Key Points
Question
Is frequent use of modern digital media platforms, such as social media, associated with occurrence of ADHD symptoms during adolescence?
Findings
In this longitudinal cohort survey study of adolescents aged 15 and 16 years at baseline and without symptoms of ADHD, there was a significant association between higher frequency of modern digital media use and subsequent symptoms of ADHD over a 24-month follow-up (odds ratio, 1.11 per additional digital media activity).
Meaning
More frequent use of digital media may be associated with development of ADHD symptoms; further research is needed to assess whether this association is causal.
Abstract
Importance
Modern digital platforms are easily accessible and intensely stimulating; it is unknown whether frequent use of digital media may be associated with symptoms of attention-deficit/hyperactivity disorder (ADHD).
Objective
To determine whether the frequency of using digital media among 15- and 16-year-olds without significant ADHD symptoms is associated with subsequent occurrence of ADHD symptoms during a 24-month follow-up.
Design, Setting, and Participants
Longitudinal cohort of students in 10 Los Angeles County, California, high schools recruited through convenience sampling. Baseline and 6-, 12-, 18-, and 24-month follow-up surveys were administered from September 2014 (10th grade) to December 2016 (12th grade). Of 4100 eligible students, 3051 10th-graders (74%) were surveyed at the baseline assessment.
Exposures
Self-reported use of 14 different modern digital media activities at a high-frequency rate over the preceding week was defined as many times a day (yes/no) and was summed in a cumulative index (range, 0-14).
Main Outcomes and Measures
Self-rated frequency of 18 ADHD symptoms (never/rare, sometimes, often, very often) in the 6 months preceding the survey. The total numbers of 9 inattentive symptoms (range, 0-9) and 9 hyperactive-impulsive symptoms (range, 0-9) that students rated as experiencing often or very often were calculated. Students who had reported experiencing often or very often 6 or more symptoms in either category were classified as being ADHD symptom-positive.
Results
Among the 2587 adolescents (63% eligible students; 54.4% girls; mean [SD] age 15.5 years [0.5 years]) who did not have significant symptoms of ADHD at baseline, the median follow-up was 22.6 months (interquartile range [IQR], 21.8-23.0, months). The mean (SD) number of baseline digital media activities used at a high-frequency rate was 3.62 (3.30); 1398 students (54.1%) indicated high frequency of checking social media (95% CI, 52.1%-56.0%), which was the most common media activity. High-frequency engagement in each additional digital media activity at baseline was associated with a significantly higher odds of having symptoms of ADHD across follow-ups (OR, 1.11; 95% CI, 1.06-1.16). This association persisted after covariate adjustment (OR, 1.10; 95% CI, 1.05-1.15). The 495 students who reported no high-frequency media use at baseline had a 4.6% mean rate of having ADHD symptoms across follow-ups vs 9.5% among the 114 who reported 7 high-frequency activities (difference; 4.9%; 95% CI, 2.5%-7.3%) and vs 10.5% among the 51 students who reported 14 high-frequency activities (difference, 5.9%; 95% CI, 2.6%-9.2%).
Conclusions and Relevance
Among adolescents followed up over 2 years, there was a statistically significant but modest association between higher frequency of digital media use and subsequent symptoms of ADHD. Further research is needed to determine whether this association is causal.
This 24-month cohort study tracks high school students in Los Angeles County, California, who were not initially assessed as having ADHD symptoms to compare frequency of use of digital media platforms with experiencing ADHD symptoms.
Introduction
Attention-deficit/hyperactivity disorder (ADHD)—a psychiatric condition involving persistent difficulty sustaining attention, hyperactivity, and impulsivity—was estimated to affect 7% of youth in a meta-analytic pooled estimate of studies published from 1981 to 2014,1 and the rate may be increasing in some populations.2 Because nongenetic environmental factors are associated with adolescent ADHD,3 increasing exposure to environmental risk factors may contribute to increasing ADHD rates in that population.
A meta-analysis of studies conducted from 1987 to 2011 found that use of traditional forms of digital media (eg, television viewing and videogame console playing) was modestly associated with ADHD and related outcomes.4 Digital media has since evolved. Modern digital platforms are diverse (eg, social networking, streaming movies or music, and texting), constantly available via mobile devices, and capable of providing rapid high-intensity stimulation. Whether the variety of modern digital media platforms currently available and the high frequency at which some teens use them increases risk of ADHD symptom occurrence is unknown.
This longitudinal cohort study of Los Angeles, County, California, high school students examined whether modern digital media-use frequency among 15- and 16-year-olds without significant ADHD symptoms was associated with subsequent ADHD symptom occurrence over a 24-month follow-up period. Secondarily, this study estimated the associations between high-frequency use of specific modern digital media platforms and ADHD symptom occurrence and between media use and ADHD symptom severity.
Methods
Participants and Procedures
Data were drawn from the Happiness & Health Study,5 a longitudinal cohort survey of adolescents in Los Angeles. Among 40 local public high schools approached, 10 schools were selected based on their interest in participating, demographic composition, and proximity. Participating school characteristics in reference to Los Angeles County, California, public schools appear in eTable 1 in the Supplement. Participants and their parents provided active assent and consent prior to enrolling in the study when in ninth grade. Semiannual assessments were administered in classrooms. Students not present completed abbreviated surveys omitting key measures and are not included in this study. The University of Southern California institutional review board approved the study.
Variables for this study were measured in fall of 10th grade, referred to herein as the baseline survey. The sample included students who completed key measures and were classified as not having ADHD symptoms at baseline based on the Current Symptoms Self-Report Form score,6 using definitions described below. Data analyzed include baseline (fall 2014, 10th grade) and 6-month (spring 2015, 10th grade), 12-month (fall 2015, 11th grade), 18-month (spring 2016, 11th grade), and 24-month (fall 2016, 12th grade) follow-ups.
