Abstract
Background
Tuberculosis (TB) is the 9th leading cause of death from a single infectious agent. Patients live in a complex health care system with both formal and informal providers, and it is important that a TB diagnosis is not missed at the first interaction with the health care system. In this study, we highlight the health seeking behavior of patients and missed opportunities for early TB diagnosis for which interventions could be instituted to ensure early TB diagnosis and prompt TB treatment initiation.
Methods
This study was nested in a cross-sectional study that assessed the accuracy of different Xpert MTB/Rif implementation strategies in programmatic settings at the referral hospitals in Uganda. We documented the symptom profile of presumptive TB patients and assessed the health seeking behavior of those with chronic cough by calculating proportion of patients that visited each type of health facility and further calculated the odds of being TB positive given the type of health facility initially visited for consultation.
Results
A total of 1,863 presumptive TB patients were enrolled of which 979 (54.5%) were male, and 1795 (99.9%) had chronic cough. A total of 1352 (75.4%) had previously sought care for chronic cough, with 805 (59.6%) seeking care from a public health facility followed by private health facility (289; 21.4%). Up to 182 (13.5%) patients visited a drug store for chronic cough. Patients whose first contact was a private health facility were more likely to have a positive GeneXpert test (adjOR 1.4, 95% CI: 1.0–1.9; p = 0.047).
Conclusions
Chronic cough is a main symptom for many of the presumptive TB patients presenting at referral hospitals, with several patients having to visit the health system more than once before a TB diagnosis is made. This suggests the need for patients to be thoroughly evaluated at first interface with the health care system to ensure prompt diagnosis and treatment initiation. Improved TB diagnosis possibly with the GeneXpert test, at first contact with the health care system has potential to increase TB case finding and break the transmission cycle in the community.
Background
Tuberculosis (TB) is the 9th leading cause of death from a single infectious agent, ranking above Human Immune deficiency virus (HIV) [1]. The 2017 WHO global TB report lists Uganda as a high HIV/TB burden country. In 2016, Uganda notified 44816 TB cases [2], and data from the TB prevalence survey put the prevalence and incidence rates at 253/100,000 and 234/100,000 respectively [3]. Uganda has a decentralized laboratory health system with laboratory services decentralized up to lower level health facilities. The country has up to 1,500 diagnostic and treatment units (DTUs) and as early as 2010, Xpert MTB/Rif technology was rolled out in the country, with up to 115 machines installed in 105 health facilities [4]. Loop holes in the health care system are some of the reasons for delayed and missed TB diagnosis. Studies have shown that patients first identified as having TB in community surveys had previously attended health services on a number of occasions with symptoms but had never been diagnosed [5].
Prompt diagnosis and early initiation of treatment remain key strategies for TB prevention and control. Diagnostic delays have been documented both at patient and health system levels [6, 7]. Factors that could lead to delay in TB diagnosis include initial visitation to a low level public healthcare facility, private practitioner consultation, or visit to a traditional healer, poverty, female gender, alcoholism and substance abuse, history of immigration, low educational status, low awareness of TB, self-prescription and stigma [5, 8–10]. Studies done in Uganda, Ghana and India found health systems as the biggest contributor of delayed TB diagnosis [8, 9, 11, 12]. Health facility delay was strongly associated with failure to perform sputum microscopy and was more common among private healthcare practitioners and rural public health facilities [11].
Patients live in a complex health care system with both formal and informal providers and it is important that a TB diagnosis is not missed at first contact with the health care system. Missed opportunities at first contact with the healthcare system do not only jeopardize the wellbeing of the patients but also have the potential to increase and sustain TB transmission in the community. In this study, we document the heath seeking behaviors of patients with chronic cough (cough of more than 2 weeks) and highlight the missed opportunities for early TB diagnosis for which interventions could be instituted to ensure early TB diagnosis and prompt treatment initiation.
Methods
Design and study setting
This study was nested in a cross-sectional study that assessed the accuracy of different Xpert MTB/Rif implementation strategies in programmatic settings at referral hospitals in Uganda [13]. We consecutively enrolled presumptive TB patients (18 years and above) at five referral hospitals in Uganda. Four of the hospitals (Mbale, Arua, Mbarara and Lacor) are regional referral hospitals serve as referral units for lower level health units in the region each with an average bed capacity of 450 beds. The other referral hospital (Mulago) is a national referral hospital that provides services to Kampala's population and surrounding districts plus upcountry referrals and has up to 1500 beds.
