Abstract
Background
Wool clothing may be perceived as a poor choice for use by individuals with sensitive skin or atopic dermatitis.
Objectives
The aims of the study were to evaluate the effect on atopic dermatitis of wearing fine Merino wool clothing versus standard clothing and to assess the effect of Merino wool clothing on quality of life in children and adults with atopic dermatitis 5 years and older.
Methods
Subjects with mild to moderate atopic dermatitis were assessed in a crossover fashion after wearing Merino wool clothing for 6 weeks and standard clothing for 6 weeks, for Eczema Area and Severity Index, Dermatology Life Quality Index, static Investigator's Global Assessment, and skin hydration.
Results
While wearing Merino wool clothing, compared with standard clothing, statistically significant improvements were seen in mean Eczema Area and Severity Index scores, Dermatology Life Quality Index scores, and static Investigator's Global Assessment scores. No significant difference was seen with skin hydration. Wearing Merino wool clothing did not produce any negative cutaneous effects compared with wearing standard clothing.
Conclusions
Merino wool clothing compared with standard clothing provided improvements in severity of atopic dermatitis as well as quality of life in atopic patients.
Human beings rely on clothing to help regulate their body temperatures and thereby achieve thermal comfort. Establishing a trapped layer of still air against the skin by the use of fibers (eg, wool, cotton, polyester, fur, feathers) provides insulation from changes in external temperature.1 However, fiber types differ in their ability to absorb and release moisture. Wool has a unique moisture absorbance capacity, far higher than other common apparel types.2–5 Wool fibers are similar to human skin in that both are composed of the protein keratin and both are highly hygroscopic. Wool's ability to transfer moisture between the body and the environment helps buffer and maintain more stable conditions in the microclimate between the skin and the fabric.2
Regions of the skin affected by atopic dermatitis lose the ability to regulate moisture, so the impact on skin health of wearing moisture-regulating clothing composed of wool is a research question of interest. However, inappropriately designed wool clothing can feel “scratchy” and “rough” and can cause itching,6 especially in individuals with sensitive skin, including those with atopic dermatitis. Fabric-evoked prickle has been shown to result from low-grade activity in nociceptors stimulated by fiber ends protruding from the fabric surface.7 The strength of the stimuli is strongly related to fiber diameter8 and is independent of fiber type.9 Fabric-evoked prickle and potential itching are generally not sensed in fine Merino wool.9,10 Properly sourced and manufactured Merino wool clothing may be well tolerated and may actually be beneficial as an adjunct to other treatments. Su et al11 showed an improvement in SCORing Atopic Dermatitis scores in children wearing superfine Merino wool as compared with cotton clothing. Properties of wool fabrics including heat transmission and release of perspiration may increase skin comfort and reduce pruritus, compared with other fabrics.2
The objectives of this study were to evaluate the effect on atopic dermatitis of wearing fine Merino wool clothing versus standard clothing and to assess the effect of fine Merino wool clothing on quality of life in children and adults with atopic dermatitis aged 5 years and older.
