Summary
Multiple subspecialties have implemented courses to teach the fundamentals to new trainees with excellent outcomes. The present study reports the results of a national needs assessment survey of residents and program directors to evaluate the optimal structure of an introductory curriculum for radiation oncology residents and the utility of a 1- to 2-day off-site “boot camp.” Using these data, a pilot introductory radiation oncology curriculum was successfully implemented at 4 programs with plans for expansion and outcome evaluation.
Purpose:
To assess the optimal structure of an introductory curriculum (IC) for radiation oncology residents, including the perceived utility of a 2-day off-site “boot camp,” and evaluate the success of a pilot introductory radiation oncology curriculum (IROC) based on these initial data.
Methods and Materials:
In the first phase, anonymous, web-based surveys were sent to US radiation oncology program directors and residents. Likert-type scores (1, not at all; 5, extremely) are reported as the median and interquartile range. Using the phase 1 results, IROC was developed, piloted, and evaluated.
Results:
Of the 89 program directors and 697 residents, 47 (53%) and 165 (24%) responded, respectively. Of the 89 program directors, 37 (79%) reported offering a formal IC. However, only 83 residents (50%) reported having a formal IC. Program directors reported resident preparation for clinical training as “moderate” (median 3, interquartile range 2–3) on entering residency and “moderate” (median 3, interquartile range 3–4) after IC completion (P = .03). However, residents only believed they were “slightly” prepared (median 2, interquartile range 1–2) on entering residency and “moderately” (median 3, interquartile range 2–3) prepared after IC completion (P < .01). Program directors believed an off-site boot camp would be of “moderate” utility (median 3, interquartile range 3–4) with participation limited by funding (57%). Residents without an IC reported that having an IC would be “quite” beneficial (median 4, interquartile range 3–5). Residents preferred instruction before the clinical training (49%) and over 1 week (40%). Both program directors and residents rated lectures on radiation emergencies and simulation highly. Using these data, IROC was developed and piloted with incoming residents at 4 institutions. After IROC, residents reported improvement in overall preparedness for clinical training (before: median 1, interquartile range 1–2; vs after: median 3, interquartile range 2–3; P < .01) and among specific practice domains.
Conclusions:
Beginning radiation oncology residents frequently lack structured introductory curricula but desire instruction before the clinical training with a focus on practical aspects (emergency management, contouring). Program directors recognize the value of both off-site and on-site boot camps. An on-site IC could mitigate funding barriers. A standardized IC, IROC, piloted at 4 programs, showed promising outcomes. © 2018 Elsevier Inc. All rights reserved.
Introduction
Medical students often receive little formal education in radiation oncology during medical school (1, 2). Future radiation oncology residents complete a 1-year internship; however, only 45% of residents believe that this year improved their skills relevant to radiation oncology (3). Formal radiation oncology training has historically used an apprenticeship-type model, with the potential for tremendous variability in the curriculum. More recently, medical education has shifted toward structured curricular programs and assessments (eg, Accreditation Council for Graduate Medical Education Milestones initiative) (4). Therefore, it is important that radiation oncology training programs also investigate the benefit of a standardized curriculum. Other medical subspecialties have addressed deficiencies by implementing short, intensive training courses, often referred to as “boot camps,” to teach new trainees fundamental skills and knowledge before entering regular clinical training (5–12).
The aims of the present study were twofold. First, we aimed to determine the current state of introductory curricula in the United States using a national survey of radiation oncology program directors and residents. The information obtained through this national needs assessment was then used to achieve the second aim: to design, implement, and evaluate a pilot introductory radiation oncology curriculum (IROC) for incoming postgraduate year (PGY)-2 residents. The results of the national survey (phase 1) and pilot IROC (phase 2) are reported.
Methods and Materials
Phase 1: Introductory curriculum and boot camp surveys
Survey development
A contact list of program directors from 89 accredited radiation oncology residency programs was compiled from the American Medical Association FREIDA (Fellowship and Residency Electronic Interactive Database) website as of September 2015. Resident e-mails were compiled through the Radiation Oncology Education Collaborative Study Group by contact with the program directors, coordinators, and residents.
A committee consisting of radiation oncology faculty, 1 radiation oncology resident, and 1 medical student developed an anonymous, Internet-based survey, one for program directors and one for current radiation oncology residents. The Research Electronic Data Capture (REDCap) platform, hosted at the University of Chicago and Virginia Commonwealth University, was used to collect and manage the study data (13). REDCap is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources. Branching logic was used; therefore, the total question number varied for each individual.
