Abstract
Age-dependent declines in muscle function are observed across species. The loss of mobility resulting from the decline in muscle function represents an important health issue and a key determinant of quality of life for the elderly. It is believed that changes in the structure and function of the neuromuscular junction are important contributors to the observed declines in motor function with increased age. Numerous studies indicate that the aging muscle is an important contributor to the deterioration of the neuromuscular junction but the cellular and molecular mechanisms driving the degeneration of the synapse remain incompletely described. Importantly, growing data from both animal models and humans indicate that exercise can rejuvenate the neuromuscular junction and improve motor function. In this review we will focus on the role of muscle-derived neurotrophin signaling in the rejuvenation of the aged neuromuscular junction in response to exercise.
Keywords: neurotrophin, neuromuscular junction, aging, retrograde signaling, exercise
INTRODUCTION
Research over the past two decades has uncovered novel roles of skeletal muscle beyond its contractile function. Today skeletal muscle is recognized as a major endocrine organ with the capacity to secrete signals and act on distal targets such as adipose tissue, liver, pancreas, brain and endothelium. In response to environmental or dietary challenges, as well as to organelle and metabolic dysfunctions, the skeletal muscle secretes signals in the form of myokines, myometabolites, neurotrophins and other muscle-derived signals to help maintain the metabolic and physiological homeostasis of the organism 1,2. In addition to communication with remote tissues, it is well established that proper development of the neuromuscular junction (NMJ) requires communication between the muscle and motor neuron. Numerous studies have identified retrograde signals originating from the muscle that are critical for normal synaptic structure and function of the NMJ during development and in the adult 3,4,5,6. Age-dependent declines in motor activity have been documented across species and in humans to represent a significant health issue for the elderly. The contributions of changes in synaptic function at the NMJ to the declines in motor function observed during aging are becoming more appreciated, but the important mechanisms underlying the effects of age on NMJ structure and function remain poorly described. For example, it is unclear the role that retrograde signaling at the NMJ plays in the declines in motor function observed during aging. Muscle-derived signaling molecules, such as neurotrophins and morphogens, are established retrograde signals with powerful effects on NMJ structure and function and, thus, represent candidate signaling systems for the maintenance of motor function during aging. Importantly, exercise induces the muscle expression of many of these neurotrophins providing a molecular explanation for the rejuvenation of the structure and function of the aged NMJ in response to exercise.
RETROGRADE TROPHIC SIGNALING AT THE NMJ
During development the increase in muscle size due to fiber growth results in a change in the resistance of the growing muscle fiber to the depolarizing input of the motor neuron. This change in the electrical properties requires a precise concomitant change in neurotransmitter release from the presynaptic nerve terminal to maintain faithful depolarization of the muscle. The mechanism coupling muscle growth and synaptic input is the production of muscle-derived retrograde trophic signaling that supports the growth of the synaptic innervation. A beautiful example of this coupling is observed during the development of the Drosophila larval NMJ. During the initial ~100 hours of larval development, the surface area of the muscle increases nearly 100-fold, which results in a large reduction in the electrical resistance of the muscle making the muscle harder to depolarize. Despite this change in the muscle, the depolarization of the muscle by the motor neuron is precisely maintained throughout development to insure normal larval motility. To maintain the consistent depolarization of the muscle, the presynaptic nerve terminal releases increasing amounts of neurotransmitter. To facilitate the increase in neurotransmission, the larval NMJ grows by increasing the number of boutons at the synapse 10-fold during developmental growth (Note: Boutons are morphometric structures of the Drosophila NMJ that is commonly used as a quantitative measure of synapse size) 7. In these studies, statistical analysis of post-synaptic electrophysiological recordings was utilized to determine precisely the total number of synaptic vesicles utilized to generate the evoked excitatory post-synaptic potential (EPSP) in the muscle. These quantal analyses reveal that the change in neurotransmission was due to the increase in the total number of synaptic vesicles released (i.e. quantal content) and not due to changes in the depolarization of the muscle in response to a single quanta of neurotransmitter (i.e. quantal size), which often indicate changes in post-synaptic neurotransmitter receptor function 8. This terminology has been adopted for this review.
The preciseness of the adjustments in neurotransmitter release during larval growth suggests that the presynaptic nerve terminal is being informed about the increasing size of the muscle. This possibility proposes a signal originating from the muscle that instructs the motor neuron, and the nerve terminal, about the size of the growing muscle. Support for this model was provided by Goodman and colleagues who showed in a series of experiments that muscle-derived bone morphogenic protein (BMP), Glass bottom boat (Gbb) and the presynaptic type II BMP receptor Wishful-thinking (Wit) function in a retrograde genetic pathway required for normal synapse growth; and the lack of either leads to a smaller than normal synapse with reduced neurotransmission 9,10. Although these studies support an important role for retrograde BMP signaling for normal synapse growth during larval development, whether retrograde BMP signaling plays a role in the maintenance of the adult NMJ is not known.
At the mammalian NMJ, a number of neurotrophins (NTs) have been shown to be required for proper development of the NMJ 5,6,11. Interestingly, NTs classically known for their role as promoters of motor neuron survival and maintenance (e.g. BDNF (brain-derived neurotrophic factor), GDNF (glial cell line-derived neurotrophic factor), NT-3 and NT-4) have been found to be expressed in adult skeletal muscles supporting the existence of retrograde trophic signaling at the adult NMJ 12,13,14,15,16,17,18,19. Further evidence that muscle-derived NTs could support the maintenance of adult NMJs comes from several observations. For example, analysis of the NMJs in transgenic mice overexpressing GDNF in muscle revealed hyperinnervation of the muscle 18,20,21. Furthermore, the nerve terminals were larger and more complex in the mice with increased muscle-derived GDNF 21. Interestingly, while overexpression of GDNF results in marked morphological changes of the synaptic terminal, similar overexpression of NT-3 or NT-4 showed no effect in these studies 18. These studies reveal a potent ability of GDNF to drive synapse growth, but its role during the development or maintenance of the NMJ is unclear.
In addition to effects on NMJ morphology, several studies have revealed potent effects of NTs on neurotransmission at the NMJ 6,22,23. In vitro and in vivo treatment with BDNF, GDNF, NT-3 and NT-4 potentiates both the spontaneous and evoked release of neurotransmitter at the NMJ 24,25,26,27,28. Importantly, these effects of BDNF and NT-4 require presynaptic TrkB receptors supporting that these NTs are functioning as retrograde signals with the ability to modulate neurotransmission 25,29. Mechanistically, GDNF has been shown to potentiate presynaptic release by increasing the expression of frequenin, which in turn increases N-type Ca2+ channel activation leading to enhanced Ca2+ influx into the nerve terminal 27. This effectively links muscle derived NTs to the presynaptic neurotransmitter release machinery. The modulation of Ca2+ influx by muscle-derived retrograde signaling has also been demonstrated at the Drosophila larval NMJ in response to genetic or pharmacologic reduction in the sensitivity of the muscle to neurotransmitter, supporting that calcium influx into the presynaptic nerve terminal represents a conserved mechanism of retrograde control of presynaptic neurotransmitter release 3,30,31.
