Abstract
Background:
The need for mentorship in aging research among postdoctoral trainees and junior faculty across medical disciplines and subspecialties is increasing, yet there is lack of senior personnel with expertise in aging to fulfill the traditional dyadic mentorship role. Facilitated peer mentorship is grounded in collaborative work among peers with the guidance of a senior mentor.
Methods and Results:
We evaluated the Columbia University Mentor Peer Aging Research (CoMPAdRE) program, an interprofessional facilitated peer mentorship program for early stage investigators, using the Reach Effectiveness Adoption Implementation and Maintenance framework.
Reach—
A total of 15 participants, of which 20% were women, from five states and across six medical specialties participated.
Efficacy—
Participants published 183 papers, of which over 20% were collaborative papers between CoMPAdRE mentees or mentees-mentor. Participants reported developing skills in negotiation, navigating the academic role, organizing a seminar, management, and leadership over the course of the program. According to the qualitative findings, the most important components of the program included alignment around the aging, learning from national leaders, and developing leadership skills and career networking.
Adoption—
Individual level factors included selecting participants with a research track record, willingness to sign a compact, and involvement in shaping the program. An institutional level factor that facilitated program adoption included strong commitment from Department leaders.
Implementation—
The program cost $3,259 per participant.
Maintenance—
CoMPAdRE is being maintained and is currently incorporating a second cohort of mentees.
Discussion:
This RE-AIM evaluation provides lessons learned and strategies for future adoption, implementation, and maintenance of an aging-focused facilitated peer mentorship program.
Keywords: Mentoring, aging, older adults, geriatrics, academic medicine, early career, faculty development, peer group, implementation science
INTRODUCTION
The traditional dyadic model between a mentee and senior mentor is the prevailing mentorship model at most academic medical centers.1,2 Challenges of this traditional model include difficulty identifying a mentor, maintaining the relationship over time, and considerable investment on the part of both partners.3 Given the scarcity of primary mentors with expertise in aging research, overreliance on the dyadic mentorship model is particularly detrimental to early stage investigators, especially women and minority faculty,4,5 in aging research.
Novel mentoring models are needed to meet the current needs of interprofessional junior faculty members who study and treat complex age-related diseases and phenotypes.6–9 One alternative is a facilitated peer mentorship model that includes elements of both dyadic and peer mentoring models.10 The peer mentorship component of this model provides a forum for mentees to discuss common needs and challenges that may have not been addressed in the dyadic mentorship relationship, including work-life balance, career advancement, negotiation, promotion, and collaborative research development. Peers effectively mentor each other through the process of brainstorming and modeling solutions to shared challenges, and in doing so may develop a sense of belonging that in turn leads to greater career satisfaction.
The Columbia Mentor Peer Aging Research Program (CoMPAdRE) was developed to address the need for facilitated peer mentorship that complements and supplements dyadic mentorship for early career clinical investigators with a focus on aging research. Instead of embarking on a quest for the perfect mentor, the underlying tenet of CoMPAdRE is for individuals to benefit from pursuing a strategy of being the “perfect” protégé-mentee, and to build a network of developmental relationships.3 At the completion of the two-year CoMPAdRE program, we evaluated the program using the implementation science of Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework.
METHODS
Participants
Fifteen early career mentees at the post-doctoral, instructor, or assistant professor levels participated in CoMPAdRE between March 2016 and May 2018 at Columbia University Medical Center. Participants were selected from across the country if they had an established mentorship from the facilitating senior mentor (MSM), and had an interest and/or track record in patient-oriented research with older adults.
Program Description
The program was structured around eight full-day retreats that occurred every four months. These day-long retreats included: 1) workshops focused on strategic key skills/knowledge necessary for success in academic medicine, 2) forums to share career aspirations and research interests, 3) time to develop collaborations, and 4) networking and mentorship from leaders in aging research. Sessions consisted of didactic sessions on career development and advancement, interactive discussions with leaders in aging research about their careers and the state of aging research, peer-to-peer discussions to address career challenges and develop collaborative investigations, and one-on-one mentorship discussions with the facilitating mentor and visiting faculty. Each participant also signed a compact of commitment, which requested that mentees commit to attending over 75% of sessions over two years (See Supplemental Table 1).
