Highlights
-
•
The main advantage of minimally invasive techniques for the treatment of retrocaval ureter is less blood loss during surgery.
-
•
Other advantages are shorter hospital stay, less postoperative pain and superior esthetic results.
-
•
Pure laparoscopic treatment (as in our two cases) seems feasible and technically reliable with excellent functional outcome.
-
•
Intracorporeal anastomosis of the ureter remains the main limiting factor.
Keywords: Retrocaval ureter, Laparoscopic surgery, Literature review, Case series
Abstract
Objectives
To expose the diagnosis and the different laparoscopic approaches for the surgical management of patients with retrocaval ureter (RCU) and to share our experience on two cases.
Methods
Updated literature review on Pubmed and debating personal experiences including ours (double j stent insertion before the surgery, use of 4 trocards, transperitoneal approach, pyelopyelostomy for the anastomosis…), concerning the laparoscopic treatment of the RCU.
Results
Laparoscopic treatment of RCU is a recommended management for many reasons: less blood loss during the surgery, a shorter hospital stay, less postoperative pain and superior esthetic results with excellent functional results. All of these findings were also a part of our experience on the two reported cases: operative time was 210 and 180 min with no significant bleeding, hospital stay was 48 h post operatively for both patients that were symptom free with no renal dilation after 2 years of close follow up. The main cause of the increased operating time is the intracorporeal anastomosis of the ureter which remains the main limiting factor of the laparoscopic surgery.
Conclusions
The literature review has clearly shown the advantages of minimally invasive techniques for the treatment of retrocaval ureter. Pure laparoscopic treatment (as in our two cases), seems feasible and technically reliable, and should be the standard surgical option for the treatment of RCU.
1. Introduction
Variations in the anatomy of the vena cava or its tributaries can be encountered and if unrecognized can lead to life-threatening complications [1]. Retrocaval ureter (RCU), or circumcaval ureter, is a rare congenital disease which can cause obstruction and related symptoms. The first recorded case was seen on autopsy and described by Hochstetter in 1893 [2]. Since then, many surgical techniques were used to deal with this anatomical abnormality. Nowadays, mini invasive surgery is used for the correction of retrocaval ureter and the outcome has been excellent in all the described cases that we found in the literature till 2018 (Table 1).
Table 1.
Summary of all reported cases of retrocaval ureter managed by mini invasive approach (PU = pyeloureteral, UU = ureteroureteral; NA = not available; PP = pyeloplasty, Lap = laparoscopic).
| Year | Study | Number of cases | Approach | Anastomosis | Complications | Operative Time (min) | Follow-up (month) |
|---|---|---|---|---|---|---|---|
| 1994 | Baba et al. [36] | 1 | Laparoscopic transperitoneal | PU | No | 560 | 2 |
| 1996 | Matsuda et al. [38] | 1 | Laparoscopic transperitoneal | UU | No | 450 | Not reported |
| 1997 | Ishitoya et al. [16] | 1 | Laparoscopic transperitoneal | UU mini laparotomy | No | 365 | 2 |
| 1998 | Polascik et al. [44] | 1 | Laparoscopic transperitoneal | UU | No | 225 | 4 |
| 1999 | Salomon et al. [29] | 1 | Retroperitoneo-scopic | UU | No | 270 | 6 |
| 1999 | Mugiya et al. [39] | 1 | Retroperitoneoscopic | Automatic suture device | Not reported | 300 | Not reported |
| 2001 | Ameda et al. [34] | 1 | Transteritoneal | UU | No | 450 | 3 |
| 1 | Retroperitoneal | UU | No | 400 | 3 | ||
| 2001 | Gupta et al. [32] | 1 | Retroperitoneal | UU | No | 210 | 3 |
| 2003 | Ramalingam et al. [37] | 1 | Transperitoneal | UU | No | 240 | 7 |
| 1 | Transperitoneal | UU | Ileus | 210 | 6 | ||
| 2003 | Bhandarkar et al. [35] | 1 | Lap Transperitoneal | PP | NA | 250 | 14 |
| 2005 | Tobias-Machado et al. [41] | 1 | Lap Retroperitoneal | UU(extracorporeal) | No | 130 | 3 |
| 2006 | Simforoosh et al. [28] | 3 | Lap Transperitoneal | PP | No | 180 (150–210) | 3 |
| 3 | |||||||
| 2006 | Nagraj et al. [45] | 1 | Lap Transperitoneal | UU | No | 100 | Not reported |
| 2006 | Guntedi et al. [43] | 1 | Robotic Transperitoneal | UU | No | 180 | 6 |
| 2008 | Chung and Gill [46] | 1 | Lap Transperitoneal | PP | No | 180 | 6 |
| 2008 | Hemal et al. [42] | 1 | Robotic transperitoneal | PU | No | Not reported | 3 |
| 2009 | Bagheri et al. [58] | 3 | Lap Transperitoneal | UU | No | 210 (mean) | 12 |
| 2009 | Xu et al. [47] | 7 | Retroperitoneoscopic | UU | No | 128.6 (97–189) | 12 |
| 2010 | Autorino et al. [48] | 1 | Trasperitoneal LESS | UU | No | 180 | 3 |
| 2012 | Nayak et al. [49] | 5 | Robotic transperitoneal | UU and PU | No | 92 (mean) | 13.5 (mean) |
| 2012 | Alkhudair et al. [50] | 1 | Robotic transperitoneal | UU | No | 90 | 3 |
| 2012 | Ding et al. [51] | 6 | Lap Transpertitonal | UU | No | 163 (145–178) | 3–30 |
| 2013 | Junior et al. [52] | 1 | Lap Transperitoneal | PU | No | 210 | 6 |
| 2014 | Ji et al. [53] | 18 | 8 Lap Trans | UU | No | Trans:85 ± 20 | 40 ± 24 |
| 10 Lap Retro | Retro :98 ± 30 | ||||||
| 2015 | Ricciardulli et al. [54] | 27 | Lap Transperitoneal | UU | 4 cases | 131 (mean) | 3, 6 and 12 |
| 2016 | El Harrech et al. [55] | 3 | Lap Transperitoneal | PP | No | 140 (110–190) | Every 3 |
| 2016 | Fidalgo et al. [56] | 1 | Lap Transperitoneal | PU | No | 170 | 3 |
| 2017 | Lijun Mao et al. [57] | 6 | Lap Retroperitoneal | PU | No | 112 (median) | 6–24 |
In this article, which has been reported in line with the PROCESS criteria [3], we describe 2 cases of retrocaval ureter treated by laparoscopic transperitoneal pyelopyelostomy, with a review of the literature on the diagnosis and laparoscopic treatment of retrocaval ureter.
