Overview
Introduction
We describe a technique consisting of simultaneous radial closing-wedge and ulnar shortening osteotomy to treat malunion of distal radial fractures.
Step 1: Preoperative Planning
Plan the radial closing-wedge osteotomy to correct the volar tilt angle to 8.5° to 15.5° and the ulnar shortening osteotomy to restore ulnar variance to −2.5 to 0.5 mm.
Step 2: Radial Closing-Wedge Osteotomy
Remove the wedge of bone from the radius and reduce the distal fragment, keeping the dorsal cortex as a hinge.

Step 3: Distal Ulnar Shortening Osteotomy
Resect the section of the ulna equivalent to the positive ulnar variance with transverse osteotomies.

Step 4: Plate Fixation of the Radial Osteotomy Site
Hold together the two fragments of the radius with a Kirschner wire and fix the osteotomy site with a volar locking plate.
Step 5: Proximal Ulnar Shortening Osteotomy
Evaluate residual ulnar positive variance with fluoroscopy and restore the ulnar variance to within a normal range by removing additional bone from the proximal fragment.

Step 6: Plate Fixation of the Ulnar Osteotomy Site
Use a compression device to close and fix the ulnar osteotomy site.

Step 7: Postoperative Management
Allow early motion immediately after the operation.
Results
We retrospectively evaluated forty-two patients at a minimum of one year after treatment of an extra-articular distal radial malunion with a radial corrective osteotomy.
What to Watch For
Introduction
We describe a technique consisting of simultaneous radial closing-wedge and ulnar shortening osteotomy to treat malunion of distal radial fractures.
Malunion is a common complication of distal radial fractures that can lead to functional disability1,2. Corrective osteotomy of the distal part of the radius can be used to treat extra-articular malunion. Because of the complexity of the deformity, the various types of malunion, and the inherent technical challenges of surgical correction, numerous techniques have been described3-13, including opening-wedge osteotomy3. Fernandez3 used iliac crest bone graft to allow simultaneous correction of angular and shortening deformities of the distal part of the radius without an ulnar osteotomy.
We previously described a simultaneous radial closing-wedge and ulnar shortening osteotomy (radial and ulnar technique)11,14 and recently evaluated the outcomes in a series of patients with distal radial malunion to determine whether conventional radial opening-wedge osteotomy or our radial and ulnar osteotomy technique provided better clinical and radiographic results15. The study indicated that the radial and ulnar osteotomy technique is significantly better than the opening-wedge technique with regard to the restoration of ulnar variance, the wrist extension-flexion arc of motion, and the Mayo wrist score.
The radial and ulnar osteotomy technique is done in seven stages:
Step 1: Preoperative planning
Step 2: Radial closing-wedge osteotomy
Step 3: Distal ulnar shortening osteotomy
Step 4: Plate fixation of the radial osteotomy site
Step 5: Proximal ulnar shortening osteotomy
Step 6: Plate fixation of the ulnar osteotomy site
Step 7: Postoperative management
Step 1: Preoperative Planning
Plan the radial closing-wedge osteotomy to correct the volar tilt angle to 8.5° to 15.5° and the ulnar shortening osteotomy to restore ulnar variance to −2.5 to 0.5 mm.
The aim of the radial closing-wedge osteotomy is to correct the volar tilt angle in the sagittal plane to within a normal range of 8.5° to 15.5°16. Plan the amount of bone wedge to be removed using radiographs of the injured wrist. The angle of the bone wedge to be removed corresponds to the dorsal tilt plus the normal volar tilt of the radius (30° + 8° = 38° in the patient shown in Fig. 1). Determine the amount of volar cortex to be removed using tracings of the radiograph (8 mm in the patient in Fig. 1 [lateral radiograph]). To improve radial inclination, the distance between the two osteotomy lines is 1 mm shorter on the radial side than on the ulnar side (Fig. 1 [posteroanterior radiograph]).
The aim of the ulnar shortening osteotomy is to restore ulnar variance to within a normal range of −2.5 to 0.5 mm16, irrespective of the radiographs of the uninjured wrist. The amount of bone to be removed with the distal osteotomy corresponds to the positive ulnar variance measured on the preoperative radiographs (7 mm in the patient shown in Fig. 1 [posteroanterior radiograph]) and that to be removed with the proximal osteotomy is determined from intraoperative radiographs after reduction and internal fixation of the distal part of the radius.
Fig. 1.
The bone wedge to be removed from the radius and the bone to be removed from the ulna are simulated on preoperative posteroanterior and lateral radiographs of the injured wrist. UV = ulnar variance, DT = dorsal tilt, A = distal osteotomy line, and B = proximal osteotomy line.
Step 2: Radial Closing-Wedge Osteotomy
Remove the wedge of bone from the radius and reduce the distal fragment, keeping the dorsal cortex as a hinge.
Place the patient in a supine position with the hand on an arm-table, apply a tourniquet to the upper arm, and inflate it to 250 mm Hg. Use regional or general anesthesia.
Make an 8-cm longitudinal skin incision over the radial edge of the flexor carpi radialis muscle.
Expose the pronator quadratus muscle through the interval between the flexor carpi radialis and the radial artery. Incise the pronator quadratus longitudinally along the radial border of the distal part of the radius at its insertion, leaving a small cuff of tissue that can be repaired during closure.
