Supplemental Digital Content is available in the text.
Abstract
Background:
Current male-to-female (MtF) sex-reassignment-surgery techniques have not been fully successful to achieve the ideal objectives. The ordeal of multiple procedures, associated complications, and suboptimal results leads to high rate of dissatisfaction. We have tried to overcome functional inadequacy and address the esthetic issues for outer genitalia and vagina with our innovative “true shape sigma-lead SRS: Kaushik’s technique,” which has now become the technique of choice for MtF genital SRS for our patients.
Methods:
Between April 2007 and April 2017, authors performed 386 sigma-lead SRS in MtF transsexuals. Results were analyzed based on complications, resurgeries, and esthetic/functional outcomes. Corrective SRS using rectosigmoid constituted 145 cases and is not a part of this study.
Results:
Maximum follow-up was 7 years (average 34 months). Seventy-eight (20.2%) patients had complications, majority being minor (97.4%). Forty-four (11.4%) required resurgeries, 10 (2.6%) were corrective for introital stricture and mucosal prolapse, whereas 34 (8.8%) opted for optional minor esthetic enhancement. The overall satisfaction rate for cosmetic and functional outcomes was 4.7 out of 5. In addition to review of the literature, innovations in the technique have been explained.
Conclusions:
Kaushik’s sigma-lead MtF SRS technique is a step short to become the gold standard of genital SRS because it has proven to be safe and reliable. It allows faster healing, minimal dilation, and nearly natural cosmetic results in the form of clitoris/clitoral hood, labia minora, labia majora along with self-lubricating, fully deep, and sensate neovagina with orgasmic capabilities. This is perhaps the largest reported series of rectosigmoid use in transsexuals carried out for primary vaginoplasty.
INTRODUCTION
The ultimate goal of male-to-female (MtF) transformation in transgenders is not only to achieve external anatomy of the female body through a series of complex and staged surgeries but also to supplement the completeness by aligning the physical self with the biopsychosocial framework of a female individual, thereby addressing the basic concept of gender identity disorder.1–3
MtF gender affirmation surgical techniques span from split-thickness graft, full-thickness graft, penile/ penoscrotal inversion, and fasciocutaneous flaps to pedicled intestinal flaps.4–14 Currently, prevalent techniques have not been fully successful in achieving the ideal objective of reconstructing the genitals that resemble the cis-female genitals in full form and function.4 The search for new and improved solutions continues because there has been a constant scope of improvement for both functionality and cosmetic outcome.4 Prolonged hormonal intake leads to penoscrotal hypoplasia making penoscrotal inversion vaginoplasty not feasible.10,15–19
Thus, we aimed to describe in this article our modified technique which has nearly overcome the functional inadequacy of the existing techniques and has addressed the esthetic issues of reconstructed outer genitalia and vagina. It has now become the technique of choice for MtF gender affirmation surgery for our patients.
PATIENTS AND METHODS
Between January 2008 and April 2017, we performed 386 sigma-lead SRS in MtF transgenders who met the World Professional Association for Transgender Health (WPATH) criteria. A total of 145 cases who underwent corrective SRS using rectosigmoid colon were excluded in the study. These patients had been operated before using other techniques and were dissatisfied with outcomes.
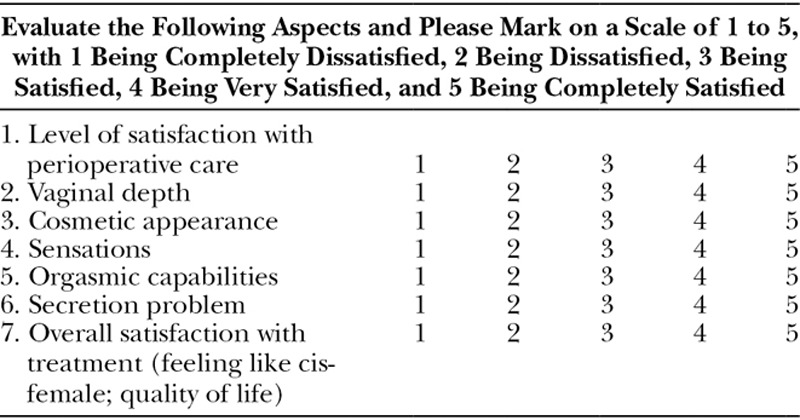
Patient records and interviews focused on age, smoking history, surgical time, complications, resurgeries, and cosmetic and functional outcomes were collected and analyzed. Outcomes were assessed according to 7 parameters (Table 1). Informed consent was obtained from each patient.
Table 1.
Questionnaire at 12 Months after Surgery
Patient Selection, Surgical Eligibility, and Preoperative Preparation
We excluded patients with body mass index >30. Patients with cardiac diseases, unfit for GA, and sigmoid colon diseases were also excluded. Sigmoid colonoscopy was carried out for those older than 50 years of age or those with a history of bowel problem related to the colon. Estrogen use and smoking were discontinued for at least 2 weeks and 2 months, respectively, before surgery. Over the past 3 years, we have implemented a nonsmoking disclosure to be signed by the patient.
