Abstract
Post-traumatic knee stiffness can present after injuries around the knee and surgery. Management is guided by the type of initial injury, amount of range-of-motion loss, time since injury, and cartilage status. Cases refractory to conservative management may conventionally be treated with manipulation under anesthesia (MUA), arthroscopic lysis of adhesions, or open quadricepsplasty. We describe our arthroscopic technique of lysis of adhesions with anterior interval release and intraoperative MUA, which has been shown to provide sustainable range-of-motion improvement in a subset of patients with severe knee arthrofibrosis. Although technically demanding, this technique benefits from being minimally invasive, allows for direct visualization of intra-articular structures, and allows all-round arthroscopic release of adhesions to improve patellar mobility and decrease the risk of fracture prior to MUA. A rigorous postoperative formal physical therapy protocol and patient compliance are imperative to achieve good outcomes.
Post-traumatic knee stiffness is common after injuries around the knee and surgery. Restricted range of motion (ROM) can be classified as extra-articular, intra-articular, or both. Management options depend on the type of initial injury (extra- or intra-articular), type of ROM loss (flexion, extension, or both), time since injury, and cartilage status. It is imperative to identify the specific cause of the knee stiffness to direct optimal surgical treatment.
Arthrofibrotic knee stiffness most commonly results from intra-articular scarring, fibrotic adhesions, tissue remodeling, periarticular tissue retraction, or bony impingement.1 Conservative treatment using anti-inflammatory medications, cortisone injections, and physical therapy (PT) has shown limited success in isolation, especially in the setting of post-traumatic knee stiffness. Manipulation under anesthesia (MUA) can be effective but may result in complications such as fracture, failure of fracture fixation, or chondral damage.
Arthroscopic lysis of adhesions with anterior interval release supplemented by intraoperative MUA has been accepted as a successful treatment modality for this condition and has provided sustainable ROM improvement in certain subsets of patients with post-traumatic stiffness.2, 3, 4, 5 A step-by-step approach is crucial and involves sequential release of scars, adhesions, and fibrotic structures in different regions of the knee. We present the arthroscopic surgical technique of the senior author (X.L.) to address severe post-traumatic or postsurgical knee stiffness (Video 1).
Technique
Setup and Patient Positioning
The indications for the described procedure include intra-articular knee arthrofibrosis refractory to conservative management including cortisone injections, anti-inflammatory medications, and prolonged PT. In addition, in patients with osteoporosis who have an increased risk of fracture with MUA alone, performing this technique first with arthroscopic lysis of adhesions along with capsular and anterior interval release would minimize their risk of complications.
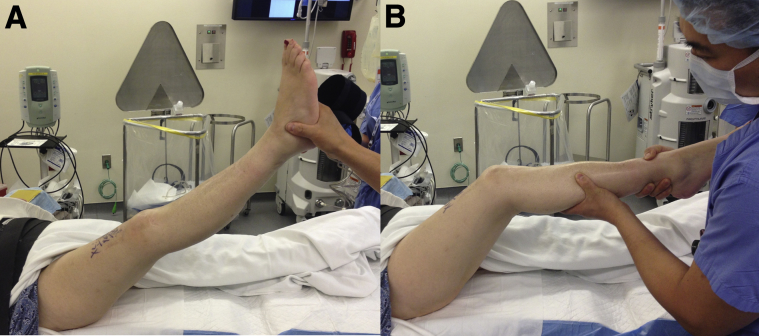
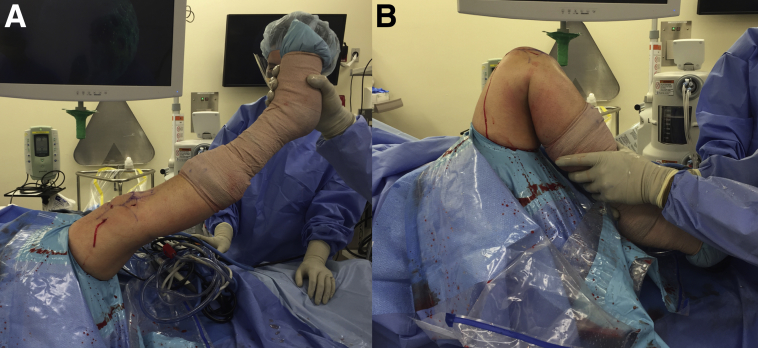
The patient is placed in the standard supine position with lateral thigh support. General anesthesia is used in all of our patients; however, regional epidural spinal anesthesia with an indwelling catheter may be an alternative for intraoperative and postoperative pain management. Preoperative ROM is recorded with the patient under anesthesia with photographs taken of knee flexion and extension (with the patient's consent) so that progress can be easily monitored postoperatively (Fig 1).
