Abstract
Increased sagittal plane posterior tibial slope has been identified as a risk factor for primary anterior cruciate ligament reconstruction (ACLR) failure. Although ACLR failure is multifactorial, correction of sagittal plane posterior tibial slope should be evaluated in patients with an ACLR graft rupture. There are limited technical descriptions of proposed decreasing tibial slope osteotomy procedures; therefore, the purpose of this Technical Note is to describe the current senior author's technique of performing an anterior closing wedge proximal tibial osteotomy to decrease sagittal plane tibial slope in patients requiring a revision ACLR.
Increased tibial slope has been identified to be a cause of increased sagittal plane knee translation and therefore has been linked to increased loading behavior in the anterior cruciate ligament (ACL).1, 2, 3 Subsequently, an increased posterior tibial slope has been associated with an increased risk of ACL reconstruction (ACLR) graft failure.4, 5 Although native tibial slope has been described to average approximately 7° to 10°, evidence suggests that an increased sagittal plane tibial slope ≥12° to be directly correlated with increased anterior tibial translation, thereby predisposing patients to ACLR graft failure.1, 4, 5
Although ACLR graft failure is multifactorial, correction of sagittal plane posterior tibial slope should be evaluated in patients with a failed ACLR; however, there are limited technical descriptions of proposed decreasing tibial slope osteotomy procedures. The purpose of this Technical Note was therefore to describe the current senior author's technique of performing an anterior closing wedge proximal tibial osteotomy to decrease sagittal plane tibial slope in patients requiring a revision ACLR.
Surgical Technique
Detailed information on the technique is shown in Video 1. Pearls and pitfalls of this technique and a step-by-step approach are described in Tables 1 and 2, respectively.
Table 1.
Pearls and Pitfalls of Anterior Closing Wedge Proximal Tibial Osteotomy
| Pearls | Pitfalls |
|---|---|
| The use of a radiolucent retractor to protect the posterior neurovascular structures allows the surgeon to fluoroscopically access the osteotomy without having to remove it | Lack of aiming device and osteotomy guide may lead to nonparallel cut |
| Closing wedge osteotomy should be performed slowly with the use of passive force to ensure appropriate closure and minimize risk of tibial fracture | Risk of fracture of the posterior tibial cortex |
| Use of multiple staples allows for fixation of closing wedge osteotomy before refixation of tibial tubercle | Requires concurrent tibial tubercle osteotomy |
| Use of a curette to complete osteotomy under live fluoroscopic imaging | Relying solely on oscillating saw to complete entire anterior bone resection may lead to penetration of posterior cortex and possible hinge fracture |
| Closing wedge osteotomy cut needs to include entire medial and lateral cortex to allow for the appropriate posterior hinge | Osteotomy is based on measured anterior cortical resection requiring free-hand pins to be converged at the posterior cortex |
Table 2.
Advantages and Disadvantages of Anterior Closing Wedge Proximal Tibial Osteotomy
| Advantages | Disadvantages |
|---|---|
| Allows for correction of sagittal plane tibial slope | Potential to increase knee hyperextension following osteotomy |
| Direct anterior approach allows for access of ACL tibial tunnel for simultaneous bone grafting of previous ACL reconstruction tunnel | Technically demanding procedure |
| Tibial osteotomy is biomechanically effective in both knee flexion and extension | Requires 8-week period of non-weightbearing |
| No risk of PCL injury as seen with other osteotomy using oblique cuts made toward the posterior joint line near the PCL tibial insertion | Risk of injury to popliteal neurovascular structures with direct anteroposterior bicortical drilling |
| Allows for distalization of the tibial tubercle to prevent extensor lag and patella alta |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Indications and Contraindications
Precise patient selection is crucial for the success of this surgical procedure. The main indication for this procedure is increased sagittal plane posterior slope ≥12° in a patient with a failed ACLR. Other relative indications include severe anterior instability as evidenced by a high-grade Lachman and pivot shift (3+) on physical examination in patients with single or multiple failed ACLRs. Measurements may be conducted on the lateral view of plain radiographs, ensuring there is sufficient visualization of the distal tibia. Longstanding radiographs should also be obtained to rule out any significant genu varus or valgus malalignment. Contraindications for a decreasing slope anterior closing wedge osteotomy include primary ACLR patients, genu recurvatum with significant knee hyperextension (e.g., >10°), posterior cruciate ligament (PCL) deficiency, significant genu varus malalignment, and end-stage tibiofemoral osteoarthritis.
