Abstract
To date, there is no consensus concerning the treatment of acute Achilles tendon ruptures. Although surgical treatment decreases the risk of a recurrent rupture, it is not without complications. In particular, percutaneous sutures may cause a lesion of the sural nerve. The purpose of this Technical Note is to describe a reliable and reproducible surgical procedure for treating these lesions. The first operative phase consists of an ultrasound detection that makes it possible to identify the tendon extremities and the sural nerve, which is necessary to secure the posterolateral arthroscopic tract as well as to perform the percutaneous suture. The entry point is thus centered on the lesion and placed at a distance from any surrounding nerve risk. The second arthroscopic phase makes it possible to release the tendon lesion, control the transtendon passage of the surgical threads, and evaluate the dynamic contact of the tendon edges. At the end of the intervention, the complete disappearance from the transillumination via the rupture also makes it possible to ensure the disappearance of the tendon gap. Achilles tendon percutaneous sutures after the ultrasound detection and under arthroscopic control thus makes it possible to control the contact of the tendon edges, while at the same time decreasing the risk of a lesion of the sural nerve, with minimal scarring.
There is no consensus concerning the treatment of acute Achilles tendon ruptures. Percutaneous sutures represent an interesting surgical alternative in view of reducing the rate of scarring complications observed.1, 2 However, this presents an increased risk of a lesion of the sural nerve1 as well as of a recurrent rupture compared with open surgery.2
The purpose of this Technical Note is to describe a reliable and reproducible percutaneous surgical procedure, after ultrasound detection and under endoscopic control. The first operative phase consists of identifying the sural nerve via ultrasound detection, with the goal of securing the arthroscopic tracts and the percutaneous suture. Endoscopic control makes it possible to control the transtendon passage of the surgical threads, as well as the closing together and contact of the tendon edges. A summary of key steps is provided in Table 1, whereas a summary of the technique is provided in Video 1.
Table 1.
Key Steps for Ultrasonography and Endoscopy-Assisted Percutaneous Achilles Tendon Repair
| Coronal ultrasonographic views for drawing the sural nerve path. Sagittal views to identify the tendons ends. |
| Vertical incision for posteromedial and posterolateral endoscopic portals in front of the tendon tear. |
| Arthroscopic debridement of the tendon ends. |
| Posteromedial portal to insert the percutaneous suture needle. |
| Endoscopic control of the needle positioning through the tendon ends (proximal tendon end and distal end). |
| Ma and Griffith's method (X or U knot). |
| Gap reduction by pulling between ends (maintain the ankle in a maximal plantar flexion). |
| Transillumination sign loss (control the contact between the tendon ends). |
| Pulling and locking the suture. |
| Cast at 30° plantar flexion. |
Surgical Technique
Positioning the Patient
The patient is place in a prone position. The lower limbs surpass the operating table to facilitate tibiotalar mobilization as well as mobilization of the positioner under the tibial crests just above the ankle (Fig. 1). This intervention can be carried out with or without a pneumatic tourniquet, which in this case is positioned on the thigh. Locoregional anesthesia, with a popliteal anesthetic block or femoral and popliteal bi-block, ensures the patient's comfort during the procedure.
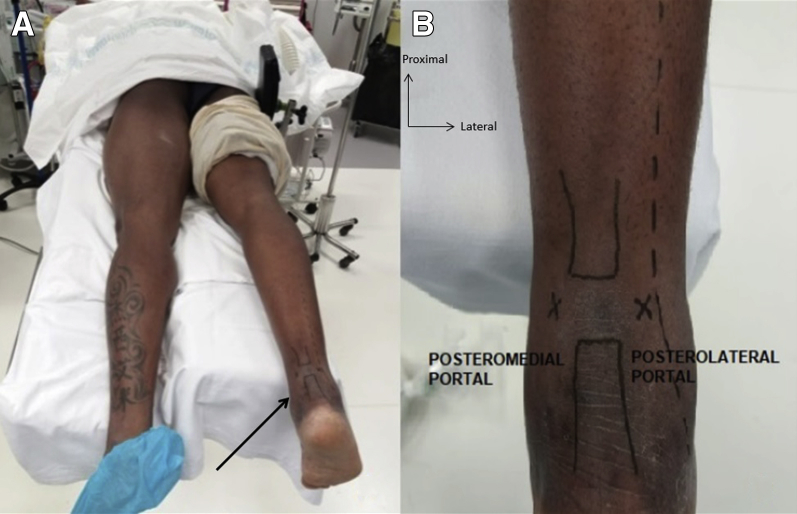
Fig 1.