Bowel is prepared using polyethylene glycol with electrolyte solution a day before surgery. Prophylactic antibiotics were administered at the start of surgery. GA with epidural analgesia was used. LMW heparin was administered in patients with a history of DVT. The DVT intermittent pneumatic pumping system was used intraoperatively and for 2 days postsurgery. The patient was placed in lithotomy position during the procedure.
Surgical Technique
We developed this surgical procedure as a modular concept. Module 1 is the creation of vulva, and module 2 is the creation of vagina using penile skin and rectosigmoid colon segment. Both modules are preferably done together as a single stage, although they can be carried out in 2 stages (see video, Supplemental Digital Content 1, which demonstrates surgical technique of sigma-lead gender affirmation surgery and postoperative results, http://links.lww.com/PRSGO/B24).
Video Graphic 1.

See video, Supplemental Digital Content 1, which displays sigma-lead MtF gender affirmation surgery demonstrating surgical technique and postoperative results, http://links.lww.com/PRSGO/B24.
Through left lateral Pfannenstiel approach, the rectosigmoid colon was freed. Preferably, the proximal pedicle, a sigmoidal branch of the inferior mesenteric artery, is chosen to get the antegrade segment. If the proximal pedicle was not reliable, a distal pedicle was identified, preferably having 2 vessels consisting of branches of the superior rectal artery. The mesentery was sequentially ligated and divided in between ligatures throughout the length of the selected segment. Bowel was washed through the colotomy incisions at proximal and distal division sites to avoid spillage of colon contents. The colon segment was divided at the proximal and distal sites (Fig. 1A). The proximal end of the graft was closed (distal end in cases of distal pedicle), making it the dome of the neovagina. About 1 cm from the anus, a posteriorly based triangular scrotal flap (4 cm base width × 6 cm length) was raised, and a cavity was created between the bladder and rectum. The colon segment was delivered gently in the created cavity. The distal end of the segment was sutured with the invaginated scrotal flap completing the posterior vaginal wall. The dome of neovagina was fixed with sacral promontory to minimize the incidence of prolapse.
Fig. 1.
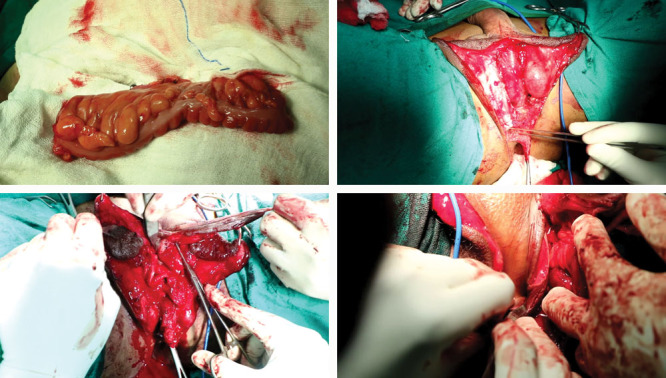
A, Harvested pedicled colon segment. B, Right orchiectomy showing fixation of cord structures until the lower end. This is done bilaterally to achieve bulk of labia majora. C, The penile skin is degloved superficial to the Buck’s fascia, leaving one-third of preputial skin attached to the glans. D and E, Dorsolateral part of glans is elevated along with dorsal tunica vaginalis containing neurovascular bundle. F, Penile skin is slit into 2 flaps except for proximal 1 inch. Clitoral shaft is made. Bilateral triangular back cut flaps to create the clitoral hood. G, Bilateral triangular flaps tucked under the tubed clitoral shaft to achieve a 1-cm hood, and glans is reshaped in the form of clitoris and fed under the hood. H, Distal two-thirds of the preputial flap attached to slit penile flap is lifted up to meet the upper third of the preputial flap attached to glans. The anchor suture being applied to define the groove between the labia majora and minora, and the labia minora are sculptured.
The midline scrotal incision was extended until the penile base ventrally. After orchiectomy, the preserved cord along with fat was fixed until the lower end to enhance labia majora bulk (Fig. 1B). About 3 inches of the proximal urethra was separated off the corpora. Penile skin was degloved superficial to the Buck’s fascia all the way, except for a small flap (4 cm × 2 cm) of inner preputial skin, which was left attached to the glans (Fig. 1C). The dorsolateral part of glans with attached preputial skin flap and dorsal tunica albuginea containing neurovascular bundle were dissected off, until the base of the penis (Fig. 1D, E). Corpora were excised.
Penile skin flap was slit into 2 halves barring a proximal 1 inch. Tube-like clitoral base/shaft was constructed by enfolding the central unslit proximal portion and was anchored to the suspensory ligament with 3-point nylon 4-0 stitch. Some amount of pubic fat is incorporated in the tube to avoid flattening. Small (1 cm × 1 cm) triangular flaps raised akin back cuts on medial aspects of either penile hemiflaps and were stitched under a clitoral tube to create an approximately 1-cm roof, achieving a clitoral hood. The trimmed reshaped clitoris was anchored under this hood (Fig. 1F, G). The side wings of small preputial flaps were sutured to the medial edge of penile skin in a “Namaste” position forming the upper one-third of labium minus.