Measures
ADHD Symptoms
At each time point, students completed the Current Symptoms Self-Report Form6 measure of the Diagnostic and Statistical Manual of Mental Disorders–4th Edition (DSM-IV)7 ADHD symptom criteria, including 9 inattention symptoms (eg, difficulty organizing and completing tasks) and 9 hyperactivity-impulsivity symptoms (eg, trouble remaining still or with task persistence). Respondents rated the frequency that they experienced each symptom in the preceding 6 months: never or rare, 0; sometimes, 1; often, 2; or very often, 3. Consistent with recommendations6 and DSM-IV criteria,7 adolescents who reported experiencing 6 more symptoms in either inattention or hyperactivity-impulsivity categories were classified as having ADHD symptoms over the past 6 months; therefore, they were considered to be positive for ADHD symptoms—our study’s primary binary outcome. Studies of self-assessment of ADHD symptoms compared with diagnoses made by clinical interviews have an estimated diagnostic sensitivity of 79% and a specificity of 60%.8,9 The ADHD symptom severity score was a secondary outcome derived from the sum of the 0- to 3-symptom frequency ratings (range, 0-54), yielding adequate concordance with clinician-derived severity scores in previous work (Pearson rs ≥.72).8
Modern Digital Media Use
At baseline and at the 12- and 24-month follow-up surveys, students were asked to indicate how frequently they engaged in each of the 14 media activities in the past week (0, 1-2 times per week; 1-2 times per day; or many times per day). Each response was dichotomized into high-frequency (many times per day) vs other frequency levels (0, 1-2 times per week, 1-2 times per day) and summed in a cumulative media-use index that ranged from 0 to 14.
Covariates
To address possible confounding influences, baseline factors previously associated with digital media use or ADHD were included as covariates.10,11,12 Self-report sociodemographic covariates were age (years), sex (male/female), and subsidized lunch eligibility, based in part on having a family income 185% or less than the US federal poverty guideline (yes/no). Because ADHD prevalence may differ by race/ethnicity,2 self-reported forced choice of 1 of 8 investigator-defined fixed race/ethnicity categories (American Indian/Alaska Native, Asian, black/African American, Hispanic/Latino, Native Hawaiian/Pacific Islander, white, multiethnic/multiracial, or other) was a covariate. American Indian/Alaska Native, Native Hawaiian/Pacific Islander, multiethnic/multiracial, or other responses constituted an other category.
Given behavioral and emotional problems in ADHD,13 additional covariates included baseline self-reported delinquent behavior, measured with a sum of the frequency of 11 behaviors in the past 6 months (eg, stealing and skipping school; range, 1 [never] to 6 [≥10 times]),14 the Center for Epidemiologic Studies Depression (CESD) scale15 sum score of ratings (0, rarely or none of the time to 3, most or all of the time) of 20 depressive symptoms, substance use (current [past month] vs past [ever use, but no use in the past month] vs never use of cigarettes, alcohol, or cannabis), and family substance-use history (ie, siblings, parents, grandparents who reportedly smoked cigarettes or had an alcohol or drug-abuse problem, yes/no).
Statistical Analysis
Descriptive Analyses
Descriptive statistics of study variables, internal consistency estimates (Cronbach αs) for continuous variables, and stability estimates of associations across time points for the digital media frequency index (Pearson rs) and ADHD symptom status (φ coefficients) variables were calculated. Bivariate correlations between digital media index scores and ADHD symptom status (Point-biserial rs) for each time point were tested.
Main Analyses
Logistic random effect–repeated measures regression modeling was used to test the association of baseline digital media use, covariates, and time with likelihood of ADHD symptoms during the 6-, 12-, 18-, and 24-month follow-ups. The primary analysis used the cumulative digital media-use index (range, 0-14) regressor and the binary ADHD symptom status outcome. Secondary analyses tested associations of (1) high-frequency engagement in each media activity with ADHD symptom status in 14 separate repeated measures logistic regression models and (2) the cumulative digital media index with ADHD symptom severity score in repeated measures linear regression adjusted for baseline ADHD symptom severity among students at all levels of baseline ADHD symptoms.
We tested unadjusted and covariate-adjusted models. The digital media–use regressor estimate indicated the mean association with ADHD symptoms across the 4 follow-ups. Digital media use × time interaction terms were added in subsequent models to test whether the rate of change of ADHD symptom status or level across time was associated with baseline media use. Additional sensitivity analyses are summarized below and detailed in the eResults section of the Supplement.