2. Case presentations
2.1. Case 1
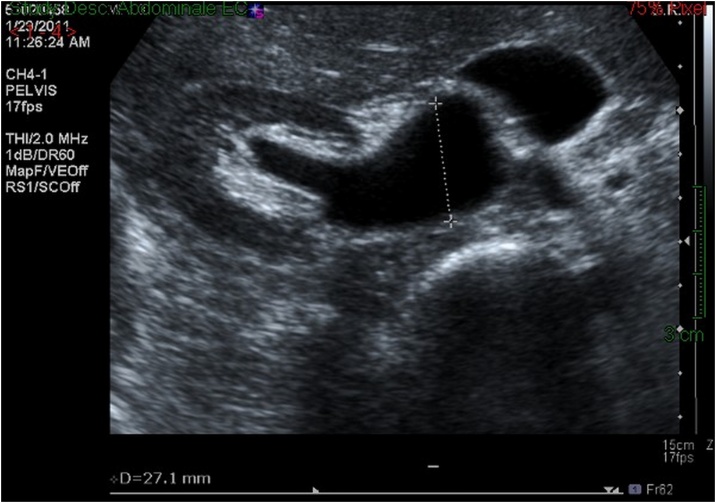
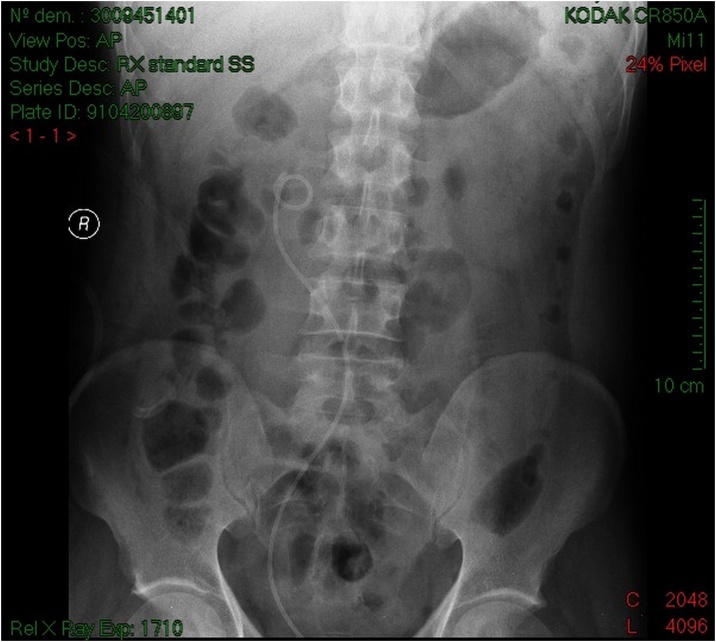
A 43-year-old previously healthy woman presented for right-sided flank pain, fever, chills with leukocytosis, history of UTI treated by antibiotics 2 weeks ago, with long history of recurrent intermittent right-sided flank pain not investigated. Renal ultrasound showed severe right-sided hydronephrosis (Fig. 1) and computed tomography scan suggested the presence of a RCU (Fig. 2).
Fig. 1.
Renal ultrasound of patient 1 showing severe right-sided hydronephrosis.
Fig. 2.
KUB scan of patient 1 suggesting the presence of a RCU.
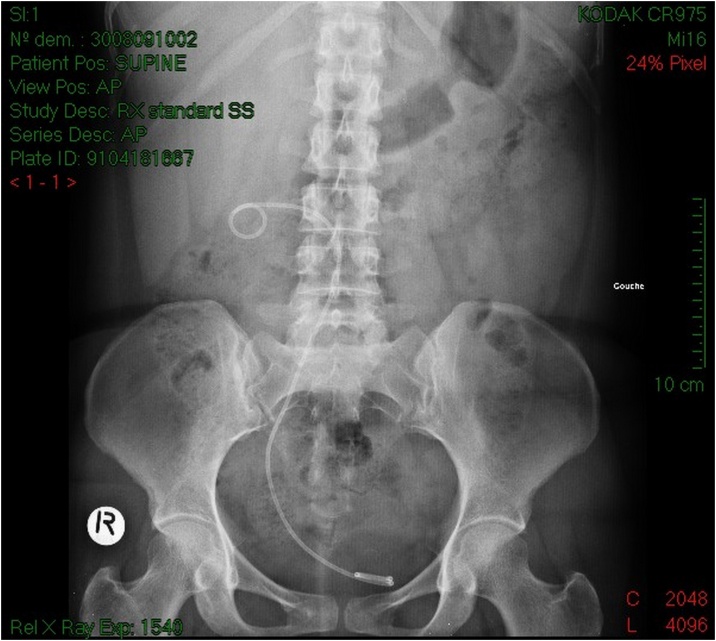
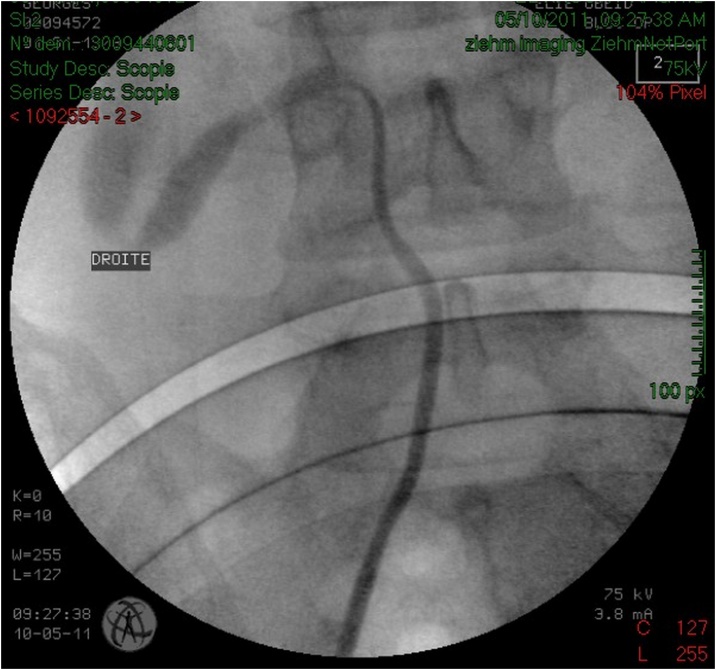
Serum testing demonstrated preserved renal function, urine culture turned positive for proteus mirabilis. The patient was treated with intravenous antibiotics and drainage of the right kidney by a double J stent (Fig. 3) with retrograde ureteropyelography that confirmed the diagnosis of retrocaval ureter (Fig. 4), antibiotic treatment continued for 2 weeks orally, and laparoscopic repair of retrocaval ureter was planned after sterilization of the urine.
Fig. 3.
KUB of patient 1 showing the double J stent that takes the S shape of the ureter.
Fig. 4.
Retrograde ureteropyelography of patient 1 confirming the diagnosis of retrocaval ureter.
2.2. Case 2
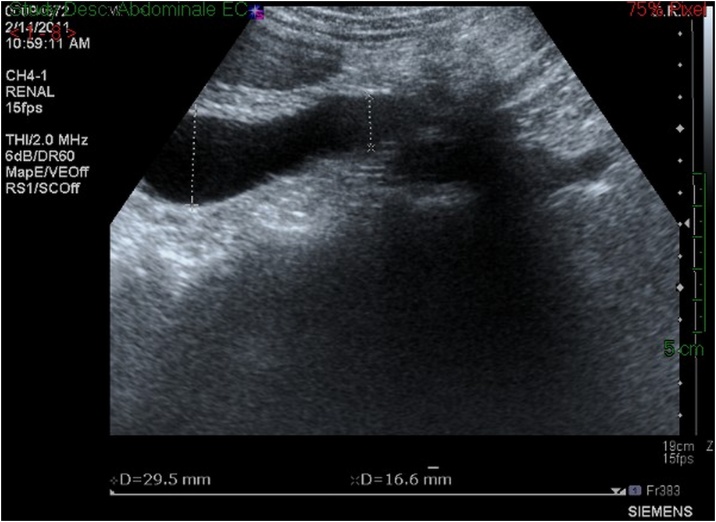
A 38-year-old man previously healthy presented for a recurrent intermittent right-sided flank pain exacerbating since about 1 year ago, aggravated by water intake and associated with irritative (urinary frequency) lower urinary tract symptoms (LUTS), history of left renal colic with spontaneous passage of small stone about 3 years ago not investigated. Renal ultrasound demonstrated sever right-sided hydronephrosis (Fig. 5) and computed tomography scan suggested the presence of a retrocaval ureter (Fig. 6), Serum testing demonstrated preserved renal function, and a laparoscopic repair of retrocaval ureter was planned, with a right retrograde ureteropyelography (Fig. 7), done just before the surgery for a retrograde double J stent placement (Fig. 8), and confirmed the diagnosis of retrocaval ureter.
Fig. 5.
Renal ultrasound of patient 2 showing severe right-sided hydronephrosis.
Fig. 6.
Computed tomography scan of patient 2 showing the presence of a retrocaval ureter.
Fig. 7.
Right retrograde ureteropyelography of patient 2 showing the S shape of the ureter.
Fig. 8.
KUB of patient 2 showing the double J stent that takes the S shape of the retrocaval ureter.