In the center of distal third of the penile flap, an anchor stitch was taken and fixed to the crural base deep in the vaginal cavity. This key stitch provided a downward pull and defined the groove between the labia majora and minora creating an inner layer of majora and outer layer of minora. The lower two-thirds of the attached preputial skin were lifted up in “Namaste” position and attached to the upper third of labium, thereby achieving full-length labia minora (Figs. 1H and 2A). The rest of the penile skin was anastomosed to the colon segment in a zig-zag, tension-free manner to complete the anterior and lateral vaginal walls. The mucocutaneous junction was typically placed beyond 2 inches (Fig. 2B).
Fig. 2.
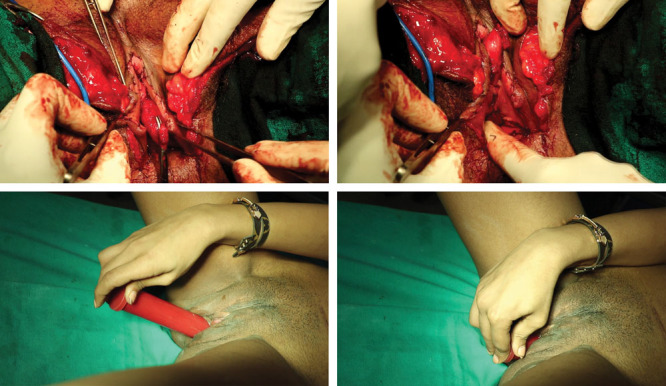
A, Sculptured labia minora with well-defined clitoris and hood. B, Vaginal introitus, zig-zag mucocutaneous junction is placed at or beyond 2 inches. C, Scrotal skin is degloved preserving dartos to achieve additional bulk to labia majora. D, Medialization of labia majora, and margin of scrotal skin is medialized and anchored to crura to place the scar medially. E, Immediate postoperative. F, Two-week postoperative. G and H, One-year postoperative.
Extra scrotal skin was deepithelialized preserving the dartos tissue to achieve the bulk of labia majora (Fig. 2C). The edges of this scrotal skin were medialized and anchored to the crural stump (Fig. 2D). The labia majora were constructed with stitching of medialized scrotal skin with outer half of slit penile flap. The urethra was slit transversely and spatulated, and corpus spongiosum was trimmed. Urethra was placed caudal to the clitoris.
Postoperative Period
Pain relief was achieved with intravenous and epidural analgesia. Intravenous antibiotics were administered for 3–5 days. Use of electrolyte solutions (potassium, calcium, and magnesium) has dramatically improved the recovery and reduced paralytic ileus incidence. Patient passed flatus within 48 hours and was allowed liquids orally. Foley’s catheter was removed after 6 days and ambulation resumed. Daily vaginal wash was done from third day onward. Hospital stay duration was 7 (5–10) days. Dilation schedule was extremely simple, which was started 7–14 days postsurgery. Dilation was performed twice daily with soft deflatable mold for 5 minutes followed by 5–10 minutes using a rigid dilator and continued for 8–16 weeks, as necessary. The patients were advised to maintain hygiene by washing the genitalia with 5% betadine solution for about 3 weeks. Sexual activity can be resumed at 6–8 weeks. Penetrative sex is counted as dilation.
RESULTS
The total number of patients was 386. Average age was 39 (22–63) years. Eighty-two patients (21.2%) had a history of smoking. Average surgical time was 5.2 (4–7) hours. None required emergency reoperation. Average follow-up was 34 (12–84) months.
Seventy-eight patients (20.2%) developed complications, with the majority (97.4%) having minor complications (Table 2). Minor healing issues were seen in 21 (5.4%) patients and were managed conservatively. Mucorrhea was reported by 24 (6.2%), which resolved after 9 months. Mucosal prolapse was seen in 6 (1.5%), especially those older than 50 years of age (n = 5). Other minor complications include introital stricture, dyspareunia, urinary retention (managed with prolonged catheter and cholinergics), wound infection, paralytic ileus, and clitoral necrosis. Major complications in the form of colon segment vascularity loss were noticed intraoperatively in 2 patients (0.5%), who had a smoking history.
Table 2.