Program Development
Six months prior to the first CoMPAdRE retreat, the facilitating mentor and a program administrator solicited suggestions for speakers, career and research related topics, and optimal dates, duration, and frequency of the retreats from participants. The first five CoMPAdRE retreats were structured around the highest ranked topics and speakers. In order to gain experience in organizing a day-long workshop, participants were asked to organize the last three CoMPAdRE sessions around self-appointed topics.
There was consensus that an all-day program that met three times a year was optimal. The structure for each session included breakfast, followed by a brief presentation by the facilitating mentor on participants’ accomplishments, including publications in the last 3 months, grants submissions and awards, academic milestones (e.g., promotions, awards, and invited lectures), and personal life events (e.g. marriage, children). A morning session began including didactics, discussion, and small-group work for 1.5 hours that focused on one of the career development topics participants initially selected, followed by the invited faculty member’s seminar. Seminars focused on how the faculty member’s career developed, including successes and failures, and suggestions for advancement, enjoyment, and scientific areas that they thought were promising and novel. Subsequently, participants had further facilitated discussions with visiting faculty about career and research advancement. The afternoon session was followed by dinner together, with the goal of further facilitating relationship development and networking.
Reach Effectiveness Adoption Implementation and Maintenance (RE-AIM) Implementation Science framework
The RE-AIM model is an implementation science framework for evaluation that focuses on the: reach of the intervention to a representative proportion of the target population; effectiveness of a program on specific outcomes; adoption of the program in a specified setting; and details of program implementation and maintenance.11,12
Data Sources and Measurements
We assessed program effectiveness based on (1) participant publications, grants, and career advancements that were achieved during the two-year program, and (2) participant feedback from a structured survey that we administered at the end of the two-year program. We ascertained participant publications, and classified them as first-author, senior author, and/or co-authored with a CoMPAdRE participant. We ascertained participant grants from NIH Reporter. Prior to each CoMPAdRE retreat, participants’ reported recent honors/awards, grant submissions, and conference presentations. At the end of the program, we used Qualtrics Survey software to administer a 16-item survey to assess improvement in grantsmanship, organizational, leadership, and research skill development on a 7-response Likert scale. The survey included solicited open-ended feedback about the strengths and weaknesses of CoMPAdRE, challenges to participation, and aspects of the program that might need to be changed or improved. The study was approved by the Columbia IRB (Protocol AAAR8784).
Data Analysis
We report standard descriptive statistics for the quantitative data. The qualitative data from the open-ended questions of the Qualtrics survey were analyzed by directed content analysis. This method uses factors from a relevant theory to guide data collection and analysis. A codebook of themes based on the factors in the RE-AIM framework was created. Qualitative data were analyzed using the codebook, and sub-themes were created when appropriate.13,14
RESULTS
Reach
There were 15 participants from 7 academic programs representing 5 states (Table 1). Overall, 20% were women, 25% were Asian and 7% Hispanic. At the start of the program, 67% of participants were faculty at the position of assistant professor or instructor, 33% were trainees and 60% of participants were federally funded (T32 programs, K23 awards, and Paul B. Beeson Emerging Leaders Career Development Award in Aging awards).
Table 1:
Reach and Effectiveness of CoMPAdRE
| Reach, participant characteristics at baseline (May 2016) (n=15) | |
| Age (mean ±SD), years | 36 (± 3.4) |
| Female Gender | 3 (20 %) |
| Race/Ethnicity | |
| White | 10 (66 %) |
| Asian | 4 (25 %) |
| Hispanic/Latino | 1 (7 %) |
| Highest Academic Degree | |
| PhD | 4 (27%) |
| MD | 11 (73%) |
| Clinical Specialty | |
| Cardiology | 9 (60%) |
| Nephrology | 1 (7 %) |
| Pulmonary-Critical Care | 1 (7%) |
| Psychology | 2 (13%) |
| Statistics | 1 (7%) |
| Nursing | 1 (7%) |
| Mentees with federal funding at baseline | 10 (66%) |
| K23 | 6 (40%) |
| T32 | 2 (13%) |
| Beeson K23 Award | 2 (13%) |
| Effectiveness, Peer-reviewed articles published, n= 183 | |
| First-authored | 76 (42%) |
| Senior-authored | 40 (22%) |
| Published by 2+ CoMPAdRE participants | 9 (5%) |
| Published by a CoMPAdRE participant and mentor | 31 (17%) |
| Effectiveness, Grantsmanship | |
| Principal Investigator awarded federal grants | 10 (66%) |
| GEMSTAR R03 | 2 (13%) |
| K99/R00 | 1 (7%) |
| KL2 | 1 (7%) |
| R21 | 3 (20%) |
| R01 (or VA equivalent) | 3 (20%) |
Effectiveness
CoMPAdRE participants published 183 publications, of which 20% were co-authored between CoMPAdRE mentees and the mentor. Mentees were awarded a total of 10, K or R-level awards as Principal Investigators. At the completion of the program, 93% of participants were federally funded as Principal Investigators on either a K or R-level awards.
