Abstract
Background:
Intestinal failure is a chronic condition related to loss of bowel length and/or function, resulting in dependence on central venous catheters for fluids and nutrition. Catheter use can be associated with significant complications, including catheter-related bloodstream infections (CRBSIs), which can lead to loss of vascular access, advancing intestinal failure associated–liver disease and death. Our objective was to evaluate the effectiveness and safety of ethanol locks as compared with standard heparin locks in pediatric intestinal failure.
Methods:
Databases, including MEDLINE and EMBASE, were searched until March 2017. Titles and abstracts were reviewed independently and relevant articles reassessed by full-text review. The main outcome was the rate of CRBSIs, while secondary outcomes were catheter replacement and repair.
Results:
Nine observational studies were included. The mean difference in rate of CRBSIs was 6.27 per 1000 catheter days (95% CI, 4.89–7.66) favoring ethanol locks, with a 63% overall reduction in infection rate. The mean difference in catheter replacement rate (per 1000 catheter days) was 4.56 (95% Cl, 2.68–6.43) favoring ethanol locks. The overall effect on catheter repair rate (per 1000 catheter days) was –1.67 (95% CI, –2.30 to –1.05), indicating lower repair rate with heparin locks.
Conclusion:
Sufficient evidence was noted showing that ethanol locks reduced CRBSIs and catheter replacements. Our findings raise questions about the effect of the ethanol lock on catheter integrity based on the noted increase in repair rate. This requires further prospective evaluation and may support selective application of ethanol locks to patients with documented CRBSIs. (JPEN J Parenter Enteral Nutr. 2018;42:690–701)
Keywords: short bowel syndrome, rehabilitation, research and diseases, outcomes research/quality, nutrition support practice, gastrointestinal access
Introduction
Intestinal failure is a chronic condition associated with significant morbidity, mortality, and high healthcare costs.1 The condition is related to loss of bowel length and/or function, leading to insufficient intestinal absorption and inability to maintain proper hydration, electrolyte profile, and growth. In the pediatric population, short bowel syndrome is the most common etiology of intestinal failure, often secondary to necrotizing enterocolitis, volvulus, gastroschisis, or intestinal atresias.2,3 Patients with intestinal failure rely on central venous catheters (CVCs) to provide fluids and parenteral nutrition (PN). Use of CVCs is associated with complications, including catheter-related bloodstream infections (CRBSIs), which can lead to loss of vascular access, advancing intestinal failure-associated liver disease, sepsis, and death.4,5 Preventing CRBSIs is therefore extremely critical in this patient population.
Previous studies in the literature have shown that ethanol lock (EL) therapy for CVCs in this patient population can be an effective modality for reducing CRBSIs.6–9 Those studies varied in EL protocol used and had small patient sample sizes. Complications possibly related to EL therapy were reported,10–12 including line repair and thrombosis, but the data on the adverse events associated with EL therapy remain very limited.
Our main objective was to systematically search and analyze the available literature regarding the effect of EL therapy as compared with the use of standard heparin lock (HL) therapy on the rate of CRBSIs in pediatric patients with intestinal failure.
Materials and Methods
This systematic review was performed and is reported according to the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).13 The process includes following an established standardized protocol for systematic reviews. The investigators included pediatric gastroenterologists (R.R., M.A.H., D.E., C.R.C.) experienced in managing pediatric intestinal failure patients through their involvement in multidisciplinary intestinal re-habilitation programs, an experienced biostatistician (L.F.), and a professional health sciences librarian (E.K.) trained in conducting systematic reviews.
Study Selection Criteria
Methods for study screening and inclusion were specified in advance and included an assessment of the population, intervention, comparison, and outcome. The population of interest was pediatric patients diagnosed with intestinal failure from any underlying condition with a CVC for PN. The intervention of interest was use of HL and EL therapy comparing the rate of CRBSIs and catheter replacement and repair between the 2 interventions. No language restrictions were imposed. In vitro animal studies and noncomparative human studies were excluded.
A protocol to address discrepancies in study inclusion and data collection was established through discussion and consensus as a first step, then by consultation with the senior study investigator if consensus was not reached. Identified studies were initially independently screened by 2 study investigators by examining the title and abstract to decide on relevance to the main study objectives and according to the prespecified inclusion and exclusion criteria. After removing irrelevant studies, the investigators screened the full study texts to assess further eligibility for inclusion. References of the selected studies were manually searched for additional missed references.
Search Strategy and Data Sources
Comprehensive searches were conducted with several databases. The search strategy was designed and conducted by a librarian with input from the other investigators. The strategy included a systematic literature search of electronic databases indexing biomedical literature. A search strategy was developed for MEDLINE with headings and keywords for terms, including “catheters,” “catheterization,” “catheter-related infections,” “ethanol,” and “alcohol.” Search strategies did not contain limits for date or language. The full and detailed search strategy is described in the Appendix. The MEDLINE database was searched with the Ovid platform; the search strategy was adapted for EMBASE. PubMed MEDLINE was searched in March 2017 to identify any “ePub ahead of print” citations not indexed in Ovid. In addition to these databases, the Cochrane Library databases, ClinicalTrials.gov, and the Conference Proceedings Citation Index within Web of Science were searched. All searches were run last in March 2017 without a set limit on year of publication before that date.
Data Abstraction
Following study identification, study investigators extracted data with a standardized electronic form that included study design, patient demographics, sample size, type of intervention, and outcomes and estimates of interest.
Grading Evidence
To provide a more comprehensive systematic review, we sought to grade the quality of the available evidence. Many checklists have been developed to provide frameworks for judging the methodological quality of published studies. We planned to use the GRADE guidelines14,15 to assess the methodological quality of randomized studies or to use a published checklist tool specific for nonrandomized studies.16
Primary and Secondary Outcomes
The primary outcome of this study was the comparison in the rate of CRBSIs between EL and HL therapy in pediatric patients with intestinal failure. Secondary outcomes were the comparisons in the rates of catheter replacement and catheter repair between the 2 interventions. Only articles clearly describing either our primary or secondary outcomes of interest were included in the meta-analysis.
