Abstract
Patellar dislocation is a major orthopaedic concern in pediatric and adult populations, with both conservative and surgical options available. Several surgical techniques of the combined or isolated reconstruction of the medial patellofemoral ligament are described in the literature using different grafts, locations, and types of fixations, providing different advantages and disadvantages. New recent developments in cadaveric dissection studies have unveiled the importance of structures that were neglected until recently, such as the medial quadriceps tendon–femoral ligament, which provides a connection between the medial femur and the quadriceps tendon component of the knee extensor mechanism. Hence, we present a surgical technique with combined reconstruction of the medial patellofemoral ligament and medial quadriceps tendon–femoral ligament without the use of hardware and with no need for patellar or femoral drilling (no physis compromise or risk of patellar fracture), which can be used concomitantly with other bony procedures.
Patellar dislocation, most often seen in young and active patients, typically disrupts the proximal medial patellofemoral complex (MPFC)1 and its 2 components, the medial patellofemoral ligament (MPFL) and the medial quadriceps tendon–femoral ligament (MQTFL). Insufficiency of the MPFC may lead to patellar maltracking and increase patellofemoral contact pressure, which will typically cause aberrant focal loads and cartilage degeneration.2 MPFL reconstruction in isolation provides good clinical and radiological results with variable rates of recurrent instability.3, 4 More recently, the roles of medial soft tissue restraints other than the MPFL have been highlighted. The MQTFL, medial patellomeniscal ligament, and medial patellotibial ligament have distinct yet closely related functions that contribute to medial patella support along with the MPFL.5, 6, 7
The MQTFL is attached to the quadriceps tendon via proximal fibers of the MPFC (Fig 1),8 thereby lending substantial support to the medial patella along with the MPFL.6 Within this line, new reconstruction techniques have emerged that use the isolated or combined reconstruction of the different knee medial ligamentous structures9 and specifically use the MQTFL.10 In light of these recent developments, we present a surgical technique for reconstruction of the both MPFL and MQTFL for patellar instability to provide a more anatomical, less invasive, and safer reconstruction for both skeletally immature and mature patients (Video 1).
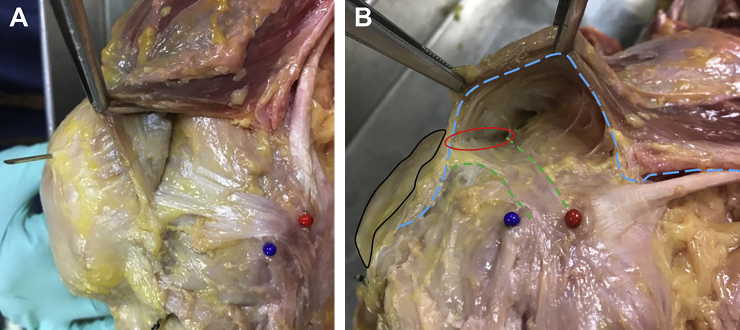
Fig 1.
Cadaveric illustration, right knee. Anatomical dissection of the medial patellofemoral ligament and the medial quadriceps tendon–femoral ligament, where it is possible to clearly identify fibers extending into the quadriceps tendon (above the patella) and vastus medialis obliquus aspect. (A) Medial patellofemoral ligament fibers extending into quadriceps tendon (intermedia) above the patella and inferior of the medial patella femoral complex fibers attach to medialis tendon, not the patella. (B) Medial quadriceps tendon–femoral ligament fibers extending and connecting with vastus medialis obliquus undersurface fascia.
Surgical Technique
Preoperative Planning and Patient Setup
The surgical decision is made after a careful imaging evaluation of the patellofemoral joint (computed tomography, magnetic resonance imaging, and radiography exams) in conjunction with physical examination and clinical history suggestive of patellar instability. The choice of anesthesia is made in conjunction with the patient, the anesthesiologist, and the surgeon, taking into account the different factors influencing the preferred anesthesia technique such as the patient comorbid medical problems.
The patient is positioned supine with (or without) the tourniquet at the proximal thigh, and the limb is disinfected (Table 1). Using a marker key, skin anatomical landmarks are drawn on the medial border of the patella, hamstrings insertion, and medial epicondyle of the femur (Fig 2).
Table 1.