Both surveys (Appendixes E1 and E2; available online at www.redjournal.org) included questions in 3 main areas: general preparedness (or perception of preparedness) of residents at training start and after introductory curricula, the timing and components of the introductory curriculum, and the need for, and logistics of, implementing a 2-day geographically centralized (to include programs in reasonable proximity) radiation oncology boot camp. The resident survey also included questions regarding formal radiation oncology didactic instruction before the residency and completion of radiation oncology clerkships during medical school. Demographic information was collected from both groups.
Using this web-based survey, 89 program directors and 697 residents were contacted on September 2, 2015, and November 14, 2016, respectively. The program director and resident surveys remained open until September 21, 2015, and December 2, 2016, respectively, each with 2 weekly reminder e-mails sent. The surveys were estimated to require 15 to 20 minutes to complete, and responses could be saved for later completion. Only completed surveys were used in the data analysis (3 resident surveys were incomplete). One PGY-1 resident completed the survey and was excluded from the analysis.
Phase 2: IROC curriculum development
The design of IROC followed the 6-step model for medical education curriculum development. These include (1) problem identification and general needs assessment; (2) targeted needs assessment; (3) goals and objectives; (4) education strategies; (5) implementation; and (6) evaluation and feedback (14). As detailed in the first phase, a targeted needs assessment was performed among both radiation oncology residents and residency program directors to characterize the perspective of each group. Using the targeted needs assessment data, goals and specific objectives were developed, and a structured introductory pilot curriculum consisting of 7 discrete educational sessions was designed to address each learning objective. A web-based survey assessment was also created to evaluate the efficacy of IROC.
In July 2017, using a multi-institutional collaborative model previously implemented to develop and evaluate a standardized curriculum for radiation oncology medical students (15–17), IROC was piloted for all incoming PGY-2 radiation oncology residents at 4 academic medical centers that participate in the Radiation Oncology Education Collaborative Study Group (ROECSG; available at: https://roecsg.uchicago.edu/) (18). To ensure the consistency of the curriculum across institutions, each participating institution delivered all 7 sessions using a preprepared PowerPoint presentation without supplementary educational lectures in a period limited to the first 2 weeks of the residency year. Additionally, didactics were reviewed in advance by all lecturers, and speaking notes were provided when appropriate to ensure uniformity during interactive components. Lecturers included radiation oncology faculty, senior residents, and dosimetrists.
On completion of IROC, all participating residents completed an anonymous computer-based survey of the curriculum to assess their preferred learning style, baseline ease with the components of clinical radiation oncology, and satisfaction with the content of the IROC curriculum. Free text and Likert-type score responses were used. The evaluation was distributed by each site’s course director. All responses were collected within 4 weeks of the initiation of the training year to minimize recall bias.
Statistical analysis
For both study phases, questions of resident preparedness and curriculum/boot camp utility were assessed using a Likert-type scale (1, not at all; 2, somewhat/slightly; 3, moderately; 4, quite; and 5, extremely), with additional yes/no and free-response questions. Likert-type results are reported as the median and interquartile range. Data were analyzed using parametric and nonparametric statistics with JMP Pro, version 11 (SAS Institute, Cary, NC) and Stata, version 14.0 (Stata-Corp, College Station, TX). Free text responses for the phase 1 survey and IROC evaluations were independently reviewed by two physicians for the needs assessment (JRG and AP) and the pilot implementation of IROC (RBJ and ECF), respectively. Overlapping themes were reported. Exemption for phase 1 was obtained from the University of Chicago institutional review board, and exemption for phase 2 was obtained from the Virginia Commonwealth University institutional review boards.
Results
Phase 1: National needs assessment for introductory curriculum and boot camp
Of the 697 residents and 89 program directors, 165 (24%) and 47 (53%) responded to the full survey, respectively (Table 1). Of the responding residents, 76 (46%) had completed 3 medical school radiation oncology clerkships and 131 (79%) had ≤3 hours of formal radiation oncology instruction before their residency. Of the 47 responding program directors, 37 (79%) reported offering formal introductory curriculum; however, only 50% of residents reported participating in an introductory curriculum (P < .01). Residents who reported having an introductory curriculum built into their residency training program reported being “slightly” (median 2, interquartile range 1–2) prepared before their introductory curriculum compared with “moderately” prepared (median 3, interquartile range 2–3) afterward (P < .01) and reported a “moderate” benefit from the curriculum (median 3, interquartile range 2–4; Table 2). Residents without an introductory curriculum reported that an introductory curriculum would be “quite” beneficial (median 4, interquartile range 3–5).
