Abstract
Background
Although almost every state medical marijuana (MM) law identifies cancer as a qualifying condition, little research supports MM’s use in oncology. We hypothesized that the discrepancy between these laws and the scientific evidence base poses clinical challenges for oncologists. Oncologists’ beliefs, knowledge, and practices regarding MM were examined in this study.
Methods
In November 2016, we mailed a survey on MM to a nationally-representative, random sample of 400 medical oncologists. Main outcome measures included whether oncologists reported discussing MM with patients, recommended MM clinically in the past year, or felt sufficiently informed to make such recommendations. The survey also queried oncologists’ views on MM’s comparative effectiveness for several conditions (including its use as an adjunct to standard pain management strategies) and its risks compared with prescription opioids. Bivariate and multivariate analyses were performed using standard statistical techniques.
Results
The overall response rate was 63%. Whereas only 30% of oncologists felt sufficiently informed to make recommendations regarding MM, 80% conducted discussions about MM with patients, and 46% recommended MM clinically. Sixty-seven percent viewed it as a helpful adjunct to standard pain management strategies, and 65% thought MM is equally or more effective than standard treatments for anorexia and cachexia.
Conclusion
Our findings identify a concerning discrepancy between oncologists’ self-reported knowledge base and their beliefs and practices regarding MM. Although 70% of oncologists do not feel equipped to make clinical recommendations regarding MM, the vast majority conduct discussions with patients about MM and nearly one-half do, in fact, recommend it clinically. A majority believes MM is useful for certain indications. These findings are clinically important and suggest critical gaps in research, medical education, and policy regarding MM.
INTRODUCTION
Although cannabis remains illegal under federal law in the United States, 30 states and the District of Columbia have enacted medical marijuana (MM) laws, with cancer as a qualifying condition in all but one.1 MM refers to the nonpharmaceutical cannabis products that health care providers may recommend for therapeutic purposes in compliance with state law, and therapeutic marijuana to nonpharmaceutical cannabis products used with medicinal intent, whether or not in compliance with state law. Medical marijuana comes in myriad strains, with differing potencies of active ingredients. It may be smoked, vaporized, ingested, taken sublingually, or applied topically.
To date, no randomized clinical trials of whole-plant MM have been conducted in oncology populations, leaving oncologists to extrapolate from research completed on pharmaceutical cannabinoids or to draw upon evidence gathered from patients with other diseases. Oral synthetic tetrahydrocannabinol (THC) has achieved US Food and Drug Administration approval for chemotherapy-induced nausea and vomiting, and a sublingual pharmaceutical cannabis extract has shown promise in the management of cancer pain. However, cannabis’ several hundred active ingredients, which include phytocannabinoids, phenols, and terpenes, work both synergistically and as inhibitors through “entourage effects.”2-4 Therefore, comparisons between whole-plant MM and pharmaceutical cannabinoids that contain one or two active ingredients are speculative. In diseases other than cancer, eight small, short, randomized controlled trials reported that whole-plant cannabis possesses analgesic properties, and two observational studies have documented that MM laws are associated with statewide reductions in opioid-related hospitalizations and deaths; however, no randomized controlled trials have compared MM with standard pain regimens.5-14 Support for other potential cancer-related uses for whole-plant cannabis (eg, nausea, vomiting, anorexia, cachexia) is based on lower-quality evidence.3,4,15
Although three prior studies examined oncologists’ views on MM, all limited their inquiries to cannabis used as an antiemetic (despite many other potential oncologic indications) and all were completed before the passage of MM laws in the United States (and some were completed before the emergence of 5HT3 receptor blockers, now standard of care for chemotherapy-induced nausea and vomiting). In the first study (N = 2,430; response rate, 43%), nearly one-half of respondents reported that they would prescribe cannabis to some of their patients it is was if legalized.16 A second study (N = 180; response rate, 78%) found that, combined, cannabis and pharmaceutical synthetic THC ranked ninth on a list of management strategies for chemotherapy-induced nausea and vomiting.17 The third study (N = 2,430; response rate, 75%) indicated that only 1% of oncologists had recommended smoked marijuana to patients in the preceding 24 months.18
To the best of our knowledge, there have been few scientific inquiries into the views of physicians practicing in the era of MM laws. A 2010 survey (N = 1,727; response rate, 30%) of family physicians practicing in Colorado demonstrated that only one-fifth of respondents believed physicians should recommend MM.19 Less than one-third thought cannabis possesses significant health benefits, and well over one-half believed it carries significant health risks. Of note, those who endorsed making MM recommendations cited cancer and cachexia as frequent indications.
Given this background, we wondered whether the absence of data from randomized controlled trials testing MM’s efficacy for treatment of cancer-related symptoms would pose challenges for medical oncologists. We surveyed a nationally representative random sample of medical oncologists in the United States regarding their attitudes toward MM’s comparative efficacy and safety, their practices around clinical discussions regarding therapeutic cannabis, and whether they considered themselves adequately informed to make recommendations on the subject. We also explored factors associated with their beliefs and practices. We hypothesized that oncologists would report being insufficiently informed about MM, reticent to discuss or recommend therapeutic marijuana clinically, and skeptical about MM’s utility in cancer care given the limited evidence base.
METHODS
Study Design
Survey development.