Fig 1.
The patient is in the supine position, and this is the right knee. Preoperative range of motion shows full extension (A) and 20° of flexion (B) with a mechanical block to range of motion.
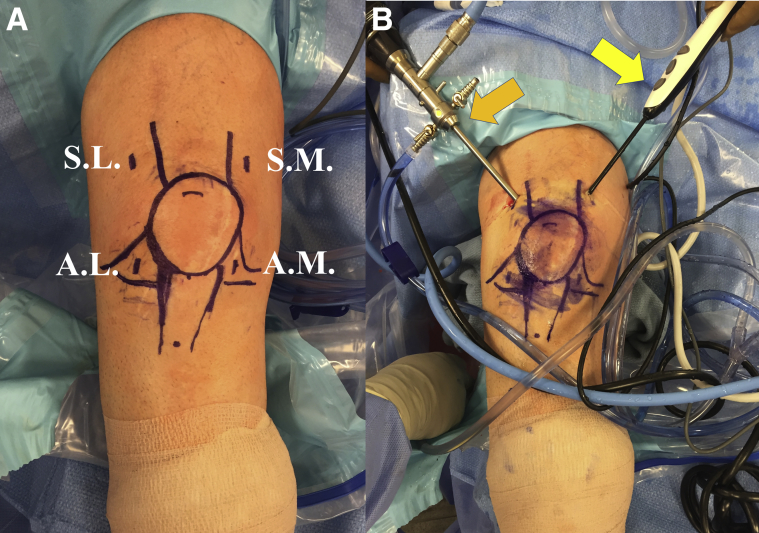
Arthroscopic Portal Positioning
The anterolateral (AL), anteromedial (AM), superomedial (SM), and superolateral (SL) portals are used for both the working portals and outflow cannula (Fig 2A). The AL and AM portals are established through the standard AL and AM soft spots (standard knee arthroscopy portal sites), whereas the SM portal is established 2 cm superior and 2 cm medial to the SM edge of the patella. The SL portal is established about 2 cm superior and 2 cm lateral to the SL edge of the patella. Both the SM and SL portals will serve as the viewing or working portals for this arthroscopic technique. These 2 portals are unrestricted and help with gaining unrestricted access to the medial or lateral retinaculum for arthroscopic release. In the senior author's experience, the first step in the arthroscopic lysis of adhesions will always start with the SL portal as the viewing portal and the SM portal as the working portal because of the limitations of knee flexion (Fig 2B). It is very difficult to start with the arthroscope in the traditional AL viewing portal when the knee is unable to be flexed past 90°. The posteromedial and posterolateral accessory portals are used only in cases in which there is a persistent extension deficit due to tight posterior capsular structures despite anterior interval as well as medial and lateral capsular release with MUA.
Fig 2.
The patient is in the supine position, and this is the right knee. (A) The arthroscopic viewing and working portals for the procedure are shown. (AL, anterolateral portal; AM, anteromedial portal; SL, superolateral portal; SM, superomedial portal.) (B) The arthroscope is inserted into the SL for viewing (orange arrow) with a radiofrequency device inserted into the superomedial working portal (yellow arrow).
Step-by-Step Approach
Debridement of Patellofemoral and Suprapatellar Compartments
A diagnostic arthroscopy using a standard 30° arthroscope (Smith & Nephew, Andover, MA) in the anterior compartment can be performed through the AL portal. However, if knee flexion is restricted to less than 60°, the viewing arthroscope should be inserted into the patellofemoral joint through the SL portal (viewing portal) and then the SM working portal is established with the knee in extension (Fig 2). To help visualize the intra-articular structures and aid with lysis of adhesions through capsular distension, 100 to 150 mL of saline solution can also be injected into the joint.
