Abstract
Purpose:
To suggest a low cost, non-contact smartphone-based screening system in retinopathy of prematurity (ROP), and to illustrate its potential clinical application as a potential future tool for teleophthalmology.
Methods:
Neonatal intensive care unit (NICU)-based bedside ROP screening done between January 2018 and May 2018. Documentation of ROP was done by using a smartphone and +40D, +28D, or +20D indirect non-contact condensing lenses. By using the coaxial light source of the phone, this system works as an indirect ophthalmoscope that creates a digital image of the fundus. With smartphone-based camera we extracted high-quality still images extracted from the video clip.
Results:
Total of 228 eyes of 114 infants screened for ROP between January 2018 and May 2018. Incidence of total ROP was 23.68%, out of which incidence of type 1 ROP was 8.77%. After initial screening with indirect ophthalmoscope, we uesd smartphone imaging to document ROP in 28 eyes out of 55 eyes having ROP. Image quality was good in 89.28% eyes. Field of view vary from 46°, 53°, and 90° with +20D, +28D, and +40D indirect condensing lenses, respectively, which gives excellent images for bedside ROP documentation.
Conclusion:
The described technique of smartphone fundus photography is a light weight, cost-effective, user friendly, high-quality wide-field fundus photographs for bedside documentation of ROP in NICUs using readily available instruments that are handy and portable with simple power sources. Smartphones has the potential to be operated with only one hand. It can also be used as a future telescreening device.
Keywords: Condensing lens-Smartphone-MIIRetCam (CSM) device assembly, neonatal intensive care unit, retinopathy of prematurity
Retinopathy of prematurity (ROP) is a leading cause of childhood blindness worldwide. In India, the incidence of ROP is increasing because of expanding neonatal care and improved neonatal survival rate. The incidence of ROP in India is reported between 38 and 51.9% in low-birth-weight infants.[1] According to early treatment for ROP early detection and prompt treatment can reduce unfavorable outcomes secondarily to type 1 high-risk prethreshold ROP.[2] In present study, early detection, image acquisition, and interpretation are done by an experienced ophthalmologist.
The current gold standard method for ROP screening requires indirect ophthalmoscope with the condensing lens.[3] Nowadays, digital fundus photography is used in ROP screening to facilitate consultation in difficult cases and also contribute to medicolegal affairs. However, it is not easy to take a fundus photograph of a newborn without professional equipment such as the RetCam system,[4] which is costly and unaffordable in most of the local medical healthcare systems. The ease of use, portability, and cost-effectiveness of smartphone fundoscopy can share the advantages of telemedicine, either to document the fundus status or to consult an experienced senior ophthalmologists and also helps in medicolegal affairs.[5] Besides, the light source of smartphones is safe for human eyes. Retinal irradiance from smartphones is less than that from an indirect ophthalmoscope.[6]
The smartphone has become the basic necessity in today's world. With advanced technology and ease of handling for capturing images smartphones are commonly used as the clinical imaging device in ophthalmology.[7] Modern smartphone camera is already equipped with a high-quality optical system and a coaxial light source, which can be used to capture high-quality retinal images. Various applications and devices are available for smartphone cameras that not only increases the image quality of fundoscopy, but also cost-effective and give ease of handling while capturing ROP images.[3,8] In this study we used condensing lens with smartphone attached to cost-effective, handy, mobile, non-contact device to capture wide-field and good bedside fundus images of ROP infants in an Indian population.
Methods
It is an observational study. Bedside fundus images of preterm infants initially screened with indirect ophthalmoscope and diagnosed having ROP were captured in neonatal intensive care unit (NICU) between January 2018 to May 2018. All infants were awake during fundus examination and smartphone imaging. Pupils were well dilated using 0.4% tropicamide +2.5% phenylephrine eye drops three times till full dilatation occurred and only 2% proparacaine drops as topical anesthesia was administered for applying a pediatric wire speculum and performing globe rotation. One nurse assisted in holding infant's head stable.
