Abstract
Pediatric obesity has become a worldwide epidemic and leads to notable effects on the developing skeleton that can have lifelong implications. Obesity in the pediatric population alters bone metabolism, increasing the risk for fracture. It can alter the presentation of common pediatric orthopaedic conditions such as scoliosis. Obesity also leads to changes in the patterns and severity of pediatric fractures as well as alters conservative fracture treatment due to increased displacement risk. Obese pediatric trauma patients place a high burden on the nationwide hospital system in a variety of ways including the increased risk of perioperative complications. Obesity is modifiable, and addressing the issue can improve the orthopaedic and overall health of children.
Obesity rates continue to climb in the United States and throughout the world, including the general pediatric population. The Centers for Disease Control currently categorizes obesity in children with body mass index (BMI) percentile for age and sex rather than BMI used in adults. Pediatric body weight categories are defined by the Centers for Disease Control as underweight (<fifth percentile), normal or healthy weight (5th to <85th percentile), overweight (85th to <95th percentile), and obese (≥95th percentile). Current rates of overweight and obese patients are up to 31.9%1 and 17% with BMI greater than 95 percentile for age.2 Obesity rates have tripled in pediatric patients aged 6 to 19 years since the 1970s,3,4 and children are the fastest growing subpopulation of obese individuals in the United States.5 Obesity rates are 50% to 75% higher in the African American and Hispanic populations and 30% lower in Asian populations when compared with Caucasians.6 Although there are known conditions that are directly related to obesity, including slipped capital femoral epiphysis and Blount disease, there is mounting evidence demonstrating that obesity itself increases the risk of complications related to fracture and surgical management along with physiologic changes to the growing skeleton compared with healthy weight patients. Because obesity is an externally modifiable risk factor, improved knowledge of these changes can improve pediatric care offered by orthopaedic surgeons. A full discussion on Blount disease and slipped capital femoral epiphysis is beyond the scope of this review, but there are multiple review articles available through the Journal of American Academy of Orthopaedic Surgeons for further information on these topics.
Obesity Effects on the Growing Skeleton
Approximately 40% of bone mineral accrual occurs within 2 years of the adolescent growth spurt,7,8 and by 18 years of age, 90% of peak bone mass occurs.9 The bone mass attained early in life is an important modifiable determinant for lifelong skeletal health,9 and skeletal deficiencies that occur at this age may persist throughout life.10 This is an important time to ensure maximum bone health. Obesity plays a strong role in altering this normal accrual because increased body fat has a negative effect on attaining peak bone mass.11 This seems counter-intuitive because Wolff law would posit that increased body mass would impart increased stress on bones due to the increased body mass and therefore increase the bone density. Various studies evaluating obese children have demonstrated that obese children have larger bones, greater bone mineral content for height, increased vertebral density, greater bone strength, increased height, and earlier maturation.3,7,12,13 Despite the increased mechanical load encouraging bone strength, endocrine-related changes and nutritional deficiencies stemming from the underlying obesity actually leads to a lower ratio of overall bone mass when compared with overall patient weight.13,14
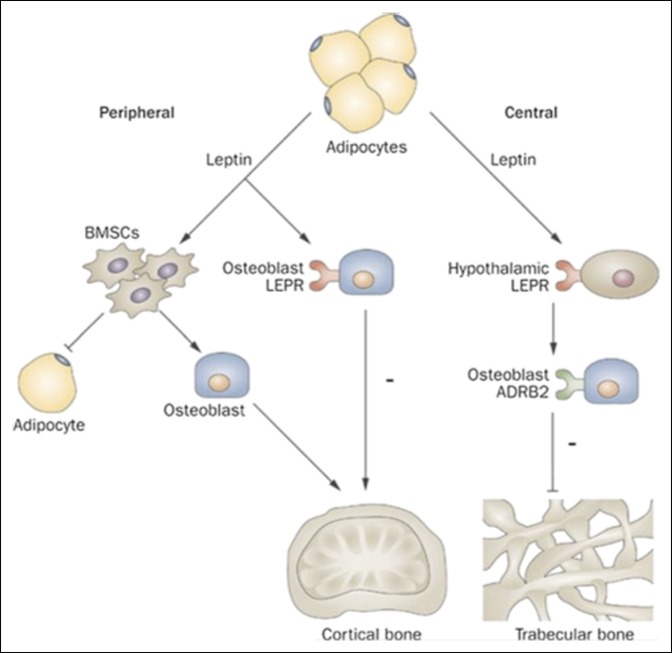
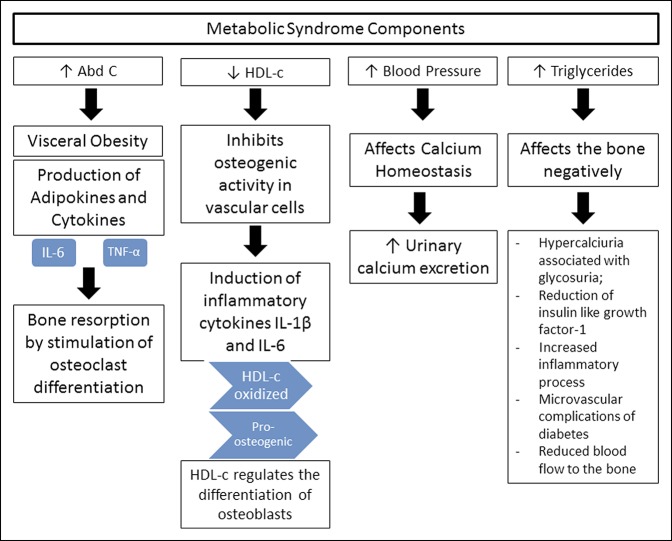
Obesity plays a strong role in bone physiology, especially through the metabolic syndrome which is a well-known condition related to abdominal obesity, altered glucose metabolism, dyslipidemia, and hypertension.8 This syndrome dysregulates the endocrine axis in multiple ways, including insulin resistance, increased inflammatory cytokine production, altered leptin production, and vitamin D deficiency.3,8,15 It has been postulated that the biggest culprit in this abnormal hormonal regulation is visceral/central adiposity rather than total adiposity.3,8 Central adiposity leads to insulin resistance, which abnormally affects the growing bone because of the effects on osteoblast/osteoclast function through the effects on leptin concentration. Leptin has been shown