2.3. Surgical technique
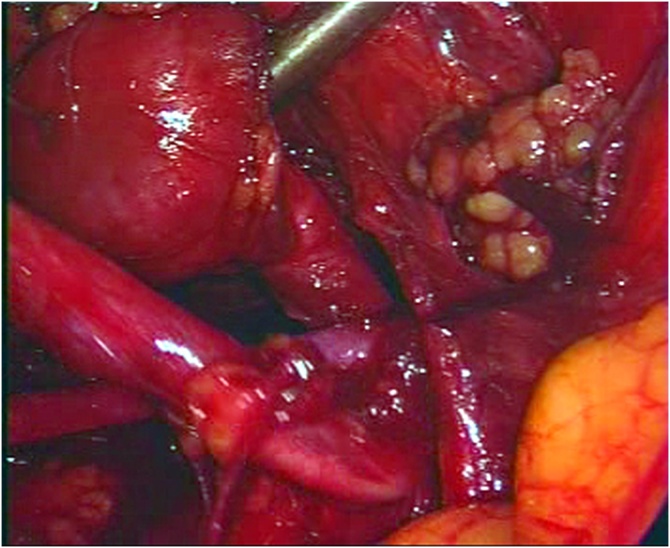
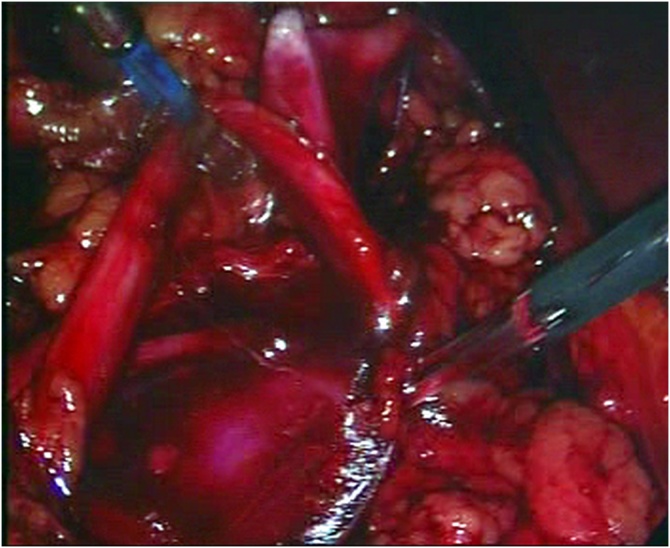
After induction of general endotracheal anesthesia an orogastric tube and a Foley catheter were inserted. The patient was positioned in a 60-degree left lateral decubitis position and a transperitoneal approach was used. A pneumoperitoneum was created using a Veress needle and ports were entered applying a 20 mm Hg intra-abdominal pressure. First, a 10-mm camera port was placed at the umbilicus level on the lateral rectus border. After the placement of the first port, the others were placed under direct vision. A 10 mm working port was placed 1 cm below the costal border on the midclavicular line, and a 5 mm port at a point on the lateral one-third of the line between the anterior superior iliac spine and the umbilicus. The 5-mm fourth trocar was placed for traction on midaxillary line at the level of the umbilicus (Fig. 9). The intracorporeal pressure was decreased to 12 mm Hg after the placement of the ports. After the incision of the Toldt line, the dilated proximal renal pelvis and ureter were found and separated from the adjacent tissue by a blunt and sharp dissection (Fig. 10). Traction of the proximal ureter by a stich of the renal pelvis through the abdominal wall, helped to identify the distal ureteral segment which was released without damaging the periureteral soft tissue. After the complete release of the ureteral segment beneath the inferior vena cava, the dilated renal pelvis was transected at the ureteropelvic junction (Fig. 11). The ureter was separated from the inferior vena cava and positioned anterior to it. The dilated renal pelvis was anastomosed (pyelopyelostomy) with 4-0 vicryl intracorporeal sutures inserted in a continuous manner posteriorly and interrupted sutures anteriorly after the introduction of the proximal curve of the double J stent inserted before the surgery. After the completion of anastomosis, a closed suction drain was placed in the operation area.
Fig. 9.
Trocars’ positions (same laparoscopic technique for the two patients).
Fig. 10.
Dilated proximal renal pelvis and ureter were found and separated from the adjacent tissue by a blunt and sharp dissection.
Fig. 11.
Transection at the ureteropelvic junction.
2.4. Results
The operative time was 210 and 180 min for patients 1 and 2 respectively. Neither intraoperative complication nor significant bleeding occurred. Urethral catheters were removed 24 h post surgery, the drains were removed 1 day after catheter removal, and the patients were discharged 48 h after the operation after return of bowel function. No significant dilatation was observed on ultrasound at the fourth week follow-up as well as after 3, 6 12 and 24 months. No patient had problems in the early postoperative period. Post-surgery, the patients were followed up with ultrasound at the fourth week and JJ stents were removed at the sixth week. At 3-month follow-up, diuretic radionuclide scan revealed no evidence of obstruction of the right kidney, and the excretory urogram revealed prompt excretion of the contrast material, with no dilatation of the repaired renal unit and a widely patent anastomosis in both patients.
Within the follow-up period patients were tracked by ultrasound at the 3rd, 6th, 12th and 24th month and questioned for the presence of postoperative symptoms. The two patients showed improvement in dilatation and had no symptoms.
3. Review of the literature
3.1. Pathologic embryology
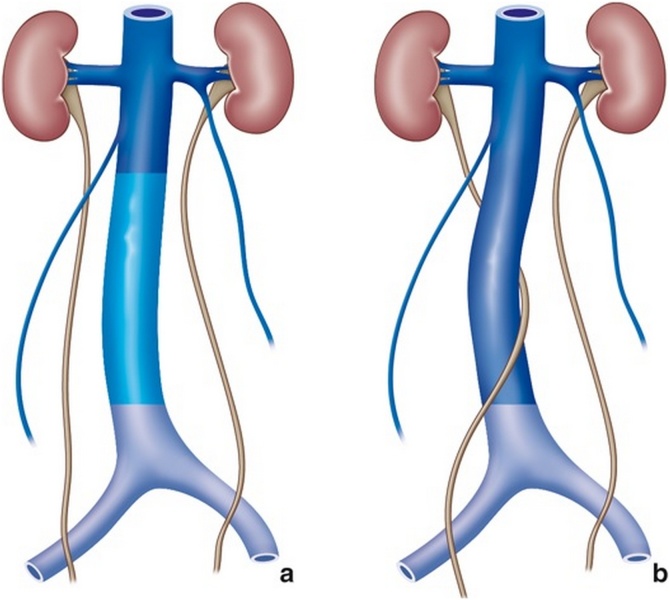
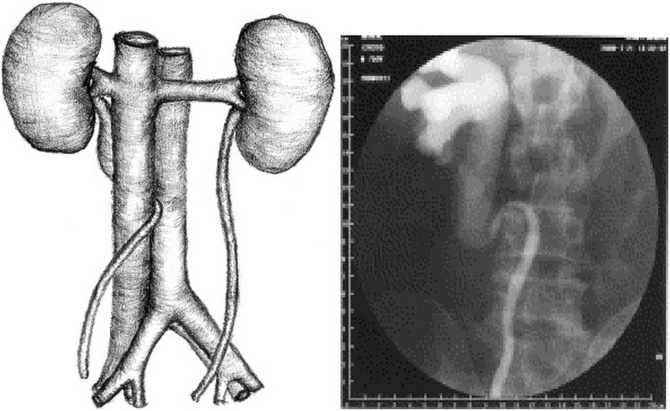
Because of the persistence of the posterior cardinal vein that is located ventral to the ureter, the ureter will become entrapped behind the vein (Fig. 12). Thus, the ureter, predominantly the right ureter, courses behind the IVC, then between the vena cava and aorta, and continues to course downward anterior and, finally, lateral to the IVC.
Fig. 12.
Persistence of the posterior cardinal vein ventral to the ureter entrapping it.
3.2. Epidemiology
The incidence has been reported as 1 in 1000 individuals [4,5].
