Supplemental Digital Content is Available in the Text.
Key Words: gender, structural drivers, masculinity, trauma, mental health, South Africa
Abstract
Background:
Qualitative research emphasizes men's experiences of trauma increase HIV risk. We seek to understand associations between experience of traumatic events and HIV-risk behaviors among heterosexual men in 2 trials in urban informal settlements in South Africa.
Methods:
Cross-sectional surveys among men in Johannesburg and Durban, South Africa, enrolled in intervention trials. Adjusted logistic regression and structural equation modeling assessed associations between men's experiences of poverty and traumatic events, and HIV-risk behaviors (inconsistent condom use, transactional sex, and number of sex partners). We explored mediated pathways from trauma to HIV risk through mental health and alcohol, and gender attitudes.
Results:
Among 2394 men, in adjusted logistic regression, transactional sex and 4 or more sex partners were associated with witnessing the murder of a family member, witnessing a murder of a stranger, experiencing excessive pain, been kidnapped, and witnessing a rape. More consistent condom use was associated with witnessing the murder of a family member, being kidnapped, and witnessing a rape. In 3 separate structural equation modeling pathways were consistent, trauma directly increased transactional sex, and past year sexual partners, and increased consistent condom use. Risk was increased through mental health pathways, and gender inequitable attitudes and practices.
Conclusion:
Men's HIV-risk behaviors in this population emerge at the confluence of poverty, traumatic experiences, and gender inequalities. Effective HIV-prevention interventions needs to reduce men's experiences of poverty and trauma, transform gender norms, and reduce the mental health impact of trauma.
INTRODUCTION
Gender inequitable masculinities are a key factor driving HIV-risk behaviors among men and contributing to the global burden of HIV.1–3 Globally, studies highlight how gender inequitable masculinities, characterized by inequitable gender attitudes, controlling behaviors, the use of intimate partner violence (IPV), and nonpartner rape, tend to cluster together with other sexual risk behaviors.4,5 For men, sexual behaviors that increase HIV risk include having more sexual partners, limited and inconsistent condom use, and engaging in transactional sex.6,7
Most research on gender inequitable masculinities has drawn on Connell's8 notion of hegemonic masculinity and argues that gender inequitable behaviors are a key way that men “perform” hegemonic masculinity.9 This argument suggests men's HIV-risk behaviors are intimately tied to male power, emerging from a position of power and control over women. Recognition of the inequitable masculinities and HIV-risk relationship has driven a major focus on interventions working with men and boys to “transform masculinities” and specifically hegemonic masculinity as a way to reduce HIV transmission.10,11 Evidence reviews have highlighted that such focus has merits, suggesting interventions “transforming masculinities” can reduce HIV-risk behaviors.3,10,12
A major critique of the masculinities literature, particularly in how it has been drawn on in the health field,13 is that it focuses far too much on men's power, without recognizing how many men, particularly in the global south, are also subjected to structural adversity and high levels of violence themselves.13,14 In particular, the disproportionate level of violence and death that poor, young, black men experience,15 and the ways in which men's emotional vulnerabilities are denied.16 Qualitative research has traced how specific configurations of masculinity—in turn shaping HIV-risk behavior—are constructed in contexts of poverty, adversity, and experiences of trauma, and social norms legitimating the use of violence, rather than from a position of power.17–20 The masculinity emerging in these contexts, while potentially being numerically dominant, cannot be considered hegemonic but are rather subordinated masculinities.9,14 Such subordinated masculinities seek to establish their authority in relation to women, and other men, through an exaggerated form of heterosexual masculinity, often using overt demonstrations of power and violence, and control over women, including in sexual relationships,4,19,21,22 has been termed by some “hypermasculinity”.23
Despite critiques of the masculinities literature as overemphasizing how all masculinities are constructed from positions of power, there has been virtually no quantitative research exploring the impact of men's experiences of poverty and their own experiences of violence and its relationship with HIV risk. Some extant research explores how childhood traumas, including physical, sexual, emotional abuse, and neglect, before the age of 18 years shape men's subsequent risk of IPV perpetration, and HIV-risk behaviors, and HIV acquisition.24,25 This literature highlights how adult depression and alcohol use are also driven by childhood traumas.24–27 In one analysis, Jewkes and Morrell28 using Latent Class Analysis showed the most violent South African men had more gender inequitable attitudes, and greater sexual risk behaviors. They also showed, using Structural Equation Modeling (SEM), that experiences of trauma in childhood impacted psychological factors, in turn shaping their violence practices. Another set of research has focused on the impact of conflict/war-related traumas and its impact on mental health, IPV, and HIV-risk behaviors.29–31 Few studies have explored among nonconflict affected populations the impact of traumatic events on men's mental health, or HIV-risk behaviors, and those that do, suggest a relationship.32,33
In this article, we aim to understand the relationship between men's experiences of traumatic experiences in their life and HIV-risk behaviors. We seek to test 3 hypotheses: (1) that men who experience traumatic events have increased HIV-risk behaviors; (2) that there is a dose response between traumatic events and HIV-risk behavior; and, (3) that the pathways between trauma experienced outside the home and HIV-risk behavior are both direct, but also mediated through poorer mental health, alcohol use, and gender inequitable masculinities.