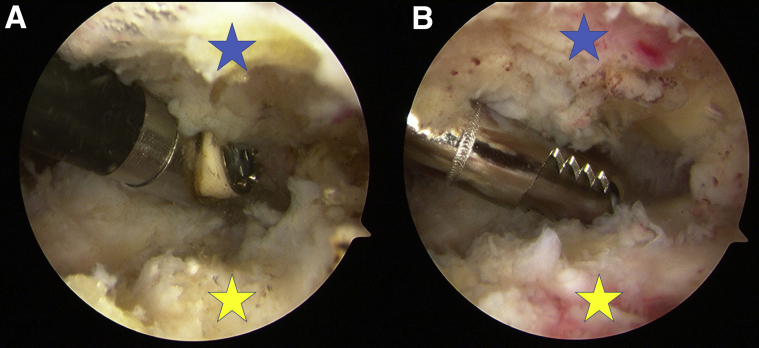
A standard arthroscopic shaver (4.5-mm Dyonics Incisor Plus Platinum; Smith & Nephew) and radiofrequency (RF) ablation device (Super TurboVac 90 Coblation wand; Smith & Nephew) are used to debride the patellofemoral joint and the suprapatellar pouch with the knee in extension, releasing all adhesions, hypertrophied synovium, and intra-articular bands (Fig 3). The deep quadriceps muscle bulk should be visualized to confirm that the releases are adequate. The suprapatellar pouch usually extends up to 3 cm proximal to the superior edge of the patella. Adhesions should be liberally released in the patellofemoral compartment to help with the patellar excursion.
Fig 3.
The patient is in the supine position, and this is the right knee. A 30° arthroscope is in the superolateral portal with the radiofrequency device in the superomedial portal. (A) Arthroscopic lysis of adhesions is performed in the patellofemoral pouch. (B) An arthroscopic shaver is inserted into the superomedial portal to debride the patellofemoral joint.
Medial and Lateral Gutter Synovectomy and Lysis of Adhesions
All adhesions in the medial and lateral parapatellar gutters should be cleared using the AL viewing portal and a combination of the shaver and ablator from the AM working portal (Fig 3). The inner aspect of the knee capsule is typically adhered to the medial and lateral aspects of the femoral condyle, and clearing this scarring helps patellar mobility on the trochlea.
Medial and Lateral Capsular Release
Lateral retinacular or capsular release is performed with the arthroscope in the SL portal and the RF device coming across the patellofemoral joint from the SM portal. The release is started laterally through the SM working portal and extends down distally, parallel to the patella. A complete lateral release is performed prior to switching the viewing portal to the SM location, and a medial retinacular or capsular release is performed arthroscopically through the SL working portal. This is extended inferiorly and medially, parallel to the patella. The senior author will shut off the pump and ablate any residual bleeding vessel from the capsular release before proceeding to the next step. After the medial and lateral capsular release, it is essential to perform a gentle MUA to gain more ROM in flexion so that the arthroscope can be placed in the AL portal for viewing. At least 70° to 80° of knee flexion is needed for the surgeon to place the scope in the AL portal and be able to visualize the notch.
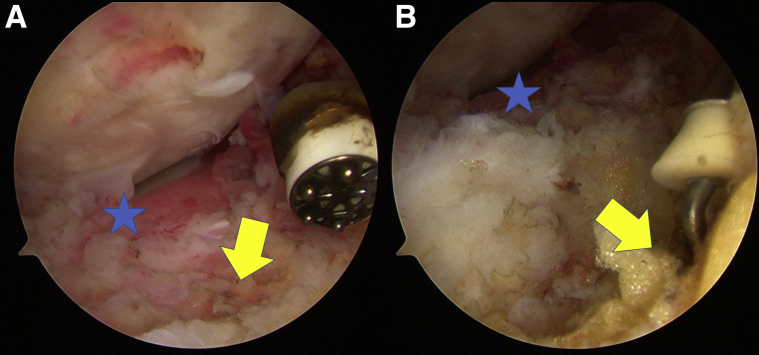
Anterior Interval Release
In cases of severe arthrofibrosis or deficits in knee flexion, it is important to release the anterior interval of the knee between the anterior tibial plateau and the patellar tendon. With the arthroscope in the AL viewing portal and the arthroscopic shaver in the AM portal, the hypertrophic scarred infrapatellar (Hoffa) fat pad and adhesions in the pretibial recess are released. This is a vascular area; therefore, a combination of the shaver and electrocautery should be used when excising adhesions in this region (Fig 4).
