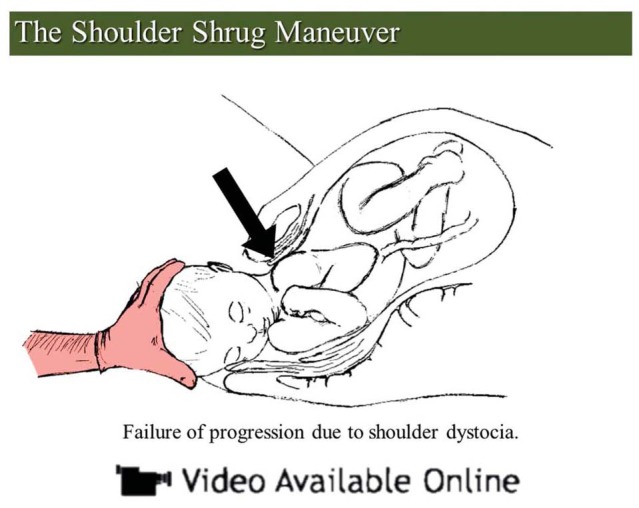
The shoulder shrug maneuver is a simple technique to learn that can aid the obstetrician in the management of shoulder dystocia.
Abstract
BACKGROUND:
Shoulder dystocia is a potential complication of vaginal delivery that increases the chances of injury to the neonate and the mother. The incidence of dystocia can be up to 3%, and sudden presentation and the lack of reliable predictors make shoulder dystocia a challenge for obstetricians.
TECHNIQUE:
The shoulder shrug technique involves shrugging the posterior shoulder and rotating the head–shoulder unit 180 degrees to resolve the shoulder dystocia.
EXPERIENCE:
We describe successful delivery in three cases of persistent shoulder dystocia using the shoulder shrug technique after the dystocia could not be resolved with McRoberts maneuver.
CONCLUSION:
When successful, the shoulder shrug maneuver may decrease the likelihood of morbidity for the neonate. The technique has resolved dystocia in three cases in which the posterior shoulder could be shrugged. Because it does not take much time to perform the shoulder shrug maneuver, it is worth considering this technique during management of unresolved shoulder dystocia.
Shoulder dystocia is a term for an obstetric emergency in which the progression of labor is halted after the delivery of the head. The incidence of shoulder dystocia ranges from 0.2–3%.1,2 It is a poorly predictable event associated with risk factors such as fetal macrosomia, maternal diabetes, previous dystocia, postterm pregnancy, male neonatal gender, and precipitous or prolonged second stage of labor, among others.3–5 Shoulder dystocia can potentially result in injuries to the neonate and the mother.6 Traditionally, shoulder dystocia is managed with McRoberts maneuver, with suprapubic pressure applied to disimpact the anterior shoulder.1 In cases in which shoulder dystocia remains unresolved after that sequence, the shoulder shrug technique can be used as an alternative to manage the dystocia and deliver the neonate. This article presents and discusses three cases of unresolved dystocia successfully managed using the shoulder shrug technique.
TECHNIQUE
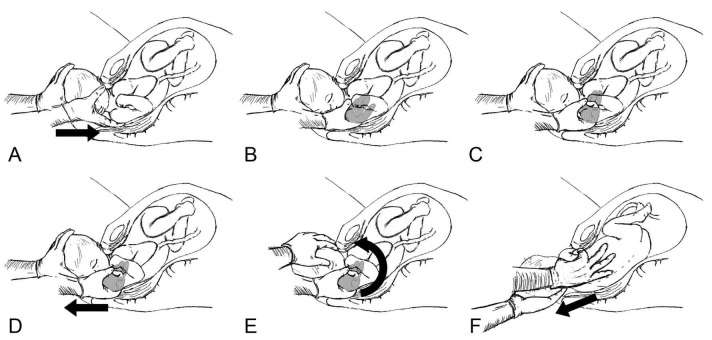
The shoulder shrug technique is a modification of previously described maneuvers that attempt to resolve a shoulder dystocia. The technique is shown in Video 1, available online at http://links.lww.com/AOG/B402. The technique requires the obstetrician to follow certain steps (Fig. 1A–F) to resolve the dystocia:
Grasp the posterior shoulder at the axilla using the obstetrician's thumb and index finger in a pincer grip so that the tips of the thumb and index finger come together in the axillary fossa.
