Abstract
Ischemic stroke is a leading cause of death and disability throughout the world and is both preventable and treatable. This review focuses on the treatment of the most severe form of ischemic stroke, namely large-vessel ischemic stroke, using endovascular techniques. Such therapies were proven effective in 2015. These therapies are among the most beneficial surgical therapies ever subjected to randomized clinical trials. Recent research has explored treating patients up to 24 h following the onset of stroke using advanced imaging techniques to select patients with brain tissue still at risk. These new findings suggest there exists a tissue clock rather than a time clock when selecting patients for therapy. Stroke systems throughout the world are now embracing endovascular stroke therapy. Improving regional stroke systems of care and expanding eligibility for patients are a major focus of current research.
Electronic supplementary material
The online version of this article (10.1007/s13311-019-00724-5) contains supplementary material, which is available to authorized users.
Key Words: Thrombectomy, large-vessel stroke, ischemic penumbra, systems of care, penumbral imaging
Burden of Ischemic Stroke
Stroke is the 5th leading cause of death and the most common cause for disability in the USA [1]. Approximately 1 in 20 Americans die from stroke, with an annual cost of over $34 billion in health costs alone. Stroke is the leading cause of death in China and the second leading of cause of death worldwide and will likely rise in incidence as life expectancy increases.
Stroke is the sudden onset of a neurological deficit produced by a vascular cause. Depending on geography and ethnicity, ischemic strokes comprise nearly 85% of all strokes while 15% are due to hemorrhage into the brain parenchyma or subarachnoid space. Ischemic strokes are best classified as caused by small-vessel or large-vessel occlusions. Small-vessel strokes—also referred to as lacunar strokes—are due to occlusion of small, typically < 0.5-mm-sized vessels, while large-vessel occlusion (LVO) stroke is caused by blockage of 1- to 4-mm-sized vessels. LVO strokes typically involve the intracranial carotid terminus (ICA-T), the proximal middle cerebral artery (MCA, M1 branch), secondary or tertiary branches of the MCA (M2 and M3 branches), the anterior cerebral artery (ACA), the basilar artery (BA), and the posterior cerebral artery (PCA).
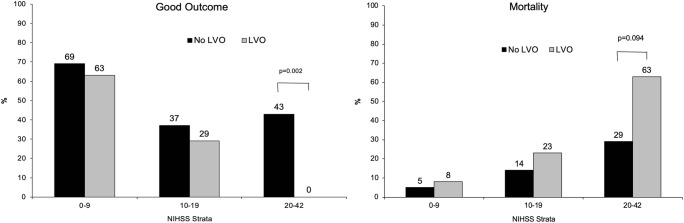
The clinical outcome following acute ischemic stroke (AIS) depends mostly on age, stroke severity, and the blood vessel(s) involved [2, 3]. The odds of a poor outcome are most dependent on age, with a year of life predicting a 5% less odds of a good outcome [3]. Stroke severity is best classified by the National Institutes of Health Stroke Scale (NIHSS) score that ranges from 0 to 42, with 0 being normal and 42 moribund. Minor stokes (NIHSS, 0-9), moderate strokes (NIHSS, 10-19), and severe strokes (NIHSS, 20 or higher) predict the probability of a good clinical outcome and mortality monotonically. The presence of LVO modifies this prediction significantly as shown in the analysis of a large cohort of stroke patients studied by CT and CT angiography (CTA). As shown in Fig. 1, no patient with LVO and NIHSS ≥ 20 had a good clinical outcome and 63% died, while mild stroke patients did well regardless of the size of the vessel [2].
Fig. 1.
Clinical outcomes of patients based on blood vessel size. Some patients were treated with IV tPA but did not receive endovascular treatment [2].
Time Dependency for Brain Infarction
Graded reduction in cerebral blood flow to values on an average of 16 to 18 ml/100 g/min is associated with neuronal depolarization and synaptic transmission failure [4]. Brain tissue sustaining this level of perfusion may survive for long periods. Long-term experiments in primate brain have not been performed, but recent human data of thrombectomy (mechanical removal of a clot from the occluded intracranial vessel) shows that this process may evolve over many hours and perhaps days if adequate collateral flow is maintained. Levels lower than this threshold will produce infarct at increasing rate depending on the magnitude of blood flow reduction. Focal ischemia of the brain (as is the case with AIS) is to be distinguished from global ischemia (cardiac arrest) in that blood flow to brain tissue rarely goes to zero for any brain region, even the tissue at the core of the brain infarct. Because of this important detail, brain tissue in AIS can survive substantially longer allowing one to intervene with revascularization therapies (thrombolysis and mechanical thrombectomy). In contrast, global ischemia for more than 10 to 20 min causes significant brain tissue death principally by apoptotic pathways.
The ischemic penumbra is a region within brain tissue where cerebral perfusion is lowered but not low enough to cause immediate infarction, while the umbra, or infarct core, is the tissue that has already infarcted [5]. The size of the core and penumbra is time dependent [6, 7]. Several lines of evidence show that if the occluded cerebral vessel remains occluded and all other physiological processes remain constant, the volume of core infraction will expand centripetally to consume the penumbra [8]. This process likely involves successive waves of cortical spreading depression where metabolic demand temporarily outstrips supply, causing epochs of expanding tissue necrosis [9, 10]. The rate of this process is likely slower than 24 h based on new thrombectomy trials (see below). Core infarcts are not salvageable with acute stroke therapies, but prevention of penumbral tissue infarction is mitigated with reperfusion therapies. Salvage of penumbral tissue is the chief goal in revascularization therapy and medical management.