Table 1.
Demographic information for residents and program directors
| Variable | Residents (n = 165) |
Program directors (n = 47) |
|---|---|---|
| PGY in training | NA | |
| 2 | 56 (34) | |
| 3 | 43 (26) | |
| 4 | 32 (19) | |
| 5 | 34 (21) | |
| Residents in program (n) | ||
| 1–4 | 11 (7) | 5 (11) |
| 5–8 | 61 (37) | 21 (45) |
| 9–12 | 52 (32) | 12 (26) |
| 13–16 | 29 (18) | 6 (13) |
| ≥17 | 12 (7) | 3 (6) |
| Exposure to RO during intern year | ||
| Yes | 4 (21) | 3 (27) |
| No | 15 (79) | 8 (73) |
Abbreviations: PGY Z postgraduate year; RO Z radiation oncology.
Data presented as n (%).
Table 2.
Preparedness for training and introductory curriculum
| Residents | Program directors | P value | ||
|---|---|---|---|---|
| Question | Value | Question | Value | |
| PGY-2 residents are prepared to function as a radiation oncology resident on July 1 | 2 (1–2) | PGY-2 residents are prepared to function as a radiation oncology resident on July 1 | 3 (2–3) | <.01 |
| Program has formal introductory curriculum | Program has formal introductory curriculum | <.01 | ||
| Yes | 83 (50) | Yes | 37 (79) | |
| No | 82 (50) | No | 10 (21) | |
| Optimal timing for curriculum | Timing for curriculum* | NA | ||
| Before any clinic | 81 (49) | Before any clinic | 18 (38) | |
| While active in clinic | 69 (42) | While active in clinic | 22 (47) | |
| Other | 15 (9) | Other | 7 (15) | |
| Optimal length of curriculum | NA | NA | NA | |
| 1d | 12 (7) | |||
| 1 wk | 66 (40) | |||
| 2 wk | 23 (14) | |||
| 1 mo | 21 (13) | |||
| First 6 mo | 19 (12) | |||
| First 12 mo | 17 (10) | |||
| Other | 7 (4) | |||
| Residents with curriculum | 83 | Programs with curriculum | 37 | |
| On completion, resident prepared for clinic | 3 (2–3) | On completion, resident prepared for clinic | 3 (3–4) | <.01 |
| Perceived benefit from formal curriculum | 3 (2–4) | Measure curriculum efficacy (yes; no) | 7 (19); 30 (81) | |
| Residents without curriculum | 82 | NA | ||
| Perceived benefit from formal curriculum | 4 (3–5) | NA | ||
| NA | NA | Length of curriculum (for 18 programs before clinic) | NA | |
| 1d | 4 (22) | |||
| 1 wk | 8 (44) | |||
| 2 wk | 3 (17) | |||
| 1 mo | 1 (6) | |||
| Other | 2 (11) | |||
| Length of curriculum (for 22 programs during clinic) | NA | |||
| >1 mo | 13 (59) | |||
| First 6 mo | 1 (5) | |||
| Throughout first year | 8 (36) | |||
Abbreviations: NA Z not applicable; PGY-2 Z postgraduate year 2.
Data presented as median (interquartile range) using the Likert-type scale (1, not at all; 2, slightly; 3, moderately; 4, quite; 5, extremely) or n (%).
Due to survey error, all programs directors (with and without curriculum) were asked about the timing of the curriculum.
Program directors reported initial resident preparation for clinical training as “moderate” (median 3, interquartile range 2–3) compared with resident reports of being “slightly” (median 2, interquartile range 1–2) prepared (P < .01). Program directors reported resident preparation for clinical training after completion of an introductory curriculum as “moderate” (median 3, interquartile range 3–4) with improvement in preparedness after the introductory curriculum (vs before the introductory curriculum; P = .03).
Residents and program directors reported that a radiation oncology boot camp would be “quite” (median 4, interquartile range 3–5) and “moderately” (median 3, interquartile range 3–4) useful, respectively (Table 3), with most (56% and 57%, respectively) citing funding as a limiting factor to participation. The top preferences for the curriculum topics for both residents and program directors included lectures on simulation and patient setup and management of radiation emergencies (Table 4).
Table 3.