to have a generalized inhibitory role on cortical bone size.14 Elevated leptin levels accelerate bone resorption and decreases bone formation through increased RANKLA expression and decreased Receptor Activator of Nuclear factor Kappa-B Ligand (RANKL) inhibition (Figure 1).8 Abdominal obesity also produces increased systemic inflammation and pro-inflammatory cytokines because of dysfunctional adipocytes, which directly induces bone resorption leading to osteopenia/osteoporosis.3,7 Figure 2 provides a summary of the general effects that the metabolic syndrome has on overall bone physiology. Animal studies have found leptin receptors in skeletal growth centers, having a dose-dependent effect on the proliferative zone of the physis and thus acts as a skeletal growth factor.16 This has been hypothesized to be one reason why obese adolescents are taller in childhood than their nonobese peers, although this also leads to early epiphyseal plate maturation with obese children reaching full adult height at an earlier age.16 It should be kept in mind that the entire hormonal axis is affected in obese children with complex interactions leading to not only growth differences but early pubertal differences as well.
Figure 1.
Illustration showing the mechanism of central and peripheral leptin signaling. ADRB2 = B2 adrenergic receptor, BMSCs = bone marrow stromal cells, LEPR = leptin receptor. (Reproduced with permission from Macmillan Publishers Ltd, Kawai M, Devlin MJ, Rosen CJ: Fat targets for skeletal health. Nat Rev Rheumatol 2009;5:365-372.)
Figure 2.
Chart showing the effects of the metabolic syndrome on skeletal physiology. Abd C = abdominal circumference, HDL-c = high density lipoprotein c, IL = interleukin, TNF = tumor necrosis factor. (Reproduced with permission from da Silva VN, Fiorelli LNM, da Silva CC, Kurokawa CS, Goldberg TBL: Do metabolic syndrome and its components have an impact on bone mineral density in adolescents? Nutrition Metab 2017;14:1.)
As a fat soluble molecule, vitamin D is sequestered in adipose tissue, decreasing available circulation for bone remodeling.13 Vitamin D deficiency has been found in 29% of overweight children, 34% of obese children, and 49% of severely obese children.15 Vitamin D deficiency and nutritionally poor diets that include high consumption levels of carbonated sweetened drinks and low intake levels of high calcium foods (i.e., green leafy vegetables) further increase the risk for osteopenia in obese children.7
Effects of Obesity in Pediatric Trauma
The effects of obesity on injury severity and outcome after fracture are well recognized in adults, and with increasing rates of childhood obesity, the body of literature related to obesity in pediatric trauma is growing. Obese children have poorer balance than normal weight age-matched controls17 and lower bone mineral content to size ratio. Because of this, obese children generate more force than normal-weight children with a comparable mechanism of injury. All of these factors contribute to an increased fracture risk in young childhood.18 Obesity also leads to differences in the pattern and severity of injury, challenges with nonsurgical and surgical fracture care, and increased morbidity from trauma.
Effects on Pattern of Injury
Obesity has an effect on both the pattern and severity of orthopaedic injuries. Pollack et al19 assessed the risk of injury in motor vehicle crashes in a cross-sectional study from the Partners for Child Passenger Safety study, a child-specific crash surveillance system. They found a similar overall rate of injury when comparing overweight and obese children with those with a normal BMI, but noted that high BMI children had a higher rate of distal extremity fractures than normal-BMI children (odds ratio of 2.64 [95% confidence interval, 1.64 to 4.77] for obese versus normal BMI). They hypothesized that the increased extremity mass increased the force of impact on the interior vehicle structures and that larger children were closer to the interior structures, hitting them with increased velocity.
Rana et al5 identified an increased incidence of extremity fractures in obese pediatric trauma patients (55% versus 40% in obese versus nonobese patients, respectively). In their retrospective review of injured patients at their level 1 trauma center, they demonstrated a higher incidence of surgical treatment of fractures in obese patients (42% versus 30% in obese and nonobese patients, respectively). Similar to Pollack et al,19 the authors theorized that mass differences contributed to altered energy transmission to the extremities leading to an increased number of distal fractures.
