Abstract
Medial patellofemoral ligament (MPFL) reconstruction is the treatment of choice for recurrent patellofemoral instability. Although attention to MPFL reconstruction in the orthopaedic literature has increased dramatically in recent years, there is no clear consensus on surgical technique, graft option, or method of fixation. Nevertheless, most studies have shown improved pain scores and low rates of recurrent dislocation in patients after surgery. Despite the early success of MPFL reconstruction, complications may occur more frequently than previously appreciated and include patellar fracture, postoperative instability, and loss of flexion. This article describes our technique for double-bundle MPFL reconstruction with an allograft while highlighting certain aspects of the procedure that are critical for achieving favorable outcomes. The main advantages of the technique include strong patellar fixation with suture anchors and anatomic graft placement at the origin and insertion of the native MPFL. In our experience, this method of reconstruction has been safe, reproducible, and effective in the treatment of patients with patellar instability.
Patellar dislocations account for approximately 3% of all knee injuries and may lead to medial patellofemoral ligament (MPFL) injury, recurrent instability, and premature arthritis.1, 2, 3 Although many factors contribute to patellofemoral instability, the MPFL is the most important restraint to lateral patellar translation.4 In complete patellar dislocations, the MPFL is frequently torn at its insertion on the superior-medial patella.5 However, midsubstance tears and injuries at the femoral attachment point are common as well.6 In either case, MPFL reconstruction is necessary to restore normal patellar stability and prevent recurrent dislocation.7 The indications for MFPL reconstruction are presented in Table 1. Although surgery is recommended in patients with ongoing patellar instability and laxity on physical examination despite conservative management, reconstruction is controversial in first-time dislocators.8 Recurrent instability may occur in 17% to 40% of patients who have been treated nonoperatively for first-time dislocations.2, 9 Young athletes and high-risk patients may benefit from surgery after a single patellar dislocation.10, 11, 12
Table 1.
Indications for MPFL Reconstruction
| Recurrent (≥2) patellar dislocations |
| Symptoms of ongoing patellar instability |
| Excessive lateral patellar laxity on physical examination |
| Failure to improve with nonoperative management |
| Concurrent osteochondral injury |
| Acute MPFL bony avulsion |
MPFL, medial patellofemoral ligament.
Several methods of MPFL reconstruction have been described.1, 9 In addition, various options are available for graft choice, patellar fixation, and femoral fixation. Although each has its advantages and disadvantages, there is currently insufficient evidence to recommend any of these grafts or fixation methods over the others.13 Despite the success of MPFL reconstruction in treating patellar instability, complication rates as high as 26.1% have been reported in the literature.14 In a meta-analysis of 25 studies, up to 16% of patients required reoperation.14 Attention to technique may help prevent complications in MPFL reconstruction, such as patellar fracture, postoperative instability, apprehension, loss of flexion, and pain. The purpose of this article was to describe our technique for double-bundle MPFL reconstruction with allograft using suture anchors for patellar fixation and an interference screw for femoral fixation.
Surgical Technique
A demonstration of the double-bundle MPFL reconstruction technique with allograft is available in Video 1. Important pearls and pitfalls are summarized in Table 2.
Table 2.
Technical Pearls and Pitfalls
| Pearls |
| Graft fixation to the patella can be reinforced by tying sutures at the end of the graft to the surrounding soft tissues. |
| The femoral tunnel placement can be adjusted if necessary after evaluation of isometry. |
| A clamp should be placed underneath the graft at the femoral incision site to prevent over-tightening. |
| Using a true lateral view, the surgeon should identify the Schöttle point for femoral tunnel placement with the help of an MPFL template. |
| The surgeon should aim the femoral Beath pin anteriorly and proximally to increase tunnel length and avoid the notch or posterior cortex of the femur. |
| Pitfalls |
| Penetration of the anterior cortex is possible while drilling the patellar tunnel. Excessive and/or incorrect drilling increases the risk of patellar fracture. |
| Over-tightening the graft may lead to excessive medial restraint. |
| Disruption of the vastus medialis on the MPFL is possible owing to superficial dissection between the patellar and femoral incisions. |
| Proximal pin placement on the femur can occur, resulting in tightness during knee flexion. |
| The femoral tunnel should be not reamed through the lateral cortex. |
MPFL, medial patellofemoral ligament.
