Abstract
Background
In sub‐Saharan Africa, surgical access is limited by an inadequate surgical workforce, lack of infrastructure and decreased care‐seeking by patients. Delays in treatment can result from delayed presentation (pre‐hospital), delays in transfer (intrafacility) or after arrival at the treating centre (in‐hospital delay; IHD). This study evaluated the effect of IHD on mortality among patients undergoing emergency general surgery and identified factors associated with IHD.
Methods
Utilizing Malawi's Kamuzu Central Hospital Emergency General Surgery database, data were collected prospectively from September 2013 to November 2017. Included patients had a diagnosis considered to warrant urgent or emergency intervention for surgery. Bivariable analysis and Poisson regression modelling was done to determine the effect of IHD (more than 24 h) on mortality, and identify factors associated with IHD.
Results
Of 764 included patients, 281 (36·8 per cent) had IHDs. After adjustment, IHD (relative risk (RR) 1·68, 95 per cent c.i. 1·01 to 2·78; P = 0·045), generalized peritonitis (RR 4·49, 1·69 to 11·95; P = 0·005) and gastrointestinal perforation (RR 3·73, 1·25 to 11·08; P = 0·018) were associated with a higher risk of mortality. Female sex (RR 1·33, 1·08 to 1·64; P = 0·007), obtaining any laboratory results (RR 1·58, 1·29 to 1·94; P < 0·001) and night‐time admission (RR 1·59, 1·32 to 1·90; P < 0·001) were associated with an increased risk of IHD after adjustment.
Conclusion
IHDs were associated with increased mortality. Increased staffing levels and operating room availability at tertiary hospitals, especially at night, are needed.
Introduction
Access to safe, timely and affordable surgical care is limited for over five billion people globally, most of whom live in low‐ and middle‐income countries (LMICs)1. Sub‐Saharan Africa bears a disproportionate burden compared with other regions, with approximately 35·7–99·4 per cent of the population unable to access surgical care2. Countries with low annual per capita healthcare expenditure (less than €350 per person) often prioritize maternal and child healthcare, and caesarean section alone can account for one‐third of all procedures in some countries3. The resulting deficit in general surgical and orthopaedic care creates a large burden of surgical disease.
Delays in surgical intervention for emergency conditions increase mortality4, 5, 6, 7, 8, 9, 10, 11, 12. The three primary sources of delay to surgical care for patients in limited‐resource settings include: delay in seeking care (pre‐hospital), delay in transferring to a facility equipped to perform the procedure (interfacility), and delay from presentation at a hospital able to provide definitive care to the start of the operative intervention (in‐hospital delays; IHDs). Numerous reasons for IHDs have been described in limited‐resource settings, including lack of human resources, infrastructure and equipment1, 13, 14. Few studies have assessed the impact of IHDs on perioperative mortality, or examined factors associated with IHDs.
Malawi is a landlocked country in south‐east Africa that can serve as a proxy for countries in the region. Access to surgical care is limited15, 16. The primary objective of the present study was to determine the effect of IHDs on in‐hospital mortality related to surgical interventions for emergency or urgent surgical conditions at a tertiary care centre. A secondary objective was to determine factors related to IHDs, in order to identify areas for future intervention. It was hypothesized that patients with emergency surgical conditions whose operations were delayed beyond 24 h after arrival in the hospital would have higher postoperative mortality than patients receiving earlier surgery.
Methods
This analysis involved a cohort of patients collected prospectively in the Emergency General Surgery database who presented with abdominal symptoms to Kamuzu Central Hospital (KCH) in Lilongwe, Malawi. KCH is a 900‐bed tertiary hospital, acting as the referral centre for about six million people in the central region of Malawi. During the study period, surgical care was provided by four full‐time general surgeons, six surgical clinical officers, and 11 Malawian general surgery residents. KCH had four fully functional operating rooms staffed by one anaesthesiologist and six clinical officer anaesthetists. There were four adult ICU beds with ventilators. Available radiographic studies included plain and contrast radiography, abdominal ultrasonography and echocardiography. CT was available inconsistently.
All surgical patients, including children, who presented to the department as an emergency with abdominal pain from September 2013 to November 2017 were entered into a prospectively developed database. Data collected included basic demographics, presentation history, clinical characteristics, admission diagnosis, surgical interventions and outcomes. The database was maintained by data clerks and updated at KCH, with oversight from surgical residents and faculty.
Patients were included in the analysis if their surgical acuity was deemed an emergency or considered urgent based on admission diagnosis, determined by the admitting surgical team. These diagnoses included generalized peritonitis, acute appendicitis, bowel or gastric perforation, volvulus, non‐reducible hernia, and overt abdominal wound dehiscence. Peritonitis was based on clinical symptoms as assessed by the surgeon, reflecting both suspected visceral perforation and primary peritonitis, an entity seen in Malawi and other LMICs17. Patients managed without surgery, or whose surgery was delayed for more than 5 days, were excluded. In‐hospital delay to operative intervention was defined as a delay of more than 24 h from admission to operation. Diagnoses where a delay of more than 24 h was considered clinically appropriate were excluded.
