersen AC, & Eichorn D (1985). The study of maturational timing effects in adolescence. Journal of Youth and Adolescence, 14(3), 149–161. [DOI] [PubMed] [Google Scholar]
- Carter R, Caldwell CH, Matusko N, Antonucci T, & Jackson JS (2011). Ethnicity, perceived pubertal timing, externalizing behaviors, and depressive symptoms among black adolescent girls. Journal of Youth and Adolescence, 40(10), 1394–1406. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H,…Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos-Ryan N, Brière FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, … Conrod P (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology, 125(8), 1039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FR, & Raine A (2018). Effects of harsh parenting and positive parenting practices on youth aggressive behavior: The moderating role of early pubertal timing. Aggressive Behavior, 44(1), 18–28. [DOI] [PubMed] [Google Scholar]
- Chorpita B, & Ebesutani C (2014). Revised children’s anxiety and depression scale user’s guide Unpublished Users Guide, University of California, Los Angeles: http://www.childfirst.ucla.edu/RCADSUsersGuide20140711.pdf. [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression Scale. Behaviour Research and Therapy, 38, 835–855. [DOI] [PubMed] [Google Scholar]
- Compas BE, Hinden BR, & Gerhardth CA (1995). Adolescent development: Pathways and processes of risk and resilience. Annual Review of Psychology, 46, 265–93. [DOI] [PubMed] [Google Scholar]
- Conley CS, Rudolph KD, & Bryant FB (2012). Explaining the longitudinal association between puberty and depression: Sex differences in the mediating effects of peer stress. Development and Psychopathology, 24(2), 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W, Shanahan L, Miller S, Costello EJ, Angold A, & Maughan B (2010). Outcomes of early pubertal timing in young women: a prospective population-based study. The American Journal of Psychiatry, 167(10), 1218–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crockett LJ, Carlo G, Wolff JM, & Hope MO (2013). The role of pubertal timing and temperamental vulnerability in adolescents’ internalizing symptoms. Development and Psychopathology, 25(2), 377–389. [DOI] [PubMed] [Google Scholar]
- Deardorff J, Hayward C, Wilson KA, Bryson S, Hammer LD, & Agras S (2007). Puberty and gender interact to predict social anxiety symptoms in early adolescence. Journal of Adolescent Health, 41(1), 102–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR (1983). SCL 90 R Administration, scoring, and procedures: Manual II. Baltimore: Clinical Psychometric Research. [Google Scholar]
- Dimler LM & Natsuaki MN (2015). The effects of pubertal timing on externalizing behaviors in adolescence and early adulthood: A meta-analytic review. Journal of Adolescence, 45, 160–170. [DOI] [PubMed] [Google Scholar]
- Dorn LD, Dahl RE, Woodward HR, & Biro F (2006). Defining the boundaries of early adolescence: A user’s guide to assessing pubertal status and pubertal timing in research with adolescents. Applied Developmental Science, 10, 30–56. [Google Scholar]
- Dorn L, Susman E, & Ponirakis A (2003). Pubertal timing and adolescent adjustment and behavior: Conclusions vary by rater. Journal of Youth and Adolescence, 32, 157–167. [Google Scholar]
- Ellis LK, & Rothbart MK (2001, April). Revision of the early adolescent temperament questionnaire. Poster presented at the 2001 Biennial Meeting of the Society for Research in Child Development, Minneapolis, MN. [Google Scholar]
- Farrell AD, Danish SJ, & Howard CW (1992). Relationship between drug use and other problem behaviors in urban adolescents. Journal of Consulting and Clinical Psychology, 60(5), 705–712. [DOI] [PubMed] [Google Scholar]
- Frances AJ, & Widiger T (2012). Psychiatric diagnosis: lessons from the DSM-IV past and cautions for the DSM-5 future. Annual Review of Clinical Psychology, 8, 109–130. [DOI] [PubMed] [Google Scholar]
- Gadow KD, & Sprafkin J (1997). Child symptom inventory-4 norm manual. Stony Brook, NY: Checkmate Plus. [Google Scholar]
- Gadow KD, & Sprafkin J (1998). Adolescent symptom inventory-4 norms manual. Stony Brook, NY: Checkmate Plus. [Google Scholar]
- Ge X & Natsuaki M (2009). In search of explanations for early pubertal timing effects on developmental psychopathology. Current Directions in Psychological Science, 186, 327–331. [Google Scholar]
