Abstract
Introduction
This study is aimed to compare kinematic gait data of patients who have undergone total and unicondylar knee replacement.
Materials and methods
This single-surgeon retrospective cohort study evaluated 13 patients with unilateral total knee arthroplasty (TKA) and 14 unicondylar knee arthroplasty (UKA). Gait analysis was carried out using a Vicon motion analysis system. The limits of knee flexion during stance phase, at heel strike and at loading response were measured.
Results
The total range of motion of the UKA knees was significantly greater than the TKA knees. UKA knees exhibited significantly greater knee extension during the stance phase than the TKA knees. Unlike TKA, UKA knees demonstrated improved knee flexion during the gait cycle when compared to the contralateral non-operated knee. The hips also demonstrated near normal hip flexion in UKA patients. Predictably, UKA knees had significantly greater varus compared with TKA in the coronal plane. Spatiotemporal variables demonstrated similar walking speed and step length to aid a fair comparison between knee replacement groups.
Conclusions
The UKA knees moved more physiologically in the sagittal plane with a greater range of motion during gait. Despite having a stiff gait pattern, the patients undergoing TKA demonstrated a more neutral alignment in the coronal plane. Neither type of knee arthroplasty restored knee kinematics to those of the non-operated side.
Keywords: Total knee arthroplasty, Unicondylar knee arthroplasty, Gait analysis, Kinematics
Introduction
The primary aim of knee replacement is to relieve pain, correct deformity and improve function. There are, however, well-documented gait abnormalities seen after surgery.1 These gait changes alter knee joint loading, which may have a detrimental effect on the prosthesis.2 Gait analysis is an important metric to objectively measure the way people walk after knee replacement surgery.3 Kinematics is the specific study to evaluate the motion of the joints during gait. Until 2015, only 13 articles reported on the kinematics of unicondylar knee arthroplasty (UKA). Four studies compared the results with total knee arthroplasty (TKA). There was no clear evidence for the kinematic or kinetic advantages of UKA. However retention of the cruciate ligaments is theoretically advantageous, so further study may determine whether a difference does exist. Some 75 studies reported on TKA kinematics, of which 19 (25.3%) measured frontal plane motion and only 7 (9.3%) measured transverse plane motion.4 In the present study, sagittal and coronal plane kinematics were studied because knee alignment in the coronal plane optimises knee joint loading.
The aim of the present study was to compare gait kinematics of patients who have had successful total and unicondylar knee replacements and to assess how operated knees differed from the non-operated knees in both groups of patients at the time of study.
Patient selection criteria
In this retrospective cohort study, patients were identified from an arthroplasty audit data base. Patients older than 60 years at the time of surgery who had undergone a unilateral UKA (Oxford® knee, Zimmer-Biomet)5 or TKA (low contact stress rotating platform, Synthes)6 for knee osteoarthritis one year prior to the study by a single senior surgeon were included. These patients were required to have well-functioning knees that were clinically successful at all time points postoperatively and be able to do level walking without using any walking aids. X-rays were not analysed but clinical alignment of the limb was recorded at the time of gait analysis. None of the patient included in this study had fixed flexion deformity at the time of gait analysis. Patients suffering from polyarthropathy, neuromuscular disease or cardiovascular disorders were excluded. Patients having other lower limb joint prostheses were excluded. The objective of the strict inclusion/exclusion criteria was to ensure that kinematic gait analysis was performed on the well-functioning knee replacements. The null hypothesis was that no kinematic difference would be seen irrespective of knee replacement type.
Equipment
Three-dimensional (3D) motion data of the lower limbs were recorded using a Vicon 3D motion capture system (Oxford Metrics; Fig 1) in the gait laboratory at the Institute of Motion Analysis and Research at the University of Dundee. This system uses 12 MX-F40 cameras and two AMTI force plates embedded into the floor. The force plates were used to identify specific events occurring during the gait cycle.
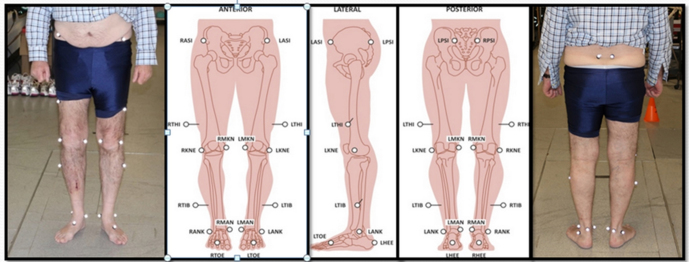
Figure 1.