The University of North Carolina institutional review board and the Malawi National Health Service review committee approved the study.
Statistical analysis
Statistical characterization and comparisons were done with mean(s.d.) values, Student's t and Pearson's χ2 test as appropriate, using Stata® version 15.1 (StataCorp, College Station, Texas, USA). Bivariable and multivariable Poisson regression modelling were used to determine the relative risk (RR) of mortality for IHDs and other patient and clinical characteristics18. A priori, the factors included were: delayed surgery; patient characteristics (sex, age, co‐morbidities and pre‐hospital delay from symptom onset); and presentation and clinical characteristics (presentation year, abnormalities in initial vital signs (shock, defined as a shock index greater than 0·7 and tachypnoea), presenting diagnosis, admission ward). Similar analyses and multivariable modelling were applied to identify patient and presentation factors associated with IHD. Factors potentially associated with delay included: age, sex, transfer status, type of referring facility, days of pre‐hospital delay from onset, admission diagnosis, initial vital signs (shock and tachypnoea), presence of co‐morbidities, types of preoperative imaging, having any preoperative laboratory results, and weekend versus weekday presentation. Variables significant at P < 0·050 were included in the multivariable model.
Results
Over the study interval, the KCH acute care surgery database enrolled a total of 2214 patients, of whom 1450 did not meet study inclusion criteria (Fig. 1). Of the 764 included patients, 281 (36·8 per cent) experienced IHD (Table 1).
Figure 1.
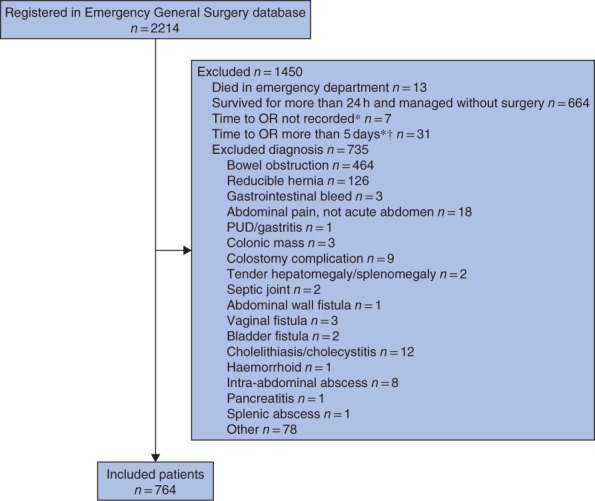
Inclusion of patients in the study. *For patients not excluded for other reasons. †Patients who waited for more than 5 days for the operating room (OR) were excluded as they were unlikely to have had an emergency condition; either misdiagnosis or clinical improvement was assumed to account for such a long delay. PUD, peptic ulcer disease
Table 1.
Details of patients with in‐hospital surgical delay and timely surgical intervention
| All patients (n = 764) | Timely surgery (n = 483) | In‐hospital surgical delay (n = 281) | P ‡ | |
|---|---|---|---|---|
| Age (years)* | 35·7(18·1) | 35·3(17·8) | 36·4(18·5) | 0·212§ |
| Sex ratio (F : M) | 155 : 609 | 82 : 401 | 73 : 208 | 0·003 |
| Transferred | 646 of 762 (84·8) | 415 of 482 (86·1) | 231 of 280 (82·5) | 0·182 |
| Transferred from | 0·187 | |||
| Health centre | 122 (18·9) | 87 (21·0) | 35 (15·2) | |
| District hospital | 425 (65·8) | 262 (63·1) | 163 (70·6) | |
| Private hospital | 85 (13·2) | 58 (14·0) | 27 (11·7) | |
| Tertiary hospital | 14 (2·2) | 8 (1·9) | 6 (2·6) | |
| Pre‐hospital delay in presentation | n = 749 | n = 474 | n = 275 | 0·003 |
| < 24 h | 129 (17·2) | 84 (17·7) | 45 (16·4) | 0·635 |
| 24–48 h | 100 (13·4) | 78 (16·5) | 22 (8·0) | 0·001 |
| 49–72 h | 110 (14·7) | 71 (15·0) | 39 (14·2) | 0·77 |
| > 3 days | 410 (54·7) | 241 (50·8) | 169 (61·5) | 0·005 |
| Weekend presentation | 163 (21·3) | 97 (20·1) | 66 (23·5) | 0·268 |
| Night‐time admission | 194 (25·4) | 101 (20·9) | 93 (33·1) | < 0·001 |
| Any co‐morbidity† | 94 of 720 (13·1) | 67 of 450 (14·9) | 27 of 270 (10·0) | 0·063 |
| Year of admission | < 0·001 | |||
| 2013 | 36 (4·7) | 24 (5·0) | 12 (4·3) | 0·660 |
| 2014 | 250 (32·7) | 171 (35·4) | 79 (28·1) | 0·038 |
| 2015 | 172 (22·5) | 119 (24·6) | 53 (18·9) | 0·065 |
| 2016 | 138 (18·1) | 87 (18·0) | 51 (18·1) | 0·962 |
| 2017 | 168 (22·0) | 82 (17·0) | 86 (30·6) | < 0·001 |
| Occupation | 0·008 | |||
| Farmer | 336 (44·0) | 210 (43·6) | 126 (44·8) | 0·733 |
| Other employment | 218 (28·6) | 144 (29·9) | 74 (26·3) | 0·296 |
| Student/child | 134 (17·6) | 93 (19·3) | 41 (14·6) | 0·100 |
| Unemployed | 75 (9·8) | 35 (7·3) | 40 (14·2) | 0·002 |
Values in parentheses are percentages unless indicated otherwise;
values are mean(s.d.)