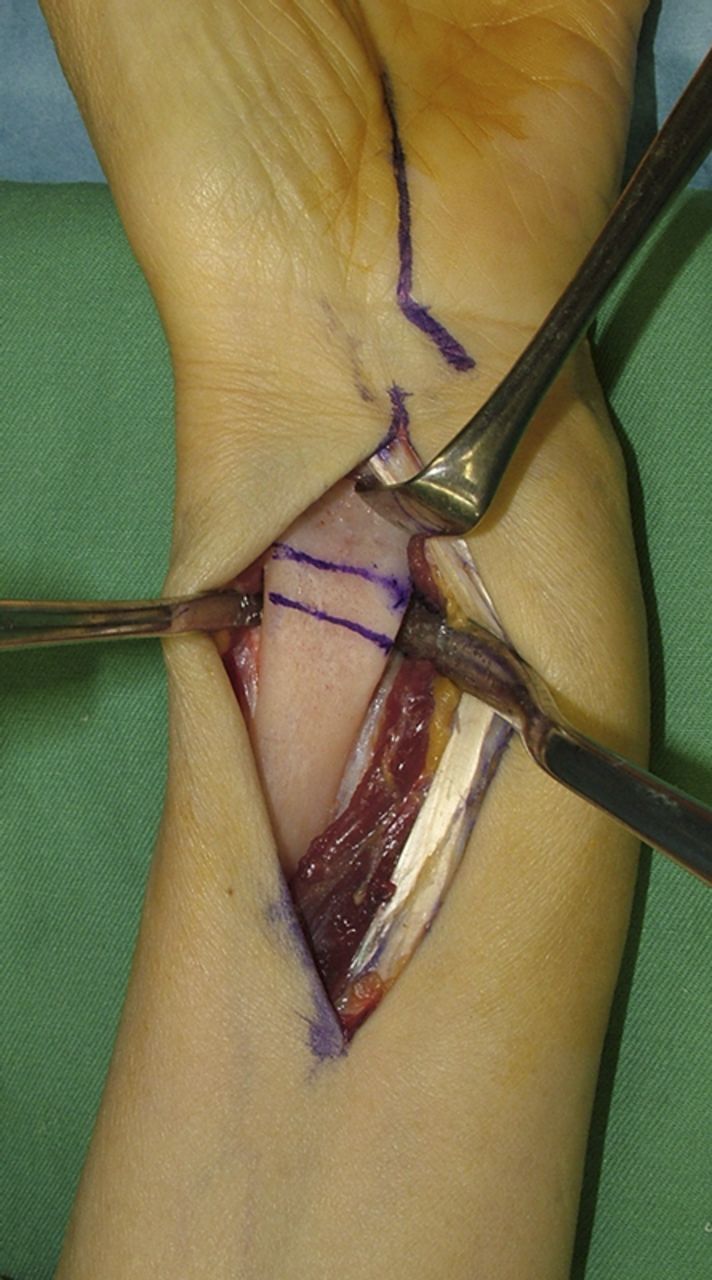
Mark two osteotomy lines, leaving enough room to place a volar locking plate on the distal fragment (Fig. 2-A). Determine the distance between the two lines using tracings of the radiographs (8 mm in the patient shown in Fig. 1). Direct the distal osteotomy approximately parallel to the joint surface with an oscillating saw, taking care to avoid a complete osteotomy of the dorsal cortex (Fig. 2-B). Then complete the proximal osteotomy and remove the wedge of bone (Fig. 2-C).
Reduce the distal fragment, keeping the dorsal cortex as a hinge. Complete reduction of the distal fragment is usually unsuccessful until the ulnar osteotomy is completed.
Fig. 2-A.
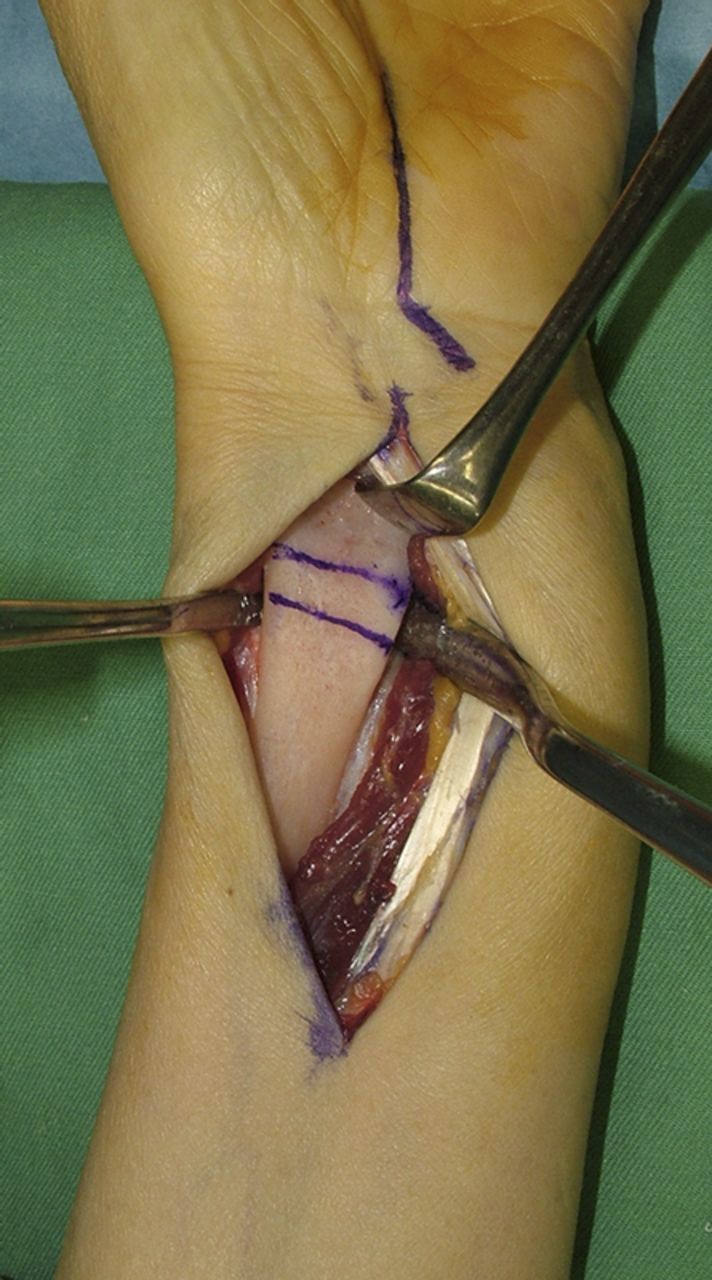
Two osteotomy lines are marked on the distal volar aspect of the radius.
