Abstract
Purpose:
The gold standard for evaluating Retinopathy of prematurity (ROP), a potentially blinding disease in preterm babies, is by indirect ophthalmoscopy which is quite subjective. Digital imaging with RetCam, an advanced wide field imaging system is more precise but it is not easily available or affordable. Smartphones are being explored as an alternate cost effective and accessible imaging tool. This is possible because of the good illumination and the built-in high resolution cameras available in modern smartphones. The aim of this study is to illustrate the utility of MII RetCam assisted smartphone based fundus imaging (MSFI) in the documentation and monitoring of ROP.
Methods:
Single-centre, retrospective observational study of all the preterm babies subjected to MSFI as part of ROP screening from September 2017 to November 2018. iPhone 4S and + 20 Diopter lens attached to the MII RetCam device was used for fundus imaging at baseline and during follow up. The statistical analysis used for the same is the SPSS statistical software.
Results:
Good quality images of central and peripheral retina could be captured in 33 out of 42 babies (78.57%) with ROP. Serial imaging done in 24 babies with ROP helped in precise monitoring of the disease and planning management. Incidentally detected non-ROP findings were also documented. Unique design of the device enabled imaging by a single examiner. Image database created was useful for academic and counselling purposes. Smaller field images which can cause difficulty in distinguishing the zones is a limitation.
Conclusion:
MSFI is a potential alternate imaging tool enabling objective documentation and monitoring of ROP in low resource settings.
Keywords: Fundus imaging, MII RetCam, retinopathy of prematurity, smartphone
The gold standard for evaluating Retinopathy of prematurity (ROP)—a potentially blinding disease in preterm babies—is by indirect ophthalmoscopy which is quite subjective.[1] Digital documentation with RetCam (Natus USA, formerly Clarity, MSI, USA) is more accurate but expensive.[2,3,4] Smartphones equipped with good illumination and high-resolution cameras have emerged as an alternate, affordable and reliable imaging tool.[5,6,7] Smartphone-based fundus imaging utilizing an innovative device “Make In India (MII) RetCam” has been found to achieve good quality imaging of central and peripheral retina.[8,9] We aim to demonstrate the utility of MII RetCam assisted smartphone-based fundus imaging (MSFI) in the documentation and monitoring of a peripheral retinal pathology like ROP, in resource limited settings.
Methods
This is a single-centre, retrospective observational study of the utility of MSFI done as part of the ROP screening from September 2017 to November 2018. Babies were referred for ocular evaluation by Neonatologist as per the screening guidelines for ROP.[10] All examinations were done by a single ophthalmologist trained in ROP (TL). Examination was done either in the ophthalmology department or in the neonatal intensive care unit (NICU). All babies remained awake during the procedure and a trained nurse assisted to hold the baby and keep the head steady. Mydriasis was achieved with Tropicamide (0.5%) with Phenylephrine (2.5%) eye drops and binocular indirect ophthalmoscopy (BIO) with scleral depression was done for complete evaluation of retinal periphery. Lid speculum placed under topical anesthesia with 0.5% Proparacaine eye drops ensured good separation of the eyelids and cornea was kept moist by applying normal saline.
This was followed by MSFI and video recording of retinal features. Smartphone used was iPhone 4S (Apple Inc., Cupertino, CA, USA) with its original settings. It was done as described below:
iPhone and Volk + 20 Dioptre (D) lens were inserted into the respective slots at either ends of the MII RetCam device. This enabled holding both with a single hand at appropriate distance in the same axis. The other hand was therefore free to manoeuvre the eyes and to perform scleral indentation
The device was held in front of the patient's eye by holding the handle near the smartphone end between the palm and fingers in such a way that the screen of the smartphone is facing up and thumb of the same hand was used to turn on/off the video mode of the camera during recording [Fig. 1a]
The constant illumination in the video mode was switched on, and once the red glow was seen through the dilated pupil, it was slowly withdrawn till a clear image of the fundus was visualized on the smartphone screen
The video mode of the camera was then switched on with the thumb and then recorded until all the desired areas were imaged. The video mode was then similarly switched off
To get a good quality image, it is important to ensure that the image fills the entire 20D lens without any light reflection. This was achieved by slight back and forth movement or tilting of the device and stabilizing the baby's eyes with infant depressor. Good mydriasis also helped to reduce reflections
The smartphone camera lens and the 20 D lens should be cleaned well before the procedure to remove any dirt which can cause artefacts
The posterior pole was examined first followed by the entire peripheral retina in a sequential manner which was facilitated with the eye ball manoeuvred towards the desired direction using the scleral depressor. Tilting the baby's head slightly to the same side made it easier to visualize the extreme periphery
After completion of recording, the chosen good quality stills were extracted from the video sequence using the screenshot option in the smartphone (click and hold the top power button and the round menu button at the bottom simultaneously). The right hand of the examiner holding the device is not supported on the baby's face and can shake in between. Hence, capturing videos rather than still images were preferred
The snapshot images and video recordings were then transferred to a laptop which had a larger storage space. They were then archived in a separate folder along with the demographic data for each baby
Babies with immature retina and ROP were followed up as per the guidelines and the same protocol was repeated at each visit.
