Abstract
Background
Chronic postoperative pain occurs in up to 21·7 per cent of patients undergoing open inguinal hernia repair. Several mesh fixation techniques using glue or self‐gripping meshes have been developed to reduce postoperative pain. The aim of this meta‐analysis was to evaluate RCTs comparing adhesional/self‐gripping and sutured single‐layer open mesh fixations in the repair of inguinal herniation, with postoperative pain as endpoint.
Methods
PubMed, Embase and Cochrane CENTRAL databases were searched systematically for RCTs according to the PRISMA guidelines; the study was registered at PROSPERO (CRD42017056373). Different fixation methods were analysed. The primary outcome, chronic pain, was defined as a postoperative visual analogue scale (VAS) score of at least 3 at 12 months. Secondary outcomes were mean VAS score at 1 week and at 1 month after surgery.
Results
Twenty‐three studies including 5190 patients were included in the meta‐analysis. Adhesional (self‐adhering or glued) or self‐gripping fixation methods were associated with a significantly lower VAS score at 1 week (mean difference –0·49, 95 per cent c.i. ‐0·81 to –0·17; P = 0·003) and at 1 month (mean difference –0·31, –0·58 to –0·04; P = 0·02) after surgery than suture fixation, but the incidence of chronic pain after 12 months was similar in the two groups (odds ratio 0·70, 95 per cent c.i. 0·30 to 1·66). Differences in recurrences and complications between groups did not reach statistical significance.
Conclusion
There was no difference in the incidence of chronic pain 12 months after different mesh repair fixation techniques despite significant reductions in short‐term postoperative pain favouring a non‐sutured technique. There were no differences in recurrence rates or in rates of other complications at 1 year.
Introduction
Inguinal herniation is a common problem, with an estimated lifetime risk of 27 per cent in men and 3 per cent in women1, 2. Some 20 million people undergo surgical repair each year worldwide3. Mesh reinforcement is widely regarded as the standard repair technique based on lower recurrence rates compared with those of primary suture closure4, 5. Guidelines from the European Hernia Society6 recommended two techniques: an open procedure and a laparoscopic totally extraperitoneal (TEP) repair. TEP is not recommended for patients with previous major abdominal surgery, large scrotal hernias, irreducible hernias or recurrences after a posterior approach6.
Among complications of inguinal hernia repair, chronic pain is thought to affect 10–21·7 per cent of patients, limiting daily activities in up to one‐quarter of these patients7, 8, 9, 10. The incidence and severity of postoperative pain after inguinal hernia repair have been reported, with wide variations largely reflecting lack of standard definitions.
Postherniorrhaphy pain syndrome has been attributed to a variety of causes including neuropathic pain, non‐neuropathic pain (periosteitis of the pubic tubercle, recurrence, adductor tendinitis, ileopectineal bursitis, osteoarthritis) and diffuse tenderness of the spermatic cord11.
The incidence of postoperative chronic pain seems higher after open hernia repair compared with a laparoscopic technique12. Age also appears to be a factor13, as younger patients report pain and functional impairment 1 year after surgery more frequently than those older than 65 years5. Patients with high preoperative pain scores also have an increased risk of developing chronic pain14.
It has been hypothesized that suture fixation increases the risk of nerve entrapment, causing postoperative pain syndromes15. This has led to the development of different mesh fixation products (self‐gripping mesh, mesh with human fibrin glue fixation and cyanoacrylate glue fixation)16, 17. Although earlier meta‐analyses18, 19, 20, 21 considered glue fixation and self‐gripping meshes, none included all self‐adhering or self‐gripping fixation methods. The aim of this meta‐analysis was to evaluate RCTs comparing adhering (glue or self‐adherent) or self‐gripping versus sutured mesh repairs, with the endpoints of chronic (primary outcome) and acute (secondary outcome) postoperative pain after a single‐layer mesh repair technique.
Methods
This meta‐analysis was performed according to the PRISMA guidelines22 and registered at PROSPERO (CRD42017056373; http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017056373).
Eligibility criteria
All RCTs comparing a flat sutured mesh versus glue or self‐gripping mesh fixation in inguinal hernia repairs in an adult population with primary, unilateral inguinal hernias were eligible for inclusion. Other study designs (non‐randomized trials, case series) were excluded. Exclusion criteria were mesh plugs and bilayer systems, and methods without fixation or with staples or tacks. Men and women were included. No limitations based on the type of sutures were made, but details were recorded. All studies reporting on postoperative pain were eligible, without limitations based on the definition of postoperative pain. No language restrictions were applied. Unpublished studies were eligible for inclusion.
Literature search
PubMed, Embase and Cochrane CENTRAL databases were searched systematically on 1 May 2017, using free‐text and Medical Subject Heading (MeSH) terms regarding the target condition (inguinal hernia, groin hernia, ‘Hernia, Inguinal’[MeSH]), operative technique (open repair, mesh repair, Lichtenstein, ‘Surgical Mesh’[MeSH]) and primary outcome (pain, ‘Pain, Postoperative’[MeSH]). The detailed search strategy was made publicly available on PROSPERO (Table S1 , supporting information). The search was designed with the help of an experienced librarian. Reference lists of included articles were searched to identify additional relevant publications.
Study selection
Results from the database searches were managed using citation manager software (EndNote™ X7; Clarivate Analytics, Philadelphia, Pennsylvania, USA). After removal of duplicates, title and abstract screening and full‐text eligibility assessment was undertaken by two independent authors. Disagreement between the reviewers was discussed. If consensus could not be reached, a third author was contacted for arbitration.
Data extraction and outcomes
Data extraction was standardized using an electronic data extraction form; the following variables were extracted: trial characteristics (first author, year, sample size, follow‐up), patient characteristics (age, sex, mean BMI, preoperative pain, type of hernia), operative characteristics (experience of the surgeon, type of mesh used, glue type, type of self‐gripping mesh, suture type, neurectomies, pain block) and outcomes (early postoperative pain, chronic postoperative pain, recurrences and procedure time). Chronic postoperative pain was defined as pain scored as 3 or more on a visual or numerical analogue scale (VAS) of 10 cm at 12 months after surgery. Authors were contacted if there were missing data, when additional data were required, or if the reported definition deviated from that mentioned previously. If the corresponding author of the original article did not respond after three reminders, data were excluded. During data extraction, if studies were found to report on the same population, only the relevant, original data were extracted to prevent duplicate inclusion23. Data from multiple reports on the same population were combined and considered as a single trial.
Quality assessment of included studies
Quality assessment was performed by two independent reviewers using the Cochrane risk‐of‐bias tool24. This considers random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome measurements, completeness of outcome data, outcome reporting and independency of funding in assessment of methodological quality. No studies were excluded from the meta‐analysis based on study quality.
Data synthesis and statistical analysis
Meta‐analysis was performed using RevMan software version 5.3 (Cochrane Collaboration, Nordic Cochrane Centre, Copenhagen, Denmark). VAS scales were converted into scales from 0 to 10 if needed. Treatment effects on binary outcomes were expressed as pooled odds ratios (ORs) with 95 per cent confidence intervals, calculated using the Mantel–Haenszel method. Differences in numerical variables were expressed as mean differences with 95 per cent confidence intervals and pooled using the inverse‐variance method. A random‐effects model was applied and heterogeneity was expressed using the I 2 statistic. In addition, 95 per cent prediction interval (PI) values were included.
