Abstract
Introduction
The avascular necrosis of the femoral head represents the death of bone tissue due to the lack of blood supply. The disease has a progressive evolution; it leads to femoral head collapse and severe arthritis when left untreated. The application of a pedicled bone flap graft is an effective treatment for femoral head necrosis. A pure Mg screw is a kind of degradable screw that can fix the grafted bone flap and prevent long-term stress occlusion and secondary dissection.
Case presentation
The report shows the results of the treatment of traumatic femoral head necrosis with a pedicled bone flap with pure Mg screw. A patient had avascular necrosis of the femoral head after 2 years of internal fixation of the femoral neck fracture. We removed the patient's internal fixation hollow nail, cleaned the necrotic bone tissue and took part of the same ipsilateral pedicle iliac bone graft in the femoral head defect with biodegradable pure Mg screw fixation. Within 2 years after the surgery, the patients had no significant progressive necrosis of the femoral head. Postoperative Harris scores showed that the patient's left hip function was significantly improved compared with his preoperative state. The pure Mg screw in the body had gradually degraded. After 2 years, the screw's diameter had been significantly reduced compared with 3 days after the surgery. The postoperative Harris score showed that the patient's left hip function was significantly improved compared with the second preoperative examination.
Discussion
The discussion includes the reasons for the choices of surgical approaches, the mode of pure Mg screw degradation and the postoperative functional assessment of the patient's left hip.
Conclusion
Pure Mg screw fixation pedicled bone flap transplantation is an effective surgical treatment for femoral head necrosis in young patients. Pure Mg screw is a biodegradable internal fixation device with good biocompatibility, which has a good clinical application prospects.
The translational potential of this article
Degradable pure Mg screw has the potential to preserve hip joint therapy for the treatment of femoral head necrosis.
Introduction
The avascular necrosis of the femoral head leads to the death of bone tissue due to the lack of blood supply [1], [2]. The logical treatment may be the removal of the dead bone and the restoration of the bony contents with a vascularized bone flap. Young people are not suitable for hip replacement surgery because of the limited life of the prosthesis. There are several surgical approaches, including core decompression [3], various osteotomies [4] and (vascularized [5], [6] or nonvascularized [7]) bone grafting, to preserve the hip for the treatment of avascular necrosis of the femoral head. Vascularized autogenous iliac crest transplantation is an effective treatment. However, there is a risk of bone flap loosening. Therefore, screw fixation is needed to increase the stability of the bone flap. But the nondegradable screw causes stress shielding and even needs to be removed by a secondary surgery. In our study, we present a case of a patient with a traumatic femoral neck fracture who developed avascular necrosis of the femoral head 2 years after hollow nail internal fixation of the femoral head. The patient was at the Association Research Circulation Osseous IIIB and used a vascular pedicled iliac crest transplantation. We chose to use a pure Mg screw to fix the flap, and the patient was provided with a written informed consent. The aim of this study was to observe the feasibility of pure Mg screw as a biodegradable material in the clinical treatment of femoral head necrosis. Postoperative radiographs were used for imaging evaluation, and the Harris scoring system was used for functional evaluation.
Case report
A 17-year-old boy had an internal fixation using compression hollow screws 2 years ago due to a femoral neck fracture 26 months ago. He was admitted to the hospital with pain in his left hip. Computed tomography (CT) showed that the patient's left femoral head had necrosis. The patient's internal fixation hollow screws (provided by Xiamen Double medical technology, China) had been removed and received an iliac flap transplantation, which was fixed with a pure Mg nail (provided by Dongguan Eontec Company, China). During the operation, the patient was placed in an oblique position at 45° to the right. A 10-cm incision was made on the proximal side of the left proximal femur. Three hollow internal fixation nails were removed, and 3 × 1 × 3 cm pedicled iliac flaps were used in the medial two-thirds of the fascia lata. A 2 × 3 window was opened at the junction of the femoral head and neck. The necrotic bone tissue was removed, and the pedicled bone flap was inserted and implanted into the cancellous bone (Fig. 1). The clinical study was approved by the Ethics Committee of General Hospital of Guangzhou Military Command of PLA, and written informed consents were obtained from the participant.
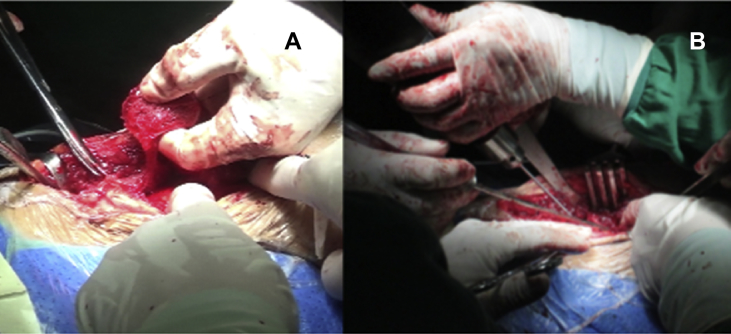
Figure 1.