Treating Acute Ischemic Stroke
Restoring cerebral blood flow quickly is the focus of acute stroke treatment. Although improving perfusion with blood pressure augmentation or changing blood rheology have been proposed and used in some circumstances, the evidence basis for such strategies is lacking and not part of routine care. Revascularization therapies, on the other hand, are the only proven therapies to mitigate brain tissue damage from AIS. Two methods have proven effective: administration of intravenous (IV) plasminogen activators (PAs) to lyse the clot, and mechanical thrombectomy (MT) where the clot is physically removed. Tissue plasminogen activator (tPA) is produced and secreted by endothelial cells and a wide array of brain tissue cells as well (for review, see [11]). As a serine protease, tPA binds to circulating plasminogen and converts it to plasmin. Circulating plasmin degrades fibrin within the clot by producing a systemic fibrinolytic state. Any intraluminal clot is the target of plasmin, and if sufficient quantities are present, clot lysis ensures recanalization of the blocked cerebral vessel.
Ischemic stroke responds favorably to administration of IV tPA if given within 4.5 h of stroke symptom onset [12–14]. In a meta-analysis of over 6500 randomized patients [13], among patients treated within 3 h of symptom onset, 33% had a good outcome compared to 23% of placebo-treated patients (OR, 1.75; 95% CI, 1.35-2.27). In the 3- to 4.5-h windows, 35% of tPA-treated patients compared to 30% of placebo-treated patients had a good outcome (OR, 1.26; 95% CI, 1.05-1.51). After 4.5 h, IV tPA was ineffective. Good outcome for these trials was considered dichotomous with a modified Rankin Scale (mRS) score of 0 to 1 versus a mRS score of 2 to 6. A mRS score of 0 is neurologically normal, 1 is with focal neurological deficit but no disability, 2 is with disability but can walk unaided, 3 requires gait assistance, 4 is wheelchair bound, 5 is bed bound, and 6 is death. Clinical outcome worsens the longer IV t-PA is started, and IV tPA becomes harmful following 4.5 h of ischemia due to intracerebral hemorrhage. On balance, clinical outcomes are improved regardless of age and stroke severity despite the risk of death and disability from intracerebral hemorrhage [13]. This “time clock” determines IVtPA eligibility in clinical practice. Many patients awaken with stroke so are unable to report when their symptoms began precluding IV tPA treatment. The standard and conservative definition of time of onset is when the patient was last known to be well. With the narrow time window for IV tPA, patients who awaken with stroke symptoms rarely receive IV tPA. However, recent data using IV tPA in patients with diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR) mismatch indicate that IV tPA eligibility may be extended in certain circumstances [15]. This mismatch exploits the time dependency how each MRI sequence reports ischemia. DWI becomes positive within minutes of ischemia while it takes hours for FLAIR signals to become positive. Patients who have a positive DW image but normal FLAIR within the same brain region are likely to have had recent stroke, and in these circumstances, IV tPA appears safe.
Beginning with the seminal publication of the NIH-sponsored trial of IV tPA efficacy in 1995 [12], IV tPA became the first proven treatment for AIS. However, it was widely recognized that LVO responds less well to IV tPA compared to small-vessel stroke. Tissue plasminogen activator needs to bind plasminogen to produce thrombolysis, but plasminogen levels inside the clot are substantially lower than in serum. The systemic thrombolytic state induced by IV tPA can only enzymatically degrade clot from the proximal and distal clot surfaces. Since LVO clots have substantially less surface area in contact with the systemic circulation than do small-vessel occlusions (considering the volume of clot), plasminogen activators should perform less well with LVO stroke than small-vessel stroke. In the NINDS trial, small-vessel strokes patients had good outcomes 47% of the time, while large-vessel thrombotic and cardioembolic strokes fared 33% and 29% respectively [12]. Although the LVO strokes did better with IV tPA, outcomes were overall poor. IV tPA only opens M1 occlusion about 18% of the time [16].