A presumptive TB patient was defined as a patient with chronic cough (at least 2 weeks), significant weight loss (more than 3Kgs), persistent fevers (more than 3 weeks) and excessive night sweats (more than 3 weeks). The participants were both HIV positive and negative adults visiting these study sites for consultation, with some having previously sought care from other health facilities. We excluded patients that were too ill to be interviewed. The study sites were well spread across the country with some sites serving cross border populations by virtue of them being near or in border towns. The study was conducted between October 2015 and August 2016.
All presumptive TB patients able to provide sputum had their sputum samples tested on the Xpert MTB/RIF assay. TB positive patients were linked into care and started on TB treatment as per the national guidelines. Xpert MTB/RIF assays were done at the study sites according to standard procedures and as have been detailed in previous work[13].
Data collection
Data were collected through use of an interviewer administered questionnaire that had been previously piloted. Interviewers were trained on how to fill the questionnaire. The questionnaire covered sociodemographic as well as health seeking history of the respondents. The interviewers ensured all questions were asked before the interview could end.
Statistical analysis
Data were double entered into an electronic database (Epidata Version 2.0 /2007) and where there were discrepancies, these were resolved by cross checking with the source documents (raw data). Data were exported to Stata v13 (Stata Corp, College Station TX, USA) for analysis. We used the exact binomial method for calculating 95% confidence intervals.
We documented the symptom profile of presumptive TB patients and assessed the health seeking behavior of those with chronic cough by calculating the proportion of patients that visited each type of health facility and further calculated the odds of being TB positive on GeneXpert given the type of health facility initially visited for consultation. Also assessed was the proportion of patients asked for a TB test at each of the facilities visited even when the patients presented with chronic cough. Variables at bivariate analysis with P-Value < 0.2 were added to a logistic regression model in a backward elimination method. Variables with P-value < 0.05 were considered statistically significant.
Ethics statement
Approval was obtained from Makerere School of Public health IRB (HDREC 093) and national approval granted by Uganda National Council for Science and Technology (HS-1904). All participants gave written informed consent.
Results
Characteristics of the study population
A total of 1,863 presumptive TB patients were enrolled, of which 66 patients had incomplete data. Only 1797 patients who had complete demographic data were included for analysis. Table 1 summarizes the demographic characteristics of the respondents (presumptive TB patients), and the study site distribution was as follows: Mbale 200 (11.1%), Arua 429 (23.9%), Mbarara 235 (13.1%), Lacor 246 (13.7%) and Mulago 687 (38.2%). The males were 979 (54.5%), 1,072 (57.5%) were in the age group of 18–38 years, subsistence farming was the dominant occupation group; 475 (26.4%) and 1065 (59.2%) respondents were married.
Table 1. Socio-demographic characteristics of adults enrolled in health care services with respiratory symptoms (n = 1797).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Sex | Male | 979 | 54.5 |
| Female | 818 | 45.5 | |
| Age | 18–38 | 1072 | 57.5 |
| 39–59 | 588 | 31.6 | |
| >60 years | 203 | 10.9 | |
| Residence | Urban | 989 | 55.0 |
| Rural | 808 | 45.0 | |
| Marital status | Single | 389 | 21.6 |
| Married | 1065 | 59.2 | |
| Separated | 184 | 10.2 | |
| Divorced | 43 | 2.4 | |
| Widowed | 88 | 4.9 | |
| Other | 28 | 1.6 | |
| Occupation | Unemployed | 277 | 15.4 |
| Housewife | 105 | 5.8 | |
| Subsistence farmer | 475 | 26.4 | |
| Market vendor | 148 | 8.2 | |
| Builder | 78 | 4.3 | |
| Health worker | 10 | 0.6 | |
| Business | 355 | 19.8 | |
| Civil servant | 67 | 3.7 | |
| Others | 282 | 15.7 |
Health seeking behavior of the presumptive TB patients with chronic cough
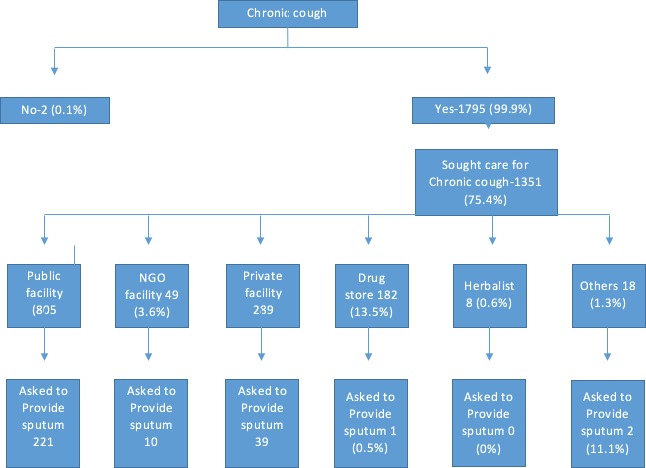
The health seeking behavior of the respondents with chronic cough is represented in Table 2 and Fig 1. Fig 1 also shows the proportion of patients at each of the facilities visited that were asked to avail a sputum sample when they presented with chronic cough. Of the respondents, 1795 (99.9%) had chronic cough as a symptom. Of these, 1351 (75.2%) had previously sought care for the chronic cough with 805 (59.6%) seeking care from a public health facility followed by 289 (21.4%) visiting a private health facility. Up to 182 (13.5%) patients visited a drug store for the chronic cough. Of the patients that consulted from a public health facility, 221 (27.5%) were asked to provide a sputum sample, while 39 (13.5%) of those that consulted from a private health facility were asked to provide a sputum sample.