Figure 1.
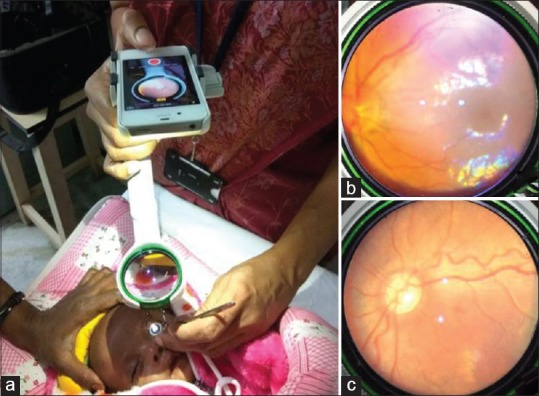
Showing (a) the technique of MII RetCam assisted fundus imaging. Fundus image is seen on the screen of the smartphone (b) Image of normal posterior pole (c) Image with plus disease
Study was approved by institutional human ethics committee and written informed consent was obtained from the parents of babies.
Results
132 babies with gestational age (GA) ranging from 27 to 39 weeks and birth weight (BW) ranging from 800 to 3400 grams were screened for ROP during the study period. Babies having GA more than 35 weeks and BW more than 1700 grams were included for screening at neonatologist's discretion. Fundus examination revealed mature retina in 52 babies. There were 36 babies with immature retina in zone 3, 19 babies with immature retina in zone 2, and 25 babies with ROP. They were all monitored according to the guidelines. During follow up, 17 more babies developed ROP resulting in a total of 42 babies (31.81%) with ROP. Types 1 ROP developed in 5 babies (3.79%) and were treated with laser.
MSFI captured good quality retinal images in 33 out of 42 babies with ROP (78.57%). In the remaining 9 babies image clarity was not good enough to assess the retinal changes. Serial imaging was done for 24 out of 33 babies with ROP, ranging from 2 to 11 imaging sessions. Imaging was also done for 4 babies with immature retina and 6 babies with mature retina which included 3 babies with incidental retinal findings. A total of 129 imaging sessions were done for 43 babies (mean 3). Posterior pole images helped to assess the disc, macula and plus disease [Fig. 1b and c]. None of the babies had Zone 1 disease. Peripheral images especially of the nasal and temporal periphery helped in accurate classification of ROP [Fig. 2]. Scleral depression made it possible to image the extreme peripheral retina till the ora. [Fig. 2g and h]. Serial recordings during follow up helped to objectively monitor the disease and to study the changes associated with progression or regression of the disease [Figs. 3 and 4]. In eyes which were lasered, it was helpful to document the changes pre and post treatment [Fig. 3]. Imaging details of all the babies with ROP and their disease pattern at the time of initial and final diagnosis are shown in the Table 1. Photo documentation was comparable to clinical evaluation with BIO except in babies with stage 1 disease in zone 3. Other posterior segment findings detected in 3 babies during evaluation could also be documented which were bilateral preretinal haemorrhage, intraretinal hemorrhage, and cystoid edema at fovea, respectively. Imaging required an additional time of approximately 5 minutes and none of the babies had any systemic issues during the procedure.