(A) Patient in prone position, right foot (arrow) beyond the table to mobilize the ankle joint, with a tourniquet on the operated limb. (B) Drawing of the endoscopic portals and the trajectory of the sural nerve (lateral side to the posterolateral endoscopic portal).
Ultrasound Detection
The first phase consists of an ultrasound detection (Fig. 2). The longitudinal cuts make it possible to identify the proximal and distal tendon edges, which are then outlined. The sural nerve is then identified and outlined in turn by using coronal cuts, which make it possible to monitor it from its emergence halfway up the leg to the external retromalleolar. Once all of these elements are marked with a dermographic pencil, the posterolateral arthroscopic tract (“soft point”) is centered on the rupture area and the percutaneous suture entry and exit points are at a distance from any risk of an iatrogenic lesion of the sural nerve.
Fig 2.
(A) Ultrasonographic method to identify the acute Achilles tendon rupture on a right ankle. (B) Longitudinal view for tendon ends identification. (C) Coronal view for the sural nerve.
Arthroscopic Release
The placement of the arthroscope with a diameter of 2.7 mm is done via infracentimetric posterolateral tract after the tissue incision of the work chamber with the Halstead forceps. The gap between the 2 tendon edges is identified via transillumination. The opposite posteromedial instrumental tract is also supported via transillumination. With the help of dorsal and plantar flexion movements, we identify the proximal and distal tendon edges (Fig. 3). The release of these extremities is carried out progressively at a minimum with the motorized knife (shaver), while taking care not to damage the peritendon. The arthroscope then remains in place for the percutaneous suture during the entire procedure to control the transtendon passage of the surgical threads and the quality of the reduction.
Fig 3.
Posterolateral and mediolateral portals for endoscopic debridement (A) of the distal tendon end (B) and the proximal tendon end (C).
Percutaneous Sutures
The percutaneous suture technique used is the one described by Ma and Griffith.3 The braided suture thread (Vicryl no. 2) is doubled and passed through the curved metal needle (Suturach, FH Orthopedics, Heimsbrunn, France). The entry point is medial, centered on the rupture area, in the direction of the proximal tendon stump. Each longitudinal transtendon passage of the surgical thread is controlled under endoscopy via the rupture area.
The suture is in the shape of an X, as shown in Figure 4. The last exit point comes back directly onto the initial entry point. The surgical threads are then tightened while keeping the foot in equinus (Fig. 5). The closing together and the contact of the tendon edges are controlled under arthroscopy. The initial transillumination signal disappears, and the tendon continuity is palpable. Suture points are carried out on the posteromedial and posterolateral arthroscopic tracts (Monocryl 3/0). The operative support maintains the plantar flexion until the fashioning of a fiberglass boot in equinus.
Fig 4.
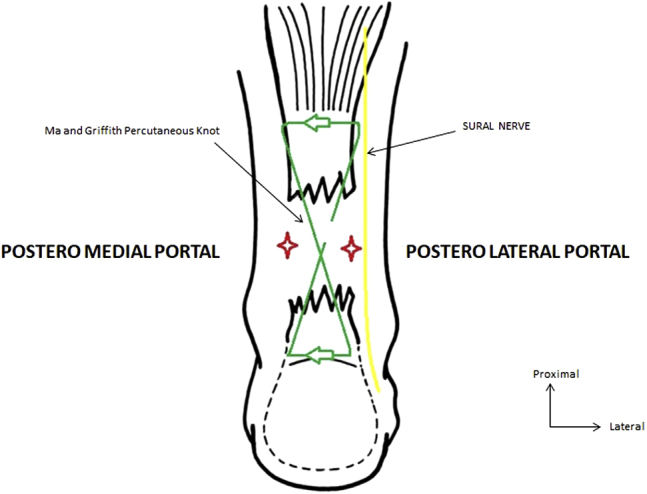
Ma and Griffith's percutaneous suture method with endoscopic portals and sural nerve identification (yellow line) on a right ankle.
