Abstract
Background
Pseudomyxoma peritonei (PMP) is a rare disease, most commonly of appendiceal origin. Treatment consists of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS–HIPEC). The aim of this study was to identify prognostic factors for recurrence and survival.
Methods
This was an observational study using a prospectively designed database containing consecutive patients with PMP originating from the appendix, undergoing CRS–HIPEC at a tertiary referral centre between 1996 and 2015. Histopathological slides were reassessed. Cox regression was used for multivariable analyses.
Results
Of 225 patients identified, 36 (16·0 per cent) were diagnosed with acellular mucin, 149 (66·2 per cent) had disseminated peritoneal adenomucinosis (DPAM) and 40 (17·8 per cent) had peritoneal mucinous carcinomatosis (PMCA). The 5‐year overall survival (OS) rates were 93, 69·8 and 55 per cent respectively. Recurrence was observed in 120 patients (53·3 per cent), 39 of whom (17·3 per cent) were treated with a second CRS–HIPEC procedure. Factors independently associated with poor disease‐free survival were six or seven affected regions (hazard ratio (HR) 6·01, 95 per cent c.i. 2·04 to 17·73), incomplete cytoreduction (R2a resection: HR 1·67, 1·05 to 2·65; R2b resection: HR 2·00, 1·07 to 3·73), and more than threefold raised carcinoembryonic antigen (CEA) and/or carbohydrate antigen (CA) 19‐9 level (HR 2·31, 1·30 to 4·11). Factors independently associated with poorer OS were male sex (HR 1·74, 1·09 to 2·77), incomplete cytoreduction (R2a resection: HR 1·87, 1·14 to 3·08; R2b resection: HR 2·28, 1·19 to 4·34), and more than threefold raised CEA and/or CA19‐9 level (HR 2·89, 1·36 to 6·16).
Conclusion
CEA and CA19‐9 levels raised more than threefold above the upper limit identify patients with PMP of appendiceal origin and poorer survival.
Introduction
Pseudomyxoma peritonei (PMP) is a rare disease with an incidence of 1–2 per million per year1, 2. PMP frequently originates from appendiceal lesions. Rarer origins include mucinous colorectal adenocarcinomas or mucinous ovarian tumours3, 4. Traditionally PMP was treated with repeated cytoreductive surgery (CRS) only, but this has been gradually replaced by CRS combined with hyperthermic intraperitoneal chemotherapy (HIPEC)4, 5, 6. After treatment with CRS–HIPEC, the 10‐year overall survival (OS) rate is 50–60 per cent4, 5, 7. Although CRS–HIPEC is a major surgical procedure that significantly impacts quality of life, many patients seem willing to undergo further CRS–HIPEC if required8, 9.
PMP is a clinicopathological syndrome with mucinous ascites, including neoplastic mucinous epithelium within the peritoneal cavity10. Most patients have symptoms at the time of initial diagnosis, with increased abdominal girth, abdominal discomfort, nausea, vomiting or weight loss11. Clinical symptoms are associated with poorer survival11. Other prognostic factors include serum tumour markers and histological findings. Serum tumour marker levels appeared to have a diagnostic and prognostic value in patients with PMP1, 12. Levels of carcinoembryonic antigen (CEA), carbohydrate antigen (CA) 19‐9 and cancer antigen 125 (CA125) may be raised in these patients. Some studies13, 14, 15 have shown that increase in one or more of these tumour markers may be associated with worse prognosis.
PMP is classified histopathologically as acellular mucin, disseminated peritoneal adenomucinosis (DPAM) or peritoneal mucinous carcinomatosis (PMCA)16. Acellular mucin has been associated with the best prognosis17. The aim of this study was to obtain more insight into the clinical course and management of PMP originating from appendiceal neoplasms in patients treated with CRS–HIPEC. Histopathology was reassessed to better determine independent prognostic factors, based on the 20‐year experience in the treatment of PMP at a single institution.
Methods
Patients and setting
This was an observational study performed in the Netherlands Cancer Institute, a tertiary oncology referral centre in Amsterdam. Data from consecutive patients who underwent CRS–HIPEC were entered in a prospectively developed database. Patients diagnosed with PMP originating from a mucinous appendiceal neoplasm who were treated with CRS–HIPEC between January 1996 and December 2015 were included in the study. PMP was defined as a clinical entity consisting of mucinous ascites. Patients were excluded if they had received extra‐abdominal treatment for PMP or had PMP with a primary origin in ovarian or colorectal carcinoma, or an unknown primary location. PMP was diagnosed either clinically or radiologically, and confirmed histologically.
This study received approval of the Translational Research Board of the Netherlands Cancer Institute (study number CFMPB515). All data were processed anonymously. Collection, storage and use of patient‐derived tissue and data were performed in compliance with the Code for Proper Secondary Use of Human Tissue in the Netherlands, Dutch Federation of Biomedical Scientific Societies, the Netherlands.
Diagnosis
Tumour marker levels of CEA and CA19‐9 were recorded for all patients before CRS–HIPEC and repeat CRS–HIPEC. CA125 level was recorded if available. CEA level was considered raised when 6 μg/l or above, CA19‐9 level when 37 kunits/l or above, and CA125 level when 20 kunits/l or more. Subgroups were constructed for CEA and CA19‐9 based on tumour marker levels three times higher than the laboratory reference range. CEA was categorized as follows: no increase, less than 6 μg/l; increase threefold or less, 6–20 μg/l; increase more than threefold, above 20 μg/l. CA19‐9 was categorized as: no increase, less than 37 kunits/l; increase less than threefold or less 37–100 kunits/l; increase more than threefold, above 100 kunits/l.
PMP was originally classified as DPAM, PMCA or PMCA‐I, according to Ronnett and colleagues18. For the present analysis, patients were reclassified as having acellular mucin, DPAM or PMCA according to the 2016 consensus paper of the Peritoneal Surface Oncology Group International group16: acellular mucin is described as mucin without epithelial cells, DPAM as PMP with low‐grade histological features, and PMCA as PMP with high‐grade histological features. Patients with acellular mucin were identified based on a review of all pathology reports. Microscopic slides were reassessed when the histopathological PMP classification was unclear or lacking, in all patients previously classified as having PMCA or PMCA‐I, and when the primary tumour location was unclear. Unidentified primary tumours were approached according to Ronnett et al.18 and classified as appendiceal neoplasms when they fit the criteria19 (following appendicectomy in the past or when no other cause was found in the abdomen).
