Abstract
Background:
Clinical variability MRI exam scanning durations can impede efficient MRI utilization. There is a paucity of data regarding the degree of variability of identically protocoled MRI studies and which non-technological factors contribute to time-length variations in MRI exams.
Purpose:
To measure the magnitude of variation in MRI exam duration for identically protocoled MRI exams and to identify potential contributors to variations in MRI exam times.
Study Type:
Retrospective
Subjects:
2705 identically protocoled MRI examinations of the cervical spine without contrast, comprehensive stroke exams, and comprehensive brain examinations performed on adult patients from 6/30/2016 through 6/30/2017.
Assessment:
MRI exam duration was obtained directly from the image data. Potential predictors for exam length variability were evaluated including patient age, patient gender, performing technologist, patient status (inpatient/outpatient/emergency department), MRI field strength, use of sedation, day of week, and the time of day.
Statistical Tests:
Linear regression analysis was performed for each individual variable after correcting for the MRI exam type. A multivariate mixed model was generated to assess for independent associations between the predictors and exam duration.
Results:
There was substantial variability in the duration of the selected clinical MRI exams, with standard deviations ranging between 19% and 29% of the mean exam length for each individual type of exam. The performing technologist was the most significant identified factor contributing to this variation in exam length,SD= 2.645 (p<0.001). Compared to outpatient exams, inpatient exams required 4.18 minutes longer to complete (p<0.001), and emergency department studies 1.86 minutes longer (p=0.005). Male gender was associated with an additional 1.36 minutes of exam time (p<0.001).
Data Conclusion:
Non-technical factors are associated with substantial variation in MRI exam times. These variations can be predicted based on relatively simple clinical and demographic factors, with implications for MRI exam scheduling, protocol design, staff training, and workflow design.
Keywords: MRI, utilization, scheduling, exam variability
INTRODUCTION:
Magnetic resonance imaging (MRI) possesses many advantages over other neuroimaging techniques including improved tissue contrast, the lack of ionizing radiation, and access to numerous advanced imaging techniques including diffusion weighted imaging, perfusion, time-resolved contrast imaging, and fMRI techniques. As a result of these and other ongoing developments in MRI, there has been an increase in demand for MRI examinations.(1, 2) This increased demand and utilization of MRI creates a corresponding incentive to maximize the utilization of MRI as MRI incurs significant overhead costs including purchase costs, depreciation, maintenance, and staffing.
In order to optimize the utilization of MRI in the most cost-efficient manner, most radiology practices attempt to optimize exam protocols and MRI scheduling to minimize wasted time and resources.(3) Typically, these efforts focus on limiting the number of acquired sequences, thereby limiting overall exam time.(4) However, process optimization emphasizes minimizing both waste and variation as key steps in process improvement.(5) The impact of exam length variability on scanner utilization, however, is often overlooked in this process. Variances in MRI exam duration impede efficient patient scheduling when exam slots are lengthened to accommodate the majority of exams and not just the median exam time. The required increase in appointment time decreases MRI scanner utilization, potentially hindering access to MRI examinations and ultimately increasing the overall system costs.(6, 7)
A greater understanding of MRI exam variability and underlying causes could allow for improvements in the overall utilization of the MRI and an increase in the overall value of MRI. To date, there is a paucity of data on the variability of MRI exam duration and no information on potential contributors to this variation. The aim of this study was to quantify the variability in exam duration for identically protocoled neuroradiology MRI examinations and identify potential clinical and demographic factors that contribute to variances in neuroradiology MRI exam duration as a first step towards broadly understanding the factors contributing to MRI exam length variability.
MATERIALS AND METHODS:
Subject Selection and Compliance
This retrospective, Health Insurance Portability and Accountability Act (HIPAA) compliant study was performed at a single large tertiary care academic medical center along with affiliated outpatient imaging sties and conducted with approval from the institutional review board, including a waiver to obtain patient consent. All consecutive MRI examinations of the cervical spine without contrast, comprehensive stroke exams, and comprehensive brain examinations with and without contrast performed from 6/30/2016 through 6/30/2017 were included in the exam cohort.
MRI Examination Equipment and Technique
All examinations were perfomed on devices manufactured by a single vendor (GE Healthcare, Waukesha, WI). A total of 14 clinical MRI scanners were included in the analysis, eight 1.5 T devices and six 3.0 T devices. The majority of scanners (8 of 14) were located in the hospital setting.