METHODS
Design
Data comes from 2 cross-sectional studies comprising baselines for the Stepping Stones and Creating Futures (SS/CF) intervention cluster-randomized control trial34 in eThekwini Municipality, South Africa, and the CHANGE cluster randomized control trial35 in Gauteng Province, South Africa. Studies were designed to enable combining of data. Both study sites are in periurban, informal settlements, characterized by poor access to services, high rates of unemployment, and limited educational opportunities.
In both studies, men were recruited, with support from the local NGOs delivering the intervention, and focused on men normally resident in the communities. The SS/CF trial had 34 clusters with between 19 and 21 participants per cluster, with data collected between October 2015 and September 2016, and specific criteria of age 18–30 years. The CHANGE trial had 18 clusters with between 120 and 150 men per cluster, with data collected between January and July 2016, aged 18–40 years. For this study, we focused on younger men, with an age restriction of 18–30 years.
After recruitment, participants signed written informed consent before being interviewed. Questionnaires were self-completed on tablets, with inbuilt logic and skip patterns. In SS/CF, questionnaires could only be read, while in the CHANGE trial, questionnaires had audio assist. Further information on the studies is available elsewhere.34,35
Measures
As a proxy for HIV risk, we measured 3 different constructs associated with HIV prevalence among men: past year transactional sex, past year consistent condom use, and past year number of sexual partners. Past year transactional sex was assessed through 5 questions developed for, and previously used, in South Africa.6 These asked about whether men thought a casual or once-off sexual partner had had sex with them because she may receive a range of items (eg, cell phone, gifts, and food). A positive answer to any item was coded as engaging in transactional sex, and a sum score was also created. A single item assessed condom use over the past year, with responses never, occasionally, sometimes, always, without reference to type of sex partners. Men were asked 3 questions about the number of sexual partners in the past year, specifically the number of main sexual partners, causal sexual partners, and once-off sexual partners. This was summed into a score for total number of sexual partners.
Men were asked about 8 types of potential traumatic experiences in their lifetime, including witnessing the death of a family member or friend, feeling or being close to death, and witnessing a rape. Participants could respond either yes or no. Traumatic experience exposure was based on the Harvard Trauma Questionnaire and previous South African surveys.36
Other measures included education level, age, and the length of time the participant had lived in the community. Household food insecurity in the past month,37 as a proxy for poverty, was assessed with 3 items, specifically, how often in the past month was there no food to eat, any member of your household go to sleep hungry, and not eating for whole day and night, because there was no money or food. A direct sum was derived (range 0–6). Depressive symptoms were assessed with the Center for Epidemiological Studies Depression scale,38 with a simple score being derived (α = 0.89). Alcohol use was assessed with the Alcohol Use Disorders (AUDIT) scale,39 again with a score being derived.
Eight items asked about male controlling behaviors in relation with female partners, with a 4-point Likert scale (α = 0.81), based on the sexual relationship power scale, which had been adapted for South Africa.40 Higher scores indicated more controlling behavior. Gender inequitable attitudes were assessed using 10 items based on the gender equitable men's scale, which had been modified for South Africa,40 with a 4-point Likert scale response. Higher scores indicated more gender inequitable attitudes (α = 0.86).
Analysis
All analyses were conducted in STATA14.1/IC, and took into account the structure of the data, and clustering. We first present summarized statistics for the sample presenting percentages and mean values and 95% confidence intervals (95% CI). Second, we assess whether there is an independent association between each HIV-risk behaviors [past year transactional sex (yes/no), past year condom use (never/occasionally vs sometimes/always), past year number of sexual partners (0–3 vs 4 or more)], and individual traumatic events, and whether there was a dose response (0 vs 1–2 vs 3–4 vs 5–6 events). We used logistic regression to estimate first unadjusted odds ratios (ORs) and then adjusted ORs (aORs), controlling for age, education, time in the community, food insecurity, controlling behaviors, depression, and study arm (intervention vs control) and study, using the survey commands in STATA. We report ORs, aORs, 95% CIs, and P-values.
