Abstract
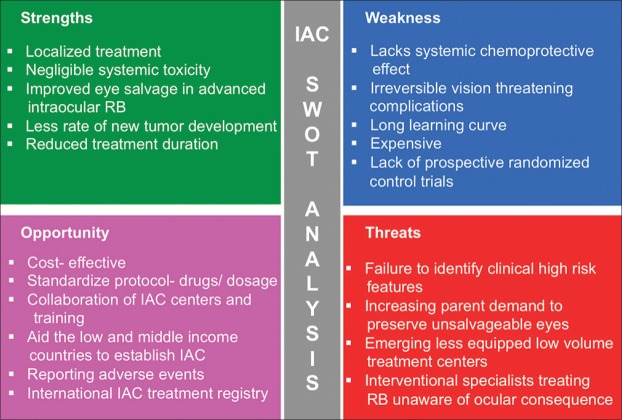
Intra-arterial chemotherapy (IAC), also known as superselective ophthalmic artery chemotherapy or chemosurgery, is currently widely accepted as one of the primary treatment modalities for intraocular retinoblastoma worldwide. Following the introduction of the technique in 1998, IAC has evolved over the past decades to be safer and more effective. Accumulated evidence shows that IAC is more effective in providing eye salvage in group D and E retinoblastoma as compared to conventional systemic intravenous chemotherapy (IVC). In contrast to IVC, IAC has the added benefits of reduced overall treatment duration and minimal systemic toxicity. This review provides a comprehensive update on the history, technique, indications, contraindications, and outcome of IAC. We have also identified the strengths, weaknesses, opportunities and threats (SWOT analysis) of the technique in this review.
Keywords: Retinoblastoma, intra-arterial chemotherapy, selective ophthalmic artery chemotherapy, superselective ophthalmic artery chemotherapy, chemosurgery
Retinoblastoma (RB) is one the most successfully treated pediatric malignancies. Targeted treatment in RB by direct delivery of chemotherapeutic agents into the ophthalmic artery (OA) has dramatically changed the approach in the management of this deadly, yet curable eye cancer.[1,2,3] This technique of intra-arterial chemotherapy (IAC) through ophthalmic artery has the advantage of higher concentration of chemotherapy drugs reaching the tumor, with negligible systemic side effects when compared with systemic intravenous chemotherapy (IVC). Over the past decade, we have witnessed expanding indications of IAC for tumor control and eye salvage in advanced and refractory retinoblastoma.[4] Prior to the IAC era, systemic IVC was used as the standard of care. Systemic IVC has shown encouraging results in salvaging nearly 100% of group A, B, and C eyes when coupled with adjunctive laser therapy and cryotherapy.[5,6,7] Advanced group D eyes with diffuse vitreous and subretinal seeds and group E eyes, however, carried a modest prognosis for eye salvage with IVC.[8] By achieving higher concentration in the target tumor, IAC has shown improved outcome in group D and E retinoblastoma.[9] With these added benefits, IAC has emerged as the first-line management option in selected cases, and its use is expanding. In refractory tumors, IAC has proven to be effective as a second-line treatment, leading to improved salvage of eyes that otherwise would have been enucleated. However, indications, patient selection, and procedure-related complications have raised some concerns.[10,11,12] IAC is an invasive method that requires an experienced multidisciplinary team including neurosurgeon, interventional neuroradiologist, pediatric oncologist, and retinoblastoma specialist.[3,13] Used with caution, and in experienced hands, the benefits of IAC outweigh the limitations. We now have data over a decade to be able to assess the long-term effects of IAC.[12] In this review, we attempt to summarize the current knowledge about IAC.
History and Evolution
In 1958, Reese performed IAC through the internal carotid artery (ICA) as an adjuvant treatment to enhance the effectiveness of external beam radiotherapy. Triethylene melamine (TEM), a nitrogen mustard analog, was injected directly into the ipsilateral internal carotid artery by placing a suture ligation for traction and hemostasis in 31 patients (61 injections). Due to unfavorable systemic toxicities of TEM, this procedure was further abandoned and discontinued.[14] A decade later, in 1968, Kiribuchi from Japan introduced the retrograde approach of infusion of opthalmic artery by way of arterial branches of external carotid artery and reported tumor regression.[15]
We credit the work of Kaneko et al. from Japan for the reintroduction of IAC that emerged as a valuable alternative to enucleation in the management of retinoblastoma.[16] Due to the cultural barriers arising from the stigma of enucleation in Japan, there was a need to salvage the eyes with retinoblastoma. Inomata and Kaneko in 1984 found that melphalan was superior to other chemotherapeutic drugs in retinoblastoma in their clonogenic assay, as an effort to improve eye salvage.[17,18] To reduce the severe myelosuppression with high-dose systemic melphalan that is required to achieve target concentration, they tried an alternate intra-arterial route for local delivery of melphalan to attain higher concentration in the intraocular tumor with negligible systemic toxicity.[16,17] This led to the pioneering work by Kaneko et al. in 1998 of a safe and effective technique of local delivery of melphalan through the opjhthalmic artery.[16] They described the technique of introducing a microballoon catheter into the cervical segment of internal carotid artery distal to the ophthalmic artery ostium through a transfemoral approach. On inflation of the balloon and occlusion of internal carotid artery, melphalan was injected into the opthalmic artery. They called this technique “selective ophthalmic artery infusion” (SOAI). They reported the initial results of the procedure in 187 patients who underwent 563 SOAIs with 97.5% technical success rate. They had a technical failure in 14 patients including nonvisualization of opthalmic artery in five eyes.[16] However, they noted that there were several small arterial branches arising proximal to the origin of opthalmic artery through which the drugs could flow making it not truly “selective.” They also suggested that if the catheter was to be introduced into the orifice of the opthalmic artery, drug flow to the other branches could be avoided, although their technique did not allow it because a guide wire was not used to advance the catheter at that time. With this, a new era was set, in treating retinoblastoma with IAC infusion, targeting the tumor directly through opthalmic artery, avoiding systemic side effects and improving globe salvage.[12,18,19,20,21,22]
Subsequently, Gobin et al. in 2006 popularized the refined technique of direct catheterization of the opthalmic artery with a guide wire that made it truly selective and they called it super-selective intraophthalmic artery chemotherapy.[23] Abramson et al. reported the initial results that were encouraging.[19] There was no looking back; IAC soon emerged as one of the first-line management options in retinoblastoma.[24] We also witnessed the various applications of IAC, such as primary and secondary IAC (first-line and second-line therapy after failure of IVC), tandem therapy (in bilateral retinoblastoma), bridge chemotherapy (sequential with systemic chemotherapy), minimal exposure (<2 sessions), and rescue IAC (for recurrence after previous IAC).[25,26,27,28,29,30] Pertinent terminologies are summarized in Table 1. According to a survey conducted in 2014, there were 31 centers in 19 countries where IAC was being performed as primary and secondary treatment for retinoblastoma, and the results were promising.[31]
Table 1.
Standard terminologies used in intraarterial chemotherapy
| Terminologies | Methods and indication of IAC administration |
|---|---|
| Primary IAC | First line of management |
| Secondary IAC | Secondary treatment after failure of previous treatment (IVC, external beam radiotherapy, plaque brachytherapy) |
| Tandem IAC | Administered bilaterally simultaneously |
| Bridge IAC | Initiating the treatment with IVC, especially in neonates, then followed by IAC |
| Rescue IAC | Re-use IAC following IAC for recurrent tumor or subretinal seeds or vitreous seeds |
Technique
The procedure is performed by a skilled neurointerventional radiologist or neurosurgeon in unison with the ocular oncologist, pediatric oncologist, anesthesiologist, pharmacist, and ancillary staff making this a truly multidisciplinary approach. IAC is performed as an outpatient procedure under general anesthesia in a well-equipped catheterization laboratory/interventional suite. Intravenous heparin (50 IU/kg body weight) is infused for anticoagulation achieving a clotting time two to three times baseline. Topical phenylephrine is routinely applied locally along the distribution of the supratrochlear artery to minimize chemotherapy flow onto the forehead. A nasal vasoconstrictor is also used routinely to minimize chemotherapy flow into the nose. The femoral artery of the ipsilateral side is accessed under aseptic precaution with a 4-French pediatric arterial sheath. This is carefully guided under fluoroscopy up the aorta, into the carotid artery, then to the internal carotid artery, and then to the ostium of opthalmic artery selectively [Fig. 1]. Serial angiograms are performed to evaluate the cerebral vasculature and identification of the vascular branches. Choroidal blush is identified in the angiogram. After ensuring the placement of the catheter at the opthalmic artery ostium with an angiogram, chemotherapeutic drugs diluted in 30 mL of normal saline are infused slowly and manually over 30 min in a pulsatile fashion to disrupt the laminar flow and homogeneous distribution of drugs along the targeted vascular anatomy. Repeat angiogram is performed after the procedure to exclude a thromboembolic event. In bilateral cases (tandem IAC), microcatheter is withdrawn upto the aorta and then redirected to the contralateral internal carotid artery upto the opthalmic artery ostium and a similar procedure is continued. Dose adjustment is done to avoid cumulative toxicity in tandem IAC. The microcatheter and guide wire are slowly removed. Use of guide wire is no longer preferred in the current technique to reduce opthalmic artery spasm. Femoral artery hemostasis is attained by manual compression followed by a compressive bandage. Patients are discharged the same day after observation for 4–6 hours. Topical corticosteroids in tapering doses along with short-acting mydriatics are prescribed. Oral aspirin in the dose of 1–2 mg/kg body weight is advised for 2 weeks postoperatively. Currently, this technique is widely accepted and practiced worldwide. Post procedure, after 7–10 days, a complete blood count is recommended for all patients.
Figure 1.