Images were captured with a smartphone, iPhone 5S (Apple Inc., Cupertino, CA, USA) and either 20D, 28D, or 40D lens (Volk Optical Inc., Mentor, OH, USA). 20D, 28D, and 40D lenses give a field of view of 46°, 53°, and 90°, respectively.[3] Since, it is an initial experience we tried capturing images from all three defined lenses randomly. Condensing lens and a smartphone (iPhone 5S) under original camera settings is used to record a video, with a constant, coaxial inbuilt light source and capturing snapshots out of the video help us in documenting ROP. MIIRetCam (an invention used for capturing adult fundus by Dr. Ashish Sharma),[9] was used to hold lens and smartphone at a fixed working distance [Fig. 1]. Alternately, a self-designed device consisting of 40 mm diameter wide and 15 cm long polyvinyl chloride (PVC) pipe painted matt black from inside (black tube), smartphone attached at one end with the help of universal mobile holder available online and condensing lens stabilized on other end of tube with the help of black electrical insulation tape, can be used to capture same quality images [Fig. 2]. The autofocus capability of smartphone camera maintains the image quality to perform indirect fundoscopy. The pupil should be fully dilated to reduce light reflections. Condensing lens-smartphone-MIIRetCam/black tube device assembly (CSD) was turned to different angles to image retinal periphery. CSD assembly was aligned in a straight axis at a particular distance, stabilized with infants forehead support by one hand and another hand can be used occasionally to rotate the globe with pediatric wire vectis, for better periphery visualization. It is a single examiner technique without the need of any assistant during image capture. Single device can hold all the lenses described with an additional lens holder. Ophthalmologist holds “lens holding cuff” of CSD assembly to take retina images.
Figure 1.
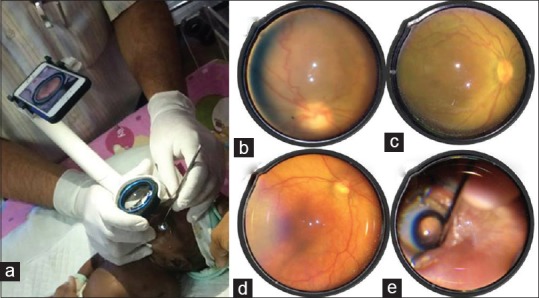
Technique of Smart retinopathy of prematurity (ROP) and field of view from different condensing lenses – (a) showing technique to hold condensing lens-smartphone-MIIRetCam (CSM) device assembly while ROP screening, (b) shows field of view of 30° from +20D lens, (c) field of view of 55° from +28D lens, (d) field of view of 90° from +40D lens, (e) showing technique to rotate the globe with pediatric wire vectis to visualize retinal periphery
Figure 2.
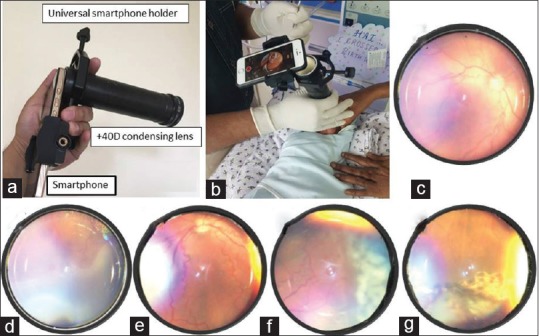
Make It Yourself (MIY) assembly and technique of Smart retinopathy of prematurity (ROP) and field of view through 40D condensing lenses – (a) showing MIY device assembly, (b) technique to hold condensing lens-smartphone-black tube (MIY) assembly while ROP screening, (c) shows field of view from +40D lens, (d) stage 3 ridge and avascular retina, (e) plus disease with dilated and tortuous vessels, (f) fresh laser marks, (g) scars marks after laser treatment
The lens should be clean without any dust particles on it. Otherwise, it may mislead the autofocus of the phone camera. The eyelids were widely opened by the use of pediatric wire speculum and pupil should be fully dilated in a minimal illuminated room to minimize glare during fundoscopy, with the nurse monitoring the infant during the course of examination. Hazy vitreous and vasculosa lentis were other reasons which hampered good quality image acquisition. The infant's cornea should be kept moist with sterile distilled water. Through a clear medium, the iPhone camera can automatically focus on the retina. The recording was done by universally available inbuilt video mode of smartphone for approximately 1 min duration and the video was kept on during the whole examination. Video mode automatically focuses to give clear imaging. If the light reflection is too severe, the light intensity can be reduced by covering the flash with a layer of micropore tape (3M, St. Paul, MN, USA).