This anomaly is almost exclusively found on the right; however, 1 case of a left-sided retrocaval ureter in association with situs inversus and 1 case of bilateral involvement [6,7] have been reported, it usually manifest in the third or fourth decade of life [8], and occurs tree more times frequently in men than in women [9].
3.3. Classification
In 1982, Bergman classified retrocaval ureter into two clinical types [10]. Type I (low loop) (Fig. 13) is the most common, with the dilated proximal ureter assuming the shape of a reverse “J”. Usually, this type of ureter is obstructed. Type II (high loop) is seen less frequently. The ureter passes behind the IVC at the level of, or just above, the pelvic-ureteral junction. This type of ureter is frequently not obstructed.
Fig. 13.
RCU Type I (low loop) with the dilated proximal ureter assuming the shape of a reverse “J”.
3.4. Associated congenital anomalies
Approximately 20% of the patients with retrocaval ureter may had accompanying congenital abnormalities including solitary kidney, contralateral renal hypoplasia or ectopia [11], horseshoe kidney [12,13], aberrant renal artery [14], Turner’s syndrome [15], Goldenhar syndrome [16], retroperitoneal fibrosis [17], and polycystic disease of the kidneys [18], nutcracker symdrome, ureterocele, ureteropelvic junction obstruction [19,20] genital malformation (hypospadias), duplicated IVC, situs inversus, intestinal malrotation, cardiovascular anomalies (coarctation of the aorta, pulmonary venous stenosis) [21], and myelomeningocele [22].
3.5. Clinical aspect
About 80% of cases are symptomatic, with no pathognomonic symptom for the RCU: Right flank pain being the most common symptom occurring in about 70% of cases, varying from a dull, persistent and well localized pain to severe renal colic according to the nature and degree of the ureteral obstruction, associated sometimes with atypical abdominal or pelvic pain, and vomiting. Hematuria either micro or gross hematuria may be present in about 20% of cases, can be isolated or associated with flank pain is related to urolithiasis in most cases.
Infection of the upper urinary tract (acute pyelonephritis) with fever, leucocyturia, bacteriuria, sometimes pyonephrosis and bacteremia may be present in about 20% of cases and should prompt urgent diagnostic and therapeutic management [23].
3.6. Diagnostic imaging
Ultrasound contributes to diagnosis because it highlights pyelo-calyceal dilatation of the right kidney signing the obstacle on the urinary tract [24]. The CT Urography is now the method of choice for diagnosing retrocaval ureter; it is the most efficacious and least invasive method of confirming the diagnosis, it allows the differential diagnosis of ureteral obstructions due to an acquired retroperitoneal pathology, especially malignant tumors and retroperitoneal fibrosis. Compared to CT Scan, MRI is equally good, has no radiation risk, and does not require an iodinated contrast. Renal scan can assess the degree of obstruction (DTPA), as well as the renal function (DMSA), and may be used for the follow up of asymptomatic patients with retrocaval ureter [[25], [26], [27]].
3.7. Conservative surgical treatment
Despite active surveillance in asymptomatic patients with normal renal scan and nephrectomy for patients with destroyed kidney, conservative surgical treatment is indicated for all symptomatic patients with preserved ipsilateral renal function.
The principle of conservative surgery for retrocaval ureter is the restoration of normal anatomic position by transpositioning of the ureter over the inferior vena cava. This can be done by open surgery, laparoscopic transperitoneal [28], laparoscopic retroperitoneal [29], as well as by robotic assisted surgery [30].
Conventionally, open access has been considered the standard procedure for the correction of RCU [31]. However, in the last decade, with the intensive growth of minimally invasive surgery the laparoscopic approach has proved to yield equivalent therapeutic results, with superior aesthetic outcomes, fewer analgesic requirements, a shorter hospital stay [32,33] and more rapid convalescence. The limiting factors are the learning curve of laparoscopic operations and the difficulty in intracorporeal suture techniques [34,35], both of which can be overcome if such patients are referred to urologic centers with laparoscopic experts. New advances in laparoscopic suturing techniques have improved dramatically in the past few years.
Table 1 resumes the different results published in the articles on the minimally invasive surgical management of the RCU from 1994 till now, it was done after a thorough literature review on Pub Med:
In 1994, Baba was the first to perform a laparoscopic pyelopyelostomy using a transperitoneal approach for retrocaval ureter [36].
Salomon et al. [29] reported the first case of retroperitoneoscopic repair of retrocaval ureter in a young man. Gupta et al. [32] used a three-port retroperitoneoscopic approach to perform ureterolysis and ureteroureteral reconstruction that lasted for 3.5 h.
The decision of whether to resect or preserve the retrocaval segment of the ureter has been controversial. Simforoosh et al. [32] reported 6 cases without excision of the retrocaval segment. They transected at the level of the dilated renal pelvis and performed pyeloplasty, with successful results. However, in all their patients, the retrocaval segment appeared grossly normal [32]. Zhang et al. [35] suggested excising the retrocaval segment if an 8F catheter could not pass through the segment easily. We think that the radiologic findings and intraoperative appearance of the ureter should be used to decide whether or not to excise the retrocaval segment. Its preservation should be considered only if this segment has had a normal appearance, without considerable kinking. In addition, with each ureteral peristalsis, the upper ureter should not dilate further and the peristaltic movement should be seen throughout the entire length of the retrocaval segment. In such cases, it is preferred to transect the ureter at the lower part of the dilated ureter, lateral to the IVC. This makes the anastomosis easier at a site with an ample blood supply and decreases the probability of stricture formation. However, if any of these findings are missing or doubt is present, one should transect the ureter medial to the IVC and resect the upper stump until a non-kinking dilated ureter and urine flow are clearly detected.
We have performed ureteroureteral or ureteropelvic end-to-end anastomosis, depending on the level of ureteral transaction, with approximately 1-cm spatulation of the lower ureteral stump and, in selected cases, of the upper ureteral stump is recommended. Insufficient spatulation can result in stricture formation at the site of anastomosis.
The choice of either a transperitoneal or a retroperitoneal approach depends on surgeon preference. There were different results in the transabdominal and retroperitoneal laparoscopic repair of the retrocaval ureter. Ramalingam and Selvarajan [37] presented their experience with transperitoneal LUUS of retrocaval ureter in 2 cases. They believed that transperitoneal intracorporeal suturing is less time-consuming and easier than retroperitoneoscopic suturing. Gupta et al. [36] found retroperitoneoscopic approach to be safer, easier, and less time-consuming, and it provided direct access to the ureter and IVC while avoiding spillage of urine into the peritoneal cavity. Mugiya et al. [43] confirmed that the retroperitoneoscopic treatment could be superior to the conventional transabdominal approach to perform the laparoscopic transposition and re-anastomosis of a retrocaval ureter, because it provides a shorter and more direct access to the ureter, without interference from intra-abdominal structures. Although the working space for laparoscopic manipulation is relatively limited, results have clearly showed that it is effective when an experienced surgeon performs reconstructive procedures for this approach. Gupta et al. [32] and Salomon et al. [29] suggested that the retroperitoneal laparoscopy represented the more direct approach to the urinary tract and the shorter time was obtained because dissection of the retroperitoneal space was not hindered by intra-abdominal organs.
The approach performed frequently is the transperitoneal approach because of a larger operation field and because of urologists who are more familiar with this approach [37,38]. The retroperitoneal approach was also described earlier because of the concerns of urine leaking into the peritoneum [39,40]. However, the surgical field is narrower in this approach, and we believe that a transperitoneal watertight anastomosis over an internal stent is straightforward and does not pose any postoperative problems. Another technique using laparoscopically-assisted extracorporeal anastomosis through a 2 cm skin incision has been described with the aim of decreasing the operative time [41]. However, this approach is not compatible with the aim and principle of laparoscopy.