Preoperative Planning
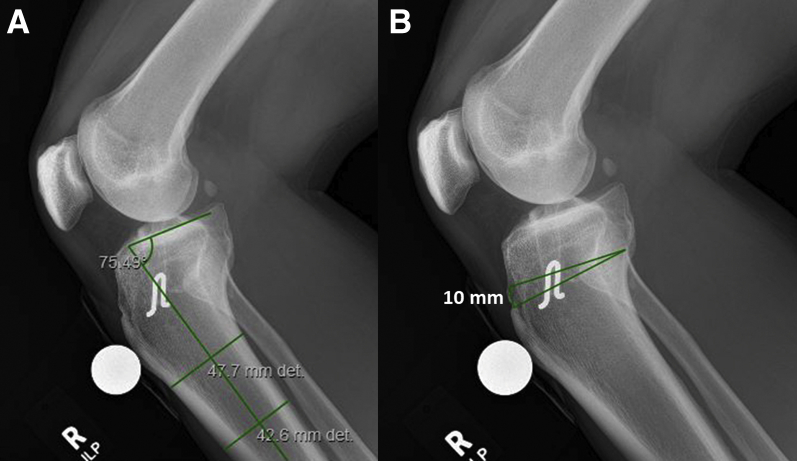
Posterior tibial slope is calculated from plain radiographs according to a previously established measurement technique.6 The amount of slope correction is measured according to the lateral radiographic image, with a target reduced slope angle of 6° to 8° (Fig 1). It is estimated that ∼1.67 mm of anterior resection of the tibia equates to ∼1° of slope correction; thus, an osteotomy aiming for a 10-mm anterior resection will correct the posterior tibial slope by 6°. Previous literature indicates a decreased tibial slope of approximately ≤5° may increase the risk for PCL injury7; therefore, careful attention should be made to not overcorrect the degree of posterior tibial slope and potentially increase the strain on the PCL.
Fig 1.
Preoperative right knee lateral radiograph measuring degree of native posterior tibial slope and desired anterior closing wedge osteotomy. (A) Lateral radiograph measuring approximately 15° native posterior tibial slope in a patient with a failed anterior cruciate ligament reconstruction. (B) A 10-mm anterior tibial resection is measured on the preoperative lateral radiograph for presurgical planning.
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After the induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent ligamentous instability and to assess knee range of motion. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, which is then placed into a leg holder (Mizuho OSI, Union City, CA) while the contralateral knee is placed into an abduction stirrup (Birkova Product, Gothenburg, NE). The foot of the operating table is then lowered, allowing the surgeon to freely manipulate the knee as needed.
Surgical Approach
Arthroscopy is performed first with debridement of the previous ACLR graft remnants, including debridement of the soft tissues in the previous ACLR femoral tunnel. The tunnel is thoroughly debrided with the aid of a 5.5-mm shaver, 4.5-mm curved shaver, and curved rasp. The menisci are also examined at this time; concomitant meniscal repair should be performed during this surgery if indicated. Next, the leg holder is removed, the foot of the operating table is raised, and the closing wedge osteotomy is then performed with the patient in the supine position.