Complications and Patient Follow-up
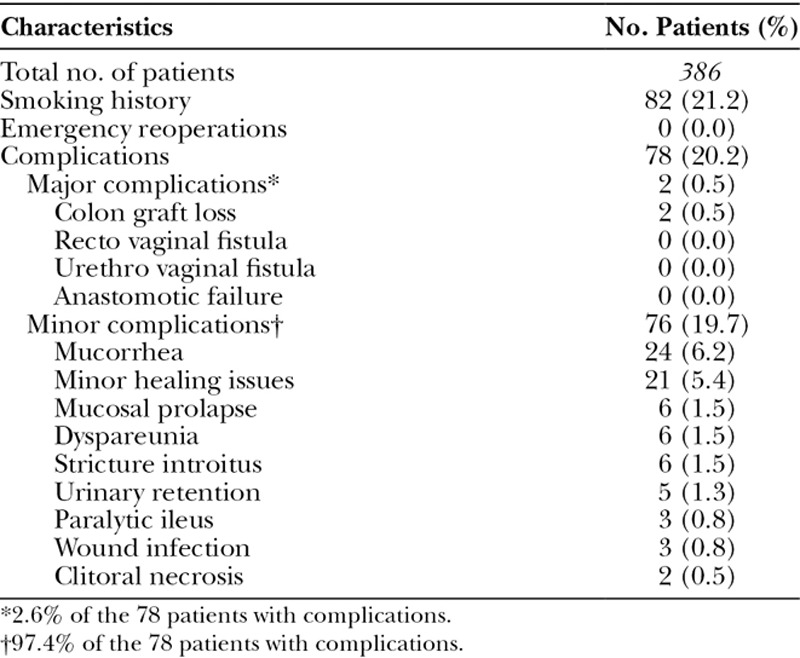
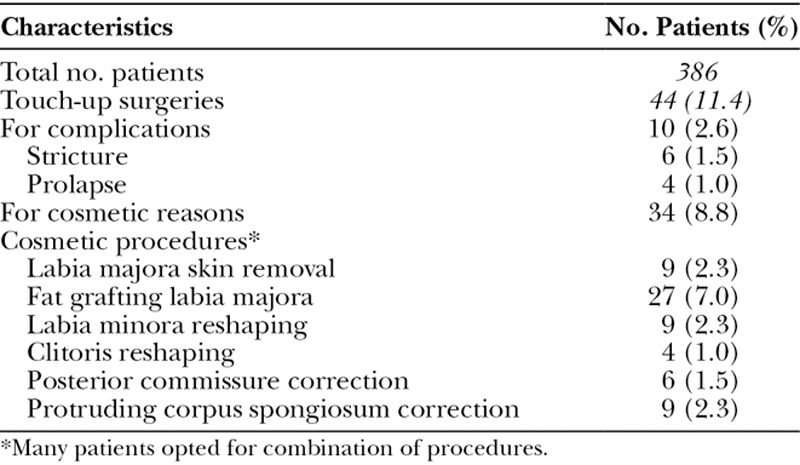
Touch-up surgeries were performed in 44 (11.4%) patients; of these, 10 (2.6%) were corrective and 34 (8.8%) were for esthetic enhancement of genitals in combination with other surgeries at a later date (Table 3). Out of the 10 who had corrective touch-ups, 6 (1.5%) were for introital strictures and 4 (1%) for mucosal prolapse.
Table 3.
Description of Corrective/Touch-up Surgeries
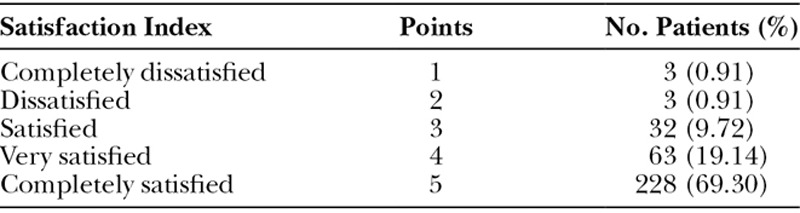
The level of satisfaction was assessed using a questionnaire at 12 months postoperatively. Response was received from 329 patients. Average overall satisfaction level was 4.7/5 (Tables 1 and 4).
Table 4.
Questionnaire Results (n = 329 Patients)
DISCUSSION
MtF vaginoplasty techniques span from split-thickness graft, full-thickness graft, penile/penoscrotal inversion, and fasciocutaneous flaps to pedicled intestinal flaps.4–14 Currently, penile inversion is the most commonly performed sex reassignment surgery (SRS) technique worldwide.11–13,20–22 This technique was pioneered by Burou,23 Gillies and Millard,24 Edgerton and Bill,25 and Pandya and Stuteville.8 In this technique, the pedicled sensitive penile skin is used, but it results in inadequate vaginal depth, disfigured outer vulva, constant and unpleasant discharge, possible vaginal vault prolapse, and painful postoperative care.7,9,26
Prolonged hormonal intake leads to penoscrotal hypoplasia making penoscrotal inversion vaginoplasty not feasible.10,15–19 To overcome the limitation of inadequate vaginal depth in transsexuals, the use of skin graft was introduced by Abraham.27 The use of full-thickness skin graft from penile skin was first reported by Fogh-Anderson28 and refined by Preecha11 and Motta et al.29
Limitations of skin graft split skin graft (SSG)/full thickness graft (FTG) vaginoplasty are inadequate graft take up, contraction of vagina due to scarring and graft shrinkage, long and painful postoperative aftercare and long-term dilation (even lifetime), introducing skin into a nonphysiological location, a vagina with poor erogenous sensations, no self-lubricating/self-cleaning properties, dyspareunia, neovaginal prolapse, donor area scarring, condylomatosis, intraepithelial neoplasia associated with human papilloma virus, and carcinoma.4,7,9,26,30,31
Forceful dilations lead to vicious cycle of breakdown and healing of patchy scars causing further stenosis necessitating lifelong painful dilation to keep the vagina patent. Should the patient leave dilation, patchy healing results in pockets with entrapped skin grafts, leading to repeated bouts of infection with purulent discharging sinuses? We have noticed these findings during corrective SRS. In corrective SRS, detaking this entrapped skin graft is challenging and poses risks to adjacent structures.