Second, we conducted SEM. We built 3 models (one for each HIV risk), with continuous outcomes of score of transactional sex (0–5), number of sexual partners, and condom use (1–4). We constructed a latent variable for food insecurity using 3 items of the household hunger scale. This was constructed through factor analysis of items comprising the latent variable, and then building latent models and testing for goodness of fit. To build the SEM, we used 3 techniques, we used theoretical assumptions about pathways, regressed each variable to one another in the pathways (eg, hunger with traumatic experiences score), and using these estimates, built the SEMs. We then fitted the structural model, and removed pathways that were nonsignificant (P < 0.05). Finally, we assessed Goodness of Fit.
RESULTS
Data from 2394 men were included in the analysis (Table 1). A total of 15.5% of men were aged 18–20 years, just under half (46.5%) were aged 21–25 years, and the rest (38.1%) were 26–30 years. Only a small proportion (6.1%) had primary education only, half (51.3%) had secondary but had not completed, whereas 42.6% had completed secondary. Almost three-quarters had lived in the informal settlement for 10 years or less, with just over a quarter (28.6%) living there for 11 or more years. For HIV-risk behaviors, two-thirds (66.3%) reported transactional sex in the past year, a quarter reported using condoms sometimes or always in the past year (27.7%), and just over half (56.3%) reported 4 or more sexual partners in the past year (Table 1).
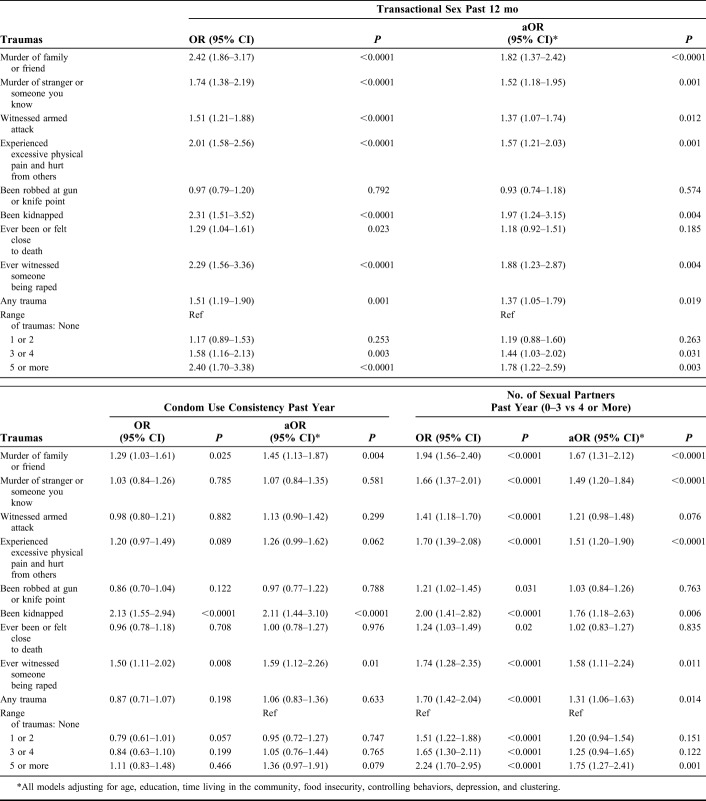
TABLE 1.
Sample Descriptive Data
Experiences of traumatic events in men's life were common (Table 1). Nearly a quarter, (22.4%) had witnessed the murder of a friend or family member in their life and 30.4% the murder of someone else. A third (34.0%) had witnessed an armed attack, and a quarter (26.5%) had experienced excessive physical pain and hurt from others. A total of 39.9% had been robbed at gun or knifepoint, 8.4% reported being kidnapped, and a third (33.6%) had felt or been close to death. A further 10.1% reported witnessing a rape. Just under two-thirds (64.2%) of men reported experiencing any traumatic event. A fifth (19.8%) had experienced 3 of 4 events, and 15.5% had experienced 5 or more events.