Fig 4.
The patient is in the supine position, and this is the right knee. (A) The arthroscope is in the anterolateral viewing portal with the radiofrequency (RF) device in the anteromedial (AM) portal. The tibial plateau (star) is seen here, and the anterior interval is labeled with an arrow. The RF device is inserted into the AM portal to start the anterior interval release. (B) With the same viewing and working portals, the hooked RF device is inserted into the AM portal to complete the anterior interval release, working from the medial to lateral direction and 2 cm under the tibial plateau.
A hooked RF device (Dyonics RF Hook; Smith & Nephew) or standard RF device is used to release the anterior interval between the tibia and the patellar tendon. The release should be performed from the medial to lateral direction and down 2 cm inferior to the tibial plateau surface (Fig 4B). The hooked RF device helps to easily dissect the scar and fat pad between the plane of the patellar tendon and the tibial plateau. The arthroscope is then switched to the AM portal, and the anterior interval release is completed at this time from the lateral to medial direction 2 cm below the plateau. It is essential to shut off the pump at this time to make sure there is no residual bleeding from this area.
Intercondylar Notch Examination and Debridement
After anterior interval release, the scar tissue in the joint is sequentially debrided, including the intercondylar notch and the medial and lateral femoral condyle, using a combination of the shaver and ablator. An arthroscopic burr is used for any bony overgrowths or spurs that may be encountered owing to the post-traumatic nature of these injuries. Care should be taken not to injure the articular cartilage or ligaments within the knee.
Manipulation Under Anesthesia
After complete lysis of adhesions in all 3 compartments, medial and lateral capsular release, and anterior interval release, gentle manipulation of the knee is performed (Fig 5). It is best to use the proximal tibia as the lever while gradually and progressively taking the knee through complete ROM in an effort to break up the adhesions and obtain maximal flexion. It is best to document this post-release ROM by taking intraoperative images (with the patient's consent), which can help with preoperative comparisons and help the patient set a target-oriented approach when pursuing PT.
Fig 5.
The patient is in the supine position, and this is the right knee. After the arthroscopic lysis of adhesions, medial and lateral capsular release, and anterior interval release, gentle manipulation under anesthesia is performed to break up the adhesions. Full extension (A) and 135° of flexion (B) are obtained in this patient with a very stiff preoperative knee.
Postoperative Care and Rehabilitation
Adequate analgesia is of prime importance to help the patient match postoperative clinical ROM with intraoperative knee motion. We advise sufficient use of oral pain medications (narcotics and anti-inflammatories) postoperatively. If regional anesthesia is used, use of the indwelling femoral nerve catheter can be continued for a few days for effective local analgesia. PT is started in the hospital on day 1, with the use of a continuous passive motion machine for the first 2 to 3 weeks. The senior author will typically admit these patients to the hospital for 1 to 2 days to work with the inpatient physical therapist prior to discharge. Formal outpatient PT along with home exercises is started at a frequency of 5 times a week for the initial 2 weeks, and the schedule is gradually decreased to 2 to 3 times per week over the next 2 months. It is essential to educate the patients on the importance of performing home stretching exercises, which will improve the success rate of this procedure.
