Arthroplasty-Cervical
P001: Intravenous and Local Steroid Use in the Management of Dysphagia After Anterior Cervical Spine Surgery: A Systematic Review of Prospective Randomized Controlled Trials
Jingwei Liu1 and Yong Hai1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: The anterior approach is commonly used to treat numerous cervical spine pathologies. Dysphagia following anterior cervical spine surgery (ACSS) is one of the most common complications, with the reported incidence from 1.7% to 88%. Previous studies indicated that dysphagia was more severe and easily occurred in the early stage postoperatively. And up to 26% patients got dysphagia persisting more than 1 year, which troubled them for a long time. A lot of preventative measures have been used to decrease the incidence of dysphagia after ACSS. The use of intravenous and local steroids has been reported an effective way but stills remains controversial. The purpose of this review was to evaluate intravenous and local steroid use in the management of dysphagia after ACSS by performing a systematic review of all randomized controlled trials (RCTs). Methods: We searched the databases PubMed, EMBASE, Clinical Key, the Cochrane Library, and the Wiley Online Library without time restriction using the terms “dysphagia” or “odynophagia” or “swallowing disorder,” “steroid,” and “anterior cervical spine surgery.” RCTs were selected, and effects of intravenous and local steroids were investigated from these studies. Results: The initial search yielded 67 citations. Six of these studied met the inclusion and exclusion criteria. All of them were prospective RCTs, which were evaluated as level 1 evidence. One study found that perioperative intravenous steroid use is not effective in reducing severity of early postoperative dysphagia after 1-level ACDF (anterior cervical discectomy and fusion), while 5 studies suggested that perioperative intravenous and local steroid use seemed to be more effective on reducing incidence and severity of early dysphagia after multilevel ACSS. One double-blinded study still found that locally administered depomedrol on a collagen sponge significantly decreases early dysphagia incidence and severity after ACSS using low-dose BMP. Conclusion: Perioperative intravenous and local steroid use could reduce incidence and severity of early dysphagia after ACSS postoperatively especially for multilevel surgeries. For the patients who underwent revision surgery or at high risk for pseudarthrosis having to use BMP during surgery locally administered depomedrol on a collagen sponge was suggested to decrease early dysphagia incidence and severity after ACSS.
P002: Total Disk Arthroplasty Combined With Fusion Versus 2-Level Fusion in Surgical Treatment of 2-Level Cervical Disk Degeneration
Vadim Byvaltsev1, Marat Aliev1, Bobur Yussupov1, Bakhyt Aglakov1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: The purpose of this study was to compare the clinical and radiologic outcomes of cervical total disc arthroplasty (CDA) combined with anterior cervical discectomy and fusion (ACDF) and 2-level ACDF in patients with 2-level cervical disc degeneration. Materials and Methods: Between 2012 and 2018, 88 patients undergoing 2-level cervical disc surgery at our clinical hospital were identified who met the following surgical indications: 2 consecutive level degenerative disc disease between C3-C4 and C6-C7; either a radiculopathy or myelopathy; and no response to conservative treatment for >6 weeks. Twenty-three patients of the hybrid surgery group were matched to 27 patients of the 2-level fusion group based on age and gender. Patients were asked to check the Neck Disability Index (NDI) and grade their pain intensity before surgery and at routine postoperative intervals of 3, 6, 12, 24, and 36 months. Dynamic flexion and extension lateral cervical radiographs were obtained in the standing position before surgery and at routine postoperative intervals of 3, 6, 12, 24, and 36 months. The angular range of motion (ROM) for C2-C7 and adjacent segments were measured using the Cobb method. Results: The hybrid surgery group had better NDI recovery 1 and 2 years after surgery (P = .034). Postoperative neck pain was less in the hybrid surgery group 3 months and 1 year after surgery (P = .027). There was no difference in arm pain relief between the groups. The hybrid surgery group showed faster C2-C7 ROM recovery. The mean C2-C7 ROM of the hybrid surgery group recovered to that of the preoperative value, but that of the 2-level fusion group did not (P = .038). The inferior adjacent segment ROM showed significant differences between the groups 6 and 12 months, and 1 and 2 years after surgery (P = .021 and P = .019, P = .042 and P = .012, respectively). Conclusion: CDA combined with ACDF is superior to 2-level fusion in terms of better NDI recovery, less postoperative neck pain, faster C2-C7 ROM recovery, and less adjacent ROM increase.
P003: Cervical Disk Arthroplasty for the Treatment of Cervical Degenerative Disk Disease: 5-Year Follow-up Results
Vadim Byvaltsev1, Marat Aliev1, Bakhyt Aglakov1, Bobur Yussupov1, Evgenii Belykh1, Ivan Stepanov1, and Andrei Kalinin1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: The purpose of this study is to present the long-term results and to evaluate the safety and effectiveness of cervical disc arthroplasty in treatment of patients with symptomatic cervical degenerative disc disease. Materials and Methods: A total of 113 patients were analyzed before surgery, after disc replacment and at 3 months, 6 months, 12 months, 24 months, 36 months, 48 months, and 60 months after total disc arthroplasty. Clinical assessments included visual analogue scale (VAS) and Neck Disability Index (NDI) scores. Radiographic assessments included cervical lordosis (CL), intervertebral disk height (IDH), and range of motion (ROM) of the total cervical spine. Complications at the 5-year follow-up were collected as well. Results: Mean follow-up period was 60.12 months. There was clinical improvement in terms of VAS and NDI from the preoperative to the final follow-up (P < .02). Overall, ROM of the total cervical spine was maintained during the follow-up. Statistically significant (P < .05) improvements in the trend of IDH and CL were noted at the follow-up. Seventeen patients were observed an appearance of heterotopic ossification at the 5-year follow-up, with 13 patients appeared at Class II and 4 patients at Class III. Adjacent segment degeneration assessed by radiographic evidence was found in 2 patients. Conclusion: Cervical disc replacement showed significant improvement in clinical outcomes at 5 years. It not only effectively preserves the motion of both total cervical spine and operated segments, but also restores normal IDH and CL up to 5 years postoperation.
P004: Does It Differ in Neck Pain, Function, and Range of Motion After Anterior Cervical Fusion, Disc Replacement, and Posterior Foraminotomy?
Guang-Xun Lin1, Jin-Sung Kim1, Akaworn Mahatthanatrakul1, and Hussam Jabri1
1Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
Introduction: Cervical radiculopathy is a condition of arm pain that causes cervical herniated disc (CHD), foraminal stenosis, and degenerative disc disease. In most patients, symptoms are resolved without surgery. However, if conservative treatment fails, surgical intervention is essential. Traditionally, anterior cervical discectomy and fusion (ACDF) has developed as a standard surgical technique for treatment of radiculopathy. It is usually reported as a safe and sufficient technique that has long-term clinical and radiological successfully outcomes. Despite these advantages, ACDF dose have inherent disadvantage, including access complications, loss in motion of segment, pseudarthrosis, and the potential accelerated degradation at adjacent segments. To preserve and decrease these problems, cervical disc replacement (CDR) and posterior cervical foraminotomy and/or discectomy (PCF) have been developed as acceptable surgical routes for treatment of radiculopathy. Recently, a minimally invasive surgery that uses a tubular retractor or a full-endoscopic system has been introduced. Although the literature reports good results in their respective surgical treatment of CDH, the results after surgery have not been directly compared among the 3 groups. The purpose of this study was to investigate the clinical and radiological results and biomechanical changes after ACDF, CDR, and PCF in individuals with unilateral single-level cervical radiculopathy. Material and Methods: Ninety-seven patients followed-up more than 12 months after surgery for cervical unilateral radiculopathy from February 2012 to August 2017 were enrolled in this study. Patients with myelopathy and large central disc herniation were excluded. Clinical outcomes included Neck Disability Index (NDI), visual analogue scale (VAS) for neck and arm pain scores, and modified Odom criteria. The range of motion (ROM) of whole cervical (C-ROM), the operated segment (S-ROM), and the upper and lower adjacent segment (U-ROM and L-ROM) were measured. Results: A total of 55 ACDFs, 21 CDRs, and 21 PCFs were performed. There were no differences in the preoperative NDI and VAS scores among the groups (P > .05). The clinical improvement in NDI and VAS scores were significantly after surgery (P < .05); however, there was no statistical significance among the groups (P > .05). The S-ROM, U-ROM, and L-ROM were slightly increased in both of CDR and PCF groups without statistical significance (P > .05). The C-ROM was significantly increased in CDR group (P = .04) and slight increase in PCF group (P = .27). In ACDF group, the C-ROM was decreased (P = .21), on the contrary, the U-ROM and L-ROM were increased (P > .05). Conclusion: ACDF, CDR, and PCF can expect a relieve pain, an improvement in neck function and ROMs for patients with unilateral radiculopathy. Comparatively, ACDF provides with the lowest reoperation rate. Perhaps the PCF may have a higher probability of reoperation, however, the ROMs after surgery is better than ACDF.
P005: Combined Use of Anterior Arthrodesis and Arthroplasty for the Treatment of Multilevel Cervical Degenerative Disc Disease: Functional and Radiological Result at 5 Years
Daniel Hernandez Acevedo1, Amado Gonzalez1, Miguel Fuentes1, Gabriel Huerta1, and Hugo Santos1
1ISSEMYM Medical Center, Ciudad de Mexico, Mexico
Introduction: Degenerative cervical disc disease (DCDD) is the second cause of consultation in the services of spinal surgery. Ten percent evolves to cervical spondylotic myelopathy being catastrophic due to its high degree of disability. The approximate start is at 35 years. Surgical decompression is an effective option for the treatment of DCDD where it mainly seeks to eliminate neural compression, decrease degeneration, preserve mobility, improve the sagittal balance, and to avoid the adjacent segment disease. Material and Methods: We evaluated the clinical, functional, and radiographic evolution of patients undergoing anterior cervical hybrid surgery by means of arthroplasty and arthrodesis in 2 or 3 segments over a period of 5 years. In a multicenter, observational, retrospective, and longitudinal study, clinical-functional evolution was determined with the Neck Disability Index (NDI) and the Nurick scale in the preoperative and a 12-month follow-up. The mobility of disc prosthesis were determined in lateral projections 12 months after surgery, and 3° to 15° is considered a good outcome. Results: A total of 91 patients, 56 females (61.53%), 35 males (38.46%), average age 46.74 years. Eighty-three patients (range of 27-63 years) underwent surgery of 2 levels (91.2%) and 8 patients undergoing surgery of 3 levels (8.8%) follow-up to 18.72 months on average (range of 12-24 months), segment C5-C6 was the most affected with 81 patients (89%), a total of 190 implants were placed, of which 99 were PEEK (polyetheretherketone) cages and 91 disc prostheses. Presurgical NDI: 2 patients (2.19%) had mild disability, 27 (29.67%) moderate, 32 (24.17%) severe, and 30 (32.96%) complete disability. Postsurgical NDI: 28 (30.76%) without disability, 51 (56.04%) mild, 10 (10.98%) moderate, and 3 (3.29%) severe or functional disability (P < .05). Nurick preoperative: 3 patients (3.29%) grade 0, 50 (54.94%) grade I, 30 patients (32.96%) grade II, 8 patients (8.79%) grade III, 0 grade IV, and 0 grade V. Nurick postoperative: 64 (70.32%) grade 0, 26 (28.57%) grade I, 0 grade II, 1 (1.09%) grade III, 0 grade IV, and 0 grade V (P < .05). In the dynamic lateral projections, 86 patients (94.5%) had adequate prosthetic mobility (3-5°), and only 5 patients (5.5%) did not have good prosthetic mobility (<3°).Seven patients (7.69%) did not have good clinical course, mainly associated with segmental instability. Of these, only 4 required revision surgery, implant removal with anterior plate placement. No patient required corpectomy. Conclusion: The use of arthrodesis of one or several cervical segments predisposes to evolve to an adjacent segment disease (ASD). It is important to consider arthrodesis in the most affected segments and arthroplasty in the least affected, especially in young patients to avoid ASD. The cervical sagittal balance should also be considered for the good evolution in postoperative patients of cervical hybrid surgery. Our study shows a favorable result with regard to the NDI and Nurick scale with statistical significance and shows good mobility of disc prothesis 12 months after surgery. There is a favorable clinical-functional and radiographic evolution in postoperative patients of anterior cervical hybrid surgery in 2 or 3 levels after 12 months of follow-up.
P006: The Feasibility of Optimal Surgical Result Prediction According to the Center of Rotation Shift After Multilevel Cervical Total Disc Replacement
Jun Ho Lee1
1Kyung Hee University Medical Centre, Seoul, Republic of Korea
Introduction: This study investigates the relationship between the shifted locations of center of rotation (COR) at each cervical level and subsequent surgical outcomes after multilevel cervical total disc replacement (MCTDR) and identifies radiological parameter that corresponded to change of COR after MCTDR. Material and Methods: The study included a consecutive series of 24 patients who were treated with MCTDR following the diagnosis of multilevel cervical disc herniation or stenosis. Numeric Rating Scale (NRS), range of motion (ROM) at both C2-7 segment and TDR implanted levels, and location of COR at TDR implanted level were evaluated at pre- and post-MCTDR. These parameters were compared between patients who experienced successful and unsuccessful pain relief. Results: The inherent CORs relatively at ventrocranial coordinates have demonstrated significant migrations to dorsocaudal locations at each cervical levels, more prominent shifts for the successful group, after MCTDR switch. The unsuccessful group showed markedly reduced C2-7 ROM and reduced angular improvement at C2-7 as well as MCTDR level after surgery in comparison to the successful group. Postoperative C2-7 ROM was related to postoperative COR along the x-axis. Conclusion: The crucial determinants for clinical success after MCTDR, other than mere preservation of the ROM both at C2-7 and TDR implanted levels, was the restoration of COR from ventrocranial location at degenerated cervical motion segment close to normal coordinates by posterior and inferior shifts after MCTDR. The position of COR along the X-axis after MCTDR was important factor to determine maintenance of C2-7 ROM.
P007: The Relation Between Laminar Closure and Plate Density After Open-Door Cervical Laminoplasty With Miniplate Fixation
Hironori Tsuji1, Haruo Misawa1, Tomoyuki Takigawa1, Yasuyuki Shiozaki1, Sosuke Muraoka1, and Toshifumi Ozaki1
1Okayama University Hospital, Okayama City, Japan
Introduction: The laminar closure (LC) is known as an early complication of open-door cervical laminoplasty, and cervical miniplates can be used for preventing LC. Though the relation between the number or the position of the miniplates and LC is unclear. The aim of this study is to evaluate between miniplate setting methods and LC after open-door cervical laminoplasty. Material and Methods: After informed consent, 46 patients who underwent open-door cervical laminoplasty using miniplates, 164 laminas are included in this study (32 men, 14 women; mean age 68.9 years; mean follow-up 9.2 months; 20 with ossification of posterior longitudinal ligament, 20 with cervical spondylosis, 2 with trauma, 2 with cervical radiculopathy, 1 with cervical herniation, and 1 with rheumatoid arthritis). The canal-to-body ratio (CBR) was determined by dividing the anteroposterior diameter of the spinal canal by that of the vertebral body at each lamina on cervical neutral lateral X-ray. LC was defined as a CBR decrease of 10% or more between immediately after the surgery and the final follow-up. We evaluated the LC frequency on each lamina with/without miniplate. The plate density (PD) was defined dividing the number of elevated laminas with miniplate by that of all elevated laminas in a patient, and we defined as group A (PD < 0.5), group B (PD = 0.5), group C (PD>0.5), and evaluated the LC frequency of each group. Results: The mean CBR were 1.02 (0.72-1.45) immediately after the surgery and 0.99 (0.68-1.44) at the final follow-up. LC occurred in 10/46 (21.7%) patients and in 13/164 (7.9%) laminas. And the LC frequency of each lamina were C3 1/15 (6.7%), C4 5/43 (11.6%), C5 4/46 (8.7%), C6 3/45 (6.7%), and C7 0/15 (0%). The LC frequency in the elevated lamina were significantly less with miniplate 2/95 (2.1%) than that of without miniplate 11/69 (15.9%; P < .01). The LC frequency of each groups were group A 5/8 (62.5%), group B 2/12 (16.7%), and group C 3/26 (11.5%), and group A showed significantly higher LC frequency than that of the other 2 groups (P < .05). Discussion: LC after open-door laminoplasty occurred in 33.3% patients and 44.7% laminas in the previous studies, while 21.7% patients and 2.1% laminas with miniplate in this study. Miniplates are thought to be a reasonable option to prevent LC. The elevated laminas of PD < 0.5 showed significantly higher LC occurrence than that of PD = 0.5 or more. Further studies are needed to establish the best PD to consider cost-effectiveness. Conclusion: The miniplates are reasonable option for preventing LC of open-door cervical laminoplasty, though the plate setting methods should be carefully considered plate density less than 0.5.
P008: Comparison of Cervical Disc Arthroplasty Versus Dynamic Cervical Implant for the Treatment of Cervical Spondylopathy: A Clinical and Radiological Study
Yong Hai1 and Li Guan1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: To evaluate the clinical and radiological outcomes of cervical disc arthroplasty versus dynamic cervical implant in the treatment of cervical spondylopathy, a retrospective clinical study was conducted. Material and Methods: All cervical spondylopathy cases from the Department of Orthopedics of Beijing Chao-Yang Hospital that received cervical disc arthroplasty versus dynamic cervical implant between February 2011 and February 2012 were analyzed retrospectively. Parameters as gender, age, body mass index, the operation time, and blood loss of all the patients were analyzed. The patients were followed 1 month, 3 months, 6 months, 12 months, and 24 months postoperatively. Neck Disability Index (NDI), Japanese Orthopaedic Association (JOA) Score, and visual analogue scale (VAS) were used to evaluate the clinical outcomes of the 2 groups. The X-ray films before and after surgery were analyzed, and cervical lordosis, the height of disc, range of motion, lordosis, olithesis, the distance between implant and wedge of vertebrae, and heterotopic ossification were measured. All statistics were done by SPSS 12.0. Results: There were 16 patients in anterior cervical disc arthroplasty group (male 8, female 8). Average age was 44 ± 4.5 years (range = 32-54 years). There were 10 cases with cervical spondylotic myelopathy, 6 cases with radicular spondylosis. In dynamic cervical implant (DCI) group were 10 cases (male 6, female 4). Average age was 44.5 ± 5.6 years (range = 33-55 years). There were 7 cases of cervical spondylotic myelopathy and 3 cases of radicular spondylosis. In the both groups, there were no significant change in the age, gender, height and weight ratio, operation time, and blood loss (P > .05). In cervical disc arthroplasty group, the preoperative JOA, NDI, and VAS of neck pain and upper extremity pain score and cervical lordosis, intervertebral disc angle were 10.3 ± 1.4, 15.2 ± 5.5, 6.2 ± 2.1, 4.1 ± 1.4, 10.0 ±2.1° and at final follow-up after operation were 15.8 ± 5.4, 3 ± 1.2, 2.9 ± 1.8, 1.8 ± 0.8, 16.6 ± 3.6°, while in DCI group preoperative were 9.5 ± 1.3, 15.6 ± 16.3, 6.4 ± 2.0, 4.5 ± 1.4, 14.9 ± 3.5° versus postoperative 9.5 ± 1.3, 2.9 ± 1.3, 2.6 ± 1.7, 1.9 ± 1.1, 22.3 ± 4.6°. In these 2 groups, preoperative compared postoperative were significantly improved (P < .01), while between final follow-up of the postoperation time had no significant difference (P > .05). There were no significant difference in the height of operation segment and the above segment, the range of motion (P > .05) at any time compared these 2 groups. Two implant were anterior olithesis 1 mm, and 3 had heterotopic ossification in cervical disc arthroplasty group, while DCI group was normal. Conclusion: Cervical disc arthroplasty and dynamic cervical implant in treatment of cervical spondylopathy can retain the range of motion, recover, and maintain the height of disc and cervical lordosis.
P009: Cervical Disc Replacement: Trends, Costs, and Complications
Nickul Jain1, Ailene Nguyen2, Blake Formanek2, Raymond Hah2, Zorica Buser2, and Jeffrey Wang2
1Southern California Orthopedic Institute, Bakersfield, CA, USA
2University of Southern California, Los Angeles, CA, USA
Introduction: Artificial cervical disc replacement (ADR) is a newer treatment option that obtained US FDA approval in 2007 that allows for effective discectomy and neural element decompression while preserving range of motion and potentially decreasing complications of pseudoarthrosis and adjacent segment disease associated with anterior cervical discectomy and fusion (ACDF). A growing body of evidence has demonstrated that ADR is both safe and efficacious with good mid- to long-term outcomes that are noninferior and potentially superior to ACDF. Methods: A retrospective database study was performed within the Humana portion of the PearlDiver Record Database (PearlDiver Inc, Warsaw, IN). Patients undergoing cervical ADR between January 1, 2007, and September 30, 2015, were identified using Current Procedural Terminology (CPT) codes. We collected annual trends, reimbursement costs, and patient demographic information, including sex, age, and inpatient or outpatient status. Patients data were collected from the time of operation to 1 year postoperative. Complications were grouped into 7 categories: pain, mechanical and bone-related complications including adjacent disc degeneration, nerve injury, dysphagia and dysphonia, infections, adverse reactions (hemorrhage, embolism, fibrosis, stenosis, thrombosis), and revision and reoperation procedures (removal of ADR, conversion to ACDF, revision ADR, and/or cervical osteotomies). Results: A total of 293 patients were identified in the Humana database receiving either single or multilevel ADR between 2009 and 2015. ADRs was most commonly performed in patients aged 40 to -54 years. With regard to complications, fewer than 3.7% of patients (<11) had new onset pain within 1 year after CDR. A total of 12.3% of patients (36) reported a mechanical and/or bone-related complication within 1 year. No patients indicated a new nerve injury within 6 months of follow-up. Fewer than 11 patients (<3.7%) presented with dysphagia or dysphonia within 6 months, infection within 3 months, or a revision or reoperation within 1 year. Due to PearlDiver limitations on privacy, exact numbers could not be obtained for incidence less than 11 patients. Average reimbursement for single-level inpatient ADR was $33 696.28 versus outpatient as $34 675.12 with no statistically significant difference (P = .29). Conclusion: Previously reported rates of complications within 1 year of ADR have been reported between 0% and10% in other large studies. Our study reported bone and mechanical related complications within 1 year of procedure to be consistent as previously reported. Additionally, rates of dysphagia or dysphonia and revision or reoperation were also similar to previously reported studies. Cost data for our study reveal no significant difference between inpatient and outpatient ADR, which has implications for health care payers. We feel that this study provides valuable data regarding inpatient versus outpatient costs and reveals a slightly higher rate of complications within the 1-year period, specifically in the mechanical and bone-related category, than may have been previously reported in the cervical ADR IDE (investigational device exemption) trials.
P010: Segmental Osteolysis Following Cervical Total Disc Replacement
Vit Kotheeranurak1, Jin-Sung Kim2, and Dong Hwa Heo3
1Queen Savang Vadhana Memorial Hospital, Sriracha, Chonburi, Thailand
2Seoul St. Mary’s Hospital, The Catholic University of Korea Seoul, Republic of Korea
3The Leon Wiltse Memorial Hospital, Suwon, Republic of Korea
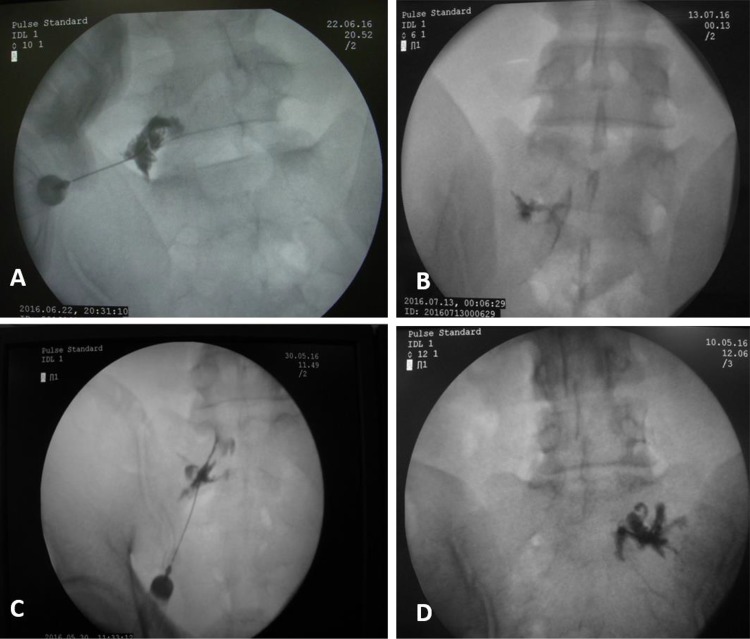
Introduction: Segmental osteolysis of the vertebral body can be considered as one of the potential complications after cervical total disc replacement (C-TDR). However, its clinical relevance is still unclear. The purpose of this study is to evaluate the rate of segmental vertebral body bone loss and its clinical outcome after single level C-TDR using ProDisc-C (Synthes Inc, West Chester, PA) with a minimum of 2 years follow-up. Material and Methods: The patients who underwent single-level C-TDR using ProDisc-C at single institute from September 2006 to January 2016 were retrospectively included. Demographic data (age, sex, operative level), radiographic parameters (true lateral neutral and dynamic X-rays), and clinical parameters (visual analogue scale [VAS] score for neck, VAS score for arm, and Neck Disability Index [NDI]) were collected. Patients that had hybrid procedure and malposition of implant insertion were excluded. We categorized patients into 3 groups according to the radiographic grading of bone loss—Group N: no bone loss; Group 1: diminish of the anterior osteophyte or minimal bone loss not extending beyond the anterior keel line; Group 2: significant bone loss that extending pass the anterior keel line. Results: Of the 57 patients (mean age = 56.89 ± 9.4, male-to-female ratio = 33:24) enrolled in our study, 13 patients (22.8%) developed heterotrophic ossification at the last follow-up visit, none of whom demonstrated any motion nor bone loss on the radiographic studies, and 9 patients (17.4%) were classified as Group N (no bone loss and preserved segmental motion). Radiographic bone loss was observed in 35 patients (61.4%), 33 patients in Group 1, and 2 patients in Group 2. Among the 2 patients in Group 2, the earliest evidence of bone loss was detected as early as 3 months postoperatively. Segmental bone loss only occurred in the motion-preserving unit, unlike ones that developed heterotrophic ossification (P < .05). Patients in Group 2 experienced more postoperative VAS for neck and less NDI reduction as compared with other groups (P < .05), but none needed any revision surgery. The mean follow-up time was 69.26 ± 34 months. Conclusion: Segmental bone loss following C-TDR can be discerned only in ones where the functional unit range of motion is preserved. Clinical outcomes are not affected by the minimal osteolysis. Nonetheless, significant bone loss after C-TDR may lead to worse postoperative outcomes.
P011: Multilevel Anterior Cervical Discectomy and Fusion Surgery Versus Hybrid Surgery for the Treatment of Cervical Disc Diseases
Matjaz Vorsic1, Janez Ravnik1, Tomaz Velnar1, and Rok Koncnik1
1University Medical Center Maribor, Maribor, Slovenia
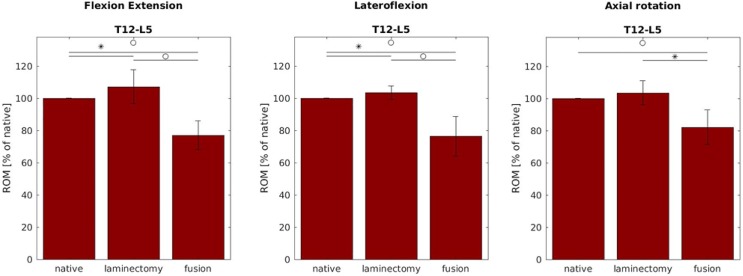
Introduction: Anterior cervical discectomy and fusion (ACDF) is still a standard treatment for cervical degenerative disc disease in the patients where conservative treatment failed. Different grafts and cages can be used to achieve the solid fusion. ACDF may contribute to adjacent segment pathology. Cervical disc arthroplasty (CDA) is an effective treatment for single-level cervical disc disease providing motion preservation and decreased reoperations at the adjacent segments. Hybrid surgery (HS), involving the combination of ACDF and CDA, has been increasingly utilized for patients with multilevel cervical degenerative disc disease. The primary aim of our study was to compare clinical results as well as the cervical range of motion (ROM) comparing the ACDF and HS in 2-level disc diseases. Methods: After applying the inclusion criteria, 50 patients with 2-level cervical degenerative disc disease where conservative treatment failed were included in the study. Half of the patients underwent the ACDF and other half the HS procedure. Clinical outcomes were assessed before and at regular intervals until 1 year after the procedure using neurological examination, the Neck Disability Index (NDI), and the visual analogue scale (VAS) for neck and arm pain, with 15% improvement in NDI and 20% in VAS defined as clinically significant. The cervical range of motion was evaluated using flexion-extension, lateral bending, and axial rotation parameters. Results: The groups were similar at baseline both clinically and statistically (P > .05) except for age and VAS for arm pain. Both groups had a statistically significant improvement in NDI and VAS for neck and arm pain (P < .05), and there was no statistically significant difference between groups at any point of investigation. The HS group had a slightly better improvement according to NDI (72% of patients in the HS group achieved ≥15% improvement in NDI and 64% of patients in ACDF group). There was a statistically significant difference in the C2-C7 ROM between the 2 groups at 12 months postoperatively (P < .05). The ROM of the HS group approached the preoperative value at 1 year. The location of the arthroplasty above or below the level of the fusion did not have a significant impact on motion. Conclusions: All implants resulted in significant pain reduction and functional outcome for the patients. The combination of fusion and arthroplasty can be adjusted to each level allowing segmental motion preservation at the affected levels and minimizing hypermobility at adjacent levels. Long fusion constructs leading to adjacent segment pathologies may be avoided.
P012: One-Inch Minimum Invasive Cervical Open-Door Laminoplasty Is Easy and Safe!
Kanji Sasaki1, Ushio Nosaka1, and Tetsutaro Mizuno1
1Seirei Hamamatsu Hospital, Hamamatsu, Japan
Introduction: Cervical laminoplasty is a procedure that aims to enlarge the whole spinal canal. Then priority is how to spread more, and to minimize surgery is not discussed so much, compared with lumbar. Thus, we often forget the complication of severe nape pain after surgery, caused by muscle or bone invasion. We devised minimum invasive laminoplasty (MIS-LP) from 2014. Using our procedure, skin incision is about 1 inch, and plate and screw for lamina fixation deliver primary strong fixation. This study aimed to analyze the usefulness and result of this procedure. Material and Methods: A total of 282 cases with MIS-LP (189 male/93 females; average 65 years old) were investigated, retrospectively. This procedure is combination of Shiraishi’s and Hirabayashi’s methods, and it needs only right-angled Gelpi’s retractors. The device is splitting spinous process above lamina reducing muscle damage with spinous process as Shiraishi’s procedure. After revealing the lamina without spinous process, we undertook open-door LP from C4 to C6 and dome LP to C3 and C7. For comparative cases, 44 cases underwent conventional LP (open-door or French-door LP: hydroxyapatite brocks, more than 3 inches). Japanese Orthopaedic Association Score (JOA Score) and Hirabayashi’s recovery rate at first outpatient day after operation, operative time, amount of bleeding, complications (including C5 palsy) and survival time, and radiographic change (lateral view) were investigated. Learning curve of this procedure was also investigated. Results: There were no cases of worsened neurological deficit nor C5 palsy, and the neurological scores (JOA) were not significantly different. In 2 hematoma cases, we should have reoperation. Recovery rates (1 year) among 2 procedures were also same. Surgical time of MIS-LP (average 75 minutes) was significantly superior to conventional procedure (103 minutes). The mean amount of bleeding during MIS procedure (average 28 g) was significantly less than conventional LP (122 g). Postoperative XP changes of cervical lordosis (MIS: 2° reduced, conventional: 3° reduced) and no significant spondylolisthesis nor slip occurred. All procedures maintained the primary alignment, and there is no remarkable change after surgery. Learning curve of this procedure is smooth, and switch from conventional or French door is very easy (surgical time reduction: open-door to MIS from 85 minutes >65 minutes at 80 cases, French-door to MIS 100 minutes > 75 minutes at 120 cases). Conclusion: To complete MIS procedure, we made gutter with microscope, taking care of the width of gutter and to be narrow than open procedure. And it has some effect to keep high-speed drills far from nerve roots. Thus, no C5 palsy was caused by the device. Our minimum invasive LP is safer and faster than old methods. This is one of the best options for minimum invasive cervical surgery, and this procedure is necessary for the future.
P013: The Effect of Body Mass Index on Long-Term Patient-Reported Outcome Scores After Anterior Cervical Discectomy and Fusion in an Asian Population: A 2-Year Study
Shao Jin Teo1 and Reuben Chee Cheong Soh1
1Singapore General Hospital, Singapore, Singapore
Introduction: With the world’s largest aging population, the incidence of cervical spondylotic myelo-radiculopathy requiring anterior cervical discectomy and fusion (ACDF) will increase rapidly in Asia. At the same time, obesity is on the rise here due to lifestyle and diet changes. However, little is known about how body mass index (BMI) affects long-term patient outcome after ACDF. The limited existing literature have focused mainly on Western populations, which vary significantly from the Asian population in BMI and body composition. This study will examine the relationship between BMI and various patient-reported outcome (PRO) scores after ACDF, up to the 2 years’ mark, in an Asian population. Material and Methods: A total of 878 patients were identified to have undergone ACDF between 2000 and 2015 in our tertiary institution. After excluding patients with previous cervical instrumentation, more than 2 levels fused, disc arthroplasty, missing BMI measurement, and neoplastic/traumatic indication for surgery, 553 patients were included. Patients were grouped according to their preoperative BMI. The grouping criterion is adopted from the WHO (World Health Organization) guidelines for Asian populations. PRO scores were collected preoperatively, and at 6 months and 2 years post surgery. A generalized linear model is used to analyze the relationship between BMI and each PRO score, adjusting for other potential factors including gender and age. The PRO scores utilized in this study are the Neck Disability Index (NDI), Numerical Pain Rating Scale for Limb Pain (NPRS-LP) and Neck Pain (NPRS-NP), American Academy of Orthopaedic Surgeons (AAOS) Neurogenic Symptom Score (AAOS-NSS), and also the JOA (Japanese Orthopaedic Association) myelopathy score for patients with a myelopathy component. Patients were also asked to rate the overall results of their treatment on a 6-point scale, adapted from Question 53 in the AAOS Cervical Instrument Questionnaire. Results: Of the 553 patients, 19 (3.4%) were underweight, 155 (28.0%) were normal weight, 112 (20.3%) were overweight, and 267 (48.3%) were obese. In the obese group, 205 (37.1%) fell into the Obese-I and 62 (11.2%) fell into Obese-II. Ethnically, 468 (84.6%) were Chinese, 32 (5.79%) were Indian, and 42 (7.59%) were Malay. The remaining 11 (1.99%) patients included a mix of Eurasian and Caucasian patients. Patients across all 5 BMI categories experienced similar levels of improvements in their PRO scores after surgery. There were no significant differences between the groups in any of the PRO scores preoperatively, and at 6 months and 2 years after surgery. The rate of reoperation was highest in the Obese II group at 8.07%, but this did not reach statistical significance. Conclusion: A high BMI is not associated with inferior outcomes, as measured by PRO scores, after 1- and 2-level ACDF. Despite Western populations showing inferior outcomes, Asian BMI-adjusted obese patients show better outcomes and are just as satisfied with the outcomes of their ACDF as the other BMI groups. The rate of reoperation is also not significantly increased in the obese.
P014: Adjacent Segment Degeneration and Adjacent Level Ossification Development in 3-Level Anterior Cervical Discectomy and Fusion: Prevalence and Risk Factors
Shao Jin Teo1 and Reuben Chee Cheong Soh1
1Singapore General Hospital, Singapore, Singapore
Introduction: Adjacent segment degeneration (ASD) is a common complication following anterior cervical discectomy and fusion (ACDF). Another related but less well-studied phenomenon is adjacent level ossification development (ALOD). Few studies have looked at these complications in the context of 3 level fusions. This study aims to examine the development and severity of radiographic ASD and ALOD in our patients following 3-level ACDF. Sagittal parameters, biologic, mechanical, and technical factors were analyzed to look for possible relationship in both conditions. Material and Methods: A prospectively collected database (2004-2015) was retrospectively reviewed to identify all 3-level ACDF cases in our tertiary institution. Ninety-four patients were identified. Forty-eight patients were excluded due to lack of follow-up, anterior plating, or/and poor radiographs. A minimum follow-up of 2 years was required for inclusion. Forty-six patients were eventually included in the study. Lateral cervical radiographs taken preoperatively, postoperatively, and at last follow-up were reviewed by a consultant spine surgeon and graded accordingly for ASD and ALOD using a previously utilized 4-level grading scale. Radiographic parameters measured were the plate to disc (P2D) distance, cervical sagittal alignment (CSA), T1 slope (T1S), and sagittal vertical axis (SVA). Patient parameters included were gender, age, body mass index (BMI), smoking, and diabetic status. Statistical analysis was performed with SPSS. Results: Of the 46 patients included in the study, there were equal number of males and females, with a mean age at surgery of 59.7 (39.8-75.8). The average length of follow-up was 60.4 (24.1-137.1) months. Evidence of ASD was present in 27 (58.7%) patients. A BMI >28 and a P2D <3 mm were significantly associated with ASD development. CSA, T1S, and SVA values were not significantly different between patients with and without ASD. Evidence of ALOD was present in 33 (71.7%) patients. No patient parameters were found to be significantly associated with ALOD. The ALOD group had significantly smaller postoperative CSA (11.58 vs 22.29, P = .03), smaller T1S (24.56 vs 29.49, P = .018), and greater SVA (22.06 vs 9.91, P = .003). One (2.17%) patient underwent reoperation for symptomatic adjacent segment disease. Conclusion: Larger T1S and larger SVA contributed to an increased incidence of ALOD. A possible relationship may be due to the greater tendency for patient to revert to a kyphotic posture, which increases anterior column stresses and results in more ossification. ASD was present in 58.7% of patients, and significantly associated factors are high BMI and small P2D distance. ALOD was present in 71.7% of patients and smaller CSA. However, ALOD and radiographic ASD do not appear to lead to worse NDI scores, and the significance of ALOD and ASD on radiograph remains to be determined.
P015: Artificial Cervical Disc Replacement Requires Proper Facet Joint Loading
Hooi Ming Tan1 and Kim Soon Oh1
1Island Hospital, Penang, Malaysia
Introduction: Cervical total disc replacement has been in practice for more than a decade now as a viable alternative to cervical fusion in suitable cases, aspiring to preserve spinal motion and prevent adjacent segment disease. Reports are rife that neck pain emerges as an annoying feature in the early postoperative period. The facet joint appears to be the most likely source of pain. Material and Methods: Sixty patients were prospectively followed-up through 7 years after having received disc replacement surgery, indicated for symptomatic soft disc herniation of the cervical spine presenting with radiculopathy. All were skeletally mature, aged 22 to 58 years. All had a failure in at least 6 months of conservative therapy with evidence of deteriorating radicular symptoms and a Neck Disability Index (NDI) exceeding 30% (scoring 15/50). We excluded those with degenerative trophic changes of the cervical spine, focal instability, trauma, osteoporosis, previous cervical spine surgery, previous infection, ossifying axial skeletal disease and inflammatory spondyloarthritides. The device used was an unconstrained implant with stabilizing teeth. Over the 7 years, we studied their postoperative comfort level via the NDI and Visual Analogue Score (VAS). Preoperative and postoperative analysis of the sagittal axis and of involved facet joints were done. Results: Twenty-five patients suffered postoperative neck pain as reflected by the NDI and VAS scores. Of these, 10 reported of neck pain even 24 months after surgery. However, none were neurologically worse, and all patients returned to their premorbid functions and were relieved of pain by 28 months. All 25 patients reported of rapid dissolution of neckache after peri-facetal injections of steroids were done under image guidance. Conclusion: We draw attention to the facet joint as the pain generator, triggered by inappropriate implant height, eccentric stresses via hybrid constructs, eccentric loading due to unconstrained devices, and unaddressed Luschka joint degeneration. Such factors require careful selection of patients for surgery, necessitate proper preoperative templating, and call for appropriate technical solutions during surgery.
Arthroplasty-Lumbar
P016: An Analysis of Heterotopic Ossification in Lumbar Disk Arthroplasty
Vadim Byvaltsev1, Yurii Pestryakov1, Valerii Shepelev1, Andrei Kalinin1, Evgenii Belykh1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: Total intervertebral disk (IVD) arthroplasty is a modern alternative method of surgical treatment of IVD degeneration. The most common complications of this type of surgical intervention is heterotopic ossification (HO). HO leads to the limitation of the amplitude of movements in the operated segment, which makes an artificial IVD cage and does not allow to protect adjacent segments from degeneration. The purpose of this study was to assess the degree of influence of HO on the amplitude of movements in the operated segment and on clinical outcomes in patients after total IVD arthroplasty. Materials and Methods: The results of total lumbar IVD arthroplasty were analyzed in 74 patients (46 men, 28 women) aged 23 to 45 years (mean age 36.7 ± 5.9 years). The follow-up period was 36 months. The amplitude of movements of the operated segments was estimated and the degree of HO. Clinical outcomes were analyzed on the basis of the study of the severity of the pain syndrome according to the visual analogue scale (VAS) and the quality of life level associated with back pain at the Oswestry Disability Index (ODI). Results: Signs of HO were found in 36.4% (n = 27) of patients. According to the degrees of HO, they were represented as follows: Class I was met in 14.8% (n = 11) cases, Class II in 18.9% (n = 14), and Class III in 2.7% (n = 2). The mean values of the amplitude of movements of the operated segment, VAS and ODI in the group of patients without signs of HO were 11.2 ± 2.70, 2.8 ± 1.2 cm, and 17.3 ± 6.5%, respectively. These indicators in the group of patients with signs of HO were 11.5 ± 1.20, 3.4 ± 1.8 cm, and 19.8 ± 7.3%, respectively. The amplitude of segment movements with HO grade III is significantly lower than in patients without HO symptoms (P = .024). Conclusion: HO after total lumbar IVD arthroplasty occurs in 36.4% of cases. High HO Classes significantly affects the amplitude of the movements of segments. We did not receive reliable effect of high-level HO grades on clinical results in patients.
P017: Lumbar Disk Arthroplasty for the Treatment of Lumbar Degenerative Disk Disease: 5-Year Follow-up Results
Vadim Byvaltsev1, Andrei Kalinin1, Yurii Pestryakov1, Valerii Shepelev1, Evgenii Belykh1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: The purpose of this study is to present the long-term results and to evaluate the safety and effectiveness of lumbar disk arthroplasty in treatment of patients with symptomatic lumbar degenerative disk disease. Materials and Methods: A total of 154 patients were analyzed before surgery, after disk arthroplasty and at 3 months, 6 months, 12 months, 24 months, 36 months, 48 months, and 60 months after total disc replacement. Clinical assessments included the visual analogue scale (VAS), and the Oswestry Disability Index (ODI) scores. Radiographic assessments included lumbar lordosis (LL), intervertebral disc height (IDH), and range of motion (ROM) of the total lumbar spine. Complications at the 5-year follow-up were collected as well. Results: Mean follow-up period was 62.17 months. There was clinical improvement in terms of VAS and ODI from the preoperative to the final follow-up (P < .01). Overall, ROM of the total lumbar spine was maintained during the follow-up. Statistically significant (P < .05) improvements in the trend of IDH and LL were noted at the follow-up. Twenty-four patients were observed an appearance of heterotopic ossification at the 5-year follow-up, with 18 patients appeared at Class II and 7 patients at Class III. Adjacent segment degeneration assessed by radiographic evidence was found in 4 patients. Conclusion: Lumbar disk replacement showed significant improvement in clinical outcomes at 5 years. It not only effectively preserves the motion of both total lumbar spine and operated segments, but also restores normal IDH and LL up to 5 years postoperation.
P018: Lumbar Total Disc Arthroplasty: Blood Product Utilization in an Ambulatory Surgery Center
Benjamin Dorenkamp1, Sharon Kelly2, and Michael Janssen3
1McLaren Greater Lansing, Lansing, MI, USA
2Presbyterian St. Luke’s Medical Center, Denver, CO, USA
3 Center for Spine and Orthopedics, Thornton, CO, USA
Introduction: Spine surgery in ambulatory surgery centers (ASC) is growing in popularity as an alternative to surgery in the hospital setting. There is little to no evidence in the literature discussing anterior lumbar spine surgery utilizing a retroperitoneal approach in the ASC setting. The main concern with the anterior approach to the lumbar spine is the potential for injury to aorta/vena cava and common iliac vessels. Due to this potential injury, it has been common practice in our facility to have 2 units of cross-matched blood in the operating room as well as utilizing intraoperative cell salvage during the procedure. We retrospectively looked at 50 cases of lumbar total disc arthroplasty (TDA) in our ASC to determine utilization of blood products. Material and Methods: Fifty consecutive patients who underwent a lumbar TDA at a single ASC were reviewed. Surgery was performed by orthopedic spine surgeons and a general surgeon with significant experience in the anterior retroperitoneal approach to lumbar spine. Surgeries were completed at the ASC and were all transferred from PACU (post-anesthesia care unit) to an attached convalescence care center (CCC), which allows up to 3 days of observation. Patients who had either a 1-level or 2-level lumbar TDA between 2007 and 2018 were included in the retrospective study. Data consisting of demographics, ASA (American Society of Anesthesiologists), length of stay, estimated blood loss (EBL), cell saver volume, transfusion, perioperative, and postoperative complications were recorded. Results: Fifty patients’ records were reviewed. The mean age was 40.86 ± 9.45, 48 (96%) patients had a 1-level lumbar TDA, 1 (2%) patient had a 2-level lumbar TDA, 1 (2%) patient had a lumbar TDA at L4/5, and an anterior lumbar interbody fusion at L5/S1. There were 0 mortalities; 0 patients had perioperative complications. Zero patients received allogenic blood transfusion, 4 (8%) were re-transfused from cell saver (2 patients receiving approximately 400 mL and 2 patients receiving approximately 200 mL of re-transfused blood). All 50 (100%) patients were discharged home in stable condition. Conclusion: The routine use of both cell saver and cross-matched blood in the operating suite for lumbar TDA may be an overutilization of health care resources. In our review of 50 patients, we had no need for transfusion of allogenic PRBCs and only 4 of 50 patients had enough blood output for re-transfusion from the cell saver. The maximum re-transfused blood was 480 mL and would likely not have resulted in need for allogenic blood transfusion even without cell saver utilization. This opens the conversation for alternatives to utilization of cross-matched PRBCs being held in the operating room. Such alternatives may be the use of cell salvage and having no blood held for patients, having only type O blood in a cooler for each patient, or keeping type O blood on constant hold in ASCs that commonly perform this procedure.
Basic Science
P019: Morphometric Analysis of Lumbar Pedicles Among Adult Kenyans Using Computer Tomography Scans
Victor Misiani Oteki1
1Department of Orthopaedics, Eldoret, Kenya
Introduction: There is a rise in spine surgeries in Kenya as the number of spine surgeons are being trained. Spine surgery complications from misplaced lumbar pedicle screws are projected to rise, with the use of free hand technique. This study was designed to provide accurate measurements of lumbar pedicle morphology for use in Kenya, as a preventive measure to a possible rise in complications from misplaced screws. Objectives: To determine the width, angulation, and chord length of the lumbar vertebrae pedicle from L1 to L5 in adult Kenyans using computed tomography (CT) scans. Materials and methods: This was a cross-sectional descriptive study conducted at St. Luke’s Hospital from January 1 to December 31, 2016. Ethical clearance was granted from IREC (Institutional Research Ethics Committee). Lumbar pedicle width, angulation, and chord length from L1 to L5 were measured on CT scans. One hundred CT scans from 468 lumbar spine scans. Data were recorded in data collection sheets, extracted, and entered into Microsoft Excel. In Excel, data were then cleaned, categorized, and transferred to SPSS version 21 for analysis. Results from the analysis were summarized as means, standard deviations, and presented in line and bar graphs. Results: One hundred CT scans were used for the study with 49 males and 51 females, with an age range of 18 to 63 years. On CT scan, pedicle width mean measurements were L1-7.2 mm, L2-7.6 mm, L3-9.2 mm, L4-10.8 mm, and L5-14. 6 mm. The mean angle of insertion on CT scan was L1 19.7°, L2 20.5°, L3 22°, L4 24.1°, and L5 29.8°, and pedicle chord length was L1 48.6 mm, L2 49.9 mm, L3 50.1 mm, L4 49.8 mm, and L5 50.1 mm. Conclusion: The pedicle width on CT scan measurements increased from 7.2 mm to 14.6 mm between L1 to L5. The angulation increased from L1 to L5 on CT scan measurements from 19.7° at L1 to 29.8° at L5. The chord length range measurement on CT scan was from 48.6 mm to 50.1 mm. Recommendations: The minimum size of screw diameter that should be used is 6.5 mm with a length of 45 mm angulated between 20° and 30° from L1 to L5. Based on the variation, there is need for measurements of the pedicle dimensions before transpedicular instrumentation. Further research should be carried out on lumbar pedicle dimensions based on age, weight, and height to assess whether their exists variations.
P020: A Comparison of Transverse Pedicle Angles Between Ethnic Groups
Robert Stockton1, Joseph Albano1, Jonathon Lentz1, Maximillian Ganz1, Kanwarpaul Grewal1, and Gus Katsigiorgis1
1Plainview Hospital, Plainview, NY, USA
Introduction: Minimally invasive spinal surgery requires an intimate understanding of pedicle morphology to provide safe and effective outcomes. Although current research has attempted to identify morphological vertebral pedicle trends, no study has utilized computed tomography (CT) scans to compare the lumbar transverse pedicle angle (TPA) with patient demographics factors in a diverse population throughout multiple hospital centers. In this study, we present novel correlations between TPA and patient demographics that may assist surgeons in estimation of pedicle screw placement trajectory. Material and Methods: Approval from our institution’s Investigational Review Board was obtained. Analysis was conducted of randomly selected CT scans of L1 to L5 of 98 individuals who received imaging over a 2-week period for non-back pain–related complaints. Each lumbar TPA was measured by creating a midline measurement from spinous process to the anterior vertebral body and measuring the angle from that midline to the mid-axis of the pedicle bilaterally. Measuring 980 TPAs in total allowed for comparison of each patients’ pedicle angle with multiple important patient-specific demographics including ethnicity, age, gender, height, and weight. Statistical analysis utilized multiple comparisons of demographics at each level with post hoc Bonferroni correction analysis to compare demographics at each level. Results: With relation to sex, age, height, or weight, no statistically significant differences were identified for TPAs at any vertebral level. However, when stratified by ethnicity, the differences in transverse pedicle angles averages (TPA-Avg) at multiple individual vertebral levels were found to be statistically significant (P = .05). At L2, individuals of Asian descent were found to have 3.11° larger TPA-Avg angle, which is significant (P = .05) when compared with black individuals. Additionally, at L2, the TPA-Avg angle of white individuals is 1.84° larger than black individuals, which was found to be significant (P = .05). When multiple comparisons were made at L3, Asian individuals were found to have a TPA-Avg of 1.95° and 2.91° larger than Hispanic and black individuals, respectively (P = .05). Conclusion: This study stands to help guide the orthopedic surgeon when preparing for minimally invasive transforaminal lumbar interbody fusion or any lumbar surgical techniques that require patient-specific knowledge of lumbar pedicle morphology. In this study, we have identified a previously unknown and statistically significant relationship between multiple ethnicities and transverse pedicle angles at several lumbar vertebral levels. These findings provide critical information that may be added to the operating surgeons’ knowledge of pedicle morphology. This novel information can assist in preoperative planning of minimally invasive pedicle screw placement and may also help decrease total operative time and improve radiographic and clinical results.
