Abstract
Objective: This study was a systematic review and meta-analysis of double-blind, randomized, placebo-controlled trials, investigating the efficacy and tolerability/safety of melatonin receptor agonists, such as ramelteon and melatonin, for patients with bipolar disorder.
Methods: We carried out a literature search through PubMed and the Cochrane Library from the date of inception to January 6, 2019. The risk ratio (RR), number needed to treat (NNT), and standardized mean difference (SMD) ±95% CI were calculated. The primary outcome was all-cause discontinuation.
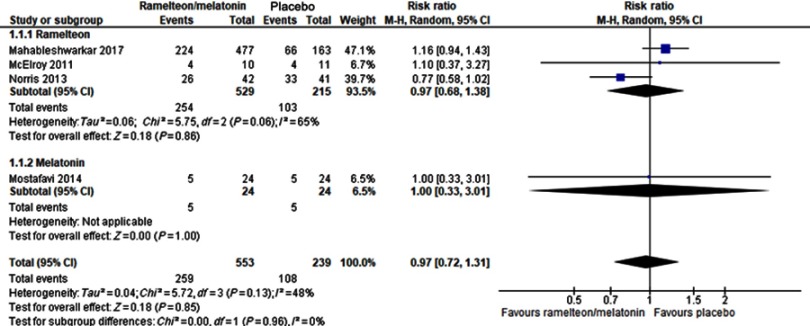
Results: We identified three ramelteon (n=746) and two melatonin (n=53) studies. One of these two melatonin studies reported only data on all-cause discontinuation, whereas the other study did not report data relevant for a meta-analysis. We found no significant differences between the treatment and placebo groups regarding all-cause discontinuation, neither individually (p: ramelteon=0.86, melatonin=1.00) nor pooled together (p=0.85). Although we found no significant differences between ramelteon and placebo regarding the relapse due to mania/hypomania or mixed episode; Pittsburgh Sleep Quality Index scores; depression scales scores; Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form scores; and the incidence of individual adverse events, such as headaches, insomnia, somnolence, anxiety, and dizziness, ramelteon was associated with a lower incidence of relapse due to depression than placebo (RR=0.67, 95% CI=0.48–0.94, p=0.02, NNT=14).
Conclusion: Ramelteon might prevent relapse due to depression in patients with bipolar disorder. However, because of the small number of studies included in the present systematic review and meta-analysis, further studies comparing ramelteon and placebo with larger samples of patients with bipolar disorder are warranted. We also did not evaluate the efficacy and safety of melatonin for patients with bipolar disorder in detail.
Keywords: ramelteon; melatonin; bipolar disorder; relapse; systematic review, meta-analysis
Introduction
Bipolar disorder is a common psychiatric disease,1 with a lifetime prevalence of approximately 1%.2 It is a potentially lifelong and disabling condition characterized by acute episodes of mania (or hypomania) and depression.3,4 Recent treatment guidelines for bipolar disorder recommend pharmacotherapy (eg, lithium, some anticonvulsants, and several antipsychotics) for the acute phase.5,6 Because patients with bipolar disorder tend to relapse repeatedly,1 pharmacotherapy (especially lithium7) is recommended to be continued during the maintenance phase.5,6 A previous cohort study has reported that only approximately 10% of patients with bipolar I disorder maintain remission for 5 years.8 Few patients achieve lifelong remission with continued existing pharmacological treatment.