The questionnaire included items from existing surveys, as well as new questions. The new items were frequently based on semistructured interviews with key oncology informants.20 The survey was pretested using five cognitive interviews with oncologists from states with and without MM. The final survey (Data Supplement) included 30 questions and took approximately 10 minutes to complete. The survey defined MM as nonpharmaceutical cannabis that health care providers recommend for therapeutic purposes. It made clear that MM does not refer to pharmaceutical-grade cannabinoids such as orally ingested synthetic THC analogs, dronabinol, and nabilone. This study was approved by institutional review boards at the Dana-Farber Cancer Institute and the University of Massachusetts Boston.
Sample.
A nationally representative sample of oncologists was drawn from commercially available data owned by SK&A Healthcare Databases (Irvine, CA).21 The sample included all board-certified oncologists in medical, gynecologic, neurologic, pediatric, and hematologic oncology who self-reported active participation in patient care. Radiation oncologists, resident physicians, retired physicians, and those in the military were excluded. From the list of 16,783, we selected a simple, random sample of 400 medical oncologists.
Administration.
The Center for Survey Research (CSR) at University of Massachusetts Boston administered the survey via US Postal Service priority mail between November 2016 and January 2017. The mailing included a prepaid return envelope, $50 cash incentive, cover letter, fact sheet, anonymous questionnaire, and anonymity-preserving postcard (linked to identifiers, mailed back separately from the survey, and used to remove names from the sample list). Approximately 1 week later, CSR sent (via first-class mail) reminder postcards to those who had not yet responded. Approximately 3 weeks after the first survey, CSR called nonrespondents and, thereafter, released a final mailing.
Measurements
Clinical discussions, recommendations, and knowledge.
The survey asked, “When you discuss MM with your oncology patients, who typically starts the conversation?” Response categories were as follows: “More often me,” “Sometimes me and sometimes patients or their families,” “More often patients and their families,” and “I have not discussed medical marijuana with my oncology patients or families.” For analyses, responses were dichotomized to “not discussed” versus “discussed.”
The survey asked, “In the past year, for about how many patients did you recommend marijuana for cancer related issues?” Respondents were to write in the number. Responses were dichotomized to “zero” versus “at least once.”
Finally, the survey asked, “Do you feel you have sufficient knowledge about the medicinal use of marijuana to make recommendations to oncology patients?” Response categories were “Yes” or “No.”
Comparative effectiveness.
The survey asked, “Compared to treatments you typically use, how would you rate the effectiveness of MM for the following cancer related conditions?” Conditions included pain, poor appetite/cachexia, nausea/vomiting, depression, anxiety, poor sleep, and general coping. Responses included the following: “Much more effective,” “Somewhat more effective,” “Equally effective,” “Somewhat less effective,” “Much less effective,” and “I do not know.” Responses were collapsed to “equally or more effective,” “less effective,” and “do not know.” For bivariate and multivariate analyses, responses were dichotomized to “equally or more effective” versus the other categories.
The survey asked, “To what extent do you think MM is a useful adjunct to standard treatments for the following cancer-related issues?” Pain was among the conditions listed. Response categories included “To a great extent,” “To some extent,” “To a very little extent,” and “Not at all.” For bivariate and multivariate analyses, responses were dichotomized to “to some or a great extent” versus “very little or not at all.”
Comparative risks.
The survey asked, “In your opinion, how do the risks of MM compare to the risk of prescription opioids?” Risks included paranoia/psychosis, anxiety, depression, confusion/impaired mentation, falls, addiction, and overdose death. Response categories included “Much higher than opioids,” “Somewhat higher than opioids,” “Comparable to opioids,” “Somewhat lower than opioids,” “Much lower than opioids,” and “I do not know.” For bivariate and multivariate analyses, responses were dichotomized to “lower than opioids,” which included “somewhat lower than opioids” and “much lower than opioids” versus other categories.
Predictors.
A priori specified independent variables included oncologists’ sex, ethnicity (categorized as white, Asian, or other), medical school (ie, foreign, US/Canada), years since medical school graduation, and whether they had a medical school appointment (yes/no). We also examined practice characteristics, including setting (ie, hospital, nonhospital), region (determined by zip code: Northeast, South, Midwest, and West), whether the practice state allowed MM use by patients with cancer (identified by zip code), and patient volume. To assess the latter, the survey asked, “In a typical week, approximately how many cancer patients do you see?” Written responses were grouped into “< 40 patients per week,” “40 to 59 patients per week,” and “≥ 60 patients per week.”
Analysis
The data were summarized using frequencies and percentages. For each outcome variable, two of the authors (Y.C. and L.Y.) conducted bivariate and multivariate analyses. In bivariate analyses, relationships between potential predictors and each outcome were examined using χ2 tests. Variables significant at the 0.1 level were considered as candidates for the multivariable logistic regression models. We used the stepwise variable selection techniques with entry and removal criteria set at P = .05. Final models were determined on the basis of evaluation of significance level and Akaike information criterion, in conjunction with sample size consideration of 10 respondents per variable. A two-sided P < .05 was considered statistically significant. Analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC).
RESULTS
Medical Oncologists’ Characteristics
Of the 400 medical oncologists sampled, 24 were ineligible because they were retired, too ill, deceased, no longer practicing, not locatable, or away from practice for the study’s duration. Of the remaining 376 eligible medical oncologists, 237 completed a survey, yielding a raw response rate of 63.0%.