The transumbilical single-port (LESS technique) approach is practical and affords a virtually scar-free result. Experience is increasing, and the first successful case of LESS repair of retrocaval ureter using the GelPoint access platform reported by Robert J. Stein et al. from the Center for Laparoscopy and Robotic Surgery, Glickman Urological and Kidney Institute, Cleveland Clinic. The procedure was technically successful and operative time at 3 h was comparable to that of reported standard laparoscopic series. LESS procedures remain somewhat cumbersome, and further refinement in instrumentation is needed before the technique may achieve the level of standardization.
Given the advances in robotic-assisted laparoscopic surgery, RCU which has been operated using pure robotic laparoscopy was reported [42,43]. The authors stated that robotic assistance eases the dissection and intracorporeal suturing and knotting. However, it is not available in every institute. Recognized benefits of the da Vinci robotic System over conventional laparoscopy include superior ergonomics, 3-dimensional optical magnification of the operative field within direct control of the console surgeon, enhanced surgeon dexterity within the field of view, and precision of surgical manipulation with tremor reduction.
Finally, for the operative time, we believe that the running re-anastomosis of the transected renal pelvis (eliminating much intracorporeal knot tying) and intraoperative placement of a Double-J® stent (thus, forgoing preliminary cystoscopy, guide wire or stent placement and patient repositioning) contributed significantly to a shorter operative time as for example in the series of Simforoosh et al. [28].
4. Conclusion
Laparoscopic treatment of retrocaval ureter is a recommended management for many reasons: less blood loss during the surgery, a shorter hospital stay, less postoperative pain and superior esthetic effect with excellent functional results. All of these findings were also a part of our experience on the two reported cases. The main cause of the increased operating time is the intracorporeal anastomosis of the ureter which remains the main limiting factor of the laparoscopic surgery.
The literature review has clearly shown the advantages of minimally invasive approaches.
Pure laparoscopic treatment of RCU seems feasible and technically reliable, and should be the standard surgical option for the treatment of RCU.
The laparoscopic magnification provides an excellent exposure, allowing an adequate dissection of ureter in situ. The retrocaval segment could easily be freed from the vena cava. Adequate dissection and mobilization of the ureter and periureteral tissue is mandatory to ensure a tension-free anastomosis while preserving its blood supply. Unnecessary dissection should be avoided to obtain the best possible results.
Conflicts of interest
No conflict of interest.
Funding
No sponsor for this article.
Ethical approval
This work is exempt from ethical approval in our institution because of its type.
Consent
Written informed consent was obtained from the patients for publication of these case reports and accompanying images. A copy of the written consents is available for review by the Editor-in-Chief of this journal on request.
Author contribution
EL KHOURY, SLEIMAN, ELIAS and ABDESSATER conceived of the presented idea and were encouraged by COLOBY to execute it.
BART, ABDESSATER, EL KHOURY and SLEIMAN were on the operating field while performing the surgeries and all of them participated to the different steps of the surgery but EL KHOURY was the main surgeon.
SLEIMAN, BART, ELIAS and ABESSATER chose and cropped the most important figures from the surgery’s video and pathology.
BART, SLEIMAN and EL KHOURY contributed to the final version of the manuscript. COLOBY supervised the work.
ABDESSATER and ELIAS took the lead in writing the manuscript when they found that It deserves to be published.
All authors provided critical feedback and helped shape the manuscript.
The 6 authors designed the model and the computational framework and analyzed the results.
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content.
Registration of research studies
Research registry 4708.
Guarantor
Patrick COLOBY and Walid SLEIMAN are the guarantors of this work.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Bartle E.J., Pearce W.H., Sun J.H. Infrarenal venous anomalies and aortic surgery avoiding vascular injury. J. Vasc. Surg. 1987;6:590–593. doi: 10.1067/mva.1987.avs0060590. [DOI] [PubMed] [Google Scholar]; Bartle E.J, Pearce W.H, Sun J.H et al. Infrarenal venous anomalies and aortic surgery avoiding vascular injury J Vasc Surg 1987 ; 6 : 590-593 [DOI] [PubMed]
- 2.Hochstetter F. Beitrage zur entwicklungsgeschichte des venen-systems der amnioten: III. Sauger. Morph Jahrb. 1893;20 542–542. [Google Scholar]; Hochstetter F. Beitrage zur entwicklungsgeschichte des venen-systems der amnioten: III. Sauger Morph Jahrb. 1893; 20:542–542.
- 3.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., SCARE Group The PROCESS 2018 statement: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2018;60:279–282. doi: 10.1016/j.ijsu.2018.10.031. [DOI] [PubMed] [Google Scholar]; Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, Orgill DP; SCARE Group. The PROCESS 2018 Statement: Updating Consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) Guidelines. Int J Surg. 2018. [DOI] [PubMed]
- 4.Crosse J.E., Soderdahl D.W., Teplick S.K. Nonobstructive circumcaval (retrocaval) ureter a report of 12 cases. Radiology. 1975;116:69–71. doi: 10.1148/116.1.69. [DOI] [PubMed] [Google Scholar]; Crosse J.E, Soderdahl D.W, Teplick S.K et al. Nonobstructive circumcaval (retrocaval) ureter A report of 12 cases Radiology 1975 ; 116 : 69-71 [DOI] [PubMed]
- 5.Murphy B.J., Casillas J., Becerra J.L. Retrocaval ureter computed tomography and ultrasound appearance. J. Comput. Tomogr. 1987;11:89–93. doi: 10.1016/0149-936x(87)90040-3. [DOI] [PubMed] [Google Scholar]; Murphy B.J, Casillas J, Becerra J.L. Retrocaval ureter computed tomography and ultrasound appearance J Comput Tomogr 1987 ; 11 : 89-93 [DOI] [PubMed]
- 6.Kenawi M.M., Williams D.I. Circumcaval ureter a report of 4 cases in children with a review of the literature and a new classification. Br. J. Urol. 1976;48:183–192. doi: 10.1111/j.1464-410x.1976.tb10197.x. [DOI] [PubMed] [Google Scholar]; Kenawi M.M, Williams D.I. Circumcaval ureter a report of 4 cases in children with a review of the literature and a new classification Br J Urol 1976 ; 48 : 183-192 [DOI] [PubMed]
- 7.Carrion H., Gatewood J., Politano V. Retrocaval ureter report of 8 cases and the surgical management. J. Urol. 1979;121:514–517. doi: 10.1016/s0022-5347(17)56849-4. [DOI] [PubMed] [Google Scholar]; Carrion H, Gatewood J, Politano V et al. Retrocaval ureter report of 8 cases and the surgical management J Urol 1979 ; 121 : 514-517 [DOI] [PubMed]
- 8.Gulmi F.A., Felsen D., Vaughan E.D., Jr. Pathophysiology of urinary tract obstruction. In: Walsh P.C., Retik A.B., Vaughan E.D. Jr., editors. Campbell’s Urology. 8th ed. W B Saunders Co.; Philadelphia, PA: 2002. p. 431. [Google Scholar]; Gulmi FA, Felsen D, Vaughan ED Jr. Pathophysiology of urinary tract obstruction. In: Walsh PC, Retik AB, Vaughan ED Jr, et al, eds. Campbell’s Urology, 8th ed. Philadelphia, PA: W B Saunders Co; 2002:431.
- 9.Pais V.M., Strandhoy J.W., Assimos D.G. Pathophysiology of urinary tract obstruction. In: Wein A.J., Kavoussi L.R., Novick A.C., Partin A.W., Peters C.A., editors. vol. 2. Saunders-Elsevier; Philadelphia, PA: 2007. pp. 1195–1226. (Campbell-Walsh Urology). [Google Scholar]; Pais VM, Strandhoy JW, Assimos DG. Pathophysiology of urinary tract obstruction. In Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, eds. Campbell-Walsh Urology, Vol 2. Philadelphia, PA: Saunders-Elsevier; 2007:1195-1226.