A recent cohort study reported that 50% of patients with bipolar disorder exhibit abnormal sleep, with 50% presenting circadian rhythm disturbances.9 A cross-sectional study revealed that in patients with bipolar disorder, circadian rhythm disturbances are associated with an increased risk of relapse.10 A recent review has suggested the occurrence of melatonin secretion abnormalities associated with the pathophysiology of bipolar disorder.11 Melatonin is a hormone secreted predominantly by the pineal gland under circadian variation, which is regulated by the central circadian pacemaker in the suprachiasmatic nuclei (SCN) of the hypothalamus.11 A previous cross-sectional study has demonstrated that patients with bipolar disorder present significantly lower serum melatonin levels than healthy controls.12 The recent cohort study has reported that patients with abnormal sleep present lower melatonin levels over 24 hrs of secretion than both controls and patients with normal sleep.9 Therefore, we hypothesized that melatonin receptor agonists, such as melatonin and ramelteon, are beneficial for the treatment of the symptoms of bipolar disorder, including insomnia. Ramelteon is a melatonin receptor full agonist with both high affinity for melatonin MT1 (which inhibits the arousal signals coming from the SCN that maintain wakefulness) and MT2 (which synchronize the circadian clock to the day–night cycle) receptors located within the SCN.13,14 The activity of ramelteon at the MT1 and MT2 receptors exerts sleep-promoting properties because these receptors, which are acted upon by endogenous melatonin, are involved in the maintenance of the circadian rhythm underlying the normal sleep–wake cycle.13
To date, three randomized placebo-controlled trials (RCTs) have been conducted to investigate the use of ramelteon for the treatment of bipolar disorder.17 However, these provided inconsistent efficacy outcomes. For example, the RCT conducted by Mahableshwarkar (2017) reported that ramelteon was superior to placebo in terms of the Quality of Life Enjoyment and Satisfaction Questionnaire short-term version (Q-LES-Q)18 score,15 whereas that conducted by McElroy (2011) did not detect an effect by ramelteon (Table 1).16 Although one RCT reported that ramelteon was associated with a longer time to relapse than placebo,17 two RCTs did not report a significant difference between the groups in terms of the relapse rate (Table 1).15,17 Such results might be caused by type II errors related to an insufficient sample size. In fact, the statistical power of relapse rate due to depression in each RCT was small (ie, approximately 30% in the study by Norris and 50% in that by Mahableshwarkar). A meta-analysis can increase the statistical power for group comparisons, thereby overcoming the limitations of sample size in underpowered studies.19 Therefore, the results of a systematic review and meta-analyses present a higher level of evidence than individual RCTs.19 Here, we conducted the systematic review and meta-analysis of RCTs comparing the efficacy and tolerability/safety of ramelteon in relation to placebo in patients with bipolar disorder. Moreover, to increase the statistical power of our study, we conducted this meta-analysis, combining data from ramelteon and melatonin RCTs, as melatonin receptor agonists. We defined all-cause discontinuation as the primary outcome because it contained various elements needed to evaluate the efficacy, safety, and tolerability of the treatment.
Table 1.
Details of the study, patients, and treatment regimens used in the double-blind, randomized, placebo-controlled trials included in the present systematic review and meta-analysis
| Study, country, funding | Study design | Inclusion criteria | Drug (mg/d)/n | Mean age (years)/male (%) | Efficacy outcomes1,2 |
|---|---|---|---|---|---|
| Mahableshwarkar 2017, USA and Latin America, industry | 12 months, DBRPCT | Adult (18–75 years) op with BDI (DSM-IV-TR) taking various MS, AAP, and/or AD. Patients were clinically stable (≥8 weeks before baseline, with the most recent mood episode between 8 weeks and 9 months before screening. MADRS≤12, YMRS≤10, CGI-S≤2, HAMA≤21 at both screening and baseline visits). | RAM-SL0.8/154 | 41.7±12.5/41.6 |