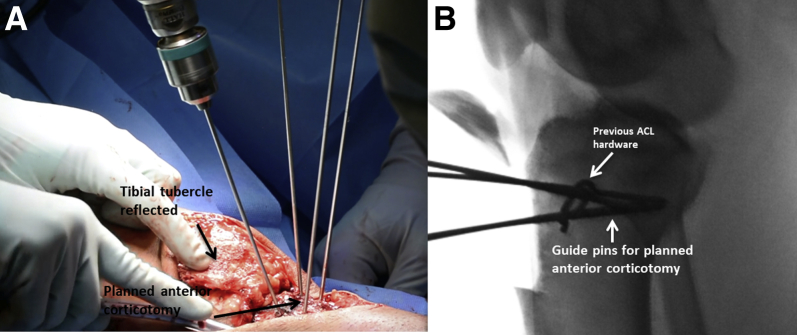
The open procedure then ensues by making an 8- to 10-cm midline incision from the midportion of the patella distally beyond the tibial tubercle. A Cobb elevator is used to elevate tissues away from the tubercle distally, medially, and laterally to allow for isolation of the tibial tubercle to prepare it for a tibial tubercle osteotomy. Next, a scalpel is used to elevate the periosteum in a proximal to distal fashion from the medial and lateral borders of the tubercle. A Cushing elevator is then passed deep to the patella tendon, just proximal to its insertion, to fully isolate and protect the distal extent of the patella tendon. A mark is made 30 mm distal to the proximal attachment of the patellar tendon. Beginning medially, the proposed bone block is marked with electrocautery ensuring adequate thickness of at least 3- to 4-mm depth of cancellous bone to prevent fracture after later fixation. A 2-mm drill bit (Synthes, West Chester, PA) is passed multiple times along the medial tibial cortex in parallel fashion on the medial side through only the near cortex from medial to lateral along the previously marked outline and then repeated from lateral to medial on the lateral side. Beginning medially, a small osteotome is passed in a unicortical fashion between the sites of the drill holes to complete the corticotomy extending to the proximal and distal corners. This is repeated on the lateral border. A single, large osteotome is passed from medial to lateral connecting the medial and lateral osteotomy sites, ensuring no bony bridges are present. Finally, a small oscillating saw (ConMed, Utica, NY) is used to complete the osteotomy distally, releasing the distal bone bridge at a 45°angle, which allows for reflection of the osteotomy in a superior direction (Fig 2).
Fig 2.
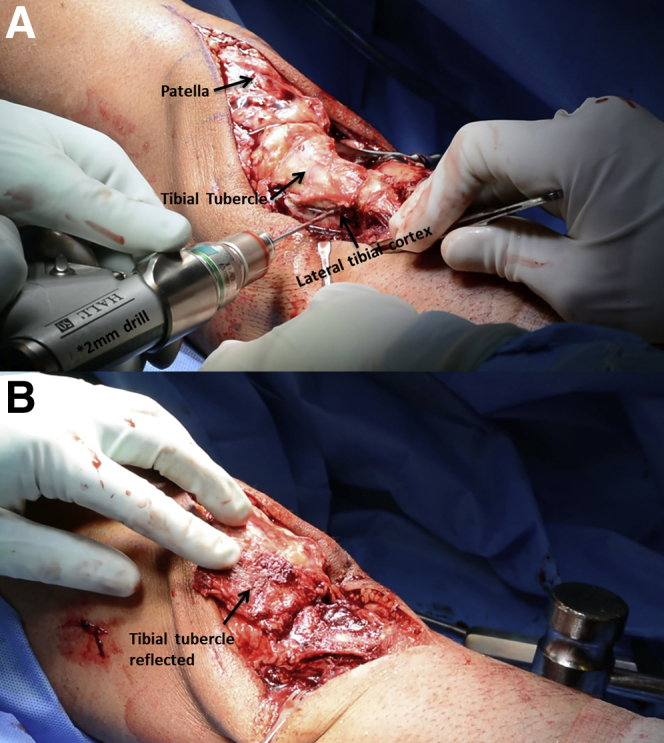
Right knee tibial tubercle osteotomy. (A) A 2-mm drill bit (Synthes) is passed multiple times along the lateral and medial tibial cortex in parallel. (B) Reflected tibial tubercle following distal detachment.
With the tubercle reflected in a superior fashion, access to the preoperative site of maximum deformity of the proximal tibia is then achieved. Soft-tissue dissection occurs both medially and laterally to the posterior borders of the tibia. Identification and clearing of the previous ACLR tibial reconstruction tunnel and removal of fixation hardware and debridement of the soft tissue within the tunnel is performed.