Fig. 2-B.
The distal osteotomy is performed with an oscillating saw.
Fig. 2-C.
The planned wedge of bone is removed while maintaining the continuity of the dorsal cortex. Note the mark on the palm for carpal tunnel release. A concomitant carpal tunnel release was performed as this patient had preoperative signs or symptoms of carpal tunnel syndrome.
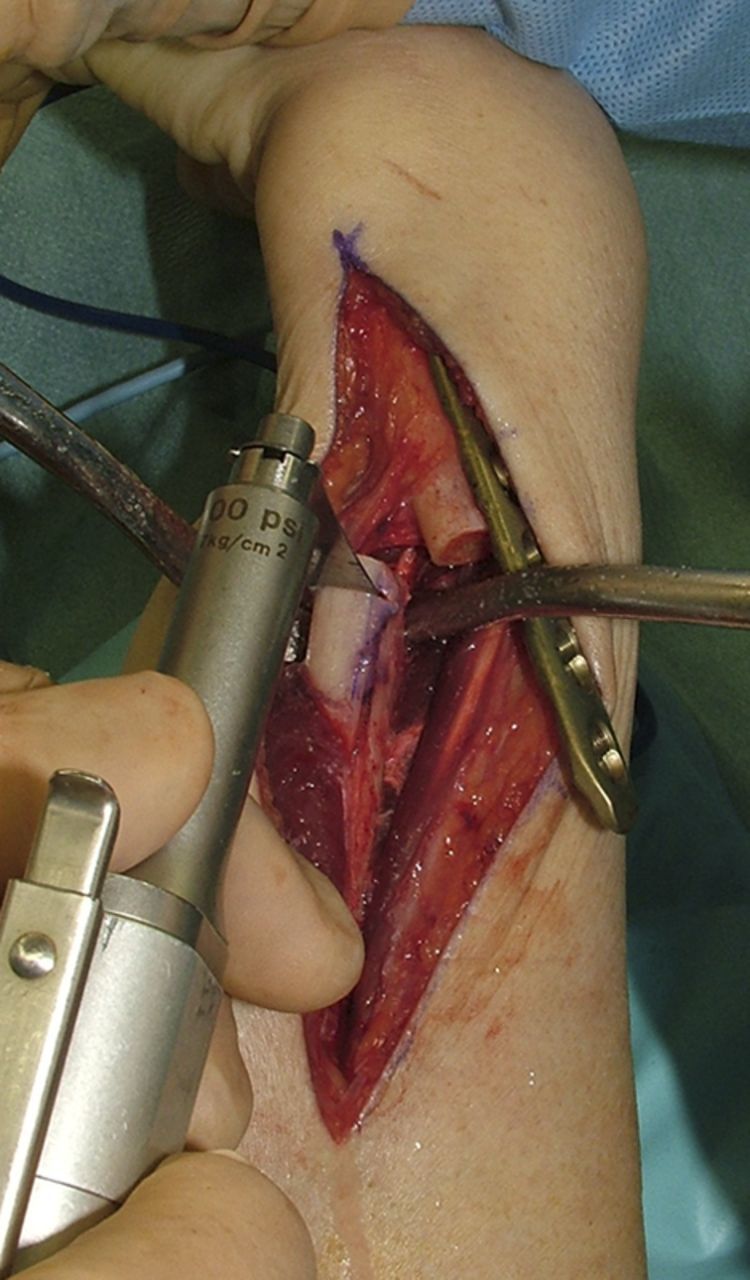
Step 3: Distal Ulnar Shortening Osteotomy
Resect the section of the ulna equivalent to the positive ulnar variance with transverse osteotomies.