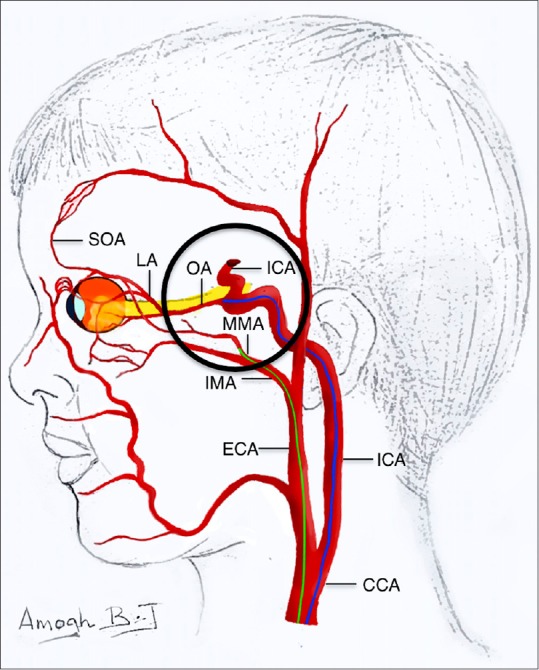
Selective ophthalmic artery chemotherapy is performed by passing the catheter via ICA through the femoral artery into the OA ostium. (route marked in blue) Alternate route is catheterization of MMA via ECA and IMA. (route marked in green). In Japanese technique, ICA distal to OA ostium is occluded with balloon. (CCA=common carotid artery; ECA= external carotid artery; ICA=internal carotid artery; IMA- internal maxillary artery; MMA= middle meningeal artery; OA= ophthalmic artery; LA= lacrimal artery; SOA= supraorbital artery)
An alternate route is used when the opthalmic artery cannot be identified due to a small arterial size or vasospasm during the procedure and difficulty in catheterization due to anatomical variation in the branching. In 7% of cases, the opthalmic artery arises from the middle meningeal artery, unlike the rest from internal carotid artery.[32] In such situations, catheterization is through the middle meningeal artery, a branch of the internal maxillary artery of the external carotid artery [Fig. 1].
The Japanese technique of microballoon catheterization and occlusion is considered as an alternative technique during difficult catheterization of opthalmic artery. By inflating the balloon just distal to the opthalmic artery, temporary balloon occlusion of the internal carotid artery is attained. This enables local delivery and prevents seepage of chemotherapeutic drugs to the anterior, middle, and posterior cerebral arteries. In this technique, the chemotherapeutic drugs are diluted in 6 cc normal saline and infused rapidly over 4 minutes followed by deflation of the balloon to prevent untoward cerebral ischemic complications [Fig. 1].[16]
Technical challenges are encountered in the intervention suite. Most commonly, there can be instability of the catheter at the face of the opthalmic artery ostium and rarely spasm of the opthalmic artery. Stenzel et al. recently reported technical interruption in 42% (29/98) cases due to meningeal collateral, difficulty in cannulating opthalmic artery, and alternative blood supply to the retina.[33] Yet another factor identified is the hemodynamic instability between ICA and external carotid artery leading to flow reversal (vascular steal) in opthalmic artery and inadequate choroidal blush. This may lead to suboptimal delivery of drugs and reduced response to IAC. To improve the drug delivery, an alternate route of middle meningeal artery was suggested by Klufas et al. in this scenario.[34] Bertelli et al. occluded external carotid artery with cyanoacrylate adhesives to prevent this instability in hemodynamics in 26 eyes undergoing 73 catheterizations.[35] In their series of 17 eyes, Quinn et al. required alternate route in five, with eye salvage in 80% (four of five). In one of the patients, there was no internal carotid artery supply to orbit; hence frontal branch of the superficial temporal artery was catheterized. The patient developed forehead necrosis and complete ptosis that required reconstructive surgery.[36]
Chemotherapeutic Agents and Dosage
Inomato and Kaneko in their initial series used melphalan as single-agent chemotherapeutic drug for IAC. In their study, melphalan was found to be the most potent agent for retinoblastoma when compared with other tumoricidal agents.[17] Later, Abramson et al. added carboplatin and topotecan, putting forward the popular triple-drug regimen.[19,23] [Table 2]. Side effects and complications mainly depend on the dosage of chemotherapeutic agents and should be titrated accordingly. Daniels et al. found excellent vitreous and retinal drug penetration of melphalan in IAC in an in vivo study in a rabbit model.[37]
Table 2.
Intra-arterial chemotherapy - drugs and dosage
| Drugs | Standard dose in mg | Dose range in mg | Indications |
|---|---|---|---|
| Melphalan* | 5 | 3-7.5 | - Drug of choice in groups B and C as single agent |
| Topotecan | 1 | 1-2 | - Advanced retinoblastoma with diffuse vitreous seeds (groups D and C) |
| Carboplatin | 20 | 15-30 | - Tandem IAC - to reduce the cumulative toxicity of melphalan, given alternatively |
| - Recurrence after IAC | |||
| - Suboptimal response to melphalan and topotecan combination |
*Melphalan has to be filtered before infusion
Melphalanis an alkylating agent that is a nitrogen mustard derivative. The effective and safe dose delivered to the eye is <0.5 mg/kg with minimal systemic absorption and negligible neutropenia. It is essential to filter melphalan before injection as the particles can embolize/crystallize the ocular vessels leading to vision-threatening complications. Suzuki et al. injected 1 mg of betamethasone after melphalan injection to prevent vasculitis. Dose ranges from 3 to 7.5 mg depending on the age of the patient [Table 2]
Topotecan, a semi-synthetic camptothecin derivative, is a topoisomerase 1 inhibitor that was popular for periocular chemotherapy in advanced RB. Periocular topotecan has less local tissue toxicity compared with periocular carboplatin. Laurie et al. reported that the effect of topotecan and carboplatin combination was superior to the vincristine, etoposide, and carboplatin combination in their animal study.[38] Dosage recommended is 0.5–2 mg [Table 2]
Carboplatin is a platinum-based derivative with fewer side effects than its precursor cisplatin. It is one of the drugs in the time-tested multiagent IVC protocol that has proven beneficial in RB. It is also used as a periocular chemotherapeutic agent. Carboplatin is used in the triple-drug protocol for unilateral IAC along with melphalan and topotecan. In bilateral IAC, to avoid the cumulative toxicity of melphalan leading to myelosuppression, dosage of melphalan is reduced with the addition of carboplatin without compromising the effect of IAC.[24] The recommended dosage is 15–30 mg [Table 2].
Treatment Protocol
Overall, the dosage of chemotherapeutic drugs for IAC depends on the patient's age and severity or extent of the disease. The largest series from Japan used melphalan as single agent in 408 eyes.[12] Abramson et al. reported beneficial effects from triple-drug regimen (melphalan, topotecan, and carboplatin).[19,23] Shields et al. primarily prefer melphalan as single agent with additional topotecan in eyes with the presence of extensive seeding.[24] Topotecan has the advantage of longer t1/2 when compared with melphalan.
Till date, there are no standardized protocols or universal consensus in place regarding drugs and dosage for IAC. In the systematic review by Yousef et al., melphalan was the most common single agent of choice. As an accepted standard of care, IAC is administered every 4 weeks for three sessions.[39] There are studies that have reported sessions beyond 3, upto 11.[24] The median number of sessions as reported by Suzuki et al., Gobin et al., and Shields et al. was 3.[12,23,25] The aim is to achieve maximum tumoricidal benefits with reduced local toxicity and vision-threatening complications. Sessions are extended in selective cases for improved response. If complete regression of the tumor can be achieved with additional transpupillary thermotherapy and/or cryotherapy post IAC, it is always preferred over additional IAC weighing the risks and benefits. Shields et al. showed excellent response to minimal exposure IAC upto two sessions for group B and C eyes. In rescue IAC, where reinitiation of IAC is performed in the post-IAC recurrence, Shields et al. reported a median of three sessions with typically higher dose melphalan and addition of topotecan for tumor control.[29] Most of the centers avoid IAC in neonates and infants <6 months of age. Chen et al. performed 27 catheterizations in 13 eyes of neonates at a mean age of 7.9 (range 4.6–10.9) weeks. One patient developed ICA spasm and the procedure was aborted.[40] Our team reported successful IAC in a 2-month-old neonate.[41]
Indications
1. Primary therapy/first-line management
- Unilateral retinoblastoma: groups B, C, and D (cT1b, cT2, cT3, cT4)
- Bilateral retinoblastoma: groups D and E (cT3)
Our team generally prefers to use IAC for unilateral disease and IVC for bilateral disease. We typically avoid tandem IAC for bilateral retinoblastoma, especially if the better eye has visual potential, to avoid unpredictable vascular toxicity of IAC leading to suboptimal vision affecting the quality of life of the child. Retinal and choroidal vasculopathy due to ischemia and/or occlusion can lead to irreversible blindness. In such situation, it is desirable to initiate systemic IVC as primary management for tumor control in both eyes along with eye and vision salvage of the better eye. However, IAC can be considered in the worse eye as secondary line of management for eye salvage.
2. Secondary therapy/second-line management after prior treatment failure
- Recurrent tumor, subretinal seeds or both
- Persistent tumor, subretinal seeds or both.
Contraindications
Eyes with neovascular glaucoma, hyphema, vitreous hemorrhage, aseptic preseptal or orbital cellulitis, and prephthisical
Radiological evidence of optic nerve extension and scleral extension
Extraocular or orbital extension of retinoblastoma
Trilateral retinoblastoma
Patients with systemic metastasis: hematogenous and central nervous system
Tumors amenable to focal transpupillary thermotherapy, cryotherapy, and/or intravitreal chemotherapy.
Unlike systemic IVC, IAC does not have systemic chemoprotective effect, as it is a localized delivery of chemotherapeutic drugs. Risk of systemic micrometastasis remains in advanced intraocular and extraocular disease. Metastasis can go undetected clinically in advanced diseases and poor prognosis for life salvage with IAC. Yousef et al. in their systematic review reported 2.1% (13/613) metastatic rate following IAC.[39]
Treatment Outcomes
Various studies have published the outcome of IAC in terms of eye salvage, recurrence, metastasis, and death. However, the choice of drugs, dosage, and techniques vary widely[12,23,24,25,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] [Table 3]. Lack of prospective randomized clinical trials is a challenge in evaluating the efficacy.