Preoperative Assessment
History and Physical Examination
Patellar dislocations typically occur when the femur internally rotates during pivoting movements.1, 4 In some cases, there may be a history of direct trauma to the medial aspect of the knee.2 Most patellar dislocations occur in adolescents or young adults during athletic activity.15 Physical examination may show a positive patellar apprehension test, a positive J sign, and more than 2 quadrants of lateral patellar translation.16
Imaging Studies
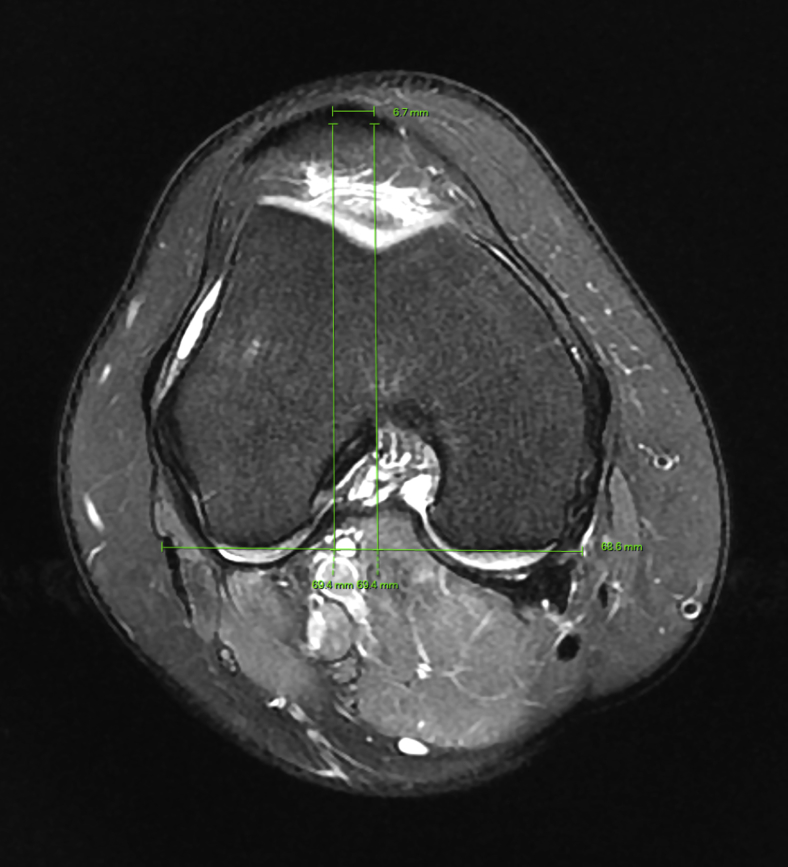
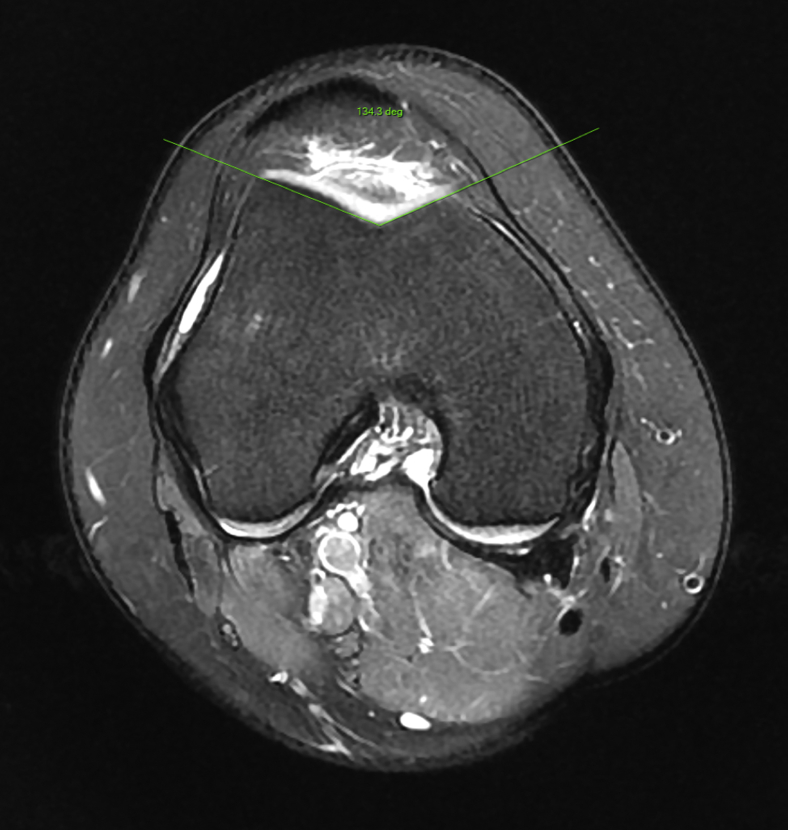
Plain radiographs of the knee including anteroposterior, lateral, and axial patellar views are used to identify fracture, osteochondral loose bodies, arthritis, and malalignment.16 Avulsion fractures of the MPFL may occur at the middle third of the patella.5 Loose bodies off the medial patellar facet or lateral trochlea may also be seen.6 A crossing sign on lateral views suggests trochlear dysplasia.16 In addition, patellar height may be measured according to the Caton and Deschamps method.17 MPFL tears are then confirmed with magnetic resonance imaging (Fig 1). The patellar tilt is assessed, and the tibial tubercle–trochlear groove (TT-TG) distance is measured (Fig 2). The TT-TG distance is a measurement of lateralization of the tibial tubercle (a normal distance is 9-13 mm).18 A TT-TG distance exceeding 20 mm requires distal realignment with anterior medialization of the tibial tubercle at the time of MPFL reconstruction.18 A cross-sectional view is also used to measure the sulcus angle (Fig 3). Of note, trochleoplasty may be considered in patients with severe trochlear dysplasia.19
Fig 1.
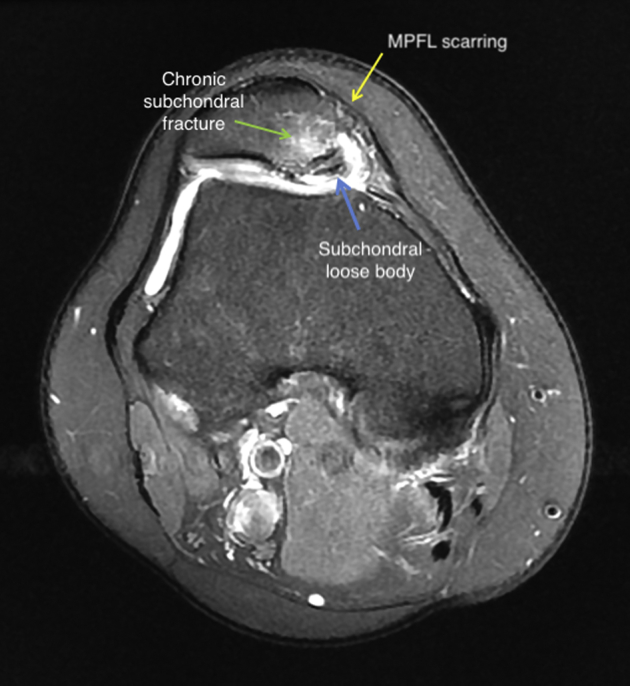
A preoperative cross-sectional view of the right knee on magnetic resonance imaging shows scarring at the anterior aspect of the medial patellofemoral ligament (MPFL). A subchondral loose body is seen between the medial patellar facet and medial femoral condyle. The articular cartilage of the medial facet is commonly injured after patellar dislocation. Magnetic resonance imaging is used to confirm injury to the MPFL and diagnose any associated pathology. Plain radiographs of the knee should also be obtained including anteroposterior, lateral, and axial patellar views.