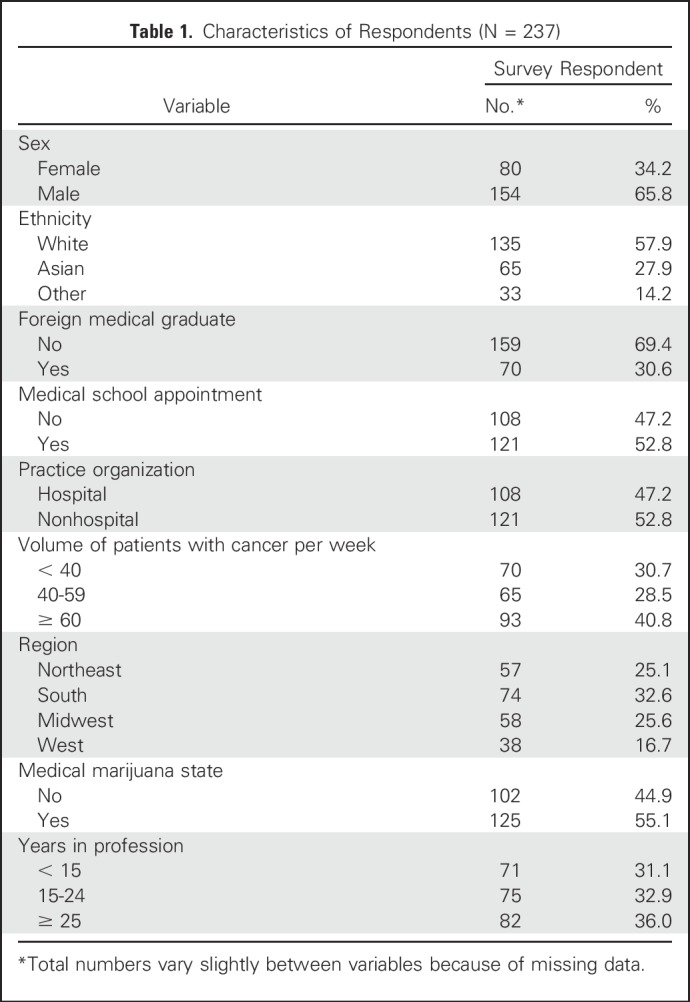
Among respondents, 65.8% were male, 57.9% were white, 36.0% completed oncology training ≥ 25 years ago, 52.8% held a medical school appointment, 52.8% practiced outside of a hospital setting, and 40.8% saw more than 60 patients per week (Table 1). The largest proportion of respondents practiced in the South (32.6%) and 55.1% practiced in a state in which MM was legalized. Limited information was available on nonrespondents; however, sex and practice region did not differ significantly between respondents and nonrespondents.
Table 1.
Characteristics of Respondents (N = 237)
Clinical Discussions, Recommendations, and Knowledge
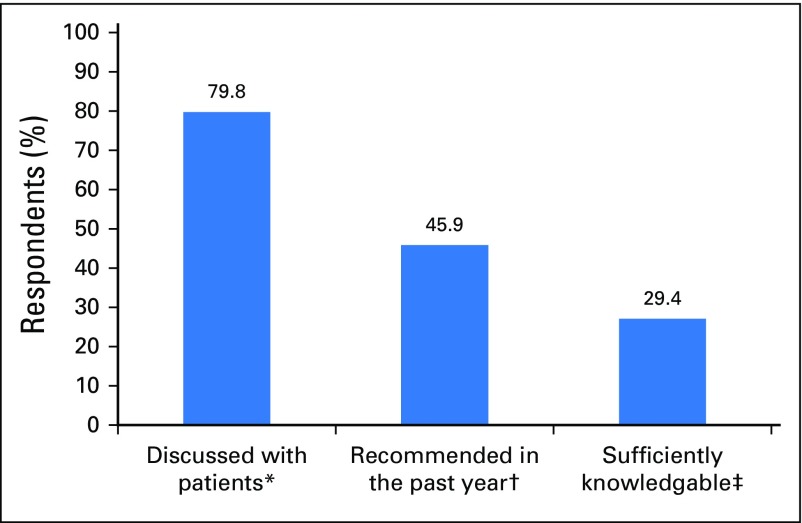
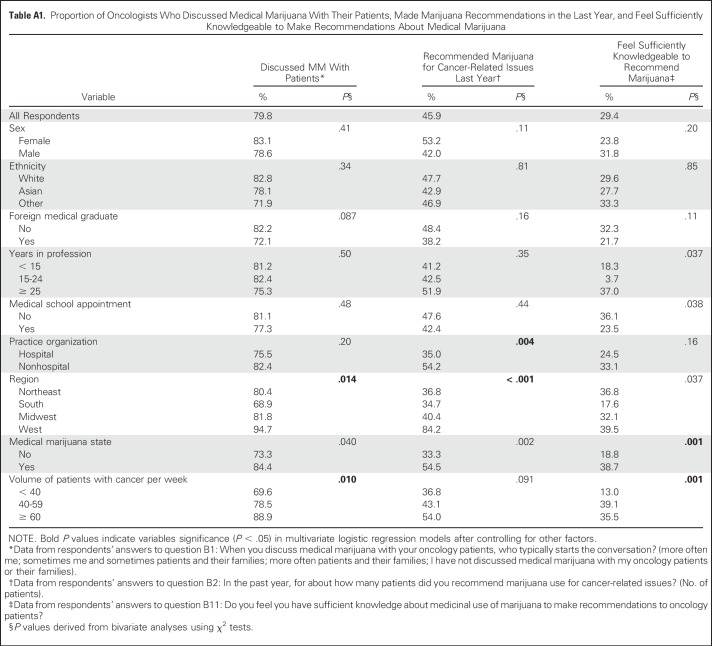
Among respondents, 79.8% reported having discussed MM with patients or their families, and 45.9% reported recommending marijuana for cancer-related issues to at least one patient in the past year (Fig 1). Oncologists practicing in the South were least likely to have discussed MM with patients or their families and those practicing in the West were most likely to have done so (68.9% v 94.7%, respectively; bivariate P = .014, multivariate P = .02). Of those in the South, 34.7% had recommended MM compared with 84.2% in the West (P < .001 in both bivariate and multivariate analyses). High practice volume (≥ 60 patients per week) was associated with an increased likelihood of an oncologist reporting having conducted MM discussions—88.9% versus 78.5% (40 to 59 patients per week) versus 69.6% (< 40 patients per week; bivariate P = .01, multivariate P = .006). Practicing outside a hospital setting was also associated with recommending MM (54.2% v 35.0% of hospital-based oncologists; bivariate P = .004, multivariate P = .008; Appendix Table A1, online only). Seventy-eight percent of the 186 oncologists who endorsed discussing MM with their patients reported that these conversations were more often initiated by the patients and their families than by the oncologist.
Fig 1.