MATERIALS AND METHODS
Subject and Enrollment Characteristics
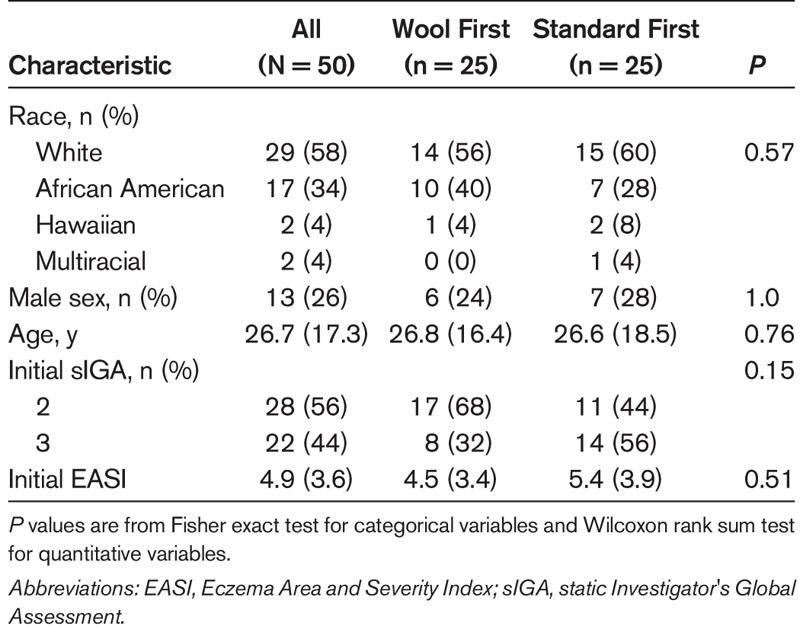
Subjects entered the study between March 13, 2017, and December 28, 2017. The final study visit occurred on March 31, 2018. Fifty-six subjects were enrolled in the study, 50 of whom completed the study, 4 of whom were lost to follow-up and unresponsive to attempts at contact, and 2 of whom were terminated early because of adverse events (AEs; 1 asthma attack and 1 flare-up of dermatitis). The results presented in all subsequent sections refer to the 50 subjects who completed the study. Table 1 provides summary statistics for participant characteristics and comparisons between assignment groups. Most subjects were white and female and had static Investigator's Global Assessment (sIGA) score of 2. The average age was 26.7 years.
TABLE 1.
Subject Characteristics at Enrollment
Although subjects obviously could not be blinded as to garment assignment, investigators were blinded when performing their assessments.
Design
Subjects were randomly allocated into 2 groups. They either wore their usual clothing for the first 6 weeks (standard first) and then switched to wool clothing for a further 6 weeks or wore the wool clothing first (wool first) followed by their usual clothing. The 2 cohorts were balanced with regard to demographic factors and initial atopic dermatitis condition. The following instructions were given to subjects:
Wear an ensemble (a top and a bottom) of your choosing for at least 6 continuous hours each day.
An ensemble may be worn as daytime wear or as nighttime wear.
Wash ensembles using Martha Gardener Country Homestead Eucalyptus Wool Mix detergent, unless otherwise authorized to use your usual washing product.
Each subject undertook an initial visit to establish baseline condition, followed by regular 3-week visits until completion of the study. The mean (SD) duration between visits was 21.8 (4.1) days. Seventy-eight percent of all visit 2 to 5 assessments occurred within 21 ± 3 days (3 weeks) of the previous assessment. Sixty-four percent of all final assessments occurred within 84 ± 3 days (12 weeks) of the initial assessment, that is, within the design window.
Garments
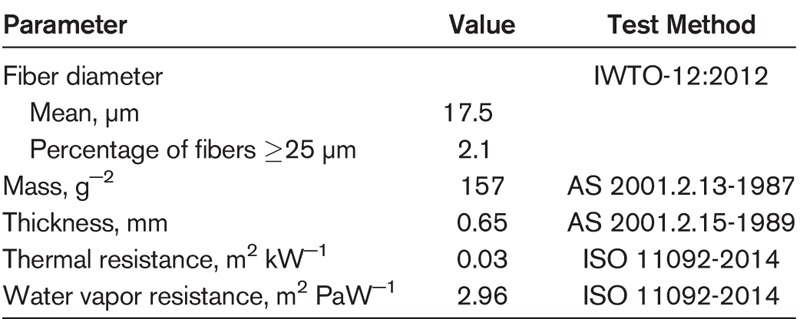
Commercially sourced 100% Merino wool base layer garments with a mean fiber diameter less than or equal to 17.5 μm were the treatment used in this study. The garments were made from 1 fabric quality, the details of which are included in Table 2. In contrast to the Merino wool used in this study, other wool fabrics often contain fibers of a larger diameter. This difference can account for the perceived “itchiness” or “roughness” noted in the past with some wool garments.