Boot camp evaluation
| Question | Program | ||
|---|---|---|---|
| Residents | directors | P value | |
| Utility of RO boot camp | 4 (3–5) | 3 (3–4) | .11 |
| Missing 1 clinic day allowed? | <.01 | ||
| Yes | 158 (96) | 38 (81) | |
| No | 7 (4) | 9 (19) | |
| Provide funding for travel? | NA | ||
| Yes | 20 (43) | ||
| No | 27 (57) | ||
| Level of funding | NA | ||
| Driving costs (<50 miles) | 6 (30) | ||
| Driving costs (50–200 miles) | 7 (35) | ||
| Airfare costs (>200 miles) | 7 (35) | ||
| Willingness to travel | NA | ||
| With funding | |||
| <50 miles | 21 (13) | ||
| 50–250 miles | 31 (19) | ||
| > 250 miles | 113 (68) | ||
| Without funding | |||
| <50 miles | 126 (76) | ||
| 50–250 miles | 31 (19) | ||
| > 250 miles | 8 (5) | ||
| Limit boot camp attendance | |||
| Missed clinic time | 49 (30) | 3 (6) | |
| Redundant educational activities |
20 (12) | 13 (28) | |
| Travel costs | 92 (56) | 27 (57) | |
| Other | 4 (2) | 4 (9) | |
Abbreviations: NA Z not applicable; RO Z radiation oncology. Data presented as median (interquartile range) using the Likert-type scale (1, not at all; 2, slightly; 3, moderately; 4, quite; 5, extremely) or n (%).
Table 4.
Components of an effective introductory curriculum/boot camp
| Component | Residents | Program directors | P value | ||
|---|---|---|---|---|---|
| Would incorporate component as part of IC |
Perceived need for component as part of boot camp (of 100) |
Includes component as part of IC |
Perceived need for component as part of boot camp (of 100) |
||
| Lecture on simulations/patient setup* | 77 (47) | 79 ± 22 | 30 (64) | 69 ± 25 | .02 |
| Lecture on management of radiation emergencies* | 76 (46) | 79 ± 23 | 35 (74) | 76 ± 22 | .40 |
| Lecture on treatment planning/dosimetry* | 68 (41) | 71 ± 25 | 29 (62) | 65 ± 23 | .18 |
| Hands-on workshop on contouring normal structures* | 67 (41) | 73 ± 28 | 16 (34) | 64 ± 26 | .06 |
| Hands-on workshop on contouring a target volume* | 66 (40) | 74 ± 27 | 15 (32) | 59 ± 26 | <.01 |
| Hands-on workshop on treatment planning* | 63 (38) | 71 ± 26 | 19 (40) | 61 ± 25 | .02 |
| Hands-on workshop on image-guidance tools* | 51 (31) | 62 ± 26 | 8 (17) | 51 ± 25 | .01 |
| Hands-on emergency monitor unit calculation | 44 (27) | 57 ± 32 | 14 (30) | 65 ± 27 | .10 |
| Lecture(s) on clinical disease sites (eg, breast, lung, prostate) | 28 (17) | 42 ± 29 | 13 (28) | 26 ± 21 | <.01 |
| Lecture(s) on radiation physics | 26 (16) | 47 ± 28 | 20 (43) | 51 ± 25 | .29 |
| Lecture(s) on radiation biology | 21 (13) | 38 ± 26 | 12 (26) | 43 ± 24 | .21 |
| Hands-on workshop on brachytherapy implants | 19 (12) | 40 ± 28 | 0 (0) | 32 ± 21 | .04 |
| Other | 4 (2) | NA | 3 (6) | NA | - |
| Lecture(s) on communication | NA | 34 ± 29 | NA | 46 ± 24 | <.01 |
| Lecture(s) on breaking bad news | NA | 37 ± 28 | NA | 47 ± 24 | .01 |
Abbreviations: IC Z introductory curriculum; NA Z not asked.
Data presented as n (%) or mean standard deviation.
Component incorporated into introductory radiation oncology curriculum.
Additional qualitative data were also analyzed. The residents advocated for introductory materials presented as basic instruction before the clinic with continuing introductory curricula intermixed during their clinical responsibilities. In additional survey comments, a web-based or virtual boot camp was suggested to decrease the resources required. Many respondents questioned possible information overload and commented that “on the job” training is also necessary. Respondents also noted that institution-specific information would be difficult to address at a centralized boot camp.