- Ge X, Brody GH, Conger RD, & Simons RL (2006). Pubertal maturation and African American children’s internalizing and externalizing symptoms. Journal of Youth and Adolescence, 35(4), 528–537. [Google Scholar]
- Ge X, Brody GH, Conger RD, Simons RL, & Murry VM (2002). Contextual amplification of pubertal transition effects on deviant peer affiliation and externalizing behavior among African American children. Developmental Psychology, 38(1), 42–54. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, & Elder GH Jr. (2001). Pubertal transition, stressful life events, and emergence of gender differences in adolescent depressive symptoms. Developmental Psychology, 37, 404–417. [DOI] [PubMed] [Google Scholar]
- Graber JA (2013). Pubertal timing and the development of psychopathology in adolescence and beyond. Hormones and Behavior, 64(2), 262–269. [DOI] [PubMed] [Google Scholar]
- Graber JA, Seeley JR, Brooks-Gunn J, & Lewinsohn PM (2004). Is pubertal timing associated with psychopathology in young adulthood?. Journal of the American Academy of Child & Adolescent Psychiatry, 43(6), 718–726. [DOI] [PubMed] [Google Scholar]
- Graber JA, Brooks-Gunn J, & Warren MP (2006). Pubertal effects on adjustment in girls: Moving from demonstrating effects to identifying pathways. Journal of Youth and Adolescence, 35(3), 391–401. [Google Scholar]
- Grills-Taquechel AE, Ollendick TH, & Fisak B (2008). Reexamination of the MASC factor structure and discriminant ability in a mixed clinical outpatient sample. Depression and Anxiety, 25(11), 942–950. [DOI] [PubMed] [Google Scholar]
- Halpern CT, Kaestle CE, & Hallfors DD (2007). Perceived physical maturity, age of romantic partner, and adolescent risk behavior. Prevention Science, 8(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Hamlat E, Stange J, Abramson L, & Alloy L (2014). Early pubertal timing as a vulnerability to depression symptoms: Differential effects of race and sex. Journal of Abnormal Child Psychology, 42, 527–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, … Vasey MW (2016). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28(4pt1), 987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley LD, … Oppenheimer CW (2015). Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology, 124(4), 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden KP, Patterson MW, Briley DA, Engelhardt LE, Kretsch N, Mann FD, … Tucker-Drob EM (2015). Developmental changes in genetic and environmental influences on rule-breaking and aggression: Age and pubertal development. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56(12), 1370–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynie DL (2003). Contexts of risk? Explaining the link between girls’ pubertal development and their delinquent involvement. Social Forces, 82(1), 355–397. [Google Scholar]
- Herman‐Giddens ME (2006). Recent data on pubertal milestones in United States children: the secular trend toward earlier development. International Journal of Andrology, 29(1), 241–246. [DOI] [PubMed] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Jin R, Ge X, Brody G, Simons R, Cutrona C, & Gibbons F (2008). Antecedents and consequences of psychiatric disorders in African-American adolescents. Journal of Youth and Adolescence, 37(5), 493–505. [Google Scholar]
- Keenan K, Culbert KM, Grimm KJ, Hipwell AE, & Stepp SD (2014). Timing and tempo: Exploring the complex association between pubertal development and depression in African American and European American girls. Journal of Abnormal Psychology, 123(4), 725–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, & Wittchen HU (1998). The World Health Organization Composite International Diagnostic Interview Short‐Form (CIDISF). International Journal of Methods in Psychiatric Research, 7(4), 171–185. [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, . . . Merikangas KR (2012). Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 69, 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Üstün TB (2004). The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, & Olino TM (2005). Toward Guidelines for Evidence-Based Assessment of Depression in Children and Adolescents. Journal of Clinical Child & Adolescent Psychology, 34(3), 412. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A Dimensional Alternative to Traditional Nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Kovacs M (1992). Children’s depression inventory: Manual. Multi-Health Systems. [Google Scholar]