Surgical treatment
Patients with PMP were treated with CRS–HIPEC after previous debulking surgery. This combined procedure has been described in detail by Verwaal and co‐workers20. The previous surgical score, according to Sugarbaker2, was assessed in all patients based on the previous debulking surgery4. A score of zero indicated diagnosis via biopsy or laparoscopy; for a score of three, the maximum score, complete debulking surgery had been performed. The extent of peritoneal disease was scored using the Dutch region count, which divides the abdomen into seven regions21. A region count of zero indicated no peritoneal disease, and seven affected regions implied peritoneal disease in all regions.
The surgical procedure started with the cytoreductive phase, with the goal of leaving no macroscopic peritoneal disease in the abdomen. The completeness of cytoreduction was recorded. R1 resection indicated no visible macroscopic disease. In R2a resections tumour nodules of less than 2·5 mm were left behind, and in R2b resections peritoneal tumour lesions larger than 2·5 mm were left behind in the abdomen. The cytoreductive phase was followed by HIPEC, designed to eliminate microscopic residual disease. The peritoneal cavity was filled with mitomycin C 35 mg/m2 at 40–41 °C for 90 min. In exceptional cases (with subsequent CRS–HIPEC procedures), oxaliplatin 460 mg/m2 was used intraperitoneally at 42–43 °C for 30 min. After completion of the HIPEC phase, anastomoses were made and stomas created as necessary. After surgery all patients were admitted to the ICU.
Postoperative complications were scored according to the Common Terminology Criteria for Adverse Events (CTCAE) v4.0322. Administration of systemic chemotherapy was not standard of care, but was considered appropriate for some patients with PMCA.
Follow‐up
Patients were scheduled for follow‐up at least annually for a minimum of 10 years after surgery or until death. Follow‐up included serum tumour markers and CT of the abdomen and pelvis annually, for up to 5 years. Thereafter, CT was performed every 2 years and serum tumour markers annually. Recurrences during follow‐up were recorded, including location and treatment. Abnormalities on CT and raised levels of tumour markers at the time of disease recurrence were also recorded.
Statistical analysis
Patient‐, surgery‐ and tumour‐related data were compared between PMP subgroups. Categorical variables were tested using Pearson's χ2 or Fisher's exact test as appropriate, and presented as numbers of patients with percentages. Ordinal and continuous variables were tested using the linear‐by‐linear or Kruskal–Wallis test, and presented as median (i.q.r.) values.
Disease‐free survival (DFS) was defined as time from first CRS–HIPEC procedure to the date of first recurrence, and patients were censored at date of last follow‐up. OS was defined as time from first CRS–HIPEC to date of death, and patients were censored at date of last follow‐up. DFS and OS curves were constructed using the Kaplan–Meier method and compared with the log rank test.
Univariable and multivariable Cox regression analyses were used to investigate prognostic factors for DFS and OS after primary CRS–HIPEC. Factors with P ≤ 0·100 in univariable models were included in the multivariable Cox regression model. Proportionality assumptions for all Cox models were checked and fulfilled. Two‐sided P < 0·050 was considered statistically significant. Statistical analyses were performed with IBM SPSS® statistics version 22.0 (IBM, Armonk, New York, USA), STATA® version 13 (StataCorp, College Station, Texas, USA) or GraphPad Prism® version 7.03 (GraphPad Software, San Diego, California, USA).
Results
Some 225 patients were included (Fig. 1). Their baseline characteristics are presented in Table 1. Most had undergone previous laparoscopy or laparotomy for PMP. Patients with acellular mucin were more often asymptomatic at time of diagnosis. Serum CEA and CA19‐9 levels, as well as number of affected regions and administration of chemotherapy, differed between the histological groups.
Figure 1.
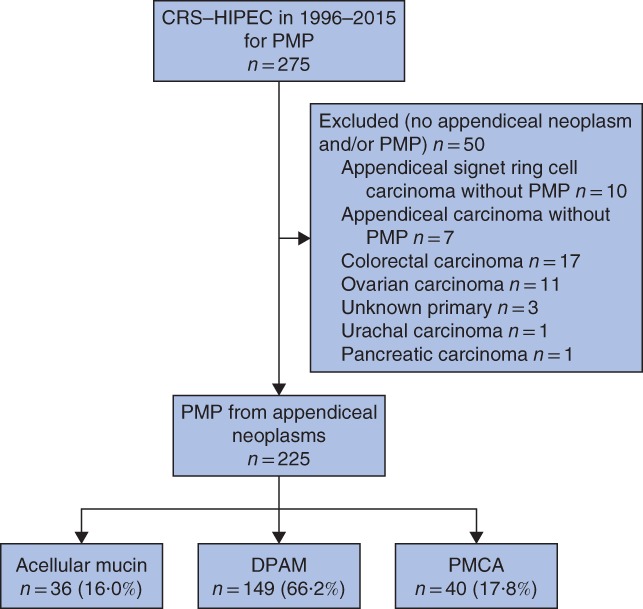
Flow diagram of patient selection. CRS, cytoreductive surgery; HIPEC, hyperthermic intraperitoneal chemotherapy; PMP, pseudomyxoma peritonei; DPAM, disseminated peritoneal adenomucinosis; PMCA, peritoneal mucinous carcinomatosis
Table 1.