P021: Relationship of Height and Weight to Lumbar Pedicle Diameter
Jonathon Lentz1, Joseph Albano1, Robert Stockton1, Maximillian Ganz1, Kanwarpaul Grewal1, and Gus Katsigiorgis1
1Plainview Hospital, Plainview, NY, USA
Introduction: Safely performing instrumented spinal fusion requires an intimate knowledge of vertebral anatomy and anatomic variations. Pedicle screw size and position can affect intraoperative and postoperative complication rates. While preoperative planning with computed tomography (CT) scan measurements may be the safest way to judge trajectory and maximal safe pedicle screw size, it is not standard practice for many spine surgeons. In this study, we aim to supplement the available anatomic data to enhance preoperative radiographic assessment and intraoperative fluoroscopic assessment methods for screw selection in posterior spinal lumbar fusion procedures. Material and Methods: We retrospectively reviewed CT scans in 270 patients (2070 pedicles) performed over a 2-week period within a single health system in a diverse area of the United States. Coronal cuts of the lumbar spine were assessed to obtain transverse outer cortical pedicle diameter (PD) as measured through the isthmus at lumbar vertebrae 1 through 5. Patient height, weight, and body mass index (BMI) were recorded at the time of CT scan for all study patients. A Pearson product-moment correlation coefficient was computed to assess the relationship between PD and each variable (height, weight, and BMI). Results: Both height and weight were found to significantly correlate with PD at all lumbar vertebrae levels (P < .01). BMI showed no statistically significant correlations with PD at any lumbar levels (P < .05). Height explained roughly 10% of the variance in PD and weight explained only 3% to 4%. BMI explained almost 0% of the variation. Conclusion: Height and weight are routinely obtained noninvasive measurements that have positive correlation with PD. These results provide additional variables for spine surgeons to consider when judging maximum safe pedicle screw diameter in patients undergoing posterior lumbar fusion. We previously reported the significant difference in PD between different races. Further studies may allow for correlation of other noninvasive data points to further augment preoperative and intraoperative radiographic assessment.
P022: Comparison of Static Testing Per ASTM F2077 Using a Constrained, Semi-Constrained, and Unconstrained Test Setups
Stacey Barber1, John DeVine2, David Gloystein2, Dawn Lissy1, and Dennis Buchanan1
1Empirical Testing Corp, Colorado Springs, CO, USA
2Medical College of Georgia at Augusta University, Augusta, GA, USA
Introduction: Spinal surgery intended for fusion has been performed since the early 1990s. ASTM F2077, a test method for intervertebral body fusion devices, was initially approved in 2000. ASTM F2077 provides a recommended test setup that consists of a universal joint for unconstrained loading; however, in the interim time between the start of spinal fusion surgery and the development of the test method, mechanical testing was being performed using several different test setups, a constrained setup, a semi-constrained setup, and an unconstrained setup. The constrained setup utilizes a rigid connection from the actuator to the specimen. A semi-constrained setup utilizes a rigid connection at the actuator with a hemispherical dome that can freely rotate to maintain equal load distribution without translation. The unconstrained test setup is the setup depicted in ASTM F2077, which uses a universal joint or a ball joint at the actuator connection in addition to a hemispherical dome that can freely rotate allowing for equal load distribution to the device. There is currently no data published to show the differences between the 3 test setups and how they affect resulting data. Material and Methods: A minimum of 6 mock PEEK (polyetheretherketone) cages were tested in each test mode: static axial compression testing, static compressive shear testing, and static torsion testing. Each static test was performed per ASTM F2077 using a constrained setup, a semi-constrained setup, and an unconstrained setup. The results were assessed to compare the differences between each test setup. Results: The null hypothesis was that there was no difference between the mechanical performance of static axial compression testing, compressive shear testing, and torsion testing in a constrained, a semi-constrained, and unconstrained test setup per ASTM F2077. No statistical difference could be shown between the constrained and semi-constrained test setups. For static axial compression testing, the testing results showed approximately a 30% lower stiffness and no statistical difference in yield in the unconstrained test setup versus both the constrained and semi-constrained setup. For static compressive shear testing, the testing results showed approximately a 30% lower stiffness and approximately a 40% lower yield in the unconstrained test setup versus both the constrained and semi-constrained setup. For static torsion testing, the results showed approximately a 22% lower stiffness and no statistical difference in yield in the unconstrained test setup versus both the constrained and semi-constrained setup. Conclusion: The purpose of this study aims to compare the test setups that are known to be used in static testing per ASTM F2077. The use of an unconstrained setup versus a semi-constrained setup or a constrained test setup results in a lower stiffness and/or yield of the device. This research will help engineers in the spinal industry determine the impact a test setup can have on the results, especially when comparing with data previously generated. This will also help clinicians to be aware of the differences in the test setups used for IBFDs (interbody fusion devices), which will allow them to appropriately compare data from 1 cage versus another.
P023: Homing of Mesenchymal Stem Cells Into Degenerated Intervertebral Discs: An Alternative to Stem Cell Injection?
Sebastian Wangler1, Marianna Peroglio1, Zhen Li1, Ursula Menzel1, Lorin M. Benneker2, R. Geoff Richards1, Mauro Alini1, and Sibylle Grad1
1AO Research Institute Davos, Davos, Switzerland
2University Hospital of Bern, Bern, Switzerland
Introduction: Injection of mesenchymal stem cells (MSCs) into degenerative intervertebral discs (IVDs) has been subject of multiple clinical trials. While most studies reported positive effects, it remains unclear whether the injected cells survive in the harsh IVD environment, and whether the needle puncture triggers a degenerative cascade. As an alternative application route, migration of MSCs from the endplate into the IVD has been described. It is hypothesized that only specific subpopulations of the naïve MSCs migrate in response to chemotactic molecules released by the IVD, allowing to get the “right cells” in the “right number” to the “right place.” We recently identified CD146 as a predictive surface marker for MSCs with enhanced migration potential toward degenerative IVDs. The aims of the present work were to investigate (1) the discogenic differentiation potential of the CD146-positive MSC subpopulation in vitro, and (2) the regenerative potential of this subpopulation following injection or migration into a trypsin-induced degenerative IVD in organ culture. Materials and Methods: Human MSCs were isolated from vertebral bone marrow aspirates by density gradient centrifugation and adherence to cell culture plastic. Cells were used at passage 2 to 3. Aim 1: In Vitro Differentiation Assay: Discogenic differentiation of CD146+ and CD146− sorted MSCs was assessed in GDF-6 supplemented pellet cultures (n = 4 MSC donors; age 61 ± 7.1 years). At day 14, gene expression was measured by real-time RT-PCR (reverse transcription polymerase chain reaction); sulfated glycosaminoglycan (sGAG) content in the pellet and medium was evaluated by DMMB (dimethylmethylene blue) assay. Aim 2: Organ Culture Regeneration Assay: CD146+ and CD146− MSCs (n = 3) were either injected into or seeded onto trypsin-degenerated bovine IVDs. After 3 weeks, sGAG synthesis rate of IVD cells was measured by sulfur-35 incorporation. Results: Aim 1: CD146+ and CD146− MSC pellets responded with a similar upregulation of aggrecan (10 times P = .025 and 8.3 times P = .014, respectively) and downregulation of collagen type X (5.0 times P = .027 and 3.3 times P = .004, respectively) compared with the day 0 populations; collagen type I and II expression did not differ after 14 days. A higher production of sGAG/DNA was observed for CD146+ MSC pellets (28.3 ± 8.6 vs 21.3 ± 7.1, P = .015). Aim 2: Both the injection- and migration-based MSC treatments induced a higher S-35 incorporation compared with the untreated control. IVDs treated with CD146− MSCs revealed a higher sGAG synthesis rate, although the difference was not significant. Conclusions: A superior disc-like differentiation in vitro was observed for the CD146+ subpopulation. In organ culture, a trend of higher sGAG synthesis rate was found after homing of CD146− MSCs, even though the number of homed MSCs was higher for the CD146+ MSCs. This is in line with previous findings that CD146+ MSCs represent a more progenitor-like, while CD146− MSCs characterize a more mature cell phenotype. Moreover, this highlights the importance of testing regenerative treatments in advanced whole organ culture models complementary to high throughput but simplified in vitro setups. Our data suggest that homing of MSCs might have a similar regenerative potential as MSC injection. Deposition of MSCs close to the endplate might therefore represent an alternative to intradiscal MSC injection.
P024: Efficacy of Freshly Isolated Adipose-Derived and Bone Marrow–Derived Stem Cells in Spinal Fusion: A Comparative Study in a Rat Model
Christina Holmes1, Alexander Perdomo-Pantoja2, Maritza Taylor2, Colson Tomberlin2, Wataru Ishida2, Ethan Cottrill2, L. Lo Sheng-Fu2, and Timothy F. Witham2
1Florida A&M University, Tallahassee, FL, USA
2Johns Hopkins University, Baltimore, MD, USA
Introduction: Bone marrow–derived stem cells (BMSCs) have been widely utilized in spinal fusion research. However, adipose-derived stem cells (ADSCs) offer several clinical advantages, including larger available tissue volumes, higher stem cell concentrations, and decreased donor site morbidity. While preclinical studies have shown that ex vivo expanded ADSCs can be successfully used in spinal fusion,1 the use of freshly isolated cells will better enable clinical translation. In this study, we compared the efficacy of freshly isolated ADSCs and BMSCs in achieving successful spinal fusion when combined with a clinical-grade bone graft substitute in a rat model. Materials and Methods: ADSCs were isolated from the inguinal fat pads, while BMSCs were isolated from the long bones of syngeneic female 6- to 8-week-old Lewis rats and combined with Vitoss (Stryker) bone graft substitute for subsequent transplantation. Posterolateral spinal fusion surgery at L4-L5 was performed on 27 female Lewis rats divided into 3 experimental groups: (1) Vitoss (Stryker) bone graft substitute only (VO group, n = 9); (2) Vitoss + 2.5 × 106 ADSCs/side (n = 9); and (3) Vitoss + 2.5 × 106 BMSCs/side (n = 9). Fusion was assessed 8 weeks postsurgery via micro–computed tomography (MicroCT) imaging and manual palpation. Manual palpation scoring was conducted by blinded researchers as follows: 0 = nonfused; 1 = partial fusion, some motion across operative joint; 2 = fused, no motion across the operated joint. MicroCT images were evaluated using ImageJ software to assess fusion mass volume and CT fusion score (0 = nonfused; 1 = unilateral fusion; 2 = bilateral fusion). Results: MicroCT imaging analyses revealed that fusion volumes and CT fusion scores in the ADSC group were significantly higher than in the VO group (19.75 mm3 vs 13.39 mm3, respectively, P = .04, and 1.5 vs 1.0, respectively, P = .03). CT volume and fusion score were not significantly different between the ADSC group and the BMSC group (19.75 mm3 vs 17.63 mm3, and 1.5 vs 1.3, respectively, P = > .05). The average manual palpation score was highest in the ADSC group compared with the BMSC and VO groups (1.3 vs 1.2 vs 0.7, respectively, P > .05). Conclusions: In a rat model, ADSCs yielded increased fusion mass volume and rates of fusion when combined with a clinical grade bone graft substitute compared with bone graft substitute alone. However, ADSCs only showed a trend toward higher fusion mass volume and rates of fusion compared with BMSCs. Ongoing histological studies will assess whether there are any differences in the quality of bone formed in the fusion masses.
Reference
1. Werner BC, Li X, Shen FH. Stem cells in preclinical spine studies. Spine J. 2014;14:542-551. doi:10.1016/j.spinee.2013.08.031
P025: Priming Adipose-Derived Stem Cells With Bone Morphogenetic Protein-2 Increases their Potency in a Rat Fusion Model
Alexander Perdomo-Pantoja1, Christina Holmes2, Ethan Cottrill1, Wataru Ishida1, L. Lo Sheng-Fu1, and Timothy F. Witham1
1Johns Hopkins University, Baltimore, MD, USA
2Florida A&M University, Tallahassee, FL, USA
Introduction: Adipose-derived mesenchymal stem cells (ADSCs) have recently become of increasing interest in spinal fusion research, as an attractive alternative to bone marrow–derived mesenchymal stem cells (BMSCs), due to higher available tissue volumes, increased stem cell concentrations, and reduced donor site morbidity. Several preclinical studies have demonstrated that ex vivo expanded ADSCs can achieve spinal fusion, particularly when combined with BMP-2.1,2 However, clinical delivery of rhBMP-2 often requires high concentrations and has been associated with various complications. Aquino-Martínez et al have previously shown that a short period of in vitro pre-priming with BMP-2 enhanced BMSC-mediated bone regeneration in vivo in a cranial defect model.3 Thus, in this study, we examine whether a brief period of in vitro pre-priming with rhBMP-2 can enhance ADSC-mediated fusion in a rat model. Materials and Methods: ADSCs were isolated from the inguinal fat pads of syngeneic female 6- to 8-week-old Lewis rats and cultured in vitro in Dulbecco’s Modified Eagle’s Medium—high glucose (Sigma-Aldrich) supplemented with 10% fetal bovine serum (Sigma-Aldrich) and 2% Pen-Strep (Sigma-Aldrich) at 37°C in 5% CO2-humidified incubator. When passage 1 (P1) ADSCs reached approximately 80% confluency, they were pre-primed for 24 hours with 1 ng of rhBMP-2 (Medtronic). After pre-priming, 2 × 106, ADSCs were seeded onto Vitoss (Stryker) bone graft substitute scaffolds for subsequent transplantation. Dorsolateral spinal fusion surgery at L4-L5 was performed on 21 female Lewis rats divided into 2 experimental groups: (1) Vitoss + ADSCs pre-primed with rhBMP-2 (n = 12); and (2) Vitoss + non–pre-primed ADSCs (n = 12). Fusion was evaluated 8 weeks postsurgery via micro–computed tomography (MicroCT) imaging and manual palpation. Manual palpation scoring was performed by blinded researchers as follows: 0 = nonfused; 1 = partial fusion, some motion across operative joint; and, 2 = fused, no motion across the operated joint. MicroCT images were used to assess fusion mass volume (mm3) via ImageJ software and determine CT fusion score (0 = nonfused; 1 = unilateral fusion; 2 = bilateral fusion). Results: Preliminary MicroCT imaging data suggest that rhBMP-2 pre-primed ADSCs (n = 11) yielded significantly higher fusion mass volumes than non-primed ADSCs (n = 10; 14.97 mm3 vs 12.78 mm3, respectively, P = .04). However, preliminary CT fusion scores were not significantly different between groups (1.7 pre-primed vs 1.5, non-primed, P = >.05). Pre-primed ADSCs also yielded significantly higher manual palpation scores than non-primed ADSCs (1.9 vs 1.3, respectively, P = .03). Conclusions: In our rat model, rhBMP-2 pre-primed ADSCs displayed an increased fusion mass volume and manual palpation score compared with non-primed ADSCs. Ongoing histological studies will evaluate whether there are any differences in the quality of bone formed within the fusion masses. Future studies will also compare whether these results are also similar in pre-primed BMSCs.
Reference
1. Werner BC, Li X, Shen FH. Stem cells in preclinical spine studies. Spine J. 2014;14:542-551. doi:10.1016/j.spinee.2013.08.031
2. Salamanna F, Sartori M, Brodano GB, et al. Mesenchymal stem cells for the treatment of spinal arthrodesis: from preclinical research to clinical scenario. Stem Cells Int. 2017;2017:3537094. doi:10.1155/2017/3537094
3. Aquino-Martínez R, Rodríguez-Carballo E, Gámez B, et al. Mesenchymal stem cells within gelatin/CaSO4 scaffolds treated ex vivo with low doses of BMP-2 and Wnt3a increase bone regeneration. Tissue Eng Part A. 2016;22:41-52. doi:10.1089/ten.TEA.2015.0181
P026: Twenty Hours to Become Good at Anything? Pedicle Screw Insertion—A Training Concept
Daren Lui1, Jan Herzog1, Jade MacKenzie2, David Morse2, Tim Bishop1, and Jason Bernard1
1St. George’s Hospital, London, UK
2K2M, London, UK
Introduction: Training around the world must become more efficient and more effective than ever before. Part of the focus arises due to restrictions such as the European Working Time Directive (EWTD) dictating a 48-hour working week. Surgical trainees have less opportunity to acquire the appropriate skills in the less amount of time. J. Kauffman (Author: The First 20 Hours) examined the K. Anders-Ericsson study that showed 10 000 hours is required to be an expert, he suggests you can be good at anything in 20 hours. Methods: Eight junior spinal surgeons and 1 control candidate (physiotherapist) attended a Cadaveric Pedicle Screw Insertion Course with 20-hour focused training. A competence pre-course and post-course questionnaire (Likert-type scale) was conducted. Examination of left/right thoracic screw, lumbosacral, cervical screw insertion by time was measured. Each candidate had 2 cadavers per person. Complications such as pedicle breaches were recorded by a senior trainer once the screws were removed with a ball-tipped probe. Results: Candidate mean time thoracic (T) were: 96.8; 72.2; 61.4; and 57.4 minutes with mean pedicle errors: 2.6; 2; 2.1; and 2.2. Mean lumbar (L): 51.9; 50.1; 42.0; and 33.7 minutes with mean errors: 0.2; 0.3; 0.7; and 0.2. Mean cervical (C): 43.6 and 44.9 minutes with mean errors: 1.2 and 0.3. Control thoracic: 142,134,145, and 93 minutes; control Lumbar: 92; 93; 65; and 60 minutes candidates total mean pre-course competence; 5.41, post-course; 7.35, change in score; +1.94 control: pre 2.4; post:5.0; Change: +2.6. Conclusion: Pedicle screw insertion can cause significant morbidity, including paralysis; and therefore as a trainee, this is not an easy skill to acquire or practice. This focused pedicle screw course deconstructed spinal surgery, isolated this single skill, and provided a concise 20 hours and the critical tools. We show that a junior spinal surgeon can achieve improved competency, effectiveness, and efficiency in 20 hours; but furthermore, a complete novice can learn to be competent.
P027: Effect of Facilitation of Endogenous Revascularization on Secondary Injury Development and Promotion of Neural Regeneration Following Traumatic Spinal Cord Injury
Vanessa Hubertus1, Peter Vajkoczy1, and Michael Fehlings2
1Charité University Medicine, Berlin, Germany
2Krembil Research Institute, University Health Network, University of Toronto, Toronto, Ontario, Canada
Introduction: Following traumatic spinal cord injury (SCI), profound vascular changes occur in the traumatized spinal cord. Following rapid changes in microvasculature and a traumatic disruption of the blood–spinal cord barrier due to primary injury, inflammation and endothelial cell death occur, spreading the secondary injury through mechanisms that include but are not limited to the resultant hypoxic environment. While endogenous revascularization including angiogenesis and vasculogenesis occur within the first days following SCI, the extent of spontaneous repair of the microvasculature is insufficient to promote neural tissue repair and regeneration. The overarching hypothesis guiding our work is that facilitation of endogenous revascularization after acute SCI will attenuate the secondary injury and promote neural repair and regeneration. Material and Methods: We conducted a comprehensive systematic review of the literature, using the established databases Medline, PubMed, PubMed Central, and the Cochrane Library for Systematic Reviews. A total of 94 key articles were reviewed. Main terms examined in these articles were vascular changes, hypoxia, blood–spinal cord barrier disruption, inflammation, and endogenous revascularization following SCI. Our search did not include a time limit and was conducted up to September 2018. Results: Endogenous revascularization occurs within the first 7 days following experimental spinal cord injury. These sprouting vessels are of inferior functional capacity, with a dysfunctional neurovascular unit due to an inchoate blood–spinal cord barrier. We review potential mechanisms to ameliorate these endogenous repair mechanisms, to establish a functional neurovascular unit in growing blood vessels to diminish hypoxic environment spreading secondary injury to surrounding healthy spinal cord regions. Building on this research, we present a new experimental model to explore the regenerative capacity of one of the most promising molecules promoting vascular repair, VEGF-A (vascular endothelial growth factor-A). Conclusion: Ameliorating the deficient neurovascular repair by endogenous revascularization following spinal cord injury will diminish secondary injury development and lead to enhanced neural repair and regeneration. For a thorough understanding of those molecules to potentially enhance these repair mechanisms, like VEGF-A, experimental models to review their regenerative capacity in detail are currently lacking and will be of great use for future research.
P028: Effect of Local Zoledronic Acid Administration in a Rat Model of Posterolateral Spinal Fusion
Ashley Strickland1, Daniel Cavanaugh2, James Raynor2, Alex Brown2, William Leatherwood2, and Paul Weinhold2
1University of Maryland, Baltimore, MD, USA
2University of North Carolina, Chapel Hill, NC, USA
Introduction: Spinal fusion is a common orthopedic procedure; however, pseudoarthrosis remains a frequently encountered complication occurring in 10% to 30% of cases. As a result, therapies to improve spinal fusion rates are needed. Systemically administered zoledronic acid (ZA) has recently been shown to have a positive impact on spinal fusion rates and fusion mass quality in animal model studies.1 In addition, studies of biologic ingrowth of implants have also shown that the local delivery of ZA can improve bone ingrowth and mechanical stability of intramedullary implants.2 Therefore, the objective of our study was to determine if local administration of ZA by soaking of bone autograft would affect the apparent bone density or the bending structural properties of the fusion mass in a rat model of posterolateral spinal fusion. Our hypothesis was that locally administered zoledronic acid would promote improved spinal fusion.3 Material and Methods: Thirty-six Sprague Dawley female rats underwent L4-L5 bilateral posterolateral spinal fusion with morselized caudal vertebral autograft. The animals were randomized by weight into 3 treatment groups based on the 0.1 mL solution used to soak the autograft prior to implantation: (1) Control: saline solution, (2) ZA20: 20 μg/mL ZA solution, (3) ZA 200: 200 μg/mL ZA solution. The fusions were carried out utilizing a bilateral Wiltse approach. Radiographs were taken to verify proper graft placement. At 8 weeks, the rats were euthanized for analysis. Evaluation consisted of micro–computed tomography (MicroCT) scan imaging (n = 10/group), 4-point bending in flexion (n = 10/group) of fusion stiffness and peak load prior to 2 mm of displacement, and histology (n = 2/group). Data were analyzed with a 1-way ANOVA (analysis of variance) with Holm-Sidak mean comparison testing. Results: MicroCT evaluation of the fusion mass demonstrated increased (P < .05) mean apparent density and bone volume fraction (Control: 0.297 ± 0.060, ZA 20: 0.466 ± 0.072, ZA 200: 0.513 ± 0054) with local ZA treatment. In contrast, improvements in linear stiffness with ZA treatment with flexion bending did not reach statistical significance (P = .213). Similarly, improvements in peak load prior to 2-mm displacement during flexion bending tests (Control: 12.1 ± 3.4, ZA 20: 17.7 ± 8.3, ZA 200: 17.8 ±7.5) also did not reach statistical significance (P = .083) with ZA treatment. Toluidine blue–stained histology sections revealed evidence of new bone formation with osteoblastic rimming of bone fragments in all specimens, as well as remodeling with multinucleated giant cells noted in all specimens. Conclusion: Our findings suggest locally administered ZA has a positive effect on the apparent density and bone volume fraction of the fusion mass during posterolateral spinal fusion. The trends for improvements in linear stiffness and peak load with local ZA administration may require larger sample sizes or more extended evaluation time points after surgery for these biomechanical improvements to be more clearly established. In addition, refinement in the local administration method may also help achieve more consistent biomechanical improvements with local ZA treatment. Local zoledronate treatment of bone autograft shows promise as a convenient method of promoting spinal fusion at the time of surgery. However, further refinement in the local administration method appears necessary to achieve more consistent improvements in biomechanical properties of the spinal fusion.
Reference
1. Yasen M, Li X, Jiang L, Yuan W, Che W, Dong J. Effect of zoledronic acid on spinal fusion outcomes in an ovariectomized rat model of osteoporosis. J Orthop Res. 2015;33:1297-1304.
2. AbuMoussa S, Ruppert DS, Lindsay C, Dahners L, Weinhold P. Local delivery of a zoledronate solution improves osseointegration of titanium implants in a rat distal femur model. J Orthop Res. 2018;36:3294-3298.
3. von Knoch F, Jaquiery C, Kowalsky M, et al. Effects of bisphosphonates on proliferation and osteoblast differentiation of human bone marrow stromal cells. Biomaterials. 2005;26:6941-6949.
Acknowledgements
Support provided by the UNC-Chapel Hill Orthopaedic Research Fund and the Aileen Stock Research Fund with histology support by NIH grant P30-DK034987. All animal work was approved by the local Institutional Animal Care and Use Committee.
P029: Increased Osteoblastc Activity Suppressed Proliferation of Multiple Myeloma Plasma Cells
Hyung-Youl Park1, Young-Hoon Kim1, Kee-Yong Ha1, Sang-Il Kim1, and Jun-Hyung Cho1
1Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
Introduction: Multiple myeloma (MM) is one of the representative hematologic malignancies that cause skeletal-related events (SREs), and dysregulation of bone remodeling is known as a key pathomechanism of disease progression and skeletal-related events. However, decreased proliferation of MM at fracture sites is frequently noted in clinical situations regardless of systemic disease activity. The purpose of this study is to investigate the impact of increased osteoblastic activity on the proliferation and survival of MM plasma cells in vitro. Material and Methods: Co-culture under various conditions was used to investigate effects of increased osteoblastic activity on survival and proliferation of MM plasma cells. MM plasma cells were cultured in culture media (control) and co-cultured with human mesenchymal stem cells (hMSCs, group I), osteoblasts (OBs) induced from hMSCs (group II), or bone morphogenic protein-2 (BMP-2, group III). Proliferation measured as ERK and IgG expression and apoptosis measured as FACS with annexin V method, and caspase-3 and stat-3 expression were assessed for cultured MM plasma cells, along with expression of sclerostin. Results: After 72 hours of co-culture, group II and III showed decreased ERK expression compared with controls. Lower IgG expression was also noted for groups II and III compared with controls. Group I did not show significantly decreased IgG and ERK expression compared with controls. Expressions of caspase-3 in groups II and III were higher than controls. Co-culture with hMSCs showed decreased caspase-3 expression compared with control. FACS with annexin V showed higher apoptosis in groups II and III. Sclerostin expression was also decreased in osteoblastic conditions compared with the control and hMSCs co-culture condition. Conclusion: Collectively, our data suggest that increased osteoblastic conditions may provide not only prevention of SREs but also anti-tumor effects on MM cells in the bone marrow environment.
P030: Methylene Blue is an Effective Disclosing Agent for Identification of Bacterial Biofilms on Orthopedic Implants
Jeremy Shaw1, Nicholas Ashton1, Jeremy Gililland1, Darrel Brodke1, Brandon Lawrence1, Erik Hansen2, and Dustin Williams1
1University of Utah, Salt Lake City, UT, USA
2University of California, San Francisco, CA, USA
Introduction: Tenacious bacterial biofilms pose a major challenge in treating deep spine infections. Biofilms provide bacteria substantial protection against antimicrobial agents, the host immune response, and are invisible to the naked eye. Biofilms are notoriously difficult to eradicate, and to that end, methylene blue has shown promise as a biofilm disclosing agent in the arthroplasty literature in both in vitro and in vivo settings. The purpose of the present study was to assess methylene blue as a biofilm disclosing agent in vitro for common biofilm forming infections and to determine performance characteristics across a range of implant materials and normal tissue types. Methods: Staphylococcus aureus and Pseudomonas aeruginosa biofilms were grown to maturity in bioreactors according to established laboratory protocol on titanium, cobalt chromium, and polyetherketone (PEEK). Biofilms were stained with 0.005% (1:100) and 0.01% (1:50) methylene blue solutions for 5 minutes and then washed with normal saline for 1 minute. Gross images were obtained to compare the visual sensitivity of the blue dye at different dilutions. Scanning electron microscopy was performed to confirm the presence or absence of biofilm on methylene blue–stained areas. Uninoculated wafers were treated with the same staining protocol and used as controls. Representative healthy adult sheep tissues were also stained to determine staining characteristics of host tissue. MATLAB digital imaging software was used to determine relative blue intensity of stained implants and tissues compared with serial dilution-based standard curves. Results: Staphylococcus aureus and Pseudomonas aeruginosa biofilms were grown for 7 days on double-sided titanium, cobalt chromium, and PEEK (n = 4 each). There appeared to be a visible dose-dependent relationship based on the staining and dye concentration. At each dilution, biofilms demonstrated visible blue staining after immersion in methylene blue solution; however, blue dye was visible only where biofilms were present as confirmed by SEM. Of healthy sheep tissues, only articular cartilage and meniscus demonstrated significant staining; bone, tendon, muscle, nerve, and fat did not stain (P < .05). Methylene did not stain any implant materials. Conclusion: Methylene blue functions as an effective disclosing agent for Staphylococcus aureus and Pseudomonas aeruginosa biofilms in vitro. Methylene blue does not stain implants, nor does it uniformly stain host tissues in vitro. Currently, there are no techniques for identifying bacterial biofilm in vivo once it has formed. Given in vitro success, methylene blue may allow surgeons to see biofilms on implants and host tissue in vivo and in so doing may allow for eradication of biofilms once visualized. Further work is needed to better elucidate this concept.
P031: A Trans-Sacroiliac Rotating Sacral Osteotomy Can Change Pelvic Incidence: Proof of Concept in Sawbone and Cadaveric Models
Darren Lui1, Jean Charles Le Huec2, Jan Herzog1, Timothy Bishop1, and Jason Bernard1
1St. George’s Hospital, London, UK
2Bordeaux University Hospital, Bordeaux, France
Introduction: The pelvic incidence (PI) is recognized to represent a signature to the individual, which is not altered after the patient reaches skeletal maturity. Roussouly is credited for linking it’s relevance to lumbar lordosis and thoracic kyphosis. There exist some challenging scenarios in spinal deformity surgery, for example, the high PI spondylolisthesis with high-grade slip or the extremely low PI or the rigid/fused spine with PILL (pelvic incidence-lumbar lordosis) mismatch. Sometimes, altering lumbar lordosis to match PI might not be possible but altering PI to suit lordosis might be an exit strategy. We describe a novel technique to alter the PI and tested this theory on a sawbone and cadaveric model. Methods: A sawbone of the pelvis and cadaveric pelvis with lumbosacral spine were utilized. Initially, a proof of concept sawbone model was developed. A single trans-sacroiliac screw across S1 was inserted. An H-type osteotomy was performed in the sacrum to allow rotation across the trans-sacroiliac screw. The models were placed in XR (X-ray) and CT (computed tomography) scan to measure spinopelvic parameters. Following proof of concept, the cadaveric specimen had the procedure repeated and was then examined closely to identify if sacral nerve roots were damaged and to establish safe distances for osteotomy cuts. Results: In the sawbone model, the osteotomy as described allows unrestricted correction of PI in an arc from 0° to 90°. In the cadaver study, pelvic floor attachments result in restriction to 15°. Ultrasonic bone cutter helped provide accurate osteotomy cuts. We therefore created a low sacral osteotomy to allow the coccyx to remain static. We show a minimum distance from the osteotomy to the sacral neuroforamina of at least 3 mm to be safe and a safety margin toward the iliac vessels and the rectum of at least 15 mm in our cadaver study on axial CT imaging. Conclusion: This novel technique to alter the PI has been shown to be feasible and possible in a proof of concept sawbone model and then an anatomical cadaveric model. Ultrasonic bone cutter was helpful to create appropriate cuts. Unlike previous S1 osteotomies similar to a PSO (pedicle subtraction osteotomy), one avoids neural structures, namely, the important L5 and S1 nerve roots. We have shown parameters to keep the procedure safe from neurovascular injury. The sawbone and cadaveric models show feasibility. Further clinical studies are required in specialized cases.
P032: Effect of Various Lumbar Spine Pathologies on Multifidus Muscle Fatty Infiltration
J. Naresh Babu1 and V. Arun Kumar1
1Mallika Spine Centre, Guntur, India
Introduction: Multifidus along with other paraspinal musculature is regarded as the primary stabilizer of spine. There has been an increased interest to better understand the various lumbar spinal pathologies and their effects on the multifidus muscle. Several recent studies have investigated the biomechanics and microstructures of the multifidus muscles in patients with lumbar disc herniation. An association between multifidus muscle degeneration and chronic low back pain, degenerative disc disease, radiculopathy, and scoliosis has been described. However, there have only been a few reports on magnetic resonance imaging (MRI) analysis of the paraspinal muscles in lumbar disc herniation (LDH), lumbar canal stenosis (LCS), and lumbar spondylolisthesis (LS) in lower lumbar levels. The present study aimed to compare the paraspinal muscle-fatty infiltration in various lumbar pathologies and determine the association between fatty infiltration in multifidus and lumbar pathologies. Material and Methods: Prospective study of 65 cases with LDH (n = 20), LCS (n = 21), and LS (n = 24). All cases underwent MRI (1.5 T) in supine position. Measurements were taken using ImageJ software (1.5i version). Measurements included total cross-sectional area (CSA), lean CSA, T1 signal intensity ratio of multifidus to psoas, ratio of lean to total CSA. The measurements were performed at the mid-discal level on bilateral sides from L1-L2 to L5-S1. The ratio of lean-to-total CSA is utilized as a measurement of fatty infiltration. Results: Of the 65 patients included in the study, 39 were female and the mean age was 42.8 ± 10.2 years. Percentage of mutifidus fatty infiltration in lower 2 lumbar levels of controls was 31.3 ± 4.3%, while in LDH patients, it was 43.5 ± 3.5%, LCS reported 38.6 ± 2.4%, and LS patients had 63.1 ± 4.6% (Figure 1). In comparison with controls, percentage of fat abnormally increased in instability patients and marginally increased in disc herniation cases. Conclusion: The fatty infiltration of the multifidus muscle was more in all the patient groups compared with controls. Multifidus fatty infiltration was noted highest in patients with lumbar spinal instability followed by lumbar disc herniation and lumbar canal stenosis.
P033: Progressive Pedicle Screw Accuracy in Clinical Utilization of Navigated, Robot-Assisted Spine Surgery
David Wallace1, Arnold Vardiman1, Neil Crawford2, Leigh Ahrendtsen2, Jessica Riggleman2, Saif Khalil2, and Charles Ledonio2
1University of Texas Health San Antonio, San Antonio, TX, USA
2Musculoskeletal Education and Research Center (MERC), A Division of Globus Medical, Inc, Audubon, PA, USA
Introduction: In the emerging field of robot-assisted spine surgery, radiographic evaluation of pedicle screw accuracy in clinical application is an area of high interest. This study describes the pedicle screw accuracy of the first 30 cases in which navigated robotic assistance was used in a private practice clinical setting. Material and Methods: A retrospective, IRB (institutional review board)–exempt review of the first 30 navigated, robot-assisted spine surgery cases was performed. Radiographic evaluation of screw tip and screw tail offset distance and angulation from preoperative plan to actual final placement based on intraoperative computed tomography (CT) images was calculated. Additionally, pedicle screw malposition, reposition, and return to operating room (OR) rates were collected. A CT-based Gertzbein and Robbins system (GRS) was used to classify pedicle screw accuracy. Results: The first 30 cases had 182 pedicle screws placed. Average age was 65 years, and 44% were female. Average body mass index was 29 kg/m2. Diagnoses for surgery were degenerative disc disease (20) and adjacent segment disease (7). The average offset from preoperative plan to actual final placement was 2.05 mm from the tip, 1.94 mm from the tail, and 2.1° of angulation. Additionally, comparing the first 91 to the last 91 screws placed, significant improvements (P < .01) were observed in accuracy by 25% in tip placement (2.34-1.75), 29% in tail placement (2.26 to 1.61), and 14% in angulation (2.25 to 1.94). Based on the GRS CT-based grading, 99.5% were graded A or B, and only 1 screw was graded C (that screw trajectory was intentionally lateralized for optimal fixation). There were more Grade A pedicle screws placed in the second half of screws (48.4% vs 41.2%) than in the first half. Two of 182 (1.09%) screws had to be aborted from the robot-assisted technique. There were no returns to the OR for screw-related complications. Conclusion: These data demonstrated a high level of accuracy in the clinical use of navigated, robot-assisted surgery, with no malpositions requiring return to the OR. Additionally, screw placement and angulation accuracy improved with experience.
P034: Minimally Invasive Sacroiliac Joint Fusion Using a Novel Hydroxyapatite-Coated Screw: 2-Year Clinical and Radiographic Outcomes
Louis Rappoport1, Torrey Shirk2, Jessica Riggleman2, and Charles Ledonio2
1Arizona Spine Consultants, Phoenix, AZ, USA
2Musculoskeletal Education and Research Center (MERC), A Division of Globus Medical, Inc, Audubon, PA, USA
Introduction: The proper diagnosis and treatment of sacroiliac joint (SIJ) pain remains a clinical challenge. Dysfunction of SIJ can produce pain in the lower back, buttocks, and extremities. Triangular titanium implants for minimally invasive SIJ fusion have achieved visual analogue scale (VAS) and Oswestry Disability Index (ODI) improvements in 83% of patients compared with nonsurgical management in a randomized clinical trial. This study reports on a novel hydroxyapatite-coated titanium screw for surgical treatment of SIJ dysfunction. Methods: Data were prospectively collected on 43 consecutive patients who underwent minimally invasive SIJ fusion with a novel hydroxyapatite-coated screw. Clinical assessments and radiographs were collected and evaluated at 12 and 24 months postoperatively. Results: Mean patient age was 54.2 ± 10.4 years, and 65.1% of patients were female. Mean operative time was 39.2 ± 18.9 minutes, and estimated blood loss did not exceed 50 cc. Overnight hospital stays were required for 88.4% of patients, while remaining patients needed a 2-day stay. Mean preoperative VAS back, left, and right leg pain scores decreased significantly by 26.3, 25.1, and 25.5 points, respectively, at 12 months postoperatively (P < .01) and by 30.1, 27.0, and 26.3 points, respectively, at 24 months postoperatively (P < .01). ODI scores significantly decreased by a mean of 21.9 points at 12 months and 28.3 points at 24 months (P < .01). All patients who were preoperatively employed returned to work within 3 months. Two patients who required revision surgery reported symptom improvement within 3 weeks and did not require subsequent surgery. Conclusions: SIJ fusion using a hydroxyapatite-coated screw to treat SIJ dysfunction significantly decreased VAS back and leg pain and ODI scores at 1 year and remained durable at 2-year follow-up.
P035: Minimally Invasive Sacroiliac Joint Fusion Using a Novel Hydroxyapatite-Coated Screw System Improves Functional Outcomes in Patients With Sacroilitis at 1-Year Follow-up
Alex Mohit1, Jessica Riggleman2, Amber Edsall2, Saif Khalil2, and Charles Ledonio2
1South Sound Neurosurgery, Puyallup, WA, USA
2Musculoskeletal Education and Research Center (MERC), A Division of Globus Medical, Inc, Audubon, PA, USA
Introduction: The sacroiliac joint (SIJ) has been implicated as a source of chronic low back pain in 15% to 30% of patients. The mainstay of therapy for disorders of the SIJ has been nonoperative treatment, including activity modification, nonsteroidal anti-inflammatory drugs, and physical therapy. SIJ injections provide diagnostic information and occasional durable therapeutic benefit. When these modalities fail, sacroiliac joint fusion may be recommended. This study describes the clinical outcomes of a novel hydroxyapatite-coated titanium screw for surgical treatment of SIJ dysfunction. Material and Methods: This study is a retrospective, institutional review board–exempt chart review on 45 consecutive patients who underwent minimally invasive SIJ fusion with a novel hydroxyapatite-coated screw system. Patients were diagnosed based on the North American Spine Society guidelines and evidence-based criteria. Clinical assessments were collected, evaluated, and compared preoperatively and at 12 months postoperatively. Results: Mean patient age was 69.4 ± 9.6 years, and 60.0% of patients were female. Mean preoperative visual analogue scale sacroiliac (VAS SI) pain scores decreased significantly by a mean of 6.1 points at 12 months postoperatively (P < .001). Oswestry Disability Index (ODI) scores significantly decreased by a mean of 41.4 points at 12 months postoperatively (P < .001). Twenty percent (9/45) of patients underwent bilateral SIJ fusion, while the remaining were unilateral. Screw size ranged from 10 × 35 mm to 10 × 50 mm. Conclusion: The clinical outcomes of SIJ fusion using a hydroxyapatite-coated screw system to treat sacroilitis significantly decreased VAS SI and ODI scores at 1 year.
P036: A Retrospective Review of Transforaminal Lumbar Interbody Fusion Patients Treated With Expandable and Static Spacers
Adam Kremer1, Jefferson Alferink1, Stacie Wynsma1, Torrey Shirk2, Saif Khalil2, and Charles Ledonio2
1The Brain + Spine Center, Holland, MI, USA
2Musculoskeletal Education and Research Center (MERC), A Division of Globus Medical, Inc, Audubon, PA, USA
Introduction: Utilization of interbody spacers for transforaminal lumbar interbody fusion (TLIF) offers favorable clinical results. Expandable devices allow for in situ expansion to optimize fit and mitigate iatrogenic endplate damage that occurs during trialing and impaction as seen in static devices. This study compared the clinical and radiographic outcomes between static and expandable spacers following TLIF. Materials and Methods: A retrospective chart review of patients from a single site was performed on 99 patients who underwent TLIF using 1 of 2 interbody spacers. Forty-eight patients received a static PEEK (polyetheretherketone) interbody spacer, and the remaining 51 patients received an expandable titanium interbody spacer. Surgical data, Oswestry Disability Index (ODI), and visual analogue scale (VAS) pain scores were collected and analyzed. Radiographs were collected and measured when available. Complication rates were compared using Fisher’s exact test. Results: Patients treated with expandable interbody spacers had significantly (P < .05) less blood loss (81.7 vs 36.2 cc) and shorter hospital stays (2.2 vs 1.4 days). Operating room time was lower for patients treated with expandable interbody spacers than static spacers (130.6 vs 149.5 minutes), although this difference was not significant (P = .07). At 3-month and final follow-up, patients treated with expandable implants had significantly lower ODI scores than patients with static implants (P < .05, 14.4 and 22.6, respectively). Disc height and neuroforaminal height increased significantly (P < .05) from baseline at the 3-month follow-up time point for both interbody spacers, although the expandable group had significantly greater neuroforaminal height (22.3 vs 20.1 mm). There was a significant (P < .05) difference in complication rates between static and 2% for expandable group. By standard of care, only patients that reported a recurrence of low back pain were required to follow-up with their surgeon past 3 months postoperatively. Only 3 of 51 (6%) patients from the expandable group had to follow-up at >24 months, compared with 12 of 48 (25%) patients in the static group. Conclusion: Patients treated with expandable interbody fusion spacers used in a transforaminal approach demonstrated significantly less blood loss, shorter length of stay, lower ODI scores, and significantly fewer complications at final follow-up than patients treated with static spacers.
P037: Tranexamic Acid in Elective Spine Surgery: A Randomized Controlled Trial Analyzing the Efficacy of Intravenous Local Infiltration, and Topical Administration of Tranexamic Acid
J. Naresh Babu1 and V. Arun Kumar1
1Mallika Spine Centre, Guntur, India
Introduction: Instrumented spine surgery can be associated with significant blood loss. Extensive blood loss leads to negative outcomes and remains a challenge. Administration of antifibrinolytic drugs such as tranexamic acid (TXA) is one of the popular blood conservation strategies. Intravenous TXA (ivTXA) has almost become a standard for bleeding management in spine surgery. However, the systemic complications associated with it may be rare but not uncommon. To negate these effects, topical application of TXA (tTXA) has been used recently with good amount of success. Although local infiltration of TXA (loTXA) has been used in trauma-related hemorrhages, till date there is no literature available examining its efficacy in spine surgery. The purpose of the study is to evaluate the safety and efficacy of TXA administered through various routes (ivTXA, tTXA, and loTXA) in instrumented spine surgeries. Methodology: A total of 104 patients requiring instrumented spinal fusion formed the study group. All participants were assigned to 4 groups (26 in each group) using simple, equal probability randomization scheme. Groups included (1) ivTXA—intravenous administration of TXA 1 hour prior to surgery; (2) loTXA—local infiltration of TXA bilaterally into the paraspinal musculature prior to incision; (3) tTXA—topical application of TXA just before wound closure; (4) Control group. Topical administration of TXA was strictly avoided in the patients with dural tear/CSF (cerebrospinal fluid) leak. Outcome measures include intraoperative blood loss (IOBL), postoperative blood loss, need for blood transfusion, length of hospital stay, and blood parameters (Hb, PCV, PT, APTT, INR). Results: The average intraoperative blood loss in control group was 344 ± 88 mL and post-operative drain collection on first POD (postoperative day) was 316.3 ± 110.1 mL. All the 3 groups with different modes of TXA administration were found to be effective compared with the control group. None of the patients had any complications related to TXA administration. Intraoperative blood loss was significantly reduced in ivTXA (223.6 ± 40.1 mL) and loTXA (256.07 ± 119 mL) groups when compared with controls (344 ± 88.5 mL). Whereas, the postoperative blood loss as measured by the total sum of the drain collection was least in tTXA followed by ivTXA, loTXA, and controls. There was 67% reduction in need for blood transfusion in tTXA group, 55.5% reduction in ivTXA group, and 33% reduction in loTXA group when compared with the control group. Conclusion: In instrumented spine surgery, there is significant postoperative blood loss almost equal to that of intraoperative blood loss. ivTXA and loTXA are found to be equally effective in reducing the intraoperative blood loss. Whereas, the topical TXA has better postoperative blood-conserving effects. This is the first study to detail about safety and efficacy on local infiltration of TXA in spine surgery, which is an effective and safe method for reducing intraoperative blood loss.
Biomarkers
P038: Malignant Primary Spinal Column Tumors: Prognostic Significance of HTERT (Human Telomerase Reverse Transcriptase) Promoter Region Mutations C228 T and C250 T for Overall Survival
Chetan Bettegowda1, Stephen Yip2, Bowen Jiang1, Wei-Lien Wang3, Michelle Clarke4, Aron Lazary5, Marco Gambarotti6, Ming Zhang1, Daniel Sciubba1, Jean-Paul Wolinsky1, Edward McCarthy1, Niccole Germscheid7, Arjun Sahgal8, Ziya Gokaslan9, Stefano Boriani10, Peter Varga5, Charles Fisher2,11, Laurence Rhines3, and AOSpine Knowledge Forum Tumor7
1Johns Hopkins University, Baltimore, MD, USA
2University of British Columbia, Vancouver, British Columbia, Canada
3MD Anderson Cancer Center, The University of Texas, Houston, TX, USA
4Mayo Clinic, Rochester, MN, USA
5National Center for Spinal Disorders and Buda Health Center, Budapest, Hungary
6Rizzoli Institute, Bologna, Italy
7AOSpine International, Davos, Switzerland
8Sunnybrook Research Institute, Toronto, Ontario, Canada
9Brown University, Providence, RI, USA
10IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
11Vancouver Coastal Health, Vancouver, British Columbia, Canada
Introduction: Primary spinal column malignancies are rare tumors with poor prognosis, few systemic treatment options, and limited understanding of the molecular drivers of neoplasia. Material and Methods: Study design was a retrospective review of prospectively collected data. An initial cohort of 1495 patients with primary spinal column tumors were treated at 13 centers within Europe, North America, and Australia between December 1985 and January 2013. Information regarding patient mortality was acquired cross-sectionally. Archived paraffin-embedded pathologic specimens were available for 133 patients from 6 of the 13 centers. Tumor DNA was extracted from the paraffin specimens and the hTERT promoter was sequenced using Sanger sequencing. The hTERT mutational status was correlated to overall survival (OS). Results: Ninety-two chordomas, 26 chondrosarcomas, 7 osteosarcomas, 3 Ewing’s sarcomas, and 5 other malignant spinal tumors were analyzed. Eight chordomas, 2 chondrosarcomas, 1 Ewing’s sarcoma, and 1 other malignant spinal tumor harbored either a C228 T mutation or a C250 T mutation in the hTERT promoter. Median OS following surgery was 5.8 years (95% confidence interval [CI] = 4.6-6.9) and median time to first local recurrence was 3.9 years (95% CI = 2.5-6.7). OS was worse in the Enneking grade II tumor group (P = .047). After controlling for standard demographic and clinical criteria, including adequacy of surgical resection and adjuvant therapy, hTERT mutational status was associated with improved survival. 100% of patients with hTERT mutation were alive at 10 years postoperative as compared with approximately 24% of patients who lacked the mutation (P = .031). Conclusion: We report for the first time that hTERT promoter mutations C228 T and C250 T are present in approximately 10% of spinal chordomas. In addition, all individuals with the hTERT mutations were alive at 10 years postoperatively compared with 24% of those lacking the mutations. Future prospective studies are required to further elucidate the role of hTERT promoter mutations in primary spinal column malignancies.
Biomechanics
P039: Parameters of Spinal Sagittal Balance in Patients with Hip-Spine Syndrome at Total Hip Replacement
Oxana Prudnikova1, Oleg Chegurov1, and Alexander Tryapichnikov1
1 Russian Ilizarov Scientific Center, Kurgan, Russian Federation
Introduction: There are controversies in the literature on sagittal balance parameters in patients with hip-spine syndrome undergoing total hip replacement surgery. Objective: To explore spinopelvic sagittal alignment in patients with hip-spine syndrome before and after total hip replacement. Material and Methods: Clinical and radiological assessment was performed for 46 patients with dysplastic (n = 14), degenerative (n = 26), and posttraumatic coxarthritis (n = 6) preoperatively, on day 7 postsurgery and at a long term. All the patients underwent primary total hip arthroplasty including 37 cementless, 7 hybrid, and 2 cemented cases. Results and Discussion: All patients had spinal pain of various intensity that indicated to hip-spine syndrome. Patients with dysplastic and posttraumatic coxarthritis showed decreased pelvic tilt (PT) and sacral slope (SS) with increased lumbar lordosis (LL). No considerable changes in spinopelvic alignment were observed in patients with degenerative coxarthritis. More evident limitations in amplitudes were seen in patients with dysplastic and posttraumatic coxarthritis. Comparison of amplitudes in the involved joint and spinopelvic parameters showed moderate correlation dependence in the cohort of patients. No correlation between spinopelvic alignment and spinal pain was noted. Pre- and postoperative Harris hip score demonstrated equally good outcomes irrespective of etiology of the disease. Only 16 patients were available for the follow-up of 161.0 ± 16.1 days (range = 96-196) after total hip replacement. No dynamics in spinopelvic alignment was noted at the time. Spinal pain persisted and was shown to improve with the Oswestry Disability Index scores and functional condition of the patients. Many authors reported changes in spinopelvic alignment coupled with pathologies of the hip joint. Biomechanical aspects of the hip-spine syndrome include flexion contracture of the hip resulting in pelvic anteversion, redistributed loading on the lumbar spine and hyperlordosis, foraminal stenosis leading to spinal pain. Parameters of spinopelvic alignment are reported to differ in patients with degenerative and secondary (resulting from hip dysplasia and dislocation) changes in the hip joint. Our findings and other series reported indicate evident osteoarthritis inducing either minimal sagittal imbalance or no changes. Conclusion: Patients with hip-spine syndrome due to degeneration showed no considerable changes in spinopelvic alignment. Dysplastic and posttraumatic coxarthritis was shown to be a predisposing factor for spinopelvic imbalance in patients undergoing total hip arthroplasty. As reported in other series, total hip arthroplasty with good functional outcome entailed no considerable changes in spinopelvic alignment.
