Overview
Introduction
Distal biceps tendon ruptures can be repaired with either a single or a double-incision technique.
Step 1 (Single-Incision Technique): Surgical Exposure and Preparation of the Tendon
Through a single anterior incision, identify the tendon and debride the distal degenerated portion.
Step 2 (Single-Incision Technique): Preparation of the Radius
Expose the bicipital tuberosity and prepare the bone for insertion of suture anchors.
Step 3 (Single-Incision Technique): Tendon Reattachment
Suture the tendon with a reduction knot technique that allows for anatomic tendon apposition to bone.
Step 1 (Double-Incision Technique): Surgical Exposure and Preparation of the Tendon
Through a small anterior incision retrieve the tendon, debride the distal degenerated portion of the tendon, and place your sutures.
Step 2 (Double-Incision Technique): Preparation of the Radius
Through a second posterolateral incision, expose the biceps tuberosity and, using a burr, create a trough for the tendon.
Step 3 (Double-Incision Technique): Tendon Reattachment
Pass the sutures through the transosseous tunnels and tension the sutures, allowing the biceps tendon to be pulled into the trough created in the bicipital tuberosity, and then tie the sutures.
Step 4: Postoperative Care
Assess tension across the repaired tendon, initiate prophylaxis against heterotopic ossification, and begin rehabilitation.
Results
We recently conducted a prospective randomized controlled trial at our center comparing the single and double-incision techniques for the repair of acute distal biceps tendon ruptures11.
What to Watch For
Introduction
Distal biceps tendon ruptures can be repaired with either a single or a double-incision technique. Both techniques have been proven to be safe and reliable, and they offer similar outcomes with respect to recovery rates and final results. Traditionally, the single-incision technique required a larger anterior exposure, placing the radial nerve at risk; this led Boyd and Anderson to describe an alternative, double-incision technique1. Unfortunately, this double-incision technique was associated with the development of heterotopic ossification and synostosis. To address this, the technique was modified by Morrey et al. to include a posterolateral muscle-splitting approach, thereby reducing the likelihood of heterotopic ossification by avoiding subperiosteal exposure of the ulna2.
There have also been advancements in the single-incision technique. As fixation methods have improved (i.e., with the use of suture anchors3, interference screws4,5, and cortical buttons6,7), less exposure has been required for the single-incision method, thereby reducing the incidence of associated nerve injuries. The current literature contains several case series and biomechanical studies that support the use of both the single and the double-incision technique for repairing distal biceps ruptures8.
The key aspects of the single and double-incision techniques are similar.
Step 1: Surgical exposure and preparation of the tendon
Step 2: Preparation of the radius
Step 3: Tendon reattachment
Step 4: Postoperative care
This article will provide a detailed description of steps 1, 2, and 3 for each of the two techniques separately. The postoperative care (step 4) is similar for the two techniques and will be described at the end.
Step 1 (Single-Incision Technique [Video 1]): Surgical Exposure and Preparation of the Tendon
Through a single anterior incision, identify the tendon and debride the distal degenerated portion.
Position the patient supine on the operating room table, use regional or general anesthesia, and place a sterile tourniquet on the upper arm.
Make an 8-cm longitudinal incision beginning at the flexion crease and extending distally following the medial aspect of the brachioradialis. Identify and protect the lateral antebrachial cutaneous nerve. If required for exposure, gently retract it laterally.
Identify the proximally retracted biceps tendon by elevating the proximal portion of the incision with a blunt retractor. Sweep the tendon down into the wound using your finger while milking the biceps muscle from above if necessary.
Debride the distal degenerated portion of the tendon.
The tendon should be oriented correctly during repair. The entire biceps complex externally rotates 90° from origin to insertion. The short-head portion of the distal biceps tendon attaches on the distal aspect of the bicipital tuberosity while the long-head portion attaches on the proximal aspect of the bicipital tuberosity. The short-head tendon can be identified by locating the origin of the lacertus fibrosus, which originates from the short-head tendon9.
Video 1.
Video depicting single-incision distal biceps repair. (Reproduced with permission of the American SHLDR and Elbow Surgeons.)
Step 2 (Single-Incision Technique [Video 1]): Preparation of the Radius
Expose the bicipital tuberosity and prepare the bone for insertion of suture anchors.
Gently retract the brachioradialis laterally and the pronator teres medially.
Identify, ligate, and divide the recurrent leash of Henry in order to expose the bicipital tuberosity.
Scrape the tuberosity with a curet or, alternatively, create an intracortical facet with a high-speed burr to promote tendon healing.
Implant two suture anchors, each loaded with a single suture (e.g., a high-strength suture such as number-2 or 3 Ethibond [Ethicon, Somerville, New Jersey] or an alternative material such as another polyester braided suture, FiberWire [Arthrex, Naples, Florida], Hi-Fi [ConMed Linvatec, Largo, Florida), or ORTHOCORD (DePuy Synthes, Raynham, Massachusetts). Place the suture anchors approximately 1 cm apart, into the ulnar aspect of the bicipital tuberosity directed toward the intramedullary cavity. Check the position of the anchors using fluoroscopy.
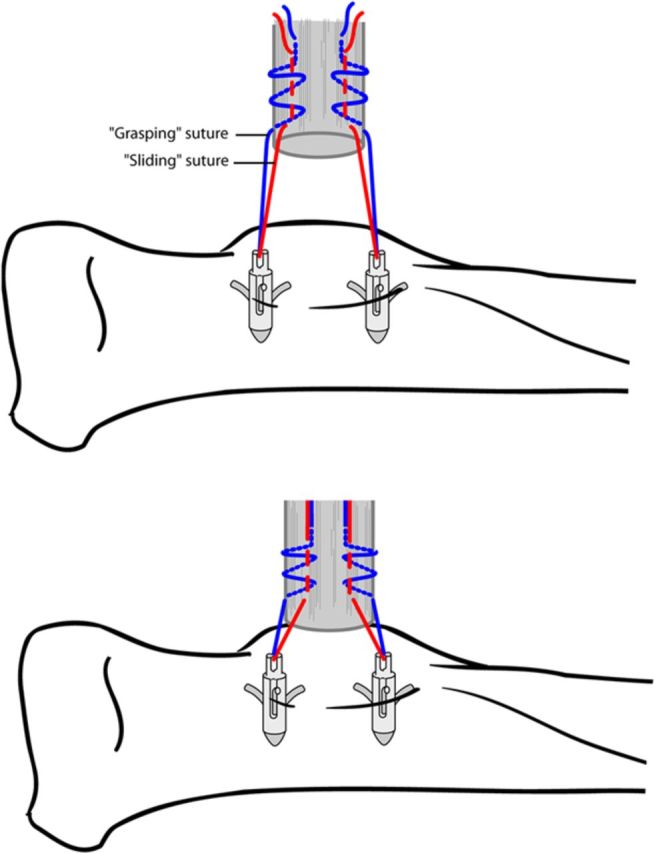
Step 3 (Single-Incision Technique [Video 1]): Tendon Reattachment
Suture the tendon with a reduction knot technique10 that allows for anatomic tendon apposition to bone.