[10] Once recording was completed, still images were captured from the video sequence by taking a screenshot (by pressing and holding home and sleep/wake button simultaneously). Videos were taken at 30 fps at 1080p resolution, with 1 min capture files were 150–200 MB in size. Screenshots were 1–2 MB at maximum resolution. However, we found that these files could be compressed on transmission through secure e-mail/WhatsApp software down to approximately 100 KB and still be adequate for clinical use. Images captured and read by a single examining ophthalmologist. These images were also transferred for explaining to (ophthalmologist and neonatologists) elsewhere by internet-guided inbuilt softwares in smartphone, customizing telemedicine in ROP screening. Examiner avoided imaging in infants with physical barriers around the eye, such as the obstructive modes of ventilatory support, poorly dilating pupil, and eyes with hazy medias, all of which may affect image quality.
Single ophthalmologist (AG) trained in ROP screening captured all images. Image quality was graded as good and poor based on ability of grader to determine the dilatation and tortuosity of vessels or presence of different stages of ROP in the images. “Good” was defined as an image in which there was a clear view of optic nerve and vessels and the grader could easily discern the dilatation and tortuosity of vessels or presence of various ROP stages with or without glare artifact, which ensured accurate diagnosis, and “poor” image in which the grader was unable to clearly visualize and determine the characteristics of the retina or vessels, and thus unable to make correct diagnosis.
Telemedicine refers to the use of telecommunication and information technologies to provide clinical healthcare at a distance. It involves capturing and transporting patient data for subsequent interpretation by a remote expert. Simultaneously, with the help of these recorded ROP images parents were also educated about the importance of ROP screening.
Table 1 highlights the comparison of different imaging modalities used for fundoscopy in infants with ROP.
Table 1.
Comparison of different imaging modalities for retinopathy of prematurity imaging
| Imaging modality | Field of view | Setting for use | Staffing requirement | Advantages | Disadvantages |
|---|---|---|---|---|---|
| SROP camera Condensing lens • +20D • +28D • +40D (attached with MIIRETCAM device) |
46 degree 53 degree 90 degree |
• Special care baby unit • Outpatient department • Theatre |
• Ophthalmologist • Nursing staff to hold baby and monitor vital signs. |
• Non-contact based • Portable • Wide field of view • Cost effective • Able to image till ora serrata through sclera depression • High-resolution images |
• Only colour imaging available |
| NIDEK Camera[3] | 30 degree | • Special care baby unit • Outpatient department • Theatre |
•Ophthalmologist | • Non-contact based • Portable |
• Low resolution images • Narrow field of view • Only colour imaging available • Unable to image till ora serrata |
| Video indirect ophthalmoscopy[3] | 53 degrees (28D lens) 46 degrees (20D lens) |