P040: Differences of the Morphology of Subaxial Cervical Spine Endplates Between Chinese and White Men and Women
Peng Yin1, Yong Hai1, Qi Yao1, and Guoan Li2
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
2Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA
Objective: Recently, there has been an increase in the use of artificial cervical disc arthroplasty (ACDA) for degenerative conditions as an alternative to spinal fusion. Endplate geometry is crucial for the design of cervical disc implants. However, no study has quantitatively investigated the overall parameters of the cervical endplate in living subjects, nor have studies focused on morphological endplate differences in different populations. The aim of this comparative anatomical study was to specifically investigate endplate morphology differences between Chinese and white men and women. Material and Methods: Three-dimensional cervical endplate models were constructed using computed tomography imaging of 41 healthy Chinese and 24 white subjects. The morphologic measurements of cervical endplate included linear parameters (EPWu, upper endplate width; EPDu, upper endplate depth; EPWl, lower endplate width; and EPDl, lower endplate depth) and area parameters with a digital measuring system. Results: All linear parameters showed constant increase from C3 to C7 except for EPDl in both the Chinese and the white subjects. An increase trend was observed on area parameters in both Chinese and white subjects. In Chinese females, the EPWu and EPWl were smaller than white females from C3 to C5 (P < .05), and the EPDu and EPDl was smaller than white females from C5 to C7 (P < .05). The ratio of EPWl/EPDl was smaller in Chinese females than white females at C3, C4, and C6 levels (P < .05). The EPAu of Chinese females was smaller than those of white females from C3 to C6 (P < .05). In Chinese males, the EPWu and EPWl were significantly smaller than white males from C3 to C5 (P < .05) and the only significant difference was observed at C6 in EPDl (P < .05). The ratio of EPWl/EPDl was significantly different between the Chinese and white Men at C4-C5 levels (P < .05). The EPAu and EPAl of Chinese males were smaller than those of white males at C3, C4, and C6 levels (P < .05). Conclusions: Our data indicate that the morphology of subaxial cervical spine endplates between Chinese and white men and women is different in most of the liner and area parameters. This information could provide guidelines for the design of CDA implants and the improvement of surgical techniques.
P041: Biomechanical Investigation of the Influence of Electrocautery on Fatigue Life of Spinal Rod-Screw Constructs
Haidara Almansour1, Robert Sonntag1, Wojciech Pepke1, J. P. Kretzer1, and Michael Akbar1
1Heidelberg University Hospital, Heidelberg, Germany
Introduction: Instrumentation failure was shown to be attributed to the cyclic loading leading to nucleation of fatigue cracks, which later propagate and result in rod fracture. Risk factors for rod failure post spine surgery have been extensively analyzed. The potential impact of electrocautery on fatigue life of orthopedic implant has been sporadically described in literature pertaining to arthroplasty. A biomechanical analysis of this impact on spinal constructs has not been performed thus far. The aim of this study is to assess the safety of Titanium (Ti) and Cobalt-Chrome (CoCr) rod-screw constructs after being treated with electrocautery. Material and Methods: This is an in vitro biomechanical investigation of fatigue life using vertebrectomy model composed of bilateral rod pedicle-screw constructs. Twelve spinal constructs with CoCr and Ti rods were examined using the ASTM F1717-01 model in a double-rod configuration. The 12 specimens were divided into 4 groups pertaining to rod material (Ti or CoCr) and to the application of monopolar electrocautery device on rods’ surface (control group [CG] and electrocautery group [EG];(n = 3 for each group). Electrocautery device was applied on each rod at 3 locations. Constructs were cycled at a load ratio of 10 between a minimum and maximum loading regime of 10/100 N and 45/450 N at a frequency of 12 Hz. Load was increased stepwise with 1 million cycles per step. Outcome measures were estimated fatigue strength, load, number of cycles to failure, and location of rod failure. Results: Ti rod constructs treated with electrocautery (Ti-EG) demonstrated significantly lower fatigue life than the intact Ti rods (Ti-CG; P = .023). Intergroup comparison of cycles to failure revealed a significant mean decrease of almost 9 × 105 cycles (P = .03). No CoCr rods failed in this experiment but all of the spinal constructs with CoCr rods failed at the Ti pedicle screw. Conclusion: Electrocautery application on the surface of Ti rods significantly reduces their fatigue life. On the other hand, CoCr constructs were not affected. Surgeons might want to consider using a classical surgical blade in the vicinity of Ti rods to mitigate the risk of rod failure.
P042: A Novel Calcium Phosphate–Based Nanocomposite for the Augmentation of Cement-Injectable Cannulated Pedicle Screw Fixation: A Cadaver and Biomechanical Study
Haolin Sun1 and Chunde Li1
1Peking University First Hospital, Beijing, China
Introduction: Although polymethylmethacrylate (PMMA) has been widely applied for the augmentation of pedicle screw fixation in the treatment of lumbar degenerative diseases in osteoporosis patients, PMMA-associated deficiencies such as monomer toxicity, high rigidity, and nondegradability are obvious side effects. To overcome the shortcomings of PMMA, a novel injectable and biodegradable calcium phosphate–based nanocomposite (CPN) for the augmentation of pedicle screw fixation was developed based on previous study, and the handling properties and biomechanical performance of CPN were evaluated and compared with clinical PMMA by means of a cadaver study. Cement-injectable cannulated pedicle screws (CICPs) augmented with CPN or PMMA were placed in the lumbar vertebrae of osteoporotic cadavers under the guidance of 3-dimensional (3D)-printed templates for each vertebra. X-ray and computed tomography (CT) scan evaluated the accuracy of screw placement and cement interdigitation. The biomechanical properties were compared using axial pullout strengths and torque values. Material properties of CPN were also characterized. Materials and Methods: Four osteoporotic lumbar vertebrae, including L1-L5, were harvested from fresh-frozen elderly female cadavers. Bone mineral density (BMD) of the lumbar vertebrae was tested. Pedicle screws were placed into the lumbar vertebrae under the guidance of 3D-printed templates, each of which was designed based on CT reconstruction of each vertebrae, and augmented with either PMMA or CPN. X-ray and CT scan were used to evaluate the accuracy of screw placement and dispersion as well as interdigitation of bone cement. The axial pullout strength and maximum torque were tested using a mechanical testing machine. Results: Forty CICPs were successfully inserted under the guidance of 3D-printed templates. It was revealed that no pedicle screws had broken through the pedicle. There was no significant difference in the projected area and dispersion volume of the 2 types of bone cement (P > .05). Results of the projection area and estimated volume revealed that CPN exhibited dispersing and interdigitation abilities similar to PMMA. But the dispersion pattern was different between CPN (surrounding the screw symmetrically) and PMMA (limited to the proximal part of the screw). Axial pullout test results showed that the axial pullout strength of CPN-augmented pedicle screws was 1194.32 ± 221.58 N, which was slightly lower than PMMA (1346.42 ± 453.12 N; P > .05), but significantly higher than the screws without cement augmentation (693.41 ± 311.50; P < .01). CPN showed average torque values of 0.72 ± 0.31 N m lower than those of PMMA (0.96 ± 0.23 N m; P > .05), but still higher than the screws without cement augmentation (0.29 ± 0.12 N m; P < .05). Conclusions: Under the guidance of 3D-printed templates, a standardized insertion process accurately places the screw into a predetermined position for the biomechanical test. CPN has dispersion and interdigitation ability similar to PMMA, although the 2 types of dispersion are different, and CPN has a better dispersion mode. CPN has biomechanical properties similar to PMMA in the application of augmentation for CICPs fixation in cadaveric vertebrae.
P043: Golden Ratio and Morphometric Differences of Vertebral Bodies Between Scoliotic and Non-Scoliotic Individuals
Josip Buric1
1Spine Surfgeryt, Forte dei Marmi, Italy
Introduction: The hypothesis was if a golden proportion exists in the vertebral column elements and if there is any statistically significant difference in proportional values between the non-scoliotic and scoliotic vertebral bodies. Material and Methods: A consecutive search of vertebral column images between 2012 and 2015. The study included images from 446 individuals for a total of 947 vertebras divided into 4 groups: young non-scoliosis subjects, adult non-scoliosis subjects, young scoliosis subjects, and adult scoliosis subjects. The measurement done was of the proportional value of the lateral aspect of a vertebral body. Results: The work showed that, under certain measurements, a vertebral body has a proportion that is close to the golden proportion value. An apparently significant and steady difference was found when measuring the proportional values of vertebral bodies of scoliotic subjects as compared with the non-scoliotic ones. Conclusion: What might be the anatomical or pathological significance of these different values is unclear although a possible genetic error in coding of the dimensions and shape of the vertebral bodies might be a possible explanation. A possible hypothesis might be that a different morphology of vertebral bodies might exhibit a substantially different stability pattern of the vertebral column.
P044: Instability After Laminectomy in Degenerative Lumbar Scoliosis: Is Spinal Fusion Really Necessary?
Christine Rustenburg1, Sayf Faraj2, Roderick Holewijn3, Agnita Stadhouder1, Barend van Royen1, Theodoor Smit1, Idsart Kingma4, and Kaj Emanuel1
1Amsterdam University Medical Center, Amsterdam, Netherlands
2Radboud University Medical Center, Nijmegen, Netherlands
3OLVG, Amsterdam, Netherlands
4Vrije Universiteit, Amsterdam, Netherlands
Introduction: Degenerative lumbar scoliosis (DLS) develops de novo as a result of degenerative processes in the lower back. Despite low Cobb angles, DLS can result in spinal stenosis, which is often accompanied with disabling symptoms. To relief patients, a single-level facet-sparing laminectomy is often performed, followed by short spinal fusion to restore stability. However, the effects of facet-sparing laminectomy as well as short fusion on the range of motion (ROM) and neutral zone stiffness (NZs) of lumbar scoliotic spines are unknown, and thus, it is not established whether fusion following a laminectomy procedure is necessary in clinical practice to stabilize the spine. Therefore, the aim of this study was to assess the ROM and stiffness around the neutral orientation of the lumbar spine after laminectomy and spinal fusion, respectively, compared with their native state. Material and Methods: Ten lumbar spines (Th12-L5) from fresh-frozen cadavers (82 ± 11 years old) with a Cobb angle ≥10° and an apex on L3 were included. A set of 3 loading cycles were applied per direction, from −4 Nm to 4 Nm in (1) flexion and extension (FE), (2) lateral bending (LB), and (3) axial rotation (AR). During the laminectomy, the laminae and spinous processes of L3 were removed, and the integrity of the supraspinous, interspinous, and flavum ligaments was lost. The spinal fusion was a short fusion from L2-L4 with pedicle screw instrumentation. Both procedures were performed by an experienced spine surgeon and were analogous to standard clinical practice. Both the laminectomy and fusion were followed by another test. The ROM and NZs were compared for differences after treatment using ANOVA (analysis of variance) with post hoc paired t tests. Results: After laminectomy, there was a minor, insignificant increase in ROM and decrease in NZs of both the lumbar spines (i,. Th12-L5) and separated segments (ie, L2-L3 and L3-L4). The spinal fusion, however, caused a significant decrease in the ROM (FE = −54%, LB = −36%, both P < .01; AR = −26%, P < .05) and increase in the NZs (FE = 118%, P < .01; LB = 50%, AR = 35%, both P < .05) of the lumbar spines compared with laminectomy. Spinal fusion decreased the ROM of the separated segments (L2-L3: FE = −33%, LB = −42%, AR −59%, all P < .05; L3-L4: FE = −46%, LB = −40%, both P < .01). There were no significant effects of the laminectomy and spinal fusion on the adjacent, non-treated segments. Conclusion: This study shows that ROM and NZs of lumbar spines with degenerative scoliosis are not affected by laminectomy. However, spinal fusion caused a severe decrease in ROM. These results indicate that a laminectomy procedure in DLS did not result in severe instability, whereas spinal fusion results in a rigid construct. Compared with previous published studies on non-scoliotic spines of the same age, the ROM of native degenerative scoliotic spines is already much lower (Figure 1). This suggests that patients with DLS would benefit from a laminectomy alone, as this would relief them from the disabling symptoms by widening the spinal canal, but that spinal fusion might not be necessary, as this only causes a severe decrease in the ROM of the lumbar spine.
Figure 1.
The changes in range of motion (ROM) after laminectomy and spinal fusion, both compared with native state, of the whole lumbar spine.
P045: Does the Addition of a Unilateral Cephalad Screw to a Standard Single Level Posterior Lumbar Fusion Construct Protect Against Future Adjacent Segment Degeneration? A Biomechanical Study Using Bovine Spine
Kenny David1 and Raunak Milton1
1Christian Medical College, Vellore, India
Introduction: Adjacent segment degeneration (ASD) remains a potential long-term complication following standard posterior lumbar interbody fusion (PLIF). We hypothesized that there would be a protective effect on adjacent segment intradiscal pressures (IDP) and motion segment stiffness by adding an additional unilateral cephalad pedicle screw to a standard 4-screw single-level fusion construct. Material and Methods: Twelve fresh bovine lumbar spine specimens were evaluated to rule out structural abnormalities. All specimens were mounted on a universal testing matching with a pulley system and were subjected to an 8-NM moment in all 6 degrees of motion. Each specimen was subjected to biomechanical testing in 3 modes—intact specimen, following application of a standard PLIF pedicle screw construct, and finally following the application of an additional unilateral cephalad pedicle screw. Superior adjacent segment IDP changes were measured using miniature pressure transducers. Range of motion (ROM) was recorded using a 3D (3-dimensional) motion tracking system using optical sensors. Results: The IDP at the superior adjacent disc was significantly increased in all except one of the tested movements when compared with the intact specimen. The mean percentage increase in flexion (FLX), extension (EXT), right lateral flexion (RLF), left lateral flexion (LLF), right axial rotation (RAR), and left axial rotation (LAR) were +13, +30, +13, +30, −9, and +13. With the addition of the unilateral cephalad pedicle screw, there was a statistically significant drop in IDP at the superior adjacent level in 4 of the 6 tested motions—FLX, EXT, RLF, and LAR. The measured values were −80, −80, −70, and −31, respectively. The ROM testing showed a statistically significant increase in construct stiffness on comparing the intact and instrumented specimens, but failed to show any further increase in stiffness on addition of the unilateral cephalad screw. Conclusion: The augmentation of a standard PLIF construct with and additional unilateral cephalad pedicle screw can mitigate increases in superior adjacent segment IDP, with no additional increase in the construct stiffness. These findings may provide insight as newer strategies evolve in the future to address the issue of ASD.
P046: Biomechanical Evaluation of Pedicle Screw Anchoring Capacity in Non-Osteoporotic and Osteoporotic Pedicles: Comparison of Straight Dual-Lead Versus Single- to Dual-Lead Threadforms
Amy A. Claeson1, Anup Gandhi1, and Amir A. Mehbod2
1Zimmer Biomet, Westminster, CO, USA
2Twin Cities Spine Center, Minneapolis, MN, USA
Introduction: Pedicle screw loosening occurs in 1% to 21%1-3 of patients at 3 to 6 months postoperatively4,5 and can lead to construct instability.6-8 Loosening has been attributed to screw insertion technique,9-11 interbody device subsidence,12,13 and compromised bone quality.11,14 Screw threadform design aims to maximize screw purchase over the spectrum of bone quality to provide superior fixation strength, resistance to loosening, and ease of insertion. Single- to dual-lead threadforms aim to provide increased fixation in dense cortical bone, but its single-lead thread provides no advantage in insertion time. Straight dual-lead threadforms provide uniform pitch over the length of the screw and have inherently decreased insertion times compared with those of single-lead screws. The objective of this study was to biomechanically assess the anchoring capacity of straight dual-lead and single- to dual-lead threadforms in axial pullout and cyclic toggle to failure, the most clinically relevant mode of pedicle screw loosening. We hypothesize both threadform designs will yield equivalent anchoring capacity, and that anchoring capacity will be greater in non-osteoporotic versus osteoporotic bone. Material and Methods: Two pedicle screw designs, a straight dual-lead pedicle screw (Zimmer Biomet) and a single- to dual-lead pedicle screw, of equal length (45 mm) and equal outer diameter (6.5 mm) were biomechanically tested in axial pullout and cyclic toggle to failure. Non-osteoporotic (n = 16, bone mineral density [BMD] >0.80 g/cm2) and osteoporotic (n = 16, BMD <.70 g/cm2) cadaveric vertebrae (T12-L5) were further stratified into axial pullout (n = 8 each) and toggle to failure (n = 8 each) groups. Trajectory was probed and tapped following respective surgical technique before one screw of each threadform was placed in each vertebra (yielding bone quality an internal control). Vertebrae were fully constrained during pullout testing, and the actuator displaced the screw axially from the pedicle at 5 mm/min to a total displacement of 10 mm; peak load recorded. Vertebral bodies were clamped axially during toggle to failure testing. A rod, secured orthogonal to the screw axis and affixed to the actuator, applied a load-controlled sinusoidal waveform beginning at −100/−10 N and increasing −50/−5 N each 200 cycles until −4 mm of displacement was achieved; load at failure recorded. Multiple Wilcoxon signed-rank tests provided statistical comparisons of anchoring capacity (peak load, failure load) based on threadform for each bone quality group. Multiple Mann-Whitney tests provided statistical comparisons of anchoring capacity based on bone quality for each threadform. Significance for all tests set to .05. Results: Neither peak load during axial pullout nor failure load during cyclic toggle were significantly different (P > .05) between threadforms in either bone quality group. Both threadforms yielded significantly larger peak (P < .05) and failure (P < .05) loads in non-osteoporotic versus osteoporotic bone. Conclusion: Straight dual-lead and single- to dual-lead threadforms yield statistically equivalent anchoring capacity within pedicles of both non-osteoporotic and osteoporotic vertebrae under nonclinical biomechanical test conditions. Time of insertion may be of consideration given equivalent anchoring capacity.
Reference
1. Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986;(203):18-33.
2. Roy-Camille R, Saillant G, Mazel C. Internal fixation of lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;(203):7-17.
3. Steffee AD, Biscup RS, Sitokowski DJ. Segmentalspine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thora-columbar spine. Clin Orthop Relat Res. 1986;(203):45-53.
4. Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg Br. 2004;86:457-461.
5. DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine Phila Pa (1976). 2006;31(19 suppl):S144-S151.
6. Heller JG, Silcox DH 3rd, Sutterlin CE 3rd. Complications of posterior cervical plating. Spine Phila Pa (1976). 1995;20:2442-2448.
7. Davne SH, Myers DL. Complications of lumbar spinal fusion with transpedicular instrumentation. Spine Phila Pa (1976). 1992;17(suppl):S184-S189.
8. Esses S, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine Phila Pa (1976). 1993;18:2231-2239.
9. Lei W, Wu Z. Biomechanical evaluation of an expansive pedicle screw in calf vertebrae. Eur Spine J. 2006;15:321-326.
10. Daftari TK, Horton WC, Hutton WC. Correlations between screw hole preparation, torque of insertion, and pullout strength for spinal screws. J Spine Disord. 1994;7:139-145.
11. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine Phila Pa (1976). 1994;19:2415-2420.
12. Tan et al. 2007.
13. Oxland TR, Lund T, Jost B, et al. The relative importance of vertebral bone density and disc degeneration in spinal flexibility and interbody implant performance. An in vitro study. Spine Phila Pa (1976). 1996;21:2558-2569.
14. Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine Phila Pa (1976). 1991;16:647-652.
P047: Effects of Inpatient Rehabilitation on Paraspinal Muscle Activity in Patients With Vertebral Body Fractures While Walking
Bernhard W. Ullrich1, Eduard Kurz2, Thomas Mendel3, Daniel Kuhn1, Klaus Fischer1, Gunther O. Hofmann5, and Philipp Schenk1
1BG Clinic “Bergmannstrost”, Halle (Saale), Germany
2Martin-Luther-University Halle-Wittenberg, Halle (Saale), Germany
3
Introduction: The inpatient rehabilitation programs of patients with vertebral spine fractures (VSF) aims to improve muscle function and reducing pain to reintegrate patients in a workplace. There is a lack in objectification and evaluation concerning muscle function due to rehabilitation effects of these inpatients. In this study, we want to investigate if it is possible to objectify changes in paraspinal muscle function due to inpatient rehabilitation. Material and Methods: Eight patients (6 male) with an age of 31 to 66 years who participated in a 4-week inpatient rehabilitation program were investigated. Intramuscular coordination was chosen to quantify intervention effects on muscle function. The intramuscular coordination was expressed as the coefficient of variation (CV) of muscle activity over the normalized stride for the lumbar and thoracolumbar regions of the paravertebral muscles. Therefore, lumbar and thoracolumbar paravertebral muscle activity was measured by bipolar surface electromyography (sampling frequency: 2048 s−1) during walking at 4 km/h for at least 30 strides on a treadmill. Distribution was checked with the Shapiro-Wilk test, and changes of the CV statistically tested with the Wilcoxon test. Due to the small sample size, Cohen’s r effect sizes are additionally given.1 Results: The samples of the CV values were not normally distributed (Shapiro-Wilk test P > .05). For the CV, the Wilcoxon tests showed significant higher values in the thoracolumbar region (P = .016, r = .84) after the rehabilitation program, but no significant change for the lumbar region (P = .367, r = .35). The results are presented in Figure 1. Discussion: Higher values of the CV mirror a greater variation of the muscle activity during the stride, which corresponds to functional activity and inactivity due to load alterations during the stride. On the other hand, lower CV values reflect a more tonic type of activity, which in turn might lead to a more rapid muscular fatigue. The inpatient rehabilitation showed a significant change for the intramuscular coordination for the thoracolumbar but not for the lumbar muscles. The rehabilitation program resulted in increased CV values with medium to large effects.
Figure 1.
Results of the coefficient of variation (CV) during the stride at 4 km/h of the paravertebral muscles in the lumbar and thoracolumbar region before and after a 4-week inpatient rehabilitation program for patients with vertebral fractures.
Reference
1. Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988.
P048: A Biomechanical Comparison of Different Posterior Lumbar Decompression Techniques in a Cadaveric Calf Spine Model
Kenny David1 and Febin Kunnath1
1Christian Medical College, Vellore, India
Introduction: A number of different surgical techniques for posterior lumbar decompression have been described with uniformly high rates of clinical success. However, the effect of these different procedures on the postoperative stability of the spine have not been as clearly understood, and previous comparative studies in this field have been of low quality. This study was designed to quantify surgery-induced spinal instability by measuring intradiscal (IDP) changes and range of motion (ROM) after different spinal decompression techniques—unilateral laminotomy, bilateral laminotomy, bilateral laminotomy with posterior ligament complex resection, and laminectomy. Material and Methods: Twelve fresh bovine lumbar spine specimens were evaluated to rule out structural abnormalities. All specimens were mounted on a universal testing machine with a pulley system and were subjected to a 7.5 NM moment in 6 degrees of motion—flexion, extension, left and right lateral flexion, and left and right axial rotations. Each specimen was subjected to biomechanical testing sequentially in 5 modes—intact specimen, unilateral laminotomy (ULM), bilateral laminotomies (BLM), bilateral laminotomies with posterior ligament resection (BLM + PLR), and finally following a complete laminectomy (LAM). Miniature pressure transducers were introduced into the disc space of the tested motion segment to measure segmental IDP changes. ROM was recorded using a 3D (3-dimensional) motion tracking system using optical sensors. Results: The IDP did not increase significantly in any of the movements tested following ULM. However, following BLM, there was a significant increase in IDP in right lateral flexion. In the BLM + PLR specimens, there was a significant increase in IDP in extension and both axial rotations. The LAM specimens showed significant increase in IDP in all 6 axes of motion tested. Segmental motion analysis showed progressively increasing ROM with increasing resection of the posterior elements. The ULM model showed increase only in right lateral flexion. The BLM specimens showed increased ROM in left lateral flexion and both axial rotations. The BLM + PLR and LAM specimens showed increased segmental motion in all the 6 planes of motion tested. Conclusion: Minimizing resection of the ligamentous and bony components of the posterior elements may be critical to preserving segmental stability and preventing postoperative instability. ULM or BLM may be preferable to laminectomy wherever lumbar decompression is indicated.
P049: Radiographic Disc Health and Biomechanics of the Cervical Spine
Vijay Permeswaran1, Vikas Patel2, Kee Kim3, Dinesh Ramanathan3, and Anup Gandhi1
1Zimmer Biomet Spine, Westminster, CO, USA
2University of Colorado, Aurora, CO, USA
3University of California, Sacramento, CA, USA
Introduction: Commonly, disc health is assessed radiographically. However, the effect of radiographically assessed disc health on biomechanics is unknown. In this study, cadaveric cervical spine specimens were graded radiographically and tested biomechanically to determine the effect of disc degeneration on range of motion. Material and Methods: Eighteen cadaveric cervical spines (C3-T1) were dissected to remove all adipose tissue and musculature while preserving ligamentous structures (11 males, 7 females, age: 59.1 ± 11.1 years). The cranial and caudal vertebrae were instrumented with bone screws, potted in high-strength resin (Bondo Body Filler, 3M), and imaged using fluoroscopy. The disc health of each level and specimen was assessed radiographically by 3 fellowship-trained surgeons, on a scale from 0 to 4, with 0 indicating a “normal or healthy” disc and 4 indicating “disc space obliteration with fusion and facet arthrosis.” Discs were then separated into healthy (≤1) and degenerated (>1) groups. Surgeon disc grading was assessed for uniformity using a Spearman’s rank-order correlation test. All specimens were instrumented and tracked using an optoelectronic motion measurement system (Optotrak Certus Motion Capture System; Northern Digital Inc, Waterloo, Canada) Each specimen was then loaded into a 6 degree of freedom kinematic testing machine (Bionix Spine Kinematics System, MTS Corporation, Minneapolis, MN) and tested in axial rotation (AR), lateral bending (LB), and flexion/extension (FE), up to a maximum of 2 Nm applied moment at a rate of 1°/s for 3 cycles. Segmental motion was recorded, and the third cycle of each motion was analyzed. The range of motion and moment data were imported into Matlab (Matlab, Mathworks, Natick, MA) for analysis. The loading phase of the third cycle for each motion was fit to the logarithmic curve θ = A ln (BM + 1), in which θ is the angle of rotation (°), M is the applied moment, and A and B are model constants. Average model constants were calculated for each disc level (overall, healthy, and degenerated) and mode of motion (AR, LB, FE). In addition, maximum range of motion for each group and mode were calculated. Results: Surgeon disc grading was found to be in good agreement. Correlations between surgeons A and B, A and C, and B and C were 0.875, 0.628, and 0.664, respectively, with all correlations being significant (P < .0001). Discs at the C5-C6 and C6-C7 levels graded significantly higher than C3-C4 discs overall (P < .01 and P = .01, respectively). For range of motion, no significant differences were seen between healthy and degenerated discs in maximum range of motion for flexion, FE, RLB, LLB, and total LB across all levels. In extension, LAR, RAR, and total AR, a significant difference was calculated between healthy and degenerated discs only at C5-C6 (E: P < .01, LAR: P = .01, RAR: P < .01, AR: P < .01). Conclusion: Although significant differences were detected between healthy and degenerated discs at each level, these differences did not translate into consistent differences in biomechanics of the cervical spine. In addition, although disc degeneration was identified at all levels, it did not appear to affect biomechanics of the spine equally.
P050: Influence of Lumbar Lordosis on Posterior Rod Strain in Long-Segment Pedicle Screws and Rods Instrumentation and Anterior Column Realignment: Cadaveric Study
Bernardo De Andrada1, Jakub Godzik1, Anna Newcomb1, Jennifer Lehrman1, Randall Hlubeck1, Juan Uribe1, Brian Kelly1, and Jay Turner1
1 St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA
Introduction: Restoration of lumbar lordosis (LL) is an essential element of spinal deformity correction surgery and differs significantly between patients. Posterior rod strain (RS) monitoring during biomechanical testing is an effective method to infer the stresses on spinal implants and predict failure mechanisms. Yet, the geometry of the final construct may have significant impact on the resultant forces. Material and Methods: Seven fresh-frozen specimens underwent standard nondestructive tests in 7.5 Nm flexion (FL), 7.5 Nm extension (EX), and 400 N compression (C) in a robotic apparatus under continuous dynamic loading. Conditions tested were the following: (1) intact; (2) pedicle screws and rods at L1-S (PSR); and (3) anterior column realignment at L3-L4 (ACR) with 30° interbody device. The posterior right rod was instrumented with strain gauges oriented in line with the long axis of the rod between L3-4 and L5-S1 pedicle screws. Lumbar lordosis spanning different levels were measured from lateral X-rays in all different conditions before loading, using the Cobb method: L5-S1, L4-S1, L3-S1, L2-S1, and L1-S1. These angles were compared with peak recorded rod strains (RS) for each test condition. Data were analyzed using Pearson correlation analysis (P < .05). Results: There were significant correlations between both intact (R 2 = .74, P = .028) and PSR (R 2 = .87, P = .007) L3-S1 angles and PSR L3-4 RS during FL, and between intact L3-S1 angle and L3-4 RS during EX (R 2 = .797, P = .018). Intact L3-S1 angle also correlated with ACR L5-S RS during C (R 2 = .86, P = .008). Intact L2-S angle correlated with PSR L3-4 RS during FL (R 2 = .86, P = .007) and EX (R 2 = .93, P = .002), as well as with PSR L5-S RS during FL (R 2 = .71, P = .030) and ACR L5-S RS during C (R 2 = .71, P = .030). Conclusion: Lumbar lordosis in both the intact spine and with PSR in place demonstrated strong correlations with in vitro posterior RS during various configurations. These relationships should be strongly considered when interpreting results of biomechanical testing in long-segment fusion models.
P051: Maximal Segmental Lordosis can be Achieved When Fixating Into Only One or Both Vertebral Bodies During Anterior Column Realignment: A Cadaveric Study
Bernardo De Andrada1, Jakub Godzik1, Anna Newcomb1, Jennifer Lehrman1, Randall Hlubeck1, Juan Uribe1, Brian Kelly1, and Jay Turner1
1St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA
Introduction: Anterior column realignment (ACR) is an effective minimally invasive technique for sagittal realignment. Osteotomy grade and extent of anterior fixation may influence ability to achieve desired correction. Many surgeons choose to fixate into only one vertebral body to ensure that corrective capacity is not limited. However, this has not been scientifically evaluated. The objective of this study was to investigate the impact osteotomy grade and anterior fixation strategies with grade 1 or 2 posterior osteotomy on ACR segmental lordosis. Material and Methods: Eight human cadaveric T12-S1 specimens were potted and instrumented. Each cadaver underwent ACR at L3/4 with a 30° implant, followed by grades 1 (G1) and 2 osteotomies (G2). Anterior fixation was achieved with an integrated plate and either a single screw into L3 vertebral body (S1) or single screw into both L3 and L4 vertebral bodies (VBs, S2). The amount of posterior compressive force (N) required to maximize lordosis was measured using strain gauges for each condition using a compressive instrument. Segmental lordosis at L3/4 interspace was measured with lateral radiographs. T test and repeat measures ANOVA were used for statistical analysis; significance was defined as P < .05. Results: Mean segmental lordosis achieved with ACR with 1 screw and no osteotomy was 16.5 ± 3.3°, with G1 osteotomy was 19.5 ± 2.3°, and with G2 osteotomy was 30.5 ± 2.8°; mean segmental lordosis achieved with ACR with 2 screws and no osteotomy was 15.5 ± 1.8°, G1 osteotomy was 19.5 ± 2.3°, and with G2 osteotomy was 28.5 ± 2.3°. There were no significant differences in segmental lordosis between 1 and 2 screws for no osteotomy, G1, or G2 osteotomies (P > .148). There was no difference in posterior compressive force required when using 1 or 2 anterior screws (P > .650); however, significantly less compressive force was required with G2 osteotomy compared with G1 osteotomy (143 vs 183 N, P = .013) and no osteotomy (143 vs 173 N, P = .048) regardless of 1 or 2 screws. Conclusion: Maximal segmental lordosis can be achieved with ACR whether fixating into one or both VBs when grade 2 osteotomies are performed.
P052: Evaluation of the Efficacy of Supraspinous/Interspinous Ligament Repair in Segment Translation Stabilization After Interlaminar Device Application for Patients Who Underwent Lumbar Decompression
Mannuel Feliciano Alican1 and Mario Ver1
1St. Luke’s Medical Center, Quezon City, Philippines
Introduction: In recent years, there have been growing evidence that decompression with application of interlaminar device (ILD; Coflex) has been performing if not better, then as satisfactory when being compared against decompression alone or posterior lumbar fusion surgery. The Coflex (Paradigm Spine, GmbH, Wurmlingen, Germany) is a single, compressible, metal, U-shaped interlaminar-interspinous device is currently being indicated for use in patient with 1 to 2 level of moderate to severe lumbar stenosis or low-grade stable spondylolisthesis from L1-L5 for adjunct decompression with load bearing and motion preservation capacity. Despite the advantages it offers, one limitation in Coflex “biomechanical property is the lack of stabilization it offers on flexion, unless bony ingrowth of spinous process to Coflex wing occurs.” Supraspinous ligament and interspinous ligament (SSL/ISL) offers stability on flexion motion on each lumbar segment where it attached. However, inherent in the technique of application of Coflex would be disruption of the ISL/SSL ligamentous complex. The study aims to assess in vitro effect of repair of ISL/SSL ligamentous complex post decompression with application of ILD in translation of lumbar segment especially in flexion motion. Material and Methods: Our group conducted a retrospective cohort, multicenter study on patients with lumbar stenosis with or without low-grade spondylolisthesis who underwent D + ILS done by single experienced spine surgeon. Patients younger than 80 years who were indicated for 1- to 2-level D + ILS procedure for lumbar stenosis with or without low-grade spondylolisthesis from June 2016 to May 2018 were included. Cohorts were classified as to those who had repair of the ISL/SSL complex and those who did not. The ISL/SSL repair cohort underwent Chevron osteotomy on the mid-spinous process of the rostral vertebra, which was done after application of Coflex. They were evaluated for lumbar segment translation after the procedure via standing lumbosacral spine AP and lateral with flexion and extension radiographs were taken preoperatively, 2 weeks, and 8 weeks post operation. Total motion of segment and motion on flexion were measured, compared, and statistically analyzed. Results: Our group was able to gather 13 patients who underwent D + ILS with repair and 20 patients who underwent who underwent D + ILS alone during the duration included in the study. There was noted decreased overall motion on both groups, with 0.95 mm and 0.55 mm on cohort with ISL/SSL repair and without, respectively. There was better reduction in overall motion observed in the repair group by 0.04 mm, but it was not statistically significant (P = .08). On both flexion motion whether with or without noting direction of motion, there was no statistically significant difference between the translation noted preoperatively and 2 weeks post operation. However, when degree of reduction of translation were compared for both with ISL/SSL repair and without group, reduction of translation noted on the ISL/SSL repair was significantly improved (P = 0). Conclusion: Despite the added effort on doing the repair intraoperatively in repairing the ISL/SSL complex post application of Coflex, further stabilization on flexion motion of the operated segment can be achieved by doing so.
P053: Evaluation of Pedicle Screw Fixation in Simulated Osteoporotic Bone
Trevor Gascoyne1, Jonathan Tan2, and Michael Goytan2
1Orthopaedic Innovation Centre, Winnipeg, Manitoba, Canada
2University of Manitoba, Winnipeg, Manitoba, Canada
Introduction: Thoracic and lumbar back pain is a highly prevalent issue in North America affecting approximately 80% of the population. To remedy, surgical intervention can include immobilization of the affected junctions of the spine through fusion of the neighboring vertebral bodies. A reasonable proportion of fusion procedures are unsuccessful for a variety of reasons. A common cause of failure is screw loosening, often as a result of reduced screw purchase in weakened, poor quality bone. The goal of this study was to quantify the effect of bone density and different screw designs on resistance to screw pullout and cantilevered fatigue loading. Materials and Methods: Three pedicle screw types were obtained for this study: (1) aggressive tapered screw with thread transition from v-type to buttress-type, (2) mild-tapered screw with moderate thread transition, and (3) non-tapered constant thread. A layered bone model was developed to mimic the path traversed by a lumbar pedicle screw, consisting of a 20 mm layer representing the pedicle channel laminated to a 30 mm layer representing the vertebral body. Four bone types were developed based on this model by selecting foams with similar mechanical properties to normal bone (40 pcf|15 pcf), mild osteoporotic (OP) bone (35 pcf|10 pcf), moderate OP bone (30 pcf|5 pcf), and severe OP bone (20 pcf|5.5 pcf open cell). Two screw pullout tests were performed per pedicle screw, per bone type, with a minimum of 5 replicates. First, an axial screw pullout test was performed per ASTM standard F543-13. Second, the pedicle screw was subjected to 100 cycles of cantilevered loading by applying tension/compression to the screw head perpendicular to the screw axis, in order to create a loosened pedicle channel. An axial pullout test was then performed on the loosened pedicle screw. Mean pullout force was compared between bone types for each pedicle screw design. Cantilever force and perpendicular displacement of the screw head during cyclic loading was also compared. Results: As bone density decreased, there was a proportionate decrease in peak pullout force; mild OP 82% to 86% of normal, moderate OP 49% to 56% of normal, and severe OP 17% to 28% of normal. Similarly, there were progressively larger decreases in pullout strength after fatigue loading with decreasing bone density; normal bone 87% to 110%, mild OP 92% to 97%, moderate OP 55% to 95%, and severe OP 30% to 80% of standard axial pullout force. Furthermore, reduced bone density allowed for larger increases in toggling distance of the pedicle screws during cyclic loading; normal bone 0.34 to 0.39 mm, mild OP 0.33 to 1.62 mm, moderate OP 0.59 to3.7 mm, and severe OP 0.82 to 5.9 mm increase from cycle 1 to cycle 100. Conclusions: Reduced bone density can greatly reduce the strength of pedicle screw fixation in lumbar fusion by as much as 85%. Axial screw pullout should not be the sole consideration when evaluating screw types in osteoporotic bone as spinal forces are multidirectional and can adversely affect screw fixation. OP bone requires special screw design and screw placement considerations in order to optimize fixation in these higher risk patients.
P054: Sagittal Vertical Axis and Spinopelvic Parameters in Chronic Low Back Pain Patients
Sai Krishna M. L. V1, Deep Sharma1, and Jagdish Menon1
1Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry, India
Introduction: With the discovery of sagittal spinopelvic parameters and their association with various spine disorders, the concept of sagittal balance has become very important. Alteration in sagittal profile has been documented to be associated with various spine disorders from degenerative diseases to deformity. Overall sagittal profile can be assessed with the help of sagittal vertical axis (SVA). SVA is defined as plumb line dropped from C7 vertebra on a lateral sagittal spine radiograph taken in standardized way and its horizontal distance measured from anterior superior corner of sacrum. Based on previous studies, the horizontal distance ranges from −4.5 to +14.9 cm. HRQOL (health-related quality of life) has highest correlation with T1 tilt, SVA, and pelvic tilt. SVA within 5 cm has been associated with better quality of life. We started our study to know the relation between SVA and spinopelvic parameters in chronic low back pain patients. Material and Methods: The study was approved by our institute review board and the ethical committee. A total of 67 patients with chronic low back pain were enrolled into the study after taking a formal consent. Lateral sagittal digital radiographs of the whole spine. The parameters measured were pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), thoracic kyphosis (TK), lumbar lordosis (LL), and SVA. All measurements were performed using the Surgimap spine software version 2.1.2. Subjects are divided into 2 groups based on SVA (≤5 cm and >5 cm.). Comparisons are drawn between the groups. Results: The mean values in the first group (SVA ≤5 cm.) are PI 48.62, PT 14.22, SS 34.59, LL 51.08, and TK 27.95. The mean values in the second group (SVA >5 cm) are PI 47.33, PT 10.63, SS 36.70, LL 49.93, and TK 25.37. Conclusion: Subjects with SVA >5 cm have higher sacral slope and lower pelvic incidence and lower pelvic tilt, but the difference was not significant.
P055: Spinopelvic Parameters on a Latin American Population
Thiago Maia1, Charbel Junior1, Igor Cardoso1, and Jose Lucas Junior1
1Santa Casa de Vitoria, Vitoria, Brazil
Introduction: Several authors have underlined the importance of the sagittal imbalance as an independent factor for pain and disability. Additionally, balance restoration after surgery becomes a substantial factor for improvement in several scores (ODI [Oswestry Disability Index], VAS [visual analogue scale], SF-36 [36-item Short-Form Health Survey], SRS-22r [Scoliosis Research Society-22r]). It is well known that there are anthropomorphic differences between human beings that inhabit different regions or continents. This may be consequence from interactions between the genotype and the environment where each individual develops. At present, we do not have databases of the Latin American population to make decisions based on local parameters. Based on previous studies published by the authors, we decided to add Argentinian and Brazilian data to approximate a Latin American profile of spinopelvic parameters. Materials and Methods: A systematic review of the literature was performed to obtain data about spinopelvic parameters on asymptomatic population from Argentina and Brazil. They were compared to evaluate similarities and differences. A comparison for pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS) was made. Results: The parameters value for the Argentinian population was: PI 48.04 (±11.71), PT 11.22 (±6.79), and SS 36.96 (±8.44). The Brazilian population parameters were PI 49.36 (±5.42), PT 11.87 (±4.72), and SS 38.15 (±1.85). Only the PT showed to be statistically different between populations. Conclusion: Spinopelvic parameters from Argentinian and Brazilian populations showed a similar profile. More studies are needed to determine if they are representative of the Latin American population.
Cell Therapy
P056: A Scoping Review of Trials for Cell-Based Therapies in Human Spinal Cord Injury
Alice Willison1, Sam Smith1, Benjamin Davies1, and Mark Kotter1
1University of Dundee, Dundee, UK
Introduction: Spinal cord injury (SCI) is associated with significant and life-long disability. Yet, despite decades of research, no regenerative treatment has reached clinical practice. Cell-based therapies are one possible regenerative strategy beginning to transfer to human trials from a more extensive preclinical basis. We, therefore, conducted a scoping review to synthesize all cell-based trials in human spinal cord injury, to consider the current state of the field, and the cell transplant type or strategy with greatest promise. Material and Methods: A search strategy of MEDLINE returned 1513 results. Results underwent title and abstract screening, before full-text screening. Data were then extracted from 43 eligible studies. All clinical trials including adult human patients with acute or chronic, compete or incomplete SCI were analyzed. Exclusion criteria included nontraumatic SCI, pediatric patients, and animal studies. Results: A total of 1068 patients were treated using cell transplantation therapy. Most frequently, cells were taken from the bone marrow (22 articles, 660 patients) or the olfactory bulb (10 articles, 245 patients). Lumbar puncture was the preferred transplantation methodology (14 articles, 511 patients). The studies are generally qualitative, observational, uncontrolled, nonrandomized, and of small sample size, using heterogeneous clinical and cellular populations. In addition, despite most using the ASIA (American Spinal Injury Association) scale, varying degrees of outcome reporting limited pooled outcome analysis. Translation of stem cell therapies remains in its infancy: 63% of trials were phase 1 or less. Of note, 86% of trials described efficacy as a primary outcome despite their low quality. Cell transplantation does appear to be safe, with no serious adverse effects being reported in the short term. Only one study exclusively included patients with acute incomplete injury, with 83% of trials performed on chronic complete SCI patients. Five studies included an adjuvant treatment. Six trials implemented multiple dosing regimens. We have not identified an emerging cell type or technique. Interestingly, the vast majority of the clinical trials took place in developing countries, which perhaps suggests more stringent regulatory requirements within Western countries. Conclusion: Cell-based transplantation translation remains in its infancy, and a number of questions remain unanswered: While short-term safety is apparent, what is the long-term safety? How should stem cells be delivered? But, most important, are they effective? Further robust clinical research is required.
P057: Cell Therapy for Treatment of Intervertebral Disc Degeneration: A Systematic Review
Hans-Joerg Meisel1, Neha Agarwal1, Andrea Skelly2, Patrick Hsieh3, Jong-Beom Park4, Jim Youssef5, Darrel Brodke6, Jeffrey Wang3, S. Tim Yoon7, and Zorica Buser3
1Bergmannstrost Hospital, Halle, Germany
2 Aggregate Analytics, Inc, Fircrest, WA, USA
3University of Southern California, Los Angeles, CA, USA
4Uijongbu St. Mary’s Hospital, The Catholic University of Korea, Uijongbu, Republic of Korea
5Spine Colorado, Durango, CO, USA
6University of Utah, Salt Lake City, UT, USA
7Emory Spine Center, Atlanta, GA, USA
Introduction: Symptomatic degenerative disc disease (DDD) is often treated with conservative therapies, minimally invasive interventions, or surgical procedures that cannot restore intervertebral disc (IVD) function or provide long-term relief. Mesenchymal stem cells (MSCs) are progenitor cells of multiple lineages with immunomodulatory capabilities, which can be beneficial for cell-based therapies. Potential of MSCs or IVD autologous cells for disc repair is being assessed by a number of ongoing clinical trials. Nevertheless, clinical evidence is lacking. The aim of the current study was to systematically review the literature for effectiveness and safety of cell-based therapies for IVD repair. Material and Methods: A systematic search of PubMed/MEDLINE, EMBASE, and ClinicalTrials.gov databases were conducted for literature published through April 2018 comparing allogenic or autologous cell therapy for intervertebral disc repair in the lumbar or cervical spine. In the absence of comparative studies, case series of ≥10 patients were considered. Primary outcome analysis included the ODI (Oswestry Disability Index), VAS (visual analogue scale) pain, SF-36 MCS (Mental Component Score), or PCS (Physical component Score), and secondary outcomes looked at disc height, HRQoL (health-related quality of life), or symptomatic adjacent segment pathology. Unpaired t tests were used to calculate mean differences and corresponding confidence intervals. Risk ratios were calculated for dichotomous outcomes from randomized clinical trials (RCTs) if differences between groups were or approached statistical significance. Results: From 1059 studies, 8 citations on IVD cell therapies in the lumbar spine met the inclusion criteria. Studies included 1 (RCT, 1 pilot study of an RCT, 5 case series, and 1 single-arm registry study. No studies for cervical IVD repair or cost analysis were identified. The RCT using allogenic MSCs showed no difference for either primary or secondary outcomes. However, the case study showed improvement in primary outcomes—ODI, SF-36, PCS, and VAS scores—as well as in secondary outcomes—disc height. Among 5 small case studies using autologous MSCs, 3 showed improved primary outcomes measured by ODI scores compared with the baseline. VAS scores also improved across most studies. Another study using hematopoietic cells from bone marrow aspirate (BMA) reported no significant changes in VAS pain scores across different time frames compared with the baseline, and one study showed no pain reduction in any of the patients. In most of the studies, no major adverse events or treatment-related adverse events were reported. The need for subsequent surgery was reported in 3 case series studies ranging from 6% to 80%. Conclusion: The overall strength of evidence for efficacy and safety of allogenic and autologous cell therapy use for lumbar IVD repair was very low. Furthermore, studies lacked tools to assess treatment heterogeneity depending on patient characteristics, co-intervention, or other factors. While no serious adverse events were generally reported across studies, sample sizes were likely inadequate to detect adverse events, particularly those considered to be rare. To evaluate efficacy and safety of IVD repair using cell therapies, high-quality comparative studies are needed.
Deformity-Cervical
P058: Cervical Deformity in Adolescent Idiopathic Scoliosis Patients: Is It Clinically Significant?
Isador Lieberman1 and Xiaobang Hu1
1Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: It has been reported that there is a significant correlation between the loss of thoracic kyphosis and the development of cervical kyphosis in adolescent idiopathic scoliosis (AIS) patients. However, the clinical significance of cervical deformity in AIS patients is not clear. The purpose of our study is to evaluate the relationship between cervical deformity and neck pain in AIS patients. Material and Methods: We retrospectively analyzed a consecutive series of AIS patients from a single center. Radiographic measurements included Cobb angle, C2-C7SVA, and C2-C7 lordosis. Cervical deformity was defined as loss of lordotic or neutral cervical angle (CK) or C2-C7SVA more than 4 cm (CPSM). Patients were stratified by the presence of CK and/or CPSM. The visual analogue scale (VAS) was used to assess the patients’ neck pain. The patients’ demographics were also recorded. Results: A total of 99 patients were included in this study. The patients’ mean age was 14 years (range = 10-18). Mean cervical lordosis and C2-C7SVA were 1.5 mm and 30.4 mm, respectively. CK and CPSM prevalence were 49% and 16%, respectively, and the prevalence of CK and/or CPSM was 59%. Twenty-six percent of the patients had neck pain, and their median pain scores were 2.3 points (range = 0.5-8.2 points). There is no correlation between CK and neck pain (26.7% vs 25.6%, P > .05), between CPSM and neck pain (42.9% vs 23.0%, P > .05), and between CK and/or CPSM and neck pain (28.8% vs 22.2%, P > .05). Conclusion: In this series, cervical deformity is present in 59% and neck pain is present in 26% of AIS patients. However, there is no correlation between cervical deformity and neck pain. Our data suggest that the loss of cervical lordosis is a compensatory maneuver in AIS patients, and it may not be clinically significant.
P059: Cervical-Thoracic Pediatric Spine Reconstruction: Etiological Structure, Clinical Signs, and Results of Surgery in Non-Trauma Pathology (10-Year 3-Center Study)
Aleksandr Mushkin1, Mikhail Schelkunov1, Sergei Ryabykh2, Egor Filatov2, Sergei Kolesov3, Alexander Kuleshov1, and Marchel Vetrile1
1St. Petersburg Research Institute of Phthisiopulmonology, St Petersburg, Russian Federation
2 Russian Scientific Ilizarov Center, Kurgan, Russian Federation
3National Medical Investigational Center of Traumatology and Orthopaedics named by N.N. Priorov, Moscow, Russian Federation
Introduction: The cervical/thoracic (C/Th) spine reconstruction in pediatric patients is rare excluded spinal trauma. The aim of the study is to establish the indications, manifested signs, principles, and results of surgery in pediatric patients with non-trauma C/Th spine pathology. Design: Multicenter retrospective study. Material and Methods: Criteria for inclusion: C7 and Th1 vertebrae are included into spinal reconstruction together. Forty-nine patients aged from 1 till 15 years underwent 51 operations on C7/Th1 zone in 3 clinics during 10 years (2008-2017). The analyzed factors: etiology, clinical signs, surgical peculiarities, and results. The average follow-up period was 3 years 9 months in average (minimum 9 months, maximum 10 years). Results: The main indications for surgery were: severe deformities (39/51 or 76.4%), chronic pain (23/51 or 45.1%), and neurological signs (11/51 or 21.6%). Congenital abnormalities were diagnosed in 24 patients (16 scoliosis and 8 kyphosis including 6 inclinations), TB (tuberculous) spondylitis in 15. Other pathologies included spinal tumors (4) and their aftereffects (3), neurofibromatosis type I (NF1; 1), purulent osteomyelitis (1), and spontaneous bone resorption (1). One-stage and multistage surgeries were in 40% and 60% (correspondingly). Posterior only approach used in 31, combined in 19, and anterior only in 1. In the preoperative period, Halo-cat was effectively applied for severe spinal instability in 8 patients. The deformity decreased or completely corrected in all cases only due to posterior instrumentation (PI; PI removed 3/5 years after surgery in 8 cases). The neurological improvement reached in 10/11 patients. Three patients had complications: increased paraplegia in 1 (NF1) and transient paresis in 2 (TB spondylitis). Despite improvement at early postoperative period, 2 patients died during 2 years after surgery due to Ewing sarcoma progression. Maximal local bayonet kyphosis (87°) was in C/Th inclination. Two reoperation done 8 years after initial surgery: the indications for reoperations were TB spondylitis progression (1) and late bone transplant resorption (1). Conclusion: The indications for C/Th surgery based on combinations and etiology and prevalent clinical symptoms. Halo-cast fixation could be effective as preoperative and intraoperative option in severe instability. The complications of surgery are rare. The posterior approach and PI had advantages for spinal reconstruction and deformity correction, but other approaches could be useful in concrete situation.