Time to relapse, relapse rate (mania, depression, mixed episode): RAM-SL0.8=PLA, RAM-SL0.4=PLA, RAM-SL0.1=PLA, Q-LES-Q-SF: RAM-SL0.8>PLA, RAM-SL0.4>PLA, RAM-SL0.1>PLA |
| RAM-SL0.4/160 | 42.9±11.7/42.5 | ||||
| RAM-SL0.1/164 | 43.0±13.3/45.7 | ||||
| PLA/164 | 44.2±12.2/41.5 | ||||
| McElroy 2011, USA, industry | 8 weeks, DBRPCT | Adult (18–65 years) op with BDI (DSM-IV-TR based on MINI) taking various MS, AAP, and/or AD. Patients experienced mild-to-moderate manic symptoms (YMRS=10–25) and had clinically significant sleep disturbance (PSQI>5). | RAM8/10 | 35.9±2.8/30.0 | PIRS, PSQI, YMRS, IDS, HAMA, Q-LES-Q-SF: RAM8=PLA |
| PLA/11 | 35.0±3.5/45.5 | ||||
| Norris 2013, USA, industry | 24 weeks, DBRPCT | Adult (18–65 years) op with euthymic BDI (DSM-IV-TR based on MINI) taking various MS, AP, and/or AD. Patients had clinically significant sleep disturbance (PSQI≥5). Patients were clinically stable (MADRS≤12 and YMRS≤12 at both screening and baseline visits). | RAM8/42 | 46.6±11.0/38.1 |
Time to relapse: RAM8>PLA PSQI, YMRS, MADRS, relapse rate (mania, depression, mixed episode): RAM8=PLA |
| PLA/41 | 45.2±10.8/36.6 | ||||
| Leibenluft 1997, USA, non-industry | 12 weeks, DBRPCCT | Adult op with rapid-cycling BD (based on SCID). Patients had at least 4 affective episodes within the past year. | Number of patients included in this study were 5 | 47.2±3.8/0.0 | Daily self-rating scale and sleep log, HAMD, hypomania interview: MEL10=PLA |
| Mostafavi 2014, Iran, non-industry | 12 weeks, DBRPCT | Adolescent (11–17 years) op with BDI (DSM-IV-TR). 18≤BMI≤25. All patients received OLA+lithium during the study. | MEL3/24 | 14.4±1.7/57.9 | SBP, T-chol: MEL3>PLA, DBP, FBS, TG, BMI: MEL3=PLA |
| PLA/24 | 14.5±1.3/47.4 |
Notes: 1Primary outcomes in each study are underlined. 2A > B: A was superior to B, A = B: A was similar to B
Abbreviations: (A)AP. (atypical) antipsychotic; AD, antidepressant; BD(I), bipolar (I) disorder; BMI, body mass index; CGI-S, Clinical Global Impressions-severity illness scale; DBP, diastolic blood pressure; DBRPCT, double-blind, randomized, placebo-controlled trial; DBRPCCT, double-blind, randomized, placebo-controlled crossover trial; DSM(-III or IV)(-TR), Diagnostic and Statistical Manual of Mental Disorders (3rd or 4th Edition) (Text Revision); FBS, fasting blood sugar; HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Depression Rating Scale; IDS, Inventory for Depressive Symptoms; MADRS, Montgomery Åsberg Depression Rating Scale; MEL, melatonin; MINI, Mini International Neuropsychiatric Interview; MS, mood stabilizer; n, number of patients; OLA, olanzapine, op: outpatient; PIRS, Pittsburg Insomnia Rating Scales (65-item version); PLA, placebo; PSQI, Pittsburgh Sleep Quality Index; Q-LES-Q, Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form; RAM(-SL), ramelteon(-sublingual administration); SBP, systolic blood pressure; SCID, Structured Clinical Interview for DSM-III-R; T-chol, total cholesterol; TG, triglyceride; USA, United States of America; YMRS, Young Mania Rating Scale.
Materials and methods
We conducted this meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (Table S1).20 This study was registered with PROSPERO (CRD42018118292, https://www.crd.york.ac.uk/prospero/).
Search strategy and studies’ inclusion criteria
Three authors (T.K., I.N., and K.S.) identified relevant RCTs by independently searching MEDLINE, the Cochrane Library, and Scopus without language restrictions from the date of inception to January 6, 2019, using the following search strategy: (ramelteon OR melatonin) AND (bipolar OR affective OR mood OR mania OR manic OR depressi*) AND (random*). The three authors (T.K., I.N., and K.S.) assessed the inclusion/exclusion criteria and independently selected the studies. References of included RCTs and review articles were also searched for citations of additional relevant published and unpublished studies, such as conference abstracts. The clinical trial registries (ClinicalTrials.gov [http://clinicaltrials.gov/] and WHO International Clinical Trials Registry Platform [http://www.who.int/ictrp/search/en/]) were also searched to include as many RCTs as possible, thereby minimizing the possibility of publication bias.