Risk of Bias
Publication bias is thought to arise from the systematic underestimation or overestimation of the effect of interest due to the selective publication of studies with statistically significant results. This can be assessed by the use of plots of sample size against effect estimate, with plot asymmetry more likely to be noted in the presence of bias.17 In this meta-analysis, an Egger’s test for asymmetry of the funnel was used to assess for publication bias.
Statistical Analysis
An important preliminary step in the statistical analysis was to derive or otherwise calculate estimated variance of effect sizes from each study—that is, mean difference in CRBSI rate, mean percentage reduction in CRBSI rate, and mean difference in catheter replacement and catheter repair rates.
To calculate the standard error (SE) of the difference in mean rates for all studies, we first estimated the correlation coefficient ρ between EL and HL therapy periods, using reported data in the publications included. When the CRBSI rate was reported as median and interquartile range and the test was nonparametric (eg, Wilcoxon), we estimated the mean difference as the difference in medians. The treatment group SE was estimated by interquartile range/1.34898. The SE of the difference in mean was imputed with a correlation coefficient of 0.20. Sensitivity analysis of this assumption of correlation coefficient was performed. For percentage reduction in CRBSI rate, we used Taylor series approximation to get a variance estimate of the mean percentage reduction.
For catheter replacement rate per 1000 catheter days, we used Mouw’s8 individual patient data to derive a correlation coefficient between treatment groups. The observed correlation coefficient was –0.125. Alternatively, when available, as suggested by Follmann et al and Elbourne et al,18,19 we inverted the reported P values of paired comparison to deduce SE of the mean difference. When an upper bound of P value was given (eg, P < .001), we used that bound as a conservative estimate. To assess for heterogeneity among studies, a test statistic (Cochran’s Q) was computed and a P value obtained for each outcome measure of interest.
Meta-Analysis Method
We compared the effect of EL and HL therapy on CRBSI rate per 1000 catheter days, catheter replacement rate per 1000 catheter days, and catheter repair rate per 1000 catheter days. The effect sizes defined were similar to those used in the prior meta-analysis from 2012 by Oliveira et al20—namely, the mean difference in CRBSI rate, mean percentage reduction in CRBSI rate, and the mean difference in catheter replacement rate between EL and HL therapy. The individual study rates were calculated from raw data that we had access to or from published results. The SEs of the effect sizes were reported in publications, calculated directly, or imputed with the methods described here. With each study’s estimated effect and SE, we calculated the weighted average of study effects and computed the Q statistic21 with inverse-variance weights. A test of homogeneity was first performed by comparing Q to a χ2 distribution with proper degrees of freedom. If the homogeneity test was rejected, a random effect model was applied to obtain the weighted average effect. Analyses were performed in R with the metafor package.22
Results
We identified 2216 potentially eligible records through search of databases and other sources as specified. The search included 316 duplicates that were excluded. A total of 14 studies satisfied the inclusion criteria and were selected for full-text review (Figure 1). Five studies were excluded for the following reasons: 1 was a prior systematic review and meta-analysis20; 1 was a prior systematic review of pediatric and adult patients with diverse medical conditions (without meta-analysis)23; 1 was to determine blood alcohol concentration and hepatic injury in infants receiving ELs11; 1 was a comparison between EL protocols (therapeutic only vs prophylactic and therapeutic)24; and 1 study was an unpublished trial identified through ClinicalTrials.gov (manuscript had not been completed or peer reviewed). The search resulted in 9 published observational studies that were included in the meta-analysis. No disagreement was noted regarding study inclusion among the independent authors who reviewed the identified records. Our findings were consistent with a systematic review20 published on this topic in 2012, the searches of which spanned 1948–2010 for MEDLINE and 1980–2010 for EMBASE and identified eligible literature starting in 2008. Our current systematic review expanded the meta-analysis to include an additional 5 studies from the last study20 in year 2012 relevant to this specific patient population.
Figure 1.
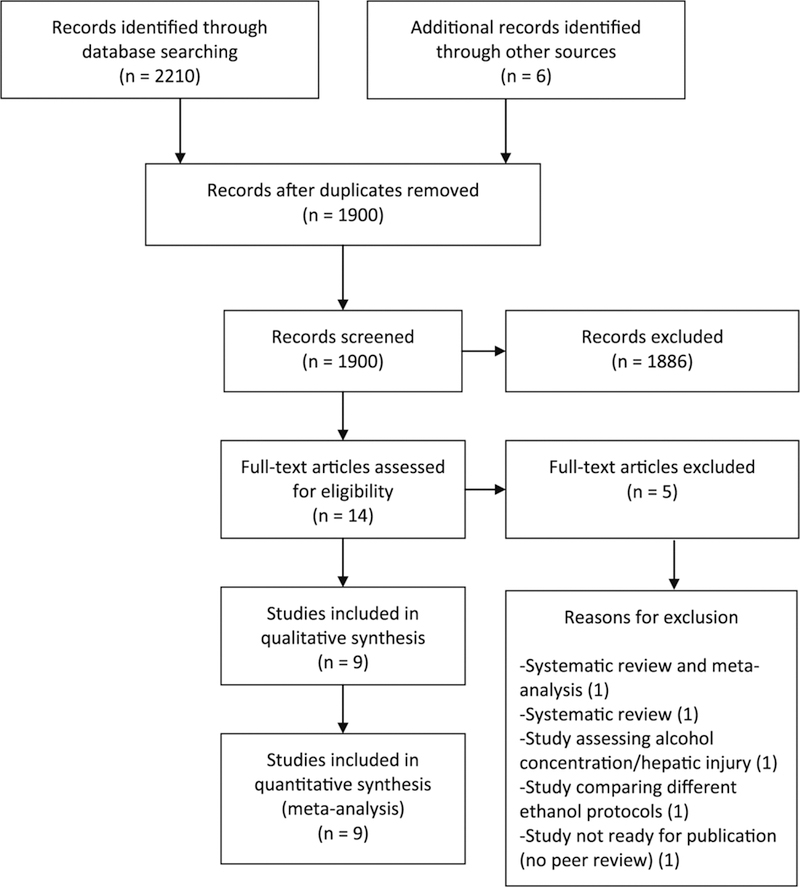
Selection process for systematic review. The systematic review resulted in 14 potentially eligible published studies. After full-text assessment, 9 studies were included in the analysis.