Ensure that the tendon is oriented correctly while placing the sutures.
Place one end of the suture as a sliding stitch 1.5 cm up from the end of the tendon.
Using the other end of the suture, place three or four grasping stitches around the sliding stitch, making sure that it still slides.
Once both pairs of sutures have been passed, pull both the sliding ends to dock the end of the tendon to the bicipital tuberosity (Fig. 1).
Tension the sutures with the elbow in 45° to 60° of flexion and full supination and then tie. To augment the strength of the suture repair, particularly if the quality of the tendon is suboptimal, the ends of the tied sutures can be used to place additional locking sutures into the more proximal aspect of the tendon.
Use copious irrigation to remove all bone debris to lessen the risk of heterotopic ossification.
Release the tourniquet and ensure hemostasis prior to wound closure.
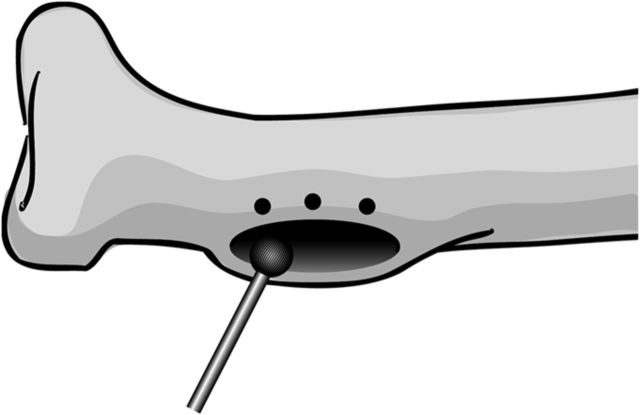
Fig. 1.

An illustration of the reduction knot technique, showing the grasping arm (blue) and the sliding arm (red). When both sliding arms are pulled, the tendon advances and becomes docked against the bone. (Reproduced, with permission, from: Drosdowech DS, Faber KJ, King GJW. Distal biceps tendon repair: one- and two-incision techniques. Tech Shoulder Elbow Surg. 2002;3:90-5.)
Step 1 (Double-Incision Technique): Surgical Exposure and Preparation of the Tendon
Through a small anterior incision retrieve the tendon, debride the distal degenerated portion of the tendon, and place your sutures.
Make a 2-cm transverse incision in the antecubital crease.
Bluntly dissect in the deeper tissue planes, ensuring that the neurovascular structures are protected as described above.
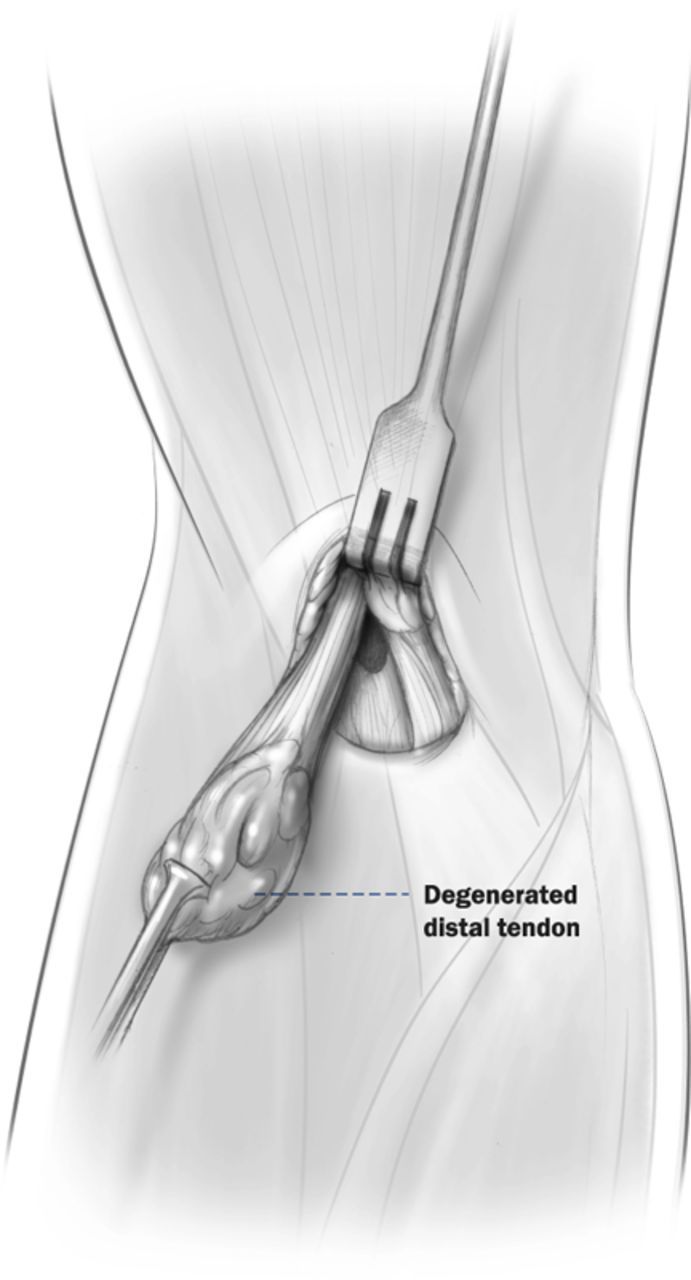
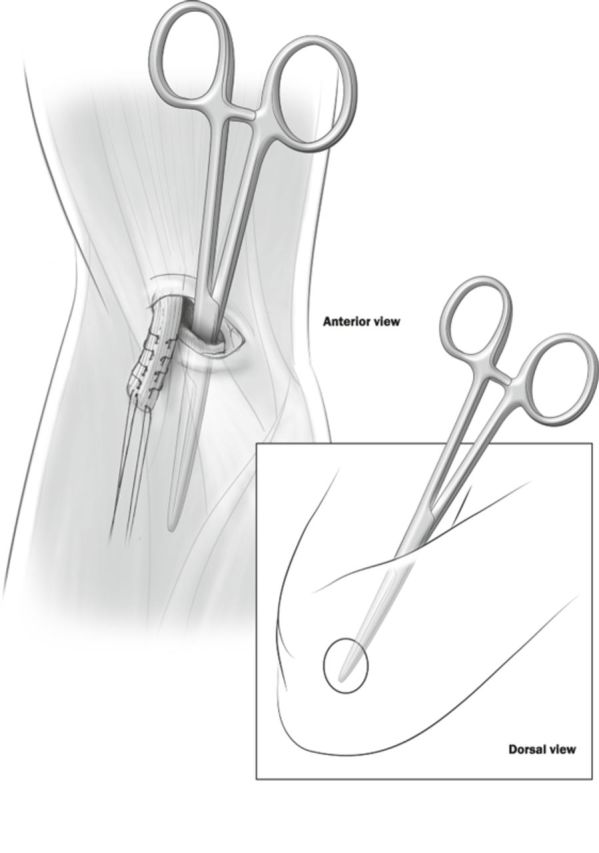
Identify the distal stump of the biceps tendon and debride the distal degenerated portion (Fig. 2-A).