Nearly all participants (91%) agreed or strongly agreed that CoMPAdRE supported their organizational and leadership skills development, particularly in regards to negotiation skills, navigating their academic role and promotion (Figure 1A). Participants reported that CoMPAdRE especially supported the development of research and grantsmanship skills in relation to interacting with peers and reviewers, and less so with learning about the geriatrics research literature or grant writing (Figure 1B). Nearly all participants agreed or strongly agreed that CoMPAdRE provided a forum to develop peer relationships, research collaboration, and a national network (Figure 1C).
Figure 1.
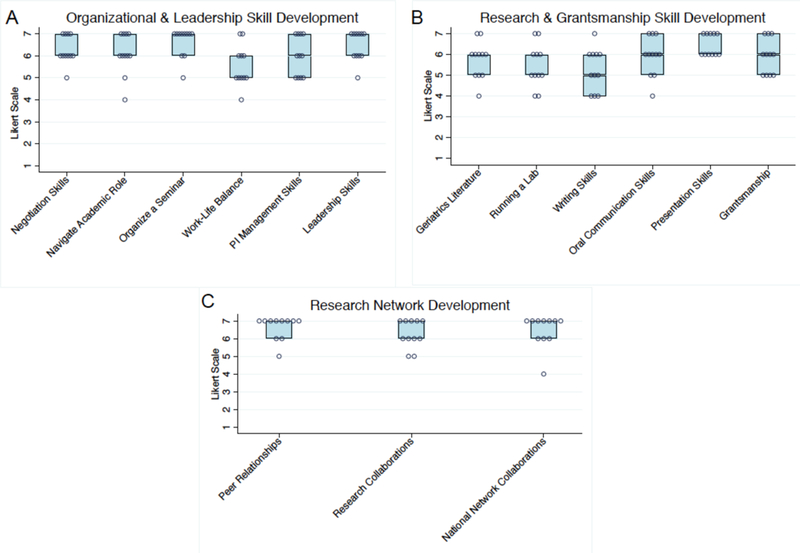
Ratings of how CoMPAdRE peer mentorship supported (A) organizational and leadership skill development, (B) research and grantsmanship skill development, and (C) research network development. Boxes represent median and interquartile ranges, and dots represent individual participant ratings. Likert Scale: Strongly Disagree (1), Disagree (2), Somewhat Disagree (3), Neither Agree nor Disagree (4), Somewhat agree (5), Agree (6), Strongly Agree (7).
Qualitative findings
There were four primary themes that emerged from the open-ended post-implementation survey which are described below: Alignment around Aging, Learning from National Leaders, Leadership and Executive Skills, and Career Networking and Promotion.
Alignment Around Aging
A core component of this program was the alignment of “like-minded individuals across multiple disciplines where aging research is the common thread.” The focus on aging brought together “peers with expertise in all different areas, but a common passion for geriatrics.” Bringing together a group of individuals from different medical disciplines and states who shared a research focus on aging provided a community that helped each participant advance their career. One participant noted that it helped to stave off the “existential crisis” that is common when facing the early academic medicine career challenges at institutions that do not have robust aging research programs with strong mentorship in place.
“CoMPAdRE provides a research network to discuss and discover new ideas for investigation. The fact that medical sub-specialists with different backgrounds come together with a shared interest in gerontology opens a younger investigator’s perspective on aging research beyond the small group of investigators that a young investigator is likely to spend most of her/his time with.”