Discussion
The estimated incidence of intra-articular fibrosis varies from 4% to 35%.6 It has been studied most extensively in patients after anterior cruciate ligament reconstruction but is also seen after trauma and total knee arthroplasty. The incidence of post-traumatic knee arthrofibrosis requiring surgical intervention has been reported to be as high as 14.5%, and it is most likely to occur in patients treated with external fixation.7
Management techniques for a stiff knee refractory to conservative treatment conventionally include MUA, open quadricepsplasty, and arthroscopic lysis of adhesions. Recent studies have documented the success of the latter procedure. Gittings et al.5 specifically looked at the results of arthroscopic lysis of adhesions in post-traumatic stiff knees treated with open reduction–internal fixation. They reported post-lysis intraoperative ROM improvement from an average of 72° immediately before surgery to 128° intraoperatively (78% improvement) and a sustained clinical improvement to mean ROM of 101° (35% improvement) at final follow-up. Furthermore, Kim and Joo4 studied the results of arthroscopic lysis of adhesions and found that among post-traumatic cases (43 of 68 total patients), an increase in ROM was seen from an average of about 70° preoperatively to 118° postoperatively at a mean final follow-up of 17.8 months.
The presented procedure has several advantages (Table 1). It is minimally invasive (unlike an open procedure such as quadricepsplasty), thus lowering the chance of postoperative wound infections and other incision-related complications and offering less morbidity and faster recovery. Patients can start active PT from postoperative day 1, minimizing the expected loss of ROM when comparing intraoperative ROM and 1-year postsurgical clinically sustained ROM.5, 8 The arthroscopic technique also allows for all-round release of adhesions that will provide greater patellar mobility and decrease the risk of fracture prior to MUA, especially in older patients with osteoporotic bone, compared with MUA performed alone. Moreover, this procedure provides an opportunity to directly inspect and evaluate intra-articular structures (ligaments, menisci, cartilage).
Table 1.
Advantages of Arthroscopic Surgical Technique
| The procedure is minimally invasive (arthroscopic) with small incisions and is cosmetically viable. |
| There is lower morbidity, a lower chance of wound complications, and a decreased overall surgical risk compared with open procedures (i.e., quadricepsplasty). |
| There is a lower chance of causing fracture (compared with MUA alone) in a stiff knee and osteoporotic bone. |
| The procedure provides the opportunity to inspect the intra-articular structures and treat lesions concomitantly without performing an open incision. |
| The patient can start aggressive PT from POD 1 and therefore start rehabilitation earlier and decrease the chance of recurrent stiffness. |
| The arthroscopic technique allows the surgeon to address all concomitant lesions within the knee. |
MUA, manipulation under anesthesia; POD, postoperative day; PT, physical therapy.
There are some drawbacks to this technique (Table 2). The procedure is technically demanding, requiring advanced arthroscopic expertise and accurate portal placement to attain complete lysis of adhesions. In severe cases, minimal flexion at the knee or extensive intercondylar notch scarring and fibrosis may present difficulty in accessing the knee joint in flexion. Thus, the senior author uses the SL and SM portals with the knee in extension as the first step in the procedure. Subsequently, medial and lateral retinacular or capsular releases are performed along with a gentle MUA to gain knee flexion, which allows the scope to be placed in the AL portal. If a posterior capsular release is warranted, advanced arthroscopic skills are required to establish posterior accessory portals and negotiate the arthroscope into the posterior compartment for arthroscopic release. There is also a risk of damaging the ligamentous or neurovascular structures. If the cause of stiffness has an extra-articular component, this surgical intervention may not suffice and might require an open quadricepsplasty and/or open posterior release. Finally, the results of this intervention are highly dependent on patient motivation and compliance in carrying out a rigorous formal PT protocol postoperatively.
Table 2.
Disadvantages of Technique
| The procedure is technically challenging, requiring expertise to achieve adequate intra-articular lysis and fibrotic release. |
| Use is restricted to post-traumatic intra-articular knee stiffness, and the expected results may not be provided when associated with extra-articular adhesions and/or scarring. These extra-articular causes cannot be addressed arthroscopically. |
| There is a chance of injury to the adjacent ligamentous and/or neurovascular structures, as well as cartilage, because of the tight intracapsular space with global fibrosis and adhesions. |
| Patient compliance, motivation, and enthusiasm required to pursue rigorous postoperative PT are essential to postoperative clinical success. |
PT, physical therapy.