- 10.Bateson E.M., Atkinson D. Circumcaval ureter: a new classification. Clin. Radiol. 1969:173–177. doi: 10.1016/s0009-9260(69)80166-2. [DOI] [PubMed] [Google Scholar]; Bateson E.M, Atkinson D. Circumcaval ureter: a new classification Clin Radiol 1969 ;173-177 [DOI] [PubMed]
- 11.Brito R.R., Zulian R., Albuquerque J., Borges H.J. Retrocaval ureter. Br. J. Urol. 1973;45:144–152. doi: 10.1111/j.1464-410x.1973.tb12131.x. [DOI] [PubMed] [Google Scholar]; Brito RR, Zulian R, Albuquerque J, Borges HJ. Retrocaval ureter. Br J Urol 1973;45:144–52. [DOI] [PubMed]
- 12.Fernandes M., Scheuch J., Seebode J.S. Horseshoe kidney with a retrocaval ureter: a case report. J. Urol. 1988;140:362–363. doi: 10.1016/s0022-5347(17)41608-9. [DOI] [PubMed] [Google Scholar]; Fernandes M, Scheuch J, Seebode JS. Horseshoe kidney with a retrocaval ureter: a case report. J Urol 1988;140:362–3. [DOI] [PubMed]
- 13.Fuyii Y., Sasabe S., Araki T. Retrocaval ureter treated by division and reanastomosis of the IVC. Acta Urol. Jpn. 1966;12:422–426. [PubMed] [Google Scholar]; Fuyii Y, Sasabe S, Araki T. Retrocaval ureter treated by division and reanastomosis of the IVC. Acta Urol Jpn 1966;12: 422–6. [PubMed]
- 14.Fletcher E.W., Lecky J.W. Retrocaval ureter obstructed by an aberrant renal artery. J. Urol. 1971;106:184–185. doi: 10.1016/s0022-5347(17)61256-4. [DOI] [PubMed] [Google Scholar]; Fletcher EW, Lecky JW. Retrocaval ureter obstructed by an aberrant renal artery. J Urol 1971;106:184–5. [DOI] [PubMed]
- 15.Cleeve D.M., Older R.A., Cleeve L.K., Bredael J.J. Retrocaval ureter in Turner syndrome. Urology. 1979;13:544–545. doi: 10.1016/0090-4295(79)90469-2. [DOI] [PubMed] [Google Scholar]; Cleeve DM, Older RA, Cleeve LK, Bredael JJ. Retrocaval ureter in Turner syndrome. Urology 1979;13:544–5. [DOI] [PubMed]
- 16.Ishitoya S., Arai Y., Waki K. Left retrocaval ureter associated with the Goldenhar syndrome (branchial arch syndrome) J. Urol. 1997;158:572–573. [PubMed] [Google Scholar]; Ishitoya S, Arai Y, Waki K, et al. Left retrocaval ureter associated with the Goldenhar syndrome (branchial arch syndrome). J Urol 1997;158:572–3. [PubMed]
- 17.Arriola P.M., el-Droubi H., Dahlen C.P. Combined retrocaval ureter and retroperitoneal fibrosis: report of a case. J. Urol. 1979;121:107–108. doi: 10.1016/s0022-5347(17)56682-3. [DOI] [PubMed] [Google Scholar]; Arriola PM, el-Droubi H, Dahlen CP. Combined retrocaval ureter and retroperitoneal fibrosis: report of a case. J Urol 1979; 121:107–8. [DOI] [PubMed]
- 18.Fujii Y., Sasabe S., Araki T. Retrocaval ureter associated with polycystic disease of the kidneys: treated by division and reanastomosis of the vena cava. Hinyokika Kiyo. 1966;12:1422–1428. [PubMed] [Google Scholar]; Fujii Y, Sasabe S, Araki T. Retrocaval ureter associated with polycystic disease of the kidneys: treated by division and reanastomosis of the vena cava. Hinyokika Kiyo 1966;12:1422–8. [PubMed]
- 19.Yarmohammadi A., Mohamadzadeh R., Feizzadeh B. Retrocaval ureter. A study of 13 cases. Urol. J. 2006;3:175–179. [PubMed] [Google Scholar]; Yarmohammadi A, Mohamadzadeh R, Feizzadeh B, et al. Retrocaval ureter. A study of 13 cases. Urol J. 2006;3:175-179. [PubMed]
- 20.Lin H.Y., Chou Y.H., Huang S.P. Retrocaval ureter: report of two cases and literature review. Kaohsiung J. Med. Sci. 2003;19:127–131. doi: 10.1016/S1607-551X(09)70460-7. [DOI] [PubMed] [Google Scholar]; Lin HY, Chou YH, Huang SP, et al. Retrocaval ureter: report of two cases and literature review. Kaohsiung J Med Sci. 2003;19:127-131. [DOI] [PubMed]
- 21.Chantepie Lesur, Ph., Lanson Y., Soret J.Y. 1983. Uretère rétrocave. - Artères et Veines; p. 491. Nov. Déc. [Google Scholar]; CHANTEPIE, LESUR Ph, LANSON Y, SORET J.Y. - Uretère rétrocave. - Artères et Veines, Nov.Déc 1983, 491.
- 22.Piercy S.L. Ventriculo-peritoneal shunt pseudocyst causing uretero-pelvic junction obstruction in a child with myelomeningocele and retrocaval ureter. J. Urol. 1984;132:345–348. doi: 10.1016/s0022-5347(17)49621-2. [DOI] [PubMed] [Google Scholar]; PIERCY SL, et al. Ventriculo-peritoneal shunt pseudocyst causing uretero-pelvic junction obstruction in a child with myelomeningocele and retrocaval ureter. J. Urol. 1984 ; 132 : 345-348 [DOI] [PubMed]
- 23.Roujas F. 1965. Contribution à l’étude de l’uretère rétrocave. - Thèse. Paris. [Google Scholar]; ROUJAS F. - Contribution à l'étude de l'uretère rétrocave. - Thèse, Paris, 1965.