Surgical Procedure Key Points
| Position patient supine with the tourniquet at the proximal thigh. |
| Correct identification of surgical landmarks on the skin. |
| Careful harvesting of the gracilis and semitendinosus tendons and subsequent cleaning and preparation by suturing both extremities. |
| Identification of the adductor magnus tendon and careful dissection until its insertion. |
| Correct placement of the incisions in the quadriceps tendon and 1 cm medial to the border of the patella. |
| Kocher's forceps are passed through the 2 medial patellar incisions and 1 of the quadriceps tendon incisions in the direction of the adductor magnus tendon insertion within the subvastus space in the second layer. |
| The grafts extremities (looped around the adductor magnus tendon) are pulled 1 at a time—the gracilis tendon in the direction of 1 of the incisions made in the quadriceps tendon and the semitendinosus in the direction of the 2 incisions made in the medial retinaculum of the patella. |
| The gracilis graft extremities are pulled through the quadriceps tendon incisions and then crossed and sutured to their own substance and quadriceps tendon, under proper tension with the knee in extension. |
| The semitendinosus 2 extremities are also sutured to the adjacent retinaculum and tensioned with the knee at full extension. |
Fig 2.

With the patient supine, skin landmarks are drawn to identify skin incision points (right knee). MBATT, medial border of the anterior tibial tuberosity; ME, medial epicondyle; PMB, patellar medial border.
Harvesting Procedures
Using an oblique incision of 4 cm medial to the anterior tibial tuberosity, the semitendinosus and gracilis tendons are harvested. The tendons are identified and isolated at the pes anserine insertion after careful dissection. The semitendinosus tendon is identified and harvested using a tendon stripper (Fig 3). The same procedural steps are followed for the gracilis tendon harvesting. Both autografts are cleaned and prepared for placement by suturing both ends with a no. 2 Vycril (Ethicon, Somerville, NJ). Make sure that both autografts are at least 22 cm in length (Fig 4).
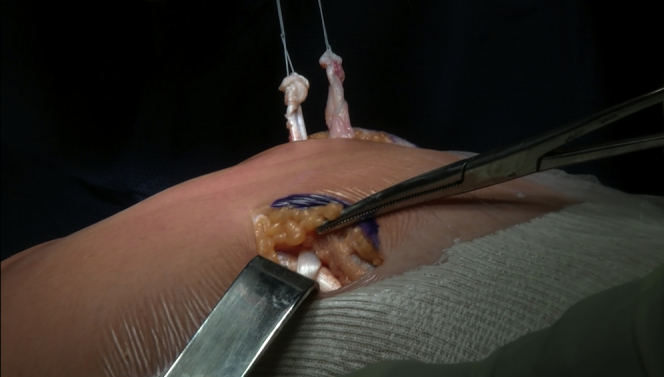
Fig 3.
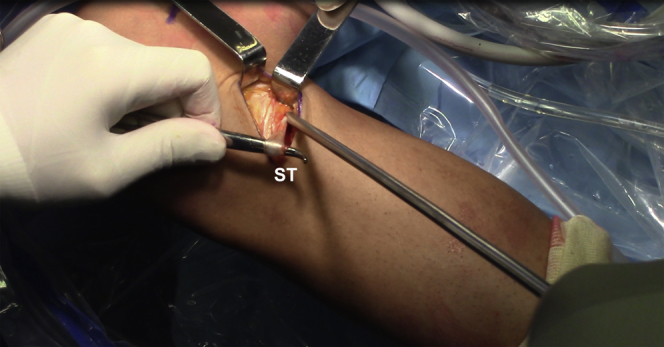
Patient supine, right knee. After careful dissection, the semitendinosus and gracilis tendons are identified and isolated at the pes anserine insertion. Subsequently, harvesting is performed using a tendon stripper. ST, semitendinosus tendon.
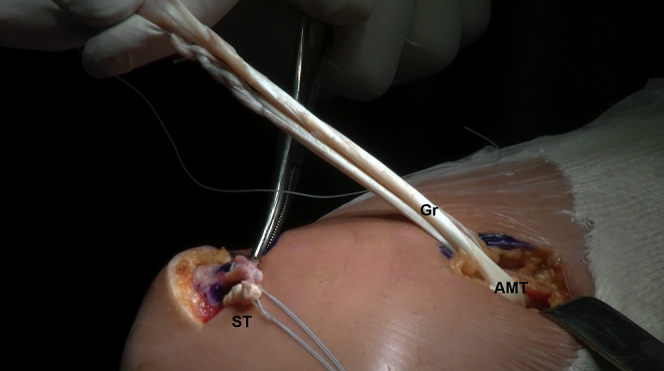
Fig 4.
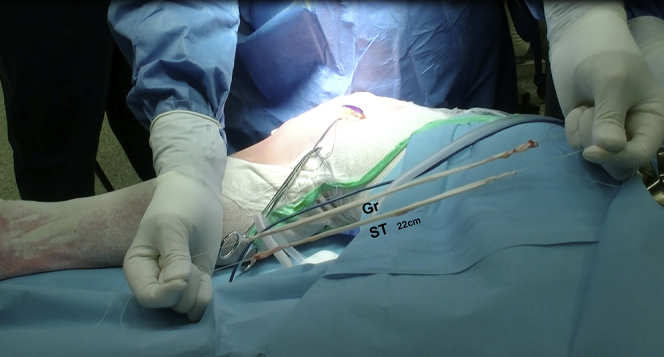
Patient supine, right knee. Both semitendinosus and gracilis autografts of at least 22 cm are cleaned and sutured at both ends. Gr, gracilis tendon; ST, semitendinosus tendon.