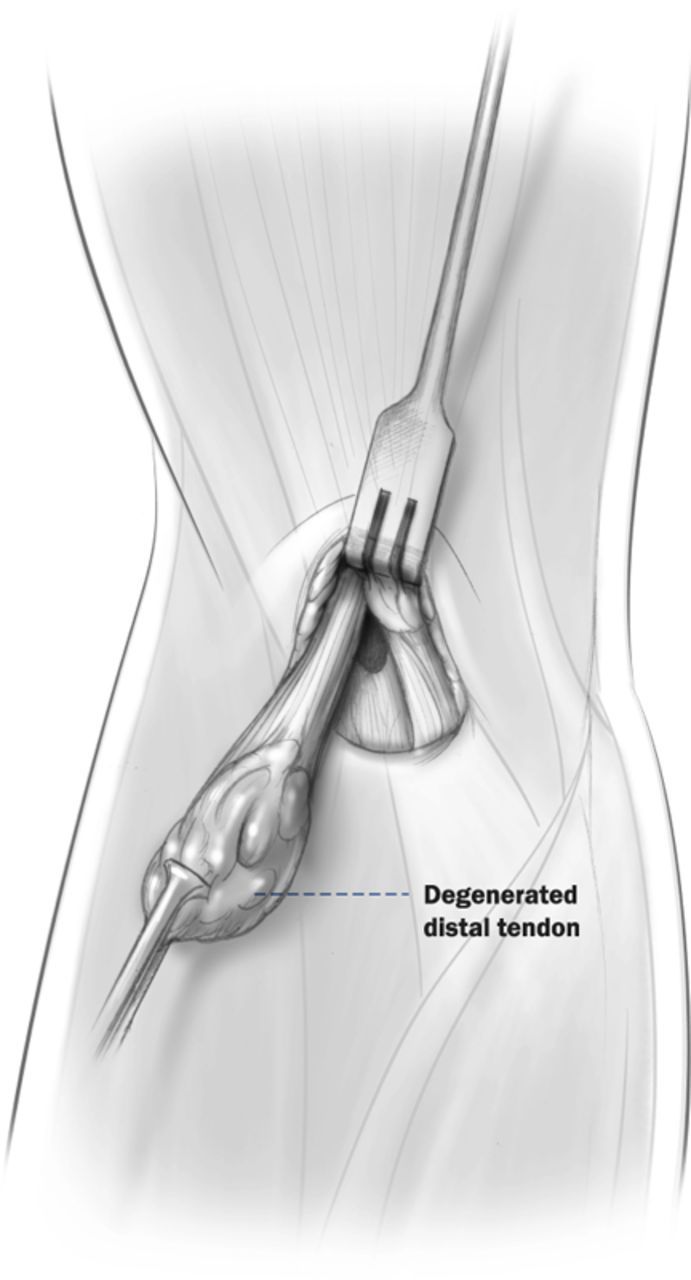
Pass two sutures (e.g., number-2 or 3 Ethibond or an alternative material such as FiberWire, Hi-Fi, or ORTHOCORD) through the distal tendon using the locking Krackow technique (Fig. 2-B).
Cut both arms of one suture shorter than the arms of the other pair. This will aid in identifying each suture arm later.
Fig. 2-A.
Distal stump of the biceps tendon with a degenerated distal end.
Fig. 2-B.
The prepared tendon, with the degenerated end debrided and locking Krackow sutures in place.
Step 2 (Double-Incision Technique): Preparation of the Radius
Through a second posterolateral incision, expose the biceps tuberosity and, using a burr, create a trough for the tendon.