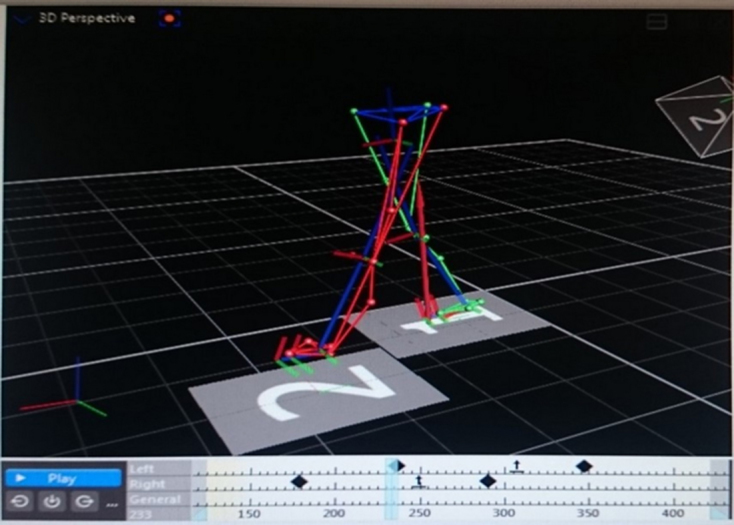
Reconstructed skeleton in the Vicon system.
Gait analysis protocol
Each patient attended the gait laboratory for a single 30-minute session. Height, leg lengths and weight were measured by the lead researcher. Body mass index (BMI) was calculated. Twenty 14-mm diameter retroreflective markers were placed on specific anatomical bony landmarks (Fig 2). The patients then walked at a comfortable pace barefoot across the two force plates, which were placed according to standard protocol of Vicon plug-in gait model,7 which is clinically accepted worldwide. A successful trial was accepted when the patient’s foot landed on the centre of the force plate. Five successful trials were collected for each leg. For those five trials, the best three based upon tracking quality were used to calculate the mean of different parameters during analysis.
Figure 2.
Retro-reflective marker placement sites (© Institute of Motion Analysis and Research, 2014; reproduced with permission).
Data analysis
Motion and force data were used to define heel contact and toe-off for stride and step identification. A gait cycle was defined as the period of time from one initial contact to ipsilateral initial contact. Hip–knee–ankle angles in two planes were calculated from the motion data obtained. There are several kinematic parameters of gait, of which ‘maximum knee flexion stance’, ‘maximum knee flexion swing’, ‘maximum hip extension’ and ‘maximum ankle plantarflexion’ are the most important in knee arthroplasty.8 Maximum and minimum angles of knee flexion during the stance phase and the gait cycle were assessed. Knee flexion at heel strike and at loading response (11% of stance phase) were also evaluated. Ankle flexion at heel strike and hip flexion during stance phase were also recorded.
Mean and standard deviation (SD) were calculated for all demographic characteristics (age at surgery, BMI, time of gait analysis from surgery). The functional Knee Society score (KSS) and total KSS were calculated at the time of study. Scores for each patient preoperatively and one year postoperatively were collected from the audit data base.
As a preliminary study, power analysis was not conducted at the beginning of the project. Following the data collection, the statistical power was checked. Using the range of motion of the knee as a primary parameter (i.e. SD eight degrees from the collected data), with 80% of power, Alpha 0.05 and 10 degrees of clinical difference, it was estimated that the sample size should be 11. Therefore, the sample size of 14 in the present study is reasonable in terms of statistical power.
SPSS Statistics, version 22, was employed for statistical analysis of the data. The general linear model for repeated measurements was used to compare the variables between the operated and non-operated sides, where the main factor was side and the between-subject factor was surgery. Considering that some parameters were not normally distributed, non-parametric tests such as Mann–Whitney or Kruskal–Wallis tests were used to compare the two surgical groups. The significance level was set at P < 0.05.
Ethics
Ethical approval was granted by University of Dundee Research Ethics Committee (UREC 15183) and the Cambridge South Research Ethics Committee (16/EE/0021). Caldicott Guardian Approval was obtained to access existing data. A written consent in accordance to ethics committee guidelines was obtained from all participants.