Subgroup analyses of self‐gripping meshes versus glue were undertaken, as well as subgroup analyses based on the type of glue (fibrin versus cyanoacrylate) and mesh weight (heavyweight versus medium weight versus lightweight). A subgroup analysis based on study quality was planned if enough eligible studies with acceptable heterogeneity were available. A funnel plot was prepared to check for publication bias and Egger's regression performed to check for asymmetry.
Results
Of 2682 articles identified by the literature search, 51 were selected for full‐text assessment and 29 articles met the inclusion criteria. After removing duplicate articles, 2516, 17, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 were included in the meta‐analysis, representing 23 studies (Fig. 1). The study population included in the meta‐analysis consisted of 5190 patients.
Figure 1.
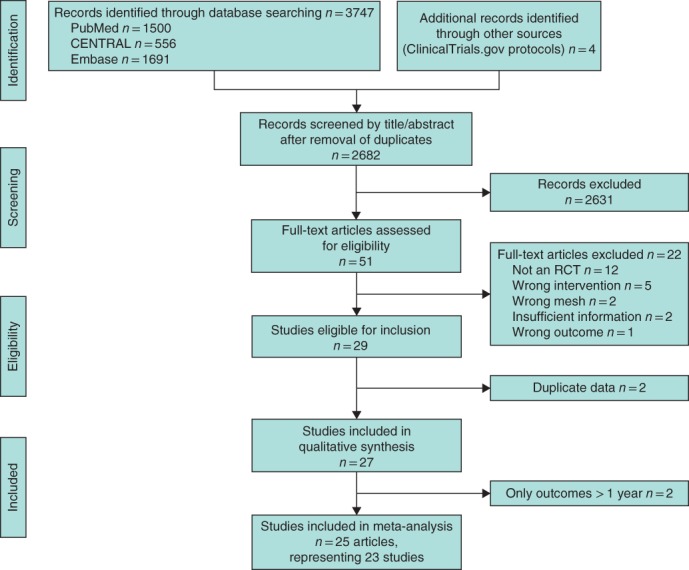
PRISMA diagram showing selection of articles for review
Fibrin glue, cyanoacrylate and ProGrip™ self‐gripping mesh (Medtronic, Minneapolis, Minnesota, USA) were the three methods of self‐adhering or self‐gripping fixation encountered in the included studies. One study45 had a multiarm trial design comparing cyanoacrylate glue fixation and ProGrip™ self‐gripping mesh with suture fixation of the mesh. Five16, 25, 30, 32, 36 studies reported on fibrin glue fixation, eight29, 33, 37, 39, 42, 43, 45, 46 on cyanoacrylate glue fixation and 1117, 26, 28, 31, 34, 35, 38, 40, 44, 45, 47 on the use of ProGrip™ self‐gripping mesh. Of the 23 articles included in the meta‐analysis, 1516, 17, 25, 26, 28, 30, 32, 33, 34, 38, 39, 43, 45, 46, 47 provided the incidence of chronic pain at 12 months, according to the definition provided in the methods. In two studies32, 33, data could be extracted directly from the manuscript. Median follow‐up was 12 (range 3–72) months. Study characteristics are summarized in Table 1.
Table 1.
Characteristics of the included studies
| Reference | Sample size (men) | Age (years)* | BMI(kg/m2)* | Intervention | Mesh (class) | Pain tool | Additional suture fixation | Pain block |
|---|---|---|---|---|---|---|---|---|
| Bracale et al. 25 | 52 (49) | 56 (46–67)† | 25·9 (23·7–27·8)† | Suture | Ultrapro® (I) | VAS 0–10 | – | No |
| 50 (48) | 59 (50–67)† | 26·0 (24·2–27·3)† | Quixil® (fibrin glue) | Ultrapro® (I) | VAS 0–10 | No | No | |
| Bruna Esteban et al. 26, 27 | 45 (38) | 49 (19–83)‡ | n.a. | Suture | Microval® (I) | VAS 0–10 | – | No |
| 45 (41) | 60 (26–80)‡ | n.a. | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VAS 0–10 | No | No | |
| Campanelli et al. 16 | 160 (160) | 59 (48–66)† | 25·5(2·6) | Suture | Polypropylene macroporous heavyweight (n.a.) | VAS 0–100 | No | Yes |
| 159 (159) | 58 (46–65)† | 25·5(2·9) | Tissucol® (fibrin glue) | Polypropylene macroporous heavyweight (n.a.) | VAS 0–100 | No | Yes | |
| Chatzimavroudis et al. 28 | 25 (23) | 62(16) | 28·8(3·1) | Suture | Prolene® (II) | VAS 0–10 | – | No |
| 25 (25) | 57(18) | 27·5(2·9) | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VAS 0–10 | Yes, non‐absorbable | No | |
| Dąbrowiecki et al. 29 | 21 (21) | 45(15) | n.a. | Suture | Prolene® (II) | VAS 0–10 | – | n.a. |
| 20 (20) | 47(13) | n.a. | Glubran® sealant (n‐butyl‐2‐cyanoacrylate) | Prolene® (II) | VAS 0–10 | No | n.a. | |
| Damiano et al. 30 | 252 (238) | 55(5) | n.a. | Suture | n.a. | NRS 0–10 | – | No |
| 216 (206) | 53(5) | n.a. | Tissucol® (fibrin glue) | n.a. | NRS 0–10 | No | No | |
| Fan et al. 31 | 23 (22) | 63(5) | n.a. | Suture | Surgipro™ (II) | VAS 0–10 | – | n.a. |
| 22 (18) | 62(16) | n.a. | Parietex™ ProGrip™ | Parietex™ ProGrip™ (III) | VAS 0–10 | Yes, non‐absorbable | n.a. | |
| Fortelny et al. 32 | 20 (18) | 54(17) | 25·9(3·2) | Suture | Infinit® (II) | VAS 0–100 | – | Yes |
| 18 (16) | 47(15) | 25·1(4·1) | Tissucol® (fibrin glue) | Infinit® (II) | VAS 0–100 | No | Yes | |
| Hoyuela et al. 33 | 182 (162) | 59(14) | 26·0(3·5) | Suture | Optilene® (I) | VAS 0–10 | – | Yes |
| 188 (170) | 61(15) | 25·7(3·6) | Histoacryl® (n‐butyl‐2‐cyanoacrylate) | Optilene® (I) | VAS 0–10 | No | Yes | |
| Jorgensen et al. 34 | 171 (171) | 60 (46–68)† | 24·8 (23·1–26·7)† | Suture | Parietene Light® (I) | VAS 0–100 | – | Yes |
| 163 (163) | 57 (40–65)† | 25·2 (23·5–27·1)† | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VAS 0–100 | No | Yes | |
| Kapischke et al. 35 | 26 (23) | 67(12) | n.a. | Suture | Optilene® (I) | VAS 0–100 | – | n.a. |
| 24 (22) | 64(13) | n.a. | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VAS 0–100 | No | n.a. | |
| Karigoudar et al. 36 | 32 (n.a.) | 44§ | n.a. | Suture | n.a. | VAS 0–100 | n.a. | n.a. |
| 32 (n.a.) | 44§ | n.a. | Fibrin glue | n.a. | VAS 0–100 | n.a. | n.a. | |
| Kim‐Fuchs et al. 37 | 133 (133) | 57 (25–83)‡ | n.a. | Suture | Vypro® II (III) | n.a. | – | n.a. |