Surgical Approach
Before skin incision, palpation of the adductor tubercle and adductor magnus tendon should be performed with the leg in a figure-of-4 position (knee flexed on about 60° and hip flexed and externally rotated). A 3-cm longitudinal incision is made 4 cm proximal to the medial epicondyle and over the adductor tubercle. After careful distal dissection, the vastus medialis and the adductor magnus tendon are identified. It is important to perform the dissection carefully and as distally as possible until the insertion of the adductor magnus tendon insertion because it represents the quasi-anatomical point of the MPFL femoral insertion (Table 2).11 Caution must be taken to not disinsert the adductor magnus tendon of the adductor tubercle as it will serve as pulley. A surgical string is then looped around the adductor magnus tendon insertion site to serve as reference for the later passage of the autografts (Fig 5).
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Correct identification of the adductor tubercle is important to perform the correct skin incision. | Overtensioning the graft can cause loss of range of motion and patellofemoral arthrosis, leading to residual pain. |
| Careful dissection of the insertion of the adductor magnus tendon to avoid proximal graft placement and consequently a nonanatomic insertion of the medial patellofemoral ligament. | Not recognizing other anatomical predisposal factors for patellar instability may lead to potential failure. |
| When performing the harvesting of the semitendinosus and gracilis tendons, care must be taken to avoid stripping the tendons. A tendon length of 22 cm is needed for reconstruction. | |
| Placing the surgical string loop around the adductor magnus tendon insertion site will help in the later passage of the autografts | |
| Appropriate tension is required in the patella and quadriceps tendon during the suture of the grafts to avoid loosening or overtension. |
Fig 5.
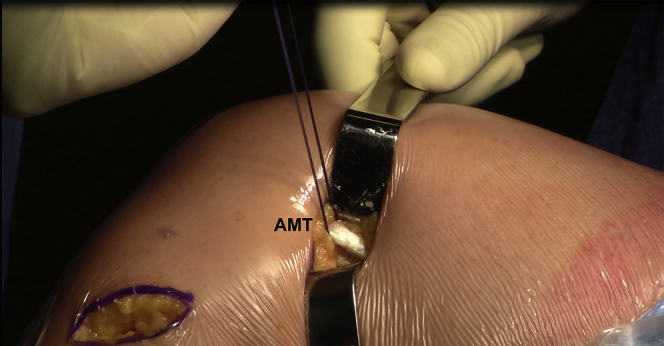
Patient supine, right knee. Surgical reference is looped around the adductor magnus tendon. AMT, adductor magnus tendon.
The next step is to perform a 5-cm longitudinal incision on the medial aspect of the patella with careful dissection of the medial insertion of the quadriceps tendon and medial retinaculum of the patella. Landmarks are drawn to identify the correct placement of both autografts. Three incisions are then made on the previously drawn landmarks: 1 at the quadriceps tendon substance, close to the vastus medialis obliquus, and the other 2 on the medial retinaculum 1 cm away from the medial aspect of the patella, with superior and inferior insertion of the MPFL (Fig 6). Kocher's forceps are passed through these small incisions, in the subvastus space (layer 2) in the direction of the adductor magnus tendon insertion. Care is taken to not damage the capsule or violate the intra-articular space. In the quadriceps tendon, just 1 of the incisions is used to pass the Kocher's forceps (Fig 7).
Fig 6.
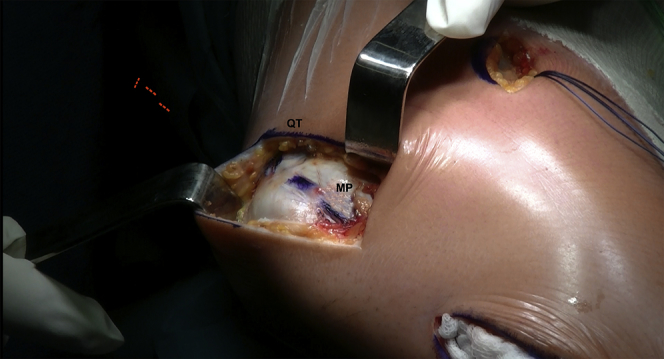
Patient supine, right knee. Two incisions are made at the medial aspect of the patella and 1 at the quadriceps tendon. MP, medial patella; QT, quadriceps tendon.
Fig 7.
