Abstract
Background
The effect of the preoperative exposure to controlled substances such as benzodiazepines and sedative/hypnotics on prolonged opioid consumption after hand surgery is not known.
Questions/purposes
(1) Is preoperative exposure to benzodiazepines and sedative/hypnotics associated with greater numbers of filled postoperative opioid prescriptions after hand surgery? (2) Is a positive history of the use of more than one controlled substance, a mood disorder, or smoking associated with greater numbers of filled opioid prescriptions after surgery? (3) Is preoperative exposure to opioids associated with greater numbers of filled postoperative opioid prescriptions after hand surgery?
Methods
Patients undergoing upper extremity surgery at one academic outpatient surgical center were prospectively enrolled. The Pennsylvania Drug Monitoring Program (PDMP) website was used to document prescriptions of opioids, benzodiazepines, and sedative/hypnotics filled 6 months before and after the procedure. Patients were grouped into exposed or naïve cohorts depending on whether a prescription was filled 6 months before surgery. Smoking history (current or previous smoking was considered positive) and a history of mood and pain disorders (as noted in the medical history), were collected from the outpatient and the operating room electronic medical record.
Results
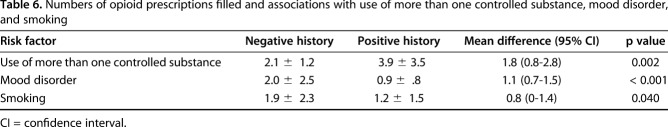
After controlling for age, gender, and other confounding variables, we found that a history of exposure to benzodiazepines is associated with a greater number of filled postoperative opioid prescriptions (not-exposed, 1.2 ± 1.3; exposed, 2.2 ± 2.5; mean difference, 1.0; 95% confidence interval [CI], 0.5–1.5; p < 0.001); likewise, exposure to sedative/hypnotics is associated with greater opioid prescription fills (not-exposed, 1.2 ± 1.4; exposed, 2.3 ± 2.9; mean difference, 1.1; 95% CI, 0.3–1.9; p = 0.006). Patients who had used more than one controlled substance had more filled opioid prescriptions when compared with those not using more than one controlled substance (3.9 ± 3.5 versus 2.1 ± 1.2; mean difference, 1.8; 95% CI, 0.8–2.8; p = 0.002); patients with mood disorders also had more filled prescriptions when compared with those without mood disorders (2.0 ± 2.5 versus 0.9 ± .8; mean difference, 1.1; 95% CI, 0.7–1.5; p < 0.001); and finally, smoking history is associated with more filled prescriptions (1.9 ± 2.3 versus 1.2 ± 1.5, mean difference, 0.8; 95% CI, 0–1.4; p = 0.040).
Conclusions
Patients exposed to benzodiazepines and sedative/hypnotics have prolonged use of opioids after surgery. Undergoing outpatient upper extremity surgery and being prescribed an opioid did not change the patterns of controlled substance use. Based on the results of this study, we are now more aware of the potential problems of patients with exposure to controlled substances, and are more attentive about reviewing their history of substance use in the PDMP website, an important resource. In addition, we now provide much more detailed preoperative counseling regarding the use and abuse of opioid medication in patients with exposure to benzodiazepines, sedatives, and those with a smoking history and mood disorders.
Level of Evidence Level II, therapeutic study.
Introduction
Several studies have found that the use of opioid analgesics in the acute setting increases the likelihood of persistent use [1, 7, 20]. Patients undergoing orthopaedic surgery have been considered to be at higher risk of developing opioid dependence in the postoperative period [10]. With regard to patients undergoing hand surgery, younger age, mental health disorders, and tobacco dependence or abuse have been some of the variables associated with prolonged opioid use. [11]
Recent studies, relying primarily on commercial, employer-based insurance company or military health provider databases, have reported conflicting data regarding the use of opioids after orthopaedic surgery in opioid-naïve patients [11, 19]. While some studies have detailed a limited degree of opioid use in those patients not exposed to these medications postoperatively, others have described prolonged opioid use regardless of exposure in the preoperative period. The reason we undertook this study, in addition to the resolving these conflicting data, was to address limitations in the current evidence. Specifically, these are database studies that exclude Medicare beneficiaries without supplemental insurance, which represent a large proportion of patients under study. In addition, these studies do not address the effect of concomitant use of controlled substances such as benzodiazepines and sedative/hypnotics on opioid use.