Results
Demographics
Fourteen UKA patients, of whom eight were male and six female, and 13 TKA patients, of whom nine were male and four female volunteered for the pilot study. There were no significant differences between the two groups in terms of age at the time of surgery and time since surgery but the TKA group was significantly heavier (P < 0.05; Table 1). No significant differences were found in spatiotemporal parameters between the groups (Table 2). No significant difference was found between the functional and total KSS of the two groups at any time point (i.e. preoperatively, one year postoperatively and at the time when the study was carried out; Table 3).
Table 1.
Demographic comparison between total knee ?arthroplasty and unicondylar knee arthroplasty.
| Group | Surgery | Mean | SD | P-value |
| Age at surgery (years) | TKA | 65.77 | 6.52 | 0.91 |
| UKA | 65.50 | 5.56 | ||
| Time since surgery (years) | TKA | 7.73 | 3.96 | 0.71 |
| UKA | 7.21 | 2.98 | ||
| BMI (kg/m2) | TKA | 30.38 | 3.62 | 0.005 |
| UKA | 26.43 | 3.10 |
BMI, body mass index; SD, standard deviation from the mean; TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty.
Table 2.
Comparison of spatiotemporal gait parameters of UKA and TKA groups.
| Measure | Mean | Std. Error | 95% Confidence interval | P-value | ||
| Lower bound | Upper bound | |||||
| Cadence (steps/min) | TKA | 102.19 | 1.91 | 98.38 | 105.99 | 0.27 |
| UKA | 105.19 | 1.91 | 101.38 | 109.00 | ||
| Speed (m/s) | TKA | 1.01 | 0.03 | 0.95 | 1.06 | 0.31 |
| UKA | 1.05 | 0.03 | 0.99 | 1.11 | ||
| Stride Length (m) | TKA | 1.18 | 0.02 | 1.14 | 1.23 | 0.72 |
| UKA | 1.20 | 0.02 | 1.15 | 1.24 | ||
SE, standard error; TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty.
Table 3.
Comparison of functional and total Knee Society scores of both groups at different time intervals.
| Knee Society score | Surgery | Mean | SD | SE | P-value |
| Functional preoperative | TKA | 55.77 | 13.97 | 3.87 | 0.28 |
| UKA | 65.00 | 27.24 | 7.28 | ||
| Functional 1 year | TKA | 92.31 | 8.32 | 2.30 | 0.97 |
| UKA | 92.14 | 14.76 | 3.94 | ||
| Functional 2016 | TKA | 96.15 | 8.69 | 2.41 | 0.77 |
| UKA | 95.00 | 11.60 | 3.10 | ||
| Total preoperative | TKA | 37.85 | 23.11 | 6.41 | 0.61 |
| UKA | 42.36 | 21.60 | 5.77 | ||
| Total 1 year | TKA | 88.62 | 8.79 | 2.43 | 0.35 |
| UKA | 91.29 | 5.58 | 1.49 | ||
| Total 2016 | TKA | 88.46 | 10.85 | 3.01 | 0.29 |
| UKA | 83.85 | 11.25 | 3.01 |
SD, standard deviation from the mean; SE, standard error; TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty.
TKA compared with UKA
When comparing the maximum angle of flexion during the stance phase and gait cycle UKA knees had higher flexion by 9.3% (P = 0.470) and 6.3% (P = 0.980), respectively, than TKA knees. The total range of motion in the UKA knees was 12.5% higher than in TKA knees (P < 0.001; Table 4; Fig 3). This was probably because UKA knees extended by 44.8% more than TKA knees during the stance phase (P < 0.001).
Table 4.
Comparison between total knee arthroplasty and unicondylar knee arthroplasty.
| Joint | Event | Group | Mean | SE | P-value |
| Knee | Maximum flexion in stance phase (sagittal plane) | TKA | 44.73 | 1.15 | 0.47 |
| UKA | 48.88 | 1.08 | |||
| Knee | Minimum angle in stance phase (sagittal plane, extension) | TKA | 7.17 | 0.97 | < 0.001 |
| UKA | 3.96 | 0.91 | |||
| Knee | Minimum angle in stance phase (coronal plane, varus) | TKA | –3.61 | 0.97 | < 0.001 |
| UKA | –4.08 | 0.80 | |||
| Knee | Maximum angle in stance phase (coronal plane, valgus) | TKA | 8.55 | 0.95 | 0.27 |
| UKA | 7.11 | 0.88 | |||
| Knee | Range of movement in gait cycle (sagittal plane) | TKA | 41.49 | 0.81 | < 0.001 |
| UKA | 46.68 | 0.77 | |||
| Knee | Maximum flexion in gait cycle (sagittal plane) | TKA | 47.97 | 1.23 | 0.98 |
| UKA | 51.01 | 1.17 | |||
| Ankle | Flexion at foot strike (sagittal) | TKA | 0.92 | 0.79 | 0.08 |
| UKA | 2.84 | 0.76 | |||
| Hip | Maximum flexion in stance phase (sagittal) | TKA | 43.87 | 1.29 | 0.01 |
| UKA | 48.43 | 1.21 |
SE, standard error; TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty.