Detailed protocols, including sequences performed and estimated times for each individual sequence are listed in Table 2. The comprehensive stroke exam included the following individual components: MRI of the head with and without contrast, MRA of the head without contrast, and MRA of the neck with and without contrast. For contrast enhanced brain examinations, acquisition of a 3-D T2 FLAIR sequence commenced immediately following the administration of intravenous contrast.. Imaging planes and field of view were manually prescribed by the technologist. No automated prescription tools were utilized during the period studied. Sequences with artifact or poor image quality were repeated at the discretion of the performing technologist.
Table 2.
MRI Protocols and Approximate Individual Sequence Times
| Cervical Spine w/o Contrast | MRI Brain with and without Contrast | Comprehensive Stroke Protocol |
|---|---|---|
| Sag T1 FSE (3:30) | Sag T1 FSE (3:30) | MRA Neck |
| Sag T2 FSE (3:30) | Axial T2 FSE (2:45) | 2D TOF (1:15) |
| Sagl STIR (3:30) | Axial DWI (0:45) | 3D TOF (5:00) |
| Axial T1 (4:15) | Axial T2*(2:30) | Time Resolved MRA (1:15) |
| Axial T2* (6:00) | Axial T1 3D SPGR (2:00) | MRA Head |
| Sag T2 FLAIR 3D FSE +C (4:30) | 3D TOF (4:30) | |
| Axial T1 3D SPGR +C (3:15) | MRI head with and without | |
| Coronal T1 3D FSE +C (2:00) | Sag T1 FSE (3:30) | |
| Axial T2 FSE (2:45) | ||
| Axial DWI (0:45) | ||
| Axial T2*(2:30) | ||
| Axial T1 3D SPGR (2:00) | ||
| DSC Perfusion +C (1:15) | ||
| Sag T2 FLAIR 3D FSE +C (4:30) | ||
| Axial T1 3D SPGR +C (3:15) | ||
| Coronal T1 3D FSE +C (2:00) |
Exams which were protocoled with added or altered sequences, those with additional technologist instructions, and exams which were performed contemporaneously with another MRI examination were excluded from the analysis. MRI examinations being performed on inpatient or emergency department patients were not routinely monitored following selection of the protocol by a radiologist. Those exams specified to be monitored were excluded from the analysis.
Exam Timing, Demographics and Exam Length Predictors
The start time of each MRI exam was defined as the time-of-day associated with the first image of the examination; the end time for each MRI examination was defined as sum of the starting time of the final sequence and the actual duration of the final sequence. The total exam duration was considered the difference between these defined start and end times. Patient transfer and set-up times were excluded from this analysis in order to focus on the duration of the acquisition portion of the examination. For all three MRI exam types included in this study, associated patient demographic, clinical, and technological factors were collected from the electronic medical record (EPIC Systems, Verona, WI) the PACS database (Change Healthcare, Vancouver, BC), and MRI vendor files (GE Healthcare, Waukesha, WI). Demographic and technical factors collected included patient age, gender, inpatient/outpatient/ED status, MRI device name, exam start time, exam day of the week, MRI field strength (1.5T or 3T), use of patient sedation or general anesthesia, and the performing MRI technologist. The exam start time was then categorized as during normal workday hours (Monday through Friday, 7am to 6pm), or after normal working hours.
Statistical Analysis
Linear regression models for patient age, gender, performing technologist, patient location (inpatient/outpatient/ED), field strength, use of sedation, and the time of day were constructed for each individual variable after correcting for MRI exam type. Differences in exam time associated with these demographic and clinical factors were assessed using a standard t-test of the regression coefficients. For individual categories with three or more variables ANOVA tables were generated, and differences assessed for using the F-test.
To assess if the demographic and clinical predictors were independently associated with variations in MRI exam duration a multivariate mixed model was created. To construct the final multivariate model, all variables were included with the exception of the individual MRI station (due to overfitting when this variable was included). The technician variable was included as a random effect to capture how technicians as a population influence MRI exam length. Variables were then stepwise selected using a likelihood ratio test and a nominal p<0.01 cut off and removing one variable at a time. Statistical analysis was performed using R version 3.4.3 (R Core Team, Vienna, Austria).
RESULTS:
A total of 2705 exams meeting the inclusion criteria were included in the analysis. These included a total of 1336 brain MRI exams with and without contrast, 850 cervical spine MRI exams without contrast, and 519 comprehensive stroke exams. Males comprised 1189 (44.0%) of the exams. The mean patient age was 52.9 (SD =17.7 years). The mean exam duration of cervical spine exams was 28.8 minutes (SD=8.4 minutes). The mean duration for comprehensive brain examinations was 34.9 minutes (SD=6.7 minutes), and the mean duration for the comprehensive stroke examination was 53.7 (SD=13.9 minutes).