Fig 5.
Endoscopic-controlled percutaneous (A) suture with a percutaneous needle (arrow) through the proximal tendon end (B) to the distal tendon end with a X-shaped suture (C).
Postsurgical Protocol
The circular fiberglass boot positioned in equinus at 30° is kept on for a month (Fig. 6). Immobilization is then modified in favor of a walking boot whose range will be reduced every 2 weeks (30°, 15°, then 0°). During the sixth week, physiotherapy and passive rehabilitation begin, and the walking boot is kept on for an additional 4 weeks. The foot is allowed to touch the ground during the third week, while using the walking boot. Preventive anticoagulation is prescribed until the foot is able to touch the ground completely. A summary of postoperative rehabilitation protocol is provided in Table 2.
Fig 6.
Final posterolateral and mediolateral portals scars (A) and immobilization with a cast at 30° of flexion (B).
Table 2.
Postoperative Rehabilitation Protocol
| Time | Therapy |
|---|---|
| Weeks 1-4 | Non–weight bearing (cast at 30° plantar flexion). |
| Weeks 4-10 | Walking boot at 30° plantar flexion. Removal of 15° per 2 weeks to obtain neutral position at week 8. Physiotherapy and passive rehabilitation at week 6. |
| Week 11 | Functional and progressive proprioceptive physical therapy. |
| Week 16 | Limited activities with pain as a guide (swimming, hiking, biking). |
| Month 6 | Return to the preinjury level of activities (competition). |
Discussion
In the literature, percutaneous sutures are criticized for 2 reasons: the postsurgical reduction in the muscle strength of the sural triceps as well as the high rate of recurrent ruptures compared with open surgery.1 Indeed, blind percutaneous sutures do not make it possible to ensure the quality of the contact of the tendon stumps.4, 5 Actually, the major advantages of endoscopy-assisted percutaneous repair are that it allows direct observation of the process of suturing the Achilles tendon and eliminates some of the disadvantages of the percutaneous repair techniques, especially the evaluation of the juxtaposition of the torn ends. In this context, endoscopic control presents a twofold advantage: visualization of the contact of the tendon edges combined with the disappearance of the transillumination signal, as well as the preservation of the peritendon, which makes it possible to optimize scarring.6 Preservation of the peritendon decreases the gliding resistance of the extrasynovial tendons after repetitive motion and increases the biological healing of the Achilles tendon suture. The pearls and pitfalls of the technique are provided in Table 3.
Table 3.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Ultrasonographic localization of the sural nerve to secure endoscopic portals and the percutaneous suture. | Sural nerve identification could be difficult and has a steep learning curve. |
| Endoscopic portals in front of the gap between tendon ends after ultrasonographic localization. | Poor tendon capture by misplacement of the percutaneous needle through the proximal and distal ends. |
| Minimal endoscopic debridement of the tendons ends (avoiding the paratenon to enhance healing). | Contraindicated in case of chronic tear (3 weeks). |
| Endoscopic control of the needle passing through the proximal and distal tendon ends. | |
| Transillumination sign loss after pulling and reducing the gap of the rupture, |
Apart from Thermann7 and Lui8 carrying out an additional superolateral endoscopic tract at the myotendinous junction, no other studies concerning sutures under endoscopic control visualized the sural nerve.6, 9 Let us emphasize that lesions of the sural nerve are primarily due to percutaneous sutures, and choosing a third superolateral arthroscopic tract did not show any significant difference concerning its iatrogenic lesion rate.10 Therefore, we chose ultrasound.