| 131 (131) | 55 (28–85)‡ | n.a. | Histoacryl® (n‐butyl‐2‐cyanoacrylate) | Vypro® II (III) | n.a. | No | n.a. | |
| Molegraaf et al. 38 | 170 (170) | 61(16) | 25·0(3·7) | Suture | Parietex™ (I) | VRS 1–6 VAS 0–100 | Yes, in 28 patients | Yes |
| 169 (169) | 63(15) | 24·9(3·4) | Parietex™ ProGrip™ | Parietex™ ProGrip™ (III) | VRS 1–6 VAS 0–100 | Yes | ||
| Moreno‐Egea39 | 52 (37) | 55(14) | 29·8(4·2) | Suture | TiMESH® (I) | VAS 0–10 | – | No |
| 50 (34) | 57(16) | 29·3(3·7) | IFABond™ (n‐hexyl‐α‐cyanoacrylate) | TiMESH® (I) | VAS 0–10 | No | No | |
| Nikkolo et al. 40, 41 | 75 (68) | 54(7) | 25·1 (16·6–34·7)‡ | Suture | Optilene LP (I) | VAS 0–100 | – | n.a. |
| 70 (65) | 58(17) | 25·0 (17·4–38·1)‡ | Parietex™ ProGrip™ | Parietex™ ProGrip™ (III) | VAS 0–100 | No | n.a. | |
| Nowobilski et al. 42 | 24 (24) | 52 (20–78)‡ | n.a. | Suture | n.a. | VAS 0–100 | – | Yes |
| 22 (22) | 60 (30–76)‡ | n.a. | Indermil™ (butyl‐2‐cyanoacrylate) | n.a. | VAS 0–100 | No | Yes | |
| Paajaanen et al. 43 | 151 (135) | 53(15) | 25(3) | Suture | Optilene® (I) | VAS 0–10, NRS 0–10 | – | Yes |
| 151 (131) | 53(15) | 25(3) | Glubran® (butyl‐2‐cyanoacrylate) | Optilene® (I) | VAS 0–10, NRS 0–10 | No | Yes | |
| Pierides et al. 44 | 196 (182) | 53(19–80)‡ | 25·0 (18·0–33·0)‡ | Suture | Parietene Light® (I) | VAS 0–10 | – | No |
| 198 (188) | 55 (20–79)‡ | 24·9 (18·2–36·0)‡ | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VAS 0–10 | No | No | |
| Rönkä et al. 45 | 197 (188) | 57(14) | 25(3) | Suture | Ultrapro® (I) | VAS 0–10 | – | Yes |
| 211 (194) | 59(14) | 25(3) | Histoacryl® (butyl‐2‐cyanoacrylate) | Optilene® (I) | VAS 0–10 | No | Yes | |
| 189 (182) | 56(14) | 25(3) | Parietex ProGrip™ | Parietex ProGrip™ (III) | VAS 0–10 | No | Yes | |
| Sanders et al. 17 | 287 (287) | 57(11) | 25·5(2·9) | Suture | Parietene Light® (I) | VAS 0–150, SPS 0–150 | – | Yes |
| 270 (270) | 57(12) | 25·4(3·0) | Parietex ™ ProGrip™ | Parietex™ ProGrip™ (III) | VAS 0–150, SPS 0–150 | Yes | Yes | |
| Shen et al. 46 | 55 (47) | 60(12) | 25(2) | Suture | ProLite Ultra™ (II) | VAS 0–10 | – | Yes |
| 55 (45) | 63(10) | 25(2) | COMPONT® medical adhesive (n‐butyl‐2‐cyanoacrylate) | ProLite Ultra™ (II) | VAS 0–10 | No | Yes | |
| Verhagen et al. 47 | 181 (179) | 58 (19–86)‡ | 25 (19–36)‡ | Suture | Standard polypropylene (n.a.) | VRS 1–6 VAS 0–150 | – | n.a. |
| 182 (175) | 60 (20–88)‡ | 25 (18–33)‡ | Parietene™ ProGrip™ | Parietene™ ProGrip™ (III) | VRS 1–6 VAS 0–150 | No | n.a. |
Values are mean(s.d.) unless indicated otherwise; values are
median (i.q.r.),
median (range) and §mean. VAS, visual analogue scale; n.a., not available; NRS, numerical rating scale; VRS, visual rating scale; SPS, surgical pain scale. Mesh classification according to Klinge et al. 48: class I, large‐pore meshes (textile porosity of 60 per cent or more, or an effective porosity of over 0 per cent); class II, small‐pore meshes (textile porosity of below 60 per cent and without any effective porosity); class III, meshes with special features; class IV, meshes with films; class V, three‐dimensional meshes; class VI, biologicals. Ultrapro®, Prolene®, Vypro® (Ethicon Products, Johnson & Johnson, Somerville, New Jersey, USA); Quixil® (Omrix Biopharmaceuticals, Zaventem, Belgium); Microval® (Microval, Saint‐Just‐Malmont, France); Parietene™ ProGrip™, Surgipro™, Parietex™ ProGrip™, Parietene Light® (Medtronic, Minneapolis, Minnesota, USA); Tissucol® (Baxter Healthcare, Deerfield, Illinois, USA); Glubran® (GEM, Viareggio, Italy); Infinit® (W. L. Gore & Associates, Newark, Delaware, USA); Histoacryl®, Optilene® (Braun, Melsungen, Germany); IFABond™ (Fimed, Domalain, France); TiMESH® (pfm medical UK, Stockport, UK); Indermil™ (Tyco Healthcare Group, Norwalk, Connecticut, USA); COMPONT® (Beijing Compont Medical Devices Beijing, China); ProLite Ultra™ (Atrium Medical, Hudson, New Hampshire, USA).
Four studies34, 38, 43, 45 were rated as having a low risk of bias (Fig. 2, Table 2). Two studies were unblinded28, 37 and two were single‐blinded17, 25. The risk of bias was estimated to be high in six studies based on incomplete outcome data16, 17, 29, 31, 33, 37, in two studies33, 37 based on loss to follow‐up and in two others17, 47 based on missing VAS scores. Two RCTs were concluded prematurely, one31 because of significant results at the interim analysis32 and one because of discontinuation of mesh production. Four studies16, 17, 44, 47 had a high risk of bias owing to the source of funding. A funnel plot for the primary outcome documented some asymmetry, owing to a lack of studies favouring conventional fixation. Egger's regression showed that the asymmetry was not significant (P = 0·756) (Fig. 3).
Figure 2.
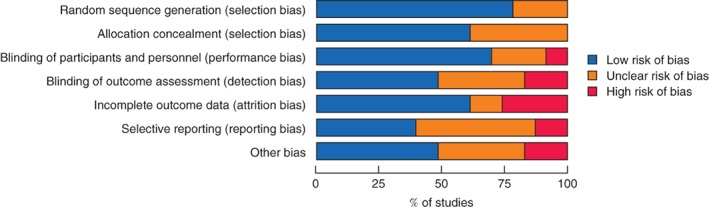
Summary of risk of bias across included studies
Table 2.
