Abstract
Medial meniscus extrusion is commonly seen in patients who have medial meniscus posterior root tear. Extruded meniscus results in faster progression of knee arthrosis. Thus, it is important to reduce the extrusion as well as treat the cause of extrusion. This Technical Note describes an all-inside arthroscopic technique to reduce the meniscus extrusion. An additional medial portal has to be made along with the standard anteromedial and anterolateral portals. A double-loaded suture anchor is used to secure the extrusion of the meniscus in its native position. Thus, making a transosseous tibial tunnel is not required. It is easy to perform and is an efficient technique.
The meniscus is made of circumferential as well as radial collagen fibers.1 Any significant disruption of the circumferential fibers leads to loss of hoop tension, causing the meniscus to extrude. Medial meniscus extrusion is considered significant if there is more than 3 mm of displacement with respect to the central margin of the medial tibial plateau.2 A common cause of meniscal extrusion is root tear. Other causes include large radial tear (>50% of meniscal width) and large complex tears (>1 cleavage plane through the meniscus).2, 3 Medial meniscus extrusion can independently cause knee pain (apart from the primary pathology). After the meniscus has extruded, the femoral condyle and the tibial plateau come into contact. Thus, there can be loss of tibiofemoral articular cartilage and acceleration of arthosis.4 Allaire et al.5 showed that the knee, after the tear of the meniscus root, behaves like a menisectomized knee. The aim of treatment is to reduce the extrusion along with the treatment of the primary cause of extrusion.6 Meniscus extrusion reduction as described by Chernchujit and Prasetia7 is a transosseous technique. It requires a tibial tunnel through which the meniscus body is pulled toward the joint and is secured over an endo button or sutured to the post.
In this Technical Note we describe an all-inside technique to reduce the extrusion arthroscopically. The extrusion is reduced and secured with a suture anchor. This eliminates the need for a tibial tunnel.
Preoperative Diagnosis
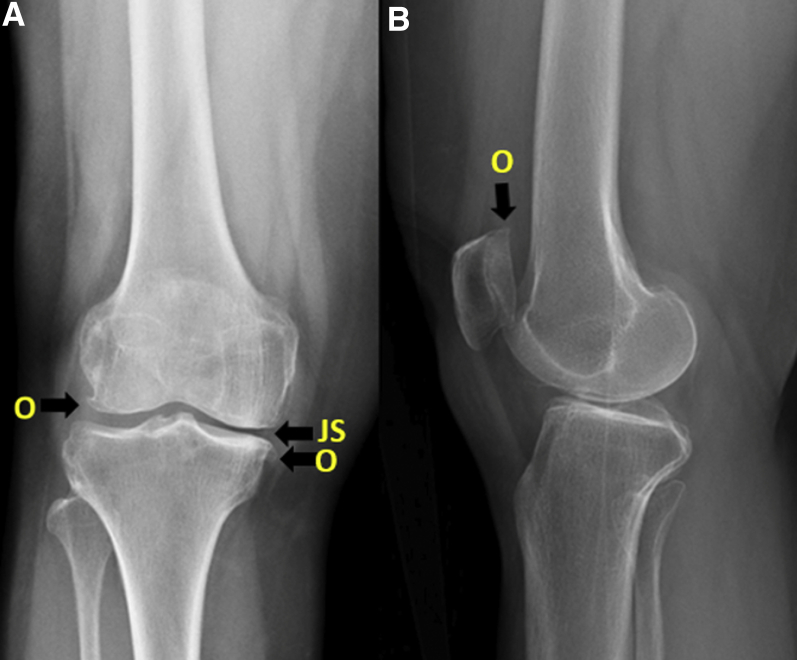
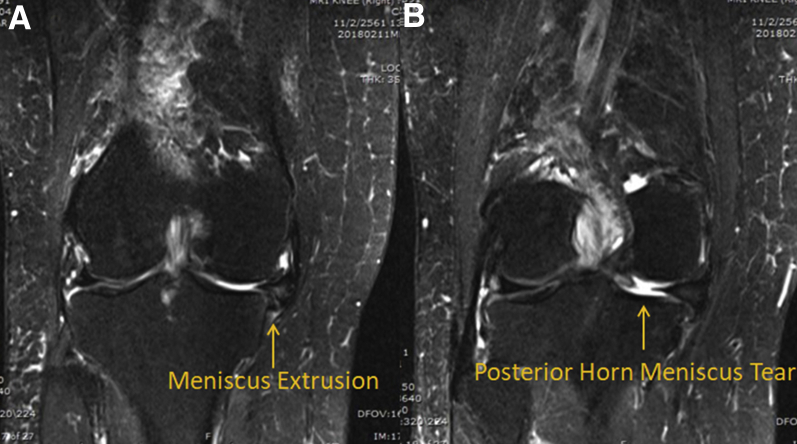
Medial joint line pain in a patient >50 years old after an episode of deep flexion should prompt a diagnosis of a meniscal tear. A sudden increase in the pain, which may at times be accompanied by a popping sound, could be an indication of meniscus extrusion. Radiographs (Fig. 1) show changes suggestive of osteoarthrosis, and the diagnosis is confirmed by magnetic resonance imaging of the knee joint. Magnetic resonance imaging shows “meniscal extrusion” along with the primary cause of extrusion (in this case a tear in the posterior horn of the medial meniscus; Fig. 2).
