Abstract
Early diagnosis and effective treatment to reduce mortality is the basis of pulmonary embolism. However, the diagnosis can be easily overlooked due to nonspecific clinical presentation. We present 9 cases of pulmonary embolism manifested by a symptom suggestive of an irritating cough due to viral upper respiratory tract infection (patients with no risk factors for PE). Pulmonary embolism should be considered in cases of irritating cough that does not respond to inhaler treatment, d-dimer positive and normal chest X-ray.
1. Introduction
Cough is often appeared by an upper respiratory viral infection and readily responds to bronchodilator therapy and anti-inflammatory. The differential diagnosis for unresponsive cough includes many other pulmonary disorders, or poorly controlled asthma [1]. The underlying etiology of cough is important in determining the diagnosis and treatment [3,4]. Physicians should maintain a high level of suspicion of PE even when complaints and signs are nonspecific [5]. Pulmonary embolism (PE) may overlook diagnosis because clinical symptoms and signs are nonspecific(6). (see Table 1, Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8, Fig. 9)
Table 1.
Characteristics of patients with Pulmonary Thromboembolism.
| Patient No | Age (yr) | D-imer(243) | Sat% | Pulse |
|---|---|---|---|---|
| 1 | 71 | 531 | 96 | 90 |
| 2 | 74 | 652 | 98 | 71 |
| 3 | 67 | 342 | 97 | 81 |
| 4 | 51 | 246 | 96 | 87 |
| 5 | 27 | 454 | 98 | 105 |
| 6 | 22 | 347 | 97 | 82 |
| 7 | 64 | 284 | 98 | 76 |
| 8 | 73 | 301 | 94 | 72 |
| 9 | 50 | 280 | 97 | 84 |
Fig. 1.
71-year-old woman with cirrhosis. CT pulmonary angiography shows pulmonary emboli with abrupt caliber change in bilateral lower lobe artery (arrows).
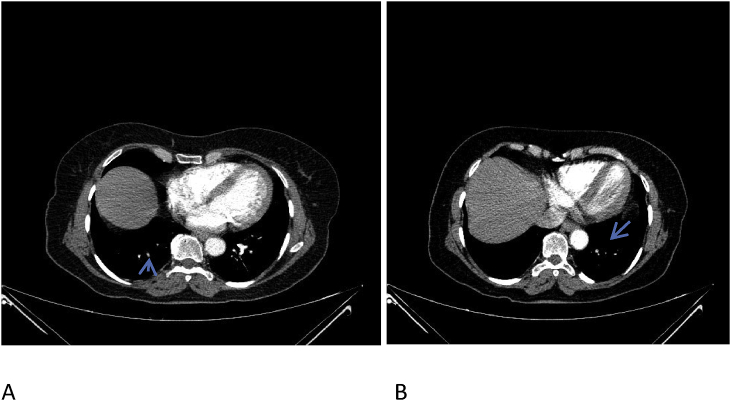
Fig. 2.
—74-year-old man with 6 months of persistent dry cough and hypothyroidism. CT pulmonary angiography shows pulmonary emboli with abrupt caliber change in right lower lobe artery (arrow in A and B).
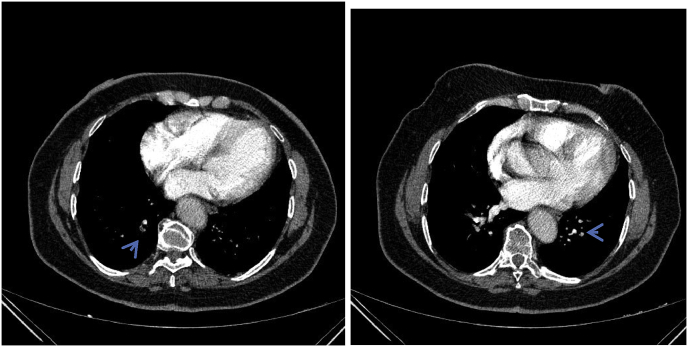
Fig. 3.
—67-year-old woman with 1 months of dry cough at night and varicose veins in legs. CT pulmonary angiography shows pulmonary emboli with obliteration in bilateral lower lobe artery (arrows in A and B).
Fig. 4.
—51-year-old man with 1 months of dry awakening cough. CT pulmonary angiography shows pulmonary emboli with obliteration in bilateral lower lobe artery (arrows in A and B).
Fig. 5.
—27-year-old woman with 1 year of all-day continuing cough, two and a half years ago traffic accident with fractures. CT pulmonary angiography shows pulmonary emboli in bilateral lower lobe artery (arrows).
Fig. 6.