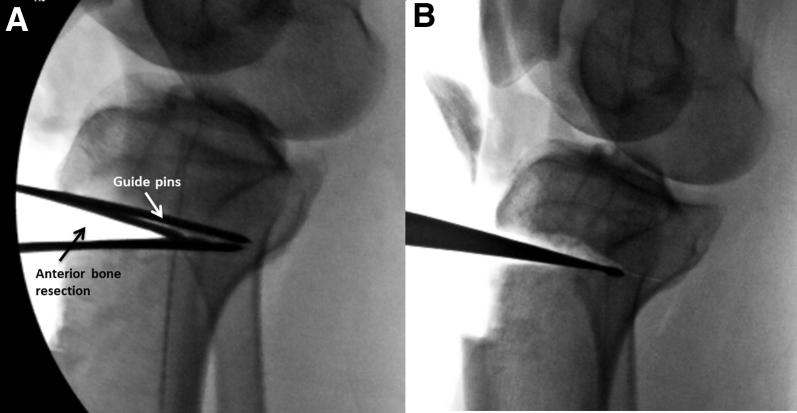
With the aid of fluoroscopy, a single 1.7-mm K-wire is passed from anterior to posterior in the medial third of proximal tibia; this pin is placed to be perpendicular to the shaft of the tibia and parallel to the tibial joint surface. This step is repeated at the same level into the lateral third of the proximal tibia. Multiple fluoroscopic images are obtained to ensure both pins are even and parallel to 1 another because they will serve as a guide for the initial corticotomy site. Using preoperative radiographs, the proposed distance to achieve adequate correction (in this case, 12 mm) is marked proximally. Two additional K-wires are placed proximal to the previously mentioned placed pins with aim of converging the pins just anterior to the posterior cortex. These 4 pins will serve as the guide for the bone cuts for the closing wedge osteotomy (Fig 3). Z-retractors are placed both medially and laterally behind the posterior tibial cortex to protect soft tissues and neurovascular structures. Using a large, oscillating saw (ConMed), the anterior, medial, and lateral cortices are breached in a unicortical fashion beginning distally. Using the proximal pins as a guide, the saw is then passed in a similar manner ensuring convergence to the prior cut corticotomy to converge anterior to the posterior tibial cortex (Fig 4). Caution is taken not to violate the posterior cortex. The remainder of the osteotomy both proximally and distally is completed with a 25-mm straight osteotome under fluoroscopic guidance to ensure no breach of the posterior tibial cortex. With adequate convergence, the wedge of bone can be removed en bloc and measured to verify adequate resection. All 4 K-wires are removed at this time. With the wedge of bone removed, the extremity is slowly hyperextended over 5 to 7 minutes to allow for closing of the osteotomy site, while preventing fracture of the posterior tibial cortex. A curette may be used to remove additional cancellous bone off the posterior cortex to aid in closing down the osteotomy (Fig 5). With the osteotomy site well opposed and compressed, a large Richards staple (Smith & Nephew, London, UK) is placed just medial to the midline to hold the osteotomy closed. Keeping the leg in hyperextension, 2 additional large staples are placed, with 1 being more posterior on the medial cortex and the other in the central aspect of the lateral tibial cortex (Fig 6). The extremity is gently ranged at this time to ensure no gapping occurs at the osteotomy site. Fluoroscopy should again be used to confirm no posterior cortex fracture. The bone wedge is then morselized and packed into the previous ACLR tibial tunnel under direct vision.
Fig 3.
Guide pins for planned anterior corticotomy in a right knee. (A) With the aid of fluoroscopy, a single 0.062-in C-wire is passed from anterior to posterior in the medial third of proximal tibia. This pin is placed to be perpendicular to the shaft of the tibia and parallel to the tibial joint surface. This step is repeated at the same level into the lateral third of the proximal tibia at the same level. A total of 4 pins are used to outline the desired anterior corticotomy area. (B) Fluoroscopic images are obtained to ensure pins are even and parallel to one another as they will serve as a guide for the initial corticotomy site.
Fig 4.