Fig 2.
A preoperative cross-sectional view of the right knee on magnetic resonance imaging is used to measure the tibial tubercle–trochlear groove (TT-TG) distance. A line is first drawn along the posterior femoral condyles, and 2 perpendicular lines bisect the trochlear groove sulcus and the tibial tuberosity. The TT-TG distance is normally less than 9 to 13 mm.18 It is considered borderline at 15 to 20 mm and abnormal if greater than 20 mm. A TT-TG distance exceeding 20 mm requires distal realignment with an osteotomy and anterior medialization of the tibial tubercle before medial patellofemoral ligament reconstruction.18
Fig 3.
A preoperative cross-sectional view of the right knee on magnetic resonance imaging is used to measure the sulcus angle. A normal sulcus angle is approximately 138°, whereas an angle greater than 145° suggests trochlear dysplasia.19 Trochlear dysplasia may also be identified on a true lateral radiograph by the presence of a crossing sign, in which the floor of the trochlea crosses the anterior border of both femoral condyles.19 Trochleoplasty may be considered in patients with severe trochlear dysplasia.19 In addition, trochlear dysplasia is an important predictor of residual patellofemoral instability after medial patellofemoral ligament reconstruction.20 The Caton and Deschamps method may also be used to measure patellar height.17 A ratio of 1.2 or greater indicates patella alta. If present, a tibial tubercle osteotomy should be considered.19
Patient Positioning
The patient is positioned supine. A small bump may be placed under the hip and knee to maintain slight flexion. The surgical site is then prepared and draped in the usual sterile fashion.
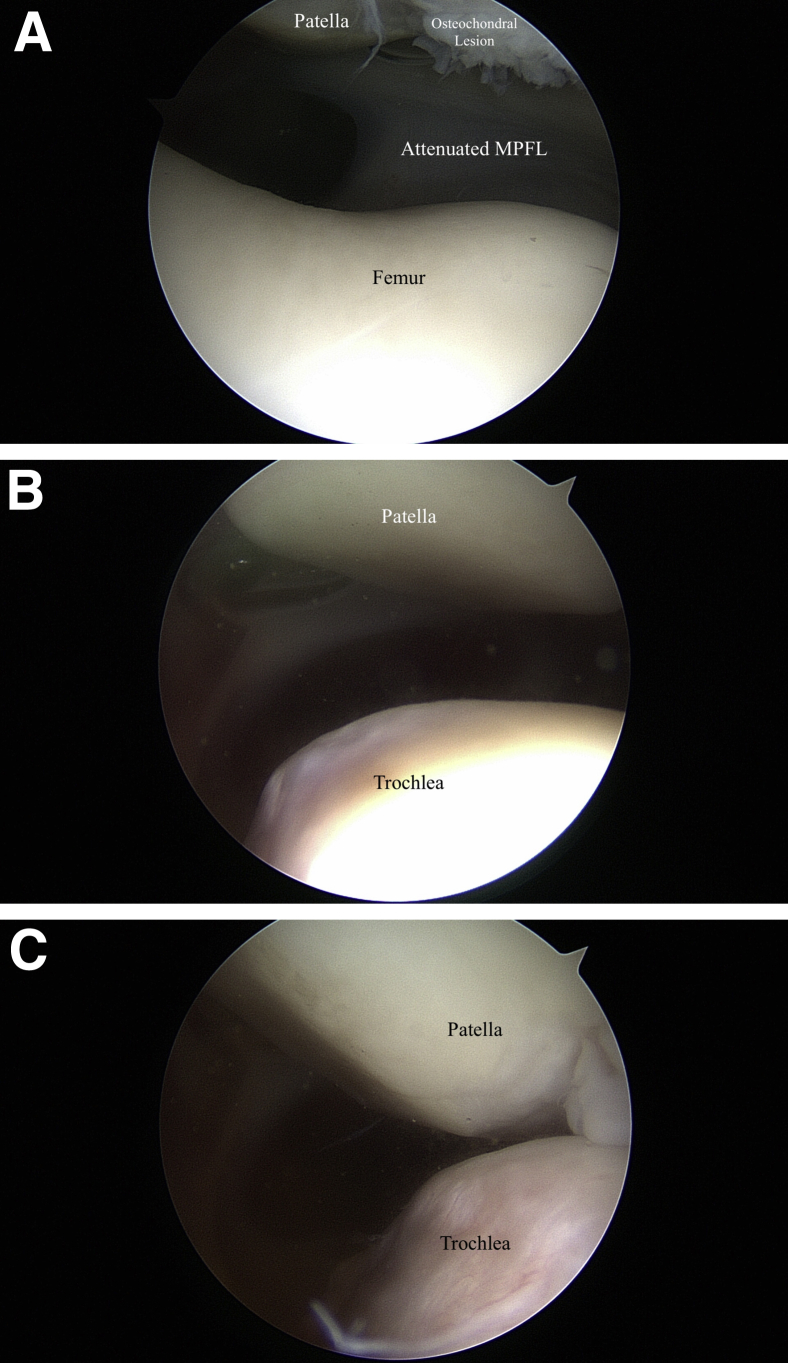
Knee Arthroscopy
A diagnostic arthroscopy is performed before MPFL reconstruction to assess patellofemoral tracking and identify concomitant pathology (Fig 4). The patellofemoral compartment is assessed for articular cartilage damage. Loose bodies are removed, and unstable cartilage flaps are treated with debridement or chondroplasty.