Therefore, we asked: (1) Is preoperative exposure to benzodiazepines and sedative/hypnotics associated with greater numbers of filled postoperative opioid prescriptions after hand surgery? (2) Is a positive history of the use of more than one controlled substance, a mood disorder, or smoking associated with greater numbers of filled opioid prescriptions after surgery? (3) Is preoperative exposure to opioids associated with greater numbers of filled postoperative opioid prescriptions after hand surgery?
Patients and Methods
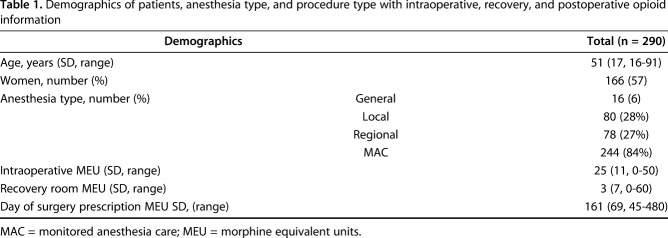
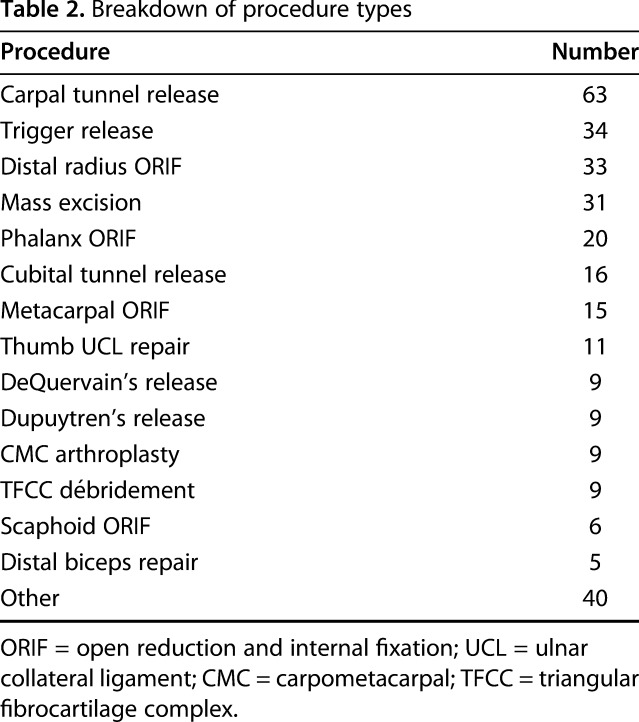
Institutional review board approval was obtained before study initiation. We prospectively enrolled patients who underwent elbow, wrist, and surgery performed by two hand surgeons (MR, PB) at one academic outpatient surgical center. The collection period was from January 4, 2017 to April 28, 2017. We initially identified 319 patients for the study. We excluded patients if they were younger than 18 years of age (n = 5) or if they underwent more than one surgical procedure (n = 24) during the study period. This study cohort was comprised of 290 patients (Fig. 1). We obtained patient demographics, including age, gender, diagnosis, and type of surgical procedure, from the electronic medical record (EMR) of the outpatient clinics (Table 1).The type of procedures were divided into bony and soft tissue (Table 2).
Fig. 1.