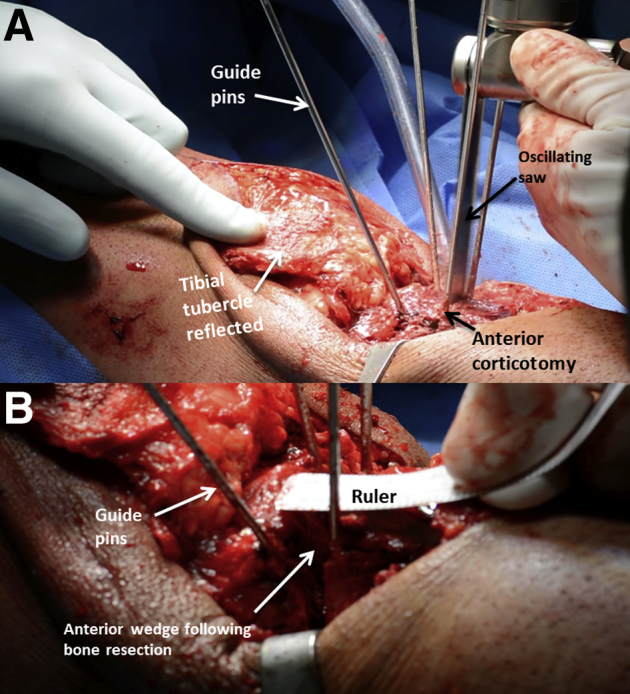
(A) Using a large oscillating saw (ConMed), the anterior, medial, and lateral cortices are breached in a unicortical fashion beginning distally in a right knee. Using the proximal pins as a guide, the saw is then passed in a similar manner, ensuring convergence to the prior cut corticotomy to converge anterior to the posterior tibial cortex. (B) Following anterior corticotomy, the closing wedge is measured to confirm desired anterior cortical resection.
Fig 5.
(A) Intraoperative fluoroscopy following anterior bone resection with an oscillating saw in a right knee. (B) Use a small curette to carefully remove additional bone without violating the posterior tibial cortex.
Fig 6.
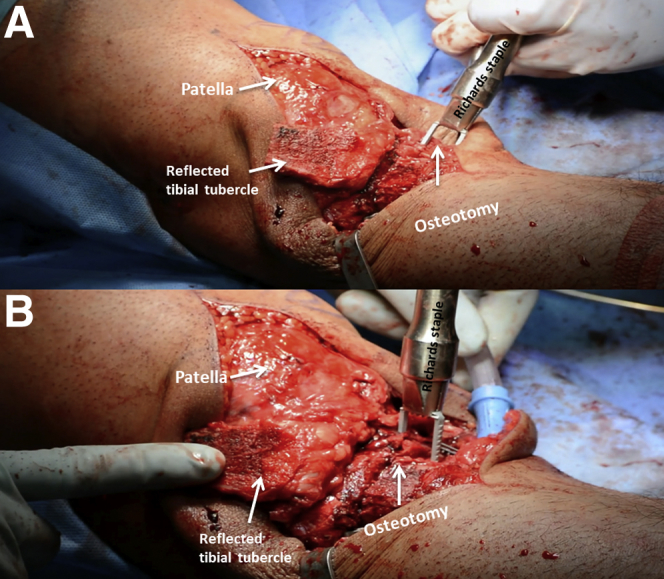
(A) With the osteotomy site well opposed and compressed, a large Richards staple (Smith & Nephew) is placed just medial to the midline to hold the osteotomy closed in a right knee. (B) Keeping the leg in hyperextension, 2 additional large staples are placed to help secure the osteotomy site. The use of 3 staples for the closing wedge osteotomy fixation allows for quick, low-profile fixation when the posterior cortex remains intact.
At the site of the prior tibial tubercle osteotomy, an additional bone distal resection is made equivalent to the amount of anterior wedge resection (in this case, 12 mm) to appropriately distalize the patella and prevent patella alta. Using the small oscillating saw, a 45° trough, 3- to 4-mm deep, is removed to facilitate a wedge-fit of the prior tibial tubercle osteotomy. Two K-wires for the cannulated 4.5-mm, fully threaded screws (Synthes) are inserted and checked with fluoroscopy. With placement and lengths confirmed, 2 fully threaded cannulated 4.5-mm screws are placed in a bicortical fashion with washers securing the osteotomy. At this time, arthroscopic placement of the allograft bone graft into the femoral tunnel is performed.