Fig 4.
A standard diagnostic arthroscopy is performed before medial patellofemoral ligament (MPFL) reconstruction to assess patellofemoral tracking and identify loose bodies or cartilage flaps. (A) Arthroscopic photograph of the patellofemoral joint of the right knee. The medial facet cartilage shows a small osteochondral lesion with fraying of the capsule and retinacular tissue at the medial facet attachment. (B) Arthroscopic photograph through the anterolateral portal of the lateral patella and trochlea. (C) Lateral subluxation of the patella relative to the trochlea while applying lateral force.
Graft Preparation
Several graft options are available for MPFL reconstruction including gracilis-semitendinosus autograft, cadaveric allograft, and synthetic graft.13 In this Technical Note, we describe the use of a hamstring allograft. The 2 ends of the allograft are whipstitched using No. 2-0 FiberWire sutures (Arthrex) to a length of 10 mm and tapered to facilitate insertion into the patellar tunnels. The graft needs to be at least 200 to 240 mm in length for the double-bundle technique and is typically 5 to 6 mm wide. A double-bundle configuration is often used to anatomically approximate the MPFL insertion as it fans out on the proximal two-thirds of the patella.4
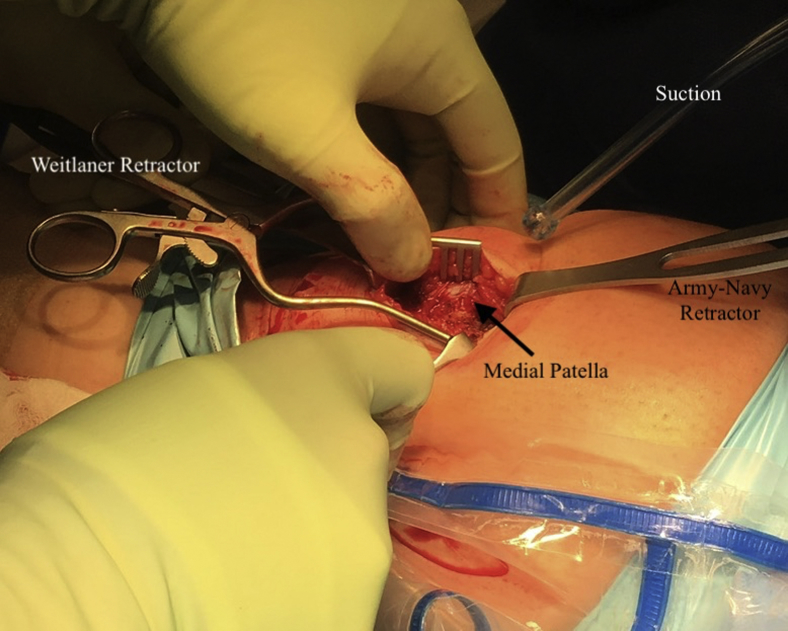
Patellar Tunnel Placement
A 3-cm longitudinal incision is made at the junction of the medial and middle thirds of the patella in line with the medial border of the patellar tendon distally. The medial patellar retinaculum and native MPFL are dissected off the patella, leaving the joint capsule layer intact (Fig 5). Two 4.5-mm drill holes are then placed in the medial patella (Fig 6). Under fluoroscopic guidance, a proximal guide pin is placed transversely, 5 mm from the superior pole, adjacent to the articular margin. A distal guide pin is placed parallel to the proximal pin at a point two-thirds down the length of the patella. The 2 patellar tunnels are then drilled using a 4-mm cannulated reamer to a depth of approximately 20 to 25 mm.
Fig 5.
Intraoperative photograph of the medial patellar approach and dissection. First, a 5-cm longitudinal incision is made at the junction of the medial and middle thirds of the patella. The medial patellar retinaculum and native medial patellofemoral ligament are identified and released, whereas the underlying joint capsule is left intact.
Fig 6.
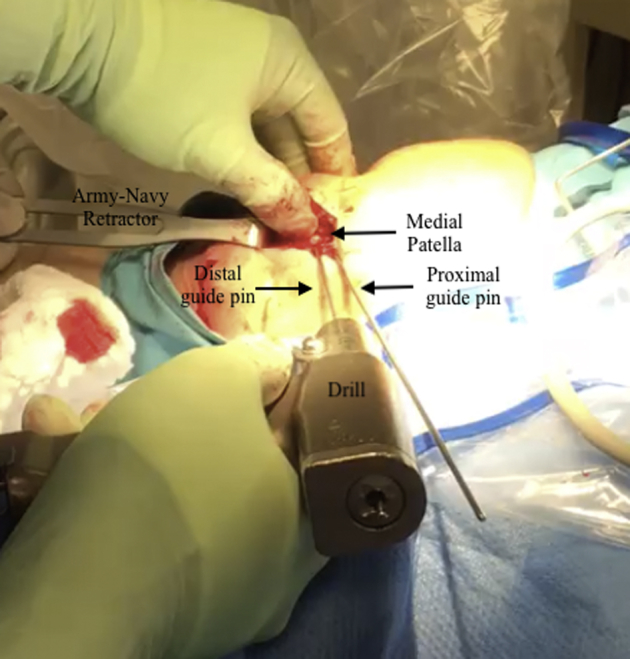
Intraoperative photograph of 2 guide pins placed on the anterior surface of the medial patella. The proximal guide pin is placed transversely, 5 mm from the superior pole, adjacent to the articular margin. The second guide pin is then placed parallel and approximately 1 to 2 cm distal to the proximal pin. Proper placement of the guide pins is confirmed on fluoroscopy. The guide pins are then over-reamed using a 4-mm cannulated reamer to a depth of 20 to 25 mm. Care should be taken so that the drill does not penetrate the anterior cortex of the patella.