Learning from National Leaders
Overall, there were 20 visiting faculty (8 from Columbia and 12 from other institutions) of diverse areas of scholarship who described their career trajectories, presented their paths of scientific discovery, and facilitated peer mentorship. Inviting leaders in gerontology gave participants the rare opportunity to speak with and learn from them directly about unique professional mechanisms for acquiring data, and specific aging-related grant mechanisms.
“It’s also been a privilege to get to hear from all the incredible speakers and because of the small size to get an opportunity to interact with them as well. I particularly appreciate that there were several highly accomplished women speakers.”
A unique aspect of the program was having highly successful visiting faculty who were willing to discuss their career paths—including successes and failures—and to have the structure of “small groups with the ability to plan programs focused on individual needs.”
“Hearing from leading gerontologic researchers (who are known for success) about both their success, and more importantly, their failures during their illustrious careers helps alleviate the stress of obstacles and failures in one’s own career.”
Leadership and Executive Skills
A core component of the program was teaching early career trainees about leadership and executive skills that many participants noted was missing from their training.
“CoMPAdRE provides a forum to formally teach leadership and executive skills. These skills, that make up the core of graduate business school education, are not taught during doctoral or post-doctoral training in medicine. However, these skills are likely just as necessary for PI’s [Principal Investigators] and other leaders in academic medicine as they may be in the business world. Having formal instruction and informal seminars about leadership and executive skills help early stage investigators progress to being effective PI’s.”
Career Networking and Promotion
CoMPAdRE was described as “widely applicable to all levels of training and career paths.” The inclusion of peer-mentees from across institutions facilitated building a network that was instrumental for mentees who made transitions from training to faculty and advancing faculty roles during the tenure of the program.
“It is so important to have friends and colleagues outside of one’s home institution in order to broaden perspectives and find other co-Investigators for multi-site studies.”
Being affiliated with CoMPAdRE facilitated sponsorship. Participants reported that the program helped with the promotion process by supporting national reputation and helped to forge collaborations with other mentees and visiting faculty.
Adoption
Both individual and institutional aspects facilitated the successful adoption of CoMPAdRE. All participants had a track record of clinical research experience in aging, signed a compact to participate in the two-year program, and had a high level of buy-in since they themselves chose the topics to address at each session. Institutional level factors that supported the adoption of CoMPAdRE program included: minimal financial commitment because the CoMPAdRE programming costs were supported by a NIA K24 award (PI: Maurer), Division and Department Chiefs agreeing to protect participants’ time away from work to participate in the day-long retreats, and travel expenses for non-local participants.
Implementation
We identified themes and lessons learned related to the implementation of the program based on participants’ feedback (Table 2). Of note the CoMPAdRE program required a facilitating mentor as well as administrator to support the logistics. Participants valued learning through interacting with other early stage investigators from diverse medical disciplines and subspecialties (e.g.: psychology, nursing, informatics, statistics). Participants preferred a balance of male and female speakers from outside of the hosting institution because it gave them the opportunity to discuss sensitive topics like promotion and tenure. Participants reported high satisfaction with being able to interact personally with internationally recognized leaders in aging research, which in some instances led to publications and grant applications with these leaders.
Table 2:
Adoption, Implementation and Maintenance: Lessons learned for future implementation
| Selection criteria | • It was beneficial to include trainees who already obtained a K award as well as those who planned to submit K award. • Participants who had not written a K award reported learning a lot from those who had been awarded one. |
| Value of diversity | • Participants should intentionally select a balance of participants across gender, race/ethnicity and professions. “I think it would have been nice to see more women in the peer group… I really appreciated the effort to bring women speakers in who were all highly accomplished.” “There can also be challenges to the group being multi-disciplinary, including struggling to form productive peer relationship if you are in an ‘underrepresented’ discipline.” |
| One-on-one time | • Participants wanted to have more one-on-one time with the visiting faculty to build those relationships and get to know them personally |
| Ongoing evaluations | • Completing a mid-term evaluation after the first year to make any suggested modifications and complete faculty evaluations at the end of each session |
| Retreat timing (frequency/duration) | • Participants noted that the frequency and duration (3 times/year for a full Friday) was ideal. |
| Retreat organization | • Participants reported that they appreciated having the first year of sessions designed for them and then taking the lead on developing a full session of programming in the second year. |