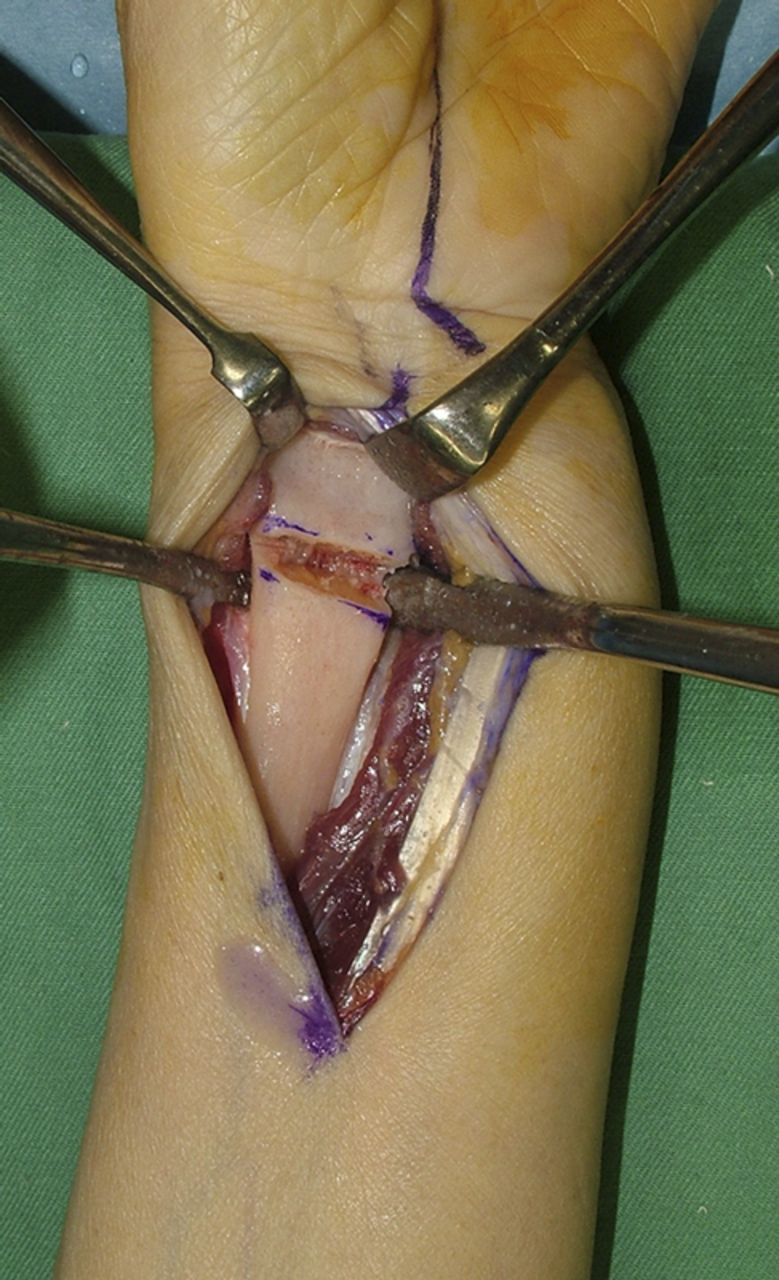
Make a 10-cm longitudinal skin incision along the distal third of the ulna. Open the interval between the extensor carpi ulnaris and flexor carpi ulnaris and expose the ulna subperiosteally dorsally.
Fit a 3.5-mm six-hole LCP to the distal part of the ulna with three distal screws. Ensure that the plate is parallel to the bone along its whole length.
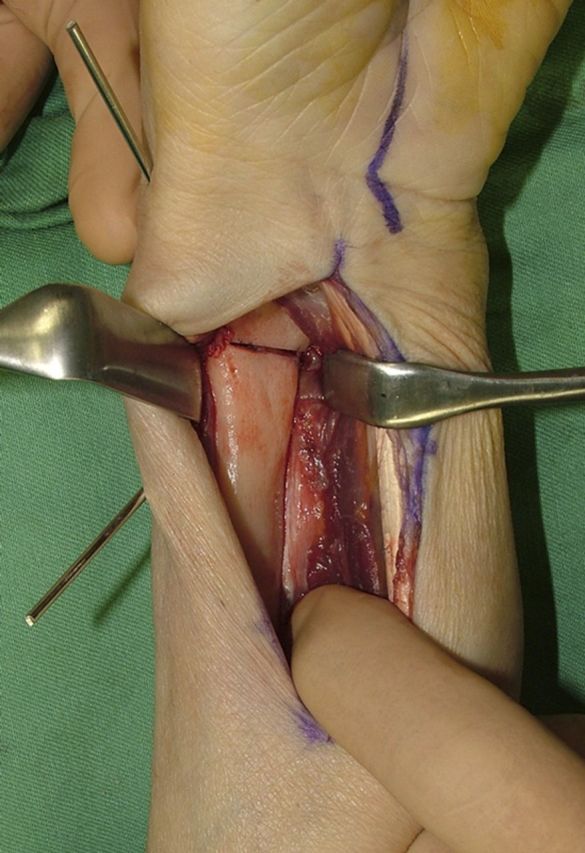
Mark the site of the osteotomy at the middle of the plate and make an aligning mark proximal to the plate (Fig. 3-A).
Remove the plate and resect the estimated section of ulna, which is equivalent to the ulnar variance, with transverse osteotomies (Fig. 3-B).
Figs. 3-A.

A 3.5-mm six-hole LCP is fit to the distal part of the ulna with three distal screws. Note the mark for the osteotomy site at the middle of the plate and the alignment mark along the edge of the plate.
Fig. 3-B.
Two parallel cuts are made with the plate temporarily removed.
