Abstract.
Cysticercosis, caused by Taenia solium, is a neglected disease that causes preventable epilepsy. We conducted an experiential learning workshop in northern Peru to educate community members on T. solium transmission and motivate participation in community-led prevention and control. The workshop included presentation of local economic and epidemiologic data, followed by hands-on participation in pig dissection, group discussion of the T. solium life cycle, and viewing of eggs and nascent tapeworms with light microscopes. Among heads of household, we used community survey data to compare knowledge of the three-stage parasite life cycle at baseline and 2 months postworkshop. Knowledge of the life cycle increased significantly after the workshop, with greater gains for workshop attendees than non-attendees. Prior knowledge and workshop attendance were significant predictors of postworkshop knowledge. The use of local evidence and experiential learning positively affected knowledge of T. solium transmission, laying the foundation for subsequent community-engaged control efforts.
Taenia solium, commonly known as pork tapeworm, causes taeniasis/cysticercosis and preventable epilepsy. Although the parasite life cycle can be interrupted by adopting basic sanitation and closed-pen pig-rearing practices, understanding the parasite life cycle and changing deeply engrained practices are two key barriers to decreasing disease prevalence in endemic areas. In our previous work, classic health promotion strategies (promotional flyers, informational talks, and radio announcements) did not decrease T. solium transmission, nor result in long-term behavior change.1 In other countries, classic health promotion approaches have had varying success increasing knowledge of the complete two-host life cycle.2–7 Strategies including community participation have demonstrated effectiveness in T. solium education and prevention.8 Participatory methods have been shown to increase disease knowledge, promote lasting community change, and decrease disease incidence when applied to community-level control efforts of other neglected infectious diseases in similarly resourced settings.8,9 To date, interventions that integrate biomedical and participatory approaches have been suggested as promising T. solium control strategies, yet have rarely been incorporated into education-focused interventions.8,10
Critical theory emphasizes the value of democratizing learning, with the goal of co-creating knowledge through equitable partnership and shared experience.11 Applied critical theory has been successfully used to develop a methodology where physical, economic, and local epidemiologic evidence sharing stimulated dialogue and community-directed dengue surveillance, prevention, and control in Nicaragua.9 We adapted this methodology to develop, pilot, and evaluate a workshop where attendees participated in each stage of a cysticercosis-infected pig necropsy (i.e., autopsy) and observed cyst evagination (birth of tapeworm from larval cyst). The goals of the workshop were to promote trust through transparent actions, improve participants’ knowledge of T. solium transmission, and stimulate interest in subsequent community-led surveillance. Observations and insights from community members, including perceptions and beliefs shared during the workshop, were incorporated into subsequent planning of a larger intervention.
In February 2017, we implemented workshops in four rural villages. This study was reviewed and approved by the Institutional Review Boards at Universidad Peruana Cayetano Heredia (UPCH) and Oregon Health & Science University (OHSU). Adult participants provided written informed consent, and parent or guardian consent was required for participation of minors. The study was reviewed and approved by the Institutional Ethics Committee for the Use of Animals at UPCH as well as the Institutional Animal Use and Care Committee at OHSU. Treatment of animals adhered to the Council for International Organizations of Medical Sciences International Guiding Principles for Biomedical Research Involving Animals. Adolescents and adults were invited by door-to-door invitation to a “Healthy Pig Fair,” and children were invited to a “Parasite Birthday Party.” Promotional posters highlighting the opportunity to view the parasite with a microscope were displayed publicly. Taenia solium–infected pigs were purchased from nearby communities enrolled in a separate control intervention. Infection was confirmed by tongue inspection and computed tomography at the Center for Global Health, Tumbes, before the workshop. One pig was killed per workshop. Later workshop iterations used pigs identified by and donated within the community where the workshop was held.
Each workshop began with pig tongue examination to demonstrate the screening method for cysticercosis in live pigs. The examination was performed by a volunteer who received guided instruction. Next, we facilitated a conversation on the economic consequences of porcine cysticercosis, weighed the pig, and calculated the monetary loss due to infection of the pig. The pig was humanely euthanized and the carcass portioned. Attendees were encouraged to observe the cyst-laden meat and ask questions. Simple village-specific figures describing the prevalence of porcine cysticercosis were presented using results from previously conducted serologic assays.