Study Characteristics
All studies included were retrospective observational cohort studies. These are summarized in Table 1. Based on our search strategy, the first study was published in 2008,20 while the most recent one was published in 2017. All studies were published in English and conducted in North America (8 in United States, 1 in Canada) for a total of 147 patients with intestinal failure using EL and HL therapy exclusively in silicone catheters. All studies except 1 required a previously documented CRBSI prior to starting EL therapy. All studies utilized EL therapy daily except for one that reported EL use for 3 days per week6 and another that reported once-weekly EL use.25 The minimal dwell time was 2 hours. Most studies reported aspirating the ethanol from the CVC at the end of the dwell, although 2 studies reported flushing the ethanol through the catheter before starting the PN infusion.8,26
Table 1.
Characteristics of Included Studies (All Observational).
| Source (Year) | Sample Size | Inclusion Criteria | Weight Range, kg | Age Range, y | Ethanol Lock Protocol | Outcomes |
|---|---|---|---|---|---|---|
| Mouw et al8 (2008) | 5 | Intestinal failure. Silicone CVC. | Not included | 0.3–2.3 | 70% ethanol, volume determined individually (max, 2 mL), applied daily, minimal dwell time of 4 h, flushed through catheter before beginning PN. | Reduction in CRBSI rate. |
| Jones et al6 (2010) | 23 | Intestinal failure. Silicone CVC. ≥ 1 documented CRBSI in the previous year. | ≥5 | 0.9–2.6 | 70% ethanol, volume determined individually, applied 3 d/wk, minimal dwell time of 4 h, aspirated at end of dwell | Significant reduction in CRBSI rate. |
| Cober et al7 (2011) | 15 | Intestinal failure. Silicone CVC. ≥2 CVCs replaced because of infection in the previous 18 mo. ≥2 documented difficult-to-clear CRB Sis or limited remaining access | ≥5(5.9–52.6) | 0.5–21.4 | 70%) ethanol, volume determined individually, applied daily, minimal dwell time of 2 h, aspirated at end of dwell | Significant reduction in CRBSI rate. |
| Wales et al26 (2011) | 10 | Intestinal failure. Silicone CVC. ≥ 1 documented CRBSI. | >5, single lumen; >9, double lumen | 2.6–10.8 | 70%o ethanol, volume determined individually (max, 3 mL), applied daily, minimal dwell time of 4 h, flushed through catheter before beginning PN | Significant reduction in CRBSI rate. Significant decrease in CVC replacements. |
| Pieroni et al25 (2013) | 14 | Intestinal failure. Silicone CVC. ≥2 documented CRBSI. | 5.7–47.3 | 0.4–19.1 | 70%o ethanol, volume of 1 mL for patient weight <30 kg and 2 mL for patient weight >30 kg, applied weekly, dwell time of 2 h, aspirated at end of dwell | Significant reduction in CRBSI rate. Significant decrease in CVC replacements. |
| Abu-El-Haija et al12 (2014) | 7 | Intestinal failure. Silicone CVC. ≥ 1 documented CRBSI. | Not included | <18 | 70%o ethanol, volume determined individually, applied daily, minimal dwell time of 4 h, aspirated at end of dwell | Significant reduction in CRBSI rate. |
| Ardura et al9 (2015) | 14 | Intestinal failure. Silicone CVC. ≥2 documented CRBSI in the previous year. | ≥5 | 0.3–18 | 70%o ethanol, volume determined individually (max, 3 mL), applied daily, minimal dwell time of 2 h, aspirated at end of dwell | Significant reduction in CRBSI rate. |
| Mezoff et al27 (2016) | 30 | Intestinal failure. Silicone CVC. >3 CRB Sis in the previous year, >2 gram-negative CRB Sis in the previous year, 1 fungal CRBSI, continuation of a referral hospital ethanol lock, or removal of 2 CVCs due to infections. | Not included | 1–20 | 70%o ethanol, volume determined individually, applied daily, minimal dwell time of 2 h, aspirated at end of dwell | Significant reduction in CRBSI rate. Significant reduction in line perforation or breakage rates. |
| Mokha et al28 (2017) | 29 | Intestinal failure. Silicone CVC. | Not included | Not included | 70%o ethanol, volume determined individually (max, 3 mL), applied daily, minimal dwell time of 2 h, aspirated at end of dwell | Nonsignificant reduction in CVC replacements due to infection. Significant increase in CVC replacements due to mechanical problems. |
CRBSI, catheter-related bloodstream infection; CVC, central venous catheter; PN, parenteral nutrition.
Methodological Quality
The studies included in the meta-analysis were all retrospective studies; therefore, the GRADE guidelines were not ideal to assess methodological quality. As mentioned in the Materials and Methods section, we utilized a published checklist tool that was better suited to evaluate nonrandomized studies. None of the studies included allocation concealment or blinding of participants and the managing medical team personnel. The number of participants per study was relatively small, ranging from 5 to 30 patients per study. All studies reported on the change in CRBSI rate with the use of EL vs HL therapy in patients with intestinal failure, with an objective outcome based on documented CRBSI.