Table 2. Table showing health facilities initially visited by patients with chronic cough (n = 1351).
| Health facility visited following chronic cough | Frequency | Percentage |
|---|---|---|
| Public health facility | 805 | 59.6 |
| Non-Governmental Organization (NGO) health facility | 49 | 3.6 |
| Private health facility | 289 | 21.4 |
| Drugstore/Pharmacy | 182 | 13.5 |
| Herbalist | 8 | 0.6 |
| Others* | 18 | 1.3 |
*Others = (friends, Ayurveda, nutritional supplements)
Fig 1. Health Seeking behavior for the presumptive TB patients with chronic cough.
GeneXpert results of the respondents given health facility initially visited
The GeneXpert results of the respondents based on the health facilities initially visited are represented in Table 3 below. Over a quarter (30%) of the respondents were TB positive by GeneXpert. Of the respondents that consulted from herbalists for the chronic cough, 50% were GeneXpert positive, while 36.1% of those that consulted from a private health facility tested positive on GeneXpert.
Table 3. GeneXpert results of the respondents given health facility initially visited (n = 1316).
| Health facility | Total | GeneXpert Positive n (%) |
|---|---|---|
| Public | 781 | 218 (27.9) |
| NGO | 48 | 14(29.2) |
| Private | 280 | 101(36.1) |
| Drug store | 182 | 52(28.6) |
| Herbalist | 8 | 4(50) |
| Others* | 17 | 6(35.3) |
| Total | 1,316 | 395(30.0) |
*Others = (friends, Ayurveda, nutritional supplements)
Probability of being GeneXpert positive given the health facility initially visited
The odds of being found GeneXpert positive given the health facility initially visited are presented in Table 4. The odds of being GeneXpert positive having initially visited a private health facility were 1.4 times higher (AdjOR 1.4, 95% CI: 1.0–1.9; p = 0.047) than when the facility initially visited was a public health facility.
Table 4. Odds of being GeneXpert positive based on health facility initially visited.
| Health facility | Un adjOR (95% CI) | P-Value | AdjOR* (95% CI) | P-Value |
|---|---|---|---|---|
| Public | Reference | Reference | ||
| NGO | 1.1 (0.6–2.0) | 0.851 | 1.0 (0.5–2.0) | 0.971 |
| Private | 1.5 (1.1–1.9) | 0.011 | 1.4 (1.0–1.9) | 0.047 |
| Drugstore | 1.0 (0.7–1.5) | 0.859 | 1.0 (0.7–1.1) | 0.844 |
| Herbalist | 2.6 (0.6–10.4) | 0.182 | 2.0 (0.5–4.2) | 0.353 |
| Others | 1.4 (0.5–3.9) | 0.505 | 1.4 (0.5–4.2) | 0.520 |
*Adjusted for age, gender, education level, bio smoke exposure, occupation
Discussion
This study done among referral hospitals shows that a significant proportion of presumptive TB patients presents with chronic cough as one of the key symptoms. Despite the fact that these patients reside in a high burden setting, they are usually misdiagnosed for TB during their initial presentation at the heath facilities. Moreover, even with this attempt of care seeking given their chronic cough, most of them were not evaluated for TB during the initial care seeking visit. We document a significant number of these patients who end up being diagnosed with TB using the GeneXpert test at the referral health facilities. Our study further shows that a number of these participants had initially presented to at least one health facility with chronic cough before TB diagnosis was made. This presents a missed opportunity for early TB diagnosis in a high TB/HIV burden setting.
This multiple healthcare contact following signs and symptoms could lead to delays in TB diagnosis [14, 15]. Provider shopping has been found to be a patient related factor contributing to TB diagnostic delays [16]. Studies done have shown that despite several visits to clinics with signs and symptoms suggestive of TB disease, patients still go un diagnosed. This could be due to lack of diagnostic awareness among health workers, as well as atypical presentation [17].
