Abstract
Clinicians can feel confident about performing mitral repair/replacement in patients who have previously undergone mammoplasty. It may also have applications in performing atrial septal defect closure, Maze procedures for atrial fibrillation, and tricuspid valve surgery in patients with breast implants.
Keywords: breast cancer, mammoplasty, minimally invasive, mitral valve surgery
1. INTRODUCTION
There is currently limited data on the risk of performing cardiac surgery in patients with prior mammoplasty. The breast implant may interfere with the ability to access the fifth intercostal space required for minimal invasive mitral valve surgery. As the number of breast implants due to cosmetic reasons, prior breast cancer and other reasons increases, there is a need to routinely manage this clinical situation. Prior research suggests that an inframammary incision, removal, and reintroduction of the implant results in favorable clinical outcome.1, 2, 3
We report on a 78‐year‐old female patient with severe mitral valve regurgitation and atrial fibrillation (AF), requiring surgical correction. The patient had previously received mammoplasty due to breast cancer. The breast implant was removed prior to the procedures through an inframammary incision, preserved in an aseptic solution, and reintroduced without damage afterward.
2. CASE HISTORY
Here, we report on a 78‐year‐old woman presenting to our cardiac surgery department with dyspnoea, NYHA class III‐IV, and persistent AF. The patient had a history of breast cancer, with left‐ and right‐sided breast implants which required surgical revision later on, but no radiation or chemotherapy performed. A detailed patient history and diagnostic workup excluded coronary artery disease. Preoperative transthoracic echocardiography (possible, but with limitations) revealed severe degenerative mitral valve regurgitation (III‐IV°) with a prolapse of the lateral (P1) and middle (P2) scallops for the posterior mitral valve leaflet. A small patent foramen ovale and macroangiopathy of the descending aorta were concomitant diagnoses. The left ventricular ejection fraction was 50%, while the right ventricular had a normal function. Tricuspid annular plane systolic excursion (TAPSE) was 17 mm.
2.1. Treatment
The patient was scheduled to undergo minimally invasive mitral valve surgery (MIMVS) and cryoablation of the AF. After a 1.5 cm skin incision, the right inguinal femoral artery and vein were prepared and, under appropriate anticoagulation and transesophageal echocardographic (TEE) control, the venous and arterial cannula were inserted to establish a cardiopulmonary bypass. As the breast implant reached from the second to the seventh intercostal space, it precluded the use of a right lateral thoracotomy at the fifth intercostal space without injuring the breast implant. Therefore, following a 7 cm skin incision under the right breast, the dense capsule of the breast implant was opened, the implant was explanted and checked for leakages. As none were noted, the implant was preserved in an aseptic solution during the cardiac intervention (Figure 1).
Figure 1.

Intraoperative explanted mammoplasty
Upon removal of the breast implant, the fifth intercostal space was opened, and a small incision was made at the third intercostal space for the camera and a further small incision for the atrial retractor for the MIMVS. The pericardium was opened, the aortic valve was clamped and Bretschneider's cardioplegia performed. After total bypass, the right atrium and interatrial septum were opened. Left atrial retraction provided excellent exposure of the mitral valve. As the patient had degenerative mitral valve disease with a retraction of the anterior and posterior leaflets and annular dilation, it required a replacement of the mitral valve with a 31 mm biological Epic Valve (Figure 2).
Figure 2.
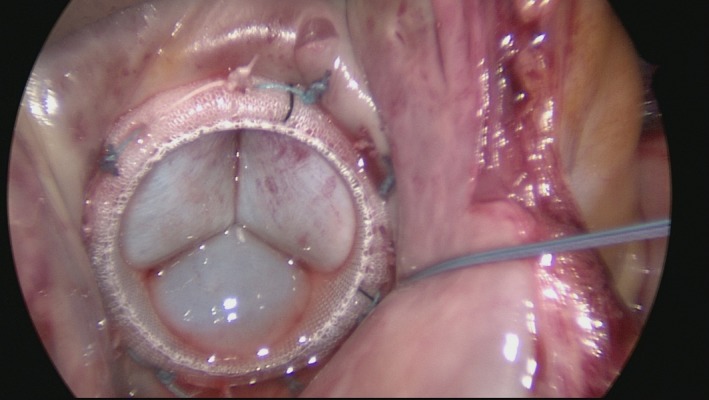
Minimally invasive mitral valve replacement
In the next step, cryoablation of the AF was performed, the interatrial septum closed, and the aortic clamp released. An adequate reperfusion was observed, and TEE demonstrated a fully functional and competent mitral valve. The patient was administered with protamine, an antidote for heparin, when the cardiopulmonary bypass was complete. The right lateral thoracotomy at the fifth intercostal space was closed with two single stiches. The aseptically preserved breast implant was reinserted and, to avoid injury to the implant, was closed with eight single stiches at the solid capsule of the implant. Finally, the subcutaneous wound of the right mini thoracotomy was closed (Figure 3, left).
Figure 3.

Clinical situation after the intervention (left) and after 18 mo of follow‐up (right)
2.2. Outcome and follow‐up
The patient spent 1 day in the intensive care unit before being transferred to a regular ward. Postoperative echocardiography revealed a competent mitral valve without regurgitation or paravalvular leak. The patient was discharged after 10 days to rehabilitation. At 6 and 18 months’ of follow‐up after the MIMVS, the patient was without wound infection and in a good general condition (Figure 3, left).