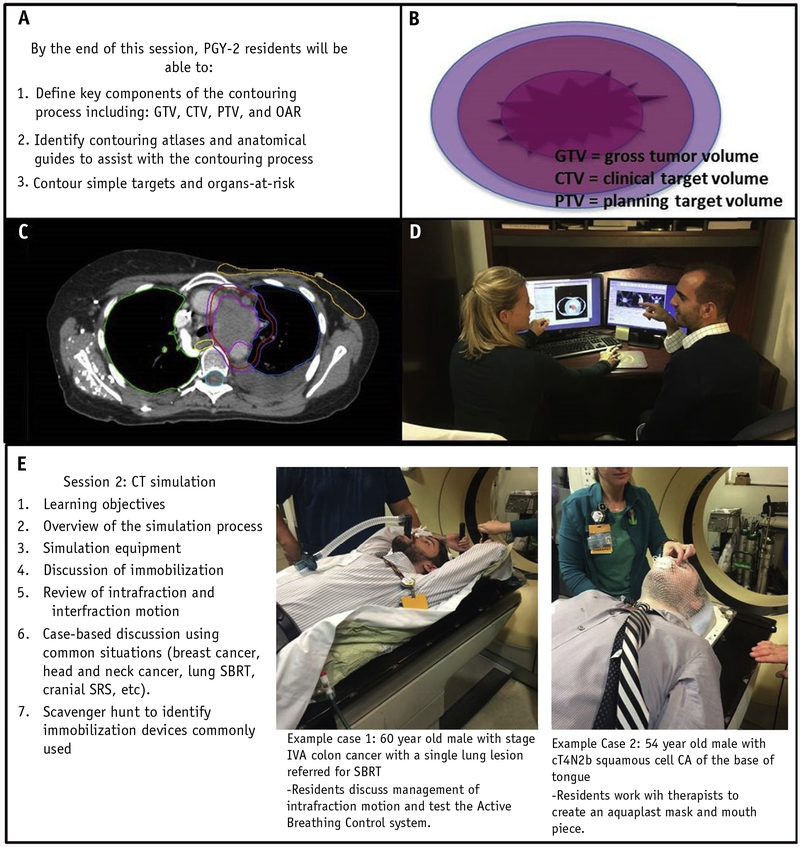
Phase 2: IROC implementation
The IROC consisted of 7 didactic sessions, ranging from 30 minutes to 2 hours in length: (1) overview of radiation oncology, including treatment workflow and frequently used radiation abbreviations; (2) patient simulation, including immobilization methods; (3) contouring; (4) plan evaluation; (5) quality assurance; (6) treatment delivery, including the composition of a linear accelerator, patient positioning, port films, and cone beam computed tomography; and (7) management of radiation oncology emergencies. These sessions were chosen based on the most highly rated components in the national needs assessment (Table 4). Specific objectives were identified and reviewed before each session (Table 5; Fig. 1). All sessions incorporated a slide-based lecture component to ensure consistency of content and a hands-on component to stimulate learner engagement and retention. For example, the third session focused on contouring and included a brief, image-rich lecture to define the basic components of a contour set (ie, gross tumor volume, clinical target volume, planning target volume) with an opportunity for residents to contour on a computed tomography image set and receive feedback. After the lecture, an interactive session was facilitated in which each resident sat at a computer and was guided through a contouring case using each institution’s treatment planning system. All sessions were designed by the faculty members and program director or assistant program directors of the residency training program with input from physicists, dosimetrists, and other clinicians, as appropriate.
Table 5.
Goals, objectives, and resident ratings of IROC didactic sessions
| Session | Title (duration) | Goals and objectives: By session end, PGY-2 residents will be able to |
How useful is knowledge presented in this session? |
How useful are skills presented in this session? |
How useful is this session to orient you to RO? |
|---|---|---|---|---|---|
| 1 | Radiation oncology overview (30 min) | Understand basics of RT and role of radiation oncologist in patient care; explain general work flow required for a patient to start RT | 4 (4–5) | 4 (3.5–4.5) | 5 (4–5) |
| 2 | Simulation (2 h) | Understand simulation process; identify common immobilization devices and how they are used; understand difference between inter- and intrafraction target motion; describe an isocenter and how it is established | 5 (4.5–5) | 5 (4–5) | 5 (4–5) |
| 3 | Contouring (2 h) | Define key components of contouring process, including GTV, CTV, PTV, and OARs; identify contouring atlases and anatomic guides to assist with contouring process; contour simple targets and OARs | 5 (4–5) | 5 (4–5) | 5 (4–5) |
| 4 | Plan evaluation (2 h) | Describe role of physician in plan generation, development, and review; understand components of a thorough plan evaluation using CB-CHOP method; evaluate simple plans | 5 (4–5) | 5 (4–5) | 5 (4–5) |
| 5 | QA/physics (30 min) | Describe purpose of QA; understand general frequency of QA processes; identify special treatment procedures that require additional QA and tools that can be used; calculate MUs for basic treatment | 5 (4–5) | 4 (3.5–5) | 5 (4–5) |
| 6 | Treatment setup and delivery (1 h) | Identify components of linear accelerator, including treatment table, gantry, collimator, and imaging panels; recognize major uses and differences between on-board imaging techniques, including megavoltage, kilovoltage, and cone beam CT | 4.5 (4–5) | 5 (4.25–5) | 5 (4–5) |
| 7 | Radiation oncology emergencies (45 min) | Recognize common radiation oncology emergencies; compose basic questions needed to communicate with referring providers in emergency situations; develop a basic understanding of how RT should be used in emergency situations | 5 (4.5–5) | 5 (4–5) | 5 (4.5–5) |
Abbreviations: CB-CHOP Z contours, beams, coverage, heterogeneity, OARs, prescription; CTV Z clinical tumor volume; GTV Z gross tumor volume; IROC Z introductory radiation oncology curriculum; MU Z monitor unit; OARs Z organs at risk; PGY-2 Z postgraduate year 2; PTV Z planning tumor volume; QA Z quality assurance; RO Z radiation oncology; RT Z radiation therapy.