First mention of intestinal vaginoplasty in MtF transsexuals dates 1974, when Markland and Hastings used cecum and sigmoid transplants.32 Ileal, ascending colon, and transverse colon segments have also been used without extra advantage, but added excessive discharge problem.12,14,29,33
The promising benefits of sigmoid colon vaginoplasty were large lumen, integral strong walls resistant to trauma, mucosal lining with self-lubricating and self-cleaning properties, excellent vaginal sensations, rapid healing, and minimal postoperative care with shorter dilation regimen.4,5,7,34,35 Studies have shown that use of pedicled sigmoid colon flap for vaginoplasty mitigates many of the issues seen with penoscrotal flap.7,36–38 Most of the studies relegate rectosigmoid transfer to MRKH syndrome, previously failed skin vaginoplasty, or in patients with previous penectomy and orchiectomy (secondary vaginoplasty).9,39 Many studies have pointed out the following complications in rectosigmoid vaginoplasty: mucorrhea, mucocele, introital stricture, unnatural reddish appearance due to the visible mucosa at the opening, neuroma formation, increased risk of bacteria entering the abdomen, postoperative ileus, and constipation.4,5,9,22,40
These limitations were minimal to nonexistent in our patients. Complications were seen in 78 patients (20.2%), with the majority (97.4%) having minor complications. Only 10 (2.6%) needed corrective surgeries mainly for introital stricture (causing dyspareunia) and mucosal prolapse. In this technique, distal 2–3 inches of penile skin is anastomosed to sensate rectosigmoid in a zig-zag, tension-free manner placing mucocutaneous junction at or beyond 2 inches, thus avoiding the unnatural red appearance and minimizing introital stricture and mucosal prolapse. Minor abdominal wound infection was noted in 3 (0.8%), which were earlier cases. Addition of intraoperative bowel wash dramatically led to practically zero wound infection rate. Incidence of mucorrhea was quite low, which was reported only in 24 patients (6.2%) and resolved within 9 months in all patients. A shorter rectosigmoid, with most parts having dehydrating properties, lessens mucorrhea, but maintains natural self-cleaning and self-lubricating properties. Studies in the literature have reported higher incidence of prolonged mucorrhea.5,9,22
Intraoperative colon graft vascularity loss was considered a major complication and was observed in 2 patients (0.5%) who had a history of smoking and claimed quitting for 2 months before surgery. In one case, the ileum was successfully used as an alternative. In another case, the ileal segment was discolored and bowel vaginoplasty was not suitable. Rectovaginal or urethrovaginal fistula in other techniques has been reported in previous studies,5,13,26,42–45 but none of our patients had these.
The primary focus in most of the genital reconstructive surgery has been to develop an optimal method of creating a neovagina that would facilitate sexual intercourse. Clitoris/clitoral hood and labia minora remain among the most difficult structures to reconstruct. Despite increasing concerns for esthetic results of vulva and clitoro-labial creation with erogenous sensations, the ideal clitoro-labiaplasty, which would yield results resembling a biological female in every aspect, has not yet been achieved.4,17,45,46
Brown used a reduced glans attached to its dorsal neurovascular pedicle. The incidence of clitoral necrosis was very high necessitating modification of techniques and secondary corrective surgeries.47–50 Maintaining the viability of full-length preputial skin necessitates preserving the bulky glans tissue, which results in bulky clitoris leading to hindrance in hood creation. This large clitoris is esthetically unacceptable and is taken as a residual penis by the patient. Additional incisions and corrections in pursuit of the perfect outcome would lead to vascular compromise to the labial minora and occasionally clitoris and hypertrophic scarring,4 which we experienced in our earlier cases.
In this technique, 3–4 inches of penile and preputial skin is utilized to create cosmetically appealing vulva parts: clitoris shaft, clitoral hooding, natural size sensate clitoris, full-length labia minora, bulky youthful full-length labia majora, and natural appearing introitus. The unslit proximal central part of penile flap is enfolded (entubed) with a 3-point anchor stitch giving a natural clitoral shaft. The incorporated fat avoids flattening of the shaft.
We developed the innovative idea of using bitriangular flaps, achieving about 1 cm hood/roof over the clitoris as in a cis-female. Clitoral hood gradually transits into the labia minora. Inclusion of dorsal tunica albuginea ensures viability of island neurovascular flap and enables the making of a small anatomical-sized clitoris and larger glanular flaps for the upper part of labia minora. The pedicle is robust and kink resistant with minimal incidence of necrosis and revision surgeries. Moreover, erogeneity is quite high owing to more nerve endings being incorporated. The whole of the preputial skin remains viable as it is used in 2 separate flaps for labia minora creation. Small flap remains attached to the clitoris in the form of glanulo-preputial flap and a larger preputial skin flap remains attached to the penile skin. The groove between the labia minora and majora was defined with an anchor stitch to penile flap, as described previously. We preserved viable fat, cord structure, and dartos tissue to achieve bulky labia majora until the lower end. Medialization of labia majora is a unique modification to achieve more esthetic natural look of the vulva in the form of apposed labia majora, deep commissure, and medially placed scar which becomes inconspicuous over the time.