Figure 3.
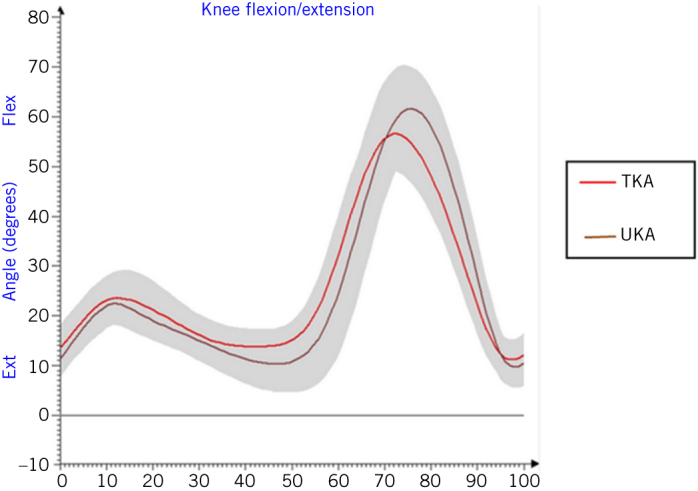
Comparison of motion at knees in both groups in sagittal plane during the gait cycle (TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty).
The UKA group of patients had a mean static alignment of 1.7 degrees of valgus while the TKA group had 4.2 degrees of valgus. The UKA knees had 13% (P < 0.05) greater dynamic varus than TKA knees but less dynamic valgus by 16.8% (P > 0.05; Table 4; Fig 4).
Figure 4.
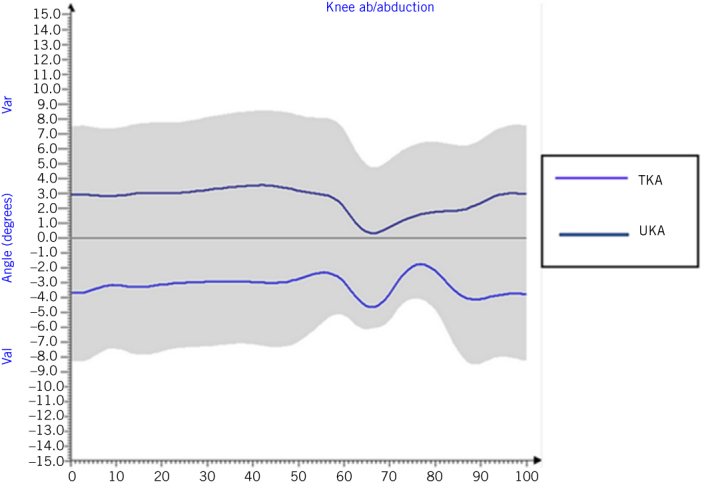
Comparison of motion at knees in both groups in coronal plane during the gait cycle (TKA, total knee arthroplasty; UKA, unicondylar knee arthroplasty).
The UKA knee patients had 10.4% greater hip flexion than the TKA knees (P = 0.011). Furthermore, the UKA group demonstrated double the amount of ankle dorsiflexion when compared with TKA during heel strike (P = 0.082; Table 4).
TKA: operated side compared with non-operated side
The maximum angle of flexion in the stance phase and during the gait cycle in the TKA group was less by 7.9% (P = 0.008) and 8.4% (P < 0.001), respectively, in comparison with the non-operated side. The total range of motion in the operated knee was less than in the non-operated knee by 9.9% (P < 0.001). TKA knees had less flexion by 3.4% (P = 0.77) at heel strike and by 11.4% (P = 0.051) during the loading response than their contralateral knees. TKA knees extended less than their contralateral side by 3.7% (Table 5).