Table 3.
Intra-arterial chemotherapy- Worldwide Review Over Two Decades from 1998-2019
| Authors (year, country) | Years of study | No. of eyes | Total no. of catheterizations (% success rate) | No. of sessions median (range) | Drugs | Indication (no.of eyes) | Eye salvage in % | Overall eye salvage in % | Metastasis n (%) | Death n (%) | Complications | Median follow up in months |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Suzukiet al.12 (2011, Japan) | 1998-2007 | 408 | 1469 (98.8) | 3 (1-18) | M | Secondary | 60* | 60 | 8 (2) | 12 (3) | Periorbital swelling Severe orbital cellulitis Diffuse chorioretinal atrophy Bradycardia Bronchospasm |
74 |
| Gobinet al.23 (2011, USA) | 2006-2010 | 95 | 259 (98.5) | 3 (1-7) | M, T, C | Primary (39) Secondary (56) | 82 58 |
70 | 2 (2) | 0 (0) | Periocular edema Hyperemia Avascular retinopathy Cataract Eyelash loss |
13 |
| Petersonet al.42 (2011, USA) | 2008-2009 | 17 | 26 (100) | 1.4 (1-2) | M | Secondary (17) | 76.5 | 76.5 | 0 (0) | 0 (0) | Delayed vitreous hemorrhage | 8.6 (mean) |
| Munieret al.43 (2011, Switzerland) | 2009-2013 | 13 | 31 (96.8) | 3 (1-3) | M | Primary (9) Secondary (4) | 100 100 |
100 | 0 (0) | 0 (0) | Choroidal vasculopathy Retinal detachment Retinal arteriolar emboli Vitreous hemorrhage |
7 (mean) |
| Muenet al.45 (2012, UK) | 2008-2010 | 15 | NA | 2 (1-3) | M | Secondary (15) | 80 | 80 | 0 (0) | 0 (0) | Orbital edema Forehead hyperemia Retinal detachment 3rd cranial nerve palsy RPE loss Epistaxis Anaphylactoid reaction |
7 |
| Thampiet al.46 (2013, USA) | 2010-2012 | 20 | 40 (100) | 2.5 (1-5)* | M | Primary (12) Secondary (8) | 66.5 87.5 |
70 | 0 (0) | 0 (0) | Eyelid edema/erythema Dacryohemorrhea Vitreous hemorrhage Cataract Choroid atrophy OA spasm Neutropenia Bronchospasm |
15* |
| Venturiet al.44 (2013, Italy) | 2008-2010 | 39 | 146 (96) | NA (1-9) | M | Primary (17) Secondary (24) | 41 96 |
79 | 0 (0) | 0 (0) | Eyelid edema, hyperemia Ptosis Retinopathy Strabismus Lash loss Frontal alopecia Choroidal atrophy Systemic toxicity |
1-27 |
| Shieldset al.25 (2014, USA) | 2009-2013 | 70 | 198 (99.5) | 3 (1-7) | M, T, C | Primary (36) Secondary (34) | 72 62 |
67 | 0 (0) | 0 (0) | Eyelid edema Blepheroptosis Forehead hyperemia Scalp alopecia BRVO Partial choroidal vascular occlusion Optic neuropathy Vitreous hemorrhage Phthisis bulbi OA spasm OA occlusion |
19 |
| Taichet al.47 (2014, Argentina) | 2011-2013 | 27 | 66 (NA) | NA | M, T | Primary (5) Secondary (22) | 100 59 |
77.8 | 0 (0) | 0 (0) | 3rd cranial N. palsy Hematological toxicity |
11.7 |
| Pararedaet al.48 (2014, Spain) | 2008-2012 | 12 | 33 (94) | 2.5 (1-5) | M | Primary (12) | 58 | 58 | 0 (0) | 0 (0) | Diffuse arteriolar sclerosis RPE hypertrophy Partial retinal atrophy OA spasm |
29.5 |
| Ghassemiet al.49 (2014, Iran) | 2009-2012 | 24 | NA | 1-2 | M, T, C | Primary (6) Secondary (18) | 84 56 |
62.5 | 0 (0) | 0 (0) | Eyelid edema Vitreous hemorrhage Choroidal ischemia CRAO Retinal hemorrhage Retinal detachment NVG Ptosis Retinal fibrosis Cyclitic membrane Phthisis |
16.8 |
| Onget al.50 (2015, Taiwan) | 2010-2013 | 17 | 49 (91) | 2.8 (1-6) | Primary (6) Secondary (11) | 66.5 54.5 |
59 | 3 (17.5) | 2 (1) | Lid edema Retinal artery occlusion Chorioretinal atrophy Vitreous hemorrhage 3rd nerve palsy 6th nerve palsy |
22 | |
| Akyuzet al.51 (2015, Turkey) | 2011-2014 | 56 | NA | 2.3 (mean) 1-7 | M | Primary (44) Secondary (12) | 75 64 |
66 | 2 (3.5) | 2 (3.5) | Transient eyelid swelling Conjunctival chemosis Ptosis Forehead hyperemia Ocular motility limitation Mild proptosis RPE alteration Optic atrophy |
|
| Abramsonet al.24 (2016, USA) | 2008-2015 | 120 | 418 (NA) | 3.4 (mean) (1-11) | M, T, C, Mtx | Primary (60) Secondary (60) | NA NA |
97 | 0 (0) | 1 (0.8) | Neutropenia | 36 |
| Tunceret al.52 (2016, Turkey) | 2011-2015 | 24 | 76 (97.3) | 3 (2-5) | M, T, C | Primary (Group D) | 67 | 67 | 0 (0) | 0 (0) | Eyelid edema Ptosis Forehead hyperemia Chorioretinal atrophy Retinal detachment Vitreous hemorrhage |
29 |
| Michaelset al.53 (2016, USA) | 2008-2013 | 19 | 87 (100) | 5 (mean) (2-10) | M, T, C | NA | NA | 58 | 0 (0) | 0 (0) | Localized erythema Eyelid edema Eyelash/brow loss Forehead skin hyperpigmentation Conjunctival chemosis Neutropenia Bronchospasm Carboplatin anaphylaxis |
13 |
| Leal- Lealet al.54 (2016, Mexico) | NA | 11 | NA | 3 (all eyes) | M, T | Secondary | 55 | 55 | 0 (0) | 0 (0) | Stroke Nausea, vomitting |
57 (mean) |
| Reddy MAet al.55 (2017, UK) | 2013-2015 | 9 | 27 (NA) | 3 (2-4) | M, T | Secondary | 66 | 66 | 0 (0) | 0 (0) | Autonomic episode Ptosis Temporary 6th nerve palsy Choroidal ischemia |
21 |
| Chenet al.56 (2017, China) | 2011-2013 | 107 | 343 (98.5) | 3.1 (2-5) | M, T | Primary (30) Secondary (77) | 93 79 |
78.5 | 0 (0) | 0 (0) | Eyelid edema Conjunctival congestion Retinal hemorrhage Vitreous hemorrhage Retinal vasculopathy OA spasm Transient myelosupression |
13.6 (mean) |
| Rishiet al.56 (2017, India) | 2013-2016 | 10 | 38 (NA) | 4 (3-5) | M, T | Primary (2) Secondary (8) | 100 75 |
80 | 0 (0) | 0 (0) | Forehead pigmentation OA spasm BRVO Cataract Optic atrophy |
28 |
| Ammanuelet al.58 (2018, USA) | 2010-2017 | 43 | 125 (100) | 2.8 | M, T, C | NA | NA | 35 | 0 (0) | 0 (0) | Stroke Systemic toxicity |
31.8 |
| Hua Jet al.59 (2018, China) | 2013-2015 | 84 | 200 (94.5) | 2.8 (mean) | M, T | Secondary | 30 | 30 | 0 (0) | 0 (0) | Eyelid edema Vitreous hemorrhage Retinal vasculopathy OA spasm Transient vomiting Transient myelosupression |
14.2 (mean) |
| Radroset al.60 (2018, Sweden) | 2012-2015 | 11 | 39 (77) | NA | M | NA | 73 | 73 | 0 (0) | 0 (0) | Cerebrovascular emboli Renal effects Groin hematoma Eyelid/periocular edema Heterophoria Exophthalmos Ptosis Periorbital erythema OA spasm Transient visual impairment Papilledema Retinal detachment |
NA |
| Rojanapornet al.61 (2019, Thailand) | 2009-2017 | 27 | 80 (94) | 3 (1-7) | M, T, C | Primary (7) Secondary (20) | 57 50 |
52 | 1 (3.7) | 1 (3.7) | TIA Occlusive vasculopathy Vitreous hemorrhage Retinal artery precipitation Strabismus |
32 (mean) |
*Calculated from the statistics available in the publication. M= melphalan; T= topotecan; C= carboplatin; Mtx= methotrexate; NA=not available; OA= ophthalmic artery; RPE= retinal pigment epithelium; CRAO= central retinal artery occlusion; NVG= neovascular glaucoma; BRVO= branch retinal vein occlusion; TIA= transient ischemic attack
Eye salvage
With IAC, group B and C eyes have an excellent outcome, ranging from 95% to 100% eye salvage, similar to IVC[25] [Figs. 2 and 3]. The beneficial effect of IAC over IVC was found to be more pronounced in group D eyes, the majority of the eyes that otherwise required external beam radiotherapy or enucleation. Various studies reported improved eye salvage in the IAC era, especially in advanced intraocular disease [Table 4].