Baseline characteristics by histological pseudomyxoma peritonei classification based on first cytoreductive surgery–hyperthermic intraperitoneal chemotherapy procedure
| Acellular mucin (n = 36) | DPAM (n = 149) | PMCA (n = 40) | P ¶ | ||
|---|---|---|---|---|---|
| Age (years)* | 58·1 (48·5–70·1) | 57·2 (47·7–64·7) | 54·5 (46·5–69·2) | 0·504# | |
| Sex ratio (M : F) | 6 : 30 | 51 : 98 | 9 : 31 | 0·067 | |
| ASA fitness grade | I | 19 (53) | 71 (47·7) | 17 (43) | 0·861 |
| II | 14 (39) | 62 (41·6) | 20 (50) | ||
| III | 3 (8) | 16 (10·7) | 3 (8) | ||
| Co‐morbidity | No | 13 (36·1) | 73 (49·0) | 22 (55) | 0·237 |
| Yes | 23 (64) | 76 (51·0) | 18 (45) | ||
| Symptoms at presentation† | Asymptomatic | 10 (28) | 20 (13·4) | 1 (3) | 0·007 |
| Abdominal | 20 (56) | 105 (70·5) | 30 (75) | 0·081 | |
| Weight loss | 1 (3) | 19 (12·8) | 4 (10) | 0·232 | |
| Nausea/vomiting | 1 (3) | 4 (2·7) | 0 (0) | 0·661 | |
| Incidental finding‡ | 10 (28) | 24 (16·1) | 7 (18) | 0·231 | |
| Colonoscopy performed before CRS–HIPEC | No | 26 (72) | 110 (73·8) | 24 (60) | 0·269 |
| Yes, no abnormalities | 9 (25) | 37 (24·8) | 16 (40) | ||
| Yes, suspicious lesions§ | 1 (3) | 2 (1·3) | 0 (0) | ||
| No. of operations before CRS–HIPEC | 0 | 7 (19) | 30 (20·1) | 7 (18) | 0·511 |
| 1 | 25 (69) | 94 (63·1) | 22 (55) | ||
| 2 | 4 (11) | 20 (13·4) | 7 (18) | ||
| 3 | 0 (0) | 4 (2·7) | 4 (10) | ||
| 4 | 0 (0) | 1 (0·7) | 0 (0) | ||
| Previous surgical score | 0 | 1 (3) | 13 (8·7) | 5 (13) | 0·105 |
| 1 | 4 (11) | 13 (8·7) | 3 (8) | ||
| 2 | 18 (50) | 41 (27·5) | 11 (28) | ||
| 3 | 6 (17) | 52 (34·9) | 14 (35) | ||
| No previous surgery | 7 (19) | 30 (20·1) | 7 (18) | ||
| Systemic chemotherapy | None | 35 (97) | 131 (87·9) | 24 (60) | < 0·001 |
| Neoadjuvant | 0 (0) | 1 (0·7) | 2 (5) | ||
| Adjuvant | 1 (3) | 17 (11·4) | 13 (33) | ||
| Perioperative | 0 (0) | 0 (0) | 1 (3) | ||
| Peritoneal disease | Synchronous | 33 (92) | 141 (94·6) | 35 (88) | 0·243 |
| Metachronous | 3 (8) | 8 (5·4) | 5 (13) | ||
| Distant metastases (before CRS–HIPEC) | No | 36 (100) | 148 (99·3) | 40 (100) | 1·000 |
| Yes | 0 (0) | 1 (0·7) | 0 (0) | ||
| Marker level before CRS–HIPEC* | CEA (μg/l) | 2 (1–3) | 12 (3–54) | 19 (3–93) | < 0·001# |
| CA19‐9 (kunits/l) | 10 (6–19) | 27 (9–174) | 66 (7–341) | 0·001# | |
| CA125 (kunits/l) | 12 (7–29) | 41 (14–81) | 37 (21–74) | 0·097# | |
| No. of CRS–HIPEC procedures | 1 | 36 (100) | 115 (77·2) | 35 (88) | 0·007 |
| 2 | 0 (0) | 29 (19·5) | 5 (13) | ||
| 3 | 0 (0) | 5 (3·4) | 0 (0) | ||
| No. of regions involved | 0–2 | 10 (28) | 17 (11·4) | 3 (8) | 0·003 |
| 3–5 | 17 (47) | 43 (28·9) | 13 (33) | ||
| 6–7 | 9 (25) | 86 (57·7) | 23 (58) | ||
| Unknown | 0 (0) | 3 (2·0) | 1 (3) | ||
| Completeness of cytoreduction | R1 | 28 (78) | 93 (62·4) | 27 (68) | 0·208 |
| R2a | 8 (22) | 37 (24·8) | 9 (23) | ||
| R2b | 0 (0) | 17 (11·4) | 4 (10) | ||
| Unknown | 0 (0) | 2 (1·3) | 0 (0) | ||
| Intraperitoneal chemotherapy | Mitomycin C | 35 (97) | 149 (100) | 40 (100) | 0·160 |
| Oxaliplatin | 1 (3) | 0 (0) | 0 (0) | ||
| CTCAE grade | 0 | 19 (53) | 48 (32·2) | 13 (33) | 0·098 |
| 1–2 | 9 (25) | 29 (19·5) | 12 (30) | ||
| 3–4 | 8 (22) | 62 (41·6) | 14 (35) | ||
| 5 | 0 (0) | 9 (6·0) | 1 (3) | ||
| Unknown | 0 (0) | 1 (0·7) | 0 (0) | ||
| In‐hospital mortality | No | 36 (100) | 140 (94·0) | 39 (98) | 0·313 |
| Yes | 0 (0) | 9 (6·0) | 1 (3) |
Values in parentheses are percentages unless indicated otherwise;
values are median (i.q.r.). †Patients could have multiple complaints at time of presentation;
patients could have an appendicitis, be suspected of having ovarian cancer, or have an inguinal or umbilical hernia;
appendiceal volcano sign, granular aspect caecum and T1 adenocarcinoma sigmoid.
DPAM, disseminated peritoneal adenomucinosis; PMCA, peritoneal mucinous carcinomatosis; CRS, cytoreducive surgery; HIPEC, hyperthermic intraperitoneal chemotherapy; CEA, carcinoembryonic antigen; CA, carbohydrate/cancer antigen; CTCAE, Common Terminology Criteria for Adverse Events22.
χ2 or Fisher's exact test, except #Kruskal–Wallis test.
Co‐morbidity related to CRS–HIPEC
Eighty patients (35·6 per cent) did not develop postoperative complications after their first CRS–HIPEC procedure. Ten patients (4·4 per cent) died from complications, five (2·2 per cent) within 30 days. Postoperative complication rates after second and third CRS–HIPEC procedures were comparable (Table S1, supporting information).
Two patients (0·9 per cent) had a stoma before the first CRS–HIPEC procedure, and afterwards 79 patients (35·1 per cent) had an ileostomy or colostomy (Table S1, supporting information). Overall stoma reversal was possible in 16 of 79 patients (20 per cent). After a second CRS–HIPEC procedure in 39 patients, a stoma was created in 19 (49 per cent). Bowel continuity was restored in none of these patients, and four of five patients had a permanent stoma after a third CRS–HIPEC procedure (Table S1, supporting information).
Management of recurrences
Of 36 patients diagnosed with acellular mucin, seven (19 per cent) had locoregional recurrence of disease. One of these patients had undergone R2a resection. In patients with DPAM, systemic recurrences, a combination of locoregional and systemic recurrences, and locoregional recurrences were observed in two (1·3 per cent), five (3·4 per cent) and 81 patients (54·4 per cent) respectively. Of 17 patients diagnosed with DPAM who had an R2b resection, four did not show recurrence of disease during follow‐up. After CRS–HIPEC for PMCA, systemic recurrences, a combination of locoregional and systemic recurrences, and locoregional recurrences were observed in one (3 per cent), five (13 per cent) and 19 patients (48 per cent) respectively. Additional data regarding locations of recurrence are shown in Table S2 (supporting information).