Primary Outcome
All 9 studies compared CRBSI rates between patients receiving EL and HL therapy (Table 2). The fixed effect pooled estimate of mean difference in rate was 6.27 CRBSIs per 1000 catheter days (95% CI, 4.89–7.66) between the 2 interventions, favoring EL therapy (Figure 2). The reduction in the risk of CRBSI with EL use ranged between 30.7% by Mezoff et al27 and 91.2% by Wales et al26 for an overall reduction in CRBSI rate by 63% (95% CI, 29.2%–96.7%; Figure 3). One study was excluded from the percentage reduction meta-analysis, as the individual group standard deviations for the rates of CRBSIs were not provided and percentage reduction SE could not be calculated.9 Test for heterogeneity among the 9 included studies revealed a Q of 9.99, with 8 degrees of freedom (P = .27). The number needed to treat (NNT), defined as the number of EL treatment days needed to observe a reduction of 1 CRBSI, ranged from 108 to 588, with an overall NNT at 159 catheter days. The Egger’s test for asymmetry of the funnel plot of the mean difference in CRBSI rate had a P value of .299, suggesting that no publication bias was detected.
Table 2.
CRBSI and Catheter Replacement Rates.
| Source (Year) | Sample Size | CRBSI per 1000 d |
Catheter Replacement Rate |
Reduction in CRBSI Rate |
Number Needed to Treat |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference (HL – EL) |
Estimated SE | Mean difference (HL – EL) |
Estimated SE | Mean Percentage |
Estimated SE | CRBSI Rate | Catheter Replacement |
||
| Mouw et al8 (2008) | 5 | 7.76 | 3.62 | 8.03 | 4.9 | 87.5 | 38.4 | 129 | 125 |
| Jones et al6 (2010) | 23 | 7.8 | 1.94 | 8.2 | 1.39 | 78.8 | 59.2 | 128 | 122 |
| Coberet al7 (2011) | 15 | 6.7 | 1.62 | — | — | 83.8 | 52.5 | 149 | — |
| Wales et al26 (2011) | 10 | 9.3 | 2.52 | 5.3 | 2.18 | 91.2 | 57.4 | 108 | 189 |
| Pieroni et al25 (20 1 3) | 14 | 7.1 | 1.68 | 3.3 | 1.53 | 72.4 | 91 | 141 | 303 |
| Abu-El-Haija et al12 (2014) | 7 | 8.9 | 4.86 | 0 | 3.93 | 86.4 | 114 | 112 | — |
| Ardura et al9 (2015) | 14 | 6.37 | 1.83 | 3 | 0.711 | 90.9 | — | 157 | 333 |
| Mezoff et al27 (20 1 6) | 30 | 1.70 | 1.71 | — | — | 30.7 | 29.2 | 588 | — |
| Mokha et al28 (2017) | 13 | 5.97 | 3.44 | 4.38 | 1.47 | 56.5 | 51.3 | 168 | 228 |
CRBSI, catheter-related bloodstream infection; EL, ethanol lock; HL, heparin lock.
Figure 2.
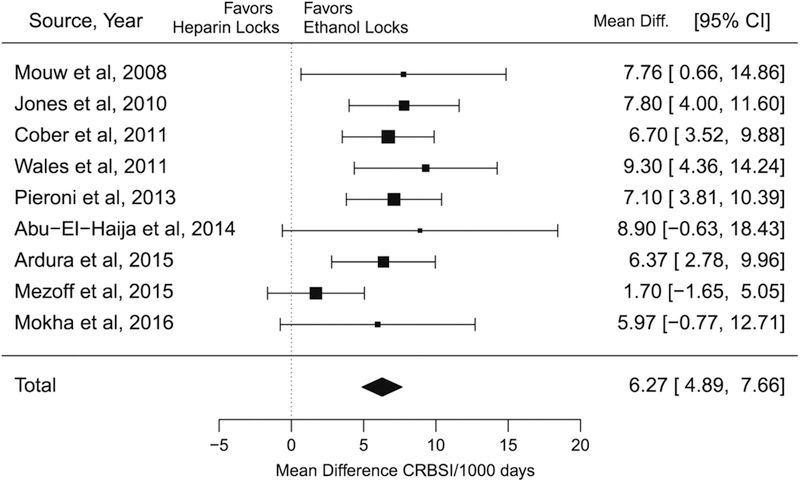
Forest plot graphing pooled mean difference of catheter-related bloodstream infection (CRBSI) rate between ethanol lock and heparin lock therapy. Each study is represented by 1 horizontal line and box, with box location and size corresponding to the point estimate and weight of each study. The diamond represents the overall effect estimate for all 9 included studies, with the width of the diamond representing the 95% CI. Diff., Difference.
Figure 3.
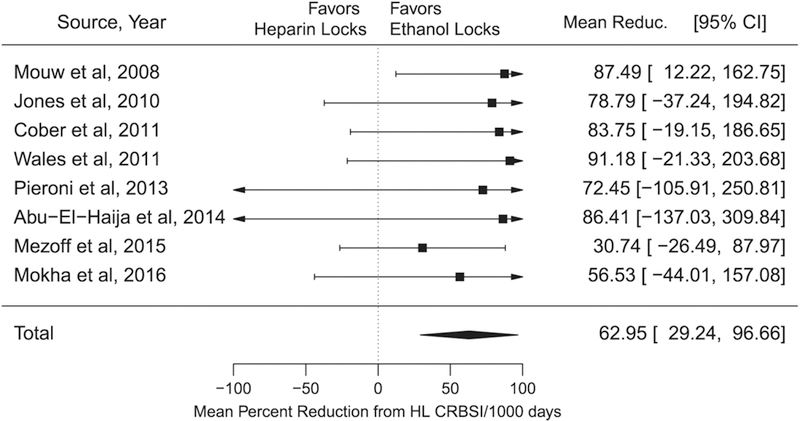
Forest plot graphing the reduction in catheter-related bloodstream infections (CRBSIs) with use of ethanol lock vs heparin lock (HL) therapy. Each study is represented by 1 horizontal line and box, with box location and size corresponding to the point estimate and weight of each study. The diamond represents the overall effect estimate for the included studies, with the width of the diamond representing the 95% CI. Reduc., Reduction.