Minor clitoral and labial necrosis was noticed only in 2 patients (0.5%), which is extremely low as compared to other studies.47–49 Minor healing issues with minor necrosis were noticed in 21 (5.4%) patients with smoking history, which were treated conservatively. The incidence is low as compared with that reported in the literature.11,42,44,52 Cosmetic enhancement was carried out in 34 patients (8.8%), which is quite low as compared with a previous report.13 Moreover, these touch-ups were optional rather than required, as these were opted in combination with other surgical procedures during revisits for possible esthetic enhancement of otherwise acceptable genitals. The protrusion of corpus spongiosum was seen in 9 (2.3%) patients in earlier part of our series. Later, we adopted trimming of the corpus spongiosum as described by Preecha.11 Incidence of protrusion in our study is quite low as compared with other studies.5
Few studies have focused on functional outcome in the form of sexual outcome after male to female (MtF) SRS.52,53 The latest articles emphasize the need of developing new instruments for evaluating gender confirmation surgery outcome as there are no valid instruments available yet.54,55 In our series, the outcome was assessed in terms of esthetic and functional outcomes, including orgasmic capabilities. Out of 329 patients who responded to the questionnaire, 323 (98.2%) were satisfied with the outcome. Overall average satisfaction level was 4.7/5. The satisfaction rate is much higher than that reported by other studies involving a lesser volume of patients.5,7,13,56–60
There are some limitations of the study. First, even though the plastic surgeon was the same for all patients, the general surgeon involved varied. This could have contributed to some variations in the outcome. Second, even though we have collected subjective data from the patients, we do feel that objective data from physical examinations are lacking. Third, even though the technique has a long learning curve, this study with a long follow-up is evidence that this technique is safe and effective.
CONCLUSIONS
The sigma-lead MtF gender affirmation surgery is a safe and reliable technique. It allows faster healing and very minimal postoperative aftercare while delivering very natural cosmetic results in all major aspects of cis-genitals, namely, the sensate clitoris, clitoral hooding, full-length stand-out labia minora, and appealing apposed youthful labia majora with minimum scarring. It also provides a self-lubricating, fully sensate deep neovagina, allowing for clitoral and vaginal sexual arousal and climaxes with minimal dilation requirement. Complications, though present, can be treated successfully with revision surgery. Moreover, this is perhaps the largest reported series of rectosigmoid transfer in MtF transsexuals performed for primary vaginoplasty.
Footnotes
Published online 2 April 2019.
Presented (Invited lecture for Video Workshop) at the 53rd Annual National Conference of Association of Plastic Surgeons of India (APSICON 2018), November 21, 2018, Lucknow, Uttar Pradesh.
Presented (Invited lecture) at the Annual Conference of Kerala Plastic Surgeons Association (KPSACON 2018), April 21, 2018.
The technique was introduced and explained during a video workshop and symposium on male-to-female sex reassignment.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.WHO. International Statistical Classification of Diseases and Related Problems, 10th Revision, 20052nd ed Geneva, Switzerland: WHO. [Google Scholar]
- 2.Ainsworth TA, Spiegel JH. Quality of life of individuals with and without facial feminization surgery or gender reassignment sur-gery. Qual Life Res. 2010;19:1019. [DOI] [PubMed] [Google Scholar]
- 3.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconform-ing people, version 7. Int J Transgenderism. 2012;13:165. [Google Scholar]
- 4.Bizic M, Kojovic V, Duisin D, et al. An overview of neovaginal reconstruction options in male to female transsexuals. Sci World J. 2014;2014:638919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrison SD, Satterwhite T, Grant DW, et al. Long-term out-comes of rectosigmoid neocolporrhaphy in male-to-female gen-der reassignment surgery. Plast Reconstr Surg. 2015;136:386. [DOI] [PubMed] [Google Scholar]
- 6.Markland C, Hastings D. Vaginal reconstruction using bowel segments in male-to-female transsexual patients. Arch Sex Behav. 1978;7:305. [DOI] [PubMed] [Google Scholar]
- 7.Laub DR, Laub DR, II, Biber S. Vaginoplasty for gender confirma-tion. Clin Plast Surg. 1988;15:463. [PubMed] [Google Scholar]
- 8.Pandya NJ, Stuteville OH. A one-stage technique for construct-ing female external genitalia in male transsexuals. Br J Plast Surg. 1973;26:277. [DOI] [PubMed] [Google Scholar]