Risk of bias in individual studies
| Random sequence generation (selection bias) |
Allocation concealment (selection bias) |
Blinding of participants and personnel (performance bias) |
Blinding of outcome assessors (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias | |
|---|---|---|---|---|---|---|---|
| Bracale et al. 25 | + | + | + | – | + | + | + |
| Bruna Esteban et al. 26, 27 | + | ? | ? | ? | + | ? | + |
| Campanelli et al. 16 | + | + | + | + | – | + | – |
| Chatzimavroudis et al. 28 | ? | ? | – | – | + | + | + |
| Dąbrowiecki et al. 29 | + | + | + | + | – | ? | ? |
| Damiano et al. 30 | ? | ? | ? | ? | ? | ? | ? |
| Fan et al. 31 | + | ? | + | + | – | + | ? |
| Fortelny et al. 32 | + | + | ? | ? | ? | ? | ? |
| Hoyuela et al. 33 | + | + | + | + | – | ? | + |
| Jorgensen et al. 34 | + | + | + | + | + | + | + |
| Kapischke et al. 35 | + | ? | + | + | + | ? | ? |
| Karigoudar et al. 36 | ? | ? | ? | ? | + | – | + |
| Kim‐Fuchs et al. 37 | + | + | – | – | – | ? | ? |
| Molegraaf et al. 38 | + | + | + | + | + | + | + |
| Moreno‐Egea39 | + | + | + | ? | + | ? | + |
| Nikkolo et al. 40 | + | + | + | ? | + | ? | + |
| Nowobilski et al. 42 | ? | ? | ? | ? | + | ? | ? |
| Paajanen et al. 43 | ? | + | + | + | + | + | + |
| Pierides et al. 44 | + | + | + | + | ? | + | – |
| Rönkä et al. 45 | + | + | + | + | + | + | + |
| Sanders et al. 17 | + | ? | + | – | – | – | – |
| Shen et al. 46 | + | ? | + | ? | + | ? | ? |
| Verhagen et al. 47 | + | + | + | + | + | – | – |
+, Low risk of bias; –, high risk of bias;?, unclear risk of bias.
Figure 3.
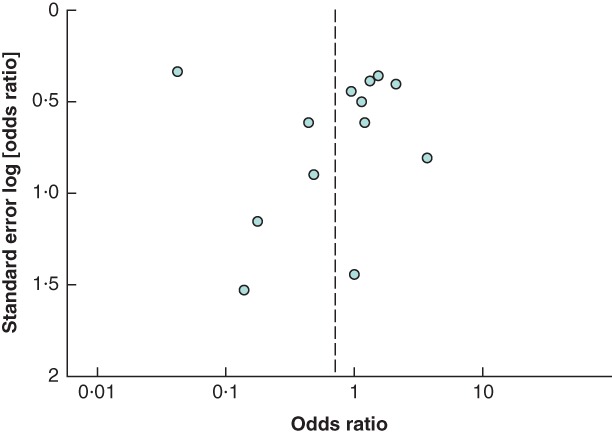
Funnel plot for primary outcome
Ten studies including 2846 participants provided pain data at 1 week, nine studies with 2740 participants at 1 month, and 15 studies with 3742 participants at 12 months (Fig. 4 ).
Figure 4.
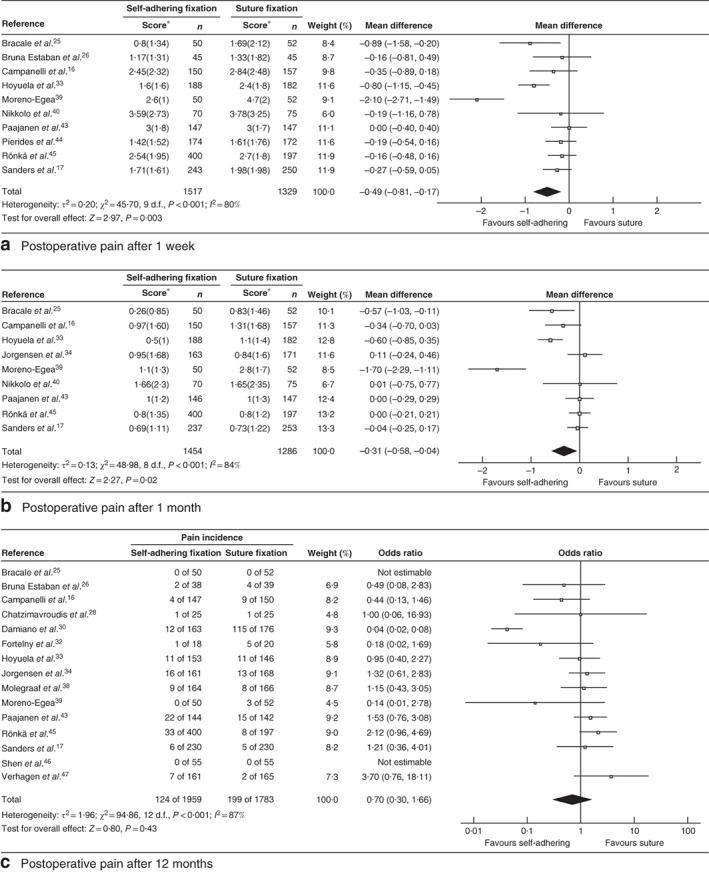
Forest plot comparing postoperative pain after hernia repair with adhesional or self‐gripping fixation versus suture fixation. a Pain scores after 1 week, b pain scores after 1 month and c incidence of pain after 12 months. Mean differences and odds ratios are shown with 95 per cent confidence intervals. An inverse‐variance (a,b) or Mantel–Haenszel (c) random‐effects model was used for meta‐analysis. *Values are mean(s.d.)
Adhering or self‐gripping fixation methods were associated with significantly lower mean VAS scores at 1 week compared with any kind of suture fixation (mean difference –0·49, 95 per cent c.i. –0·81 to –0·17; P = 0·003; I 2 = 80 per cent; 95 per cent PI –1·99 to 1·01). After 1 month, the mean VAS score still favoured the non‐sutured group (mean difference –0·31, –0·58 to –0·04; P = 0·02; I 2 = 84 per cent; 95 per cent PI –1·70 to 1·08). After 12 months, however, there was no significant difference in the incidence of chronic pain between the two groups (OR 0·70, 95 per cent c.i. 0·30 to 1·66; P = 0·43; I 2 = 87 per cent; 95 per cent PI 0·03 to 12·86).
Subgroup analysis showed a significant reduction in mean VAS score for glue fixation versus suture fixation after 1 week (mean difference –0·71, –1·22 to –0·20; P = 0·007; I 2 = 87 per cent; 95 per cent PI –2·90 to 1·48) and 1 month (mean difference –0·48, –0·86 to –0·11; P = 0·01; I 2 = 87 per cent; 95 per cent PI –2·30 to 1·34) of follow‐up (Figs S1 and S2 , supporting information). In a comparison of glue fixation with suture fixation at 12 months, the difference in the incidence of chronic pain was not significant (OR 0·43, 0·11 to 1·74; P = 0·24; I 2 = 92 per cent; 95 per cent PI 0·01 to 21·25) (Fig. S3 , supporting information).