Analyses were tested in Mplus16 version 7 using 2-level random effects.17 Time was nested within students, and school-level random effects were included. Missing data were managed with full information maximum likelihood estimation. Odds ratios (ORs) or regression weights (bs) with 95% CIs were reported with statistical significance set at P < .05 (2-tailed). Benjamini-Hochberg multiple-testing corrections were applied to control the false-discovery rate at .05.18
Results
Study Sample
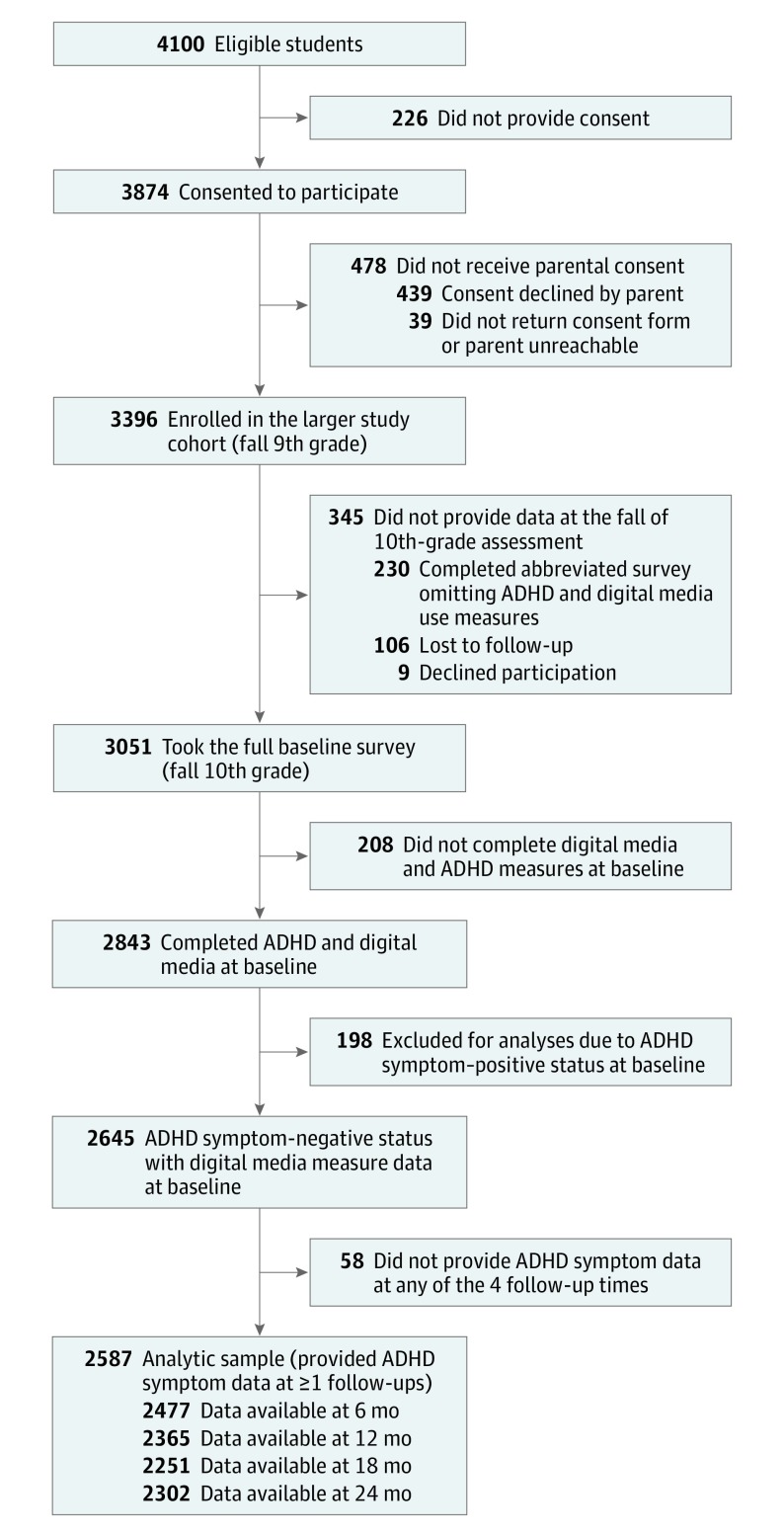
Participant accrual, sample size, and exclusions from the analytic sample are depicted in Figure 1. Among 4100 eligible ninth-grade students, 3874 (94.5%) assented, for whom 3396 (87.7%) provided consent and enrolled. Of the 3051 participants administered the baseline full-length survey, 2843 (93.2%) completed digital media and ADHD symptom measures, of whom, 2645 were below baseline ADHD symptom thresholds. After excluding 58 students (2.2%) who did not have follow-up data for 1 or more time points (eTable 2 in the Supplement depicts follow-up completion patterns), the primary analytic sample was 2587. Some groups of students excluded from the primary analysis were significantly older, had greater proportions of students eligible for subsidized lunch, and had different sex and race/ethnicity compositions (eTable 3 in the Supplement).
Figure 1. Accrual of Adolescents in Study of Digital Media Use and ADHD.
Participants who did not provide data at the 4 follow-ups represent students who were not present during in-class data collections due to absence or being no longer enrolled at 1 of the study schools. See eTable 2 in the Supplement for the number of students completing 1 or multiple follow-up assessments. ADHD indicates attention-deficit/hyperactivity disorder.
Descriptive Analyses
Of the 2587 students (63%) in the analytic sample, 54.4% were girls; 47.5%, Hispanic; 17.4%, Asian; 4.2%, black; 15.2%, white; and 15.7%, other. They were a mean (SD) age of 15.5 years (0.5 years) at baseline (Table 1).
Table 1. Descriptive Statistics and Internal Consistency of Baseline Digital Media Use and Study Covariates in Participating Students.
| Baseline Variable | No. (%) of Students (n=2587) |
Available No.a | Cronbach αb |
|---|---|---|---|
| Girls | 1406 (54.3) | 2587 | |
| Age, mean (SD), y | 15.5 (0.5) | 2518 | |
| Race/ethnicity | 2528 | ||
| Hispanic | 1201 (47.5) | ||
| Asian | 439 (17.4) | ||
| Black | 105 (4.2) | ||
| White | 385 (15.2) | ||
| Otherc | 398 (15.7) | ||
| Receiving subsidized lunch | 1130 (48.2) | 2343 | |
| Substance use | 2566 | ||
| Never | 1369 (53.4) | ||
| Past | 607 (23.7) | ||
| Current | 590 (23.0) | ||
| Family history of substance use | 983 (39.9) | 2467 | |
| Delinquent behavior, mean (SD)d | 14.3 (4.2) | 2585 | .73 |
| CESD scale for depressive symptomse | |||
| Mean (SD) | 14.3 (12.1) | 2559 | .82 |
| Median (IQR) | 15.8 (5.3-21.1) | ||
| No. of digital media activities used at a high frequency ratef | |||
| Mean (SD) | 3.6 (3.3) | 2587 | .86 |
| Median (IQR) | 4.0 (1.0-5.0) |
Abbreviations: CESD, Center for Epidemiologic Studies Depression; IQR, interquartile range.
The number of students with (nonmissing) data available for the respective variable and denominators for percentages reported for categorical variables.
Chronbach α estimate of internal consistency reliability in study sample.