Final intraoperative fluoroscopic radiographs confirming the desired decreased posterior tibial slope are obtained (Fig 7). Repeat Lachman and pivot shift examinations are performed demonstrating increased stability of the knee because of the decreased tibial slope.
Fig 7.
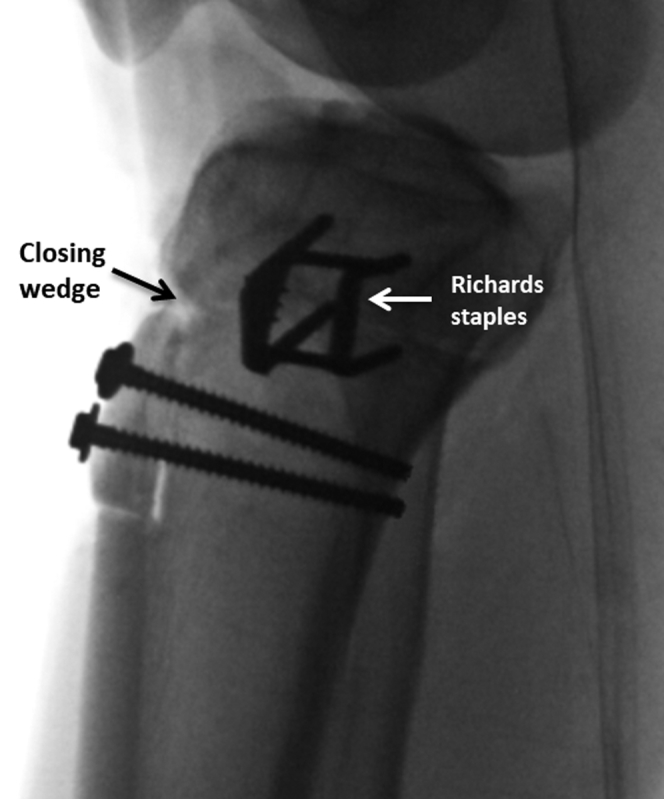
Intraoperative fluoroscopy demonstrating completion of anterior closing wedge osteotomy and reduced posterior tibial slope to 6° (lateral view, right knee).
Postoperative Protocol
After the procedure, the patient is to remain non-weightbearing for 8 weeks on crutches and in a knee immobilizer brace. Physical therapy begins on postoperative day 1 with a focus on pain control, reducing edema, and knee motion. Additionally, plain radiographs are taken 1 day postoperatively to ensure adequate slope correction and allow for baseline imaging of bone grafting of previous ACL reconstruction tunnels (Fig 8). During the first 2 weeks, passive range of motion is limited from 0° to 90° and then may progress as tolerated thereafter. After 8 weeks, weightbearing is gradually increased, based on clinical and radiographic evidence of bone healing, starting at 25% body weight, and increased by 25% body weight each week over a 4-week period. Revision ACLR may be performed after there is adequate bony healing around the osteotomy site, which may require up to 6 months.
Fig 8.

Postoperative day 1 right knee radiographs following anterior closing wedge osteotomy with the corrected posterior tibial slope measuring 7°. (A) Anteroposterior radiograph demonstrating reduced posterior tibial slope. (B) Lateral radiograph demonstrating normal surgical hardware that is in proper position with no displacement.
Discussion
An anterior closing wedge osteotomy to reduce posterior tibial slope has become increasingly recognized because of its efficacy in restoring knee stability and reducing the risk of further revision ACLR graft failure.4, 5 Although considered an invasive surgery, it has been suggested that a slope-decreasing osteotomy is necessary for patients wishing to return to sports or for those who need to restore necessary stability for demanding day-to-day activities after a failed ACLR and who have a tibial slope ≥12°.4, 5, 8 This is because it has been reported that increased tibial slope is directly correlated to increased anterior tibial translation, and has been shown to increase the forces experienced by the native ACL.1, 3, 9, 10 Clinical studies have supported these biomechanical findings, because an increased tibial slope has been reported to increase the risk of ACL graft failure, namely those ≥12°.4, 5, 8 In our experience, we find intraoperatively that solely decreasing tibial slope before the second-stage ACL revision surgery can independently reduce anterior tibial translation.