Includes tuberculosis, history of recent treatment for malaria, hypertension, diabetes, known cancer and mental disability.
χ2 test, except §Student's t test.
The mean age of all patients was 35·7(18·1) years, with no age difference between patients with IHD and those with a timely surgical intervention. Children under the age of 16 years represented 9·9 per cent (76 patients) of the total population. Women comprised 20·3 per cent (155 patients) of the entire cohort, but 26·0 per cent (73 women) of the IHD cohort (P = 0·003).
Most patients (646, 84·8 per cent) were transferred from another facility. Transfer rates did not differ between the IHD and timely intervention groups, nor did the type of transferring facility (Table 1). Weekday or weekend presentation was not associated with IHD (P = 0·268), neither was shock or tachypnoea on arrival (Table 2). Overall, only 13·1 per cent of patients had any co‐morbidity, which, again, was not associated with IHD (Table 1). The two most common diagnoses were generalized peritonitis (26·7 per cent) and incarcerated hernia (26·2 per cent) (Table 2). Admission diagnoses did not differ between patients subjected to IHD and those considered to have received timely intervention.
Table 2.
Admission details for patients with timely surgery intervention and in‐hospital surgical delay
| All patients (n = 764) | Timely surgery (n = 483) | In‐hospital surgical delay (n = 281) | P † | |
|---|---|---|---|---|
| Admission diagnosis | 0·165 | |||
| Acute abdomen/peritonitis | 204 (26·7) | 122 (25·3) | 82 (29·2) | |
| Acute appendicitis | 104 (13·6) | 63 (13) | 41 (14·6) | |
| Bowel or gastric perforation | 109 (14·3) | 66 (13·7) | 43 (15·3) | |
| Volvulus | 135 (17·7) | 84 (17·4) | 51 (18·1) | |
| Hernia, irreducible | 200 (26·2) | 142 (29·4) | 58 (20·6) | |
| Other | 12 (1·6) | 6 (1·2) | 6 (2·1) | |
| Admission ward | n = 763 | n = 482 | n = 281 | 0·604 |
| To operating room | 6 (0·8) | 5 (1·0) | 1 (0·4) | |
| Surgical ward | 671 (87·9) | 417 (86·5) | 254 (90·4) | |
| Children's ward | 58 (7·6) | 40 (8·3) | 18 (6·4) | |
| Other ward | 5 (0·7) | 4 (0·8) | 1 (0·4) | |
| Intermediate care | 14 (1·8) | 9 (1·9) | 5 (1·8) | |
| ICU | 9 (1·2) | 7 (1·5) | 2 (0·7) | |
| Admission BP | n = 511 | n = 313 | n = 198 | 0·934 |
| Hypotensive | 21 (4·1) | 13 (4·2) | 8 (4·0) | |
| Normotensive | 401 (78·5) | 244 (78·0) | 157 (79·3) | |
| Hypertensive | 89 (17·4) | 56 (17·9) | 33 (16·7) | |
| Admission heart rate | n = 522 | n = 322 | n = 200 | 0·068 |
| Bradycardia | 21 (4·0) | 18 (5·6) | 3 (1·5) | |
| Normal | 290 (55·6) | 177 (55·0) | 113 (56·5) | |
| Tachycardia | 211 (40·4) | 127 (39·4) | 84 (42·0) | |
| Shock* | 312 of 510 (61·2) | 185 of 312 (59·3) | 127 of 198 (64·1) | 0·274 |
| Admission respiratory rate | n = 445 | n = 279 | n = 166 | 0·735 |
| Bradypnoea | 2 (0·4) | 1 (0·4) | 1 (0·6) | |
| Normal | 192 (43·1) | 117 (41·9) | 75 (45·2) | |
| Tachypnoea | 251 (56·4) | 161 (57·7) | 90 (54·2) |
Values in parentheses are percentages.
Defined as shock index (heart rate/systolic blood pressure) above 0·7.
χ2 test.