Data presented as median (interquartile range) using the Likert-type scale (1, not at all; 2, slightly; 3, moderately; 4, quite; 5, extremely).
Fig. 1.
(A) Goals and objectives for contouring session. (B, C) Images from lecture component defining gross tumor volume, clinical target volume, and planning target volume. (D) Interactive contouring session. (E) Simulation session with interactive resident participation.
Fifteen residents completed the IROC and completed the postcurriculum evaluation. Twelve nonparticipating training programs consisting of a total of 32 PGY-2 residents received the postintroductory curriculum survey, with 15 of the 32 residents (47%) completing it. Both groups expressed a preference for visual and hands-on learning (each group, 11 of 15 [68.8%]).
Before the orientation curriculum, residents reported being “not at all” prepared (median 1, interquartile range 1–2) prepared for clinical training. After completion of IROC, residents reported being “moderately” prepared (median 3, interquartile range 2–3; P < .01).
All sessions were evaluated by the participants and rated as useful on a Likert-type scale (Table 5). In addition, IROC participants reported that they expected the introductory curriculum would “moderately” help them work independently as a resident (median 3, interquartile range 2.5–3). The Likert-type scores of preparedness associated with each didactic session topic improved significantly after participation in the IROC (Table 6). In the qualitative responses, the IROC residents requested more hands-on time with contouring and plan evaluation and access to IROC materials to review during their clinical training.
Table 6.
Resident pre- and post-IROC subjective evaluations
| Question | Pre-IROC evaluation score | Post-IROC evaluation score | P value |
|---|---|---|---|
| How well did you understand the role of RO? | 3 (2–3) | 4 (3–4) | <.01 |
| How prepared are you to attend simulation? | 1 (1–2) | 3 (2–3) | <.01 |
| How prepared are you to contour? | 2 (1–2) | 2 (2–3) | <.01 |
| How prepared are you to evaluate a plan? | 1 (1–2) | 2 (2–3) | <.01 |
| How prepared are you to evaluate a port film? | 1 (1–2) | 2 (1–3) | <.01 |
| How prepared are you to write a prescription? | 1 (1–1) | 2 (1–2) | <.01 |
Abbreviations: IROC Z introductory radiation oncology curriculum; RO Z radiation oncology.
Data presented as median (interquartile range) using the Likert-type scale (1, not at all; 2, slightly; 3, moderately; 4, quite; 5, extremely).
Discussion
Residents receive variable amounts of formalized instruction pertaining to radiation oncology during medical school or internship. Formalized radiation oncology exposure during medical school has been successfully achieved with a structured didactic curriculum for the radiation oncology clerkship (16, 17, 19), existing core radiology clerkships (20), and second-year medical school curriculum (21). However, the results of our national survey demonstrated that many radiation oncology residents believe they are underprepared at the start of residency training, and program directors reported only moderate resident preparedness for clinical responsibilities before and after the introductory curricula currently in use. Our national survey also demonstrated that beginning radiation oncology residents desire a formalized introductory curriculum, and both residents and program directors value instruction on practical topics. Development of a centralized boot camp could be effective, although residents and program directors cited funding as a barrier to participation.