Secondary Outcomes
Catheter replacement.
Seven studies provided data on changes in catheter replacement rates and were included in the analysis. The estimated mean difference in the catheter replacement rate (number of replacements per 1000 catheter days) in a random effect model was 4.56 (95% Cl, 2.68–6.43) between the 2 interventions, favoring EL therapy (Figure 4). Test for heterogeneity showed a Q value of 13.43, with 6 degrees of freedom (P = .037), suggesting significant heterogeneity across the 7 studies included. The NNT ranged from 122 to 333, with an overall NNT of 219 catheter days. The Egger’s test for asymmetry of the funnel plot for the mean difference in the catheter replacement rate had a P value of .89, which suggests that no publication bias was identified. It was not possible to further assess the impact of either lock therapy on the specific reasons for catheter replacement. Most studies included multiple reasons (catheter malfunction, occlusion, or infection) for replacement when reporting catheter replacement rates before and after introduction of EL therapy.6,9,26 Very few studies provided details on line replacement reasons, with results ranging from no statistical difference in replacement rate based on reason12 to significant reduction in line replacement due to infections, with a significant increase in line replacement due to mechanical events with EL therapy.28
Figure 4.
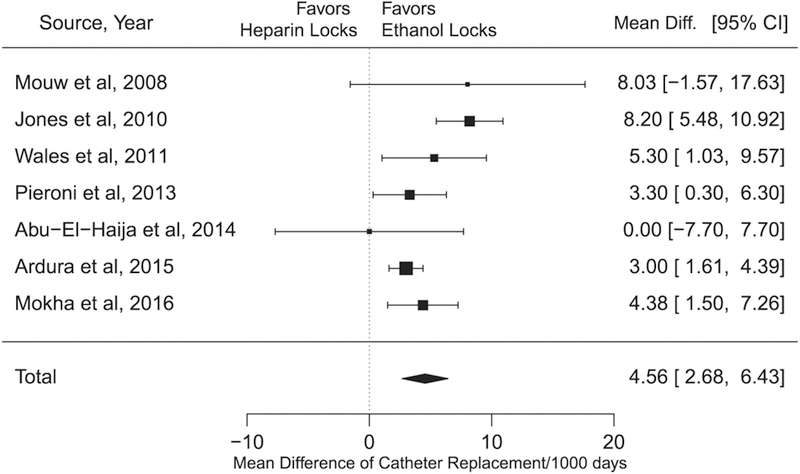
Forest plot graphing the pooled mean difference of catheter replacement rates between ethanol and heparin locks. Each study is represented by 1 horizontal line and box, with box location and size corresponding to the point estimate and weight of each study. The diamond represents the overall effect estimate for the included studies, with the width of the diamond representing the 95% CI. Diff., Difference.
Catheter repair.
Only 3 studies included data on catheter repair rates.7,12,28 The estimated overall effect on catheter repair rate (number of repairs per 1000 catheter days) in a fixed effect model was –1.67 (95% CI, –2.30 to –1.05), indicating a significantly lower repair rate in HL vs EL therapy (Figure 5). The study by Mokha et al28 was highly influential due to its low reported variability. If this study was not included, this finding would not be statistically significant with an overall effect of –4.42 (95% CI, –9.15 to 0.31). The test for heterogeneity showed a Q value of 1.68, with 2 degrees of freedom (P = .43), suggesting that there was no significant heterogeneity among the included studies, although we realize that this test included a small number of studies. It was not possible to determine if catheter breaks were related to catheter age, as only 1 study included a subanalysis based on catheter age, which showed a longer duration for HL therapy (vs EL) before a repair was needed.12
Figure 5.
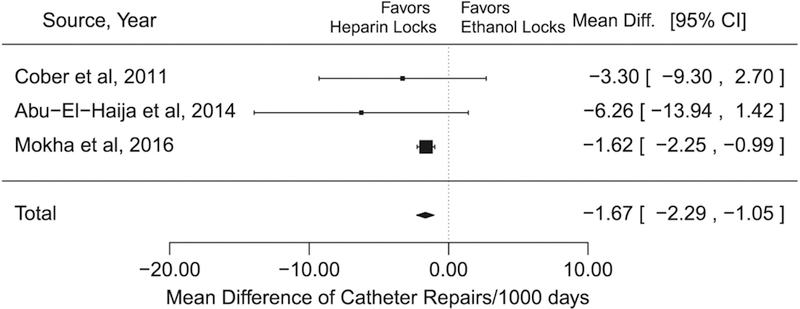
Forest plot graphing the pooled mean difference of catheter repair rates between ethanol and heparin locks. Each study is represented by 1 horizontal line and box, with box location and size corresponding to the point estimate and weight of each study. The diamond represents the overall effect estimate for the included studies, with the width of the diamond representing the 95% CI. Diff., Difference.