P060: C1-C2 Pedicle Screw Fixation for Atlantoaxial Dislocation in Pediatric Patients Younger Than 12 Years: A Case Series of 36 Patients
Yuehui Zhang1, Jia Song1, Jing Zhang1, and Jiang Shao1
1Xin Hua Hospital Affiliated to Shanghai Jiao Tong University, Shanghai, China
Introduction: Traditional surgical wiring techniques for posterior atlantoaxial fixation are associated with high complication and low bone fusion rates. Transarticular screw fixation has been widely used in adults, but it is associated with risk of vertebral injury in children because of the smaller bony anatomy. C1-C2 pedicle screw fixation has become popular for providing excellent bony purchase and successfully avoiding neurovascular complications. However, this procedure may be technically challenging in children. The objective of this study is to investigate the safety and efficacy of C1-C2 pedicle screw fixation for atlantoaxial dislocation (AAD) in pediatric patients younger than 12 years, and to evaluate the preliminary clinical and radiographic results. Methods: During a 10-year period, 36 patients with a mean age of 6.9 years (range = 2-12 years) underwent C1-C2 pedicle screw fixation for AAD; at least 1 C1 pedicle screw was incorporated as part of the posterior atlantoaxial fusion construct. The etiology, surgical technique, instrumentation, and clinical and radiographic results were analyzed. Results: Diagnoses included os odontoideum in 12 patients, prior odontoid fracture in 6, dens aplasia/hypoplasia in 4, acute odontoid fracture in 5, atlantoaxial rotatory fixed dislocation in 7, and transverse ligament laxity in 2. Nineteen patients had preoperative neurologic deficits. Anterior release using a retropharyngeal approach was performed in 8 cases. Fixation of 135 C1 and C2 pedicle screws was performed successfully without neurovascular complications. Anatomical and partial reductions occurred in 28 and 8 cases, respectively. Solid fusion was achieved in 34 patients (94.4%) during a mean follow-up of 36.5 months (range = 12-111 months). Two patients (5.6%) experienced complications: one had prolonged immobilization for a loose C1 pedicle screw, and 1 had unintended fusion due to allograft absorption. All patients showed radiographic stability and symptom resolution. Conclusion: C1-C2 pedicle screw fixation for AAD is safe and effective even in children younger than 12 years. Further studies with more cases are required to evaluate long-term efficacy and safety.
P061: A New Strategy of Staged Thoracolumbar and Cervical Osteotomies for Correcting Severe Kyphotic Deformity Caused by Ankylosing Spondylitis
Guoquan Zheng1, Yan Wang1, Xuesong Zhang1, Zheng Wang1, Tianhao Wang1, and Diyu Song1
1Chinese Peoples’ Liberation Army General Hospital, Beijing, China
Introduction: Ankylosing spondylitis (AS) causes characteristic spinal deformity leading to impaired ability of walking, standing, and looking straight ahead in the late stages. There are 2 main goals of osteotomy to correct kyphotic deformity in AS: one is restoration of sagittal balance, and another is restoration of forward gaze. When thoracolumbar kyphosis (TLK) combined with cervical ankylosis, these 2 main goals are not able to be achieved at the same time. Usually, a smaller angle is considered to be the ideal one for osteotomy to keep horizontal gaze, which sacrifices the correction of sagittal imbalance to some extent. This study puts forward a new osteotomy strategy for AS thoracolumbar kyphotic deformity combined with fused cervical spine. Material and Methods: A 36-year-old man had severe TLK accompanied with fused cervical spine caused by ankylosing spondylitis. The preoperative thoracic kyphosis (TK), TLK, lumbar lordosis (LL), and sagittal vertical axis (SVA) were 93.8 mm, 30.8 mm, 10.3 mm, and 259 mm, respectively. Although having severe thoracolumbar kyphotic deformity and unmovable neck, the patient was still able to look horizontally with chin-brow vertical angle (CBVA) of 21°. Because of the fused cervical spine, a traditional 1-stage thoracolumbar osteotomy was not able to achieve an ideal correction result. Therefore, a 2-staged surgery planning was managed. For the first stage, an interrupt 2-level osteotomy was performed at thoracolumbar area to reconstruct sagittal balance without concern for CBVA. Cervical osteotomy was performed for the second stage to make the patient having horizontal visual field. A flexion osteotomy was performed at C7, using anterior-posterior-anterior approaches. Results: After the first-stage surgery, TK, TLK, LL, and SVA reduced to 65.0, 17.3, −43.6 and 131.2 mm, respectively. The sagittal imbalance was corrected but the CBVA came to −22°. After the second-stage cervical osteotomy with correction of 32.6°, CBVA came to 2.9°. Both sagittal imbalance and gaze angle of the patient were improved markedly. Three months after surgical treatment, the osteotomy sites were documented fused. Complications were not observed during and after operation. Conclusion: The aim of osteotomy for AS deformity is to reestablish sagittal balance and improve forward gaze and the visual field. When treating TLK combining with cervical ankylosis, a thoracolumbar osteotomy is allowed to be performed without consideration of CBVA. A staged cervical osteotomy is an alternative to reduce cervical lordosis to obtain normal gaze angle. Anterior-posterior-anterior approach is recommended for cervical osteotomy.
P062: Combined Laminoplasty With Unilateral Lateral Mass Screw Fixation in Acute Cervical Cord Injury Preexisting Ossification of the Posterior Longitudinal Ligament
Sang Gu Lee1
1Gachon University Gil Medical Center, Incheon, Republic of Korea
Introduction: Multilevel laminoplasty may be very vulnerable state for cervical stability in OPLL (ossification of the posterior longitudinal ligament) with acute cord injury. To explore and analyze the outcomes and factors that affect the prognosis of open-door laminoplasty with unilateral lateral mass screw fusion in acute cervical cord injury preexisting cervical ossification posterior longitudinal ligament (C-OPLL). Material and Methods: From January 2011 to December 2016, combined surgery was performed for acute cervical cord injury preexisting C-OPLL in single spine center. The subjects of this study were 14 men and 3 women of mean age 65 ± 11 years (range = 51-81) with a mean follow-up of 22.8 months. All MR (magnetic resonance) imaging studies showed multiple C-OPLL with spinal cord signal change. A retrospective review of clinical outcomes, radiological changes, and surgical data were conducted. Results: The cause was slip down on 8 cases, traffic accident 1, but unknown was 8. Average laminoplasty level was 3.9, and the average screw fixation level was 4.0. Including C2 fusion case were 10, and C7 fusion level were 6. Modified Japanese Orthopedic Association score improved from an average of 7.3 ± 3.6 to 10.9 ± 4.0 points. According to Nurick’s grades, symptom improvement was 3.7 ± 1.0 to 2.4 ± 1.5 statistically significant. The overall of changing in C2-7 SVA (sagittal vertical axis) was 26.1 mm to 31.9 mm. The average of preoperative cervical curvature was 10.3 ± 9.5° and postoperative cervical curvature was 10.6 ± 6.9° and last follow-up was 7.5 ± 7.0°. No significant surgical complication was encountered without 3 screw halo evidences. In C2 fixation, the change of cervical curvature angle was 8.6 ± 4.6° to 7.7 ± 3.9° but in skipped C2 fixation, 13.6 ± 8.8° to 7.2 ± 9.9°. Conclusion: Despite the small cohort and the short follow-up duration, combined open-door laminoplasty and unilateral lateral mass screw fixation can help maintain cervical curvature and stability without obvious complication in multilevel cervical OPLL with acute cord injury. Including C2 fixation was superior to keep the C2-7 lordotic angle during the follow-up period in multilevel C-OPLL.
P063: The Use of Zero-Profile Cage Plate for the Management of Cervical Disc Disease
Abdulrazzaq Alobaid1, Abdulaziz Al-Mutair2, Islam Elsayed2, and Tamer Ramadan1
1Wara Hospital, Kuwait City, Kuwait
2Alrazi Hospital, Kuwait City, Kuwait
Introduction: Several studies reported fusion rates are higher with anterior cervical decompression and fusion (ACDF) procedure if supplemented with a plate. However, plates may be associated with postoperative morbidity and higher rates of dysphagia. Zero-P implant for stand-alone cage plate used in ACDF was developed to avoid complications associated with anterior cervical plates owing to the zero profile of the construct. Aim: The aim of this study to evaluate the functional as well as radiological outcome of Zero-P cage plate for the management of cervical disc disease. Materials and Methods: Thirty patients (16 males and 14 females) were selected to undergo ACDF with Zero-P implant, the mean age was 47.93 (±10.9) years, a total of 43 operated levels (20 patients 1 level operated, 7 patients 2 levels operated, and 3 patients 3 levels operated), and the mean follow-up was 12.3 months. These patients underwent pre- and postoperative clinical and neurological evaluation and scoring systems using visual analogue scale (VAS) for neck and radicular pain, Neck Disability Index (NDI) and Bazaz-Yoo dysphagia index for postoperative dysphagia. Postoperative X-ray evaluation was done for evaluation of fusion- and implant-associated complications at 1,3,6,9, and 12 months. Results: All patients had significant reduction in arm and neck pain, and NDI maintained over the follow-up period, P value was (<.0001) with reduction of VAS for neck pain from 7.33 preoperatively to 1.37 at 12-month follow-up and also VAS for radicular pain from 8.70 preoperatively to 0.27 at 12-month follow-up, and reduction of NDI from 68.87% preoperatively to 8.60% at 12-month follow-up. None had dysphagia after 6 months postoperatively, 1 patient developed back out of one of the implant screws that was extracted, and otherwise no other implant-related complications. Conclusion: The Zero-P implant is a valid alternative to anterior cervical plating after ACDF with a very low incidence of chronic dysphagia and implant-related complications.
P064: Intraoperative Image-Guided Transoral Odontoidectomy After Posterior Reduction and Fixation in Basilar Invagination and/or Atlantoaxial Dislocation
Fengzeng Jian1, Longbing Ma1, Zan Chen1, Hao Wu1, Xingwen Wang1, Wanru Duan1, Kai Wang1, Zhenlei Liu1, Qingyu Yao1, and Can Zhang1
1Xuanwu Hospital, Capital Medical University, Beijing, China
Introduction: For patients with irreducible atlantoaxial dislocation (AAD) complicated by compression of the ventral spinal cord, odontoidectomy was used to be one of the treatment options. With the improvement of posterior reduction and correction techniques, the need of odontoid resection is decreasing. This study reports a series of cases of basilar invagination (BI) with AAD treated by transoral odontoidectomy after posterior reduction and fixation under neuronavigation aiming to illustrate the indications, techniques, and outcomes of this operation. Material and Methods: We reported 10 patients with BI or AAD who have previously accepted posterior reduction and fixation, including 3 males and 6 females, from December 2011 to June 2018 (mean age 39.9, range from 13 to 66). Preoperative computed tomography (CT) reconstruction and magnetic resonance imaging (MRI) were used to assess the severity and type of deformity and the degree of spinal cord compression, as well as the symptoms and previous surgical history. During the operation, CT images were obtained in advance and matched and registered with the neuronavigation system. All patients received microscopic or under the endoscopic transoral odontoidectomy under the navigation. After operation, the changes of spinal nerve function were evaluated by clinical symptoms and imaging results. Results: In this series, mean follow-up time was 47.9 months, ranging from 6 to 81 months. No deterioration after surgery. Eight patients were diagnosed BI with AAD, 1 AAD with syringomyelia, and 1 os odontoidem with AAD. All 10 patients had received posterior decompression of the occipital foramen with or without internal fixation and fusion. One had received anterior transoral reduction and posterior decompression. Three patients received endoscopic transoral odontoidectomy, and 7 patients microscopic. One death (7 days after surgery, during sleeping, unknown reason). Incomplete decompression in 4 cases, and reoperation in 3 cases. The mean JOA (Japanese Orthopaedic Association) score improved from 8.5 to 12.3 postoperatively. The mean cervicomedullary angle improve from 105° to 113°. Conclusion: Transoral odontoidectomy as salvage surgery is indicated in some selected patients of BI and/or AAD after posterior reduction and fixation. Transoral odontoidectomy is safe and effective in indicated patients in which posterior reduction was not satisfactory, and MRI showed that there was still compression with no improvement in clinical symptoms. Patients with CVJ (craniovertebral junction) bone fusion can also benefit from the operation. Intraoperative image-guided navigation is feasible and can provide accurate location of lesions during operation, thus allowing more complete resection of odontoid process and avoiding serious complications, especially for irregular odontoid process, which is common in basilar invagination and/or AAD.
P065: Outcomes of Surgical Correction of Atlantoaxial Instability in Patients With Down Syndrome: A Systemic Review and Meta-Analysis
Ryan Hofler1, Nathan Pecoraro2, and G. Alexander Jones1
1Loyola University Medical Center, Maywood, IL, USA
2Loyola University Chicago, Chicago, IL, USA
Introduction: Atlanto-axial instability (AAI) is a common cause of neurologic dysfunction and pain in patients with Down syndrome (DS), frequently requiring stabilization of the upper cervical spine. Despite this, optimal treatment strategy is controversial. Methods and Materials: A systematic review of the literature was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement to identify patients with AAI and DS that were treated with fusion of the upper cervical spine. Patient demographics, preoperative symptoms, fixation type, and outcome measures including complications, neurologic outcomes, and bony fusion status were gathered for the patients in the included publications. Meta-analysis was performed to compare outcomes of different types of fixation constructs. Results: Of the 1191 publications retrieved, 51 met inclusion criteria, yielding 137 patients. Six fixation strategies were identified: wiring (n = 77), wiring with rods (n = 14), screw fixation (n = 33), noninstrumented (n = 6), hook and rod fixation (n = 2), and screw and wire fixation (n = 5). The latter 3 groups were excluded from statistical analysis due to small sample size. Among the first 3 groups, constructs with screws and rods had greater bony union (P = .003) and lower rate of revision surgery (P = .047), loss of reduction or pseudoarthrosis (P = .009), halo utilization (P < .001), and early neurologic decline (P = .004), compared with wiring alone. Constructs with wires and rods had greater bony union (P = .036) than wiring alone. Conclusion: Numerous fixation strategies exist for AAI in patients with DS. Utilizing a combination of screws, rods, and wiring in appropriately selected patients may help reduce the high rate of surgical complications in these patients.
P066: Vertebral Artery Variant in Patients With Congenital Cervical Scoliosis
Tian Xia1
1Peking University Third Hospital, Beijing, China
Introduction: Congenital cervical scoliosis is a rare disease in children or young adults. Vertebral artery (VA) injury might be one of the most concerning and life-threatening intraoperative complications during osteotomy or other procedures. Evaluation of bilateral vertebral arteries might be one of the most important preparation for planning. To our knowledge, no observation of VA variants in patients with congenital cervical scoliosis was reported. Methods: Patients with congenital cervical scoliosis treated in the Peking University Third Hospital was reviewed. We collected clinical data such as age, gender, and diagnosis. We measured Cobb angle from computed tomography (CT) scan of cervical spine, and we observed bilateral VA, all VA variant was recorded, we measured their diameter in each segment through CT angiograph of head and neck. The bilateral diameter of VA in each patient was compared, respectively, and we explored the relation between VA variant and severity of cervical spinal deformity. Result: There were 38 patients with congenital cervical scoliosis treated in our department. All of whom received cervical spinal CT scan and CT angiography of head and neck. Thirty-two out of 38 patients had variants in their vertebral arteries, 7 patients with bilateral variants and 25 patients with unilateral variants. The comparison and analyzability of the diameter vertebral arteries on both sides. Twenty-four patients (63.2%) had 1 vertebral significantly thinner (P < .05) than the one on the opposite side. The side with the thinner VA is not related to neither concave side nor convex side of the cervical spine. Patients with asymmetry vertebral arteries had larger Cobb angle than other patients (P < .05). Another common variant was the courses of the vertebral arteries. Eleven patients, with variant in the entry, C5, C4, and C7 was the most common segments in which the VAy entered the transverse foramen. Seven patients with variant of the segments in which vertebral artery enter the cranium. In 6 patients, vertebral arteries entered the cranial cavity between atlas and odontoid vertebra. In 1 patient, his right VA runs directly in to cranium from base of the skull. One patient’s left VA did not enter the transverse foramen at all. In 1 patient, her left VA arising from right subclavian artery. In another patient, his left VA arise directly from the aorta arch. Variant of common carotid artery and internal carotid artery were also observed in these patients. Conclusion: VA variant in patients with congenital cervical scoliosis was very common. The most common variant was asymmetrical thinness of VA, and abnormal courses were obviously more often seen in these patients than in normal people. Evaluation of the VA was important before operation, in order to avoid iatrogenic VA injury.
P067: Therapeutic Strategy for Cervical Kyphosis With Type I Neurofibromatosis
Yawei Li1, Guohua Lv1, and Bing Wang1
1The Second Xiangya Hospital of Central South University, Changsha, China
Introduction: Severe cervical kyphosis requiring surgical treatment is rare in patients with neurofibromatosis type 1 (NF1). Although surgery is a common treatment to correct the deformity, there are no universally accepted treatment guidelines. The aim of this study was to discuss the therapeutic strategy for cervical kyphosis with NF1. Materials and Methods: From February 2002 to February 2016, 21 patients of cervical kyphosis with NF1, including 15 males and 6 females, were surgically treated in our institution. The age ranged from 12 to 42 years, and the mean age was19.7 years. According to cervical kyphotic flexibility and Cobb angle, 6 cases (flexibility ≥30% and Cobb angle <50°) underwent anterior or posterior correction and fusion alone; 8 cases (flexibility ≥30% and Cobb angle 50-90°) underwent combined anterior and posterior correction and fusion; 7 cases (flexibility <30% or Cobb angle >90°) underwent anterior and posterior correction, and fusion followed skull traction. Results: The average follow-up was 58.6 months (18-78 months), the average kyphotic Cobb angle was 74.3° (40-128°) and 32.6° (15-53°) (P < .01) before and after the surgical correction, respectively. The final correction rate was 56.1% (40.2% to 65.4%). There were 3 cases of transient C5 root palsy, 5 cases of esophageal foreign body sensation, and 2 cases of fixation failure (posterior correction and fusion alone). Conclusions: The surgical treatment of severe cervical kyphosis in NF1 is complicated by dystrophic changes in the cervical vertebrae that make rigid fixation and sufficient bone fusion challenging. The appropriate strategy of surgical selection could effectively correct the patients’ kyphosis deformity and improve the symptom.
Deformity-Thoracolumbar (Adolescent)
P068: Comparison of Surgical Treatment Outcomes of Scoliosis Associated With Intraspinal Abnormalities Without Neurologic Symptoms and Adolescent Idiopathic Scoliosis
Jingwei Liu1 and Yong Hai1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: Adolescent idiopathic scoliosis (AIS) is a common type of idiopathic scoliosis. Previous studies reported that the incidence of intraspinal abnormalities among the presumed idiopathic scoliosis was 13% to 43%. Intraspinal abnormalities were also considered increasing the risks of progressing of scoliosis and neurological complications following scoliosis corrective surgery. The surgical strategy of scoliosis with intraspinal abnormalities remains controversial. The purpose of this study was to investigate whether surgical guidelines of AIS appropriate for the presumed AIS patients associated with intraspinal abnormalities without neurologic symptoms. Materials and Methods: Thirty-eight patients with intraspinal abnormalities without preoperative neurological symptoms were matched with 183 AIS patients for sex, age, blood loss, operating time, and curve magnitude. Patients were evaluated before surgery, within 1 week after surgery, and more than 3 years at the last follow-up for complications and changes in main curve correction, global coronal balance, thoracic kyphosis, and sagittal vertical axis. Results: On average, the duration of follow-up was 52.5 months in the INNAs group compared with 51.6 months in the AIS group. The major coronal curve, global coronal balance, TK (thoracic kyphosis), and SVA (sagittal vertical axis) significantly improved after surgery and maintained to the last follow-up in the 2 groups. No statistical difference of the parameters between the 2 groups were observed at the last follow-up. The progression of more than 10° was found in 8% of intraspinal abnormalities patients and 7% of AIS patients. The neurological complications were observed in 5% of intraspinal abnormalities patients and 4% of AIS patients. Conclusion: Routine MRI (magnetic resonance imaging) was suggested for the presumed idiopathic scoliosis patients. Single-stage corrective surgery is safe and effective in scoliosis patients associated with intraspinal abnormalities without preoperative neurological symptoms when and the radiographic and clinical outcomes were comparable to AIS patients. Two- to 4-week preoperative halo-gravity traction and intraoperative monitoring of spinal cord and wake-up test is required for all the scoliosis patients with intraspinal abnormalities.
P069: Surgical Strategy of Severe Scoliosis Associated With Intraspinal Abnormalities Without Neurologic Symptoms
Yong Hai1 and Jingwei Liu1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: Severe scoliosis is a relatively uncommon 3-dimensional spinal deformity most often presenting with severe and rigid kyphoscoliosis, which can increase the risks of progressing of scoliosis and cardiopulmonary distress. With the development of magnetic resonance imaging (MRI), intraspinal abnormalities have been discovered increasingly in patients with presumed idiopathic scoliosis (PIS). The incidence of intraspinal abnormalities in severe scoliosis was reported high to 42.6% in the published study. Surgical strategy for them was difficult due to the combined greater risks of developing neurological complications after spinal corrective surgery. The purpose of this study was to investigate whether single-stage corrective surgery without proceeding neurologic intervention appropriate for asymptomatic severe scoliosis patients associated with intraspinal abnormalities Materials and Methods: Twenty-three consecutive patients associated with severe scoliosis and intraspinal abnormalities from January 2012 to December 2015 who underwent single-stage posterior spinal corrective surgery were identified. The average age was 14.3 years (range = 11-21). All patients received MRI (magnetic resonance imaging) and Chiari deformity was found in 4 patients, syringomyelia was found in 9 patients, syringomyelia with Chiari deformity was found in 6 patients, syringomyelia with tethered cord was found in 2 patients, and splitcord was found in 2 patients. All the patients were asymptomatic before surgery. Safety and efficacy of surgery were conducted. Results: The preoperative mean major coronal curve was 122° (range 95-146°) and improved to 66° (range 56-83°) at the last follow-up for a 42% of correction. The mean TK (thoracic kyphosis) was 87° (range 74-114°) preoperatively and was measured 65° (range 46-82°) at the last follow-up. No neurological deteriorations were observed at last follow-up. Conclusion: Single-stage posterior spinal corrective surgery with polysegmental Ponte osteotomy is safe and effective for asymptomatic severe scoliosis patients associated with intraspinal abnormalities when performed in conjunction with adequate preoperative traction and intraoperative spinal tissue monitoring and wake-up test.
P070: Spinal Deformity in a Child With Sanjad-Sakati Syndrome: A Case Report From the Sultanate Of Oman
Samuel Johnson1, Idris Malik1, and Ahmed Al Jahwari1
1Armed Forces Hospital, Seeb, Oman
Introduction: Sanjad-Sakati syndrome (SSS) is a genetic disorder found exclusively in people of Arabian origin inherited by an autosomal recessive pattern of inheritance. The principal features of SSS are hypoparathyroidism, seizures, severe growth, developmental retardation, and dysmorphic features (microcephaly, facial, eye, dental anomalies). Additional manifestations of SSS have been gradually discovered. However, there has been no published documentation of the spinal deformity in SSS. Supportive treatment in the form of vitamin D and growth hormone is offered to patients with SSS. In OMIM (241 410), SSS is listed as hypoparathyroidism-retardation-dysmorphism syndrome (HDR). Disorder is caused by “Bedouin Mutation” c.155-166del of the TBCE gene. This is a report of a 13-year-old girl with SSS investigated for her spinal deformity to identify its cause. So, this case study supports the first documented spinal manifestation in SSS by reporting a Scoliosis deformity. Material and Methods: A 13-year-old girl with SSS was brought to our clinic by her parents. Diagnosed SSS on prenatal CVS (chorionic villus sampling) during mother’s pregnancy. The parents noticed a progressive curvature of the back and a limp. Short statured, with facial dysmorphic features and microcephaly. Walks unaided with a non-antalgic, asymmetrical gait. On standing, the spine shows a curvature toward the left side, which is more pronounced in the lumbar region. Shoulders are balanced, and a left lateral pelvic tilt is seen. Can sit only with support of her arms. No wasting or contractures of the paraspinal, hip, and lower extremity musculature. No tenderness along the curvature of the spine, or at the sacroiliac joint. Her spine movements are restricted in right flexion alone. On squaring the pelvis, the lower limbs are of equal length with a full range of movements. Intact neurological examination of the upper extremities, trunk, and lower extremities. Results: Blood investigations revealed low serum calcium, very low PTH (parathyroid hormone) with normal alkaline phosphatase and lymphocyte levels. Peak expiratory flow yielded normal results. The sleep apnea study revealed mild Apnea-Hypopnea Index. Anteroposterior (AP), right, left side-bending, lateral, and AP stretch radiograph views of the spine revealed osteopenia, no collapse, abnormal vertebrae, spina bifida, or kyphosis. Cobb’s angle measured from T12-L4 was 40° correctable to 21° on left side–bending view. The pelvic tilt was correctable from 24° to 8° on stretch view. Investigations including MRI (magnetic resonance imaging) reported no abnormalities in the cord and spinal canal. A 2D (2-dimensional) echocardiography revealed normal cardiac function, and an ultrasonogram of the kidney was normal. Bone mineral density (BMD) revealed a Z score −3.0. Conclusion: SSS is closely related with autosomal recessive Kenny Caffey Syndrome in that both are chaperone diseases caused by a genetic defect in the tubulin assembly pathway. Idiopathic scoliosis is further classified based on the age of diagnosis into infantile idiopathic, juvenile idiopathic, and adolescent idiopathic. Osteopenia and osteoporosis as the etiology for idiopathic scoliosis remains controversial. However, the prevalence of osteopenia in scoliosis is 20% to 38%, and it has been proved that the spinal architecture found in patients with osteopenia may aggravate the spinal deformity. Since this child has osteopenia on blood, imaging, and BMD studies, we attribute osteopenia to be the cause of her scoliosis. Hence, we conclude that children suffering from SSS have the possibility of developing scoliosis based on the fact that they have osteopenia due to hypoparathyroidism.
P071: Can We Predict Pedicle Dimensions in Adolescent Idiopathic Scoliosis: A Morphometric Analysis of Transverse Process and Ipsilateral Pedicle
Sudarshan Munigangaiah1, Gautam Reddy1, Mohamed Mohamed1, Colin Bruce1, Neil Davidson1, and Jayesh Trivedi1
1Alder Hey Children’s Hospital, Liverpool, UK
Introduction: In adolescent idiopathic scoliosis (AIS), the pedicle sizes dramatically vary in dimensions and are not possible to visualize dimensions of pedicle during the posterior approach to the spine. We hypothesize that we can use the transverse process intraoperatively as a guide to predict pedicle size and as a result the size of pedicle screw. Material and Methods: This retrospective review was carried out of all patients diagnosed with AIS at our institution over the past 2 years (186 patients), and 6 patients were identified who have had preoperative computer tomography (CT) scans. The apical vertebra was determined, and 3 vertebral levels cranial and caudal to this were identified. The transverse process width (TPW) and height (TPH), and the pedicle width (PW) and height (PH) on the concave side were measured from agreed reference points. Results: Six patients were included in this study, 4 females and 2 males, with an average age of 14 (13-16) years. The average Cobb angle was 79° (67-91°). Forty-two vertebral levels measurements showed TPW 16.57 ± 4.61, TPH 10.81 ± 1.42, PH 8.24 ± 2.27 and PW 5.27 ± 2.45. There was no significance correlation between TPH and PH (P = .359) or TPH and PW (P = .412). Spearman’s rank analysis demonstrated a significant negative correlation between TPW PH (P = .01) and TPW PW (P = 0.02). The ratios of TPW/TPW = 8.2/0.18 and PH/TPW = 12.2/0.2 were evident. Conclusion: Width of the transverse process of thoracic spine in AIS can predict pedicle height and pedicle width (pedicle dimensions). This can help surgeon intraoperatively predict pedicle dimensions and aid selecting suitable levels of instrumentation.
P072: Posterior 4-Rod Instrumentation and Fusion for Neuromuscular Scoliosis in Patients With Cerebral Palsy (GMFCS Level V)
Daniel Adler1 and Michael Akbar1
1Ruprecht-Karls-University Heidelberg, Heidelberg, Germany
Introduction: Children with infantile cerebral palsy (ICP) show pronounced scoliotic deformities in addition to neurological symptoms. The progression of pelvic and shoulder obliquity leads to the loss of sitting ability. Lung and organ function are also negatively affected. Conservative measures alone are not sufficient but necessary for the therapy. Long-segmented instrumentation and fusion to os ilium is required to improve the quality of life. Material and Methods: It is a retrospective clinical and radiological study. In 2017, a total of 19 patients (mean age = 15.5 years) with neuromuscular scoliosis in cerebral palsy (GMFCS [Gross Motor Function Classification System] level V) were surgically corrected under neuromonitoring. Sixteen patients were treated with a conventional 2-rod system and 3 patients with a 4-rod system. Sufficient pedicle screws are placed in the cranial and caudal segments of the spine for stable anchorage using the 4-rod system. Subsequently, the 2 overlapping rods are fixed with connectors and clamps. The extent of correction (Cobb angle, shoulder, and pelvic obliquity) were analyzed on the pre- and postoperative radiographs. Furthermore, operation time and intraoperative blood loss were compared. Results: Postoperative radiological and clinical findings as well as complications were determined in 4-rod and 2-rod patients. Using the 4-rod system, an improved correction of Cobb angle as well as pelvic and shoulder obliquity were detected. Surgical time, blood loss, and postoperative ICU (intensive care unit) stay were not significantly different. Conclusion: Modified posterior instrumentation and fusion in neuromuscular scoliosis using the 4-rod system has an improved correction potential concerning Cobb angle and shoulder/pelvic obliquity compared with the 2-rod system. Equivalent implant costs, surgery time, and blood loss were detected.
P073: Posterior Instrumentation and Fusion in Children With Cerebral Palsy (GMFCS Level V)
Daniel Adler1 and Michael Akbar1
1Ruprecht-Karls-University Heidelberg, Heidelberg, Germany
Introduction: Children with cerebral palsy (CP) show pronounced scoliotic spinal deformities in >80% of cases, especially with loss of walking ability (GMFCS [Gross Motor Function Classification System] level IV/V). In contrast to idiopathic scoliosis, neuromuscular scoliosis stiffs early and shows to be progressive even after completion of longitudinal growth. Progression of pelvic and shoulder obliquity leads to the loss of sitting ability, and the lung and organ function are also negatively affected. Conservative treatment alone is not sufficient, but necessary for the therapy. Long-segmented spondylodesis from the upper thoracic spine (TH2/3) to os ilium is necessary to improve the quality of life in these patients. Material and Methods: It is a retrospective clinical and radiological study. In the years 2014 to 2016, a total of 31 patients (mean age = 15.5 years, 11 females, 20 males) with neuromuscular scoliosis in infantile cerebral palsy (GMFCS level V) were surgically corrected under neuromonitoring. In each patient, a long-segmented posterior spondylodesis was performed by means of a screw-and-rod system from TH2 to the os ilium. The minimum follow-up was 1 year. For 25 patients, there was a pre-and postoperative evaluation using a modified CPCHILD questionnaire. Results: Pre- and postoperative radiological and clinical results were determined and compared with the current literature. Preoperative traction recordings were used to estimate the correction potential. The preoperative Cobb angle averaged 91° (133-54°) and was corrected postoperatively to an average of 24° (45-4°). The shoulder obliquity preoperatively averaged 10.9° (32-3°) and postoperatively 2.5° (8-0°). The pelvic obliquity was corrected from a preoperative average of 24.9° (52-3°) to postoperatively 4.7° (12-0°). Postoperatively, a pelvic obliquity of >10° persisted in 2 patients. The average operating time was 320 minutes (203-459 minutes), the average operative blood loss 1837 mL (1500- 6300 mL). In 2 patients, a 2-staged asymmetric pedicle subtraction osteotomy (PSO) was required for definitive scoliosis correction. The evaluation of the modified CPCHILD questionnaires showed an improved score postoperatively and thus a benefit for the infantile cerebral palsy (ICP) patients. Conclusion: Posterior spondylodesis of neuromuscular scolioses using a screw-and-rod system is the proven standard in surgical scoliosis therapy in ICP patients. Long-segmented spinal fusion from the upper thoracic spine (TH2/3) to the os ilium are indicated in patients with loss of walking ability (GMFCS level IV/V). The shoulder and pelvic obliquity can be addressed adequately. Using HRQOL (health-related quality of life) questionnaires (eg, modified CPCHILD), patient benefit can be demonstrated for surgical therapy.
P074: Evaluation of Axial Rotation, Coronal Correction, and Sagittal Profile Post Implantation of Magnetically Controlled Growing Rods in the Setting of Adolescent Idiopathic Scoliosis
Wojciech Pepke1, Haidara Almansour1, and Michael Akbar1
1Heidelberg University Hospital, Heidelberg, Germany
Introduction: Magnetically controlled growing rods (MCGR) enable distraction without anesthesia. Therefore, this system constitutes an important alternative within the scope of adolescent idiopathic scoliosis (AIS) treatment at Risser stage 0-2 (Sanders 1-3). The aim of this study was to determine the postoperative result in relation to the coronal and sagittal parameters as well as the vertebral axial rotation and compare them with preoperative values. Material and Methods: Twenty-one AIS patients who underwent surgical implantation of MCGR were included. Full-spine X-ray radiographs of these patients were retrospectively analyzed. Based on previously published sagittal profile normative data, patients were stratified into a hypokyphotic and a normokyphotic group for thoracic kyphosis (TK). Furthermore, patients were divided by the sagittal vertical axis (SVA) into SVA <0 and SVA ≥0. Spinopelvic parameters (PI [pelvic incidence], PT [pelvic tilt], SS [sacral slop]), regional parameters (LL [lumbar lordosis], TK [thoracic kyphosis], T1T3 angle, T1T4 angle, CL, C1C2 angle), global balance parameters (SVA, cSVA, T1SPi, T9SPi), and the axial rotation of the apical vertebrae (Raimondi angle) were determined. The coronal correction of the structural and compensatory curves was evaluated using the Cobb angle. Results: The preoperative mean Cobb angle of the structural curve was 64°, and that of the compensatory curve was 44°. The postoperative Cobb angle of the structural curve could be reduced to 36° (▵= 28°; P = .001), and that of the compensatory curve to 27° (▵ = 17°; P = .001). T1/T12 kyphosis decreased by an average of 10° postoperatively (P = .001). In the normokyphotic group, there was a significant flattening of the TK (P < .05) and reciprocal decrease in lordosis (P < .05). The hypokyphotic group showed a tendency of a decreased TK, however, not statistically significant (P = .075). The SVA <0 mm group revealed a significant decrease in TK (P < .001) and also showed a reciprocal decrease in LL after surgery (P = .046). Finally, among all stratified groups, the axial rotation of the apical vertebra (Raimondi angle) was significantly improved in the thoracic curves (P < .05). On the other hand, lumbar curves showed an improvement; however, it was not statistically significant. Conclusion: This is one of the few studies that addresses postoperative sagittal correction and apical vertebral rotation of the spine in patients with AIS who underwent implantation of MCGR. Our data show that the application of these innovative growing rods leads to a significant improvement of the coronal profile and apical vertebral rotation. However, the possible changes in the sagittal profile (loss of TK and a possible reciprocal loss of LL) should be taken into account by the surgeon. Positioning of actuators has to be considered while MCGR implantation.
P075: Analysis of Vertebral Rotation, Sagittal Alignment, and Reliability in Surgically Treated Adolescent Idiopathic Scoliosis Patients via Tridimensional Reconstruction of the Spine
Wojciech Pepke1, Haidara Almansour1, and Michael Akbar1
1Heidelberg University Hospital, Heidelberg, Germany
Introduction: Low-dose 3-dimensional (3D) stereoradiography improves analysis and determination of spino-pelvic parameters and allows for better planning and management of scoliosis by acquiring and analyzing rotational components of each vertebra. The purpose of this study was to analyze 3D correction of postoperative adolescent idiopathic scoliosis (AIS) patients and to compare it with its preoperative values. Furthermore, parameters were measured by 2 raters in order to test the inter-rater reliability and reproducibility of this method. Material and Methods: Spines of 17 consecutive patients with AIS and full-spine biplanar stereoradiographs were reconstructed in 3 dimensions. Spino-pelvic parameters, rotation of each vertebra (T1-L5) for 3 planes (frontal, lateral, and axial), and sagittal parameters were measured pre- and postoperatively. Paired t tests were used to compare pre- and postoperative changes. Two independent raters who were trained on the software and were blinded to patients’ data analyzed the aforementioned parameters in all 3 planes to determine agreement between their measurements using ICC (intraclass correlation coefficient). Results: Mean Cobb angle for primary scoliotic curve was 53°, and for the secondary curve was 39° After surgery, mean of Cobb angle for the primary curve was 16° and for the secondary curve was 12°. T1/T12 kyphosis revealed an increase of 8° after surgery. Postoperatively, frontal rotation of the vertebrae was significantly (P < .05) changed in the middle (T4-T7) and lower (T11-T12) thoracic spine. Rotation of the other vertebrae was too small to be considered statistically significant. Postoperative lateral rotation of vertebrae was significantly changed in the lower thoracic spine (T7-T12) and middle lumbar spine (L2-L4). Inter-rater reliability and reproducibility that reflects agreement between the 2 raters revealed excellent agreement (all over 91%) for all parameters in this study with the exception of axial rotation, which showed moderate agreement especially in the region of upper and middle thoracic spine. In contrast, axial rotation measurements of the 2 raters showed substantial improvement postoperatively. Conclusion: Tridimensional reconstruction of the spine via low-dose biplanar stereoradiography software seems to be a competent tool for measuring the correction of spino-pelvic parameters. Furthermore, it seems to conduct a reliable analysis of frontal and lateral vertebral rotation. However, measurement of axial rotation seems to be problematic in upper and middle thoracic spine, which might be complicated by the severity of the curve and increased difficulty to delineate anatomical landmarks in this region.
P076: Experimental Substantiation of Technique of Guided Growth of Vertebral Bodies in Management of Scoliosis in Children
Andrey Kobizev1
1Russian Ilizarov Scientific Center, Kurgan, Russian Federation
Introduction: Among factors influencing growth of bone tissue, there are genetic, vascular, hormonal, neurogenic, and biomechanical factors. In the middle of the 19th century, a regularity of mechanical influence on bone growth in longitudinal direction was described as the Hueter-Volkmann law: “the growth is delayed under influence of excessive compressing mechanical stress and vice versa.” Methods: On 21 experimental animals, the method for correction of scoliosis of the spinal column using controlled growth of vertebrae was developed with application of Π-shaped nickelide titanium brackets with partial disorder of nutrition of vertebrae by the metal plate. Results: Contrasting with the influence of asymmetric stress on the growth plate in formation of deformity in clinical practice, there is a concept of “guided growth,” which uses ability of growing bones to subject to plastic deformities under influence of change of growth process of epiphyseal plates. The purpose of the study is to substantiate the technique of guided growth of vertebral bodies. Conclusion: Application of this technique allows for stopping of progress of experimental scoliosis in growing animals and also leads to improvement of tissue microcirculation, stabilization of fibrillogenesis, and recovery of spinal column tissues.
P077: Modified Growth Guidance Technique Through Posterior Approach for Early-Onset Scoliosis Correction
Alaaeldin Ahmad1 and Loai Aker2
1 Polytechnique University, Ramallah, Occupied Palestinian Territory
2 Annajah Medical School, Nablus, Occupied Palestinian Territory
Introduction: We hypothesize that wedging of the deformed vertebrate in immature scoliosis can be corrected through posterior tethering of the convex side to halt the progression phase of scoliosis, restores the loss of height of the wedged side. Non-fusion procedure (combined guided growth + compression based technique) is performed, by placing pedicular screws in the convex side above and below the wedged vertebrae. This procedure will redistribute the pressure on the vertebral body by correcting the mechanical stress before its precipitous period, and remodulate the scoliosis deformity during the growth period. Methods: Retrospective review of 12 EOS (early-onset scoliosis) patients whom all had MRI (magnetic resonance imaging) or computed tomography (CT) scan preoperatively and 3D (3-dimensional) CT in the last follow-up, with a minimum of 24-month follow-up. Patients underwent posterior tethering proximal and distal to the peak of the deformity as an adjunct to distraction-based growth-friendly, or the Shilla implants. The rate of change was calculated for the wedged apical vertebrae at the concave and convex heights in scoliosis and kyphosis. Control group had the same parameters measured for the vertebrae outside the tethering effect. Cobb angle and spinal height were also measured. Results: Mean age at surgery: 45 months. Conclusion: Posterior tethering in EOS will asymmetrically modulate the apical vertebrae, correcting the deformity with non-fusion technique.
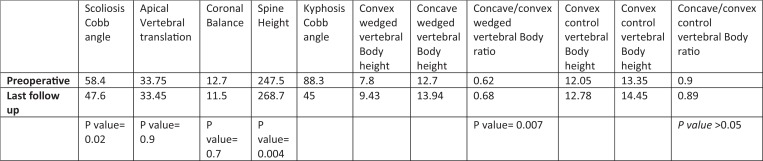
|
P078: Hooks and Screws Versus Screws Only, In Adolescent Idiopathic Scoliosis: A Case-Control Study
Javier Ernesto Matta Ibarra1, Victor Elias Arrieta Maria1, Fabio Alexander Diaz Otero1,Orlando Villarreal Barrera1, Heber Mauricio Torres Moreno1, Kerly Yulieth Ponguta Marquez1, Edgar Fabian Manosalva Cortes1, Maria Cristina Ramos1, and Andres Enrique Cobar Bustamante2
1Department of Orthopedic Surgery/Spine Surgery, Bogota, Colombia
2Department of Orthopedic Surgery/Spine Surgery, Guatemala, Guatemala
Introduction: Adolescent idiopathic scoliosis (AIS) affects 1% to 3% of children at risk from 10 to 18 years of age. The etiopathogenesis of this disorder remains unknown; it consists in the presentation of a structural curvature in the coronal plane with a rotational component—of the vertebral column that appears among healthy children around puberty. The diagnosis is based on exclusion, and it is made only when other causes of scoliosis have been ruled out, such as vertebral malformation, neuromuscular disorder, and syndromic disorders. Some surgeons still advocate for the use of laminar or pedicular hooks because of the lower surgical risks these involve. Objectives: To compare surgical complications, surgery time, percentage of instrumented vertebrae, height gain, fusion rates, Cobb correction results, and hospitalization days between AIS patients corrected with hooks and screws versus the use of pedicular screws for the whole correction. Methods: Observational retrospective study, case-control type, on patients with a diagnosis of AIS, between 10 and 19 years of age, with a panoramic anteroposterior and lateral simple radiography that met surgical criteria. Group 1 (56 cases) corresponds to patients included in a study made in the year 2009, treated surgically with hybrid instrumentation, and group 2 (20 cases) treated with thoracic and lumbar pedicle screws. Student’s t and χ2 tests were utilized for qualitative and quantitative variables. The sociodemographic, clinical, and radiological variables were analyzed, as were the correction of thoracic and lumbar curvatures following surgical intervention, surgical time, and in the same manner, the gain in postsurgical stature and the percentage of instrumented vertebrae. A P value below .05 was considered statistically significant. Results: From the sociodemographic point of view, the study population in the 2 groups is homogeneous; results indicate that the stature gain, surgical time, sagittal balance, and complications were similar, the percentage of correction of structured curvatures was greater for group 2 as opposed to group 1 (75.4% vs 65.4%) in spite of a lower percentage of instrumented vertebrae (69.1% vs 76.8%). Greater correction of proximal thoracic curve was observed in group 2 (P = .04). The improvement of coronal balance was greater for group 2. Conclusions: Similar results were found for the 2 techniques, regarding surgical time used, stature gain, and associated complications. Results were better for the pedicle surgical technique on both regions in relation to coronal balance and correction of structured curves, primarily on main thoracic curvatures.
P079: Providence Nighttime Bracing Are Effective in Treatment of Adolescent Idiopathic Scoliosis, Even in Curves Larger than 35°
Ane Simony1, Mikkel Osterheden Andersen1, Stig Mindedahl Jespersen2, and Leah Yaccat Carreon1
1Sector for Sppine Surgery & Research, Middelfart, Denmark
2 University Hospital Odense, Odense, Denmark
Introduction: In 2007, the primary conservative treatment of adolescent idiopathic scoliosis (AIS) in Denmark, went from full-time bracing to nighttime bracing. The purpose of this study is to evaluate the effectiveness of nighttime bracing in a cohort of AIS patients, with curves from 20° to 45°. Material and Methods: Patients diagnosed with AIS, skeletally immature, and initial Cobb angle between 20° and 45° was included in this study. All patients had curves with apex at T6 or below and was instructed to wear the Providence nighttime brace at least 7 to 8 hours per night. No other previous treatments were accepted, and no physiotherapy was applied during brace treatment. Treatment was continued until 2 years post menarche or for male patients until growth arrest for 6 months was observed. All patients had their last follow-up radiograph, at least 12 months out of brace. Cross-measured X-rays was used to compare the primary Cobb angle, the in-brace correction, and the outcome Cobb angle. The brace treatment was considered failed if progression occurred was more than 5° and if surgery was performed. Results: A total of 124 consecutive patients were included in this study, 80 patients completed brace treatment and 12-months follow-up. A total of 68 females and 12 males were included in this study. To evaluate the effect of bracing in curves >35°, the patients were divided into groups, according to Cobb when treatment was initiated 20° to 29°, 30° to 39°, and 40° to 45°, see Table 1 for further demographics. Brace treatment was effective in 83.3%, and progression of the deformity was observed in 16.7% of the patients. Only 5% of the patients were referred to surgical treatment. Conclusion: Providence nighttime braces are effective, as a treatment in AIS patients. This study reports a success rate of 88.7%, and the results are comparable to full-time treatment with Boston braces or other TLSO (thoraco-lumbo-sacral-orthosis). The brace correction is crucial in part-time bracing, and we recommend at least 70% curve correction, if part-time bracing should be considered.
P080: Curvature Types in Adolescence Idiopathic Scoliosis According to Lenke Classification
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, Marcos Silva2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: Idiopathic scoliosis is a common deformity of the spine characterized mainly by a change in alignment in the coronal plane, sagittal plane hypokyphosis, and rotational deformity in the axial plane.1,2 The Lenke and associates classification system of adolescent idiopathic scoliosis (AIS) was developed to provide a comprehensive and reliable means to categorize all surgical AIS curvatures.3 The purpose of this study is to characterize, according to the Lenke classification, the most common type of curvatures in a population with AIS. Material and Methods: We conducted a retrospective study of 80 patients with AIS. Inclusion criteria incorporated patients with a PA (posterioanterior) and lateral full-length radiographs. Patients excluded from the study were those who underwent surgery, those who have initiated orthotic treatment, and with low-quality radiography. Results: In relation to the scoliotic curvatures, 36 patients presented with a type 1 curvature (main thoracic), 3 with a type 2 (double thoracic), 10 with a type 3 (double major), 1 patient with a type 4 (triple major), 25 with a type 5 curvature (thoracolumbar/lumbar), and 5 patients with a type 6 curvature (thoracolumbar/lumbar-main thoracic). Regarding the lumbar spine modifier, 40.0% were type A, 36.3% were type B, and 23.8% were type C. We found 24 different curvatures according to Lenke classification. The types most frequently found were 1AN (25.0%), 1BN (13.8%), 5BN (11.3%), 5AN (7.5%), 5CN (7.5%), and 6CN (5%), making a total of 70.1% of the sample. Conclusion: From this study, we can draw conclusions about the type of curvatures most common in a population with AIS, essential parameters in the clinical and therapeutic evaluation of this pathology.4,5
P081: Leg Length Discrepancy <1 cm in Idiopathic Adolescent Scoliosis: Is it Important?
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: Leg length discrepancy (LLD) causes pelvic obliquity in the frontal plane.1 On the other hand, it leads to posture deformation, gait asymmetry, low back pain, discopathy as well as gonarthrosis, coxarthrosis, and hip flexion contracture on the side of the longer extremity or ankle joint contracture in the equinal position on the side of the shorter extremity.2-9 The objective of this study is to evaluate LLD in adolescence idiopathic scoliosis. Material and Methods: Our study population included 80 patients with adolescence idiopathic scoliosis. The parameters evaluated were age, sex, sagittal and coronal balance, and LLD assessed through the difference between the femoral heads and through assessment of pelvic obliquity (PO). Results: The majority of patients with AIS demonstrated a mild LLD (<1 cm). The mean LLD value was significantly different (P < .01) between the scoliotic population with a main thoracolumbar curvature relatively to the ones with a main lumbar curvature. When there was a LLD, the left limb was shortened in most of the cases. The side of the shortened or elongated lower limb was of great interest in relation to the decompensation of the coronal balance (P < .05). Conclusion: From this study, we verified that in an AIS population with small LLD values, the magnitude of the shortening has a stronger impact on the location rather than on the dimension of the main scoliotic curvature. These results raise the importance of a more in-depth study regarding the importance of LLD <1 cm in the development of AIS and coronal imbalance.
P082: Skeletal Maturity in Adolescent Idiopathic Scoliosis
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: Joseph C. Risser first described what is now known as Risser sign in 1958.1 Risser noted that the state of ossification of the iliac apophysis was associated with skeletal maturity and proved to be an excellent physiological sign of the end of vertebral growth, valuable information in the current adolescence idiopathic scoliosis (AIS) approach.1 In AIS, the best predictors of curve progression are growth potential and velocity, both of which are extremely dependent on skeletal maturity.2,3 This parameter guides the interval of follow-up, duration of treatment with vest, the decision to operate, and the timing of the surgery. Therefore, physicians who treat AIS use skeletal maturity, such as skeletal age, menarche, and the Risser stage as an assistant in the therapeutic decision. Of these, the Risser stage is likely to be the most widely used parameter in assessing skeletal maturity.4,5 The objective of this study is to evaluate a relationship between Risser stage, triradiated cartilage, and the scoliotic curvature dimension. Material and Methods: Eighty patients with AIS were analyzed. The parameters evaluated were age, sex, Risser stage, trirradiate cartilage state, and scoliotic curvatures differentiated according to the Lenke classification. Results: The population in study presented a mean age of 12.44 years (s = 2.38 years). The Risser stage most frequently found was 0, corresponding to 43.8% of the sample. The TC was found to be mostly closed (67.5% of the study population). On the other hand, all the patients with open TC presented a Risser stage of 0. The TC presented a statistically significant and inverse correlation with the coronal main Cobb angle, indicating that patients with an open triradiate cartilage, and therefore skeletally very immature, presented smaller scoliotic curvatures (P < .05). It was corroborated that patients with open TC had a primary scoliosis curvature angle of 16.29° (s = 9.73°) versus 24.31 (s = 17.43°) in those with closed computed tomography (CT) scan. The difference in scoliotic curvature angle between these 2 groups was statistically significant (P < .05). Conclusion: Skeletal maturity was of great importance in the progression of the scoliotic curve, with TC having a huge importance in the potential of progression of scoliotic curvature. On the other hand, we observed a scoliotic curvature progression with increasing skeletal maturity. However, it is important to note that this progression does not appear to be continuous, but presents its highest peak within the Risser stage 0, until the closure of the CT.