EXERCISE INCREASES RETROGRADE TROPHIC SIGNALING
One of the most remarkable properties of the NMJ is its ability to maintain normal function in the face of physical stresses such as extended periods of increased physical activity. During increased physical activity, the release of neurotransmitter from the presynaptic nerve terminal must be sufficient for each contraction without exhausting the store of synaptic vesicles. A number of studies have demonstrated that both endurance and resistance training stimulate extensive morphological adaptations of the presynaptic nerve terminal of the NMJ. Examinations of the NMJ morphology of the soleus, extensor digitorum longus (EDL), plantaris and gluteus maximus muscles in both mice and rats revealed that strenuous physical training induces NMJ hypertrophy leading to an increase in the degree and length of nerve terminal branching 32,33,34,35,36. In addition to morphology, exercise training was also found to increase the presynaptic release of neurotransmitter at the NMJs of the EDL and gluteus maximum muscles 34,37. The most likely possibility is that the increase in synapse growth, and the subsequent increase in neurotransmission, is an adaptive response of the NMJ to support the increased demands upon the system.
The changes observed at the NMJ in response to increased physical activity suggest the existence of an exercise-induced muscle-derived retrograde signal(s) that can modify the morphological and functional properties of the NMJ to adapt to the demands on neurotransmitter release. To that end, several studies have demonstrated elevated BDNF, GDNF, NT-3, and NT-4 levels in skeletal muscles post involuntary and voluntary exercise 38,39,40,41,42,43,44. For example, four weeks of walk-training on a treadmill resulted in an increase in GDNF levels in the skeletal muscle, while hind limb unloaded animals resulted in a decrease in GDNF levels 39. These studies are consistent with the model that NT expression is closely tied to muscle activity, even during bouts of normal activity. In another study, cycling exercise resulted in >10 fold increase of BDNF and GDNF expression in exercised rat soleus muscles 41. Furthermore, low intensity walking preferentially increases GDNF expression in slow twitch soleous myofibers, while the same type of training decreases GDNF expression in the fast-twitch EDL myofibers 42. On the other hand, high intensity exercise caused an increase in GDNF expression in fast-twitch muscle fibers demonstrating that regulation of NT expression in the muscle is a property of both slow- and fast-twitch fibers 44. Importantly, in addition to the changes in skeletal muscle GDNF levels following an increase in physical activity, several studies have demonstrated morphological changes at the same NMJs, demonstrating the relationship between exercise-induced GDNF muscle expression level and exercise-induced NMJ remodeling 43,44. Thus, exercise and increased expression of NTs elicit similar responses at the NMJ both at the level of synaptic morphology and neurotransmission. Collectively, these data support the model that the adaptation of the NMJs to exercise is the result of muscle-derived retrograde NT signaling (Figure 1B).
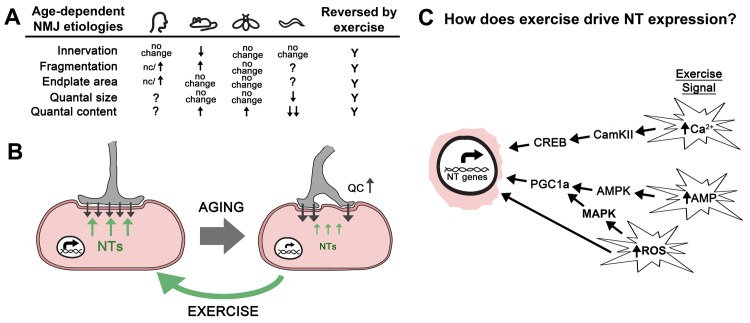
Figure 1. FIGURE 1: Exercise rejuvenates the neuromuscular junction by stimulating retrograde signaling.
(A) Table contains the changes to the synaptic structure and function of the NMJ during aging from humans, mice, flies, and worms discussed in this review article. Inconsistent results about fragmentation at human NMJs are indicated. Exercise reverses all of these changes.
(B) Aging results in reduced neurotrophin expression (NT; green arrows) leading to a loss of synaptic morphology and a compensatory increase in neurotransmitter release (quantal content = QC) at the neuromuscular junction (black arrows). Exercise increases the expression of multiple neurotrophin genes (NT genes; green arrows) resulting in improved structure and function of the neuromuscular junction.
(C) Exercise results in increased cytosolic levels of calcium, reactive oxygen species (ROS), and an increase in the AMP:ATP and ADP:ATP ratios. We propose that these events initiate signaling cascades that result in the expression of neurotrophin (NT) genes via the activity of transcription factors such as CREB and PGC1a. It is expected that mechanical stress and oxidative stress help to modulate these signal transduction pathways. It’s also possible that the oxidation of DNA directly alters expression of NT genes.
RETROGRADE SIGNALING DURING AGING
The progressive declines in skeletal muscle mass, referred to as sarcopenia, and muscle strength are broadly observed in mammals and represents one of the first hallmarks of aging. Numerous studies in rodent models have demonstrated that the loss of motor function with age is accompanied with changes in the structural integrity of the NMJ 45, but the contribution of these changes in synaptic morphology to the loss of motor function is still unclear. These morphologies include the increased branching of nerve terminals, the progressive fragmentation of the nerve terminal including the post-synaptic acetylcholine receptor (AChR) clusters, increased extra-junctional AChRs, and myofiber denervation (Figure 1A) 46,47,48,49,50,51,52,53,54. Despite the significant fragmenting of the synaptic area, most studies support that total endplate area is unchanged (or even increased) during aging 45,55,56. It should be noted that some of these synaptic changes are due to the re-innervation of new fibers resulting from the continual turnover of myofibers and the loss of fiber type diversity of the motor units 57,58. In humans, studies investigating the morphology of the NMJs formed on the intercostal muscles of the rib cage suggested extensive remodeling of the NMJ, similar to mice 59,60. But a recent study of the NMJs of the lower leg (extensor digitorum, soleus, peroneus longus, and peroneus brevis) from 21 amputees found that these NMJs, when compared to young adult mice, were significantly smaller with thinner pre-terminal axons, had less complex endplates, and showed differential organization of active zone components 61. In addition, these human NMJs were remarkably stable with little fragmentation or morphological change from the 4th to the 10th decade of life 61. This study further investigated the differences in the synaptic proteome between the mouse and human NMJ and found significant differences in the protein composition of the synapses including proteins involved directly in NGF, GDNF receptor, and TRK receptor signaling 61. Interestingly, most of the proteins linked to neurotrophin signaling were found to be less abundant at human NMJs compared to mouse NMJs suggesting that these signaling systems are more operative at the mouse NMJ.