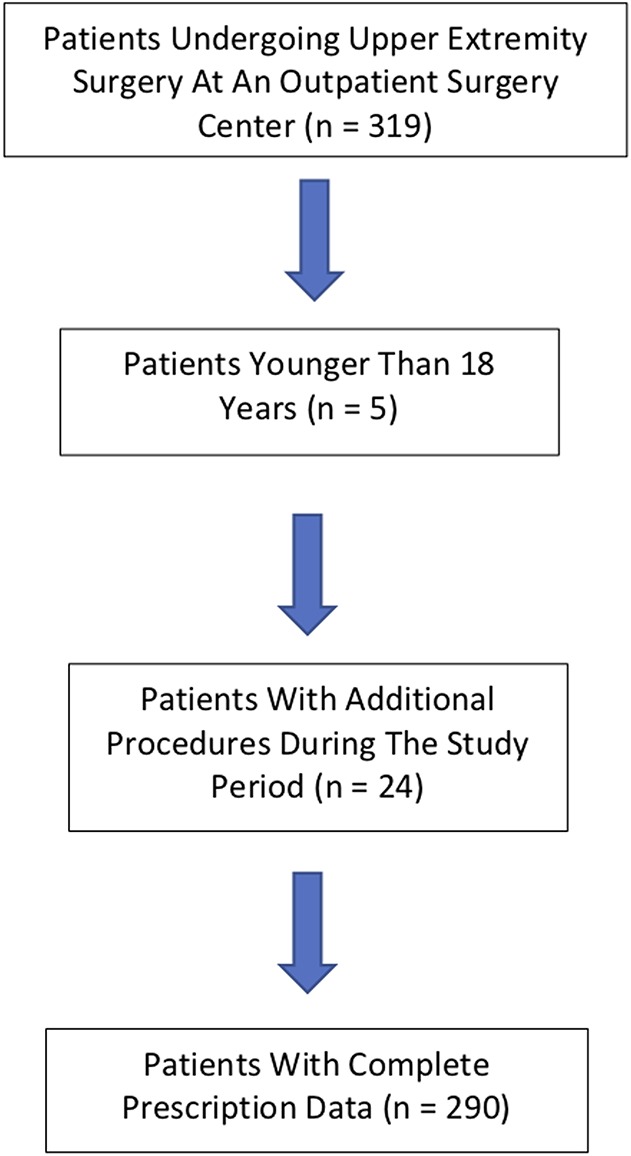
STROBE flow study diagram detailing inclusion and exclusion criteria for study patients.
Table 1.
Demographics of patients, anesthesia type, and procedure type with intraoperative, recovery, and postoperative opioid information
Table 2.
Breakdown of procedure types
Social history, such as a history of smoking (current or previous smoking was considered positive), and history of mood and pain disorders (as noted in the medical history), were collected from the outpatient and the operating room EMR. Intraoperative information regarding anesthesia type, opioids provided intraoperatively, in the recovery room, and in the discharge opioid prescription in the form of morphine equivalent units (MEUs) were tabulated from the operating room EMR [11].
Whether an opioid prescription was provided during the day of surgery, and the type and amount of medication prescribed was left to the discretion of the treating physician. The average MEUs prescribed by the physicians was 155.6 per prescription when one was provided on discharge from the surgical center (range, 137–178 MEUs). A 155.6 MEU is equivalent to 35 pills of Tylenol #3 or 21 pills of oxycodone 5 mg.
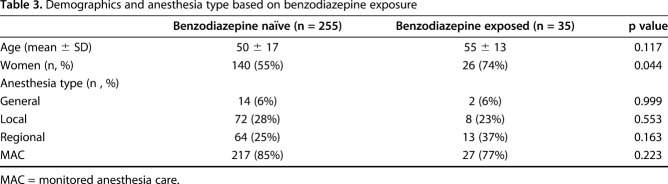
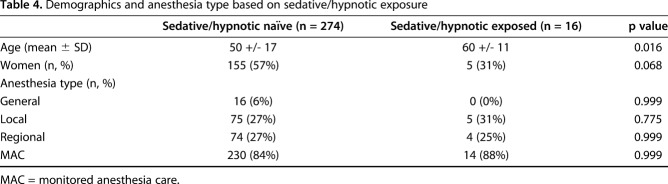
The Pennsylvania Drug Monitoring Program (PDMP) website [15] was used to document all prescriptions of controlled substances filled 6 months before and after the surgical procedure. The PA PDMP website search engine included links to the database for Connecticut, Delaware, District of Columbia, Illinois, Maine, Maryland, Massachusetts, Minnesota, New Jersey, New York, Ohio, Oklahoma, South Carolina, Texas, Virginia, and West Virginia [15]. Patient first name, last name, and date of birth were entered into the website search engine. All prescriptions listed on the website were recorded; this included opioid pain medications, such as oxycodone, codeine, hydrocodone, etc; benzodiazepines, like diazepam, lorazepam, alprazolam, etc; and sedative/hypnotics, for instance, zolpidem, trazodone, etc. The website included the date the prescription was written, the date the prescription was filled, patient name, patient date of birth, medication name, medication dosage, amount prescribed, pharmacy/dispenser location, and prescriber name. The website prescription information was cross-referenced with the prescription documented in the operating room EMR. Per the methodology of Johnson et al. [11 ], a perioperative opioid prescription was defined as one filled within 1 month before the surgical procedure to account for prescriptions given before surgery for postoperative pain management. Based on the website information, patients were grouped into exposed or not-exposed cohorts dependent upon their exposure in the 6 months before the surgery. This resulted in six groups: opioid naïve, opioid exposed, benzodiazepine naïve, benzodiazepine exposed, sedative/hypnotic naïve or sedative/hypnotic exposed. We examined the demographics of patients with and without exposure to benzodiazepines (Table 3) as well as the demographics of patients with and without exposure to sedative/hypnotics (Table 4). In addition, patients with exposure to more than one controlled substance were grouped and compared with those with exposure to only one controlled substance. Prolonged opioid use was defined as the proportion of patients who filled a prescription 90 to 180 days after the surgical event. This definition was used by previous surgical studies evaluating opioid consumption after hand surgery [3, 11].