Oncologists’ practices and knowledge regarding medicinal marijuana. (*) Data from respondents’ answers to question B1: When you discuss medical marijuana with your oncology patients, who typically starts the conversation? (More often me; sometimes me and sometimes patients and their families; more often patients and their families; I have not discussed medical marijuana with my oncology patients or their families). (†) Data from respondents’ answers to question B2: In the past year, for about how many patients did you recommend marijuana use for cancer-related issues? (No. of patients). (‡) Data from respondents’ answers to question B11: Do you feel you have sufficient knowledge about medicinal use of marijuana to make recommendations to oncology patients? (Yes/No).
Slightly more than one-quarter (29.4%) of oncologists felt sufficiently knowledgeable to make recommendations regarding MM. Among the 45.9% who reported recommending marijuana clinically in the past year, 56.2% did not consider themselves to have sufficient knowledge to make a recommendation. In multivariate analyses, oncologists practicing in states with MM laws and those with high practice volumes (≥ 60 patients per week) were more likely to report feeling knowledgeable enough to make recommendations (both P = .002; Appendix Table A1).
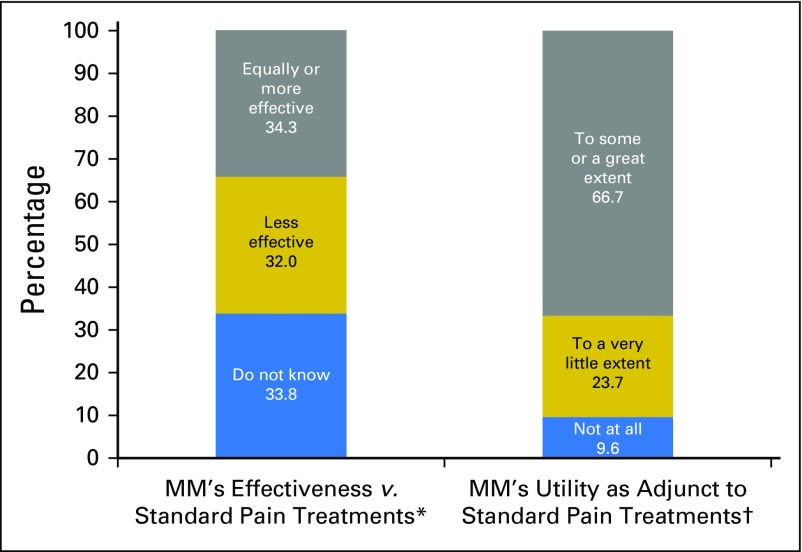
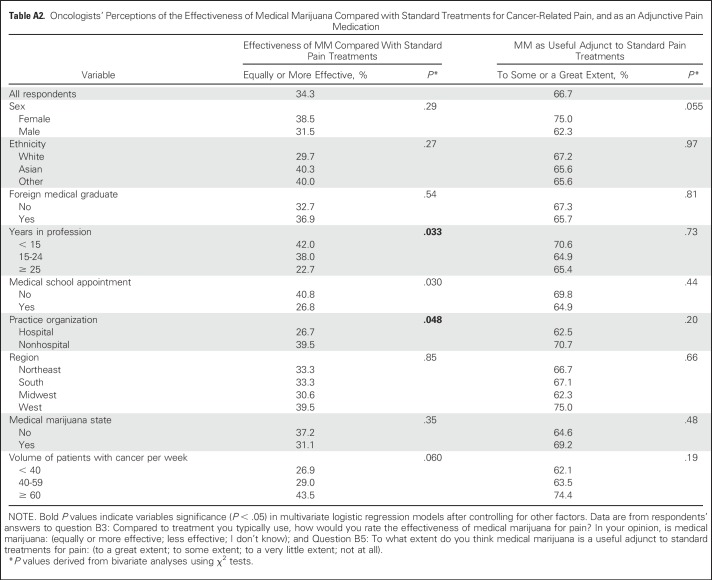
Comparative Effectiveness of Medical Marijuana
Oncologists were divided in their perceptions of MM as an analgesic: 34.3% viewed MM as equal or more effective than standard pain treatments, 32.0% perceived it as less effective, and 33.8% reported they did not know. When asked whether MM is a useful adjunct to standard pain therapies, 66.7% responded “to a great extent” or “to some extent,” 23.7% responded “to a very little extent,” and 9.6% gave the response of “not at all” (Fig 2). In multivariate analyses, oncologists who were < 15 years from their terminal degree were more likely than those > 25 years from their terminal degree to describe MM as equally or more effective than standard treatments for pain (42.0% v 22.7%, respectively; bivariate P = .03, multivariate P = .047); the same was true for those practicing in nonhospital settings v those practicing in hospital settings (39.5% v 26.7%, respectively; bivariate P = .048, multivariate P = .049; Appendix Table A2, online only).
