Elevated blood pressure (BP) is still a leading health risk worldwide. Active efforts toward achieving and maintaining BP below the target level are essential to improve cardiovascular outcome. The first step is to prescribe appropriate BP lowering medications bearing in mind the comorbidities of the patient. However, it does not guarantee optimal results. A multifaceted approach to improve the ‘quality’ of BP control targeting each individual as well as the whole population is needed.1),2),3),4) In this regard, the study by Lee et al.5) had great implications for clinicians, public health providers, and policymakers. This nationwide study explored temporal and regional trends of hypertension management in those who were treated for hypertension between 2002 and 2016. The major findings are as follows. Drug adherence level substantially improved nationwide, and inter-regional difference in drug adherence decreased. Moreover, combination therapy and complication screening rates were less heterogeneous across regions. On the other hand, the recent decreasing trend in the combination therapy rate should be noted but its clinical implication is still unclear. Regarding complication screenings, the blood test rate has modestly improved, but still remains below 60% across regions. The urine test rate for complication screenings remains below 50% across regions. Particularly, the urine microalbuminuria test rate still remains below 30% without improvement over the last 15 years.
Patients with uncontrolled hypertension usually present with more cardiovascular diseases and target organ damage. Multi-level factors, such as patient, provider and healthcare system factors, have been associated with an inadequate control of hypertension.6) In the Lee et al.'s study,5) the authors classified the quality of hypertension management according to three domains: 1) adherence rates, 2) combination therapy rate, and 3) complication screening rates.
First, medication adherence is a very important issue in the quality of BP control. The authors defined ‘adherence’ as the regular use of prescribed medicines for at least 80% of the time in one year, which more precisely refers to ‘persistence’ of medication. Although adherence is a narrow concept concerning only whether patients follow the prescribed interval and dose,7) medication adherence is often used as a broader concept incorporating both adherence (amount and frequency of drug use during the drug therapy) and persistence (overall duration of drug therapy).1) The results of the study are encouraging as the increase in the overall adherence rates over the last 15 years is nearly threefold (from 24% to 72%); furthermore, the disparities between regional adherence rates have been resolved. Intriguingly, the initial regional disparities and decreased regional gap over the period were independent of individual social/economic factors, suggesting the importance of establishing and developing necessary infrastructures (which corresponds to system level factor). In regards to medical adherence, multi-level factors should be considered at patient, therapy, and healthcare system levels (Table 1). To improve drug adherence, all of these factors should be addressed. Although it is often neglected in a clinical setting, counseling patients regarding their medicines (confirmation of medication use and any side effects) is an essential component for the management of medication adherence.
Table 1. Multi-level factors for medication adherence.
| Levels | Examples |
|---|---|
| Patient | Age, comorbidity, mental status (depression), cognitive status (dementia), race, physical impairment (vision, hearing, move), literacy, education, economic status, social support |
| Therapy | Complexity of regimen, side effects |
| Healthcare system | Easy access to healthcare system, quality of provider-patient relationship, communications between provider and patient, continuity of care, education and campaign, establishing infrastructure (transportation, street, facilities for communication) |
Second, a combination therapy (Single pill combination [SPC]) has been known to improve BP control, and the recent 2018 European guidelines for hypertension emphasized the role of initial SPC therapy.2) Indeed, this correlates to the therapy level in drug adherence by alleviating the complexity of taking medication. A recent study demonstrated the benefit of SPC in medication adherence as well as in clinical outcomes.8) Furthermore, SPC could effectively manage BP, by targeting multiple mechanisms such as blocking the renin-angiotensin system or inducing vasodilation/diuresis. Although the exact causes for the recent plateau in the use of SPC are not well understood, the use of SPC is expected to increase according to the updated hypertension guidelines.2) In addition, physician therapeutic inertia is another reason for uncontrolled hypertension. The use of SPC when initiating antihypertensive medication may be effective to help overcome physician therapeutic inertia.6)