Obese patients have also been show to display different injury patterns and complexity in lower energy mechanisms than their nonobese counterparts. In their review of all injured patients presenting to a level 1 urban trauma center over a 3-year period, Pomerantz et al20 found that obese children were more likely to sustain lower extremity injuries than upper extremity injuries when compared with nonobese patients, and less likely to sustain head and facial injuries. In a recent multicenter retrospective review of lateral condyle and supracondylar fractures, Fornari et al21 found a higher rate of obesity in the lateral condyle cohort than the supracondylar group. The authors hypothesized that the balance and mobility limitations seen in obese children cause them to have more difficulty bracing their fall on a fully extended arm. The resulting varus stress on the partially flexed elbow results in a lateral condyle fracture. Furthermore, within the lateral condyle group, obese children were more likely than normal-weight children to sustain notable displacement and articular incongruity.
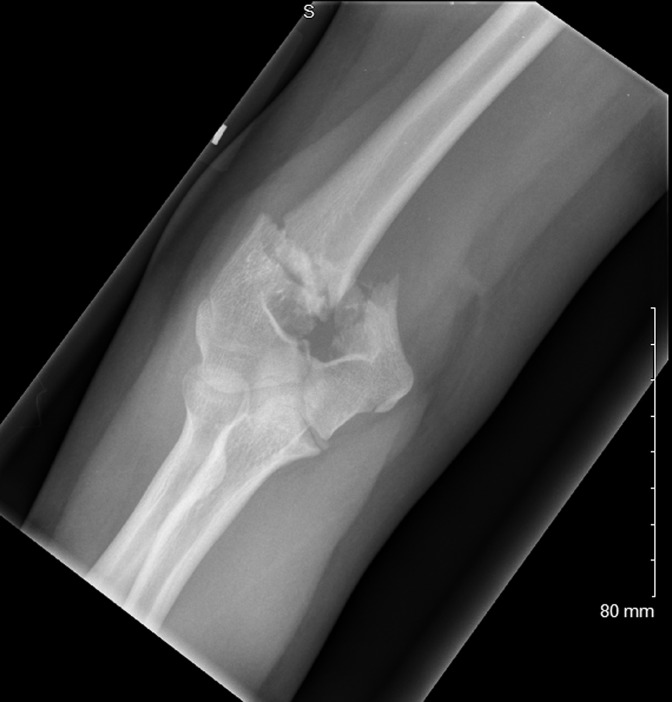
The fact that obese children are more likely to sustain severe injury patterns has been supported by others. In their evaluation of supracondylar humerus fractures, Seeley et al22 demonstrated a higher rate of complex fracture patterns, nerve palsies, and postoperative complications in obese children compared with normal-weight children, even when sustained through low energy mechanisms (Figure 3). Chang et al23 also found that obese patients had a higher risk of postoperative varus malalignment and pin complications after surgical treatment of type III supracondylar humerus fractures. Li et al24 found obese children between the ages of 8 and 12 were 4 times more likely than nonobese patients to require an open reduction in the setting of a supracondylar humerus fracture. They hypothesized that the excess subcutaneous fat was a likely cause for the difficulty in fracture manipulation along with the more severe injury patterns as found by Seeley et al.22 Gilbert et al25 found that obese patients were more than twice as likely to sustain a fracture of the physis than nonobese patients in lower extremity fractures stemming from blunt trauma. They theorized that the combination of increased force created during the injury along with the physiologic effects of obesity on the physis may lead to the higher incidence of physeal fractures in obese children. These studies support the idea that as body mass increases, so does the force generated from a comparable mechanism of injury, thus leading obese children to sustain more severe injury patterns than their nonobese peers (Figure 4).
Figure 3.
AP elbow radiograph of a 10 years, 9 months year-old female patient with a T-type supracondylar humerus fracture after falling from a standing height. BMI at the time of injury was 25.7 (97% for age). This fracture pattern is more commonly seen in adults. Obesity influences early epiphyseal plate closure, leading to more adult fracture patterns in younger children.
Figure 4.
A, PA wrist radiograph of 12 years, 8 months-year-old patient after fall from standing height while camping. A displaced distal radius physeal fracture is observed in addition to an ulnar styloid fracture. The patient also sustained minimally displaced contralateral distal radius fracture. BMI at the time of injury was 29.7 (98 percentile for age). B, Lateral wrist radiograph of patient (A) demonstrating comminution with loss of radial height and large metaphyseal volar fragment. At the time, patient did not demonstrate any carpal tunnel syndrome. Intraoperatively, the volar fragment was devascularized and required resection to ensure proper reduction and fixation. C, Lateral CT scan of the patient demonstrating comminution and height loss. D, PA wrist radiograph of the patient 4 weeks after closed reduction pin fixation noting full healing of distal radius fracture. E, Lateral wrist radiograph of the patient noting healed fracture and filling in of a previous volar bone defect. F, PA wrist radiograph of the same patient 8 months after fracture fixation, now demonstrating distal radius physeal arrest and ulnar overgrowth. Patient subsequently underwent distal ulna epiphysiodesis.