Step 4: Plate Fixation of the Radial Osteotomy Site
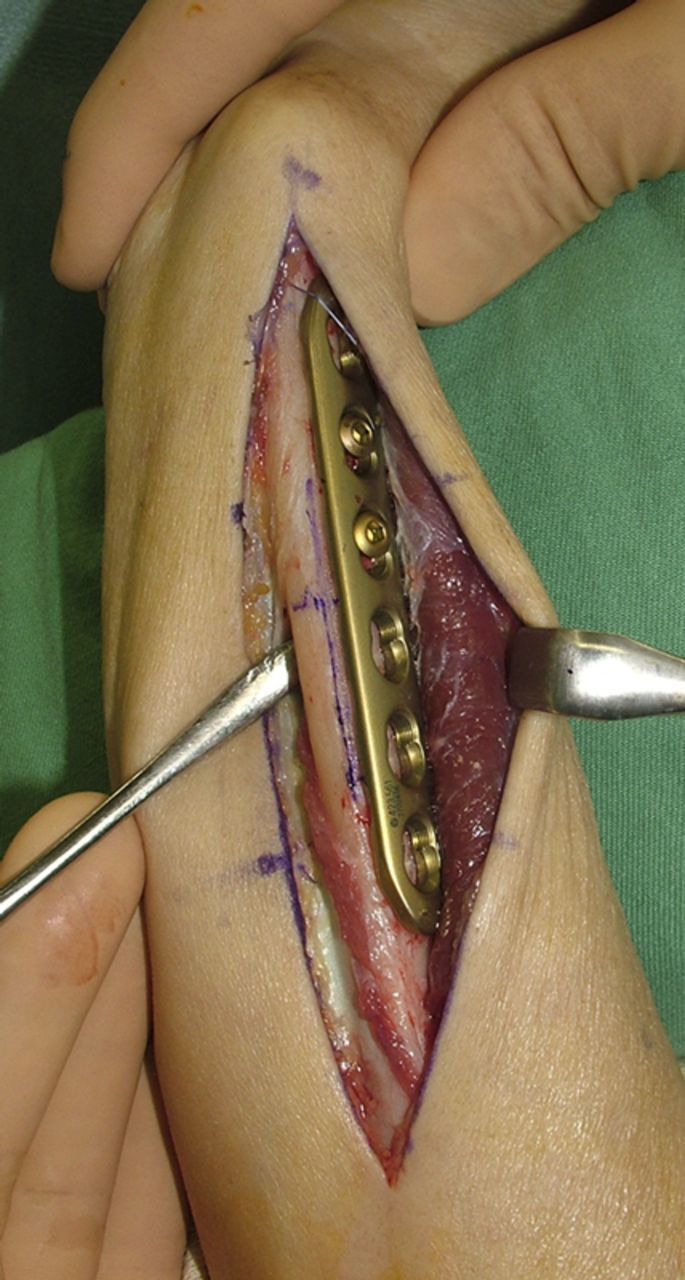
Hold together the two fragments of the radius with a Kirschner wire and fix the osteotomy site with a volar locking plate.
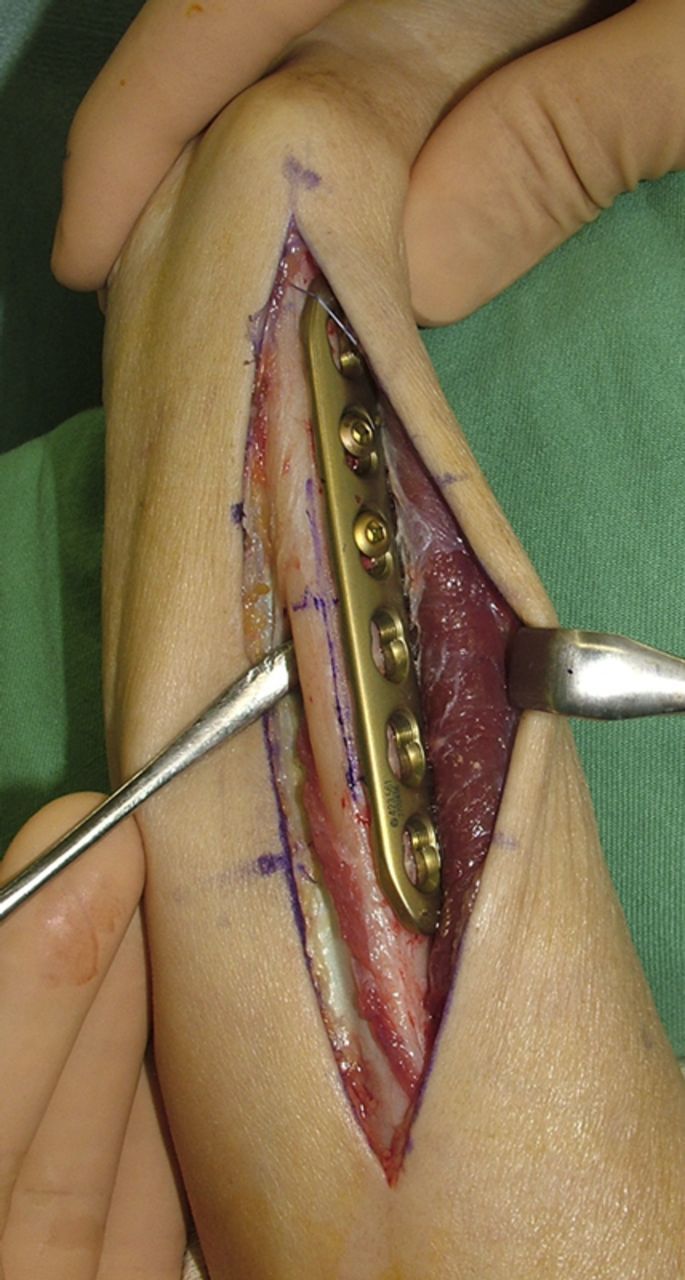
Reapproximate and hold together the two fragments of the radius with a 1.8-mm Kirschner wire (Fig. 4).