Patients admitted at night (between 18·00 and 06·00 hours) experienced more IHDs than those with daytime admission (33·1 versus 20·9 per cent respectively; P < 0·001), and more patients in the IHD group were unemployed (14·2 versus 7·3 per cent; P = 0·002). The overall pre‐hospital delay from first symptoms to presentation at KCH differed between the two groups (P = 0·003). Delays before arrival at KCH were common; only 129 patients (17·2 per cent) presented within 24 h of the onset of symptoms (Table 1). In univariable regression analysis, patients presenting to KCH within 24–48 h of symptom onset were less likely to experience IHD (P = 0·001) than those who presented within 24 h of symptom onset, whereas patients who presented more than 3 days after symptoms started were more likely to experience IHD (P = 0·005). Patients who presented within 24 h of symptom onset were less likely to have shock (39·1 per cent versus 60·9 per cent in those with a later presentation; P < 0·001).
Most patients were admitted to the surgical ward (87·9 per cent) (Table 2). Only six patients (0·8 per cent) went directly to the operating room before admission to a ward, although this did not necessarily mean expedited surgical care. Admissions to intermediate care (1·8 per cent) and ICU (1·2 per cent) were rare. Admission location was not associated with IHD (P = 0·604).
Clinical and demographic factors associated with an increased risk of IHD are shown in Table 3. Univariable analysis indicated that female sex (RR 1·38, 95 per cent c.i. 1·13 to 1·68; P = 0·002), night‐time admission (RR 1·54, 1·29 to 1·85; P < 0·001), generalized peritonitis (RR 1·39, 1·05 to 1·82; P = 0·020) and time to obtain laboratory results at KCH (RR 1·60, 1·31 to 1·95; P < 0·001) were associated with a greater risk of delay. Duration of pre‐hospital delay, including delays in presentation and in transfer from a referring facility, were associated with IHD, with pre‐hospital delay of 24–48 h having a lower risk (RR 0·63, 0·41 to 0·98; P = 0·039). Except for generalized peritonitis, these factors remained significant in the multivariable model (Table 3), whereas patient age, type of referring facility, abnormal vital signs or shock on admission, year of admission, admission ward and preoperative imaging were not associated with IHD.
Table 3.
Univariable and multivariable Poisson regression of factors associated with in‐hospital delay to surgery
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| Relative risk | P | Relative risk | P | |
| Age category (years) | ||||
| 0–10 | 0·93 (0·63, 1·37) | 0·707 | ||
| 11–20 | 0·73 (0·52, 1·01) | 0·055 | ||
| 21–40 | 1·00 (reference) | |||
| 41–60 | 0·91 (0·71, 1·15) | 0·429 | ||
| > 60 | 1·11 (0·85, 1·46) | 0·447 | ||
| Female sex | 1·38 (1·13, 1·68) | 0·002 | 1·33 (1·08, 1·64) | 0·007 |
| Transferred | 0·85 (0·67, 1·07) | 0·168 | ||
| Transferred from | ||||
| Health centre | 1·00 (reference) | |||
| District hospital | 1·34 (0·99, 1·81) | 0·062 | ||
| Private hospital | 1·11 (0·73, 1·68) | 0·634 | ||
| Tertiary hospital | 1·49 (0·77, 2·91) | 0·238 | ||
| Pre‐hospital delay in presentation | ||||
| < 24 h | 1·00 (reference) | 1·00 (reference) | ||
| 24–48 h | 0·63 (0·41, 0·98) | 0·039 | 0·63 (0·41, 0·96) | 0·031 |
| 49–72 h | 1·01 (0·72, 1·44) | 0·927 | 0·93 (0·67, 1·30) | 0·667 |
| > 3 days | 1·18 (0·91, 1·54) | 0·213 | 1·07 (0·83, 1·38) | 0·600 |
| Shock | 1·14 (0·90, 1·43) | 0·279 | ||
| Initial respiratory rate | ||||
| Normal | 1·00 (reference) | |||
| Tachypnoea | 0·92 (0·72, 1·17) | 0·472 | ||
| Admission diagnosis | ||||
| Acute abdomen/peritonitis | 1·39 (1·05, 1·82) | 0·020 | 1·24 (0·94, 1·63) | 0·134 |
| Acute appendicitis | 1·36 (0·98, 1·88) | 0·062 | 1·37 (0·99, 1·89) | 0·059 |
| Bowel or gastric perforation | 1·36 (0·99, 1·87) | 0·058 | 1·19 (0·86, 1·63) | 0·295 |
| Volvulus | 1·30 (0·96, 1·77) | 0·091 | 1·29 (0·94, 1·76) | 0·108 |
| Hernia, irreducible | 1·00 (reference) | 1·00 (reference) | ||
| Other | 1·72 (0·94, 3·16) | 0·078 | 1·45 (0·82, 2·59) | 0·205 |
| Year of admission | ||||
| 2013 | 1·00 (reference) | |||
| 2014 | 0·95 (0·58, 1·56) | 0·833 | ||
| 2015 | 0·92 (0·55, 1·54) | 0·764 | ||
| 2016 | 1·11 (0·67, 1·85) | 0·692 | ||
| 2017 | 1·54 (0·94, 2·49) | 0·083 | ||
| Weekend presentation | 1·13 (0·91, 1·40) | 0·259 | ||
| Night‐time admission | 1·54 (1·29, 1·85) | < 0·001 | 1·59 (1·32, 1·90) | < 0·001 |
| Admission ward | ||||
| To operating room | 1·00 (reference) | |||
| Surgical ward | 2·27 (0·38, 13·60) | 0·370 | ||
| Children's ward | 1·86 (0·30. 11·60) | 0·506 | ||
| Other ward | 1·20 (0·10, 14·70) | 0·887 | ||
| Intermediate care | 2·14 (0·31, 14·70) | 0·437 | ||
| ICU | 1·33 (0·15, 11·60) | 0·795 | ||
| Preoperative imaging* | ||||
| None | 0·92 (0·75, 1·13) | 0·415 | ||
| X‐ray | 1·00 (0·83, 1·22) | 0·982 | ||
| Ultrasound | 1·22 (0·98, 1·52) | 0·073 | ||
| CT | 0·39 (0·06, 2·38) | 0·305 | ||
| Time to obtain laboratory results | 1·60 (1·31, 1·95) | < 0·001 | 1·58 (1·29, 1·94) | < 0·001 |
Values in parentheses are 95 per cent confidence intervals.