See the Methods section for definition.
Score ranges from 11 to 66, with higher scores indicating greater frequency of engaging in 11 different delinquent behaviors. Each behavior is rated from 1 (never) to 6 (10 or more times) for 11 behaviors.
Scores range from 0 to 60, with higher scores indicating greater severity of past-week depressive symptoms. Each symptom rated 0 (rarely or none of the time; 0-1 day) to 3 (most or all of the time; 5-7 days) for 20 symptoms.
Score ranges from 0 to 14, higher scores indicate greater digital media use. Total number of 14 different digital media activities engaged in at a high frequency rate (many times per day) over the preceding week.
The distribution of high-frequency digital media activities had a mean (SD) of 3.62 (3.30) and was positively skewed (the number of students at each use-frequency level are reported along the horizontal axis of Figure 2E), with 2090 (80.9%) students reporting high-frequency use of at least 1 activity. Among study participants, 172 (6.9%) at 6 months; 113 (4.8%) at 12 months; 129 (5.7%) at 18 months, and 135 (5.9%) at 24 months had experienced ADHD symptoms in the 6-month intervals between surveys. Media-use index and ADHD symptom status internal consistency, stability, and bivariate association estimates were statistically significant at all time points (eTable 4 in the Supplement).
Figure 2. Attention-Deficit/Hyperactivity Disorder (ADHD) Symptom Prevalence at Follow-ups, by Baseline Cumulative Digital Media Use Index Score of Participating High School Students.
See the Methods section for determining ADHD symptoms. Score ranges from 0 to 14, higher scores indicate greater digital media use. Total number of 14 different digital media activities engaged in at a high-frequency rate (many times per day) over the preceding week. Panel E shows the ADHD mean symptom prevalence, across all 4 follow-up time points, weighted by the number of available observations, presented with error bars representing 95% CIs by the baseline level of digital media use.
Primary Analysis
In the unadjusted logistic regression model, each additional baseline high-frequency digital media activity used was associated with significantly higher odds (OR, 1.11; 95% CI, 1.06-1.16) of positive (vs negative) ADHD symptom occurrence during the 6-months intervals between administration of the follow-up surveys (Table 2). Time and digital media use × time estimates indicate the ADHD symptom prevalence across follow-ups did not significantly change overall, and the rate of change in symptoms over time was not associated with media use.
Table 2. Association of Baseline Cumulative Digital Media Use Index With Attention-Deficit/Hyperactivity Disorder Symptom Status Across Follow-upsa.
| Regression Variable | Past 6-Month ADHD Symptoms at Follow-ups, Odds Ratio (95% CI)b | P Valueb |
|---|---|---|
| Unadjusted Modelc | ||
| Digital media activities used at a high-frequency rate, No.d | 1.11 (1.06-1.16) | <.001 |
| Timee | 0.95 (0.87-1.04) | .29 |
| No. of digital media activities used at a high-frequency rate × timef | 0.98 (0.96-1.01) | .11 |
| Adjusted Modelg | ||
| Digital media activities used at a high-frequency rate, No.d | 1.10 (1.05-1.15) | <.001 |
| Timee | 0.95 (0.87-1.05) | .33 |
| No. of digital media activities used at a high-frequency rate × timef | 0.99 (0.97-1.01) | .30 |
| Girls vs boys | 0.41 (0.30-0.56) | <.001 |
| Age (continuous variable)h | 1.03 (0.79-1.32) | .85 |
| Race/ethnicity | ||
| Hispanic | 1 [Reference] | |
| Asian | 0.86 (0.48-1.51) | .59 |
| Black | 1.58 (0.72-3.49) | .26 |
| White | 0.99 (0.59-1.66) | .96 |
| Otheri | 1.09 (0.64-1.84) | .76 |
| Eligible for subsidized lunch (yes vs no) | 0.73 (0.51-1.06) | .10 |
| Substance use | ||
| Never | 1 [Reference] | |
| Past | 1.29 (0.88-1.89) | .15 |
| Current | 1.40 (0.83-2.39) | .24 |
| Family history of substance use (yes vs no) | 1.12 (0.81-1.55) | .49 |
| Delinquent behavior (continuous variable)h,j | 1.36 (1.15-1.61) | <.001 |
| CESD scale for depressive symptoms (continuous variable)h,j | 1.90 (1.58-2.29) | <.001 |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; AIC, Akaike information criterion; BIC, Bayesian information criteria, CESD, Center for Epidemiologic Studies Depression.
Includes 2587 participating students who did not surpass the ADHD self-report symptom scale threshold for the past 6-month ADHD symptoms (see the Methods section for determining ADHD symptoms).
The estimate of the association of the respective regressor with ADHD symptom-positive (vs negative) status across follow-ups in repeated measures binary logistic regression models, including school random effects.
Unadjusted model included the time-invariant baseline digital media use cumulative index variable and time variable as sole regressors (fit statistics: AIC, 3782.89; BIC, 3811.48).
See the Methods section for frequency-use score determination.
Time continuous variable (scored at 6 month, 0; 12 months, 1; 18 months, 2; and 24 months, 3).
Interaction term added in subsequent models; ORs for other regressors are from models excluding the interaction term.
The adjusted model included the time-invariant baseline digital media-use cumulative index variable, the time variable, and all baseline time-invariant covariates as simultaneous regressors (fit statistics: AIC, 73500.95, BIC, 73863.13).
Rescaled (mean, 0; SD, 1) such that the odds ratios indicate the change in odds in the outcome associated with 1 SD higher on the regressor variable.
See the Methods section for definition of the “Other” race category.
See Table 1 footnote for score determination.
The covariate-adjusted association between the index of digital media use and ADHD symptom status remained significant (OR, 1.10; 95% CI, 1.05-1.15). In this model, boys (vs girls) and adolescents with more depressive symptoms and delinquent behaviors were at greater odds of experiencing ADHD symptoms during follow-up; other covariates were not associated with ADHD symptoms (Table 2).