Challenges of Fracture Treatment
Challenges created by obesity during fracture care are well documented in the adult orthopaedic literature. In children, obesity also presents an additional hurdle to fracture care, in a setting where many fractures can traditionally be treated with cast immobilization. Successful cast treatment is dependent on a cast's ability to control the injured bone. As a patient's soft-tissue envelope increases, the distance from the cast to the bone increases, making it harder to adequately maintain fracture reduction. Because of this effect, several studies have evaluated the effect of obesity on cast treatment of various fractures. Okoraofor et al26 evaluated 129 children, 42% of whom were obese, with both bone forearm fractures and found that obese or overweight children were more likely to fail nonsurgical treatment than normal-weight children (34% versus 18%, respectively). They calculated an odds ratio of 3.3 for failure of nonsurgical management in obese patients. DeFrancesco et al27 found obese children were 6 times more likely than nonoverweight patients to lose reduction of complete both bone diaphyseal fractures. Likewise, Auer et al28 showed that obese children had an increased risk of displacement requiring repeat reduction of distal radius fractures. With the findings of these studies, it is recommended that obese patients with fractures treated conservatively be followed up closely to assure maintenance of fracture alignment along with family counseling on the risk of reduction loss and need for possible surgical fixation.
Obesity-Related Morbidity From Trauma
Overweight children are thought to be at higher risk of nonorthopaedic complications during generalized trauma care and may have a higher cost burden than nonobese patients, although there is some disagreement in the literature regarding the effect of obesity on hospitalized patients. Fleming-Dutra et al1 did not find a notable difference in the cost of acute care for overweight children compared with normal-weight children. However, they did find that patients hospitalized with fractures or dislocations had higher hospital costs in overweight children compared with those with normal weight. Rana et al5 did not reveal a notable difference in length of stay, ICU days, ventilator days, or mortality between obese and nonobese patients. In contrast, Brown et al29 showed longer ICU and hospital stays in obese patients; but similar to Rana et al,5 did not show a difference in mortality rates. Both studies demonstrated increased complications in obese patients, including deep vein thrombosis (DVTs), decubitus ulcers, post-op fistulas, wound infections, and sepsis.29 Backstrom et al30 found that obese patients were more likely to be admitted in the ICU and die in the hospital, but these differences were insignificant when adjusted for injury severity score. A recent systematic review,2 which included the abovementioned studies, concluded that obese trauma pediatric patients have a higher mortality rate than nonobese patients. However, only one of the included studies came to a similar conclusion and the review methods did not control for injury severity, which eliminated significance in the only report that demonstrated a higher mortality rate.30 This conclusion should therefore be taken with caution.
Effects of Obesity on Common Pediatric Orthopaedic Conditions
Obesity has been posited to delay the diagnosis or alter the natural history of various common pediatric orthopaedic conditions. Neal et al31 investigated the effects of obesity as related to Legg-Calvé-Perthes disease (LCPD). In this single site investigation, the odds of undergoing a containment procedure was 2.4 times less for obese patients and 2.8 times less for bony procedures. They found a notable correlation between increasing BMI and later Waldenstrom stage at initial presentation. With 28% of their patients being obese and 16% overweight, the authors postulated that traditional Perthes demographics are changing, creating a scenario for delayed diagnosis, which may ultimately produce worsened hip deformity that can trigger aberrant hip forces leading to poor long-term outcomes. In a separate region of the United States, Kessler and Cannamela32 assessed the demographics of LCPD and also found a high association between obesity and LCPD; 30.9% of their overall cohort was obese and 45.2% was overweight or obese, similar to Neal et al.31 The overall odds ratio of LCPD was 3.4 in obese patients compared with normal-weight patients.32 Given the changes in demographics in a condition routinely managed by pediatric orthopaedic surgeons, researchers should use results such as this in fine-tuning specific studies on the effects obesity has on other musculoskeletal conditions.
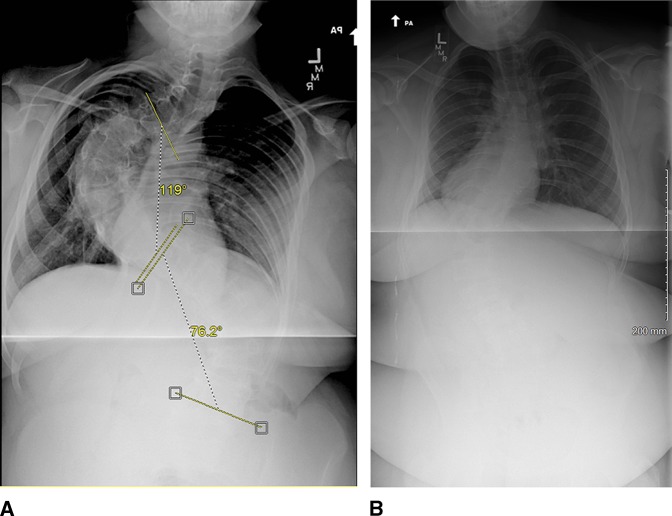
Gilbert et al33 assessed the effects of obesity on adolescent idiopathic scoliosis (AIS) evaluation. They found a notable association between BMI and curve magnitude although the linear correlation was not strong. This did not carry over to surgical level or progressive curves, which was found to be similar between healthy-weight and obese patients. Despite this, the increased soft-tissue envelope hides higher magnitude curves creating the risk for a later diagnosis (Figure 5).
Figure 5.
A, Radiograph showing initial PA scoliosis of an obese patient with very severe scoliosis that was not readily evident on physical examination because of her large body habitus. BMI at the time of presentation was 34. B, Second obese patient with an initial PA scoliosis view demonstrating a surgical level curve. BMI at the time of presentation was 47.2.