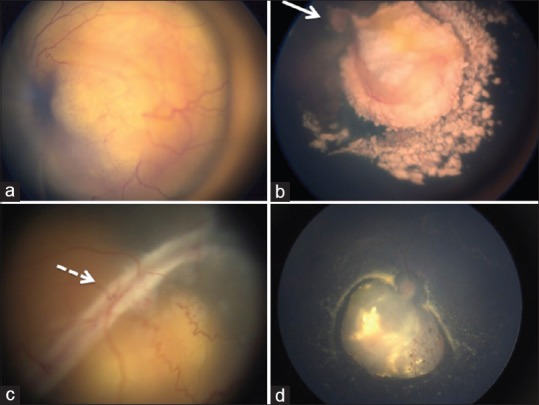
Figure 2.
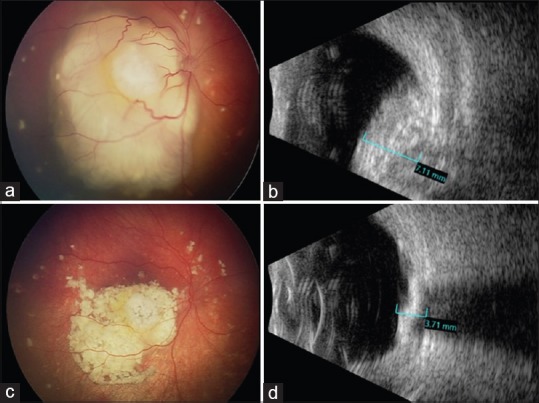
(a) Fundus photograph of a 10-month-old Caucasian infant showing solitary exophytic macular retinoblastoma with focal subretinal seeds and subretinal fluid in the right eye (OD), classified as group C. (b) B-scan ultrasonography confirming a calcified intraocular measuring 7.11 mm in thickness. After receiving three sessions of IAC, (c) the tumor is completely regressed (Type 1) with resolution of subretinal fluid and (d) the tumor has reduced to 3.71 mm thickness
Figure 3.
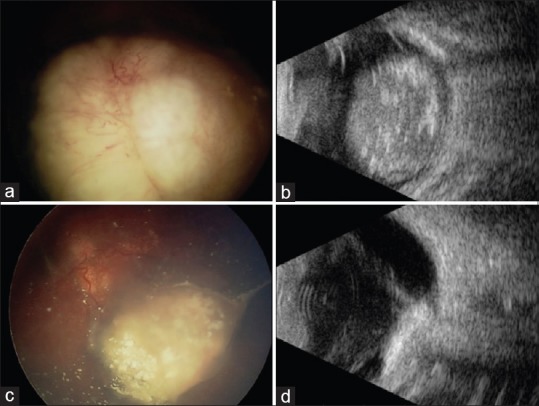
(a) Fundus photograph of a 6-month-old Caucasian infant showing solitary endophytic retinoblastoma with diffuse subretinal and vitroeus seeds in the left eye (OS). (b) B-scan ultrasonography confirming a large calcified intraocular mass occupying >50% of globe and measuring 12.20 mm thickness. After receiving four sessions of IAC, (c) tumor is regressed (Type 3) with calcified subretinal and vitreous seeds and (d) the tumor has reduced to 5.00 mm thickness, with visible partial posterior vitreous detachment
Table 4.
Outcome of IAC according to International Classification of Intraocular RB
| Authors (no.of eyes) | Eye salvage according to groups in % | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Suzuki et al (408)12 | 100 | 88 | 65 | 45 | 30 |
| Abramson et al (120)24 | 100 | 100 | 100 | 100 | 90 |
| Chen et al (107)56 | NA | 100 | 100 | 78.5 | 62 |
| Shields et al (70)25 | NA | 100 | 100 | 94 | 36 |
| Ammanuel et al (43)58 | 0 | 90 | 64 | 69 | 50 |
| Ronjanaporn et al (27)61 | NA | 100 | 100 | 75 | 9 |
| Munier et al (25)63 | NA | NA | NA | 100 | NA |
| Tuncer et al (24)52 | NA | NA | NA | 67 | NA |
| Ghassemi et al (24)49 | NA | 100 | 0 | 72 | 66 |
| Thampi et al (20)46 | 100 | 100 | 100 | 50 | 33 |
| Ong et al (17)50 | NA | 67 | 100 | 100 | 57 |
| Parareda et al (12)48 | NA | 100 | 100 | 50 | NA |
| Leal-Leal et al (11)54 | NA | 50 | 100 | 30 | NA |
*Most ocular oncologists do not treat group A with IAC due to potential toxicities and they treat with local laser therapy like laser photocoagulation and cryotherapy
Shields et al. compared IAC (n = 49) and IVC (n = 42) treated eyes with unilateral retinoblastoma. Eye salvage rate was significantly higher (91%) in group D eyes with IAC, compared with the IVC group (48%).[62] Munier et al. compared group D eyes treated with IAC versus IVC and showed 100% globe salvage with IAC and 60% with IVC. The relapse rate of IAC was 24% compared with 52% with IVC.[63] The treatment duration was shorter in IAC for tumor control, 6.7 months in IAC versus 14.2 months in IVC.[63] Abramson et al. reported 78.6% eye salvage in group D eyes with IAC. They also estimated the 2-year probability of 64% eye salvage after IAC in eyes with vitreous seeds, 83% in eyes with subretinal seeds, and in 80% with both. Eye salvage in advanced retinoblastoma was significantly better in treatment-naïve eyes compared with non-naïve eyes (80.2% vs 58.4%).[64] Tuncer et al. reported 66.6% eye salvage in treatment-naïve group D eyes [Figs. 4 and 5].
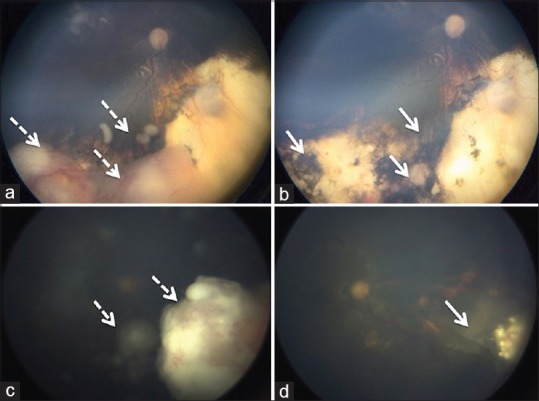
Figure 4.
(a) Fundus photograph of a 7-month-old Chinese infant showing large, exophytic, retinoblastoma in the OS with retinal detachment, subretinal seeds and no view of optic disc, and (b) following two sessions of IAC, the tumor is completely regressed (Type 1) and the optic nerve (arrow) is visible. (c) Fundus photograph of a 9-month-old Indian infant showing large, exophytic, retinoblastoma in OD with total retinal detachment (arrow), subretinal seeds, and no view of optic disc, and (d) following three sessions of IAC, the tumor is regressed (Type 3) and there is complete resolution of subretinal fluid with visible optic disc
Figure 5.
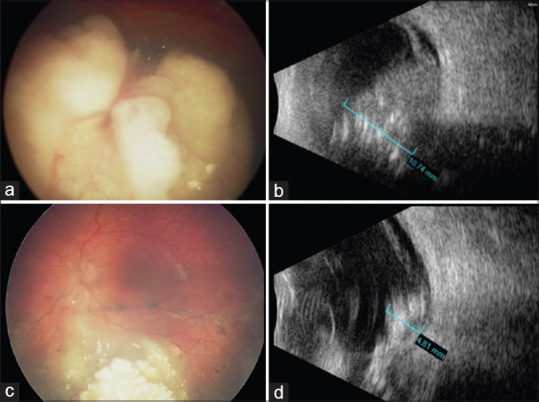
(a) Fundus photograph of a 2-year-old Caucasian infant showing large, exophytic/endophytic (group D) with vitreous and subretinal seeds, overlying the optic nerve in OS. (b) B-scan ultrasonography confirming a large calcified intraocular mass measuring 10.74 mm thickness. After receiving four sessions of IAC, (c) the tumor is regressed (Type 3) and located away from the optic disc with flat fovea and potential for vision. (d) The tumor has reduced to 4.81 mm thickness
Currently, the combination of two localized treatment strategies, IAC with intravitreal chemotherapy (IvitC), has further improved the outcome.[52] Shields et al. showed significant improvement in the outcome of IAC with additional administration of IvitC compared with IAC alone. They noted that there was a difference (IAC vs IAC plus IvitC as needed) in the need for enucleation overall (44% vs 15%, P = 0.01), especially for group E eyes (73% vs 27%, P = 0.04).[65] Dalvin et al. compared eyes that received IAC alone with those who required additional IvitC for vitreous seeds and subretinal seeds. Of the 49 eyes classified as groups D and E, 20 eyes required additional IvitC where 50% eyes had vitreous seeds in all four quadrants. In these eyes, enucleation or radiation was eliminated in 75% with IAC alone and 65% with combined IvitC.[66] Francis et al. reported similar estimated 1-year ocular survival with IAC in the pre-IvitC era (96%) and IvitC era (96%).[67] In the review by Yousef et al., overall eye salvage was 66% in 502 eyes, 86% in groups A–C, and 57% in groups D and E.[39] Primary IAC had better eye salvage rate than secondary IAC. From the two largest studies, eye salvage after primary IAC was 72%–86% and 58%–62% with secondary IAC.[12,25] Peterson et al. achieved 76.5% eye salvage (n = 17) with IAC in eyes with vitreous seeds that were refractory to prior treatments and were awaiting enucleation.[42] In 12 eyes, melphalan doses were escalated upto 7.5 mg for optimal response.[42] According to Gobin et al., Kaplan–Meier estimate for eye survival rates at 2 years was 82% and 58% for primary (n = 39) and secondary (n = 56) IAC, respectively [Fig. 6c and d].[23]
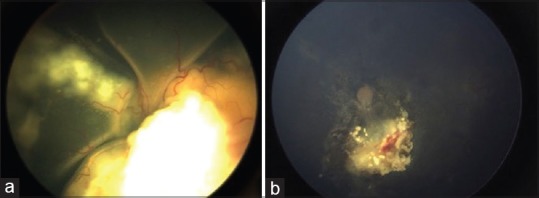
Figure 6.