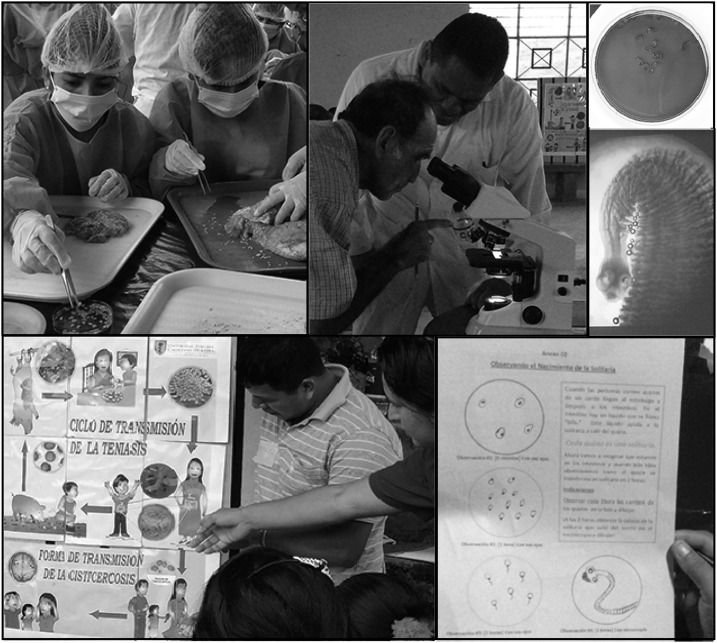
Next, attendees were invited to dissect the carcass in groups of 8–12, each led by two study staff. A biosecurity demonstration highlighted principles for safe dissection and use of personal protective equipment. Participants removed cysts from pig meat using forceps and scalpels, placing the cysts in distilled water (Figure 1A). After 15–20 minutes of dissection and informal discussion about cysticercosis, intact cysts were placed in Petri dishes containing bovine bile and incubated using a water bath maintained at 37°C for 1.5–2.0 hours.
Figure 1.
Images from evidence workshops (clockwise from top left): (A) Community members participate in pig dissection and remove cysticerci (Taenia solium larvae) from infected meat; (B) a community member looks at larvae through a microscope with assistance from a study team member; (C) Taenia solium larvae in bile solution after cyst evagination; (D) projection of the tapeworm viewed under the microscope; (E) completed worksheet showing community member’s observations during the workshop; (F) community members and a study team member discuss the T. solium life cycle. This figure appears in color at www.ajtmh.org.
Participants observed the process of evagination, tapeworm emergence from cysts, making observations every 30 minutes and sketching on a worksheet (Figure 1B–E). The purpose of the activity was to link the T. solium cyst stage in pigs to the adult tapeworm stage in humans—a link which our previous studies had demonstrated was conceptually difficult to grasp. Between observations, attendees practiced explaining the taeniasis–cysticercosis life cycle using figures on a poster board (Figure 1F). Once the cysts evaginated, attendees individually viewed the nascent tapeworm under the light microscope at 100× total magnification. A video of the view through the microscope was made using a cell phone for participants who had difficulty using the microscope. The role of microscopic eggs in human–human and human–pig transmission was explored by comparing varying egg sizes (chicken versus quail versus T. solium), followed by viewing a smear of T. solium eggs under the microscope (400× total magnification) and sketching the view on a worksheet. Smear slides were handled exclusively by the study staff to ensure the biosecurity of participants.
The workshop was adapted for children. Key differences included age-appropriate discussion of the life cycle and meat dissection led by the study staff. The children played games (including completion of a puzzle of the life cycle, explaining the life cycle to one another in groups, and forming a tapeworm conga line), completed the worksheet, and were encouraged to compare their sketches with their parents to reinforce parasite life-cycle understanding and encourage dialogue at the household level. Children’s understanding of the T. solium life cycle was observed during the session but was not formally assessed before or following the workshop.
Knowledge change before and after the workshop was measured by conducting head-of-household surveys 2 months pre-workshop and 2 months post-workshop. The survey included three open-ended questions: “What is the primary reason pigs have cysts?” “What is the primary reason humans get brain cysts?” “What is the primary reason humans get tapeworms?” Answers were classified as correct or incorrect. Additional qualitative data were gathered in focus group discussions 1 month post-workshop.