Pull the axilla out toward the head of the neonate to shrug the shoulder and retract the shoulder toward the vaginal opening.
Maintain the pincer grip of the shrugged shoulder and, using the opposite hand, hold the head and retracted shoulder together as a unit
Rotate this unit toward the neonate's face 180 degrees (this will allow the impacted anterior shoulder to roll toward neonate’s chest as it moves toward the posterior position). If unable to rotate toward the face, the opposite direction may be attempted.
As long as the shrugged shoulder remains inferior to the symphysis pubis, it will be deliverable anteriorly.
Now proceed with delivery of the remaining shoulder posteriorly. On rotation, the trapped anterior shoulder should be deliverable posteriorly.
Fig. 1. Failure of progression due to shoulder dystocia. Flex the neck toward the anterior shoulder, then slide hand behind the posterior shoulder (A). Clamp the thumb and index finger around the posterior shoulder (B). With the thumb and index finger, form a pincer grip through the axilla, resembling an “OK” sign (C). Retract the posterior shoulder toward the shrug position (elevation of the shoulder). Arrow represents movement of the posterior shoulder to the shrug position (D). Restore the head toward the body's axis to form the head–shoulder unit and rotate this unit 180 degrees in the direction of the chest. Arrow represents counterclockwise rotation of the head and shoulder unit (E). On rotation, the anterior shoulder is now posterior and has advanced from the dystocia; normal delivery now proceeds with minimal forward traction. Arrow represents delivery of the neonate (F).
Sancetta. Shrug Maneuver for Shoulder Dystocia. Obstet Gynecol 2019.
Video 1. The shoulder shrug maneuver. The video highlights a new technique to facilitate delivery during shoulder dystocia. Video created by Ricardo Leante, MS. Used with permission.
EXPERIENCE
The following three clinical cases involve situations in which McRoberts maneuver and suprapubic pressure failed to resolve shoulder dystocia. We used the technique described above, which was discovered by chance during a difficult delivery. Consents were obtained for all three patients. This case series does not require review and approval under DHHS 45 CFR 46 by the policies of the Baptist Health South Florida institutional review board.
The first patient is a 46-year old woman, G8P6, with a history of six vaginal deliveries, including that of a macrosomic neonate weighing 9 lbs. 5 oz. At 39 weeks of gestation, her spontaneous labor included a 2-hour first stage and a second stage that lasted less than 30 minutes. She delivered the head while the obstetrician was en route to the hospital. Two neonatologists and assisting obstetrics nurses were unable to deliver the neonate using routine maneuvers. On arrival at the hospital, the obstetrician attempted the McRoberts maneuver, which failed, and then proceeded to deliver the posterior arm with traction at the axilla using the thumb and index finger of the right hand. The posterior shoulder was able to be shrugged outward toward the fetal head. Having concern regarding the possibility of fracture of the humerus during extraction of the posterior arm, the head and the shrugged shoulder were held together as a unit that was then rotated 180 degrees counterclockwise. At that point, the posterior shoulder was positioned anterior and inferior to the symphysis pubis and the previously impacted shoulder was posterior. Delivery then proceeded without complication. Apgar scores at 1 and 5 minutes for the neonate were 9 and 9, and birth weight was 10 lbs. 6 oz. The neonate had no injuries. Maternal injury was limited to first-degree tear.
The second patient was a 37-year old woman, G5P2, with a previous successful vaginal birth after cesarean delivery of 9 lb 0 oz neonate. She was at 41 3/7 weeks of gestational age when she was admitted in active labor. Her labor progressed normally, with a 4-hour first stage and an 18-minute second stage. A shoulder dystocia with an anteriorly impacted left shoulder could not be relieved with McRoberts maneuver and suprapubic pressure. The shoulder shrug maneuver of the right shoulder then was performed as described. This enabled the impacted shoulder to be dislodged as it moved posteriorly, and the delivery then was carried out uneventfully. However, it was noted that the rotation was successful only in the clockwise direction. The neonate weight 9 lb 2 oz and was had Apgar scores of 9 and 9 at 1 and 5 minutes. A mild left brachial plexus palsy resolved by the 2-week follow-up visit. This brachial plexus palsy involved the neonate's anterior impacted shoulder.