- 9.Kwun Kim S, Hoon Park J, Cheol Lee K, et al. Long-term results in patients after rectosigmoid vaginoplasty. Plast Reconstr Surg. 2003;112:143. [DOI] [PubMed] [Google Scholar]
- 10.Djordjevic ML, Stanojevic DS, Bizic MR. Rectosigmoid vagino-plasty: clinical experience and outcomes in 86 cases. J Sex Med. 2011;8:3487. [DOI] [PubMed] [Google Scholar]
- 11.Wangjiraniran B, Selvaggi G, Chokrungvaranont P, et al. Male-to-female vaginoplasty: Preecha’s surgical technique. J Plast Surg Hand Surg. 2015;49:153. [DOI] [PubMed] [Google Scholar]
- 12.Reed HM. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin Plast Surg. 2011;25:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buncamper ME, van der Sluis WB, van der Pas RS, et al. Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women. Plast Reconstr Surg. 2016;138: 999. [DOI] [PubMed] [Google Scholar]
- 14.Manrique OJ, Sabbagh MD, Ciudad P, et al. Gender-confirmation surgery using the pedicle transverse colon flap for vaginal re-construction: a clinical outcome and sexual function evaluation study. Plast Reconstr Surg. 2018;141:767. [DOI] [PubMed] [Google Scholar]
- 15.Bouman MB, van der Sluis WB, Buncamper ME, et al. Primary total laparoscopic sigmoid vaginoplasty in transgender women with penoscrotal hypoplasia: a prospective cohort study of sur-gical outcomes and follow-up of 42 patients. Plast Reconstr Surg. 2016;138:614e. [DOI] [PubMed] [Google Scholar]
- 16.Ozkan O, Akar ME, Ozkan O, et al. The use of vascularized je-junum flap for vaginal reconstruction: clinical experience and results in 22 patients. Microsurgery. 2010;30:125. [DOI] [PubMed] [Google Scholar]
- 17.Bouman MB, Buncamper ME, van der Sluis WB, et al. Total lapa-roscopic sigmoid vaginoplasty. Fertil Steril. 2016;106:e22. [DOI] [PubMed] [Google Scholar]
- 18.Bouman MB, van der Sluis WB, van Woudenberg Hamstra LE, et al. Patient-reported esthetic and functional outcomes of prima-ry total laparoscopic intestinal vaginoplasty in transgender wom-en with penoscrotal hypoplasia. J Sex Med. 2016;13:1438. [DOI] [PubMed] [Google Scholar]
- 19.Chen HC, Chana JS, Feng GM. A new method for vaginal re-construction using a pedicled jejunal flap. Ann Plast Surg. 2003;51:429. [DOI] [PubMed] [Google Scholar]
- 20.Sutcliffe PA, Dixon S, Akehurst RL, et al. Evaluation of surgi-cal procedures for sex reassignment: a systematic review. J Plast Reconstr Aesthet Surg. 2009;62:294; discussion 306. [DOI] [PubMed] [Google Scholar]
- 21.Selvaggi G, Bellringer J. Gender reassignment surgery: an over-view. Nat Rev Urol. 2011;8:274. [DOI] [PubMed] [Google Scholar]
- 22.Hage JJ, Karim RB, Asscheman H, et al. Unfavorable long-term results of rectosigmoid neocolpopoiesis. Plast Reconstr Surg. 1995;95:842; discussion 849. [PubMed] [Google Scholar]
- 23.Burou G. Laub DR, Gandy P. Male to female transformation. In: Proceedings of the Second Interdisciplinary Symposium on Gender Dysphoria Syndrome. 1973:Palo Alto, CA: Stanford University Press; 188. [Google Scholar]
- 24.Gillies H, Millard RD., Jr Genitalia. In: The Principles and Art of Plastic Surgery, Volume II. 1957: London, UK: Butterworth; 369. [Google Scholar]
- 25.Edgerton MT, Bull J. Surgical construction of the vagina and la-bia in male transsexuals. Plast Reconstr Surg. 1970;46:529. [DOI] [PubMed] [Google Scholar]
- 26.Rossi Neto R, Hintz F, Krege S, et al. Gender reassignment surgery–a 13 year review of surgical outcomes. Int Braz J Urol. 2012;38:97. [DOI] [PubMed] [Google Scholar]
- 27.Abraham F. Genitalumwandlung an zwei m¨annlichen Transvestiten. Zeitschrift f¨ur Sexualwissenschaft und Sexualpolitik. 1931;18:223. [Google Scholar]
- 28.Fogh-Anderson P. Transvestism and trans-sexualism: surgical treat-ment in a case of auto-castration. Act Med Leg Soc. 1956;9:33. [PubMed] [Google Scholar]
- 29.Motta GL, Tavares PM, Silva GVM, et al. Full-thickness skin mesh graft vaginoplasty: a skin sparing technique. Int Braz J Urol. 2017;43:1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steffanoff DN. Late development of squamous cell carcinoma in a split-skin graft lining a vagina. Case report. Plast Reconstr Surg. 1973;51:454. [DOI] [PubMed] [Google Scholar]
- 31.Fernandes HM, Manolitsas TP, Jobling TW. Carcinoma of the neovagina after male-to-female reassignment. J Low Genit Tract Dis. 2014;18:E43. [DOI] [PubMed] [Google Scholar]
- 32.Markland C, Hastings D. Vaginal reconstruction using cecal and sigmoid bowel segments in transsexual patients. J Urol. 1974;111:217. [DOI] [PubMed] [Google Scholar]
- 33.Wu JX, Li B, Liu T, et al. Eighty-six cases of laparoscopic vagi-noplasty using an ileal segment. Chin Med J (Engl). 2009;122: 1862. [PubMed] [Google Scholar]
- 34.Rajimwale A, Furness PD, III, Brant WO, et al. Vaginal construc-tion using sigmoid colon in children and young adults. BJU Int. 2004;94:115. [DOI] [PubMed] [Google Scholar]