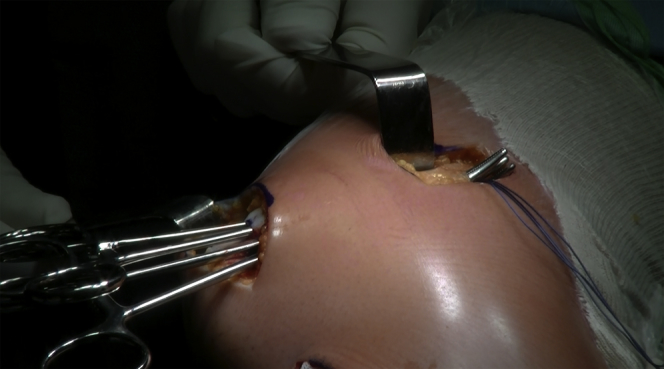
Patient supine, right knee. Kocher's forceps are passed through the 2 medial patellar incisions and another at the quadriceps tendon incision in the direction of the adductor magnus tendon insertion within the subvastus space in the second layer.
The semitendinosus graft is looped around the adductor magnus tendon as distally as possible (Fig 8), and both extremities are pulled through layer 2, in the direction of the patella, and passed within the first 2 incisions in the medial retinaculum (Fig 9). Then the gracilis graft is also looped around the adductor magnus tendon (Fig 10), and both extremities are pulled in the direction to the quadriceps tendon through the previously made incisions (Fig 11).
Fig 8.
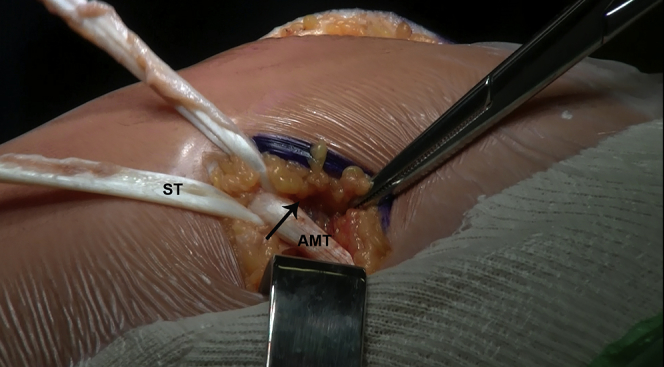
Patient supine, right knee. The semitendinosus autograft is looped around the adductor tendon. The arrow indicates the graft passage. AMT, adductor magnus tendon; ST, semitendinosus.
Fig 9.
Patient supine, right knee. The semitendinosus autograft is passed through the 2 incisions made in the medial aspect of the patella.
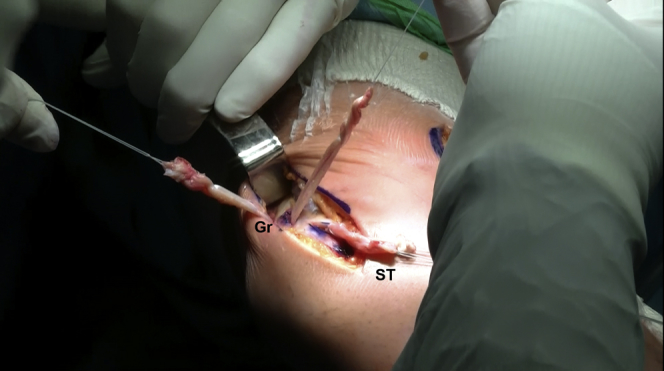
Fig 10.
Patient supine, right knee. The gracilis autograft is also looped around the adductor tendon. AMT, adductor magnus tendon; Gr, gracilis tendon; ST, semitendinosus tendon.
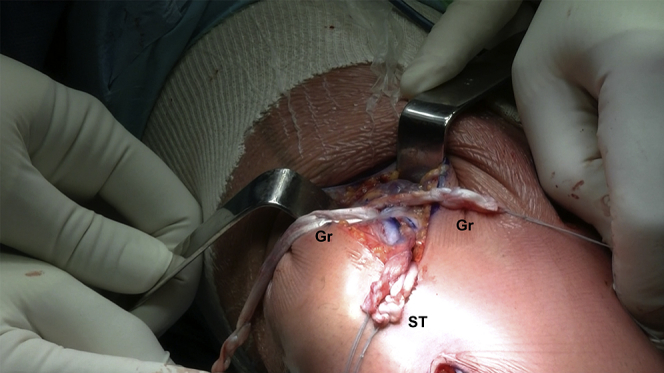
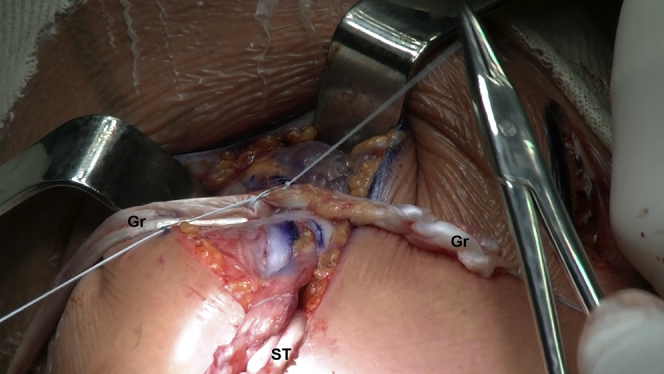
Fig 11.