Shortage of health workers particularly laboratory technicians could also lead to failure to diagnose patients for TB at their initial visit [17]. The failure to diagnose TB in these facilities could also be due to absence of diagnostics which could be further complicated by stock outs of consumables e.g. sputum mugs, reagents among others. There is a need to further decentralize TB services including roll out of the GeneXpert technology to lower facilities to aid in diagnosis of TB patients. GeneXpert has been found to be more sensitive than microscopy [13].
In this study, chronic cough was the most common symptom among the presumptive TB patients as has been documented elsewhere [16, 18]. However in a survey done in Zambia, cough was documented a secondary symptom to chest pain[19], probably due to the fact that this was a community prevalence survey which tends to find TB in patients without cough.
Our study further found that most of the patients sought initial care at a public health facility. This is probably because of the decentralized public health system setting in Uganda which goes as low as the village level. Furthermore, this could also be due to the fact that most of the respondents were subsistence farmers, and services in public health facilities are free of charge. This is in agreement with studies done in rural South Africa and Zambia which found that TB patients often presented initially to public hospitals [19, 20]. Interestingly, the 21% of the participants in our study who sought initial TB care services at the private health facility had 1.5 times chance of being diagnosed with TB using GeneXpert. This could be due to the fact that patients in private health facilities are usually misdiagnosed for TB as a result of low suspicion index coupled with lack of TB diagnostics at the private health facilities. Studies have shown that patients who seek care from a private health facility incur delays in the diagnostic pathway [21, 22]. There are many reasons patients resort to private health facilities such as drug stores/pharmacies including other informal health providers. These include convenience, affordability and social and cultural effects [23]. Pharmacies and drug stores lack adequately trained professionals, provide advice for common symptoms which is not in accordance with guidelines and inappropriately prescribe medicines. There are also gaps in knowledge and provider practice [23, 24]. Important to note, patients that sought care from herbalists were 2.6 times more likely to have a positive GeneXpert result, although not statistically significant. Herbs could be an easy option for most financially handicapped TB presumptive patients as they are a cheaper option.
The main sample for TB diagnosis is sputum, however despite patients presenting to a health facility with chronic cough, most of them were never asked to avail a sputum sample. This further presents a missed opportunity for early TB diagnosis and could facilitate continued community TB transmission [20]. In a Zambian TB survey, only a small proportion of patients (12.1%) that had visited a facility for consultation were asked for a sputum sample [19]. Provider related factors have been found to contribute to delays in TB diagnosis [16], and to further complicate TB control [25]. This thus calls for a high index of suspicion for TB in health facilities if early TB diagnosis is to be realized.
Limitations
We were unable to document any other visits between the initial visit to the health care provider and the study site. This would have documented a complete pathway the study patients went through before a diagnosis was made. Furthermore, it would have helped us estimate the time between onset of cough and diagnosis to be able to document the magnitude of diagnostic delay. We were also unable to ascertain the level of the public health facility initially visited and also ascertain the test results for those patients that had been asked to provide a sputum sample on initial consultation. The level of the public health facility would have helped us understand whether the facility had the necessary diagnostics or not, while by understanding the results from the sputum, we would have been able to document whether a diagnostic test was done or not when sputum sample was requested.
Conclusion
Chronic cough is a main symptom for majority of the presumptive TB patients presenting at referral hospitals, with several patients having to visit the health system more than once before having a diagnosis. This suggests the need for patients to be thoroughly evaluated at first interface with the health care system to ensure prompt diagnosis and treatment initiation. Improved TB diagnosis possibly with the GeneXpert test, at first contact with the health care system has potential to increase TB case finding and break the transmission cycle in the community. Patients who first seek TB care from private facilities are 1.5 times more likely to have a positive sputum GeneXpert test result compared to those who first seek care in public health facilities. This stresses the need to strengthen the Public Private Partnerships in Uganda in order to improve TB control.
Supporting information
(DTA)
(PDF)
Acknowledgments
Participants in the study sites, participating sites, National TB program, Research team
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was conducted with funding from the World Bank under the East African Public Health Laboratory Networking Project (EAPHLNP). he funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Organization WH. Tuberculosis patient cost surveys: a handbook. 2017.
- 2.Organisation WH. Global Tuberculosis Report 2017. 2017.
- 3.Nugussie DA, Mohammed GA, Tefera AT. Prevalence of Smear-Positive Tuberculosis among Patients Who Visited Saint Paul’s Specialized Hospital in Addis Ababa, Ethiopia. BioMed research international. 2017;2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uganda M. NTLP Annual Report 2015–2016. 2017.