| Timing in tandem with a conference to minimize travel | For those who are traveling for the retreats one suggestion was to hold them in tandem with a national conference and getting the program approved for CMEs. “At the least, it seems like we could try to get the [geographically local] people together or potentially try to arrange something at meetings such as AGS.” |
| Participant involvement | • Facilitating more of the speakers to give talks on their current research so that it was clear where points of collaboration may be. • Tapping the resources within the group also enables more of a shared understanding of methods, consistent outcome measurement and methods for measurement that are applicable to all participants. • New ideas include inviting basic scientists to present to broaden perspectives and knowledge about basic scientific principles and how they inform a translational perspective. |
| Communication between meetings | There are some modifications that were suggested moving forward with the program including more electronic communication between meetings: “It would be great to continue to have some electronic interaction and way of keeping up with the group as a whole….I know it’s a challenge with people being all over the country and at different institutions to consider something in person.” |
| Grantsmanship | • Moving forward one suggestion is to focus a retreat topic exclusively on co-writing grants so that more collaborative grants can come from this group. “It would be really helpful to have opportunities to come together for day-long grant writing or manuscript writing sessions together to carve out time to make that happen.” “I wasn’t in the right stage of my career to write a collaborative R01—I needed to get my first one.” |
| Addressing barriers | • For individuals, the largest reported barrier to collaboration was balancing that with competing clinical, administrative and research demands. |
Funding for the implementation of the program was provided through a NIA K24 mentoring grant. In all, the program functioned for two years at a total cost of $48,898, which is equivalent to $3,259 per participant. The top three areas for spending included travel for participants and faculty (37%), renting space and lodging for out-of-town participants and guest faculty (27%), and catering (17%) (Supplemental Figure 1).
Maintenance
The development of the program around the needs of the CoMPAdRE participants was the most important dimension to support maintenance of the program—in this case, supporting mentees in their transitions from early stage investigators to independent investigators was the primary aim. Participants noted a strong need to develop administrative and management skills, and mentoring skills as they themselves become mentors. Topics that participants wanted more of in the future included: 1) continued leadership and executive training, 2) reviewing grants collaboratively and with strategic scheduling in order to provide one another with feedback at least 2 months prior to submission deadlines, and 3) having peer participants present more of their own work in order to generate new perspectives within the peer mentorship group, and to be able to think through the development of grant ideas together. Overall, CoMPAdRE provided a strong peer network such that participants chose to continue the program after the last session in May of 2018. One of the primary reasons was the ongoing opportunity to connect with peers at other universities:
“I could foresee that this network would continue as we start to mentor our own trainees, and we can put these trainees in touch with our CoMPAdRE peers and perhaps their trainees.”
DISCUSSION
An evaluation of the CoMPAdRE facilitated peer mentorship program using the RE-AIM framework provides insights for dissemination to other institutions. The principal findings of this evaluation were that the CoMPAdRE aging facilitated peer mentoring program supported the development of participants’ executive skills and overall career advancement towards becoming independent clinical investigators. The program expanded and strengthened participants’ interprofessional networks in aging. In turn, participants published collaborative research projects, secured faculty jobs, and were promoted.
There is a lack of diversity in leadership in academic medicine, particularly among women and racial and ethnic minorities.15,16 Facilitated peer mentorship may of particular benefit to minority groups by facilitating a professional network that is requisite to obtaining national reputation and academic promotion.4 Facilitated peer mentorship programs may be one mechanism to address the disparities that exist at the associate and full professor levels at the majority of academic medical centers and major universities.17,18
The facilitated peer mentor model also benefits the facilitating mentor by providing a regularly scheduled opportunity to meet with mentees both collectively and individually during the one-day retreats. In CoMPAdRE, the facilitating mentor was able to provide mentorship to a larger cadre of mentees than would be feasible with a traditional dyad model of mentorship.9 While the facilitating mentor continued to provide one-on-one feedback to mentees, the feedback was focused on specific projects rather than broader mentorship topics which were addressed in the CoMPAdRE sessions. Our finding is in contrast to a systematic literature review that concluded that significant time commitment by mentors is a barrier to creating peer mentorship programs.19
Strengths and Limitations
The geographic diversity of participants was both a strength and a weakness of the program. The geographic diversity provided a more diverse perspective on career development and research challenges, and created an opportunity for cross-institution networking and yet it also made it more expensive (due to airfare and hotel costs) and more complex to schedule the retreats. A limitation of the first CoMPAdRE cohort was a lack of gender and racial/ethnic diversity; however, this has been addressed in the second CoMPAdRE cohort.