Allograft Fixation to Patella
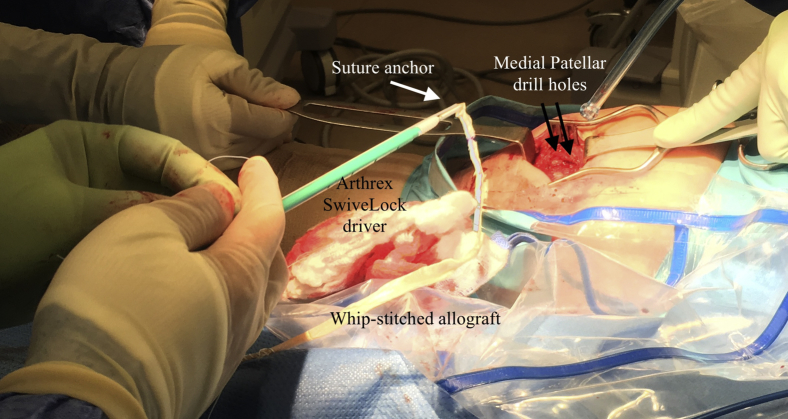
In this Technical Note, we describe the use of Arthrex SwiveLock suture anchors for allograft fixation to the patella. The suture tails from 1 end of the whipstitched allograft are passed through the eyelet of the first suture anchor, which is then inserted into the proximal drill hole (Fig 7). The suture tails from the other end of the allograft are then similarly passed through the eyelet of a second suture anchor, which is inserted into the distal drill hole. After removal of the SwiveLock drivers, each free suture is passed through the graft using a free needle and tied down to reinforce patellar fixation. With the 2 ends of the allograft fixed to the medial patella, a double-bundle loop has been created (Fig 8). The allograft may be covered with moist gauze while the femoral tunnel is subsequently being prepared.
Fig 7.
Intraoperative photograph of the first SwiveLock suture anchor used for allograft fixation to the patella. The suture tails from 1 end of the whipstitched hamstring allograft are passed through the eyelet of the suture anchor, which is then inserted into the proximal patellar drill hole. The suture tails from the other end of the hamstring allograft are then similarly passed through the eyelet of a second suture anchor, which is inserted into the distal patellar drill hole.
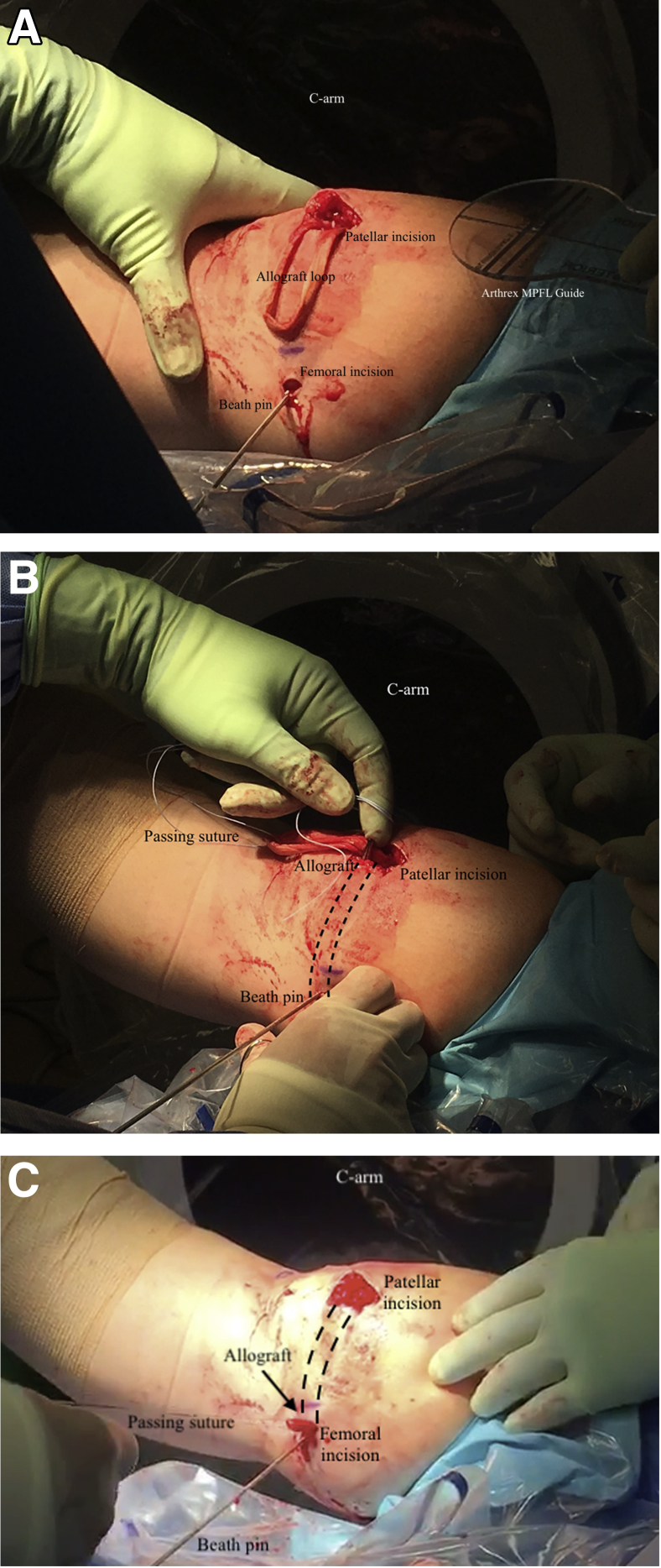
Fig 8.