The observation of substantial NMJ remodeling during aging suggested the possibility that neurotransmission might be compromised during aging. But nearly all studies in both mice and flies have reported increased release of neurotransmitter from aged NMJs compared to young NMJs 34,54,56,62,63,64. Perhaps the increase in the release of neurotransmitter from the presynaptic nerve terminal of the NMJ is compensatory for decreasing muscle contraction and/or changes in the sensitivity of the muscle to neurotransmitter. For example, a pharmacological, pathological, or genetic reduction of the postsynaptic neurotransmitter receptor sensitivity at the NMJ leads to a compensatory increase in presynaptic neurotransmitter release (quantal content) across species to insure appropriate muscle depolarization 64,65,66,67,68,69,70,71. These data support the existence of a conserved retrograde signaling system that can alter presynaptic neurotransmitter release. Thus, it is possible that the increase in neurotransmission during aging is the result of impaired homeostatic control mechanisms associated with this form of plasticity. Intriguingly, synaptic homeostasis at the Drosophila larval NMJ requires TOR signaling within the muscle, a known cellular signaling system important for adaptive responses to aging 72,73. But most studies investigating the functional properties of the NMJ find that the sensitivity of the muscle to neuotransmitter (i.e. quantal size) is unchanged during aging 34,55,62,64,74,75,76,77 (Figure 1A). Thus, the critical signal for the homeostatic increase in neurotransmission is not observed during aging. Furthermore, synaptic homeostasis in Drosophila requires the presynaptic Ephexin receptor 65. Analysis of neurotransmission across age in Drosophila reveals that mutations in the ephexin gene do not block the increase in neurotransmission observed during aging 64. In addition, this study demonstrated that synaptic homeostasis was functioning robustly at older NMJs and that the age-dependent increase in neurotransmission included a re-setting of the homeostatic set-point of the NMJ 64. It is unclear if the increase in neurotransmitter release observed at aged NMJs in rodents also represents a change in the set-point of the synapse.
Another possibility is that the age-dependent increase in neurotransmission observed at the NMJ is in response to declining muscle function. The CM9 muscle group in Drosophila is one of 13 muscle groups required for the extension of the adult proboscis during feeding 78. Analysis of the velocity of proboscis extension revealed a steady decrease in velocity across age that correlated well with other measures of locomotion 79. Because the release of neurotransmitter is found to increase at the CM9 NMJ during the same period 64, it is possible that the increase in neurotransmission is compensatory for the reduced muscle function. Kreko-Pierce and colleagues fed adult flies the S107 drug to improve CM9 muscle function during aging to see if this was sufficient to block the increase in neurotransmission 79. Studies from rodents have shown that the age-dependent oxidation of the ryanodine receptor (RyR) results in the dissociation of the FK506-BP2/Calstabin protein from the RyR resulting in impaired excitation:contraction coupling and reduced muscle contraction 80,81,82,83,84. The S107 drug re-establishes the binding of FKBP2-506/Calstabin to the oxidized RyR resulting in a reversal of the age-dependent declines in muscle function 84. Aged flies fed S107 for one week had a complete reversal of the declines in proboscis extension velocities and a reduction neurotransmission 79. In control experiments it was observed that feeding S107 to young flies had no effect on proboscis extension velocities or neurotransmission. These data support the model that the age-dependent increases in neurotransmission observed at the CM9 NMJ is in response to reduced muscle function and suggests the existence of a muscle-derived retrograde signal that normally informs the motor neuron about muscle contraction.
AGING, EXERCISE, AND NEUROTROPHINS
Given the important role of muscle-derived neurotrophin signaling on NMJ structure and function, it seems possible that changes in muscle-derived neurotrophin signaling during aging are responsible for the changes in synapse function and morphology. Although there is paucity of data surrounding NT expression during aging, there are studies showing that neurotrophin gene expression in muscles declines with age, including NT-3, NT-4, and BDNF 85,86,87,88,89, although gene encoding GDNF increases expression during aging 90,91. Thus it is possible that the change in neurotrophin gene expression in aging muscle contributes to the loss of synapse structure and function of the NMJ during aging. In support are the similar synaptic phenotypes of mice harboring mutations in the trkB gene (encoding the receptor for BDNF and NT-4) the NT-4 KO mouse 86,92. Because NT expression is sensitive to muscle activity, this model would predict that exercise should have positive effects on NMJ structure and function. This is consistent with what has been observed in rodent models where exercise has been found to reverse the age-related morphological changes of the NMJ including active zone structures and post-synaptic receptors (Figure 1B) 46,93,94. In addition to morphology, there is also evidence that exercise in aged animal leads to a more youthful functional profile 34. Taken together, these data support the model that exercise-dependent increases in NT gene expression in skeletal muscles is a significant contributor to the positive effects of exercise on synapse function and structure at the NMJ.
Currently it is unknown how muscle activity might increase NT gene expression. It is established that increased physical activity activates a number of important signaling systems within the muscle resulting in a change in muscle metabolism and cellular physiology to meet the demands of increased activity 95 (Figure 1C). For example, the increase in muscle contraction is predicted to result in an increase in the ratios of AMP:ATP and ADP:ATP leading to the activation of AMP Kinase (AMPK) 96,97. The activation of AMPK is known to increase the transcription of genes predominantly through the activation of the transcriptional co-factor PGC-1α (Figure 1C). It is currently unknown if this signaling system is responsible for the increases in NT expression in muscle observed after exercise. Interestingly, PGC-1α has been shown to be required for the increase in expression of the myokine ENDC5, which is cleaved and secreted as irisin from the muscle after exercise 98. In addition to changes in adipose tissues, increased peripheral irisin is able to increase BDNF expression throughout the brain 99. Perhaps increased peripheral irisin levels can also up-regulate BDNF expression in motor neurons providing the benefits of retrograde BDNF signaling via ENDC5.
It is also known that the increase in contraction will lead to an increase in cytosolic Ca2+ levels. In the muscle, this increase in calcium is known to activate CamKII leading to the phosphorylation and activation of the CREB transcription factor 100,101. Importantly, CREB binding sites are found in the promoter regions of NT-3, BDNF, and GDNF, although whether this signal transduction pathway is involved in the effects of exercise on NT expression has not been demonstrated 102,103,104,105. Thus, it’s possible that increased actions of the contractile machinery during exercise could lead to an increase in NT expression via the activation of CamKII and subsequent phosphorylation of CREB. In addition, exercise is also known to increase reactive oxygen species (ROS) leading to the activation of ROS-sensitive signaling systems such as MAPK, or by directly altering promote activity 106,107,108. It’s also possible that these signals must coincide in order to drive NT gene expression.
It’s important to consider how aging affects these exercise-related signaling systems and whether this plays a role in the changes in NT expression with age. The effects of oxidative stress on cellular physiology have been extensively reviewed 109, so we will focus our discussion on calcium signaling. Many studies have shown that calcium handling changes during aging in the muscle fiber leading to compromised contraction 110,111,112,113. Importantly, aged muscles have reported both a loss of L-type calcium channel function and impaired sarcoplasmic reticulum discharge during depolarization, which would predict that during contraction peak cytosolic calcium levels are reduced compared to young muscles, possibly leading to altered calcium signaling (i.e. CamKII) 111,112,113,114,115,116,117,118. Other studies suggest that resting cytosolic calcium signaling could be increased due to a calcium leak from the sarcoplasmic reticulum due to oxidation and CamKII phosphorylation of the ryanodine receptor 84,119. What effects these changes in calcium handling have on calcium-dependent signaling processes within the muscle cell, especially CamKII, should be a focus of future research.