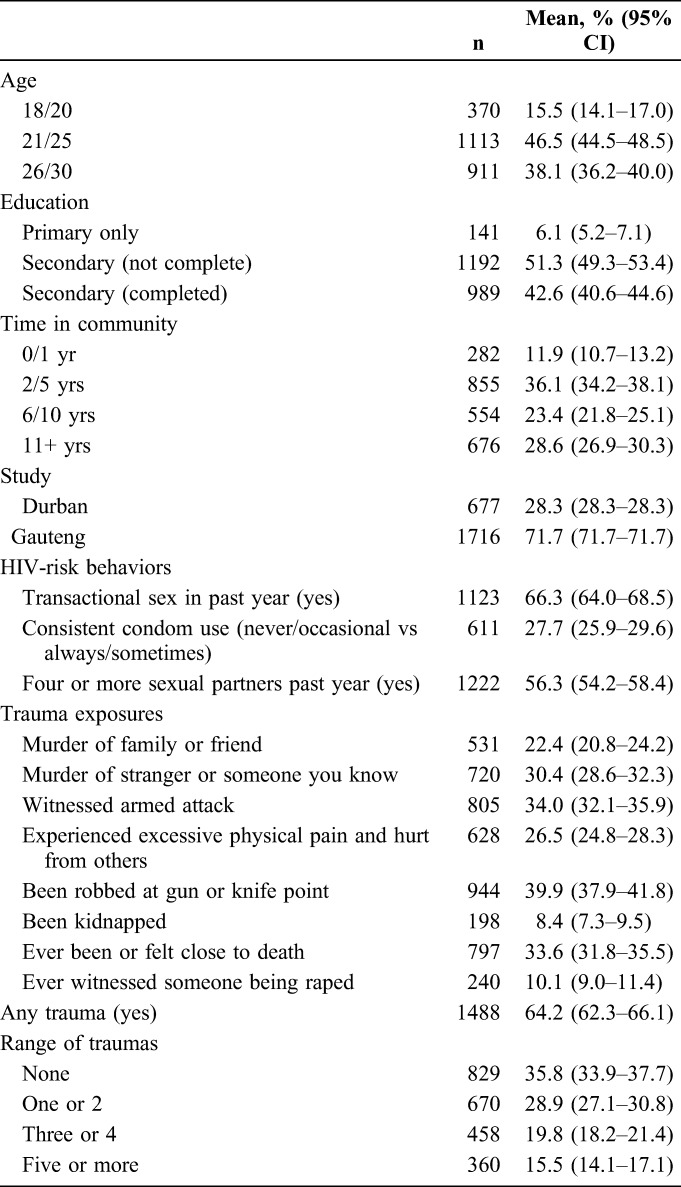
Unadjusted and aORs of associations between trauma experience and the 3 HIV-risk behaviors are reported in Table 2. In adjusted analysis, past year transactional sex was associated with witnessing the murder of a family member or friend, the murder of another person, witnessing an armed attack, experiencing excessive pain from another, being kidnapped, feeling close to death or witnessing a rape. In addition, reporting any trauma and experiencing 3 or 4, or 5 or more traumas were also associated in adjusted analysis with transactional sex. More consistent condom use was associated with witnessing the murder of a family member or friend, being kidnapped, or witnessing a rape. Reporting 4 or more sexual partners was associated with witnessing the murder of a family member or friend, witnessing the murder of another person, experiencing excessive pain from another, being kidnapped, or witnessing a rape, and reporting any trauma, and reporting 5 or more traumas (Table 2).
TABLE 2.
Unadjusted and Adjusted Associations Between HIV-Risk Behaviors and Men's Traumatic Experiences
The 3 SEMs showed a consistent set of associations, but also some variation (Figs. 1–3, see Tables 1–3, Supplemental Digital Content, http://links.lww.com/QAI/B291). In all 3 SEMs, food insecurity was associated with increased experiences of trauma. Food insecurity was also associated with more depressive symptoms, and more gender inequitable attitudes. In all models, more gender inequitable attitudes were associated with the HIV risk (ie, more transactional sex, a greater number of sexual partners, and reduced condom use). Gender inequitable attitudes were also associated with more controlling behaviors (Figs. 1–3).
FIGURE 1.
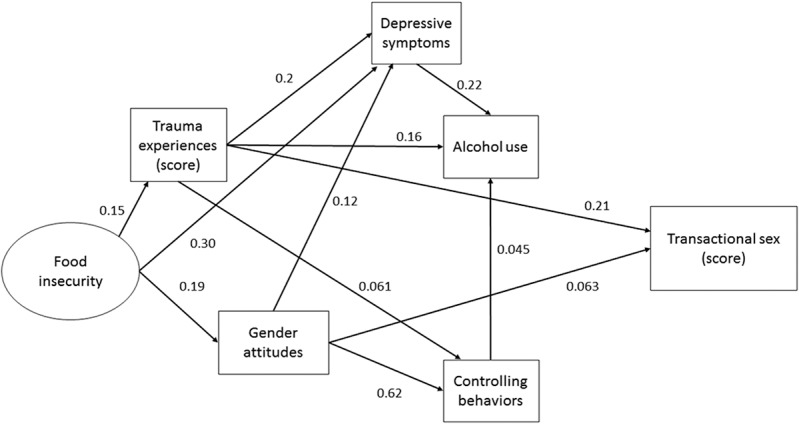
Structural equation model showing pathways between food insecurity, trauma, and transactional sex.
FIGURE 3.