TABLE 2.
Details of the Wool Fabric Used in the Trial
Subjects were provided with a maximum of 4 different garment groups, as shown in Appendix 1.
No wool garments were included in the standard clothing.
Atopic Dermatitis and Quality-of-Life Assessment
At the initial and each subsequent visit, the following data were obtained: Eczema Area and Severity Index (EASI) score,12 Dermatology Life Quality Index (DLQI),13 and sIGA. Skin hydration was assessed with a Courage + Khazaka Corneometer, Model MDD 4 (Multi Display Device), using a CM825 probe. The device was able to be calibrated and had an ambient condition sensor for room temperature and relative humidity.
Statistical Methods
Baseline demographic and clinical characteristics were summarized with counts and percentages for categorical variables and means, standard deviations, medians, and extrema for quantitative variables. Comparison of baseline characteristics was analyzed using Fisher exact test for categorical variables and the Wilcoxon rank sum test for quantitative variables.
Two linear mixed-effects models were fitted for each of the EASI, DLQI, and skin hydration measurements:
The first model included the following 3 fixed factors: (1) time period, parametrized as weeks 1 to 6 versus weeks 7 to 12; (2) assigned group, parameterized as wool first or standard first; and (3) clothing material, parameterized as wool or standard. The model included random intercepts per subject. Standard analysis of variance tests of each factor was conducted.
The second model included 10 fixed factors—1 for each of the 5 visits for each of the 2 assigned groups—and no intercept. Tests comparing changes from visit to visit were conducted as appropriate linear contrasts applied to the fixed effects, for example, week 3 versus week 0 for the wool-first group. Random intercepts per subject were included in the model.
The EASI, DLQI, and skin hydration retention were summarized at baseline, week 6, and week 12 with means and standard deviations. Means and 95% confidence intervals were derived at each visit for each assignment group from the second mixed-effects model. The sIGA scores were summarized at each visit in each group with counts and percentages. Visit-to-visit changes within each group were tested with the Wilcoxon signed rank test and compared between groups with the Wilcoxon rank sum test. All analyses were conducted in the open source R software environment (R: A language and environment for statistical computing, version 3.5.0; R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Eczema Area and Severity Index Score and Investigator Assessment (sIGA)
Significant decreases in mean EASI scores from baseline to week 3 were seen in both groups, that is, those who wore regular clothing (standard first) and those who wore Merino wool (wool first). These decreases were sustained but did not further improved from week 3 to week 6. Those who switched to Merino wool at week 6 experienced a further significant decrease in EASI scores, in contrast to those who switched to regular clothing (Table 3, Fig. 1).
TABLE 3.
Results Associated With the Second Linear Mixed-Effects Model
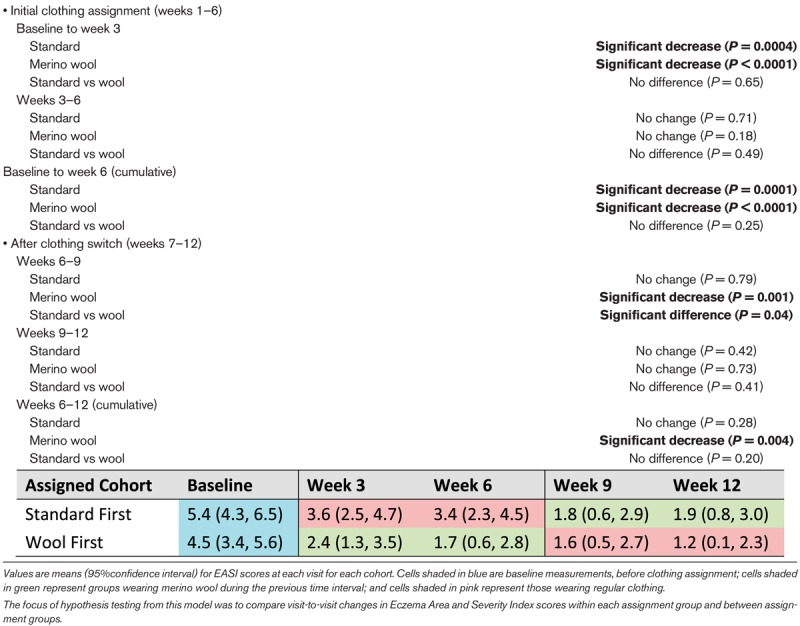
Figure 1.