During these early trials, there was debate among stroke investigators whether the best approach for treating LVO was to use plasminogen activators intravenously or intra-arterially [17, 18]. Based on small case series, intra-arterial (IA) plasminogen activator delivery had been reported and looked promising. The first Prolyse in Acute Cerebral Thromboembolism (PROACT I) [19] and second PROACT (PROACT II) [20] trials were designed to study such IA plasminogen activator therapy in a homogenous population of patients with M1 occlusions. Prolyse (also called pro-urokinase) is a glycosylated 411-amino acid single-chain proenzyme precursor of urokinase and is rapidly hydrolyzed in vivo when delivered via catheter. It has a short half-life so when delivered by catheter into the intracranial clot, the systemic risks of hemorrhage should be minimized. PROACT I randomized patients to IA pro-urokinase versus intra-arterial saline. Showing significant recanalization efficacy of 58% versus 14%, investigators designed the PROACT II as a pivotal phase III trial of clinical efficacy. Patients were randomized to IA pro-urokinase (a plasminogen activator) versus medical therapy (IV heparin) in a 2:1 ratio. IA pro-urokinase opened vessels 66% of the time versus 18% in medical therapy, and a good clinical outcome was seen in 40% compared to 25%. In these studies, a good clinical outcome was more broadly defined as mRS 0 to 2, rather than mRS 0 to 1 used in the IV tPA trials. Intracerebral hemorrhage was higher in this cohort than in patients treated with IV tPA; however, like the experience with IV tPA, this complication was uncommon enough that it did not overwhelm to positive benefits of recanalization. In 1999, this trial provided the first randomized evidence that opening large intracranial vessels within 8 h improved clinical outcomes. These trials also established the time windows of 6 h to treatment initiation and 8 h to treatment end (IA infusion lasted 2 h), as well as the mRS 0 to 2 endpoints at 3 months. All subsequent trials through 2015 were designed using this time window and primary outcome.
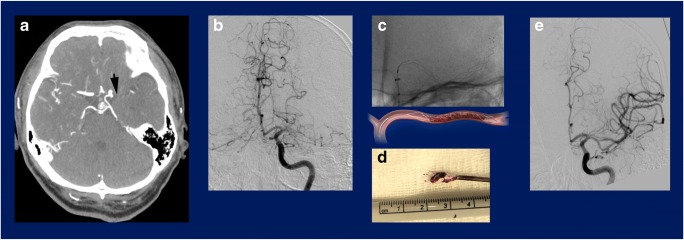
MT was conceived as an improved strategy over IA plasminogen activators principally because it would not raise the risk of intracerebral hemorrhage caused by a plasminogen activator (Fig. 2). The FDA had previously approved a corkscrew-like device invented at UCLA for use in retrieving errant coils placed during intracranial aneurysm embolization. The inventor began using the device off-label for MT and convinced others that the device could safely open LVOs. The rights to the device were licensed by industry, and the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial was initiated to investigate the safety and recanalization efficacy of this device in a single-armed prospective trial [21]. The device opened 48% of intracranial occlusions and, when compared to the historical control of the PROACT II trial, was cleared by the FDA as the first mechanical device for use in AIS in 2005. This was not without controversy, principally because of the high mortality among treated patients and the fact that the trial was not randomized [22, 23]. Nonetheless, the device and 2 subsequent families of devices were rapidly approved with better efficacy [24, 25].
Fig. 2.
Illustration of mechanical thrombectomy. (a) CTA of a patient with a left middle cerebral artery (MCA) occlusion (arrow). (b) Anterior-posterior (AP) digital subtraction angiogram (DSA) of the left internal carotid artery performed 21 min after the CTA, confirming the left MCA occlusion. (c) AP fluoroscopic view showing a suction catheter in the intracranial internal carotid artery with stent deployed through the MCA clot; below is a cartoon of the anatomy drawn to scale of the image in (c). (d) Photograph of the stent/suction catheter removed from the brain, revealing clot engaged in the stent interstices. (e) AP DSA of the left internal carotid artery, confirming complete recanalization of the left MCA. The procedure time was 35 min from groin puncture to restoration of blood flow.
The first randomized trials of MT in AIS concluded no benefit in 2013, largely because of trial design and use of less effective MT devices. The first was the Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy (MR RESCUE) trial whereby patients with radiographic LVO who were not IV tPA candidates were randomized to thrombectomy with the MERCI device and medical therapy [26]. The trial was designed to select patients with ischemic penumbra using the mismatch concept identified on perfusion imaging (more later). The trial recruited slowly because of the challenges in obtaining perfusion imaging at the time, and many patients were treated with the open-label MERCI device outside of the trial. This led to older patients with more severe strokes being randomized. Overall, only 118 patients were studied, and despite achieving a recanalization rate of 67%, there was no difference in outcomes at 90 days. The second major trial was the Interventional Management of Stroke (IMS) III trial [27]. This was a trial lasting 6 years that randomized patients with moderate to severe stroke to IV tPA versus IV tPA followed by endovascular stroke treatment (MT). This pragmatic trial focused on whether MT of any type was beneficial. The trial was stopped early for futility, and in the final analysis, the primary outcome of clinical benefit at 90 days was neutral (40.8% and 38.7% good clinical outcome, MT vs IV tPA alone). In retrospect, this trial likely failed for 2 main reasons. The first is that many of the patients were selected based on their NIHSS rather than proving that they had an LVO. This was because CTA was not in routine use until about 2/3 the way through the trial to properly screen for eligibility. Twenty percent of patients who were randomized to MT failed to have LVOs when they arrived in the angiography suite or the LVO was inaccessible. This diluted the treatment effect and compromised the study power. In a subgroup analysis, including only patients who had an LVO on CTA prior to randomization, the MT was superior to medical therapy. The second reason for failure was the relatively lower efficacy of the MERCI retriever in opening vessels compared to later devices. The impact of these 2 negative trials caused MT to decline dramatically for 2 years.