(A) Intraoperative photograph of the allograft loop fixed to the patella. In addition, the Beath pin is seen at the femoral incision and projects anteriorly and proximally. (B) Intraoperative photograph in which passing sutures are secured to the allograft loop. After blunt dissection, the allograft is placed between the vastus medialis and joint capsule layers and shuttled from the patellar incision to the femoral incision using the passing suture (the path is indicated by the dashed lines). (C) Allograft loop at the femoral incision site. MPFL, medial patellofemoral ligament.
Femoral Tunnel Placement
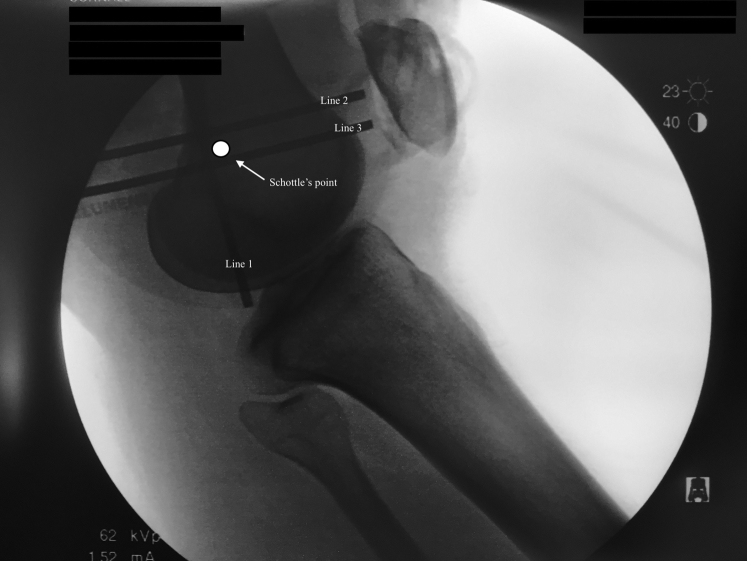
A 1-cm longitudinal incision is made just anterior to the adductor tubercle of the medial femoral condyle. Using a perfect lateral view on fluoroscopy, the surgeon identifies the femoral insertion point, or Schöttle point, which lies (1) just anterior to the posterior femoral cortex extension line, (2) 2.5 mm distal to the posterior border of the medial femoral condyle, and (3) just proximal to the level of the most posterior point of the Blumensaat line (Fig 9).21 A Beath pin is aimed anteriorly and proximally so that it exits through the lateral soft tissues. The knee is then flexed and extended to evaluate graft isometry.22 If graft lengthening occurs in flexion, the pin is too proximal and should be placed more distally. If lengthening occurs in extension, the pin is too distal and should be placed more proximally. Once final placement of the Beath pin site is accepted, a 7-mm drill hole is reamed over it to a depth of approximately 25 mm.
Fig 9.
Schöttle point on a lateral view of the right knee. Using a perfect lateral view on fluoroscopy, the surgeon identifies the femoral insertion point, or Schöttle point, which lies just anterior to the posterior femoral cortex extension line (line 1), approximately 2.5 mm distal to the posterior border of the medial femoral condyle (line 2), and just proximal to the level of the most posterior point of the Blumensaat line (line 3).21 This point represents the anatomic insertion of the medial patellofemoral ligament on the femur.4 We use an Arthrex medial patellofemoral ligament template to precisely identify the Schöttle point.
Allograft Passage and Fixation to Femur
After blunt dissection, the allograft is placed between the vastus medialis and joint capsule layers and shuttled to the femoral incision using passing sutures (Fig 8). Dissection between these layers from the patellar incision to the femoral incision is preferred because blind superficial dissection may disrupt the insertion of the vastus medialis on the anterior portion of the MPFL.23 A clamp may be placed underneath the graft at the medial incision site to prevent over-tightening. The graft should not be over-tensioned because it serves as a checkrein for lateral patellar displacement.4 A nitinol wire is inserted into the reamed femoral tunnel for later guidance of the interference screw. The knee is flexed at 30° to engage the patella in the trochlea and maintain proper graft tension. The shuttle sutures previously tied to the graft are then passed through the eyelet of the previously placed Beath pin and pulled out through the lateral skin, sinking the graft into the femoral tunnel. A 6.25-mm biocomposite interference screw is placed over the nitinol wire and screwed into the tunnel (Fig 10). Patellar stability is rechecked arthroscopically, and the absence of subluxation is confirmed.
Fig 10.
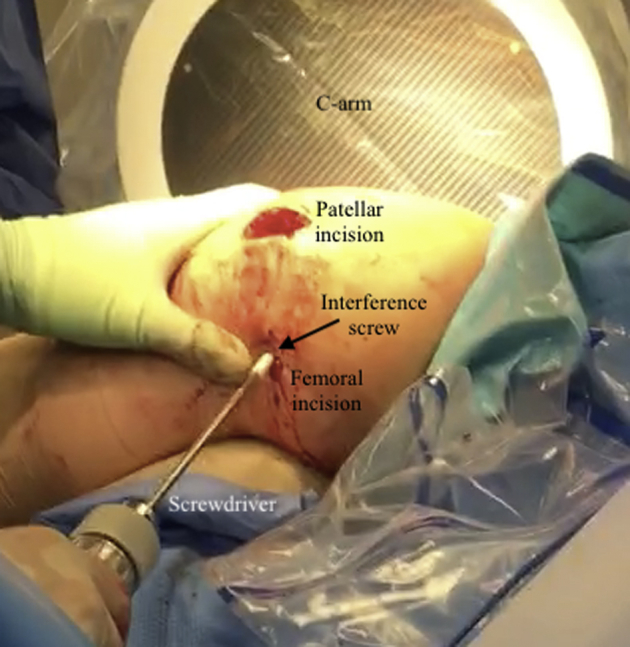
Intraoperative photograph of interference screw fixation into the femur. The allograft is fixed into place with a 6.25-mm biocomposite screw inside a 7-mm drill hole at the Schöttle point. The trajectory of the socket is anterior and proximal to increase tunnel length and avoid the notch or posterior cortex of the femur.