Ultrasound coronal cuts make it possible to detect the sural nerve.11, 12 Furthermore, its sensitive lateral calcaneal branch is nearly impossible to identify via ultrasound. Its route is more medial than the sural nerve itself, with a risk of a significant iatrogenic lesion, regardless of the percutaneous suture technique.13 To date, no publication has addressed the complication rate via the iatrogenic lesions of this sensitive branch. A prospective study concerning the technique described is ongoing, to measure its rate of neurologic complications encountered via the impairment of the sural nerve and, in particular, of its lateral calcaneal branch. In the near future, as Lui10 suggests, a new all-inside suture technique under endoscopic control would make it possible to prevent any iatrogenic peripheral neurologic lesions.
Another interest for endoscopy could be to pair percutaneous sutures with a tendon support, such as the transfer of the flexor hallucis longus14, 15 or an increase in the small plantar tendon.8 An epidemiology study that makes it possible to target patients with recurrent rupture risk factors could prompt the surgeon to perform an associated strengthening or augmenting plastic surgery procedure (e.g. associated preexisting tendonitis, diabetes, iatrogeny).
Achilles tendon percutaneous sutures after ultrasound detection and under arthroscopic control make it possible to control the contact of the tendon edges, to preserve the peritendon, and to identify the route of the sural nerve to optimally secure the suture. The functional outcomes and complication rates of this surgical technique must be the subject of future large-scale prospective work.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The video shows a technique of percutaneous repair of acute Achilles tendon rupture under ultrasonographic and endoscopic assistance. The patient is in the prone position, with a tourniquet on the operated limb, the foot beyond the table to mobilize the ankle joint. Ultrasonography will allow the surgeon to identify the tendon extremities in longitudinal planes, and the sural nerve will be observed on coronal views. Posterolateral and posteromedial endoscopic portals can be drawn, centered on the rupture and keeping distance from the sural nerve. The entry point is posterolateral, and transillumination with the endoscope allows the surgeon appreciate the gap between the ends of the tendon extremities. Transillumination also helps for the posteromedial portal incision. Debridement of the tendons extremities is performed using the shaver, from proximal to distal, being careful not to injure the peritendon. We check the good mobilization of the proximal tendon end with a Kocher forceps. The percutaneous suture is X shaped according to the technique described by Ma and Griffith. The needle is introduced through the distal portion of the tendon, up to the proximal portion, under endoscopic guidance. After a transverse crossing in the proximal portion from medial to lateral with the needle, the longitudinal gap crossing from proximal to distal is controlled under endoscopic vision. We then finish by the transverse crossing in the distal tendon end, which then comes out through the posteromedial portal. While maintaining the ankle in plantar flexion, we tighten and tie the suture until a good reduction of the tendon ends is obtained under endoscopic guidance. At the end of the surgery, the transillumination signal must disappear, as an indirect sign of good reduction of the tendon ends. A cast is then applied to keep the ankle at 30° of flexion.
References
- 1.Yang B., Liu Y., Kan S. Outcomes and complications of percutaneous versus open repair of acute Achilles tendon rupture: A meta-analysis. Int J Surg. 2017;40:178–186. doi: 10.1016/j.ijsu.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Karabinas P.K., Benetos I.S., Lampropoulou-Adamidou K., Romoudis P., Mavrogenis A.F., Vlamis J. Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol. 2014;24:607–613. doi: 10.1007/s00590-013-1350-7. [DOI] [PubMed] [Google Scholar]
- 3.Ma G.W., Griffith T.G. Percutaneous repair of acute closed ruptured achilles tendon: A new technique. Clin Orthop Relat Res. 1977;128:247–255. [PubMed] [Google Scholar]
- 4.Carmont M.R., Maffulli N. Modified percutaneous repair of ruptured Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2008;16:199–203. doi: 10.1007/s00167-007-0411-z. [DOI] [PubMed] [Google Scholar]