Fig 2.
Oncologists’ views on the effectiveness of medical marijuana for pain management. (*) Data from respondents’ answers to question B3b: Compared to treatment you typically use, how would you rate the effectiveness of medical marijuana for pain? In your opinion, is medical marijuana: (much more effective; somewhat more effective; equally effective; somewhat less effective; much less effective; I don’t know). Responses were regrouped into the categories listed in the first bar. (†) Data from respondents’ answers to question B5a: To what extent do you think medical marijuana is a useful adjunct to standard treatments for pain? (to a great extent; to some extent; to a very little extent; not at all). Responses were regrouped into the categories listed in the right bar.
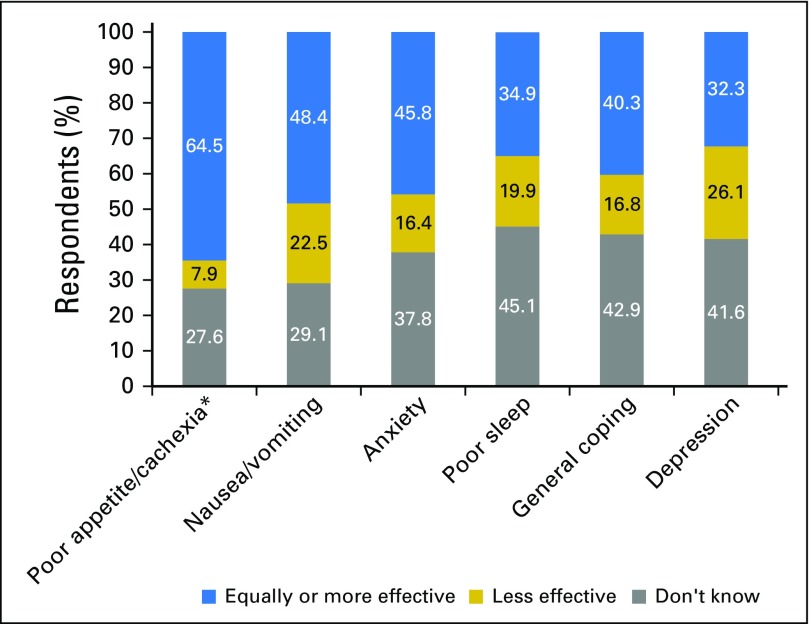
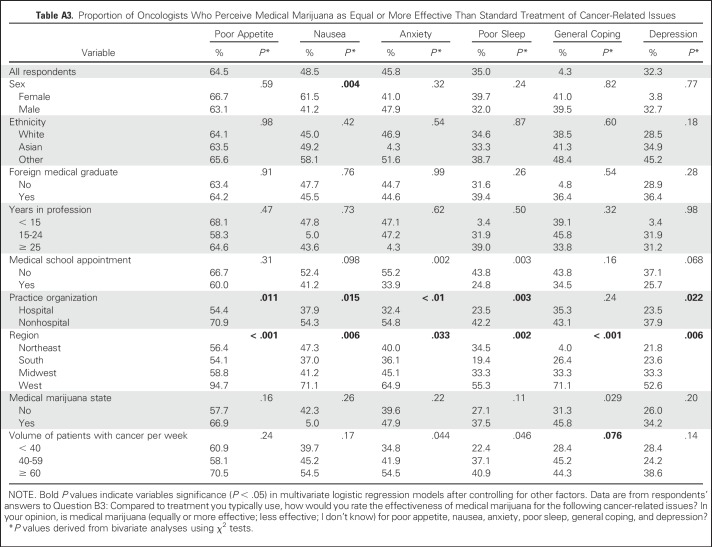
Regarding poor appetite/cachexia, 64.5% of oncologists considered MM equally or more effective than standard treatments. For cancer-related nausea and vomiting, fewer than one-half (48.4%) reported MM to be equally or more effective than standard treatments. Oncologists’ perceptions of MM for other indications, relative to standard treatments, were similar: 45.8% indicated it was equally or more effective for anxiety; 40.3%, for general coping; and 34.9%, for poor sleep (Fig 3). Oncologists also frequently responded, “I do not know,” although responses differed by condition (ranging from 27.6% for poor appetite/cachexia to 45.1% for poor sleep; Appendix Table A3, online only).