After 12 months, fibrin glue showed a significant reduction in the incidence of chronic pain compared with suture fixation (OR 0·14, 0·02 to 0·78; P = 0·03, I 2 = 83 per cent), but the same did not apply to cyanoacrylate glue (OR 1·36, 0·77 to 2·42; P = 0·29; I 2 = 29 per cent) (Fig. S3 , supporting information). Cyanoacrylate glue showed a larger decrease in mean VAS score 1 week after surgery (mean difference compared with suture fixation –0·77, –1·48 to –0·05; P = 0·04; I 2 = 92 per cent) than fibrin glue (mean difference –0·58, –1·10 to –0·06; P = 0·03; I 2 = 31 per cent) (Fig. S1 , supporting information). At 1 month, the decrease in VAS score was comparable between cyanoacrylate and fibrin glue (Fig. S2 , supporting information).
There was no significant difference in VAS score between ProGrip™ and suture fixation at 1 week (mean difference –0·17, –0·35 to 0·02; P = 0·08; I 2 = 0 per cent; 95 per cent PI –1·40 to 1·06) and 1 month (–0·00, –0·14 to 0·14; P = 0·99; I 2 = 0 per cent; 95 per cent PI –0·41 to 0·41) respectively after operation (Figs S4 and S5 , supporting information). As regards the incidence of chronic pain at 12 months' follow‐up, there was no significant difference between ProGrip™ and suture fixation (OR 1·45, 0·92 to 2·28; P = 0·11; I 2 = 0 per cent; 95 per cent PI 0·19 to 10·73) (Fig. S6 , supporting information).
Subgroup analysis comparing heavyweight and lightweight meshes was abandoned. The small number of articles reporting medium weight or heavyweight meshes was thought to make such an analysis unreliable.
Recurrence
Nineteen studies16, 17, 25, 26, 28, 29, 30, 31, 32, 33, 34, 37, 38, 39, 43, 44, 45, 46, 47 including 4531 patients analysed recurrence. No significant difference was found in recurrence rates between the intervention and control groups after 1 year of follow‐up (OR 1·11, 95 per cent c.i. 0·65 to 1·90; P = 0·69; I 2 = 0 per cent; 95 per cent PI 0·15 to 8·23) (Fig. 5). In subgroup analyses, ProGrip™ (OR 0·98, 0·52 to 1·86; P = 0·96; I 2 = 0 per cent; 95 per cent PI 0·15 to 6·60), fibrin glue (OR 1·34, 0·25 to 7·07; P = 0·73; I 2 = 0 per cent; 95 per cent PI not estimable) and cyanoacrylate glue (OR 1·53, 0·48 to 4·86; P = 0·47; I 2 = 0 per cent; 95 per cent PI 0·11 to 22·11) showed no significant difference in recurrence rate in separate comparisons versus suture fixation.
Figure 5.
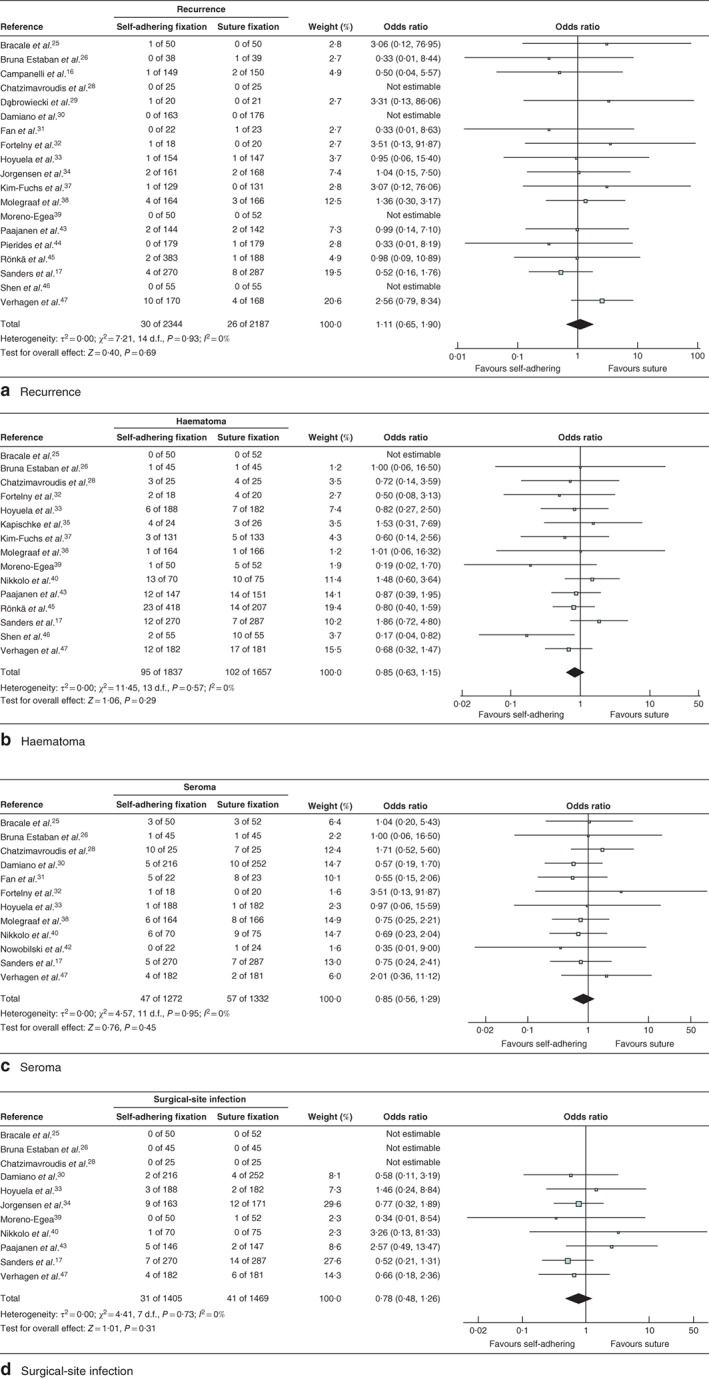
Forest plot comparing rates of recurrence, haematoma, seroma and surgical‐site infection after hernia repair with adhesional or self‐gripping fixation versus suture fixation. Rates of a recurrence, b haematoma, c seroma and d surgical‐site infection. Odds ratios are shown with 95 per cent confidence intervals. A Mantel–Haenszel random‐effects model was used for meta‐analysis
Other complications
One study36 was excluded as it did not report on complications. Fifteen studies17, 25, 26, 28, 32, 33, 35, 37, 38, 39, 40, 43, 45, 46, 47 reported on haematoma formation, 1217, 25, 26, 28, 30, 31, 32, 33, 38, 40, 42, 47 on seroma formation and 1117, 25, 26, 28, 30, 33, 34, 39, 40, 43, 47 on surgical‐site infection. Only studies that reported specifically on haematoma, seroma or surgical‐site infection were included in the meta‐analysis. No significant differences were detected between self‐adhering or self‐gripping fixation methods and suture fixation in the occurrence of haematoma (OR 0·85, 95 per cent c.i. 0·63 to 1·15; P = 0·29; I 2 = 0 per cent; 95 per cent PI 0·18 to 4·02), seroma (OR 0·85, 0·56 to 1·29; P = 0·45; I 2 = 0 per cent; 95 per cent PI 0·19 to 3·76) or surgical‐site infection (OR 0·78, 0·48 to 1·26; P = 0·31; I 2 = 0 per cent; 95 per cent PI 0·10 to 6·12 (Fig. 5). Furthermore, subgroup analysis for glue fixation or ProGrip™ mesh versus suture fixation showed no significant differences in occurrence of haematoma, seroma or surgical‐site infection (Table S2 , supporting information).