An expected challenge of the program was attrition of active attendance at the sessions (~13%). There were a few attendees who were not able to attend as frequently because of the travel and other work-life demands. To adjust for attrition after two years, we invited new participants into the second CoMPAdRE cohort.
One of the original hypotheses of the program was that it would support multi-PI R01 grants; however, there were no multi-PI R01s submitted in the first two years of the program. At the start of CoMPAdRE, none of the participants had an R01. Thus, grantsmanship skill development focused on either obtaining either a K or the first R01 award, rather than multi-PI awards. In addition, all of the reported effectiveness outcomes (i.e. grants and publications) associated with the CoMPAdRE program are not necessarily due to skills and networks created by the program.
A typical challenge for peer-mentorship programs is that they are typically funded through time-restricted funds,19 which limits long-term sustainability. The CoMPAdRE program could be implemented for less if mentees were within the same geographic area (obviating the need for travel costs). Additional savings could also accrue through local access to more economical food and venue choices.
CONCLUSION
Advancing aging research that addresses the unmet needs of older adults with complex phenotypes from heterogeneous populations requires interdisciplinary collaboration between faculty who are traditionally siloed by medical specialty or discipline at large academic medical centers. The CoMPAdRE program shows that a facilitated peer mentorship program can bring together diverse individuals to collaborate on high-quality multidisciplinary aging research, and in turn, collectively promote career advancement. A facilitated peer mentorship program focused on aging might be most effective for participants from institutions which do not already offer a comprehensive geriatric medicine training program, of which there are few.20 For those that already have such a program, this might augment the resources already being provided and extend the reach of the program. Topically-focused facilitated peer mentorship programs could be expanded to many other research areas that require interprofessional collaboration, including immunology, neuroscience, and minority health among others. As such, there is strong potential for broad generalizability and potential to be an important and cost-effective resource for early career faculty members. A cost-effectiveness analysis was conducted at the UCSD National Center for Academic Medicine and found that peer-mentorship programs are cost-effective.21
Supplementary Material
This figure shows the breakdown of total costs for the CoMPAdRE peer mentorship program.
Columbia Mentor Peer Aging Research Program compact
Curriculum for the first eight CoMPAdRE sessions including themes, topics, exercises, assignments and faculty speakers
Impact Statement
The need for mentorship for the development of early career investigators is especially critical for the care of older adults in which an interdisciplinary approach is necessary. Yet, there is a relative lack of senior investigators in aging research across medical subspecialties to meet this growing demand for mentorship. A group of early stage investigators focused on patient-oriented research and practice participated in an interprofessional facilitated peer mentorship program, Columbia University Mentor Peer Aging Research Program (CoMPAdRE), with the aim of facilitating career growth towards becoming independent clinical investigators in aging research. We evaluated the program using the Reach Effectiveness Adoption Implementation and Maintenance (RE-AIM) framework. This work is novel insofar as we employed a standardized implementation science approach to identify multiple factors that facilitated and supported the adoption, implementation, and maintenance of a facilitated peer-mentorship program for early stage investigators focused on aging research. The potential impact of this research includes dissemination of a facilitated peer mentorship model to support interprofessional early career mentorship in aging research.
Acknowledgements
We would like to acknowledge the administrative assistance of Dr. Sergio Teryua and Samantha Guadalupe from the Clinical Cardiovascular Research Laboratory for the Elderly, Allen Hospital of New York Presbyterian, Columbia University Irving Medical Center. We would also like to thank all of the CoMPAdRE members for their commitment to the facilitated mentorship program. Finally, we would like to acknowledge the guest faculty (named in Supplemental Table 2), most of whom volunteered their time to come and speak to the CoMPAdRE participants.
Funding sources:
National Institutes of Health/National Institute on Aging (NIA)
Mid-Career Mentoring Award in Geriatric Cardiology, K24: AG036778 (PI: Maurer)
National Institutes of Health/National Institute of Nursing Research, R00: NR016275 (PI: Masterson Creber)
National Institutes of Health/National Institute on Aging (NIA) K23: AG045560 (PI: Baldwin)
National Institute for Mental Health, K23: MH099097 (PI: Brown)
NIH/National Institute on Aging, Patient Oriented Career Development Award, K23 AG052463 (PI: Dodson)
National Institutes of Health/National Institute on Aging (NIA)
R03:AG053294 (PI: Rao)
National Institutes of Health/National Institute on Aging (NIA)
R03: AG056446 (PI: Goyal)
Veterans Administration
5I01 CX001636 (PI: Hummel)
Sponsor’s Role: None
Footnotes
Conflict of interest:
No authors have any COI to disclose.