Table 3.
Demographics and anesthesia type based on benzodiazepine exposure
Table 4.
Demographics and anesthesia type based on sedative/hypnotic exposure
To answer our primary research question regarding whether exposure to benzodiazepines and sedative/hypnotics is associated with greater numbers of filled postoperative opioid prescriptions after surgery, we evaluated the number of controlled substance prescriptions filled by patients with preoperative exposure (defined as one prescription filled 6 months before surgery) to these medications. One secondary question was: Is a positive history of the use of more than one controlled substance, a mood disorder, or smoking associated with greater numbers of filled opioid prescriptions after surgery? We answered this by evaluating the number of controlled substance prescriptions filled by patients with a history of multiple controlled substance use, mood disorders (as documented in the patient’s medical history), and a smoking history (as defined as a history of previous or current tobacco use in the patient’s medical record). Another secondary questions was: Is preoperative exposure to opioids, defined as one prescription filled 6 months before surgery, associated with greater numbers of filled postoperative opioid prescriptions after hand surgery? We answered this by evaluating the number of opioid prescriptions filled by patients with preoperative exposure to these medications.
For the statistical analysis of our data, we chose three different analytic approaches. First, to compare the number of postoperative prescriptions filled between the naïve and exposed groups, we created a model that would control for confounding variables such as age, gender, and procedure type among others. For this purpose, we used a generalized linear model specifying a Poisson distribution and a log-link function given that our data had a non-normal distribution. The models were run with and without covariates, including intraoperative and postoperative prescription MEUs as well as age, gender and procedure type (bony versus soft tissue). These covariates were selected based on preliminary analyses (bivariate Poisson models) that helped to identify variables that were related to one or more of the outcomes (p < 0.2). Second, for the evaluation of any change in “use status” from the pre- to the postoperative period, we used the McNemar test in which nonsignificant results indicated consistency or the absence of change over time. Third, group differences on the status use of controlled substance used after surgery were tested using the Pearson chi-square tests. Power was computed on a post-hoc basis for the obtained results for the primary outcome (total number of postoperative opioid prescriptions filled) for all three (Poisson model, McNemar’s, and Pearson chi-square) analyses. We had 95% power at an alpha of < 0.05 to detect a difference of one prescription between the exposed and unexposed groups for all three (opioid, benzodiazepine, and sedative/hypnotic) substances evaluated.
Results
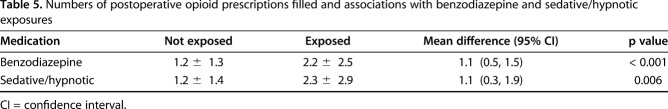
Preoperative exposure to benzodiazepines and sedative/hypnotics was associated with greater numbers of filled postoperative opioid prescriptions after hand surgery. A history of exposure to benzodiazepines is associated with greater number of filled postoperative opioid prescriptions (not-exposed, 1.2 ± 1.3; exposed, 2.2 ± 2.5; mean difference, 1.0; 95% CI, 0.5–1.5; p < 0.001); likewise, exposure to sedative/hypnotics is associated with greater opioid prescription fills (not-exposed, 1.2 ± 1.4; exposed, 2.3 ± 2.9; mean difference, 1.1; 95% CI, 0.3–1.9; p = 0.006) (Table 5) Opioid-exposed patients were more likely to fill benzodiazepine prescriptions when compared with opioid-naïve patients (10 of 55 versus 21 of 235; risk ratio [RR], 2.0, 95% CI, 1.0–4.1; p = 0.045); they were also more likely to fill sedative/hypnotic prescriptions (7 of 55 versus 7 of 235; RR, 4.3, 95% CI, 1.6–11.7; p = 0.001).