Data extraction, synthesis and outcome measures
The three authors (T.K., I.N., and K.S.) independently extracted data from the included articles. Our meta-analysis was based on either an intention-to-treat (ITT) or a modified ITT analysis. Although we planned to contact the RCTs’ authors and request unpublished data whenever data required for the meta-analysis were missing, this was not done because unpublished data were not required for the meta-analysis.
We defined all-cause discontinuation as the primary outcome. Secondary outcomes were the study-defined relapse rate due to manic/hypomania, mixed episode, or depression; Young Mania Rating Scale (YMRS) score21 depression scales (ie, the Montgomery–Åsberg Depression Rating Scale22 used in the study by Norris17 and the Inventory for Depressive Symptoms23 used in the study by McElroy16); the Pittsburgh Sleep Quality Index (PSQI)24 or Q-LES-Q-SF at the study endpoint; discontinuation due to adverse events; and individual adverse events. For four-arm studies (ie, those including sublingual administration of ramelteon at 0.1 mg, 0.4 mg, 0.8 mg, and placebo),15 data pertaining to all ramelteon treatment doses were combined into the ramelteon group to avoid a unit-of-analysis error.19 The pharmacokinetic study showed that the exposure (measured as the area under the concentration–time curve) attained with sublingual ramelteon at 0.5 mg was similar to that attained with an oral formulation of ramelteon at 8 mg.15
Meta-analytic methods
We conducted meta-analyses using the Review Manager (RevMan) (Computer program). Version 5.3. The Nordic Cochrane Centre, The Cochrane Collaboration, 2014; Copenhagen, Denmark. A random-effects model was selected because of potential heterogeneity across studies. For each meta-analysis, we estimated the risk ratio (RR) along with its 95% CI. Whenever the RR revealed significant differences between the groups in terms of efficacy or adverse events, we calculated the number needed to treat (NNT) from the risk difference (RD) using the following formula: NNT=1/RD. For continuous data, we calculated standardized mean differences (SMDs).25 We investigated study heterogeneity using the Chi-square test of homogeneity (p<0.05) together with the I2 statistic, considering a level of I2≥50% as indicative of considerable heterogeneity.26 Our meta-analysis showed that the effect of ramelteon was superior to that of placebo regarding relapse rate due to depression. Although we included Mahableshwarkar’s study15 in this meta-analysis, it concerned the administration of sublingual ramelteon at 0.8 mg/day (equivalent to an oral administration of 12.8 mg/day), which was estimated to exceed the approved dose (ie, oral ramelteon, 8 mg/day). Because the sublingual administration of ramelteon at 0.8 mg/day might influence the results of relapse rate due to depression, we added a subgroup meta-analysis, which excluded the arm receiving sublingual ramelteon at 0.8 mg/day from Mahableshwarkar’s study. We assessed the methodological quality of the included articles using the Cochrane risk-of-bias tool.19 We did not explore potential publication bias because there were more than 10 studies to examine publication bias using funnel plots.
Results
Details of the RCTs included in the current study
Among the 1,403 results retrieved by the search, we removed 1,394 as duplicates or articles excluded based on information provided by the abstract or title. Additionally, we excluded four articles after full-text review, including three review articles27-29 and one study30 is the same as Mostafavi 2014 study,31 which resulted in five included RCTs (Figure S1).15–17,31,32 Moreover, we did not retrieve any additional RCTs by searching review articles and clinical trial registries; therefore, we conducted the meta-analysis with only five RCTs (three ramelteon [n=746] and two melatonin [n=53] RCTs). Details of each study are presented in Table 1. The methodological quality of each RCT, based on the Cochrane risk-of-bias tool, is presented in Figure S2. All RCTs were double-blind. The study duration ranged from 8 weeks to 12 months. Although all ramelteon RCTs were industry sponsored, they used either an ITT or a modified ITT analysis. Mahableshwarkar;’s study (2017) used sublingual ramelteon, which was an off-label formulation.15 Three RCTs included only adult outpatients with bipolar I disorder.15–17 Another RCT (Mostafavi 2014) included adolescent outpatients with bipolar I disorder and reported only data pertaining to all-cause discontinuation.31 The remaining one RCT (Leibenluft’s study) including adult outpatients with rapid-cycling bipolar disorder was a crossover RCT of melatonin and did not report any relevant available data to be included in a meta-analysis.32 Patients included in all five RCTs took psychotropic drugs, such as mood stabilizers, antipsychotics, and/or antidepressants, at the study baseline.