Patients may have had more than one type of imaging study.
The mortality rate for patients in the IHD group was higher than that for patients who had timely surgery: 47 of 281 (16·7 per cent) versus 43 of 483 (8·9 per cent) respectively (P = 0·001) (Fig. 2). Based on these mortality rates, a post hoc power calculation using the χ2 test demonstrated a power of 88·5 per cent.
Figure 2.
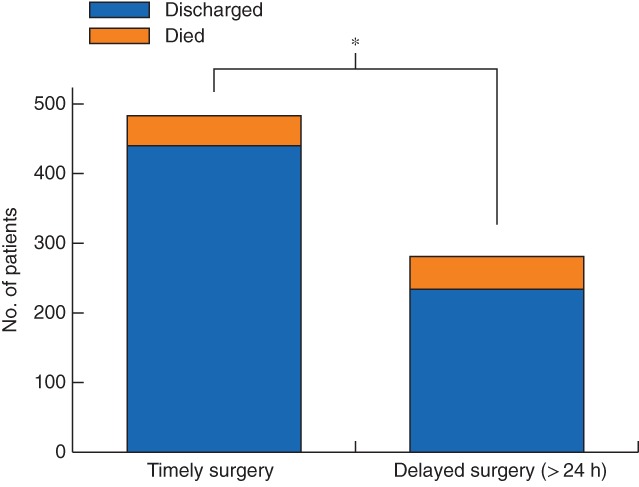
Mortality for timely and delayed emergency abdominal surgery in a central hospital in Malawi. *P = 0·001 (χ2 test)
In adjusted multivariable analysis, IHD of more than 24 h was associated with a relative mortality risk of 1·68 (95 per cent c.i. 1·01 to 2·78; P = 0·045) (Table 4). Although older age and a pre‐hospital delay of more than 3 days were associated with mortality in univariable analysis, in adjusted analysis only IHD and admission diagnoses (generalized peritonitis: RR 4·49, 1·69 to 11·95, P = 0·003; gastrointestinal perforation: RR 3·73, 1·25 to 11·08, P = 0·018) remained associated with an increased mortality risk.
Table 4.
Univariable and multivariable Poisson regression of factors related to mortality
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| Relative risk | P | Relative risk | P | |
| In‐hospital surgical delay | 1·88 (1·28, 2·77) | 0·001 | 1·68 (1·01, 2·78) | 0·045 |
| Age category (years) | ||||
| 0–10 | 0·22 (0·03, 1·57) | 0·131 | 0·00 (0·00, 0·00) | < 0·001 |
| 11–20 | 1·20 (0·64, 2·25) | 0·577 | 1·01 (0·40, 2·50) | 0·991 |
| 21–40 | 1·00 (reference) | 1·00 (reference) | ||
| 41–60 | 1·68 (1·04, 2·73) | 0·035 | 1·57 (0·85, 2·88) | 0·151 |
| > 60 | 2·37 (1·41, 3·99) | 0·001 | 1·50 (0·71, 3·18) | 0·293 |
| Female sex | 1·05 (0·65, 1·82) | 0·836 | 0·68 (0·34, 1·38) | 0·287 |
| Pre‐hospital delay in presentation | ||||
| < 24 h | 1·00 (reference) | 1·00 (reference) | ||
| 24–48 h | 1·15 (0·46, 2·86) | 0·770 | 0·35 (0·08, 1·62) | 0·180 |
| 49–72 h | 1·43 (0·62, 3·33) | 0·403 | 0·72 (0·25, 2·08) | 0·548 |
| > 3 days | 2·13 (1·09, 4·17) | 0·027 | 1·18 (0·54, 2·60) | 0·681 |
| Shock | 1·43 (0·87, 2·34) | 0·159 | 1·28 (0·71, 2·33) | 0·416 |
| Initial respiratory rate | ||||
| Normal | 1·00 (reference) | 1·00 (reference) | ||
| Tachypnoea | 0·70 (0·43, 1·13) | 0·143 | 0·66 (0·40, 1·07) | 0·090 |
| Admission diagnosis | ||||
| Acute abdomen/peritonitis | 6·54 (2·83, 15·10) | < 0·001 | 4·49 (1·69, 11·95) | 0·003 |
| Acute appendicitis | 1·28 (0·37, 4·45) | 0·695 | 1·35 (0·34, 5·42) | 0·673 |
| Bowel or gastric perforation | 7·65 (3·23, 18·10) | < 0·001 | 3·73 (1·25, 11·08) | 0·018 |
| Volvulus | 3·70 (1·47, 9·32) | 0·005 | 2·64 (0·84, 8·26) | 0·097 |
| Hernia, irreducible | 1·00 (reference) | 1·00 (reference) | ||
| Other | 0·00 (0·0, 0·00) | < 0·001 | 0·00 (0·00, 0·00) | < 0·001 |
| Any co‐morbidity | 0·89 (0·48, 1·66) | 0·709 | 0·74 (0·27, 2·02) | 0·552 |
Values in parentheses are 95 per cent confidence intervals.