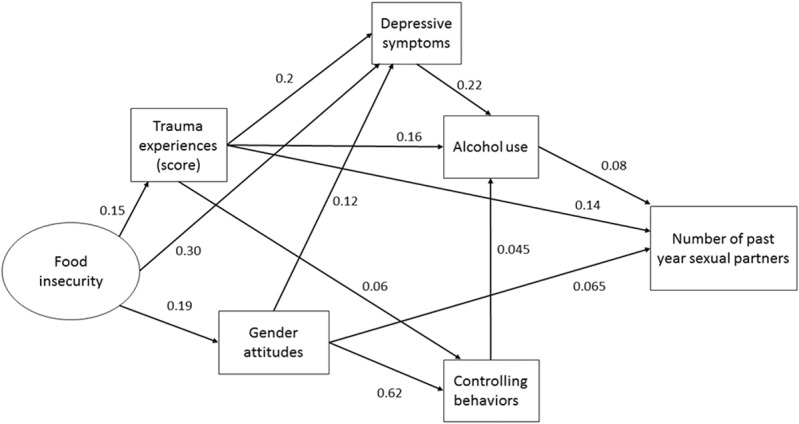
Structural equation model for pathways between food insecurity, trauma experiences, and past year sex partners.
The coefficients between trauma and past year transactional sex, and number of partners indicated that more traumas were associated with increased reporting of these (Figs. 1 and 3); however, there was an inverse association for condom use in the past year, whereby increased traumas was associated with increased consistent condom use (Fig. 2).
FIGURE 2.
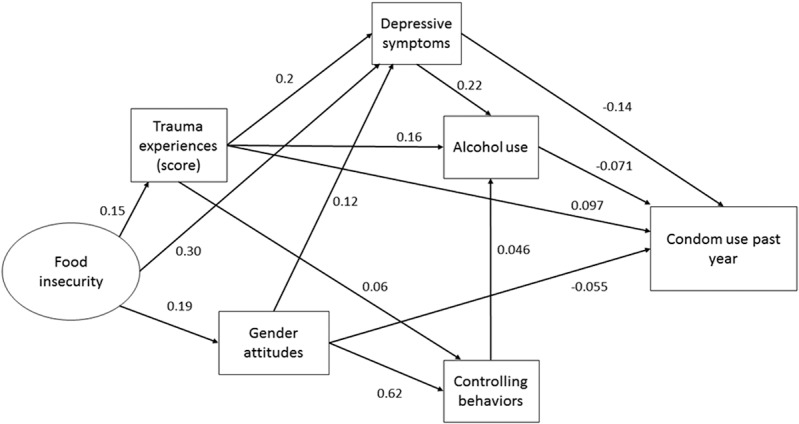
Structural equation model for pathways between food insecurity, trauma, and past year condom use.
In all models, poor mental health mediated pathways from trauma to HIV risk. Trauma was associated with increased depressive symptoms and alcohol use, and depression was associated with increased alcohol use. For condom use, depression and alcohol use, both decreased consistent condom use (Fig. 2), and alcohol use was associated with increased number of past year sex partners (Fig. 3).
For all models, another set of pathways, linked to masculinity, mediated the relationship between trauma and HIV risk. More trauma was associated with more controlling behaviors, which was in turn associated with greater alcohol use. In the models gender inequitable attitudes were directly associated with more transactional sex, reduced condom use and a greater number of sex partners. All SEMs had satisfactory Goodness of Fit statistics (see Tables, Supplemental Digital Content, http://links.lww.com/QAI/B291).
DISCUSSION
The analysis supports the hypothesis that men's experiences of lifetime traumatic events are overall associated with increased transactional sex and numbers of sexual partners. First, in adjusted logistic regression, transactional sex and number of sexual partners were associated with experience of traumatic events, and there was also a dose response to more traumatic events. Second, in the SEMs, more traumatic events were directly associated with more transactional sex and a greater number of sexual partners. And these were exacerbated in the context of household food insecurity.
We also showed a dose response between traumatic events and transactional sex and number of sexual partners, supporting the second hypothesis. Previous work on childhood traumas (typically related to violence and abuse in the home, or at school) has shown they increase men's subsequent risky sexual behaviors25 as have men's experiences of trauma during conflict.30 This study focused on a broader measure of overall trauma in men's lives, outside of conflict settings, the home or before the age of 18 years, suggesting that overall contexts of violence, both witnessing and experiencing it, are central in understanding some of men's sexual risk behaviors.
The association between past year condom use and traumatic events was inverse. For 3 traumatic events, witnessing the murder of a family member or friend and witnessing a rape were associated with more consistent condom use in the past year. And in the SEM, there was also a direct association, whereby more traumatic events were associated with more consistent condom use. The association between trauma and more consistent condom use parallels that seen in some studies of women experiencing IPV, who report higher contraceptive use, than women not experiencing IPV.41 It may be that the impact of experiences of trauma is emotionally distancing, and in contexts where condoms are markers of emotional separation,42 use of condoms more consistently may therefore be a separation strategy and an instrumental response.