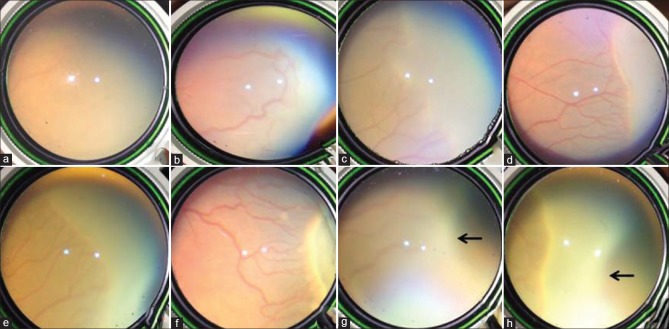
Figure 2.
Showing (a) Immature retina (b) Vascular loops (c) Stage 1 ROP (d, e) Stage 2 ROP in the temporal and nasal periphery (f) Stage 3 ROP with plus disease and “ popcorn” lesions (g and h) extreme periphery till ora (black arrow) in an eye (g) with mature retina and (h) with Stage 2 ROP
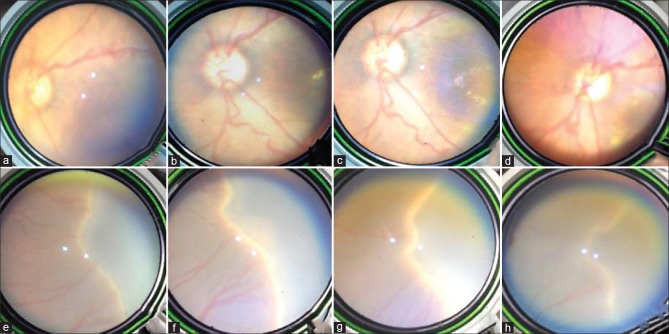
Figure 3.
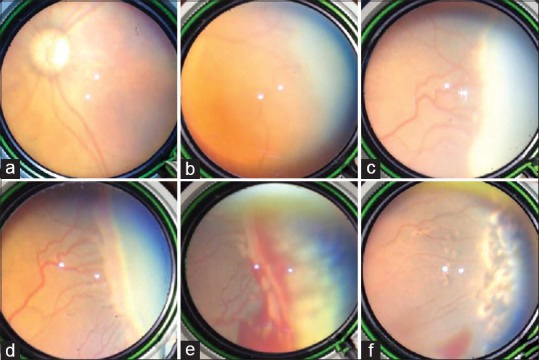
Serial imaging of a baby lasered for Type 1 ROP showing (a) posterior pole (b-d) progression of ROP from Stage 1 to 3 with plus disease (e) Immediate post laser with hemorrhage over ridge (f) 1 month post laser with decrease in plus disease and haemorrhage
Figure 4.
Serial imaging of the central (a-d) and peripheral retina (e-h) showing delayed natural regression. Stage 2 ROP noted at 36 weeks post conceptual age, worsened to Stage 3 with plus disease by 38 weeks, early regression by 40 weeks and further regression by 49 weeks
Table 1.
The imaging data of babies with ROP
| Zone/Stage of ROP | No of babies evaluated with BIO at initial diagnosis (n=42) | No of babies evaluated by MSFI at initial diagnosis (n=33) | No of babies evaluated with BIO at final diagnosis (n=42) | No of babies evaluated by MSFI at final diagnosis (n=33) |
|---|---|---|---|---|
| Zone 2 Stage 1 | 5 | 5 | 0 | 0 |
| Zone 2 Stage 2 | 5 | 4 | 1 | 0 |
| Zone 2 Stage 3 | 1 | 1 | 3 | 3 |
| Zone 3 Stage 1 | 20 | 13 | 19 | 12 |
| Zone 3 Stage 2 | 11 | 10 | 17 | 16 |
| Zone 3 Stage 3 | 0 | 0 | 2 | 2 |
ROP: Retinopathy of prematurity; BIO: Binocular indirect ophthalmoscopy; n: Number; MSFI: MII RetCam assisted smartphone based fundus imaging
Discussion
Modern smartphones with its constant, coaxial and powerful light source, coupled with 20D lens, creates a BIO like optical system enabling visualization of the fundus and the built-in automatic focus camera enables imaging of the fundus. The utility of smartphone imaging in ROP was first reported by Lin et al., who recorded fundus images of 6 infants with ROP using the original settings of the camera in the smartphone.[7] Biju Raju et al. and Oluleye TS et al., have documented ROP by smartphone based imaging and have found it to be effective.[11,12] Oluleye et al. used the app Filmic Pro to capture the images and app Aviary to edit the images. In all these techniques, the examiner holds the mobile phone in one hand and 20D lens in the other hand, and so an assistant is required for eye ball manipulation. The technique is thus more challenging to visualize the periphery, which is crucial in ROP. Also, all reports are based on single imaging session on a smaller number of babies.