Procedure time
Eighteen studies reported the duration of operation, including 2247 intervention and 2111 control procedures. There was a significant reduction of 5·94 (95 per cent c.i. –8·09 to −3·79; P < 0·001; I 2 = 94 per cent; 95 per cent PI –14·50 to 2·62) min in procedure time favouring a self‐adhering or self‐gripping mesh fixation over suture fixation (Fig. 6).
Figure 6.
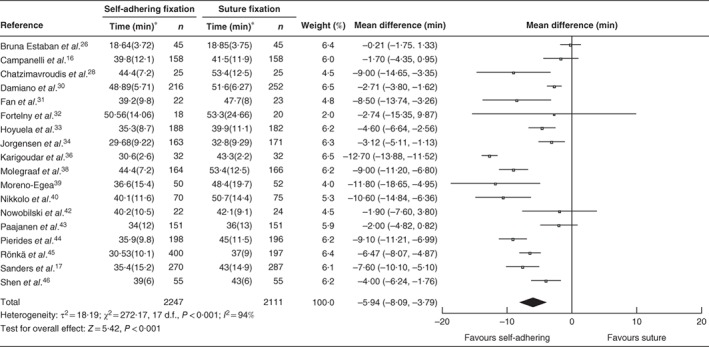
Forest plot comparing procedure times after hernia repair with adhesional or self‐gripping fixation versus suture fixation. Mean differences are shown with 95 per cent confidence intervals. An inverse‐variance random‐effects model was used for meta‐analysis. *Values are mean(s.d.)
Discussion
This meta‐analysis compared RCTs on adhesional and self‐gripping mesh fixation in open inguinal hernia repair, providing significant data regarding the outcome postoperative pain. Discrepancies in the definition of chronic pain between studies were dealt with by directly contacting the authors, asking them to rearrange their data to a preset definition.
Although chronic pain was defined previously as pain persisting 3 months after surgery, most trials reported on chronic pain at 12 months, and this endpoint was chosen as the primary outcome accordingly. On the other hand, a VAS score of 3 was selected arbitrarily as the cut‐off, because this value approaches the tipping point from mild to moderate pain, although variation in cut‐off points of VAS score is evident49, 50, 51.
RCTs included in the analysis were investigated for risk of bias. Even when this was assessed as being relatively low, the non‐significant asymmetry in the funnel plot could be caused by heterogeneity for the primary outcome. Other causes of heterogeneity could be the variety of meshes used in the different studies. Lightweight meshes have been associated with less chronic pain and discomfort, less foreign body sensation and reduced sensory impairment or tenderness compared with heavyweight meshes52.
No significant difference in chronic pain at 12 months was found in a comparison of adhesional or self‐gripping methods of fixation versus suture fixation. In subgroup analysis, fibrin glue was associated with a significant reduction in the incidence of chronic pain at 12 months. One included study30 reported a remarkably high incidence of chronic pain at 12 months' follow‐up in the control group. In this study, only P values were mentioned regarding VAS scores at 1‐week and 6‐month follow‐up, so the data were not included in the meta‐analysis. A significant difference was reported at 1 week and 12 months, but not at the 6‐month time point30. In the present meta‐analysis, glue fixation of the mesh was associated with a significantly lower VAS score at 1 week and 1 month compared with suture fixation, with pooled mean reduction in postoperative pain score of 0·71 and 0·48 respectively. At 1 week, a greater reduction in VAS score was observed in the cyanoacrylate group in comparison with suture fixation, than for fibrin glue in comparison with suture fixation. The results were largely affected by a single study39 with a mean score of 4·7 in the control group, so conclusions should be drawn carefully. The reduction in mean VAS score was comparable at 1 month for cyanoacrylate and fibrin glue (–0·52 and –0·43 respectively).
Optimum VAS cut‐off points after a groin hernia repair were previously defined as a score ranging from 0 to 0·8 (no pain), 0·9–3·2 (mild pain), 3·3–7·1 (moderate pain) and over 7·1 (severe pain) on a 10‐cm scale49. Furthermore, a VAS score of 0–3 cm is considered to indicate successful analgesia during treatment50. Bearing this in mind, a reduction of 0·71 in a patient group with mild pain already will not constitute a clinically relevant effect and the impact on use of analgesics would be expected to be negligible. Moreover, results of the comparison between glues should be interpreted cautiously and more RCTs are needed to enable definitive conclusions to be drawn.
ProGrip™ self‐gripping mesh provided no benefit compared with suture fixation with respect to postoperative pain at 1 week, 1 month or 12 months after surgery. The resorbable polylactic acid microgrips possibly caused more trauma or induced a less favourable tissue reaction than cyanoacrylate or fibrin glue. Reports included in this meta‐analysis described the use of an occasional additional single suture at the pubic tubercle to facilitate placement and ensure adequate medial overlap, which might also be a cause of pain due to periosteitis of the pubic tubercle11 and influence the results.
Subgroup analysis did not detect a difference in recurrence rates for the different adhesional and self‐gripping fixation methods compared with suture fixation. A previous series53 documented a high recurrence rate in patients treated with ProGrip™ self‐gripping mesh compared with suture fixation at 3 years of follow‐up, although a high rate of loss to follow‐up affected the analysis. Another study41 reported no recurrences in the ProGrip™ self‐gripping group after 3 years, but these results should be further validated. There were no significant differences in rates of other complications such as haematomas, seromas or surgical‐site infection between glue and self‐gripping fixation methods compared with suture fixation. As expected, the procedure time was significantly shorter for non‐sutured methods than for suture fixation although the mean difference was about 6 min, which may not be meaningful.
Supporting information
Figure S1. Forest plot comparing mean VAS‐score of glue‐fixation and suture fixation at 1 week postoperatively.
Figure S2. Forest plot comparing mean VAS‐score of glue‐fixation and suture fixation at 1 month postoperatively.
Figure S3. Forest plot comparing the incidence of chronic pain (VAS > 3) of glue‐fixation and suture fixation at 12 month postoperatively.
Figure S4. Forest plot comparing mean VAS‐score of ProGripÔ and suture fixation at 1 week postoperatively.
Figure S5. Forest plot comparing mean VAS‐score of ProGripÔ and suture fixation at 1 month postoperatively.
Figure S6. Forest plot comparing the incidence of chronic pain (VAS > 3) of ProGripÔ and suture fixation at 12 months postoperatively.
Table S1. Search in Embase, Cochrane CENTRAL, Pubmed
Table S2. complications after mesh placement; hematoma, seroma or surgical site infection. Comparing glue fixation to suture fixation and ProGripÔ to suture fixation.
