Abstract
IMPORTANCE:
Practice guidelines recommend that clinicians engage patients in treatment decisions and explain atherosclerotic cardiovascular disease (ASCVD) risk, but do not describe how to communicate risk most effectively.
OBJECTIVE:
To determine how the ASCVD risk time horizon, outcome, and presentation format affect risk perceptions and treatment preferences.
DESIGN:
Participants were presented 3 independent scenarios (representing the same hypothetical patient) and asked to rate perceived risk and willingness to take medication to lower risk: 1) 15% 10-year ASCVD event risk, 2) 4% 10-year cardiovascular disease (CVD) death risk, and 3) 50% lifetime ASCVD event risk.
SETTING:
140 U.S. cardiology, primary care, and endocrinology practices from May 27, 2015, through November 12, 2015.
PARTICIPANTS:
3566 participants from the Patient and Provider Assessment of Lipid Management Registry.
EXPOSURES:
Participants were randomized to receive risk estimates using numbers only, a bar graph, or a face pictogram.
RESULTS:
Of 3566 eligible participants, 2708 responded (76.9%, median age 67 years, 10.3% African American, 55.1% male). When shown lifetime ASCVD risk, respondents were more likely to consider risk “high to very high” than when presented 10-year ASCVD risk or CVD death risk (70.1% vs 31.4% vs 25.7%, respectively; both P<.0001). Treatment willingness was also highest for lifetime ASCVD risk (77.9% very willing) followed by 10-year ASCVD risk (68.1%) and 10-year CVD death risk (63.1%, both P<.0001). Compared with participants shown a bar graph or no graphic, those shown risk information with a pictogram had the lowest perception of disease severity and the lowest willingness to consider therapy. These findings were robust across demographic and socioeconomic subgroups.
CONCLUSIONS AND RELEVANCE:
The format, time horizon, and outcome used for risk estimation can all affect patient perceptions and should be considered when designing risk communication tools. When shown lifetime risk estimates, patients had higher risk perception and willingness for therapy than when shown 10-year estimates. Pictogram risk displays may decrease risk perception and consideration for treatment.
Keywords: cardiovascular disease, patient perception, risk estimation
Patient cardiovascular risk estimates are increasingly recommended to guide treatment decisions for atherosclerotic cardiovascular disease (ASCVD) prevention, including statin initiation and blood pressure treatment.1–3 Current practice guidelines recommend that providers engage patients as active participants in treatment decisions. Such shared decision-making requires that patients understand their individual risk and the potential benefit of prevention treatments.2 While current guidelines recommend discussing individual ASCVD risk with patients, less guidance is provided on the optimal risk estimate to provide and how to display it.
A variety of different ASCVD risk calculators are available. The current U.S. cholesterol and hypertension guidelines emphasize 10-year risk of myocardial infarction or stroke based on the Pooled Cohorts Equations, but also recommend considering treatment for those with a high lifetime risk of disease.2 Current European cholesterol guidelines emphasize the Systematic Coronary Risk Evaluation (SCORE) risk, which estimates a patient’s risk for cardiovascular disease (CVD) death in the next 10 years.4 Regardless of the tool used, the data presentation format may also affect patient perceptions. Many individuals have little understanding of numeracy and probability; therefore, studies have previously suggested that incorporating visual aids to portray risk (bar charts or face pictograms) may improve patient understanding and satisfaction.5–7
To date, research on risk communication has focused on the impact of risk communication approaches on patients’ overall risk perception, knowledge, and satisfaction.8–10 A recent systematic review suggests that communicating ASCVD risk may improve treatment of ASCVD risk factors, but the authors noted that research remains limited.11
Given that risk estimates are increasingly recommended to guide therapy, we sought to evaluate how different risk estimation and presentation formats affected patient perception of risk and patient willingness to initiate medication therapy. Specifically, we determined 1) whether an individual’s perception of disease risk severity varied depending on whether he or she was presented with an estimate of 10-year ASCVD risk, lifetime ASCVD risk, or 10-year risk of CVD death for a given patient risk factor scenario; 2) whether changing these risk estimate types affected an individual’s reported willingness to take medication therapy to reduce the risk of ASCVD; 3) whether the format of visual aids that accompanied the risks estimate would alter either disease perception and/or treatment preferences; and 4) the degree to which these conclusions were robust across a variety of patient age, education, or numeracy levels.
METHODS
The Patient and Provider Assessment of Lipid Management (PALM) registry was conducted across 140 U.S. cardiology, primary care, and endocrinology practices from May 27, 2015, through November 12, 2015.12,13 Participants in the registry provided signed informed consent at the time of their physician visit, after which they completed an electronic survey, administered via an iPad. The survey was designed to collect information about participants’ prior statin use and beliefs about ASCVD. Patient characteristics, including education, income, and race were obtained by self-report. Numeracy was assessed using the Subjective Numeracy ability subscale, a four-item scale to assess an individual’s perceived numerical ability.14 Medical record abstractions for clinical characteristics were performed by trained study coordinators at each site.