The management of PMP recurrences is shown in Fig. 2. After the first CRS–HIPEC procedure, 105 patients (46·7 per cent) remained disease‐free after a median of 68·8 (i.q.r. 27·1–125·7) months of follow‐up. Recurrences were diagnosed in the remaining 120 patients (53·3 per cent) after a median of 16·3 (8·1–41·1) months. Patients with recurrence had a median OS of 85·2 (38·4–171·6) months. When recurrence developed after the first CRS–HIPEC procedure, 39 patients (32·5 per cent) underwent a second course of CRS–HIPEC (Fig. 2). Thirty (77 per cent) of these 39 patients developed further recurrences at a median survival of 59·4 (32·1–124·5) months. For the nine patients with no recurrence after a second CRS–HIPEC procedure, median survival was not reached. Five patients (17 per cent) treated with a third CRS–HIPEC procedure had a median OS of 23·5 (21·5 to infinity) months. The other treatment options for recurrences and extrasurgical treatments are shown in Fig. 2.
Figure 2.
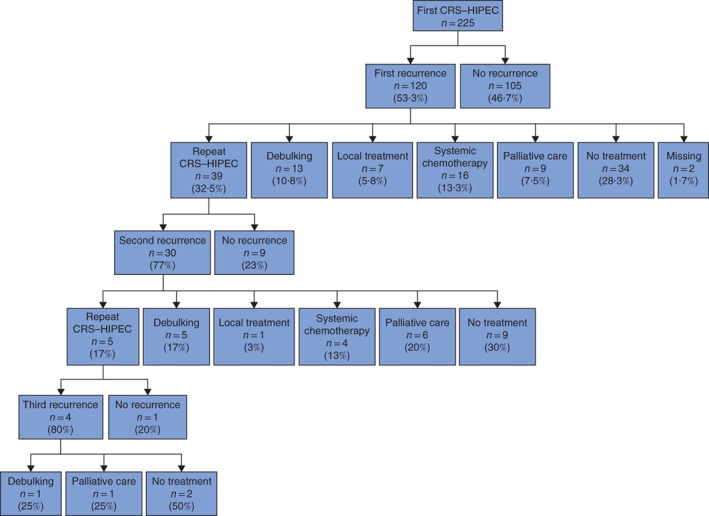
Management of peritoneal recurrence in patients with pseudomyxoma peritonei. No treatment was given in 34 patients (28·3 per cent) after first recurrence: watchful waiting (21 patients), poor physical condition (due to postoperative complications) (5), no available treatment options (5) or other reason (3)
Survival
Median follow‐up after the first CRS–HIPEC procedure was 68·1 (i.q.r. 32·7–124·2) months. Median DFS until first recurrence was significantly longer in patients with acellular mucin (median DFS not reached) compared with that in patients with DPAM (41·9 (10·6–207·9) months) or PMCA (28·1 (11·1 to infinity) months (Fig. 3 a). Factors associated with poor DFS in multivariable analysis were six or seven affected regions (hazard ratio (HR) 6·01, 95 per cent c.i. 2·04 to 17·73), incomplete cytoreduction (R2a resection: HR 1·67, 1·05 to 2·65; R2b resection: HR 2·00, 1·07 to 3·73), and more than threefold increased CEA and/or CA19‐9 level (HR 2·31, 1·30 to 4·11) (Table 2).
Figure 3.
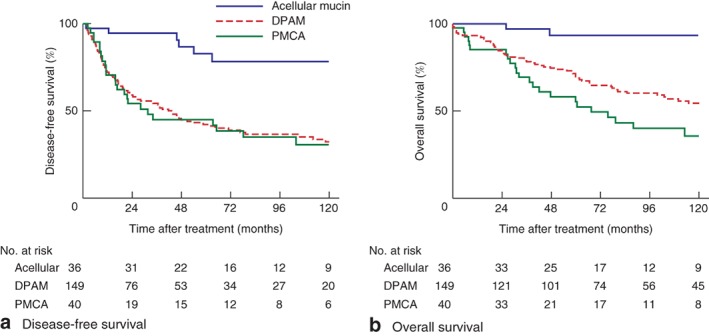
Kaplan–Meier analysis of survival in 225 patients with pseudomyxoma peritonei by histological classification. DPAM, disseminated peritoneal adenomucinosis; PMCA, peritoneal mucinous carcinomatosis. a,b P < 0·001 (log rank test)
Table 2.
Univariable and multivariable Cox regression analysis of disease‐free survival in all patients
| Univariable DFS | Multivariable DFS | |||||
|---|---|---|---|---|---|---|
| DFS (months)* | Hazard ratio | P | Hazard ratio | P | ||
| Age | 0·99 (0·97, 1·00) | 0·062 | ||||
| Sex | M | 26·0 (8·3–112·4) | 1·85 (1·26, 2·73) | 0·002 | 1·49 (0·94, 2·34) | 0·088 |
| F | 78·3 (17·2–207·9) | 1·00 (reference) | 1·00 (reference) | |||
| ASA grade | 0·783 | |||||
| I | 58·9 (15·6–207·9) | 1·00 (reference) | ||||
| II | 46·7 (11·1–∞) | 1·14 (0·78, 1·67) | 0·492 | |||
| III | 51·0 (14·3–∞) | 1·11 (0·59, 2·06) | 0·751 | |||
| Abdominal symptoms | No | 71·2 (16·6–170·3) | 1·00 (reference) | |||
| Yes | 54·1 (11·0–207·9) | 1·11 (0·74, 1·68) | 0·608 | |||
| Weight loss ± loss of appetite | No | 64·7 (14·3–∞) | 1·00 (reference) | 1·00 (reference) | ||
| Yes | 36·8 (5·3–207·9) | 1·62 (1·02, 2·59) | 0·043 | 0·76 (0·44, 1·30) | 0·309 | |
| Nausea or vomiting | No | 61·3 (12·2–207·9) | 1·00 (reference) | |||
| Yes | 26·0 (11·0–∞) | 1·10 (0·35, 3·47) | 0·870 | |||
| Incidental finding | 0·838 | |||||
| None | 63·0 (11·7–207·9) | 1·00 (reference) | ||||
| Hernia inguinalis/umbilicalis | n.a. (11·3–∞) | 0·70 (0·28, 1·75) | 0·445 | |||
| Ovarian mass | 37·1 (11·3–46·9) | 1·22 (0·53, 2·79) | 0·640 | |||
| Appendicitis | 45·7 (28·1–136·9) | 1·01 (0·53, 1·95) | 0·968 | |||
| Timing of CRS–HIPEC | 1996–2005 | 43·3 (11·3–207·9) | 1·41 (0·97, 2·05) | 0·069 | 0·88 (0·58, 1·33) | 0·537 |
| 2006–2015 | n.a. (15·9–∞) | 1·00 (reference) | 1·00 (reference) | |||
| No. of regions involved | < 0·001 | 0·001 | ||||
| 0–2 | n.a. | 1·00 (reference) | 1·00 (reference) | |||
| 3–5 | 136·9 (43·4–∞) | 3·62 (1·27, 10·33) | 0·016 | 2·82 (0·96, 8·26) | 0·060 | |
| 6–7 | 18·2 (8·3–61·3) | 11·12 (4·07, 30·43) | < 0·001 | 6·01 (2·04, 17·73) | 0·001 | |
| Completeness of cytoreduction | < 0·001 | 0·025 | ||||
| R1 | 104·1 (24·0–207·9) | 1·00 (reference) | 1·00 (reference) | |||
| R2a | 28·1 (9·3–∞) | 1·77 (1·16, 2·70) | 0·008 | 1·67 (1·05, 2·65) | 0·030 | |