Patient supine, right knee. The gracilis autograft extremities are pulled into the quadriceps tendon incision. Gr, gracilis tendon; ST, semitendinosus tendon.
The 2 extremities of the gracilis graft are crossed on each other (Fig 12) and sutured to their own substance (Fig 13) and to the quadriceps tendon (Fig 14) with a 2-0 FiberWire (Arthrex, Naples, FL) while applying proper tensioning in the patella with the knee in extension. The graft tips are resected. Then the 2 arms of the semitendinosus graft that have been passed by the 2 medial patellar incisions are sutured to the adjacent retinaculum with 2-0 FiberWire (Fig 15), while applying proper tensioning with the knee in full extension. A total of 25% of lateral patellar displacement is allowed. The remaining graft tips are cut off, and the final revision of the procedure is made (Fig 16). Patellofemoral examination is performed to confirm optimum tension. Subcutaneous Vicryl sutures and staples are used for skin closure.
Fig 12.
Patient supine, right knee. The 2 arms of the gracilis autografts are crossed on each other. Gr, gracilis tendon; ST, semitendinosus tendon.
Fig 13.
Patient supine, right knee. The 2 crossed arms of the gracilis autografts are sutured to their own substance under proper tension. Gr, gracilis tendon; ST, semitendinosus tendon.
Fig 14.
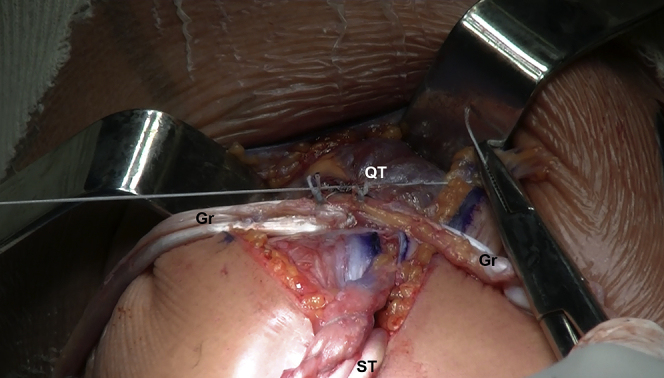
Patient supine, right knee. After it is sutured to its own substance, the gracilis autograft suture is reinforced by suturing to the quadriceps tendon. Gr, gracilis tendon; QT, quadriceps tendon; ST, semitendinosus tendon.
Fig 15.
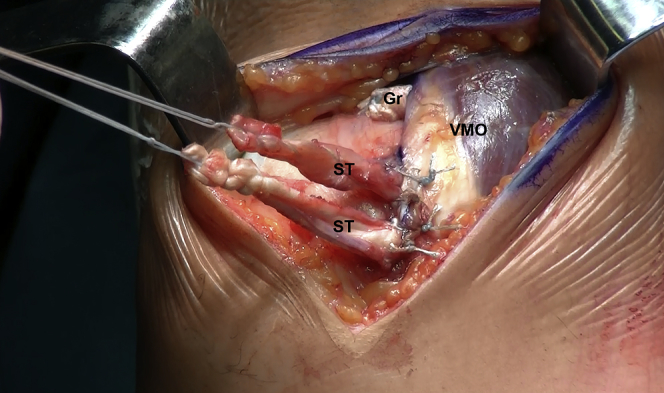
Patient supine, right knee. The 2 arms of the semitendinosus autograft that have been previously passed through the 2 incisions placed just medial to the patella are now sutured to the adjacent retinaculum with the knee at full extension. Gr, gracilis tendon; ST, semitendinosus tendon; VMO, vastus medialis obliquus.
Fig 16.
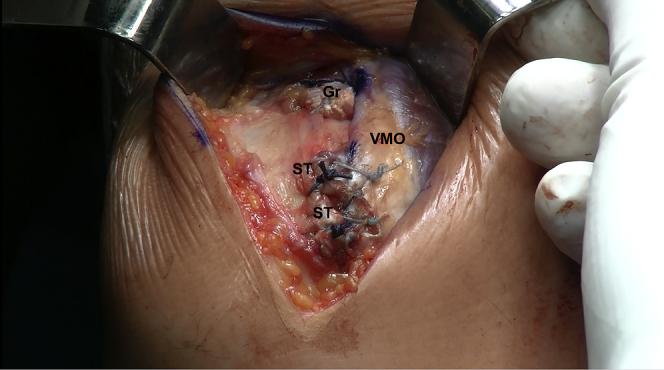
Patient supine, right knee. Revision of all sutures have been placed correctly. Gr, gracilis tendon; ST, semitendinosus tendon; VMO, vastus medialis obliquus.