O'Neill et al34 specifically assessed the effect of being overweight on brace treatment of AIS. Overweight and obese patients had a higher mean curve progression during brace treatment over those who were not overweight (9.6° versus 3.6°). The in-brace correction percentage was markedly lower in overweight patients (41% versus 26%), had less bracing treatment success rate (26% versus 52 %), and greater progression to a curve ≥ 45° (45% versus 28%). Overall, overweight patients treated with bracing treatment for AIS were 3.1 times less likely to succeed than nonoverweight patients. In a more recent study, Zaina et al35 demonstrated no effect of obesity on brace efficacy for AIS. This group used a different type of brace than that used by O'Neill et al34 (Sforezco brace versus Boston brace), but in their discussion, felt that their results were related more to improved daily brace compliance than obesity itself. Further study on brace effectiveness in obese patients is needed.
Perioperative Complications Related to Obesity
Anesthetic Risks
In obese patients, routine sedation and anesthesia contains a higher risk level for obese pediatric patients because drug volumes of distribution of anesthesia drugs, most notably inhaled anesthetics, are altered. For many commonly used sedation drugs, the metabolism of these drugs is unpredictable due to increased adiposity because they are lipid soluble.36 In the study by Hirsch et al,37 patients who required sedation for long bone fracture reduction were assessed. Obese patients experienced twice the oxygen desaturation rates of all patients studied, especially when propofol was used in older patients (12 to 17 years of age). Dosing of anesthetic agents is usually based on lean or ideal body weight rather than total body weight, and there are charts available outlining the optimal specific body weight for these drugs.36
Morbid obesity is associated with a decrease in all respiratory functions, as well as increased risk for asthma and sleep apnea.14 Sleep apnea has been found in 2% of children and is associated with increasingly difficult intubation and acute respiratory failure requiring prolonged ventilation. In their study, Nafiu et al38 found obese patients had increased American Society of Anesthesiologists (ASA) scores because of increased medical comorbidities such as hypertension, type II diabetes, and bronchial asthma. Surgeons should be aware of these risks before performing any elective procedure in obese children and should consider preoperative anesthesia and pulmonary consults to optimize pulmonary health.
Perioperative Complications
Multiple studies have assessed perioperative complications related to obese pediatric patients. In assessing short-term complications associated with pediatric orthopaedic procedures, Basques et al39 found the most common complication risk was a return to the operating room, with the factors related to any complication risk being obesity (odds ratio of 2.3), American Society of Anesthesiologists score ≥ 3, and impaired cognitive status. In the single-center National Surgical Quality Improvement Program study by Blackwood et al,40 underweight, overweight, and obese patients had greater surgical site infection risk than normal-weight patients. Patients with an increased number of cardiac risk factors (found in obese patients) were also at greater risk for surgical site infection.
Georgopoulos et al41 evaluated the risk of DVT and pulmonary embolism (PE) in the pediatric orthopaedic patient undergoing elective surgery. They found a low incidence of overall DVT and PE in this group (5.1 per 10,000 admissions) but noted an increased risk in patients who were of older age, who had complications associated with an implanted device or surgical procedure, and who had a metabolic condition/obesity/syndrome. Their analysis grouped this last group together, which had a 6.1 times increased DVT/PE risk over the general population, with 25% of the lumped group being obese. Coupled with the increased DVT risk in obese pediatric trauma patients,5 Georgopoulos et al41 recommended routine mechanical prophylaxis in patients older than 12 years undergoing procedures longer than 1 hour with chemical prophylaxis to be considered in long procedures such as hip and spine surgeries.
Fedorak et al4 assessed complications related to external fixators used for various pediatric conditions and found no risk difference between obese and normal-weight patients. In the peri-acetabular osteotomy population, Novais et al42 evaluated patients less than 19 years of age. They found that obesity was the only variable that increased postoperative complication risk, finding a 10-fold increased risk. The most common complications included superficial and deep infection as well as wound hematomas despite comparable correction rates between groups. Finding similar results, Davila et al43 implemented mandatory weight intervention for all patients with a BMI > 95th percentile being considered for a peri-acetabular osteotomy. The studies by Leet et al44 and Weiss et al45 found higher complication risk in obese patients after femur fracture fixation, including malunion, wound infection, osteomyelitis, wound dehiscence, compartment syndrome, and broken implant.46
In scoliosis surgery, Upasani et al47 did not find increased risk in postoperative morbidity between obese and normal-weight patients with the Scoliosis Research Society scores and coronal deformity correction being maintained at 2 years postoperative in both groups. Hardesty et al48 found similar curve correction rates between obese and normal-weight patients, but their obese patients had longer operative times, had increased intraoperative blood loss, and increased intraoperative crystalloid requirements. Newton et al49 evaluated a multicenter spine fusion registry of patients who returned to the operating room within 90 days of initial spinal fusion. They found that BMI percent for age was the only factor related to increased infection risk (odds ratio 7.6), likely related to impaired systemic functions stemming from obesity, including cardiorespiratory, metabolic, and hemostatic function.
Implant-related Complications
Implant failure is a known complication risk when treating obese patients with guided growth techniques. Burghardt et al50 performed a Pediatric Orthopaedic Society of North America member survey and found that 15% of members reported mechanical failures of guided growth implant. Failures were related to the cannulated nature of the screws and occurred at the region of the screw shank at the metaphyseal bone-plate junction. Ninety-three percent of patients with broken implants were overweight or obese. This has led surgeons who treat angular deformities to use solid screws more often along with plates that have options for multiple screws on either side of the physis.