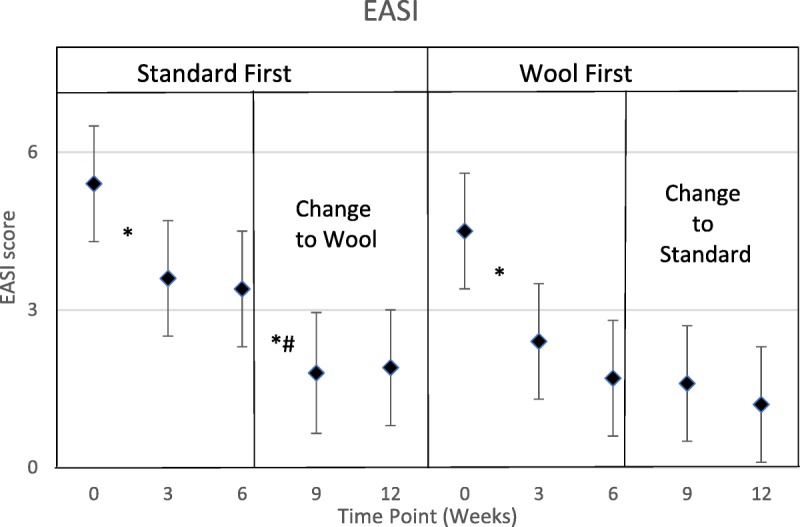
Mean EASI over time for the 2 study cohorts. The asterisk (*) indicates a significant reduction in EASI scores during the given interval. The dagger (#) indicates that the mean change in EASI scores was significantly different between the 2 cohorts. The results are associated with the second linear mixed-effects model.
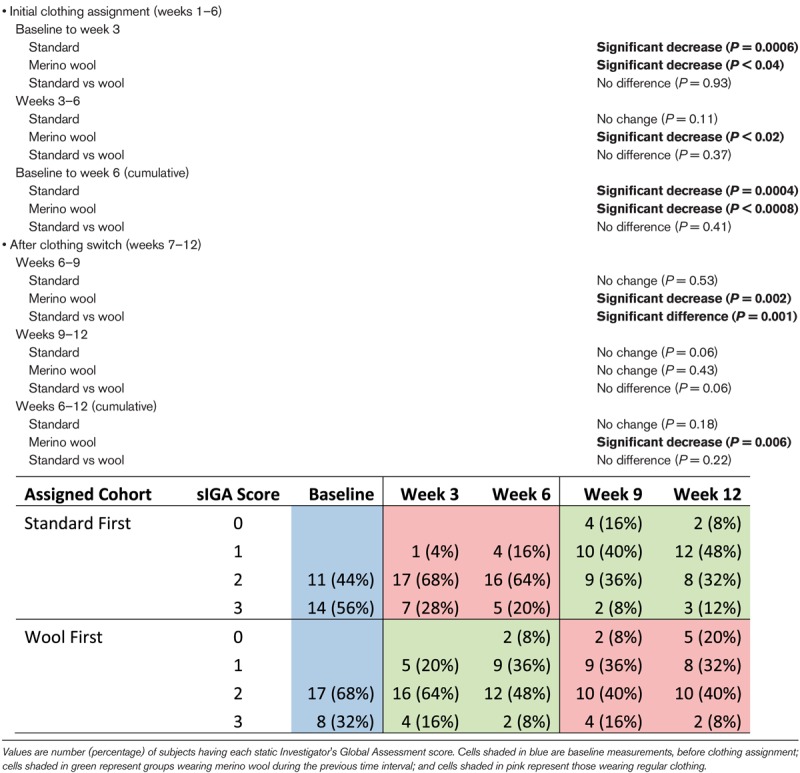
All subjects experienced decreases in sIGA in the initial study period from baseline to week 3 and cumulatively from baseline to week 6. Those wearing Merino wool experienced a significant decrease from week 3 to week 6. However, there were no differences in sIGA over the period from baseline to week 6. After the week 6 switch in clothing, the Merino wool group experienced significant decreases in sIGA from week 6 to week 9 and cumulatively from week 6 to week 12. Those wearing regular clothing did not exhibit any significant changes from week 6 to week 9 or to week 12. Those wearing Merino wool from week 6 to week 9 experienced significantly greater reductions in sIGA than those wearing regular clothing, but no other differences were significant, as shown in Table 4.