P083: Sagittal Balance and Scoliosis: What Can We Expect?
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: The human standing posture involves a delicate balance between the spine and pelvis.1 Many studies2-5 have demonstrated that sagittal balance rather than coronal balance is significantly correlated with health-related quality of life (HRQOL). Others have found great impacts of lumbar lordosis (LL) and thoracic kyphosis (TK) on maintenance and prediction of sagittal balance, which are considered novel regional predictors for sagittal balance.6,7 Satisfactory treatment for adolescent idiopathic scoliosis (AIS) includes maximum correction in the coronal plane, in addition to adequate restoration of the sagittal spinal alignment and vertebral rotation. The objective of this study is to achieve a better understanding of the parameters that influence the sagittal balance in a population with AIS. Material and Methods: The inclusion criteria were 80 scoliotic patients between 10 and 18 years of age with a posteroanterior (PA) and lateral full-length radiographs, excluding those subjected to surgery or orthotic treatment, with other spinal disease or with poor X-ray quality. The parameters evaluated were age, sex, pelvic incidence (PI), sacral slop (SS), pelvic tilt (PT), sagittal balance (SB), coronal balance (CB), lumbar lordosis (LL), thoracic kyphosis (TK) divided in to high (T1-T5) and low (T5-T12), and cervical spine alignment (CSA). Results: The group in study presented a mean SB of −1.14 cm (s = 3.30 cm), 29 patients with a negative sagittal deviation (<−2 cm), only 9 with a positive deviation (>2 cm), and the remainder were considered balanced (with SB greater than −2 cm and less than 2 cm). Regarding the SB, it demonstrated a significant statistical correlation with the cervical shape (P < .01) and the upper portion of the thoracic spine (from T1 to T5; P < .05) but not with the other variables. Conclusion: SB is a parameter influenced by multiple factors. In fact, it is extremely related to the cervical shape. We verified a positive deviation of the sagittal balance with an increase in cervical lordosis. On the other hand, the SB is related to the severity of thoracic kyphosis, mainly with its upper portion.
P084: Spinopelvic Parameters in Adolescent Idiopathic Scoliosis
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: The sagittal curvature of the spine and the pelvic balance swing together to maintain a stable posture and horizontal gaze. Once this sagittal alignment is lost, more energy is needed so that the body remains balanced without any external support.1 The importance of sagittal spinopelvic organization in spine pathology and the crucial necessity of its restoration after surgical treatment are now recognized in the literature.2 Effectively, the lumbar spine has a close relationship with the pelvic orientation expressed in particular by the sacral slope, which is influenced by the pelvic incidence.3 When evaluating patients with structural deformities of the cervical spine, an in-depth understanding of the spinopelvic parameters is crucial. Pelvic morphology may influence sagittal spinal alignment and balance.4,5 The objective of this study is to evaluate the spinopelvic parameters and their relationship with lumbar lordosis in a population with adolescent idiopathic scoliosis. Material and Methods: We conducted a retrospective study of 80 patients with adolescence idiopathic scoliosis. The parameters evaluated were age, sex, pelvic incidence (PI), sacral slop (SS), pelvic tilt (PT), sagittal balance (SB), coronal balance (CB), lumbar lordosis (LL), cervical spine alignment (CSA), and thoracic kyphosis (TK) divided in to high (between T1 and T5) and low (between T5 and T12). Results: Spinopelvic parameters were strongly related to each other (P < .01) and presented mean values similar to those found in previous studies with a PI of 50.79° (s = 14.31°), a SS of 42.48° (s = 10.51°) and PT with a mean of 8.68° (s = 9.94°). LL has a strong influence on the lower portion of the thoracic curvature (from T5 to T12) and is strongly influenced by the PI and SS. Conclusion: In a population with adolescent idiopathic scoliosis, the spinopelvic parameters are significantly correlated with each other and with lumbar lordosis. This study confirms the existence of a strong connection between the pelvic geometry and lumbar lordosis.
P085: The Influence of Gender on Adolescent Idiopathic Scoliosis
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: The impact of gender on adolescent idiopathic scoliosis (AIS) remains controversial. Vialle et al reported significant differences in lumbar lordosis (LL) and pelvic incidence (PI) between male and female subjects.1 In addition, Zhu et al found a significant gender difference in LL.2 Conversely, as in this sample, other researchers did not demonstrate significant gender differences in any spinopelvic parameter.3-5 The objective of this study is to evaluate the influence of gender in the spine of a population with AIS. Material and Methods: Eighty patients with AIS were included in the study. The parameters evaluated were PI, sacral slop (SS), pelvic tilt (PT), global sagittal balance (GSB), Cobb angle of the main scoliotic curvature, LL, and thoracic sagittal Cobb angle between T1-T5, T5-T12, and T1-T12. Results: A total of 76.3% of the population was female versus 23.8% male. However, when comparing the gender variable with other variables in the study, there were no significant differences between male and female patients. Conclusion: In this study, among the population with AIS, the female gender was much more prevalent. However, the magnitude of the curvatures, spinopelvic parameters, and sagittal balance were not significantly different among male and female patients. Thus, although the female population seemed to be more susceptible to developing AIS, the spine parameters evaluated were not significantly different from the male population.
P086: Thoracic Kyphosis and Adolescent Idiopathic Scoliosis
Eduardo Moreira Pinto1, Artur Teixeira1, Jorge Alves2, and António Miranda1
1Entre Douro e Vouga Hospital Center, Santa Maria da Feira, Portugal
2Tâmega e Sousa Hospital Center, Penafiel, Portugal
Introduction: The thoracic kyphotic angle depends on postural and morphological parameters that will influence the distribution of loads and, consequently, the biomechanical environment of the spine.1-5 Hilibrand et al reported that a hypokyphotic phenomenon of the thoracic spine was found in the adolescent idiopathic scoliosis (AIS) before the operation.6 The objective of this study is to achieve a better understanding of the relationship between hipokyphosis and AIS. Material and Methods: We conducted a retrospective study of 80 patients with AIS. The parameters evaluated were age, sex, scoliotic curvatures differentiated according to Lenke classification, and thoracic sagittal Cobb angle (between T1-T5, T5-T12, and between T1-T12) following the Scoliosis Research Society classification. Results: We can infer that the sagittal profile of the scoliotic spine differs from what is considered normal. The parameters analyzed in this study were in agreement with previous studies concerning the relation of scoliosis with dorsal hypokyphosis, since our population presented an inverse correlation between the severity of the scoliotic curvature and the angle of kyphosis, but only in the inferior segments (T5-T12; P < .05). On the other hand, the thoracic Cobb angle is not uniform between the 12 vertebrae, having a superior inclination in the upper portion (T1-T5) compared with the lower (T5-T12). Conclusion: It is concluded that the existence of a relation between AIS and a decrease in the angle of thoracic kyphosis, namely in its lower segment.
P087: Pedicle Screw Fixation Is Easier With Additive Manufacturing in Adolescent Idiopathic Scoliosis
Alpaslan Senkoylu1, Mehmet Cetinkaya1, Ali Eren2, Elshan Necefov1, Erdem Aktas3, and Dino Samartzis4
1Gazi University, Ankara, Turkey
2Gumushane Kelkit Government Hospital, Gumushane, Turkey
3TOBB University, Ankara, Turkey
4Hong Kong University, Hong Kong, Hong Kong
Introduction: Freehand pedicle screw placement to a scoliotic spine is technically difficult and demanding procedure. Computer-assisted pedicle screw installation has shown to be more accurate. However, it has disadvantages such as high radiation exposure, long operation time, and need of expensive devices. However, devices manufactured with 3DRP (3-dimensional rapid prototyping) technology and are usable intraoperatively may promise similar outcomes. Methods: Eleven adolescent idiopathic scoliosis (AIS) patients were included in this study from a single institution. After deciding to fusion levels and fixation points, 3D printing (3DP) guides were produced for all individual levels. Preoperatively, 0.625 mm thickness sliced computed tomography (CT) scan images were transferred to materialize interactive medical image control system, and 3D bone models of each vertebra were created. Safe pedicular trajectories were determined in all 3 planes on these models. The 3D guides were modelled according to these trajectories and manufactured with a 3D printer from a biocompatible material (Figure 1). The 3DP guides were used during surgeries of AIS patients. All screws were evaluated and scored with CT images that obtained postoperatively. Class 1 (Accurate) screw axis deviates by less than 2 mm from the planned trajectory, Class 2 (Inaccurate) 2 mm or more but less than 4 mm, and Class 3 (Deviated) 4 mm or more (Figure 2). The mean angle between the inserted pedicle screw and the intended trajectory (ASIT) and the mean distance between the central longitudinal axis of a screw and pedicle (DBSP) were also measured (Figures 3 and 4). Results: The cost of 3DP guide per level was €2. On concave and convex sides, the mean medial malposition was 0.5 ± 0.78 to 0.4 ± 0.62, the mean lateral malposition was 1.43 ± 2.33 to 0.83 ± 1.27, ASIT was 4.18 ± 4.63 and 4.28 ± 5.99, and DBSP was 1.45 ± 2.11 and 0.93 ± 1.24, respectively. There was 29 screws having no penetration, 117 Class-1, 14 Class-2, and 3 Class-3 penetration (Table 1). The accuracy was 92.5% of 134 inserted screws. There was no screw-related complication. Conclusion: Current pilot study showed that 3DP guides facilitate pedicle screw insertion even in rotated vertebrae. They are also safe devices, which promise usage in complex deformities and revision cases.
P088: Treatment of Severe Rigid Idiopathic Scoliosis With Posterior-Only Approach by Less Invasive Osteotomies: Alternative to Vertebral Column Resection
Babak Mirzashahi1
1Tehran University of Medical Sciences, Tehran, Iran
Introduction: Treatment of severe rigid idiopathic scoliosis, curves with less than 25% of correction on bending films and major curve over 90, is a challenging issue among spine surgeons treating this kind of deformity. To achieve maximal correction, adequate mobilization of this type of deformity is necessary, often requiring more extensive surgical intervention, with care taken to avoid clinical and neurological complications. The aim of this study is to evaluate the result of surgical treatment of these patients with stand-alone posterior-only approach. Methods: Fifteen patients with severe rigid idiopathic scoliosis were enrolled in this study. Thirteen females and 2 males with mean age of 15.7 (range = 14-19) and mean curve size of 97 (range = 90-130) were treated with posterior-only approach. Demographic data were collected from the profiles. Before the completion of surgery, radiographic examination including standing anteroposterior and lateral views, bending views, and MRI (magnetic resonance imaging) was carried on. Results: The mean final curve size was 22.6 (range = 5-55). The mean hospital stay was 5 days (range= 4-7). There was no neurologic complication, infection, and any other problem among patients. The mean follow-up was 18 months (range = 11-60 months). Conclusion: As much as the aim of surgical treatment of scoliosis is restoration of sagittal and coronal balance and acceptable spinal alignment, it seems that posterior-only approach is reasonable approach with favorable results.
P089: The Role of Traction Radiographs in the Preoperative Planning of Pediatric Scoliosis
Oded Hershkovich1, Wai Weng Yoon1, Edward Bayley1, and Michael Paul Grevitt1
1Queen’s Medical Centre, Nottingham, UK
Introduction: Preoperative planning for pediatric scoliosis requires a full understanding of the spine as well as evaluation of its flexibility. Radiographs are the first step, with added supine side-bending as the most common method to assess flexibility. The accuracy of this method was questionable and showed a great difference between preoperatives to the postsurgical results. Traction radiographs under general anesthesia (TRUGA) are being used in our institute as an added tool to assess and predict flexibility for cases with high curves especially when an anterior approach is considered or when cooperation of the patient in prone side bending is not expected. The use of TRUGA allows the team to manipulate the spine similar to the surgical procedure without supporting on the patient cooperation. As TRUGA are being used regularly in our institute, our aim was to study their impact on the preoperative planning and predict the final outcome. Our hypothesis was that traction radiographs under general anesthesia will have a significant role in the preoperative planning of pediatric scoliosis (PS) and will be able to predict postoperative results and assist in the decision about the surgical approach chosen. Methods: Retrospective analysis of all cases underwent TRUGA in QMC (Queen’s Medical Centre) since January 2015, based on the surgical registry records. Patients were assessed for demographics and clinical information including their type of scoliosis, its magnitude, the type of surgery chosen, and the surgical outcomes as being presented in Table 1. Results: We summed 31 patients who had TRUGA, 10 AIS, 13 NM and 8 were EOS. Average Cobbs were 84.3 (TH) and 54.1 (L). A total of 25 cases operated, in which 19 had posterior correction, 3 had combined approach, and 3 were treated with growing rod systems. HFT was used in 6 cases (TH Cobb of 93.3 in this group) with most been operated using posterior correction only. The surgical group had an overall correction rate of 56.6% in the thoracic region and 70.4% in the lumbar region. Metal density average was less than 70%. Conclusion: TRUGA predicted success in extreme scoliosis cases, most cases can be treated with posterior only correction with HFT added if a rigid curve is identified. Summary: Preoperative planning for pediatric scoliosis requires a full understanding of the spine and also of its flexibility. TRUGA allows manipulating the spine similar to the surgical procedure without supporting on patient cooperation. As TRUGA are being used regularly in our institute, our aim was to study their impact on the preoperative planning and predict the final outcome. We found that TRUGA predicted success in extreme scoliosis cases. Most cases treated posterior-only, HFT added, if rigid curve was identified.
Reference
1. Polly DW Jr, Sturm PF. Traction versus supine side bending. Which technique best determines curve flexibility? Spine (Phila Pa 1976). 1998;23:804-808.
2. Vedantam R, Lenke LG, Bridwell KH, Linville DL. Comparison of push-prone and lateral-bending radiographs for predicting postoperative coronal alignment in thoracolumbar and lumbar scoliotic curves. Spine (Phila Pa 1976). 2000;25:76-81.
3. Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am. 1997;79:1144-1150.
4. Luk KD, Cheung KM, Lu DS, Leong JC. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine (Phila Pa 1976). 1998;23:2303-2307.
5. King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302-1313.
6. Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis: Is it warranted? Spine (Phila Pa 1976). 1996;21:1241-1249.
7. Hamzaoglu A, Talu U, Tezer M, Mirzanli C, Domanic U, Goksan SB. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30:1637-1642.
8. Kuklo TR, Lenke LG, Won DS, et al. Spontaneous proximal thoracic curve correction after isolated fusion of the main thoracic curve in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2001;26:1966-1975.
9. Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton J. Prospective comparison of flexibility radiographs in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2001;26:E74-E79.
10. Kleinman RG, Csongradi JJ, Rinksy LA, Bleck EE. The radiographic assessment of spinal flexibility in scoliosis: a study of the efficacy of the prone push film. Clin Orthop Relat Res. 1981;(162):47-53.
11. Lenke LG, Betz RR, Haher TR, et al., Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine (Phila Pa 1976). 2001;26:2347-2353.
12. Cheh G, Lenke LG, Lehman RA Jr, Kim YJ, Nunley R, Bridwell KH. The reliability of preoperative supine radiographs to predict the amount of curve flexibility in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2668-2672.
13. Takahashi S, Passuti N, Delécrin J. Interpretation and utility of traction radiography in scoliosis surgery. Analysis of patients treated with Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976). 1997;22:2542-2546.
14. Aronsson DD, Stokes IA, Ronchetti PJ, Richards BS. Surgical correction of vertebral axial rotation in adolescent idiopathic scoliosis: prediction by lateral bending films. J Spinal Disord. 1996;9:214-219.
15. Watanabe K, Kawakami N, Nishiwaki Y, et al. Traction versus supine side-bending radiographs in determining flexibility: what factors influence these techniques? Spine (Phila Pa 1976). 2007;32:2604-2609.
16. Kirk KL, Kuklo TR, Polly DW Jr. Traction versus side-bending radiographs: is the proximal thoracic curve the stiffer curve in double thoracic curves? Am J Orthop (Belle Mead NJ). 2003;32:284-288.
17. Davis BJ, Gadgil A, Trivedi J, Ahmed el-NB. Traction radiography performed under general anesthetic: a new technique for assessing idiopathic scoliosis curves. Spine (Phila Pa 1976). 2004;29:2466-2470.
18. Vaughan JJ, Winter RB, Lonstein JE. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 1996;21:2469-2473.
19. Byrd J 3rd, Scoles PV, Winter RB, Bradford DS, Lonstein JE, Moe JH. Adult idiopathic scoliosis treated by anterior and posterior spinal fusion. J Boint Joint Surg Am. 1987;69:843-850.
20. Mccall RE, Bronson W. Criteria for selective fusion in idiopathic scoliosis using Cotrel-Dubousset instrumentation. J Pediatr Orthop. 1992;12:475-479.
21. Large DF, Doig WG, Dickens DR, Torode IP, Cole WG. Surgical treatment of double major scoliosis. Improvement of the lumbar curve after fusion of the thoracic curve. J Bone Joint Surg Br. 1991;73:121-124.
22. Chan CY, Kwan MK, Saravanan S, Saw LB, Deepak AS. The assessment of immediate post-operative scoliosis correction using pedicle screw system by utilising the fulcrum bending technique. Med J Malaysia. 2007;62:33.
P090: The Safety and Efficacy of Corrective Surgery Only for Spinal Deformity Associated With Intro-Canal Abnormalities Without Clinical Symptom
Yong Hai1 and Shuo Zhang1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: Intro-canal abnormalities were often seen in spinal deformities such as congenital scoliosis. Whether or not to perform intro-canal intervention for patients who had intro-canal abnormalities has been controversial in the past. In order to evaluate the safety and efficacy of correction surgery only for patients, who had spinal deformity associated with introspinal abnormalities without clinical symptoms, a retrospective study was conducted. Methods: One hundred thirty-five AIS patients without nervous system complications and 38 spinal deformity patients associated with intro-spinal abnormalities from January 2011 to January 2015, 22 of them associated with spinal cord untethering, 24 of them associated with syringomyelia, and15 of them associated with tethered spinal cord. Both groups only had correction surgery without surgery for intro-spinal abnormalities. The mean major curves preoperatively, operating time, blood loss, mean major curves correction rate postoperatively, correction loss after 2 years, and complication rate were compared between the 2 groups. Results: The mean major curves preoperatively, operating time, blood loss, mean major curves correction rate postoperatively, correction loss after 2 years of 2 groups have no statistical differences. Three patients had neurologic complications in intro-spinal abnormalities group postoperatively, 1 of them had lower limbs motor dysfunction, 2 of them had lower limb sensory dysfunction, all were recovered after conservative treatment in 3 months. In addition, 1 patient had superficial infection and 1 patient had rod fracture. No neurologic deteriorations in 2groups were observed in last follow-up more than 2 years. Conclusion: The correction surgical treatment for spinal deformity associated with intro-spinal abnormalities provides a satisfactory option to effectively improve the spinal deformity compared with correction surgery to AIS patient. In addition, correction surgical treatment for spinal deformity associated with intro-spinal abnormalities have no significant neurologic deteriorations in long-term follow-up.
P091: Radiographic Follow-Up of Idiopathic Scoliosis Fusion Surgery: Challenging the Consensus
Raf Mens1, M. van Hooff1, R. Geuze1, M. Spruit1, P. Horsting1, M. de Kleuver2, and L. de Klerk1
1Sint Maartenskliniek, Nijmegen, Netherlands
2Radboudumc, Nijmegen, Netherlands
Introduction: For patients with adolescent idiopathic scoliosis (AIS), undergoing fusion surgery, international consensus exists that a 2-year radiographic follow-up is needed to evaluate surgical success. This standard lacks empirical evidence. The purpose of this study was to investigate the radiographic follow-up after fusion surgery in adolescent and young adult patients with AIS, from preoperative assessment until 2 years after surgery. Material and Methods: Sixty-three patients, surgically treated for AIS in the period March 2014 to March 2016, age ≤25 (mean 14 years [SD = 3, range = 11-22 years]), providing 2-year radiographic follow-up, were enrolled. Prospectively gathered data of a single-center outcomes registry, following a cohort study design, was analyzed retrospectively. Most recent preoperative and postoperative radiographs at 1- and 2-year follow-up were used. A series of coronal and sagittal angle and balance parameters were measured on every radiograph, with the major Cobb angle as the primary outcome measure. Change in Cobb angle over time was analyzed using Friedman’s ANOVA (P < .05). Measurement error was assumed to be 5°. Results: The major Cobb angle did change significantly between preoperative and 1-year postoperative (Z = −6.85, P < .01), but not between 1- and 2-year follow-up (Z = −0.96, P = .34). Radiographs of 7/63 patients showed a change exceeding the error of measurement (5°) from 1- to 2-year follow-up (maximum change 7.5°). Curve progression was seen in only 2 patients, the other 5 showed a decrease in curve size. These 7 patients did not differ significantly from the complete cohort on patient characteristics or baseline radiographic measurements. None of the secondary outcome parameters changed significantly beyond the error of measurement, between 1- and 2-year follow-up. Specifically, no change was seen in lumbar curves that were not fused in surgery (lowest instrumented vertebra L2 or higher). Conclusion: No statistically significant change in major Cobb angle was found from 1- to 2-year postsurgical follow-up. Findings of this study are not supportive of routine radiographs 2 years after fusion surgery in AIS patients. This length of follow-up has no added value but does add to the exposure of these young patients to radiation that is potentially harmful. A critical evaluation of the frequency of radiographic follow-up is needed.
P092: Anatomical Characteristics of Vertebral Bodies in Patients With Adolescent Idiopathic Scoliosis Using Hounsfield Unit Values Obtained From Multiplanar Computed Tomography
Masaaki Chazono1
1Utsunomiya National Hospital, Utsunomiya, Tochigi, Japan
Introduction: The etiology of adolescent idiopathic scoliosis (AIS) has been multifactorial including genetic and environmental factors. What happens inside the vertebral body at the apex level in AIS patients? The aim of this study was to evaluate the anatomical characteristics of vertebral bodies (VB) in patients with AIS in terms of Hounsfield unit (HU) values obtained from diagnostic computed tomography (CT) scan. Material and Methods: Forty-one patients (males 5, females 36) of AIS with a mean age of 14 years and a right thoracic curve of Lenke type 1 or 2 were included in this study. The mean thoracic Cobb angle was 26.8° (10-50) at the initial visit (S-group). In contrast, 21 control subjects (males 17, females 4) with a mean age of 14 years who had undergone chest and abdominal CT examinations (N-group). Axial CT images of the largest pedicle diameters were selected from T1 to L5. The mean HU value of each VB was calculated after 3 square ROIs (region of interests; 1 × 1 cm) were selected in the right (convex) side and left (concave) side of each VB. The average HU values of VB were compared between the S-group and the N-group with regard to the right-left side and each spine level. In addition, linear regression analysis was performed to examine the degree of correlation between the HU values of the periapex VB and age, BMI (body mass index), and Cobb angle. Results: The smallest and the largest mean HU value was 244 HU at T7 and 303 HU at T1 in the S-group, 231 HU at L4 and 295 HU at T1 in the N-group, respectively. The mean HU values of the left side on the periapex VB in the S-group were significantly greater than those of the right side at T7-T9 (264 HU vs 234 HU). However, there was no significant difference between the right and the left side in the N-group at all spine level. Furthermore, the correlation coefficient was 0.51 between the Cobb angle and the difference between the left-right HU values at the periapex VB. Conclusion: The present study indicates that the difference between the left-right HU values at the periapex VB is a significant predictive indicator for curve progression in patients with AIS. The overgrowth of VB on the concave side and/or secondary mechanical loading, often referred to as the “Hueter-Volkmann Law,” may influence the onset and AIS curve progression.
P093: Axial Rotation Pattern May Define the Sagittal Alignment in Adolescent Idiopathic Scoliosis Patients: A Case-Control Study
Hongda Bao1, Zhen Liu1, Xu Sun1, Jun Jiang1, Saihu Mao1, Bangping Qian1, Bin Wang1, Yang Yu1, Zezhang Zhu1, and Yong Qiu1
1 Drum Town Hospital, Nanjing University, Nanjing, China
Introduction: A recent study based on 3-dimensional (3D) analysis revealed that increasing severity of coronal curvature is associated with a progressive loss of 3D thoracic kyphosis in adolescent idiopathic scoliosis (AIS). The aim of this study is to investigate the relationship between axial rotation pattern and sagittal alignment in AIS patients. The relationship between axial rotation and sagittal alignment has not been identified in thoracic AIS patients. This study revealed that the mean thoracic rotation in hypokyphosis, AIS, and the direction of the thoracic and lumbar curve rotation should be evaluated in the preoperative surgical planning. Material and Methods: This study prospectively enrolled a series of Lenke type 1A female AIS patients. Hypokyphotic patients (thoracic kyphosis [TK] <10°, DTK) and patients with normal TK (TK >20°, NTK) were matched by major Cobb angle, apex, Risser grade, and Lenke classification. The biplanar full-spine images were taken before and 3 weeks after surgery, and the curvature was reconstructed with dedicated software. Axial rotation parameters were obtained from reconstruction, including mean vertebral rotation of the major thoracic curve (MTR), mean vertebral rotation of the proximal thoracic curve (PTR), and mean vertebral rotation of the lumbar curve (LR). The paired t test was performed between the normal TK group and the hypokyphotic group. Results: A total of 24 patients (12 pairs) were included (mean age = 13.7 years) with baseline Cobb angle of 52.4°. The mean preoperative TK of NTK groups was 28.2°, while in DTK group was 11.2°. There was a significant difference in the average vertebral rotation of the major thoracic curve between the 2 groups. The MTR of NTK group was significantly smaller than that of DTK group (10.2° vs 12.7°, P < .001), and there was a significant correlation between TK and MTR (r = .30, P = .03). As for the lumbar curve rotation, the LR of the NTK group was significantly smaller than the DTK group (P = .002), but the absolute value of the 2 groups was similar (P = .31). The lumbar Cobb angle correction rate was significantly greater in patients with thoracic and lumbar curve rotating in the same direction than that in the opposite direction (81.1% vs 61.9%, P = .005). Conclusion: After matching the coronal deformity, the MTR of the hypokyphotic patients was significantly larger. The direction of the thoracic and lumbar curve rotation was also required to be well concerned in the preoperative surgical planning.
P094: Comparative Analysis of Treatment Results of Patients With Congenital Spinal Deformity Secondary to Hemivertebrae: Systematic Review
Egor Filatov1, Sergey Ryabykh1, and Dmitriy Savin1
1Ilizarov Center, Kurgan, Russian Federation
Introduction: Retrospective analysis of treatment results of patients with congenital spinal deformity secondary to hemivertebrae with a comparison group formed on the basis of literature data. Purpose of the Study: To analyze the results of surgical correction of hemivertebrae in children. Material and Methods: A total of 1055 patients with a spinal deformity secondary to hemivertebrae, among them 937 on the basis of 36 publications in the past 15 years and 118 patients of the Ilizarov Center treated in 2010 to 2018. All patients underwent extirpation of the hemivertebrae and posterior instrumentation. Depending on the variant of approach for extirpation of hemivertebrae, patients were divided into 3 groups: I—combined; II—dorsal; III—pedicular. Results: In group I, the average age of 203 patients was 59.6 ± 14.9 months. Scoliosis before surgery was on average of 38.3 ± 2.8°, correction was 70.5%. Kyphosis before surgery was 23.3 ± 6.0°; correction 76.8%. Blood loss 504 ± 210.1 mL. Operation time 284.4 ± 35.7 minutes. Complications were wound infection 6, implant-dependent complications 4, neurological complications 1, progress of deformity 13, and other 10. In group II, the average age of 734 patients was 93.2 ± 9.7 months. Scoliosis before surgery was 41.2 ± 1.5°, correction 68.9%. Kyphosis before surgery was 30.5 ± 2.5°; correction 66.9%. Blood loss 512.5 ± 70.9 mL. Operation time 227.6 ± 11.1 minutes. Complications were wound infection 17, implant-dependent complications 28, neurological complications 15, progress of deformity 18, and other 3. In the group III, the average age of 118 patients was 84.7 ± 5.1 months. Scoliosis before surgery was 36.1 ± 1.2°, correction 78.1%. Kyphosis before surgery was 47.4 ± 4.4°; correction 83.8%. Blood loss 389.0 ± 30.9 mL. Operation time 224.3 ± 9.5 minutes. Complications were wound infection 1, implant-dependent complications 6, neurological complications 6, progress of deformity 9, and other 1. Discussion: Correction of the scoliotic deformity in all groups is identical (P ≥ .05). Correction of the kyphotic deformity is significantly better in group III at P ≤ 0.002. The volume of blood loss is significantly lower when performing pedicle extirpation than in other groups: by 123.4 ± 72.3 mL dorsal approach (P = .017) and 115.4 ± 212.3 mL combined approach (P = .611). The operation time in groups 2 and 3 is the same, compared with the combined method—the difference on average is 60 minutes (P ≥ 0.1). There are statistically insignificant differences with combined access; however, we note the high variability of this parameter in the analyzed sample, as it is impossible to obtain an adequate comparison group due to sharp reduction of hemivertebrectomies by combined approach over the past 15 years. The number of postoperative complications in the groups is comparable with each other. The choice of the method of extirpation of the hemivertebra at this stage of development of surgery is at the discretion of the surgeon, while the pedicular approach for extirpation of the hemivertebra has a number of advantages.
P095: Magnetically Controlled Growth Rods: A Single-Center, Single Surgeon Experience of 18 Consecutive Patients
Saurabh Kapoor1, Olakunle Badmus1, Sarang Sapare1, and Darko Stipic1
1Queen’s Medical Center, Nottingham, UK
Introduction: To evaluate the outcome of 18 consecutive patients treated with magnetically controlled growing rods (MCGR) over a 6-year period in a single center. Methods: We implanted MCGR in 18 patients with skeletally immature spines with the goal of achieving trunk growth and maintaining correction while avoiding repeated surgeries. Clinic letters and radiographs were scrutinized for patient demographics, truncal growth, curve correction, complications, planned, and unplanned return to theaters. Results: The study included 8 males and 10 female patients with an average age of 7.2 years at the time of surgery. Diagnosis included idiopathic (N = 5), syndromic (N = 5), neuromuscular (N = 6), and congenital (N = 2) scoliosis. Twelve out of 18 patients had a follow-up of at least 12 months allowing meaningful calculation of Cobb’s correction and truncal heights. The average Cobb’s angle for main thoracic curve improved from 45° to 22° postoperatively and 23° at the latest follow-up. The corresponding values for proximal thoracic curve and lumbar curves were 33°, 20°, 35°, and 34°, 17° 15°, respectively. The average preoperative T1-12 height improved from 186 mm to 201 mm immediate postoperatively and was 226 mm at the last follow-up. This shows average immediate postoperative increase in T1-12 height of 14 mm and 39 mm at last follow-up. The average follow-up period was 39 (12-69) months. The average blood loss was 165 mL (50-400) and average length of hospital stay was 10 days (6-24). Three patients (17%) had unplanned returned to theater including 1 rod breakage and 2 proximal screw pullouts. Two (67%) out of 3 had single growing rod of 4.5 mm diameter. Two patients reached end of distraction out of which one was implanted with a new set of rods electively. Two patients were converted to definitive fusion at an average of 46 months after index procedure. Because of the controversy over raised metal ions in these patients, we have recently started measuring these, and so far in our measurements, this has not been proven. Conclusion: MCGR provide reliable correction of deformity and longitudinal truncal growth. Single rod and smaller 4.5-mm rods increases the risk of unplanned return to theater.
P096: Radiation Exposure in Young Patients Undergoing Scoliosis Surgery
Saurabh Kapoor1, Corrado Lucantoni1, Wai Weng Yoon1, Nasir Quraishi1, Michael Grevitt1, and Phillip Sell1
1Queen’s Medical Center, Nottingham, UK
Purpose: Audit the frequency and role of postoperative radiographs following surgery for adolescent idiopathic scoliosis. Methods: Retrospective review of 91 consecutive patients treated surgically for AIS (age = 10-18 years) from 2011 to 2016. Seven were excluded, 1 was pregnant, 3 had a research implant with a set radiographic protocol, and 3 were lost to follow-up. The context of postoperative radiation exposure and clinical records were assessed in 84 patients with a minimum 2-year follow-up. Results: Seventy (83%) patients out of 84 had an uneventful clinical course. That is, no complaints of increasing back pain, deterioration in body image, or new neurological symptoms. Average age at surgery was 14.6 years and 17 years at last radiological examination. There were 8 radiographs (5-11 taken) on an average before clinic discharge. None of these altered clinical management. There was no standardized protocol for postoperative radiographs within or between different surgeons. Fourteen (17%) patients had clinically important adverse events. These included 9 patients with worsening pain. In 2 patients, it was attributed to screw malposition. Distal add on in 3, screw-rod disengagement in 1, infection in 2, and proximal junctional kyphosis (PJK) in 1. Two patients presented with symptom of worsening cosmesis, due to PJK in 1 and distal add on in another. Two presented with new neurology caused by malposition of a T5 screw in one, and a T4 pedicle fracture causing PJF in another. One case with a malpositioned T7 screw in possible contact with the aorta was revised after being detected on radiographs. This was the only case where an X-ray alone influenced management. Overall radiographs assisted in 10 of the 14 cases with a symptomatic presentation. In 2 cases of infection, MRI (magnetic resonance imaging) proved more useful than radiographs. The 2 cases of malpositioned screw radiographs missed the findings initially. Conclusion: Routine postoperative radiographs can and should be minimized in patients with an uneventful clinical course. Vigilance and review of the immediate imaging is essential, and early subsequent imaging should be reserved for clinically symptomatic patients.
P097: Early Outcome of Staged Posterior Surgery for Rigid Scoliosis
Mohamed Fawzy Khattab1, Sherief El-Ghamry1, and Youssry El-Hawary1
1Orthopedic And Spine, Cairo, Egypt
Introduction: No standardized surgical technique for severe rigid scoliosis management with few reports on the use of perioperative halo-gravity traction in treating severe rigid scoliosis. A retrospective study. To evaluate safety and efficacy of staged posterior surgery of severe rigid scoliosis correction. First stage is posterior facetal osteotomies and pedicular screw fixation. Second stage is halo-gravity traction for 3 weeks. Third stage is final correction maneuver techniques with rods application. Materials and Methods: Ten patients with a minimum 1-year follow-up who underwent 3-stage correction techniques for severe rigid scoliosis (Cobb angle above 100°) were analyzed (First stage: posterior facetal osteotomies and pedicular screws application. Second stage: halo-gravity traction for 3 weeks. Third stage: definite correction techniques doing multiple chevron osteotomies, apical sublaminar wires if needed, and rods application with derotation, compression distraction techniques). Patients demography age at date of examination (range = 11-28 years; mean = 15.6 years), sex (6 females, 4 males), major coronal curve magnitude (range = 106-148°; average = 123°), and major sagittal curve magnitude (range = 70-110°; average = 90°). Complications related to the procedures were reviewed. Results: Radiographic outcomes showed Cobb angle improvement of 29% after halo traction, and it measured 55° (range = 43-85°) at the last follow-up, for a 58% correction. Kyphosis improved to 59° (range = 42-74°) at last follow-up. T1-S1 increased by about 88 mm. There were no permanent neurological deficits in this series. Conclusions: Treatment of severe rigid scoliosis is very challenging. With modern instrumentation methods, posterior-only staged surgeries with Halo-gravity traction is a safe, tolerated method of applying gradual, traction to maximize final correction. There were no permanent neurologic deficits in this series.

P098: Removal of a Urinary Catheter Prior to Discontinuation of Epidural Analgesia is Associated With an Increased Risk of Postoperative Urinary Retention and Hospital Episode Costs in Patients Undergoing Surgical Correction for Adolescent Idiopathic Scoliosis
Assem Sultan1, Ryan Berger1, William Cantrell1, Linsen Samuel1, Erin Ohliger1, Joshua Golubovsky1, Salam Bachour1, Selena Pasadyn1, Jaret Karnuta1, Pierre Tamer1, Phuc Le1, Thomas Kuivila1, David Gurd2, and Ryan Goodwin1
1Cleveland Clinic, Cleveland, OH, United States
Introduction: Epidural analgesia (EA) has been widely utilized as part of a multimodal regimen for postoperative pain control in adolescent idiopathic scoliosis (AIS) patients undergoing posterior spinal instrumented fusion (PSIF). In these patients, removing the indwelling Foley catheter, inserted for intraoperative monitoring of urine output, is indicated in the early postoperative period. However, controversy exists as to whether the Foley catheter should be removed before or after the EA has been discontinued. Early removal may decrease the incidence of urinary tract infections, while removal after discontinuation of the EA may avoid urinary retention (UR) and recatheterization. Therefore, the purpose of this study was to answer the following questions: (1) Is there a difference in UR rates among patients who had early (before discontinuation of EA) versus late (after discontinuation of EA) removal of their indwelling Foley catheters? (2) Does early versus late Foley catheter removal carry an independent risk for UR and recatheterization? and (3) Is there an incurred cost? Methods: We evaluated prospectively collected data from a single-institution, longitudinally maintained database of pediatric scoliosis patients. The database query returned 703 patients. To identify the study cohort, the following inclusion criteria were applied: (1) patients between 10 to 25 years of age, (2) who were diagnosed with adolescent idiopathic scoliosis, (3) who underwent PSIF, and (4) who received EA delivered by epidural catheter insertion during surgery. All patients received hydromorphone alone as their EA. Additionally, the following exclusion criteria were applied: (1) patients with neuromuscular, congenital, and juvenile scoliosis, (2) AIS patients outside the age range, (3) AIS patients who did not receive EA using inserted epidural catheters, and (4) patients with AIS who met the inclusion criteria but suffered a neurological sequelae following the surgery. This yielded a study cohort of 297 patients who were included in our final analysis. Patient characteristics and the order and timing of removing the urinary and epidural catheters were collected. Rates of UR were statistically compared in patients who had early versus late urinary catheter removal. A univariate and multivariate regression analysis was conducted to identify independent risk factors for UR development. Results: Patients who had early (n = 66, 22%) versus late (n = 231,78%) urinary catheter removal had a significantly higher incidence of UR requiring recatheterization (15 vs 64.7%, P = .007). Patient with early removal were almost 4 times more likely to develop UR requiring recatheterization (odds ratio [OR] = 3.8, 95% confidence interval [CI] = 1.5-9.7, P = .005). UR incurred additional costs averaging $15 000/patient (P = .204). Conclusion: In patients who had PSIF for AIS, removal of a urinary catheter before discontinuation of EA is an independent risk factor for postoperative urinary retention requiring recatheterization and may be associated with an additional hospital episode cost potentially related to the treatment of urinary retention in this pediatric population. In our experience, these patients required more medical consultations, multiple bladder ultrasound scans, and at times, insertion of the catheter under general anesthesia. This may be particularly relevant to clinical practice guidelines and care pathways.
P099: A Novel Method for the Measurement of the Apical Vertebral Rotation Angle Using 2-Dimensional Radiographs in Scoliosis Cases
Yupeng Zhang1, Xing Wei2, Yamin Shi1, Zhaopin Duan3, and Tujun Weng1
1The First Affiliated Hospital of PLA General Hospital, Beijing, China
2Aerospace Central Hospital, Beijing, China
3Zhongyi Hospital of Zhongmou County, Zhengzhou, China
Introduction: Adolescent idiopathic scoliosis (AIS) is a 3-dimensional spinal deformity. There has been increasing emphasis on the apical vertebrae rotation (AVR) angle these years. Despite computed tomography (CT) scan and magnetic resonance imaging (MRI) having high accuracy in evaluating the AVR, they have some limitations in the radiation exposure and cost. Consequently, quantification of AVR with 2D (2-dimensional) radiographs is significant. Many methods have been developed to meet the requirement; however, most of them have limitations for their requirements of some hardware, software, or complex mathematical formulae. We have developed a novel method to solve the problem based on the theory of solid geometry. Material and Methods: A set of CT data from T1 to L5 level (17 vertebrae, normal group) were collected from a healthy candidate, and then imported into the reverse engineering software. For each vertebrae, a virtual sphere was attached to the tip of the spinous process as a marker so as for the accuracy and visibility on the posteroanterior (PA) and lateral radiographs (when performed in patients, a steel ball can be attached on the skin close to the tip of the spinous process as a clear marker). After initialization, each vertebrae was rotated from 0° to 45°every 5° Accordingly, virtual X-ray was performed to obtain the PA and lateral radiographs every 5° (ie, 5°, 10°,…, 45°). A vertical line was drawn from the center of the vertebrae body, and the horizontal distance (d1) from the center of the virtual sphere to the line above was measured on PA view. In same way, another horizontal distance (d2) was measured on lateral view. A right triangle was then drawn, with the length of the 2 legs were d1 and d2. The opposite angle of the leg with the length d1 was measured. This angle was the predicted AVR, which was compared with the actual AVR, and then the error was calculated. The CT data of 9 AIS cases were imported into the software. There were 10 apical vertebrae in total (scoliosis group). For each apical vertebrae, the error was obtained in the same way as above. Then the errors were compared with that of the normal group with student t test. The Pearson correlation coefficient between the actual and predicted AVR was calculated. Results: The measurement error of the normal group ranged from −2.9° to 2.6°, with an average of −0.4 ± 1.0°. The error of the scoliosis group ranged from −3.0 to 1.8°, with an average of −0.6 ± 1.1°. The difference between errors of the 2 groups was not significant (P = .1104). The Pearson correlation coefficient of the normal group was 0.997 (P < .01), and that of the scoliosis group was also 0.997 (P < .01). Conclusion: This novel method is accurate, simple, and easy to use to quantitatively evaluate the AVR of scoliosis. The measurement may be finished in a few seconds by surgeons.
P100: Special Considerations in Patients With Hydrocephalus and Early-Onset Scoliosis
Fernando Alvarado-Gomez1, Kemel Gothme Gothme1, Jorge Uribe1, Jose Dangond Milla1, Yuli Fuentes-Barreiro1, and Kenny Lopez-Gomez1
1Hospital Universitario Fundacion Santa Fe de Bogota, Bogota, Colombia
Introduction: One of the most common causes of malfunction of the ventriculoperitoneal shunt (VPS) is due to mechanical failure secondary to migration, obstruction, or catheter disconnection. An uncommon cause least reported are those surgical procedures that intervene with the position of the VPS system such as growing systems for early onset of scoliosis, in patients who usually have spinal dysraphisms and hydrocephalus that may require the use of both systems simultaneously. Material and Methods: A 9-year-old female with lumbar spina bifida, tethered cord, thoracic syrinx, and Arnold Chiari II with secondary hydrocephalus required VPS system, additionally had a neuromuscular early-onset scoliosis and kyphosis. A growing system with 2 rods was applied and 4 months postoperatively, disconnection of the VPS catheter is documented. A search of the literature was carried out using the PubMed database with the following strategy: (“Scoliosis”[Mesh] AND “Hydrocephalus”[Mesh]) AND “Ventriculoperitoneal Shunt”[Mesh]. Results: The illustration of this case shows one of the many causes of failure of the VPS system. In this particular case, it is shown how in patients with neuromuscular scoliosis of early onset that require the use of growing rods, which to our knowledge is very rare and poorly described in the literature. It is of utmost importance that in cases that need both the VPS and growing systems, the surgeons most prevent that one interfere with the other since the elongation of the rods may cause the disconnection of the VPS catheter. Conclusion: Mechanical failure of the VPS systems may be associated with improper assessment of it when instrumentation with growing systems of the spine is necessary. Correct analysis of the previous systems installed in images communication between spinal surgeons and neurosurgeons and clinical follow-up looking for signs of VPS dysfunction are pivotal in preventing and diagnosing such complications.
P101: Fusionless Posterior Technique for the Treatment of Neuromuscular Scoliosis in the Pediatric Population: A Case Series
Panagiotis Krallis1, Anastasia Pilichou1, Georgia Antoniou1, Fragiskos Angelis1, and John Anastasopoulos1
1Agia Sofia General Children’s Hospital, Athens, Greece
Introduction: The treatment of neuromuscular scoliosis has solemnly depended on techniques of posterior fusion. With numerous complications being described in literature and a variety of instrumentation in the hands of orthopedic surgeons, the purpose of this report is to illustrate the results of a Fusionless Posterior Technique (FPT) based on the concept described by Dr Miladi of Necker-Enfants Malades Hospital in Paris. Material and Methods: Within the past 3 years, 25 patients with scoliosis were operated at “Agia Sofia” General Children’s Hospital, Athens, out of which 17 have a follow-up of 2 years. With a mean age of 12.6 years (range = 8-16.5 years), our patients were diagnosed with cerebral palsy (6), spinal cord atrophy (4), congenital muscular dystrophy (2), arthrogryposes (2), Rett syndrome (1), Dravet syndrome (1), and Freidreich syndrome (1). The technique used is following the concept of “Growing Rods” adapted for neuromuscular scoliosis and is composed of 2 telescopic rods cephalically based on 4 hooks on either side, forming 2 claws and a distal pelvic fixation provided by 2 ilio-sacral screws. Two-way ANOVA test was used to analyze the data. Minimum follow-up time is 1.5 years. Results: Through the FPT, we have managed to postoperatively reduce the Cobb angle (mean = 83.6° to 42.2°, P < .001), the apical vertebral translation (mean = 78 to 42.6 mm), and the trunk balance (mean = 38.5 to 25 mm, P = .0001). On the sagittal plane, the improvements calculated were of kyphosis (mean = 59° to 18.5°, P = .0006), lumbar lordosis (mean = −46.5° to −32.5°), and sagittal balance (mean = 20.8 to −5.7 mm). The mean operative time was 200 minutes, and blood transfusion was not necessary during the process. Distraction was performed in 5 patients approximately 8 months after FPT due to trunk lengthening or increased Cobb angle by 10°. Conclusion: Based on our 3-year experience with FPT, we feel confident that this is an effective method to address neuromuscular scoliosis in the pediatric population. Our technique applied on the appropriate timing is reliable, quick, and safe, providing the ability to lengthen the spine as our patients grow. Future follow-up will reveal possible difficulties and improvements of FPT with current results being extremely promising.
P102: Surgeon-Directed Monitoring in Pediatric Spinal Correction Surgery: Visual Observation of Lower Limb Waveform Predicts Intact Neurological Function
Andrea Chan1, Purnajyoti Banerjee1, Nasiur Rehman1, Cristina Lupu1, Tim Bishop1, Jason Bernard1, and Darren Lui1
1St. George’s Hospital, London, UK
Introduction: Surgeon-directed monitoring (SDM) of transcranial motor–evoked potentials (TcMEP) is valuable in spinal cord monitoring. This article advocates that maintenance of visually observed lower-limb (LL) waveforms indicate intact spinal cord function, while waveform disappearance predicts potential motor deficit. Gold standard 80% amplitude reduction was investigated. Material and Methods: Surgeon-directed NIM-Eclipse MEP monitoring equipment was utilized in 142 scoliosis correction surgeries (2012-2017). Cases included 120 AIS, 9 syndromic scoliosis, 9 neuromuscular scoliosis, 2 Scheuermann’s kyphosis, and 2 high-grade lumbar spondylolisthesis. Mean age was 13.9 years (range = 5-17 years), male–female = 28:114. Potential deficit warning was persistent disappearance of LL-waveforms from the monitoring screen. Amplitude data was analyzed to numerically quantify LL-MEP reduction equivalent to signal disappearance. Results: Mean neuromonitoring duration was 302.5 minutes (SD = 105.7 minutes) averaging 20 stimulations per case. Three cases had complete visual loss of LL signals that did not resolve with restimulation, anesthetic stabilization, or reversed surgical maneuver, and required staged surgery. No neurological dysfunction on waking was recorded. Staged cases with persistent signal loss had up to >95% reduction in LL-MEP amplitude. Signal “disappearance” was quantitively up to 95% reduction, due to background electrical noise. Greater than 98% amplitude criterion did not correlate with disappearance cases, produced false negative results. Conclusion: Success of the disappearance criteria suggests gold standard >80% amplitude criterion too sensitive. A safe and appropriately sensitive amplitude criterion is likely between 80% and 95%. SDM of visual LL-waveform maintenance is a safe method of MEP monitoring superior to literature standard >80% criterion. It is a cost effective alternative to neurophysiology directed neuromonitoring.
P103: Increased Prevalence of Idiopathic-Like Scoliosis in Patients Treated for Childhood Hematopoietic Malignancy
Francis C. J. Sim1, Peter Loughenbury1, Almas Khan1, and Peter Millner1
1Leeds General Infirmary, Leeds, UK
Introduction: Idiopathic scoliosis is a spinal curvature with no identifiable cause. The prevalence of curves with a Cobb angle >10° ranges from 0.5 to 3 per 100 children and adolescents in the United States.1 In the United Kingdom, the prevalence of idiopathic scoliosis ranges from 0.1% in 6- to 8-year-olds, 0.3% in 9- to 11-year-olds, and 1.2% in 12- to 14-year-olds.2-5 More severe curves are less common, with a prevalence of 0.04% to 0.3% in curves of 40° or more.6,7 There is no literature that identifies an increased risk of idiopathic-like scoliosis in patients who have had childhood hematopoietic malignancy; however, we perceived an unexpectedly higher number of these patients being referred to our spinal deformity service. Material and Methods: Patients with a history of lymphoma and leukaemia, with a current age of 12 to 26 years, were identified from the regional pediatric oncology database. The casenotes and radiographic studies were reviewed and any spinal deformity characterized. Treatment of the malignancy and the spinal deformity, if any, was noted. Results: From a cohort of 346 patients, 19 (5.5%) had radiographic evidence of scoliosis (defined as a Cobb angle >10°). Five patients (1.4% of total cohort) had a Cobb angle of 40° or more, all of whom had corrective surgery. All the patients with scoliosis had no other pathology as an attributable cause of their deformity and all had been treated with high-dose steroids for leukemia (either acute or chronic myeloid or acute lymphoblastic). Conclusion: There is an increased prevalence of idiopathic-like scoliosis and larger curves (Cobb angle >40°) associated with childhood leukemia and lymphoma. Causative factors may relate to the underlying disease process and/or the treatment of the condition.
P104: Efficacy of Halo-Gravity Traction in the Management of Severe Rigid Spinal Deformities: A Prospective Analysis of 26 Patients
Shanmuganathan Rajasekaran1, Ajoy Prasad Shetty1, Rishi Mugesh Kanna1, and Dilip Chand Raja1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: The clinical appearance of a spinal deformity depends on curve magnitude, truncal shift (TS), coronal imbalance (CI), shoulder height difference (SHD), and sagittal profile. Halo-gravity traction (HGT) improves all these components of deformity and thus restores overall balance. Acute correction of severe rigid curves requires multiple osteotomies. These malnourished patients have poor cardiopulmonary reserve and major procedures carry high morbidity complications. HGT obtains around 15% to 30% correction in scoliosis and 17% to 35% in kyphosis. There are limited studies on the pan spinal effects of homogenous HGT. Materials and Methods: Patients with primary curve Cobb angle >120° or sum of Cobb angle >150° underwent preoperative HGT. Radiographic parameters analyzed were Cobb angles of curves—major scoliosis (MSCA), compensatory (CSCA 1 and 2), and kyphosis (MKCA)—Flexibility Index, costo iliac impingement (CILD), SHD, and sagittal profile. Pulmonary function was assessed by respiratory rate (RR), breath-holding count (BC), and pulmonary function testing. Results: Fourteen males and 12 females with mean age of 18.5 years were studied. The mean weight and height gained were 3.6 kg and 4.4 cm, respectively. The correction efficacy of homogenous HGT in MSCA, CSCA1, and CSCA2 were 15.6, 13.3, and 18.7%, respectively. Significant improvements were noted in MKCA, CILD, CI, and TS. Mean SHD improved from 2 to 1.1 cm. Mean FVC (forced vital capacity) improved from 43.3% to 48.5% and FEV1 (forced expiratory volume in 1 second) from 37.1% to 41.9%. Similar improvements were noted in RR and BC. There were no instances of neurological worsening or failure of instrumentation. Five complications included 2 dural tears, 1 pin tract infection, 1 pleural tear, and 1 wound dehiscence. Conclusion: HGT, safely and effectively increases the flexibility of major curves as well as compensatory curves in severe rigid spinal deformities. It improves the overall balance of the patient by reducing the TS, CI, and SHD. It also provides adequate time to optimize the patient for major surgical undertaking and minimizes complications.