The estimated mean symptom prevalence in the preceding 6 months across follow-ups by baseline of use of digital media derived from the unadjusted model are reported in eFigure 1 in the Supplement. Raw ADHD symptom prevalence across follow-ups, by baseline digital media-use index score are presented in Figure 2. The mean ADHD symptom prevalence was 4.6% for those who reported not using any digital media activity at a high frequency at baseline compared with 9.5% for those who reported 7 high-frequency activities (difference, 4.9%; 95% CI, 2.5%-7.3%) and 10.5% for those who reported 14 high-frequency activities (difference, 5.9%; 95% CI, 2.6%-9.2%).
Secondary Analyses
The prevalence of high-frequency use of each media activity are presented in Table 3 (left-hand columns). For example, 1398 adolescents (54.1%; 95% CI, 52.1%-56.0%) indicated checking social media sites at a high-frequency rate, the most common high-frequency activity reported. The next columns report the difference in mean ADHD symptom prevalence associated with high-frequency use (yes/no) for each activity. For 10 activities, high-frequency use was associated with an increased odds of ADHD symptoms across follow-ups after covariate adjustment.
Table 3. Prevalence of High-Frequency Use of Each Digital Media Activity and Association With Attention-Deficit/Hyperactivity Disorder Symptom Status Across Follow-upsa.
| Digital Media Activity | Prevalence of High-Frequency Use, No. (%) of Students (n=2587)b |
ADHD Symptom Prevalence Over Follow-ups Difference, % (95% CI)c | Association of High-Frequency Use With ADHD Symptoms at Follow-ups | |||
|---|---|---|---|---|---|---|
| Unadjustedd | Adjustede | |||||
| OR (95% CI)f | P Valuef | OR (95% CI)f | P Valuef | |||
| Checking social media sites | 1398 (54.1) | 1.2 (0.2 to 2.1) | 1.36 (1.01 to 1.82) | .04g | 1.53 (1.11 to 2.10) | .009g |
| Texting | 1340 (52.1) | 0.7 (−0.4 to 1.7) | 1.17 (0.87 to 1.57) | .29 | 1.21 (0.89 to 1.65) | .22 |
| Browsing or viewing images or videos | 1105 (42.9) | 1.9 (0.9 to 2.8) | 1.58 (1.17 to 2.13) | .003g | 1.45 (1.06 to 1.97) | .02g |
| Streaming or downloading music | 992 (38.5) | 2.1 (1.1 to 3.0) | 1.60 (1.19 to 2.14) | .002g | 1.50 (1.10 to 2.05) | .01g |
| Liking or commenting on others’ statuses, wall posts, or pictures | 734 (28.5) | 2.0 (0.9 to 3.0) | 1.69 (1.23 to 2.32) | .001g | 1.67 (1.23 to 2.27) | .001g |
| Chatting online | 680 (26.4) | 1.1 (−0.2 to 2.3) | 1.30 (0.94 to 1.79) | .10 | 1.34 (0.95 to 1.88) | .09 |
| Streaming television or movies | 649 (25.2) | 2.1 (1.0 to 3.1) | 1.58 (1.15 to 2.17) | .005g | 1.45 (1.04 to 2.02) | .03g |
| Playing games by yourself on a console, computer, or smartphone | 463 (18.0) | 3.9 (2.6 to 5.1) | 2.18 (1.54 to 3.09) | <.001g | 1.97 (1.40 to 2.78) | <.001g |
| Reading online blogs, articles, news, forums, or books | 456 (17.7) | 2.4 (1.1 to 3.6) | 1.65 (1.15 to 2.35) | .006g | 1.54 (1.06 to 2.23) | .02g |
| Playing games with friends or family on a console, computer, or smartphone | 394 (15.3) | 2.3 (0.6 to 4.0) | 1.57 (1.07 to 2.31) | .02g | 1.40 (0.95 to 2.04) | .09 |
| Sharing others’ photographs, images, videos, status updates, blogs, articles, or news | 330 (12.8) | 2.4 (1.0 to 3.8) | 1.74 (1.18 to 2.55) | .005g | 1.58 (1.08 to 2.30) | .02g |
| Posting own photographs, images, videos, status updates, or blogs | 316 (12.2) | 2.0 (0.2 to 3.7) | 1.52 (0.98 to 2.34) | .06 | 1.43 (0.92 to 2.23) | .12 |
| Online shopping or browsing | 261 (10.1) | 2.5 (0.9 to 4.1) | 1.81 (1.16 to 2.81) | .008g | 1.71 (1.11 to 2.64) | .02g |
| Video chatting | 226 (8.8) | 4.8 (3.1 to 6.5) | 2.36 (1.52 to 3.66) | <.001g | 2.11 (1.39 to 3.22) | <.001g |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; OR, odds ratio.
Includes students who reported experiencing 5 or less inattentive or 5 or less hyperactive-impulsive symptoms often or very often at baseline.
See the Methods section for frequency-use definitions.
Mean ADHD symptom-positive prevalence across follow-ups among baseline high-frequency digital media users of respective activity subtracted by mean ADHD symptom-positive prevalence across follow-ups among students who did not report high-frequency use of respective activity, weighted by the number of available observations at each time point.
Unadjusted models included a single time-invariant baseline high-frequency use binary variable for the respective media activity (yes/no) and the time variable as sole regressors.
Adjusted models included a single time-invariant baseline high-frequency use binary variable for the respective media activity (yes/no), the time variable, and all baseline time-invariant covariates listed in Table 2 as simultaneous regressors.
Estimate of association of high-frequency use of respective digital media activity at baseline (yes vs no) with ADHD symptom-positive (vs negative) status across follow-ups in repeated measures binary logistic regression models, including school random effects.
Statistically significant after Benjamini-Hochberg corrections for multiple testing to control false-discovery rate at .05 (based on 2-tailed corrected P value).