Recall that expression of NT-3, NT-4, and BDNF genes all decline during aging, except for GDNF which has been reported to increase with age 85,86,87,88,89,90,91. This is also clearly different than what occurs during exercise when the expression of these NTs genes changes in unison. But it is interesting to note that GDNF expression, which has strong positive effects on neurotransmission 27, is up-regulated during aging. This suggests that the increase in neurotransmission observed at aged NMJs is the result of increased GDNF retrograde signaling. We would predict a similar scenario at the aging fly NMJ although the identity of the retrograde trophic signal is unknown. It is possible that the altered calcium signaling in the aging muscle is responsible for the increase in GDNF expression, similar to what occurs during exercise. But because the increased calcium with age is not accompanied with other potential signals generated by exercise, such as mechanical stress or an abrupt increase in reactive oxygen species, the response in terms of NT expression is incomplete. Because of the therapeutic potential of increased NT expression, it will be important to identify the important signaling systems involved in the responses of the muscle to exercise. This will include deciphering the signaling mechanisms important for the regulation of NT genes in the muscle in response to exercise. Targeting these mechanisms would be expected to help both the elderly patients struggling with mobility issues and patients suffering from neuromuscular disorders that target the NMJ such as amyotropic lateral sclerosis (ALS) and muscular dystrophy (MD).
Acknowledgments
The authors would like to thank Jorge Azpurua for comments on an earlier version of the manuscript.
Abbreviations
- BDNF
brain-derived neurotrophic factor
- BMP
bone morphogenic protein
- EDL
extensor digitorum longus
- GDNF
glial cell line-derived neurotrophic factor
- NMJ
neuromuscular junction
- NT
neurotrophin
- RyR
ryanodine receptor
References
- 1.Rai M, Demontis F. Systemic Nutrient and Stress Signaling via Myokines and Myometabolites. Annu Rev Physiol. 2016;78(1):85–107. doi: 10.1146/annurev-physiol-021115-105305. [DOI] [PubMed] [Google Scholar]
- 2.Demontis F, Piccirillo R, Goldberg AL, Perrimon N. Mechanisms of skeletal muscle aging: insights from Drosophila and mammalian models. Dis Model Mech. 2013;6(6):1339–1352. doi: 10.1242/dmm.012559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank CA. Homeostatic plasticity at the Drosophila neuromuscular junction. Neuropharmacology. 2013;78:63–74. doi: 10.1016/j.neuropharm.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deschenes MR. Motor unit and neuromuscular junction remodeling with aging. Curr Aging Sci. 2011;4:209–220. doi: 10.2174/1874609811104030209. [DOI] [PubMed] [Google Scholar]
- 5.Fitzsimonds RM, Poo MM. Retrograde signaling in the development and modification of synapses. Physiol Rev. 1998;78(1):143–170. doi: 10.1152/physrev.1998.78.1.143. [DOI] [PubMed] [Google Scholar]
- 6.Pitts EV, Potluri S, Hess DM, Balice-Gordon RJ. Neurotrophin and Trk-mediated signaling in the neuromuscular system. Int Anesthesiol Clin. 2006;44(2):21–76. doi: 10.1097/00004311-200604420-00004. [DOI] [PubMed] [Google Scholar]
- 7.Schuster CM, Davis GW, Fetter RD, Goodman CS. Genetic dissection of structural and functional components of synaptic plasticity. 1996;(4):641–654. doi: 10.1016/s0896-6273(00)80198-1. [DOI] [PubMed] [Google Scholar]
- 8.del Castillo J, Katz B. Quantal components of the end-plate potential. J Physiol. 1954;124(3):560–573. doi: 10.1113/jphysiol.1954.sp005129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aberle H, Haghighi AP, Fetter RD, McCabe BD, Magalhães TR, Goodman CS. wishful thinking encodes a BMP type II receptor that regulates synaptic growth in Drosophila. Neuron. 2002;33(4):545–558. doi: 10.1016/s0896-6273(02)00589-5. [DOI] [PubMed] [Google Scholar]
- 10.McCabe BD, Marqués G, Haghighi AP, Fetter RD, Crotty ML, Haerry TE, Goodman CS, O'Connor MB. The BMP homolog Gbb provides a retrograde signal that regulates synaptic growth at the Drosophila neuromuscular junction. Neuron. 2003;39(2):241–254. doi: 10.1016/s0896-6273(03)00426-4. [DOI] [PubMed] [Google Scholar]
- 11.Huang EJ, Reichardt LF. Neurotrophins: Roles in Neuronal Development and Function. Annu Rev Neurosci. 2001;24(1):677–736. doi: 10.1146/annurev.neuro.24.1.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henderson CE, Phillips HS, Pollock RA. GDNF: a potent survival factor for motoneurons present in peripheral nerve and muscle. Science. 1994;266(5187):1062–1064. doi: 10.1126/science.7973664. [DOI] [PubMed] [Google Scholar]
- 13.Henderson CE, Camu W, Mettling C. Neurotrophins promote motor neuron survival and are present in embryonic limb bud. Nature. 1993;363(6426):266–270. doi: 10.1038/363266a0. [DOI] [PubMed] [Google Scholar]
- 14.Springer JE, Seeburger JL, He J. cDNA sequence and differential mRNA regulation of two forms of glial cell line-derived neurotrophic factor in Schwann cells and rat skeletal muscle. Exp Neurol. 1995;131(1):47–52. doi: 10.1016/0014-4886(95)90006-3. [DOI] [PubMed] [Google Scholar]
- 15.Griesbeck O, Parsadanian AS, Sendtner M, Thoenen H. Expression of neurotrophins in skeletal muscle: quantitative comparison and significance for motoneuron survival and maintenance of function. J Neurosci Res. 1995;42(1):21–33. doi: 10.1002/jnr.490420104. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki H, Hase A, Miyata Y, Arahata K, Akazawa C. Prominent expression of glial cell line-derived neurotrophic factor in human skeletal muscle. J Comp Neurol. 1998;(3):303–312. doi: 10.1002/(sici)1096-9861(19981221)402:3<303::aid-cne2>3.3.co;2-9. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki H, Hase A, Kim BY, Miyata Y, Nonaka I, Arahata K, Akazawa C. Up-regulation of glial cell line-derived neurotrophic factor (GDNF) expression in regenerating muscle fibers in neuromuscular diseases. Neurosci Lett. 1998;257(3):165–167. doi: 10.1016/s0304-3940(98)00817-9. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen QT, Parsadanian AS, Snider WD, Lichtman JW. Hyperinnervation of neuromuscular junctions caused by GDNF overexpression in muscle. Science. 1998;279(5357):1725–1729. doi: 10.1126/science.279.5357.1725. [DOI] [PubMed] [Google Scholar]