Intraoperative photo. (A) Dissection of the pedicled iliac bone flap; (B) Fixation of the pedicled iliac bone flap with pure Mg screw.
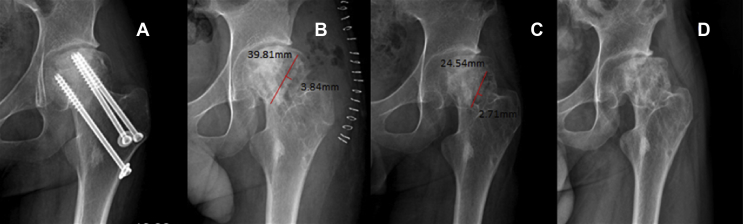
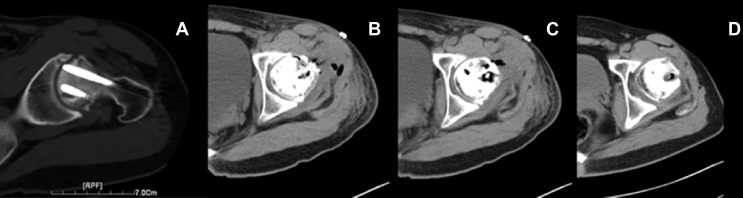
The operation duration was 125 min. About 200 mL of blood was lost during the operation. The incision healed 2 weeks after surgery. After operation, the X-ray image showed a pure Mg screw with a length of 39.81 mm and a diameter of 3.84 mm. One year later, the pure Mg screw with a length of 24.54 mm and a diameter of 2.71 mm was observed; the volume of the pure Mg screw decreased by about 69.5% after surgery in 1 year. There was no obvious pure Mg screw shadow in the X-ray image after 2 years (Fig. 2). One year after surgery, CT showed that the volume of the pure Mg screw was significantly reduced compared with 3 days after operation. The position of the bone flap was good, and it was fused with the surrounding bone. Two-year after operation, the pure Mg screw shadow was not obvious. The bone flap was almost completely fused, and the cortical bone was almost healed (Fig. 3). The preoperative Harris score was 37, the hip function was poor and the postoperative recovery score was 74 after walking. The hip function was better, and the hip function score was good 1 year after surgery. Compared with 1 year after surgery, the patient can walk farther after 2 years (Table 1).
Figure 2.
Radiographic images of the femoral head hip over time. (A) The patient was implanted with three compression hollow screws for femoral neck fracture, and the femoral head had necrosis after 26 months; (B) 3 days postoperatively; (C) 1 year postoperatively and (D) 2 years postoperatively. The femoral head was dislocated laterally.
Figure 3.
Representative CT diagram of the pure Mg screw over time. (A) The patient was implanted with three compression cannulated screws for femoral neck fracture, and the femoral head had necrosis after 26 months; (B) 3 days postoperatively; (C) 1 year postoperatively and (D) 2 years postoperatively. The pure Mg screw gradually degraded, and the bone flaps gradually almost merged.
Table 1.
Harris hip score at different time points.
| Project | Preoperative | Postoperative | One year | Two years |
|---|---|---|---|---|
| Pain | 10 | 35 | 40 | 40 |
| Daily activities | 4 | 10 | 13 | 13 |
| Gait | 13 | 16 | 16 | 16 |
| Distance | 2 | 4 | 5 | 8 |
| Deformity | 4 | 4 | 4 | 4 |
| Range of activity | 4 | 5 | 5 | 5 |
| Total | 37 | 74 | 83 | 86 |
Of 100 points, 90 points or more is excellent, 80–89 is better, 70–79 is still acceptable, less than 70 is poor. The patient had poor hip function before surgery, and the hip function was better after 1 year; compared with 1 year after surgery, the patient can walk farther after 2 years.
Discussion
There are many causes of femoral head necrosis. The pathogenesis is not clear. If it is not diagnosed and treated properly in time, the disease will easily lead to serious deterioration, affecting the patient's ability to work [8]. Early clinical diagnosis and treatment of the disease can effectively protect the joints and delay joint replacement time. Currently, there are many surgical methods, including femoral head decompression and osteotomy, for hip protection. Pedicled bone transplantation is categorized into vascular and nonvascular types [9]. Vascularized bone flap transplantation provides blood to the bone graft and transports osteoinductive growth factors and osteoblasts into the femoral head to promote the fusion of the bone flap to the femoral head.