Among the 2843 students above or below the baseline ADHD symptom cut point, 2777 (97.7%) provided ADHD symptom data for at least 1 follow-up, constituting the analytic sample for the secondary outcome. Repeated measures linear regression models adjusted for baseline ADHD symptom level found that each additional baseline high-frequency digital media activity used (range, 0-14) was associated with 0.11 (95% CI, 0.02-0.20) points higher on the ADHD symptom severity score (range, 0-54) across follow-ups (unadjusted b, 0.11; 95% CI, 0.02-0.20); the covariate-adjusted association was also statistically significant (b, 0.10; 95% CI, 0.01-0.19; all regression weights are reported in eTable 6 in the Supplement).
Sensitivity Analyses
Sensitivity analyses examining different approaches to handling missing data, adjusting for baseline subclinical ADHD symptoms, and bidirectional associations between media use and ADHD symptoms found significant associations between digital media use and subsequent ADHD symptoms in all cases (eFigure 2 and eResults in the Supplement). Psychometric analyses of the digital media-use measure offered preliminary support of the measure’s validity and did not find that reliability differences between digital media use and ADHD measures explain their association across time (eResults and eTable 7 in the Supplement).
Discussion
In this study, high-frequency use of multiple forms of modern digital media was associated with increased odds of ADHD symptom occurrence over a 24-month period of midadolescence. Most previously reported relations of digital media use with ADHD symptoms were cross-sectional.4 Prior longitudinal studies of this topic assessed exposure to traditional forms of media (television or videogame console playing), having collected data prior to the widespread availability of modern media platforms.4 Modern and traditional digital media are not comparable due to marked differences in operating speed, level of stimulation, and potential for high-frequency exposure. Although some emerging research indicates that ADHD levels and use of certain forms of modern media may be concurrently associated,19,20 the role of modern digital media use in ADHD risk largely remains unclear from the prior literature due to limitations in exposure assessment and the application of designs incapable of supporting temporal or causal inferences. The current study provides new longitudinal evidence on this topic using a 5-wave prospective design and comprehensive assessment across a wide continuum of digital media exposure, including numerous media platforms currently popular among youth.
In midadolescence, there is an inherent drive to develop social identity and cultivate interpersonal relationships.21 Modern media platforms provide unprecedented opportunities for social connection. Teens can converse with dozens of peers simultaneously via group text messages. Social media permits instantaneous communication with thousands. Video chatting enables immediate face-to-face interactions. Midadolescence is also a period of high neural plasticity during which brain circuitry underlying attention and behavioral control mature rapidly and may be vulnerable to exposures that disrupt neurodevelopment.22,23
The course of ADHD is heterogeneous, and different symptom courses have been associated with distinct sources of risk.24 Originally considered a childhood-onset persistent disorder, recent evidence demonstrates that adolescent- or adult-onset of ADHD symptoms that follow volatile trajectories across time are common and associated with adverse health and social outcomes.25,26 Volatile ADHD symptom patterns across follow-ups were also observed in this cohort. Whether high-frequency modern digital media use is associated with other ADHD symptom courses, including early childhood- or adult-onset presentations, warrants future inquiry.
The observed association between modern digital media use and subsequent ADHD symptoms may reflect noncausal mechanisms, including reverse causation. Attention-deficit/hyperactivity disorder is associated with sensation seeking,27 which could promote pursuit of digital media to satisfy a drive for stimulation among youth who have ADHD symptoms. Although an association between ADHD level and subsequent modern digital media use was not found herein (eFigure 2 and eResults in the Supplement), an association between attention problems and subsequent videogame playing has been previously reported.28
Digital media use might have resulted from or be a proxy for subthreshold or undiagnosed ADHD, which was not detected at baseline and later manifested during follow-up. A sensitivity analysis addressing this explanation found that the primary association remained after adjusting for the subclinical ADHD symptom score—a covariate presumably associated with those with ADHD whose symptoms were undetected. The problem of overestimating or underestimating psychiatric disease due to misclassifying individuals with symptom levels close to diagnostic cut points can be reduced by using continuous symptom measures; digital media use was also associated with a continuous ADHD symptom score in this study. Nevertheless, because this study did not assess diagnostic history, it remains possible that undetected baseline ADHD influenced the findings.
The association could also derive from shared risk factors. Common genetic or environmental influences may increase both ADHD symptoms and digital media access. Parents with ADHD, substance use problems, or other impulsive tendencies may apply lax parenting styles without restricting offspring digital media use.29,30,31 Additionally, teens who admit frequent media use may be willing to report stigmatized conditions, such as ADHD, which may increase associations between these variables. Statistical adjustment for familial factors and other stigmatized behaviors sensitive to reporting biases, including family history of substance use, depressive symptoms, and delinquency, did not meaningfully affect the association. Still, the possibility that media use and ADHD symptoms are secondary to unknown (and unmeasured) common factors that operate across multiple time points cannot be ruled out.
Although alternative explanations remain possible, modern digital media use could play a role in the development of ADHD symptoms. The primary symptoms of ADHD are inattention (eg, distractibility, trouble with organization) and hyperactivity-impulsivity (eg, difficulty waiting, interrupting others, restlessness). Modern media devices immediately notify users when new text messages, social media postings, or videogame play invitations arrive. Exposure to such notifications may draw attention away from focal tasks. Frequent distractions could disrupt normative development of sustained attention and organization skills.32 Additionally, modern media platforms provide instantaneous access to highly stimulating experiences and rapid feedback in response to user input. An array of information, music, television programs, movies, videogames, or digital social interactions are immediately accessible with modern media. Consequently, high-frequency modern digital media users may become accustomed to rapid feedback, which could disrupt development of impulse control and patience.