• Special care baby unit • Outpatient department • Theatre |
• Ophthalmologist • Nursing staff to monitor vital signs |
• Non-contact based • Portable • Cost effective • Able to image till ora serrata through scleral indentation |
• Low resolution images • Only colour imaging available |
| 3Netra Neo widefield camera[13] | 120 degrees | • Special care baby unit • Outpatient department • Theatre |
• Ophthalmologist • Nursing staff to monitor vital signs |
• Portable • Wide fundal field of view • Fast image acquisition |
• Contact based • Heavy weight camera • Unable to image out to ora serrata • Costly |
| RetCam Widefield camera[14,15] | 130 degrees | • Special care baby unit • Outpatient department • Theatre |
•Ophthalmologist • Nursing staff to monitor vital signs |
• Portable • Wide fundal field of view • Fast image acquisition • Colour and fluorescein angiographic imaging available |
• Contact based • Heavy weight camera • Sedation or general anaesthesia essential only for high quality angiograms • Unable to image out to ora serrata • Costly |
| Optos ultrawidefield camera[17] | 200 degrees | • Outpatient department | •Ophthalmologist • Nursing staff to monitor vital signs • Ophthalmic photographer |
• Non-contact based • Fast image acquisition • High resolution images • Widel field of view • Colour and angiographic imaging available • No sedation required |
• Non-portable • Unable to image out to ora serrata • Costly • Ophthalmic photographer needed for image capture |
Results
A total of 228 eyes of 114 preterm infants were initially screened with indirect ophthalmoscope for ROP in NICUs of 17 referral hospitals in Kochi, Kerala between January 2018 and May 2018. All infants <1750 g birth weight and <34 weeks gestational age were screened according to the National Neonatology Forum (NNF) Clinical Practise Guidelines.[11] ROP was observed in 54 eyes with an incidence of 23.6% out of which type 1 high-risk prethreshold ROP was seen in 20 eyes with an incidence of 8.7%. Smartphone-based fundoscopy was used to document ROP in 28 out of 54 eyes diagnosed as ROP. Image quality was “good” in 25 out of 28 (89.2%) eyes undergone smartphone imaging. Three eyes showing poor vessel and retinal differentiation were graded as “bad”. Six eyes with zone 1 ROP were documented without globe contact or rotation. Glare and artifacts were seen in 20 out of these 28 eyes (71.4%) but did not hamper in image clarity in most of the eyes. Using different condensing lenses varying from +20D, +28D, and +40D give us visualization with a field of view of 46 °, 53°, and 90,° respectively. Fig. 1 showing the technique of Smart ROP image capture (video 1) and comparison of various images taken from different condensing lenses. Working distance from infant's eye to condensing lens measured was approximately 5 inches, 3 inches, and 1.5 inches with +20D, +28D, and +40D lens, respectively. We observed comparatively small field of view with +20D lens and more chances of peripheral lens edge glare with +40D condensing lens. Wide-field visualization and peripheral retinal fundoscopy till ora serrata was possible in eyes imaged with +28D or +40D lens (video 2, video 3). Various presentations of ROP are seen in Fig. 3. Fig. 4A shows fundus images of zone 1 ROP before and after anti-vascular endothelial growth (VEGF) injection and rescue laser treatment. Fig. 4B shows retinal images of aggressive posterior ROP (APROP) before and after laser monotherapy.
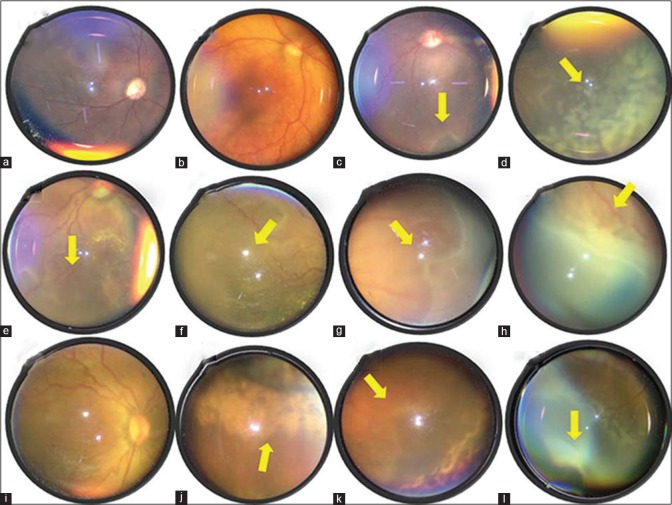
Figure 3.