- 35.Perovic S, Stanojevic D, Djordjevic M, et al. Refinements in recto-sigmoid vaginoplasty. Eur Uro. 1998;33:156. [Google Scholar]
- 36.Gatti C, Del Rossi C, Lombardi L, et al. Sexuality and psychoso-cial functioning in young women after colovaginoplasty. J Urol. 2010;184(4 Suppl):1799. [DOI] [PubMed] [Google Scholar]
- 37.Kapoor R, Sharma DK, Singh KJ, et al. Sigmoid vaginoplasty: long-term results. Urology. 2006;67:1212. [DOI] [PubMed] [Google Scholar]
- 38.Tu D, Badalato G, Reiley EA, et al. Colovaginoplasty using the Yang-Monti modification. J Pediatr Urol. 2012;8:477. [DOI] [PubMed] [Google Scholar]
- 39.Lima M, Ruggeri G, Randi B, et al. Vaginal replacement in the pe-diatric age group: a 34-year experience of intestinal vaginoplasty in children and young girls. J Pediatr Surg. 2010;45:2087. [DOI] [PubMed] [Google Scholar]
- 40.Parsons JK, Gearhart SL, Gearhart JP. Vaginal reconstruction utilizing sigmoid colon: complications and long-term results. J Pediatr Surg. 2002;37:629. [DOI] [PubMed] [Google Scholar]
- 41.Perovic SV, Stanojevic DS, Djordjevic ML. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. 2000;86:843. [DOI] [PubMed] [Google Scholar]
- 42.Krege S, Bex A, Lümmen G, et al. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. 2001;88:396. [DOI] [PubMed] [Google Scholar]
- 43.Raigosa M, Avvedimento S, Yoon TS, et al. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. 2015;12:1837. [DOI] [PubMed] [Google Scholar]
- 44.Sigurjonsson H, Rinder J, Möllermark C, et al. Male to female gender reassignment surgery: Surgical outcomes of consecutive patients during 14 years. JPRAS Open. 2015;6:69. [Google Scholar]
- 45.Belgrano E, Lissiani A. Belgrano E, Fabris B, Trombetta C. La femminilizzazione dei genital esterni e la creazione della neovagina. In: Il Transessualismo. 1999: Milan, Italy: Editrice Kurtis; 87. [Google Scholar]
- 46.Sohn M, Bosinski HA. Gender identity disorders: diagnostic and surgical aspects. J Sex Med. 2007;4:1193; quiz 1208. [DOI] [PubMed] [Google Scholar]
- 47.Brown J. Marchac D, Hueston JT. Creation of a functional clitoris and aesthetically pleas-ing introitus in sex conversion. In: Transactions of the Sixth International Congress of Plastic and Reconstructive Surgery. 1976: Masson, Paris, France; 654. [Google Scholar]
- 48.Rubin SO. A method of preserving the glans penis as a clitoris in sex conversion operations in male transsexuals. Scand J Urol Nephrol. 1980;14:215. [DOI] [PubMed] [Google Scholar]
- 49.Eldh J. Construction of a neovagina with preservation of the glans penis as a clitoris in male transsexuals. Plast Reconstr Surg. 1993;91:895; discussion 901. [PubMed] [Google Scholar]
- 50.Szalay L. Construction of a neoclitoris in male transsexuals. Plast Reconstr Surg. 1994;93:646. [PubMed] [Google Scholar]
- 51.Goddard JC, Vickery RM, Qureshi A, et al. Feminizing genito-plasty in adult transsexuals: early and long-term surgical results. BJU Int. 2007;100:607. [DOI] [PubMed] [Google Scholar]
- 52.De Cuypere G, Janes C, Rubens R. Psychosocial functioning of transsexuals in Belgium. Acta Psychiatr Scand. 1995;91: 180. [DOI] [PubMed] [Google Scholar]
- 53.Lawrence AA. Patient-reported complications and functional outcomes of male-to-female sex reassignment surgery. Arch Sex Behav. 2006;35:717. [DOI] [PubMed] [Google Scholar]
- 54.Barone M, Cogliandro A, Di Stefano N, et al. A systematic review of patient-reported outcome measures following transsexual sur-gery. Aesthetic Plast Surg. 2017;41:700. [DOI] [PubMed] [Google Scholar]
- 55.Andréasson M, Georgas K, Elander A, et al. Patient-reported out-come measures used in gender confirmation surgery: a system-atic review. Plast Reconstr Surg. 2018;141:1026. [DOI] [PubMed] [Google Scholar]
- 56.De Cuypere G, T’Sjoen G, Beerten R, et al. Sexual and physi-cal health after sex reassignment surgery. Arch Sex Behav. 2005;34:679. [DOI] [PubMed] [Google Scholar]
- 57.Lief HI, Hubschman L. Orgasm in the postoperative transsexual. Arch Sex Behav. 1993;22:145. [DOI] [PubMed] [Google Scholar]
- 58.Labus LD, Djordjevic ML, Stanojevic DS, et al. Rectosigmoid vaginoplasty in patients with vaginal agenesis: sexual and psycho-social outcomes. Sex Health. 2011;8:427. [DOI] [PubMed] [Google Scholar]
- 59.Borkowski A, Czaplicki M, Dobronski P. Twenty years of expe-rience with Krzeski’s cystovaginoplasty for vaginal agenesis in Mayer-Rokitansky-Küster-Hauser syndrome: anatomical, his-tological, cytological and functional results. BJU Int. 2008;101: 1433. [DOI] [PubMed] [Google Scholar]
- 60.Weyers S, Elaut E, De Sutter P, et al. Long-term assessment of the physical, mental, and sexual health among transsexual women. J Sex Med. 2009;6:752. [DOI] [PubMed] [Google Scholar]