Overall, 3566 of the PALM participants were randomly selected to answer a series of questions about ASCVD risk based on a hypothetical patient with elevated 10-year and lifetsime risk. First, each patient was asked to imagine that their doctor told them that they had a 15% chance of a heart attack or stroke in the next 10 years. They were then asked to rate the severity of the risk estimate using a sliding scale (very low, low, medium, high, and very high), and to indicate their willingness to take a medication to reduce their risk of disease by approximately one third (very unwilling, slightly unwilling, possibly, somewhat willing, or very willing). Next, the patient was asked the same questions, but instead of a 15% 10-year risk of stroke or MI, was asked to consider a 4% chance of CV death in 10-years. Finally, the questions were repeated for a lifetime risk of stroke or MI of 50%. These scenarios were presented independently. However, the scenarios were constructed based on a hypothetical individual with high short- and long-term risk. The thresholds were chosen to represent an individual at high short- and long-term risk and for whom current U.S. guidelines would recommend statin therapy. Among those presented with these survey questions, participants were further randomized to be presented with the risk scenarios in one of 3 different formats: 1) questions presented as text only, 2) questions presented with an accompanying bar graph, or 3) questions presented with an accompanying face pictogram (eFigure 2 in the Supplement). All PALM surveys were conducted on an app designed for this study, which took patients through the informed consent process and the survey; randomization was conducted by the app itself. The sample size for this analysis was determined by the sample size of the overall PALM registry. We prespecified that half of participants would receive these risk questions, with equal distribution into the three arms (bar graph, pictorgram, or text).
Participants who skipped the risk questions or who reported “I don’t know” or “I don’t understand” were excluded from analyses comparing risk perception and therapy willingness. The proportion of participants who reported perceived risk as high or very high was compared for 10-year ASCVD risk, SCORE CVD death risk, and lifetime ASCVD risk information. Similarly, the proportions of adults who reported being “willing or very willing” to take therapy based on that risk were compared across risk information groups using McNemar’s tests. To determine the association between perceived risk and willingness to take therapy, the odds that a participant reporting willingness for therapy given a high to very high perceived risk were calculated within each scenario using conditional logistic regression to account for within-participant correlation.
The potential effect of risk presentation format was evaluated by comparing the proportions of participants who reported high to very high perceived risk and willingness for therapy when shown information using a bar graph, a face pictogram, or text alone for each question. Logistic regression was used to estimate differences in the odds of reporting high perceived risk or high therapy willingness by type of visual support used, stratified by age, education, numeracy, ASCVD status, and statin utilization. The impact of age (< or ≥65 years), numeracy (top 50th percentile vs bottom 50th percentile), education (at least some college vs no college), ASCVD status, and statin treatment status on risk perception and therapy willingness was evaluated using logistic regression. Interaction terms were created to assess whether differences in risk perception or therapy willingness seen by risk horizon varied by age, education, numeracy, ASCVD, or statin utilization.
To account for multiple comparisons, a 2-tailed test with an alpha of .01 was used to establish statistical significance. Sites obtained local institutional review board approval. The PALM Registry was registered in clinicaltrials.gov (). For this analysis, a prespecified statistical analysis plan was followed, with primary analyses conducted between November 2016 and January 2017.
RESULTS
Of the 3566 PALM participants randomized for this analysis, 1022 were shown questions with text alone, 1489 were shown a bar graph, and 1046 were shown face pictograms. Of these, 858 participants (24.1%) either skipped the risk questions or marked “I don’t know” or “I don’t understand,” for a final sample size of 2708. Characteristics of those participants are presented in Table 1. Among responders, the median age was 67.0 years, 55.1% were male, 46.1% had prior ASCVD, 87.4% self-reported white race, and 63.3% had private insurance.
Table 1.