| R2b | 8·9 (2·3–17·2) | 4·44 (2·59, 7·60) | < 0·001 | 2·00 (1·07, 3·73) | 0·029 | |
| CTCAE grade | 0·017 | 0·856 | ||||
| 0 | 104·9 (22·0–∞) | 1·00 (reference) | 1·00 (reference) | |||
| 1–2 | 65·3 (17·2–∞) | 1·05 (0·63, 1·76) | 0·840 | 0·77 (0·43, 1·39) | 0·385 | |
| 3–4 | 28·2 (9·0–120·8) | 1·84 (1·22, 2·78) | 0·004 | 0·89 (0·51, 1·54) | 0·674 | |
| 5 | n.a. | n.a. | n.a. | n.a. | n.a. | |
| Histological classification of PMP | 0·001 | 0·184 | ||||
| Acellular mucin | n.a. (136·9–∞) | 1·00 (reference) | 1·00 (reference) | |||
| DPAM | 41·9 (10·6–207·9) | 4·47 (2·07, 9·66) | < 0·001 | 2·21 (0·95, 5·13) | 0·066 | |
| PMCA | 28·1 (11·1–∞) | 4·65 (2·01, 10·77) | < 0·001 | 2·06 (0·79, 5·34) | 0·139 | |
| Peritoneal disease | Synchronous | 61·3 (14·3–207·9) | 1·00 (reference) | 1·00 (reference) | ||
| Metachronous | 16·0 (9·3–63·4) | 1·83 (1·05, 3·20) | 0·034 | 2·02 (0·95, 4·31) | 0·068 | |
| No. of raised tumour markers (before first CRS–HIPEC)† | < 0·001 | 0·005 | ||||
| 0 | 170·3 (48·3–∞) | 1·00 (reference) | 1·00 (reference) | |||
| 1–2 raised threefold or less | 64·7 (45·7–∞) | 1·54 (0·83, 2·86) | 0·167 | 1·09 (0·54, 2·19) | 0·815 | |
| 1–2 raised more than threefold | 16·7 (7·4–61·3) | 4·31 (2·78, 6·68) | < 0·001 | 2·31 (1·30, 4·11) | 0·004 | |
| Systemic chemotherapy | No | 65·3 (15·9–207·9) | 1·00 (reference) | 1·00 (reference) | ||
| Yes | 20·2 (8·3–120·8) | 1·66 (1·07, 2·56) | 0·024 | 1·38 (0·78, 2·43) | 0·269 | |
Values in parentheses are 95 per cent c.i. unless indicated otherwise;
values are median (i.q.r.).
Tumour markers: carcinoembryonic antigen and carbohydrate antigen 19‐9. DFS, disease‐free survival; n.a., not applicable (median survival not reached); CRS, cytoreductive surgery; HIPEC, hyperthermic intraperitoneal chemotherapy; CTCAE, Common Terminology Criteria for Adverse Events22; PMP, pseudomyxoma peritonei; DPAM, disseminated peritoneal adenomucinosis; PMCA, peritoneal mucinous carcinomatosis.
Median OS was not reached in patients with acellular mucin, whereas median OS for patients with DPAM was 130·8 (i.q.r. 47·7–201·6) months and that in patients with PMCA was 67·6 (30·7 to infinity) months (Fig. 3 b). OS rates after 3, 5 and 10 years were 97, 93 and 93 per cent for acellular mucin, 78·1, 69·8 and 54·5 per cent for DPAM, and 69, 55 and 36 for PMCA. Two patients were lost to follow‐up after 5 years. Factors associated with worse OS were male sex (HR 1·74, 95 per cent c.i. 1·09 to 2·77), incomplete cytoreduction (R2a resection: HR 1·87, 1·14 to 3·08; R2b resection: HR 2·28, 1·19 to 4·34), and greater than threefold raised CEA and/or CA19‐9 level (HR 2·89, 1·36 to 6·16) (Table 3).
Table 3.
Unvariable and multivariable Cox regression analysis of overall survival in all patients
| Univariable OS | Multivariable OS | |||||
|---|---|---|---|---|---|---|
| OS (months)* | Hazard ratio | P | Hazard ratio | P | ||
| Age | 1·01 (0·99, 1·03) | 0·238 | ||||
| Sex | M | 78·9 (25·3–171·6) | 2·15 (1·43, 3·24) | < 0·001 | 1·74 (1·09, 2·77) | 0·020 |
| F | 161·4 (63·0–217·5) | 1·00 (reference) | 1·00 (reference) | |||
| ASA grade | 0·002 | 0·077 | ||||
| I | 201·6 (77·4–∞) | 1·00 (reference) | 1·00 (reference) | |||
| II | 79·6 (31·4–200·5) | 2·19 (1·42, 3·37) | < 0·001 | 1·54 (0·91, 2·49) | 0·113 | |
| III | 124·8 (35·8–191·9) | 1·72 (0·89, 3·32) | 0·106 | 0·75 (0·35, 1·59) | 0·450 | |
| Abdominal symptoms | No | 160·6 (85·2–217·5) | 1·00 (reference) | 1·00 (reference) | ||
| Yes | 124·8 (36·1–∞) | 1·72 (1·04, 2·86) | 0·035 | 1·00 (0·56, 1·80) | 0·999 | |
| Weight loss ± loss of appetite | No | 160·6 (58·2–217·5) | 1·00 (reference) | 1·00 (reference) | ||
| Yes | 78·9 (27·8–171·6) | 1·83 (1·14, 2·94) | 0·012 | 1·18 (0·69, 2·02) | 0·555 | |
| Nausea or vomiting | No | 132·2 (47·7–217·5) | 1·00 (reference) | |||
| Yes | n.a. (47·7–∞) | 0·96 (0·24, 3·91) | 0·958 | |||
| Incidental finding | 0·757 | |||||
| None | 137·1 (42·1–217·5) | 1·00 (reference) | ||||
| Hernia inguinalis/umbilicalis | 160·6 (85·2–∞) | 0·66 (0·24, 1·82) | 0·425 | |||
| Ovarian mass | 61·9 (50·8–∞) | 1·29 (0·52, 3·20) | 0·588 | |||
| Appendicitis | 121·6 (78·9–∞) | 0·83 (0·38, 1·81) | 0·646 | |||
| Timing of CRS–HIPEC | 0·142 | 0·941 | ||||
| 1996–2005 | 127·3 (37·5–217·5) | 1·40 (0·89, 2·21) | 0·98 (0·60, 1·61) | |||