Table 5.
Numbers of postoperative opioid prescriptions filled and associations with benzodiazepine and sedative/hypnotic exposures
Patients who used more than one controlled substance had more filled opioid prescriptions compared with those not using more than one controlled substance (3.9 ± 3.5 versus 2.1 ± 1.2; mean difference, 1.8; 95% CI, 0.8–2.8; p = 0.002); patients with mood disorders also had more filled prescriptions when compared with those without mood disorders (2.0 ± 2.5 versus 0.9 ± .8; mean difference, 1.1; 95% CI, 0.7–1.5; p < 0.001); and finally, smoking history was associated with more filled prescriptions (1.9 ± 2.3 versus 1.2 ± 1.5; mean difference, 0.8; 95% CI, 0–1.4; p = 0.040) (Table 6).
Table 6.
Numbers of opioid prescriptions filled and associations with use of more than one controlled substance, mood disorder, and smoking
Patients in the opioid exposed group were more likely to have postoperative exposure to opioids than opioid naïve patients, (50 of 55 versus 171 of 235, RR, 1.2, 95% CI, 1.1–1.4; p < 0.001). Not surprisingly, compared with opioid naïve patients, opioid-exposed patients filled more prescriptions (3.3 ± 2.6 versus 0.8 ± 0.6; p < 0.001).
The surgical procedure was not associated with a change in “use status” of opioids, benzodiazepines, or sedative/hypnotics in the postoperative compared with the preoperative period. Two hundred twenty-two of 290 patients (76%) filled the first postoperative opioid prescription regardless of their initial use status. After the first postoperative prescription, opioid-naïve patients remained unexposed to opioids in the followup period (McNemar p = 0.750). Similarly, patients’ controlled use patterns generally remain the same after surgery as they were before surgery. In other words, having an opioid prescribed after a carpal tunnel release or a fracture of the distal radius will generally not lead to a patient becoming habituated to benzodiazepines or sedative hypnotics (McNemar p = 0.500 and 0.600 respectively).
Discussion
Opioid abuse is a public health problem, though other controlled substances such as benzodiazepines and sedative/hypnotics should not be overlooked and can substantially contribute to the problem [2, 4, 5, 9, 12]. There is a limited amount of data available regarding the use of opioid medication in the setting of hand surgery [21], and most of that data is derived from large insurance database studies [11]. The interaction between the preoperative exposure of opioids and other controlled substances, while common, has not been generally addressed in the orthopaedic evidence. In this study, we found that patients exposed to benzodiazepines and sedative/hypnotics filled a greater number of opioid prescriptions postoperatively. We also found that patients with a current or remote history of smoking and mood disorders also filled a greater number of opioid prescriptions postoperatively. Finally, we found that patients without exposure to opioid medication had limited use of those medications after hand surgery.
There are several limitations to our study. First, there was no differentiation in the amount of opioid used before surgery in the exposed group. For example, a patient habituated to a fentanyl patch was pooled together with a patient who filled one prescription of Tylenol with codeine before surgery. This methodology has been traditionally used in studies evaluating opioid consumption in patients after hand surgery [11]. Further study evaluating how the degree of opioid use before surgery leads to postoperative use patterns is warranted. Second, although the database we used includes data from 17 states, it is possible that some patients may have obtained their pain medication in a state that does not report to the PDMP database we used. Although a weakness, this is unlikely to have materially affected our results since the database includes information from most of the states in the Northeastern and mid-Atlantic regions of the United States, the geographic region where this study was conducted. Third, our study measured prescriptions filled and not the actual amount of medication used. Fourth, it is possible that some patients may have obtained their opioid medications from sources other than their prescriptions, which may have led to an underestimation of the number of patients who used opioids or other controlled substances. Fifth, it is possible that the websites do not accurately reflect the prescriptions filled, either due to pharmacy noncompliance or clerical errors. Given the substantial attention to this issue and heavy penalties assessed for noncompliance, we believe that the magnitude of this error is likely small. Sixth, due to limitations in our medical record, we counted a current or remote smoking history as positive, which may not accurately reflect the actual smoking status at the time of surgery. Similarly, the use of alcohol and mood disorders was dichotomized as a yes/no answer; we did not consider the amount of alcohol consumed or whether or not the patient reported a mood disorder was consistent with the list of medications. Finally, results of this study are subject to bias since the study cohort is not population-based, but rather a single-center study from the patient population of two hand surgeons.