Endovascular surgeons had realized around the time that an LVO can be opened simply by stenting open the vessel. Later, investigators learned that if the stent was not detached but pulled back, an embolic clot could be easily removed [28–30]. Two major “stent-trievers” were designed to enhance clot capture and strengthen the connections between the stent wire and the stent itself. One of these devices was proven more effective in a randomized trial against prior devices [24]. Six randomized trials were launched to test the clinical efficacy of these more effective devices. Important to the design of these 6 trials was the requirement that all patients had a CTA or MRA documenting an LVO prior to randomization, thus increasing the study power compared to the IMS III trial. The first trial to complete and report its results was the Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN) [31]. This European trial randomized 500 patients within 6 h of stroke symptom onset with anterior circulation LVO to MT versus the best medical therapy. Overall, 33% of MT cases had a good outcome compared with 19% of medically treated patients (OR, 1.67; 95% CI, 1.21-2.30). Immediately, the 4 other ongoing trials of similar design halted enrollment and all met their primary endpoint with as few as 70 randomized patients.
The analysis of the pooled MT trials of 2015 (MR CLEAN, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) [32], Randomized Trial of Revascularization with Solitaire FR Device Versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting within Eight Hours of Symptom Onset (REVASCAT) [33], Solitaire with the Intention for Thrombectomy as Primary Endovascular Treatment for Acute Ischemic Stroke (SWIFT PRIME) [34], and Extending the Time for Thrombolysis in Emergency Neurological Deficits — Intra-Arterial (EXTEND IA) [35]) by the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaborators included the primary data of 1287 patients from these 5 trials. This meta-analysis showed that MT was associated with a 46% chance of a good outcome compared to 26.5% (OR, 2.49; 95% CI, 1.76-3.53; p < 0.0001) [36]. This means that for every 2.6 patients treated, 1 patient will have their disability reduced by 1 point on the mRS. Stated otherwise, 1 in 5 patients treated will have a good outcome when otherwise they would be disabled. Treatment was beneficial regardless of age or baseline stroke severity. Patient selection varied in each trial somewhat, but considering that 5 independent trials all met their endpoint (and a 6th trial later [37]) confirms MT efficacy. At the international stroke conference in February 2015, a notable investigator stated that “the standard of care of large vessel stroke changes world-wide today.” MT is among the most highly effective surgical therapies for any disease ever tested in a randomized fashion.
Time to Thrombectomy and Perfusion Imaging
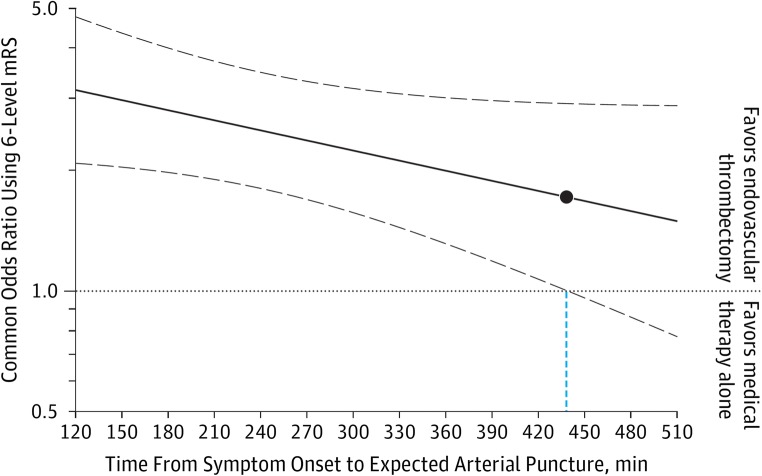
The HERMES collaboration also showed that clinical outcome depends on time to MT [38]. Figure 3 shows the odds of improved outcome over time. Using the lower 95% CI of these data, significant efficacy is lost around 440 min (7.3 h) with the confidence interval widening around this time. Because of trial eligibility, fewer patients were observed in the 8-h time window compared to earlier. This supports the concept of a time clock for clinical efficacy for MT and confirms animal models of stroke showing a clear time dependency to tissue infarction [4]. However, the wider time frame is remarkable as most animal models of MCAO show completed strokes within a few hours.
Fig. 3.
Time dependency of clinical outcome from mechanical thrombectomy. The solid line is the odds ratio of improved clinical outcome and the dashed lines are the 95% confidence intervals for that estimate. The solid circle indicates the point beyond which benefit is uncertain. Reproduced with permission [38].