All 3 behaviors, transactional sex, more condom use, and a greater number of sex partners can all be conceptualized as men's emotional disengagement in relationships, and a response to trauma. Research has emphasized men with greater psychopathic tendencies (specifically lack of emotions) are more likely to rape43 and require viewing women in instrumental, rather than emotional terms. In the context of trauma, the numbing of emotions is clearly a common response, which could shape all these behaviors.
The analysis is supportive of the third hypothesis that traumatic events have mediated pathways through mental health, and masculinities that increase HIV-risk behaviors, although not all the hypothesized pathways were significant for all HIV-risk behaviors. One set of pathways was through poorer mental health, whereby greater traumas increased depressive symptoms and alcohol use, condom use was decreased through increased depressive symptoms and alcohol use, and alcohol use was associated with increased number of sex partners. The importance of unresolved trauma, manifesting itself in depression and alcohol use, for increasing some HIV risk for men, is rarely considered in HIV-prevention programming. Typically men's alcohol use is conceptualized solely as an expression of a gender inequitable masculinity; however, this model suggests the importance of resolving men's trauma, depression, and alcohol use, to reduce HIV-risk behaviors for men.
A second set of pathways showed how poverty and trauma intersected with gender attitudes and practices to increase HIV-risk. Men's experiences of trauma were associated with more controlling behaviors, and then greater alcohol use, and then HIV risk. Gender inequitable attitudes, partly shaped by poverty, were directly associated with HIV risk and indirectly through increasing controlling behaviors, and then alcohol use. Qualitative research has suggested more gender inequitable forms of masculinity emerge in the contexts of poverty and trauma18,19 and the SEMs support this, showing the multiple pathways through which this happens. This reinforces the importance of working on transforming masculinities as a central approach to reducing men's HIV-risk behaviors.3
A critique of the health literature on masculinities has been that it has implied that hegemonic masculinity is necessarily associated with men's use of power and violence.13 Rather an argument has been put forward that most HIV risk is practiced by a smaller number of men,28 who construct a “hypermasculinity,”23 which uses sexual power over women (and violence) as a way to legitimate their identity.17,19,20 Within Connell's8 hierarchy of masculinities, this is a subordinated masculinity, emphasizing how men can both be powerful, but also subjected to intense vulnerability.13,15,16 The SEMs clearly shows how this particular form of masculinity emerges from poverty, and men's experiences of trauma, and intersects with wider gender inequitable attitudes and practices, shaping their control over women through sex.
The study has a number of limitations. The sample is self-selecting to be part of 2 separate intervention studies, and data are therefore not generalizable, but it is unclear how self-selection would affect the associations. Measures were self-reported, which is “state of the science” for assessing violence and risky sexual behavior, but is considered less rigorous than clinical assessment for mental health. There was also a very high level of reported trauma in the population. We did not include all forms of trauma that men could experience, particularly childhood traumas, which are associated with HIV acquisition, and HIV risk.25 We only included depression in the analysis, yet other forms of mental health, such as post-traumatic stress disorder, and anxiety, may be important, but we did not assess these. Data are cross-sectional, and the temporality of associations is not necessarily clear, suggesting that future analyses with longitudinal data would be important to confirm the pathways identified here. We did multiple tests of association without adjusting for this in reporting, and future research should formally test these hypotheses with adequate sample sizes. Finally, women experience huge levels of trauma, and this is associated with HIV risk,24,25 our analysis did not consider women, and this specific analysis is not generalizable to women.
Men living in urban informal settlements in 2 different provinces in South Africa reported high levels of traumatic events, and this was associated directly with transactional sex and a greater number of sexual partners, and more condom use. There were also indirect pathways through gender inequitable attitudes and practices, and poorer mental health. The analysis illustrates how the form of masculinity these young men constructed was a subordinated masculinity emerging from poverty and adversity, and partly through lack of emotional engagement, used sexual behavior to legitimate their position.13,18,20,28
The analysis has a number of important implications for interventions to reduce HIV risk among men. First, interventions “transforming masculinities” need to be more specific about the forms of masculinities they are working on, and the implications of this for practice,14 specifically, whether the intervention is targeting a hegemonic masculinity and broader constructions of masculinity, or specific formulations, such as a subordinated masculinity. Second, any successful intervention to transform subordinated masculinities needs to work on reducing the violence men experience in their daily life in informal settlements, through working to reduce poverty and eliminating community-level forms of violence. Strategies such as deconcentration and urban upgrading may have positive effects on these,44,45 but there remains little research on the impact of reducing poverty on men's HIV-risk behaviors.46 Third, analysis supports the importance of working to reduce gender inequitable attitudes and practices as central to working with men on reducing HIV risk.1,3 Finally, the central role of poor mental health in shaping HIV risk requires HIV-prevention interventions to consider programming to improve mental health, be this through working to reduce the impact of traumatic experiences on mental health,47 or reducing the accessibility of alcohol.48 Broadly, the work of preventing HIV-risk behaviors among young men living in urban informal settlements cannot be achieved without tackling the wider structural contexts in which men live.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the participants in the studies who gave their time and information.