Preoperative use of benzodiazepines or sedatives/hypnotics were risk factors for prolonged opioid use. Our study confirms the findings of an earlier report [6], which found that patients exposed to benzodiazepines undergoing major surgical procedures were more likely to continue taking opioid medications beyond 90 days postoperatively. Our findings expand on these findings by suggesting that even patients undergoing minor hand surgical procedures will continue opioid use. The findings of that early research and our study indicate that patients who are on benzodiazepine or sedative/hypnotic medications preoperatively should be considered to be at greater risk for prolonged opioid use postoperatively.
Patients with a history of smoking and mood disorders also demonstrated increased opioid use postoperatively. Moreover, these effects appear to be additive, since patients with exposure to more than one controlled substance filled more opioid, benzodiazepine, and sedative/hypnotic prescriptions than those with exposure to one substance.
We found that patients unexposed to opioids preoperatively had very limited use of opioid medication after hand surgery. Our findings are in contrast to other studies evaluating opioid use after hand surgery. In a study using an insurance database to assess postoperative opioid usage in opioid-naïve patients, Johnson et al. [11] found that 13% of patients continued to fill opioid prescriptions after 90 days. Although the reason for the discrepancy between this study and ours is unclear, one potential explanation is that patients in that investigation were not excluded if they had repeat surgery during the study period. Many conditions in hand surgery are bilateral and need staged surgery within a short period, and as such, repeat opioid prescriptions are not infrequent and related to having repeat surgery and not to opioid habituation.
Much of our knowledge with regard to postoperative opioid use is based on investigations relying on insurance databases for patient information. While database studies do allow the evaluation of a large number of patients, substantial weaknesses, such as populating patient cohorts with diagnostic and procedural codes, are inherent in these studies. Moreover, these studies do not have the capacity to assess which patients received an opioid prescription and decided not to fill it. As such, these patients are typically excluded from the analysis, likely biasing the results toward those patients who would be more likely to use or overuse opioid medications. Finally, many of these studies define persistent or prolonged use as those who filled a prescription in the 90- to 180-day period after surgery, which can be misleading, especially in the opioid-naïve population.
Due to the large difference in narcotic prescription fills between opioid-exposed and naïve patients, an effort to minimize or completely wean patients off these medications before elective surgeries may help. Studies have highlighted the need for opioid weaning programs to close the gap highlighted in our study [13]. Decreasing dependence on opioids in chronic pain patients may improve postoperative outcomes, but further study is needed to better define how much of a decrease in opioid use, and for what period of time, is necessary. In 2001, the Joint Commission indicated in its Pain Management Standards that pain should be thought of as the “fifth vital sign” in response to the perception that pain was being undertreated [16]. In light of the opioid epidemic, however, some are looking to the Joint Commission to reexamine these policies [8]. Regardless, pain management is an appropriate, and expected, part of postsurgical care for patients undergoing hand surgery. We believe that creating dependence or habituation in an opioid-, benzodiazepine-, or sedative-naïve patient after a single short-course opioid regimen after hand surgery is rare. The vast majority of our patients who were given opioid prescriptions did not require further narcotics.