Discussion
At a tertiary care facility in Malawi capable of delivering definitive surgical care for abdominal emergencies, 36·8 per cent of patients who met indications for emergency or urgent surgery on admission waited for longer than 24 h for their procedure. IHDs of more than 24 h for abdominal emergencies increased the risk of in‐hospital mortality by 67 per cent, compared with the risk in patients who received timely interventions (less than 24 h), after controlling for relevant co‐variables including pre‐hospital delay. Only female sex, night‐time admission and obtaining any laboratory results increased the risk of IHDs on adjusted analysis.
Existing data suggest that delays to surgical intervention are common in low‐resource settings, resulting in worse clinical outcomes. Timely operative intervention is a guiding surgical principle of acute abdominal emergencies8, 12, 19. The rate of IHDs of 36·8 per cent in the present study was similar to that in an earlier study20 at a well staffed teaching hospital in Nigeria, where 50 per cent of patients waited over 24 h, and 16 per cent waited more than 48 h for operative intervention. At a regional hospital in Uganda21 48 per cent of 31 operations were delayed (median delay 14·8 h), and in the Ivory Coast10 86 per cent of patients had a delay of more than 24 h from symptom onset to surgery, with more than 36 per cent waiting over 48 h. Delays were defined in the present study as longer than 24 h. Most surgeons would agree that this is too long to wait for emergency care, and several other studies, especially in LMICs, have used this definition8, 11, 12, 22, although some high‐income countries (HICs) have used shorter times7, 8, 22, 23. Future research to measure specific time intervals, including time to decision to operate, time to diagnostic studies and exact times to procedures, should clarify the length of an acceptable in‐hospital wait.
IHDs have been associated with worse outcomes in both HICs and LMICs7, 10. The overall mortality rate in the present study of 11·8 per cent was similar to rates of 10–19 per cent seen in other series10, 15, 24, 25 of abdominal operations in the region. In HICs, delays are often considered to have shorter intervals of less than 6 or 12 h7, 8, 22. Even these shorter delays are associated with increased mortality for emergency abdominal surgery7, 8, 12, as well as specific conditions including perforated diverticulitis11 and peptic ulcer disease9. In two Danish cohort studies9, 12, each hour of operative delay was associated with a 2 per cent reduction in survival. In sub‐Saharan Africa, limited data suggest that IHDs are also associated with worse outcomes for specific conditions. Patients with perforated peptic ulcer disease in the Ivory Coast had a hazard ratio for mortality of 15·6 if surgery was delayed more than 24 h from symptom onset10, and in patients with traumatic brain injury in Uganda IHDs increased mortality26.
Patients in LMICs encounter multiple types of delay, pre‐hospital, intrafacility and in‐hospital, that can affect mortality. Pre‐hospital delay was controlled for in this analysis to investigate the specific impact of in‐hospital delay on mortality. Interestingly, patients with 24–48 h of pre‐hospital delay were least likely to have IHD, whereas both shorter and longer pre‐hospital delays were associated with IHD. In a setting where long pre‐hospital delays are common, providers often observe patients and may not prioritize surgery for patients arriving with less than 1 day of symptoms. Similarly, when patients have a very long pre‐hospital delay, providers may assume less urgency because the patients have already tolerated their symptoms for several days. It is also possible that those with the greatest pre‐hospital delay, who had a higher rate of shock on arrival, experienced IHD as a result of the need for preoperative resuscitation. Much work in LMICs has focused on decreasing pre‐hospital delays by improving patient access to facilities where surgery can be performed. This study highlights that hospital arrival alone did not lead to rapid surgical intervention for many emergency surgical patients. Quality improvement efforts must identify and address the specific drivers of IHDs to decrease perioperative mortality in this population.