Even if modern digital media use is somehow implicated in risk of ADHD symptoms, any resulting public health or clinical implications are uncertain. The change in ADHD symptoms associated with each increment of media exposure in this study was modest and residual confounding could account for some of this association. Although the exposure-risk association was cumulative, appreciable differences in ADHD symptoms emerged primarily in comparisons of low and high ends of the media use continuum. Some adolescents in this study reported high-frequency use of numerous modern digital media platforms; however, they constituted a minor portion of the sample. Whether adolescent media exposure levels (and corresponding ADHD symptom risk) will change as digital technology further evolves remains to be seen.
Limitations
This study has several limitations. First, the ADHD symptom scale is capable only of identifying symptoms consistent with the disorder. The scale includes 18 items keyed exactly to the 18 DSM-IV ADHD symptoms, permitting classifications that correspond with DSM-IV diagnostic thresholds (≥6 inattention or hyperactivity-impulsivity symptoms). While moderate concordance between ADHD symptom status obtained by self-rating scales and ADHD diagnoses yielded from diagnostic interviews have been reported,8,9 self-rating scales are insufficient for rendering ADHD diagnoses. Second, the media use measure’s validity had not been previously established. Although this study found preliminary evidence of validity, evidence of the measure’s concordance with objective digital device use indicators is needed to establish its validity. Third, the study focused on a targeted age range, used convenience sampling that resulted in 10 of 40 partnering schools from one region, and excluded students without data—a group that differed from the analytic sample on some demographic characteristics, which may affect generalizability. Fourth, the possibility that reverse causality or undetected baseline ADHD symptoms influenced the association cannot be ruled out.
Conclusions
Among adolescents followed up over 2 years, there was a statistically significant but modest association between higher frequency of digital media use and subsequent symptoms of ADHD. Further research is needed to determine whether this association is causal.
eResults
eFigure 1. Estimated mean prevalence of ADHD symptoms across follow-ups, by baseline modern digital media use frequency index derived from the primary unadjusted logistic regression model
eFigure 2. Cross-lagged model of associations between modern digital media use frequency index and ADHD symptom severity among students at all levels of baseline ADHD symptoms
eTable 1. Sociodemographic characteristics of participating schools in reference to Los Angeles county schools
eTable 2. Number of students with ADHD symptom data available at each follow-up in the primary analytic sample of baseline ADHD symptom-negative students
eTable 3. Sociodemographics of students included in (vs. excluded from) the primary analytic sample and estimated sociodemographics of students eligible to enroll in the cohort
eTable 4. Estimates of internal consistency, stability, and associations of cumulative digital media use index and ADHD symptom status across time points among baseline ADHD symptom-negative students
eTable 5. ADHD symptom prevalence across follow-ups, by baseline cumulative digital media use index score among baseline ADHD symptom-negative students
eTable 6. Regression weights from repeated measures linear regression models testing association with ADHD symptom severity at follow-ups among students at all baseline ADHD symptom levels
eTable 7. Estimates of internal consistency, stability, and associations among modern digital media use and ADHD symptom severity across time points among students at all levels of baseline ADHD symptoms
eReferences
References
- 1.Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135(4):e994-e1001. doi: 10.1542/peds.2014-3482 [DOI] [PubMed] [Google Scholar]
- 2.Nyarko KA, Grosse SD, Danielson ML, Holbrook JR, Visser SN, Shapira SK. Treated prevalence of attention-deficit/hyperactivity disorder increased from 2009 to 2015 among school-aged children and adolescents in the United States. J Child Adolesc Psychopharmacol. 2017;27(8):731-734. doi: 10.1089/cap.2016.0196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larsson J-O, Larsson H, Lichtenstein P. Genetic and environmental contributions to stability and change of ADHD symptoms between 8 and 13 years of age: a longitudinal twin study. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1267-1275. doi: 10.1097/01.chi.0000135622.05219.bf [DOI] [PubMed] [Google Scholar]
- 4.Nikkelen SW, Valkenburg PM, Huizinga M, Bushman BJ. Media use and ADHD-related behaviors in children and adolescents: a meta-analysis. Dev Psychol. 2014;50(9):2228-2241. doi: 10.1037/a0037318 [DOI] [PubMed] [Google Scholar]
- 5.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700-707. doi: 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barkley RA. Attention-Deficit Hyperactivity Disorder: A Clinical Workbook. 2nd ed New York, NY: Guilford Press; 1998. [Google Scholar]
- 7.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed, Text Revision Washington, DC: American Psychiatric Publishing; 2004. [Google Scholar]
- 8.Adler LA, Shaw DM, Spencer TJ, et al. Preliminary examination of the reliability and concurrent validity of the attention-deficit/hyperactivity disorder self-report scale v1.1 symptom checklist to rate symptoms of attention-deficit/hyperactivity disorder in adolescents. J Child Adolesc Psychopharmacol. 2012;22(3):238-244. doi: 10.1089/cap.2011.0062 [DOI] [PubMed] [Google Scholar]
- 9.Sonnby K, Skordas K, Olofsdotter S, Vadlin S, Nilsson KW, Ramklint M. Validation of the World Health Organization Adult ADHD Self-Report Scale for adolescents. Nord J Psychiatry. 2015;69(3):216-223. doi: 10.3109/08039488.2014.968203 [DOI] [PubMed] [Google Scholar]
- 10.Sibley MH, Pelham WE, Molina BS, et al. The delinquency outcomes of boys with ADHD with and without comorbidity. J Abnorm Child Psychol. 2011;39(1):21-32. doi: 10.1007/s10802-010-9443-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Connor DF, Edwards G, Fletcher KE, Baird J, Barkley RA, Steingard RJ. Correlates of comorbid psychopathology in children with ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42(2):193-200. doi: 10.1097/00004583-200302000-00013 [DOI] [PubMed] [Google Scholar]
- 12.Yen J-Y, Ko C-H, Yen C-F, Wu H-Y, Yang M-J. The comorbid psychiatric symptoms of Internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia, and hostility. J Adolesc Health. 2007;41(1):93-98. doi: 10.1016/j.jadohealth.2007.02.002 [DOI] [PubMed] [Google Scholar]
- 13.Elia J, Ambrosini P, Berrettini W. ADHD characteristics, I: concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2(1):15. doi: 10.1186/1753-2000-2-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson MP, Ho CH, Kingree JB. Prospective associations between delinquency and suicidal behaviors in a nationally representative sample. J Adolesc Health. 2007;40(3):232-237. doi: 10.1016/j.jadohealth.2006.10.016 [DOI] [PubMed] [Google Scholar]
- 15.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149-166. doi: 10.1007/BF01537606 [DOI] [PubMed] [Google Scholar]
- 16.Muthén LK, Muthén BO. Mplus, Statistical Analysis With Latent Variables Version Los Angeles, CA: Unviersity of California; 2007;3.