Fig 1.
Preoperative anteroposterior (A) and lateral (B) radiographs of the right knee. (A) There are marginal osteophytes (O) on the femoral condyle as well as tibial plateau. The medial joint space (JS) is reduced. (B) On the lateral view, osteophytes (O) on the patella are evident. Apart from the features of osteoarthrosis, there are no other obvious significant abnormalities in the radiographs.
Fig 2.
Coronal view cuts of magnetic resonance imaging of the right knee. (A) The meniscus is extruded out of the medial compartment of the knee and is impinging on the medial collateral ligament. This results in pain in the medial joint line. (B) Tear in the posterior horn of the medial meniscus near the root. This is the primary pathology leading to medial meniscus extrusion in this patient.
Surgical Technique
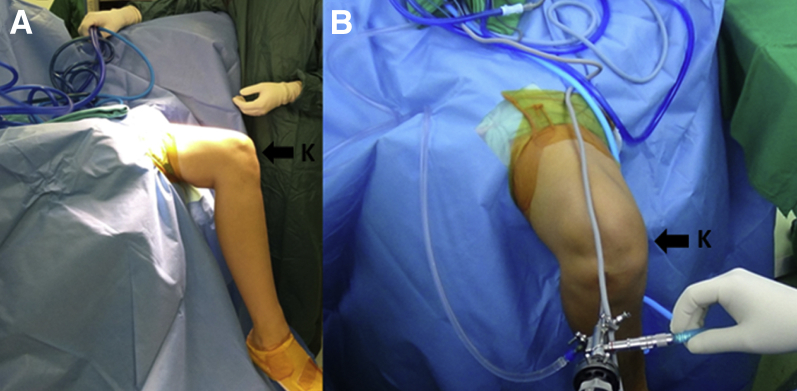
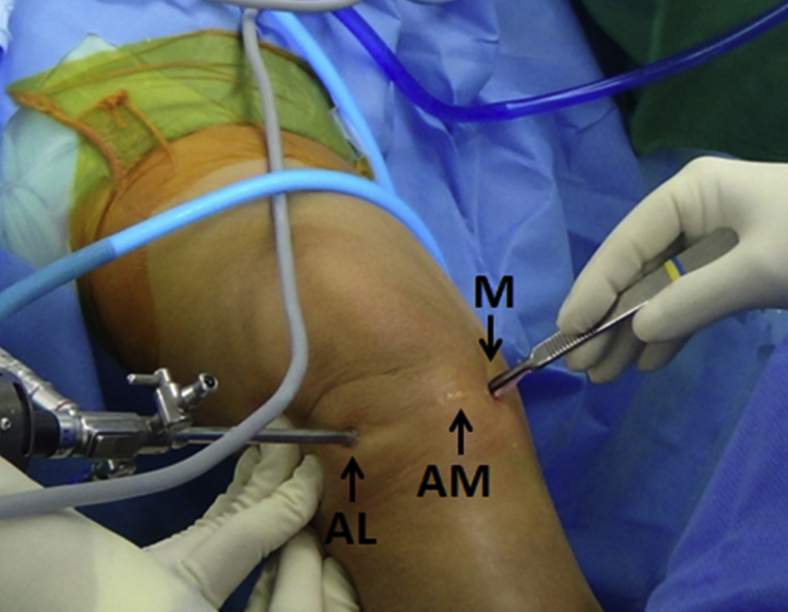
We prefer using adductor canal block along with spinal anesthesia. The patient is positioned on the operating table. The nonoperating lower limb is placed on an abduction post. Tourniquet is placed as high as possible on the affected lower limb. A sandbag is placed under the distal thigh on the operative limb so that the knee is in 90° of flexion. Scrubbing and painting of the operative limb are done. Draping is done in such a way to leave the operative limb free for movement during the surgery (Fig. 3). After painting and draping, standard anterolateral and anteromedial portals are made and diagnostic arthroscopy of the knee is done. In most cases it is necessary to release the superficial medial collateral ligament percutaneously to get access to the medial compartment of the knee. After reconfirming the diagnosis arthroscopically, we make another portal at the medial joint line just proximal to the medial meniscus under vision from the arthroscope, the midmedial portal (Fig. 4; Video 1). A drill bit of size 1.9 mm is used to drill a hole on the edge of the medial tibial plateau from the midmedial portal for the suture anchor (Fig. 5). A double-loaded suture anchor (SutureFix 1.9 mm double-loaded anchor; Smith & Nephew) is buried in the previously drilled hole through the same portal (Fig. 6). The spectrum (Conmed) is passed through the rim of the meniscus