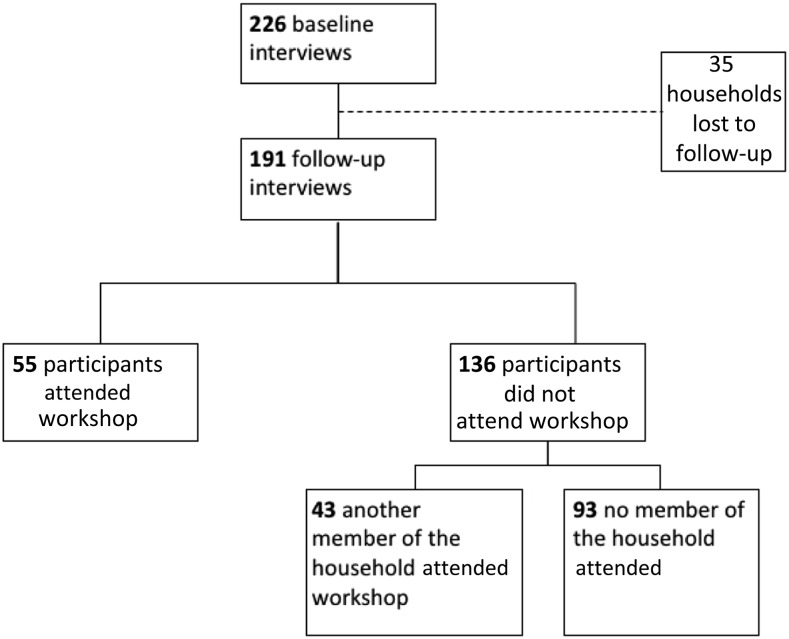
At baseline, there were 235 households in four villages. Adult education level was homogenous across villages. Workshop participation of ≥ 1 adult per household was 41/84 (49%), 25/34 (74%), 29/68 (43%), and 15/49 (31%) per village (Figure 2). Eighty-nine children (age range 9–16 years) attended the workshops adapted for children. Among the 55 heads of households who attended and participated in pre- and post-knowledge surveys, 20 were from households in which at least one child also attended the workshop. Among the 136 heads of households who did not attend and participated in pre- and post-knowledge surveys, 29 were from households in which at least one child attended. At follow-up, overall village-level knowledge gains were statistically significant, with greater gains among workshop attendees than non-attendees. Knowledge of human-to-pig transmission increased by 38% (P < 0.01) for attendees and 23% (P < 0.01) for non-attendees, whereas knowledge of pig-to-human transmission increased by 42% (P < 0.01) and 9% (P < 0.05), respectively (McNemar’s exact test). Only workshop attendees had statistically significant gains in knowledge of human-to-human transmission (12%, P < 0.05 versus 5%, P = 0.13). There were no significant differences in knowledge gains for people who lived with a household member who attended the workshop compared with households without workshop attendees. Binomial logistic regression was conducted to model the effects of baseline knowledge, workshop attendance, gender, and age on post-workshop knowledge (Table 1). For pig-to-human and human-to-pig transmission, baseline life-cycle knowledge and workshop attendance significantly predicted post-workshop knowledge. Knowledge of human-to-human transmission was not significantly predicted by any variable in the model.
Figure 2.
Summary of community participation in baseline and follow-up surveys by workshop attendance. According to community census, there were 235 households in the four intervention villages; of these, 226 households participated in the baseline survey.
Table 1.
Binominal logistic regression, predictors of postworkshop knowledge
| Stage of life cycle | Human-to-pig transmission | Pig-to-human transmission | Human-to-human transmission | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Baseline knowledge | 3.10 | 1.52–6.33 | *0.002 | 4.28 | 2.03–9.08 | *0.000 | 3.01 | 0.54–16.88 | 0.211 |
| Workshop attendance | 2.67 | 1.23–5.78 | *0.012 | 3.498 | 1.76–6.94 | *0.000 | 1.88 | 0.73–4.87 | 0.193 |
| Gender | 1.06 | 0.53–2.13 | 0.859 | 0.97 | 0.47–1.96 | 0.922 | 2.11 | 0.62–7.14 | 0.232 |
| Age | 0.99 | 0.97–1.01 | 0.380 | 0.997 | 0.98–1.02 | 0.797 | 0.99 | 0.96–1.03 | 0.73 |
Indicates statistical significance at 0.05 alpha level.
This workshop applied critical pedagogy to explore whether experiential learning could engage communities in dialogue about the health and economic consequences of T. solium. Attendees demonstrated improved knowledge of the T. solium life cycle, although improvement was not shared at the household level for non-attendees. Whereas baseline knowledge was the most significant predictor of post-workshop knowledge, workshop attendance was the second strongest predictor of knowledge gains, suggesting baseline knowledge likely primed people to augment their existing knowledge when they attended the workshop.
Limitations of this study include the need for technically trained staff to prepare materials, coordinate acquisition of pigs, and prepare laboratory materials. The use of experimental animals for educational purposes, although potentially controversial, was carried out in accordance with international animal welfare standards and was not described as distasteful by workshop participants, who are accustomed to animal slaughter in rural villages. The pigs used in the workshops were infected with T. solium and were otherwise subject to condemnation according to local public health regulations to protect the health of the community. These factors should be considered in planning similar workshops in other settings.