- 19.Yan Q, Matheson C, Lopez OT. In vivo neurotrophic effects of GDNF on neonatal and adult facial motor neurons. Nature. 1995;373(6512):341–344. doi: 10.1038/373341a0. [DOI] [PubMed] [Google Scholar]
- 20.Zwick M, Teng L, Mu X, Springer JE, Davis BM. Overexpression of GDNF Induces and Maintains Hyperinnervation of Muscle Fibers and Multiple End-Plate Formation. Exp Neurol. 2001;171(2):342–350. doi: 10.1006/exnr.2001.7753. [DOI] [PubMed] [Google Scholar]
- 21.Keller-Peck CR, Feng G, Sanes JR, Yan Q, Lichtman JW, Snider WD. Glial cell line-derived neurotrophic factor administration in postnatal life results in motor unit enlargement and continuous synaptic remodeling at the neuromuscular junction. J Neurosci. 2001;21(16):6136–6146. doi: 10.1523/JNEUROSCI.21-16-06136.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poo MM. Neurotrophins as synaptic modulators. Nat Rev Neurosci. 2001;2(1):24–32. doi: 10.1038/35049004. [DOI] [PubMed] [Google Scholar]
- 23.Schinder AF, Poo M. The neurotrophin hypothesis for synaptic plasticity. Trends Neurosci. 2000;23(12):639–645. doi: 10.1016/s0166-2236(00)01672-6. [DOI] [PubMed] [Google Scholar]
- 24.Lohof AM, Ip NY, Poo MM. Potentiation of developing neuromuscular synapses by the neurotrophins NT-3 and BDNF. Nature. 1993;363(6427):350–353. doi: 10.1038/363350a0. [DOI] [PubMed] [Google Scholar]
- 25.Wang XH, Poo MM. Potentiation of developing synapses by postsynaptic release of neurotrophin-4. Neuron. 1997;19(4):825–835. doi: 10.1016/s0896-6273(00)80964-2. [DOI] [PubMed] [Google Scholar]
- 26.Boulanger LM, Poo MM. Presynaptic depolarization facilitates neurotrophin-induced synaptic potentiation. Nat Neurosci. 1999;2:346–351. doi: 10.1038/7258. [DOI] [PubMed] [Google Scholar]
- 27.Wang CY, Yang F, He X, Chow A, Du J, Russell JT, Lu B. Ca(2+) binding protein frequenin mediates GDNF-induced potentiation of Ca(2+) channels and transmitter release. Neuron. 2001;32(1):99–112. doi: 10.1016/s0896-6273(01)00434-2. [DOI] [PubMed] [Google Scholar]
- 28.Mantilla CB, Zhan W-Z, Sieck GC. Neurotrophins improve neuromuscular transmission in the adult rat diaphragm. Muscle Nerve. 2004;29(3):381–386. doi: 10.1002/mus.10558. [DOI] [PubMed] [Google Scholar]
- 29.Greising SM, Stowe JM, Sieck GC, Mantilla CB. Role of TrkB kinase activity in aging diaphragm neuromuscular junctions. Exp Gerontol. 2015;72:184–191. doi: 10.1016/j.exger.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frank CA, Kennedy MJ, Goold CP. Mechanisms underlying the rapid induction and sustained expression of synaptic homeostasis. Neuron. 2006;52(4):663–677. doi: 10.1016/j.neuron.2006.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Müller M, Davis GW. Transsynaptic Control of Presynaptic Ca. Curr Biol. 2012;22(12):1102–1108. doi: 10.1016/j.cub.2012.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waerhaug O, Dahl HA, Kardel K. Different effects of physical training on the morphology of motor nerve terminals in the rat extensor digitorum longus and soleus muscles. Anat Embryol. 1992;186(2):125–128. doi: 10.1007/bf00174949. [DOI] [PubMed] [Google Scholar]
- 33.Deschenes MR, Maresh CM, Crivello JF, Armstrong LE, Kraemer WJ, Covault J. The effects of exercise training of different intensities on neuromuscular junction morphology. J Neurocytol. 1993;22(8):603–615. doi: 10.1007/bf01181487. [DOI] [PubMed] [Google Scholar]
- 34.Fahim MA. Endurance exercise modulates neuromuscular junction of C57BL/6NNia aging mice. J Appl Physiol. 1997;83(1):59–66. doi: 10.1152/jappl.1997.83.1.59. [DOI] [PubMed] [Google Scholar]
- 35.Deschenes MR, Judelson DA, Kraemer WJ, Meskaitis VJ, Volek JS, Nindl BC, Harman FS, Deaver DR. Effects of resistance training on neuromuscular junction morphology. Muscle Nerve. 2000;23(10):1576–1581. doi: 10.1002/1097-4598(200010)23:10<1576::AID-MUS15>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 36.Deschenes MR, Kressin KA, Garratt RN, Leathrum CM, Shaffrey EC. Effects of exercise training on neuromuscular junction morphology and pre- to post-synaptic coupling in young and aged rats. Neuroscience. 2016;316:167–177. doi: 10.1016/j.neuroscience.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dorlöchter M, Irintchev A, Brinkers M, Wernig A. Effects of enhanced activity on synaptic transmission in mouse extensor digitorum longus muscle. J Physiol. 1991;436(1):283–292. doi: 10.1113/jphysiol.1991.sp018550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Funakoshi H, Belluardo N, Arenas E, Yamamoto Y, Casabona A, Persson H, Ibáñez CF. Muscle-derived neurotrophin-4 as an activity-dependent trophic signal for adult motor neurons. Science. 1995;268(5216):1495–1499. doi: 10.1126/science.7770776. [DOI] [PubMed] [Google Scholar]
- 39.Wehrwein EA, Roskelley EM, Spitsbergen JM. GDNF is regulated in an activity-dependent manner in rat skeletal muscle. Muscle Nerve. 2002;26(2):206–211. doi: 10.1002/mus.10179. [DOI] [PubMed] [Google Scholar]
- 40.Gómez-Pinilla F, Ying Z, Roy RR, Molteni R, Edgerton VR. Voluntary exercise induces a BDNF-mediated mechanism that promotes neuroplasticity. J Neurophysiol. 2002;88(5):2187–2195. doi: 10.1152/jn.00152.2002. [DOI] [PubMed] [Google Scholar]
- 41.Dupont-Versteegden EE, Houlé JD, Dennis RA, Zhang J, Knox M, Wagoner G, Peterson CA. Exercise-induced gene expression in soleus muscle is dependent on time after spinal cord injury in rats. Muscle Nerve. 2004;29(1):73–81. doi: 10.1002/mus.10511. [DOI] [PubMed] [Google Scholar]
- 42.McCullough MJ, Peplinski NG, Kinnell KR, Spitsbergen JM. Glial cell line-derived neurotrophic factor (GDNF) protein content in rat skeletal muscle is altered by increased physical activity in vivo and in vitro. Neuroscience. 2011;174:234–244. doi: 10.1016/j.neuroscience.2010.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCullough MJ, Gyorkos AM, Spitsbergen JM. Short-term exercise increases GDNF protein levels in spinal cord of young and old rats. Neuroscience. 2013;240:258–268. doi: 10.1016/j.neuroscience.2013.02.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gyorkos AM, Spitsbergen JM. GDNF content and NMJ morphology are altered in recruited muscles following high‐speed and resistance wheel training. Physiol Rep. 2014;2(2):e00235. doi: 10.1002/phy2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Willadt S, Nash M, Slater C. Age-related changes in the structure and function of mammalian neuromuscular junctions. Ann N Y Acad Sci. 2017;6:99. doi: 10.1016/0531-5565(92)90030-4. [DOI] [PubMed] [Google Scholar]