| 2006–2015 | n.a. (61·6–∞) | 1·00 (reference) | 1·00 (reference) | |||
| No. of regions involved | < 0·001 | 0·136 | ||||
| 0–2 | n.a. | 1·00 (reference) | 1·00 (reference) | |||
| 3–5 | 200·5 (88·2–200·5) | 5·21 (1·22, 22·30) | 0·026 | 2·93 (0·66, 13·08) | 0·158 | |
| 6–7 | 78·9 (30·7–191·9) | 12·93 (3·17, 52·76) | < 0·001 | 4·05 (0·93, 17·71) | 0·063 | |
| Completeness of cytoreduction | < 0·001 | 0·010 | ||||
| R1 | 201·6 (75·9–∞) | 1·00 (reference) | 1·00 (reference) | |||
| R2a | 103·2 (34·9–191·9) | 2·03 (1·28, 3·22) | 0·003 | 1·87 (1·14, 3·08) | 0·014 | |
| R2b | 31·1 (15·9–67·6) | 5·10 (2·94, 8·87) | < 0·001 | 2·28 (1·19, 4·34) | 0·012 | |
| CTCAE grade | 1·000 | |||||
| 0 | n.a. (121·6–∞) | 1·00 (reference) | ||||
| 1–2 | 160·6 (60·6–∞) | 1·00 (0·59, 1·71) | 1·000 | |||
| 3–4 | 110·2 (39·2–201·6) | 1·00 (0·64, 1·57) | 1·000 | |||
| 5 | 0·7 (0·3–1·4) | 1·00 (0·02, 47·33) | 1·000 | |||
| Histological classification of PMP | 0·002 | 0·095 | ||||
| Acellular mucin | n.a. | 1·00 (reference) | 1·00 (reference) | |||
| DPAM | 130·8 (47·7–201·6) | 8·81 (2·16, 35·91) | 0·002 | 3·04 (0·70, 13·30) | 0·139 | |
| PMCA | 67·6 (30·7–∞) | 12·68 (2·99, 53·83) | 0·001 | 4·61 (0·99, 21·59) | 0·052 | |
| Peritoneal disease | Synchronous | 137·1 (50·8–217·5) | 1·00 (reference) | |||
| Metachronous | 138·1 (42·1–171·6) | 1·09 (0·56, 2·10) | 0·799 | |||
| No. of raised tumour markers (before first CRS–HIPEC)† | < 0·001 | 0·009 | ||||
| 0 | 201·6 (200·5–∞) | 1·00 (reference) | 1·00 (reference) | |||
| 1–2 raised threefold or less | n.a. (121·6–∞) | 1·31 (0·58, 2·96) | 0·523 | 1·33 (0·54, 3·30) | 0·540 | |
| 1–2 raised more than threefold | 61·9 (24·3–138·1) | 4·91 (2·85, 8·43) | < 0·001 | 2·89 (1·36, 6·16) | 0·006 | |
| Systemic chemotherapy | No | 160·6 (58·2–217·5) | 1·00 (reference) | |||
| Yes | 115·3 (38·4–∞) | 1·30 (0·80, 2·11) | 0·289 | |||
Values in parentheses are 95 per cent c.i. unless indicated otherwise;
values are median (i.q.r.).
Tumour markers: carcinoembryonic antigen and carbohydrate antigen 19‐9. OS, overall survival; n.a., not applicable (median survival not reached); CRS, cytoreductive surgery; HIPEC, hyperthermic intraperitoneal chemotherapy; CTCAE, Common Terminology Criteria for Adverse Events22; PMP, pseudomyxoma peritonei; DPAM, disseminated peritoneal adenomucinosis; PMCA, peritoneal mucinous carcinomatosis.
Serum tumour markers
CEA level before CRS–HIPEC was increased in four (11 per cent), 98 (65·8 per cent) and 25 patients (63 per cent) with acellular mucin, DPAM and PMCA respectively. CA19·9 level was raised in no patient, 66 (44·3 per cent) and 21 patients (53 per cent) with acellular mucin, DPAM and PMCA respectively.
Of patients with DPAM and PMCA, DFS was significantly shorter in those with one or two markers raised more than threefold (median 16·7 (i.q.r. 7·4–61·3) months) compared with that in patients with markers raised threefold or less (64·7 (45·7 to infinity) months) or those with no increased tumour markers (170·3 (48·3 to infinity) months) (Fig. 4 a).
Figure 4.
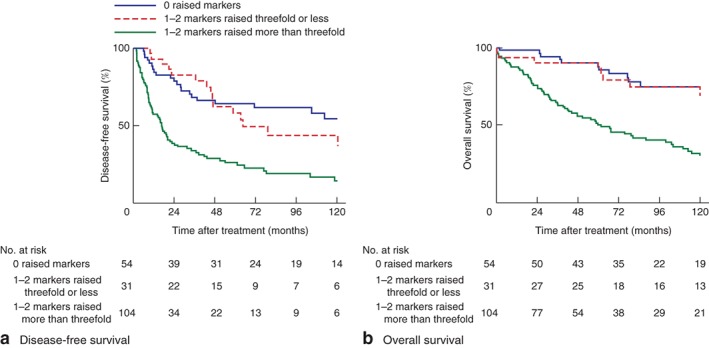
Kaplan–Meier analysis of survival in relation to levels of tumour markers in 189 patients with disseminated peritoneal adenomucinosis or peritoneal mucinous carcinomatosis. a Disease‐free and b overall survival. Tumour markers: carcinoembryonic antigen or carbohydrate antigen 19‐9. a,b P < 0·001 (log rank test)
OS was shorter in patients with DPAM and PMCA with one or two tumour markers raised more than threefold (median 61·9 (24·1–138·1) months) than in patients with one or two tumour markers increased by threefold or less (median OS not reached) or those with no increased markers (201·6 (200·5 to infinity) months) (Fig. 4 b).
Timing of CRS–HIPEC
Significant differences were observed between patients who were operated on between 1996 and 2005 and those who had the procedure between 2006 and 2015. In the later cohort, patients were less often treated with systemic chemotherapy, fewer postoperative complications were observed, and ICU and hospital stay were significantly shorter (Table S3, supporting information). Acellular mucin was more often diagnosed and fewer patients had recurrence of disease in the later period. The 5‐year OS rate was 66·0 per cent in the 1996–2005 cohort and 76·2 per cent in the 2006–2015 cohort.