about 1 cm posterior to the level of the suture anchor from the midmedial portal (Fig. 7; Video 1). The PDS (Ethicon, Johnson and Johnson; from the spectrum), along with a limb of the blue suture (from the suture anchor), is pulled out through the anteromedial portal. The blue suture is engaged in the PDS suture and pulled out of the midmedial portal passing through the meniscus (Fig. 8). The spectrum is passed again at the rim of the meniscus at the level of the suture anchor from the midmedial portal. The same process is repeated, but this time the remaining limb of blue and one limb of tiger blue sutures (from the suture anchor) are pulled. To make it easier to take a bite into the meniscus anterior at the level of suture anchor, the spectrum is now passed into the joint through the anteromedial portal (Fig. 9; Video 1). The PDS suture from the upper surface of the meniscus is pulled out of the midmedial portal and the remaining limb of tiger blue suture, and the PDS from the lower surface of the meniscus is pulled out of the anteromedial portal. The tiger blue suture is engaged in the PDS suture and pulled out through the midmedial portal. Both limbs of tiger blue sutures are then pulled out through the anteromedial portal (this is done to prevent entanglement of the sutures while tying the knots). The 2 limbs of blue sutures are pulled out through the midmedial portal, and knots are tied (Fig. 10). The sutures are cut (Video 1). The tiger blue sutures are pulled out through the midmedial portal, and knots are tied (Fig. 11). After knot tying, the sutures are cut. The rim of the meniscus comes to lie over the rim of the tibial plateau, thus reducing the extrusion and securing it in its position (Fig. 12; Video 1).
Fig 3.
Position of the patient on the operating table. (A) The position viewed from the side; (B) the position as seen head on. The left lower limb is kept on an abduction post and covered with drapery. This provides more space in the operating field. The right limb is seen hanging freely with the knee (K) at 90° of flexion. This is the working position for the procedure as no assistance is required to hold the lower limb. The free hanging position is also helpful if the limb has to be moved or maneuvered during the procedure.