Discussion
Significant progress has been made in the management of pediatric patients with intestinal failure, including the introduction of multidisciplinary intestinal rehabilitation programs.29,30 This has resulted in improved patient out-comes likely related to several factors, such as changes in use of lipid emulsions, surgical interventions, and initiation of standardized care bundles for CVCs. Recurrent CRBSIs are associated with extended hospital days and increased cost of care, as well as major contributors to patient morbidity and mortality.20,31,32 A variety of organisms contribute to CRBSIs in this patient population, making targeted antimicrobial therapy challenging.33 Ethanol has been an attractive option to address CRBSIs, as it is inexpensive, has wide antimicrobial properties with no known resistance, and is capable of penetrating biofilms.20,34,35 Several observational studies published supportive evidence for using EL therapy, but few studies reported mechanical line problems and thrombosis following this approach.10,12,28
No published randomized trials were found in this systematic review of studies on the effect of EL therapy on rate of CRBSI in pediatric patients with intestinal failure. All included studies were single-sequence crossover, with all patients undergoing a period of HL therapy, followed by EL therapy. This design confounds time effect with treatment effect, making it difficult to completely delineate the general reduction of infection rate over time from EL therapy. The population was heterogeneous. As mentioned, all included studies had pediatric patients with intestinal failure, but there was variability in the number of prior infections required for inclusion. All studies utilized 70% ethanol, but somewhat heterogeneous protocols were noted, including minimal and maximum dwell time and frequency. Although most studies included in the meta-analysis utilized EL therapy daily, some reported less frequent administration (once weekly or 3 days per week), and these studies showed significant reduction in CRBSI rate.6,25 Our search did not reveal published literature on use of lower EL concentrations (<70%) in this patient population. In some studies, ethanol use was also restricted when patients were receiving metronidazole because of concern for a disulfiram-like reaction, while other studies mentioned no restriction with concurrent use. Only 1 study failed to show a significant reduction in the rate of CRBSIs with EL therapy.28 This study may have included a broader population of patients, as it did not require any prior documented CRBSIs before initiating EL therapy. Prospectively designed studies are therefore needed to better evaluate these protocols and provide opportunities to identify the most cost-effective practices, including ethanol concentration, dwell time, and frequency of administration.
The effect of EL therapy on line integrity and the association of EL with line repair rates were evaluated in 3 studies, with 1 study28 noted to be highly influential, having low reported variability as compared with the 2 other studies (Figure 4). It is possible that this association with higher repair rates may be underappreciated since the available studies were retrospective in nature and therefore dependent on available documentation. Potential mechanisms for ethanol leading to increased line repair rates include a direct negative effect on line integrity and intraluminal catheter occlusion through precipitation or thrombosis, leading to use of higher infusion/flushing pressure. Available in vitro studies have shown potential changes in the mechanical properties of CVCs following ethanol exposure, but these were more pronounced in polyurethane rather than silicone catheters. One study did not show significant alterations in multiple catheter types, with 70% EL exposure for up to 10 weeks, but noted increased catheter wall thickness only with polyurethane CVCs.36 Another study showed no increased damage to the inner luminal surface of silicone catheters following 15 days of immersion in 95% ethanol, as compared with controls and according to scanning electron microscopy.37 The authors of this study noted significant release of polydimethylsiloxanes with exposure to 95% ethanol solution, as compared with normal saline and 60% ethanol solution. Other studies focusing on polyurethane catheters showed that EL exposure resulted in lower force needed at time of catheter breakage.38 Catheter occlusion can be attributed to ethanol interaction with plasma protein or heparin. Solutions with ethanol have been shown to induce plasma protein precipitation.39 This is possible with EL therapy, as the catheter lock content can leak into the bloodstream from the distal catheter end, allowing blood to enter the catheter lumen with subsequent mixing of plasma proteins and the ethanol solution.40,41 Several studies have described precipitated material or clots with the use of EL therapy.10,28,42 It is also known that ethanol and heparin can exhibit precipitation in a dose-dependent fashion.43 Such precipitation can be minimized by removing heparin from all solutions, including the PN solution. The addition of an anticoagulant agent, such as citrate, may reduce intraluminal thrombus formation, but it is unclear if this would have a beneficial effect on plasma precipitation. For the time being, it would be reasonable to use the shortest EL dwell time at the lowest concentration necessary to eradicate the bacterial or fungal organisms in the biofilm to help reduce the risk of ethanol seepage and plasma precipitation. These considerations deserve further observation and would be best explored in prospective studies.
It is also important to mention alternative catheter lock options to decrease the rate of CBRSI, which include the prophylactic use of taurolidine lock solution. This is thought to have broad antimicrobial properties and can prevent biofilm formation.44 Few published retrospective studies of pediatric and adult patients receiving chronic PN showed reduced rates of CBRSI and/or occlusion with use of taurolidine catheter locks, either as an isolated intervention or as part of line care bundles.45–47 Studies directly comparing the efficacy of taurolidine and EL therapy are lacking.
Conclusion
The currently available literature provides sufficient evidence to support the use of EL therapy to reduce the risk for CRBSIs and reduce the need for catheter replacement in the high-risk population of pediatric patients with intestinal failure, particularly those with known prior CRBSIs. A small number of studies reported increased catheter repair rates after initiating EL therapy, suggesting a potential negative impact of EL on catheter integrity. Prospective randomized studies, preferably crossover, are needed to further study the impact of EL on central lines in the pediatric population. Such study design will help address the limitation of the current literature in regard to the impact of catheter age on outcomes, especially catheter repair and replacement rates.
Supplementary Material
Clinical Relevancy Statement.
Catheter-related bloodstream infection remains a serious complication in patients with intestinal failure who are dependent on intravenous access for survival. Such complications may have long-term implications that can negatively affect patient outcome. Several interventions have been attempted to reduce infection risk in this patient population, including the use of ethanol locks. However, available studies on ethanol lock use have been limited by sample size and included retrospective study designs with single-center experiences. Therefore, this systematic review and meta-analysis aim to assess the pooled effect of ethanol locks on catheter-related bloodstream infections in children with intestinal failure. The study also assesses the pooled impact of ethanol locks on catheter replacement and line integrity through measuring the need for line repairs.
Appendix
MEDLINE (Ovid)
exp Catheters/ or exp Catheterization/ or Catheter-Related Infections/
“catheter*.”tw
1 or 2
Alcohols/ or exp Anti-Infective Agents/ or Ethanol/
(ethanol* or alcohol*) adj10 (locks or lock)
4 or 5
3 and 6
exp Epidemiologic studies/
(cohort or longitudinal or prospective or retrospective or cross sectional).tw.
8 or 9
(infan* or child* or pediatric*).tw.