Characteristics of Patients Participating in PALM Registry Survey Risk Questions
| Non-Responder
Characteristics N=858 |
P-value* | Overall Responder
Characteristics N=2708 |
Text Only (N=757) |
Bar Graph (N=1164) |
Pictogram (N=787) |
|
|---|---|---|---|---|---|---|
| Age, y (median, IQR) | 69.0 (61.0–76.0) | <.0001 | 67 (59.0–74.0) | 67 (59.0–74.0) | 67 (59.0–74.0) | 67 (59.0–75.0) |
| Numeracy score (median, IQR) | 15.0 (9.3–20.0) | <.0001 | 17 (12.0–21.0) | 16 (12.0–21.0) | 17 (12.0–21.0) | 16 (12.0–21.0) |
| Prior ASCVD | 385 (44.9%) | 0.5217 | 1249 (46.1%) | 348 (46.0%) | 548 (47.1%) | 353 (44.9%) |
| Male sex | 440 (51.3%) | 0.0530 | 1491 (55.1%) | 424 (56.0%) | 651 (55.9%) | 416 (52.9%) |
| Race | <.0001 | |||||
| White | 694 (80.9%) | 2366 (87.4%) | 664 (87.7%) | 1020 (87.6%) | 682 (86.7%) | |
| Black | 138 (16.1%) | 280 (10.3%) | 73 (9.6%) | 120 (10.3%) | 87 (11.1%) | |
| Other/unknown | 26 (3.0%) | 62 (2.3%) | 20 (2.6%) | 24 (2.1%) | 18 (2.3%) | |
| Education | <.0001 | |||||
| Below college | 326 (38.0%) | 922 (34.0%) | 254 (33.6%) | 379 (32.6%) | 289 (36.7%) | |
| College or above | 508 (59.2%) | 1760 (65.0%) | 493 (65.1%) | 778 (66.8%) | 489 (62.1%) | |
| Missing | 24 (2.8%) | 26 (1.0%) | 10 (1.3%) | 7 (0.6%) | 9 (1.1%) | |
| Income | 0.0927 | |||||
| <35,000 | 219 (25.5%) | 620 (22.9%) | 178 (23.5%) | 260 (22.3%) | 182 (23.1%) | |
| 35,000–75,000 | 207 (24.1%) | 607 (22.4%) | 156 (20.6%) | 268 (23.0%) | 183 (23.3%) | |
| 75,000–100,000 | 54 (6.3%) | 229 (8.5%) | 59 (7.8%) | 108 (9.3%) | 62 (7.9%) | |
| ≥100,000 | 107 (12.5%) | 383 (14.1%) | 111 (14.7%) | 177 (15.2%) | 95 (12.1%) | |
| Missing/refused/don’t know | 271 (31.6%) | 869 (32.1%) | 253 (33.4%) | 351 (30.2%) | 265 (33.7%) | |
| Insurance | 0.0077 | |||||
| Private | 498 (58.0%) | 1715 (63.3%) | 478 (63.1%) | 748 (64.3%) | 489 (62.1%) | |
| Medicare | 279 (32.5%) | 758 (28.0%) | 218 (28.8%) | 318 (27.3%) | 222 (28.2%) | |
| Medicaid | 26 (3.0%) | 92 (3.4%) | 18 (2.4%) | 37 (3.2%) | 37 (4.7%) | |
| No insurance | 14 (1.6%) | 56 (2.1%) | 16 (2.1%) | 25 (2.1%) | 15 (1.9%) | |
| Others | 21 (2.4%) | 57 (2.1%) | 16 (2.1%) | 29 (2.5%) | 12 (1.5%) | |
| Missing | 20 (2.3%) | 30 (1.1%) | 11 (1.5%) | 7 (0.6%) | 12 (1.5%) | |
| Clinic type | 0.0047 | |||||
| Cardiology | 263 (30.7%) | 996 (36.8%) | 276 (36.5%) | 462 (39.7%) | 258 (32.8%) | |
| Primary care | 376 (43.8%) | 1075 (39.7%) | 300 (39.6%) | 445 (38.2%) | 330 (41.9%) | |
| Other | 219 (25.5%) | 637 (23.5%) | 181 (23.9%) | 257 (22.1%) | 199 (25.3%) | |
| Aspirin use | 412 (48.0%) | 0.0443 | 1407 (52.0%) | 382 (50.5%) | 631 (54.2%) | 394 (50.1%) |
| Statin use | 600 (69.9%) | 0.0242 | 2000 (73.9%) | 543 (71.7%) | 887 (76.2%) | 570 (72.4%) |
| BP medication use | 670 (78.1%) | 0.3293 | 2071 (76.5%) | 585 (77.3%) | 893 (76.7%) | 593 (75.3%) |
P-value comparing responders to nonresponders
Data are n (%) except where indicated.
ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; PALM, Patient and Provider Assessment of Lipid Management.
Information about those who did and did not answer the questions about risk (defined as complete responses to all questions regarding risk) is also shown in Table 1. Those who did not respond to risk questions were older (median age 69 vs 67 years, P<.001), had lower subjective numeracy scores (median 15 vs 17, P<.001), were more often black race (16.1% vs 10.3%, P<.001), completed less education (59.2% had at least some college vs 65.0%, P<.001), and were less likely to have private insurance (58.0 vs 63.3%, P=.007). There was no difference in aspirin (52.0 vs 48.0%, P=.04) or statin (73.9 vs 69.9, P=.02) utilization between the 2 groups. There was no difference in survey response rate by which format patients were presented (no graphic, bar graph, or pictogram, P=.09), nor were there statistically significant differences in the characteristics of patients randomized to the pictogram, bar graph, or text-only version of the survey (eTable 1 in the Supplement). Many patients had partial responses to the survey, therefore the response rates for individual questions were higher than the response rate for the complete set of risk questions. eTable 2 shows question-specific response rates. Characteristics of subgroups of participants presented with face pictograms, bar graphs, and text-only versions of the survey, as well as characteristics of non-responders by version type, are shown in eTables 3–5.