An anterior closing wedge osteotomy to reduce posterior tibial slope has been shown to be an effective procedure to reduce the risk of ACLR graft failure in clinical studies4, 5; therefore, it is suggested that this procedure should be considered for patients in which soft-tissue reconstruction alone is inadequate. Different surgical techniques for performing an anterior closing wedge osteotomy have been described.4, 5 One of the most significant differences between the current technique is the management of the tibial tubercle. In our preferred technique, an osteotomy is performed at the level of the tibial tubercle, requiring its location to be migrated distally to reduce the risk of secondary knee hyperextension. Although there is no consensus regarding the proper management of the tibial tubercle, it is important to ensure that neither patella alta or baja is created because of this procedure. In addition, the use of 3 staples for the closing wedge osteotomy fixation allows for quick, low-profile fixation when the posterior cortex remains intact. The use of a plate would be necessary if the posterior tibia cortex is violated and stronger fixation with increased rotational control is required; however, plates are not well contoured for this area of the tibia without additional soft-tissue disruption or significant modification to the plate. Furthermore, an anterior closing wedge osteotomy, rather than other described medial techniques, is indicated when patients do not require varus correction.11, 12, 13, 14, 15
This Technical Note describes our preferred technique to decrease posterior tibial slope via an anterior closing wedge osteotomy. We believe that our technique is a reproducible and effective procedure to reduce the risk of revision ACLR graft failure and improves patient outcomes concurrent to revision ACLR procedures. Further clinical studies are needed to develop a consensus among the various described techniques in the literature for slope-reducing anterior closing wedge osteotomy procedures.
This Technical Note describes the senior author's preferred technique for an anterior closing wedge osteotomy to reduce the amount of sagittal plane posterior tibial slope for patients with failed ACLR and significant increased posterior tibial slope.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. is a consultant and receives royalties from Smith & Nephew, OSSUR, and Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Following patient positioning (supine position, right knee), an 8- to 10-cm midline incision from the midportion of the patella distally beyond the tibial tubercle is made, and isolation of the tibial tubercle is performed. Once the periosteum has been elevated, a drill bit is passed multiple times along the medial tibial cortex in parallel fashion followed by a small osteotome in a unicortical fashion to complete the corticotomy. A small oscillating saw is then used to complete the osteotomy, allowing for reflection of the osteotomy in a superior direction. With the tubercle reflected in a superior fashion, a K-wire is passed from anterior to posterior, perpendicular to the shaft of the tibia and parallel to the tibial joint surface. This step is repeated at the same level into the lateral third of the proximal tibia. Two additional K-wires are placed proximal to the previously mentioned placed pins with aim of converging the pins just anterior to the posterior cortex. Using a large oscillating saw, the anterior, medial, and lateral cortices are breached in a unicortical fashion beginning distally and the remainder of the osteotomy is completed with a straight osteotome. Fluoroscopic guidance should be used throughout the procedure to ensure the direction and extent of the osteotomy. Once the wedge of bone has been removed, the extremity is slowly hyperextended over 5 to 7 minutes to allow for closing of the osteotomy site while preventing fracture of the posterior tibial cortex. The osteotomy site is then closed by large Richards staples just medial to the midline, posterior on the medial cortex, and in the central aspect of the lateral tibial cortex. At the site of the prior tibial tubercle osteotomy, an additional bone distal resection is made to distalize the patella and prevent patella alta. Two K-wires for cannulated fully threaded screws are then inserted and checked with fluoroscopy, securing the osteotomy.