Table 5.
Kinematic comparisons between total knee arthroplasty operated and non-operated knees.
| Joint | Event | Side | Mean | Std. Error | P-value |
| Knee | Flexion at heel strike (sagittal plane) | Non-operated | 20.18 | 1.35 | 0.77 |
| Operated | 19.50 | 1.35 | |||
| Knee | Flexion at loading response (sagittal plane) | Non-operated | 23.64 | 0.84 | 0.05 |
| Operated | 20.96 | 1.03 | |||
| Knee | Maximum flexion in stance phase (sagittal plane) | Non-operated | 48.55 | 0.99 | 0.008 |
| Operated | 44.73 | 1.04 | |||
| Knee | Minimum angle in stance phase (sagittal plane, extension) | Non-operated | 6.91 | 0.82 | 0.68 |
| Operated | 7.17 | 0.73 | |||
| Knee | Minimum angle in stance phase (coronal plane, varus) | Non-operated | –4.25 | 1.06 | 0.28 |
| Operated | –3.61 | 0.97 | |||
| Knee | Maximum angle in stance phase (coronal plane, valgus) | Non-operated | 8.38 | 1.40 | 0.85 |
| Operated | 8.55 | 1.09 | |||
| Knee | Range of movement in gait cycle (sagittal plane) | Non-operated | 46.06 | 0.72 | < 0.001 |
| Operated | 41.49 | 0.68 | |||
| Knee | Maximum flexion in gait cycle (sagittal plane) | Non-operated | 52.34 | 1.09 | < 0.001 |
| Operated | 47.97 | 0.99 | |||
| Ankle | Flexion at foot strike | Non-operated | 1.85 | 0.81 | 0.52 |
| Operated | 0.92 | 0.84 | |||
| Hip | Maximum flexion in stance phase | Non-operated | 47.09 | 1.30 | 0.03 |
| Operated | 43.87 | 1.18 |
The TKA knees had less dynamic varus (minimum angle of adduction) by 15.05% and greater dynamic valgus (maximum angle of abduction) by 2% than their contralateral side (P > 0.05; Table 5).
The hips in the TKA operated limb flexed less (6.8%, P = 0.032) than hips in the non-operated limb. At heel strike, ankles in the TKA operated limb dorsiflexed less (50.2%, P = 0.523) than the ankles on the contralateral non-operated side (Table 5).
UKA: operated side compared with non-operated side
The UKA knees had higher maximum angle of flexion during the stance phase and during the gait cycle than the non-operated knees by 5.1% (P = 0.026) and 4.7% (P = 0.00), respectively. The total range of motion in the UKA knees was greater than on the non-operated sides by 3.9% (P = 0.006; Table 6). UKA knees had greater flexion by 10.4% (P = 0.51) at heel strike and 8.8% (P = 0.112) during loading response than their contralateral knees (Table 6). UKA knees extended more than the other side by 18.91%. The UKA knees had 4.7 times the varus than their contralateral side on gait analysis (Table 6).
Table 6.
Kinematic comparisons between unicondylar knee arthroplasty operated and non-operated knees.
| Joint | Event | Side | Mean | Std. Error | P-value |
| Knee | Flexion at heel strike (sagittal plane) | Non-operated | 16.73 | 1.44 | 0.51 |
| Operated | 18.47 | 1.54 | |||
| Knee | Flexion at loading response (sagittal plane) | Non-operated | 20.96 | 0.85 | 0.11 |
| Operated | 22.82 | 1.01 | |||
| Knee | Maximum flexion in stance phase (sagittal plane) | Non-operated | 46.52 | 1.19 | 0.03 |
| Operated | 48.88 | 1.16 | |||
| Knee | Minimum angle in stance phase (sagittal plane, extension) | Non-operated | 3.33 | 1.10 | 0.12 |
| Operated | 3.96 | 1.07 | |||
| Knee | Minimum angle in stance phase (coronal plane, varus) | Non-operated | –0.71 | 0.75 | < 0.001 |
| Operated | –4.08 | 0.80 | |||
| Knee | Maximum angle in stance phase (coronal plane, valgus) | Non-operated | 9.91 | 0.77 | 0.002 |
| Operated | 7.11 | 0.75 | |||
| Knee | Range of movement in gait cycle (sagittal plane) | Non-operated | 44.91 | 0.84 | 0.006 |
| Operated | 46.68 | 0.86 | |||
| Knee | Maximum flexion in gait cycle (sagittal plane) | Non-operated | 48.71 | 1.46 | < 0.001 |
| Operated | 51.01 | 1.35 | |||
| Ankle | Flexion at foot strike | Non-operated | 1.51 | 0.80 | 0.29 |
| Operated | 2.84 | 0.71 | |||
| Hip | Maximum flexion in stance phase | Non-operated | 46.22 | 1.38 | 0.23 |
| Operated | 48.43 | 1.29 |
The hips in the UKA operated limb flexed more (4.8%, P = 0.228) than hips on the non-operated limb (Table 6). The ankles in the UKA operated limb dorsiflexed more (88.1%, P = 0.287) than ankles in the non-operated limb at heel strike (Table 6).