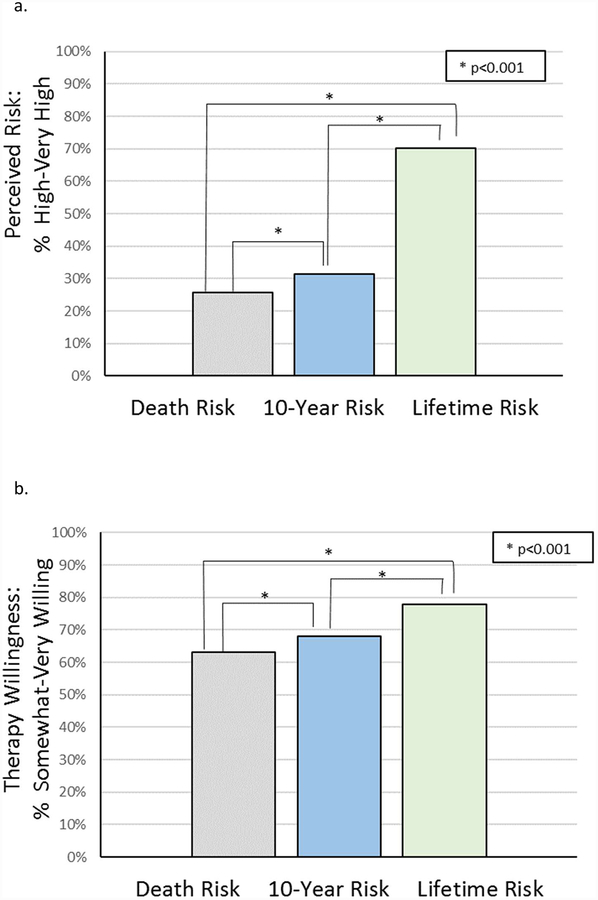
Figure 1 shows participant-perceived risk severity and willingness for therapy for each risk estimate (15% 10-year ASCVD risk, 50% lifetime ASCVD risk, and 4% 10-year CVD death risk). Participants reported the lowest perceived risk when shown risk of CVD death and highest perceived risk when shown lifetime ASCVD risk; 70.1% of participants perceived a lifetime risk of 50% to be “high to very high,” compared with 31.4% when shown a 10-year ASCVD risk of 15%, and 25.7% when shown a 10-year CVD death risk of 4%. Similarly, participants were most likely to report being willing to take medication therapy to lower their risk of heart attack or stroke when presented with a 50% lifetime ASCVD risk. However, the differences by time horizon were attenuated for therapy willingness compared with what was observed for risk perception. When shown a 50% lifetime risk, 77.9% of participants reported willingness to take medication therapy, compared with 68.1% (P<.001) of participants when shown a 15% 10-year risk, and 63.1% of participants when shown a 4% 10-year CVD death risk (P<.001).
Figure 1:
Patient-perceived risk severity (a) and willingness for drug therapy (b) when shown 10-year atherosclerotic cardiovascular disease (ASCVD) death risk of 4%, 10-year ASCVD risk of 15%, or lifetime ASCVD risk of 50%.
Participants who reported higher perceived risk also reported increased willingness to take therapy to reduce risk. When shown a 10-year ASCVD risk of 15%, participants who reported perceived risk to be high to very high had a 2.1-fold increased odds of also reporting being very willing to take therapy to lower that risk (OR, 2.1; 95% confidence interval [CI], 1.86–2.44). Similar associations were seen between perceived risk and willingness for therapy when shown a 4% 10-year CVD death risk (OR, 3.45; 95% CI, 3.00–3.98) and when shown a 50% ASCVD lifetime risk (OR, 3.27; 95% CI, 2.89–3.70).
Subgroup Analysis by Age, Education, Numeracy, ASCVD Status, and Statin Use
Differences in risk perception and therapy willingness were compared by education, numeracy, age, ASCVD status, and statin utilization (Table 2). Statin use (OR, 1.27; 95% CI, 1.14–1.41), prior ASCVD (OR, 1.28; 95% CI, 1.16–1.39), younger age (OR, 1.20; 95% CI, 1.09–1.32), and higher educational levels (OR, 1.18; 95% CI, 1.06–1.30) were all associated with increased perceived risk. Statin use (OR, 2.13; 95% CI, 1.85–2.44), prior ASCVD (OR, 1.61; 95% CI 1.43–1.82), higher education (OR, 1.33; 95% CI, 1.16–1.52), and higher numeracy scores (OR, 1.45; 95% CI, 1.28–1.64) were associated with increased willingness for therapy. The association between these factors and perceived risk and willingness for therapy was generally consistent by risk estimate used, i.e. younger adults were more likely to report risk as high compared with older adults across all 3 scenarios (10-year ASCVD: 33.8% vs 29.7%, 10-year CVD death 27.4% vs 24.6%, or lifetime ASCVD risk 74.3% vs 67.4%).