- Kozak MJ, & Cuthbert BN (2016). The NIMH Research Domain Criteria Initiative: Background, issues, and pragmatics. Psychophysiology, 53, 286–297 [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting Comorbidity: A Model-Based Approach to Understanding and Classifying Psychopathology. Annual Review of Clinical Psychology, 2(1), 111–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger R (1999). The structure of common mental disorders. Archives of General Psychiatry, 56, 921–926. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, & Silva PA (1998). The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological study. Journal of Abnormal Psychology, 107(2), 216–227. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, & Ormel J (2003). A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. Journal of Abnormal Psychology, 112, 437–447. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, & Rathouz PJ (2011). Higherorder genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry, 68(2), 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143(2), 142–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynne SD, Graber JA, Nichols TR, Brooks-Gunn J, & Botvin GJ (2007). Links between pubertal timing, peer influences, and externalizing behaviors among urban students followed through middle school. Journal of Adolescent Health, 40(2), 181.e7–181.e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau K, Ram N, Houts RM, Grimm KJ, & Susman EJ (2011). Individual differences in boys’ and girls’ timing and tempo of puberty: Modeling development with nonlinear growth models. Developmental Psychology, 47(5), 1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau K, Neiderhiser JM, Lichtenstein P, & Reiss D (2012). Genetic and environmental influences on the association between pubertal maturation and internalizing symptoms. Journal of Youth and Adolescence, 41(9), 1111–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): Factor Structure, Reliability, and Validity. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 554–565. [DOI] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, Mari JJ, … Salum GA (2017). A general psychopathology factor (P Factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology, 126(1), 137–148. [DOI] [PubMed] [Google Scholar]
- Mendle J & Ferrero J (2012). Detrimental outcomes associated with pubertal timing in adolescent boys. Developmental Review, 32, 49–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendle Turkheimer, & Emery (2007). Detrimental psychological outcomes associated with early pubertal timing in adolescent girls. Developmental Review, 27, 151–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Elliott M, Gilliland MJ, Grunbaum JA, Tortolero SR, Cuccaro P, & Schuster M (2008). Positive parenting and early puberty in girls: Protective effects against aggressive behavior. Archives of Pediatrics & Adolescent Medicine, 162(8), 781–786. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User’s Guide (7 ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nadeem E, & Graham S (2005). Early puberty, peer victimization, and internalizing symptoms in ethnic minority adolescents. The Journal of Early Adolescence, 25(2), 197–222. [Google Scholar]
- Natsuaki MN, Biehl MC, & Ge X (2009). Trajectories of depressed mood from early adolescence to young adulthood: The effects of pubertal timing and adolescent dating. Journal of Research on Adolescence, 19(1), 47–74. [Google Scholar]
- Natsuaki MN, Samuels D, & Leve LD (2015). Puberty, Identity, and Context In The Oxford Handbook of Identity Development (pp. 389–405). Oxford University Press. [Google Scholar]
- Negriff S & Susman E (2011).Pubertal timing, depression, and externalizing problems: A framework, review, and examination of gender differences. Journal of Research on Adolescence, 21, 717–746. [Google Scholar]
- Orvaschel H (1995). Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic (Version 5). Ft. Lauderdale, FL: Nova Southeastern University, Center for Psychological Studies. [Google Scholar]
- Ostojic D, & Miller CJ (2016). Association between pubertal onset and symptoms of ADHD in female university students. Journal of Attention Disorders, 20(9), 782–791. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, & Boxer A (1988). A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence, 17(2), 117. [DOI] [PubMed] [Google Scholar]