Discussion
Patients with the acellular mucin histological subtype of PMP have an excellent prognosis after CRS–HIPEC. Serum levels of CA19‐9 and CEA were independent prognostic factors, together with sex, number of affected regions and completeness of cytoreduction. CRS–HIPEC procedures were safe in these selected patients. Almost half of the patients with PMP remained disease‐free after treatment with CRS–HIPEC.
The prevalence of histological subtypes for PMP is comparable with that in the literature16, 17, 23. Acellular mucin is associated with the best prognosis, with a 5‐year survival rate of 93 per cent, compared with 69·8 per cent for DPAM and 55 per cent for PMCA. Similar survival rates have been described elsewhere17, 24. Several other studies11, 25, 26, 27 focused on repeat CRS–HIPEC procedures and concluded that this was feasible, with a large group of patients remaining disease‐free afterwards. Recurrence rates after first CRS–HIPEC in the present series were slightly higher than those in other studies, with reported recurrence rates tending to be below 50 per cent3, 11, 28.
Predictors of poorer survival identified in this study have been described previously28, 29, 30, 31. Male sex is a poor prognostic factor for survival, although the difference between the sexes remains unexplained5, 29, 30, 31. Raised levels of tumour markers have been associated with poorer survival in other studies1, 32, 33. In the present study, increased marker levels were associated with worse prognosis, in particular when CEA was above 20 μg/l and/or CA19‐9 was more than 100 kunits/l. Compared with histological subtype, serum tumour markers are easily determined and might therefore be used to guide the timing of CRS–HIPEC, counsel patients and tailor follow‐up. Levels of these tumour markers were increased only sporadically in patients with acellular mucin, possibly reflecting the absence of tumour cells in the mucinous peritoneal deposits. In DPAM and PMCA, tumour marker levels raised more than threefold were stronger predictors of worse prognosis than histological subtype. A substantial number of patients with PMCA were treated with adjuvant systemic chemotherapy on the basis that in the majority of patients the condition arises from mucinous appendiceal adenocarcinomas, with risk of systemic recurrence.
Bias is inherently present in this study owing to its observational nature, the inclusion of patients who underwent CRS–HIPEC and the long study interval. Time plays an important role, as surgical teams and protocols have changed over the years, with improvements in surgical technique and perioperative care. Definitions and awareness of PMP have also changed during this interval, and pathologists have gained greater experience in recognizing this rare disease with its histopathological subtypes. This could also explain the increase of patients diagnosed with acellular mucin over time.
No RCTs have been performed because PMP is a rare disease, although this might be overcome by greater international collaborative efforts. Until then, observational data remain useful in highlighting management difficulties and pointing the way to worthwhile prospective studies.
Supporting information
Table S1 Treatment characteristics and related morbidity by first, second and third CRS–HIPEC procedures
Table S2 Recurrences, tumour marker levels and imaging abnormalities after first, second and third CRS–HIPEC procedures
Table S3 CRS–HIPEC by time period (first procedure)
Acknowledgements
The authors acknowledge the Core Facility – Molecular Pathology and Biobank of the Netherlands Cancer Institute for supplying Biobank material.
Disclosure: The authors declare no conflict of interest.
Funding information
No funding
References
- 1. Baratti D, Kusamura S, Martinetti A, Seregni E, Laterza B, Oliva DG et al Prognostic value of circulating tumor markers in patients with pseudomyxoma peritonei treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol 2007; 14: 2300–2308. [DOI] [PubMed] [Google Scholar]
- 2. Sugarbaker PH. Cytoreductive surgery and perioperative intraperitoneal chemotherapy: a new standard of care for appendiceal mucinous tumors with peritoneal dissemination. Clin Colon Rectal Surg 2005; 18: 204–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lord AC, Shihab O, Chandrakumaran K, Mohamed F, Cecil TD, Moran BJ. Recurrence and outcome after complete tumour removal and hyperthermic intraperitoneal chemotherapy in 512 patients with pseudomyxoma peritonei from perforated appendiceal mucinous tumours. Eur J Surg Oncol 2015; 41: 396–399. [DOI] [PubMed] [Google Scholar]
- 4. Moran B, Baratti D, Yan TD, Kusamura S, Deraco M. Consensus statement on the loco‐regional treatment of appendiceal mucinous neoplasms with peritoneal dissemination (pseudomyxoma peritonei). J Surg Oncol 2008; 98: 277–282. [DOI] [PubMed] [Google Scholar]
- 5. Chua TC, Moran BJ, Sugarbaker PH, Levine EA, Glehen O, Gilly FN et al Early‐ and long‐term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol 2012; 30: 2449–2456. [DOI] [PubMed] [Google Scholar]
- 6. Mukherjee A, Parvaiz A, Cecil TD, Moran BJ. Pseudomyxoma peritonei usually originates from the appendix: a review of the evidence. Eur J Gynaecol Oncol 2004; 25: 411–414. [PubMed] [Google Scholar]
- 7. Jimenez W, Sardi A, Nieroda C, Sittig M, Milovanov V, Nunez M et al Predictive and prognostic survival factors in peritoneal carcinomatosis from appendiceal cancer after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol 2014; 21: 4218–4225. [DOI] [PubMed] [Google Scholar]
- 8. Stearns AT, Malcomson L, Punnett G, Abudeeb H, Aziz O, Selvasekar CR et al Long‐term quality of life after cytoreductive surgery and heated intraperitoneal chemotherapy for pseudomyxoma peritonei: a prospective longitudinal study. Ann Surg Oncol 2018; 25: 965–973. [DOI] [PubMed] [Google Scholar]
- 9. Kirby R, Liauw W, Zhao J, Morris D. Quality of life study following cytoreductive surgery and intraperitoneal chemotherapy for pseudomyxoma peritonei including redo procedures. Int J Surg Oncol 2013; 2013: 461041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buell‐Gutbrod R, Gwin K. Pathologic diagnosis, origin, and natural history of pseudomyxoma peritonei. Am Soc Clin Oncol Educ Book 2013: 221–225. [DOI] [PubMed] [Google Scholar]
- 11. Chua TC, Al‐Zahrani A, Saxena A, Liauw W, Zhao J, Morris DL. Secondary cytoreduction and perioperative intraperitoneal chemotherapy after initial debulking of pseudomyxoma peritonei: a study of timing and the impact of malignant dedifferentiation. J Am Coll Surg 2010; 211: 526–535. [DOI] [PubMed] [Google Scholar]