Postoperative Rehabilitation
The patient is allowed to immediately start active flexion of the knee. However, during the first 4 weeks flexion is limited to 90°. Partial weight bearing is maintained during the initial 6 weeks. After 6 weeks, range of motion is increased as tolerated and full weight bearing is gradually permitted. Rehabilitation is focused on restoring full knee range of motion, patellar mobilization, preoperative quadriceps muscle activation and strength, effusion control, and pain management. Return to sport is restricted to a minimum of 4 months and only allowed when isokinetic and functional testing are 90% of the contralateral lower limb.
Discussion
Several techniques for the treatment of patellar instability have been developed over the years, and multiple options are described in the literature.3, 9 The most commonly used autografts are the gracilis or semitendinosus tendon autografts, frequently using an interference screw for femoral fixation and bone tunnels for patellar fixation.3 The traditional “1-arm” fixation to the patella has been the current standard, although the “2-arm” fixation method has gained ground due to a more anatomical reconstruction and potentially provides improved outcomes compared with the single-bundle MPFL reconstructions.9 The use of the adductor magnus tendon insertion as a quasi-anatomical point of the MPFL insertion has shown isometry from 0° to 90° of knee flexion, providing biomechanical behavior similar to bony femoral insertion of the MPFL.11 The distance from the femoral insertion of the MPFL to the adductor tubercle is less variable than the distance to the medial femoral epicondyle,12 which makes the adductor tubercle often used for femoral fixation in MPFL reconstructions. Moreover, radiographic identification of Schöttle points does not guarantee the precise anatomic location of the femoral fixation site.13 Besides providing a stronger fixation (bony attachment), placing the femoral fixation more proximally at the adductor magnus tendon will increase the distances between the femoral and patellar attachments points during knee flexion and augment the tension to the patella.14 Using the adductor tubercle for femoral fixation has been shown to not change the patellofemoral joint contact area and pressure.15 Similarly, using the adductor magnus tendon as a pulley for femoral fixation has been previously described16 and does not lead to clinical signs of patellofemoral overload or radiographic osteoarthritis, and the quasi-isometric behavior produced may prevent overconstraining of the patellofemoral joint.16
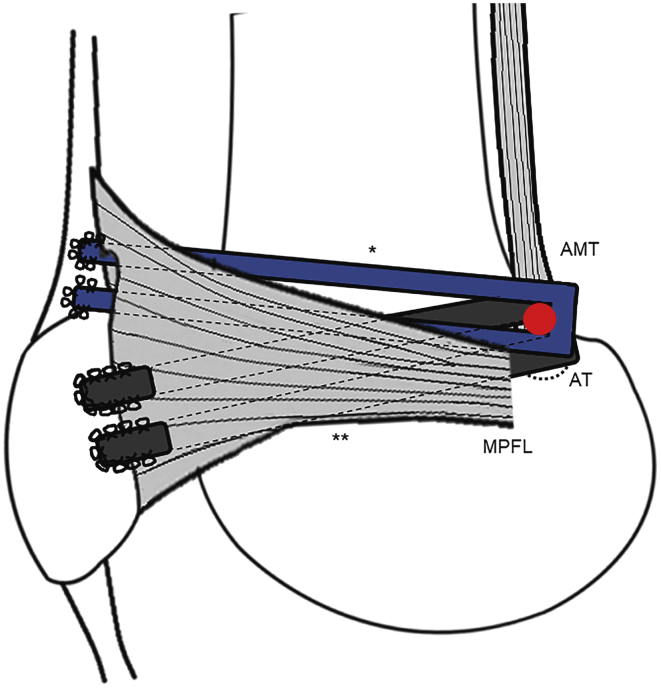
This technique uses a 2-arm all soft tissue reconstruction (Fig 17), decreasing the risk of overtensioning, patellofemoral pain, and degenerative changes. The overtension can be compensated by the mobility of the medial retinaculum and adductor magnus tendon. Since no drilling, anchors, or screws are used, there is no risk of patellar fracture, articular cartilage damage, or physis compromise in skeletally immature cases (Table 3). Moreover, this technique simplifies revision procedures in case of failure as it does not use tunnels or hardware. Despite the changes to the traditional MPFL reconstruction technique, the associated distal realignment bony procedures can still be performed concomitantly. Another important advantage is that it is not necessary to use concomitant radiological procedures, eliminating the exposure to radiation for the surgical staff and the patient.