In our study, MSFI was successful in objectively documenting ROP in 78.57% of patients. Though this is slightly less than that reported with the professional wide field imaging systems,[3] it has several practical advantages. The device is more affordable[8] compared to the RetCam, and a smartphone and 20D lens are available with any ophthalmologist. The technique can be learned with minimal practice within a week's time if one is well-versed with BIO and smartphone photography. As both imaging and globe manipulation is done by the same person, there is better control and coordination than the other smartphone-based models. The unique design of the device automatically ensured that smartphone and 20D lens were aligned in the same axis as the patient's eyes especially when eyeballs are rotated to the sides for peripheral examination. This ability to visualize the peripheral retina to the same extent as BIO is one of the distinct advantages of MSFI, making it superior to RetCam in evaluating the Zone 3 in premature babies. It has been found that, in comparison to BIO, RetCam had more difficulty in imaging peripheral retina till ora due to the restricted mobility of the equipment.[13]
Serial imaging helped in improved monitoring of the course of disease over time by comparing with baseline photographs and to plan appropriate management. It also helped in more precise evaluation of plus disease, which is often inaccurately assessed by the limited bedside examination with BIO. To the best of our knowledge, serial imaging of ROP by smartphone fundoscopy has not been previously documented. This simple, non-contact, portable and user-friendly innovation can be practiced in any setting, irrespective of the systemic status of the baby or the location. Another advantage is the option to share these digital images directly from the smartphone because of its connectivity, for second opinion, in difficult situations avoiding direct referral of babies. The only other report of fundus photo documentation using MII RetCam for ROP is by Behera et al.[9] They used it for adult and pediatric cases and found it particularly useful in pediatric cases due to its portability. Till date, there is no published data comparing the quality of images obtained by smartphone in ROP to that with RetCam images or clinical examination. However, in a recent meta-analysis, smartphone image quality was found to agree substantially with the gold standards of clinical or photographic exams for evaluating other posterior segment pathologies like diabetic retinopathy.[14] We could also document other incidental posterior segment pathologies like retinal hemorrhages and foveal cystic changes. Routine ocular digital imaging in preterm babies have been emphasized by other authors who serendipitously detected significant and even life threatening conditions during ROP screening enabling timely intervention for treatable conditions.[15]
We used the iPhone 4S as it has been proved to be safe in retinal imaging.[16] Moreover, the technical feasibility of an iPhone as an ocular imaging device was found to be comparable to that of RetCam in a study by Jalil et al., and the authors recommend iPhone imaging in situations where expensive and complicated imaging equipment is unavailable.[17] They opine that flash illumination and autofocus in iPhones is well designed for ophthalmic imaging without the need for additional apps or much manual adjustment. Several apps like MII RetCam App, HopeScope App and Ullman Indirect App are available with different functionalities like data storage, brightness control and even short video recording, but we preferred the original settings in the iPhone and so no additional app was tried. Other authors have reported satisfactory imaging with different smartphones like iPhone 5, HTC One, Blackberry Z-10, Samsung S3 and Note3.[7,11,12,18] Another recommendation is to use micropore tapes to reduce unwanted reflections.[7]
Similar to previous reports,[8] we found that real time display of the fundus features on the smartphone screen during video recording was superior to conventional theoretical teaching of the residents in the evaluation of ROP. It was especially useful to demonstrate the peripheral retinal changes in ROP to the residents who were not competent in performing BIO in neonates. It also avoided too many doctors from directly handling the preterm babies and thus reduced the duration of examination as well as the risk of infection. Incorporating MSFI as a part of ROP screening will help to create a large image library useful for presentations, publications and research activities. It can be used as an easily available and inexpensive tool to train eye care workers.[18] It was extremely helpful in parental counselling, convincing them regarding treatment when needed and ensuring better compliance with follow up. Thus, it is a real asset in the practice of evidence-based medicine and can be a valuable proof in medico-legal situations.[8]