- 12. Carmignani CP, Hampton R, Sugarbaker CE, Chang D, Sugarbaker PH. Utility of CEA and CA 19‐9 tumor markers in diagnosis and prognostic assessment of mucinous epithelial cancers of the appendix. J Surg Oncol 2004; 87: 162–166. [DOI] [PubMed] [Google Scholar]
- 13. Kozman MA, Fisher OM, Rebolledo BJ, Valle SJ, Alzahrani N, Liauw W et al CA 19‐9 to peritoneal carcinomatosis index (PCI) ratio is prognostic in patients with epithelial appendiceal mucinous neoplasms and peritoneal dissemination undergoing cytoreduction surgery and intraperitoneal chemotherapy: a retrospective cohort study. Eur J Surg Oncol 2017; 43: 2299–2307. [DOI] [PubMed] [Google Scholar]
- 14. Elias D, Honoré C, Ciuchendéa R, Billard V, Raynard B, Lo Dico R et al Peritoneal pseudomyxoma: results of a systematic policy of complete cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Br J Surg 2008; 95: 1164–1171. [DOI] [PubMed] [Google Scholar]
- 15. Canbay E, Ishibashi H, Sako S, Mizumoto A, Hirano M, Ichinose M et al Preoperative carcinoembryonic antigen level predicts prognosis in patients with pseudomyxoma peritonei treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. World J Surg 2013; 37: 1271–1276. [DOI] [PubMed] [Google Scholar]
- 16. Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González‐Moreno S et al; Peritoneal Surface Oncology Group International . A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) modified Delphi process. Am J Surg Pathol 2016; 40: 14–26. [DOI] [PubMed] [Google Scholar]
- 17. Huang Y, Alzahrani NA, Chua TC, Morris DL. Histological subtype remains a significant prognostic factor for survival outcomes in patients with appendiceal mucinous neoplasm with peritoneal dissemination. Dis Colon Rectum 2017; 60: 360–367. [DOI] [PubMed] [Google Scholar]
- 18. Ronnett BM, Shmookler BM, Sugarbaker PH, Kurman RJ. Pseudomyxoma peritonei: new concepts in diagnosis, origin, nomenclature, and relationship to mucinous borderline (low malignant potential) tumors of the ovary. Anat Pathol 1997; 2: 197–226. [PubMed] [Google Scholar]
- 19. Ronnett BM, Zahn CM, Kurman RJ, Kass ME, Sugarbaker PH, Shmookler BM. Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. A clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to ‘pseudomyxoma peritonei’. Am J Surg Pathol 1995; 19: 1390–1408. [DOI] [PubMed] [Google Scholar]
- 20. Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H et al Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 2003; 21: 3737–3743. [DOI] [PubMed] [Google Scholar]
- 21. Swellengrebel HA, Zoetmulder FA, Smeenk RM, Antonini N, Verwaal VJ. Quantitative intra‐operative assessment of peritoneal carcinomatosis – a comparison of three prognostic tools. Eur J Surg Oncol 2009; 35: 1078–1084. [DOI] [PubMed] [Google Scholar]
- 22. US Department of Health and Human Services , National Institutes of Health and National Cancer Institute. Common Termininology Criteria for Adverse Events (CTCAE) v4.03; 2010. https://www.eortc.be/services/doc/ctc/CTCAE_4.03_2010‐06‐14_QuickReference_5x7.pdf [accessed 11 January 2018].
- 23. Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. Survival analysis of pseudomyxoma peritonei patients treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg 2007; 245: 104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Baratti D, Kusamura S, Milione M, Bruno F, Guaglio M, Deraco M. Validation of the recent PSOGI pathological classification of pseudomyxoma peritonei in a single‐center series of 265 patients treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol 2018; 25: 404–413. [DOI] [PubMed] [Google Scholar]
- 25. Golse N, Bakrin N, Passot G, Mohamed F, Vaudoyer D, Gilly FN et al Iterative procedures combining cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for peritoneal recurrence: postoperative and long‐term results. J Surg Oncol 2012; 106: 197–203. [DOI] [PubMed] [Google Scholar]
- 26. Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. Progression of pseudomyxoma peritonei after combined modality treatment: management and outcome. Ann Surg Oncol 2007; 14: 493–499. [DOI] [PubMed] [Google Scholar]
- 27. Klaver YL, Chua TC, Verwaal VJ, de Hingh IH, Morris DL. Secondary cytoreductive surgery and peri‐operative intraperitoneal chemotherapy for peritoneal recurrence of colorectal and appendiceal peritoneal carcinomatosis following prior primary cytoreduction. J Surg Oncol 2013; 107: 585–590. [DOI] [PubMed] [Google Scholar]
- 28. Alexander‐Sefre F, Chandrakumaran K, Banerjee S, Sexton R, Thomas JM, Moran B. Elevated tumour markers prior to complete tumour removal in patients with pseudomyxoma peritonei predict early recurrence. Colorectal Dis 2005; 7: 382–386. [DOI] [PubMed] [Google Scholar]
- 29. Chua TC, Liauw W, Morris DL. Early recurrence of pseudomyxoma peritonei following treatment failure of cytoreductive surgery and perioperative intraperitoneal chemotherapy is indicative of a poor survival outcome. Int J Colorectal Dis 2012; 27: 381–389. [DOI] [PubMed] [Google Scholar]
- 30. Elias D, Gilly F, Quenet F, Bereder JM, Sidéris L, Mansvelt B et al; Association Française de Chirurgie . Pseudomyxoma peritonei: a French multicentric study of 301 patients treated with cytoreductive surgery and intraperitoneal chemotherapy. Eur J Surg Oncol 2010; 36: 456–462. [DOI] [PubMed] [Google Scholar]
- 31. Ansari N, Chandrakumaran K, Dayal S, Mohamed F, Cecil TD, Moran BJ. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in 1000 patients with perforated appendiceal epithelial tumours. Eur J Surg Oncol 2016; 42: 1035–1041. [DOI] [PubMed] [Google Scholar]
- 32. Koh JL, Liauw W, Chua T, Morris DL. Carbohydrate antigen 19‐9 (CA 19‐9) is an independent prognostic indicator in pseudomyxoma peritonei post cytoreductive surgery and perioperative intraperitoneal chemotherapy. J Gastrointest Oncol 2013; 4: 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Taflampas P, Dayal S, Chandrakumaran K, Mohamed F, Cecil TD, Moran BJ. Pre‐operative tumour marker status predicts recurrence and survival after complete cytoreduction and hyperthermic intraperitoneal chemotherapy for appendiceal pseudomyxoma peritonei: analysis of 519 patients. Eur J Surg Oncol 2014; 40: 515–520. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Treatment characteristics and related morbidity by first, second and third CRS–HIPEC procedures
Table S2 Recurrences, tumour marker levels and imaging abnormalities after first, second and third CRS–HIPEC procedures
Table S3 CRS–HIPEC by time period (first procedure)