- 24.Schaffer R.M. Retrocaval ureter: sonographic appearance. J. Ultrasound Med. 1985;4:199–201. doi: 10.7863/jum.1985.4.4.199. [DOI] [PubMed] [Google Scholar]; SCHAFFER RM, et al. Retrocaval ureter : sonographic appearance. J. Ultrasound Med. 1985 ; 4 : 199-201 [DOI] [PubMed]
- 25.Feldman S.L., Dimarco R., Tencer T., Ross L.S. Retrocaval ureter: radiographic techniques directing surgical management. Br. J. Urol. 1982;54:212–215. doi: 10.1111/j.1464-410x.1982.tb06960.x. [DOI] [PubMed] [Google Scholar]; FELDMAN SL, DIMARCO R, TENCER T, ROSS LS Retrocaval ureter : radiographic techniques directing surgical management. Br. J. Urol. 1982 ; 54 : 212-215 [DOI] [PubMed]
- 26.Gefter W.B., Arger P.H., Mulhern C.B., Pollack H.M., Wein A.J. Computed tomography of circumcaval ureter. Am. J. Roentgenol. 1978;131:1086–1987. doi: 10.2214/ajr.131.6.1086. [DOI] [PubMed] [Google Scholar]; GEFTER WB, ARGER PH, MULHERN CB, POLLACK HM, WEIN AJ Computed tomography of circumcaval ureter. Am. J. Roentgenol. 1978 ; 131 : 1086-1987 [DOI] [PubMed]
- 27.Sasai K., Sano A., Imanaka K. Right periureteric venous ring detected by computed tomography. J. Comput. Assist. Tomogr. 1986;10:349–351. doi: 10.1097/00004728-198603000-00040. [DOI] [PubMed] [Google Scholar]; SASAI K, SANO A, IMANAKA K, et al. Right periureteric venous ring detected by computed tomography. J. Comput. Assist. Tomogr. 1986 ; 10 : 349-351 [DOI] [PubMed]
- 28.Simforoosh N., Nouri-Mahdavi K., Tabibi A. Laparoscopic pyelopyelostomy for retrocaval ureter without excision of the retrocaval segment: first report of 6 cases. J. Urol. 2006;175:2166–2169. doi: 10.1016/S0022-5347(06)00269-2. [DOI] [PubMed] [Google Scholar]; Simforoosh N, Nouri-Mahdavi K, Tabibi A. Laparoscopic pyelopyelostomy for retrocaval ureter without excision of the retrocaval segment: first report of 6 cases J. Urol. 2006 ; 175 : 2166-2169 [DOI] [PubMed]
- 29.Salomon L., Hoznek A., Balian C., Gasman D., Chopin D.K., Abbou C.C. Retroperitoneal laparoscopy of a retrocaval ureter. BJU Int. 1999;84:181–182. doi: 10.1046/j.1464-410x.1999.00183.x. [DOI] [PubMed] [Google Scholar]; Salomon L, Hoznek A, Balian C, Gasman D, Chopin D.K, Abbou C.C. Retroperitoneal laparoscopy of a retrocaval ureter BJU Int. 1999 ; 84 : 181-182 [DOI] [PubMed]
- 30.Gundeti M.S., Duffy P.G., Mushtaq I. Robotic-assisted laparoscopic correction of pediatric retrocaval ureter. J. Laparoendosc. Adv. Surg. Tech. A. 2006;16:422–424. doi: 10.1089/lap.2006.16.422. [DOI] [PubMed] [Google Scholar]; Gundeti M.S, Duffy P.G, Mushtaq I. Robotic-assisted laparoscopic correction of pediatric retrocaval ureter J. Laparoendosc. Adv. Surg. Tech. A 2006 ; 16 : 422-424 [DOI] [PubMed]
- 31.Zhang X.D., Hou S.K., Zhu J.H. Diagnosis and treatment of retrocaval ureter. Eur. Urol. 1990;18:207–210. doi: 10.1159/000463911. [DOI] [PubMed] [Google Scholar]; Zhang X.D, Hou S.K, Zhu J.H, et al. Diagnosis and treatment of retrocaval ureter Eur Urol 1990 ; 18 : 207-210 [DOI] [PubMed]
- 32.Gupta N.P., Hemal A.K., Singh I. Retroperitoneoscopic ureterolysis and reconstruction of retrocaval ureter. J. Endourol. 2001;15:291–293. doi: 10.1089/089277901750161818. [DOI] [PubMed] [Google Scholar]; Gupta N.P, Hemal A.K, Singh I, et al. Retroperitoneoscopic ureterolysis and reconstruction of retrocaval ureter J Endourol. 2001 ; 15 : 291-293 [DOI] [PubMed]
- 33.Soundappan S.V., Barker A.P. Retrocaval ureter in children: a report of two cases. Pediatr. Surg. Int. 2004;20:158–160. doi: 10.1007/s00383-003-1038-x. [DOI] [PubMed] [Google Scholar]; Soundappan S.V, Barker A.P. Retrocaval ureter in children: a report of two cases Pediatr Surg Int. 2004 ; 20 : 158-160 [DOI] [PubMed]
- 34.Ameda K., Kakizaki H., Harabayashi T. Laparoscopic ureteroureterostomy for retrocaval ureter. Int. J. Urol. 2001;8:71–74. doi: 10.1046/j.1442-2042.2001.00255.x. [DOI] [PubMed] [Google Scholar]; Ameda K, Kakizaki H, Harabayashi T, et al. Laparoscopic ureteroureterostomy for retrocaval ureter Int J Urol. 2001 ; 8 : 71-74 [DOI] [PubMed]
- 35.Bhandarkar D.S., Lalmalani J.G., Shivde S. Laparoscopic ureterolysis and reconstruction of a retrocaval ureter. Surg. Endosc. 2003;17:1851–1852. doi: 10.1007/s00464-003-4513-5. [DOI] [PubMed] [Google Scholar]; Bhandarkar D.S., Lalmalani J.G., Shivde S. Laparoscopic ureterolysis and reconstruction of a retrocaval ureter Surg Endosc. 2003 ; 17 : 1851-1852 [DOI] [PubMed]
- 36.Baba S., Oya M., Miyahara M. Laparoscopic surgical correction of circumcaval ureter. Urology. 1994;44:122–126. doi: 10.1016/s0090-4295(94)80023-5. [DOI] [PubMed] [Google Scholar]; Baba S., Oya M., Miyahara M, et al. Laparoscopic surgical correction of circumcaval ureter Urology 1994 ; 44 : 122-126 [DOI] [PubMed]
- 37.Ramalingam M., Selvarajan K. Laparoscopic transperitoneal repair of retrocaval ureter: report of two cases. J. Endourol. 2003;17:85–87. doi: 10.1089/08927790360587397. [DOI] [PubMed] [Google Scholar]; Ramalingam M., Selvarajan K. Laparoscopic transperitoneal repair of retrocaval ureter: report of two cases J Endourol. 2003 ; 17 : 85-87 [DOI] [PubMed]
- 38.Matsuda T., Yasumoto R., Tsujino T. Laparoscopic treatment of a retrocaval ureter. Eur. Urol. 1996;29:115–118. doi: 10.1159/000473729. [DOI] [PubMed] [Google Scholar]; Matsuda T., Yasumoto R., Tsujino T. Laparoscopic treatment of a retrocaval ureter Eur Urol. 1996 ; 29 : 115-118 [DOI] [PubMed]
- 39.Mugiya S., Suzuki K., Ohhira T. Retroperitoneoscopic treatment of a retrocaval ureter. Int. J. Urol. 1999;6:419–422. doi: 10.1046/j.1442-2042.1999.00083.x. [DOI] [PubMed] [Google Scholar]; Mugiya S, Suzuki K, Ohhira T, et al. Retroperitoneoscopic treatment of a retrocaval ureter Int J Urol. 1999 ; 6 : 419-422 [DOI] [PubMed]
- 40.Kumar M., Kumar R., Hemal A.K. Complications of retroperitoneoscopic surgery at one centre. BJU Int. 2001;87:607–612. doi: 10.1046/j.1464-410x.2001.02137.x. [DOI] [PubMed] [Google Scholar]; Kumar M, Kumar R, Hemal AK, et al. Complications of retroperitoneoscopic surgery at one centre. BJU Int. 2001;87:607- 612. [DOI] [PubMed]
- 41.Tobias-Machado M., Lasmar M.T., Wroclawski E.R. Retroperitoneoscopic surgery with extracorporeal uretero-ureteral anastomosis for treating retrocaval ureter. Int. Braz. J. Urol. 2005;31:147–150. doi: 10.1590/s1677-55382005000200009. [DOI] [PubMed] [Google Scholar]; Tobias-Machado M, Lasmar MT, Wroclawski ER. Retroperitoneoscopicsurgery with extracorporeal uretero-ureteral anastomosis for treating retrocaval ureter. Int Braz J Urol. 2005;31:147- 150. [DOI] [PubMed]
- 42.Hemal A.K., Rao R., Sharma S. Pure robotic retrocaval ureter repair. Int. Braz. J. Urol. 2008;34:734–738. doi: 10.1590/s1677-55382008000600008. [DOI] [PubMed] [Google Scholar]; Hemal AK, Rao R, Sharma S, et al. Pure robotic retrocaval ureter repair. Int Braz J Urol. 2008;34:734-738. [DOI] [PubMed]