- 5.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC public health. 2008;8(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiwuwa MS, Charles K, Harriet MK. Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health. 2005;5(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oola J. Factors influencing delayed Diagnosis of Tuberculosis in Mukono District, Uganda. 2001.
- 8.Kiwuwa MS, Charles K, Harriet MK. Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health. 2005;5(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. The International Journal of Tuberculosis and Lung Disease. 2002;6(9):789–95. [PubMed] [Google Scholar]
- 10.Xu B, Jiang Q, Xiu Y, Diwan V. Diagnostic delays in access to tuberculosis care in counties with or without the National Tuberculosis Control Programme in rural China. The International Journal of Tuberculosis and Lung Disease. 2005;9(7):784–90. [PubMed] [Google Scholar]
- 11.Lawn S, Afful B, Acheampong J. Pulmonary tuberculosis: diagnostic delay in Ghanaian adults. The International Journal of Tuberculosis and Lung Disease. 1998;2(8):635–40. [PubMed] [Google Scholar]
- 12.Liam C, Tang B. Delay in the diagnosis and treatment of pulmonary tuberculosis in patients attending a university teaching hospital. The International Journal of Tuberculosis and Lung Disease. 1997;1(4):326–32. [PubMed] [Google Scholar]
- 13.Muttamba W, Ssengooba W, Sekibira R, Kirenga B, Katamba A, Joloba M. Accuracy of different Xpert MTB/Rif implementation strategies in programmatic settings at the regional referral hospitals in Uganda: Evidence for country wide roll out. PloS one. 2018;13(3):e0194741 10.1371/journal.pone.0194741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osei E, Akweongo P, Binka F. Factors associated with DELAY in diagnosis among tuberculosis patients in Hohoe Municipality, Ghana. BMC Public Health. 2015;15(1):721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yimer SA, Bjune GA, Holm-Hansen C. Time to first consultation, diagnosis and treatment of TB among patients attending a referral hospital in Northwest, Ethiopia. BMC infectious diseases. 2014;14(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mistry N, Lobo E, Shah S, Rangan S, Dholakia Y. Pulmonary tuberculosis in Patna, India: Durations, delays, and health care seeking behaviour among patients identified through household surveys. Journal of epidemiology and global health. 2017;7(4):241–8. 10.1016/j.jegh.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demissie M, Lindtjorn B, Berhane Y. Patient and health service delay in the diagnosis of pulmonary tuberculosis in Ethiopia. BMC public health. 2002;2(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lorent N, Mugwaneza P, Mugabekazi J, Gasana M, Van Bastelaere S, Clerinx J, et al. Risk factors for delay in the diagnosis and treatment of tuberculosis at a referral hospital in Rwanda. The International Journal of Tuberculosis and Lung Disease. 2008;12(4):392–6. [PubMed] [Google Scholar]
- 19.Chanda-Kapata P, Kapata N, Masiye F, Maboshe M, Klinkenberg E, Cobelens F, et al. Health seeking behaviour among individuals with presumptive tuberculosis in Zambia. PloS one. 2016;11(10):e0163975 10.1371/journal.pone.0163975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pronyk P, Makhubele M, Hargreaves J, Tollman S, Hausler H. Assessing health seeking behaviour among tuberculosis patients in rural South Africa. The International Journal of Tuberculosis and Lung Disease. 2001;5(7):619–27. [PubMed] [Google Scholar]
- 21.Getnet F, Demissie M, Assefa N, Mengistie B, Worku A. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: systematic review and meta-analysis. BMC pulmonary medicine. 2017;17(1):202 10.1186/s12890-017-0551-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Wyk S, Enarson D, Beyers N, Lombard C, Hesseling A. Consulting private health care providers aggravates treatment delay in urban South African tuberculosis patients. The International Journal of Tuberculosis and Lung Disease. 2011;15(8):1069–76. 10.5588/ijtld.10.0615 [DOI] [PubMed] [Google Scholar]
- 23.Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PloS one. 2013;8(2):e54978 10.1371/journal.pone.0054978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith F. The quality of private pharmacy services in low and middle-income countries: a systematic review. Pharmacy world & science. 2009;31(3):351–61. [DOI] [PubMed] [Google Scholar]
- 25.Claassens M, Jacobs E, Cyster E, Jennings K, James A, Dunbar R, et al. Tuberculosis cases missed in primary health care facilities: should we redefine case finding? The International Journal of Tuberculosis and Lung Disease. 2013;17(5):608–14. 10.5588/ijtld.12.0506 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DTA)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.