TABLE 4.
Summary Statistics for sIGA Scores by Week and Cohort
The factor of primary interest is the clothing type factor, which compares mean EASI when Merino wool is being worn with mean EASI when it is not being worn. This factor was significant (P = 0.02), because mean EASI was lower when Merino wool was being worn. In addition, mean EASI tended to decrease over time for all cohorts. The assignment group factor was not significant (P = 0.13), indicating that the order in which subjects wore Merino wool and regular clothing did not significantly impact mean EASI.
Quality of Life (DLQI)
Reduction in mean DLQI scores occurred only when Merino wool was worn, and these reductions occurred for the first 3 weeks of wearing Merino wool, that is, from baseline to week 3 in the wool-first cohort and from week 6 to week 9 in the standard clothing–first cohort, as shown in Table 5 and Figure 2.
TABLE 5.
Summary Statistics for DLQI Scores by Time Period and Cohort
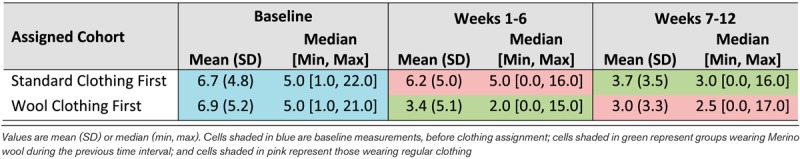
Figure 2.
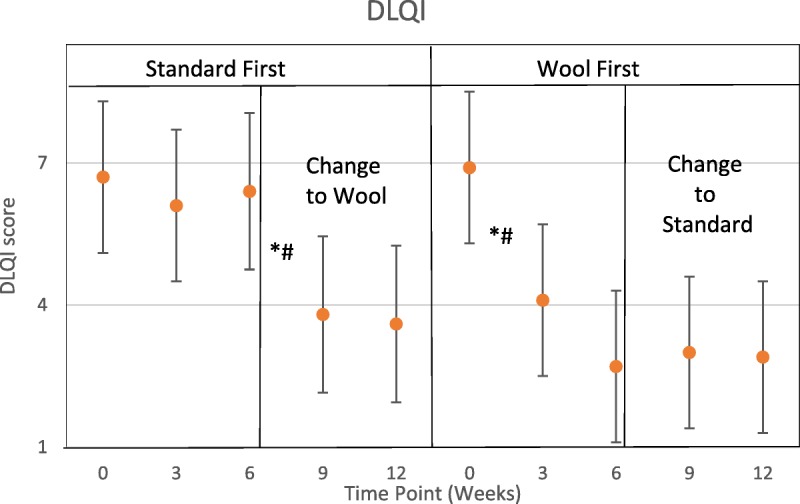
Mean DLQI over time for the 2 study cohorts. The asterisk (*) indicates a significant reduction in DLQI scores during the given interval. The dagger (†) indicates that the mean change in DLQI scores was significantly different between the 2 cohorts.