There are certain pearls advocated by the senior author to help obtain optimal outcomes from this technique and achieve ideal postoperative results (Table 3). Limitations of this technique are listed in Table 4. The timing of surgical intervention is important. The best results are obtained when the procedure is performed within 6 to 7 months of the inciting event (ideally between 3 and 6 months), before there is chronic contracture of the adjacent musculature.4 Appropriate management of immediate postoperative pain with multimodal techniques is vital to decrease inflammation and muscle spasms and to prevent recurrent stiffness, which will also allow the patient to comply with PT exercises.
Table 3.
Preoperative and Intraoperative Pearls
| Preoperative |
| 1. The diagnosis of intra-articular arthrofibrosis should be supported by a thorough clinical examination and ancillary investigations to rule out other causes of knee stiffness (extra-articular). The best outcomes will be obtained only in this subset of patients. |
| 2. ROM restriction may occur in flexion (patellofemoral, suprapatellar, intercondylar, and/or anterior interval), extension (posterior capsule), or a combination of both. A detailed stepwise evaluation and systematic approach are important and should be planned preoperatively. |
| 3. Preoperative patient counseling should reinforce the importance of postoperative PT. |
| 4. Documenting preoperative and intraoperative ROM under anesthesia helps in monitoring patients' progress. It also helps patients set targets and work toward set goals. |
| Intraoperative |
| 1. In a knee that is severely stiff, the viewing portal should start in the superolateral location with the working portal in the superomedial location. |
| 2. Both medial and lateral capsular releases are performed first to allow a gentle MUA to gain knee flexion. The pump must be turned off to evaluate for bleeding in the retinacular area. |
| 3. Once knee flexion around 70° to 80° is obtained, the anterolateral portal is used for viewing and the anteromedial portal may be used as the working portal. |
| 4. Releasing the anterior interval and re-establishing the pretibial recess help patellar excursion and mobility. Use of the hooked RF device is ideal to achieve this. Release is performed from the medial to lateral direction between the tibial plateau and the patellar tendon about 2 cm below the tibial surface. It is essential to shut off the pump and evaluate for bleeding after the completion of the anterior interval release. |
| 5. Lysis of adhesions should be performed in all 3 compartments including the patellofemoral pouch. |
| 6. MUA should be performed after release, lysis of adhesions, and anterior interval release, and the proximal two-thirds of the tibia should be used as the primary lever to avoid intraoperative fracture. |
| 7. Posterior releases (arthroscopic or open) should be added whenever there is an extension deficit despite a complete anterior release with MUA. |
| 8. A combination of an arthroscopic shaver and RF electrocautery device is needed to achieve a bloodless intraoperative field. Closure should be preceded by dry arthroscopy to check and confirm complete hemostasis. |
| 9. Postoperative pain management with multiple modalities (regional anesthesia, short-acting opioids, and NSAIDs) will alleviate pain and muscle stiffness and help the patient continue with a scheduled aggressive rehabilitation protocol. |
| 10. The senior author prefers to admit the patient to the hospital for 1 to 2 days to work with the physical therapist right after surgery. Formal PT is started with 5 d/wk for the first 2 wk and then trending down to 2 to 3 times per week in 2 mo. |
MUA, manipulation under anesthesia; NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physical therapy; RF, radiofrequency; ROM, range of motion.
Table 4.