The reasons for delays in resource‐limited environments are context‐dependent. The Lancet Commission on Global Surgery proposed various reasons for IHD, including inadequate infrastructure and personnel, in addition to lack of consumables to address emergencies1, 14. Other studies have categorized delays as administrative, logistical or process‐based13. Although the present study found only female sex, night‐time presentation and obtaining laboratory results to be associated with IHD in adjusted analysis, it is acknowledged that the study was unable to consider several administrative and system factors. Availability of surgeons, supporting staff and operating room facilities, along with standards and speed of resuscitation, may all have been contributors to delay.
The disparities in delay to surgical care by sex have not been described previously. Female patients' abdominal symptoms may initially be diagnosed as gynaecological, delaying general surgical evaluation. Data regarding presurgical evaluation by other services were not available. Gender biases may influence providers' willingness to expedite surgical and anaesthetic care, decreasing the chances of timely intervention for women. Sociocultural norms may affect how women present, leading to downplaying of symptoms or providers attributing symptoms to ‘hysteria’.
IHDs were more common at night at KCH, a phenomenon also noted in Nigeria20. IHDs have consequences beyond increased mortality for emergency surgical patients admitted at night, as the backlog that develops can compound delays the following day for surgical services. Increasing operating room availability and staffing, including an on‐call or backup team to staff additional operating theatres, and improved access to equipment could significantly reduce IHDs associated with night‐time admissions.
Studies on risk of IHD to surgery in both low‐ and high‐resource settings have identified patient‐related constraints14. In Nigeria, financial constraints and delays for investigations were considered important factors leading to delays for abdominal emergencies20. In that healthcare system, patients must provide their own antibiotics and intravenous fluids. Although the role of patient resources in IHDs at KCH was not evaluated specifically, available supplies at KCH were provided free to patients, so this element was unlikely to have delayed operations significantly. Conversely, limited access to transport, shortages or malfunctions in key equipment, including sterilization and operative supplies, were not uncommon at KCH, although the extent of their contribution to delays was not evaluated.
Several studies7, 8, 13, 20, 26, 27 have noted delays associated with obtaining diagnostic test results. Preoperative imaging was not associated with IHDs in this cohort, but the minority of patients who had preoperative laboratory assessments did experience more delay. Although haemoglobin results were usually available within a few hours, biochemistry results could be delayed for days at KCH. The reason why obtaining laboratory work delayed surgery remains unclear.
A number of limitations reflect the design of the present study. In selecting only surgical patients with recorded times to intervention for whom the admission diagnosis was consistent with the need for urgent surgery, a specific cohort of patients were analysed from the registry. It is possible that some patients were thought to have improved after initial evaluation, resulting in longer times to intervention. The study may have underestimated the impact of IHDs on mortality, as patients who never made it to the operating room were excluded, as were those delayed as a result of initial misdiagnosis and patients for whom exact times from admission or decision to operate to surgery were not recorded.
Surgical delays for emergency general surgery conditions were common in this population in Malawi, with over one‐third of patients who experienced delays having a significantly higher risk of mortality. Quality improvement work focused on IHDs could decrease mortality in sub‐Saharan Africa. These efforts should focus on improving delivery of surgical care, not just at central hospitals but across all levels of the healthcare system, including district hospitals, to decrease in‐hospital and other sources of patient delay.
Acknowledgements
Trauma registry data are maintained for use by the Malawi Ministry of Health. Access to data is available with approval from the ministry.
Disclosure: The authors declare no conflict of interest.
Presented to the Scientific Forum at the American College of Surgeons Clinical Congress, Boston, Massachusetts, USA, October 2018
Funding information
No funding
References
- 1. Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386: 569–624. [DOI] [PubMed] [Google Scholar]
- 2. Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA et al. Global access to surgical care: a modelling study. Lancet Glob Health 2015; 3: e316–e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe‐Leitz T et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 2016; 94: 201F–209F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bulters D, Belli A. A prospective study of the time to evacuate acute subdural and extradural haematomas. Anaesthesia 2009; 64: 277–281. [DOI] [PubMed] [Google Scholar]