Footnotes
Supported by the What Works to Prevent Violence? A Global Programme on Violence Against Women and Girls (VAWG) funded by the United Kingdom Government's Department for International Development (DFID). And funds were managed by the South African Medical Research Council.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Fleming PJ, DiClemente RJ, Barrington C. Masculinity and HIV: dimensions of masculine norms that contribute to men's HIV-related sexual behaviors. AIDS Behav. 2016;20:788–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dworkin SL. Men at Risk: Masculinity, Heterosexuality and HIV Prevention. New York and London: NYU Press; 2015. [Google Scholar]
- 3.Jewkes R, Flood M, Lang J. From work with men and boys to changes of social norms and reduction of inequities in gender relations: a conceptual shift in prevention of violence against women and girls. Lancet. 2015;385:1580–1589. [DOI] [PubMed] [Google Scholar]
- 4.Jewkes R, Morrell R. Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. J Int AIDS Soc. 2010;13:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jewkes R, Nduna M, Jama Shai N, et al. Understanding the relationship between gender inequitable behaviours, childhood trauma and socio-economic status in single and multiple perpetrator rape in rural South Africa: structural equation modelling. PLoS One. 2016;11:e0154903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunkle KL, Jewkes R, Nduna M, et al. Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Social Sci Med. 2007;65:1235–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunkle KL, Jewkes RK, Nduna M, et al. Perpetration of partner violence and HIV risk behaviour among young men in the rural Eastern Cape, South Africa. AIDS. 2006;20:2107–2114. [DOI] [PubMed] [Google Scholar]
- 8.Connell R. Masculinities. 2nd ed Cambridge, United Kingdom: Polity; 2005. [Google Scholar]
- 9.Connell R, Messerschmidt J. Hegemonic masculinity: rethinking the concept. Gend and Soc. 2005;19:829–859. [Google Scholar]
- 10.Barker G, Ricardo C, Nascimento M, et al. Questioning gender norms with men to improve health outcomes: evidence of impact. Glob Public Health. 2010;5:539–553. [DOI] [PubMed] [Google Scholar]
- 11.Peacock D, Barker G. Working with men and boys to prevent gender-based violence principles, lessons learned, and ways forward. Men Masculinities. 2014;17:578–599. [Google Scholar]
- 12.Dworkin SL, Treves-Kagan S, Lippman S. Gender-transformative interventions to reduce HIV risks and violence with heterosexually-active men: a review of the global evidence. AIDS Behav. 2013;17:2845–2863. [DOI] [PubMed] [Google Scholar]
- 13.Morrell R, Jewkes R, Lindegger G, et al. Hegemonic masculinity: reviewing the gendered analysis of men's power in South Africa. S Afr Sociol Rev. 2013;44:3–21. [Google Scholar]
- 14.Jewkes R, Morrell R, Hearn J, et al. Hegemonic masculinity: combining theory and practice in gender interventions. Cult Health Sex. 2015;17(suppl 2):96–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ratele K. Subordinate black South African men without fear. Cahiers d'Etudes Africaines. 2013;LIII:247–268. [Google Scholar]
- 16.Seidler V. Transforming Masculinities: Men, Cultures, Bodies, Power, Sex and Love. London, United Kingdom: Routledge; 2005. [Google Scholar]
- 17.Bourgois P. In Search of Respect: Selling Crack in El Barrio. Cambridge, United Kingdom: Cambridge University Press; 2002. [Google Scholar]
- 18.Gores-Green C. Hegemonic and subordinated masculinities: class, violence and sexual performance among young Mozambican men. Nordic J Afr Stud. 2009;18:286–304. [Google Scholar]
- 19.Gibbs A, Sikweyiya Y, Jewkes R. “Men value their dignity”: securing respect and identity construction in urban informal settlements in South Africa. Glob Health Action. 2014;7:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mathews S, Jewkes R, Abrahams N. “I had a hard life”: exploring childhood adversity in the shaping of masculinities among men who killed an intimate partner in South Africa. Br J Criminol. 2011;51:960–977. [Google Scholar]
- 21.Ragnarsson A, Townsend L, Ekstrom A, et al. The construction of an idealised urban masculinity among men with concurrent sexual partners in a South African township. Glob Health Action. 2010;3:5092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Townsend L, Jewkes R, Mathews C, et al. HIV risk behaviours and their relationship to intimate partner violence (IPV) among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Behav. 2011;15:132–141. [DOI] [PubMed] [Google Scholar]
- 23.Herek GM. On heterosexual masculinity some psychical consequences of the social construction of gender and sexuality. Am Behav Scientist. 1986;29:563. [Google Scholar]