Various retinopathy of prematurity (ROP) presentations – (a) glare due to mid-dilated pupil, (b) wide-field view of a normal retina, (c) plus disease with ridge (arrow) in zone 1, (d) laser marks (arrow), (e) aggressive posterior ROP in zone 1, (f) demarcation between vascular and avascular retina (arrow), (g) ridge (arrow) in zone 2, (h) stage 3 fibrovascular proliferation in zone 2 (arrow), (i) dilated tortuous vessels in all four quadrants s/o plus disease, (j) laser scar marks in periphery, (k) skip area between normal retina and laser marks (arrow), (l) ora serrata nicely seen with scleral depression
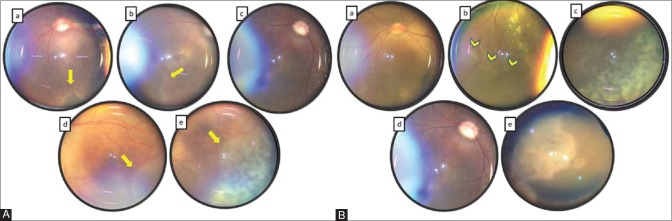
Figure 4.
(A) Case of zone 1 retinopathy of prematurity (ROP) showing (a) plus disease with ridge (arrow) in the right eye, (b) zone 1 with ridge (arrow) in the left eye, (c) complete resolution of plus disease and ridge after anti-vascular endothelial growth (VEGF) injection in the left eye, (d) recurrence of ridge (arrow) after 4 weeks of anti-VEGF injection, (e) shows rescue laser treatment marks (arrow) anterior to ridge in the left eye. (B) Case of aggressive posterior ROP (APROP) showing (a) plus disease in zone 1, (b) demarcation between vascular and avascular retina (arrowheads) at zone 1 edge, (c) laser marks, (d) complete regression of plus disease, (e) laser scar marks (arrow) in retinal periphery
Discussion
Use of smartphone to capture retinal images has several advantages with small learning curve. First, a smartphone has an almost coaxial, constant, and powerful light source that can directly illuminate the retina and easy to photograph. Second, the smartphone camera can adjust automatically both, exposure time and focus on the retina. Third, fundoscopy with a smartphone is an inexpensive, easy, non-contact, and portable way to record the retinal condition of patients with ROP. Fourth, the smartphone and MIIRetCam or black PVC tube being a light weight gadget, the CSD assembly can be supported with a single hand to capture retina pictures, thus no need of multiple costly gadgets or additional assistants to hold and carry them. This is probably the best and the only way for a single ophthalmologist who has to visit multiple NICU setups on the same day to achieve good documentation. We have found that good documentation greatly improves the communication with the parents concerned and thereby ensures better compliance in treatment and follow-up. Fifth, easy availability and quick data transfer facility make it useful and effective telescreening tool to share and discuss ROP even in remote places. Use of +28D and +40D in addition to +20D condensing lenses have an advantage of wide-field visualization of retina. It can also help in visualization till far periphery without much scleral depression. Although the quality of the picture is not equivalent to those taken by professional equipment like RetCam, the cost performance has more value in developing countries like India. In addition, availability of a smartphone in local and remote hospitals or relatively poor medical healthcare environments is easy nowadays. This technique is also helpful in general patient consultation by experienced ophthalmologists, and the ease of sharing images makes smartphone fundoscopy an extremely useful technique for ROP screening and telemedicine.[10]
Stabilizing CSD device assembly in one hand and using other hand for eyeball rotation and/or sclera depression ease us to capture retinal periphery images equivalent to professional wide field fundus imaging systems. According to Lin et al., direction of light and lens should be manually adjusted for good recording but our device assembly facilitates automatically adjusted coaxial image with minimum effort.[10] On an average, the time taken by an experienced ophthalmologist for a full examination under topical anesthesia is approximately 1 min, which is slightly longer than that required by a professional wide-field retinal imaging system. Still, cost-affectivity, portability, ease of handling, and telescreening facility makes smartphone imaging more useful than any other imaging modality.