Fig 17.
Two-arm fixation of the semitendinosus and gracilis autografts and the quasi-anatomical point of the MPFL insertion. AMT, adductor magnus tendon; AT, adductor tubercle; MPFL, medial patellofemoral ligament. ∗Under medial retinaculum. ∗∗Under medial retinaculum via vastus medialis obliquus.
Table 3.
Advantages, Risks, and Limitations of the Presented Technique
| Advantages | Risks and Limitations |
|---|---|
| Allows the reconstruction of both the medial patellofemoral ligament and medial quadriceps tendon–femoral ligament. | Inherent residual pain resulting from harvesting the semitendinosus and gracilis tendons. |
| Reduced risk of overtensioning, patellofemoral pain, and degenerative changes because of the soft tissue attachments. | Improper identification of the subvastus space in the second layer can lead to capsule lesion and an inadequate graft position. |
| Can be used with open physis. | Soft tissue fixation is biomechanically weaker than the traditional bone fixation. |
| No use of anchors or screws for fixation (less cost). | Improper adductor magnus tendon dissection can lead to a nonanatomical graft placement as wekk as to a iatrogenic tendon rupture. |
| No risk of patellar iatrogenic fracture (no patella or femoral drilling). | Improper graft tensioning may lead to postoperative complications and recurrent instability (surgeon experience and “sensibility”). |
| More reliable for femoral fixation insertion than the radiographic Schöttle point. | |
| No radiation exposure for either the surgical staff or the patient. | |
| Can be used concomitantly with other bony procedures (e.g. trochleoplasty or anterior tibial tuberosity realignment). | |
| Simplifies revision procedures as it does not use tunnels or hardware. |
A potential limitation of this technique is related to the graft tensioning, which is influenced by the surgeons' experience and “sensibility.” Thus, it crucial to not apply too much tension to avoid overtensioning the grafts and consequently overload the medial patellar facet, leading to pain and degenerative changes. An important step is the careful dissection of the adductor magnus tendon insertion to avoid residual pain. Nevertheless, residual pain from gracilis and semitendinosus tendon harvesting is a potential complication. The use of soft tissue suture fixation rather than the traditional tunnels or suture anchor fixation is prone to fail with lower loads. Nonetheless, there are no statistically or clinically significant differences in functional outcomes over time.17
In conclusion, we present an alternative technique combining the reconstruction of the MPFL and MQTFL using soft tissue fixation, avoiding the inherent risks of drilling and screw fixation. It is a simple and effective technique, with reduced associated hardware costs, and can more closely recreate the medial patellofemoral complex.
Acknowledgments
The authors thank André Silva for his valuable help with the construction and management of the video and figures.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for combined reconstruction of the medial patellofemoral ligament and medial quadriceps tendon–femoral ligament. The patient is placed supine with the tourniquet at the proximal right thigh. Skin landmarks are made at the medial border of the patella, medial border of the anterior tibial tuberosity, and medial epicondyle of the femur. The gracilis and semitendinosus tendons are carefully dissected and prepared by cleaning and suturing both ends. The adductor magnus tendon insertion is identified, and careful dissection is done until its insertion. Incisions are made, 2 at the quadriceps tendon substance, close to the vastus medialis obliquus, and the other 2 are made 1 cm to the medial border of the patella. Kocher's forceps are passed through the 2 medial patellar incisions and 1 of the quadriceps tendon incisions in the direction of the adductor magnus tendon insertion within the subvastus space in the second layer. Both autografts looped around the adductor magnus tendon are pulled 1 at a time. The gracilis extremities are pulled in the direction of the quadriceps tendon incisions. The semitendinosus is pulled to the 2 incisions made in the medial aspect of the patella. The gracilis graft extremities are crossed and sutured to the quadriceps tendon substance and to each other. This is done with proper tension and the knee in extension. The 2 semitendinosus arms are also sutured to the adjacent retinaculum. Tension is placed with the knee at full extension.