Pediatrics/ OR exp Child/
11 or 12
7 and 10 and 13
714 results retrieved (search run on March 28, 2017)
Embase
‘catheter’/exp OR ‘catheterization’/exp OR ‘catheter complication’/exp
‘antiinfective agent’/exp OR ‘alcohol’/exp
(ethanol* OR alcohol*) NEAR/10 (locks OR lock)
2 OR 3
1 AND 4
cohort OR longitudinal OR prospective OR ret-rospective OR cross NEAR/1 sectional OR ‘case control’
5 AND 6
‘pediatrics’/exp OR ‘child’/exp
infan* OR child* OR pediatric*
8 OR 9
7 AND 10
1496 results retrieved (search run on March 28, 2017)
Footnotes
Financial disclosure: None declared.
Statement of Authorship
R. Rahhal, M. A. Abu-El-Haija, D. Ebach, and C. R. Cole equally contributed to the conception and design of the research; E. Kiscaden and L. Fei contributed to the design of the research; all authors contributed to the acquisition and analysis of the data; L. Fei and C. R. Cole contributed to the interpretation of the data; and R. Rahhal drafted the manuscript. All authors critically revised the manuscript, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Supplementary Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Conflicts of interest: None declared.
References
- 1.Wales PW, de Silva N, Kim J, Lecce L, To T, Moore A. Neonatal short bowel syndrome: population-based estimates of incidence and mortality rates. J Pediatr Surg. 2004;39(5):690–695. [DOI] [PubMed] [Google Scholar]
- 2.Guarino A, De Marco G. Natural history of intestinal failure, investigated through a national network-based approach. J Pediatr Gastroenterol Nutr. 2003;37(2):136–141. [DOI] [PubMed] [Google Scholar]
- 3.Khan FA, Squires RH, Litman HJ, et al. Predictors of enteral autonomy in children with intestinal failure: a multicenter cohort study. J Pediatr. 2015;167(1):29–34, e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diamanti A, Basso MS, Castro M, Calce A, Pietrobattista A, Gambarara M. Prevalence of life-threatening complications in pediatric patients affected by intestinal failure. Transplant Proc. 2007;39(5):1632–1633. [DOI] [PubMed] [Google Scholar]
- 5.Sondheimer JM, Asturias E, Cadnapaphornchai M. Infection and cholestasis in neonates with intestinal resection and long-term parenteral nutrition. J Pediatr Gastroenterol Nutr. 1998;27(2): 131–137. [DOI] [PubMed] [Google Scholar]
- 6.Jones BA, Hull MA, Richardson DS, et al. Efficacy of ethanol locks in reducing central venous catheter infections in pediatric patients with intestinal failure. J Pediatr Surg. 2010;45(6):1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cober MP, Kovacevich DS, Teitelbaum DH. Ethanol-lock therapy for the prevention of central venous access device infections in pediatric patients with intestinal failure. JPEN J Parenter Enteral Nutr. 2011;35(1):67–73. [DOI] [PubMed] [Google Scholar]
- 8.Mouw E, Chessman K, Lesher A, Tagge E. Use of an ethanol lock to prevent catheter-related infections in children with short bowel syndrome. J PediatrSurg. 2008;43(6):1025–1029. [DOI] [PubMed] [Google Scholar]
- 9.Ardura MI, Lewis J, Tansmore JL, Harp PL, Dienhart MC, Balint JP. Central catheter-associated bloodstream infection reduction with ethanol lock prophylaxis in pediatric intestinal failure: broadening quality improvement initiatives from hospital to home. JAMA Pediatr. 2015;169(4):324–331. [DOI] [PubMed] [Google Scholar]
- 10.Wong T, Clifford V, McCallum Z, et al. Central venous catheter thrombosis associated with 70% ethanol locks in pediatric intestinal failure patients on home parenteral nutrition: a case series. JPEN J Parenter Enteral Nutr. 2012;36(3):358–360. [DOI] [PubMed] [Google Scholar]
- 11.Kayton ML, Garmey EG, Ishill NM, et al. Preliminary results of a phase I trial of prophylactic ethanol-lock administration to prevent mediport catheter-related bloodstream infections. J Pediatr Surg. 2010;45(10):1961–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abu-El-Haija M, Schultz J, Rahhal RM. Effects of 70% ethanol locks on rates of central line infection, thrombosis, breakage, and replacement in pediatric intestinal failure. J Pediatr Gastroenterol Nutr. 2014;58(6):703–708. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 14.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4): 401–406. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407–415. [DOI] [PubMed] [Google Scholar]
- 16.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323(7304):101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45(7):769–773. [DOI] [PubMed] [Google Scholar]
- 19.Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. Int J Epidemiol. 2002;31(1):140–149. [DOI] [PubMed] [Google Scholar]
- 20.Oliveira C, Nasr A, Brindle M, Wales PW Ethanol locks to prevent catheter-related bloodstream infections in parenteral nutrition: a meta-analysis. Pediatrics. 2012;129(2):318–329. [DOI] [PubMed] [Google Scholar]
- 21.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 22.Viechtbauer W Conducting meta-analyses in R with the metafor package. JStat Softw. 2010;36:1–48. [Google Scholar]
- 23.Mermel L, Alang N. Adverse effects associated with ethanol catheter lock solutions: a systematic review. J Antimicrob Chemother. 2014;69:2611–2619. [DOI] [PubMed] [Google Scholar]
- 24.Kawano T, Kaji T, Onishi S, et al. Efficacy of ethanol locks to reduce the incidence of catheter-related bloodstream infections for home parenteral nutrition pediatric patients: comparison of therapeutic treatment with prophylactic treatment. Pediatr Surg Int. 2016;32(9): 863–867. [DOI] [PubMed] [Google Scholar]