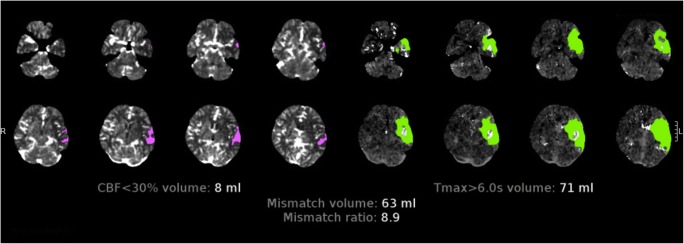
The HERMES studies all used some form of angiography to select patients for treatment, and a subset employed some form of perfusion imaging as well. Perfusion imaging is a technique to identify patients who have brain tissue at risk of subsequent infarction and, therefore, more likely to benefit from revascularization therapy (Fig. 4). It is accomplished by performing repeated cross-sectional images of the brain during the administration of an IV contrast infusion. MR perfusion (MRP) employs administration of gadolinium that changes MR susceptibility as it passes in and out of the brain. CT perfusion (CTP) uses iodinated IV contrast that increases brain radiopacity in an analogous fashion. MRP is the best studied and provides the advantage that DWI predicts death of cerebral tissue accurately and, therefore, is the gold standard to image the ischemic core of tissue. CTP utilizes brain regions below a certain cerebral blood flow threshold to define the core infarct. In most clinical scenarios, CTP core infarct estimation is accurate but can be falsely positive depending on when the imaging is performed relative to the onset of tissue ischemia and if there is a chronic infarct within the reported core. However, CTP is significantly easier to perform and is more widely available. Following estimation of the core infarct, MRP and CTP use the kinetics of tracer wash-in and wash-out to estimate the brain tissue at risk of subsequent infarction. The region of hypoperfusion but not within the core infarct is termed the ischemic penumbra. A patient with a left M1 occlusion who underwent CTP is shown in Fig. 4. Perfusion imaging reports a small region of relative CBF reduction totaling 8 ml of the brain, yet 71 ml of the brain that is hypoperfused, providing an estimate of 63 ml of the ischemic penumbra. This patient exhibits “target-mismatch” where the volume of underperfused brain far exceeds the volume of infarcted tissue.
Fig. 4.
Illustration of CT Perfusion (CTP) imaging for a patient with an acute left MCA stroke. This shows a small area of decreased cerebral blood flow (CBF, 8 ml) and a larger volume of perfusion delay (71 ml). This patient has a 63 ml volume of mismatch. The region of low CBF is predictive of the brain that is irreversibly injured while the region of perfusion delay is predictive of the region of the brain at risk of infarction if the left MCA is not opened. CTP is not as accurate at predicting core infarct as MRI DWI adding caveats to interpretation; however, CTP is preferred due to ease and patient tolerance.
Perfusion imaging allows testing the hypothesis that patients with LVO and no ischemic penumbra likely will not benefit from revascularization, while patients with LVO and a sizable ischemic penumbra would be expected to benefit from revascularization. If true, the concept of a “tissue clock” rather than a “time clock” relied upon for IV tPA treatment may be a better selection criterion for intervention. This concept that penumbral imaging can identify patients who benefit from MT was supported by the Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke (DEFUSE) 2 trial [39]. This was an observational prospective cohort study whereby LVO patients with cerebral ischemia of up to 12-h duration had baseline perfusion imaging and underwent MT. Custom software calculated the core infract volume and the volume at risk and compared outcomes of patient with and without penumbral tissue (see Fig. 4). Patients with favorable penumbral imaging and successful MT had substantially smaller infarct growth and better clinical outcome, while patients without favorable imaging did not benefit from MT.
Definitive validation of the tissue clock came from 2 recent randomized trials: the DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention with Trevo (DAWN) [40] and the DEFUSE 3 [41] trials. The DAWN trial used CTP or MRP to select patients with small core infarcts but a larger volume of the brain at risk based on various thresholds to define the penumbra up to 24 h following the onset of stroke. The inclusion criteria were complex. Based on prior studies showing that younger patients could tolerate larger core infarcts, both age and CTP results were used to determine eligibility within 3 groups. Patients were randomized 1:1 for MT versus best medical therapy. The trial had an adaptive design and a planned interim analysis to trigger adaption. At this first interim step with only 206 patients enrolled, the trial was stopped by the data safety management committee for efficacy defined by a preplanned charter. Patients treated with MT had a 49% chance of good outcome, while medial therapy afforded a 13% good outcome. The median time from onset to treatment was 13.6 h. The DEFUSE 3 trial had similar design and used MRP or CTP imaging, a time window of 6 to 16 h, and more inclusive perfusion criteria for patient selection. This trial was ongoing when the DAWN trial was stopped, prompting the DEFUSE 3 investigators to halt enrollment and examine their data. Despite being far below planned enrollment, patients treated in the DEFUSE 3 trial enjoyed markedly better outcomes. A total of 182 patients were randomized. Patients treated with MT had a significantly higher proportion with a good outcome compared to medical therapy alone (48% vs 17%, p < 0.001), and mortality was reduced from 26 to 14% (marginally significant OR, 0.55; 95% CI, 0.30-1.02).
Comparing the results of the DAWN and DEFUSE 3 trials to the HERMES collaboration results, the proportion of good outcome is similar (48-49% vs 46%). The surprise was the significantly lower proportion of good outcomes in the control arms. In the HERMES collaboration, 25% of control arm patients did well, while in the DAWN and DEFUSE 3 trials, only 13 to 17% did well. The explanation of this is complex [41]. All of the patients in the DAWN and DEFUSE 3 trials were not treated with IV tPA while 85% of the HERMES collaboration were tPA treated. No data yet exist to test whether IV tPA pretreatment is helpful; by definition, all patients in these trials had persistent LVO at the time of MT, and there was no association of recanalization following MT with IV tPA pretreatment.