Acknowledgements
S.v.S. and L.K.v.V. contributed equally to this study. This meta‐analysis was preregistered at PROSPERO (CRD42017056373). Medtronic was in possession of the data from one of the included studies, and a data‐sharing agreement was signed in order to retrieve these data. Medtronic had no influence on the design of this review and meta‐analysis, on the collection, analysis and interpretation of the data, nor on the writing of the report or the decision to submit the article for publication.
Disclosure: The authors declare no conflict of interest.
Funding information
No funding
References
- 1. Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 1996; 25: 835–839. [DOI] [PubMed] [Google Scholar]
- 2. Dabbas N, Adams K, Pearson K, Royle G. Frequency of abdominal wall hernias: is classical teaching out of date? JRSM Short Rep 2011; 2: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet 2003; 362: 1561–1571. [DOI] [PubMed] [Google Scholar]
- 4. Amato B, Moja L, Panico S, Persico G, Rispoli C, Rocco N et al. Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 2012; (4)CD001543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bay‐Nielsen M, Perkins FM, Kehlet H; Danish Hernia Database . Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 2001; 233: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Simons MP, Aufenacker T, Bay‐Nielsen M, Bouillot JL, Campanelli G, Conze J et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009; 13: 343–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 2003; 19: 48–54. [DOI] [PubMed] [Google Scholar]
- 8. Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 2005; 95: 69–76. [DOI] [PubMed] [Google Scholar]
- 9. Eklund A, Montgomery A, Bergkvist L, Rudberg C; Swedish Multicentre Trial of Inguinal Hernia Repair by Laparoscopy (SMIL) study group . Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg 2010; 97: 600–608. [DOI] [PubMed] [Google Scholar]
- 10. Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R. Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 2007; 194: 394–400. [DOI] [PubMed] [Google Scholar]
- 11. Loos MJ, Roumen RM, Scheltinga MR. Classifying post‐herniorrhaphy pain syndromes following elective inguinal hernia repair. World J Surg 2007; 31: 1760–1765. [DOI] [PubMed] [Google Scholar]
- 12. Grant AM; EU Hernia Trialists Collaboration . Laparoscopic versus open groin hernia repair: meta‐analysis of randomised trials based on individual patient data. Hernia 2002; 6: 2–10. [DOI] [PubMed] [Google Scholar]
- 13. Nienhuijs SW, Boelens OB, Strobbe LJ. Pain after anterior mesh hernia repair. J Am Coll Surg 2005; 200: 885–889. [DOI] [PubMed] [Google Scholar]
- 14. Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U. Risk factors for long‐term pain after hernia surgery. Ann Surg 2006; 244: 212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heise CP, Starling JR. Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg 1998; 187: 514–518. [DOI] [PubMed] [Google Scholar]
- 16. Campanelli G, Pascual MH, Hoeferlin A, Rosenberg J, Champault G, Kingsnorth A et al. Randomized, controlled, blinded trial of Tisseel/Tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trial. Ann Surg 2012; 255: 650–657. [DOI] [PubMed] [Google Scholar]
- 17. Sanders DL, Nienhuijs S, Ziprin P, Miserez M, Gingell‐Littlejohn M, Smeds S. Randomized clinical trial comparing self‐gripping mesh with suture fixation of lightweight polypropylene mesh in open inguinal hernia repair. Br J Surg 2014; 101: 1373–1382. [DOI] [PubMed] [Google Scholar]
- 18. Colvin HS, Rao A, Cavali M, Campanelli G, Amin AI. Glue versus suture fixation of mesh during open repair of inguinal hernias: a systematic review and meta‐analysis. World J Surg 2013; 37: 2282–2292. [DOI] [PubMed] [Google Scholar]
- 19. Zhang C, Li F, Zhang H, Zhong W, Shi D, Zhao Y. Self‐gripping versus sutured mesh for inguinal hernia repair: a systematic review and meta‐analysis of current literature. J Surg Res 2013; 185: 653–660. [DOI] [PubMed] [Google Scholar]
- 20. Liu H, Zheng X, Gu Y, Guo S. A meta‐analysis examining the use of fibrin glue mesh fixation versus suture mesh fixation in open inguinal hernia repair. Dig Surg 2014; 31: 444–451. [DOI] [PubMed] [Google Scholar]
- 21. Sajid MS, Farag S, Singh KK, Miles WF. Systematic review and meta‐analysis of published randomized controlled trials comparing the role of self‐gripping mesh against suture mesh fixation in patients undergoing open inguinal hernia repair. Updates Surg 2014; 66: 189–196. [DOI] [PubMed] [Google Scholar]
- 22. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA Statement. PloS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Higgins JPT, Deeks J. Selecting studies and collecting data. In Cochrane Handbook for Systematic Reviews of Interventions, Version 510; updated March 2011. The Cochrane Collaboration. http://handbook‐5‐1.cochrane.org [accessed 1 April 2017].
- 24. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bracale U, Rovani M, Picardo A, Merola G, Pignata G, Sodo M et al. Beneficial effects of fibrin glue (Quixil) versus Lichtenstein conventional technique in inguinal hernia repair: a randomized clinical trial. Hernia 2014; 18: 185–192. [DOI] [PubMed] [Google Scholar]
- 26. Bruna Esteban M, Cantos Pallarés M, Artigues Sánchez De Rojas E. [Use of adhesive mesh in hernioplasty compared to the conventional technique. Results of a randomised prospective study.] Cir Esp 2010; 88: 253–258. [DOI] [PubMed] [Google Scholar]
- 27. Bruna Esteban M, Cantos Pallarés M, Artigues Sánchez de Rojas E, Vila MJ. [Prospective randomized trial of long‐term results of inguinal hernia repair using autoadhesive mesh compared to classic Lichtenstein technique with sutures and polypropylene mesh.] Cir Esp 2014; 92: 195–200. [DOI] [PubMed] [Google Scholar]
- 28. Chatzimavroudis G, Papaziogas B, Koutelidakis I, Galanis I, Atmatzidis S, Christopoulos P et al. Lichtenstein technique for inguinal hernia repair using polypropylene mesh fixed with sutures vs. self‐fixating polypropylene mesh: a prospective randomized comparative study. Hernia 2014; 18: 193–198. [DOI] [PubMed] [Google Scholar]
- 29. Dąbrowiecki S, Pierściński S, Szczęsny W. The Glubran 2 glue for mesh fixation in Lichtenstein's hernia repair: a double‐blind randomized study. Wideochir Inne Tech Maloinwazyjne 2012; 7: 96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Damiano G, Gioviale MC, Palumbo VD, Spinelli G, Buscemi S, Ficarella S et al. Human fibrin glue sealing versus suture polypropylene fixation in Lichtenstein inguinal herniorrhaphy: a prospective observational study. Chirurgia (Bucur) 2014; 109: 660–663. [PubMed] [Google Scholar]