3. DISCUSSION
Here, we described the case of a 78‐year‐old female patient with breast implants that needed to undergo MIMVS and cryoablation of the AF. Minimally invasive heart surgery using a limited thoracotomy offers many potential benefits including reduction in blood loss, shorter hospital stay, faster recovery time, decreased pain, and improved cosmesis but requires access to the intercostal space. Therefore, the breast implant needed to be temporarily removed to facilitate the cardiac surgery and retrointroduced after the procedure. The case illustrates the feasibility and safety of performing MIMVS in this specific patient population and as such may help in the future clinical decisions.
Although there is an increasing need to perform cardiac surgery in patients with breast implants, there is little evidence reported so far in the literature on the approach and potential outcomes: A 32 patient cohort study published in 2016 described the outcomes of patients with a history of breast cancer with a need to undergo cardiac bypass or combined CABG surgery.1 No significant differences vs a 99 patient control group regarding duration of surgery, internal mammary artery (IMA) utilization, incidence of infections and postoperative complications or mortality were observed. The authors concluded that CABG surgery can safely be performed with good results over a mean follow‐up of 67 years. Shafii et al reported on the outcomes of six patients undergoing surgery because of isolated degenerative mitral valve in 2009 where a prior breast implant was removed through an inframammary incision and reintroduced after performing the minimal invasive surgery.2 This approach is comparable to the one we chose. The mitral valve was repaired in five patients and replaced in one patient. No conversion to median sternotomy, no bleeding complications, and no infections were reported, and the procedure had a satisfactory cosmetic result. Baker et al published a series of patients in 2012 with prior mammoplasty undergoing minimal invasive cardiac surgery of the aortic valve in one patient and mitral valve repair in four patients.3 The authors also chose an inframammary access for the removal and reinsertion of the breast implant. Two of the patients with mitral valve repair underwent a concomitant MAZE procedure for AF. Including a follow‐up of 2‐12 month, they reported no significant postoperative complications such as infections, hematoma, or need for reoperation. Long‐term outcomes have been hardly presented and as such observation made by Fong (in 2011) and Songcharoen (in 2015) are noteworthy. Both groups reported on late complications of MIMVS in patients with breast implants with a delayed migration of the subpectoral implant into the chest cavity through an iatrogenic defect after the MIMVS.4, 5
4. CONCLUSIONS
Both the number of patients with breast implants and the ones in need of valvular heart surgery are on the rise. Minimal invasive surgery is usually preferred as it has been associated with reduced blood loss, shorter postprocedural hospital stay, a faster recovery time and decreased pain for the patient and improved cosmesis.3 The breast implant though prevents access to the second, third, fourth, or fifth intercostal space and therefore needs to be temporarily removed. Here, we report on a successful combined mitral valve replacement and cryoablation of concomitant AF in a patients with breast implants. As a wider acceptance of this approach is gained, clinicians can feel confident about performing mitral repair/replacement in patients who have previously undergone mammoplasty. It may also have applications in performing atrial septal defect closure, Maze procedures for AF, and tricuspid valve surgery in patients with breast implants.
CONFLICT OF INTEREST
None of the authors has a conflict of interest with respect to the present article.
AUTHOR CONTRIBUTIONS
AC, AB, SH, MR, and MS: treated the patient and recorded the information for the case report. AC and PB: developed the concept. PB: wrote the first draft of the manuscript. It was carefully revised by all authors and all agree with the submission.
ACKNOWLEDGMENT
None.
Cetinkaya A, Borsche A, Hein S, Bramlage P, Schoenburg M, Richter M. Explantation and reimplantation of a breast implant to facilitate minimally invasive mitral valve surgery and cryoablation of atrial fibrillation. Clin Case Rep. 2019;7:1181–1184. 10.1002/ccr3.2185
REFERENCES
- 1. Leistner M, Sommer S, Aleksic I, et al. Cardiac surgery is safe in female patients with a history of breast cancer. Ann Thorac Cardiovasc Surg. 2016;22(3):168‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shafii AE, Su JW, Hendrickson M, Mihaljevic T, Gillinov AM. Right inframammary mini‐thoracotomy approach to the mitral valve in women with breast implants. Innovations (Phila). 2009;4(5):278‐281. [DOI] [PubMed] [Google Scholar]
- 3. Baker RY, Nguyen TJ, Hernandez AM, Wong AK, Baker CJ, Starnes VA. Breast implants and minimally invasive cardiac surgery: a case series. Ann Plast Surg. 2012;69(1):10‐13. [DOI] [PubMed] [Google Scholar]
- 4. Songcharoen SJ, McClure M, Aru RG, Songcharoen S. Intrathoracic migration of a breast implant after minimally invasive cardiac surgery. Ann Plast Surg. 2015;74(3):274‐276. [DOI] [PubMed] [Google Scholar]
- 5. Fong TC, Hoffmann B. Images in clinical medicine. Disappearance of a breast prosthesis during pilates. N Engl J Med. 2011;365(24):2305. [DOI] [PubMed] [Google Scholar]