Linear regression models were created for each factor of interest. As MRI exam type (spine, brain or stroke) was a clear confounding factor given the intrinsic differences in protocol design and coverage, each individual linear model was created with MRI exam type as a correcting factor. After correcting for exam type, age was not found to be a significant predictor of MRI exam duration. However, male gender was associated with an increase in exam duration of 1.67 minutes, p<0.001, 95% CI [0.986, 2.357]. The day of the week, “on call” status and the MRI field strength were not found to be associated with a statistical significant difference in MRI exam duration.
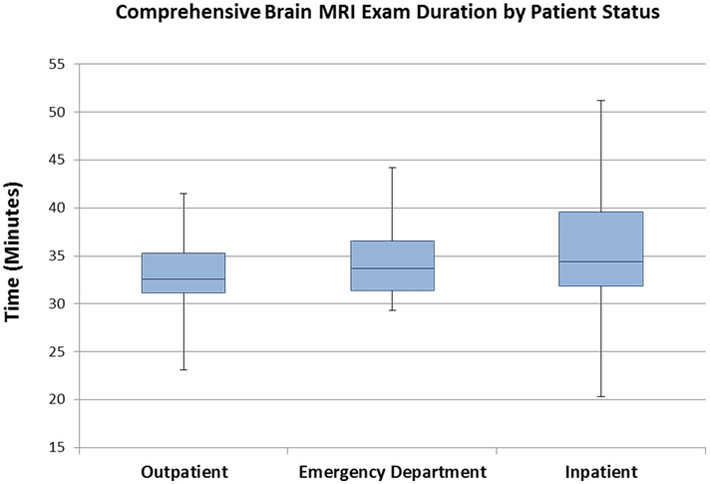
A statistically significant difference between in the duration of inpatient and emergency department MRI examination was found, with inpatient exams requiring an additional 1.87 minutes to complete compared to emergency department exams (95% CI [0.585, 3.150], p=0.004). Outpatient MRI exams times trended towards being shorter than emergency department exam times by 1.16 minutes, but failed to reach statistical significance (95% CI [−2.429, 0.109], p=0.073). Figure 1 illustrates the range in scan times of comprehensive brain examinations versus patient status.
Figure 1.
Box plot demonstrating the variation in exam times of comprehensive brain studies by patient status.
Technologists were found to contribute to exam length variation in the individual linear model (F=3.83, p<0.001). A plot demonstrating the variation in cervical spine MRI exam time versus performing technologist is included as Figure 2. Full statistical results of the individual linear regression models are provided in Table 3. For models with three or more variables ANOVA tables were generated (Table 4).
Figure 2.
Box plot demonstrating variation in MRI cervical spine duration by performing technologist (limited to those technologists performing >10 cervical spine exams).
Table 3.
Results of Individual Models
| Predictor | Estimate (Minutes) |
95% Confidence Interval |
p-value |
|---|---|---|---|
| Brain Exam (vs C-spine) | 6.105 | (5.328, 6.881) | < 0.001 |
| Comprehensive Stroke (vs C-spine) | 24.9 | (23.91, 25.89) | < 0.001 |
| Age (per year) | 0.004 | (−0.015, 0.024) | 0.660 |
| Gender Male (vs female) | 1.672 | (0.986, 2.357) | <0.001 |
| Field Strength 3T (vs 1.5T) | 0.110 | (−0.615, 0.835) | 0.766 |
| Inpatient (vs ED) | 1.868 | (0.585, 3.150) | 0.004 |
| Outpatient (vs ED) | −1.16 | (−2.429, 0.109) | 0.073 |
| Anesthesia / Sedation (vs none) | 0.451 | (−0.607, 1.508) | 0.403 |
Table 4.
ANOVA Table for Individual Models with 3 or More Factors
| Variable | F value | p-value |
|---|---|---|
| Day of Week | 1.67 | 0.124 |
| Patient Status (inpatient, outpatient, ED) | 23.56 | < 0.001 |
| Technician | 3.83 | < 0.001 |
| MRI station | 6.57 | < 0.001 |
Exam type, patient status, and male gender remained statistically significant predictors of exam length in the multivariate model. Technicians were also found to be a significant contributor to exam length variability in the multivariate model, with a standard deviation attributable to the technologist of 2.6 minutes (p<0.01, 95% CI [1.94, 3.49]). Full results from the multivariate model are given in Table 5.