- 46.Valdez G, Tapia JC, Kang H, Clemenson GD Jr, Gage FH, Lichtman JW, Sanes JR. Attenuation of age-related changes in mouse neuromuscular synapses by caloric restriction and exercise. Proc Natl Acad Sci USA. 2010;107(33):14863–14868. doi: 10.1073/pnas.1002220107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jang YC, Lustgarten MS, Liu Y, Muller FL, Bhattacharya A, Liang H, Salmon AB, Brooks SV, Larkin L, Hayworth CR, Richardson A, Van Remmen H. Increased superoxide in vivo accelerates age-associated muscle atrophy through mitochondrial dysfunction and neuromuscular junction degeneration. FASEB J. 2010;24(5):1376–1390. doi: 10.1096/fj.09-146308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fujisawa K. Some observations on the skeletal musculature of aged rats-III. Abnormalities of terminal axons found in motor end-plates. . Exp Gerontol. 1976;11(1-2):43–47. doi: 10.1016/0531-5565(76)90010-3. [DOI] [PubMed] [Google Scholar]
- 49.Rosenheimer JL, Smith DO. Differential changes in the end-plate architecture of functionally diverse muscles during aging. J Neurophysiol. 1985;53(6):1567–1581. doi: 10.1152/jn.1985.53.6.1567. [DOI] [PubMed] [Google Scholar]
- 50.Gutmann E, Hanzlikova V. Basic mechanisms of aging in the neuromuscular system. Mech Ageing Dev. 1973;1(5):327–349. doi: 10.1016/0047-6374(72)90078-4. [DOI] [PubMed] [Google Scholar]
- 51.Rudolf R, Khan MM, Labeit S, Deschenes MR. Degeneration of neuromuscular junction in age and dystrophy. Front Aging Neurosci. 2014;6:99. doi: 10.3389/fnagi.2014.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sousa-Victor P, García-Prat L, Serrano AL, Perdiguero E, Muñoz-Cánoves P. Muscle stem cell aging: regulation and rejuvenation. Trends Endocrinol Metab. 2015;26(6):287–296. doi: 10.1016/j.tem.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Shigemoto K, Kubo S, Mori S, Yamada S, Akiyoshi T, Miyazaki T. Muscle weakness and neuromuscular junctions in aging and disease. Geriatr Gerontol Int . 2010;10(Suppl 1):S137–47. doi: 10.1111/j.1447-0594.2010.00608.x. [DOI] [PubMed] [Google Scholar]
- 54.Wood SJ, Slater CR. Safety factor at the neuromuscular junction. Prog Neurobiol. 2001;64(4):393–429. doi: 10.1016/s0301-0082(00)00055-1. [DOI] [PubMed] [Google Scholar]
- 55.Anis NA, Robbins N. Acetylcholine receptors at mature and aged mouse neuromuscular junctions. Neurobiol Aging. 1988;9:303–306. doi: 10.1016/s0197-4580(88)80069-1. [DOI] [PubMed] [Google Scholar]
- 56.Willadt S, Nash M, Slater CR. Age-related fragmentation of the motor endplate is not associated with impaired neuromuscular transmission in the mousediaphragm. Sci Rep. 2016;6:24849. doi: 10.1038/srep24849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Li Y, Lee YI, Thompson WJ. Changes in Aging Mouse Neuromuscular Junctions Are Explained by Degeneration and Regeneration of Muscle Fiber Segments at the Synapse. J Neurosci. 2011;31(42):14910–14919. doi: 10.1523/JNEUROSCI.3590-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hepple RT, Rice CL. Innervation and neuromuscular control in ageing skeletal muscle. J Physiol. 2015;594(8):1965–1978. doi: 10.1242/dev.038711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wokke JH, Jennekens FG, van den Oord CJ, Veldman H, Smit LM, Leppink GJ. Morphological changes in the human end plate with age. J Neurol Sci. 1990;95(3):291–310. doi: 10.1016/0022-510x(90)90076-y. [DOI] [PubMed] [Google Scholar]
- 60.Oda K. Age changes of motor innervation and acetylcholine receptor distribution on human skeletal muscle fibres. J Neurol Sci. 1984;66(2-3):327–338. doi: 10.1016/0022-510x(84)90021-2. [DOI] [PubMed] [Google Scholar]
- 61.Jones RA, Harrison C, Eaton SL, Llavero Hurtado M, Graham LC, Alkhammash L, Oladiran OA, Gale A, Lamont DJ, Simpson H, Simmen MW, Soeller C, Wishart TM, Gillingwater TH. Cellular and Molecular Anatomy of the Human Neuromuscular Junction. Cell Rep. 2017;21(9):2348–2356. doi: 10.1016/j.celrep.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Banker BQ, Kelly SS, Robbins N. Neuromuscular transmission and correlative morphology in young and old mice. J Physiol. 1983;339(1):355–377. doi: 10.1113/jphysiol.1983.sp014721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kelly SS. The effect of age on neuromuscular transmission. J Physiol. 1978;274(1):51–62. doi: 10.1113/jphysiol.1978.sp012133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mahoney RE, Rawson JM, Eaton BA. An age-dependent change in the set point of synaptic homeostasis. J Neurosci. 2014;34(6):2111–2119. doi: 10.1523/JNEUROSCI.3556-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Frank CA, Pielage J, Davis GW. A presynaptic homeostatic signaling system composed of the Eph receptor, ephexin, Cdc42, and CaV2.1 calcium channels. . Neuron. 2009;61(4):556–569. doi: 10.1016/j.neuron.2008.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Petersen SA, Fetter RD, Noordermeer JN, Goodman CS, DiAntonio A. Genetic analysis of glutamate receptors in Drosophila reveals a retrograde signal regulating presynaptic transmitter release. Neuron. 1997;19(6):1237–1248. doi: 10.1016/s0896-6273(00)80415-8. [DOI] [PubMed] [Google Scholar]
- 67.Davis GW, DiAntonio A, Petersen SA, Goodman CS. Postsynaptic PKA controls quantal size and reveals a retrograde signal that regulates presynaptic transmitter release in Drosophila. Neuron. 1998;20(2):305–315. doi: 10.1016/s0896-6273(00)80458-4. [DOI] [PubMed] [Google Scholar]
- 68.Cull-Candy SG, Miledi R, Uchitel OD. Diffusion of acetylcholine in the synaptic cleft of normal and myasthenia gravis human endplates. Nature. 1980;286(5772):500–502. doi: 10.1038/286500a0. [DOI] [PubMed] [Google Scholar]
- 69.Cull-Candy SG, Miledi R, Trautmann A, Uchitel OD. On the release of transmitter at normal, myasthenia gravis and myasthenic syndrome affected human end-plates. J Physiol. 1980;299(1):621–638. doi: 10.1113/jphysiol.1980.sp013145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Plomp JJ, van Kempen GT, Molenaar PC. Adaptation of quantal content to decreased postsynaptic sensitivity at single endplates in alpha-bungarotoxin-treated rats. J Physiol. 1992;458(1):487–499. doi: 10.1113/jphysiol.1992.sp019429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sandrock AW Jr, Dryer SE, Rosen KM, Gozani SN, Kramer R, Theill LE, Fischbach GD. Maintenance of acetylcholine receptor number by neuregulins at the neuromuscular junction in vivo. Science. 1997;276(5312):599–603. doi: 10.1126/science.276.5312.599. [DOI] [PubMed] [Google Scholar]