Discussion
The most important finding in this kinematic gait study, balanced for age and patient-reported outcome measures, was the significantly greater range of motion found in UKA patients when compared with TKA patients. Pre- and postoperative Knee Society scores were calculated, which took the knee range of movement into consideration. There was significant difference between the pre- and postoperative scores in each group. The increase in KSS after surgery is due to pain relief and deformity correction. In this study, the preoperative KSS scores of TKA and UKA group of patients were not significantly different; this makes both groups comparable.
TKA compared with UKA
In the present study, the total range of motion was significantly higher by 12.5% in UKA knees than TKA knees in the sagittal plane. A reduction in flexion in TKA during the swing and stance phases leading to a reduced total range of motion during the gait cycle has been described as ‘TKA stiff knee gait pattern’.9 It has been suggested that decreased knee flexion occurs along with a decreased knee extensor moment, resulting in the stiff attitude of the TKA knee. This may act as a mechanism to protect the quadriceps muscles.10 Stance-phase knee extension is important for providing stability and power generation for propulsion.11 Fixed flexion deformity after TKA can contribute to a lack of extension during the stance phase. None of the patients had a fixed flexion deformity. The UKA knees extended statistically significantly more than the TKA knees by three degrees but this may not be clinically significant.
There was a correlation between knee alignment after surgery and peak adduction moments during the stance phase of gait. The peak adduction moments during gait increase in magnitude in direct proportion to the amount of varus of the limb after surgery. The load on the prosthesis significantly increases if residual varus is greater than four degrees.12 In the present study, both groups had greater than one degree static valgus alignment.
Implant retrieval studies have found that wear on the medial compartment was greater than on the lateral compartment after primary total knee arthroplasty surgery.13 A larger knee adduction angle on the normal side than on the operated side has been associated with higher dynamic loading on the normal side. This may predispose the normal knee to a higher risk of osteoarthritis incidence and progression.14 Thus, it is very important to study coronal plane kinematics.
It is important to monitor other associated joints in order to detect if any compensatory mechanisms are present. The maximum angle of flexion was significantly greater at the hip on the operated limbs of the UKA group than in the TKA group during the stance phase. This can be explained by prolonged activity of rectus femoris without co-contractions of the hamstrings found in the Oxford UKA group of patients.15
TKA: operated side compared with non-operated side
Different studies have reported a significantly reduced maximum angle of flexion during the stance phase in TKA patients.1,16 There has been variation in reports regarding the change in maximum knee flexion angle during the stance phase.17 In the present study, the same angle was significantly less, than on the non-operated side in the TKA group.
McClelland et al reported reduced flexion at the knee during the loading phase of gait in TKA patients in comparison with healthy control groups.18 In the present study, the TKA knees had 11.37% greater flexion than non-operated knees. Thus, flexion does improve after TKA but when compared to that of healthy controls, TKA knee flexion is reduced and would be far from normal standards.18
In both groups, there was no significant difference in extension of the knees between operated and non-operated knees. McClelland et al reported that TKA knees extended less than their control patient knees at comfortable as well as fast walking speeds.16 The authors concluded that prolonged hamstring activity and impaired gluteal and quadriceps muscle function may cause a limitation of extension but they suggested that further research was required to come to a conclusion.
At heel strike, flexion in TKA knees did not have significant difference in comparison to their contralateral knees. This was similar to the findings of Levinger et al, who compared knee flexion in 11 unilateral UKA and 8 TKA patients at heel strike to their contralateral non-operated knee.19
Reduced ankle dorsiflexion was found in the present standard protocol of Vicon plug in-gait model study of the operated limb compared with the non-operated limb in the TKA group.7 This is similar to the findings of Levinger et al.19 However results from the present study suggest that UKA, unlike TKA, improves ankle dorsiflexion on the operated limb.