Results of the meta-analysis
Neither pooled nor individual melatonin agonists differed from the placebo in terms of the primary outcome (Figure 1). Although we found no significant differences between the ramelteon and placebo groups regarding the relapse due to mania/hypomania or mixed episode; PSQI scores; depression scale scores; Q-LES-Q-SF scores; and the incidence of individual adverse events, such as headache, insomnia, somnolence, anxiety, and dizziness, ramelteon was associated with a lower incidence of relapse due to depression than placebo (RR=0.67, 95% CI=0.48–0.94, p=0.02, NNT=14) (Table 2), which was consistent with results of a subgroup meta-analysis excluding the arm receiving sublingual ramelteon at 0.8 mg/day in Mahableshwarkar’s study (RR=0.63, 95% CI=0.44–0.91, p=0.01, NNT=13).
Figure 1.
All-cause discontinuation. Abbreviation: M-H, Mantel–Haenszel.
Table 2.
Meta-analysis results: ramelteon versus placebo
| Efficacy | ||||||
|---|---|---|---|---|---|---|
| Outcome | N | n | I2 | Effect size | 95% CI | p |
| Relapse rate due to mania/hypomania | 2 | 705 | 0% | RR=1.05 | 0.43–2.59 | 0.91 |
| Relapse rate due to mixed episodes | 2 | 705 | 5% | RR=0.95 | 0.34–2.67 | 0.92 |
| Relapse rate due to depression | 2 | 705 | 0% | RR=0.67 | 0.48–0.94 | 0.02* |
| Depression scales | 2 | 102 | 0% | SMD=0.07 | −0.32 to 0.46 | 0.71 |
| PSQI | 2 | 102 | 61% | SMD=−0.04 | −0.83 to 0.74 | 0.91 |
| Q-LES-Q-SF | 2 | 641 | 0% | SMD=−0.04 | −0.22 to 0.13 | 0.63 |
| Safety | ||||||
| Outcome | N | n | I2 | Effect size | 95% CI | p |
| Discontinuation due to adverse events | 3 | 744 | 0% | RR=0.90 | 0.62–1.29 | 0.57 |
| Abnormal dream | 2 | 104 | 68% | RR=0.67 | 0.03–15.76 | 0.80 |
| Anxiety | 2 | 723 | 46% | RR=1.54 | 0.19–12.78 | 0.69 |
| Dizziness | 2 | 723 | 0% | RR=1.08 | 0.32–3.64 | 0.90 |
| Fatigue | 2 | 723 | 3% | RR=0.64 | 0.23–1.81 | 0.40 |
| Headache | 3 | 744 | 0% | RR=1.00 | 0.56–1.78 | 0.99 |
| Insomnia | 2 | 723 | 0% | RR=0.82 | 0.42–1.61 | 0.57 |
| Somnolence | 3 | 744 | 0% | RR=1.45 | 0.63–3.32 | 0.39 |
| Diarrhea | 3 | 744 | 0% | RR=0.92 | 0.42–2.04 | 0.84 |
| Nausea | 2 | 661 | 22% | RR=0.62 | 0.17–2.32 | 0.48 |
| Upper respiratory tract infection | 2 | 661 | 0% | RR=0.71 | 0.36–1.39 | 0.31 |
Notes: *Number need to treat=14, p=0.04.
Abbreviations: N, Number of studies; n, number of patients; PSQI, Pittsburgh Sleep Quality Index; Q-LES-Q-SF, Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form; RR, risk ratio; SMD, standardized mean difference.