References
- 1.Tanaka M.J., Voss A., Fulkerson J.P. The anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Joint Surg Am. 2016;98:1199–1205. doi: 10.2106/JBJS.15.01182. [DOI] [PubMed] [Google Scholar]
- 2.Stephen J.M., Kader D., Lumpaopong P., Deehan D.J., Amis A.A. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res. 2013;31:1423–1429. doi: 10.1002/jor.22371. [DOI] [PubMed] [Google Scholar]
- 3.McNeilan R.J., Everhart J.S., Mescher P.K., Abouljoud M., Magnussen R.A., Flanigan D.C. Graft choice in isolated medial patellofemoral ligament reconstruction: A systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic pptions. Arthroscopy. 2017;34:1340–1354. doi: 10.1016/j.arthro.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 4.Schneider D.K., Grawe B., Magnussen R.A. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: A systematic review and meta-analysis. Am J Sports Med. 2016;44:2993–3005. doi: 10.1177/0363546515624673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaPrade M.D., Kallenbach S.L., Aman Z.S. Biomechanical evaluation of the medial stabilizers of the patella. Am J Sports Med. 2018;46:1575–1582. doi: 10.1177/0363546518758654. [DOI] [PubMed] [Google Scholar]
- 6.Kruckeberg B.M., Chahla J., Moatshe G. Quantitative and qualitative analysis of the medial patellar ligaments: An anatomic and radiographic study. Am J Sports Med. 2018;46:153–162. doi: 10.1177/0363546517729818. [DOI] [PubMed] [Google Scholar]
- 7.Hinckel B.B., Gobbi R.G., Demange M.K. Medial patellofemoral ligament, medial patellotibial ligament, and medial patellomeniscal ligament: Anatomic, histologic, radiographic, and biomechanical study. Arthroscopy. 2017;33:1862–1873. doi: 10.1016/j.arthro.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 8.Mochizuki T., Nimura A., Tateishi T., Yamaguchi K., Muneta T., Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21:305–310. doi: 10.1007/s00167-012-1993-7. [DOI] [PubMed] [Google Scholar]
- 9.Baumann C.A., Pratte E.L., Sherman S.L., Arendt E.A., Hinckel B.B. Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26:2920–2933. doi: 10.1007/s00167-018-4833-6. [DOI] [PubMed] [Google Scholar]
- 10.Fulkerson J.P., Edgar C. Medial quadriceps tendon–femoral ligament: Surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;2:e125–e128. doi: 10.1016/j.eats.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pérez-Prieto D., Capurro B., Gelber P.E. The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2017;25:2420–2423. doi: 10.1007/s00167-015-3865-4. [DOI] [PubMed] [Google Scholar]
- 12.Viste A., Chatelet F., Desmarchelier R., Fessy M.-H. Anatomical study of the medial patello-femoral ligament: Landmarks for its surgical reconstruction. Surg Radiol Anat. 2014;36:733–739. doi: 10.1007/s00276-014-1270-1. [DOI] [PubMed] [Google Scholar]
- 13.Sanchis-Alfonso V., Ramírez-Fuentes C., Montesinos-Berry E., Elía I., Martí-Bonmatí L. Radiographic location does not ensure a precise anatomic location of the femoral fixation site in medial patellofemoral ligament reconstruction. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117739252. 2325967117739252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monllau J.C., Erquicia J.I., Ibañez M. Reconstruction of the medial patellofemoral ligament. Arthrosc Tech. 2017;6:e1471–e1476. doi: 10.1016/j.eats.2017.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melegari T.M., Parks B.G., Matthews L.S. Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. Am J Sports Med. 2008;36:747–752. doi: 10.1177/0363546508314410. [DOI] [PubMed] [Google Scholar]
- 16.Monllau J.C., Masferrer-Pino À., Ginovart G., Pérez-Prieto D., Gelber P.E., Sanchis-Alfonso V. Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25:2453–2459. doi: 10.1007/s00167-015-3934-8. [DOI] [PubMed] [Google Scholar]
- 17.Stupay K.L., Swart E., Stein B.E.S. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: A systematic review. Arthroscopy. 2015;31:1372–1380. doi: 10.1016/j.arthro.2014.12.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for combined reconstruction of the medial patellofemoral ligament and medial quadriceps tendon–femoral ligament. The patient is placed supine with the tourniquet at the proximal right thigh. Skin landmarks are made at the medial border of the patella, medial border of the anterior tibial tuberosity, and medial epicondyle of the femur. The gracilis and semitendinosus tendons are carefully dissected and prepared by cleaning and suturing both ends. The adductor magnus tendon insertion is identified, and careful dissection is done until its insertion. Incisions are made, 2 at the quadriceps tendon substance, close to the vastus medialis obliquus, and the other 2 are made 1 cm to the medial border of the patella. Kocher's forceps are passed through the 2 medial patellar incisions and 1 of the quadriceps tendon incisions in the direction of the adductor magnus tendon insertion within the subvastus space in the second layer. Both autografts looped around the adductor magnus tendon are pulled 1 at a time. The gracilis extremities are pulled in the direction of the quadriceps tendon incisions. The semitendinosus is pulled to the 2 incisions made in the medial aspect of the patella. The gracilis graft extremities are crossed and sutured to the quadriceps tendon substance and to each other. This is done with proper tension and the knee in extension. The 2 semitendinosus arms are also sutured to the adjacent retinaculum. Tension is placed with the knee at full extension.