We evaluated postoperative rehabilitation using X-ray films, CT images, and Harris scores [10]. Magnesium ions are absorbed by the body and participate in metabolism [11], [12], [13]. Physiological Mg ions are regulated by the kidneys and intestines. Magnesium ions participate in the formation of more than 200 enzymes and new bones in the body. A small proportion is used by muscles and other tissues, and the remaining is metabolized [14], [15], [16], [17]by the liver and kidneys. The serum magnesium levels of the patient were normal before and after surgery, and the patient's liver and kidney function was normal [18], [19]. Other degradable biomaterials include polylactic acid [20], polylactide carbonate, and polylactic-co-glycolic acid, but the use of screws made from these materials may cause implant breakage [21], adverse immune reactions [22], and other complications [23]. No studies have revealed that these complications may occur when pure Mg screws are used.
Harris score is an important clinical indicator of hip function recovery [24]. The Harris score of the patient was significantly improved compared with that before the operation, although X-ray analysis showed that the hip joint was subluxated after 1-year and 2-year postsurgery observations. X-ray and CT images showed that there was no continued necrosis of the femoral head because this procedure rebuilt the blood supply for the femoral head [25] and the pure Mg screw fixed the graft bone flap [26]. To the best of our knowledge, this is the first report of treatment of trauma-induced femoral head necrosis with pure Mg screw-fixed iliac flap with a 2-year follow-up. The surgical treatment was effective. For young people, it can effectively delay the time of total hip arthroplasty, avoiding multiple replacements due to the age of the joint prosthesis. Owing to the lack of available metal artifact reduction sequence magnetic resonance facility, it is difficult to show the changes of soft tissue during follow-up, which is one of the shortcomings of this study. As this study is a case report, the follow-up time is short and there is a lack of comparison to the efficacy of other surgical studies. Studies incorporating long-term follow-up and prospective multisample case are a necessity to confirm the clinical efficacy.
Ethics statement
The clinical study was approved by the Ethics Committee of General Hospital of Guangzhou Military Command of PLA, and written informed consents were obtained from the participant.
Conflicts of interest
The authors have no conflicts of interest to disclose in relation to this article.
Funding/support statement
The study was funded by the National Key Research and Development Program of China (2016YFB0700800, 2017YFB0702604); Science and Technology Planning Project of Guangdong Province (No.2017B030314139, 2015A030312004, 2014A020215025); The National Natural Science Foundation of China (31700880, 81601884), the Medical Center of Assessment, Prevention, Treatment of Bone & Joint Diseases and the Key Laboratory of Trauma & Tissue Repair of Tropical Area.
Contributor Information
Dewei Zhao, Email: zhaodewei2000@163.com.
Qingshui Yin, Email: gzgk_yqs@126.com.
Yu Zhang, Email: luck_2001@126.com.
References
- 1.Surgery J. 2007. Femoral-neck fractures in young adults in Young Adults * normal. [Google Scholar]
- 2.Moyaangeler J., Gianakos A.L., Villa J.C., Ni A., Lane J.M. Current concepts on osteonecrosis of the femoral head. World J Orthoped. 2015;6(8):590–601. doi: 10.5312/wjo.v6.i8.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mont M.A., Carbone J.J., Fairbank A.C. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res. 1996;324(324):169–178. doi: 10.1097/00003086-199603000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Matsusaki H., Noguchi M., Kawakami T., Tani T. Use of vascularized pedicle iliac bone graft combined with transtrochanteric rotational osteotomy in the treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 2005;125(2):95–101. doi: 10.1007/s00402-004-0777-z. [DOI] [PubMed] [Google Scholar]
- 5.Rd A.J., Urbaniak J.R. Avascular necrosis of the femoral head: role of vascularized bone grafts. Orthop Clin N Am. 2007;38(1):13. doi: 10.1016/j.ocl.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Eisenschenk A., Lautenbach M., Schwetlick G., Weber U. Treatment of femoral head necrosis with vascularized iliac crest transplants. Clin Orthop Relat Res. 2001;386(386):100–105. doi: 10.1097/00003086-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Urbaniak J.R., Coogan P.G., Gunneson E.B., Nunley J.A. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77(5):681–694. doi: 10.2106/00004623-199505000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Rd A.J., Urbaniak J.R. Avascular necrosis of the femoral head: role of vascularized bone grafts. Orthop Clin N Am. 2007;38(1):13–22. doi: 10.1016/j.ocl.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Zhao D., Xu D., Wang W., Cui X. Iliac graft vascularization for femoral head osteonecrosis. Clin Orthop Relat Res. 2006;442(442):171–179. doi: 10.1097/01.blo.0000181490.31424.96. [DOI] [PubMed] [Google Scholar]
