A female born at 36 weeks of gestation with a birth weight of 1800 grams and history of seizures and respiratory distress was referred for retinopathy of prematurity screening at the age of 4 weeks. On general physical examination, multiple gray brown vesiculopapular skin lesions were noted on the flexor aspects of all four limbs, sides of the abdomen, and in the genital area [Fig. 1]. Dilated fundus examination revealed tortuous and dilated vessels at posterior pole along with large vascular loops limited to zone 1. There was the presence of Roth spots and multiple flame-shaped hemorrhages [Fig. 2]. Fundus fluorescein angiography (FFA) was done using RetCam (Clarity Medical Systems, Pleasanton, CA, USA). It revealed delayed arm-to-retina circulation time of more than 5 sec. Retinal arteries were seen only till posterior to the equator with large mid-peripheral vascular loops. Gross peripheral capillary nonperfusion and peripapillary capillary plexus were seen for about two to four disc diameters in both eyes. The right eye showed leakage from the disc and the left eye showed leakage from the tortuous vessels [Figs. 3 and 4]. Scatter laser of the avascular retina was done in both the eyes sparing the presumed macular area. The follow-up showed vitreous hemorrhage in the right eye and the left eye showed raised neovascular frond at the disc for which supplement laser treatment of the remaining avascular area sparing the macula was done. The right eye progressed to inoperable retinal detachment and the neovascularization of the left eye regressed [Fig. 5]. In view of the diagnosis of incontinentia pigmenti (IP), retrospective birth history and examination of mother revealed a history of two male stillbirths before this baby and a history of seizure early in the neonatal period. However, no fundus or dental abnormalities were seen in the mother. The parents refused any genetic evaluation of the baby or the mother. FFA clearly revealed the avascular loops for which aggressive laser could be done sparing the macula.
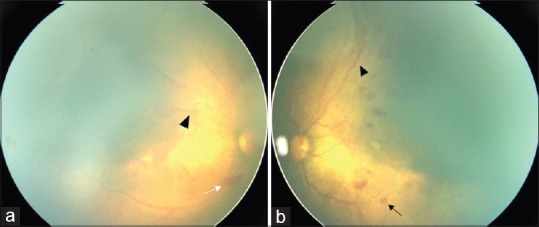
Figure 1.

Multiple grayish-brown vesiculopapular skin lesions visible on the flexor aspects of limbs and sides of the abdomen
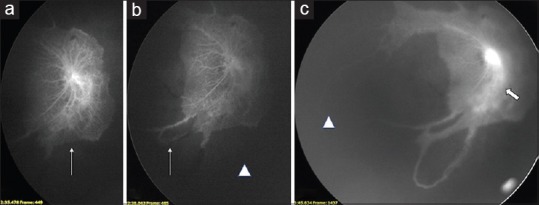
Figure 2.
Dilated fundus photograph of the (a) right and (b) left eyes showing tortuous and dilated vessels (black arrowheads) at posterior pole along with large vascular loops in zone 1. (b) There was the presence of Roth spots (black arrow) and multiple flame-shaped hemorrhages (white arrow) as well
Figure 3.
(a and b) FFA photographs of right eye: The retinal arteries were seen only till posterior to the equator with large mid-peripheral vascular loops (white arrows). There was gross peripheral capillary nonperfusion and peripapillary capillary plexus could be seen for about two to four discs diameter (arrowheads). (c) Late phase shows leakage from the disc (white arrows)
Figure 4.
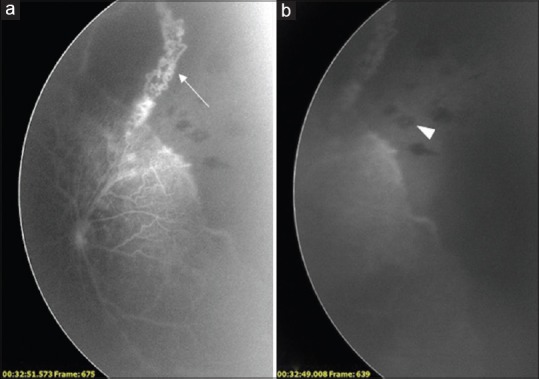
FFA photographs of the left eye show similar findings like large nonperfused area, vascular loops (a) and Roth spots (b) as right eye
Figure 5.
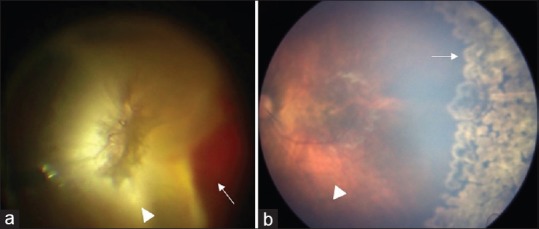
(a) Right eye developed vitreous hemorrhage (arrow) and retinal detachment (arrowhead) during follow-up period. (b) Left eye shows regressed neovascularization with scatter laser marks (arrow) with attached retina (arrowhead)
Discussion
IP is a rare X-linked dominant syndrome, also known as an oculo-dento-cerebro-cutaneous syndrome, which is characterized by gray to brown skin lesions.[1] The typical IP skin rash, avascularity in the eye with a history of seizures in the baby, and the history of stillbirth of previous male siblings clinched the diagnosis of IP.[2] The avascular ischemic retina leads to the release of the Vascular endothelial growth factors (VEGFs) and vasoproliferation. If left untreated, it can lead to advanced retinal complications such as traction retinal detachment.[3,4] We recommend an early FFA to document retinal avascularity in patients of IP and an early and aggressive laser treatment sparing the macula to prevent terminal complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Carney RG. Incontinentia pigmenti. A world statistical analysis. Arch Dermatol. 1976;112:535–42. [PubMed] [Google Scholar]
- 2.Minic S, Trpinac D, Obradovi’c M. Incontinentia pigmenti diagnostic’criteria update. Clin Genet. 2014;85:536–42. doi: 10.1111/cge.12223. [DOI] [PubMed] [Google Scholar]
- 3.Chen CJ, Han IC, Goldberg MF. Variable expression of retinopathy in a pedigree of patients with incontinentia pigmenti. Retina. 2015;35:2627–32. doi: 10.1097/IAE.0000000000000615. [DOI] [PubMed] [Google Scholar]
- 4.Tzu JH, Murdock J, Parke DW, 3rd, Warman R, Hess DJ, Berrocal AM. Use of fluorescein angiography in incontinentia pigmenti: A case report. Ophthalmic Surg Lasers Imaging Retina. 2013;44:91–3. doi: 10.3928/23258160-20121221-20. [DOI] [PubMed] [Google Scholar]