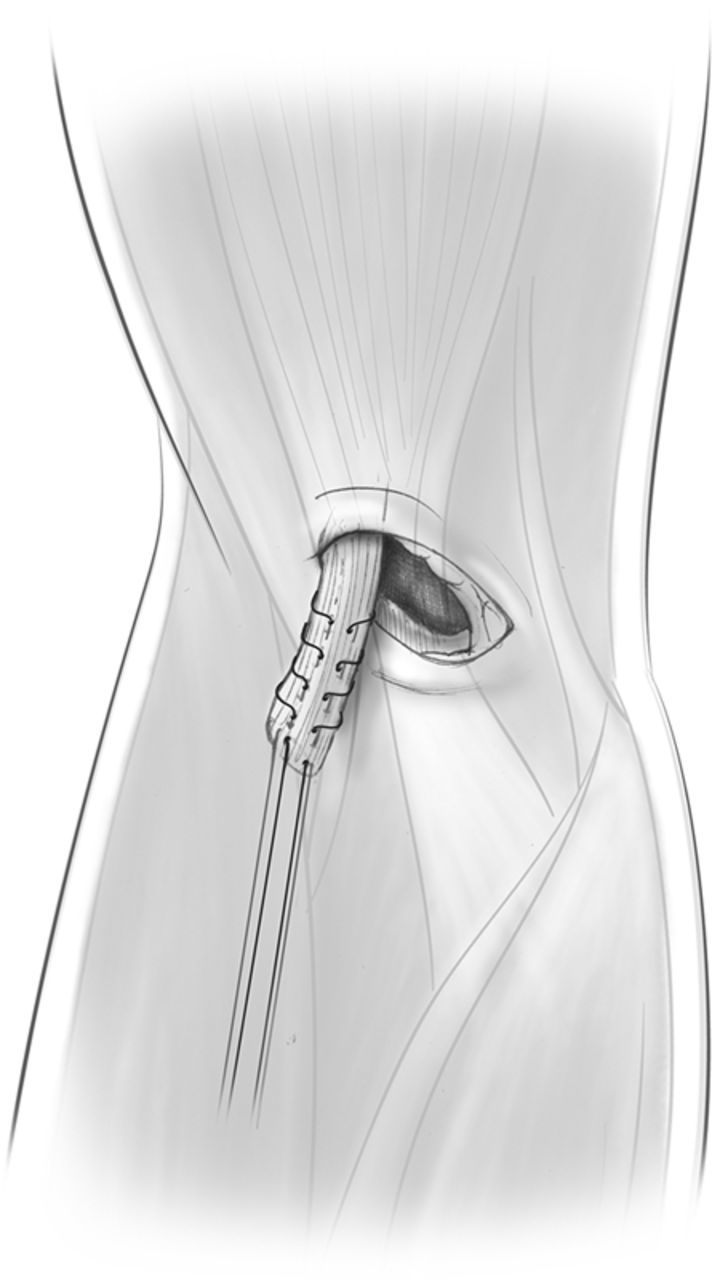
Palpate the biceps tuberosity with your index finger through the anterior incision and pass a curved clamp (carrying the four suture arms) ulnar to it. Direct the clamp through the interosseous space toward the dorsal aspect of the forearm, with the curved portion of the clamp facing laterally. Hold the forearm in maximal pronation to protect the posterior interosseous nerve while passing the clamp.
Maintain contact with the radius at all times and stay away from the ulna.
Advance the clamp through the common extensor musculature (Fig. 3), avoiding the subperiosteal ulnar interval. The clamp will be seen tenting the skin over the dorsal aspect of the proximal part of the forearm (Fig. 3).
Make a 3 to 4-cm incision directly over the clamp.
Expose the tuberosity with a muscle-splitting technique with the forearm maximally pronated.
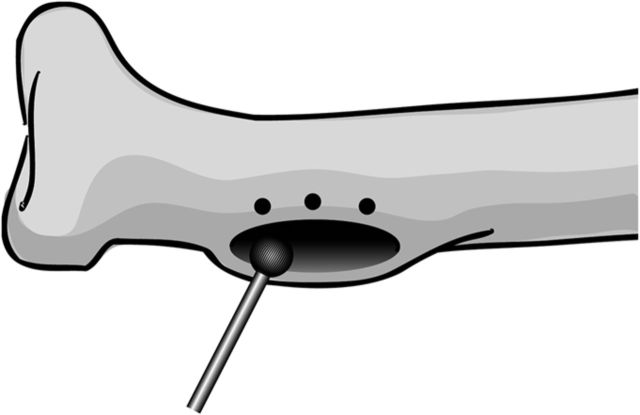
Use a small round burr to create an oval trough in the ulnar aspect of the bicipital tuberosity that communicates with the intramedullary cavity (Fig. 4). The trough should be large enough to allow the tendon to be docked into the radius.
Fig. 3.
The clamp advanced toward the common extensor muscle. The clamp is seen tenting the skin dorsally (circle), which is the site of the second incision.
Fig. 4.
Prepared bicipital tuberosity. (Reproduced, with permission, from: Drosdowech DS, Faber KJ, King GJW. Distal biceps tendon repair: one- and two-incision techniques. Tech Shoulder Elbow Surg. 2002;3:90-5.)
Step 3 (Double-Incision Technique): Tendon Reattachment
Pass the sutures through the transosseous tunnels and tension the sutures, allowing the biceps tendon to be pulled into the trough created in the bicipital tuberosity, and then tie the sutures.
Maintain the forearm in maximal pronation throughout the procedure to allow for maximal exposure of the docking site and to protect the posterior interosseous nerve.
Drill three 2.0-mm drill holes anterior to the trough, ensuring that these holes are at least 5 mm apart and 2 mm away from the cortical edge.
Use caution to avoid breaking the bone bridges when passing and tying the sutures.