- 31. Fan JKM, Yip J, Foo DCC, Lo OSH, Law WL. Randomized trial comparing self gripping semi re‐absorbable mesh (PROGRIP) with polypropylene mesh in open inguinal hernioplasty: the 6 years result. Hernia 2017; 21: 9–16. [DOI] [PubMed] [Google Scholar]
- 32. Fortelny RH, Petter‐Puchner AH, Redl H, May C, Pospischil W, Glaser K. Assessment of pain and quality of life in Lichtenstein hernia repair using a new monofilament PTFE mesh: comparison of suture vs. fibrin‐sealant mesh fixation. Front Surg 2014; 1: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hoyuela C, Juvany M, Carvajal F, Veres A, Troyano D, Trias M et al. Randomized clinical trial of mesh fixation with glue or sutures for Lichtenstein hernia repair. Br J Surg 2017; 104: 688–694. [DOI] [PubMed] [Google Scholar]
- 34. Jorgensen LN, Sommer T, Assaadzadeh S, Strand L, Dorfelt A, Hensler M et al.; Danish Multicentre DANGRIP Study Group . Randomized clinical trial of self‐gripping mesh versus sutured mesh for Lichtenstein hernia repair. Br J Surg 2013; 100: 474–481. [DOI] [PubMed] [Google Scholar]
- 35. Kapischke M, Schulze H, Caliebe A. Self‐fixating mesh for the Lichtenstein procedure – a prestudy. Langenbecks Arch Surg 2010; 395: 317–322. [DOI] [PubMed] [Google Scholar]
- 36. Karigoudar A, Gupta AK, Mukharjee S, Gupta N, Durga CK. A prospective randomized study comparing fibrin glue versus Prolene suture for mesh fixation in Lichtenstein inguinal hernia repair. Indian J Surg 2016; 78: 288–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kim‐Fuchs C, Angst E, Vorburger S, Helbling C, Candinas D, Schlumpf R. Prospective randomized trial comparing sutured with sutureless mesh fixation for Lichtenstein hernia repair: long‐term results. Hernia 2012; 16: 21–27. [DOI] [PubMed] [Google Scholar]
- 38. Molegraaf MJ, Grotenhuis B, Torensma B, de Ridder V, Lange JF, Swank DJ. The HIPPO trial, a randomized double‐blind trial comparing self‐gripping Parietex Progrip mesh and sutured Parietex mesh in Lichtenstein hernioplasty: a long‐term follow‐up study. Ann Surg 2017; 266: 939–945. [DOI] [PubMed] [Google Scholar]
- 39. Moreno‐Egea A. Is it possible to eliminate sutures in open (Lichtenstein technique) and laparoscopic (totally extraperitoneal endoscopic) inguinal hernia repair? A randomized controlled trial with tissue adhesive (n‐hexyl‐α‐cyanoacrylate). Surg Innov 2014; 21: 590–599. [DOI] [PubMed] [Google Scholar]
- 40. Nikkolo C, Vaasna T, Murruste M, Seepter H, Suumann J, Tein A et al. Single‐center, single‐blinded, randomized study of self‐gripping versus sutured mesh in open inguinal hernia repair. J Surg Res 2015; 194: 77–82. [DOI] [PubMed] [Google Scholar]
- 41. Nikkolo C, Vaasna T, Murruste M, Suumann J, Kirsimägi Ü, Seepter H et al. Three‐year results of a randomized study comparing self‐gripping mesh with sutured mesh in open inguinal hernia repair. J Surg Res 2017; 209: 139–144. [DOI] [PubMed] [Google Scholar]
- 42. Nowobilski W, Dobosz M, Wojciechowicz T, Mionskowska L. Lichtenstein inguinal hernioplasty using butyl‐2‐cyanoacrylate versus sutures. Preliminary experience of a prospective randomized trial. Eur Surg Res 2004; 36: 367–370. [DOI] [PubMed] [Google Scholar]
- 43. Paajanen H, Kössi J, Silvasti S, Hulmi T, Hakala T. Randomized clinical trial of tissue glue versus absorbable sutures for mesh fixation in local anaesthetic Lichtenstein hernia repair. Br J Surg 2011; 98: 1245–1251. [DOI] [PubMed] [Google Scholar]
- 44. Pierides G, Scheinin T, Remes V, Hermunen K, Vironen J. Randomized comparison of self‐fixating and sutured mesh in open inguinal hernia repair. Br J Surg 2012; 99: 630–636. [DOI] [PubMed] [Google Scholar]
- 45. Rönkä K, Vironen J, Kössi J, Hulmi T, Silvasti S, Hakala T et al. Randomized multicenter trial comparing glue fixation, self‐gripping mesh, and suture fixation of mesh in lichtenstein hernia repair (FinnMesh Study). Ann Surg 2015; 262: 714–719. [DOI] [PubMed] [Google Scholar]
- 46. Shen YM, Sun WB, Chen J, Liu SJ, Wang MG. NBCA medical adhesive (n‐butyl‐2‐cyanoacrylate) versus suture for patch fixation in Lichtenstein inguinal herniorrhaphy: a randomized controlled trial. Surgery 2012; 151: 550–555. [DOI] [PubMed] [Google Scholar]
- 47. Verhagen T, Zwaans WA, Loos MJ, Charbon JA, Scheltinga MR, Roumen RM. Randomized clinical trial comparing self‐gripping mesh with a standard polypropylene mesh for open inguinal hernia repair. Br J Surg 2016; 103: 812–818. [DOI] [PubMed] [Google Scholar]
- 48. Klinge U, Klosterhalfen B. Modified classification of surgical meshes for hernia repair based on the analyses of 1000 explanted meshes. Hernia 2012; 16: 251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Loos MJ, Houterman S, Scheltinga MR, Roumen RM. Evaluating postherniorrhaphy groin pain: visual analogue or verbal rating scale? Hernia 2008; 12: 147–151. [DOI] [PubMed] [Google Scholar]
- 50. Mantha S, Thisted R, Foss J, Ellis JE, Roizen MF. A proposal to use confidence intervals for visual analog scale data for pain measurement to determine clinical significance. Anesth Analg 1993; 77: 1041–1047. [DOI] [PubMed] [Google Scholar]
- 51. Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE. Cut‐off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014; 155: 2545–2550. [DOI] [PubMed] [Google Scholar]
- 52. Sajid MS, Leaver C, Baig MK, Sains P. Systematic review and meta‐analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg 2012; 99: 29–37. [DOI] [PubMed] [Google Scholar]
- 53. Zwaans WAR, Verhagen T, Wouters L, Loos MJA, Roumen RMH, Scheltinga MRM. Groin pain characteristics and recurrence rates: three‐year results of a randomized controlled trial comparing self‐gripping Progrip mesh and sutured polypropylene mesh for open inguinal hernia repair. Ann Surg 2018; 267: 1028–1033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Forest plot comparing mean VAS‐score of glue‐fixation and suture fixation at 1 week postoperatively.
Figure S2. Forest plot comparing mean VAS‐score of glue‐fixation and suture fixation at 1 month postoperatively.
Figure S3. Forest plot comparing the incidence of chronic pain (VAS > 3) of glue‐fixation and suture fixation at 12 month postoperatively.
Figure S4. Forest plot comparing mean VAS‐score of ProGripÔ and suture fixation at 1 week postoperatively.
Figure S5. Forest plot comparing mean VAS‐score of ProGripÔ and suture fixation at 1 month postoperatively.
Figure S6. Forest plot comparing the incidence of chronic pain (VAS > 3) of ProGripÔ and suture fixation at 12 months postoperatively.
Table S1. Search in Embase, Cochrane CENTRAL, Pubmed
Table S2. complications after mesh placement; hematoma, seroma or surgical site infection. Comparing glue fixation to suture fixation and ProGripÔ to suture fixation.