Table 5.
Results of the Mixed Multivariate Model
| Predictor | Estimate (minutes) |
95% Confidence Interval |
p-value |
|---|---|---|---|
| Gender (male) | 1.362 | (0.698, 2.026) | <0.001 |
| Inpatient (vs ED) | 2.323 | (1.066, 3.575) | <0.001 |
| Outpatient (vs ED) | −1.857 | (1.066, 3.575) | 0.005 |
| Technician SD | 2.645 | (1.943, 3.485) | < 0.001 |
| Residual SD | 8.628 |
DISCUSSION:
There is significant variation in time to completion for identically protocoled MRI exams. In this work, the standard deviation of the duration of each MRI exam type was between 19% and 29% of the mean exam length, despite identical MRI exam protocols for each of the neuroradiology exams evaluated. These results agree with previous studies which have also found substantial variation between idealized and experienced MRI examination times. (8, 9)This is approximately the time required for an additional two or more MRI sequences, emphasizing the importance of accounting for this variation in both clinical scheduling and when considering MRI protocol design. In actual practice, the impact is far greater and operationally significant. These data suggest that in order to accommodate 95% of scheduled patients in a given appointment slot (assuming a normal distribution of exam times), exam appointments would need to be scheduled with the addition of 1.7 standard deviations to the mean exam time – a significant and costly accommodation. As an illustrative example, our mean cervical spine examination time was 28.8 minutes, but would require at least a 43 minute appointment slot to accommodate 95% of our patients. When extrapolated over the course of a clinical day (and months and years), the additive costs (both real and unrealized) of accounting for exam variability increase substantially.
If the individual sequence times of the protocols are summed, the minimum protocol times would be approximately 35 minutes for the comprehensive stroke protocol, 21 minutes for the cervical spine exam, and 22 minutes for the MRI brain with and without contrast. The mean exam times actually achieved were 53.7, 28.8, and 34.9 minutes respectively. Some of this difference is attributable to scout sequences, calibration scans, and repeated sequences. However, a large portion is likely attributable to patient communication, sequence prescription, and other time during which the scanner is inactive. For example, one work on abdominal MRI found that image acquisition only occurred during 58% of total table time.(8) The magnitude of this difference between ideal and realized scan times is less than that found in other recent works on fast brain imaging, and emphasizes the importance of accounting for more than just sequence time when predicting total examination time.(9) In our study, MR technologists were the largest potentially modifiable source of variation in MRI exam duration in this study. However, it should be noted that there is a significant residual standard deviation in the final model after accounting for the portion attributable to the technologist with a much larger variation between exams than between technologists. The cause of the variation attributable to the technologist could not be assessed with this data set and future work to explore the underlying causal reasons for this variation are of ongoing interest. Potential reasons contributing to this variation could be attributable to a number of factors, including individual differences in workflow efficiency or to a greater diligence in repeating compromised MRI sequences. Previous works have examined automation of intersequence adjustments, with favorable impacts on overall examination time and a decrease in exam length variability(9, 10) Automation of these tasks could provide a method to decrease the exam time variability associated with the performing technologist while also freeing the technologist to perform other clinical tasks.
Other factors found to correlate with variation in MRI exam duration include male gender (patient) and inpatient/outpatient/emergency room status. The gender variation could be in part attributable to differences in patient size and resultant scan field of view, but that is not fully addressed in this data set. Variation due to inpatient/outpatient/emergency room status may well be due to the presence of distracting pain, injuries, or other acute care challenges. Surprisingly, the use of sedation did not influence exam time. However, this may be due to offsetting effects of decreased motion with the need for increased patient monitoring.
However, these factors do not explain the majority of the exam variability found in the statistical model. This suggests there could be other factors outside of those examined in this work which could be influencing MRI exam length variation. More extensive modeling, perhaps utilizing a non-linear (e.g., artificial intelligence) approach to more completely assess for predictors within the PACS and the electronic medical record data could be revealing. In addition to working to minimize the underlying variability, MRI workflow could be designed to minimize the impact of variability on scheduling efficiency. If identically capable MRI devices are “co-scheduled” such that the next available patient is placed in the next available scanner, the individual variability can be spread over the pool of MRI devices, such that the overall scanner variability is reduced by the square root of the number of linked MRI devices.