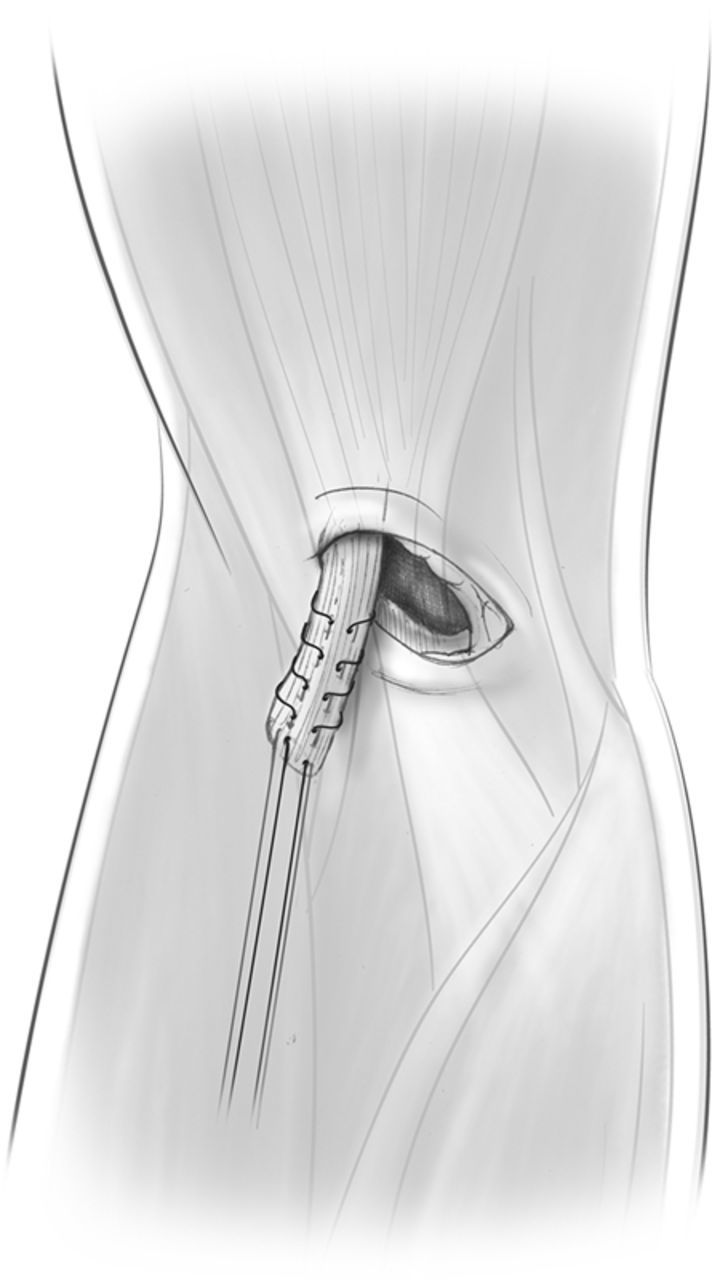
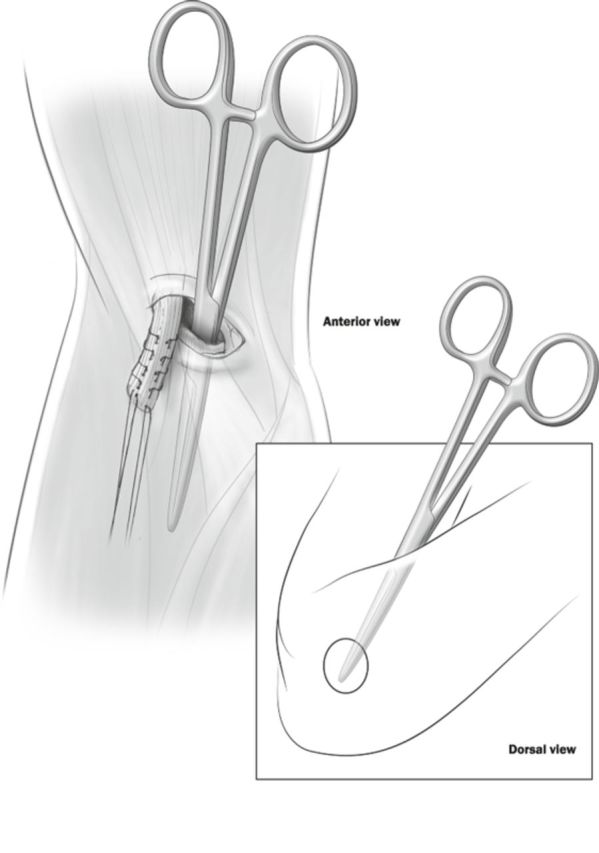
Using a suture retriever, pass the tendon sutures through the trough, exiting through the drill holes above.
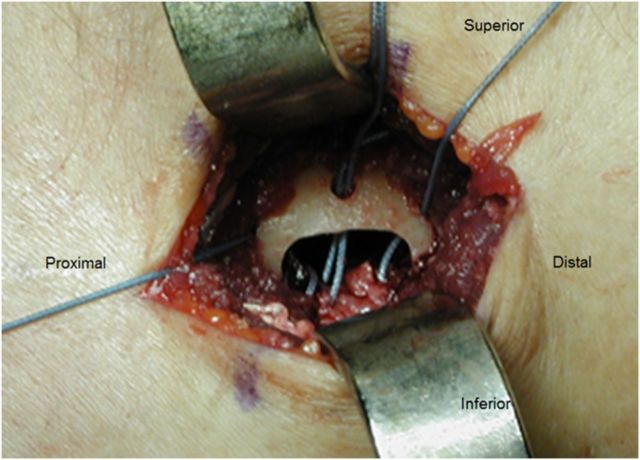
Ensuring that the orientation of the tendon is correct, pass one long and one short suture through the middle hole and one in each of the proximal and distal holes (Fig. 5).
With the elbow in 90° flexion and the forearm in neutral rotation, pull the biceps tendon into the trough created in the bicipital tuberosity and tension the sutures.
Tie the long sutures to each other and the short sutures to each other over a different bone bridge.
Use copious irrigation to remove all bone debris to lessen the risk of heterotopic ossification.
Deflate the tourniquet and ensure hemostasis prior to wound closure.
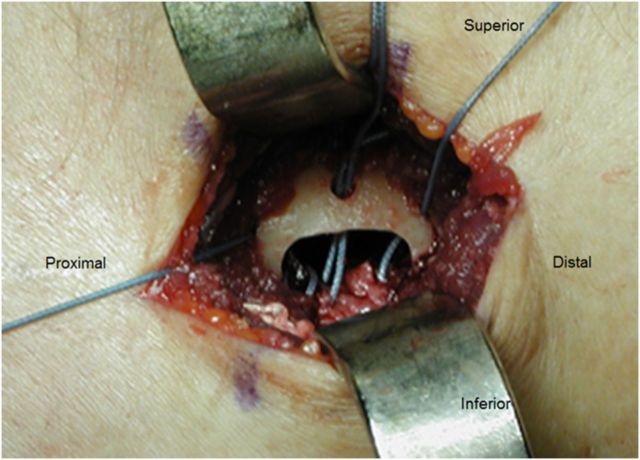
Fig. 5.
Distal biceps tendon with sutures advanced through the transosseous tunnels in preparation for docking of the tendon in the trough.