- 5.Rebeccato A., Santini S., Salmaso G., Nogarin L. Repair of the achilles tendon rupture: A functional comparison of three surgical techniques. J Foot Ankle Surg. 2001;40:188–194. doi: 10.1016/s1067-2516(01)80018-1. [DOI] [PubMed] [Google Scholar]
- 6.Doral M.N., Bozkurt M., Turhan E. Percutaneous suturing of the ruptured Achilles tendon with endoscopic control. Arch Orthop Trauma Surg. 2009;129:1093–1101. doi: 10.1007/s00402-009-0880-2. [DOI] [PubMed] [Google Scholar]
- 7.Thermann H., Tibesku C.O., Mastrokalos D.S., Pässler H.H. Endoscopically assisted percutaneous achilles tendon suture. Foot Ankle Int. 2001;22:158–160. doi: 10.1177/107110070102200214. [DOI] [PubMed] [Google Scholar]
- 8.Lui T.H. Arthroscopy and endoscopy of the foot and ankle: Indications for new techniques. Arthroscopy. 2007;23:889–902. doi: 10.1016/j.arthro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Fortis A.P., Dimas A., Lamprakis A.A. Repair of achilles tendon rupture under endoscopic control. Arthroscopy. 2008;24:683–688. doi: 10.1016/j.arthro.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Lui T.H. Editorial commentary: Is endoscopy really helpful during repair of acute rupture of the Achilles tendon? Arthroscopy. 2018;34:1270–1271. doi: 10.1016/j.arthro.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 11.Lacoste S., Féron J.M., Cherrier B. Percutaneous Tenolig(®) repair under intra-operative ultrasonography guidance in acute Achilles tendon rupture. Orthop Traumatol Surg Res. 2014;100:925–930. doi: 10.1016/j.otsr.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Giannetti S., Patricola A.A., Stancati A., Santucci A. Intraoperative ultrasound assistance for percutaneous repair of the acute Achilles tendon rupture. Orthopedics. 2014;37:820–824. doi: 10.3928/01477447-20141124-04. [DOI] [PubMed] [Google Scholar]
- 13.Appy-Fedida B., Vernois J., Krief E., Gouron R., Mertl P., Havet E. Risk of sural nerve injury during lateral distal Achilles tendinoscopy: A cadaver study. Orthop Traumatol Surg Res. 2015;101:93–96. doi: 10.1016/j.otsr.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 14.Vega J., Vilá J., Batista J., Malagelada F., Dalmau-Pastor M. Endoscopic flexor hallucis longus transfer for chronic noninsertional Achilles tendon rupture. Foot Ankle Int. 2018;39:1464–1472. doi: 10.1177/1071100718793172. [DOI] [PubMed] [Google Scholar]
- 15.Lui T.H., Chan W.C., Maffulli N. Endoscopic flexor hallucis longus tendon transfer for chronic Achilles tendon rupture. Sports Med Arthrosc Rev. 2016;24:38–41. doi: 10.1097/JSA.0000000000000086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video shows a technique of percutaneous repair of acute Achilles tendon rupture under ultrasonographic and endoscopic assistance. The patient is in the prone position, with a tourniquet on the operated limb, the foot beyond the table to mobilize the ankle joint. Ultrasonography will allow the surgeon to identify the tendon extremities in longitudinal planes, and the sural nerve will be observed on coronal views. Posterolateral and posteromedial endoscopic portals can be drawn, centered on the rupture and keeping distance from the sural nerve. The entry point is posterolateral, and transillumination with the endoscope allows the surgeon appreciate the gap between the ends of the tendon extremities. Transillumination also helps for the posteromedial portal incision. Debridement of the tendons extremities is performed using the shaver, from proximal to distal, being careful not to injure the peritendon. We check the good mobilization of the proximal tendon end with a Kocher forceps. The percutaneous suture is X shaped according to the technique described by Ma and Griffith. The needle is introduced through the distal portion of the tendon, up to the proximal portion, under endoscopic guidance. After a transverse crossing in the proximal portion from medial to lateral with the needle, the longitudinal gap crossing from proximal to distal is controlled under endoscopic vision. We then finish by the transverse crossing in the distal tendon end, which then comes out through the posteromedial portal. While maintaining the ankle in plantar flexion, we tighten and tie the suture until a good reduction of the tendon ends is obtained under endoscopic guidance. At the end of the surgery, the transillumination signal must disappear, as an indirect sign of good reduction of the tendon ends. A cast is then applied to keep the ankle at 30° of flexion.