Although workshop attendance resulted in substantial knowledge gains, community participation in the workshops was incomplete and knowledge gains did not diffuse to community members who did not participate in the workshop. Post-workshop focus groups suggested differences may have been because of seeing physical evidence of the parasite firsthand. One attendee shared, “You have to go and listen and see with your own eyes, not just tell us or lie to us, but you have to go and see to believe.” Another attendee said, “I didn’t completely know the tapeworm and then, we saw it, in person, directly… the cysts developing for hours… it was something true that they gave us… to see how it really is.” These comments suggest observing the connection between pig cysts and human-dwelling tapeworms offered a substantial shift in understanding. Collectively, our quantitative and qualitative findings demonstrate the importance of hands-on learning and a physical connection to a previously abstract or invisible aspect of T. solium transmission. The workshop could be improved by highlighting physical evidence of human–human egg transmission in a separate module.
Presentation of locally relevant economic and epidemiologic evidence helped community members view T. solium endemicity as a community issue compared with previous efforts where disease epidemiology and consequences were vaguely discussed.1 In facilitated discussions, participants shared personal experiences with human and pig infection alongside other community members and explored the emotional effects of the disease, rather than solely rational aspects. Following the workshop, attendees linked what they saw under the microscope to a broader community problem, articulating, “The consequence of the parasite is that it can affect us, the pig parasite is affecting humans, and (taeniasis) in a person it can affect us all. No one is free… we can continue to affect (others). We are not free of the parasite.” Having identified the parasite as a problem, community members moved toward imagining solutions: “It is something very important where we should actually unite together so that we can fight this, because, as they say, ‘union makes strength,’ and all I know is that we all want our farms and our community to be clean of the parasite.” The workshop could be improved by having more dialogue surrounding the economic effects of cysticercosis in the community, and opportunity to discuss community prevention, surveillance, and treatment strategies. Behavior change was assessed as part of a larger intervention and is not included in this short report. This relatively low-cost and potentially scalable participatory workshop incorporated principles of critical theory, improved life-cycle knowledge, helped participants better understand the community’s risks of T. solium infection, and generated interest for future community organizing for T. solium surveillance, prevention, and control.
REFERENCES
- 1.Beam M, et al. 2018. Barriers to participation in a community-based program to control transmission of Taenia solium in Peru. Am J Trop Med Hyg 98: 1748–1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarti E, et al. 1997. Development and evaluation of a health education intervention against Taenia solium in a rural community in Mexico. Am J Trop Med Hyg 56: 127–132. [DOI] [PubMed] [Google Scholar]
- 3.Mwidunda SA, Carabin H, Matuja WBM, Winkler AS, Ngowi HA, 2015. A school based cluster randomised health education intervention trial for improving knowledge and attitudes related to Taenia solium cysticercosis and taeniasis in Mbulu District, northern Tanzania. PLoS One 10: e0118541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wohlgemut J, Dewey C, Levy M, Mutua F, 2010. Evaluating the efficacy of teaching methods regarding prevention of human epilepsy caused by Taenia solium neurocysticercosis in western Kenya. Am J Trop Med Hyg 82: 634–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alexander AM, Mohan VR, Muliyil J, Dorny P, Rajshekhar V, 2012. Changes in knowledge and practices related to taeniasis/cysticercosis after health education in a south Indian community. Int Health 4: 164–169. [DOI] [PubMed] [Google Scholar]
- 6.Ngowi HA, Carabin H, Kassuku AA, Mlozi MRS, Mlangwa JED, Willingham AL, 2008. A health-education intervention trial to reduce porcine cysticercosis in Mbulu District, Tanzania. Prev Vet Med 85: 52–67. [DOI] [PubMed] [Google Scholar]
- 7.Ngowi HA, Mlangwa JE, Mlozi MR, Tolma EL, Kassuku AA, Carabin H, Willingham AL, III, 2009. Implementation and evaluation of a health-promotion strategy for control of Taenia solium infections in northern Tanzania. Int J Health Promot Educ 47: 24–34. [Google Scholar]
- 8.Carabin H, et al. 2018. Effectiveness of a community-based educational programme in reducing the cumulative incidence and prevalence of human Taenia solium cysticercosis in Burkina Faso in 2011–14 (EFECAB): a cluster-randomised controlled trial. Lancet Glob Health 6: e411–e425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andersson N, et al. 2015. Evidence based community mobilization for dengue prevention in Nicaragua and Mexico (Camino Verde, the Green Way): cluster randomized controlled trial. BMJ 351: h3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bardosh K, Inthavong P, Xayaheuang S, Okello AL, 2014. Controlling parasites, understanding practices: the biosocial complexity of a one health intervention for neglected zoonotic helminths in northern Lao PDR. Soc Sci Med 120: 215–223. [DOI] [PubMed] [Google Scholar]
- 11.Freire P, 2000. Pedagogy of the Oppressed, 3rd edition New York, NY: Continuum. [Google Scholar]