Fig 3.
Proportion of oncologists who view medical marijuana as equally or more effective than standard treatments for cancer-related conditions. (*) Data from respondents’ answers to question B3: Compared to treatment you typically use, how would you rate the effectiveness of medical marijuana for the following cancer-related issues? In your opinion, is medical marijuana: (much more effective; somewhat more effective; equally effective; somewhat less effective; much less effective, I don’t know). Responses were regrouped into the following categories for each condition: Equally or more effective (blue), less effective (gold), do not know (gray).
Compared with other regions, oncologists practicing in the South were less likely, and those practicing in the West were more likely, to view MM as equally or more effective than standard treatments (eg, 54.1% v 94.7%, respectively, for poor appetite; bivariate P < .001, multivariate P = .005). Oncologists practicing outside of hospitals were more likely than hospital-based oncologists to view MM as equally or more effective than standard treatments for most indications (eg 54.8% v 32.4%, respectively for anxiety; bivariate P < .001, multivariate P = .001). Women were more likely than men to view MM as equally or more effective than standard treatments for nausea or vomiting (61.5% v 41.2%, respectively; bivariate P = .004, multivariate P = .014).
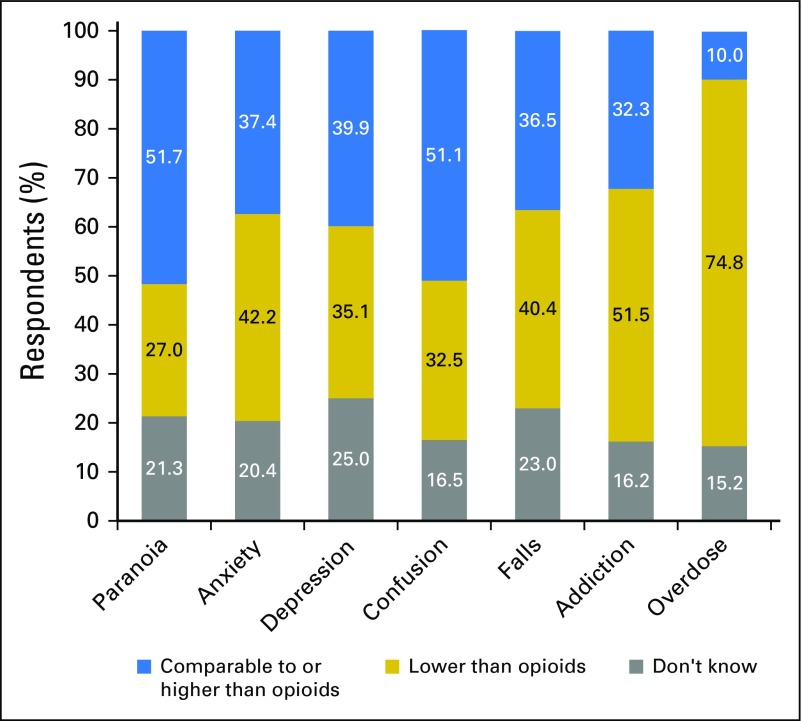
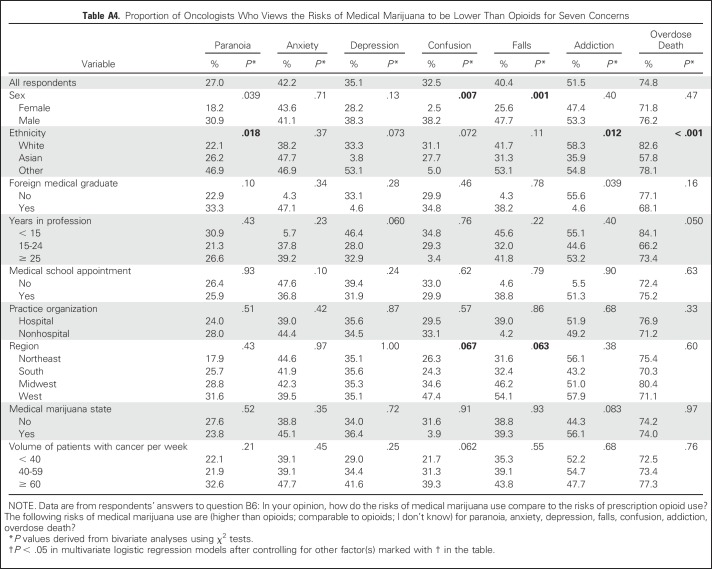
Risks of Medical Marijuana Versus Opioids
Most respondents viewed MM as presenting a lower risk than opioids for overdose death (74.8%) and addiction (51.5%); however, they perceived MM as presenting a comparable or higher risk than opioids for paranoia (51.7%) and confusion (51.1%; Fig 4). These findings varied by sex and racial group (Appendix Table A4, online only).
Fig 4.
Oncologists’ views on the comparative risks of medical marijuana versus opioids for adverse outcomes. Data from respondents’ answers to question B6: In your opinion, how do the risks of medical marijuana use compare to the risks of prescription opioid use? The following risks of medical marijuana use are: (much higher than opioids; somewhat higher than opioids; comparable with opioids; somewhat lower than opioids; much lower than opioids, I don’t know). Responses were regrouped into the following categories for each risk: Comparable to or higher than opioids (blue), lower than opioids (gold), do not know (gray).