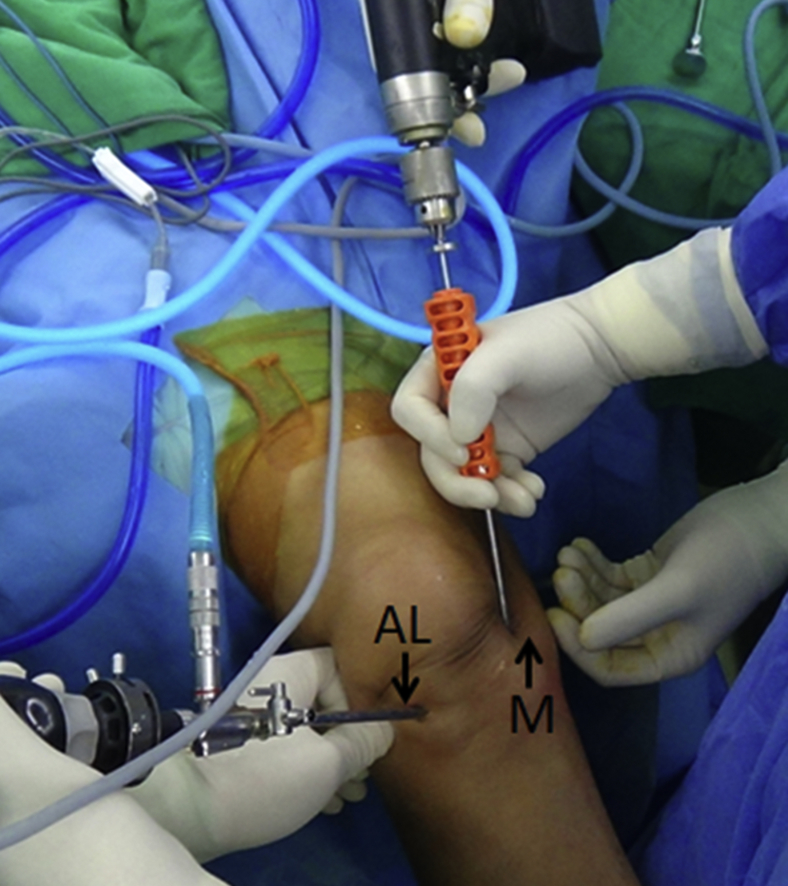
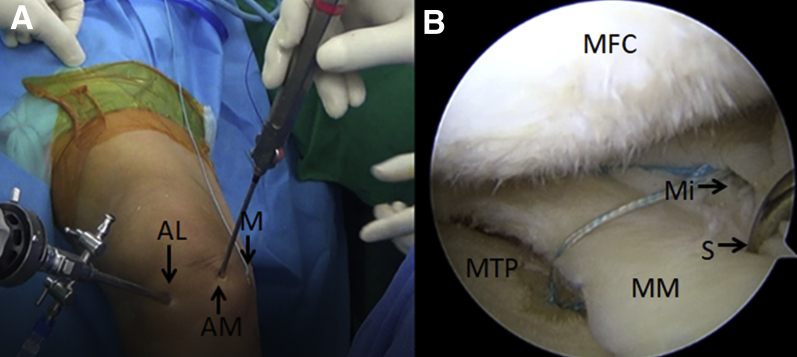
Fig 4.
Portals made in the right knee joint during the procedure. Standard anterolateral (AL) and anteromedial (AM) portals are made on the anterior aspect of the knee lateral and medial to the patellar tendon. A midmedial (M) portal is made on the medial surface of the joint. AL is the viewing portal throughout the procedure, while AM and M are the working portals.
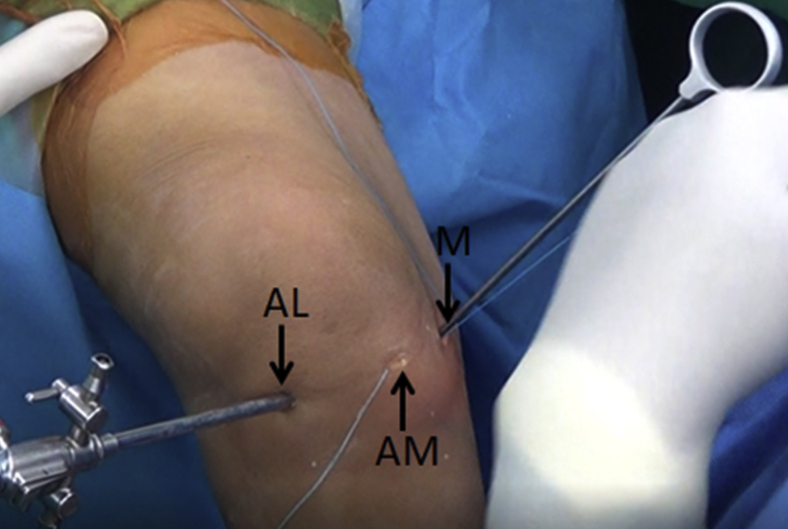
Fig 5.
Outside view of the right knee. The anterolateral portal (AL) is used as the viewing portal. The midmedial (M) portal is used to drill a hole at the edge of the medial tibial plateau for placement of the suture anchor. A 1.9-mm drill bit is used for this purpose. The direction of the drill bit is perpendicular to the tibial plateau so that it does not slip on the surface.