Multiple medical subspecialties have successfully implemented boot camps at the medical school (6–9), residency (10, 11), and fellowship (12) training levels. A previous national survey assessed the efficacy of current radiation oncology resident orientations (22), with only 11.3% of respondents reporting that their orientation was essential. The Stanford residency program developed a formalized PGY-2 curriculum (four 2-hour sessions, once weekly) and reported it to be either very (50%) or extremely (50%) useful (23). A Canadian boot camp for radiation oncology residents showed improvement in quantitative and qualitative contouring outcomes (24). These previous reports and the survey results we have reported suggest that radiation oncology residents should receive a structured introductory curriculum early in their training.
Challenges are associated with implementation of an off-site boot camp. Financial support for travel and accommodations is required. Other subspecialty boot camps have been sponsored by industry, and this option could be explored for radiation oncology. Alternatively, both residents and program directors suggested a virtual boot camp to reduce resource requirements, although some activities are better experienced in a hands-on format (eg, demonstrations of patient simulation). The concerns expressed regarding “information overload” could be mitigated by an initial introduction to general radiation oncology principles during the boot camp that would be built on with subsequent educational activities interspersed throughout the early residency using a standardized curriculum. In terms of boot camp curriculum, practical topics such as emergency management, treatment planning, and contouring were valued by both residents and program directors and should be considered by all residency programs for incorporation into current individualized clinic orientations and introductory curricula.
The reported national needs assessment data are unique in that they allow for comparisons of resident and program director opinions on current introductory educational resources. The data are limited by the moderate response rate, typical survey biases, and limitations in direct comparisons of resident and program director opinions because the respondents were not necessarily from the same training programs.
These results subsequently provided a data-driven design for the IROC curriculum, with the goal of using a structured introductory curriculum at a resident’s home institution to obviate the resource and time commitments necessary for an off-site boot camp and provide a high-quality standardized education. The IROC covered the key concepts of radiation oncology identified in the needs assessment to boost resident clinical preparedness. The IROC, which was successfully piloted at 4 institutions in 2017, had several strengths. First, the didactic sessions were designed to be visual and hands-on, the 2 modes of learning that participating residents reported to be most conducive to their learning. Second, the curriculum was comprehensive, allowing residents to understand many of the components of routine radiation oncology care early in their clinical experience. Third, the sessions were standardized and discrete, permitting training programs to tailor the timing of the educational program to their individual needs.
These efforts resulted in the successful pilot of the IROC. Inherent limitations were present with this pilot program, including the small sample size, the potential variability in teaching style, and inconsistency or nonoptimal timing or order of the sessions. However, the results of the pilot evaluation were positive, suggesting further expansion of the IROC to additional institutions for a more robust evaluation is warranted.
Conclusions
The work we have presented, both the national survey results and the pilot of the IROC, provides valuable information to program directors of radiation oncology residency programs. These results have demonstrated that residents desire formalized introductory curricula. The results also provide direction for further development of a national introductory curriculum using the IROC pilot as a framework. Standardized introductory curricula could significantly affect radiation oncology education by facilitating earlier achievement of Accreditation Council for Graduate Medical Education milestones. The success of the pilot program is encouraging. With the support of Radiation Oncology Education Collaborative Study Group institutions and the assistance of the Association for Directors of Radiation Oncology Programs, the IROC will be expanded to additional radiation oncology programs in 2018. The efficacy and value of any implemented introductory curriculum will need to be carefully evaluated with both qualitative and quantitative measures to guide future introductory curriculum improvements.
Supplementary Material
Acknowledgments
This work was supported in part by the National Institutes of Health (grant UL1 TR000430) and the National Center for Advancing Translational Sciences (award UL1TR000058).
This work was presented in part at the American Society for Radiation Oncology Annual Meeting, San Diego, California, September 24–27, 2017.
Footnotes
Conflict of interest: Dr. Golden reports a financial interest in RadOncQuestions, LLC.
Supplementary material for this article can be found at www.redjournal.org.
References
- 1.Dennis KE, Duncan G. Radiation oncology in undergraduate medical education: A literature review. Int J Radiat Oncol Biol Phys 2010;76: 649–655. [DOI] [PubMed] [Google Scholar]
- 2.Jagadeesan VS, Raleigh DR, Koshy M, et al. A national radiation oncology medical student clerkship survey: Didactic curricular components increase confidence in clinical competency. Int J Radiat Oncol Biol Phys 2014;88:51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker SR, Romero MJ, Geannette C, et al. The value of the internship for radiation oncology training: Results of a survey of current and recent trainees. Int J Radiat Oncol Biol Phys 2009;74:1203–1206. [DOI] [PubMed] [Google Scholar]
- 4.Radiation Oncology Milestones, 2015. 7/2013. Available at: http://www.acgme.org/acgmeweb/portals/0/pdfs/milestones/radiationoncologymilestones.pdf. Accessed September 15, 2017.