Our study has certain limitations as well. One of the important drawbacks of this technique is the limited field of view (<45°) when using the 20D lens, unlike the RetCam which provides a wide 130° field. This can cause difficulty in distinguishing the zones from a single static image. Using higher plus power lenses like 40 or 60D lens can increase the field up to 90°.[14] A superior option would be to use montage software programs for automated construction of mosaic photographs from multiple individual images as has been reported by Patel et al.[19] In their study, ROP experts interpreted individual fundus photographs and mosaic photographs of wide-angle retinal images and found that mosaic photographs were more accurate in image based diagnosis of clinically significant ROP. This is because mosaic photographs not only provides high resolution wide field images but also allows a continuous view with improved visualization of the ridge and vascular changes. In a novel study by Kim TN et al., software intelligence and automation-assisted smartphone based retinal imaging produced high quality 100° photomontages from 5 overlapping images in under one minute fully on-phone revealing various retinal abnormalities.[20] It was validated against clinical examination in diabetic retinopathy screening and found to have a sensitivity of 93.3% and specificity of 56.8%. More studies are needed to know if such automation techniques can enhance smartphone based imaging in ROP. Another deficiency of our study is the lack of objective grading of the quality of images by masked observers and validating it against the gold standard of BIO. The technique was more challenging in eyes with poor mydriasis, hazy media and in older babies due to the more active movements by the baby and these factors accounted for the difficulty in obtaining good images in 9 of our babies with ROP. Better case selection and availability of smartphones/apps with option of small pupil imaging can help to overcome these difficulties.
Smartphones have been successfully used as a diagnostic interface in teleophthalmology for ROP wherein retinal images taken using RetCam Shuttle at remote locations are transmitted electronically and viewed on smartphone using viewer software by experts.[21,22] Though telemedicine has tremendously improved the screening and management of ROP, it involves a significant initial investment to implement the telemedicine system (RetCam costs USD 83,500/- whereas MII RetCam device costs USD 380/-).[4,23] The availability of easily accessible and good quality imaging using smartphone offers a low cost substitute for RetCam imaging, adding another dimension to telescreening for ROP.
Conclusion
MSFI is a potential alternate imaging tool enabling objective documentation and monitoring of ROP in low resource settings. Creation of an image data base is useful for academic and research purposes. Prospective, double blinded study with a larger sample size and with comparison to RetCam will help to assess the sensitivity and specificity of this imaging modality. Improvements in software and automation techniques have the potential to widen its utility as a teleROP screening tool in future.
Financial support and sponsorship
Nil.
Conflicts of interest
One of the co-authors (Dr Ashish Sharma) has financial/proprietary interest in MII RetCam.
Acknowledgement
Mr Anoop T., for his valuable help.
References
- 1.Trese MT. What is the real gold standard for ROP screening? Retina Phila Pa. 2008;28(3 Suppl):S1–2. doi: 10.1097/IAE.0b013e31816a5587. [DOI] [PubMed] [Google Scholar]
- 2.Chiang MF, Wang L, Busuioc M, Du YE, Chan P, Kane SA, et al. Telemedical retinopathy of prematurity diagnosis: Accuracy, reliability, and image quality. Arch Ophthalmol. 2007;125:1531–8. doi: 10.1001/archopht.125.11.1531. [DOI] [PubMed] [Google Scholar]