(a) Fundus picture showing tumor and vitreous seeds’ recurrence in OD post IAC four sessions in a group D eye (arrow with dotted lines) of a 2-year-old Chinese boy. (b) After rescue IAC two sessions, tumor and seeds completely regressed. (c) Tumor recurrence with vitreous clouds after six cycles of systemic chemotherapy in a 3-year-old Indian boy in OS. (d) Following three sessions of IAC, tumor is totally calcified and vitreous is clear
Local tumor recurrence
New tumor formation in eyes treated with systemic IVC has been reported as 23%–48%.[68,69,70,71] In an early report, Shields et al. found that IAC alone provided excellent solid tumor and seed control.[20] Following IAC (mean three sessions), they demonstrated complete control of solid tumor in 88%, subretinal seeds in 82%, and vitreous seeds in 67%.[20] Later, use of IvitC added further control to vitreous seeds.[65] Abramson et al. analyzed similar cohort of heritable RB patients who underwent IVC and IAC (primary and secondary) for new tumor occurrence after treatment and found new tumors in 2.4% of treatment-naïve eyes (primary IAC) and 8% in secondary IAC compared with 47% in the IVC group.[72]
Francis et al. recently reported the overall estimate of recurrence-free survival (RFS) post IAC at 1 year and 2 years as 76.3% and 70%, respectively.[67] They evaluated 407 eyes, of which 111 eyes had recurrence. Of these eyes, 54% received focal laser or cryotherapy, plaque brachytherapy, and IvitC, and 29% required only focal cryotherapy and laser. Additional IAC was performed in 30% of eyes with recurrence. It was also estimated that RFS was 92% at 2 years if the eyes remained recurrence-free at the end of 1 year.[67]
The strategy of reusing IAC after initial IAC for both primary and secondary retinoblastomas was termed as rescue IAC by Shields et al.[30] Repeat cycles of IAC (recue IAC) were performed following tumor recurrence in 12 eyes at a mean of 5 months after the last IAC cycle. Dosage was escalated upto 7.5 mg of melphalan, and additional topotecan 1 mg was generally infused leading to eye salvage (rescue IAC) at 67% (n = 8) [Fig. 6a and b].
Systemic metastasis
The primary goal of retinobalstoma management has always been life salvage. Since IAC is a local therapy but not systemically chemoprotective, the concern of undetected systemic micrometastasis in advanced retinoblastoma prevails. In the largest series of IAC by Suzuki et al., there were 12 deaths, of which 8 were due to metastasis of central nervous system (CNS) (n = 1) and multiple other sites (n = 5).[12] A recent multicenter survey including six prominent IAC centers from the United States (n = 2), Europe (n = 2), Brazil (n = 1), and Argentina (n = 1) analyzed metastatic deaths.[72] Over a period of 10 years, 3 of 1139 patients were reported to have metastasis from one center alone (Argentina).[73] Gobin et al. from the United States had previously reported 2 of 78 patients who developed metastasis at a median follow-up of 13 months.[23] From Australia, Mathew et al. reported a case of hematogenous metastasis in a child with group E unilateral retinoblastoma who received four sessions of IAC, and subsequently required high dose of systemic chemotherapy and radiation.[74] Ronjanaporn et al. from Thailand had 1 patient out of 27 (4%) who died due to CNS metastasis.[61] Akyuz et al. from Turkey reported two deaths post-enucleation in a progressive disease following IAC.[51] Both the patients had histopathological high-risk features: choroid and anterior chamber invasion in one and optic nerve cut end involvement in the other. Three patients (3/17, 17.5%) had metastasis to CNS as reported by Ong et al. from Taiwan. It was classified as group E in two patients and group B in one patient where all eyes were enucleated for vitreous hemorrhage after IAC. All three eyes had histopathological high-risk features with choroid and optic nerve invasion. Despite adjuvant chemotherapy post-enucleation, two patients died.[50] Our team has been fortunate to have used IAC for nearly 12 years in carefully selected hundreds of cases of retinoblastoma and we have had no incidence of metastasis or death.[20,25,27,29,62,65,66]
Kaliki et al. analyzed histopathological features in 519 enucleated eyes and found high-risk invasive features in 17% of group D eyes and 24% of group E.[75] Taking this into account, IAC should be avoided in eye with clinical risk factors for systemic metastasis (neovascular glaucoma, hyphema, vitreous hemorrhage, preseptal cellulitis, orbital cellulitis, tumor filing the eyeball, prephthisis, and phthisis bulbi).
Yousef et al. in their review showed 2.1% of metastatic disease in 613 patients.[39] There is a strong belief that the risk of metastasis and death is not worth in these eyes that has poor prognosis for eye and vision salvage. Rodriguez et al. attempted high-dose IAC for extraocular retinoblastoma with chiasmal invasion using carboplatin combined with intrathecal topotecan, and after three sessions there was radiological evidence of partial resolution of the orbital mass and chiasmal lesion, and the eye was enucleated. Remission was documented in CNS – cerebrospinal fluid cytology after three sessions of intrathecal topotecan. Thereafter, the child was lost to follow-up and further status was not known on stability or recurrence or metastasis or death.[76]
Occurrence of secondary primary malignancies (SPMs) is well established in heritable retinoblastoma group of patients especially when exposed to radiation. Suzuki et al. reported SPM in 11 patients out of the 343 patients undergoing IAC at a mean follow-up of 6.2 years, all of whom have undergone radiotherapy and 9 had bilateral retinoblastoma. The estimated cumulative incidence was 1.3% at 5 years.[12] Habib et al. analyzed 214 patients with heritable and/or bilateral retinoblastoma who received IAC over a period of 10 years (2006–2016) with a mean follow-up of 36 months. Four patients had pinealoblastoma at an interval of 13–21 months after detection of retinoblastoma and were estimated to be 2.7% at 5 years that is comparable to studies pre-IAC era.[77]
Treatment Complications
IAC has proven time and again to be efficacious in tumor control with potential eye and vision salvage. But it is not completely devoid of vision-threatening ocular vascular events, mostly related to chemotherapeutic drug toxicity. We have witnessed higher complication rates in the past when compared with the current scenario probably due to the learning curve in the technique and the modality of administration of drugs.[12,78,79,80] There has been no death reported due to the procedure itself.
Systemic side effects
The major advantage of IAC was to reduce morbidity related to systemic toxicity of chemotherapeutic agents. However, grades 1–4 neutropenia was reported with IAC in few cases. Overall, 5.9% suffered neutropenia, of which only 0.2% required blood transfusion. Others were bronchospasm and autonomic episodes. Ophthalmic artery spasm was reported that lead to aborting the procedure or alternate route for completion of the procedure. Being a neuroinvasive procedure, IAC carries the risk of neurological complications. Ronjanaporn et al. reported transient ischemic attack in one case.[61] Three cases of stroke following IAC were reported so far.[54,58,80] One case of stroke presenting as seizures related to cerebral ischemia in the territory of ipsilateral internal carotid artery after selective ophthalmic artery IAC was reported. However, the patient made complete neurological recovery.[58] The other was a child with atrial septal defect who presented with status epilepticus after 2 days followed by upper extremity weakness. Magnetic resonance imaging revealed cerebral infarction in the ipsilateral middle cerebral artery territory and an incomplete circle of Willis.[80]
Ocular side effects
The common and self-resolving complications are periocular edema and hyperemia (34%), ptosis (13.5%), focal madarosis (10.5%), and forehead erythema (3%). Application of sympathomimetic drugs topically over the forehead can reduce the periorbital signs to some extent [Fig. 7]. Neurological complications included third and sixth cranial nerve palsy. Muen et al. reported 6 of 17 (40%) cases with third cranial nerve palsy with ptosis and pupillary involvement.[45] All except one case resolved within 2–6 months. Shields et al. reported a case of optic neuropathy, and three cases of optic atrophy are reported.[25,51,57] The procedure carries the risk of permanent vision-threatening complications. Associated ischemic and occlusive chorioretinopathy, central retinal artery occlusion, vitreous hemorrhage, and retinal detachment remain a major concern when vision salvage is one of the major goals of procedure. Especially in those patients with remaining one eye having visual potential, be it unilateral or bilateral IAC [Fig. 8].
Figure 7.

(a) Forehead hyperemia along the distribution of supraorbital artery and blepheroptosis in a 6-month-old Chinese girl after first session of IAC in OD. (b) Ipsilateral alopecia in a 2-year-old Chinese boy following IAC in OD
Figure 8.