DISCUSSION
To our knowledge, this study represents the first nationally representative investigation of medical oncologists’ attitudes, knowledge, and practices regarding MM since the advent of MM laws in the United States. Most respondents (80%) reported conducting discussions about MM with patients, and 46% reported recommending use of MM in the past year. These data highlight the salience of MM in today’s cancer care. However, our data also reveal concerning gaps in efficacy data and education; only 30% of oncologists reported feeling sufficiently knowledgeable to make MM recommendations, and more than one-half (56%) of those who made clinical recommendations considered themselves insufficiently knowledgeable to do so. Although our survey could not determine why oncologists recommend MM, it may be because they regard MM as an alternative therapy that is difficult to evaluate given sparse randomized controlled trial data. Alternatively, oncologists may have anecdotal experience with MM or respond to patient pressure in the face of a wave of state MM legalizations. Indeed, more than three-quarters of respondents reported that clinical conversations around MM are initiated by patients and their families more often than by the oncologists.
One focus of the study was the comparative effectiveness of MM as a treatment of cancer-related issues, including pain. Although our data demonstrate a lack of professional consensus regarding MM as a primary treatment of pain, more than two-thirds of respondents supported using MM as an adjunct to standard pain management strategies. These findings may reflect oncologists’ familiarity with the positive results of several small, randomized, placebo-controlled trials of MM for pain (although none in cancer populations, and none comparing MM to standard of care). These findings may also reflect the majority belief, identified in this study, that MM carries lower risk than opioids for addiction and overdose death.
Nearly two-thirds of oncologists reported that MM is equally or more effective than standard therapies for anorexia/cachexia. Given the lack of empirical evidence to support this assertion, the finding is surprising. It may reflect the extremely limited options available to treat anorexia/cachexia, or the fact that oncologists are extrapolating from their clinical experience with dronabinol, a synthetic THC pharmaceutical frequently used in oncology and approved by the US Food and Drug Administration for these indications.4 Less surprising was that a large percentage of oncologists reported not knowing the comparative effectiveness of MM for cancer-related issues. This finding likely reflects a lack of empirical evidence regarding the therapeutic use of MM in general.
We observed significant differences in the attitudes and practices of oncologists based on nonclinical factors. For example, oncologists practicing in the South were more likely to hold negative views—and those practicing in the West, positive views—of MM’s comparative effectiveness. This finding may be due to MM’s status as a politicized health issue and regional sociopolitical differences.22 Unfortunately, our data did not permit us to examine political party or religious affiliations. Similarly, hospital-based oncologists were less likely to recommend marijuana as therapy, compared with those practicing outside hospital systems. This finding may be due to hospital administrations’ reluctance to draft policies permitting health care providers to recommend MM (for fear of losing federal licensure).23 Such findings deserve additional investigation.
Our study has several limitations, including a modest sample size, which can result in overestimates of effect sizes and low reproducibility of results, particularly for subgroup analyses. However, the sample size was sufficient to detect significant differences regarding several explanatory factors. As with all surveys, this study is vulnerable to nonresponse bias if nonrespondents differed systematically from respondents. However, we did not detect differences between respondents and nonrespondents based on sex or location of practice. Because of the nature of variable selection methods in general, other multivariable models may be plausible for some study outcomes. Finally, results are not generalizable to physicians in other specialties or those practicing in countries that have legalized MM on a federal level.
Despite these limitations, the study provides important national data on oncologists’ attitudes and practices regarding MM. Our data demonstrate that the vast majority of oncologists hold clinical discussions regarding MM and, generally, consider it a good augmentation strategy for cancer pain and equally or more effective than standard treatments for poor appetite/cachexia. Nearly one-half of oncologists have recommended medicinal use of marijuana, despite the study’s finding that a significant proportion do not feel sufficiently knowledgeable to make recommendations. Taken together, these findings identify a clinically problematic discrepancy between oncologists’ beliefs and practices and perceived knowledge regarding MM. They highlight a crucial need for expedited clinical trials exploring marijuana’s potential medicinal effects in oncology (eg, as an adjunctive pain management strategy or as a treatment of anorexia /cachexia) and the need for educational programs about MM, to inform oncologists who frequently confront questions regarding MM in daily practice.4 Last, state and institutional policies are needed that incentivize trainings of clinicians on this important issue.
Appendix
Table A1.
Proportion of Oncologists Who Discussed Medical Marijuana With Their Patients, Made Marijuana Recommendations in the Last Year, and Feel Sufficiently Knowledgeable to Make Recommendations About Medical Marijuana
Table A2.
Oncologists’ Perceptions of the Effectiveness of Medical Marijuana Compared with Standard Treatments for Cancer-Related Pain, and as an Adjunctive Pain Medication
Table A3.
Proportion of Oncologists Who Perceive Medical Marijuana as Equal or More Effective Than Standard Treatment of Cancer-Related Issues
Table A4.