There are some limitations to this study including the single institution nature of the evaluation. This study also focused on commonly performed neuroradiology related MRI examinations in order to provide a more homogenous study population and to avoid potential confounders due to differences in MRI protocoling practices between academic sections. The definition of exam length is somewhat arbitrary and in this case was defined to allow a fully automated measurement of exam times and avoid reliance on self-reported exam end times. A more comprehensive definition of exam length would likely include patient positioning and set-up times, as well as patient transfer and room cleaning times. Further studies are necessary to quantify the variation in MRI exam length across different practice settings, across the spectrum of MRI exam types, and to assess the contribution of positioning, transfer and room preparation to MRI availability.
In conclusion, there is a substantial variation in measured MRI exam duration for neuroradiology related MRI exams, even when exams are performed with identical MRI protocols. Factors associated with increased examination times include inpatient status, emergency department status, male gender and the performing technologist. While the performing technologist was found to have the greatest contribution to exam length variation in the multivariate model, it should be noted that there is still a greater variation between exams than between technologists.
Table 1.
Clinical Characteristics of Patients and MRI Examinations
| Characterstic | Number of cases (%) |
|---|---|
| Sex | |
| Female | 1516 (56%) |
| Male | 1189 (44%) |
| MRI Field Strength | |
| 1.5 T | 1813 (67%) |
| 3.0 T | 892 (33%) |
| Sedation or Anesthesia | 324 (12%) |
| Patient Status | |
| Inpatient | 484 (18%) |
| Outpatient | 1780 (66%) |
| Emergency Department | 441 (16%) |
Acknowledgments
Statistical support for this project was provided by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. J-P.J.Y was supported by the Department of Radiology at the University of Wisconsin-Madison School of Medicine and Public Health, the Brain and Behavior Research Foundation (NARSAD) Young Investigator Grant, and the University of Wisconsin Institute for Clinical and Translational Research KL2 Scholars Program (NCATS UL1TR000427). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosures:
The authors have no conflicts of interest related to the material discussed in this article.
REFERENCES:
- 1.Flaherty S, Mortele KJ, and Young GJ, Utilization Trends in Diagnostic Imaging for a Commercially Insured Population: A Study of Massachusetts Residents 2009 to 2013. J Am Coll Radiol, 2018. 15(6): p. 834–841. [DOI] [PubMed] [Google Scholar]
- 2.Rosman DA, Duszak R Jr., Wang W, et al. , Changing Utilization of Noninvasive Diagnostic Imaging Over 2 Decades: An Examination Family-Focused Analysis of Medicare Claims Using the Neiman Imaging Types of Service Categorization System. AJR Am J Roentgenol, 2018. 210(2): p. 364–368. [DOI] [PubMed] [Google Scholar]
- 3.Beker K, Garces-Descovich A, Mangosing J, et al. , Optimizing MRI Logistics: Prospective Analysis of Performance, Efficiency, and Patient Throughput. AJR Am J Roentgenol, 2017. 209(4): p. 836–844. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien JJ, Stormann J, Roche K, et al. , Optimizing MRI Logistics: Focused Process Improvements Can Increase Throughput in an Academic Radiology Department. AJR Am J Roentgenol, 2017. 208(2): p. W38–W44. [DOI] [PubMed] [Google Scholar]
- 5.Kruskal JB, Reedy A, Pascal L, et al. , Quality initiatives: lean approach to improving performance and efficiency in a radiology department. Radiographics, 2012. 32(2): p. 573–87. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, Hefke A, Figiel J, et al. , Enhancing same-day access to magnetic resonance imaging. J Am Coll Radiol, 2011. 8(9): p. 649–56. [DOI] [PubMed] [Google Scholar]
- 7.Edelstein WA, Mahesh M, and Carrino JA, MRI: time is dose--and money and versatility. J Am Coll Radiol, 2010. 7(8): p. 650–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roth CJ, Boll DT, Chea YW, et al. , Implementation of graphic user interface screen capture solution for workflow assessment of abdominal MR examinations valuable tool to analyze discrepancies in expected and experienced MR table time. Acad Radiol, 2009. 16(10): p. 1286–91. [DOI] [PubMed] [Google Scholar]
- 9.Prakkamakul S, Witzel T, Huang S, et al. , Ultrafast Brain MRI: Clinical Deployment and Comparison to Conventional Brain MRI at 3T. J Neuroimaging, 2016. 26(5): p. 503–10. [DOI] [PubMed] [Google Scholar]
- 10.Moenninghoff C, Umutlu L, Kloeters C, et al. , Workflow efficiency of two 1.5 T MR scanners with and without an automated user interface for head examinations. Acad Radiol, 2013. 20(6): p. 721–30. [DOI] [PubMed] [Google Scholar]