(a) Group D unilateral RB in a 2 year-old Indian boy with total retinal detachment in OS. (b) After three sessions of IAC, the tumor and retinal detachment have completely resolved, but ophthalmic artery occlusion has lead to optic nerve atrophy and diffuse retinal atrophy with arteriolar narrowing
Dalvin et al. compared the early era (2009–2011) and current era (2012–2017) to evaluate the vascular complications and found a reduction from 59% to 9%.[79] Spasm of ophthalmic artery was 27% in the early era, whereas 0% in the current era. Choroidal ischemia had reduced from 14% to 4%.[79] In a case–control study, Maidana et al. evaluated subfoveal choroidal thickness with spectral domain optical coherence tomography in 18 eyes. Thickness was significantly reduced in treated eyes versus healthy control eyes, with or without clinical evidence of choroidal atrophy.[81]
The cause of vascular events is still unclear, whether it is related to technique, cumulative drug toxicity, pH, or drug distribution, and is often unpredictable. Francis et al. correlated electroretinogram (ERG) responses with chemotherapeutic drugs (melphalan, topotecan, carboplatin) and found that cumulative melphalan was associated with modest change in ERG amplitudes although temporary.[82] Tse et al. evaluated the histopathological changes in nonhuman primate model (Maccaca mullatta) after selective ophthalmic artery IAC with melphalan (5 mg) and carboplatin (30 mg). Ocular and orbital vasculature showed significant toxic effects.[83] Steinle et al. found that there was direct effect of the drugs (melphalan and carboplatin) to the vascular endothelium and monocytes.[84]
Visual outcome
Not many studies have reported the final visual acuity (VA) post-IAC. Suzuki et al. evaluated VA with Landolt ring test in 197 eyes of 246 salvaged eyes. In eyes with tumors sparing the foveola, 51% retained >20/40 and 36% retained 20/20.[12] Of the nine eyes that underwent IAC, none had visual deterioration post-IAC as reported by Reddy et al. Best-corrected VA was ≥20/40in 71% (5/7 eyes) pre-IAC when compared with 77% (7/9) post-IAC. All eyes recorded normal ERG post-IAC except one who had subtle reduction in rod and cone b-waves. The cumulative melphalan dose was the highest (20 mg) in this cohort.[55] Recently, Levin et al. assessed the pretreatment ERG with posttreatment VA in 157 group D and E eyes. Lower pretreatment ERG was associated with higher visual impairment posttreatment.[85] Munier et al. assessed the final VA in 12 group D eyes, of which 7 eyes had extramacular tumors; 42% (n = 3) maintained ≥20/40.[63]
Conclusion
IAC has emerged as a promising option for eye salvage, particularly in advanced intraocular retinoblastoma as primary and secondary line of management. This modality has gained tremendous popularity in the developed world. A major concern in the low- and middle-income countries is the financial constraint due to high treatment cost. Safer techniques and optimal dosage of chemotherapeutic agents can minimize treatment-associated complications. Despite the expertise, vascular complications are unpredictable and can still occur in the most experienced hands. Vision salvage has a crucial role in a certain set of patients with retinoblastoma. Therefore, risks and benefits have to be thoroughly assessed, and treatment strategy has to be chosen accordingly. Collaboration of IAC treatment centers and merging as one single platform to standardize drugs, dosage, and technique may further improve the outcome. Lack of systemic chemoprotective effect of IAC poses a major threat in certain clinically advanced disease with high risk of systemic micrometastasis. We have elaborated this in our strengths/weaknesses/opportunities/threats (SWOT) analysis of IAC [Fig. 9]. With a decade of experience, the long-term prognosis of IAC is yet to be established.
Figure 9.
SWOT analysis of IAC
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Mr. Amogh B.J, Medical Undergraduate, 2015 M.B.B.S batch, Government Medical College, Thiruvananthapuram, Kerala, India for the artistic sketch [Fig. 1].
References
- 1.Shields CL, Shields JA. Intra-arterial chemotherapy for retinoblastoma: The beginning of a long journey. Clin Exp Ophthalmol. 2010;38:638–43. doi: 10.1111/j.1442-9071.2010.02297.x. [DOI] [PubMed] [Google Scholar]
- 2.Anderson HJ, Pointdujour-Lim R, Shields CL. Treatments for retinoblastoma then and now. JAMA Ophthalmol. 2017;135:e164652. doi: 10.1001/jamaophthalmol.2016.4652. [DOI] [PubMed] [Google Scholar]
- 3.Wyse E, Handa JT, Friedman AD, Pearl MS. A review of the literature for intra-arterial chemotherapy used to treat retinoblastoma. Pediatr Radiol. 2016;46:1223–33. doi: 10.1007/s00247-016-3554-6. [DOI] [PubMed] [Google Scholar]
- 4.Abramson DH, Francis JH, Gobin YP. What's new in intra-arterial chemotherapy for retinoblastoma? Int Ophthalmol Clin. 2019;59:87–94. doi: 10.1097/IIO.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 5.Shields CL, DePotter P, Himelstein BP, Shields JA, Meadows AT, Maris JM. Chemoreduction in the initial management of intraocular retinoblastoma. Arch Ophthalmol. 1996;114:1330–38. doi: 10.1001/archopht.1996.01100140530002. [DOI] [PubMed] [Google Scholar]
- 6.Murphree AL, Villablanca JG, Deegan WF, Sato JK, Malogolowkin M, Fisher A, et al. Chemotherapy plus local treatment in the management of intraocular retinoblastoma. Arch Ophthalmol. 1996;114:1348–56. doi: 10.1001/archopht.1996.01100140548005. [DOI] [PubMed] [Google Scholar]
- 7.Gallie BL, Budning A, DeBoer G, Thiessen JJ, Koren G, Verjee Z, et al. Chemotherapy with focal therapy can cure intraocular retinoblastoma without radiotherapy. Arch Ophthalmol. 1996;114:1321–8. doi: 10.1001/archopht.1996.01100140521001. [DOI] [PubMed] [Google Scholar]
- 8.Manjandavida FP, Honavar SG, Reddy VA, Khanna R. Management and outcome of retinoblastoma with vitreous seeds. Ophthalmology. 2014;121:517–24. doi: 10.1016/j.ophtha.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 9.Schaiquevich P, Fabius AW, Francis JH, Chantada GL, Abramson DH. Ocular pharmacology of chemotherapy for retinoblastoma. Retina. 2017;37:1–10. doi: 10.1097/IAE.0000000000001275. [DOI] [PubMed] [Google Scholar]
- 10.Abramson DH, Shields CL, Munier FL, Chantada GL. Treatment of retinoblastoma in 2015: Agreement and disagreement. JAMA Ophthalmol. 2015;133:1341–7. doi: 10.1001/jamaophthalmol.2015.3108. [DOI] [PubMed] [Google Scholar]
- 11.Shields CL, Lally SE, Leahey AM, Jabbour PM, Caywood EH, Schwendeman R, et al. Targeted retinoblastoma management: When to use intravenous, intra-arterial, periocular, and intravitreal chemotherapy. Curr Opin Ophthalmol. 2014;25:374–85. doi: 10.1097/ICU.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 12.Suzuki S, Yamane T, Mohri M, Kaneko A. Selective ophthalmic arterial injection therapy for intraocular retinoblastoma: The long-term prognosis. Ophthalmology. 2011;118:2081–7. doi: 10.1016/j.ophtha.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Jabbour P, Chalouhi N, Tjoumakaris S, Gonzalez LF, Dumont AS, Chitale R, et al. Pearls and pitfalls of intraarterial chemotherapy for retinoblastoma. J Neurosurg Pediatr. 2012;10:175–81. doi: 10.3171/2012.5.PEDS1277. [DOI] [PubMed] [Google Scholar]
- 14.Reese AB, Hyman GA, Tapley ND, Forrest AW. The treatment of retinoblastoma by x ray and triethylene melamine. AMA Arch Ophthalmol. 1958;60:897–906. doi: 10.1001/archopht.1958.00940080917010. [DOI] [PubMed] [Google Scholar]
- 15.Kiribuchi M. [Radiation therapy for malignant intraocular tumors] Ganka. 1966;8:268–303. [PubMed] [Google Scholar]
- 16.Yamane T, Kaneko A, Mohri M. The technique of ophthalmic arterial infusion therapy for patients with intraocular retinoblastoma. Int J Clin Oncol. 2004;9:69–73. doi: 10.1007/s10147-004-0392-6. [DOI] [PubMed] [Google Scholar]
- 17.Inomata M, Kaneko A. Chemosensitivity profiles of primary and cultured human retinoblastoma cells in a human tumor clonogenic assay. Jpn J Cancer Res. 1987;78:858–68. [PubMed] [Google Scholar]
- 18.Kaneko A, Suzuki S. Eye-preservation treatment of retinoblastoma with vitreous seeding. Jpn J Clin Oncol. 2003;33:601–7. [PubMed] [Google Scholar]
- 19.Abramson DH, Dunkel IJ, Brodie SE, Kim JW, Gobin YP. A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma initial results. Ophthalmology. 2008;115:1398–404. doi: 10.1016/j.ophtha.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Shields CL, Bianciotto CG, Jabbour P, Ramasubramanian A, Lally SE, Griffin GC, et al. Intra-arterial chemotherapy for retinoblastoma: Report No.1, control of retinal tumors, subretinal seeds, and vitreous seeds. Arch Ophthalmol. 2011;129:1399–406. doi: 10.1001/archophthalmol.2011.150. [DOI] [PubMed] [Google Scholar]
- 21.Vajzovic LM, Murray TG, Aziz-Sultan MA, Schefler AC, Wolfe SQ, Hess D, et al. Supraselective intra-arterial chemotherapy: Evaluation of treatment-related complications in advanced retinoblastoma. Clin Ophthalmol. 2011;5:171–6. doi: 10.2147/OPTH.S12665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shields CL, Bianciotto CG, Jabbour P, Griffin GC, Ramasubramanian A, Rosenwasser R, et al. Intra-arterial chemotherapy for retinoblastoma: Report No.2, treatment complications. Arch Ophthalmol. 2011;129:1407–15. doi: 10.1001/archophthalmol.2011.151. [DOI] [PubMed] [Google Scholar]