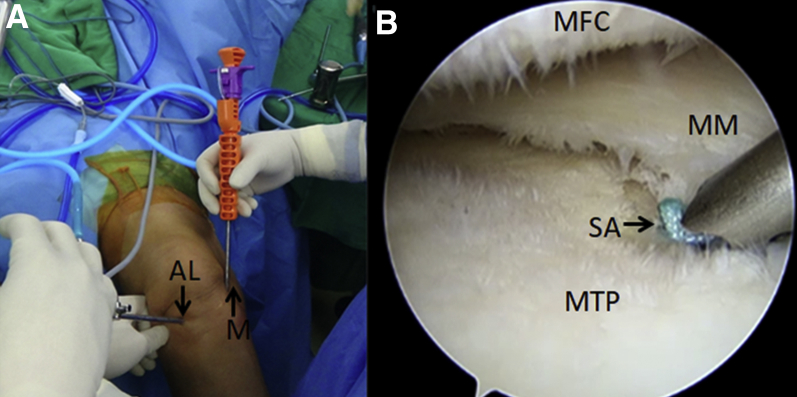
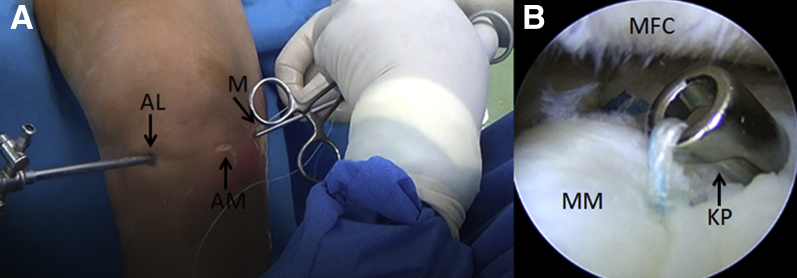
Fig 6.
Placement of a double-loaded 1.9-mm suture anchor (1.9 mm SutureFix) in the previously drilled hole in the medial edge of the right tibial plateau. (A) Outside view; (B) view from the arthroscope. Panel A shows the suture anchor being placed in the drill hole previously made by the drill bit. The direction of the suture anchor is same as the drill bit. Panel B shows the suture anchor entering the hole. A mallet is used to bury the suture anchor completely onto the hole. AL, anterolateral portal; M, midmedial portal; MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau; SA, suture anchor.
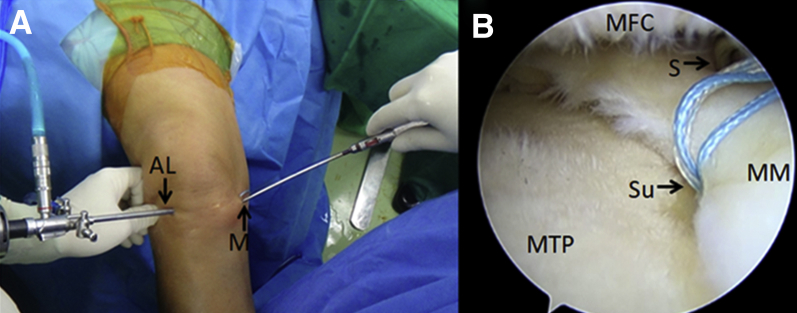
Fig 7.
Spectrum being passed in the medial meniscus of the right knee. (A) Outside view; (B) arthroscopic view. Panel A shows that the spectrum is inserted through the midmedial (M) portal into the joint, while the anterolateral (AL) portal is the viewing portal. Panel B shows that the spectrum is posterior to the level of suture anchor. The spectrum is passed posterior to the level of the suture anchor through the rim of the medial meniscus. MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau; S, spectrum; Su, sutures from suture anchor.
Fig 8.
The spectrum is passed posterior to the level of the suture anchor through the rim of the medial meniscus of the right knee. The PDS suture from the spectrum and 1 blue suture of the suture anchor are pulled out of the anteromedial portal (AM). The blue suture is engaged in the PDS and pulled out through the midmedial portal (M). AL, anterolateral portal.
Fig 9.
The spectrum (S) being passed from the anteromedial portal (AM) of the right knee. (A) The outside view of the joint, in which we can see that the arthroscope is in the anterolateral portal (AL), that is, it is the viewing portal. The spectrum is passed through the AM. Sutures are visible in the midmedial portal (M). (B) Arthroscopic view of the spectrum being passed in the meniscus through the AM. MFC, medial femoral condyle; Mi, inside view of the M portal; MM, medial meniscus; MTP, medial tibial plateau.