- 25.Pieroni KP, Nespor C, Ng M, et al. Evaluation of ethanol lock therapy in pediatric patients on long-term parenteral nutrition. Nutr Clin Pract. 2013;28(2):226–231. [DOI] [PubMed] [Google Scholar]
- 26.Wales PW, Kosar C, Carricato M, de Silva N, Lang K, Avitzur Y. Ethanol lock therapy to reduce the incidence of catheter-related bloodstream infections in home parenteral nutrition patients with intestinal failure: preliminary experience. J Pediatr Surg. 2011;46(5):951–956. [DOI] [PubMed] [Google Scholar]
- 27.Mezoff EA, Fei L, Troutt M, Klotz K, Kocoshis SA, Cole CR. Ethanol lock efficacy and associated complications in children with intestinal failure. JPENJ Parenter Enteral Nutr. 2016;40(6):815–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mokha JS, Davidovics ZH, Samela K, Emerick K. Effects of ethanol lock therapy on central line infections and mechanical problems in children with intestinal failure. JPEN J Parenter Enteral Nutr. 2017;41(4):625–631. [DOI] [PubMed] [Google Scholar]
- 29.Stanger JD, Oliveira C, Blackmore C, Avitzur Y, Wales PW. The impact of multi-disciplinary intestinal rehabilitation programs on the outcome of pediatric patients with intestinal failure: a systematic review and meta-analysis. J Pediatr Surg. 2013;48(5):983–992. [DOI] [PubMed] [Google Scholar]
- 30.Infantino BJ, Mercer DF, Hobson BD, et al. Successful rehabilitation in pediatric ultrashort small bowel syndrome. J Pediatr. 2013;163(5):1361–1366. [DOI] [PubMed] [Google Scholar]
- 31.O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51(RR-10):1–29. [PubMed] [Google Scholar]
- 32.Wales PW, de Silva N, Kim JH, Lecce L, Sandhu A, Moore AM. Neonatal short bowel syndrome: a cohort study. J Pediatr Surg. 2005;40(5):755–762. [DOI] [PubMed] [Google Scholar]
- 33.Drews BB, Sanghavi R, Siegel JD, Metcalf P, Mittal NK. Characteristics of catheter-related bloodstream infections in children with intestinal failure: implications for clinical management. Gastroenterol Nurs. 2009;32(6):385–390. [DOI] [PubMed] [Google Scholar]
- 34.Chambers ST, Peddie B, Pithie A. Ethanol disinfection of plastic-adherent micro-organisms. J Hosp Infect. 2006;63(2):193–196. [DOI] [PubMed] [Google Scholar]
- 35.Metcalf SC, Chambers ST, Pithie AD. Use of ethanol locks to prevent recurrent central line sepsis. J Infect. 2004;49(1):20–22. [DOI] [PubMed] [Google Scholar]
- 36.Crnich CJ, Halfmann JA, Crone WC, Maki DG. The effects of prolonged ethanol exposure on the mechanical properties of polyurethane and silicone catheters used for intravascular access. Infect Control Hosp Epidemiol. 2005;26(8):708–714. [DOI] [PubMed] [Google Scholar]
- 37.Guenu S, Heng AE, Charbonne F, et al. Mass spectrometry and scanning electron microscopy study of silicone tunneled dialysis catheter integrity after an exposure of 15 days to 60% ethanol solution. Rapid Commun Mass Spectrom. 2007;21(2):229–236. [DOI] [PubMed] [Google Scholar]
- 38.Bell AL, Jayaraman R, Vercaigne LM. Effect of ethanol/trisodium citrate lock on the mechanical properties of carbothane hemodialysis catheters. Clin Nephrol. 2006;65(5):342–348. [DOI] [PubMed] [Google Scholar]
- 39.Schilcher G, Schlagenhauf A, Schneditz D, et al. Ethanol causes protein precipitation—new safety issues for catheter locking techniques. PLoS One. 2013;8(12):e84869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Polaschegg HD. Catheter locking-solution spillage: theory and experimental verification. BloodPurif. 2008;26(3):255–260. [DOI] [PubMed] [Google Scholar]
- 41.Agharazii M, Plamondon I, Lebel M, Douville P, Desmeules S. Estimation of heparin leak into the systemic circulation after central venous catheter heparin lock. Nephrol Dial Transplant. 2005;20(6): 1238–1240. [DOI] [PubMed] [Google Scholar]
- 42.Laird J, Soutar R, Butcher I. Complications of the ethanol-lock technique in the treatment of central venous catheter sepsis. J Infect. 2005;51(4):338. [DOI] [PubMed] [Google Scholar]
- 43.Restrepo D, Laconi NS, Alcantar NA, et al. Inhibition of heparin precipitation, bacterial growth, and fungal growth with a combined isopropanol-ethanol locking solution for vascular access devices. J Pediatr Surg. 2015;50(3):472–477. [DOI] [PubMed] [Google Scholar]
- 44.Shah CB, Mittelman MW, Costerton JW, et al. Antimicrobial activity of a novel catheter lock solution. Antimicrob Agents Chemother. 2002;46(6):1674–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bisseling TM, Willems MC, Versleijen MW, Hendriks JC, Vissers RK, Wanten GJ. Taurolidine lock is highly effective in preventing catheter-related bloodstream infections in patients on home parenteral nutrition: a heparin-controlled prospective trial. Clin Nutr. 2010;29(4):464–468. [DOI] [PubMed] [Google Scholar]
- 46.Chu HP, Brind J, Tomar R, Hill S. Significant reduction in central venous catheter-related bloodstream infections in children on HPN after starting treatment with taurolidine line lock. J Pediatr Gastroenterol Nutr. 2012;55(4):403–407. [DOI] [PubMed] [Google Scholar]
- 47.Olthof ED, Versleijen MW, Huisman-de Waal G, Feuth T, Kievit W, Wanten GJ. Taurolidine lock is superior to heparin lock in the prevention of catheter related bloodstream infections and occlusions. PLoS One. 2014;9(11):e111216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