Confirm the position of the radius with regard to volar tilt and radial inclination on fluoroscopic views. The acceptable range of volar tilt is 1° to 21° and that of radial inclination is 13° to 30°17.
Secure permanent fixation with a volar locking plate (Video 1).
Fig. 4.

Two fragments of the radius are brought together and held with Kirschner wires, following which the osteotomy site is fixed with a volar locking plate.
Video 1.
A video demonstrating the procedure.
Step 5: Proximal Ulnar Shortening Osteotomy
Evaluate residual ulnar positive variance with fluoroscopy and restore the ulnar variance to within a normal range by removing additional bone from the proximal fragment.
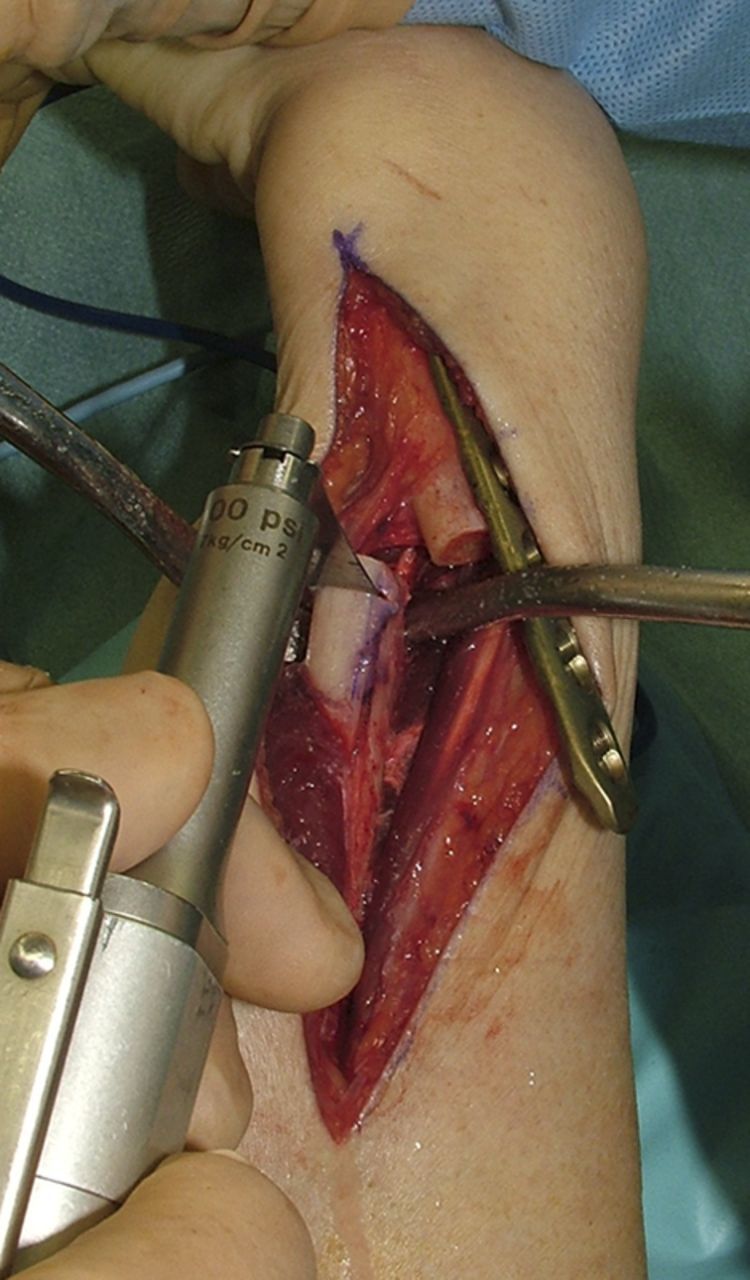
Reapply the 3.5-mm six-hole LCP to the distal ulnar fragment with three screws. Realign the hand and wrist rotationally, using the previously made longitudinal aligning mark. Use a reduction forceps to hold the plate temporarily against the proximal fragment. If it is difficult to close the osteotomy, fix an AO compression device (Synthes, Paoli, Pennsylvania) to the proximal fragment with a unicortical screw, having engaged the mobile arm in the most proximal plate-hole (Fig. 5-A). Tighten the compression device to close the osteotomy site.
Evaluate residual ulnar positive variance, which is usually 3 to 4 mm, with fluoroscopy. For the proximal ulnar osteotomy, loosen the AO compression device and release the plate from the proximal fragment. It is not necessary to unscrew the plate from the distal fragment. Shorten the ulna further as needed by removing additional bone from the proximal fragment (Fig. 5-B).
Fig. 5-A.