Postoperative Care
Immediately after surgery, the patient is placed in a knee brace held in full extension (Fig 11). Weight bearing is allowed as tolerated with 50°, 75°, and 90° of passive knee flexion at postoperative weeks 0 to 2, weeks 2 to 4, and weeks 4 to 6, respectively. At 6 weeks, use of the brace and crutches is discontinued, and patients begin quadriceps-strengthening exercises. Patients continue physical therapy and resume sport-specific activities between 12 and 18 weeks postoperatively. Anatomic placement of the patellar suture anchors and interference screw is confirmed on postoperative radiographs (Fig 12).
Fig 11.
Postoperative bracing. Immediately after surgery, the patient is placed in a knee brace locked in full extension. Weight bearing is allowed as tolerated. At 6 weeks, use of the brace and crutches is discontinued. Patients return to sport-specific activities at around 12 to 18 weeks postoperatively.
Fig 12.

Postoperative radiograph showing a lateral view of the right knee (R). Anatomic placement of the patellar suture anchors is confirmed. The interference screw is seen at the Schöttle point of the femur.
Discussion
Attention to MPFL reconstruction in the orthopaedic literature has increased dramatically in recent years, with over 200 peer-reviewed publications since 2014.13 Previous studies have suggested that MPFL reconstruction results in improved pain scores, low rates of recurrent instability, and high rates of return to sport after surgery and rehabilitation.24, 25 Despite the early success of the procedure, complications may occur more frequently than previously appreciated.14, 26 In addition, several factors are associated with recurrent instability after surgery, including the sulcus angle and presence of trochlear dysplasia.20 Of note, a meta-analysis of 34 studies by Stupay et al.27 suggested that complication rates have decreased with recent widespread use of MPFL reconstruction whereas functional outcomes and pain scores have remained unchanged.
The purpose of this article was to describe a safe and reproducible technique for MPFL reconstruction that optimally restores patellofemoral stability and contact mechanics. The advantages of our technique include strong patellar fixation with SwiveLock suture anchors and anatomic graft placement at the origin and insertion of the native MPFL. Use of an allograft also shortens the operative time and avoids donor-site morbidity. Although we recommend drilling the patellar tunnels to a depth of 20 to 25 mm to reduce the risk of fracture, some surgeons advocate techniques that use 1 tunnel28 or avoid drilling of the patella altogether29 because reported rates of fracture are as high as 3.6%.26 Patellar fracture, improper anatomic placement of the allograft, and over-tightening are the main risks of MPFL reconstruction. Increased attention to these critical aspects of the procedure may lead to decreased rates of complications and recurrent patellar instability particularly among high-risk patients.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.C. is an educational consultant for Arthrex and reports personal fees outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Plain radiographs of the knee (anteroposterior, lateral, and axial patellar views) and a magnetic resonance imaging (MRI) scan should be reviewed as part of the preoperative assessment. Axial MRI findings of the right knee included medial patellofemoral ligament (MPFL) scarring, a subchondral loose body, and chronic subchondral fracture. The patellar tilt and tibial tubercle–trochlear groove (TT-TG) distance should be measured preoperatively on MRI as well. A diagnostic arthroscopy is performed before MPFL reconstruction. There is often clear lateral subluxation of the patella from the trochlear groove when a lateral translation force is applied. Damage to the articular cartilage should be addressed at this time. A 5-cm longitudinal incision is then made over the MPFL. The medial patellar retinaculum and native MPFL are released from the patella, and two 4.5-mm drill holes are placed in the medial patella. The hamstring allograft is fixed at these sites with 2 SwiveLock suture anchors. The free suture ends are passed through the graft using a needle and tied down to the suture anchors. We then turn our attention to femoral tunnel placement and allograft fixation. A 3-cm longitudinal incision is made just anterior to the adductor tubercle of the medial femoral condyle. By use of a true lateral view on fluoroscopy, a Beath pin is placed at the Schöttle point and advanced through the skin on the lateral side. Once final placement of the Beath pin site is accepted, a 7-mm drill hole is reamed over it to a depth of approximately 25 mm. The allograft loop is shuttled from the patellar incision to the femoral incision using passing sutures. The allograft is fixed to the femoral socket with a biocomposite interference screw. Patellar stability is rechecked arthroscopically, and the absence of subluxation is confirmed. Postoperative radiographs of the right knee show proper anatomic placement of both the patellar suture anchors and the interference screw.