Table 2.
Impact of Education, Numeracy, Age, Prior ASCVD, and Statin Use on Perceived Risk and Therapy Willingness
| Education | Numeracy | Age | Prior ASCVD | Statin | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <College | At least some college | P-value | Bottom 50th percent | Top 50th percent | P-value | <65 | ≥65 | P-value | No Prior ASCVD | Prior ASCVD | P-value | No Statin | On Statin | P-value | |
| 15% 10-year ASCVD risk | |||||||||||||||
| Perceived risk: high to very high, n (%) | 318 (29.9%) | 655 (32.3%) | .17 | 504 (33.1%) | 472 (29.9%) | .05 | 419 (33.8%) | 563 (29.7%) | .016 | 475 (28.3%) | 507 (34.9%) | <.0001 | 235 (28.2%) | 747 (32.5%) | .023 |
| Therapy willingness: somewhat to very, n (%) | 714 (64.3%) | 1486 (70.7%) | .0002 | 1036 (64.1%) | 1170 (72.9%) | <.0001 | 891 (69.3%) | 1322 (67.2%) | .20 | 1096 (62.7%) | 1117 (74.3%) | <.0001 | 480 (56.1%) | 1733 (72.3%) | <.0001 |
| 4% 10-year CVD death risk | |||||||||||||||
| Perceived risk: high to very high, n (%) | 315 (27.8%) | 518 (24.6%) | .045 | 470 (28.9%) | 367 (22.6%) | <.0001 | 354 (27.4%) | 490 (24.6%) | .078 | 405 (23.0%) | 439 (28.9%) | .0001 | 195 (22.2%) | 649 (27.0%) | .005 |
| Therapy willingness: somewhat to very, n (%) | 705 (61.0%) | 1379 (64.7%) | .037 | 1002 (60.2%) | 1088 (66.7%) | <.0001 | 838 (64.4%) | 1259 (62.2%) | .20 | 1038 (57.7%) | 1059 (69.4%) | <.0001 | 436 (49.2%) | 1661 (68.2%) | <.0001 |
| 50% lifetime ASCVD risk | |||||||||||||||
| Perceived risk: high to very high, n (%) | 721 (62.5%) | 1616 (74.8%) | <.0001 | 1110 (66.7%) | 1236 (74.4%) | <.0001 | 979 (74.3%) | 1374 (67.4%) | <.0001 | 1221 (67.5%) | 1132 (73.2%) | .0003 | 577 (64.3%) | 1776 (72.3%) | <.0001 |
| Therapy willingness: somewhat to very, n (%) | 859 (73.5%) | 1746 (81.1%) | <.0001 | 1256 (74.5%) | 1358 (82.5%) | <.0001 | 1035 (78.9%) | 1586 (77.3%) | .29 | 1356 (74.8%) | 1265 (81.6%) | <.0001 | 601 (67.1%) | 2020 (81.9%) | <.0001 |
| Odds ratio across all horizons (95% CI) | At least some college vs none | Top 50th percentile vs bottom | Age <65 vs ≥65 | Prior ASCVD vs none | On statin vs none | ||||||||||
| Perceived risk | 1.18 (1.06–1.30) | .002 | 0.97 (0.88–1.06) | .56 | 1.20 (1.09–1.32) | .0001 | 1.28 (1.16–1.39) | .0000 | 1.27 (1.14–1.41) | .0000 | |||||
| Therapy willingness | 1.33 (1.16–1.52) | .0000 | 1.45 (1.28–1.64) | .0000 | 1.09 (0.97–1.24) | .16 | 1.61 (1.43–1.82) | .0000 | 2.13 (1.85–2.44) | .0000 | |||||
Statistical significance for P-values <.01 due to multiple comparisons.
ASCVD, atherosclerotic cardiovascular disease; CVD, cardiovascular disease.
In formal interaction testing, the magnitude of the differences in risk perception by scenario, but not the directionality of those differences, varied by education and numeracy, but not by age, prior ASCVD, or statin use. Specifically, across educational groups perceived risk was higher for 10-year ASCVD risk compared with 10-year CVD death risk, but that difference was greater in those with at least some college (p=0.002). Similarly, perceived risk was higher with lifetime risk compared with 10-year ASCVD risk across both educational groups and numeracy levels. However, this difference was amplified in those with higher numeracy (p<0.001) and higher education (p<0.001). There was no interaction between the impact of risk estimate provided and willingness for therapy by education, numeracy, age, prior ASCVD, or statin use.