The third patient was a 28-year old woman, G3P2, who had a history of shoulder dystocia with her second delivery. She underwent induction of labor at 41 3/7 weeks of gestation. She had cervical ripening with Foley bulb technique, followed by induction with Pitocin. Her first stage was 10 hours, and her second stage was 2 minutes. McRoberts maneuver and suprapubic pressure were attempted but were unsuccessful in relieving a shoulder dystocia. The shoulder shrug maneuver was completed, with delivery without complications. Apgar scores for the neonate were 9 and 9 at 1 and 5 minutes, and birth weight was 9 lb 14 oz. Maternal injury consisted of second-degree tear, which was repaired. The neonate had no injuries.
DISCUSSION
Historically, maneuvers for management of shoulder dystocia were introduced through articles in the literature and at conferences. Woods7 maneuver was described in 1942, in which a screw-like rotation maneuver was presented to alleviate the need for excessive traction to the head during delivery, in an attempt to reduce the likelihood of brachial plexus palsy and facilitate delivery. This technique uses a rotation inside the anatomic structures of the symphysis pubis, sacral promontory, and coccyx while simultaneously applying downward external pressure on the neonate's buttock. In 1964, Rubin's8 maneuver was introduced and showed a method to reduce the transverse diameter of the shoulder. In the Rubin's maneuver, finger pressure is directed on the posterior aspect of both anterior and posterior shoulders in an effort to adduct the shoulder toward the chest, thereby reducing the overall circumference of the shoulder to allow delivery. Unfortunately, these techniques do not always work and often simply replace the position of the two shoulders, which still remain behind the symphysis pubis, leaving the dystocia unresolved. Additionally, these two maneuvers have been associated with higher rates of injury in large cohort studies.6,9
The McRoberts maneuver was introduced in 1983, involving maternal repositioning, and is currently accepted as the initial maneuver for management of shoulder dystocia.10 The American College of Obstetricians and Gynecologists’ current recommendation is to start with McRoberts maneuver and suprapubic pressure, with a success rate of 24–62%.9,11 If unsuccessful, an empiric management proceeds to delivery of the posterior shoulder as secondary maneuver.12 This is successful in about 84% of cases.6,13 Another useful technique includes the Zavanelli maneuver, which, when performed promptly after failed initial procedures, has a high success rate.14–16
Current data indicate that the total rate of neonatal injury from shoulder dystocia is around 5.2%; most of these are brachial plexus, humerus, and clavicle injuries, which increase morbidity yet commonly resolve without long-term sequelae.6,17 When faced with a shoulder dystocia that fails to resolve after the McRoberts maneuver with suprapubic pressure sequence, it is important to proceed with an alternative that reduces neonatal and maternal injury. Delivery of the posterior arm is a possible maneuver, yet it requires that the neonate's hand be accessible to sweep across the chest. This can be very difficult in large neonates or with constricted maternal anatomy.18 Also, aggressive attempts during this process can lead to humeral or clavicular fractures. Although this will allow for delivery, it is not an ideal outcome. Conversely, the shoulder shrug technique advances the posterior shoulder to the introitus, reducing the transverse diameter of the shoulders, and the posterior hand is not manipulated. As well, by moving the posterior shoulder and head as a single unit, additional traction forces on the brachial plexus are avoided. Once the head–shoulder unit is rotated 180 degrees, the delivery proceeds rapidly, without the need to completely deliver the posterior arm.
The requirement of this technique is a posterior shoulder that is capable of being shrugged inferiorly toward the neonate's head. Special attention is paid to minimizing stretch of the brachial plexus. The shrugged shoulder should have no stretch whatsoever because the direction of traction is toward the head. If rotation of the unit is toward the neonate's face, as recommended, the anterior impacted shoulder would move toward the neonate's chest during rotation and, likewise, would not have significant traction on the brachial plexus. In addition, the shoulders would be adducted, hence reducing the transverse diameter to aid delivery.8
In certain circumstances, the posterior shoulder can be trapped by the sacral promontory and not able to be shrugged. In the author's experience, in two cases (not discussed in this article) in which this has occurred, return to McRoberts maneuver resulted in delivery of the anterior shoulder. Perhaps, in these circumstances, the angle of the anterior shoulder is in a more favorable position for delivery.