- 3.Chiang MF, Melia M, Buffenn AN, Lambert SR, Recchia FM, Simpson JL, et al. Detection of clinically significant retinopathy of prematurity using wide-angle digital retinal photography. Ophthalmology. 2012;119:1272–80. doi: 10.1016/j.ophtha.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chee R-I, Patel SN, Jonas KE, Gupta MP, Chiang MF, Chan RVP, et al. Current trends in telemedicine for retinopathy of prematurity. Vis Pan-Am Pan-Am J Ophthalmol. 2017;16:7–11. [Google Scholar]
- 5.Lord RK, Shah VA, Filippo ANS, Krishna R. Novel uses of smartphones in ophthalmology. Ophthalmology. 2010;117:1274–1274.e3. doi: 10.1016/j.ophtha.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Bastawrous A. Smartphone fundoscopy. Ophthalmology. 2012;119:432–433.e2. doi: 10.1016/j.ophtha.2011.11.014. author reply 433. [DOI] [PubMed] [Google Scholar]
- 7.Lin SJ, Yang CM, Yeh PT, Ho TC. Smartphone fundoscopy for retinopathy of prematurity. Taiwan J Ophthalmol. 2014;4:82–5. [Google Scholar]
- 8.Sharma A, Subramaniam SD, Ramachandran KI, Lakshmikanthan C, Krishna S, Sundaramoorthy SK. Smartphone-based fundus camera device (MII Ret Cam) and technique with ability to image peripheral retina. Eur J Ophthalmol. 2016;26:142–4. doi: 10.5301/ejo.5000663. [DOI] [PubMed] [Google Scholar]
- 9.Behera S, Pradhan A. MII Ret Cam: A boon towards retinal disease imaging and documentation. J Clin Exp Ophthalmol. 2017;8:1–3. [Google Scholar]
- 10.Jalali S, Anand R, Kumar H, Dogra MR, Azad R, Gopal L. Programme planning and screening strategy in retinopathy of prematurity. Indian J Ophthalmol. 2003;51:89–99. [PubMed] [Google Scholar]
- 11.Raju B, Raju NSD, Akkara JD, Pathengay A. Do it yourself smartphone fundus camera – DIYretCAM. Indian J Ophthalmol. 2016;64:663–7. doi: 10.4103/0301-4738.194325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oluleye TS, Rotimi-Samuel A, Adenekan A. Mobile phones for retinopathy of prematurity screening in Lagos, Nigeria, sub-Saharan Africa. Eur J Ophthalmol. 2016;26:92–4. doi: 10.5301/ejo.5000666. [DOI] [PubMed] [Google Scholar]
- 13.Shah PK, Narendran V, Saravanan VR, Raghuram A, Chattopadhyay A, Kashyap M. Screening for retinopathy of prematurity--A comparison between binocular indirect ophthalmoscopy and RetCam 120. Indian J Ophthalmol. 2006;54:35–8. doi: 10.4103/0301-4738.21612. [DOI] [PubMed] [Google Scholar]
- 14.Vilela MA, Valença FM, Barreto PK, Amaral CE, Pellanda LC. Agreement between retinal images obtained via smartphones and images obtained with retinal cameras or fundoscopic exams-systematic review and meta-analysis. Clin Ophthalmol Auckl NZ. 2018;12:2581–9. doi: 10.2147/OPTH.S182022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jayadev C, Vinekar A, Bauer N, Mangalesh S, Mahendradas P, Kemmanu V, et al. Look what else we found--Clinically significant abnormalities detected during routine ROP screening. Indian J Ophthalmol. 2015;63:373–7. doi: 10.4103/0301-4738.159859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim DY, Delori F, Mukai S. Smartphone photography safety. Ophthalmology. 2012;119:2200–1. doi: 10.1016/j.ophtha.2012.05.005. author reply 2201. [DOI] [PubMed] [Google Scholar]
- 17.Jalil M, Ferenczy SR, Shields CL. iPhone 4s and iPhone 5s imaging of the eye. Ocul Oncol Pathol. 2017;3:49–55. doi: 10.1159/000448721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ademola-Popoola DS, Olatunji VA. Retinal imaging with smartphone. Niger J Clin Pract. 2017;20:341–5. doi: 10.4103/1119-3077.201428. [DOI] [PubMed] [Google Scholar]
- 19.Patel SN, Klufas MA, Douglas CE, Jonas KE, Ostmo S, Berrocal A, et al. Influence of computer-generated mosaic photographs on retinopathy of prematurity diagnosis and management. JAMA Ophthalmol. 2016;134:1283–9. doi: 10.1001/jamaophthalmol.2016.3625. [DOI] [PubMed] [Google Scholar]
- 20.Kim TN, Myers F, Reber C, Loury PJ, Loumou P, Webster D, et al. A smartphone-based tool for rapid, portable, and automated wide-field retinal imaging. Transl Vis Sci Technol. 2018;7:21. doi: 10.1167/tvst.7.5.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, et al. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62:41–9. doi: 10.4103/0301-4738.126178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kulkarni S, Kakade N, Khandekar R, Narwadkar P, Deshpande M. Use of the smart phone as a diagnostic interface for detecting severe retinopathy of prematurity: A pilot study. J Ophthalmic Vis Res. 2017;12:447–8. doi: 10.4103/jovr.jovr_207_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma A. Emerging simplified retinal imaging. Dev Ophthalmol. 2017;60:56–62. doi: 10.1159/000459690. [DOI] [PubMed] [Google Scholar]