Patients without exposure to opioid, benzodiazepine, or sedative/hypnotic medications are unlikely to develop a long-term need for opioid medication. Having outpatient hand surgery and being prescribed an opioid does not appear to change the usage patterns of controlled substances. While often ignored, benzodiazepine and sedative/hypnotic use can contribute to increased opioid use in the postoperative period. Patients with preoperative exposure to controlled substances require much greater scrutiny, a more-detailed discussion regarding expectations, and a plan regarding postoperative pain management. Based on the results of this study, we are now more aware of the potential problems of patients with exposure to controlled substances, and we are more attentive about reviewing their history of substance use in the PDMP website, which is an important resource [14, 17, 18]. In addition, we now provide much more detailed preoperative counseling regarding the use and abuse of opioid medication in patients with exposure to benzodiazepines, sedatives, and those with a smoking history and mood disorders. Future studies evaluating the interaction between these controlled substances and the effect of the degree of opioid exposure in the preoperative period will help to improve the practitioner’s understanding of these complex interactions.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172:425-430. [DOI] [PubMed] [Google Scholar]
- 2.Bao Y, Pan Y, Taylor A, et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff (Millwood). 2016;35:1045-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, Bohnert ASB, Kheterpal S, Nallamothu BK. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152:e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll I, Barelka P, Wang CKM, Wang BM, Gillespie MJ, McCue R, Younger JW, Trafton J, Humphreys K, Goodman SB, Dirbas F, Whyte RI, Donington JS, Cannon WB, Mackey SC. A pilot cohort study of the determinants of longitudinal opioid use after surgery. Anesth Analg. 2012;115:694-702. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Annual Surveillance Report of Drug-Related Risks and Outcomes — United States, 2017. Surveillance Special Report 1. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Published August 31, 2017. Available at: https://www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf. Accessed January 2, 2019. [Google Scholar]
- 6.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315:1624-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fiore K. Opioid Crisis: Scrap Pain as 5th Vital Sign? Groups call on JC and CMS to re-evaluate policies that could lead to opioid overprescribing. https://www.medpagetoday.com/publichealthpolicy/publichealth/57336. Accessed December 18, 2017.
- 9.Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54:901-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang X, Orton M, Feng R, Hossain E, Malhotra NR, Zager EL, Liu R. Chronic opioid usage in surgical patients in a large academic center. Ann Surg. 2017;265:722-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson SP, Chung KC, Zhong L, Shauver MJ, Engelsbe MJ, Brummett C, Waljee JF. Risk of prolonged opioid use among opioid-naïve patients following common hand surgery procedures. J Hand Surg Am. 2016;41:947-957. [DOI] [PubMed] [Google Scholar]
- 12.Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV . Opioid epidemic in the United States. Pain Physician. 2012;15:ES9-38. [PubMed] [Google Scholar]
- 13.McAnally H. Rationale for and approach to preoperative opioid weaning: a preoperative optimization protocol. Perioper Med (Lond). 2017;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.New Jersey Division of Consumer Affairs. New Jersey Prescription Monitoring Program. Available at http://www.njconsumeraffairs.gov/pmp/Pages/default.aspx. Accessed December 6, 2017.
- 15.Pennsylvania Department of Health. Pennsylvania Prescription Drug Monitoring Program. Available at http://www.health.pa.gov/Your-Department-of-Health/Offices%20and%20Bureaus/PaPrescriptionDrugMonitoringProgram/Pages/Prescribers.aspx#.WgnDFUoo7Gh. Accessed December 6, 2017.
- 16.Phillips DM. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA. 2000;284:428-429. [DOI] [PubMed] [Google Scholar]
- 17.Prescription Drug Monitoring Program Training and Technical Assistance Center. PDMP mandatory enrollment of prescribers and dispensers. Available at: http://www.pdmpassist.org/pdf/Mandatory_Enrollment_5.pdf. Accessed December 7, 2017.
- 18.Rutkow L, Smith KC, Lai AY, Vernick JS, Davis CS, Alexander GC. Prescription drug monitoring program design and function: A qualitative analysis. Drug Alcohol Depend. 2017;180:395-400. [DOI] [PubMed] [Google Scholar]
- 19.Schoenfeld AJ, Nwosu K, Jiang W, Yau AL, Chaudhary MA, Scully RE, Koehlmoos T, Kang JD, Haider AH. Risk factors for prolonged opioid use following spine surgery, and the association with surgical intensity, among opioid-naive patients. J Bone Joint Surg Am. 2017;99:1247-1252. [DOI] [PubMed] [Google Scholar]
- 20.Webster BS, Verma SK, Gatchel RJ. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine. 2007;32:2127-2132. [DOI] [PubMed] [Google Scholar]
- 21.Weinheimer K, Michelotti B, Silver J, Taylor K, Payatakes A. A prospective, randomized, double-blinded controlled trial comparing ibuprofen and acetaminophen versus hydrocodone and acetaminophen for soft tissue hand procedures. J Hand Surg Am. [Published online ahead of print November 27, 2018]. DOI: 10.1016/j.jhsa.2018.10.014. [DOI] [PubMed]