Discussion
The present study constitutes the first meta-analysis of RCTs examining the efficacy and safety of melatonin receptor agonists (ramelteon and melatonin) compared with placebo for the treatment of bipolar disorder. The meta-analysis was focused on a single outcome (ie, all-cause discontinuation) obtained from pooled data from ramelteon and melatonin RCTs. Although ramelteon and placebo had similar relapse rates due to mania/hypomania or mixed episodes, ramelteon was superior to placebo in preventing depression relapse. Two RCTs were included in relapse due to depression, each of which failed to demonstrate that ramelteon was superior to placebo in terms of this outcome.15,17 Therefore, the positive effect of ramelteon on relapse due to depression was detected by raising the statistical power through the use of a meta-analysis. Because we failed to detect significant heterogeneity in this outcome, they were considered similar in terms of study design (the long duration of double-blind, randomized, placebo-controlled trial) and participants’ characteristics (clinically stable adults patients with bipolar I disorder). Because we found no significant differences between the ramelteon and placebo groups regarding adverse events, ramelteon was considered to be well-tolerated. Given the above evidence, we suggested that ramelteon is useful to prevent relapse due to depression in adult patients with clinically stable bipolar I disorder.
Although ramelteon is a hypnotic agent, our study showed that it did not improve the PSQI score compared with placebo. Unfortunately, our study did not evaluate other outcomes related to sleep disturbances because data available were insufficient to conduct a meta-analysis. In fact, only two RCTs on ramelteon included patients with sleep disturbances.16,17 Moreover, the sample size in these RCTs was small. Recent systematic reviews have reported that melatonin receptor agonists decrease diastolic blood pressure, fat mass, and blood triglycerides among psychiatric patients using atypical antipsychotics.27,29 However, our study did not examine whether melatonin receptor agonists were beneficial for these outcomes because no relevant data were available in RCTs including only patients with bipolar disorder. Therefore, further studies using larger samples are needed to investigate whether melatonin receptor agonists improve sleep disturbances and antipsychotic induced metabolic side effects in patients with bipolar disorder.
The present study had other limitations. First, the total number of included studies and patients was small; second, the efficacy of melatonin was not evaluated; third, because all RCTs on ramelteon were industry sponsored, the results might reflect an industry-sponsored bias19 fourth, because funnel plots are generally used only if 10 or more studies are included in the meta-analysis, these were not used to explore potential publication bias19 fifth, the duration of RCTs included in the present study was relatively short (ie, the longest study lasted 12 months); and finally, the study conducted by Mahableshwarkar used sublingual ramelteon,15 which is a formulation lacking approval worldwide. Further studies using larger samples are needed to examine whether oral ramelteon prevents relapse due to depression in adult patients with clinically stable bipolar I disorder. It also needs to examine whether ramelteon has a benefit for the treatment of other types of bipolar disorder (eg, bipolar II or cycling patients) and gender of patients. In addition, a study using actigraphy is needed to examine whether ramelteon influences circadian activity and sleep patterns in bipolar disorder.
Conclusion
In conclusion, ramelteon may exert a benefit in preventing relapse due to depression in adult patients with clinically stable bipolar I disorder. However, further RCTs of melatonin versus placebo using larger samples of patients with bipolar disorder are needed to confirm this potential benefit.
Acknowledgments
We thank Takeda Pharmaceutical Company Limited (1-1, Nihonbashi-Honcho 2-chome, Chuo-ku, Tokyo, Japan 〒103-0027) for providing detailed information about sublingual ramelteon. We also thank Mr. Miyanohara for his technical support. The present study was supported by the Health and Labor Sciences Research Grants (H29-seishin-ippan-001).