Step 4: Postoperative Care
Assess tension across the repaired tendon, initiate prophylaxis against heterotopic ossification, and begin rehabilitation.
Assess the range of elbow extension intraoperatively. If it is limited, take note of the angle beyond which the tendon is felt to be tight. Limit extension beyond this point in the early postoperative period to ensure that excessive tension is not placed across the repaired tendon.
Splint the elbow in 90° of flexion and full supination.
Consider prophylaxis against heterotopic ossification if no contraindications exist. We typically prescribe 25 mg of indomethacin (orally three times daily) along with a cytoprotective agent for three weeks.
Begin elbow mobilization two to three days postoperatively. During our study11, patients were instructed to perform active extension, active pronation, passive flexion, and passive supination exercises. A removable splint was worn at all times, except when the patients performed the prescribed exercises. Nonadherence to active-use restrictions was the primary reason for rupture; thus, when making immobilization choices and precautions, consider indicators of a lack of adherence to the postoperative plan.
Limit extension if full elbow extension was not easily achieved intraoperatively, allowing a 10° increase per week until full extension is achieved.
At six weeks, discard the resting splint and begin unlimited active range-of-motion exercises. Strengthening can begin between ten and twelve weeks postoperatively. Unrestricted activity can begin between four and six months.
Results
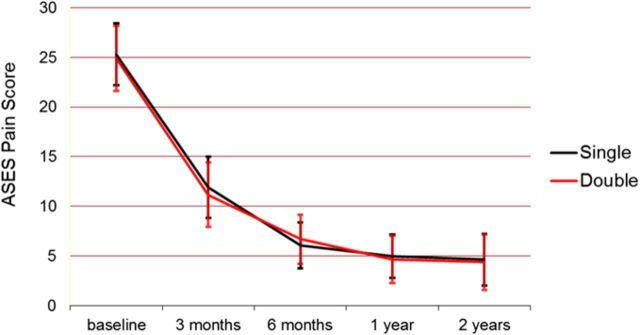
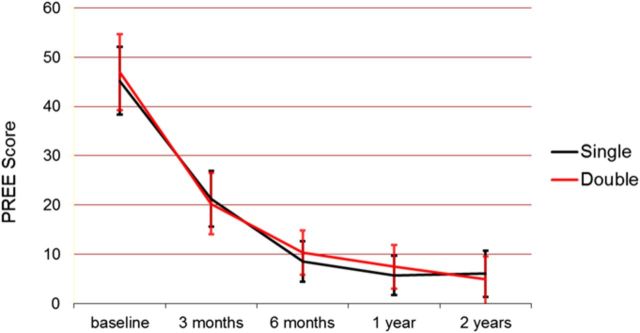
We recently conducted a prospective randomized controlled trial at our center comparing the single and double-incision techniques for the repair of acute distal biceps tendon ruptures11. Ninety-one patients were recruited and randomized (forty-four in the double-incision group and forty-seven in the single-incision group). Seventy-two (79%) of the ninety-one patients completed a minimum of one year of follow-up (both outcome questionnaires and range-of-motion/strength assessment). An additional eleven patients could not return for clinical assessment but completed outcome questionnaires at two years. In total, eighty-three (91%) of the ninety-one patients completed outcome questionnaires at the time of the two-year follow-up.
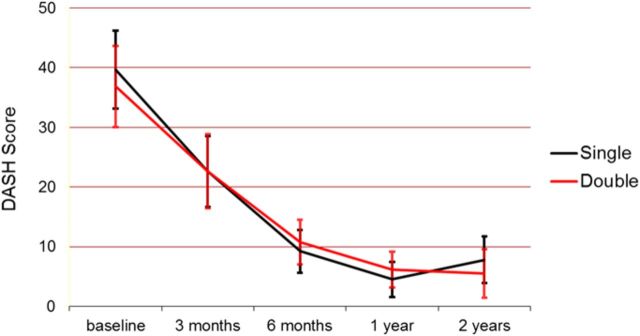
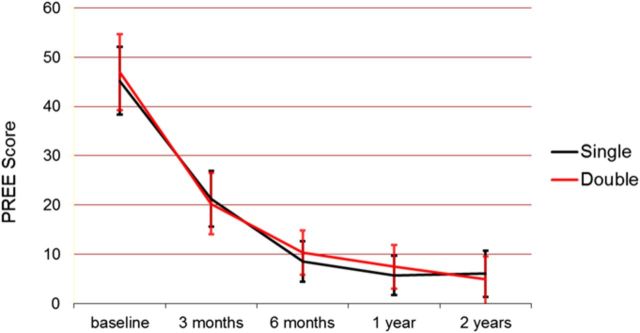
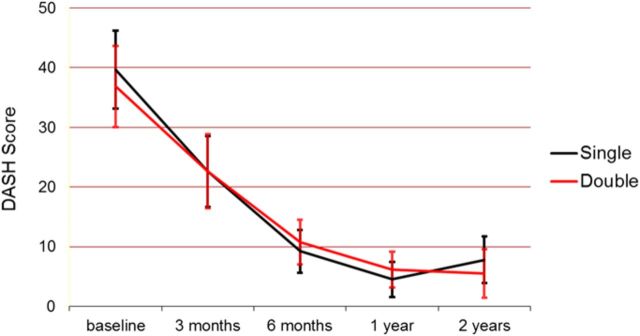
There was no difference in the mean outcome scores (the American Shoulder and Elbow Surgeons [ASES] elbow score, Patient-Rated Elbow Evaluation [PREE] score, or Disabilities of the Arm, Shoulder and Hand [DASH] score) between the two groups in either the short term (three to six months) or the long term (twelve to twenty-four months) (Figs. 6-A, 6-B, and 6-C). The single-incision technique resulted in a significantly higher overall complication rate, primarily due to a high number of early transient neurapraxias involving the lateral antebrachial cutaneous nerve (nineteen of forty-seven in the single-incision group and three of forty-three in the double-incision group, p < 0.001). Most neurapraxias in the single-incision group resolved; however, three patients remained symptomatic beyond six months, and two of them continued to have mild symptoms at the time of final follow-up. Four tendon reruptures were observed (three of forty-seven in the single-incision group and one of forty-three in the double-incision group), all of which were related to noncompliance or reinjury during the early postoperative period and appeared to be unrelated to the fixation technique (p = 0.3). Two patients developed very mild heterotopic ossification, with no resultant loss of elbow or forearm motion.