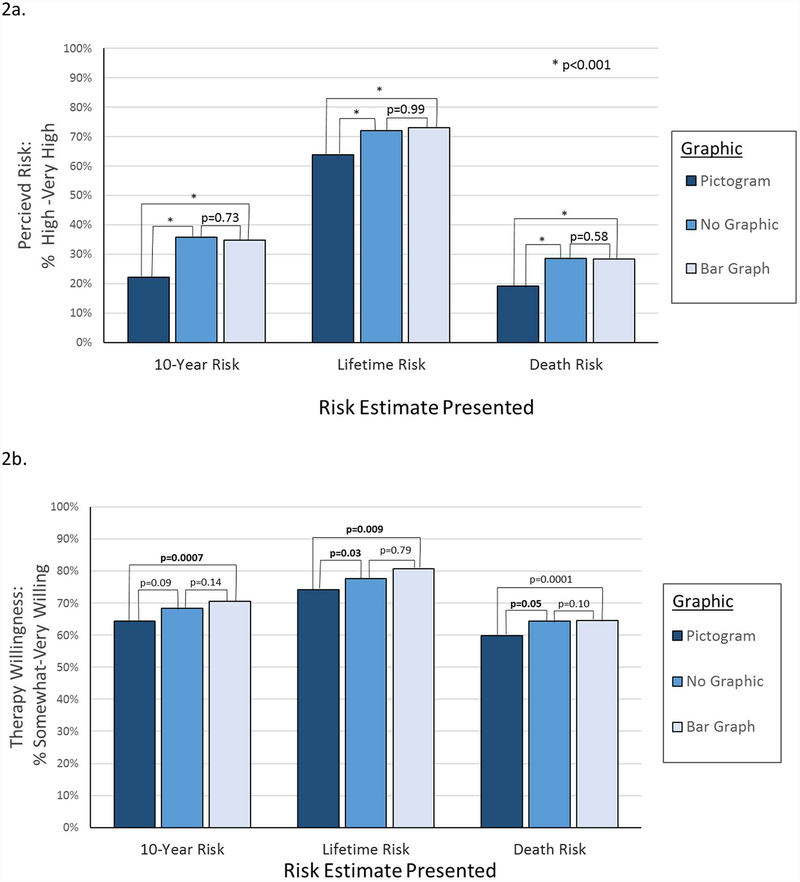
Format of Risk Presentation
Figure 2 shows the proportions of participants reporting high perceived risk or high willingness for drug therapy when shown a face pictogram, bar graph, or no graphic, stratified by each risk estimate horizon used. When risk estimates were shown with a pictogram, perceived risk was consistently lower than when presented as a bar graph or without a graphic for all 3 risk estimate horizons. For example, when asked about a 10-year ASCVD event risk of 15%, 22.1% of individuals shown a pictogram reported high perceived risk, compared with 35.7% shown no graphic and 34.8% shown a bar graph (P<.001 for both). Similarly, approximately 10% fewer adults shown a pictogram reported high perceived risk than those shown a bar graph or no graphic for lifetime ASCVD risk and 10-year CVD death risk. There was no significant difference in perceived risk between groups shown a bar graph or no graphic. Similarly, willingness for drug therapy was somewhat lower when presented with a face pictogram compared with a bar graph, although the magnitude of difference was lower. Across all 3 risk scenarios, 5–6% more adults reported high therapy willingness when shown a bar graph compared to a pictogram.
Figure 2:
Perceived risk (a) and willingness for therapy (b) by risk estimate when shown with text only, bar graphs, or pictogram.
DISCUSSION
There are multiple means to provide risk estimates to adults to estimate their risk for CVD events, including 10-year risk of ASCVD event, lifetime risk of ASCVD events, and risk of CVD death. In a representative community-based sample, we found that perception of the severity of risk as well as potential willingness to take medication therapy to lower that risk varied by which calculator was used, as well as how the calculator was presented. Severity of risk perception and willingness to take therapy were highest when individuals were shown a 10-year lifetime ASCVD risk of 50% and lowest when shown a 10-year risk of CVD death of 4%, even though these estimates could represent the same patient. When the same disease risk estimates were shown with a faces pictogram compared with a bar graph or no graphics, participants had significantly lower disease risk perception and willingness to take therapies.