—22-year-old man with 3.5 months of dry awakening cough and 4 months ago tonsillar operation. CT pulmonary angiography shows pulmonary emboli with obliteration in left lower lobe artery(arrow).
Fig. 7.
—64-year-old woman with two weeks of all-day continuing cough. CT pulmonary angiography shows pulmonary embolism with band in A, the parenchymal infiltration in B and abrupt caliber change in C in lower lobe artery (arrows).
Fig. 8.
—73-year-old woman with two weeks of all-day continuing cough. CT pulmonary angiography shows pulmonary emboli in bilateral lower lobe artery (arrows).
Fig. 9.
—50-year-old woman with two weeks of all-day continuing cough. CT pulmonary angiography shows pulmonary emboli in bilateral lower lobe artery (arrows).
2. Case series
We present 9 case of pulmonary embolism with cough as the sole presenting symptom. Cough of the cases continued between 1 month and 12 months. None of them had leg swelling and pain on calf palpation. They refused dyspnea, chest pain, or palpitations. Their signs and physical examination results were normal.
Their blood test results were within normal limits. Chest x-rays were normal. There are no cases previous report in the literature of troublesome cough as the sole presenting symptom of a verified pulmonary embolism. Because d-dimer is positive and the inhaler does not respond to treatment, the patient was sent for a contrast-enhanced chest tomography. These indicated left and right lower lobar pulmonary emboli (Figure). The patient was started on heparin and transitioned to riveroxaban. The patient reported that cough of their subsided 7–15 days after anticoagulation was started during follow-up.
3. Discussion
Pulmonary embolism among the uncommon causes of cough as the sole presenting symptom is the important clinical problem. If a patient has shortness of breath, high heart rate, or chest pain, this may be a PE. However, the diagnosis of pulmonary embolism is difficult because it has different presenting symptoms. Cough is the major or presenting symptom in nonpulmonary disorders and many uncommon pulmonary [2]. A strong doubt index is important to consider and diagnose the uncommon causes of cough [2]. The diagnosis of acute PE is among the most challenging problems encountered in clinical practice [6]. Present cases demonstrate that pulmonary embolism can only present as troublesome cough, which is currently not a noticeable symptom of this entity. Pulmonary embolism should be considered in the differential diagnosis of troublesome cough cases with normal chest X-ray and not responding to inhaled steroid and β2 agonist treatment. The mechanism of cough due to pulmonary embolism is not well known. It is likely that stimulation of pressure receptors in pulmonary vessels or right atrial or C-fibers in the pulmonary vessels will produce cough beyond causing dyspnea, which is associated with pulmonary embolism [7].
Pulmonary embolism should be considered in cases of irritating cough that does not respond to inhaler treatment, d-dimer positive and normal chest X-ray. Thus, early diagnosis of the pulmonary embolism is very important, and may prevent mortality via effective treatment.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2019.100861.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ricketti P.A., Ricketti A.J., Cleri D.J., Seelagy M., Unkle D.W., Vernaleo J.R. A 41-year-old male with cough, wheeze, and dyspnea poorly responsive to asthma therapy. Allergy Asthma Proc. 2010;31(4):355–358. doi: 10.2500/aap.2010.31.3344. [DOI] [PubMed] [Google Scholar]
- 2.Prakash U.B.S. Uncommon causes of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1 Suppl):206S–219S. doi: 10.1378/chest.129.1_suppl.206S. [DOI] [PubMed] [Google Scholar]
- 3.Stein P.D., Willis P.W., DeMets D.L. History and physical examination in acute pulmonary embolism in patients without preexisting cardiac or pulmonary disease. Am. J. Cardiol. 1981;47:218–223. doi: 10.1016/0002-9149(81)90388-x. [DOI] [PubMed] [Google Scholar]
- 4.Bĕlohlávek J., Dytrych V., Linhart A. Pulmonary embolism, part I: epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism. Exp. Clin. Cardiol. 2013;18(2):129–138. [PMC free article] [PubMed] [Google Scholar]
- 5.Lee D.Z., Whittaker M., Al-Mohammad A. An unusual presentation of pulmonary embolism. BMJ Case Rep. 2012 8:2012. doi: 10.1136/bcr-2012-006210. pii: bcr2012006210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang S.Y., Chen H., Di L.G. Caution for acute submassive pulmonary embolism with syncope as initial symptom: a case report. J. Thorac. Dis. 2014;6(10):E212–E216. doi: 10.3978/j.issn.2072-1439.2014.08.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manning H.L., Schwartzstein R.M. Pathophysiology of dyspnea. N. Engl. J. Med. 1995 7;333(23):1547–1553. doi: 10.1056/NEJM199512073332307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.