REFERENCES
- 1.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Academic medicine : journal of the Association of American Medical Colleges. 2013;88(7):1029–1037. [DOI] [PubMed] [Google Scholar]
- 2.White HK, Buhr GT, Pinheiro SO. Mentoring: a key strategy to prepare the next generation of physicians to care for an aging America. J Am Geriatr Soc. 2009;57(7):1270–1277. [DOI] [PubMed] [Google Scholar]
- 3.Beyond the Myth of the Perfect Mentor: Building a Network of Developmental Relationships. Harvard business review. 1998:1–12. [Google Scholar]
- 4.Varkey P, Jatoi A, Williams A, et al. The positive impact of a facilitated peer mentoring program on academic skills of women faculty. BMC medical education. 2012;12:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson JC, Williams B, Jayadevappa R. Mentoring program for minority faculty at the University of Pennsylvania School of Medicine. Academic medicine : journal of the Association of American Medical Colleges. 1999;74(4):376–379. [DOI] [PubMed] [Google Scholar]
- 6.Maurer MS. Heart Failure With a Normal Ejection Fraction (HFNEF): Embracing Complexity. Journal of Cardiac Failure. 2009;15(7):561–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maurer MS, Mancini D. HFpEF: is splitting into distinct phenotypes by comorbidities the pathway forward? J Am Coll Cardiol. 2014;64(6):550–552. [DOI] [PubMed] [Google Scholar]
- 8.Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric Syndromes: Clinical, Research and Policy Implications of a Core Geriatric Concept. Journal of the American Geriatrics Society. 2007;55(5):780–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pololi LH, Knight SM, Dennis K, Frankel RM. Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program. Academic medicine : journal of the Association of American Medical Colleges. 2002;77(5):377–384. [DOI] [PubMed] [Google Scholar]
- 10.DeCastro R, Sambuco D, Ubel PA, Stewart A, Jagsi R. Mentor networks in academic medicine: moving beyond a dyadic conception of mentoring for junior faculty researchers. Academic medicine : journal of the Association of American Medical Colleges. 2013;88(4):488–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999;89(9):1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. 2006;21(5):688–694. [DOI] [PubMed] [Google Scholar]
- 13.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 14.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse education today. 2004;24(2):105–112. [DOI] [PubMed] [Google Scholar]
- 15.Yedidia M, Bickel J. Why Aren’t There More Women Leaders in Academic Medicine? The Views of Clinical Department Chairs. Academic Medicine. 2001;76(5):453–465. [DOI] [PubMed] [Google Scholar]
- 16.Lewis D, Paulsen E. Proceedings of the Diversity and Inclusion Innovation Forum: Unconscious Bias in Academic Medicine Washington DC2017. [Google Scholar]
- 17.American Association of Medical Colleges. Striving Toward Excellence: Faculty Diversity in Medical Education. 2009. [Google Scholar]
- 18.Efstathiou JA, Drumm MR, Paly JP, et al. Long-term impact of a faculty mentoring program in academic medicine. PLoS One. 2018;13(11):e0207634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Academic medicine : journal of the Association of American Medical Colleges. 2013;88(4):541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller AP, Maurer M, Alexander KP. Geriatric Cardiology. Journal of the American College of Cardiology. 2018;71(25):2970–2973. [DOI] [PubMed] [Google Scholar]
- 21.Wingard DL, Garman KA, Reznik V. Facilitating faculty success: outcomes and cost benefit of the UCSD National Center of Leadership in Academic Medicine. Academic medicine : journal of the Association of American Medical Colleges. 2004;79(10 Suppl):S9–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This figure shows the breakdown of total costs for the CoMPAdRE peer mentorship program.
Columbia Mentor Peer Aging Research Program compact
Curriculum for the first eight CoMPAdRE sessions including themes, topics, exercises, assignments and faculty speakers