General Recommendations for Orthopaedic Surgeons
Patient visit times in current medical practice place a notable strain on all physicians to provide a comprehensive preventive health review, and orthopaedic surgeons are no exception. Although orthopaedic surgeons are not primary care physicians, they can and should be advocates for the general health of their patients. Orthopaedic surgeons can best focus on those areas that directly relate to musculoskeletal health and do not to be laborious in scope. For obese pediatric patients, the following points can be discussed or performed efficiently and do not necessitate in-depth discussion or work-up to provide sufficient information. Emphasis should be placed on a diet rich in nutritious foods (i.e., fruits and vegetables, whole grains) and low in junk food and sugar-laden drinks such as soda and juice.51 All children should be encouraged to be as active as possible, with preschool aged children being active throughout the day in a variety of activities. Children aged 6 to 17 years should have 60 minutes or more of moderate to vigorous physical activity every day emphasizing aerobic, muscle-strengthening, and bone-strengthening activities.52 A referral to a local healthy weight or obesity center can be made to assist patients in receiving the information and follow-up necessary to help attain a future healthy weight. Vitamin D screening is recommended in obese patients especially before major elective procedures, such as posterior spinal fusion or osteotomies,53 and should be considered for obese patients posttrauma to improve future bone health. Fractures treated conservatively should be followed up closely in obese pediatric patients, and if loss of reduction occurs, surgical fixation should be strongly considered. Caution should be high when performing fracture reductions on obese children with appropriate resuscitation equipment readily available in case of oxygen desaturation. Preoperative cleansing baths and prophylactic antibiotic dosing/re-dosing should be strictly observed to deter postoperative infection risk. Finally, as discussed previously, intraoperative mechanical DVT/PE prophylaxis should be performed in all patients older than 12 years with a procedure expected to last more than 1 hour.
Summary
Obesity markedly alters the physiologic and mechanical forces in pediatric patients. This is a modifiable factor that can be positively altered, leading to decreased postoperative complication risk and improved patient health and safety. Orthopaedic surgeons who take care of children should be aware of the effects of obesity on the growing skeleton in an effort to improve care in the long run, encouraging patients and families to be proactive in helping themselves achieve lifelong orthopaedic health. Orthopaedic surgeons should also work closely with primary care providers with screening of the secondary physiologic effects related to obesity to improve long-term patient health.
Footnotes
Dr. Nowicki or an immediate family member serves as an paid consultant to Orthopediatrics; serves as a board member, owner, officer, or committee member of American Academy of Orthopaedic Surgeons, Pediatric Orthopaedic Society of North America. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Kemppainen, Dr. Maskill, and Dr. Cassidy.
References
- Levels of evidence are described in the table of contents. In this article, reference 6 is a level 1 studies. References 2, 4, 5, 12, 17, 19-21, 25, 26, 29, 30, 37, 38, 40, 41, 44, and 47 are level 2 studies. References 1, 10, 15, 18, 22, 23, 27, 28, 31, 33-35, 39, 42, 43, 45, and 49 are level 3 studies. References 24, 32, 48, and 50 are level 4 studies. References 3, 7-9, 11, 13, 14, 16, 36, 46, 51-54 are level 5 studies.
- 1.Fleming-Dutra KE, Mao J, Leonard JC: Acute care costs in overweight children: A pediatric urban cohort study. Child Obes 2013;9:338-345. [DOI] [PubMed] [Google Scholar]
- 2.Kim SJ, Ahn J, Kim HK, Kim JH: Obese children experience more extremity fractures than nonobese children and are significantly more likely to die from traumatic injuries. Acta Pediatrica 2016;105:1152-1157. [DOI] [PubMed] [Google Scholar]
- 3.Pollock NK: Childhood obesity, bone development, and cardiometabolic risk factors. Mol Cel Endocrinol 2015;410:52-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fedorak GT, Cuomo AV, Otsuka NY: Does pediatric body mass index affect surgical outcomes of lower-extremity external fixation? J Pediatr Orthop 2015;35:391-394. [DOI] [PubMed] [Google Scholar]
- 5.Rana AR, Michalsky MP, Teich S, Groner JI, Caniano DA, Schuster DP: Childhood obesity: A risk factor for injuries observed at a level-1 trauma center. J Pediatr Surg 2009;44:1601-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman DS, Wang J, Thornton JC, et al. : Racial/ethnic differences in body fatness among children and adolescents. Obesity (Silver Spring) 2008;16:1105-1111. [DOI] [PubMed] [Google Scholar]