- 43.Gundeti M.S., Duffy P.G., Mushtaq I. Robotic-assisted laparoscopic correction of pediatric retrocaval ureter. J. Laparoendosc. Adv. Surg. Tech. A. 2006;16:422–424. doi: 10.1089/lap.2006.16.422. [DOI] [PubMed] [Google Scholar]; Gundeti MS, Duffy PG, Mushtaq I. Robotic-assisted laparoscopic correction of pediatric retrocaval ureter. J Laparoendosc Adv Surg Tech A. 2006;16:422-424. [DOI] [PubMed]
- 44.Polascik T.J., Chen R.N. Laparoscopic ureteroureterostomy for retrocaval ureter. J. Urol. 1998;160:121–122. [PubMed] [Google Scholar]; Polascik TJ, Chen RN. Laparoscopic ureteroureterostomy for retrocaval ureter. J Urol. 1998;160:121-122. [PubMed]
- 45.Nagraj H.K., Kishore T.A., Nagalakshmi S. Transperitoneal laparoscopic approach for retrocaval ureter. J. Minim. Access Surg. 2006;2(2):81–82. doi: 10.4103/0972-9941.26647. [DOI] [PMC free article] [PubMed] [Google Scholar]; Nagraj HK, Kishore TA, Nagalakshmi S. Transperitoneal laparoscopic approach for retrocaval ureter. J Minim Access Surg. 2006; 2(2):81-2. [DOI] [PMC free article] [PubMed]
- 46.Chung B.I., Gill I.S. Laparoscopic dismembered pyeloplasty of a retrocaval ureter: case report and review of the literature. Eur. Urol. 2008;54(6):1433–1436. doi: 10.1016/j.eururo.2008.09.010. [DOI] [PubMed] [Google Scholar]; B. I. Chung and I. S. Gill, Laparoscopic dismembered pyeloplasty of a retrocaval ureter: case report and review of the literature. European Urology. 2008; 54(6):1433–1436 [DOI] [PubMed]
- 47.Xu D.F., Yao Y.C., Ren J.Z., Liu Y.S., Gao Y., Che J.P., Cui X.G., Chen M. Retroperitoneal laparoscopic ureteroureterostomy for retrocaval ureter: report of 7 cases. Urology. 2009;74(6):1242–1245. doi: 10.1016/j.urology.2009.04.097. [DOI] [PubMed] [Google Scholar]; Xu DF, Yao YC, Ren JZ, Liu YS, Gao Y, Che JP, Cui XG, Chen M. Retroperitoneal laparoscopic ureteroureterostomy for retrocaval ureter: report of 7 cases.Urology.2009;74(6):1242-5 [DOI] [PubMed]
- 48.Autorino R., Khanna R., White M.A. Laparoendoscopic single-site repair of retrocaval ureter: first case report. Urology. 2010;76(6):1501–1505. doi: 10.1016/j.urology.2010.01.031. [DOI] [PubMed] [Google Scholar]; R. Autorino, R. Khanna, M. A.White et al. Laparoendoscopic single-site repair of retrocaval ureter: first case report. Urology.2010; 76 (6):1501–1505. [DOI] [PubMed]
- 49.Nayak B., Dogra P.N., Gupta N.P. Robotic repair of retrocaval ureter: a case series. Afr. J. Urol. 2012;18(3):135–137. [Google Scholar]; B. Nayak, P. N. Dogra, and N. P. Gupta, “Robotic repair of retrocaval ureter: a case series,” African Journal of Urology. 2012; 18(3):135–137.
- 50.Alkhudair W.K., Seyam R., Al Zahrani H.M., Al Otaibi M.F., Al Taweel W. Robotic uretero-ureterostomy of the retrocaval ureter without excision of the retrocaval segment. Can. Urol. Assoc. J. 2012;6(2):38–41. doi: 10.5489/cuaj.10121. [DOI] [PMC free article] [PubMed] [Google Scholar]; W. K. Alkhudair, R. Seyam, H. M. Al Zahrani, M. F. Al Otaibi, and W. Al Taweel, “Robotic uretero-ureterostomy of the retrocaval ureter without excision of the retrocaval segment,” Canadian Urological Association Journal. 2012; 6(2):38– 41. [DOI] [PMC free article] [PubMed]
- 51.Ding G.Q., Xu L.W., Li X.D., Li G.H., Yu Y.L., Yu D.M. Pure transperitoneal laparoscopic correction of retrocaval ureter. Chin. Med. J. (Engl.) 2012;125:2382–2385. [PubMed] [Google Scholar]; Ding GQ, Xu LW, Li XD, Li GH, Yu YL, Yu DM, et al. Pure transperitoneal laparoscopic correction of retrocaval ureter. Chin Med J (Engl) 2012;125:2382–5 [PubMed]
- 52.Junior O.A., Bechara G.R., Vieiralves R.R., J´unior J.A.D., Assunc¸˜ao H.G., De souza T.A. Laparoscopic treatment of obstrutive uropathy due to retrocaval ureter: literature review and case report. Braz. J. Videoendosc. Surg. 2013;6(4):179–185. [Google Scholar]; O. A. Junior, G. R. Bechara, R. R. Vieiralves, J. A. D. J´unior, H.G. Assunc¸˜ao, and T. A. De souza, “Laparoscopic treatment of obstrutive uropathy due to retrocaval ureter: literature review and case report,” Brazilian Journal of Videoendoscopic Surgery. 2013; 6(4):179–185.
- 53.Ji C., Zhang G., Zhang S., Zhao X., Lian H., Li X. Transperitoneal and retroperitoneal laparoscopic ureteroureterostomy for retrocaval ureter. Zhonghua Wai Ke Za Zhi. 2014;52:580–583. [PubMed] [Google Scholar]; Ji C, Zhang G, Zhang S, Zhao X, Lian H, Li X, et al. Transperitoneal and retroperitoneal laparoscopic ureteroureterostomy for retrocaval ureter. Zhonghua Wai Ke Za Zhi. 2014; 52:580–3. [PubMed]
- 54.Ricciardulli S., Ding Q., Zhang X., Li H., Spagni M. Retroperitoneal laparoscopic approach for retrocaval ureter: our experience on 27 cases. J. Urol. Res. 2015;2(4):1033. [Google Scholar]; S. Ricciardulli, Q. Ding, X. Zhang, H. Li, M. Spagni et al.“Retroperitoneal laparoscopic approach for retrocaval ureter: our experience on 27 cases,” Journal of Urology and Research. 2015; 2(4):1033.
- 55.El Harrech Y., Ghoundale O., Kasmaoui E.H., Touiti D. Transperitoneal laparoscopic pyelopyelostomy for retrocaval ureter without excision of the retrocaval segment: experience on three cases. Adv. Urol. 2016;2016 doi: 10.1155/2016/5709134. [DOI] [PMC free article] [PubMed] [Google Scholar]; El Harrech Y, Ghoundale O, Kasmaoui EH, Touiti D. Transperitoneal laparoscopic pyelopyelostomy for retrocaval ureter without excision of the retrocaval segment: Experience on three cases. Adv Urol. 2016; 2016:5709134. [DOI] [PMC free article] [PubMed]
- 56.Fidalgo N., Pinheiro H., Ferronha F., Morales J., Campos Pinheiro L. Minimally invasive approach of a retrocaval ureter. Case Rep. Urol. 2016;2016 doi: 10.1155/2016/3591832. [DOI] [PMC free article] [PubMed] [Google Scholar]; Fidalgo N, Pinheiro H, Ferronha F, Morales J, Campos Pinheiro L. Minimally invasive approach of a retrocaval ureter. Case Rep Urol. 2016; 2016:3591832. [DOI] [PMC free article] [PubMed]
- 57.Mao Lijun, Xu Kai, Ding Meng, Pan Jun, Guo Zhicheng. Comparison of the efficacy and safety of retroperitoneal laparoscopic and open surgery for the correction of retrocaval ureter. Ther. Clin. Risk Manag. 2017;13:697–701. doi: 10.2147/TCRM.S139113. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lijun Mao, Kai Xu, Meng Ding, Jun Pan, Zhicheng Guo. Comparison of the efficacy and safety of retroperitoneal laparoscopic and open surgery for the correction of retrocaval ureter. Therapeutics and Clinical Risk Management.2017; 13:697–701 [DOI] [PMC free article] [PubMed]
- 58.Bagheri Fariborz, Pusztai Csaba, Szántó Árpád. Laparoscopic repair of circumcaval ureter: one-year follow-up of three patients and literature review. Urology. 2009;74:148–153. doi: 10.1016/j.urology.2009.02.048. [DOI] [PubMed] [Google Scholar]; Fariborz Bagheri, Csaba Pusztai, Árpád Szántó, et al. Laparoscopic Repair of Circumcaval Ureter: One-year Follow-up of Three Patients and Literature Review. UROLOGY.2009; 74: 148 –153. [DOI] [PubMed]