The phenomenon of progressive cerebral infarction over hours to days can be termed “ischemic creep” and is likely due to progressive loss of collateral flow to the ischemic penumbra. DAWN and DEFUSE 3 were the first clinical trials to document the existence of this clinical phenomenon. Given that this subgroup is readily definable, further therapies might address how blood pressure augmentation, volume expansion, changes in blood rheology, and neuroprotection might be helpful to mitigate stroke progression.
Systems of Care
Mechanical thrombectomy for AIS is now common practice throughout the developed world. Now that recanalization rates are high with current-generation thrombectomy devices, the most important factor that affects outcome is access to care. MT is expensive primarily because of the cost of angiography equipment, thrombectomy devices, and payments to physicians who require extensive training to safely perform the procedures. Using accreditation data from the USA, there are 191 Joint Commission–accredited centers to perform MT (comprehensive stroke center (CSC) or thrombectomy-ready centers) and 1286 primary stroke centers (PSCs) [42]. Most US CSCs are concentrated in major metropolitan centers [43], as are PSCs, leaving community hospitals with no advanced capability to treat AIS. In other countries with a more programmed approach to stroke care (principally, Europe), CSCs and PSCs are more evenly distributed so transport times are more homogenous.
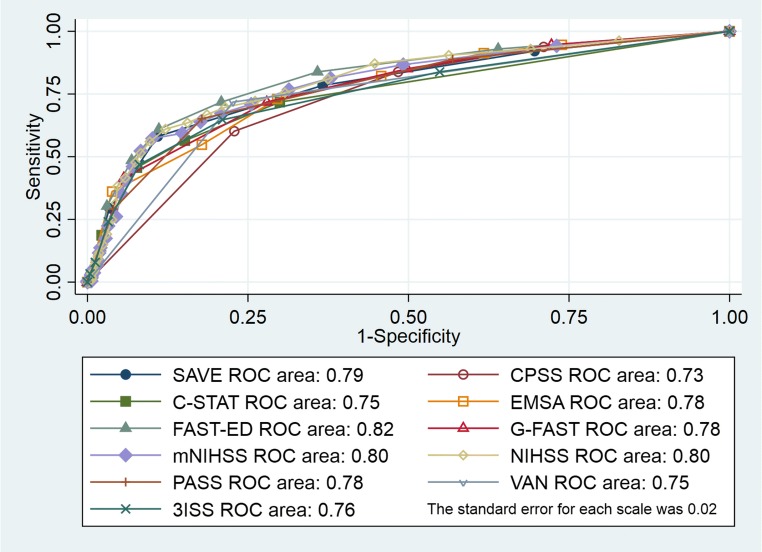
A worldwide problem, however, is identifying LVO stroke patients rapidly so patients can be accurately triaged directly to CSCs to decrease time to treatment. Such a system would send LVO patients to the nearest CSC bypassing PSCs and send non-LVO patients to the nearest PSC. A substantial amount of time can be lost if the LVO patient is transported first to a PSC, imaged, IV tPA treated, then transported to a CSC [44, 45]. To better triage LVO patients, many municipalities have created triage systems based on the clinical examination of the patient by first responders [46]. First responders in the USA have a wide range of training from simply basic life support–trained volunteers in rural areas, emergency medicine technologists (EMTs), paramedics, and, in rare circumstances, neurologists with video or physical presence in the ambulance. EMTs and paramedics receive structured training and need to pass certification before practicing, yet little education is directed at stroke recognition. Even vascular neurologists certified to perform the NIHSS are only about 80% accurate when examining a patient, chiefly because of stroke mimics [46, 47]. For example, a patient with a new right hemiparesis and global aphasia most likely has a left MCA stroke but may also have a left hemisphere intracerebral hemorrhage, a post-ictal paralysis, a migraine, or an old stroke that is unmasked by some metabolic insult. Therefore, the application of various “stroke scales” alone to identify LVO will never be completely accurate. In Fig. 5, an analysis of the major published scales for LVO detection shows a 0.73 to 0.82 area under the receiver operating characteristic curve for each scale for a large cohort of acute stroke patients. At best, choosing the best cut-point to maximize sensitively and specificity, only about 80% of patients can be properly triaged by clinical examination alone. Therefore, even if first responders are trained to the level of neurologists, detection of LVO by examination alone will lead to many patients triaged improperly.
Fig. 5.
Receiver operating characteristic curves for each neurological exam-based scale. ROC = receiver operating characteristic; SAVE = Speech Arm Vision Eyes; EMSA = Emergency Medical Stroke Assessment; FAST-ED = Field Assessment Stroke Triage for Emergency Destination; mNIHSS = modified National Institutes of Health Stroke Scale; NIHSS = National Institutes of Health Stroke Scale; CPSS = Cincinnati Prehospital Stroke Scale; C-STAT = Cincinnati Stroke Triage Assessment Tool; G-FAST = Gaze, Face, Arm, Speech, and Time; PASS = Prehospital Acute Stroke Severity; VAN = Vision, Aphasia, and Neglect; 3ISS = 3-Item Stroke Scale; reproduced with permission [47].