P105: Long-Term Outcome of Selective Thoracic Fusion Using Both Rod Derotation and Direct Vertebral Rotation in the Treatment of Thoracic Idiopathic Scoliosis
Dong-Gune Chang1, Jin-Hyok Kim2, Se-Il Suk1, Ki-Youl Nam1, Kang-Un Kim1, Jae Hyuk Yang3, Seung-Woo Suh3, Kwang-Sup Song4, Jong-Beom Park5, and Jung-Hee Lee6
1Inje University Sanggye Paik Hospital, Seoul, Republic of Korea
2CM Hospital, Seoul, Republic of Korea
3Korea University Guro-Hospital, Seoul, Republic of Korea
4Chung-Ang University Hospital, Seoul, Republic of Korea
5Uijeongbu St Mary’s Hospital, Uijeongbu, Republic of Korea
6Kyung Hee University Hospital, Seoul, Republic of Korea
Introduction: The goal of surgical treatment of adolescent idiopathic scoliosis (AIS) is to achieve deformity correction, trunk balance, and preservation of motion segments. Postoperative compensation and maintenance of the unfused lumbar curve after selective thoracic fusion (STF) is very important factor for the satisfactory results in the treatment of thoracic AIS. Materials and Methods: Sixty-five patients with thoracic AIS treated with STF from the neutral vertebra (NV) to NV or NV-1 with rod derotation (RD) and direct vertebral rotation (DVR) were retrospectively analyzed with a minimum 10-year follow-up. Patients were divided into 2 groups: satisfactory (n = 52) and unsatisfactory groups (n = 13). Unsatisfactory results were defined as an adding-on, a lowest instrumented vertebra (LIV) tilt of more than 10°, or coronal balance greater than 15 mm. Results: No significant differences were observed in the main thoracic curve between the satisfactory and unsatisfactory groups postoperatively (P = .218) and at the last follow-up (P = .636). Significant improvements of LIV tilt and disc angle were observed in both groups, but these improvements deteriorated during the follow-up period in the unsatisfactory group. Significant differences of apical vertebra (AV) and end vertebra (EV) were observed postoperatively (AV: P = .001, EV: P = .001) and at the last follow-up (AV: P < .000, EV: P < .000) between the 2 groups. Conclusions: STF using RD and DVR can achieve satisfactory deformity correction for thoracic AIS with satisfactory compensatory lumbar curve that was maintained over long-term follow-up. Progression of unfused lumbar curve closely related with LIV tilt and disc angle showing insufficient DVR. Therefore, STF with sufficient DVR is required to achieve satisfactory deformity correction and prevent a distal adding-on phenomenon in the treatment of thoracic.
P106: Rib Hook Versus Pedicle Screw as Proximal Anchor in Distraction-Based Growth Rod Technique for Early-Onset Scoliosis
Shanmuganathan Rajasekaran1, Nikhil K. V.1, Ajoy Prasad Shetty1, and Rishi Mugesh Kanna1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Traditional and hybrid growth rods are still commonly used for early-onset scoliosis (EOS) due to high cost of magnetically controlled growth rods. Curve correction and complications in growth rod technique (GRT) is influenced by the choice of proximal anchor. Pedicle screws or rib hooks is used as proximal anchor in these technique. The outcome and complications between these 2 proximal anchors is still unclear. The outcome and complications between pedicle screw and rib hook as proximal anchor in GRT for EOS is compared in this study. Materials and Methods: All children with EOS treated with GRT at a single center with minimum of 2 years of follow-up were included and grouped into standard group (SG) and hybrid group (HG) based on use of pedicle screw or rib hook, respectively, as proximal anchors. Fusion was not done at anchor sites. Medical records and radiographs of patients were evaluated for curve correction, T1-S1 length, space available for lung ratio (SAL), and complications. Results: A total of 28 patients (SG =13; HG = 15) were included in the study. The mean age, sex, Cobb’s angle, T1-S1 length, and SAL were comparable in both groups. The mean scoliosis Cobb’s angle improved in SG from 72.4° to 44.2° and in HG from 70.8° to 51.6° (P = .67), T1-S1 improved from 24.19 to 31.87 in SG and 26.21 to 31.03 in HG (P = .55) with no statistical difference between both groups. Fifteen (SG: n = 7, HG: n = 8) complications were noted in 14 patients (3 screw pull-out, 5 hook dislodgement, 6 curve decompensation, and 1 infection) with similar complication rates between both groups (P = .461). Twelve (SG = 4, HG = 8) surgeries were unplanned, which included 5 hook revisions (HG = 5), 3 screw revisions (SG = 2, HG = 1), and 4 implant removal (SG = 2, HG = 2). Conclusion: There are no statistical differences in radiological outcome and complications between GRT using either pedicle screw or rib hook as proximal anchor. However, in patients with thin or anomalous pedicles and upper thoracic curves, use of rib hooks is preferred and pedicle screws can be used as salvage technique.
P107: Thoracic Inlet Measurements as a Predictor of Pulmonary Dysfunction With Varying Curve Magnitude and Thoracic Cage Parameters in Thoracic Kyphoscoliotic Deformities
Shanmuganathan Rajasekaran1, Vyom Sharma1, Ajoy Prasad Shetty1, and Rishi Mugesh Kanna1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Kyphoscoliotic thoracic curves cause secondary effects and complications like significant pulmonary dysfunction and reduction in thoracic cage volumes. This study aims to analyze the effects of varying curve magnitude on thoracic inlet dimensions and pulmonary dysfunction. Material and Methods: Eighty patients were included in this prospective study over 1 year excluding patients <8 years, congenital heart or lung disease, curve <30°, and lumbar curves. Patients were divided into 3 groups based on Cobb’s angle 31° to 50°, 51° to 80°, and greater than 80°. Thoracic inlet dimensions were measured in MRI at the level of manubrium (TII A) and innominate crossing (TII I) in all patients and in 20 age-matched controls. Pulmonary function was recorded with spirometry (pulmonary function test [PFT]) and measurement of transverse thoracic diameter, hemithorax height, rib apex distance, and number of vertebrae recorded on chest radiograph. Results: The mean age was 14.91 years (range = 8-3, SD = 4.4) with 56 (70%) female patients and 24 (30%) male patients. The most common etiology was congenital scoliosis in 34 (42.5%) patients, 32 (42.5%) with AIS, and 8 (10%) with neurofibromatosis. The mean Cobb’s angle was 69.8° (SD = 14.96, standard error [SE] = 1.67), maximum of 114.8°. The mean TII A for all the patients was 3.72 (1.84 – 7.35 + 0.91, SE = 0.10) and TII I was 3.27 (2.50 – 6.39 + 1.64, SE = 0.18), maximum TII A was 7.35 in group 3 and minimum being 1.84 in group 1. In control group, mean age was 12.94 years (SD = 2.24 years), TII A was 3.23 (SD = 0.43, SE = 0.09), and TII I was 3.39 (SD = 0.52, SE = 0.11). The highest TII A obtained in age-matched control was 4.00 and TII I of 4.71. The mean forced expiratory volume in 1 second (FEV1) of the cohort was 70.5 (SD = 11.1, SE = 1.24), forced vital capacity (FVC) was 67.1 (SD = 11.23, SE = 1.25), and mean FEV1/FVC of 1.05 (SD = 0.03, SE = 0.004). There was moderate restrictive pulmonary dysfunction in group 3, which was statistically significant in congenital scoliosis patients (P < .001) as compared with mild impairment in group 2 (Cobb’s angle = 51° to 80°) that was not statistically significant. Moderate to severe respiratory dysfunction was observed in TII I greater than 5.6 in group 3 curves, associated with thoracic hypokyphosis. Curve apex between T1 and T4 had a significant correlation with worsening PFT and curve angle. Transverse thoracic diameter, height of hemithorax, rib-apex distance and number of vertebrae were weakly correlated with PFT. Conclusion: TII I >5.6 compared with age-matched controls is a strong predictor of pulmonary impairment with worsening curve magnitude more than 80° in proximal thoracic congenital curves with apex between T1 to T4 and T1 to T5 hypokyphosis <10° whereas the probability is weak with height of hemithorax on convex side, rib-apex distance, transverse thoracic diameter, and number of vertebrae in the curve.
P108: Long-Term Impact of Radiation Exposure on Children/Adolescents With Scoliosis: A Systematic Review
Fu-Jun Luan1, Yi Wan2, Dino Samartzis3, and Hai-Qiang Wang4
1Yongchuan Hospital Chongqing Medical University, Chongqing, China
2Fourth Military Medical University, Xi’an, China
3Rush University Medical Center, Chicago, IL, USA
4Shaanxi University of Chinese Medicine, Xi’an, China
5The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
Introduction: For adolescent idiopathic scoliosis (AIS) patients, currently, clinical decisions are based on the severity and progression potential judged by whole-spine radiographs. The natural history of treated and untreated AIS patients is of paramount importance for adolescents in terms of cumulative radiation exposure, cancer risk, and adverse reproduction event issues. Methods: A systematic review was performed, covering PubMed, EMBASE, Web of Science, CINAHL, Scopus, and Cochrane database according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Both MeSH (Medical Subject Heading) terms were used to identify literature, regarding AIS and radiation exposure. Rates of cancer, rates of mortality, rates of productive events, scores of pulmonary function, and physical activity level were the outcome measures. Results: Nine AIS cohort studies with long-term follow-up were identified. In total, 18 863 global AIS patients were studied, mainly including Iowa prospective AIS cohort with 117 untreated cases (studying 50 years), Minneapolis cohort with 976 AIS cases (studying 25.6 years), Denmark retrospective AIS cohort with 205 analyzed cases (studying 24.5 years), US scoliosis cohort with 5 513 analyzed cases (studying 47 years), Ste-Justine AIS cohort with 1292 analyzed women (studying on reproductive events), and Swedish cross-sectional study with 1278 cases (studying longer than 30 years to describe physical activity level). Treated AIS patients in different eras experienced various radiation exposure doses. Cumulative radiation exposure obviously increased the morbidity of cancer, especially breast cancer in women, mortality, and rate of adverse reproduction event. Untreated AIS patients were healthy and functional productive. Conclusions: There is a paucity of evidence regarding the treatment benefits for AIS patients. Importantly, radiation exposure and cancer risks from repeated anterior-posterior projection radiographs should not be neglected.
Funding
The authors are supported by the National Natural Science Foundation of China (Grant Number: 81572182).
P109: The “Beak Sign”: A Predictor of Progressive Thoraco-Lumbar Kyphosis in Pediatric Patients
Saurabh Kapoor1 and Malik Ahmad1
1Queen’s Medical Center, Nottingham, UK
Purpose: All published case series discuss the clinical features and management of differing etiologies, but none talks about the etiology of the progressive kyphotic deformity. We have identified a vertebral “beak-sign” in the radiographs of pediatric patients that subsequently developed progressive thoraco-lumbar kyphosis. Progression is explained by “Heuter-Volkman” law, which governs longitudinal growth of vertebra. Methods: Six pediatric patients with one or more beak vertebrae were prospectively followed-up with serial radiographs and computed tomography scans when indicated. A record was maintained of age at presentation, number of beak vertebrae, and segmental Cobb’s angle across the beak vertebrae at subsequent visits. Results: Patient cohort included 3 with Hurler’s syndrome (mucopolysaccharidoses), 2 with achondroplasia, and 1 with a chromosomal anomaly. Average age at presentation was 5.5 years (range = 4-10 years) with each having at least 1 beak vertebra (range = 1-3). The most common beak vertebra was L1 (5) followed by D12 (2), L2 (1), and D11 (1). The average segmental Cobb’s angle across the beaked vertebrae was 47° (range = 21° to 74°), which increased to 74° (range = 52° to 109°) at last follow-up in untreated cases. This indicates a mean increase of 28° (range = 6° to 53°) over a mean follow-up of 5 years in untreated cases. The average increase in Cobb’s angle per year was 5.5°. Conclusion: We introduce “beak sign” to be a predictor of thoracolumbar kyphosis in pediatric population, irrespective of underlying pathology. Early recognition in predisposed patients should alert the surgeon to possible progression and need for closer follow-up.
P110: Safety of Surgeon-Directed Motor-Evoked Potential Monitoring: A Dual Center Study
Andrea Chan1, Mirza Bišcevic2, Purnajyoti Banerjee1, Babara Smrke3, Nasiur Rehman1, Šejla Bišcevic2, Cristina Lupu1, Ferid Krupic4, Tim Bishop1, Merita Tiric-Campara2, Jason Bernard1, and Darren Lui1
1St. George’s Hospital, London, UK
2Clinical Centre University of Sarajevo, Sarajevo, Bosnia and Herzegovina
3University Medical Center Ljubljana, Ljubljana, Slovenia
4Sahlgrenska Academyat University of Gothenburg, Gothenburg, Sweden
Introduction: Intraoperative neuromonitoring (IONM) is essential in monitoring spinal cord function during spinal deformity correction surgery. However, there is little evidence evaluating surgeon-directed monitoring (SDM). This international study describes the demographics of the combined group of patients who underwent this method of IONM and the outcome of these surgeries. Material and Methods: Surgeon-directed version of NIM-Eclipse monitoring device was used in 204 pediatric scoliosis correction surgeries across our 2 centers. Classification of type of spinal deformity: 167 adolescent idiopathic scoliosis, 9 syndromic scoliosis, 9 neuromuscular scoliosis, 7 Scheuermann’s kyphosis, 2 high-grade spondylolisthesis, 4 Marfan lordoscoliosis, and 6 hemivertebrae. Mean age of patient group was 14.0 years (range = 5-18 years) with male: female ratio = 53:15. Mean preoperative Cobb angle was 62.9° (SD = 19.3°). During surgery, the operating surgeon monitored and interpreted motor-evoked potentials (MEP) for signal changes indicating potential deficit outcome. In such cases, the surgical team attempted to stabilize signals by reducing distractive forces or adjusting of anesthesia intraoperatively. Results: Mean duration of surgery was 282.3 minutes (SD = 107.9 minutes). None of our patients had postoperative neurological deficit. Three cases had persistent loss of lower-limb MEP signals, requiring staged surgery. All other patients had either stable MEPs throughout surgery or experienced temporary decreases in MEPs, which were promptly restored. Conclusion: SDM is a simple and reliable method that predicts motor outcome in pediatric spinal deformity surgeries. Compared with neurophysiologist-led spinal cord monitoring, SDM reduces reliance on staff and lowers cost, without adding to operating time.
P111: Scoliosis Has High Prevalence of Negative Sagittal Balance
James Todd1, Jan Herzog1, Niv Bhamber1, Timothy Bishop1, Jason Bernard1, and Darren Lui1
1London, UK
Introduction: Positive sagittal balance is linked to increased pain and social difficulty due to reduced ability to maintain horizontal gaze. The impact of negative sagittal balance is less well understood. AIS is known to be hypo-kyphotic and is well recognized by Stagnara to have a thoracic lordosis. The importance of negative sagittal vertical alignment (−SVA) and spinal pelvic parameters warrant investigation. Materials and Methods: This was a retrospective review of 116 AIS first-presentation cases presenting from 2015 to 2016. Eighty-five of these had lateral radiographs, 72 had (−SVA). Schwabb modifiers were used to categorize pelvic tilt (PT) and pelvic incidence lumbar lordosis (PI-LL) mismatch. Lenke categorization of thoracic kyphosis (TK) and all other spinopelvic parameters analyzed with SVA. Results: A total of 83.5% of patients had a (−SVA). Mean (−SVA) = −41.43 mm; mean (+SVA) = 22.99 mm. New classifications of (−SVA) were developed: A = 0 mm to > −35 mm; B = −35 mm to > −65 mm; and C = < −65 mm. Respective means were A = −19.82 mm, B = −46.59 mm, and C = −75.40 mm. Group mean SVA. A: mean LL = 53.38°; mean PI-LL = −4.3°; mean PT = 11.43°; mean TK = 24.68° B: mean LL = 58.83°; mean PI-LL = −7.2°; mean PT = 10.29°; mean TK = 20.71° C: mean LL = 58.41°; mean PI-LL = −16.8°; mean PT = 5.40°; mean TK = 27.86° (−SVA) with PI-LL (R 2 = .92), PT (R 2 = .90), LL (R 2 = .67) and TK (R 2 = .21). Lenke. TK 0-20: 39.3%; n = 26; 12.92°; SVA = −42.43 mm 20-40: 48.48%; n = 32; 27.62°; SVA = −43.09 mm >40: 12.12%; n = 8; 44.75°; SVA = −34.57 mm PI-LL 0-10: 90.14%; n = 64; -10.94°; SVA = −43.16 mm 10-20: 8.97%; n = 7; 16.14°; SVA = −33.26 mm PT 0-20: 91.55%; n = 65; 7.28°; SVA = −42.78 mm 20-30: 2.60%; n = 2; 24.00°; SVA = 35.40 mm >30: 5.33%; n = 4; 40.25°; SVA = −35.85 mm. Conclusion: We believe that we are the first to show there is a high incidence of negative SVA in AIS patients. Severe (−SVA) is associated with a high PI-LL mismatch with compensatory low (antegrade) PT in order to lower LL. Spinopelvic parameters are compensatory to negative sagittal balance. Thoracic hyperkyphosis leads to less negative SVA.
P112: Kyphosis Correction Surgery: The Distal Vertebral Instrumentation Selection Using the Posterior Sacral Vertical Line
Fred U. N. Ukunda1
1University of the Witwatersrand, Johannesburg, South Africa
Introduction: The distal vertebral instrumentation is key in preventing lower junctional kyphosis or failure in the posterior surgical treatment of kyphotic and kypho-scoliotic deformities. This selection remains controversial. Several methods are recommended, especially in the management of Scheuermann disease is made for (thoracic hyperkyphosis). In our setting, various indications besides Scheuermann are also considered for posterior surgical correction. And selecting the distal vertebral instrumentation remains a challenge. As a result, the orthopedic spine unit decided to use “The Sagittal Stable Vertebra Concept” described by Kyu-Jung Cho et al, by using the posterior sacral vertical line (PSVL) in all kyphotic and kypho-scoliotic deformities. Hence, this study intends to review the unit early results. Materials and Methods: This is a retrospective review of a prospectively collected data from the orthopedic spine unit, between 2015 and 2018. Nineteen consecutive patients with kyphotic deformities underwent posterior spine deformity surgery. The PSVL was drawn to touch the expected fusion lower instrumented vertebra. Results: Post tuberculosis kyphosis (n = 5), neurofibromatosis Type 1 (n = 1), congenital kyphosis and kyphoscoliosis (n = 9), Scheuermann disease (n = 1), and adolescent idiopathic scoliosis with associated kyphosis (n = 2). The mean age at presentation was 15 years (range = 5-30 years). The mean kyphosis angle was 79° (range = 40° to 105°). Conclusion: The distal instrumented vertebral touched by the PSVL looked adequate and safe in preventing early lower junctional kyphosis or failure in the posterior surgical treatment of kyphotic and kypho-scoliotic deformities.
P113: Reducing Allogenic Blood Transfusion in Pediatric Scoliosis Surgery: Reporting 15 Years of a Multidisciplinary, Evidence-Based Quality Improvement Project
Alastair G. Dick1, Richard J. Pinder2, Shirley A. Lyle1, Thomas Ember1, Claire Mallinson1, and Jonathan Lucas1
1Guy’s and St. Thomas’ NHS Foundation Trust, London, UK
2Imperial College London, London, UK
Introduction: Pediatric scoliosis corrective surgery can involve substantial bleeding and has historically been associated with high rates of transfusion of blood products. Our aim was to evaluate the efficacy of a care pathway developed at our institution since 2003 with a focus on reducing the need for blood transfusions in children undergoing scoliosis correction surgery. The care pathway includes: nurse-led clinics facilitating preoperative hemoglobin optimization, intraoperative cell-salvage, the use of tranexamic acid, and a transfusion criteria awareness program. Material and Methods: Retrospective review of our institution’s prospectively recorded spinal surgery and transfusion databases including all cases of scoliosis surgery in patients 18 years and younger between 2001 and 2015. Results: A total of 1039 procedures were included in the analysis. Overall 24.4% of patients received a transfusion. The proportion of patients transfused was 89.2% in 2001 to 2003, 39.6% in 2003 to 2006, 16.5% in 2006 to 2009, 15.6% in 2009 to 2012, and 20.1% in 2012 to 2015. The volume of blood products transfused in those undergoing transfusion was 9.1 units in 2001 to 2003, 4.8 units in 2003 to 2006, 5.0 units in 2006 to 2009, 2.3 units in 2009 to 2012, and 2.1 units in 2012 to 2015. A multivariate logistic regression demonstrated adjusted odds ratios for the probability of receiving any transfusion of 5.45 (95% confidence interval = 3.62-8.11) for patients with neuromuscular diagnoses and 11.17 (95% confidence interval = 5.02-24.86) for those undergoing combined anterior and posterior surgical approach. Conclusion: We have demonstrated over a 15-year period that the introduction of a multifaceted, multidisciplinary pathway can dramatically and sustainably reduce the need for blood transfusions and their attendant risks in pediatric scoliosis surgery. These data lend weight to the adoption of such a care pathway in pediatric scoliosis surgery.
P114: Sagittal Vertical Axis and Spinopelvic Parameters in Spondylolisthesis
Sai Krishna M. L. V.1, Deep Sharma1, and Jagdish Menon1
1 Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Introduction: With the discovery of sagittal spinopelvic parameters and their association with various spine disorders, the concept of sagittal balance has become very important. Alteration in sagittal profile has been documented to be associated with various spine disorders from degenerative diseases to deformity. Overall sagittal profile can be assessed with the help of sagittal vertical axis (SVA). SVA is defined as plumb line dropped from C7 vertebra on a lateral sagittal spine radiograph taken in standardized way and its horizontal distance measured from anterior superior corner of sacrum. Based on previous studies, the horizontal distance ranges from −4.5 to +14.9 cm. HRQOL (Health-Related Quality of Life) has highest correlation with T1 tilt, SVA, and pelvic tilt (PT). SVA within 5 cm has been associated with better quality of life. We started our study to know the relation between SVA and spinopelvic parameters in spondylolisthesis patients. Material and Methods: The study was approved by our institutional review board and the ethical committee. A total of 79 spondylolisthesis patients were enrolled into the study after taking a formal consent. Lateral sagittal digital radiographs of the whole spine. The parameters measured were pelvic incidence (PI), PT, sacral slope (SS), thoracic kyphosis (TK), lumbar lordosis (LL), and SVA. All measurements were performed using the Surgimap spine software version 2.1.2. Subjects are divided into 2 groups based on SVA (≤5 cm and >5 cm.). Comparisons are drawn between the groups. Results: The mean values in the first group (SVA ≤ 5 cm.) are PI = 64.91, PT = 21.43, SS = 43.59, LL = 60.87, and TK = 26.20. In the second group (SVA > 5 cm.) are PI = 66.20, PT = 21.04, SS = 45.28, LL = 59.08, and TK = 23.96. Conclusion: Subjects with SVA > 5 cm have higher PI, SS, and lower PT, but the difference was not significant
P115: Return to Play in the Athlete With Adolescent Idiopathic Scoliosis: Spinal Fusion Is Compatible With Sports Participation
Courtney Toombs1, Baron Lonner2, Andrea Castillo2, Yuan Ren2, John Flynn3, and Suken Shah4
1Yale New Haven Hospital, New Haven, CT, USA
2Mount Sinai Beth Israel Hospital, New York, NY, USA
3Children’s Hospital of Philadelphia, Philadelphia, PA, USA
4Alfred I. DuPont Hospital, Wilmington, DE, USA
Introduction: Adolescent idiopathic scoliosis (AIS) is largely an asymptomatic condition with little effect on function in a young, active population. Families often inquire about the impact of a spinal fusion on the ability of the patient to resume sports after surgery. The purpose of this study was to assess sports participation following AIS surgery. Materials and Methods: A total of 101 consecutive AIS patients who were engaged in an organized sport before surgery were enrolled (retrospectively n = 50 and prospectively n = 51) and evaluated postoperatively. Three (2 validated, 1 customized) questionnaires were administered and analyzed. Level of contact (LOC), physical potential, and time spent in the sport were analyzed using Wilcoxon signed-rank test for pre-/postoperative comparisons. Multivariate analysis of factors predictive of sport return was performed. Results: Age at surgery was 14.4 years, 72.3% female; 94 posterior, 6 combined, and 1 anterior procedures; levels fused 10.4; mean FU (follow-up) 1.5 years. Lowest instrumented vertebra (LIV) was 30 patients L1 or above, 63 to L2 or L3, and 8 to L4. Eighty-eight (87%) resumed a sport, 69% remained in the same LOC, and 83.3% returned to their previous or a higher level of physical potential. Number of levels fused and LIV did not correlate with LOC or physical potential; however, a higher postoperative visual analogue scale score was associated with less physical potential (P = .0069). For those who participated in contact sports (n = 18), 11 changed to light or noncontact sports, 3 did not return to sport. Among these 14 patients with diminished LOC, 7 (50%) were fused to or caudal to L3. Median time in sport remained 6 to 10 h/wk pre- to post-operatively. Conclusions: The majority of patients (87%) returned to sports following surgery for AIS. Although there was no change in self-reported physical potential or time in sports, LOC decreased in 32% of patients. Contact sports were dropped in 14/18; half had a LIV of L3 or distal.
P116: Adolescent Idiopathic Scoliosis: Surgical Series Analysis of Demographics, Risk Factors for Complications, and the Effect of an Accelerated Recovery Program on the Outcomes
Darren Lui1, Jason Bernard1, Tim Bishop1, Magda Garzon1, and Cristina Lupu1
1St George’s Hospital, London, UK
Introduction: Adolescent idiopathic scoliosis (AIS) is the most common form of scoliosis. In this study, the authors investigated patient demographics, clinical and hospital characteristics affecting short-term outcomes in adolescent patients undergoing surgical deformity correction for idiopathic scoliosis (10-18 years old). Analysis of complications included infection, bleeding, respiratory and neurological deficit, mortality, and management practices. Material and Methods: Using the hospital records and PACS (picture archiving and communication system) imaging, we created a database identifying adolescent patients undergoing surgical deformity correction for AIS between January 2016 and December 2017. Multivariable regression techniques were employed to assess the association of risk factors as postsurgical complications with length of hospital stay and discharge disposition. Results: Sixty-four adolescent patients underwent surgical deformity correction during this period of time, 69.8% girls and 30.2% boys. The mean age at the time of surgery was 14.1 years (range = 10-18.2 years, SD = 1.1). This elective surgery occurred on Mondays and Thursdays, and the distribution was random (Monday, 20 patients; and 44 on Thursday). The mean length of stay (LoS) for the whole cohort was 7.5 days, median LoS was 7 days (range = 6.1-9.2 days, SD = 3.2) for patients operated on Monday and 8.9 days for patients operated on Thursdays (range = 6.5-10.9 days, SD = 5.4). Associated to the complexity of this procedures, 13 patients presented postsurgical complications (22.8% of the total cohort), which is similar to previous studies; infection was the commonest and accounted for 11.1% (1 deep and 6 superficial wound infection), others were decrease in power 1.6%, need for change of hardware 1.6%, urinary retention 1.6%, and need for surgical revision 6.3%. We have not had cardiac or respiratory complications and no venous thromboembolic events. In all cases, the complications were transitory. There was trend in decrease in the LoS after the implementation of a standard postoperative program that included early mobilization and physiotherapy; however, we found a significant relationship between the day of surgery: Monday versus Thursday, the presence of complications, particularly infections (6 patients operated on Thursday and 1 on Monday) affecting LoS; the mean LoS was 6.9 days in patients with no complications (range = 5.8-7.5 days, SD = 2.8), and 11.4 (range = 5-15.4 days, SD = 3.9) days in patients with complications (P = .006). We identified that there availability of physiotherapy services was reduced during the weekends, affecting particularly the patients operated on Thursdays. The mortality rate in our cohort was 0% and all patients were discharged home. Conclusion: This study provides insight into the clinical characteristics of AIS patients and their postoperative outcomes, particularly after the implementation of an accelerated recovery program that involved early physiotherapy and mobilization. It also provides information regarding independent risk factors for postsurgical complications, we could identify increased risk of complications and longer stay due to lack of physiotherapy on the weekends, and this allowed us to change our practices while observing how trends in management affect outcomes. Further study is needed to validate this report.
P117: Main Thoracic Curve Correction in Correlation to Pedicle Screw Density in Adolescent Idiopathic Scoliosis
Mohammad El-Sharkawi1 and Wael Gad1
1Assiut University Hospital, Assiut, Egypt
Introduction: There is consensus on whether using high screw density (100% of the available pedicles) is better than low screw density on achieving better correction. However lower screw density is theoretically better, as it is associated with less operative time, less bleeding, less risk of neuronal injury, and of course less cost. The aim of this study is to determine if there is a correlation between screw density and main thoracic curve correction. Materials and Methods: Twenty-five patients presenting to our institute with adolescent idiopathic scoliosis (AIS). All of them underwent posterior only correction and fusion. Nine were males and 16 were females. Preoperative radiographs and 24 months follow-up radiographs were reviewed. Main thoracic curve correction ratio was calculated by the following formula: (preoperative Cobb’s angle − follow-up Cobb’s angle)/preoperative Cobb’s angle. Pedicle screw density was the percentage of the number of screws to the number of available pedicles. Mean correction was 58% and mean screw density was 76%. Correlation between correction ratio and pedicle screw density was done using SPSS software. Results: There is no correlation between correction ratio and pedicle screw density (r = .29, P = .158). Conclusion: Low screw density could be as good as high screw density for achieving correction in AIS.
P118: Evaluation of the Amplitude of Motor-Evoked Potential Intraoperatory Transcranial, Pre- and Post-Correction in Adolescents With Idiopathic Scoliosis
Thiago Maia1, Charbel Junior1, Igor Cardoso1, and Jose Lucas Junior1
1Santa Casa de Vitoria, Vitoria, Brazil
Introduction: The present study proposes to contribute about the elucidation of differences found in the literature and in the medical practice about the subject, in order to find more concrete answers, since some authors demonstrated significant improvement of the patients through objective evaluation parameters, while others did not. Materials and Methods: For this, in order to have a theoretical basis, a bibliographic review was made, followed by this descriptive and retrospective cross-sectional study, in which intraoperative, presurgical, and postsurgical correction of deformity were evaluated in adolescents submitted to this treatment for idiopathic scoliosis. Electroneuromyography was used to analyze the motor-evoked potential at the moments to be studied, as well as statistical methods to determine the significance of the results. Results: The results showed that they were indeed significant, indicating that the motor-evoked potential gain was probably also influenced by external factors (anesthetic and hemodynamic variations inherent to the surgical act), not only by the correction itself. Conclusion: Thus, it is concluded that there is a need for the use of some important materials for this evaluation in order to exclude this bias, such as bispectral index, in addition to new studies that complement the knowledge presented here.
P119: The Impact of Column Arthrodesis on the Quality of Life of the Patient Caregiver With Neuromuscular Scoliosis
Thiago Maia1, Charbel Junior1, Igor Cardoso1, and Jose Lucas Junior1
1Santa Casa de Vitoria, Vitoria, Brazil
Introduction: As a condition associated with other disorders, neuromuscular scoliosis is often accompanied by multisystemic dysfunctions, and patient care consists of multiprofessional treatment. The most appropriate therapeutic option is surgical intervention, the purpose of which is to stabilize the deformity. The caregiver is responsible for the well-being of the neuromuscular scoliosis patient, becoming a fundamental part of care, and in many cases, the family members themselves assume this role. Several studies address the impact of surgery on the patient’s life; however, few investigate changes in caregivers’ lives. Improving the quality of life of the caregiver means promoting their satisfaction, which will directly reflect on patient care. Materials and Methods: An analytical study of the qualitative approach of caregivers of 7 patients with neuromuscular scoliosis who underwent spinal surgery between 2008 and 2015. Of the 7 patients, 5 were female and 2 were male, all between 15 and 20 years old and only one patient had complications in the late postoperative period. The patients were reassessed ambulatorily and their caregivers answered a questionnaire of 20 questions based on the work of Sidoli et al, on changes in the care of the patient after the intervention. The data was submitted to statistical analysis and the results were expressed through frequencies and percentages. Results: A total of 85.7% of the caregivers stated that there was improvement in dressing or taking off clothes, putting splints, and time spent in wheelchairs showed a positive evaluation by all. Most report that there has been progress to sit in the common chair and in the length of stay in this. In general, most caregivers report that there was no change in the occurrence of medical problems after surgery. A positive evaluation of aesthetic improvement was made by all caregivers. Importantly, 100% say they would undergo surgery again and recommend the procedure. None of the questions addressed were evaluated negatively with worsening after intervention. Conclusion: One can observe great satisfaction of the caregivers after the procedure in the column with high index of positive evaluation of all the questions. It is very important to point out that there was no negative evaluation and all the caregivers affirm that the patients are happier and present an improvement of the deformity.
P120: Evaluation of the Reproducibility of the Suk and Lenke Classifications for Adolescent Idiopathic Scoliosis
Thiago Maia1, Charbel Junior1, Igor Cardoso1, and Jose Lucas Junior1
1Santa Casa de Vitoria, Vitoria, Brazil
Introduction: Over time, several authors have described several classifications with the aim of homogenizing the diagnosis, establishing treatment protocols, facilitating research, and improving communication among health professionals. Among the most commonly used systems are the Lenke and Suk classifications. The objective of this study is to evaluate the interobserver and intraobserver accentuation of the Lenke and Suk scores for adolescent idiopathic scoliosis. Materials and Methods: An observational study was performed. The sample consisted of 5 spine surgeons from Espírito Santo. Ten clinical cases were assembled, each surgeon classified the types of scoliosis in the sequence of cases assembled by the researchers. Three months after the first evaluation, there was a new evaluation. The obtained data were examined for intraobserver and interobserver precision and accuracy. The concordance evaluation was performed using the chi-square test using the kappa index, with a significance of 5%. Results: In the interobserver analysis of Lenke’s classification, the majority had a moderate concordance kappa index (between 0.40 and 0.59). In this same analysis of the Suk classification, the majority had a kappa index of fair agreement (between 0.20 and 0.39). In Lenke’s intraobserver analysis, the majority had a kappa index of fair agreement (between 0.20 and 0.39); in Suk’s, we obtained the majority with the kappa index of moderate agreement (between 0.40 and 0.59). Conclusion: The classification of Lenke obtained greater reproducibility and the classification of Suk obtained greater repetitiveness.
Deformity-Thoracolumbar (Adult)
P121: Impact of Complications on Heatlh-Related Quality of Life in Spine Deformity Surgery
Manuel Fernández González1, Julio Villar Perez1, Domingo Lombao Iglesias1, Marta Esteban Blanco1, Ana Estany Gestal2, Andrés Blanco Hortas1, Jose Angel Hernández Encinas1, Ana Lozano Muñoz1, Jesús Betegón Nicolás1, and Ignacio Fernandez Bances1
1Fundación Instituto de Estudios de Ciencias de la Salud de Castilla y León, Soria, Spain
2Fundación Instituto de Investigación Sanitaria de Santiago de Compostela (FIDIS), Santiago de Compostela, Spain
Introduction: The rate of major complications in deformity surgery is 40%, so its objective is to analyze the impact on the quality of life of patients who suffer complications in adult spine deformity surgery. Material and Methods: Retrospective analysis of a patient cohort created in 2014 that has undergone deformity surgery. Includes 4 or more instrumented vertebrae and a minimum of 1 year of follow-up. We create 2 groups based on whether patients have complications or not. The quality of life questionnaires were the visual analogue scale (VAS), Oswestry Disability Index (ODI), and the Scoliosis Research Society (SRS)-22. Statistical analysis was performed using Student’s t and Mann-Whitney U tests depending on the variables were adjusted to normal or not for the independent samples and for the related tests using Wilcoxon W. P < .05 was considered as statistically significant difference. Results: Sixty-five patients were included from primary surgery who fulfilled all the protocols, (75.4% women) with a median age of 68 years (range = 56.5-74 years), 7 instrumented levels (5-8), and 406.50 cc bleeding (270-682.25) an average body mass index (BMI) of 27.73 kg/m2 (4.78 kg/m2) and 305.47 minutes (62.7 minutes) of average surgical time. Twenty-two patients had complications (proximal junctional kyphosis [10], bar rupture [4], mobilization material [3], fracture of last instrumented inferior vertebra [1], and infection [6]). The results of the quality of life of patients with complications, showing a significant statistical improvement in all parameters, except the subdomain function (precomplication = 2.55 [0.66]; postcomplication = 2.93 [0.85]; P = .082) and satisfaction function (precomplication = 3.25 [1.25]; postcomplication = 3.84 [0.91]; P = .095) of the SRS-22 regarding the preoperative. The disability that the ODI shows is better and statistically significant than the preoperative one, although it remains at high levels (precomplication = 57.58 [16.01]; postcomplication = 43.47 [17.1]). Considering the pain in the back function (precomplication = 8 [5.50-9]; postcomplication = 4 [1.50-7.50]) and leg function (precomplication = 8 [5-8]; postcomplication = 2 [0.50-5]) it significantly improves after complication. We also analyze the final values of the groups of patients. Patients who suffered complications have worse quality of life than patients who have not been reoperated for any complication but the differences between the 2 groups were not statistically significant. Conclusion: The impact on health-related quality of life is reflected in the results of the surgery. Patients with complications have greater functional limitation and worse values of the sd22 subdomains.
P122: Influence of the Latest Instrumentated Vertebra (LIV) on the Quality of Life in Patients Involved in Deformity of the Adult
Manuel Fernández González1, Julio Villar Perez1, Domingo Lombao Iglesias1, Marta Esteban Blanco1, Ana Estany Gestal2, Andrés Blanco Hortas1, Jose Angel Hernández Encinas1, Ana Lozano Muñoz1, Jesús Betegón Nicolás1, and Igancio Fernandez Bances1
1Fundación Instituto de Estudios de Ciencias de la Salud de Castilla y León, Soria, Spain
2Fundación Instituto de Investigación Sanitaria de Santiago de Compostela (FIDIS), Santiago de Compostela, Spain
Introduction: The principal consequence of spinal instrumentation is the functional limitation that patients acquire after surgery. The literature suggests that the instrumentation to iliac limits more the activities of the patients so our objective was to analyze the quality of life of our patients in function of the last inferior instrumented vertebra (LIV). Material and Methods: Retrospective analysis of 3 patient cohorts that were divided into 3 groups according to their LIV: group 1: iliac, group 2: S1, and group 3: L5. We analyzed their age, gender, body mass index (BMI), number of instrumented levels, surgical time, and percentage of reinterventions. The quality of life questionnaires used were the visual analogue scale (VAS), Oswestry Disability Index (ODI), and Scoliosis Research Society (SRS)-22. The statistical analysis was performed by means of an analysis of variance (ANOVA) for normal samples and in the case of nonnormal variables was that of Kruskall Wallis. We analyzed which group was different by a 2 by 2 test with the Mann-Whitney U test for nonnormal samples and Student t test for samples that follow a normal distribution. Results: A total of 160 patients with more than 1 year of follow-up and 4 or more instrumented vertebrae were included. The baseline characteristics of the groups with similar body mass index (BMI), less median age in group 3 (58 [39.25-71.75]), and higher number of instrumented levels (8 [8-14]) in group 1 where the surgical time was also longer (390 [330-510]). The percentage of reoperation in group 1 (38%), group 2 (29.5%), and group 3 (21.4%). We analyze which group differs from the analyzed variables and is similar to the basal characteristics by adding the gender variable; the group that differs is the group 1: iliac. When comparing the groups studied, we did not find statistically significant differences in the quality of life questionnaires. ODI (group 1: 40.57 [20,31], group 2: 37.46 [20.59], group 3: 39.65 [22,03]; P = .736), VAS back (group 1: 4 [1.75-7], group 2: 4 [1-6.75], group 3: 5 [1.75-7]; P = .863), VAS leg (group 1: 5 [1-8.50], group 2: 3 [1-5.50], group 3: 3.50 [2.00-8.00]; P = .189), SRS-22_function leg (group 1: 3.00 [2.20-3.60], group 2: 2.80 [2.40-3.40], group 3: 2.80 [2.40-3.20]; P = .886), SRS-22_pain (group 1: 3.00 [2.20-3.90], group 2: 2.90 [2.40-3.40], group 3: 3.20 [2.70-4.00]; P = .974), SRS-22_selfimage (group 1: 3.18 [0.80], group 2: 3.07 [0.71], group 3: 3.24 [0.72]; P = .345), SRS-22_mentalhealth (group 1: 3.80 [2.80-3.90], group 2: 3.80 [2.65-4.00], group 3: 3.20 [2.70-4.00]; P = .451), SRS-22_satisfaction (group 1: 4.50 [4.00-5.00], group 2: 4.00 [3.50-4.50], group 3: 4.50 [4.00-4.86]; P = .295), and SRS-22_total (group 1: 3.21 [0.82], group 2: 3.19 [0.68], group 3: 3.14 [0.67]; P = .946). Conclusion: In our sample of patients, we did not find that LIV had an influence on quality of life, despite the differences between the groups studied and the percentage of reoperation is greater in group 1.
P123: Deformities of the Thoracic and Lumbar Spine in Adults Secondary to Congenital Pathology
Oxana Prudnikova1 and Alexander Kotelnikov2
1Russian Ilizarov Scientific Center, Kurgan, Russian Federation
2Kurgan
Introduction: Frequency, tactical aspects, and prognosis of deformities of the thoracic and lumbar spine in adults secondary to congenital pathology are not currently defined. The aim of the study was to determine the structure and specifics of tactical approaches in adult patients with deformity of the thoracic and lumbar spine secondary to congenital pathologies. Materials and Methods: Prospective monocentric cohort (n = 130): 50 males (38.4%), 80 females (61.5%). The period of patient recruitment was 2015 to 2018. Age varied from 19 to 69 years (range = 45.0 ± 11.4 years). Long-term results varied from 6 months to 3 years. Methods of research: Clinical, radiographic (X-rays and roentgenometry [Wiasis v.2.03, Medical viewer], CT [computed tomography]), MRI (magnetic resonance imaging); statistical (SPSS). Evaluation criteria: degree of deformity; neurological status, visual analogue scale (VAS), Oswestry Disability Index (ODI), and Scoliosis Research Society–22 (SRS-22); types of interventions; and structure of complications. Results: Deformities secondary to congenital pathology were observed in 19.2% (25 patients); secondary to congenital diseases (cerebral palsy and neuro-muscular scoliosis)—6.2% (8 patients); spondylolysis and spondylolisthesis—74.6% (97 patients). Deformities of the spine secondary to disorders of formation and segmentation of the vertebrae (n = 10): Cobb 12° to 52°, kyphosis 43° to 160°; pain (8), mild paraparesis (2). Surgical treatment was performed in 7 patients: posterior spinal fixation (PSF; 1); PSF+ variants of vertebrotomies (Smith-Petersen osteotomy [SPO] = 3, VSR = 3). After treatment: Cobb 5° to 32°, kyphosis 34° to 90°. VAS (before/after): 43/28, ODI (before/after): 39/29, and positive dynamics for SRS-22 domains in all cases. Spinal deformities secondary to SCD (n = 4): Cobb 28° to 70°, lumbar hyperlordosis 38° to 46°; pain (3), lower monoparesis (1). Surgical treatment was primary in 2 stages; one-stage (1), revision (1). Spinal deformities secondary to MMC (n = 3): Cobb 12° to 56°; pain (3), low paraparesis (3). Surgical treatment was not done. Spinal deformities secondary to neurofibromatosis (n = 4): Cobb 28° to 150°; kyphosis 23° to 100°; pain (2), low moderate paraparesis (1). Surgical treatment was PSF (3). Spinal deformities in achondroplasia (n = 4): kyphosis 11° to 113°; pain (2), lower moderate paraparesis (2). Surgical treatment included laminoplasty + PSF (2), laminoplasty (2). Spinal deformities secondary to cerebral palsy (n = 3): Cobb 38° to 150°, kyphosis 26° to 130°; pain (3), tetraparesis (3); functional status: GMFCS III-V, MACS I-III, CFCS III, and FMS N-2 . Surgical treatment was done in one patient: PSF (1). Spinal deformities secondary to neuromuscular diseases (n = 5): Cobb 85° to 105°, kyphosis-lordosis 80° to 92°; pain (5), tetraparesis (3), paraparesis (2). Surgical treatment was done in 3 patients: PSF + SPO. Spondylolysis and vertebral displacement (n = 97): displacement 1.3 ± 0.4 cm, pathological mobility—100% of cases, L5/L4/L3—71/25/1; myelopathy (9), radiculopathy (41), and vertebral pain syndrome (47). Surgical treatment in all patients: PSF + PLIF (posterior lumbar interbody fusion). The displacement after the treatment was 0.6 ± 0.5 cm; VAS (before/after): 45/32, ODI (before/after) 40/32. Deformities of the thoracic and lumbar spine of adults secondary to congenital pathology and diseases accounted for 5.2% of patients discharged during this period. We did not analyze the anomalies of spina bifida S1 and facet joint tropism. Surgical treatment was performed in 92% of patients. Complications occurred in 21.8%: neurological in 7.5%; instability of fixation in 14.3%. Discussion: Distinctive features of adult spinal deformities secondary to developmental defects and congenital diseases are as follows: the nature of progression due to addition of degenerative changes, rigidity of deformities, progressive myelopathy, neurological disorders, overrun of clinical symptoms, and somatic and functional status. Conclusion Tactics of treatment is determined by individual starting data; it should take into account risks of possible complications and be aimed at maximum preservation of the starting functional abilities of patients.
P124: Spinal Surgery in Adult Patients With Neurogenic Diseases: Problems and Solutions
Oxana Prudnikova1
1Russian Ilizarov Scientific Center, Kurgan, Russian Federation
Introduction: Spinal surgery in patients with neurogenic diseases is characterized by high level of complications and reoperations. Purpose of the study: To determine variants of surgical treatment of patients with spinal pathology secondary to neurogenic diseases. Material and Methods: Clinical and radiographic analysis of results of surgical treatment of 15 patients with spinal pathology secondary to Parkinson disease (9 patients) and infantile cerebral palsy (6 patients) was performed. Indications for surgical treatment in 5 cases were spinal deformities, and in 10—clinical manifestations of degenerative dystrophic diseases of the spine. Results: Three patients with spinal deformities (1—Pisa syndrome, 2—kyphoscoliosis secondary to infantile cerebral palsy) underwent extensive posterior instrumentation + SPO (Smith-Petersen osteotomy) with correction of sagittal and frontal balance. Formation of PJF (proximal junction failure) syndrome was observed in all patients in the postoperative period. In 2 patients with posttraumatic deformities in pathological fractures, decompression laminectomy with fixation with augmented transpedicular screws was performed without progression in the postoperative period. In 9 patients with variants of lumbar spinal stenosis 1-level decompression-stabilization interventions were performed: decompression facetectomy + posterior spinal fixation (PSF) + posterior lumbar interbody fusion (PLIF)—5 patients, microsurgical bilateral decompression—4 patients. In one case, in multilevel cervical stenosis, laminoplasty with posterior instrumentation was performed. Poor treatment result with progression of deformity secondary to Parkinson disease was diagnosed in one female patient. Discussion: According to literature data, incidence of spinal deformities secondary to neurogenic diseases (Parkinson disease and infantile cerebral palsy) is 60% to 77%. Degenerative and dystrophic changes of the spine lead to rigid deformities, secondary progression, and multiple clinical manifestations. Posterior instrumentation in segments with vertebrotomies in infantile cerebral palsy allows for deformity correction by 53% to 66% improving the functional class. Incidence of complications here is up to 32% (proximal junction kyphosis [PJK], migration of screws, and neurological deficit). In Parkinson disease, patients in surgical interventions of various extension and levels of fixation reoperations were done in 33.3% to 86% of cases. Main reasons for this were instability of construction, progression of deformity, and infection complications. In the presented study of instrumental correction of spinal deformities secondary to Parkinson disease and infantile cerebral palsy in all t3 cases secondary to deformity correction formation of PGF syndrome was diagnosed during 2 to 6 months after treatment and it required revision surgeries. Decompression stabilization interventions in posttraumatic deformities in pathological fractures in patient with Parkinson disease using transpedicular augmented fixation allowed for achievement of satisfactory clinical and radiographic treatment results. Monosegmental decompressive interventions in lumbar spinal stenosis appeared effective practically in all cases with regress of pain and neurological manifestations. Poor treatment result was observed only in one case. Conclusion. Evaluation of risk of surgical intervention considering possible complications and potential treatment result determines approach to spinal surgery in these patients considering possibilities of noninvasive and minimally invasive treatment techniques.
P125: Systemic Changes After Surgical Treatment of Kyphotic Deformity Secondary to Ankylosing Spondylitis: A Systematic Review
Jingwei Liu1 and Yong Hai1
1Beijing Chaoyang Hospital, Capital Medical University,Beijing, China
Purpose: In addition to changes of skeletal system after spinal osteotomy for treatment of kyphotic deformity in advanced stage ankylosing spondylitis (AS) patients, many other changes related to the patients’ quality of life were reported. To conduct a systematic review of literature to determine systemic changes after surgical treatment of kyphotic deformity secondary to AS. Methods: On June 19, 2017, we searched the databases PubMed, EMBASE, Clinicalkey, and Cochrane Library without time restriction. Selected articles were assessed by published guidelines. We investigated systemic changes after surgical treatment of AS kyphosis. Results: The initial search yielded 888 citations. Ten of these studies met the inclusion and exclusion criteria. None of them was level I or level II evidence studies, one was level III evidence study, and 9 were level IV evidence studies. Changes were reported including aorta length, abdominal morphology, digestive function, cardiopulmonary function, psychological status, and sexual activity. Conclusions: In addition to skeletal changes after spinal osteotomy for treatment of kyphotic deformity in advanced stage AS patients, many other changes were reported. Spine surgeons should pay more attention to these life quality–related changes and be aware of potential risks when performing osteotomy for advanced stage AS patients.
P126: Anterior Approach Is a Viable Technique to Retrieve Tlif Cages for Lumbar Revision Surgeries
M. Burhan Janjua1 and Vincent Arlet2
1UT Southwestern Medical Center, Dallas, TX, USA
2Philadelphia, PA, USA
Introduction: Symptomatic pseudoarthrosis after transforaminal lumbar interbody fusion (TLIF) could result in sagittal malalignment. Revision posterior surgery with TLIF cage removal poses a challenge intraoperatively. The authors have proposed salvage anterior approach for cage removal and have discussed unique experience with the correction in their deformity patients. Methods: All patients with symptomatic pseudoarthrosis and malalignment operated from January of 2012 to February of 2018 were included in the study. TLIF cage removal followed by anterior lumbar interbody fusion (ALIF) surgery was performed in all patients. Radiographic sagittal parameters including thoracic kyphosis (TK; T4-12), sagittal vertical axis (SVA), transverse pedicle angle (TPA), lumbar lordosis (LL), pelvic incidence LL (PI-LL), sacral slope (SS), pelvic tilt (PT), and PI were analyzed. Results: Six patients (mean age of 57 years, 83% female) underwent TLIF retrieval through anterior approach and ALIF with hyperlordotic cages (HLCs), followed by posterior spinal fusion surgery. Described technique entails use of tailored instruments with sequential gentle distraction of endplates with TLIF spreader could facilitate in the cage removal. Mean number of interbody levels fused pre as well as post were 1.5. The radiographic sagittal parameters from preoperative versus postoperative standing: T4-12 TK (16° vs 37.6°), LL (−25° vs −47.6°), PT (36° vs 26°), PI-LL (35° vs 12.4°), SVA (12° vs 5.6°), TPA (44° vs 25°) with P < .001. Mean number of instrumented level fused were 8.1. Using linear regression analysis, change from pre- to postoperative standing in LL predicted pre- to postoperative change in SVA and TPA for global correction. (R = −.30, and −.80, respectively). Conclusions: Anterior approach is a suitable technique for TLIF cage removal while, preserving the endplates for subsequent optimal interbody fusion at the index level in symptomatic pseudoarthrosis. ALIF with HLCs with or without Ponte osteotomy can restore the segmental and the overall sagittal alignment.
