A 6-year-old male child presented with diminution of vision in left eye since 2 months. His corrected distant visual acuity in right eye was 6/18 and OS had no light perception. Systemic examination revealed hypopigmented skin lesions over arms, trunk, and legs [Fig. 1]. Retinal examination of right eye showed gliosis over the disc with dilated and tortuous retinal arteries and veins in the superotemporal quadrant with a large area of avascular retina and neovascularization [Fig. 2a]. Left eye was prepthisical. Fundus fluorescein angiography (FFA) showed extensive areas of retinal capillary non-perfusion (CNP) temporal to macula with leaking retinal neovascularisation [Fig. 2b]. Optical coherence tomography (OCT) of right eye showed a blunted foveal pit and irregular outer plexiform layer with inner retinal thinning temporal to the fovea [Fig. 3a]. OCT angiography (OCTA) revealed loss of the superficial and deep capillary plexus, with an intact choriocapillaris superotemporal to the fovea. Foveal avascular zones of both superficial and deep capillary plexus were very small (area of 0.143 mm2) with abnormal vessels suggestive of foveal hypoplasia [Fig. 3b]. From the history, dermatological and ocular findings; a diagnosis of incontinentia pigmenti (IP) was made.[1,2] Laser photocoagulation was done to the CNP areas. At 4 months post laser follow-up, the BCVA was stable at 6/18 [Fig. 4].
Figure 1.

Clinical photograph showing facial pigmentation on the cheeks and sparse, wiry hair, and hypopigmentation along Blaschko's lines
Figure 2.
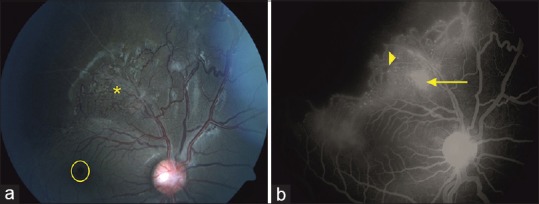
Fundus picture at presentation showing gliosis over the disc, macular pseudohole (yellow circle) with superotemporal neovascularization (asterisk) and avascular retina (a). FFA at presentation shows the small FAZ, pin point leaks at the site of aneurysms (arrowhead), and leakage at the site of neovascularization with extensive CNP superotemporally (b)
Figure 3.
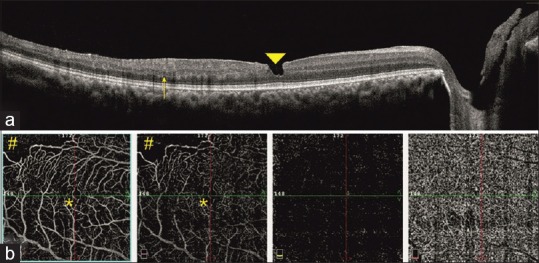
OCT at presentation shows the ERM, inner layer loss at the macula (arrowhead). In addition, it demonstrates the loss of retinal architecture temporal to the fovea (arrow) with retinal thinning (a). OCTA shows the superotemporal flow voids in the region of retinal ischemia (hashtag) with a small FAZ in the superficial and deep capillary plexus (asterisk) (b)
Figure 4.
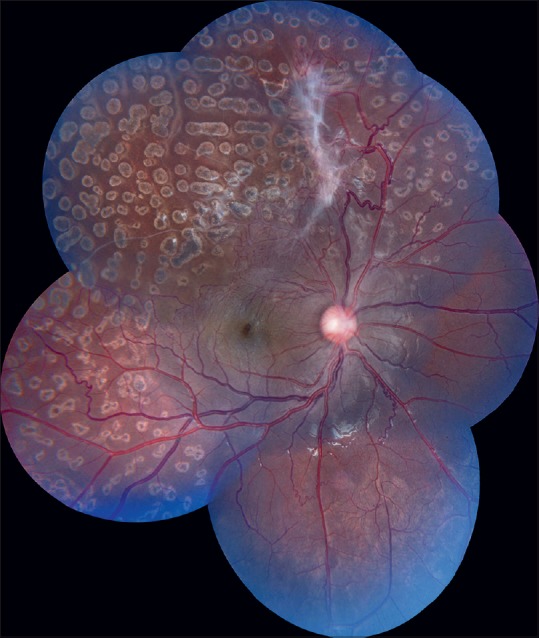
Fundus picture 4 months post laser shows regression of the retinal neovascularization with fibrous proliferation and laser scars
Discussion
We report this unique case of IP in a male with a normal male karyotype. We presumed his survival was because of somatic mosaicism. OCT suggests that the retinal vascular changes in IP may involve the inner retinal vasculature more than the choroidal vasculature causing more inner retinal layer abnormalities than the RPE and ellipsoid zone, which was also noted by Liu et al. and Basilius et al.[3,4] This is probably the first time that foveal hypoplasia was documented on OCTA in a case of IP.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Landy SJ, Donnai D. Incontinentiapigmenti (Bloch-Sulzberger syndrome) J Med Genet. 1993;30:53–9. doi: 10.1136/jmg.30.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minić S, Trpinac D, Obradović M. Incontinentiapigmenti diagnostic criteria update. Clin Genet. 2014;85:536–42. doi: 10.1111/cge.12223. [DOI] [PubMed] [Google Scholar]
- 3.Liu TYA, Han IC, Goldberg MF, Linz MO, Chen CJ, Scott AW. Multimodal retinal imaging in incontinentiapigmentiincluding optical coherence tomography angiography findings from an older cohort with mild phenotype. JAMA Ophthalmol. 2018;136:467–72. doi: 10.1001/jamaophthalmol.2018.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basilius J, Young MP, Michaelis TC, Hobbs R, Jenkins G, Hartnett ME. Structural abnormalities of the inner macula in incontinentiapigmenti. JAMA Ophthalmol. 2015;133:1067–72. doi: 10.1001/jamaophthalmol.2015.1700. [DOI] [PMC free article] [PubMed] [Google Scholar]