The clothing type factor was significant (P = 0.001), indicating that mean DLQI scores were lower when Merino wool was worn. The time period factor was significant (P < 0.0001), indicating that mean DLQI tended to decrease over time. The assignment group factor was nonsignificant (P = 0.06), indicating that the order in which subjects wore Merino wool and regular clothing did not significantly impact mean DLQI.
Skin Hydration
Increases in mean skin hydration occurred for both clothing types for the first 6 weeks. These increases were not significantly improved upon after the first 6 weeks. No statistically significant differences between Merino wool and regular clothing were observed. However, in those who wore wool first, hydration tended to decline after switching to standard clothing, and in those who wore standard clothing first, hydration tended to improve when switching to wool, as shown in Table 6 and Figure 3.
TABLE 6.
F Statistics and P Values for Study Factors From Model of Skin Hydration Scores
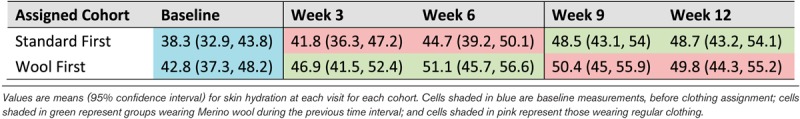
Figure 3.
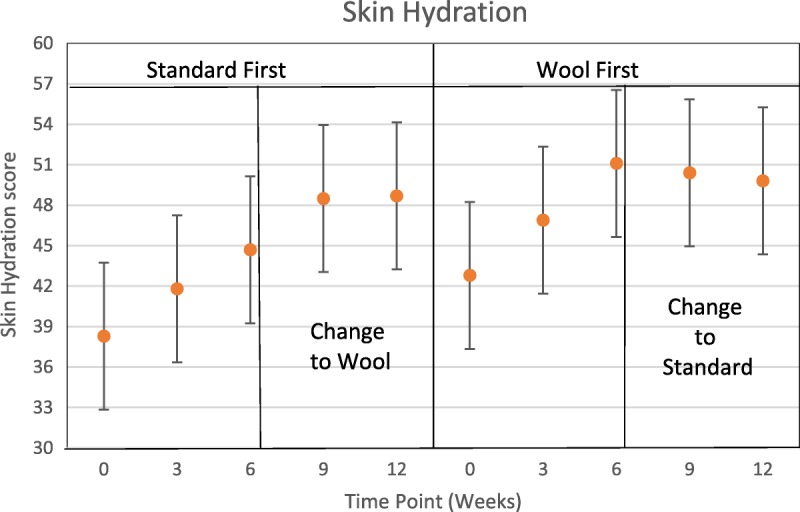
Mean skin hydration over time for the 2 study cohorts. No visit-to-visit comparisons were significant (only cumulative, 6-week comparisons).
Adverse Events
Fourteen AEs occurred involving 12 subjects, none of which was serious. One event was not resolved by the end of the study; all others were resolved. All AEs were single episode, except the unresolved AE that is continuous. Ten AEs were of moderate severity, and 4 were of mild severity. No AEs were related to clothing or to detergent use. Although all the AEs required medication, only 2 subjects required a prohibited concomitant medication and were discontinued from the study.
No AEs were related to clothing or detergent use; however, 5 events occurring in 4 subjects were of interest per protocol—that is, they occurred during or immediately after wearing the wool ensemble. Of these 4 subjects with AEs of interest, 2 were discontinued because of the need for a prohibited medication and therefore not included in the outcome measures. Adverse events of interest per the protocol and incidences in the study are listed hereinafter in parentheses.