- 23.Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH. Intra-arterial chemotherapy for the management of retinoblastoma: Four-year experience. Arch Ophthalmol. 2011;129:732–7. doi: 10.1001/archophthalmol.2011.5. [DOI] [PubMed] [Google Scholar]
- 24.Abramson DH, Marr BP, Francis JH, Dunkel IJ, Fabius AW, Brodie SE, et al. Simultaneous bilateral ophthalmic artery chemosurgery for bilateral retinoblastoma (tandem therapy) PLoS One. 2016;11:e0156806. doi: 10.1371/journal.pone.0156806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shields CL, Manjandavida FP, Lally SE, Pieretti G, Arepalli SA, Caywood EH, et al. Intra-arterial chemotherapy for retinoblastoma in 70 eyes: Outcomes based on the international classification of retinoblastoma. Ophthalmology. 2014;121:1453–60. doi: 10.1016/j.ophtha.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 26.Gobin YP, Dunkel IJ, Marr BP, Francis JH, Brodie SE, Abramson DH. Combined, sequential intravenous and intra-arterial chemotherapy (bridge chemotherapy) for young infants with retinoblastoma. PLoS One. 2012;7:e44322. doi: 10.1371/journal.pone.0044322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shields CL, Kaliki S, Al-Dahmash S, Rojanaporn D, Leahey A, Griffin G, et al. Management of advanced retinoblastoma with intravenous chemotherapy, then intra-arterial chemotherapy as alternative to enucleation. Retina. 2013;33:2103–9. doi: 10.1097/IAE.0b013e318295f783. [DOI] [PubMed] [Google Scholar]
- 28.Hutchinson A, Kaliki S, Shields CL. Two-dose exposure of intra-arterial chemotherapy for group D retinoblastoma. J Pediatr Ophthalmol Strabismus. 2012;49 doi: 10.3928/01913913-20120320-01. [DOI] [PubMed] [Google Scholar]
- 29.Dillon AB, Douglass A, Jabbour P, Shields CL. Minimal exposure intra-arterial chemotherapy for children with retinoblastoma and 13q syndrome. Oman J Ophthalmol. 2016;9:164–6. doi: 10.4103/0974-620X.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shields CL, Say EA, Pointdujour-Lim R, Cao C, Jabbour PM, Shields JA. Rescue intra-arterial chemotherapy following retinoblastoma recurrence after initial intra-arterial chemotherapy. J Fr Ophtalmol. 2015;38:542–9. doi: 10.1016/j.jfo.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Grigorovski N, Lucena E, Mattosinho C, Parareda A, Ferman S, Catalá J, et al. Use of intra-arterial chemotherapy for retinoblastoma: Results of a survey. Int J Ophthalmol. 2014;7:726–30. doi: 10.3980/j.issn.2222-3959.2014.04.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dilenge D, Ascherl GF., Jr Variations of the ophthalmic and middle meningeal arteries: Relation to the embryonic stapedial artery. Am J Neuroradiol. 1980;1:45–54. [PMC free article] [PubMed] [Google Scholar]
- 33.Stenzel E, Göricke S, Temming P, Biewald E, Zülow S, Göbel J, et al. Feasibility of intra-arterial chemotherapy for retinoblastoma: Experiences in a large single center cohort study. Neuroradiology. 2019;61:351–7. doi: 10.1007/s00234-019-02153-9. [DOI] [PubMed] [Google Scholar]
- 34.Klufas MA, Gobin YP, Marr B, Brodie SE, Dunkel IJ, Abramson DH. Intra-arterial chemotherapy as a treatment for intraocular retinoblastoma: Alternatives to direct ophthalmic artery catheterization. Am J Neuroradiol. 2012;33:1608–14. doi: 10.3174/ajnr.A3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertelli E, Leonini S, Galimberti D, Moretti S, Tinturini R, Hadjistilianou T, et al. Hemodynamic and anatomic variations require an adaptable approach during intra-arterial chemotherapy for intraocular retinoblastoma: Alternative routes, strategies, and follow-up. Am J Neuroradiol. 2016;37:1289–95. doi: 10.3174/ajnr.A4741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quinn C, Tummala R, Anderson J, Dahlheimer T, Nascene D, Jagadeesan B. Effectiveness of alternative routes of intra-arterial chemotherapy administration for retinoblastoma: Potential for response and complications. Interv Neuroradiol. 2019:1591019919831953. doi: 10.1177/1591019919831953. doi: 10.1177/1591019919831953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daniels AB, Froehler MT, Pierce JM, Nunnally AH, Calcutt MW, Bridges TM, et al. Pharmacokinetics, tissue localization, toxicity, and treatment efficacy in the first small animal (rabbit) model of intra-arterial chemotherapy for retinoblastoma. Invest Ophthalmol Vis Sci. 2018;59:446–54. doi: 10.1167/iovs.17-22302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laurie NA, Gray JK, Zhang J, Leggas M, Relling M, Egorin M, et al. Topotecan combination chemotherapy in two new rodent models of retinoblastoma. Clin Cancer Res. 2005;11:7569–78. doi: 10.1158/1078-0432.CCR-05-0849. [DOI] [PubMed] [Google Scholar]
- 39.Yousef YA, Soliman SE, Astudillo PP, Durairaj P, Dimaras H, Chan HSL, et al. Intra-arterial chemotherapy for retinoblastoma: A systematic review. JAMA Ophthalmol. 2016;134:584–91. doi: 10.1001/jamaophthalmol.2016.0244. [DOI] [PubMed] [Google Scholar]
- 40.Chen M, Zhao J, Xia J, Liu Z, Jiang H, Shen G, et al. Intra-arterial chemotherapy as primary therapy for retinoblastoma in infants less than 3 months of age: A series of 10 case-studies. PLoS One. 2016;11:e0160873. doi: 10.1371/journal.pone.0160873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magan T, Khoo CT, Jabbour PM, Shields CL. Intra-arterial chemotherapy for retinoblastoma in a 2-month-old infant. Retin Cases Brief Rep. 2017;11:24–6. doi: 10.1097/ICB.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 42.Peterson EC, Elhammady MS, Quintero-Wolfe S, Murray TG, Aziz-Sultan MA. Selective ophthalmic artery infusion of chemotherapy for advanced intraocular retinoblastoma: Initial experience with 17 tumors. J Neurosurg. 2011;114:1603–8. doi: 10.3171/2011.1.JNS10466. [DOI] [PubMed] [Google Scholar]
- 43.Munier FL, Beck-Popovic M, Balmer A, Gaillard MC, Bovey E, Binaghi S. Occurrence of sectoral choroidal occlusive vasculopathy and retinal arteriolar embolization after superselective ophthalmic artery chemotherapy for advanced intraocular retinoblastoma. Retina. 2011;31:566–73. doi: 10.1097/IAE.0b013e318203c101. [DOI] [PubMed] [Google Scholar]
- 44.Venturi C, Bracco S, Cerase A, Cioni S, Galluzzi P, Gennari P, et al. Superselective ophthalmic artery infusion of melphalan for intraocular retinoblastoma: Preliminary results from 140 treatments. Acta Ophthalmol. 2013;91:335–42. doi: 10.1111/j.1755-3768.2011.02296.x. [DOI] [PubMed] [Google Scholar]
- 45.Muen WJ, Kingston JE, Robertson F, Brew S, Sagoo MS, Reddy MA. Efficacy and complications of super-selective intra-ophthalmic artery melphalan for the treatment of refractory retinoblastoma. Ophthalmology. 2012;119:611–6. doi: 10.1016/j.ophtha.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 46.Thampi S, Hetts SW, Cooke DL, Stewart PJ, Robbins E, Banerjee A, et al. Superselective intra-arterial melphalan therapy for newly diagnosed and refractory retinoblastoma: Results from a single institution. Clin Ophthalmol. 2013;7:981–9. doi: 10.2147/OPTH.S43398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taich P, Ceciliano A, Buitrago E, Sampor C, Fandino A, Villasante F, et al. Clinical pharmacokinetics of intra-arterial melphalan and topotecan combination in patients with retinoblastoma. Ophthalmology. 2014;121:889–97. doi: 10.1016/j.ophtha.2013.10.045. [DOI] [PubMed] [Google Scholar]
- 48.Parareda A, Català J, Carcaboso AM, Sola T, Cruz O, Díaz J, et al. Intra-arterial chemotherapy for retinoblastoma. Challenges of a prospective study. Acta Ophthalmol. 2014;92:209–15. doi: 10.1111/aos.12295. [DOI] [PubMed] [Google Scholar]
- 49.Ghassemi F, Ghanaati H, Karkhaneh R, Boujabadi L, Tabatabaie SZ, Rajabi MT. Outcome of retinoblastoma following limited sessions of intra-arterial chemotherapy in Iran. Iran J Radiol. 2014;11:e16958. doi: 10.5812/iranjradiol.16958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ong SJ, Chao AN, Wong HF, Liou KL, Kao LY. Selective ophthalmic arterial injection of melphalan for intraocular retinoblastoma: A 4-year review. Jpn J Ophthalmol. 2015;59:109–17. doi: 10.1007/s10384-014-0356-y. [DOI] [PubMed] [Google Scholar]
- 51.Akyüz C, Kıratlı H, Şen H, Aydın B, Tarlan B, Varan A. Intra-arterial chemotherapy for retinoblastoma: A single-center experience. Ophthalmologica. 2015;234:227–32. doi: 10.1159/000439357. [DOI] [PubMed] [Google Scholar]
- 52.Tuncer S, Sencer S, Kebudi R, Tanyıldız B, Cebeci Z, Aydın K. Superselective intra-arterial chemotherapy in the primary management of advanced intra-ocular retinoblastoma: First 4-year experience from a single institution in Turkey. Acta Ophthalmol. 2016;94:e644–51. doi: 10.1111/aos.13077. [DOI] [PubMed] [Google Scholar]
- 53.Michaels ST, Abruzzo TA, Augsburger JJ, Corrêa ZM, Lane A, Geller JI. Selective ophthalmic artery infusion chemotherapy for advanced intraocular retinoblastoma: CCHMC early experience. J Pediatr Hematol Oncol. 2016;38:65–9. doi: 10.1097/MPH.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 54.Leal-Leal CA, Asencio-López L, Higuera-Calleja J, Bernal-Moreno M, Bosch-Canto V, Chávez-Pacheco J, et al. Globe salvage with intra arterial topotecan-melphalan chemotherapy in children with a single eye. Rev Invest Clin. 2016;68:137–42. [PubMed] [Google Scholar]