- 7.Kelley JC, Crabtree N, Zemel BS: Bone density in the obese child: Clinical considerations and diagnostic challenges. Calcif Tissue Int 2017;100:514-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Da Silva VN, Fiorelli LNM, da Silva CC, Kurokawa CS, Goldberg TBL. Do metabolic syndrome and its components have an impact on bone mineral density in adolescents? Nuttrition Metab 2017;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golden NH, Abrams SA: Optimizing bone health in children and adolescents. Pediatrics 2014;134:e1229-e1243. [DOI] [PubMed] [Google Scholar]
- 10.Skaggs DL, Loro ML, Pitukcheewanont P, Tolo V, Gilsanz V: Increased body weight and decreased radial cross-sectional dimensions in girls with forearm fractures. J Bone Min Res 2001;16:1337-1342. [DOI] [PubMed] [Google Scholar]
- 11.Chan G, Chen CT: Musculoskeletal effects of obesity. Curr Opin Pediatr 2009;21:65-70. [DOI] [PubMed] [Google Scholar]
- 12.Leonard MB, Shults J, Wilson BA, Tershakovec AM, Zemel BS: Obesity during childhood and adolescence augments bone mass and bone dimensions. Am J Clin Nutr 2004;80:514-523. [DOI] [PubMed] [Google Scholar]
- 13.Bialo SR, Gordon CM: Underweight, overweight, and pediatric bone fragility: Impact and management. Curr Osteoporos Rep 2014;12:319-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lazar-Antman MA, Leet AI: Effects of obesity on pediatric fracture care and management. J Bone Joint Surg Am 2012;94:855-861. [DOI] [PubMed] [Google Scholar]
- 15.Turer CB, Lin H, Flores G: Prevalence of Vitamin D deficiency among overweight and obese U.S. children. Pediatrics 2013;131:e152-e161. [DOI] [PubMed] [Google Scholar]
- 16.Shalitin S, Kiess W: Putative effects of obesity on linear growth and puberty. Horm Res Paediatr 2017;88:101-110. [DOI] [PubMed] [Google Scholar]
- 17.Goulding A, Jones IE, Taylor RW, Piggot JM, Taylor D: Dynamic and static tests of balance and postural sway in boys: effects of previous wrist bone fractures and high adiposity. Gait Posture 2003;17:136-141. [DOI] [PubMed] [Google Scholar]
- 18.Davidson PL, Goulding A, Chalmers DJ: Biomechanical analysis of arm fracture in obese boys. J Paediatr Child Health 2003;39:657-664. [DOI] [PubMed] [Google Scholar]
- 19.Pollack KM, Xie D, Arbogast KB, Durbin DR: Body mass index and injury risk among US children 9-15 years old in motor vehicle crashes. Inj Prev 2008;14:366-371. [DOI] [PubMed] [Google Scholar]
- 20.Pomerantz WJ, Timm NL, Gittelman MA: Injury patterns in obese versus nonobese children presenting to a pediatric emergency department. Pediatrics 2010;125:681-685. [DOI] [PubMed] [Google Scholar]
- 21.Fornari ED, Suszter M, Roocroft J, Bastrom T, Edmonds EQ, Schlechter J: Childhood obesity as a risk factor for lateral condyle fractures over supracondylar humerus fractures. Clin Orthop Relat Res 2013;471:1193-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seeley MA, Gagnier JJ, Srinivasan RC, et al. : Obesity and its effects on pediatric supracondylar humeral fractures. J Bone Joint Surg Am 2014;96:e18. [DOI] [PubMed] [Google Scholar]
- 23.Chang CH, Kao HK, Lee WC, Yang WE: Influence of obesity on surgical outcomes in type III paediatric supracondylar humeral fractures. Injury 2015;46:2181-2184. [DOI] [PubMed] [Google Scholar]
- 24.Li NY, Bruce WJ, Joyce C, Decker NM, Cappello T: Obesity's influence on operative management of pediatric supracondylar humerus fractures. J Pediatr Orthop 2018;38:e118-e121. [DOI] [PubMed] [Google Scholar]
- 25.Gilbert SR, MacLennan PA, Backstrom I, Creek A, Sawyer J: Altered lower extremity fracture characteristics in obese pediatric trauma patients. J Orthop Trauma 2015;29:e12-e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okoroafor UC, Cannada LK, McGinty JL: Obesity and failure of nonsurgical management of pediatric both-bone forearm fractures. J Hand Surg Am 2017;42:711-76. [DOI] [PubMed] [Google Scholar]
- 27.DeFrancesco CJ, Rogers BH, Shah AS: Obesity increases risk of loss of reduction after casting for diaphyseal fractures of the radius and ulna in children: An observational cohort study. J Orthop Trauma 2018;32:e46-e51. [DOI] [PubMed] [Google Scholar]
- 28.Auer RT, Mazzone P, Robinson L, Nyland J, Chan G: Childhood obesity increases the risk of failure in the treatment of distal forearm fractures. J Pediatr Orthop 2016;36:e86-e88. [DOI] [PubMed] [Google Scholar]
- 29.Brown CV, Neville AL, Salim A, Rhee P, Cologne K, Demetriades D: The impact of obesity on severely injured children and adolescents. J Pediatr Surg 2006;41:88-91. [DOI] [PubMed] [Google Scholar]