References
- 1.Giffin J.R., Vogrin T.M., Zantop T., Woo S.L., Harner C.D. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 2.Hohmann E., Bryant A., Reaburn P., Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc. 2011;19(suppl 1):S109–S114. doi: 10.1007/s00167-011-1547-4. [DOI] [PubMed] [Google Scholar]
- 3.Fening S.D., Kovacic J., Kambic H., McLean S., Scott J., Miniaci A. The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: A human cadaveric study. J Knee Surg. 2008;21:205–211. doi: 10.1055/s-0030-1247820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dejour D., Saffarini M., Demey G., Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846–2852. doi: 10.1007/s00167-015-3758-6. [DOI] [PubMed] [Google Scholar]
- 5.Sonnery-Cottet B., Mogos S., Thaunat M. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:1873–1880. doi: 10.1177/0363546514534938. [DOI] [PubMed] [Google Scholar]
- 6.Utzschneider S., Goettinger M., Weber P. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19:1643–1648. doi: 10.1007/s00167-011-1414-3. [DOI] [PubMed] [Google Scholar]
- 7.Gwinner C., Weiler A., Roider M., Schaefer F.M., Jung T.M. Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: A prospective 5- to 15-year follow-up. Am J Sports Med. 2017;45:355–361. doi: 10.1177/0363546516666354. [DOI] [PubMed] [Google Scholar]
- 8.Salmon L.J., Heath E., Akrawi H., Roe J.P., Linklater J., Pinczewski L.A. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: The catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46:531–543. doi: 10.1177/0363546517741497. [DOI] [PubMed] [Google Scholar]
- 9.Agneskirchner J.D., Hurschler C., Stukenborg-Colsman C., Imhoff A.B., Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: A biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthopaed Trauma Surg. 2004;124:575–584. doi: 10.1007/s00402-004-0728-8. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi K.T., Cheung E.C., Markolf K.L. Effects of anterior closing wedge tibial osteotomy on anterior cruciate ligament force and knee kinematics. Am J Sports Med. 2018;46:370–377. doi: 10.1177/0363546517736767. [DOI] [PubMed] [Google Scholar]
- 11.Dean C.S., Chahla J., Moulton S.G., Nitri M., Serra Cruz R., LaPrade R.F. Anterolateral biplanar proximal tibial opening-wedge osteotomy. Arthrosc Tech. 2016;5:e531–e540. doi: 10.1016/j.eats.2016.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dejour H., Neyret P., Boileau P., Donell S.T. Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthopaed Related Res. 1994;229:220–228. [PubMed] [Google Scholar]
- 13.Trojani C., Elhor H., Carles M., Boileau P. Anterior cruciate ligament reconstruction combined with valgus high tibial osteotomy allows return to sports. Orthop Traumatol Surg Res. 2014;100:209–212. doi: 10.1016/j.otsr.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 14.Feucht M.J., Mauro C.S., Brucker P.U., Imhoff A.B., Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21:134–145. doi: 10.1007/s00167-012-1941-6. [DOI] [PubMed] [Google Scholar]
- 15.Tischer T., Paul J., Pape D. The impact of osseous malalignment and realignment procedures in knee ligament surgery: A systematic review of the clinical evidence. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117697287. 2325967117697287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Following patient positioning (supine position, right knee), an 8- to 10-cm midline incision from the midportion of the patella distally beyond the tibial tubercle is made, and isolation of the tibial tubercle is performed. Once the periosteum has been elevated, a drill bit is passed multiple times along the medial tibial cortex in parallel fashion followed by a small osteotome in a unicortical fashion to complete the corticotomy. A small oscillating saw is then used to complete the osteotomy, allowing for reflection of the osteotomy in a superior direction. With the tubercle reflected in a superior fashion, a K-wire is passed from anterior to posterior, perpendicular to the shaft of the tibia and parallel to the tibial joint surface. This step is repeated at the same level into the lateral third of the proximal tibia. Two additional K-wires are placed proximal to the previously mentioned placed pins with aim of converging the pins just anterior to the posterior cortex. Using a large oscillating saw, the anterior, medial, and lateral cortices are breached in a unicortical fashion beginning distally and the remainder of the osteotomy is completed with a straight osteotome. Fluoroscopic guidance should be used throughout the procedure to ensure the direction and extent of the osteotomy. Once the wedge of bone has been removed, the extremity is slowly hyperextended over 5 to 7 minutes to allow for closing of the osteotomy site while preventing fracture of the posterior tibial cortex. The osteotomy site is then closed by large Richards staples just medial to the midline, posterior on the medial cortex, and in the central aspect of the lateral tibial cortex. At the site of the prior tibial tubercle osteotomy, an additional bone distal resection is made to distalize the patella and prevent patella alta. Two K-wires for cannulated fully threaded screws are then inserted and checked with fluoroscopy, securing the osteotomy.