- 55.Reddy MA, Naeem Z, Duncan C, Robertson F, Herod J, Rennie A, et al. Reduction of severe visual loss and complications following intra-arterial chemotherapy (IAC) for refractory retinoblastoma. Br J Ophthalmol. 2017;101:1704–8. doi: 10.1136/bjophthalmol-2017-310294. [DOI] [PubMed] [Google Scholar]
- 56.Chen M, Jiang H, Zhang J, Shen G, Jiang Y, Li H, Liu Z. Outcome of intra-arterial chemotherapy for retinoblastoma and its influencing factors: A retrospective study. Acta Ophthalmol. 2017;95:613–8. doi: 10.1111/aos.13333. [DOI] [PubMed] [Google Scholar]
- 57.Rishi P, Sharma T, Sharma M, Maitray A, Dhami A, Aggarwal V, et al. Intra-arterial chemotherapy for retinoblastoma: Two-year results from tertiary eye-care center in India. Indian J Ophthalmol. 2017;65:311–5. doi: 10.4103/ijo.IJO_843_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ammanuel S, Alexander MD, Damato B, Cooke DL, Halbach VV, Amans MR, et al. Improved procedural safety following protocol changes for selective ophthalmic arterial infusion of chemotherapy for treatment of ocular retinoblastoma. Interv Neuroradiol. 2018;24:345–50. doi: 10.1177/1591019918755088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hua J, Gang S, Yizhou J, Jing Z. Intra-arterial chemotherapy as second-line treatment for advanced retinoblastoma: A 2-year single-center study in China. J Cancer Res Ther. 2018;14:106–110. doi: 10.4103/jcrt.JCRT_722_17. [DOI] [PubMed] [Google Scholar]
- 60.Radros J, All-Eriksson C, Pal N, Holm S, Seregard S, Söderman M, et al. Intra-arterial chemotherapy for retinoblastoma in Sweden – Evaluation of treatment efficacy and complications. Acta Ophthalmol. 2018;96:e1040–1. doi: 10.1111/aos.13796. [DOI] [PubMed] [Google Scholar]
- 61.Rojanaporn D, Chanthanaphak E, Boonyaopas R, Sujirakul T, Hongeng S, Ayudhaya SSN. Intra-arterial chemotherapy for retinoblastoma: 8-year experience from a tertiary referral institute in Thailand. Asia Pac J Ophthalmol (Phila) 2019 doi: 10.22608/APO.2018294. doi: 10.22608/APO.2018294. [DOI] [PubMed] [Google Scholar]
- 62.Shields CL, Jorge R, Say EA, Magrath G, Alset A, Caywood E, et al. Unilateral retinoblastoma managed with intravenous chemotherapy versus intra-arterial chemotherapy. Outcomes based on the international classification of retinoblastoma. Asia Pac J Ophthalmol (Phila) 2016;5:97–103. doi: 10.1097/APO.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 63.Munier FL, Mosimann P, Puccinelli F, Gaillard MC, Stathopoulos C, Houghton S, et al. First-line intra-arterial versus intravenous chemotherapy in unilateral sporadic group D retinoblastoma: Evidence of better visual outcomes, ocular survival and shorter time to success with intra-arterial delivery from retrospective review of 20 years of treatment. Br J Ophthalmol. 2017;101:1086–93. doi: 10.1136/bjophthalmol-2016-309298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abramson DH, Marr BP, Dunkel IJ, Brodie S, Zabor EC, Driscoll SJ, et al. Intra-arterial chemotherapy for retinoblastoma in eyes with vitreous and/or subretinal seeding: 2-year results. Br J Ophthalmol. 2012;96:499–502. doi: 10.1136/bjophthalmol-2011-300498. [DOI] [PubMed] [Google Scholar]
- 65.Shields CL, Alset AE, Say EA, Caywood E, Jabbour P, Shields JA. Retinoblastoma control with primary intra-arterial chemotherapy: Outcomes before and during the intravitreal chemotherapy era. J Pediatr Ophthalmol Strabismus. 2016;53:275–84. doi: 10.3928/01913913-20160719-04. [DOI] [PubMed] [Google Scholar]
- 66.Dalvin LA, Kumari M, Essuman VA, Shohelly Shipa S, Ancona-Lezama D, Lucio-Alvarez JA, et al. Primary intra-arterial chemotherapy for retinoblastoma in the intravitreal chemotherapy era: Five years of experience. Ocul Oncol Pathol. 2019;5:139–46. doi: 10.1159/000491580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Francis JH, Levin AM, Zabor EC, Gobin YP, Abramson DH. Ten-year experience with ophthalmic artery chemosurgery: Ocular and recurrence-free survival. PLoS One. 2018;13:e0197081. doi: 10.1371/journal.pone.0197081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shields CL, Shelil A, Cater J, Meadows AT, Shields JA. Development of new retinoblastomas after 6 cycles of chemoreduction for retinoblastoma in 162 eyes of 106 consecutive patients. Arch Ophthalmol. 2003;121:1571–6. doi: 10.1001/archopht.121.11.1571. [DOI] [PubMed] [Google Scholar]
- 69.Wilson MW, Haik BG, Billups CA, Rodriguez-Galindo C. Incidence of new tumor formation in patients with hereditary retinoblastoma treated with primary systemic chemotherapy: Is there a preventive effect? Ophthalmology. 2007;114:2077–82. doi: 10.1016/j.ophtha.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 70.Lee TC, Hayashi NI, Dunkel IJ, Beaverson K, Novetsky D, Abramson DH. New retinoblastoma tumor formation in children initially treated with systemic carboplatin. Ophthalmology. 2003;110:1989–94. doi: 10.1016/S0161-6420(03)00669-9. [DOI] [PubMed] [Google Scholar]
- 71.Schueler AO, Anastassiou G, Jurklies C, Havers W, Wieland R, Bornfeld N. De novo intraocular retinoblastoma development after chemotherapy in patients with hereditary retinoblastoma. Retina. 2006;26:425–31. doi: 10.1097/01.iae.0000238548.97497.4c. [DOI] [PubMed] [Google Scholar]
- 72.Abramson DH, Francis JH, Dunkel IJ, Marr BP, Brodie SE, Gobin YP. Ophthalmic artery chemosurgery for retinoblastoma prevents new intraocular tumors. Ophthalmology. 2013;120:560–5. doi: 10.1016/j.ophtha.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 73.Abramson DH, Shields CL, Jabbour P, Teixeira LF, Fonseca JRF, Marques MCP, et al. Metastatic deaths in retinoblastoma patients treated with intraarterial chemotherapy (ophthalmic artery chemosurgery) worldwide. Int J Retina Vitreous. 2017;3:40. doi: 10.1186/s40942-017-0093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mathew AA, Sachdev N, Staffieri SE, McKenzie JD, Elder JE. Superselective intra-arterial chemotherapy for advanced retinoblastoma complicated by metastatic disease. J AAPOS. 2015;19:72–4. doi: 10.1016/j.jaapos.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 75.Kaliki S, Shields CL, Rojanaporn D, Al-Dahmash S, McLaughlin JP, Shields JA, et al. High-risk retinoblastoma based on international classification of retinoblastoma: Analysis of 519 enucleated eyes. Ophthalmology. 2013;120:997–1003. doi: 10.1016/j.ophtha.2012.10.044. [DOI] [PubMed] [Google Scholar]
- 76.Rodriguez A, Zugbi S, Requejo F, Deu A, Sampor C, Sgroi M, et al. Combined high-dose intra-arterial and intrathecal chemotherapy for the treatment of a case of extraocular retinoblastoma. Pediatr Blood Cancer. 2018;65:e27385. doi: 10.1002/pbc.27385. [DOI] [PubMed] [Google Scholar]
- 77.Habib LA, Francis JH, Fabius AW, Gobin PY, Dunkel IJ, Abramson DH. Second primary malignancies in retinoblastoma patients treated with intra-arterial chemotherapy: The first 10 years. Br J Ophthalmol. 2018;102:272–275. doi: 10.1136/bjophthalmol-2017-310328. [DOI] [PubMed] [Google Scholar]
- 78.Shields CL, Bianciotto CG, Jabbour P, Griffin GC, Ramasubramanian A, Rosenwasser R, et al. Intra-arterial chemotherapy for retinoblastoma: Report No.2, treatment complications. Arch Ophthalmol. 2011;129:1407–1415. doi: 10.1001/archophthalmol.2011.151. [DOI] [PubMed] [Google Scholar]
- 79.Dalvin LA, Ancona-Lezama D, Lucio-Alvarez JA, Masoomian B, Jabbour P, Shields CL. Ophthalmic vascular events after primary unilateral intra-arterial chemotherapy for retinoblastoma in early and recent eras. Ophthalmology. 2018;125:1803–11. doi: 10.1016/j.ophtha.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 80.De la Huerta I, Seider MI, Hetts SW, Damato BE. Delayed cerebral infarction following intra-arterial chemotherapy for retinoblastoma. JAMA Ophthalmol. 2016;134:712–4. doi: 10.1001/jamaophthalmol.2016.0025. [DOI] [PubMed] [Google Scholar]
- 81.Maidana DE, Pellegrini M, Shields JA, Shields CL. Choroidal thickness after intraarterial chemotherapy for retinoblastoma. Retina. 2014;34:2103–9. doi: 10.1097/IAE.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 82.Francis JH, Abramson DH, Gobin YP, Marr BP, Tendler I, Brodie SE, et al. Efficacy and toxicity of second-course ophthalmic artery chemosurgery for retinoblastoma. Ophthalmology. 2015;122:1016–22. doi: 10.1016/j.ophtha.2014.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tse BC, Steinle JJ, Johnson D, Haik BG, Wilson MW. Superselective intraophthalmic artery chemotherapy in a nonhuman primate model: Histopathologic findings. JAMA Ophthalmol. 2013;131:903–11. doi: 10.1001/jamaophthalmol.2013.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Steinle JJ, Zhang Q, Thompson KE, Toutounchian J, Yates CR, Soderland C, et al. Intra-ophthalmic artery chemotherapy triggers vascular toxicity through endothelial cell inflammation and leukostasis. Invest Ophthalmol Vis Sci. 53:2439–45. doi: 10.1167/iovs.12-9466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Levin AM, Francis JH, McFadden M, Brodie S, Gobin YP, Abramson DH. Association of electroretinography with visual outcomes after ophthalmic artery chemosurgery for retinoblastoma in ICRb D and E eyes. PLoS One. 2019;14:e0210647. doi: 10.1371/journal.pone.0210647. [DOI] [PMC free article] [PubMed] [Google Scholar]