P127: Application of Free-Hand S2 Alar-Iliac Screw Combined With Posterior Column Osteotomy for the Treatment of Adult Spinal Deformity
Wei-Hu Ma1, Yun-Lin Chen1, and Nan-Jian Xu1
1Ningbo, China
Introduction: More and more evidence proved that pelvic fixation may be the standard for long fusions in adult spinal deformity. Galveston iliac rods or iliac screws improve the fusion rates, but most patients complained with implant prominence. S2 alar-iliac (S2AI) screws are biomechanically as stable as iliac screws, but has lower complication rates. Methods: Eight patients who underwent sacropelvic fixation using S2AI screws combined with posterior column osteotomies (PCOs) were included. In each case, the S2AI screws were placed utilizing a free-hand technique without fluoroscopic or image guidance. Clinical and radiographic assessments were evaluated. Results: The average number of fusion levels was 9.25 vertebral bodies. The mean operation time was 355.88 minutes (range = 330-395 minutes), mean estimated blood loss was 1999.37 mL (range = 1300-2950 mL). There was no case of neurological deficit, infection, and S2AI screw–related vascular or neurological complication. PCOs were performed form the T12/L1 level to the L5/S1 level. The average number of osteotomy levels was 4.25 ± 0.7 (range = 3-5). Mean kyphosis correction per PCO was 7.2°. There is no case of sacroiliac (SI) joint pain, degeneration, or fusion after SI joint fixation. Cobb angle, sagital vertical axis, and visual analogue scale scores were significant and improved after operation. Conclusion: Free-hand S2AI screw was a safe and effective method for pelvic fixation. SI joint pain and degeneration was rare. Free-hand S2AIs combined with PCOs were an alternative method for the correction of ASDs.
P128: Prospective Study of Radiological and Clinical Outcomes Following Surgical Correction of Adult Spine Deformity
Babak Mirzashahi1 and Saeed Panahi1
1Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Islamic Republic of Iran
Introduction: Radiological assessments are necessary for evaluation of deformity magnitude and choosing the appropriate surgical technique. Some previous studies have demonstrated that radiological parameters are correlated with pain and disability. However, few studies have evaluated changes in both coronal and sagittal radiological parameters following surgical treatment of adult spinal deformity (ASD) and its correlation with clinical outcomes. Materials and Methods: Eligible patients diagnosed with ASD referred for correction surgery were included. Six radiologic parameters (PT [pelvic tilt], pelvic incidence [PI], sacral slope (SS), lumbar lordosis [LL], and PI minus LL [PI-LL], and Cobb’s angle) and 3 clinical measures, visual analogue scale (VAS), Oswestry Disability Index (ODI), and Short Form–36 Health Survey (SF-36), were assessed at baseline and after surgery. Results: A total of 95 patients were included. Mean VAS scores and ODI significantly improved from 7.09 ± 2.1 and 61.07 ± 13.6 to 2.64 ± 1.6 and 31.8 ± 16.1 after surgery (both P < .001). All items of the SF-36 Survey as well as all radiologic measures improved significantly following surgery (both P < .001). We found a significant negative correlation between preoperation SS and VAS (r = −.307, P = .002), and energy (r = −.262, P = .010) and social functioning (r = −.248, P = .015) scales of SF-36. PI-LL was positively associated with ODI (r = .223, P = .030) before surgery and energy scale (r = −.262, P = .010) of SF-36 after surgery. Conclusions: This study showed that surgical correction of ASD improves both radiological and clinical outcome. In line with previous studies, we believe that sagittal alignment has a more important role in patients’ function and quality of life.
P129: Characteristics of Gastric Esophageal Reflux Symptoms Related to Spinal Sagittal Malalignment in Elderly Patients
Yutaka Nakamura1, Masayoshi Kanai1, and Satoshi Asano1
1Higashi Saitama General Hospital, Satte, Japan
Introduction: It is known that the quality of life for aging patients who have spinal kyphosis deformity is frequently affected by symptoms of gastric esophageal reflux disease (GERD). There is scattered mention in case study literature where refractory GERD has been seen to improve rapidly after correction of sagittal deformity. The purpose of this study was to evaluate with the use of questionnaires the characteristics of GERD symptoms related to spinal sagittal alignment. Material and Methods: A total of 1314 consecutive patients seen at our osteoporosis outpatient clinic between September 2009 and January 2018 were asked to complete 2 questionnaires, the Frequency Scale for the Symptoms of GERD (FSSG) and the Questionnaire for the Diagnosis of Reflux Disease (QUEST). After excluding scoliosis patients, 1283 patients (211 males, 1072 females) remained who had completed both questionnaires and for whom whole spine radiographs were available. Patients who scored positively on both questionnaires (8 or more on the FSSG and 4 or more on the QUEST) were assigned to the GERD group. Conversely, only those who scored negatively on both questionnaires were included in the non-GERD group. A total of 122 (9.4%) patients were included in the GERD group. In all, 532 (41.5%) patients were included in the non-GERD group. For spinal sagittal alignment, the thoracolumbar kyphosis (TLK) angle was measured. Spearman correlation analysis was used to compare between TLK and the questionnaire responses. From DEXA scan data, we also calculated total bone mass density at L2-5, the femoral neck, and total femur. Results: TLK averages (T10-L2) were 26.6° and 17.4° for the GERD group and non-GERD groups, respectively (P < .05). Average FSSG values were Q 1: (1.47/0.28), Q 2: (1.41/0.49), Q 3: (1.78/0.23), Q 4: (1.13/0.11), Q 5: (0.78/0.12), Q 6: (1.34/0.17), Q 7: (1.09/0.2), Q 8: (1.19/0.39) Q 9: (0.91/0.26), Q 10: (1.25/0.22), Q 11 (1.44/0.46), Q 12: (0.94/0.07), gastroesophageal reflux (8.13/1.31), upper gastrointestinal dysmotility-like dyspepsia (6.59/1.67), and total number (14.72/2.99). QUEST values were Q1: (3.75/0.03), Q2: (1.28/0.02), Q3: (1.63/0.24), Q4: (0.84/0.05), Q5: (0.22/0.03), Q6: (0.22/0.01), Q7: (0.56/0.00), and total: (8.16/0.32). Items correlating with TLK were acid reflux: 0.13, dysmotility-like dyspepsia: 0.06, F-scale total: 0.03, and total QUEST: 0.03. BMD (bone mineral density) averages (g/cm2) were 0.701/0.730 (lumbar), 0.505/0.517 (femoral neck), and 0.610/0.615 (total femur). There was no significant difference between the 2 groups. Conclusion: This study identified the characteristics of GERD related to spinal sagittal malalignment. The GERD questionnaire, in addition to typical symptoms of heartburn and acid reflux was also useful for the detection of gastroesophageal reflux and dysmotility. The correlation between sagittal spinopelvic alignment and symptoms of GERD found in this study suggest an increased abdominal pressure that exacerbates upper gastrointestinal dysmotility and acid reflux. It follows that treatment options for GERD, particularly when hiatal hernia is involved, must be expanded beyond proton pump inhibitors to address other underlying pathologies.
P130: Late Atraumatic Fusion Mass Fractures Occurring Between Non-Bridged Constructs in Patients Requiring Fusions Distal to Adolescent Idiopathic Scoliosis Fusions
Tan Chen1, Mohammed Obeidat1, So Kato1, Anupreet Bassi1, and Stephen Lewis1
1University of Toronto, Toronto, Ontorio, Canada
Introduction: Distal degeneration requiring fusion is a common problem following surgery for adolescent idiopathic scoliosis (AIS). Controversy exists on how best to manage the old implants in the face of a solid fusion mass. Two cases of late fractures through the junctional fusion mass are presented in patients where the new distal implants were not bridged to the original constructs. Materials and Methods: A retrospective chart and radiographic review was performed on 2 patients sustaining atraumatic fractures in the fusion mass between the original proximal construct and the newly added distal construct. Results: A 57-year-old female underwent a Harrington rod instrumentation at the age of 12 years and subsequent L3-S1 fusion for distal segment degeneration at age 40 years without connection between the constructs. She presented with a transverse fracture through the pedicles and vertebral body of L3 with kyphosis. The second patient is a 39-year-old female who underwent T5-L1 fusion at age 12 years, presented 6 months following a T11-L5 revision posterior decompression and fusion without bridging of the constructs. A kyphotic compression fracture at T11 occurred, with resultant severe back pain and loss of alignment. Both patients underwent revision of posterior spinal instrumentation and correction of kyphotic deformity. In the first case, on positioning of the patient in extension on the operating room table, significant anterior gapping at the fracture site occurred, leading to full correction of the kyphotic deformity and resulted in significant epidural bleeding with subsequent hematoma requiring evacuation. The distal construct was revised and connected to the Harrington distraction rod through rod-to-rod side connectors. Further revision was required for anterior stabilization and rod exchange. In the second case, the proximal construct was removed and a new construct was placed from the proximal thoracic region to the pelvis. Both patients fully recovered and were asymptomatic at the 2-year follow-up. Conclusion: Unprotected fusion masses between constructs in the revision of old AIS posterior spinal constructs are vulnerable to fracture. This complication is preventable with bridging or overlapping of the original and new constructs. Sagittal malalignment and osteoporosis are likely significant contributors to these fractures. When extending AIS constructs secondary to distal degeneration, protecting the entire fusion mass with the new construct can prevent atraumatic fusion mass fractures.
P131: Influence of Total Propofol Dose on Transcranial Motor–Evoked Potentials Monitoring During Adult Spinal Deformity Surgery: The Phenomenon of Anesthetic Fade
Hiroki Ushirozako1, Go Yoshida1, Tomohiko Hasegawa1, Yu Yamato1, Tatsuya Yasuda1, Tomohiro Banno1, Hideyuki Arima1, Shin Oe1, Yuki Mihara1, Daisuke Togawa1, and Yukihiro Matsuyama1
1Hamamatsu University, Hamamatsu, Japan
Introduction: Intraoperative neuromonitoring is important for avoiding neurological injury. However, there have been multiple reports of false-positive transcranial motor–evoked potentials (TcMEPs) alerts. Surgeons or anesthesiologists should assess total anesthetic dose to rule out false-positive TcMEPs alerts. The purpose of this retrospective study is to clarify the risk factor of TcMEPs alerts during adult spinal deformity surgery. Material and Methods: We analyzed 317 patients with multichannel TcMEPs monitoring under total intravenous anesthesia during adult spinal deformity surgery between 2010 and 2017 (53 men, 264 women; mean age: 61.5 years; follow-up period: ≥6 months). Cases with severe preoperative motor deficits and inhalational anesthesia were excluded. We defined our alarm point as final TcMEPs amplitudes <30% of baseline, the global TcMEPs alerts as alerts in bilaterally one or more different muscles of the lower extremities, and the focal TcMEPs alerts as the other alerts. Patients with false-positive alerts were classified into 2 groups: the group with global TcMEPs alerts, who may have the phenomenon of “anesthetic fade,” and the group with focal TcMEPs alerts. Results: There were 17 true-positive cases, 15 rescue cases, a false-negative case, 218 true-negative cases, and 66 false-positive cases (20.8%), comprising 36 cases with global TcMEPs alerts and 30 cases with focal TcMEPs alerts. Sensitivity and specificity were 94% and 77%, respectively. Compared with the true-negative cases, the false-positive cases had a significantly larger estimated blood loss and longer length of surgery (P < .01).Compared with the true-negative cases, the false-positive cases with global TcMEPs alerts had a significantly higher total propofol dose (1950 vs 1500; P < .01), and the false-positive cases with focal TcMEPs alerts had a significantly higher total propofol dose (1780 vs 1500; P < .05). The cutoff level of total propofol dose for predicting false-positive global TcMEPs alerts was 1520 mg with the best sensitivity and specificity. A multivariate logistic analysis revealed that total propofol dose >1520 mg (odds ratio = 3.47; 95% confidence interval = 1.51-8.01; P < .01) and length of surgery >360 minutes (odds ratio = 3.56; 95% confidence interval = 1.66-8.15; P < .01) were independently associated with false-positive global TcMEPs alerts. Conclusion: Intraoperative total propofol dose >1520 mg and length of surgery > 360 minutes are independently associated with false-positive global TcMEPs alerts during adult spinal deformity surgery. Total propofol dose is clinically useful for ruling out false-positive alerts.
P132: Utilization of Artificial Intelligence–Based Hierarchical Cluster Analysis of Patient Baseline Characteristics and Surgical Invasiveness Provides Novel Insights on 2-Year Outcomes and Complications Through Pattern Recognition
Christopher P. Ames1, Miquel Serra-Burriel2, Justin S. Smith3, Michael P. Kelly4, Ahmet Alanay5, Emre R. Acaroglu6, Francisco Javier Sánchez Pérez-Grueso7, Frank Kleinstück8, Ibrahim Obeid9, Virginie Lafage10, Frank J. Schwab10, Christopher I. Shaffrey3, Douglas C. Burton11, Shay Bess12, Ferran Pellisé13; International Spine Study Group (ISSG)10; European Spine Study Group (ESSG)13
1University of California, San Francisco, CA, USA
2Universitat Pompeu Fabra, Barcelona, Spain
3University of Virginia Medical Center, Charlottesville, VA, USA
4Washington University in St Louis, St. Louis, MO, USA
5Acibadem University, Istanbul, Turkey
6Ankara ARTES Spine Center, Ankara, Turkey
7Hospital Universitario La Paz, Madrid, Spain
8Schulthess Klinik, Zurich, Switzerland
9Bordeaux University Hospital, Bordeaux, France
10Hospital for Special Surgery, New York, NY, USA
11University of Kansas Medical Center, Kansas City, KS, USA
12Presbyterian St. Luke’s/Rocky Mountain Hospital for Children, Denver, CO, USA
13Hospital Vall d’Hebron, Barcelona, Spain
Introduction: Adult spinal deformity (ASD) is a heterogeneous condition with a broad range of surgical options. Unsupervised machine–based pattern clustering of patient types based on radiographic parameters and quality of life measures alongside combinations of surgical options may simplify ASD patient types, procedures, and outcomes. Artificial intelligence (AI)–based pattern recognition may augment preoperative decision-making for surgeons in real time by identifying similarity patterns in ASD patient types when combined with procedure groups. Material and Methods: Two prospective cohorts were retrospectively queried for surgical ASD patients with SRS-22/ODI/SF-36 (Scoliosis Research Society–22/Oswestry Disability Index/Short Form–36 Health Survey) data at baseline, 1 year, and 2 years. AI-based hierarchical cluster analysis was utilized to identify 12 empirically driven groups for ASD surgery. Classification built on delineation of 3 patient types and 4 surgery types facilitates statistical prediction of quality of life improvements and major complications (MC) rates. Two dendrograms on the same observations were fitted, one with surgical features and one with patient characteristics. Both were built with Ward distances and optimized with the Gap method. For each of the possible “n” patient clusters by “m” surgeries, normalized average improvement at 2 years, and adjusted MC rates were computed. Results: Three optimal patient types were identified based on 570 patients: Young with coronal plane deformity (YC) (n = 195), older with prior spine surgeries (ORev) (n = 194), and older without prior spine surgery (OPrim) (n = 218). Osteotomy type, instrumentation, and interbody fusion were combined to define 4 optimal average surgical options. Two-year normalized average improvement ranged from −0.074% for SF-36 MCS (mental component summary) score in cluster (1.3) to 100.2% for SRS self-image score in cluster (2.1). MC rates at 2 years ranged from 0% to 51.8% (Figure). Conclusion: Unsupervised AI hierarchical clustering can identify subtle patterns and classification clusters that may augment preoperative decision making through construction of a 2-year risk benefit grid. In addition to enhancing outcome and complication prediction, pattern identification may facilitate treatment optimization by educating surgeons on which treatment patterns yield optimal benefit with lowest risk.
P133: Development of Preoperative Computer Models That Accurately Predict Answers to All Individual Questions on SRS-22 at 2-Year Follow-up: A Step Toward Individualized Medicine
Miquel Serra-Burriel1, Ferran Pellisé2, Michael P. Kelly3, Justin S. Smith4, Jeffrey L. Gum5, Ahmet Alanay6, Emre R. Acaroglu7, Francisco Javier Sánchez Pérez-Grueso8, Frank Kleinstück9, Ibrahim Obeid10, Virginie Lafage11, Frank J. Schwab11, Christopher I. Shaffrey4, Douglas C. Burton12, Shay Bess13, Christopher P. Ames14; European Spine Study Group (ESSG)12; International Spine Study Group (ISSG)11
1Universitat Pompeu Fabra, Barcelona, Spain
2Hospital Vall d’Hebron, Barcelona, Spain
3Washington University in St Louis, St. Louis, MO, USA
4University of Virginia Medical Center, Charlottesville, VA, USA
5Norton Leatherman Spine Center, Louisville, KY, USA
6Acibadem University, Istanbul, Turkey
7Ankara ARTES Spine Center, Ankara, Turkey
8Hospital Universitario La Paz, Madrid, Spain
9Schulthess Klinik, Zürich, Switzerland
10 Bordeaux University Hospital, Bordeaux, France
11Hospital for Special Surgery, New York, NY, USA
12University of Kansas Medical Center, Kansas City, KS, USA
13Presbyterian St. Luke’s/Rocky Mountain Hospital for Children, Denver, CO, USA
14University of California, San Francisco, CA, USA
Introduction: Health-related quality of life (HRQoL) instruments are essential in a value-driven health care economy. Informed decision-making requires patient comprehension of expected outcomes of surgery. HRQoL measures may be difficult for patients to interpret and appreciate. The purpose of this study was to create a predictive model for individual Scoliosis Research Society–22 (SRS-22) questions at 1 and 2 years after adult spinal deformity (ASD) surgery. Material and Methods: Two prospective observational cohorts were retrospectively queried for ASD patients with SRS-22 data at baseline, 1 year, and 2 years after surgery. A total of 150 covariates were used in the training models and included demographic data, surgical data, and perioperative complication data. Outcomes as answers of the SRS-22r were dichotomized as “good” (4, 5) or “bad” (1-3). Six different prediction algorithms were trained with 3-time horizons: baseline to 1 year, baseline to 2 years, and 1 year to 2 years. External validation was accomplished via an 80/20 data split for training and testing each model, respectively. Goodness of fit was measured using the area under receiver operating characteristic curves (AUROC) in the test set. Variable importance were calculated. Results: A total of 561 patients met inclusion criteria. The AUROC of most models were approximately 75% to 80% indicating successful fits. Items regarding back pain in the past 6 months (q1), level of activity (q5), domestic activity (q12), and feeling attractive with the current back condition (q19) of the SRS-22 questionnaire were most accurately predicted. The models were less sensitive to questions regarding financial difficulties (q15), depression (q16), and days of sick leave or ceasing domestic activity in the past 3 months (q17). Conclusion: Preoperative models to predict answers to each of the SRS-22 questions at 2-year follow-up were created with 75% to 80% accuracy. Items related to pain, function, and self-image were most accurately predicted. The ability to predict individual question responses may be useful in preoperative counseling of patients in the age of individualized medicine.
P134: Development of Deployable Predictive Models for MCID of 2-Year Outcomes Across All Commonly Used HRQOL Instruments in Adult Spinal Deformity Surgery: Results in 570 Patients from 17 Hospitals
Miquel Serra-Burriel1, Ferran Pellisé2, Michael P. Kelly3, Justin S. Smith4, Jeffrey L. Gum5, Ahmet Alanay6, Emre R. Acaroglu7, Francisco Javier Sánchez Pérez-Grueso8, Frank Kleinstück9, Ibrahim Obeid10, Virginie Lafage11, Frank J. Schwab11, Christopher I. Shaffrey4, Douglas C. Burton12, Shay Bess13, Christopher P. Ames14; European Spine Study Group (ESSG)2; International Spine Study Group (ISSG)11
1Universitat Pompeu Fabra, Barcelona, Spain
2Hospital Vall d’Hebron, Barcelona, Spain
3Washington University in St Louis, St. Louis, MO, USA
4University of Virginia Medical Center, Charlottesville, VA, USA
5Norton Leatherman Spine Center, Louisville, KY, USA
6Acibadem University, Istanbul, Turkey
7Ankara ARTES Spine Center, Ankara, Turkey
8Hospital Universitario La Paz, Madrid, Spain
9Schulthess Klinik, Zürich, Switzerland
10Bordeaux University Hospital, Bordeaux, France
11Hospital for Special Surgery, New York, NY, USA
12University of Kansas Medical Center, Kansas City, KS, USA
13Presbyterian St. Luke’s/Rocky Mountain Hospital for Children, Denver, CO, USA
14University of California, San Francisco, CA, USA
Introduction: Adult spinal deformity (ASD) surgery is costly with variable outcomes; in some series, only 50% of patients achieve minimum clinically important difference (MCID) improvements. Predictive analytics may accurately model health-related quality of life (HRQOL) improvements after ASD surgery. Predictive modeling may be useful in shared decision-making and surgical planning. The objective of this study was to model HRQOL overall improvement, including the likelihood of achieving clinically important improvement, at 2 years postoperatively. Material and Methods: Two prospective observational cohorts were queried for ASD patients with SRS-22/ODI/SF-36 v2 (Scoliosis Research Society–22/Oswestry Disability Index/Short Form–36 Health Survey version 2) data at baseline, 1 year, and 2 years after surgery. Seventy-five variables were used in the training of the models including demographic data, enrollment HRQOL, and modifiable surgical data. Eight different prediction algorithms were trained with 3-time horizons: baseline to 1 year, baseline to 2 years, and 1 year to 2 years. External validation was accomplished via an 80/20 data split for training and testing each model, respectively. Fivefold cross validation within the training sample was performed. Accuracy was measured as the mean average error (MAE; smaller is better) and R 2 values. Results: A total of 570 patients were included in the analysis. Models with the lowest MAE for each of the 5 time-points were selected; ultimately the model had 82.4% predictive power. Patients with lower enrollment HRQOL were likely to appreciate the greatest improvements in HRQOL at 2-year follow-up. Addition of surgeon and site to preoperative data increased the predictive power 1.8%. Site- and surgeon-fixed effects played a crucial role in explaining outcome variance. Conclusion: We present an accurate and consistent way of predicting outcome scores for ASD surgery in the largest-to-date prospective operative multicenter cohort with 2-year follow-up. This study has significant clinical implications for shared decision-making, surgical planning, and postoperative counseling. Surgeon and site were important components of the model, explaining variance in predicted 2-year HRQOL.
P135: Minimally Invasive Scoliosis Surgery With Oblique Lateral Lumbar Interbody Fusion: Single-Surgeon Feasibility Study
Hamid Abbasi1
1Tristate Brain & Spine Institute, Minneapolis, MN, USA
Introduction: Degenerative deformities of the spine have traditionally been treated with extensive open surgeries. However, these open procedures are associated with a high degree of surgical morbidity. In this study, we explore whether clinical improvement in patients with spinal deformities can be achieved using a new minimally invasive surgery (MIS) called oblique lateral lumbar interbody fusion (OLLIF). OLLIF is a MIS single-surgeon procedure in which the disc is approached through Kambin’s triangle. OLLIF can achieve correction of spinal deformities through careful cage placement. The purpose of this study is to establish the safety and efficacy of using OLLIF to correct spinal deformities and to collect early outcome data. Collected data include perioperative outcomes, patient-reported outcomes, and radiographic outcomes. Material and Methods: This study is a retrospective review of 37 OLLIF surgeries in 36 patients with symptomatic degenerative spinal deformity. Collected perioperative data included surgery time, blood loss, and hospital stay. Follow-up was conducted at least 150 days postsurgery. We recorded complications and patient-reported outcomes such as Oswestry Disability Index (ODI) and pain scale. Imaging was conducted pre- and postsurgery. Fusion rates and changes in Cobb angle were also measured. Results: A total of 37 surgeries that treated 100 vertebral levels were performed. For 2- and 3-level procedures, respectively, the mean blood loss was 83 and 178 mL, the average surgery time was 74 and 158 minutes, and the average hospital stay was 2.6 and 3.3 days. All the patients, except 2, ambulated within 24 hours. The patients reported pain improvements on the 10-point pain scale from 8.3 to 3.7 (P < .001) and on the ODI from 53% to 32%. Cobb angles decreased from 16° to 9.3° (P < .001), amounting to 2.5° of correction per level of surgery. Detailed imaging was reviewed by independent radiologists for 24 cases and 100% interbody fusion was achieved along with 71% right posterolateral and 74% left posterolateral fusion. There were 3 cases of mild nerve irritation/neuropraxia and no infections. Conclusion: OLLIF is a safe and effective MIS technique to correct adult degenerative scoliosis. Unlike alternative procedures, OLLIF is technically less complex than comparable procedures and can safely be used from the thoracolumbar junction to S1.
P136: Does the Amount of Sagittal Plane Correction in a Posterior Spinal Fusion for Adult Spinal Deformity Have an Impact on the Development of Proximal Junctional Kyphosis?
Bryce Basques1, Jonathan Markowitz1, Jannat Khan1, Michael Nolte1, Michael Berkowitz1, Kamran Movassaghi2, Howard An1, and Christopher Dewald1
1Rush University, Chicago, IL, USA
2University of California, San Francisco,CA, USA
Introduction: Correction of sagittal imbalance has become a pivotal focus in adult spinal deformity surgery. Studies have shown that the overall clinical impact of adult spinal deformity has been largely predicted by the sagittal plane. Proximal junctional kyphosis (PJK) following instrumentation with long posterior spinal fusion remains a common complication in this patient population. The purpose of this study was to evaluate the role of sagittal plane correction on the development of PJK following posterior spinal fusion for adult spinal deformity. Methods: A retrospective cohort study was performed using consecutive patients who underwent a posterior spinal fusion for adult spinal deformity with 2 years minimum follow-up. Patients who previously had a fusion to treat a thoraco-lumbar fracture or infection or were younger than 18 years at the time of surgery were excluded. Radiographic assessments included: sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), thoracic kyphosis (TK), T1 pelvic angle (TPA), and PJK. PJK was defined as kyphosis greater than 10° and more than a 10° increase at 2 levels above the upper instrumented vertebra in the preoperative film. Baseline patient characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare radiographic outcomes between the 2 groups. Multivariate analyses controlled for differences in baseline patient characteristics. To control for multiple statistical comparisons, a Bonferroni correction was used, which lowered the threshold for statistical significance to P < .008. Results: A total of 142 patients with a minimum of 2 years follow-up were included in the study. Average follow-up was 52.8 ± 29.1 months. Average age was 58.7 ± 11.6 years, average body mass index was 28.9 ± 7.7 kg/m2, and 85.3% of patients were female. Using multivariate analysis to control for baseline differences in patient and operative characteristics, greater preoperative to postoperative correction of TK was associated with significantly increased PJK rates (OR = 1.11 per degree, P < .001). An increase of TK from postoperative to final follow-up was associated with PJK development (OR = 1.11, P < .001) on multivariate analysis as well. No significant associations between any other radiographic parameters and the development of PJK were found. Conclusion: In this study, adult spinal deformity patients who had a greater magnitude of correction of TK following posterior spinal fusion had increased rates of PJK. Increased TK may be physiologic for certain patients, and further research should assess the benefits of incomplete correction of TK to accommodate these patients and potentially reduce the development of PJK.
P137: Does the Rod Metal Composition Affect the Odds of Developing Proximal Junctional Kyphosis in Posterior Spine Fusions for Adult Spinal Deformity?
Bryce Basques1, Philip Louie1, Michael Nolte1, Jannat Khan1, Kamran Movassaghi2, Jonathan Markowitz1, Dong Gue Oh1, Howard An1, and Christopher Dewald1
1Rush University, Chicago, IL, USA
2University of California, San Francisco, CA, USA
Introduction: Rods utilized for posterior spinal fusion (PSF) can be made using one, or several, metallic compounds with specific mechanical properties. Long constructs, commonly placed in patients undergoing PSF for adult spinal deformity, carry a large moment arm and place a considerable amount of stress on the rod construct. Varying rod stiffness may play a role in the development of proximal junctional kyphosis (PJK). The purpose of this study was to evaluate the odds of developing PJK and radiographic outcomes following the placement of titanium, stainless steel, or cobalt chrome rod constructs, in patients undergoing PSF for adult spinal deformity. Methods: A retrospective cohort study was performed using patients who underwent elective PSF for adult deformity with a minimum of 2 years of follow-up at a single academic institution from 2008 to 2014. Patients who previously had a fusion to treat a thoraco-lumbar fracture or infection or were younger than 18 years at the time of surgery were excluded. Patients were grouped by type of rod they received: cobalt chrome, stainless steel, or titanium. Radiographic assessments included: sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), thoracic kyphosis (TK), T1 pelvic angle (TPA), and PJK. At 2 levels above the upper instrumented vertebra (UIV + 2), kyphosis greater than 10° and more than a 10° increase from the preoperative film was defined as PJK. Reoperation data were also obtained. Baseline patient characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare radiographic outcomes between the 3 groups. Multivariate analyses controlled for differences in baseline patient characteristics. Results: A total of 125 patients fulfilled inclusion criteria. Average follow-up length was 52.8 ± 29.1 months. There were no significant differences in demographic characteristics between the 3 groups. Average age was 58.5 ± 11.4 years, average body mass index was 29.1 ± 7.7 kg/m2, and 85.4% of patients were male. On multivariate analysis, stainless steel rods had a significantly decreased rate of PJK compared with those with stainless steel rods (OR = 0.3; P = .049), but no significant difference with titanium rods (P = .095). Patients with titanium rods had significantly greater correction of SVA compared with those with cobalt chrome rods (+43.0°; P = .042). Stainless steel had significantly decreased correction of TK compared with those with cobalt chrome rods (−13.9°; P = .002) from preoperative to immediate postoperative radiographs. This significant decrease in TK correction with stainless steel compared with cobalt chrome rods was observed at final follow-up as well (−12.0°; P = .046). There were no other significant differences in preoperative, postoperative, or final radiographic parameters. Reoperation (cobalt chrome 22.0% vs stainless steel 27.5% [P = .338] vs titanium 27.3% [P = .338]) and pseudoarthrosis (cobalt chrome 12.2% vs stainless steel 15.0% [P = .514] vs titanium 15.9% [P = .381]) rates were similar between the 3 groups. Conclusion: Our results indicate that adult spinal deformity patients who underwent PSF with stainless steel rods had decreased rates of PJK at a minimum of 2 years compared with those with cobalt chrome rods.
P138: The Impact of Sagittal Balance and Spinopelvic Parameters on the Development of Proximal Junctional Kyphosis Following Posterior Spinal Fusion for Adult Spinal Deformity
Bryce Basques1, Michael Nolte1, Philip Louie1, Jannat Khan1, Kamran Movassaghi2, Michael Berkowitz1, Joseph Michalski1, Howard An1, and Christopher Dewald1
1Rush University, Chicago, IL, USA
2University of California, San Francisco, CA, USA
Introduction: Achieving global sagittal balance and optimizing spino-pelvic parameters have been found to be important goals for adult spinal deformity correction. The overall impact and outcomes of adult spinal deformity surgery have been largely predicted by the sagittal plane and spino-pelvic relationships. However, proximal junctional kyphosis (PJK) remains a common complication following this procedure. The role of spino-pelvic parameters in the development of PJK remain largely undefined. The purpose of this study was to evaluate the impact of sagittal balance and spino-pelvic parameters on the development of PJK following posterior spinal fusion (PSF) for adult spinal deformity. Methods: A retrospective cohort study was conducted of consecutive patients who underwent elective PSF fusion for adult deformity at a single academic institution from 2008 to 2014 with a minimum of 2 years postoperative follow-up. Patients who previously had a fusion to treat a thoraco-lumbar fracture or were younger than 18 years at the time of surgery were excluded. Radiographic assessments included sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), thoracic kyphosis (TK), and T1 pelvic angle (TPA). PJK was assessed using the 2 most common methods, at 1 and 2 levels above the upper instrumented vertebra (UIV + 1, UIV + 2). At UIV + 1, PJK was defined as a greater than 15° increase from the preoperative film. Using the UIV + 2 method, PJK was defined as kyphosis greater than 10° and more than a 10° increase at 2 levels above the UIV in the preoperative film. Baseline patient characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Bivariate and multivariate logistic regression were subsequently used to test the association between increasing degrees of PI and LL mismatch (>10°, >20°, and >30°mismatch) and development of PJK while controlling for differences in patient and operative characteristics. Results: A total of 142 patients were included. Average follow-up length was 52.8 ± 29.1 months (range = 24-120 months). On multivariate analysis, PJK occurred at a significantly greater rate in patients with a postoperative PI-LL mismatch >10° (UIV + 1 odds ratio [OR] = 4.5, P = .001; UIV + 2 OR = 3.6 P = .008), >20° (UIV + 1 OR = 12.3, P < .001; UIV + 2 OR = 6.3, P < .001), and >30° (UIV + 1 OR = 15.8, P < .001; UIV + 2 OR = 11.3, P < .001) had significantly increased rates of PJK, with a larger mismatch corresponding to greater odds of PJK. Similarly, significantly increased rates of PJK were found with PI-LL mismatch >10°, >20°, and >30° at final follow-up (multivariate P value range <.001-.031). Conclusion: Following PSF for adult spinal deformity, patients who presented with a PI-LL mismatch >10° developed PJK at 4 to 16 times the rate than patients that achieved a PI-LL mismatch <10°, with a larger mismatch corresponding to greater odds of PJK. Special attention should be paid to the amount of sagittal alignment and spino-pelvic parameter correction during surgery in this patient population.
P139: Patients With Osteoporosis Undergoing Deformity Correction Spinal Fusion for Adult Spinal Deformity Are at Greater Risk of Developing Proximal Junctional Kyphosis
Michael Nolte1, Bryce Basques1, Jannat Khan1, Philip Louie1, Kamran Movassaghi2, Jonathan Markowitz1, Oscar Chen1, Howard An1, and Christopher Dewald1
1Rush University, Chicago, IL, USA
2University of California, San Francisco, CA, USA
Introduction: Osteoporosis is a significant comorbidity that can increase the risk and technical difficulty of spine surgery, especially during the correction of adult spinal deformity. Proximal junctional kyphosis (PJK) remains a common complication after long instrumented spinal fusion surgery; however, the relationship with osteoporosis has not been explored. The goal of this study was to compare patients diagnosed with osteoporosis to non-osteoporotic patients and evaluate the occurrence of PJK following deformity correction surgery for adult spinal deformity. Methods: A retrospective cohort study of patients who underwent elective posterior spinal fusion for adult deformity at a single academic institution from 2008 to 2014 was performed. Patients were considered osteoporotic if their bone mineral density (BMD) score revealed T score <−2.5. Radiographic assessments included: sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), thoracic kyphosis (TK), T1 pelvic angle (TPA), and PJK. At two levels above the upper instrumented vertebra (UIV + 2), kyphosis greater than 10° and more than a 10° increase from the preoperative film was defined as PJK. Multivariate logistic regression was used to test the association between osteoporosis and development of PJK while controlling for differences in patient and operative characteristics. Multivariate linear regression was used to test the association of osteoporosis with radiographic measurements. Results: A total of 206 patients fulfilled the inclusion criteria. Average follow-up was 52.8 ± 29.1 months. Patients with osteoporosis were older (64.7 ± 12.6 vs 56.7 ± 8.6 years; P < .001) and less often presented with spinal stenosis (26.7% vs 48.3%; P = .028). Patients with osteoporosis presented with significantly more instances of PJK (80.0% vs 54.5%; multivariate odds ratio [OR] = 3.9, P = .028) compared with those who did not have osteoporosis. Otherwise, there were no other significant findings in the radiographic parameters. Reoperation (osteoporosis 36.7% vs no osteoporosis 27.5%: P = .188) and pseudoarthrosis (osteoporosis 13.3% vs no osteoporosis 16.9%: P = .764) rates were similar between the 2 groups. Conclusion: Patients diagnosed with osteoporosis may be at greater risk of developing PJK following deformity-correction spine fusion for adult spinal deformity compared with those with more robust BMD. These concerns, as well as ultimate health-related quality of life, provide additional support toward the importance of preoperative BMD optimization and expectations prior to surgery.
P140: What Risk Factors Are Associated With Dural Tears During Posterior Spine Fusion for Adult Spinal Deformity?
Michael Nolte1, Bryce Basques1, Jannat Khan1, Philip Louie1, Oscar Chen1, Kamran Movassaghi2, Jonathan Markowitz1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
2University of California, San Francisco, CA, USA
Introduction: Dural tears are a well-known complication faced during posterior spinal fusion procedures. The impact of this complication can be magnified in more extensive spine procedures as long posterior spine fusion in patients with adult spinal deformity. The volume and complexity of spinal surgeries is increasing, leading to a greater prevalence of dural tears. During posterior spinal fusion for adult spinal deformity, patients who have undergone one or more prior spine surgeries are at an increased risk for a dural tear compared with patients with no history of prior of spine surgery. The purpose of this study is to examine if patients with a history of spine surgery or preoperative central stenosis have an increased risk for experiencing a dural tear during posterior spinal fusion for adult spinal deformity. Methods: A retrospective cohort study was performed for consecutive patients who underwent a spinal fusion, by 1 of 2 spine surgeons, from the thoracic spine to the sacrum or pelvis for adult spinal deformity. Patients who previously had a fusion to treat a thoraco-lumbar fracture or infection, postoperative follow-up less than 24 months prior, or were younger than 18 years at the time of surgery were excluded. Patient demographics and intraoperative variables were collected. The presence of a dural tear was diagnosed based on intraoperative findings by the surgical team. Bivariate and multivariate regressions were used to determine factors that were associated with the presence of a dural tear. Multivariate analyses controlled for differences in baseline patient characteristics. Results: A total of 145 patients fulfilled inclusion criteria, of which 18 (12.4%) experienced a dural tear. Our results showed that patients who previously underwent spine surgery were at an increased risk for dural tear compared with those with no prior spine surgery, when baseline characteristics were controlled for via multivariate analysis (odds ratio [OR] = 6.44, P = .038). Patients with central stenosis were also at a greater risk for dural tear compared with those without central stenosis; however, this was not quite statistically significant (OR = 3.28, P = .097). Conclusion: We conclude that during posterior spinal fusion for adult spinal deformity, patients with a history of prior spine surgery had an increased risk of experiencing a dural tear.
P141: The “Soft Landing”: Proximal Laminar Hooks Are Associated With Decreased Rate of Proximal Junctional Kyphosis in Spinal Fusion for Adult Spinal Deformity Compared With Pedicle Screw Fixation
Bryce Basques1, Philip Louie1, Michael Nolte1, Jannat Khan1, Kamran Movassaghi2, Dong Gue Oh1, Joseph Michalski1, Howard An1, Christopher Dewald1
1Rush University, Chicago, IL, USA
2University of California, San Francisco, CA, USA
Introduction: Proximal junctional kyphosis (PJK) is a significant concern following long posterior spinal fusion. Biomechanically, the placement of hooks at the upper instrumented vertebra (UIV) has been shown to allow a more gradual transition to normal motion, compared with pedicle screws in a long posterior instrumented spinal fusion. The purpose of this study was to evaluate the risk of developing PJK with sublaminar hooks versus pedicle screw fixation at the UIV of a posterior spine fusion for adult spinal deformity. Methods: We conducted a retrospective cohort study of consecutive patients who underwent elective posterior spinal fusion for adult deformity at a single academic institution from 2008 to 2014 with a minimum of 2 years of follow-up. Patients with proximal hooks and those with proximal screws were separated into 2 groups. Preoperative, initial postoperative, and final postoperative standing full-length spine radiographs were reviewed. Radiographic assessments included: sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), thoracic kyphosis (TK), T1 pelvic angle (TPA). PJK was assessed using the 2 most common methods, at 1 and 2 levels above the UIV (UIV + 1, UIV + 2). At UIV+1, PJK was defined as a greater than 15° increase from the preoperative film. Using the UIV+2 method, PJK was defined as kyphosis greater than 10° and more than a 10° increase at 2 levels above the UIV in the preoperative film. Multivariate logistic regression was used to test the association between proximal hooks or pedicle screws and the development of PJK while controlling for differences in patient and operative characteristics. Results: A total of 142 patients with minimum 2 years follow-up were included. Average follow-up length was 52.8 ± 29.1 months (range = 24-120 months).The proximal hooks group had more males (93.9% vs 79.8%; P = .027), and a lower rate of ASA (American Society of Anesthesiologists) 3 and above (38.0% vs 60.9%; P = .009). On multivariate analysis, patients with sublaminar hooks at the UIV presented with lower rates of PJK using UIV+1 (odds ratio [OR] = 0.34; P = .027) and UIV+2 (OR = 0.36; P = .048) measurements compared with those who received pedicle screws at the UIV (Table 2). Patients with proximal laminar hooks had greater preoperative TK (+9.6°, P = .015), but similar postoperative TK (P > .05). Proximal laminar hooks also had better postoperative SVA (−35 mm, P = .044) and final SVA (−49 mm, P = .005) compared with pedicle screws. Reoperation and pseudoarthrosis rates were similar between the 2 groups (P > .05). Conclusion: Laminar hooks at the UIV were associated with reduced rates of PJK compared with pedicle screws in patients who underwent deformity-correcting spine fusion for adult spinal deformity. When planning proximal fixation, this information may be useful, in association with other factors, to minimize the occurrence of PJK after adult deformity surgery.
P142:Effect of Tobacco Smoking on Outcomes of Complex Spine Deformity Correction: Analysis of 270 Patients From the Prospective, Multicenter Scoli-RISK-1 Study of Complex Adult Spinal Deformity Surgery
Jamie R. F. Wilson1, Fan Jiang1, Jetan H. Badhiwala1, Leah Y. Carreon2, Kenneth M. C. Cheung3, Benny T. Dahl4,5, Christopher I. Shaffrey6, Stephen Lewis1, Lawrence G. Lenke7, and Michael Fehlings1
1Toronto Western Hospital, Toronto, Ontario, Canada
2Norton Leatherman Spine Centre, Louisville, KY, USA
3University of Hong Kong, Hong Kong, SAR China
4Texas Children’s Hospital, Houston, TX, USA
5Baylor College of Medicine, Houston, TX, USA
6Duke University, Durham, NC, USA
7The Spine Hospital, Columbia University Medical Center, New York, NY, USA
Introduction: Tobacco smoking has been identified in retrospective studies as a predictor for complications after adult deformity surgery; however, little is known regarding the effect of smoking on patient-reported outcomes after spinal deformity surgery. The goal of this study is to analyze the impact of smoking on generic and disease-specific outcomes in patients undergoing high-risk adult spine deformity surgery. Material and Methods: The Scoli-RISK-1 study enrolled 272 patients who had undergone high-risk complex adult spinal deformity surgery from 15 centers, with a follow-up of 2 years. Outcome measures (Short-Form–36 [SF-36], Scoliosis Research Society [SRS]-22, Oswestry Disability Index [ODI] scores, and back/leg pain Numerical Rating Scale [NRS]) in patients with a history of tobacco smoking (n = 26) were compared with the nonsmoking patients (n = 244) using a mixed effects model for repeated measures with an unstructured covariance. The Wilcoxon rank sum test was used to compare leg pain NRS scores. Results: No difference was observed in the number of levels or complexity of surgery in both cohorts. At 6 weeks post-surgery, the nonsmoking group demonstrated a significantly higher SF-36 mental component score (44.6, 95% CI [42.8-46.4]) compared with the smoking group (37.7, [32.2-43.3]; P = .021), but this effect was not maintained at 6 months and 24 months (46.8 [45.0-48.7] vs 43.3 [37.7-49.0], P = .248; 47.2 [45.4-49.1] vs 45.6 [39.6-51.6], P = .605). ODI scores were similar between both groups at 6 weeks (48.3 [45.9-50.7] vs 47.3 [39.9-54.8]; P = .802), 6 months (35.3 [32.7-37.8] vs 38.9 [31.2-46.6]; P = .377), and 24 months (32.4 [29.6-35.2] vs 37.5 [28.7-46.3]; P = .281). The mean change in scores between baseline SF-36 physical component, SF-36 mental component, SRS-22 score, ODI, and pain NRS were not significantly different between groups at the 6-week, 6-month, or 24-month follow-up intervals. The median leg pain NRS scores were significantly lower in the nonsmoking group at 6 weeks (1.00 vs 3.50; P = .020), but this effect was no longer significant at 6 months and 24 months (1.00 vs 2.00, P = .103; 2.00 vs 3.00, P = .206). The median change in leg pain NRS scores from baseline was not significant between the groups at any follow-up interval (6 weeks = −1.00 [range = −10.00 to 8.00] vs −1.00 [−6.00 to 5.00], P = .604; 6 months −1.00 [−10.00 to 8.00] vs −1.00 [−7.00 to 8.00], P = .834; 24 months 0.00 [−10.00 to 8.00] vs 0.00 [−5.00 to 6.00], P = .652). Conclusion: In this large, multicenter prospectively collected study, patients with a history of smoking reported similar outcomes to nonsmoking patients at baseline, 6-week, 6-month, and 24-month postoperative intervals. At 6 weeks, the smoking group had significantly worse scores for 2 outcome measures, but the changes in mean scores from baseline for each outcome measure across 2 years were not significant. In conclusion, short-term outcomes may be adversely affected by smoking status, where outcomes at long-term follow-up are similar between smokers and nonsmokers. The authors accept that this sub-analysis was likely underpowered to measure the true effects of smoking; nonetheless, we advise patients who smoke undertake an active smoking cessation program prior to undergoing complex adult spinal deformity surgery.
P143: Determinants of Postoperative Spinal Height Change Among Adult Spinal Deformity Patients with Long Construct Circumferential Fusion
Colleen Rentenberger1, Ichiro Okano1, Stephan N. Salzmann1, Toshiyuki Shirahata2, Jennifer Shue1, Andrew A. Sama1, Frank P. Cammisa1, Federico P. Girardi1, and Alexander P. Hughes1
1Hospital for Special Surgery, Weill Cornell Medical College, New York, NY, USA
2Showa University, Tokyo, Japan
Introduction: Spinal corrective surgeries can affect body height and this height change can be a potential concern of patients. Previous studies have only focused on young patients with adolescent idiopathic scoliosis (AIS). Whereas recent advances of surgical technique and implants allow surgeons to treat more challenging adult spinal deformity (ASD) cases surgically, it is still unknown whether AIS height change results can be applied to ASD cases. The aim of this study was to examine predictive factors of spinal height (SH) among ASD patients who underwent circumferential lumbar fusion with instrumentation. Material and Methods: We retrospectively reviewed clinical and imaging data of ASD patients who underwent lumbar corrective circumferential fusion (combined anterior and posterior approaches) of 3 or more levels between 2007 and 2018 at a single academic institution (n = 106). SH was defined as the vertical distance between the midpoint of the C2 endplate and the horizontal line from the posterosuperior aspect of the S1 endplate on a standing lateral image. Height change was calculated as the difference between preoperative and postoperative SH measurements from whole spine lateral radiographs. As potential predictors of height change, the number of lateral lumbar interbody fusion (LLIF) levels, change in spino-pelvic parameters, total number of levels fused, and pedicle subtraction osteotomies (PSO) were documented. Univariate and multivariate linear regression analyses were performed to identify predictors of postoperative height change. Results: The mean age (± standard deviation [SD]) of the 106 patients was 64.9 ± 9.6 (range = 33-82). The mean SH change was −2.39 mm ± 50.8 mm (range = −160 to 172). The univariate analyses showed that the number of LLIF levels (coefficient = 10.9, P = .03), the absolute coronal vertical axis (CVA) change (coefficient = 0.6, P = .01), and the absolute Cobb angle change (coefficient = −0.9, P = .03) were significant predictors for height change. Patients with PSO (n = 14) tended to have a shorter height postoperatively (coefficient = −26.1), but this was not statistically significant (P = .07). Multivariate analyses conducted variables with P < .20 (sex, absolute amounts of CVA and Cobb change, pelvic tilt [PT] change, LLIF levels, and PSO) showed that PT change is an independent contributor to SH change (coefficient = −0.99, P = .04, R 2 = 0.11). Conclusion: In this study, we utilized a modified definition of SH used in previous ASI studies to include characteristics of ASD. The results of our study demonstrated that patients with ASD can lose SH postoperatively, which is less likely to occur in AIS patients. We found that PT change was an independent contributor of SH change. Further investigations with greater numbers are needed to identify the impact of SH change on patients’ clinical outcomes and satisfaction of the treatment.
P144: Incidence and Risk Factors for Multiple Medical Complications in Adult Degenerative Scoliosis Long-Level Fusion
Yong Hai1 and Xinuo Zhang1
1Beijing Chaoyang Hospital, Capital Medical University of China, Beijing, China
Introduction: Adult degenerative scoliosis (ADS) surgery is known for its high incidence of complications. The propose of this study was to determine current complication rates and the predictors of medical complications in surgically treated ADS patients. Material and Methods: A retrospective study of 153 ADS patients who underwent long-level spinal fusion with 2-year follow-up between 2012 and 2017 was conducted in our department. The patient- and surgical-related risk factors for each individual medical complication were identified by using univariate testing. All patients were divided into groups with and without medical complication, infection, neurological complications, and cardio-pulmonary complications, respectively. Potential risk factors were identified using univariate testing. Multivariate logistic regression was used to evaluate independent predictors of medical complications. Results: The total medical complication incidence was 26.1%. Patient-related independent risk factors for the development of medical complications included diabetes, smoking; for infection were diabetes and smoking; for neurological complications were body mass index (BMI) and diabetes; and for cardiopulmonary complications were hypertension, smoking, and cardiac comorbidity. Surgical-related independent risk factors for the development of medical complications were fusion level, operative time, osteotomy, blood transfusion, and length of hospital stay (LOS); for infection were fusion level, blood transfusion, and LOS; for neurological complication were fusion level, osteotomy, and blood transfusion; and for cardiopulmonary complications were fusion level. Diabetes and smoking were the most common patient-related independent risk factors that increase the development of each individual medical complication. On the other hand, fusion levels and blood transfusion were the most common surgical-related independent risk factors that increase the development of each individual medical complication. Prevention of these risk factors can reduce the incidence of complications in Chinese patients with ADS surgery. Conclusion: Risk factor analysis of medical complications improved our ability to predict an individual’s risk profile result in better medical optimization for surgery ultimately safer.