Fig. 6-A.
Mean ASES elbow pain score.
Fig. 6-B.
Mean PREE score.
Fig. 6-C.
Mean DASH score.
What to Watch For
Indications
Acute distal biceps rupture (less than four weeks postinjury)
Patients whose recreational and vocational activities require optimal supination and flexion strength
Contraindications
Medical comorbidities that preclude surgery
Pitfalls & Challenges
Obtaining exposure of the operative site and maintaining correct forearm and elbow positioning require at least one dedicated assistant.
Single-incision technique: Care must be taken to avoid aggressive retraction of the lateral antebrachial cutaneous nerve.
Double-incision technique: To minimize the risk of developing heterotopic bone formation, care must be taken to avoid subperiosteal exposure of the ulna during tendon passage and to remove bone debris created by use of the burr.
Chronic distal biceps tendon ruptures may require additional considerations such as the use of autografts or allografts.
Clinical Comments
Which approach do you recommend?
The literature demonstrates similar clinical outcomes and recovery rates between the two techniques8,11-13. Biomechanical cadaveric studies comparing the strengths of the two types of repair have also demonstrated similar results. Some studies have demonstrated transosseous sutures (the double-incision technique) to have a greater load to failure compared with suture anchors (the single-incision technique)14,15 whereas the results of other studies have favored suture anchors16. Some authors have reported that the double-incision technique results in a more anatomic repair17,18, possibly offering an advantage with regard to recovery of supination strength18. This has not yet been proven in a clinical trial, to our knowledge. Results are generally successful and reliable regardless of the technique that is used. We recommend that surgeons use the approach with which they are most familiar.
Will I have better results if I use a stronger suture material such as FiberWire?
Number-2 Ethibond was the suture material used for tendon repair in the randomized controlled trial comparing the single and double-incision techniques at our center11; however, other polyester braided sutures or other high-strength suture materials can also be used. In recent years, newer suture materials (i.e., FiberWire, Hi-Fi, and ORTHOCORD) have been introduced in orthopaedics; however, it is not known whether they offer any significant advantages over the standard suture material. Bisson et al. compared Ethibond with FiberWire in a cadaveric model using the two-incision technique for repair of the distal biceps tendon19. They reported no difference in the maximal failure strength of the sutures, but a greater percentage of the FiberWire sutures failed with repetitive cyclic loading. Failure occurred as a result of shredding of the tendon by the Bunnell suture. Whether similar results would be seen with the more commonly used Krackow stitch is unknown.
Have any advantages been seen with fixation techniques other than those described above?
There has been recent interest in the use of alternative fixation techniques, such as interference screws or cortical buttons, for the repair of distal biceps tendons. To date, they have not been proven to be clinically superior to suture anchors and were not included as a part of our study11.
Biomechanical studies have demonstrated that cortical buttons have superior pullout strength when compared with transosseous tunnels, suture anchors, and interference screws20-22, with favorable clinical results demonstrated in small case series7,23-25. Reported complications have included osteolysis with interference screws26, interference screw failure27, and EndoButton failure28, including possible radial neck fractures29. However, to our knowledge, there have not been any clinical trials comparing these techniques.
Can I be more aggressive with my postoperative rehabilitation protocol?
With both the single and the double-incision repair, recent trends are moving toward more aggressive rehabilitation, particularly when fixation is performed with a cortical button. Since the completion of our randomized trial11, we have also followed the trends toward earlier, more aggressive rehabilitation; however, at present, this approach is unproven. Increasingly, our postoperative immobilization consists only of a soft sling, allowing active flexion and supination of the elbow immediately. We have patients discontinue using the sling at six weeks and begin resisted exercises at ten weeks. We might consider more traditional rigid removable splints for patients who, for whatever reason, appear to be at risk of nonadherence to postoperative activity restrictions during the first six-week interval. While the literature does support the safe use of early range-of-motion protocols following acute distal biceps tendon repairs19,30, this was not evaluated in our study and we recommend caution as potential failure is likely to occur at the weakest link—the degenerated tendon.
Based on an original article: J Bone Joint Surg Am. 2012 Jul 3;94(13):1166-74.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Boyd H Anderson L. A method for reinsertion of the distal biceps brachii tendon. J Bone Joint Surg Am. 1961;43A:1041-3. [Google Scholar]
- 2. Morrey BF Askew LJ An KN Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985 Mar;67(3):418-21. [PubMed] [Google Scholar]
- 3. Khan AD Penna S Yin Q Sinopidis C Brownson P Frostick SP. Repair of distal biceps tendon ruptures using suture anchors through a single anterior incision. Arthroscopy. 2008 Jan;24(1):39-45. Epub 2007 Nov 28. [DOI] [PubMed] [Google Scholar]
- 4. Khan W Agarwal M Funk L. Repair of distal biceps tendon rupture with the Biotenodesis screw. Arch Orthop Trauma Surg. 2004 Apr;124(3):206-8. Epub 2004 Feb 3. [DOI] [PubMed] [Google Scholar]