- 24.Gibbs A, Dunkle K, Washington L, et al. Childhood traumas as a risk factor for HIV-risk behaviours amongst young women and men living in urban informal settlements in South Africa: a cross-sectional study. PLoS One. 2018;13:e0195369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jewkes RK, Dunkle K, Nduna M, et al. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34:833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Norman RE, Byambaa M, De R, et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9:e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatcher AM, Gibbs A, Jewkes R, et al. Effect of childhood poverty and trauma on adult depressive symptoms among young men in peri-urban South African settlements. J Adolesc Health. 2019;64:79–85. [DOI] [PubMed] [Google Scholar]
- 28.Jewkes R, Morrell R. Hegemonic masculinity, violence, and gender equality: using latent class analysis to investigate the origins and correlates of differences between men. Men Masc. 2018;21:547–571. [Google Scholar]
- 29.Jewkes R, Jama-Shai N, Sikweyiya Y. Enduring impact of conflict on mental health and gender-based violence perpetration in Bougainville, Papua New Guinea: a cross-sectional study. PLoS One. 2017;12:e0186062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haskell SG, Gordon KS, Mattocks K, et al. Gender differences in rates of depression, PTSD, pain, obesity, and military sexual trauma among Connecticut War Veterans of Iraq and Afghanistan. J Womens Health (Larchmt). 2010;19:267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steel Z, Chey T, Silove D, et al. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA. 2009;302:537–549. [DOI] [PubMed] [Google Scholar]
- 32.Raja S, Holland C, Du Bois SN, et al. History of traumatic events in HIV-positive individuals: risk behavior implications in an urban clinic setting. J HIV AIDS Soc Serv. 2015;14:110–128. [Google Scholar]
- 33.Closson K, Dietrich JJ, Nkala B, et al. Prevalence, type, and correlates of trauma exposure among adolescent men and women in Soweto, South Africa: implications for HIV prevention. BMC Public Health. 2016;16:1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gibbs A, Washington L, Willan S. The Stepping Stones and Creating Futures intervention to prevent intimate partner violence and HIV-risk behaviours in Durban, South Africa: study protocol for a cluster randomized control trial, and baseline characteristics. BMC Public Health. 2017;17:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Christofides N, Hatcher AM, Pino A, et al. A cluster randomized controlled trial to determine the effect of community mobilization and advocacy on men's use of violence in peri-urban South Africa: study protocol. BMJ Open. 2018;8:e017579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Machisa MT, Christofides N, Jewkes R. Structural pathways between child abuse, poor mental health outcomes and male-perpetrated intimate partner violence (IPV). PLoS One. 2016;11:e0150986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. Food and Nutrition Technical Assistance Project. Washington, DC: Academy for Educational Development; 2007. [Google Scholar]
- 38.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 39.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. [DOI] [PubMed] [Google Scholar]
- 40.Jewkes RK, Dunkle K, Nduna M, et al. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376:41–48. [DOI] [PubMed] [Google Scholar]
- 41.Alio AP, Daley EM, Nana PN, et al. Intimate partner violence and contraception use among women in Sub-Saharan Africa. Int J Gynecol Obstet. 2009;107:35–38. [DOI] [PubMed] [Google Scholar]
- 42.Jama Shai N, Jewkes R, Levin J, et al. Factors associated with consistent condom use among rural young women in South Africa. AIDS Care. 2010;22:1379–1385. [DOI] [PubMed] [Google Scholar]
- 43.Jewkes R, Sikweyiya Y, Morrell R, et al. Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: findings of a cross-sectional study. PLoS One. 2011;6:e29590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cassidy T, Inglis G, Wiysonge C, et al. A systematic review of the effects of poverty deconcentration and urban upgrading on youth violence. Health Place. 2014;26:78–87. [DOI] [PubMed] [Google Scholar]
- 45.Brown-Luthango M, Reyes E, Gubevu M. Informal settlement upgrading and safety: experiences from Cape Town, South Africa. J Housing Built Environ. 2017;32:471–493. [Google Scholar]
- 46.Gibbs A, Kerr-Wilson A, Jacobson J. A global comprehensive review of economic interventions to prevent intimate partner violence and HIV risk behaviours. Glob Health Action. 2017;10:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lambert JE, Alhassoon OM. Trauma-focused therapy for refugees: meta-analytic findings. J Couns Psychol. 2015;62:28–37. [DOI] [PubMed] [Google Scholar]
- 48.Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. 2009;373:2234–2246. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.