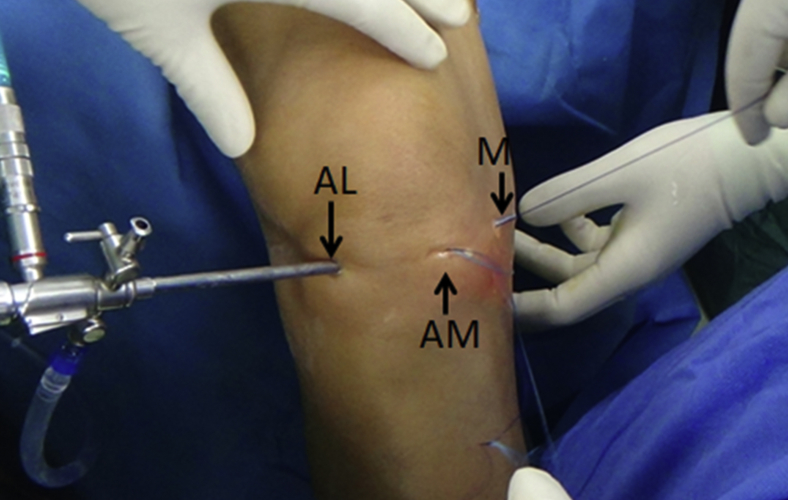
Fig 10.
Outside view of the right knee. The anterolateral portal (AL) is the viewing portal. The tiger sutures are pulled out of the anteromedial portal (AM). The midmedial portal (M) is used to tie the knots in the 2 blue sutures that are pulled through it. Tiger sutures are pulled out of AM to prevent entangling of these sutures with the blue sutures.
Fig 11.
Process of knot tying in the tiger blue sutures in right knee. (A) The anterolateral portal (AL) is the viewing portal. The tiger blue sutures are pulled through the midmedial portal (M) from the anteromedial portal (AM). Knots are tied in the tiger blue sutures. (B) Arthroscopic view of knot tying in the tiger blue sutures. The cut ends of the blue sutures after the knots have been tied are also visible. KP, knot pusher; MFC, medial femoral condyle; MM, medial meniscus.
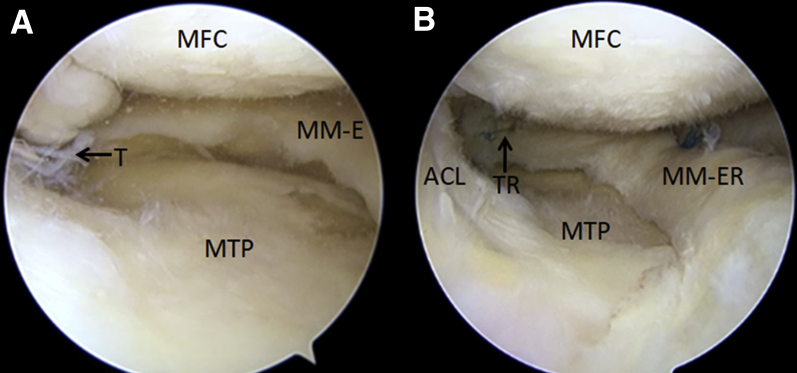
Fig 12.
Comparison of the preoperative and postoperative arthroscopic view of the medial compartment of the right knee of the patient. (A) There is a tear in the posterior horn of the medial meniscus (T). This results in the extrusion of the medial meniscus (MM-E). This is evident as the whole of the medial tibial plateau (MTP) is completely visible with an osteochondral defect in it. The defect may be a result of the loss of the protective effect of the meniscus as the meniscus is extruded from the joint. MFC, medial femoral condyle. (B) The postoperative arthroscopic view of the medial compartment of the knee. The tear in the posterior horn has been repaired (TR). After the procedure, the extruded meniscus has been reduced (MM-ER) and covers the MTP. The cut ends of the sutures can be seen. A part of the anterior cruciate ligament (ACL) is also visible.
Following this, the primary cause for extrusion is treated. In the above case the posterior horn radial tear was repaired using FAST-FIX (Smith & Nephew). Portals are closed with 3-0 prolene (Ethicon, Johnson and Johnson). Dressings are put on, and the patient is moved to the recovery room.