- 30.Backstrom IC, MacLennan PA, Sawyer JR, Creek AT, Rue LW, III, Gilbert SR: Pediatric obesity and traumatic lower-extremity long-bone fracture outcomes. J Trauma Acute Care Surg 2012;73:966-971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neal DC, Alford TH, Moualeu A, Jo CH, Herring JA, Kim HK: Prevalence of obesity in patients with Legg-Calvé-Perthes disease. J Am Acad Orthop Surg 2016;24:660-665. [DOI] [PubMed] [Google Scholar]
- 32.Kessler JI, Cannamela PC: What are the demographics and epidemiology of Legg-Calve-Perthes disease in a large Southern California integrated health system? Clin Orthop Relat Res 2018;476:2344-2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbert SR, Savage AJ, Whitesell R, Conklin MJ, Fineberg NS: BMI and magnitude of scoliosis at presentation to a specialty clinic. Pediatrics 2015;135:e1417-e1424. [DOI] [PubMed] [Google Scholar]
- 34.O'Neill PJ, Karol LA, Shindle MK, et al. : Decreased orthotic effectiveness in overweight patients with adolescent idiopathic scoliosis. J Bone Joint Surg 2005;87-A:1069-1074. [DOI] [PubMed] [Google Scholar]
- 35.Zaina F, Donzelli S, Negrini S: Overweight is not predictive of bracing failure in adolescent idiopathic scoliosis: Results from a retrospective cohort study. Eur Spine J 2017;26:1670-1675. [DOI] [PubMed] [Google Scholar]
- 36.Samuels PJ, Sjoblom MD: Anesthetic considerations for pediatric obesity and adolescent bariatric surgery. Curr Opin Anesthesiol 2016;29:327-336. [DOI] [PubMed] [Google Scholar]
- 37.Hirsch DG, Tyo J, Wrotniak BH: Desaturation in procedural sedation for children with long bone fractures: Does weight status matter? Am J Emerg Med 2017;35:1060-1063. [DOI] [PubMed] [Google Scholar]
- 38.Nafiu OO, Reynolds PI, Bamgbade OA, Tremper KT, Welch K, Kasa-Vubu JZ: Childhood body mass index and perioperative complications. Pediatr Anesth 2007;17:426-430. [DOI] [PubMed] [Google Scholar]
- 39.Basques BA, Lukasiewicz AM, Samuel AM, et al. : Which pediatric orthopaedic procedures have the greatest risk of adverse outcomes? J Pediatr Orthop 2017;37:429-434. [DOI] [PubMed] [Google Scholar]
- 40.Blackwood BP, Gause CD, Harris JC, et al. : Overweight and obese pediatric patients have an increased risk of developing a surgical site infection. Surg Infections 2017;18:491-497. [DOI] [PubMed] [Google Scholar]
- 41.Georgopoulos G, Hotchkiss MS, McNair B, Siparsky G, Carry PM, Miller NH: Incidence of deep vein thrombosis and pulmonary embolism in the elective pediatric orthopaedic patient. J Pediatr Orthop 2016;36:101-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Novais EN, Potter GD, Sierra RJ, et al. : Surgical treatment of adolescent acetabular dysplasia with a periacetabular osteotomy: Does obesity increase the risk of complications? J Pediatr Orthop 2015;35:561-564. [DOI] [PubMed] [Google Scholar]
- 43.Davila N, Vess J, Johnson EE: Identification and management of obese patients in a pediatric orthopaedic clinic. Orthop Nurs 2017;36:194-200. [DOI] [PubMed] [Google Scholar]
- 44.Leet AI, Pichard CP, Ain MC: Surgical treatment of femoral fractures in obese children: Does excessive body weight increase the rate of complications? J Bone Joint Surg Am 2005;87-A:2609-2613. [DOI] [PubMed] [Google Scholar]
- 45.Weiss JM, Choi P, Ghatan C, Skaggs DL, Kay RM: Complications with flexible nailing of femur fractures more than double with child obesity and weight >50 kg. J Child Orthop 2009;3:53-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gettys FK, Jackson JB, Frick SL: Obesity in pediatric orthopaedics. Orthop Clin North Am 2011;42:95-105. [DOI] [PubMed] [Google Scholar]
- 47.Upasani VV, Caltoum C, Petcharaporn M, et al. : Does obesity affect surgical outcomes in adolescent idiopathic scoliosis? Spine 2008;33:295-300. [DOI] [PubMed] [Google Scholar]
- 48.Hardesty CK, Poe-Kochert C, Son-Hing JP, Thompson GH: Obesity negatively affects spinal surgery in idiopathic scoliosis. Clin Orthop Relat Res 2013;471:1230-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Newton P, Bastrom TP, Yaszay B: Patient-specific risk adjustment improves comparison of infection rates following posterior fusion for adolescent idiopathic scoliosis. J Bone Joint Surg Am 2017;99:1846-1850. [DOI] [PubMed] [Google Scholar]
- 50.Burghardt RD, Specht SC, Herzenberg JE: Mechanical failures of eight-plate guided growth system for temporary hemiepiphysiodesis. J Pediatr Orthop 2010;30:594-597. [DOI] [PubMed] [Google Scholar]
- 51.Daniels SR, Hassink SG: The role of the pediatrician in primary prevention of obesity. Pediatrics 2015;136:e275-e292. [DOI] [PubMed] [Google Scholar]
- 52.U.S. Department of Health and Human Services. Physical Activtiy Guidelines for Americans, ed 2. Washington, DC:U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 53.Clarke NM, Page JE: Vitamin D deficiency: a paediatric orthopaedic perspective. Curr Opin Pediatr 2012;24:46-49. [DOI] [PubMed] [Google Scholar]
- 54.Kawai M, Devlin MJ, Rosen CJ: Fat targets for skeletal health. Nat Rev Rheumatol 2009;5:365-372. [DOI] [PMC free article] [PubMed] [Google Scholar]