Disclosure
Dr. Kishi has received speaker’s honoraria from Daiichi Sankyo, Dainippon Sumitomo, Eisai, Janssen, Otsuka, Meiji, MSD, Yoshitomi, and Tanabe-Mitsubishi and has received a Health Labour Sciences Research Grant and a Fujita Health University School of Medicine research grant. Dr. Sakuma has received speaker’s honoraria from Otsuka and Torii. Dr. Nomura has received speaker’s honoraria from Meiji, MSD, Torii, Janssen, and Otsuka. Dr. Kitajima has received speaker’s honoraria from Eisai, Tanabe-Mitsubishi, Otsuka, Takeda, Eli Lilly, MSD, Meiji, Yoshitomi, Dainippon-Suimitomo, Fukuda, Shionogi, and Novo Nordisk and has had research grants from Eisai, Takeda, MSD. Dr. Mishima has received research support from the Japanese Ministry of Health, Labour and Welfare, the Japanese Ministry of Education, Science, and Technology, and the National Center of Neurology and Psychiatry Intramural Research Grant for Neurological and Psychiatric Disorders. He has also received speaker’s honoraria from Eisai, MSD, Takeda, Astellas, and Janssen Pharmaceutical along with research grants from Eisai, Nobelpharma, and Takeda. Dr. Iwata has received speaker’s honoraria from Astellas, Dainippon Sumitomo, Eli Lilly, GlaxoSmithKline, Janssen, Yoshitomi, Otsuka, Meiji, Shionogi, Novartis, and Pfizer and has had research grants from GlaxoSmithKline, Meiji, and Otsuka. Dr. Tsuyoshi Kitajima reports grants, personal fees from Eisai, Takeda, and MSD, He has also received personal fees from Tanabe-Mitsubishi, Otsuka, Eli Lilly, Meiji, Yoshitomiyakuhin, Dainippon-Suimitomo, Fukuda, Shionogi, and Novo Nordisk, during the conduct of the study; Professor Kazuo Mishima reports grants from the Japanese Ministry of Health, Labour and Welfare, the Japanese Ministry of Education, Science, and Technology, the National Center of Neurology and Psychiatry, Eisai Co., Ltd., Nobelpharma Co., Ltd., and Takeda Pharmaceutical Co., Ltd., he has also received personal fees from Eisai Co., Ltd., MSD Inc., Takeda Pharmaceutical Co., Ltd., Astellas Pharma Inc., and Janssen Pharmaceutical KK, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet. 2016;387(10027):1561–1572.Availble from: https://www.fujita-hu.ac.jp/~psychi/html/kenkyunaiyoyakuri.html. Accessed May 07, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kendall T, Morriss R, Mayo-Wilson E, Marcus E. Guideline development group of the national institute for H, care E. Assessment and management of bipolar disorder: summary of updated NICE guidance. BMJ. 2014;349:g5673. [DOI] [PubMed] [Google Scholar]
- 4.Grunze H, Vieta E, Goodwin GM, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J Biol Psychiatry. 2013;14(3):154–219. [DOI] [PubMed] [Google Scholar]
- 5.Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fountoulakis KN, Yatham L, Grunze H, et al. The International College of Neuro-Psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 2: review, grading of the evidence, and a precise algorithm. Int J Neuropsychopharmacol. 2017;20(2):121–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fornaro M, De Berardis D, Koshy AS, et al. Prevalence and clinical features associated with bipolar disorder polypharmacy: a systematic review. Neuropsychiatr Dis Treat. 2016;12:719–735. doi: 10.2147/NDT.S100846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keller MB, Lavori PW, Coryell W, Endicott J, Mueller TI, Bipolar I. a five-year prospective follow-up. J Nerv Ment Dis. 1993;181(4):238–245. [DOI] [PubMed] [Google Scholar]
- 9.Bradley AJ, Webb-Mitchell R, Hazu A, et al. Sleep and circadian rhythm disturbance in bipolar disorder. Psychol Med. 2017;47(9):1678–1689. doi: 10.1017/S0033291717000186 [DOI] [PubMed] [Google Scholar]
- 10.Jones SH, Hare DJ, Evershed K. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disord. 2005;7(2):176–186. [DOI] [PubMed] [Google Scholar]
- 11.Takaesu Y. Circadian rhythm in bipolar disorder: A review of the literature. Psychiatry Clin Neurosci. 2018;72(9):673–682. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy SH, Kutcher SP, Ralevski E, Brown GM. Nocturnal melatonin and 24 hr 6-sulphatoxymelatonin levels in various phases of bipolar affective disorder. Psychiatry Res. 1996;63(2–3):219–222. doi: 10.1016/0165-1781(96)02910-1 [DOI] [PubMed] [Google Scholar]
- 13.Rozerem FDA (Ramelteon) tablets drug approval package; 2005; Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/021782s000_RozeremTOC.cfm. Accessed January 6, 2019.