- 5. Chan G, Butterworth SA. Audit of emergent and urgent surgery for acutely ill pediatric patients: is access timely? J Pediatr Surg 2016; 51: 838–842. [DOI] [PubMed] [Google Scholar]
- 6. Harfouche M, Hosseinipour M, Kaliti S, Wilkinson J. Quality indicators and outcomes of emergency caesarean deliveries at a district‐level maternity hospital. Afr J Reprod Health 2015; 19: 61–67. [PubMed] [Google Scholar]
- 7. McIsaac DI, Abdulla K, Yang H, Sundaresan S, Doering P, Vaswani SG et al. Association of delay of urgent or emergency surgery with mortality and use of health care resources: a propensity score‐matched observational cohort study. CMAJ 2017; 189: E905–E912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ong M, Guang TY, Yang TK. Impact of surgical delay on outcomes in elderly patients undergoing emergency surgery: a single center experience. World J Gastrointest Surg 2015; 7: 208–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buck DL, Vester‐Andersen M, Møller MH; Danish Clinical Register of Emergency Surgery . Surgical delay is a critical determinant of survival in perforated peptic ulcer. Br J Surg 2013; 100: 1045–1049. [DOI] [PubMed] [Google Scholar]
- 10. Gona SK, Alassan MK, Marcellin KG, Henriette KY, Adama C, Toussaint A et al. Postoperative morbidity and mortality of perforated peptic ulcer: retrospective cohort study of risk factors among Black Africans in Côte d'Ivoire. Gastroenterol Res Pract 2016; 2016: 2640730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mozer AB, Spaniolas K, Sippey ME, Celio A, Manwaring ML, Kasten KR. Post‐operative morbidity, but not mortality, is worsened by operative delay in septic diverticulitis. Int J Colorectal Dis 2017; 32: 193–199. [DOI] [PubMed] [Google Scholar]
- 12. Vester‐Andersen M, Lundstrøm LH, Buck DL, Møller MH. Association between surgical delay and survival in high‐risk emergency abdominal surgery. A population‐based Danish cohort study. Scand J Gastroenterol 2016; 51: 121–128. [DOI] [PubMed] [Google Scholar]
- 13. Kumar V, Khajanchi M, Raykar NP, Gerdin M, Roy N. Waiting at the hospital door: a prospective, multicentre assessment of third delay in four tertiary hospitals in India. Lancet 2015; 385(Suppl 2): S24. [DOI] [PubMed] [Google Scholar]
- 14. Raykar NP, Yorlets RR, Liu C, Greenberg SL, Kotagal M, Goldman R et al. A qualitative study exploring contextual challenges to surgical care provision in 21 LMICs. Lancet 2015; 385(Suppl 2): S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gallaher JR, Cairns B, Varela C, Charles AG. Mortality after peritonitis in sub‐Saharan Africa: an issue of access to care. JAMA Surg 2017; 152: 408–410. [DOI] [PubMed] [Google Scholar]
- 16. Lavy C, Tindall A, Steinlechner C, Mkandawire N, Chimangeni S. Surgery in Malawi – a national survey of activity in rural and urban hospitals. Ann R Coll Surg Engl 2007; 89: 722–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Savoie PH, Peycru T, Mingoutaud L, Sow A, Biance N, Pauleau G et al. [Primary peritonitis in sub‐Saharian Africa: a 15 case series.] Med Trop (Mars) 2007; 67: 154–158. [PubMed] [Google Scholar]
- 18. Chen W, Qian L, Shi J, Franklin M. Comparing performance between log‐binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol 2018; 18: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schneider C, Tyler LE, Scull EF, Pryle BJ, Barr H. A case–control study investigating factors of preoperative delay in emergency laparotomy. Int J Surg 2015; 22: 131–135. [DOI] [PubMed] [Google Scholar]
- 20. Adamu A, Maigatari M, Lawal K, Iliyasu M. Waiting time for emergency abdominal surgery in Zaria, Nigeria. Afr Health Sci 2010; 10: 46–53. [PMC free article] [PubMed] [Google Scholar]
- 21. Nwanna‐Nzewunwa OC, Ajiko MM, Kirya F, Epodoi J, Kabagenyi F, Batibwe E et al. Barriers and facilitators of surgical care in rural Uganda: a mixed methods study. J Surg Res 2016; 204: 242–250. [DOI] [PubMed] [Google Scholar]
- 22. Vogel TR, Dombrovskiy VY, Lowry SF. In‐hospital delay of elective surgery for high volume procedures: the impact on infectious complications. J Am Coll Surg 2010; 211: 784–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dobson H, Ranasinghe WK, Hong MK, Bray LN, Sathveegarajah M, Vally F et al. Waiting for definitive care: an analysis of elapsed time from decision to surgery or transfer in a rural centre. Aust J Rural Health 2015; 23: 155–160. [DOI] [PubMed] [Google Scholar]
- 24. McConkey SJ. Case series of acute abdominal surgery in rural Sierra Leone. World J Surg 2002; 26: 509–513. [DOI] [PubMed] [Google Scholar]
- 25. Aderounmu AO, Adeoti ML, Oguntola AS, Oboro VO, Fadiora SO, Akanbi OO et al. Pattern and outcome of emergency surgery in a new Nigerian teaching hospital the LAUTECH Osogbo experience. Niger Postgrad Med J 2006; 13: 172–175. [PubMed] [Google Scholar]
- 26. Vaca SD, Kuo BJ, Nickenig Vissoci JR, Staton CA, Xu LW, Muhumuza M et al. Temporal delays along the neurosurgical care continuum for traumatic brain injury patients at a tertiary care hospital in Kampala, Uganda. Neurosurgery 2019; 84: 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Garfield JL, Birkhahn RH, Gaeta TJ, Briggs WM. Diagnostic pathways and delays on route to operative intervention in acute appendicitis. Am Surg 2004; 70: 1010–1013. [PubMed] [Google Scholar]