- 5.Selden NR, Origitano TC, Burchiel KJ, et al. A national fundamentals curriculum for neurosurgery PGY1 residents: The 2010 Society of Neurological Surgeons boot camp courses. Neurosurgery 2012;70: 971–981. [DOI] [PubMed] [Google Scholar]
- 6.Neylan CJ, Nelson EF, Dumon KR, et al. Medical school surgical boot camps: A systematic review. J Surg Educ 2016;74:384–389. [DOI] [PubMed] [Google Scholar]
- 7.Burns R, Adler M, Mangold K, et al. A brief boot camp for 4th-year medical students entering into pediatric and family medicine residencies. Cureus 2016;8:e488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lamba S, Wilson B, Natal B, et al. A suggested emergency medicine boot camp curriculum for medical students based on the mapping of Core Entrustable Professional Activities to Emergency Medicine Level 1 milestones. Adv Med Educ Pract 2016;7:115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bontempo LJ, Frayha N, Dittmar PC. The internship preparation camp at the University of Maryland. Postgrad Med J 2017;93:8–14. [DOI] [PubMed] [Google Scholar]
- 10.Davidson EH, Barker JC, Egro FM, et al. A national curriculum of fundamental skills for plastic surgery residency: Report of the inaugural ACAPS boot camp. Ann Plast Surg 2017;78:121–126. [DOI] [PubMed] [Google Scholar]
- 11.Esch LM, Bird AN, Oyler JL, et al. Preparing for the primary care clinic: An ambulatory boot camp for internal medicine interns. Med Educ Online 2015;20:29702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ceresnak SR, Axelrod DM, Motonaga KS, et al. Pediatric cardiology boot camp: Description and evaluation of a novel intensive training program for pediatric cardiology trainees. Pediatr Cardiol 2016;37: 834–844. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)da metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas PA, Kern DE, Hughes MT, et al. , editors. Curriculum Development for Medical Education: A Six-Step Approach. 3rd ed. Baltimore: Johns Hopkins University Press; 2016. [Google Scholar]
- 15.Golden DW, Spektor A, Rudra S, et al. Radiation oncology medical student clerkship: Implementation and evaluation of a bi-institutional pilot curriculum. Int J Radiat Oncol Biol Phys 2014;88:45–50. [DOI] [PubMed] [Google Scholar]
- 16.Ye JC, Mohindra P, Spektor A, et al. Medical student perspectives on a multi-institutional clerkship curriculum: A report from the Radiation Oncology Education Collaborative Study Group. Int J Radiat Oncol Biol Phys 2015;92:217–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radiation Oncology Education Collaborative Study Group, Radiation Oncology Education Collaborative Study Group Writing Committee, Golden DW, Braunstein S, Jimenez RB, et al. Multi-institutional implementation and evaluation of a curriculum for the medical student clerkship in radiation oncology. J Am Coll Radiol 2016;13:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radiation Oncology Education Collaborative Study Group. https://roecsg.uchicago.edu. Accessed september 15, 2017.
- 19.Oskvarek JJ, Brower JV, Mohindru P, et al. Educational impact of a structured radiation oncology clerkship curriculum: An interinstitutional comparison. J Am Coll Radiol 2017;14:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hirsch AE, Handal R, Daniels J, et al. Quantitatively and qualitatively augmenting medical student knowledge of oncology and radiation oncology: An update on the impact of the oncology education initiative. J Am Coll Radiol 2012;9:115–120. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal A, Shah A, Shah B, et al. The impact of a radiation oncologist led oncology curriculum on medical student knowledge. J Cancer Educ 2017; 10.1007/s13187-017-1227-2 [e-pub ahead of print]. Accessed september 15, 2017. [DOI] [PubMed] [Google Scholar]
- 22.Diavolitsis VM, Shirazi H, Boyle J, et al. Residents’ educational needs during transition into radiation oncology residency. J Am Coll Radiol 2011;8:785–788. [DOI] [PubMed] [Google Scholar]
- 23.Kumar KA, Chang DT. A pilot curriculum for transitioning radiation oncology residents. Presented at the Stanford Innovations in Medical Education Conference (SIMEC II), May 28, 2016, Palo Alto, CA. [Google Scholar]
- 24.Jaswal J, D’Souza L, Johnson M, et al. Evaluating the impact of a Canadian national anatomy and radiology contouring boot camp for radiation oncology residents. Int J Radiat Oncol Biol Phys 2015;91: 701–707. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.