The following AEs were recorded if they occurred during or immediately after wearing wool ensemble:
Increased irritation of the skin (1 subject had atopic flare, not in area of clothing, discontinued)
Increased skin dryness (none)
Increased pruritus (none)
Rash/allergic contact dermatitis (1 subject had poison ivy dermatitis on bilateral arms)
Irritation of the respiratory tract (1 subject had asthma and pneumonia and was discontinued; 1 had an upper respiratory tract infection)
Irritation of the eye (none)
Irritation of the nose (none)
Irritation of the gastrointestinal tract (none)
DISCUSSION
This study assessed atopic dermatitis severity using the EASI score and a static investigator's assessment. Both of these metrics showed improvement after subjects wore the wool clothing as compared with their own usual clothing. Those who wore the wool clothing first showed improvement as soon as 3 weeks after starting the program. When they switched back to their regular clothing, their scores remained stable, perhaps as a reflection of the improvement made while wearing the wool clothing. Those who started the study by staying with their regular clothing showed some initial improvement by week 3, likely because they were taking better care of their skin because they were enrolled in a research project. When they switched to the wool clothing after 6 weeks, they showed more marked improvement, however.
Of the 25 subjects with “mild” (17) to “moderate” (8) eczema by sIGA who wore the wool clothing initially, 2 were rated “clear” and 9 were scored as “mild” by week 6. Only 2 of 8 with a rating of “moderate” at baseline were still rated “moderate” at week 6. Of the 25 subjects (11 by “mild” and 14 by “moderate”) who started the study by staying with their regular clothing, only 4 improved to a “mild” score and none improved to “clear” by week 6.
Most important to our patients is their own rating of the severity of their eczema and their comfort. As measured by the DLQI, their severity was significantly improved when wearing the wool clothing, a fact that was surprising to some of them. A decrease in the symptoms of itchy, scratchy, and painful skin was the largest improvement, followed closely by a decrease in feelings of embarrassment and being self-conscious of skin appearance.
The only parameter we measured that did not demonstrate statistically significant improvement by wearing the fine-diameter Merino wool garments was skin hydration. However, the results of this measurement showed that there was a trend toward increased skin hydration when wearing wool, although it did not meet statistical significance. If a significant improvement in skin hydration is not the reason for improvement in atopic symptoms, it is uncertain why the improvement was seen. Perhaps, the improvement in hydration, although not meeting the definition of statistical significance, was enough to allow for symptom improvement. In addition, the Merino garments likely caused less frictional irritation than conventional clothing. Reduced cutaneous itch and pain were noted by our subjects, which also was likely to lead to improved EASI and sIGA scores for “the itch that rashes.”
Limitations
Although investigators were blinded as to clothing assignment when performing their assessments, subjects could not be when answering DLQI and adverse reaction questions.
CONCLUSIONS
The typical recommendation for clothing use by people with eczema has been to wear cotton or sometimes silk.14 It has been felt that these fibers offer superior softness and comfort compared with other types of fabrics. This study has demonstrated that wearing fine-diameter Merino wool garments may actually improve signs and symptoms in patients with mild to moderate atopic dermatitis. This is in contrast to the opinion of some patients and professionals15 who feel that wool clothing is necessarily scratchy and exacerbates irritation in individuals with sensitive skin. The Merino wool fiber used in the clothing for this study was all of fine diameter, which has been demonstrated to be comfortable to wear.10
Interestingly, a recent study of the use of silk clothing in individuals with moderate to severe atopic dermatitis showed no demonstrable benefit from wearing silk.16 This study and those of Su et al11 and Spelman et al17 show that fine-diameter Merino wool clothing should be considered acceptable for people with eczema and seems to be therapeutic to patients with mild to moderate atopic dermatitis.
Appendix 1

Plate 1. Illustration of the garment types used in the trial.
Wear ensemble (a top and a bottom) of your choosing for at least 6 continuous hours.
Ensemble may be worn as daytime wear or as nighttime wear.
Wash ensembles using Martha Gardener Country Homestead Eucalyptus Wool Mix, unless otherwise authorized to use your usual washing product.