Rapid imaging using CT and CTA in the prehospital setting has emerged as 1 solution. First reported in East Berlin, using a mobile stroke unit (ambulance capable of housing and using a portable CT scanner) and administering IV tPA on-site have emerged as a strategy to provide tPA quicker [48]. Furthermore, since CTA is performed, LVO patients with gold standard accuracy can then be triaged directly to CSCs, minimizing treatment times. In some cases, a neurologist of advanced healthcare provider is present in the ambulance, while in others, a medical professional joins by video/audio link. Mobile stroke units are now operating in multiple metropolitan areas within the USA. At present, no proven biometric other than CTA is available to accurately identify LVO patients in the prehospital setting but it is the subject of research.
Future Research
MT is proven effective, yet more than 50% of LVO patients do not have a good outcome. Given the time it takes to provide effective therapy, it is unlikely that revascularization therapy will be completely effective, and it remains unclear where this plateau in clinical benefit will ultimately fall. The concept of neuroprotection, widely tested in the 1990s, now has a new platform for testing. Since the degree of brain injury prior to thrombectomy and the timing of reperfusion is measured, better designed trials of neuroprotection are now possible. The no-reflow concept of microvascular reperfusion is an important target and has not been tested outside of animal models. Drugs that prolong ischemia time may have benefit if administered prior to MT. The hypothesis that the absence of an ischemic penumbra portends no benefit from MT has been not been adequately tested nor has the process of treating all patients with LVO regardless of imaging findings. Efforts are underway to define these additional populations that may benefit. This includes direct triage to thrombectomy without brain imaging based on a biometric, analogous to how the portable electrocardiogram allows for direct triage of acute ST depression myocardial infarction to the angiography suite. Once at a CSC, combining cross-sectional imaging with angiography capability in the same room (a “stroke room”) is gaining popularity, allowing teams to rotate around the patient rather than having the patient travel between hospital locations. Validating and implementing these systems will take effort, but a continued focus on decreasing the time to treatment will improve outcomes for this morbid form of stroke.
Electronic supplementary material
(PDF 498 kb)
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Center for Health Statistics [online]. Available at: https://www.cdc.gov/nchs/fastats/deaths.htm.
- 2.Smith WS, Lev MH, English JD, et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke. 2009;40:3834–3840. doi: 10.1161/STROKEAHA.109.561787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weimar C, Konig IR, Kraywinkel K, Ziegler A, Diener HC, German Stroke Study C. Age and National Institutes of Health Stroke Scale Score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke. 2004;35:158–162. doi: 10.1161/01.STR.0000106761.94985.8B. [DOI] [PubMed] [Google Scholar]
- 4.Jones TH, Morawetz RB, Crowell RM, et al. Thresholds of focal cerebral ischemia in awake monkeys. J Neurosurg. 1981;54:773–782. doi: 10.3171/jns.1981.54.6.0773. [DOI] [PubMed] [Google Scholar]
- 5.Heiss WD. The ischemic penumbra: correlates in imaging and implications for treatment of ischemic stroke. The Johann Jacob Wepfer award 2011. Cerebrovasc Dis. 2011;32:307–320. doi: 10.1159/000330462. [DOI] [PubMed] [Google Scholar]
- 6.Astrup J, Siesjo BK, Symon L. Thresholds in cerebral ischemia—the ischemic penumbra. Stroke. 1981;12:723–725. doi: 10.1161/01.STR.12.6.723. [DOI] [PubMed] [Google Scholar]
- 7.Astrup J, Symon L, Branston NM, Lassen NA. Cortical evoked potential and extracellular K+ and H+ at critical levels of brain ischemia. Stroke. 1977;8:51–57. doi: 10.1161/01.STR.8.1.51. [DOI] [PubMed] [Google Scholar]
- 8.Heiss WD. The ischemic penumbra: how does tissue injury evolve? Ann N Y Acad Sci. 2012;1268:26–34. doi: 10.1111/j.1749-6632.2012.06668.x. [DOI] [PubMed] [Google Scholar]
- 9.Hossmann KA. Viability thresholds and the penumbra of focal ischemia. Annals of neurology. 1994;36:557–565. doi: 10.1002/ana.410360404. [DOI] [PubMed] [Google Scholar]
- 10.Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab. 2011;31:17–35. doi: 10.1038/jcbfm.2010.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Docagne F, Parcq J, Lijnen R, Ali C, Vivien D. Understanding the functions of endogenous and exogenous tissue-type plasminogen activator during stroke. Stroke. 2015;46:314–320. doi: 10.1161/STROKEAHA.114.006698. [DOI] [PubMed] [Google Scholar]
- 12.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–1587. [DOI] [PubMed]
- 13.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–1935. doi: 10.1016/S0140-6736(14)60584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 15.Thomalla G, Simonsen CZ, Boutitie F, et al. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med. 2018;379:611–622. doi: 10.1056/NEJMoa1804355. [DOI] [PubMed] [Google Scholar]
- 16.Alexandrov AV, Molina CA, Grotta JC, et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med. 2004;351:2170–2178. doi: 10.1056/NEJMoa041175. [DOI] [PubMed] [Google Scholar]