- Piekarski DJ, Johnson CM, Boivin JR, Thomas AW, Lin WC, Delevich K, ... & Wilbrecht L (2017). Does puberty mark a transition in sensitive periods for plasticity in the associative neocortex?. Brain Research, 1654, 123–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt JM, Colich NL, McLaughlin KA, Gary D, & Keyes KM (2017). Transdiagnostic psychiatric disorder risk associated with early age of menarche: A latent modeling approach. Comprehensive Psychiatry, 79, 70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Reardon LE, Leen-Feldner EW, & Hayward C (2009). A critical review of the empirical literature on the relation between anxiety and puberty. Clinical Psychology Review, 29(1), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, & Troop-Gordon W (2010). Personal-accentuation and contextualamplification models of pubertal timing: Predicting youth depression. Development and Psychopathology, 22(2), 433–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanislow CA (2016). Connecting psychopathology meta-structure and mechanisms. Journal of Abnormal Psychology, 125(8), 1158–1165. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Dahl RE, & Pollak SD (2009). Pubertal development: Correspondence between hormonal and physical development. Child Development, 80(2), 327–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel J, Yancey A, Anseshensel C, & Schuler R (1999). Body image, perceived pubertal timing, and adolescent mental health. Journal of Adolescent Health, 25, 155–165. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, … Hankin BL (2015). Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology, 109(6), 1132–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong homotypic continuity in common psychopathology, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science, 5(1), 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sontag LM, Graber JA, Brooks-Gunn J, & Warren MP (2008). Coping with social stress: Implications for psychopathology in young adolescent girls. Journal of Abnormal Child Psychology, 36(8), 1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susman EJ, Dockray S, Schiefelbein VL, Herwehe S, Heaton JA, & Dorn LD (2007). Morningness/eveningness, morning-to-afternoon cortisol ratio, and antisocial behavior problems during puberty. Developmental Psychology, 43(4), 811. [DOI] [PubMed] [Google Scholar]
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Wu M (2001). Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 168–179. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, Van Hulle C, Waldman I, Krueger RF, & Rathouz PJ (2013). Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of abnormal Psychology, 122(4), 1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teunissen HA, Adelman CB, Prinstein MJ, Spijkerman R, Poelen EA, Engels RC, & Scholte RH (2011). The interaction between pubertal timing and peer popularity for boys and girls: An integration of biological and interpersonal perspectives on adolescent depression. Journal of Abnormal Child Psychology, 39(3), 413–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uher R, & Rutter M (2012). Basing psychiatric classification on scientific foundation: problems and prospects. International Review of Psychiatry, 24(6), 591–605. [DOI] [PubMed] [Google Scholar]
- Ullsperger JM, & Nikolas MA (2017). A meta-analytic review of the association between pubertal timing and psychopathology in adolescence: Are there sex differences in risk?. Psychological Bulletin, 143(9), 903. [DOI] [PubMed] [Google Scholar]
- Van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, & Huizink AC (2009). The developmental course of anxiety symptoms during adolescence: The TRAILS study. Journal of Child Psychology and Psychiatry and Allied Disciplines, 50(10), 1209–1217. [DOI] [PubMed] [Google Scholar]
- White RM, Deardorff J, & Gonzales NA (2012). Contextual amplification or attenuation of pubertal timing effects on depressive symptoms among Mexican American girls. Journal of Adolescent Health, 50(6), 565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winer JP, Parent J, Forehand R, & Breslend NL (2016). Interactive effects of psychosocial stress and early pubertal timing on youth depression and anxiety: Contextual amplification in family and peer environments. Journal of Child and Family Studies, 25(5), 1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.