Footnotes
This research is funded by Australian Wool Innovation Limited (AWI) which receives matching R&D funding from the Australian Government.
The authors have no funding or conflicts of interest to declare.
REFERENCES
- 1.Performance Apparel Markets. Temperature Control Fabrics: Optimising Wearer Comfort. Textile Intelligence Limited, 1st Quarter. Wilmslow, UK: Fulshaw Hall; 2013. [Google Scholar]
- 2.Li Y, Holcombe B, Apcar F. Moisture buffering behavior of hygroscopic fabric during wear. Text Res J 1992;62(11):619–627. [Google Scholar]
- 3.Schneider A, Holcombe B, Stephens L. Enhancement of coolness to the touch by hygroscopic fibers: part I: subjective trials. Text Res J 1996;66(8):515–520. [Google Scholar]
- 4.Li Y, Holcombe B, De Dear R. Enhancement of coolness to the touch by hygroscopic fibers: part II: physical mechanisms. Text Res J 1996;66(9):587–594. [Google Scholar]
- 5.Barnes J, Holcombe B. Moisture sorption and transport in clothing during wear. Text Res J 1996;66(12):777–786. [Google Scholar]
- 6.Bendsoe N, Björnberg A, Asnes H, et al. Itching from wool fibres in atopic dermatitis. Contact Dermatitis 1987;17(1):21–22. [DOI] [PubMed] [Google Scholar]
- 7.Garnsworthy RK, Gully RL, Kenins P, et al. Identification of the physical stimulus and the neural basis of fabric-evoked prickle. J Neurophysiol 1988;59:1083–1097. [DOI] [PubMed] [Google Scholar]
- 8.Naylor GRS, Stanton JH, Speijers J. Skin comfort of base layer wool garments. Part 2: fiber diameter effects on fabric and garment prickle. Text Res J 2014;84:1506. [Google Scholar]
- 9.Naylor GRS, Veitch CJ, Mayfield RJ, et al. Fabric-evoked prickle. Text Res J 1992;62(8):487–493. [Google Scholar]
- 10.McGregor BM, Naebe M, Stanton J, et al. Relationship between wearer prickle response with fibre and garment properties and Wool Comfort Meter assessment. J Text I 2013;104(6):618–627. [Google Scholar]
- 11.Su JC, Dailey R, Zallmann M, et al. Determining Effects of Superfine Sheep wool in Infantile Eczema (DESSINE): a randomized paediatric crossover study. Br J Dermatol 2017;177(1):125–133. [DOI] [PubMed] [Google Scholar]
- 12.Hanifin JM, Thurston M, Omoto M, et al. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp Dermatol 2001;10(1):11–18. [DOI] [PubMed] [Google Scholar]
- 13.Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19(3):210–216. [DOI] [PubMed] [Google Scholar]
- 14.Ricci G, Patrizi A, Bellini F, et al. Use of textiles in atopic dermatitis: care of atopic dermatitis. Curr Probl Dermatol 2006;33:127–143. [DOI] [PubMed] [Google Scholar]
- 15.Zallmann M, Smith PK, Tang MLK, et al. Debunking the myth of wool allergy: reviewing the evidence for immune and non-immune cutaneous reactions. Acta Dermatol Verereologica 2017;97:906–915. [DOI] [PubMed] [Google Scholar]
- 16.Thomas KS, Bradshaw LE, Sach TH, et al. Silk garments plus standard care compared with standard care for treating eczema in children: a randomised, controlled, observer-blind, pragmatic trial (CLOTHES Trial). PLoS Med 2017;14(4):e1002280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spelman LJ, Supranowicz MJ, Davidson KA, et al. An investigator blinded, clinical trial assessing the efficacy of Superfine Merino Wool Base Layer Garments (SMWBG) in children with atopic dermatitis (AD) measuring SCORAD, EASI, POEM and DSA scores. Biomed J Sci Tech Res 2018;7(1):46–52. [Google Scholar]