Proportion of Oncologists Who Views the Risks of Medical Marijuana to be Lower Than Opioids for Seven Concerns
Footnotes
Listen to the podcast by Dr Tanco at ascopubs.org/jco/podcasts
AUTHOR CONTRIBUTIONS
Conception and design: Ilana M. Braun, John Peteet, Fremonta L. Meyer, David P. Yuppa, Dragana Bolcic-Jankovic, Lida Nabati, Eric G. Campbell
Collection and assembly of data: Ilana M. Braun, Dragana Bolcic-Jankovic, Jessica LeBlanc, Eric G. Campbell
Data analysis and interpretation: Ilana M. Braun, Alexi Wright, Fremonta L. Meyer, Dragana Bolcic-Jankovic, Yuchiao Chang, Liyang Yu, Manan M. Nayak, James A. Tulsky, Joji Suzuki, Eric G. Campbell
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Medical Oncologists’ Beliefs, Practices, and Knowledge Regarding Marijuana Used Therapeutically: A Nationally Representative Survey Study
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Ilana M. Braun
No relationship to disclose
Alexi Wright
No relationship to disclose
John Peteet
No relationship to disclose
Fremonta L. Meyer
Honoraria: UpToDate, American Physician Institute
David P. Yuppa
No relationship to disclose
Dragana Bolcic-Jankovic
No relationship to disclose
Jessica LeBlanc
No relationship to disclose
Yuchiao Chang
No relationship to disclose
Liyang Yu
No relationship to disclose
Manan M. Nayak
No relationship to disclose
James A. Tulsky
No relationship to disclose
Joji Suzuki
No relationship to disclose
Lida Nabati
Patents, Royalties, Other Intellectual Property: Royalties from Wolters Kluwer from UptoDate publication
Eric G. Campbell
Expert Testimony: Law firms that I assume are for-profit companies
REFERENCES
- 1.National Conference of State Legislatures : State medical marijuana laws http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx
- 2.Johnson JR, Burnell-Nugent M, Lossignol D, et al. : Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage 39:167-179, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Whiting PF, Wolff RF, Deshpande S, et al. : Cannabinoids for medical use: A systematic review and meta-analysis. JAMA 313:2456-2473, 2015 [DOI] [PubMed] [Google Scholar]
- 4.McCormick MC: The Health Effects of Cannabis and Cannabinoids: Current State of Evidence and Recommendations for Research. Washington, DC, National Academies Press, 2017 [PubMed] [Google Scholar]
- 5.Wallace M, Schulteis G, Atkinson JH, et al. : Dose-dependent effects of smoked cannabis on capsaicin-induced pain and hyperalgesia in healthy volunteers. Anesthesiology 107:785-796, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Abrams DI, Jay CA, Shade SB, et al. : Cannabis in painful HIV-associated sensory neuropathy: A randomized placebo-controlled trial. Neurology 68:515-521, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Wilsey B, Marcotte T, Tsodikov A, et al. : A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain 9:506-521, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ellis RJ, Toperoff W, Vaida F, et al. : Smoked medicinal cannabis for neuropathic pain in HIV: A randomized, crossover clinical trial. Neuropsychopharmacology 34:672-680, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ware MA, Wang T, Shapiro S, et al. : Smoked cannabis for chronic neuropathic pain: A randomized controlled trial. CMAJ 182:E694-E701, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corey-Bloom J, Wolfson T, Gamst A, et al. : Smoked cannabis for spasticity in multiple sclerosis: A randomized, placebo-controlled trial. CMAJ 184:1143-1150, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilsey B, Marcotte T, Deutsch R, et al. : Low-dose vaporized cannabis significantly improves neuropathic pain. J Pain 14:136-148, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace MS, Marcotte TD, Umlauf A, et al. : Efficacy of inhaled cannabis on painful diabetic neuropathy. J Pain 16:616-627, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi Y: Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend 173:144-150, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bachhuber MA, Saloner B, Cunningham CO, et al. : Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med 174:1668-1673, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vinciguerra V, Moore T, Brennan E: Inhalation marijuana as an antiemetic for cancer chemotherapy. N Y State J Med 88:525-527, 1988 [PubMed] [Google Scholar]
- 16.Doblin RE, Kleiman MA: Marijuana as antiemetic medicine: A survey of oncologists’ experiences and attitudes. J Clin Oncol 9:1314-1319, 1991 [DOI] [PubMed] [Google Scholar]
- 17.Schwartz RH, Beveridge RA: Marijuana as an antiemetic drug: how useful is it today? Opinions from clinical oncologists. J Addict Dis 13:53-65, 1994 [DOI] [PubMed] [Google Scholar]
- 18.Schwartz RH, Voth EA, Sheridan MJ: Marijuana to prevent nausea and vomiting in cancer patients: A survey of clinical oncologists. South Med J 90:167-172, 1997 [DOI] [PubMed] [Google Scholar]
- 19.Kondrad E, Reid A: Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med 26:52-60, 2013 [DOI] [PubMed] [Google Scholar]
- 20.Braun IM, Meyer FL, Gagne JJ, et al. : Experts’ perspectives on the role of medical marijuana in oncology: A semistructured interview study. Psychooncology 26:1087-1092, 2017 [DOI] [PubMed] [Google Scholar]
- 21. http://www.skainfo.com/ SK&A Web Site.
- 22.Hersh ED, Goldenberg MN: Democratic and Republican physicians provide different care on politicized health issues. Proc Natl Acad Sci USA 113:11811-11816, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Durkin M: Medical marijuana…in the hospital? https://acphospitalist.org/archives/2017/01/marijuana-policies-hospital.htm