- 5. Silva J Eskander MS Lareau C DeAngelis NA. Treatment of distal biceps tendon ruptures using a single-incision technique and a Bio-Tenodesis screw. Orthopedics. 2010 Jul 13;33(7):477 doi: 10.3928/01477447-20100526-09. [DOI] [PubMed] [Google Scholar]
- 6. Greenberg JA. Endobutton repair of distal biceps tendon ruptures. J Hand Surg Am. 2009 Oct;34(8):1541-8. [DOI] [PubMed] [Google Scholar]
- 7. Peeters T Ching-Soon NG Jansen N Sneyers C Declercq G Verstreken F. Functional outcome after repair of distal biceps tendon ruptures using the endobutton technique. J Shoulder Elbow Surg. 2009 Mar-Apr;18(2):283-7. Epub 2008 Dec 19. [DOI] [PubMed] [Google Scholar]
- 8. Keener JD. Controversies in the surgical treatment of distal biceps tendon ruptures: single versus double-incision repairs. J Shoulder Elbow Surg. 2011 Mar;20(2 Suppl):S113-25. [DOI] [PubMed] [Google Scholar]
- 9. Athwal GS Steinmann SP Rispoli DM. The distal biceps tendon: footprint and relevant clinical anatomy. J Hand Surg Am. 2007 Oct;32(8):1225-9. [DOI] [PubMed] [Google Scholar]
- 10. Drosdowech DS Faber KJ King GJW. Distal biceps tendon repair: one- and two-incision techniques. Tech Shoulder Elbow Surg. 2002;3:90-5. [Google Scholar]
- 11. Grewal R Athwal GS MacDermid JC Faber KJ Drosdowech DS El-Hawary R King GJW. Single versus double-incision technique for the repair of acute distal biceps tendon ruptures: a randomized clinical trial. J Bone Joint Surg Am. 2012 Jul 3;94(13):1166-74. [DOI] [PubMed] [Google Scholar]
- 12. Citak M Backhaus M Seybold D Suero EM Schildhauer TA Roetman B. Surgical repair of the distal biceps brachii tendon: a comparative study of three surgical fixation techniques. Knee Surg Sports Traumatol Arthrosc. 2011 Nov;19(11):1936-41. Epub 2011 Jun 29. [DOI] [PubMed] [Google Scholar]
- 13. El-Hawary R Macdermid JC Faber KJ Patterson SD King GJ. Distal biceps tendon repair: comparison of surgical techniques. J Hand Surg Am. 2003 May;28(3):496-502. [DOI] [PubMed] [Google Scholar]
- 14. Berlet GC Johnson JA Milne AD Patterson SD King GJ. Distal biceps brachii tendon repair. An in vitro biomechanical study of tendon reattachment. Am J Sports Med. 1998 May-Jun;26(3):428-32. [DOI] [PubMed] [Google Scholar]
- 15. Pereira DS Kvitne RS Liang M Giacobetti FB Ebramzadeh E. Surgical repair of distal biceps tendon ruptures: a biomechanical comparison of two techniques. Am J Sports Med. 2002 May-Jun;30(3):432-6. [DOI] [PubMed] [Google Scholar]
- 16. Lemos SE Ebramzedeh E Kvitne RS. A new technique: in vitro suture anchor fixation has superior yield strength to bone tunnel fixation for distal biceps tendon repair. Am J Sports Med. 2004 Mar;32(2):406-10. [DOI] [PubMed] [Google Scholar]
- 17. Hasan SA Cordell CL Rauls RB Bailey MS Sahu D Suva LJ. Two-incision versus one-incision repair for distal biceps tendon rupture: a cadaveric study. J Shoulder Elbow Surg. 2012 Jul;21(7):935-41. Epub 2011 Aug 3. [DOI] [PubMed] [Google Scholar]
- 18. Schmidt CC Weir DM Wong AS Howard M Miller MC. The effect of biceps reattachment site. J Shoulder Elbow Surg. 2010 Dec;19(8):1157-65. Epub 2010 Oct 8. [DOI] [PubMed] [Google Scholar]
- 19. Bisson LJ de Perio JG Weber AE Ehrensberger MT Buyea C. Is it safe to perform aggressive rehabilitation after distal biceps tendon repair using the modified 2-incision approach? A biomechanical study. Am J Sports Med. 2007 Dec;35(12):2045-50. Epub 2007 Aug 16. [DOI] [PubMed] [Google Scholar]
- 20. Kettler M Lunger J Kuhn V Mutschler W Tingart MJ. Failure strengths in distal biceps tendon repair. Am J Sports Med. 2007 Sep;35(9):1544-8. Epub 2007 Mar 29. [DOI] [PubMed] [Google Scholar]
- 21. Mazzocca AD Burton KJ Romeo AA Santangelo S Adams DA Arciero RA. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007 Feb;35(2):252-8. Epub 2006 Dec 27. [DOI] [PubMed] [Google Scholar]
- 22. Greenberg JA Fernandez JJ Wang T Turner C. EndoButton-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2003 Sep-Oct;12(5):484-90. [DOI] [PubMed] [Google Scholar]
- 23. Dillon MT Bollier MJ King JC. Repair of acute and chronic distal biceps tendon ruptures using the EndoButton. Hand (N Y). 2011 Mar;6(1):39-46. Epub 2010 Jul 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gupta RK Bither N Singh H Kapoor S Chhabra A Garg S. Repair of the torn distal biceps tendon by endobutton fixation. Indian J Orthop. 2012 Jan;46(1):71-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Heinzelmann AD Savoie FH 3rd Ramsey JR Field LD Mazzocca AD. A combined technique for distal biceps repair using a soft tissue button and biotenodesis interference screw. Am J Sports Med. 2009 May;37(5):989-94. Epub 2009 Apr 3. [DOI] [PubMed] [Google Scholar]
- 26. Potapov A Laflamme YG Gagnon S Canet F Rouleau DM. Progressive osteolysis of the radius after distal biceps tendon repair with the bioabsorbable screw. J Shoulder Elbow Surg. 2011 Jul;20(5):819-26. Epub 2011 May 24. [DOI] [PubMed] [Google Scholar]
- 27. Naidu SH. Interference screw failure in distal biceps endobutton repair: case report. J Hand Surg Am. 2010 Sep;35(9):1510-2. [DOI] [PubMed] [Google Scholar]
- 28. Desai SS Larkin BJ Najibi S. Failed distal biceps tendon repair using a single-incision EndoButton technique and its successful treatment: case report. J Hand Surg Am. 2010 Dec;35(12):1986-9. Epub 2010 Nov 5. [DOI] [PubMed] [Google Scholar]
- 29. Sutton KM Dodds SD Ahmad CS Sethi PM. Surgical treatment of distal biceps rupture. J Am Acad Orthop Surg. 2010 Mar;18(3):139-48. [DOI] [PubMed] [Google Scholar]
- 30. Cil A Merten S Steinmann SP. Immediate active range of motion after modified 2-incision repair in acute distal biceps tendon rupture. Am J Sports Med. 2009 Jan;37(1):130-5. Epub 2008 Oct 28. [DOI] [PubMed] [Google Scholar]