- 17.Vittinghoff E, Glidden DV, Shiboski SC, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models. New York, NY: Springer Science & Business Media; 2011. [Google Scholar]
- 18.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289-300. [Google Scholar]
- 19.Zheng F, Gao P, He M, et al. Association between mobile phone use and inattention in 7102 Chinese adolescents: a population-based cross-sectional study. BMC Public Health. 2014;14(1):1022. doi: 10.1186/1471-2458-14-1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.George MJ, Russell MA, Piontak JR, Odgers CL. Concurrent and subsequent associations between daily digital technology use and high-risk adolescents’ mental health symptoms. Child Dev. 2018;89(1):78-88. doi: 10.1111/cdev.12819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palmonari A, Pombeni ML, Kirchler E. Peergroups and evolution of the self-system in adolescence. Eur J Psychol Educ. 1989;4(1):3. doi: 10.1007/BF03172757 [DOI] [Google Scholar]
- 22.Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann N Y Acad Sci. 2004;1021(1):77-85. doi: 10.1196/annals.1308.009 [DOI] [PubMed] [Google Scholar]
- 23.Szymanski K, Sapanski L, Conway F. Trauma and ADHD–association or diagnostic confusion? a clinical perspective. J Infant Child Adolesc Psychother. 2011;10(1):51-59. doi: 10.1080/15289168.2011.575704 [DOI] [Google Scholar]
- 24.Moffitt TE, Houts R, Asherson P, et al. Is adult ADHD a childhood-onset neurodevelopmental disorder? evidence from a four-decade longitudinal cohort study. Am J Psychiatry. 2015;172(10):967-977. doi: 10.1176/appi.ajp.2015.14101266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caye A, Rocha TB-M, Anselmi L, et al. Attention-deficit/hyperactivity disorder trajectories from childhood to young adulthood: evidence from a birth cohort supporting a late-onset syndrome. JAMA Psychiatry. 2016;73(7):705-712. doi: 10.1001/jamapsychiatry.2016.0383 [DOI] [PubMed] [Google Scholar]
- 26.Agnew-Blais JC, Polanczyk GV, Danese A, Wertz J, Moffitt TE, Arseneault L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry. 2016;73(7):713-720. doi: 10.1001/jamapsychiatry.2016.0465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White JD. Personality, temperament and ADHD: a review of the literature. Pers Individ Dif. 1999;27(4):589-598. doi: 10.1016/S0191-8869(98)00273-6 [DOI] [Google Scholar]
- 28.Gentile DA, Swing EL, Lim CG, Khoo A. Video game playing, attention problems, and impulsiveness: evidence of bidirectional causality. Psychol Pop Media Cult. 2012;1(1):62. doi: 10.1037/a0026969 [DOI] [Google Scholar]
- 29.Johnston C, Mash EJ, Miller N, Ninowski JE. Parenting in adults with attention-deficit/hyperactivity disorder (ADHD). Clin Psychol Rev. 2012;32(4):215-228. doi: 10.1016/j.cpr.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Padilla-Walker LM, Coyne SM, Fraser AM, Dyer WJ, Yorgason JB. Parents and adolescents growing up in the digital age: latent growth curve analysis of proactive media monitoring. J Adolesc. 2012;35(5):1153-1165. doi: 10.1016/j.adolescence.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 31.Smith VC, Wilson CR; Committee on Substance Use and Prevention . Families affected by parental substance use. Pediatrics. 2016;138(2):e20161575. doi: 10.1542/peds.2016-1575 [DOI] [PubMed] [Google Scholar]
- 32.Chen Q, Yan Z. Does multitasking with mobile phones affect learning? a review. Comput Human Behav. 2016;54:34-42. doi: 10.1016/j.chb.2015.07.047 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eResults
eFigure 1. Estimated mean prevalence of ADHD symptoms across follow-ups, by baseline modern digital media use frequency index derived from the primary unadjusted logistic regression model
eFigure 2. Cross-lagged model of associations between modern digital media use frequency index and ADHD symptom severity among students at all levels of baseline ADHD symptoms
eTable 1. Sociodemographic characteristics of participating schools in reference to Los Angeles county schools
eTable 2. Number of students with ADHD symptom data available at each follow-up in the primary analytic sample of baseline ADHD symptom-negative students
eTable 3. Sociodemographics of students included in (vs. excluded from) the primary analytic sample and estimated sociodemographics of students eligible to enroll in the cohort
eTable 4. Estimates of internal consistency, stability, and associations of cumulative digital media use index and ADHD symptom status across time points among baseline ADHD symptom-negative students
eTable 5. ADHD symptom prevalence across follow-ups, by baseline cumulative digital media use index score among baseline ADHD symptom-negative students
eTable 6. Regression weights from repeated measures linear regression models testing association with ADHD symptom severity at follow-ups among students at all baseline ADHD symptom levels
eTable 7. Estimates of internal consistency, stability, and associations among modern digital media use and ADHD symptom severity across time points among students at all levels of baseline ADHD symptoms
eReferences