Pitfalls and Limitations
| Functional outcomes are dependent on the time lapse between index post-traumatic surgery and arthroscopic lysis of adhesions. The best results are obtained when the procedure is performed within 6-7 mo after the index operation. Therefore, time since first surgical procedure is a prognostic factor, and the expected results may not be provided in cases of chronic stiffness or regional muscle contracture. |
| Establishing the right expectations with the patient is very important. In the senior author's experience, intraoperative motion after MUA will always be higher than the final motion at the final follow-up. |
| In cases of severe knee stiffness, the patient will never obtain full knee ROM after surgery. A reasonable expectation is about 100° to 110° after surgery. |
| Inadequate pain management in the immediate postsurgical phase can hinder patient compliance in following an aggressive rehabilitation program. Postoperative pain management is important to help translate the intraoperative gain of ROM into a sustained clinical postoperative gain of motion. All efforts should be made to help decrease the chance of postoperative hemarthrosis, muscle spasms, and inflammation. |
MUA, manipulation under anesthesia; ROM, range of motion.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: X.L. receives equity and is on the editorial board of the Journal of Medical Insight. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic technique of lysis of adhesions, medial and lateral capsular release, and anterior interval release supplemented with subsequent intraoperative manipulation under anesthesia (MUA) for severe post-traumatic or postsurgical knee stiffness. The patient is in the supine position with lateral thigh support. This is the right knee with 4 arthroscopic portals used for this procedure: anterolateral (AL), anteromedial (AM), superomedial (SM), and superolateral (SL) portals. The AL and AM portals are established through the standard AL and AM soft spots (standard knee arthroscopy portal sites), whereas the SM portal is established 2 cm superior and 2 cm medial to the SM edge of the patella. The SL portal is established about 2 cm superior and 2 cm lateral to the SL edge of the patella. Both the SM and SL portals will serve as the viewing or working portals for this arthroscopic technique. These 2 portals are unrestricted and help with gaining unrestricted access to the medial or lateral retinaculum for arthroscopic release. The first step in the arthroscopic lysis of adhesions will typically start with the SL portal as the viewing portal and the SM portal as the working portal because of the limitations of knee flexion. It is very difficult to start with the arthroscope in the traditional AL viewing portal when the knee is unable to be flexed past 90°. The posteromedial and posterolateral accessory portals are used only in cases in which there is a persistent extension deficit due to tight posterior capsular structures despite anterior interval as well as medial and lateral capsular release with MUA. A standard arthroscopic shaver and radiofrequency (RF) ablation device are used to debride the patellofemoral joint and the suprapatellar pouch with the knee in extension, releasing all adhesions, hypertrophied synovium, and intra-articular bands. All adhesions in the medial and lateral parapatellar gutters should be cleared using the AL viewing portal and a combination of the shaver and ablator from the AM working portal. Medial and lateral retinacular or capsular release is performed with an RF device. After the release, it is essential to perform a gentle MUA to gain more range of motion (ROM) in flexion so that the arthroscope can be placed in the AL portal for viewing. At least 70° to 80° of knee flexion is needed for the surgeon to place the scope in the AL portal and be able to visualize the notch. Anterior interval release between the tibia and the patellar tendon is performed with the hooked RF device or standard RF device. The release should be performed from the medial to lateral direction and down 2 cm inferior to the tibial plateau surface. It is essential to shut off the pump at this time to make sure there is no residual bleeding from this area. After anterior interval release, the scar tissue in the joint is sequentially debrided, including the intercondylar notch and the medial and lateral femoral condyle, using a combination of the shaver and RF ablator. After complete lysis of adhesions in all 3 compartments, medial and lateral capsular release, and anterior interval release, gentle manipulation of the knee is performed. It is best to use the proximal tibia as the lever while gradually and progressively taking the knee through complete ROM in an effort to break up the adhesions and obtain maximal flexion. This patient's right knee regained full ROM after this arthroscopic procedure with intraoperative MUA.