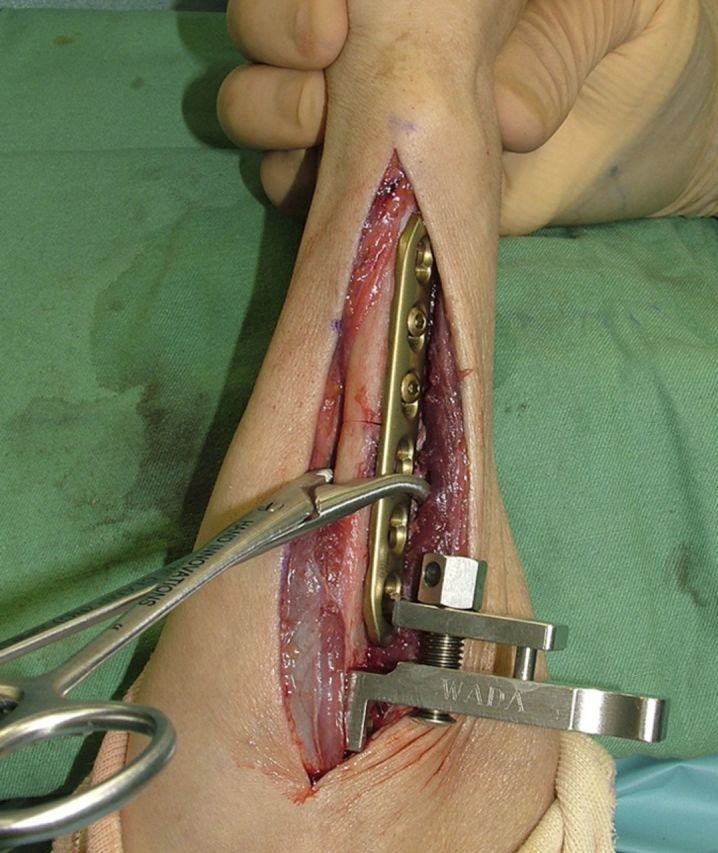
The ulnar osteotomy site is closed by tightening the AO compression device, and the ulnar variance is evaluated on intraoperative radiographs.
Fig. 5-B.
A wafer of bone that corresponds to the residual ulnar variance is removed, and the plate and proximal screws are placed.
Step 6: Plate Fixation of the Ulnar Osteotomy Site
Use a compression device to close and fix the ulnar osteotomy site.
Again, clamp the plate to the proximal fragment and fix the AO compression device. Reapply compression until the two fragments of the ulna abut (Fig. 6), and confirm this with fluoroscopic views.
Insert the proximal screws and remove the compression device. If more compression is desired, use the off-center drill guide.
Repair the pronator quadratus muscle and close the wound in layers.
Fig. 6.

Postoperative posterolateral and lateral radiographs.
Step 7: Postoperative Management
Allow early motion immediately after the operation.
Apply a volar short-arm plaster splint until the soft tissues heal. Finger motion is encouraged immediately after the operation.
Schedule the first postoperative clinic visit at ten to fourteen days for wound inspection and suture removal, at which time the hand therapist can supply the patient with a removable static volar wrist splint and start the rehabilitation program.
Obtain radiographs every month postoperatively until union is achieved. After complete union of both radial and ulnar osteotomy sites has occurred, allow the patient to resume full normal activities. We do not recommend plate removal unless the patient has irritation from the implants.
Results
We retrospectively evaluated forty-two patients at a minimum of one year after treatment of an extra-articular distal radial malunion with a radial corrective osteotomy15. Twenty-two patients were treated with radial opening-wedge osteotomy and interpositional bone graft or bone-graft substitute (opening-wedge cohort), and twenty were treated with the radial and ulnar osteotomy technique (closing-wedge cohort). The surgical procedure was selected by the surgeon. The mean follow-up period for the opening and closing-wedge cohorts was thirty-six months (range, twelve to 101 months) and twenty-eight months (range, twelve to eighty-seven months), respectively. Complications were comparable between the two techniques. Postoperative volar tilt and ulnar variance improved significantly compared with their preoperative status in each cohort. Restoration of ulnar variance to within defined criteria (−2.5 to 0.5 mm) was significantly more frequent in the closing-wedge cohort than it was in the opening-wedge cohort (p < 0.001). The mean postoperative wrist extension-flexion arc was 108° (range, 65° to 159°) in the opening-wedge cohort and 154° (range, 115° to 180°) in the closing-wedge cohort, and the mean postoperative Mayo wrist score was 86 points (range, 70 to 95 points) in the closing-wedge cohort and 78 points (range, 55 to 100 points) in the opening-wedge cohort. The postoperative mean extension-flexion arc of the wrist (p < 0.001) and Mayo wrist score (p = 0.008) were significantly better in the closing-wedge cohort. Differences between the two cohorts in pronation-supination arc, grip strength, pain rating score, and Disabilities of the Arm, Shoulder and Hand (DASH) scores were not significant.
What to Watch For
Indications
Extra-articular distal radial malunion.
Reduced wrist motion or pain with the activities of daily living.
No absolute criteria for the degree of deformity were used.
Contraindications
Advanced degenerative changes or substantial incongruity of the distal radioulnar or radiocarpal joint.
Pitfalls & Challenges
Reduction of the distal part of the radius after radial closing-wedge osteotomy is rarely accomplished unless the ulnar osteotomy is performed.
True-positive ulnar variance is difficult to evaluate until dorsal angulation of the radius is restored.
Ulnar variance should be restored to within a normal range of −2.5 to 0.5 mm16, irrespective of the radiographs of the uninjured wrist. The uninjured wrist may not provide a better reference than normal values obtained from a database16,18.
Clinical Comments
-
What technique have you found to be effective in achieving normal ulnar variance with ulnar shortening osteotomy?
True-positive ulnar variance is difficult to evaluate on preoperative radiographs as dorsal angulation gives a false impression of shortening of the radius. Ulnar shortening osteotomy should be performed in two stages. In the distal osteotomy, a wafer of bone that corresponds to the ulnar variance should be removed. Following correction and internal fixation of the distal radial fragment, the residual ulnar variance should be evaluated on intraoperative radiographs. If normal ulnar variance has not yet been achieved, the ulna should be further shortened by removing additional bone from the proximal fragment.