- 14.Dubocovich ML, Rivera-Bermudez MA, Gerdin MJ, Masana MI. Molecular pharmacology, regulation and function of mammalian melatonin receptors. Front Biosci. 2003;8:d1093–1108. [DOI] [PubMed] [Google Scholar]
- 15.Mahableshwarkar AR, Calabrese JR, Macek TA, et al. Efficacy and safety of sublingual ramelteon as an adjunctive therapy in the maintenance treatment of bipolar I disorder in adults: A phase 3, randomized controlled trial. J Affect Disord. 2017;221:275–282. doi: 10.1016/j.jad.2017.06.044 [DOI] [PubMed] [Google Scholar]
- 16.McElroy SL, Winstanley EL, Martens B, et al. A randomized, placebo-controlled study of adjunctive ramelteon in ambulatory bipolar I disorder with manic symptoms and sleep disturbance. Int Clin Psychopharmacol. 2011;26(1):48–53. doi: 10.1097/YIC.0b013e3283400d35 [DOI] [PubMed] [Google Scholar]
- 17.Norris ER, Karen B, Correll JR, et al. A double-blind, randomized, placebo-controlled trial of adjunctive ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorder. J Affect Disord. 2013;144(1–2):141–147. doi: 10.1016/j.jad.2012.06.023 [DOI] [PubMed] [Google Scholar]
- 18.Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: a new measure. Psychopharmacol Bull. 1993;29(2):321–326. [PubMed] [Google Scholar]
- 19.Higgins J, Green S Cochrane handbook for systematic reviews of interventions version 5.1.0 The Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org. Accessed January 6, 2019.
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. [DOI] [PubMed] [Google Scholar]
- 22.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. [DOI] [PubMed] [Google Scholar]
- 23.Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C. The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Res. 1986;18(1):65–87. doi: 10.1016/0165-1781(86)90060-0 [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang HR, Woo YS, Bahk WM. The role of melatonin and melatonin agonists in counteracting antipsychotic-induced metabolic side effects: a systematic review. Int Clin Psychopharmacol. 2016;31(6):301–306. doi: 10.1097/YIC.0000000000000135 [DOI] [PubMed] [Google Scholar]
- 28.De Crescenzo F, Lennox A, Gibson JC, et al. Melatonin as a treatment for mood disorders: a systematic review. Acta Psychiatr Scand. 2017;136(6):549–558. doi: 10.1111/acps.12755 [DOI] [PubMed] [Google Scholar]
- 29.Igwe SC, Brigo F. Does melatonin and melatonin agonists improve the metabolic side effects of atypical antipsychotics?: A systematic review and meta-analysis of randomized controlled trials. Clin Psychopharmacol Neurosci. 2018;16(3):235–245. doi: 10.9758/cpn.2018.16.3.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mostafavi SA, Solhi M, Mohammadi MR, Akhondzadeh S. Melatonin for reducing weight gain following administration of atypical antipsychotic olanzapine for adolescents with bipolar disorder: a randomized, double-blind, placebo-controlled trial. J Child Adolesc Psychopharmacol. 2017;27(5):440–444. doi: 10.1089/cap.2016.0046 [DOI] [PubMed] [Google Scholar]
- 31.Mostafavi A, Solhi M, Mohammadi MR, Hamedi M, Keshavarzi M, Akhondzadeh S. Melatonin decreases olanzapine induced metabolic side-effects in adolescents with bipolar disorder: a randomized double-blind placebo-controlled trial. Acta Med Iran. 2014;52(10):734–739. [PubMed] [Google Scholar]
- 32.Leibenluft E, Feldman-Naim S, Turner EH, Wehr TA, Rosenthal NE. Effects of exogenous melatonin administration and withdrawal in five patients with rapid-cycling bipolar disorder. J Clin Psychiatry. 1997;58(9):383–388. [DOI] [PubMed] [Google Scholar]