- 10.Staiger M., Pietak A., Huadmai J., Dias G. Magnesium and its alloys as orthopedic biomaterials: a review. Biomaterials. 2006;27(9):1728–1734. doi: 10.1016/j.biomaterials.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Wang J., Witte F., Xi T., Zheng Y., Ke Y., Yang Y. Recommendation for modifying current cytotoxicity testing standards for biodegradable magnesium-based materials. Acta Biomater. 2015;21:237–249. doi: 10.1016/j.actbio.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Wang J., Xu J., Song B., Chow D.H., Shuhang P.Y., Qin L. Magnesium (Mg) based interference screws developed for promoting tendon graft incorporation in bone tunnel in rabbits. Acta Biomater. 2017;63:393–410. doi: 10.1016/j.actbio.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y., Xu J., Ruan Y.C., Yu M.K., O'Laughlin M., Wise H. Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat Med. 2016;22(10):1160–1169. doi: 10.1038/nm.4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao D., Witte F., Lu F., Wang J., Li J., Qin L. Current status on clinical applications of magnesium-based orthopaedic implants: a review from clinical translational perspective. Biomaterials. 2017;112:287–302. doi: 10.1016/j.biomaterials.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 15.Wang J., Wu Y., Li H., Liu Y., Bai X., Chau W. Magnesium alloy based interference screw developed for ACL reconstruction attenuates peri-tunnel bone loss in rabbits. Biomaterials. 2018;157:86. doi: 10.1016/j.biomaterials.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Tian L., Sheng Y., Huang L., Chow H.K., Chau W.H., Tang N. An innovative Mg/Ti hybrid fixation system developed for fracture fixation and healing enhancement at load-bearing skeletal site. Biomaterials. 2018:180. doi: 10.1016/j.biomaterials.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 17.Saris N.E., Mervaala E., Karppanen H., Khawaja J.A., Lewenstam A. Magnesium. An update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294(1–2):1–26. doi: 10.1016/s0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 18.Wang J., Xu J., Liu W., Li Y., Qin L. Biodegradable magnesium (Mg) implantation does not impose related metabolic disorders in rats with chronic renal failure. Sci Rep. 2016;6:26341. doi: 10.1038/srep26341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saris N.E., Mervaala E., Karppanen H., Khawaja J.A., Lewenstam A. Magnesium. An update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294(1–2):1–26. doi: 10.1016/s0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 20.Song B., Li W., Chen Z., Fu G., Li C., Liu W. Biomechanical comparison of pure magnesium interference screw and polylactic acid polymer interference screw in anterior cruciate ligament reconstruction—a cadaveric experimental study. J Orthop Translat. 2017;8(C):32–39. doi: 10.1016/j.jot.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lembeck B., Wülker N. Severe cartilage damage by broken poly-L-lactic acid (PLLA) interference screw after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(4):283–286. doi: 10.1007/s00167-004-0545-1. [DOI] [PubMed] [Google Scholar]
- 22.Mastrokalos D.S., Paessler H.H. Allergic reaction to biodegradable interference poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Arthroscopy: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2008;24(6):732. doi: 10.1016/j.arthro.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 23.Bach F.D., Carlier R.Y., Elis J.B., Mompoint D.M., Feydy A., Judet O. Anterior cruciate ligament reconstruction with bioabsorbable polyglycolic acid interference screws: MR imaging follow-up. Radiology. 2002;225(2):541–550. doi: 10.1148/radiol.2252010357. [DOI] [PubMed] [Google Scholar]
- 24.Mahomed N.N., Arndt D.C., Mcgrory B.J., Harris W.H. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16(5):575–580. doi: 10.1054/arth.2001.23716. [DOI] [PubMed] [Google Scholar]
- 25.Liu W.C., Chen S., Zheng L., Qin L. Angiogenesis assays for the evaluation of angiogenic properties of orthopaedic biomaterials - a general review. Adv Healthc Mater. 2017;6(5) doi: 10.1002/adhm.201600434. [DOI] [PubMed] [Google Scholar]
- 26.Zhao D., Huang S., Lu F., Wang B., Yang L., Qin L. Vascularized bone grafting fixed by biodegradable magnesium screw for treating osteonecrosis of the femoral head. Biomaterials. 2016;81(1):84–92. doi: 10.1016/j.biomaterials.2015.11.038. [DOI] [PubMed] [Google Scholar]