The first cut of the ulnar osteotomy (Step 3) can be made before the radial osteotomy. This allows the bone to overlap, which may help to determine how much of the ulna needs to be resected. In our experience, however, the amount of overlap is smaller than the amount of ulna requiring resection to establish the normal ulnar variance.
-
What prophylactic measures have you found to be effective in minimizing the risk of delayed union after ulnar shortening osteotomy?
The plate should be attached to the distal fragment with screws prior to the osteotomy, as the distal fragment is very mobile after the osteotomy and it is difficult to screw the plate to it.
Any kind of compression device can be used to close the osteotomy site.
The total amount of the ulna to be resected may reach >10 mm. It is sometimes difficult to close the osteotomy site even if a compression device is used. In such cases, the interosseous membrane attached to the distal fragment of the ulna should be released. Undue tension may result in a fracture of the distal fragment or loosening of the plate.
Based on an original article: J Bone Joint Surg Am. 2011 Sep 7;93(17):1619-26.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Cooney WP 3rd Dobyns JH Linscheid RL. Complications of Colles’ fractures. J Bone Joint Surg Am. 1980;62(4):613-9. [PubMed] [Google Scholar]
- 2. Hirahara H Neale PG Lin YT Cooney WP An KN. Kinematic and torque-related effects of dorsally angulated distal radius fractures and the distal radial ulnar joint. J Hand Surg Am. 2003 Jul;28(4):614-21. [DOI] [PubMed] [Google Scholar]
- 3. Fernandez DL. Correction of post-traumatic wrist deformity in adults by osteotomy, bone-grafting, and internal fixation. J Bone Joint Surg Am. 1982 Oct;64(8):1164-78. [PubMed] [Google Scholar]
- 4. Fernandez DL. Radial osteotomy and Bowers arthroplasty for malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1988 Dec;70(10):1538-51. [PubMed] [Google Scholar]
- 5. Watson HK Castle TH Jr. Trapezoidal osteotomy of the distal radius for unacceptable articular angulation after Colles’ fracture. J Hand Surg Am. 1988 Nov;13(6):837-43. [DOI] [PubMed] [Google Scholar]
- 6. Posner MA Ambrose L. Malunited Colles’ fractures: correction with a biplanar closing wedge osteotomy. J Hand Surg Am. 1991 Nov;16(6):1017-26. [DOI] [PubMed] [Google Scholar]
- 7. Jupiter JB Ruder J Roth DA. Computer-generated bone models in the planning of osteotomy of multidirectional distal radius malunions. J Hand Surg Am. 1992 May;17(3):406-15. [DOI] [PubMed] [Google Scholar]
- 8. Jupiter JB Ring D. A comparison of early and late reconstruction of malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1996 May;78(5):739-48. [DOI] [PubMed] [Google Scholar]
- 9. Shea K Fernandez DL Jupiter JB Martin C Jr. Corrective osteotomy for malunited, volarly displaced fractures of the distal end of the radius. J Bone Joint Surg Am. 1997 Dec;79(12):1816-26. [DOI] [PubMed] [Google Scholar]
- 10. Ring D Roberge C Morgan T Jupiter JB. Osteotomy for malunited fractures of the distal radius: a comparison of structural and nonstructural autogenous bone grafts. J Hand Surg Am. 2002 Mar;27(2):216-22. [DOI] [PubMed] [Google Scholar]
- 11. Wada T Isogai S Kanaya K Tsukahara T Yamashita T. Simultaneous radial closing wedge and ulnar shortening osteotomies for distal radius malunion. J Hand Surg Am. 2004 Mar;29(2):264-72. [DOI] [PubMed] [Google Scholar]
- 12. Lubahn JD Hood JM Nechleba J Williams DP Green T. Gradual reduction of distal radial malunion using distraction osteogenesis. J Hand Surg Am. 2007 Jul-Aug;32(6):795-800. [DOI] [PubMed] [Google Scholar]
- 13. Sato K Nakamura T Iwamoto T Toyama Y Ikegami H Takayama S. Corrective osteotomy for volarly malunited distal radius fracture. J Hand Surg Am. 2009 Jan;34(1):27-33, 33.e1. [DOI] [PubMed] [Google Scholar]
- 14. Wada T Tsuji H Iba K Aoki M Yamashita T. Simultaneous radial closing wedge and ulnar shortening osteotomy for distal radius malunion. Tech Hand Up Extrem Surg. 2005 Dec;9(4):188-94. [DOI] [PubMed] [Google Scholar]
- 15. Wada T Tatebe M Ozasa Y Sato O Sonoda T Hirata H Yamashita T. Clinical outcomes of corrective osteotomy for distal radial malunion: a review of opening and closing-wedge techniques. J Bone Joint Surg Am. 2011 Sep 7;93(17):1619-26. [DOI] [PubMed] [Google Scholar]
- 16. Prommersberger KJ Van Schoonhoven J Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg Br. 2002 Feb;27(1):55-60. [DOI] [PubMed] [Google Scholar]
- 17. Gartland JJ Jr Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951 Oct;33-A(4):895-907. [PubMed] [Google Scholar]
- 18. Schuind F Alemzadeh S Stallenberg B Burny F. Does the normal contralateral wrist provide the best reference for X-ray film measurements of the pathologic wrist? J Hand Surg Am. 1996 Jan;21(1):24-30. [DOI] [PubMed] [Google Scholar]