Although our survey was piloted for understanding, many individuals (up to 1 in 4) were unable to answer or understand the questions about risk. While we cannot fully determine the proportion of patients who skipped these questions due to lack of understanding versus a desire to complete the survey more quickly, few (<2%) skipped demographic questions about insurance or education, which were placed after the risk questions in the survey. The higher rate of missing responses for these questions may have been due to poor comprehension of the concept of risk estimation. Individuals with missing responses were older, had lower education, income, and numeracy, and were less likely to have private insurance. However, over half of those who skipped the risk questions had at least some college, and there was considerable overlap in numeracy scores between the 2 groups. Thus, clinicians cannot rely on objective measures of education to determine who may or may not understand concepts of risk. When discussing risk with their patients, regardless of the risk horizon estimate used, clinicians should explain risk in qualitative terms (e.g., high vs low) or put risk into context using vascular age or standardized risk percentiles.15
Individual characteristics such as age, education, and numeracy may affect not only risk comprehension but also qualitative interpretation of risk. Across all risk horizons estimates, therapy willingness was generally higher in those who had at least some college compared to no college, and in those in the top half of numeracy compared with the bottom half. Younger adults generally reported greater perceived risk severity than older adults, but this did not translate into differences in willingness to take therapy by age group. Although adults were asked to consider a hypothetical patient, those with prior ASCVD had consistently higher perceived risk and therapy willingness than those without.
Perceived disease risk varied considerably when individuals were presented risk estimates generated from different risk tools. This underscores how the qualitative perception of risk can vary even when “accurate” or “unbiased” risk estimates are used. A provider who communicates that an individual has a 50% chance of a heart attack or stroke in his or her lifetime may be as factually correct as a provider who informs the same individual about a 4% chance of dying from a heart attack or stroke in the next 10 years, but the impact of these “equivalent” pieces of information on the patient may be markedly different. In general, a lifetime risk estimate in a person will be much higher than 10-year CVD risk up to age 55, which will be higher than 10-year risk of CVD mortality. Our data suggest that individuals are most affected by the estimate that produces the highest absolute number.
Participants with higher risk perception were more likely to report higher willingness to take drug therapy to lower their risk for all risk estimates presented. As a result, the proportion of adults reporting willingness to take drug therapy to lower their risk was highest for lifetime risk, followed by 10-year risk, and then mortality risk. Nearly 15% more participants reported willingness to take drug therapy when shown a 50% lifetime risk than when shown a 4% chance of CVD death in the next 10 years. However, the differences in willingness to take drug therapy were lower than differences in risk perception. Although only 25.7% of participants shown a 4% 10-year risk of CVD death reported risk to be high to very high, over 60% reported willingness to take therapy to lower risk. This demonstrates that perceived risk is only one of many factors individuals consider when deciding whether to initiate preventive therapies.
Beyond the risk calculator used, differences in how that risk is communicated to patients may affect both patient-perceived risk and willingness to engage initiate drug therapy. Across all scenarios, when participants were shown a risk estimate with a corresponding pictogram, perceived risk and willingness for therapy was lower than when the risk estimate was shown as a bar graph. While pictograms may help individuals better understand the concept of a proportion, the number of “happy” faces in the diagram may lead to qualitatively lower risk estimates. This reinforces the need to test the impact of decision aids not only on patient satisfaction and risk understanding, but also on therapy uptake and adherence.16 In the future, guidelines around risk estimation may also consider providing evidence-based guidance around risk communcation.
This study has several limitations. First, all participants received the same 10-year and lifetime risk estimates meant to correspond to a high-risk patient rather than personalized risk scores. Second, we evaluated willingness for drug therapy based on a hypothetical medication that would “lower risk by about a third.” We did not specify a particular medication in order to prevent individual preconceived biases about specific therapies from affecting the results. Third, in order to focus on risk perception, we did not test different formats for showing therapeutic effectiveness (e.g., relative vs absolute risk reduction or number needed to treat), which may impact willingness for drug therapy. Fourth, we presented the risk estimates individually to patients, whereas in clinical practice, clinicians may present multiple risk estimates. Finally, nearly 1 in 4 survey respondents skipped the questions about risk, with nonresponders having lower numeracy and education, higher age, and less likely to have private insurance. Thus, the generalizability of these findings to populations with less education, insurance, and overall numeracy may be limited.
CONCLUSION
Integrating risk-based treatment paradigms into clinical practice requires effective strategies to accurately communicate risk with patients. Individuals may perceive their risk to be higher and be more willing to engage in therapy when shown lifetime risk compared with 10-year fatal or nonfatal risk estimates, regardless of education, numeracy level, or age. Using face pictograms to display risk may lead to lower qualitative assessments of perceived risk. Effective risk communication tools should consider both which risk score is used and also how risk estimates are displayed.
Supplementary Material
Key Points.
Question:
How do different presentation formats for atherosclerotic cardiovascular disease (ASCVD) risk affect patient perceptions and treatment preferences?
Findings:
Risk perception and therapy willingness were highest when patients were shown estimates for lifetime risk, followed by 10-year ASCVD risk, then 10-year cardiovascular disease death risk. Using a pictogram led to lower risk perception and therapy willingness than a bar graph or no graphic.
