Sir,
The submandibular gland is located in the submandibular triangle, inferomedial to the mandibular body. The submandibular gland consists of a superficial portion and a deep portion, which are divided by the mylohyoid muscle (Fig. 1A).1 Usually, botulinum toxin type A (BTX-A, Botox; Allergan Inc. Irvine, California) can be injected in the submandibular gland to treat sialorrhea. BTX-A is effective and known to provide effective volume reduction as a side effect.2,3 The esthetic purpose of BTX-A injection is to reduce the bulging area inferior to the mandibular angle and offer a smooth and attractive jawline.
Fig. 1.
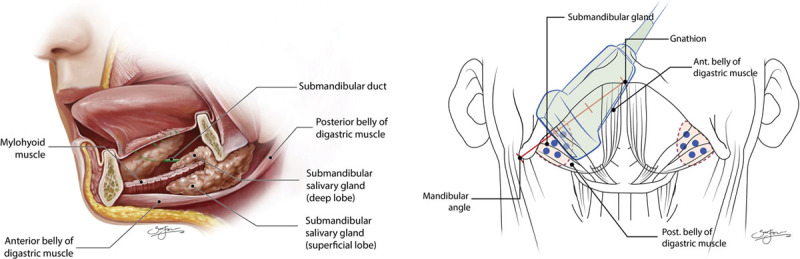
Anatomy of the submandibular gland and injection point. A, The submandibular gland is located in the submandibular triangle, inferior to the mandibular border between the anterior and posterior belly of the digastric muscle with the platysma muscle forming the roof. The submandibular gland consists of a superficial portion and a deep portion, which are divided by the mylohyoid muscle. B, The distance from the angle of the mandible to the gnathion was divided into thirds, and ultrasonography was used to measure the mediolateral diameter at the lateral two-thirds point preoperatively and at 1, 2, 3, 4, 5, and 6 months postoperatively (blue dot: injection point).
During this study, we administered submandibular gland injections in 20 patients from January to March 2018. The gland thickness was preoperatively measured using ultrasonography (Prosound Alpha7; Hitachi Aloka Medical, Tokyo, Japan). The distance from the angle of the mandible to the gnathion was divided into thirds, and ultrasonography was used to measure the mediolateral diameter at the lateral two-thirds point, with the ultrasonography probe placed in the direction as shown in Figure 1B. We then injected a total of 40 units, placing 20 units at 5 points on each side under ultrasonography guidance to ensure accuracy and to identify the salivary glands and surrounding structures. Ultrasonography-guided injection enabled dynamic and real-time monitoring during the procedure. It is noninvasive and fast, and bears no risk of exposure to radiation.4 We injected at a high concentration of 20 units per 0.2 ml of normal saline. We used a 0.5-inch 30-gauge needle to inject in 5 points, 5 mm apart, in an area closest to the submandibular gland on ultrasonography (Fig. 1B). The mediolateral diameter was measured at the same point every month for the next 6 months. The mean (±SD) measurements were 15.2 ± 4.2 mm preoperatively, and 10.8 ± 3.7, 10.1 ± 3.2, 12.5 ± 4.1, 13.8 ± 3.5, 14.5 ± 3.1, and 15.1 ± 3.9 mm at 1, 2, 3, 4, 5, and 6 months postoperatively, respectively. To prevent dysphagia and dysarthria caused by the injection spreading botulinum toxin into structures around the submandibular gland, such as the mylohyoid muscle and subcutaneous fat tissue, administration of the injections at a high concentration is recommended. Volume reduction peaked around the second month and lasted about 6 months before the effect almost completely disappeared. Saliva production was not reduced, which is believed to be due to the normal function of the parotid and sublingual glands.
The procedure is relatively simple, and with appropriate patient selection, the therapeutic effect can be favorable and result in high patient satisfaction. With the popularization of esthetic standards favoring a narrow face, demand is growing rapidly. Salivary gland enlargement can be caused by various diseases, including hereditary diseases, malformations, human immunodeficiency virus infections, blockage of the salivary duct, and malignant tumors. If the salivary glands are noticeably enlarged or asymmetrical, it is essential to first evaluate the patient for underlying conditions.5 As maintaining proper salivary gland function is important, the risks and benefits should be addressed before performing esthetic treatments. Therefore, clinicians should be aware of the general recommendations to use the smallest possible dose and the longest possible treatment duration.
ACKNOWLEDGMENT
The authors thank Sun Joo Kim (VOM LAB) for the preparation of the excellent medical illustrations and graphic design.
Footnotes
Published online 1 April 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Lee JH, Lee BN, Kwon SO, et al. Anatomical localization of submandibular gland for botulinum toxin injection. Surg Radiol Anat. 2010;32:945. [DOI] [PubMed] [Google Scholar]
- 2.Petracca M, Guidubaldi A, Ricciardi L, et al. Botulinum toxin A and B in sialorrhea: long-term data and literature overview. Toxicon. 2015;107(Pt A):129. [DOI] [PubMed] [Google Scholar]
- 3.Restivo DA, Panebianco M, Casabona A, et al. Botulinum toxin A for sialorrhoea associated with neurological disorders: evaluation of the relationship between effect of treatment and the number of glands treated. Toxins (Basel). 2018;10:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.So JI, Song DH, Park JH, et al. Accuracy of ultrasound-guided and non-ultrasound-guided botulinum toxin injection into cadaver salivary glands. Ann Rehabil Med. 2017;41:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel VN, Hoffman MP. Salivary gland development: a template for regeneration. Semin Cell Dev Biol. 2014;25–26:52. [DOI] [PMC free article] [PubMed] [Google Scholar]