- 17.Smith WS, Furlan AJ. Brief History of Endovascular Acute Ischemic Stroke Treatment. Stroke. 2016;47:e23–26. doi: 10.1161/STROKEAHA.115.010863. [DOI] [PubMed] [Google Scholar]
- 18.del Zoppo GJ, Poeck K, Pessin MS, et al. Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Annals of neurology. 1992;32:78–86. doi: 10.1002/ana.410320113. [DOI] [PubMed] [Google Scholar]
- 19.del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998;29:4–11. doi: 10.1161/01.STR.29.1.4. [DOI] [PubMed] [Google Scholar]
- 20.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999;282:2003–2011. doi: 10.1001/jama.282.21.2003. [DOI] [PubMed] [Google Scholar]
- 21.Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36:1432–1438. doi: 10.1161/01.STR.0000171066.25248.1d. [DOI] [PubMed] [Google Scholar]
- 22.Becker KJ, Brott TG. Approval of the MERCI clot retriever: a critical view. Stroke. 2005;36:400–403. doi: 10.1161/01.STR.0000153056.25397.ff. [DOI] [PubMed] [Google Scholar]
- 23.Tomsick TA. Mechanical embolus removal: a new day dawning. Stroke. 2005;36:1439–1440. doi: 10.1161/str.36.7.1439. [DOI] [PubMed] [Google Scholar]
- 24.Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380:1231–1240. doi: 10.1016/S0140-6736(12)61299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith WS. Results of the Multi-MERCI trial. Stroke 2006. [DOI] [PubMed]
- 26.Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368:914–923. doi: 10.1056/NEJMoa1212793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893–903. doi: 10.1056/NEJMoa1214300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castano C, Serena J, Davalos A. Use of the New Solitaire (TM) AB Device for Mechanical Thrombectomy when Merci Clot Retriever Has Failed to Remove the Clot. A Case Report. Interventional Neuroradiology: journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences. 2009;15:209–214. doi: 10.1177/159101990901500212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hauck EF, Mocco J, Snyder KV, Levy EI. Temporary endovascular bypass: a novel treatment for acute stroke. AJNR Am J Neuroradiol. 2009;30:1532–1533. doi: 10.3174/ajnr.A1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelly ME, Furlan AJ, Fiorella D. Recanalization of an acute middle cerebral artery occlusion using a self-expanding, reconstrainable, intracranial microstent as a temporary endovascular bypass. Stroke. 2008;39:1770–1773. doi: 10.1161/STROKEAHA.107.506212. [DOI] [PubMed] [Google Scholar]
- 31.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 32.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 33.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 34.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 35.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–1018. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 36.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 37.Bracard S, Ducrocq X, Mas JL, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. The Lancet Neurology. 2016;15:1138–1147. doi: 10.1016/S1474-4422(16)30177-6. [DOI] [PubMed] [Google Scholar]
- 38.Saver JL, Goyal M, van der Lugt A, et al. Time to Treatment With Endovascular Thrombectomy and Outcomes From Ischemic Stroke: A Meta-analysis. JAMA. 2016;316:1279–1288. doi: 10.1001/jama.2016.13647. [DOI] [PubMed] [Google Scholar]
- 39.Lansberg MG, Straka M, Kemp S, et al. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): a prospective cohort study. The Lancet Neurology. 2012;11:860–867. doi: 10.1016/S1474-4422(12)70203-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med 2017. [DOI] [PubMed]
- 41.Albers GW, Marks MP, Kemp S, et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med. 2018;378:708–718. doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stroke Centers [online]. Available at: https://www.stroke.org/understand-stroke/recognizing-stroke/emergency-stroke-center-locations/.
- 43.Schieb LJ, Casper ML, George MG. Mapping Primary and Comprehensive Stroke Centers by Certification Organization. Circ Cardiovasc Qual Outcomes. 2015;8:S193–194. doi: 10.1161/CIRCOUTCOMES.115.002082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Froehler MT, Saver JL, Zaidat OO, et al. Interhospital Transfer Before Thrombectomy Is Associated With Delayed Treatment and Worse Outcome in the STRATIS Registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke) Circulation. 2017;136:2311–2321. doi: 10.1161/CIRCULATIONAHA.117.028920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McTaggart RA, Moldovan K, Oliver LA, et al. Door-in-Door-Out Time at Primary Stroke Centers May Predict Outcome for Emergent Large Vessel Occlusion Patients. Stroke. 2018;49:2969–2974. doi: 10.1161/STROKEAHA.118.021936. [DOI] [PubMed] [Google Scholar]
- 46.Keenan KJ, Kircher C, McMullan JT. Prehospital Prediction of Large Vessel Occlusion in Suspected Stroke Patients. Curr Atheroscler Rep. 2018;20:34. doi: 10.1007/s11883-018-0734-x. [DOI] [PubMed] [Google Scholar]
- 47.Keenan KJ, Smith WS. The Speech Arm Vision Eyes (SAVE) scale predicts large vessel occlusion stroke as well as more complicated scales. J Neurointerv Surg 2018. [DOI] [PubMed]
- 48.Kunz A, Nolte CH, Erdur H, et al. Effects of Ultraearly Intravenous Thrombolysis on Outcomes in Ischemic Stroke: The STEMO (Stroke Emergency Mobile) Group. Circulation. 2017;135:1765–1767. doi: 10.1161/CIRCULATIONAHA.117.027693. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 498 kb)