ROP imaging from KIDROP differs from Smart ROP in various aspects. Firstly, KIDROP composed of 3–4 trained ophthalmic staff, RetCam shuttle, and a laptop equipped with additional special software to record ROP images which are assessed by ophthalmologist elsewhere.[12] While, Smart ROP needs single-trained person (mainly ophthalmologist) and a mobile light weight device to hold smartphone and condensing lens using inbuilt video settings of phone to record ROP. Probe weight of contact imaging devices like 3 netra neo is 310 g and that of RetCam shuttle is still heavier exerting undue pressure over eyeball during examination, especially in the hands of beginners and trainees. Smartphone-based fundus camera have reasonably good field of view of 53° with +28D and 90° with +40D condensing lens, which is not wide as 3 netra neo (120°),[12] RetCam (130°),[13] or Optos imaging system (200°).[3,14] RetCam and 3 netra neo can through excessive pressure on the eye affect the accurate diagnosis of plus disease, a problem that would not be expected of a non-contact system.[14] Non-contact technique used in the Smart ROP though has lesser field of view as compared to previously mentioned techniques but has ease of portability and the amount of pressure exerted on globe is practically negligible. Moreover, cost of MIIRetCam device, in addition to condensing lens easily available in clinic and personal smartphone, is far less than the price of 3 netra neo, RetCam shuttle, or Optos fundus camera. Using black tube with universal smartphone holder further makes it affordable even for beginners. Smart ROP screening is possible with all the smartphones available in market.
Smartphone-based fundus camera was able to obtain “good” images of the retina with wide enough field of view and sufficient quality to grade the presence of ROP in 89.28% eyes of screened premature infants. We found good quality image in 89.28% eyes captured for ROP which is comparable with 90–99% good quality image seen in Pictor non-contact camera,[15] RetCam,[13,16] 3 netra neo,[12] and Optos dual wavelength scanning laser ophthalmoscope.[14] It is anticipated that newer smartphone-based cameras with better image acquisition will aid in increasing this percentage even further.
Smartphone fundoscopy has certain limitations. Limitation of MIIRetCam or black tube is the learning curve involved and poor image quality while using 20D lens. The nursing assistant needs to hold the head and pupil has to be well dilated. Light emitted by the flash is much strong and divergent than the light source of binocular indirect ophthalmoscope or professional wide-field imaging systems. As of now the technology is used mainly for documentation of ROP in infants already diagnosed after ROP screening by indirect ophthalmoscopy. There are some online available applications which have the advantage of multiple inbuilt light control options. Covering the flash with tape can be an alternate way to reduce light intensity.[17] It is an initial experience with this novel technique of mobile smartphone ROP imaging, stabilizing, and capturing images with only single hand. Presence of increased working eye to lens distance and comparatively small field of view with +20D lens suggest +28D and +40D lens as preferred condensing lenses for initial experience in wide-field ROP imaging. Presence of a single examiner for capturing and accessing ROP images warrants more studies to test image accuracy. The strength of this study is using single hand for stabilizing mobile smartphone over the infant's eye, use of non-contact technique, utilizing second hand of same examiner for visualizing retinal periphery, and without the use of bulky and costly imaging cameras, we were able to capture wide-field fundus images for ROP screening and documentation. Our initial experience using portable, high data storage capacity, cost-effective mobile smartphone can suggest that a mobile phone-based retinal camera can play an important role in infants with ROP.