The postoperative protocol is based on the primary pathology of the meniscus. Considering the above case of a tear in the posterior horn of the medial meniscus near the root, we here describe our protocol after repair of the meniscus tear near the posterior root. The patient is encouraged to walk non–weight bearing, and flexion more than 90° is not permitted for about 3 weeks. Physiotherapy for strengthening the quadriceps is started. The patient is permitted to progressively bear weight after 3 weeks, and full weight bearing is allowed at 6 weeks. Squatting and deep flexion are allowed after 6 months.
Discussion
A transtibial suture pull-out technique has been described by Chernchujit and Prasetia.7 The technique is in many ways similar to the transtibial suture pull-out technique for root repair. Comparative studies showing the results of transtibial suture pullout and all-inside meniscus root repair with suture anchor fail to demonstrate whether any technique has better results than the other.8 Feucht et al.9 in their study concluded that the suture anchor technique provided superior biomechanical properties compared with the transtibial suture pull-out technique.9 Choi et al.10 noted the risk of suture abrasion in the tunnel during range of motion exercises. The risk of crowding or collision of the tibial tunnel when accompanied by other ligament reconstruction surgeries or high tibial osteotomy and the possibility of cartilage damage while inserting the tibial guide for making the tunnel are some other disadvantages of the transtibial suture pull-out technique.8 The all-inside technique with suture anchor avoids these disadvantages and has the advantage of being technically less demanding than the suture pull-out technique. It has less of a bungee cord effect because the suture construct is short.11 However, care needs to be taken to prevent medial collateral ligament and medial meniscus iatrogenic injuries while making the midmedial portal (Table 1). To avoid injuries to these structures, the following precautions must be taken. The stab incision should be made in the longitudinal direction, that is, in line with the fibers of the medial collateral ligament, and the capsular incision should be made under vision with the arthroscope to avoid injury to the medial meniscus. Caution is also required while drilling the hole on the edge of the tibial plateau. The drill sleeve should be held gently but firmly on the edge till the suture anchor is buried in the tibia. Otherwise the drill bit or the suture anchor can slip off the edge. A disadvantage of this technique is that there is a possibility of loosening of the suture anchor over time (Table 2).11
Table 1.
Pearls and Pitfalls of the All-Inside Medial Meniscus Extrusion Reduction Technique
| Pearls | Pitfalls |
|---|---|
| It is a technically less demanding, efficient technique. | The midmedial portal should be made under vision so as not to damage the meniscus. |
| There is no need for the transosseous tunnel, so a low-profile aiming device instrument is not required. | The portal should be made in a longitudinal direction to prevent iatrogenic injury to the medial collateral ligament. |
| The midmedial portal is the working portal, which makes the passage of the suture in the posterior part of meniscus easier. | The drill guide should be held firmly on the edge of the tibial plateau; otherwise it can slip off from the edge. |
Table 2.
Advantages and Disadvantages of the All-Inside Medial Meniscus Extrusion Technique
| Advantages | Disadvantage |
|---|---|
| There is no bungee cord effect and minimal micromotion as the fixation is near the suture anchor. | There is a risk of loosening the suture anchor over time. |
| There is no risk of suture abrasion. | |
| Tunnel management is easier when accompanied by other procedures that require intraosseous tunnels. |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
After preoperative assessment and laboratory workup, written consent was taken and the patient was scheduled for surgery. In the operating room, after spinal anesthesia was administered, the patient was positioned supine on the operating table. The leg ends of the table were removed. The left lower limb was placed on an abduction post, and painting and draping were done to allow the right lower limb to hang free with the knee in 90° of flexion. This position gives enough room in the operating field. A standard anterolateral knee portal was made, which was the viewing portal, and diagnostic arthroscopy of the knee was done. On diagnostic arthroscopy we found a radial tear in the posterior horn on medial meniscus, extrusion of the medial meniscus, and an osteochondral defect in the medial tibial plateau. These findings correlated with the findings of the preoperative radiographic findings. The fat tissue was removed with the shaver for better visualization. The medial joint compartment space was decreased and was hindering the vision in the posterior part, so pie-crusting of the superficial medial collateral ligament was done to increase the medial joint space. A midmedial portal was established. The anteromedial and midmedial portals were the working portals. A hole was drilled through the midmedial portal at the edge of the medial tibial plateau using a 1.9-mm drill bit. A double-loaded suture anchor (SutureFix 1.9 mm) was buried in the predrilled hole. The sutures were passed through the outer rim of the meniscus posterior, anterior, and at the level of the suture anchor. Anteriorly and posteriorly, 1 limb of sutures of different colors was pulled though the meniscus, and 2 sutures, each of different color, were pulled at the level of the suture anchor. The same color sutures were then taken together through the midmedial portal, and knots were tied. The meniscus extrusion was thus reduced. The tear in the posterior horn was repaired with FAST-FIX. After the procedure, there was adequate coverage of the medial tibial plateau with the meniscus and enough meniscus tissue between the medial femoral condyle and the medial tibial plateau.