References
- 1.Mariani P.P., Santori N., Rovere P., Della Rocca C., Adriani E. Histological and structural study of the adhesive tissue in knee fibroarthrosis: A clinical-pathological correlation. Arthroscopy. 1997;13:313–318. doi: 10.1016/s0749-8063(97)90027-x. [DOI] [PubMed] [Google Scholar]
- 2.Reider B., Belniak R.M., Preiskorn D. Arthroscopic arthrolysis for flexion contracture following intraarticular reconstruction of the anterior cruciate ligament. Arthroscopy. 1996;12:165–173. doi: 10.1016/s0749-8063(96)90006-7. [DOI] [PubMed] [Google Scholar]
- 3.Sprague N.F., O’Connor R.L., Fox J.M. Arthroscopic treatment of postoperative knee fibroarthrosis. Clin Orthop Relat Res. 1982;166:165–172. [PubMed] [Google Scholar]
- 4.Kim Y.M., Joo Y.B. Prognostic factors of arthroscopic adhesiolysis for arthrofibrosis of the knee. Knee Surg Relat Res. 2013;25:202–206. doi: 10.5792/ksrr.2013.25.4.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gittings D., Hesketh P., Dattilo J., Zgonis M., Kelly J., Mehta S. Arthroscopic lysis of adhesions improves knee range of motion after fixation of intra-articular fractures about the knee. Arch Orthop Trauma Surg. 2016;136:1631–1635. doi: 10.1007/s00402-016-2561-2. [DOI] [PubMed] [Google Scholar]
- 6.Lindenfeld T.N., Wojtvs E.M., Husain A. Surgical treatment of arthrofibrosis of the knee. Instr Course Lect. 2000;49:211–221. [PubMed] [Google Scholar]
- 7.Haller J.M., Holt D.C., McFadden M.L., Higgins T.F., Kubiak E.N. Arthrofibrosis of the knee following a fracture of the tibial plateau. Bone Joint J. 2015;97-B:109–114. doi: 10.1302/0301-620X.97B1.34195. [DOI] [PubMed] [Google Scholar]
- 8.Sassoon A.A., Adigweme O.O., Langford J., Koval K.J., Haidukewych G.J. Manipulation under anesthesia: A safe and effective treatment for posttraumatic arthrofibrosis of the knee. J Orthop Trauma. 2015;29:464–468. doi: 10.1097/BOT.0000000000000395. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic technique of lysis of adhesions, medial and lateral capsular release, and anterior interval release supplemented with subsequent intraoperative manipulation under anesthesia (MUA) for severe post-traumatic or postsurgical knee stiffness. The patient is in the supine position with lateral thigh support. This is the right knee with 4 arthroscopic portals used for this procedure: anterolateral (AL), anteromedial (AM), superomedial (SM), and superolateral (SL) portals. The AL and AM portals are established through the standard AL and AM soft spots (standard knee arthroscopy portal sites), whereas the SM portal is established 2 cm superior and 2 cm medial to the SM edge of the patella. The SL portal is established about 2 cm superior and 2 cm lateral to the SL edge of the patella. Both the SM and SL portals will serve as the viewing or working portals for this arthroscopic technique. These 2 portals are unrestricted and help with gaining unrestricted access to the medial or lateral retinaculum for arthroscopic release. The first step in the arthroscopic lysis of adhesions will typically start with the SL portal as the viewing portal and the SM portal as the working portal because of the limitations of knee flexion. It is very difficult to start with the arthroscope in the traditional AL viewing portal when the knee is unable to be flexed past 90°. The posteromedial and posterolateral accessory portals are used only in cases in which there is a persistent extension deficit due to tight posterior capsular structures despite anterior interval as well as medial and lateral capsular release with MUA. A standard arthroscopic shaver and radiofrequency (RF) ablation device are used to debride the patellofemoral joint and the suprapatellar pouch with the knee in extension, releasing all adhesions, hypertrophied synovium, and intra-articular bands. All adhesions in the medial and lateral parapatellar gutters should be cleared using the AL viewing portal and a combination of the shaver and ablator from the AM working portal. Medial and lateral retinacular or capsular release is performed with an RF device. After the release, it is essential to perform a gentle MUA to gain more range of motion (ROM) in flexion so that the arthroscope can be placed in the AL portal for viewing. At least 70° to 80° of knee flexion is needed for the surgeon to place the scope in the AL portal and be able to visualize the notch. Anterior interval release between the tibia and the patellar tendon is performed with the hooked RF device or standard RF device. The release should be performed from the medial to lateral direction and down 2 cm inferior to the tibial plateau surface. It is essential to shut off the pump at this time to make sure there is no residual bleeding from this area. After anterior interval release, the scar tissue in the joint is sequentially debrided, including the intercondylar notch and the medial and lateral femoral condyle, using a combination of the shaver and RF ablator. After complete lysis of adhesions in all 3 compartments, medial and lateral capsular release, and anterior interval release, gentle manipulation of the knee is performed. It is best to use the proximal tibia as the lever while gradually and progressively taking the knee through complete ROM in an effort to break up the adhesions and obtain maximal flexion. This patient's right knee regained full ROM after this arthroscopic procedure with intraoperative MUA.