Third, the evaluation of target organ damage is an important part of hypertension management.9) Although the guidelines of the Korean Society of Hypertension recommend an annual test for microalbuminuria or proteinuria, strikingly, the overall urine test rate is below 50%, and the microalbuminuria test rate is even lower (<30%). Urinalysis is a simple, cost-effective method that could identify kidney damage. Evaluation of hypertension-mediated target organ damage could help stratify cardiovascular risk. Furthermore, in case of asymptomatic target organ damage in patients with hypertension, early active interventions for BP might influence clinical outcomes.2)
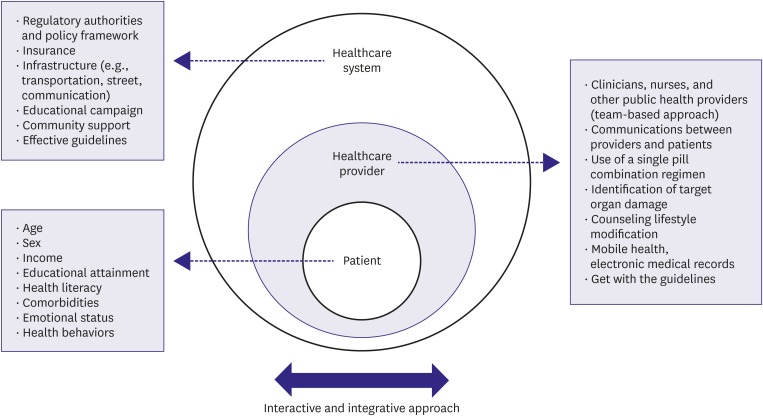
Last, there are several other factors related to inadequate control of hypertension. Lifestyle modification (exercise, low salt diet, and moderation of alcohol) is also an essential part of the quality of hypertension management.3) Considering its cost-effectiveness and additional benefits, proactive counseling regarding lifestyle modification is fundamental. Other factors include inaccurate BP measurement, inadequate patient education, low patient and/or provider awareness of BP target, absence of a usual source of care, and lack of access to health care. Lower health literacy is one of the main problems in the quality control of chronic diseases. However, this could be effectively managed by multiple level concerted interventions.10) Recent advances in mobile technology shed new light on bridging these gaps. Policy support such as reimbursement for home BP monitoring and promotion of educational programs is warranted (Figure 1).
Figure 1. Multifaceted approach for improving the quality of hypertension management.
In summary, comprehensive and multifaceted strategies that incorporate an individual patient-oriented approach and systematic population-based approach are jointly needed to improve overall cardiovascular health.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Ihm SH.
- Supervision: Ihm SH.
- Writing - original draft: Jung MH, Ihm SH.
- Writing - review & editing: Ihm SH.
The contents of the report are the author's own views and do not necessarily reflect the views of the Korean Circulation Journal.
References
- 1.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 2.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041. doi: 10.1097/HJH.0000000000001940. [DOI] [PubMed] [Google Scholar]
- 3.Lee CJ, Kim JY, Shim E, et al. The effects of diet alone or in combination with exercise in patients with prehypertension and hypertension: a randomized controlled trial. Korean Circ J. 2018;48:637–651. doi: 10.4070/kcj.2017.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HJ, Yoon SJ, Oh IH, Lim JH, Kim YA. Medication adherence and the occurrence of complications in patients with newly diagnosed hypertension. Korean Circ J. 2016;46:384–393. doi: 10.4070/kcj.2016.46.3.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee H, Park S, Kim HC. Temporal and geospatial trends of hypertension management in Korea: a nationwide study 2002–2016. Korean Circ J. 2019;49:514–527. doi: 10.4070/kcj.2018.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and control of hypertension: JACC health promotion series. J Am Coll Cardiol. 2018;72:1278–1293. doi: 10.1016/j.jacc.2018.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 8.Verma AA, Khuu W, Tadrous M, Gomes T, Mamdani MM. Fixed-dose combination antihypertensive medications, adherence, and clinical outcomes: a population-based retrospective cohort study. PLoS Med. 2018;15:e1002584. doi: 10.1371/journal.pmed.1002584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung MH, Ihm SH, Lee DH, Chung WB, Jung HO, Youn HJ. Prehypertension is associated with early complications of atherosclerosis but not with exercise capacity. Int J Cardiol. 2017;227:387–392. doi: 10.1016/j.ijcard.2016.11.044. [DOI] [PubMed] [Google Scholar]
- 10.Halladay JR, Donahue KE, Cené CW, et al. The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: the heart healthy lenoir trial. Patient Educ Couns. 2017;100:542–549. doi: 10.1016/j.pec.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]