The shoulder shrug maneuver is a technique that can be added to any obstetrician's management of shoulder dystocia. Because the maneuver involves only the obstetrician's hands and no use of additional tools, it can be easily learned during simulation training and used during cases of dystocia.1
Footnotes
Department of Obstetrics and Gynecology, Baptist Hospital of Miami, Miami, Florida; St. George's University, Great River, New York; and Ross University School of Medicine, Miramar, Florida.
Financial Disclosure The authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/B387.
REFERENCES
- 1.Shoulder dystocia. Practice Bulletin No. 178. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e123–68. [DOI] [PubMed] [Google Scholar]
- 2.Mehta SH, Sokol RJ. Shoulder dystocia: risk factors, predictability, and preventability. Semin Perinatol 2014;38:189–93. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie IZ, Shah M, Lean K, Dutton S, Newdick H, Tucker DE. Management of shoulder dystocia: trends in incidence and maternal and neonatal morbidity. Obstet Gynecol 2007;110:1059–68. [DOI] [PubMed] [Google Scholar]
- 4.Ouzounian JG, Gherman RB. Shoulder dystocia: are historic risk factors reliable predictors? Am J Obstet Gynecol 2005;192:1933–5. [DOI] [PubMed] [Google Scholar]
- 5.Fetal macrosomia. Practice Bulletin No. 173. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;128:e195–209. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman MK, Bailit JL, Branch DW, Burkman RT, Van Veldhusien P, Lu L, et al. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Obstet Gynecol 2011;117:1272–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woods CE. A principle of Physics as applicable to shoulder delivery. Am J Obstet Gynecol 1943;45:796–804. [Google Scholar]
- 8.Rubin A. Management of shoulder dystocia. JAMA 1964;189:835–7. [DOI] [PubMed] [Google Scholar]
- 9.Spain JE, Frey HA, Tuuli MG, Colvin R, Macones GA, Cahill AG. Neonatal morbidity associated with shoulder dystocia maneuvers. Am J Obstet Gynecol 2015;212:353.e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonik B, Stringer CA, Held B. An alternate maneuver for management of shoulder dystocia. Am J Obstet Gynecol 1983;145:882–4. [DOI] [PubMed] [Google Scholar]
- 11.Lok ZLZ, Cheng YKY, Leung TY. Predictive factors for the success of McRobert's manoeuvre and suprapubic pressure in relieving shoulder dystocia: a cross-sectional study. BMC Pregn Childbirth 2016;16:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM. Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol 2006;195:657–72. [DOI] [PubMed] [Google Scholar]
- 13.Gilstrop M, Hoffman MK. An update on the acute management of shoulder dystocia. Clin Obstet Gynecol 2016;59:813–19. [DOI] [PubMed] [Google Scholar]
- 14.Sandberg EC. The Zavanelli maneuver: a potentially revolutionary method for the resolution of shoulder dystocia. Am J Obstet Gynecol 1985;152:479–84. [DOI] [PubMed] [Google Scholar]
- 15.Sandberg EC. The Zavanelli maneuver: 12 years of recorded experience. Obstet Gynecol 1999;93:312–17. [DOI] [PubMed] [Google Scholar]
- 16.Poujade O, Azria E, Ceccaldi PF, Davitian C, Khater C, Chatel P, et al. Prevention of shoulder dystocia: a randomized controlled trial to evaluate an obstetric maneuver. Eur J Obstet Gynecol Reprod Biol 2018;227:52–9. [DOI] [PubMed] [Google Scholar]
- 17.Menticoglou S. Shoulder dystocia: incidence, mechanisms, and management strategies. Int J Womens Health 2018;10:723–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol 2003;101:1068–72. [DOI] [PubMed] [Google Scholar]