If a TKA is in varus there may be eccentric loading and consequent rocking of the components. This could result in loosening due to tension stresses at the implant-bone interface on the unloaded side of the component.20 In the present study, the maximum and minimum angle of abduction (valgus and varus, respectively) in the coronal plane in TKA patients was not significantly different from the contralateral sides. Different implant retrieval studies have found that wear on the medial compartment was greater than on the lateral following primary total knee arthroplasty.13 A larger knee adduction angle on the normal side than on the operated side has been associated with higher dynamic loading on the normal side. This may predispose the normal knee to a increased risk of osteoarthritis.14
UKA: operated side compared with non-operated side
In the present study, the maximum angle of flexion during the gait cycle was significantly higher in UKA knees when compared with the non-operated knees. Webster et al compared unilateral UKA with the contralateral knee and found increased flexion throughout the gait cycle in the majority of UKA patients.21 This is similar to the findings in the present study.
At heel strike, flexion in UKA knees was not significantly different from their non-operated knees, which was similar to the findings of Levinger et al.19 There was no significant difference in knee extension between operated and non-operated knees.
There was far more dorsiflexion at the ankle in operated UKA limbs than contralateral limbs at heel strike. Excessive dorsiflexion at the ankle has previously been reported in UKA (Oxford) patients.15 This may be associated with over activity of the tibialis anterior muscle and greater walking speeds found in patients who have had UKA in comparison to TKA. A near normal range of motion of adjacent joints allows more normal physiological loading which has been seen in patients walking downhill when compared with healthy controls and TKA patients.22
The effect of limb alignment on the functional outcome of UKA was evaluated by Gulati et al.20 It was concluded that 25% of patients seen had varus malalignment. This did not seem to compromise the functional outcome and accordingly varus malalignment may not increase the rate of failure from wear or loosening. The authors claimed that the centre of force lies near to the centre of the component irrespective of the alignment of the leg. This would cause compression of the implant bone interface and thus prevent loosening. In the present study, the UKA knees were in significantly more varus position than the non-operated sides and still all patients were asymptomatic at a mean of 7.21 years after surgery.
Limitations of the study
The principle weakness of the present study is the small number of patients and the lack of preoperative gait data to determine the functional change attributed to a particular knee prosthesis. TKA patients were also significantly heavier than the UKA patients, which could influence the ability to perform some more challenging activities. Despite this, both patient groups were matched with near identical gait speed and stride length to facilitate a fair comparison of joint movement. The analysis of the contralateral ‘normal’ side ensured a control limb for comparison. Furthermore, all patients were on average greater than seven postoperative years, a period which has been shown to be worse for UKA due to failures and higher rates of revision. It also evaluated other adjacent joints which are of interest to inform patients and other healthcare workers of the potential risks and benefits of one type of prosthesis over the other. Lastly, the findings of the study reflect only a single type of mobile bearing UKA and a single brand of rotating platform TKA and the findings may not be applicable to other knee arthroplasties. Considering this, ideally, future studies should be done prospectively with a range of speeds to encompass the entire spectrum of function which could be attributed to a particular type of knee arthroplasty.
Conclusion
Even though there were several significant differences in the kinematics of operated and non-operated limbs during the gait cycle, patients were clinically asymptomatic and had an acceptable gait. Neither type of arthroplasty restored knee kinematics to those of the contralateral side. The UKA knees appeared to move more physiologically in the sagittal plane while TKA knees had a ‘TKA stiff knee gait pattern’. The TKA knees were not significantly different from the non-operated knees in the coronal plane. It seems that varus alignment of UKA did not compromise the functional outcome. It is important to monitor other adjacent joints to record the compensatory mechanisms taking place there. This study, despite being underpowered, demonstrated significantly better function in UKA knees than age and gender-matched TKA knees.
Acknowledgements
We would like to thank Mrs. Sheila Gibbs for her help in developing polygon graphs and Mr Ian Christie for his help in editing the work.