A portable hand-held smartphone can obtain fundoscopy of good quality. Condensing lens-Smartphone-MIIRetCam device assembly is light weight, non-contact, portable technology with a coaxial light source for fundoscopy. Smartphone fundoscopy can serves as an effective educational tool for educating NICU staff and parents which may help with compliance. It also provides reliable, defensible medicolegal documentation. Smartphone-based fundoscopy can be used to visualize fundus till ora serrata. Digital fundus photographs can be sent immediately and conveniently through the WhatsApp or e-mails. For non- institutional practise and single practitioners cost and portability of the instrument remains a major issue. This technique is relatively easy to master and cost-effective, and above all, with proper training of observers, this technique has a potential advantage of expanding smartphone fundoscopy for telemedicine in developing country like India where cost and availability is a considerable problem. Our initial experience with SROP can help anyone who wishes to perform a ROP imaging and make appropriate diagnosis in a cost-effective manner.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.ijo.in
References
- 1.Sen P, Rao C, Bansal N. Retinopathy of prematurity: An update. Sci J Med Vis Res Foun. 2015;XXXIII:93–6. [Google Scholar]
- 2.Revised indications for treatment of retinopathy of prematurity: Results of early treatment of retinopathy of prematurity randomized trial. Early Treatment for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 2003;121:1684–96. doi: 10.1001/archopht.121.12.1684. [DOI] [PubMed] [Google Scholar]
- 3.Fung TH, Smith LM, Patel CK. Contemporary imaging of retinopathy of prematurity. Infant. 2014;10:143–6. [Google Scholar]
- 4.Ells AL, Holmes JM, Astle WF, Williams G, Leske DA, Fielden M, et al. Telemedicine approach to screening for severe retinopathy of prematurity: A pilot study. Ophthalmology. 2003;110:2113–7. doi: 10.1016/S0161-6420(03)00831-5. [DOI] [PubMed] [Google Scholar]
- 5.Bastawrous A. Smartphone fundoscopy. Ophthalmology. 2012;119:432–3. doi: 10.1016/j.ophtha.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Kim DY, Delori F, Mukai S. Smartphone photography safety. Ophthalmology. 2012;119:2200–1. doi: 10.1016/j.ophtha.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Lord RK, Shah VA, San Filippo AN, Krishna R. Novel uses of smartphones in ohthalmology. Ophthalmology. 2010;117:1274. doi: 10.1016/j.ophtha.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Maamari RN, Keenan JD, Fletcher DA, Margolis TP. A mobile phone-based retinal camera for portable wide field imaging. Br J Ophthalmol. 2014;98:438–41. doi: 10.1136/bjophthalmol-2013-303797. [DOI] [PubMed] [Google Scholar]
- 9.Sharma A, Subramaniam SD, Ramachandran KI, Lakshmikanthan C, Krishna S, Sundaramoorthy SK. Smartphone-based fundus camera device (MII Ret Cam) and technique with ability to image peripheral retina. Eur J Ophthalmol. 2016;26:142–4. doi: 10.5301/ejo.5000663. [DOI] [PubMed] [Google Scholar]
- 10.Lin SJ, Yang CM, Yeh PT, Chang Ho T. Smartphone fundoscopy for retinopathy of prematurity. Taiwan J Ophthalmol. 2014;4:82–5. [Google Scholar]
- 11.Pejaver RK, Vinekar A, Bilagi A. National Neonatology Forum's Evidence Based Clinical Practice Guidelines 2010. Retinopathy of Prematurity (NNF India, Guidelines). [cited 2015 Jun 29] [Last accessed on 2015 Jun 15]. Available from: http:// www.ontop-in.org/ontop-pen/Week-12-13/ROP NNFGuidelines.pdf .
- 12.Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, et al. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62:41–9. doi: 10.4103/0301-4738.126178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiang MF, Wang L, Busuioc M, Du YE, Chan P, Kane SA, et al. Telemedical retinopathy of prematurity diagnosis: Accuracy, reliability, and image quality. Arch Ophthalmol. 2007;125:1531–8. doi: 10.1001/archopht.125.11.1531. [DOI] [PubMed] [Google Scholar]
- 14.Patel CK, Fung THM, Muqit MMK, Mordant DJ, Brett J, Smith L, et al. Ultrawide field imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye (Lond) 2013;27:589–96. doi: 10.1038/eye.2013.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sasipan GP, David KW, Sharon FF. Retinal imaging in premature infants using the Pictor noncontact digital camera. J AAPOS. 2014;18:321–6. doi: 10.1016/j.jaapos.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thanos A, Yonekawa Y, Todorich B, Moshfeghi D, Trese MT. Screening and treatments using telemedicine in retinopathy of prematurity. Eye Brain. 2016;8:147–51. doi: 10.2147/EB.S94440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haddock LJ, Kim DY, Mukai S. Simple, inexpensive technique for high-quality smartphone fundus photography in human and animal eyes. J Ophthalmol 2013. 2013 doi: 10.1155/2013/518479. doi: 10.1155/2013/518479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.