References
- 1.Koh J.L., Stewart C. Patellar instability. Clin Sports Med. 2014;33:461–476. doi: 10.1016/j.csm.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Fithian D.C., Paxton W.E., Stone M.L. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 3.Mäenpää H., Lehto M.U. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. doi: 10.1097/00003086-199706000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Loeb A.E., Tanaka M.J. The medial patellofemoral complex. Curr Rev Musculoskelet Med. 2018;11:201–208. doi: 10.1007/s12178-018-9475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elias D.A., White L.M., Fithian D.C. Acute lateral patellar dislocation at MR imaging: Injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–743. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 6.Zhang G.Y., Zheng L., Feng Y. Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in adults: An MRI evaluation. Injury. 2015;46:2413–2421. doi: 10.1016/j.injury.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 7.Krebs C., Tranovich M., Andrews K., Ebraheim N. The medial patellofemoral ligament: Review of the literature. J Orthop. 2018;15:596–599. doi: 10.1016/j.jor.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hinton R.Y., Sharma K.M. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34:385–396. doi: 10.1016/s0030-5898(03)00033-6. [DOI] [PubMed] [Google Scholar]
- 9.Reagan J., Kullar R., Burks R. MPFL reconstruction: Technique and results. Orthop Clin North Am. 2014;46:159–169. doi: 10.1016/j.ocl.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 10.Bitar A.C., D'Elia C.O., Demange M.K., Viegas A.C., Camanho G.L. Randomized prospective study on traumatic patellar dislocation: Conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop. 2011;46:675–683. doi: 10.1016/S2255-4971(15)30324-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nwachukwu B.U., So C., Schairer W.W., Green D.W., Dodwell E.R. Surgical versus conservative management of acute patellar dislocation in children and adolescents: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:760–767. doi: 10.1007/s00167-015-3948-2. [DOI] [PubMed] [Google Scholar]
- 12.Shubin Stein B.E., Gruber S., Brady J.M. MPFL in first-time dislocators. Curr Rev Musculoskelet Med. 2018;11:182–187. doi: 10.1007/s12178-018-9473-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNeilan R.J., Everhart J.S., Mescher P.K., Abouljoud M., Magnussen R.A., Flanigan D.C. Graft choice in isolated medial patellofemoral ligament reconstruction: A systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy. 2018;34:1340–1354. doi: 10.1016/j.arthro.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atkin D.M., Fithian D.C., Marangi K.S., Stone M.L., Dobson B.E., Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;4:472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy M.A., Bollier M.J. Medial patella subluxation: Diagnosis and treatment. Iowa Orthop J. 2015;35:26–33. [PMC free article] [PubMed] [Google Scholar]
- 17.Caton J., Deschamps G., Chambat P. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–325. [in French] [PubMed] [Google Scholar]
- 18.D’Amore T., Tanaka M.J., Cosgarea A.J. When and how far to move the tibial tuberosity in patients with patellar instability. Sports Med Arthrosc Rev. 2017;25:78–84. doi: 10.1097/JSA.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 19.Dietrich T.J., Fucentese S.F., Pfirrmann C.W. Imaging of individual anatomical risk factors for patellar instability. Semin Musculoskelet Radiol. 2016;20:65–73. doi: 10.1055/s-0036-1579675. [DOI] [PubMed] [Google Scholar]
- 20.Kita K., Tanaka Y., Toritsuka Y. Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med. 2015;43:2988–2996. doi: 10.1177/0363546515606102. [DOI] [PubMed] [Google Scholar]
- 21.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 22.Smith M.K., Werner B.C., Diduch D.R. Avoiding complications with MPFL reconstruction. Curr Rev Musculoskelet Med. 2018;11:241–252. doi: 10.1007/s12178-018-9479-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monllau J.C., Erquicia J.I., Ibanez M. Reconstruction of the medial patellofemoral ligament. Arthrosc Tech. 2017;6:e1471–e1476. doi: 10.1016/j.eats.2017.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schneider D.K., Grawe B., Magnussen R.A. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations. A systematic review and meta-analysis. Am J Sports Med. 2016;44:2993–3005. doi: 10.1177/0363546515624673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackay N.D., Smith N.A., Parsons N., Spalding T., Thompson P., Sprowson A.P. Medial patellofemoral ligament reconstruction for patellar dislocation: A systematic review. Orthop J Sports Med. 2014;2 doi: 10.1177/2325967114544021. 2325967114544021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schiphouwer L., Rood A., Tigchelaar S., Koeter S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc. 2017;1:245–250. doi: 10.1007/s00167-016-4245-4. [DOI] [PubMed] [Google Scholar]
- 27.Stupay K.L., Swart E.S., Shubin Stein B.E. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: A systematic review. Arthroscopy. 2015;31:1372–1380. doi: 10.1016/j.arthro.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 28.Zanon G., Marullo M., Benazo F. Double-bundle medial patellofemoral ligament reconstruction with a single patellar tunnel. Arthroscopy. 2013;2:401–404. doi: 10.1016/j.eats.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bedeir Y.H., Summers M.A., Patel D.J., Grawe B.M., Colosimo A.J. Anatomic medial patellofemoral ligament reconstruction without bone tunnels or anchors in the patella. Arthroscopy. 2018;7:611–615. doi: 10.1016/j.eats.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Plain radiographs of the knee (anteroposterior, lateral, and axial patellar views) and a magnetic resonance imaging (MRI) scan should be reviewed as part of the preoperative assessment. Axial MRI findings of the right knee included medial patellofemoral ligament (MPFL) scarring, a subchondral loose body, and chronic subchondral fracture. The patellar tilt and tibial tubercle–trochlear groove (TT-TG) distance should be measured preoperatively on MRI as well. A diagnostic arthroscopy is performed before MPFL reconstruction. There is often clear lateral subluxation of the patella from the trochlear groove when a lateral translation force is applied. Damage to the articular cartilage should be addressed at this time. A 5-cm longitudinal incision is then made over the MPFL. The medial patellar retinaculum and native MPFL are released from the patella, and two 4.5-mm drill holes are placed in the medial patella. The hamstring allograft is fixed at these sites with 2 SwiveLock suture anchors. The free suture ends are passed through the graft using a needle and tied down to the suture anchors. We then turn our attention to femoral tunnel placement and allograft fixation. A 3-cm longitudinal incision is made just anterior to the adductor tubercle of the medial femoral condyle. By use of a true lateral view on fluoroscopy, a Beath pin is placed at the Schöttle point and advanced through the skin on the lateral side. Once final placement of the Beath pin site is accepted, a 7-mm drill hole is reamed over it to a depth of approximately 25 mm. The allograft loop is shuttled from the patellar incision to the femoral incision using passing sutures. The allograft is fixed to the femoral socket with a biocomposite interference screw. Patellar stability is rechecked arthroscopically, and the absence of subluxation is confirmed. Postoperative radiographs of the right knee show proper anatomic placement of both the patellar suture anchors and the interference screw.