Meaning:
Patient perceptions of ASCVD disease severity and treatment preferences can be affected by the tool used for risk communication, and risk perception can affect patient willingness to consider therapy.
Funding:
This study was supported by Sanofi Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Navar is supported by the National Institutes of Health, National Heart, Lung, and Blood Institute grant K01HL133416.
Role of the Funder/Sponsor: The sponsor contributed to the design of the study, interpretation of the data, and critical review of the manuscript, but played no role in data collection, management, or analysis. The decision to submit the manuscript for publication was controlled by authors at the Duke Clinical Research Institute.
Footnotes
Disclosures:
Navar: Dr. Navar reports research support from Amgen, Sanofi, and Regeneron; consulting fees from Amgen and Sanofi.
Wang: Dr. Wang reports research support from AstraZeneca, Boston Scientific, Bristol Myers Squibb, Daiichi Sankyo, Eli Lilly, Gilead, Pfizer, Regeneron; consultant/advisory/education from Merck, Gilead, Sanofi.
Mi: Dr. Mi reports no relevant disclosures.
Robinson: Dr. Robinson reports research support from Amarin, Amgen, Astra-Zeneca, Eli Lilly, Esai, GlaxoSmithKline, Merck, Pfizer, Regeneron/Sanofi, Takeda; consultant for Amgen, Eli Lilly, Merck, Pfizer, Regeneron, Sanofi.
Virani: Dr. Virani reports research support from American Diabetes Association, American Heart Association, U.S. Department of Veterans Affairs; honorarium from American College of Cardiology, National Lipid Association.
Roger: Dr. Roger reports no relevant disclosures.
Wilson: Dr. Wilson reports no relevant disclosures.
Goldberg: Dr. Goldberg reports research support from Amarin, Amgen, Pfizer, Regeneron/Sanofi; consulting for Regeneron/Sanofi, and Esperion; honorarium for editorial work Merck Manual.
Peterson: Dr. Peterson reports research support from Amgen, AstraZeneca, Merck, Sanofi; consulting for Amgen, AstraZeneca, Merck, and Sanofi Aventis.
References
- 1.Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. The Expert Panel. Arch Intern Med. 1988;148(1):36–69. [PubMed] [Google Scholar]
- 2.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017. November 7 pii: S0735–1097(17)41519–1. doi: 10.1016/j.jacc.2017.11.006. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Authors/Task Force Members: Catapano AL, Graham I, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) developed with the special contribution of the European Assocciation for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis. 2016;253:281–344. [DOI] [PubMed] [Google Scholar]
- 5.Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161(4):270–280. [DOI] [PubMed] [Google Scholar]
- 6.Goodyear-Smith F, Arroll B, Chan L, Jackson R, Wells S, Kenealy T. Patients prefer pictures to numbers to express cardiovascular benefit from treatment. Ann Fam Med. 2008;6(3):213–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards A, Thomas R, Williams R, Ellner AL, Brown P, Elwyn G. Presenting risk information to people with diabetes: evaluating effects and preferences for different formats by a web-based randomised controlled trial. Patient Educ Couns. 2006;63(3):336–349. [DOI] [PubMed] [Google Scholar]
- 8.Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koelewijn-van Loon MS, van der Weijden T, Ronda G, et al. Improving lifestyle and risk perception through patient involvement in nurse-led cardiovascular risk management: a cluster-randomized controlled trial in primary care. Prev Med. 2010;50(1–2):35–44. [DOI] [PubMed] [Google Scholar]
- 10.Krones T, Keller H, Sonnichsen A, et al. Absolute cardiovascular disease risk and shared decision making in primary care: a randomized controlled trial. Ann Fam Med. 2008;6(3):218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karmali KN, Persell SD, Perel P, Lloyd-Jones DM, Berendsen MA, Huffman MD. Risk scoring for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;3:CD006887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navar AM, Wang TY, Li S, et al. Lipid management in contemporary community practice: Results from the Provider Assessment of Lipid Management (PALM) registry. Am Heart J. 2017;193:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navar AM, Wang TY, Goldberg AC, et al. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) registry. Am Heart J. 2015;170(5):865–871. [DOI] [PubMed] [Google Scholar]
- 14.Fagerlin A, Zikmund-Fisher BJ, Ubel PA, Jankovic A, Derry HA, Smith DM. Measuring numeracy without a math test: development of the Subjective Numeracy Scale. Med Decis Making. 2007;27(5):672–680. [DOI] [PubMed] [Google Scholar]
- 15.Navar AM, Pencina MJ, Mulder H, Elias P, Peterson ED. Improving patient risk communication: Translating cardiovascular risk into standardized risk percentil. Am Heart J. 2018;198:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann DM, Ponieman D, Montori VM, Arciniega J, McGinn T. The Statin Choice decision aid in primary care: a randomized trial. Patient Educ Couns. 2010;80(1):138–140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.