Video Still.
References
- 1.Rath E., Richmond J.C. The menisci: Basic science and advances in treatment. Br J Sports Med. 2000;34:252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lerer D.B., Umans H.R., Hu M.X., Jones M.H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol. 2004;33:569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 3.Costa C.R., Morrison W.B., Carrino J.A. Medial meniscus extrusion on knee MRI: Is extent associated with severity of degeneration or type of tear? Am J Roentgenol. 2004;183:17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 4.Swamya N., Wadhwaa V., Bajaja G., Chhabrab A., Pandeya T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–124. doi: 10.1016/j.ejrad.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 6.Chung K.S., Ha J.K., Ra H.J., Nam G.W., Kim J.G. Pullout fixation of posterior medial meniscus root tears: Correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45:42–49. doi: 10.1177/0363546516662445. [DOI] [PubMed] [Google Scholar]
- 7.Chernchujit B., Prasetia R. Arthroscopic direct meniscal extrusion reduction: Surgical tips to reduce persistent meniscal extrusion in meniscal root repair. Eur J Orthop Surg Traumatol. 2018;28:727–734. doi: 10.1007/s00590-018-2138-6. [DOI] [PubMed] [Google Scholar]
- 8.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.R. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 9.Feucht M.J., Grande E., Brunhuber J. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med. 2014;42:187–193. doi: 10.1177/0363546513502946. [DOI] [PubMed] [Google Scholar]
- 10.Choi N.H., Son K.M., Victoroff B.N. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: A technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16:891–893. doi: 10.1007/s00167-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 11.LaPrade R.F., LaPrade C.M., James E.W. Recent advances in posterior meniscal root repair techniques. J Am Acad Orthop Surg. 2015;23:71–76. doi: 10.5435/JAAOS-D-14-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
After preoperative assessment and laboratory workup, written consent was taken and the patient was scheduled for surgery. In the operating room, after spinal anesthesia was administered, the patient was positioned supine on the operating table. The leg ends of the table were removed. The left lower limb was placed on an abduction post, and painting and draping were done to allow the right lower limb to hang free with the knee in 90° of flexion. This position gives enough room in the operating field. A standard anterolateral knee portal was made, which was the viewing portal, and diagnostic arthroscopy of the knee was done. On diagnostic arthroscopy we found a radial tear in the posterior horn on medial meniscus, extrusion of the medial meniscus, and an osteochondral defect in the medial tibial plateau. These findings correlated with the findings of the preoperative radiographic findings. The fat tissue was removed with the shaver for better visualization. The medial joint compartment space was decreased and was hindering the vision in the posterior part, so pie-crusting of the superficial medial collateral ligament was done to increase the medial joint space. A midmedial portal was established. The anteromedial and midmedial portals were the working portals. A hole was drilled through the midmedial portal at the edge of the medial tibial plateau using a 1.9-mm drill bit. A double-loaded suture anchor (SutureFix 1.9 mm) was buried in the predrilled hole. The sutures were passed through the outer rim of the meniscus posterior, anterior, and at the level of the suture anchor. Anteriorly and posteriorly, 1 limb of sutures of different colors was pulled though the meniscus, and 2 sutures, each of different color, were pulled at the level of the suture anchor. The same color sutures were then taken together through the midmedial portal, and knots were tied. The meniscus extrusion was thus reduced. The tear in the posterior horn was repaired with FAST-FIX. After the procedure, there was adequate coverage of the medial tibial plateau with the meniscus and enough meniscus tissue between the medial femoral condyle and the medial tibial plateau.