- 72.Penney J, Tsurudome K, Liao EH, Elazzouzi F, Livingstone M, Gonzalez M, Sonenberg N, Haghighi AP. TOR Is Required for the Retrograde Regulation of Synaptic Homeostasisat the Drosophila Neuromuscular Junction. Neuron. 2012;74(1):166–178. doi: 10.1016/j.neuron.2012.01.030. [DOI] [PubMed] [Google Scholar]
- 73.Goel P, Li X, Dickman D. Disparate Postsynaptic Induction Mechanisms Ultimately Converge to Drive the Retrograde Enhancement of Presynaptic Efficacy. Cell Rep. 2017;21(9):2339–2347. doi: 10.1016/j.celrep.2017.10.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu J, Zhang B, Lei H, Feng Z, Liu J, Hsu AL, Xu XZ. Functional Aging in the Nervous System Contributes to Age-Dependent Motor Activity Decline in C. elegans. . Cell Metab. 2013;18(3):392–402. doi: 10.1016/j.cmet.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li LB, Lei H, Arey RN, Li P, Liu J, Murphy CT, Xu XZ, Shen K. The Neuronal Kinesin UNC-104/KIF1A Is a Key Regulator of Synaptic Aging and Insulin Signaling-Regulated Memory. Curr Biol. 2016;26(5):605–615. doi: 10.1016/j.cub.2015.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kelly SS, Robbins N. Progression of age changes in synaptic transmission at mouse neuromuscular junctions. J Physiol. 1983;343(1):375–383. doi: 10.1113/jphysiol.1983.sp014898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ivannikov MV, Van Remmen H. Sod1 gene ablation in adult mice leads to physiological changes at the neuromuscular junction similar to changes that occur in old wild-type mice. Free Radic Biol Med. 2015;84:254–262. doi: 10.1016/j.freeradbiomed.2015.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schwarz O, Bohra AA, Liu X. Motor control of Drosophila feeding behavior. Elife. 2017;6:e19892. doi: 10.7554/eLife.19892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kreko-Pierce T, Azpurua J, Mahoney RE, Eaton BA. Extension of Health Span and Life Span in Drosophilaby S107 Requires the calstabinHomologue FK506-BP2. J Biol Chem. 2016;291(50):26045–26055. doi: 10.1074/jbc.M116.758839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ondrias K, Marx SO, Gaburjakova M, Marks AR. FKBP12 modulates gating of the ryanodine receptor/calcium release channel. Ann N Y Acad Sci. 1998;853(1):149–156. doi: 10.1111/j.1749-6632.1998.tb08263.x. [DOI] [PubMed] [Google Scholar]
- 81.Umanskaya A, Santulli G, Xie W, Andersson DC, Reiken SR, Marks AR. Genetically enhancing mitochondrial antioxidant activity improves muscle function in aging. Proc Natl Acad Sci U S A. 2014;111(42):15250–15255. doi: 10.1073/pnas.1412754111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wehrens XH, Lehnart SE, Reiken S, van der Nagel R, Morales R, Sun J, Cheng Z, Deng SX, de Windt LJ, Landry DW, Marks AR. Enhancing calstabin binding to ryanodine receptors improves cardiac and skeletal muscle function in heart failure. Proc Natl Acad Sci USA. 2005;102(27):9607–9612. doi: 10.1073/pnas.0500353102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bellinger AM, Reiken S, Dura M, Murphy PW, Deng SX, Landry DW, Nieman D, Lehnart SE, Samaru M, LaCampagne A, Marks AR. Remodeling of ryanodine receptor complex causes "leaky" channels: A molecular mechanism for decreased exercise capacity. Proc Natl Acad Sci USA. 2008;105(6):2198–2202. doi: 10.1073/pnas.0711074105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Andersson DC, Betzenhauser MJ, Reiken S, Meli AC, Umanskaya A, Xie W, Shiomi T, Zalk R, Lacampagne A, Marks AR. Ryanodine Receptor Oxidation Causes Intracellular Calcium Leak and Muscle Weakness in Aging. Cell Metab. 2011;14(2):196–207. doi: 10.1016/j.cmet.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ming Y, Bergman E, Edström E, Ulfhake B. Reciprocal changes in the expression of neurotrophin mRNAs in target tissues and peripheral nerves of aged rats. Neurosci Lett. 1999;273(3):187–190. doi: 10.1016/s0304-3940(99)00655-2. [DOI] [PubMed] [Google Scholar]
- 86.Kulakowski SA, Parker SD, Personius KE. Reduced TrkB expression results in precocious age-like changes in neuromuscular structure, neurotransmission, and muscle function. J Appl Physiol. 2011;111(3):844–852. doi: 10.1152/japplphysiol.00070.2011. [DOI] [PubMed] [Google Scholar]
- 87.Personius KE, Parker SD. TrkB expression at the neuromuscular junction is reduced during aging. Muscle Nerve. 2012;47(4):532–538. doi: 10.1002/mus.23616. [DOI] [PubMed] [Google Scholar]
- 88.Johnson H, Hokfelt T, Ulfhake B. Expression of p75(NTR), trkB and trkC in nonmanipulated and axotomized motoneurons of aged rats. Mol Brain Res. 1999;69(1):21–34. doi: 10.1016/s0169-328x(99)00068-6. [DOI] [PubMed] [Google Scholar]
- 89.Johnson H, Hokfelt T, Ulfhake B. Decreased expression of TrkB and TrkC mRNAs in spinal motoneurons of aged rats. Eur J Neurosci. 1996;8(3):494–499. doi: 10.1111/j.1460-9568.1996.tb01233.x. [DOI] [PubMed] [Google Scholar]
- 90.Ming Y, Bergman E, Edström E, Ulfhake B. Evidence for increased GDNF signaling in aged sensory and motor neurons. Neuroreport. 1999;10(7):1529–1535. doi: 10.1097/00001756-199905140-00025. [DOI] [PubMed] [Google Scholar]
- 91.Trupp M, Rydén M, Jörnvall H. Peripheral expression and biological activities of GDNF, a new neurotrophic factor for avian and mammalian peripheral neurons. J Cell Biol. 1995;130(1):137–148. doi: 10.1083/jcb.130.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Belluardo N, Westerblad H, Mudó G, Casabona A, Bruton J, Caniglia G, Pastoris O, Grassi F, Ibáñez CF. Neuromuscular Junction Disassembly and Muscle Fatigue in Mice Lacking Neurotrophin-4. Mol Cell Neurosci. 2001;18(1):56–67. doi: 10.1006/mcne.2001.1001. [DOI] [PubMed] [Google Scholar]