References
- 1.McGinnis K, Snyder-Mackler L, Flowers P, Zeni J. Dynamic joint stiffness and co-contraction in subjects after total knee arthroplasty. Clin Biomech 2013; (2): 205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatfield GL, Hubley-Kozey CL, Wilson JL, Dunbar MJ. The effect of total knee arthroplasty on knee joint kinematics and kinetics during gait. J Arthroplasty 2011; (2): 309–318. [DOI] [PubMed] [Google Scholar]
- 3.Minns RJ. The role of gait analysis in the management of the knee. Knee 2005; (3): 157–162. [DOI] [PubMed] [Google Scholar]
- 4.Komnik I, Weiss S, Pagani CF, Potthast W. Motion analysis of patients after knee arthroplasty during activities of daily living: a systematic review. Gait Posture 2015; (2): 370–377. [DOI] [PubMed] [Google Scholar]
- 5.Zimmer Biomet Oxford® Partial Knee System. http://oxfordknee.com/oxford.cfm (cited February 2019).
- 6.DePuy Synthes LCS® COMPLETE Knee System. www.depuysynthes.com/hcp/knee/products/qs/LCS–COMPLETE–Knee–System (cited February 2019).
- 7.Vicon Plug-in Gait Model Details. www.vicon.com/downloads/documentation/plug–in–gait–model–details (cited February 2019).
- 8.Liebensteiner MC, Herten A, Gstoettner M et al. Correlation between objective gait parameters and subjective score measurements before and after total knee arthroplasty. Knee 2008; (6): 461–466. [DOI] [PubMed] [Google Scholar]
- 9.Benedetti MG, Catani F, Bilotta TW et al. Muscle activation pattern and gait biomechanics after total knee replacement. Clin Biomech 2003; (9): 871–876. [DOI] [PubMed] [Google Scholar]
- 10.Mandeville D, Osternig LR, Lantz BA et al. The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clin Biomech 2008; (8): 1,053–1,058. [DOI] [PubMed] [Google Scholar]
- 11.Olney SJ. Gait. In: Levangie PK, Norkin CC. Joint Structure And Function: A Comprehensive Analysis, 4th ed Philadelphia, PA: FA Davis; 2005, pp. 541–542. [Google Scholar]
- 12.Chassin EP, Mikosz RP, Andriacchi TP, Rosenberg AG. Functional analysis of cemented medial unicompartmental knee arthroplasty. J Arthroplasty 1996; (5): 553–559. [DOI] [PubMed] [Google Scholar]
- 13.Collier MB, Engh Jr CA, McAuley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. JBJS 2007; (6): 1,306–1,314. [DOI] [PubMed] [Google Scholar]
- 14.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res 2011; (5): 647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Catani F, Benedetti MG, Bianchi L et al. Muscle activity around the knee and gait performance in unicompartmental knee arthroplasty patients: a comparative study on fixed- and mobile-bearing designs. Knee Surg Sports Traumatol Arthrosc 2012; (6): 1,042–1,048. [DOI] [PubMed] [Google Scholar]
- 16.McClelland JA, Webster KE, Feller JA, Menz HB. Knee kinematics during walking at different speeds in people who have undergone total knee replacement. Knee 2011; (3): 151–155. [DOI] [PubMed] [Google Scholar]
- 17.Sosdian L, Dobson F, Wrigley TV et al. Longitudinal changes in knee kinematics and moments following knee arthroplasty: a systematic review. Knee 2014; (6): 994–1008. [DOI] [PubMed] [Google Scholar]
- 18.McClelland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: a systematic review. Knee 2007; (4): 253–263. [DOI] [PubMed] [Google Scholar]
- 19.Levinger P, Webster KE, Feller J. Asymmetric knee loading at heel contact during walking in patients with unilateral knee replacement. Knee 2008; (6): 456–460. [DOI] [PubMed] [Google Scholar]
- 20.Gulati A, Pandit H, Jenkins C et al. The effect of leg alignment on the outcome of unicompartmental knee replacement. Bone Joint J 2009; (4): 469–474. [DOI] [PubMed] [Google Scholar]
- 21.Webster KE, Wittwer JE, Feller JA. Quantitative gait analysis after medial unicompartmental knee arthroplasty for osteoarthritis. J Arthroplasty 2003; (6): 751–759. [DOI] [PubMed] [Google Scholar]
- 22.Lindström M, Felländer-Tsai L, Wredmark T, Henriksson M. Adaptations of gait and muscle activation in chronic ACL deficiency. Knee Surg Sports Traumatol Arthrosc 2010; (1): 106–114. [DOI] [PubMed] [Google Scholar]