- 93.Nishimune H, Numata T, Chen J, Aoki Y, Wang Y, Starr MP, Mori Y, Stanford JA. Active Zone Protein Bassoon Co-Localizes with Presynaptic Calcium Channel, Modifies Channel Function, and Recovers from Aging Related Loss by Exercise. PLoS ONE. 2012;7(6):e38029. doi: 10.1371/journal.pone.0038029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cheng A, Morsch M, Murata Y, Ghazanfari N, Reddel SW, Phillips WD. Sequence of Age-Associated Changes to the Mouse Neuromuscular Junction and the Protective Effects of Voluntary Exercise. PLoS ONE. 2013;8(7):e67970. doi: 10.1371/journal.pone.0067970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Egan B, Zierath JR. Exercise Metabolism and the Molecular Regulation of Skeletal Muscle Adaptation. Cell Metab. 2013;17(2):162–184. doi: 10.1016/j.cmet.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 96.Jørgensen SB, Richter EA, Wojtaszewski JFP. Role of AMPK in skeletal muscle metabolic regulation and adaptation in relation to exercise. J Physiol. 2006;574(1):17–31. doi: 10.1113/jphysiol.2006.109942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jessen N, Sundelin EIO, Møller AB. AMP kinase in exercise adaptation of skeletal muscle. Drug Discov Today. 2014;19(7):999–1002. doi: 10.1016/j.drudis.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 98.Boström P, Wu J, Jedrychowski MP, Korde A, Ye L, Lo JC, Rasbach KA, Boström EA, Choi JH, Long JZ, Kajimura S, Zingaretti MC, Vind BF, Tu H, Cinti S, Højlund K, Gygi SP, Spiegelman BM. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481(7384):463–468. doi: 10.1038/nature10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wrann CD, White JP, Salogiannnis J, Laznik-Bogoslavski D, Wu J, Ma D, Lin JD, Greenberg ME, Spiegelman BM. Exercise Induces Hippocampal BDNF through a PGC-1α/FNDC5 Pathway. Cell Metab. 2013;18(5):649–659. doi: 10.1016/j.cmet.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Egan B, Carson BP, Garcia-Roves PM, Chibalin AV, Sarsfield FM, Barron N, McCaffrey N, Moyna NM, Zierath JR, O‘Gorman DJ. Exercise intensity-dependent regulation of peroxisome proliferator-activated receptor γ coactivator-1α mRNA abundance is associated with differential activation of upstream signalling kinases in human skeletal muscle. J Physiol . 2010;588(Pt 10):1779–1790. doi: 10.1113/jphysiol.2010.188011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rose AJ, Kiens B, Richter EA. Ca 2+-calmodulin-dependent protein kinase expression and signalling in skeletal muscle during exercise. J Physiol. 2006;574(3):889–903. doi: 10.1113/jphysiol.2006.111757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Saavedra A, Baltazar G, Duarte EP. Driving GDNF expression: The green and the red traffic lights. Prog Neurobiol. 2008;86(3):186–215. doi: 10.1016/j.pneurobio.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 103.Choi-Lundberg DL, Bohn MC. Ontogeny and distribution of glial cell line-derived neurotrophic factor (GDNF) mRNA in rat. Dev Brain Res. 1995;85(1):80–88. doi: 10.1016/0165-3806(94)00197-8. [DOI] [PubMed] [Google Scholar]
- 104.Baecker PA, Lee WH, Verity AN, Eglen RM, Johnson RM. Characterization of a promoter for the human glial cell line-derived neurotrophic factor gene. Brain Res Mol Brain Res. 1999;69(2):209–222. doi: 10.1016/s0169-328x(99)00106-0. [DOI] [PubMed] [Google Scholar]
- 105.Heinrich G. A novel BDNF gene promoter directs expression to skeletal muscle. BMC Neurosci. 2003;4:11. doi: 10.1186/1471-2202-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Milton VJ, Jarrett HE, Gowers K, Chalak S, Briggs L, Robinson IM, Sweeney ST. Oxidative stress induces overgrowth of the Drosophila neuromuscular junction. Proc Natl Acad Sci U S A. 2011;108(42):17521–17526. doi: 10.1073/pnas.1014511108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Egan B, Hawley JA, Zierath JR. SnapShot: Exercise Metabolism. Cell Metab. 2016;24(2):342–342. doi: 10.1016/j.cmet.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 108.Lu T, Pan Y, Kao SY, Li C, Kohane I, Chan J, Yankner BA. Gene regulation and DNA damage in the ageing human brain. Nature. 2004;429:883–891. doi: 10.1038/nature02661. [DOI] [PubMed] [Google Scholar]
- 109.Schieber M, Chandel NS. ROS Function in Redox Signaling and Oxidative Stress. Curr Biol. 2014;24(10):R453–R462. doi: 10.1016/j.cub.2014.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Delbono O. Expression and regulation of excitation-contraction coupling proteins in aging skeletal muscle. Curr Aging Sci. 2011;4(3):248–259. doi: 10.2174/1874609811104030248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lamboley CR, Wyckelsma VL, Dutka TL, McKenna MJ, Murphy RM, Lamb GD. Contractile properties and sarcoplasmic reticulum calcium content in type I and type II skeletal muscle fibres in active aged humans. J Physiol. 2015;593(11):2499–2514. doi: 10.1113/jp270179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Payne AM, Jimenez-Moreno R, Wang ZM, Messi ML, Delbono O. Role of Ca2+, membrane excitability, and Ca2+ stores in failing muscle contraction with aging. Exp Gerontol. 2009;44(4):261–273. doi: 10.1016/j.exger.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Russ DW, Wills AM, Boyd IM, Krause J. Experimental Gerontology. Exp Gerontol. 2014;50:40–44. doi: 10.1016/j.exger.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 114.Wang ZM, Messi ML, Delbono O. L-Type Ca(2+) channel charge movement and intracellular Ca(2+) in skeletal muscle fibers from aging mice. Biophys J. 2000;78(4):1947–1954. doi: 10.1016/s0006-3495(00)76742-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Luin E, Lorenzon P, Wernig A, Ruzzier F. Calcium current kinetics in young and aged human cultured myotubes. Cell Calcium. 2008;44(6):554–566. doi: 10.1016/j.ceca.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 116.Delbono O, O'Rourke KS, Ettinger WH. Excitation-calcium release uncoupling in aged single human skeletal muscle fibers. J Membr Biol. 1995;148(3):211–222. doi: 10.1007/bf00235039. [DOI] [PubMed] [Google Scholar]
- 117.Weisleder N, Brotto M, Komazaki S, Pan Z, Zhao X, Nosek T, Parness J, Takeshima H, Ma J. Muscle aging is associated with compromised Ca 2+spark signaling and segregated intracellular Ca 2+release. J Cell Biol. 2006;174(5):639–645. doi: 10.1083/jcb.200604166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang ZM, Tang S, Messi ML, Yang JJ, Delbono O. Residual sarcoplasmic reticulum Ca2+ concentration after Ca2+ release in skeletal myofibers from young adult and old mice. Pflugers Arch. 2012;463(4):615–624. doi: 10.1007/s00424-012-1073-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Guo X, Yuan S, Liu Z, Fang Q. Oxidation- and CaMKII-mediated sarcoplasmic reticulum Ca(2+) leak triggers atrial fibrillation in aging. J Cardiovasc Electrophysiol. 2014;25(6):645–652. doi: 10.1111/jce.12395. [DOI] [PubMed] [Google Scholar]