P145: Increased Pelvic Tilt/Sacral Slope May Play an Important Role in the Pathogenesis of Lumbar Spondylolisthesis With Degenerative Lumbar Scoliosis
Jinlei Zhang1 and Yong Hai2
1Zhoukou City Central Hospital, Xinxiang Medical University, Zhoukou, China
2Beijing Chaoyang Hospital, Capital Medical University of China, Beijing, China
Introduction: Recently, many authors have suggested the role of sacro-pelvic morphology and balance in the pathogenesis of various spinal disorders, including degenerative spondylolisthesis, adolescent idiopathic scoliosis, and adult spinal deformity. However, there have been few studies specifically describing the sacro-pelvic morphology and balance in patients with lumbar spondylolisthesis and degenerative lumbar scoliosis (LSDLS), especially patients with spondylolysis. To explore the clinical and spinopelvic features in patients with LSDLS and those with stand-alone lumbar spondylolisthesis (SALS). Material and Methods: We retrospectively analyzed 130 patients with lumbar spondylolisthesis seen between May 2013 and December 2016 in our hospital. Propensity score matching was used to reduce an age distribution imbalance between the 2 groups. Clinical and spinopelvic parameters were compared by independent-samples t test and chi-square test. Nonlinear binary logistic regression analysis was used to analyze the independent factors. Results: There was no significant difference between groups for body mass index, level of inter-crest line, level of spondylolisthesis, grade of spondylolisthesis, sagittal translation, segmental angulation, thoracic kyphosis, or sagittal vertical axis. The LSDLS group had significantly lower lumbar lordosis (LL) than the SALS group. The LSDLS group showed significantly greater pelvic tilt (PT) and ratio of PT to SS (sacral slope) (PT/SS), and lower SS. The PI (pelvic incidence) was not significantly different. The LSDLS group showed stronger significant differences in PT/SS compared with the SALS group. With each 0.1 increase in PT/SS, the risk of LSDLS increased 1.465 times. Conclusion: Patients with spondylolysis are less prone to development of DLS. Lower LL and SS and higher PT are associated with the occurrence of LSDLS. Increased PT/SS may play an important role in the pathogenesis of LSDLS.
P146: Factors Associated With a Marked Adult Sagittal Deformity: A Cohort-Based Risk Factor Analysis
Dalsung Ryu1 and Seung-Hwan Yoon1
1Inha University Hospital, Incheon, Republic of Korea
Introduction: Adult spinal deformity is deemed the result of accumulated degenerative process. However, the pathogenesis of adult spinal deformity has not been fully understood until now. This study was conducted to compare the predisposing factors in patients with nonpathologic, moderate deformity versus marked deformity and determine which is the key factor for marked sagittal deformity. Material and Methods: This study was a retrospective analysis of prospectively collected data on patients with ASD. According to global sagittal alignment of the SRS-Schwab classification, total 124 patients were divided into non pathologic, moderate deformity (sagittal vertical axis [SVA] < 9.5 cm) versus marked deformity (SVA > 9.5 cm). Sagittal alignment and pelvic parameter were measured at standing whole spine X-ray. Lumbar spine magnetic resonance imaging (MRI) were reviewed to evaluate following predisposing factors; disc degeneration using Pfirrmann scale at all lumbar segments, disc protrusion or extrusion, moderate to severe canal stenosis, preexisting fracture, spondylolisthesis, Modic endplate change. Cross-section area (CSA) and fatty infiltration by Goutallier classification were measured to demonstrate quantity and quality of multifidus (MF), erector spinae (ES), and psoas muscles (PS). Results: Demographics of marked deformity groups revealed quite different female dominant, lower height and weight, lower lumbar bone mineral density (BMD) than that of mild to moderate deformity group although age was similar (P < .05). Pfirrmann disc degeneration grading were higher at all lumbar discs with marked deformity group (P < .05). And marked deformity group showed higher fatty infiltration grading and lower CSA in MF, ES, and PS (P < .05). Preexisting fracture, L5/S1 disc degeneration, and smaller CSA of MF and PS demonstrated correlation with marked deformity group with multivariate logistic regression analysis (OR = 7.79, 1.91, and 0.99; 95% CI 1.527-39.768, 1.086-3.382, 0.991-0.998, and 0.994-0.999). Conclusion: Marked deformity group showed statistically different characteristics with mild to moderate deformity group. Especially, smaller CSA of MF and PS, higher L5/S1 Pfirrmann grading, and preexisting VF were associated with marked deformity group.
P147: Stage Correction of Adult Spinal Deformity With the Use of Minimally Invasive Technologies
Vladimir Klimov1, Ivan Vasilenko1, and Alexey Evsyukov1
1 Novosibirsk, Russian Federation
Objective: To study the results of treatment of patients with adult spinal deformity who were underwent by lateral lumbar interbody fusion (LLIF), anterior lumbar interbody fusion (ALIF), and minimally invasive surgery (MIS) posterior fixation procedure. Materials and Methods: Ninety-five patients with adult spinal deformity (ASD) from January 2014 to October 2017 (24 men and 71 women). The patients’ age was from 53 to 82 years old (average age was 61.8/62 [57; 64]). The follow-up 12 months after: X-ray study, SCT, and MRI of lumbar spine. Questionnaire: visual analogue scale (VAS), Oswestry Disability Index (ODI) and the Short Form-36 (SF–36). Scoliosis was classified according to SRS (Scoliosis Research Society)-Schwab classification. Parameters of sagittal balance were estimated: PI (pelvic incidence), SS (sacral slope), PT (pelvic tilt), LL (lumbar lordosis), SVA (sagittal vertical axis), SSA (spino sacral angle), segment angle L4-S1. Eighty-one patients underwent LLIF procedure with MIS posterior fixation. Six patients were operated by ALIF method with MIS posterior fixation. The combination of the LLIF, ALIF, and MIS posterior fixation methods was 8 cases. Results: Twelve months after the surgery decrease of leg pain according to VAS from 5.4/5 [4; 8] till 2.5/3 [2; 3] scores (P = .002468), it was statistically significantly noted. Also, decrease of back pain according to VAS from 6.4/7 [4;8] till 2.2/2 [2;2] scores (P = .003736) was statistically significant 12 months after the surgery. It was observed improvement of functional adaptation according to ODI from 46.6/44.5 [35.4;54.3] till 32.6/32.5 [28;35.5] (P = .03979). According to SF-36, PH before the surgery in average was 24.9/22.7 [22.2; 27.8] scores, 12 months after the surgery was 37.5/38.7 [35.2;39.8] (P = .0002441). MH in average 27/26.5 [20.7; 32.3] scores, 12 months later was 39.2/40.6 [36.6; 40.9] (P = .0002441). LL before the surgery was 37.4°/40° [27°; 47°], 12 months later it was LL was 51.8°/53° [46°; 59°] (P = .009577). PT before the surgery was 22.2°/20° [18°; 23°], 12 months later it was 16.6°/18° [15°; 20°] (P = .02456). PI-LL was 14.8°/14° [8°; 24°], 12 months later 1.5°/2° [−5°; 7°] (P = .009577). SSA before the surgery was 116.6°/114° [107°; 126°], 12 months later 127.5°/130° [124°; 132°] (P = .007097). SVA was 56.2/50 [38; 87] mm, after the surgery 0.4/2 [0;18] mm (P = .002358). Segment angle L4-S1 was 22.8°/25° [19°; 30°], 12 months later 32.2°/35° [29°; 36°] (P = .01664). Deformation Cobb angle before the surgery was 22.6°/23° [13°; 31°], during check-up examination it was 4.7°/5° [2°; 6°] (P = .00164). Conclusion: ALIF and LLIF in combination with MIS transcutaneous, transpedicular fixation provides restoration of impaired vertebral-pelvic relationships in the sagittal and frontal planes in patients with ASD. After combined MIS, significantly there were fewer early and late postoperative complications, less intraoperative blood loss, and shorter time of hospital stay.
P148: L5 Corpectomy and Reconstruction: A Systematic Review of Outcomes Following Conventional 2-Stage Posterior-Anterior, Anterior-Only, or Posterior-Only Approaches
Daniel D’Aquino1, Aaron Hilis1, Nigil Sadanandan2, Kedar Deogaonkar2, and Nasir Quraishi1
1Queen’s Medical Centre, Nottingham, UK
2P.D. Hinduja National Hospital and Medical Research Centre, Mumbai, Maharashtra, India
Introduction: Surgical approaches to pathologies of the L5 vertebra constitute a significant challenge on account of the anatomical features of the lumbosacral junction. There is some consensus in the literature regarding the conventional wisdom of a 2-stage combined posterior-anterior procedure to offer early and effective stabilization of the spine. There are, however, acknowledged problems with comprehensive 360° reconstruction strategies in terms of a significantly higher risk of major complications, blood loss, and length of stay in comparison to anterior- or posterior-only procedures. To date, there have not been any systematic attempts to synthesise the evidence in the literature to compare the relative safety and efficacy of anterior- or posterior-only approaches versus conventional 2-staged approaches to L5 reconstruction. Materials and Methods: A systematic review of the English language literature was undertaken for articles published between 1970 to March 2018. Electronic databases and reference lists of key articles were searched to identify studies evaluating surgical approaches and outcomes for L5 corpectomy and reconstruction across the range of presenting pathologies. Cases regarding the management of multi-segment pathology of the lumbosacral junction were excluded. The presentation and reporting of the findings followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two independent reviewers assessed the quality and level of evidence according to established Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria and disagreements were resolved by consensus. Results: We identified 5 articles meeting our inclusion criteria. Overall, all 3 surgical approaches shared high fusion rates (94%) and relatively low complication rates. There were no instances of neurological injury reported for either anterior or posterior approaches to L5 corpectomy. However, surgical strategies incorporating an anterior approach were notable for vascular complications (4% to 7%) as well as perioperative mortality (9%) not seen in the posterior-only surgery group. The burden of perioperative complications almost exclusively related to the anterior surgical approach. Blood loss was also notably much higher for the 2-stage posterior-anterior surgery group (mean = 3.2 L) than the posterior-only surgery group (mean = 744 mL). Conclusions: The strength of evidence presented in this systematic review is limited by its source data solely originating in case series. Nevertheless, there appears to be a fairly consistent finding of good fusion rates in association with relatively low complication rates across all studies and surgical strategies. Ultimately, when considering the appropriate surgical strategy for L5 pathology, the individual patients’ anatomical and pathological considerations are paramount, as is the operating surgeon’s level of experience and comfort of the anterior anatomy of the lumbosacral junction. However, where there is clinical equipoise regarding the choice of an anterior-incorporating versus posterior-only surgical access strategy, this current review indicates an advantage in the posterior-only strategy in terms of lower complication rates, blood loss, and time-to-mobilization without apparent compromise to fusion and construct stability.
P149: Two Different Types of Stooping Posture After Sacropelvic Fixation for Degenerative Sagittal Imbalance
Hyung-Youl Park1, Young-Hoon Kim1, Kee-Yong Ha2, Sang-Il Kim2, and Jun-Hyung Cho2
1Seoul St. Mary’s Hospital, Seoul, Republic of Korea
2The Catholic University of Korea, Seoul, Republic of Korea
Introduction: Rigid lumbosacral fusion with iliac screw fixation has been recommended to reduce stooping posture. However, few studies have addressed stooping posture without proximal junctional kyphosis (PJK) and with PJK, which are different types of sagittal malalignment after sacropelvic fixation. The purpose of this study is to investigate different risk factors between stooping posture without PJK and with PJK after long instrumented fusion with sacropelvic fixation in degenerative sagittal imbalance (DSI). Material and Methods: Eighty patients who had undergone surgical correction for DSI were included. Univariate and multivariate analysis for clinical and radiological factors including paravertebral muscles were conducted for respective risk factors. In subgroup analysis, the comparison including clinical outcomes was evaluated between 2 different stooping postures. Results: Forty patients (50%) developed stooping posture. Out of these, 22 patients developed PJK (27.5%) and stooping posture without PJK in 18 patients (22.5%). The independent risk factors in global stooping posture were more fusion levels (hazard ratio [HR] = 3.109), less change in sacral slope (SS) (HR = 1.221), and less change in thoracic kyphosis (HR = 1.264), while great postoperative pelvic tilt (HR = 1.105) and less change in SS (HR = 1.084) in PJK. Global stooping group was found in patients who had undercorrection of sagittal parameters such as changes in lumbar lordosis (LL), postoperative PI (pelvic incidence)-LL, postoperative sagittal vertical axis (SVA), and optimal correction as well as paravertebral muscle weakness directly compared with PJK group. Regarding clinical outcomes, the back visual analog scale (VAS) at last follow-up was significantly higher in PJK group and reoperations were also different. Conclusion: Undercorrection of sagittal parameters was a risk factor of both stooping posture without and with PJK. Global stooping posture was significantly associated with lesser correction of sagittal alignment in conjunction with weakness of the paravertebral muscles. Clinical outcomes were also significantly different between 2 groups.
P150: Spinal Sharp Angel Deformity: Why Without Using Titanium Mesh as Support in Posterior Vertebral Column Decancellation
Yan Wang1, Guoquan Zheng1, Tianhao Wang1, Xuesong Zhang1, and Zhijun Xin1
1Chinese Peoples’ Liberation Army General Hospital, Beijing, China
Introduction: To explore the safety and effectiveness of bony cage rather than titanium mesh in posterior vertebral column decancellation (PVCD) in the management of spinal sharp angel deformity. Material and Methods: Prospective analysis of 17 patients with spinal sharp angel deformity underwent PVCD from March 2011 to August 2014, with a minimum follow-up of 2 year and a maximum follow-up of 6 years. There were 10 males and 7 females with an average age of 29.3 ± 5.8 years old. Among them, the number of apical vertebrae located in thoracic region, thoracolumbar region and lumbar region was 7, 9 and 1, respectively. 3 patients were in grade C, 4 patients were in grade D and 10 patients were in grade E according to ASIA scale. The perioperative data were recorded, which included preoperative Cobb angle, postoperative Cobb angle, final follow-up Cobb angle, apical vertebrae, the length difference of anterior column and posterior column, operation time, perioperative blood loss and complications. Results: The average operation time was 339.2 ± 62.6mins. The average blood loss was 2172.5 ± 839.2ml. Complications were noted in 6 patients. 3 cases were complicated with transient neurological deficits and 3 cases with cerebrospinal fluid (CSF) leak. The kyphosis Cobb angle decreased from 119.8° ± 13.8° to 19.2° ± 7.4°, with a correction rate of (84.0 ± 4.6)%. The average time of follow-up was 36.2 ± 7.9 months. The Cobb angle was 25.1° ± 7.4°, and the loss of correction was 5.7% in the final follow-up. The anterior column increased by 4.8 ± 2.5cm while posterior column shortened by 3.1 ± 1.5cm. Among 6 patients with preoperative neurological deficit, 3 patients with ASIA C improved to ASIA D, 3 patients improved from ASIA D to ASIA E, one patient with ASIA D did not recover in the last follow-up. Conclusion: PVCD without using conventional titanium mesh is a safe and effective option for spinal sharp angel deformity.
P151: Clinical and Radiographic Outcomes of PSO Combined With SPOS for Adult Spinal Deformity With Severe Sagittal Plane Imbalance: A Minimum 2-Year Follow-Up Study
Xudong Hu1 and Weihu Ma1
1Ningbo No. 6 Hospital, Ningbo, China
Introduction: As modern analysis of adult spinal deformity (ASD) has correlated sagittal imbalance with pain, inability to stand upright, and fatigue with increased activities, realignment of sagittal imbalance has become essential for spinal reconstruction. Pedicle subtraction osteotomy (PSO) and Smith-Petersen osteotomies (SPOs) are the most commonly used surgical procedures for correction of the fixed sagittal imbalance. To our knowledge, no articles have been published that analyze the treatment of ASD with severe sagittal plane imbalance by one level PSO combined with SPOs, so we aim to evaluate the safety and efficacy of these procedures for this kind of patients. Material and Methods: This is a retrospective study of 35 patients with severe sagittal plane imbalance due to ASD who underwent single-level PSO combined with SPOs between January 2011 and January 2015, the operative time, blood loss, and perioperative complications were documented, spinal-pelvic radiographic parameters were measured and compared preoperative, postoperative, and at the final follow-up (minimum of 2-year), including sagittal vertical axis (SVA), lumbar lordosis (LL), pelvic tilt (PT), sacral slope (SS), and mismatch between pelvic incidence and LL (PI-LL). The Oswestry disability index (ODI) was used to evaluate the clinical efficacy. Results: The mean total operative time was 362.2 ± 57.3 minutes, the blood loss during surgery and vir drainage was 1198.2 ± 255.7 mL and 780.1 ± 126.5 mL, respectively. No serious complications happened during the perioperative period, 7 patients (20%) had transient neurological deficit and recovered within 6 months. The average follow-up period was 29.3 ± 7.5 months (range = 26-52 months). There was a significant improvement in SVA, LL, SS, PT, and PI-LL (P < .05) from preoperative to postoperative and preoperative to final follow-up. The ODI score significantly decreased from 45.3% ± 13.6% preoperative to 22.6% ± 3.29% at the final follow-up (P < .05). Conclusion: Single-level PSO combined with SPOs is effective to realignment ASD with severe sagittal plane imbalance, and the quality of life can be improved.
P152: Complication Rate After Degenerative Scoliosis Surgery at a District General Hospital
Kathryn Ramshaw1, Anne-Marie Rowley1, James Hadfield1, and Palaniappan Lakshmanan1
1 City Hospitals Sunderland, East Boldon, UK
Introduction: Degenerative scoliosis can seriously mpact a person’s quality of life and affect their health. Surgical correction is known to improve function, however, due to the complex nature of such cases, and with an aging population, perioperative complications can occur and be of serious concern. Proximal junctional failure/kyphosis is a common clinical pathology in this patient group and often necessitates revision surgery. The purpose of this study is to analyze the complication rate after degenerative scoliosis surgery at a district general hospital; considering intraoperative complications, postoperative complications, and complications found at a follow-up clinic. Materials and Methods: Between March 2011 and September 2017, 23 patients with degenerative scoliosis had correction surgery in a district general hospital. Data relating to intraoperative complications, postoperative complications, and complications found at a follow-up clinic were entered prospectively into a local database in the hospital. Complications was classified as major or minor using Glassman’s accepted list of complications. Results: No major or minor complications occurred intraoperatively; although 2 patients had decreased monitoring intraoperatively with no postoperative neurological deficit. In the postoperative period, there were no minor complications, while 22% of patients suffered major complications, which were resolved prior to discharge. In follow-up clinics, no minor complications were found, while 43% of patients had major complications. Twenty-two percent of patients had junctional kyphosis. Thirteen percent of patients went on to have revision surgery. Conclusion: In this complex patient group while major complications are common in the follow-up period, the need for revision surgery is low. Postoperative major complications are fairly common in these patients who have had complex and extensive surgeries. All postoperative complications were noted to relate to hypotension or low hemoglobin and were resolved appropriately prior to discharge. Of the 43% of major complications found at clinic follow-up, 1 related to the discovery of a deep vein thrombosis while the others were attributed to instrumentation or junctional failure. The outcome of this study is in line with existing evidence these complex surgeries, demonstrating that a District General Hospital is suitable for degenerative scoliosis correction.
P153: Mechanical Complications in Adult Spinal Deformity Surgery: Can the Alignment Explain Everything?
Alisson R. Teles1, W. Bradley Jacobs2, Fred H. Nicholls2, Kenneth C. Thomas2, Ganesh Swamy2
1McGill University, Montreal, Quebec, Canada
2 University of Calgary, Calgary, Alberta, Canada
Introduction: Restoration of normal sagittal alignment is a critical goal in adult spinal deformity (ASD) surgery to achieve favorable outcomes. Mechanical complications including the radiographical and implant-related remain a challenge for the spinal deformity surgeon. It has been proposed that these complications are related to the postoperative spinal alignment. Recently, the European Spine Study Group described and validated the Global Alignment and Proportional (GAP) score, which is a predictive score based on postoperative spinal alignment that predicts mechanical complications in ASD surgery. The authors suggested that setting patients to sagittal parameters according to the GAP score could decrease rate of mechanical complications in this population. Our goal was to verify the accuracy of the GAP score in predicting mechanical complications in ASD surgery. Material and Methods: Retrospective review of consecutive primary ASD cases who underwent deformity correction in the same institution over a 5-year period. Inclusion/exclusion criteria and definition of complications were similar to the original study describing the GAP score. Only primary (no-previous fusion) ASD (scoliosis >20°, sagittal vertical axis [SVA] > 5 cm, pelvic tilt [PT] > 25°, and/or thoracic kyphosis [TK] >60°) who underwent 4 or more levels fusion were included. From 112 patients with primary ASD identified during the study period, 11 patients were excluded because of absence of adequate radiological assessment and 17 patients without minimum follow-up of 6 months (N = 84). Fifty-three patients had at least 2 years follow-up. For assessment of proximal junctional pathology and other mechanical complications, a minimum of 6 months and 2 years was established, respectively. Results: A total of 84 patients were included, with a mean age of 65.04 (±9.41), and 69% were female. First standing X-ray showed a matched PI-LL in 81% of patients. Only 3 patients in this cohort underwent 3-column osteotomy in the index surgery. Upper instrumented vertebra (UIV) was L1-L2 in 7.2%, T11 in 28.6%, T10 in 48.8%, T9 in 6%, and upper thoracic spine in 9.6%. LIV (last inferior instrumented vertebra) was L4 in 1.2%, L5 in 1.2%, S1 in 17.9% and pelvis in 79.8%. Cement augmentation of the UIV and UIV+1 was performed in 19% of cases. Mechanical complications occurred in 58.3% of patients, including proximal junctional kyphosis (45.2%), proximal junctional failure (25%), rod breakage (10.7%), pseudoarthrosis at L5-S1 (21.4%), and other implant-related complications (20.2%). According to GAP score, 52.3% of patients were proportioned, 27.3% moderately disproportioned, and 20.4% severely disproportioned postoperatively. The incidence of mechanical complications was similar in each group (proportioned: 59.1%, moderately disproportioned: 56.5%, and severely disproportioned: 58.8%; P = .979). Risk factors for pseudoarthrosis at L5-S1 were absence of iliac fixation (adjusted odds ratio [OR] = 6.19; P = .004) and TLIF (transforaminal lumbar interbody fusion) 51 (in comparison with anterior-based approaches, adjusted OR = 4.18; P = .04). Mechanical complications were associated with first X-ray showing PT > 20 (P = .036), and SVA > 4 cm (P = .011). Conclusion: This external validation study do not support the use of GAP score as a predictor for mechanical complication in ASD surgery.
P154: Lateral Lumbar Inter-Body Fusion in Lumbar Adult Deformities: Fusion Rate and Results
Alessandro Ramieri1, Stefano Forcato2, Sokol Trungu2, Alessandro Pesce3, Pietro Familiari3, Massimo Miscusi3, Giuseppe Costanzo1, and Antonino Raco3
1Sapienza University of Rome, Rome, Italy
2Cardinal Panico Hospital, Tricase, Italy
3Sant’Andrea Hospital, Sapienza University of Rome, Rome, Italy
Introduction: From literature, fusion rate of lateral lumbar inter-body fusion (LLIF) cages, assessed by computed tomography (CT) scan, ranged between 85% and 93%. Aims of our study were the following: to estimate inter-body fusion by 3-dimensional (3D) CT scan in LLIF procedures for adult lumbar deformities; to evaluate clinical results related to fusion quality. Materials and Methods: Eighty LLIFs (62 titanium, 18 peeks) performed in 55 adult degenerative lumbar scoliosis and spondylolisthesis were evaluated by 3D CT scan at least 1 year follow-up, distinguishing complete fusion (Grade 2), partial (G1), and pseudoarthrosis (G0), as well as subsidence and/or mobilization. Patients were also clinically evaluated with VAS (visual analogue scale) and ODI (Oswestry Disability Index) scores and clinical results such as the quality of different bone grafts (bovine bone mineral and collagen; calcium phosphate granules or paste; and paste of demineralized bone matrix) were analyzed in relation to the degree of fusion. Results: We recorded 75% G2 fusion, prevalent by bovine bone mineral plus collagen, 19% G1, and 6% pseudoarthrosis. Pseudoarthrosis involved 3 titanium and 2 peek cages. Particularly exposed to subsidence or settling were middle cages in 3-level of LLIFs. The worst clinical outcome was related to pseudoarthrosis cases with loss of segmental correction. Conclusions: The rate of fusion in our case series, consisting of only adult deformities, at 1 year follow-up, was lower than those reported in the literature. Bovine bone mineral plus collagen seems superior compared with other bone substitutes applied. Pseudoarthrosis, cage settling, and loss of correction were factors that negatively affected our clinical outcomes.
P155: Two-Year Follow-up of Multilevel Oblique Lumbar Interbody Fusion Using Hyperlordotic Porous Metal Cages Versus Pedicle Subtraction Osteotomy Has Lower Neurological Injury Rates
Darren Lui1, Hai Ming Yu1, Susanne Selvadurai2, Obiekezie Agu2, and Sean Molloy2
1St. George’s Hospital, London, UK
2Royal National Orthopaedic Hospital, London, UK
Introduction: Complex adult spinal deformity (CASD) represents a challenging cohort of patients. The Scoli-RISK-1 study of adults undergoing correction for ASD has shown a 22.18% perioperative risk of neurological injury in the perioperative period. Restoration of sagittal parameters is associated with good outcome in ASD. Pedicle subtraction osteotomies (PSO) is an important technique for sagittal balance in ASD but is associated with significant morbidity. The multilevel oblique lumbar interbody fusion (MOLIF) approach allows access through an extensile single incision from L1 to S1, and staged multilevel MOLIF may obviate PSO. Methods: Single-surgeon series 2007 to 2015. Prospectively collected data. Scoli-RISK-1 criteria were refined to only include stiff or fused spines otherwise requiring a PSO. Roentograms examined preoperatively and 1 year postoperatively. Primary outcome measure was the motor decline in American Spinal Injury Association (ASIA) at hospital discharge, 6 weeks and 6 months, 1 year and 2 years. Patient-reported oucome measures (PROMs), demographics, blood loss, operative time, spinopelvic parameters measured, and spinal cord monitoring (SCM) events were recorded. Results: Sixty-eight consecutive patients. Thiry-four each. Group 1 (MOLIF) mean age 62.9 years and group 2 (PSO) mean age of 66.76 years. Gender MOLIF: 64.7% female versus PSO 76.5%. Body mass index (BMI) group 1 (MOLIF) 28.05 and group 2 (PSO) 27.17. Group 1 (MOLIF) neurological injury 2.94% at discharge but resolved by 6 weeks. Group 2 (PSO) 5 neurological deficits (14.7%) with no recovery by 6 months to 2 years. SCM events: group 1 (MOLIF) 2.94% versus group 2 (PSO) 8.88%. Conclusion: Scoli RISK 1 trial shows that a true propsective trial regarding neurological injury in adult deformity surgery is higher than previously reported. The use of PSO as a technique is well established but known to carry morbidity particularly neurological. A multistage MOLIF approach followed by PSF (posterior spinal fixation) in this study was safer than PSO in CASD with stiff or fused spines. Over 2 years, MOLIF showed a lower perioperative neurological injury rate compared with PSO indicating it can be a safer operative technique while achieving superior spinopelvic harmony.
P156: Lumbar Cement Discoplasty: A Treatment Modality in Lumbar Degenerative Deformity With Axial Low Back Pain
Ali Haghnegahdar1, Mohammad Hosein Ashraf1, Amir Reza Mesbahi1, Mohammad Sadegh Masoudi1, and Keyvan Eqbal1
1Shiraz University of Medical Sciences, Shiraz, Islamic Republic of Iran
Objectives: Advanced lumbar degenerative disc disease causes deformity and low back pain (LBP) in eldery. Different kind of surgical intervention are suggested for treating these patients. Percutaneous application of polymethylmethacrylate (PMMA) as intervertebral spacers in the disc space may achieve immediate stability and reach a wide contact surface between the endplate and the interbody implant. The aim of the present study was to determine how the effect of percutaneous cement discoplasty (PCD) is in reducing pain and improving quality of life in patients with adult degenerative deformity with high risk of open surgical procedure. Methods: Ten patients enrolled in this study. They were older than 60 years. Their chief complaint was axial LBP, which did not respond to 6-week conservative therapy. This study designed and performed in Shiraz University of Medical Sciences over an 18-month period. All patients had vacuum sign of lumbar discs with no significant extrusion, no significant annulus fibrosus tearing or vertebral body fracture in radiographic studies. Scoliosis ≥25°, kyphosis ≥10°, instability ≥4 mm were among exclusion criteria. LBP was measured by visual analogue Pain Scale (VAS). Quality of life was evaluated by the Iranian version of Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ) before operation, at 1 and 6 months following PCD. Results: A total of 18 discs in 10 patients were treated by PCD. The mean VAS was 9.000 ± 0.267 before the intervention. Immediate postoperative VAS reduced significantly to 4.500 ± 0845, (P = .001). Total mean score of JOA was 134.80 ± 35.34 in preoperative state and increased to 251.90 ± 59.78 at first month follow-up and 280.41 ± 84.67 at 6 months after intervention. Mean Cobb angle correction was 4.47 ± 4.07°, mean kyphotic deformity was increasing by 0.38 ± 3.56° and mean disc space height increased 5.85 ± 2.80 mm. But there was no statistical correlation between these corrections and improving in VAS or JOA score. Conclusions: Old patients who are at high risk for open surgery of degenerative spine are good candidates for performing new and safe minimally invasive method. The clinical results of PCD are immediate, and this intervention has low risk of morbidity or mortality.
P157: Combined Approach Versus Posterior Approach in the Treatment of Adult Degenerative Scoliosis
Axel García Villaseñor1, Javier Guerra Garza1, Carla García Ramos1, and Alejandro Reyes Sánchez1
1National Institute of Rehabilitation, Mexico City, Mexico
Introduction: Adult degenerative scoliosis (ADS) is a 3-dimensional deformity, involving the coronal, sagittal, and axial planes, in a skeletally mature individual, with a Cobb angle in the coronal plane >10°. The prevalence is 6% to 68%. The male-female ratio is 1:1. Different surgical techniques have been described in order to correct the magnitude of the curve and restore the sagital balance of the spine. Controversy exists about the correction of the deformity, the clinical outcomes, and the quality of life achieved with a stand-alone posterior approach compared with a combined approach. Material and Methods: This is an ambipective, longitudinal, observational, and comparative study. Sixty-four patients with ADS, treated at our institute from 1995 to 2015. Inclusion criteria: De novo ADS, age >40, treated with a stand-alone posterior approach or a combined approach (ALPA [anterolateral transpsoatic approach] + posterior). Body mass index (BMI) < 30 kg/m2. Demographic (genere, age, and BMI), clinical (VAS [visual analogue scale], Roland-Morris [RM], and Short-Form-36 Health Survey [SF-36]), radiographic (Cobb angle, lumbar lordosis [LL], and pelvic parameters: pelvic tilt [PT], pelvic incidence [PI], and sacral slope [SS]), surgical variables (operation time, anestethic time, hospital stay, and blood loss), and complications were analyzed. The follow-up was 2 years. Results: Thirty-five patients treated with posterior approach, 8 with a combined approach. The mean age was 63.2 years, magnitude of the curve was 10° to 42° (mean = 22.45°). No difference in VAS, ODI (Oswestry Disability Index), or RM were observed. SF-36 showed improvement in the MCS (Mental Component Summary) in those treated with a combined approach (P = .050). Correction of the curve was similar in both groups. LL and pelvic parameters were not altered. Operation time and anesthetic time were longer in the second group (5:33 vs 4:03 and 6:37 vs 4:42, respectively; P = .068; P = .023). Blood loss and hospital stay were similar in both groups. Conclusion: There is not enough evidence supporting the superiority of one of the treatment modalities in the correction of the curve. Both groups showed similar improvement in quality of life and pain. There is no difference in hospital stay among groups. The stand-alone posterior approach avoids long operation time, anesthetic time, and also the need of transfusion required with the combined approach.
P158: Spontaneous Resolution of Thoracic Disc Herniations Associated With Proximal Junctional Failure Following Proximal Extension of Fusions
Ian Wong1, Robert Ravinsky1, So Kato1, and Stephen Lewis1
1 Toronto Western Hospital, University of Toronto, Toronto, Ontario, Canada
Introduction: Proximal junctional kyphosis (PJK) is a common complication following long segmental instrumented fusion surgery for adult spinal deformity. Increased loading in adjacent segments to the instrumentation combined with progressive degeneration, including disruption of posterior ligaments, fractures, instrumentation failure, malalignment, and/or facet violation, contribute to the development of PJK. Multiple classification schemes for PJK have been proposed in the literature. However, disc herniation has not been described in any of these classifications. The presence of kyphosis at the junction can further exacerbate the impact of the disc herniation on the compression of the spinal cord. There is little guidance in the literature on how to manage the disc herniation in this setting. The present case report demonstrates 3 cases of spontaneous resolution of thoracic disc herniations following proximal posterior extension of the fusion with a posterior decompression alone, without direct removal of the herniated discs. Material and Methods: A retrospective chart and radiograph reviews of an 82-year-old male, 69-year-old male, and a 69-year-old female who sustained PJK-related disc herniation was performed. Results: Three patients presented with incomplete spinal cord injuries (American Spinal Injury Association [ASIA] D in 2 cases, ASIA C in 1 case) due to disc herniation at the level proximal to a low thoracic to pelvis fusion. All 3 patients underwent posterior-only proximal extension of the constructs to the upper thoracic spine in conjunction with posterior decompression through laminectomy. The herniated discs were not removed. Postoperatively, following a short course of inpatient rehabilitation, all patients regained full neurological function. Repeat magnetic resonance imaging at minimum 6 months postoperatively demonstrated resolution of the herniated discs in all 3 cases. Conclusion: Proximal posterior extension of the instrumented fusion with posterior decompression without formal discectomy was associated with spontaneous resolution of thoracic disc herniations in the setting of PJK in these 3 cases. The morbidity and risks associated with removal of the thoracic discs through either transthoracic or costotranversectomy approaches was avoided and likely not necessary when appropriate posterior stabilization of the region can be achieved.
P159: Iliac Screw Versus S2 Alar-Iliac Screw Fixation in Adults: A Meta-Analysis
Rafael De la Garza Ramos1, Jonathan Nakhla2, Michael Longo1, Yaroslav Gelfand1, Murray Echt1, Merrit Kinon1, Daniel Sciubba3, and Reza Yassari1
1Montefiore Medical Center, Bronx, NY, USA
2Brown University, Providence, RI, USA
3Johns Hopkins University, Baltimore, MD, USA
Introduction: Iliac screws (IS) and S2 alar-iliac (S2AI) screws are 2 popular techniques in lumbopelvic fixation. The purpose of this study is to compare outcomes after IS versus S2AI screw fixation in adult patients. Methods: A PubMed/MEDLINE database search was performed for studies comparing the IS versus S2AI technique in adults. Levels of evidence were assigned based on the North American Spine Society guidelines. Three outcomes were examined: (1) revision surgery rate secondary to mechanical failure or wound complications, (2) surgical site infection rate, and (3) screw prominence/pain. Data were pooled and outcomes compared between techniques. Absolute risk reductions (ARRs) were also calculated for outcome measures. Results: Five retrospective cohort studies (all level III evidence) were included in our analysis. A total of 323 adult patients were included—147 in the IS group (45.5%) and 176 in the S2AI group (54.5%). Overall, the revision surgery rate due to mechanical failure or wound complications was 66/323 (20.4%)—27.9% in the IS group and 14.2% in the S2AI group (13.7% ARR; P < .001). Four studies reported wound infections among 278 total patients, with a rate of 35/278 (12.6%)—25.4% in the IS group and 2.6% in the S2AI group (22.8% ARR, P < .001). Three studies examined development of screw prominence/pain. Combined, these studies reported 21/215 cases (9.8%)—18.1% in the IS group and 1.8% in the S2AI group (16.3% ARR; P < .001). Conclusion: S2AI screw fixation in adults has a significantly lower mechanical failure and complication rate compared with the IS technique based on the current best available evidence.
P160: Proximal Junctional Kyphosis in Patients With Adult Spinal Deformity Undergoing Corrective Surgery With a Long Spinal Fusion from T10 to Pelvis
Aaron Hilis1, Daniel D’Aquino1, and Nasir Quraishi1
1Queen’s Medical Centre, Nottingham University Hospital, Nottingham, UK
Introduction: Proximal junctional kyphosis (PJK) is not uncommon after sagittal realignment surgery. Surgery for sagittal imbalance aims to restore optimal lumbar lordosis, in particular at L4/S1, where there is approximately 2/3 of the total lumbar lordosis. To the best of our knowledge, no studies have correlated the correction of segmental lumbar lordosis, from L1/4 and L4/S1, with the occurrence of PJK. Methods: Following institutional review board approval, a retrospective review was performed of 37 consecutive adult spine deformity (ASD) patients who underwent spinal fusion from T10 to pelvis. Demographic and surgical data were compiled from a review of medical records; intra- and postoperative complications were recorded. Segmental (L1-L4; L4-S1) lordosis, global lumbar lordosis (LL), sagittal vertical axis (SVA), and pelvic incidence (PI) were analyzed on preoperative, early postoperative, and final follow-up standing sagittal radiographs. PJK was defined as kyphosis of ≥10° between the lower endplate of the uppermost instrumented vertebra (UIV) and the upper endplate of the 2 supra adjacent vertebrae. Proximal junctional failure (PJF) included patients requiring revision for vertebral fracture, implant failure with/out neurological deterioration. The Charlson Comorbidity Index (CCI) was used to study complications. The Oswestry Disability Index (ODI) and Scoliosis Research Society–30 (SRS-30) scores were collected preoperatively and at each follow-up visit. Results: For the 37 patients (25 female: 12 male; mean age = 60.7 years (range = 34.1-78.1 years) included, the mean follow-up was 3.19 years (range = 1-5.9 years). The surgeries included pedicle subtraction osteotomies (23), posterior column osteotomies (14); 11 patients had anterior and posterior approach, and 26 patients had only posterior approach. Interbody cages were also used: posterior cages (PLIF/TLIF; 9), antero-lateral cages (6) and anterior cages (6). The mean SVA decreased significantly from 12.53 cm (range = 2-22.3 cm) preoperatively, to 5.69 cm (range = 4-9 cm) postoperatively. The mean preoperative global LL was 24.8° (−30° to 48°), L1-L4 lordosis 6.3° (−13° to 22°), and L4-S1 lordosis 19.06° (−11 to 33°), which all improved postoperatively to 42.9° (25-64°; P = .012), 11.9° (8-21°; P = .02), and 30.03° (14-48°; P = .012), respectively. The preoperative L1-L4/LL and L4-S1/LL ratio were 0.39 (0.10-0.62) and 0.62 (0.23-1), respectively. The postoperative L1-L4/LL ratio was 0.26 (0.003-0.63) and L4-S1/LL ratio was 0.76 (0.45-0.96) (P = .021). The incidence of PJK was 8/37 (23.7%) while the PJF rate was 5/37 (12.2%). Both PJK and PJF had significant correlation with high L1-L4/LL and low L4-S1/LL (P = .011); the Pearson correlation coefficient was 0.84. Other complications included broken rods in 4 patients, which required revision surgery, and wound infection (5) with 1 patient requiring metalwork removal. The average CCI score for the patient cohort was 0.92. A higher CCI was associated with a greater likelihood of occurrence of any complication (P = .0093). Both ODI (67.6 vs 19.8) and SRS questionnaire scores (47.9 vs 76.3) improved significantly from preoperative to the last follow-up (P = .043). Conclusions: Realignment surgery for adult spine surgery can be immensely successful, restoring harmonious sagittal alignment and functional outcomes. Adequate restoration of lordosis with greater proportion at L4/S1 can reduce the incidence of PJK and PJF.
P161: Do Intraoperative Radiographs in Adult Deformity Surgery Reflect the Final Radiographic Result?
Aaron Hilis1, Daniel D´Aquino1, Khalid Salem1, and Nasir Quraishi1
1Centre for Spinal Studies and Surgery Queen’s Medical Centre, Nottingham University Hospital, Nottingham, UK
Introduction: One of the main goals of adult spine deformity surgery is to obtain a balanced fused spine. Although preoperative planning remains essential, intraoperative radiographs are the only available tool during the procedure to verify accurate correction. The aim of this study was to show whether intraoperative radiographs of the sagittal correction accurately reflects the final radiographic result during correction of adult deformity surgery. Material and Methods: We retrospectively reviewed 47 patients with adult spine deformity (ASD) who underwent long spinal corrective surgery with pedicle subtraction osteotomies (PSO). We analyzed the preoperative, intraoperative (after instrumentation and correction), early, and last follow-up postoperative upright sagittal radiographic for the segmental lumbar lordosis (SLL) at the PSO level. Results: A retrospective study was performed on 47 (31 female, 16 male: mean age = 62.7 years [range = 31.4-77.3 years]) consecutive ASD patients treated with PSOs (29°at L3, 17° at L4). The mean follow-up was 3.9 years (range = 1-6.7 years). There were 30 patients who had a T9/10-pelvis fusion and 17 patients with T2/4 to pelvis. Of these, 16 patients had a combined anterior/posterior procedure and 31 patients had only posterior approach. The mean gain of the SLL intraoperatively after a single PSO was 28.9° (range = 21° to 34.6°; P = .045). This correction decreased slightly at the immediate standing sagittal X-ray to 26.7° (range = 20.9° to 23.6°; P = .63). At the last follow-up, the mean SLL value of 23.4° (range = 18.3° to 28.6°; P = .03), decreasing by an average of 5°. Conclusion: The routine use of intraoperative measurement for ASD provides the surgeon with a valuable tool to guide intraoperative decision-making. PSO is highly efficient to restore segmental lordosis but our results show that there is approximately 5° loss of this correction with time. This should be considered when planning corrective surgery for sagittal imbalance.
P162: Factors Affecting Restoration of Lumbar Lordosis in Adult Degenerative Scoliosis Patients Treated With Lateral Interbody Fusions
Sultan Aldebeyan1, Sarup Sridharan1, Ahmed Aoude1, Kenneth Thomas1, Roger Cho1, and Ganesh Swamy1
1University of Calgary, Calgary, Alberta, Canada
Introduction: Adult degenerative scoliosis (ADS) is a 3-dimensional deformity of the spine with a relative loss of lumbar lordosis (LL) and spinopelvic alignment. Correcting LL and restoring spinopelvic harmony correlates strongly with successful postoperative outcomes. Lateral lumbar transpsoas interbody fusion (LLIF) has been used with success as a surgical option to generate LL and does so with fewer complications than a traditional open procedure. However, factors that aid in generating LL with this procedure have not yet been elucidated. The aim of this study was to measure the effect of Materials and Methods: ADS patients undergoing LLIFs of L1 to L5 (±T12) and had second-stage percutaneous instrumentation and had a minimum 6-month follow-up were included in our study. All LLIFs implants used were of a fixed AP width and lordosis (6°). Digital Cobb technique was used for measuring segmental and regional angles. We studied whether LLIF improved segmental sagittal balance (SSB) and decreased the mismatch between pelvic incidence (PI) and LL. Second, we determined the role of degree of anterior cage placement (DACP), disc height (dh), and the ratio between cage to vertebral body length (CL-VB) in lordosis creation though a multivariate regression analysis. Results: LLIF significantly increased LL (−36.5 ± 12.5° preoperatively, −47.6 ± 10.5° postoperatively) and decreased the mismatch between PI and LL (21.8 ± 13.6° preoperatively, 11.0 ± 12.5° postoperatively). Preoperative SSB (P = .036), CL-VB (P = .015), and DACP (P = .003) were all significant variables in change in SSB, as per our regression analysis. When the variables were modeled in combination, it resulted in increasing DACP and decreased preoperative SSB as the most significant factors correlating to increased change in SSB. When SSB was held at zero and DACP was assumed to be zero (maximum anterior placement of the cage), the model predicted the maximum lordosis at every level to be greater than 6° (P < .05). Conclusion: LLIF in combination with percutaneous instrumentation can significantly increase LL and decrease PI-LL mismatch in primary ADS. The most significant technical factor under the surgeon’s control is cage placement. Increasing anterior placement of the cages was the most significant variable in increasing lordosis postoperatively, particularly at the lower lumbar levels.
P163: Appropriateness of Decompression Without Fusion in Patients With Degenerative Scoliosis: Findings From the RAND/UCLA Appropriate Use Criteria Study
Michael Daubs1, Sukanta Maitra1, Laura Raaen2, Peggy Guey-Chi Chen1, and Teryl Nuckols3
1University of Nevada, Las Vegas, NV, USA
2RAND Corporation, Santa Monica, CA, USA
3Cedars Sinai Hospital Los Angeles, Los Angeles, CA, USA
Introduction: The RAND/UCLA Appropriateness Method has been applied to at least 16 different surgical procedures, and several studies have documented that adherence to the resulting appropriateness criteria was associated with improved clinical outcomes. The appropriateness of various surgical procedures for the treatment of degenerative lumbar scoliosis (DLS) has not been universally agreed upon. The appropriateness of decompression without fusion in the setting of degenerative scoliosis remains controversial. The purpose of this study was to evaluate the indications and appropriateness of decompression without fusion in patients with degenerative scoliosis. Material and Methods: We used a variation of the RAND/UCLA Appropriateness Method, which includes a systematic review of the literature and a multidisciplinary modified-Delphi panel process. The panel included 3 neurosurgeons, 3 orthopedic spine surgeons, 2 physiatrists, 1 researcher/physical therapist, and 1 geriatrician. We developed 260 scenarios based on 7 different clinical characteristics, including imbalance. Panelists discussed the balance of risks and benefits and then rated the appropriateness of 5 surgical procedures (decompression alone, fusion alone, decompression and fusion, fusion and deformity correction, decompression and fusion and deformity correction) for each scenario. Results: Decompression without fusion was appropriate in patients with moderate to severe symptoms, at least moderate stenosis at 1 or 2 levels, and curve magnitude less than 30° without sagittal imbalance or progression. It was not appropriate in patients with curves greater than 30°, patients with greater than 2 levels of stenosis, and the presence of sagittal imbalance or progression. Decompression without fusion was indicated and necessary in patients with curves less than 30°, stenosis limited to 2 levels, and no sagittal imbalance. Conclusion: A decompression procedure without fusion in the setting of DLS is appropriate and necessary in patients with moderate to severe symptoms, curve magnitude less than 30° without progression, stenosis affecting 2 levels, and no sagittal imbalance. It is inappropriate in patients with curves greater than 30° and stenosis at greater than 2 levels.
P164: Progression of Adult Spinal Deformity in the Coronal and Sagittal Plane: A Radiographic Analysis
Sayf Faraj1, Niek te Hennepe2, Miranda van Hooff2, Martin Pouw2, Marinus de Kleuver1, and Maarten Spruit2
1Radboud University Medical Center, Nijmegen, Netherlands
2Sint Maartenskliniek, Nijmegen, Netherlands
Introduction: Currently, no studies have been reported on the course of progression in the coronal and sagittal plane in adult spinal deformity (ASD). This makes it challenging for health care providers to inform patients about prognosis, the need for follow-up examinations, and the timing of possible interventions. The objective of this study is to evaluate progression in the coronal and sagittal plane in ASD patients after a minimum follow-up of 2 years. Methods: A retrospective analysis of a single-center database of nonsurgical ASD patients between 2005 and 2017. Inclusion criteria were the following: age ≥40 years, diagnosis with adult degenerative scoliosis or idiopathic scoliosis, and a minimum follow-up of 2 years between the initial and final radiograph. Previous reported prognostic factors for coronal progression at initial presentation were studied: position of the intercrest line L4 or L5, direction of scoliosis, and curve magnitude. When full spine anteroposterior (AP) and lateral radiographs were available, progression in the sagittal plane was studied. Results: A total of 58 patients met the inclusion criteria with a mean follow-up of 59.8 ± 34.5 months. Mean initial and final Cobb angle were 37.2 ± 14.6° and 40.8 ± 16.5°, respectively. No significant differences were found in the mean increase in the Cobb angle in left versus right-sided scoliosis (3.3 ± 7.1° vs 3.7 ± 5.4°, P = .81), initial Cobb angle <30° versus ≥30° (2.6 ± 5.0° vs 4.3 ± 6.5°, P = .30), or when the intercrest line passed through L4 rather than L5 vertebra (3.4 ± 5.0° vs 3.8 ± 7.1°, P = .79). Of the 58 patients, 27 (47%) patients had full spine AP and lateral radiographs. No significant differences were found in sagittal spinopelvic parameters between initial presentation and final follow-up. Conclusion: To our knowledge, this is the first study that describes progression in the coronal and sagittal plane in a nonsurgical cohort of patients with ASD. Our results appear to indicate that progression occurs in a nonsignificant rate over a mean follow-up of 5 years in the coronal and sagittal plane. In contrast with previous studies, direction of scoliosis, curve magnitude, and the position of the intercrest line were found not to be associated with progression. The results of the present study provide more insight in the course of progression in ASD and may aid health care providers to inform patients about their prognosis and the need for clinical follow-up examinations.
P165: Intraoperative Ultrasound in Adult Spinal Deformity Surgery
Aaron Hilis1, Daniel D´Aquino1, Ameet Kulkarni1, Luca Boriani2, and Nasir Quraishi1
1The Centre for Spinal Studies and Surgery Queen’s Medical Centre, Nottingham University Hospital, Nottingham, UK
2Nottingham
Introduction: Intraoperative ultrasound (IUS) has been described in numerous papers as an effective tool in spinal surgery. In particular, the utility of IUS in the real-time localization of intradural lesions is well recognized. However, little attention has been paid to the use of IUS in surgery for adult spinal deformity. Here, we describe our experience of the use of IUS across a number of spinal pathologies—inclusive of adult spinal deformity correction—and describe certain surgical scenarios during which this technique might be useful. Materials and Methods: A retrospective review of cases where IUS was applied in patients undergoing spinal surgery at The Queen’s Medical Centre, Nottingham, between August 2017 and September 2018. Illustrative cases were selected and reviewed in detail. Intraoperative standard B-mode images were acquired using a 3- to 11-MHz linear US probe. The contribution of IUS to the final outcome of the case was defined. Results: Ten representative cases were identified covering the range of cervical, thoracic, and lumbar pathology. This cohort included cases with classical indications for IUS, such as acute disc and degenerative compressive pathology. The traditional use of IUS to determine the adequacy of surgical decompression is described. Furthermore, the extension of IUS to visualize a safe working corridor, ventral to the theca, while performing a posterior subtraction osteotomy (PSO) is introduced as a novel application of IUS. Conclusion: Based on our surgical experience, we advocate the use of IUS not only for the identification of spinal pathology but also to confirm the adequacy of neural decompression where indicated. Moreover, the real-time visualization of anatomy around and ventral to the theca using IUS lends itself well to establishing safe and satisfactory corridors during deformity correction procedures such as subtraction osteotomies.
P166: What Should an Ideal Adult Spinal Deformity Classification System Consist of? A Narrative Review and Conceptual Proposal for Future Classifications
J. Naresh Babu1, V. Arun Kumar1, Manabu Ito2, and Jong-Beom Park3
1Mallika Spine Centre, Guntur, India
2National Hospital Organization, Hokkaido Medical Center, Hokkaido, Japan
3Uijeongbu St. Mary’s Hospital, The Catholic University of Korea, Uijeongbu, Republic of Korea
Introduction: Adult spinal deformity (ASD) comprises combination of pathologies like radiological deformity, coexistence of spinal canal stenosis, radiculopathy, and multiple comorbidities. The available classifications of ASD are predominantly based on radiological parameters. The existing classifications of ASD do not consider associated clinical conditions into account. The purpose of this study is to review existing classifications related to ASD and to identify potential clinical factors or comorbidities to included in the classification. Material and Methods: A narrative review with search limited to English language was conducted of PubMed/MEDLINE using Medical Subject Heading (MeSH) terms. The terms specific to the review were: degenerative scoliosis OR adult spinal deformity OR adult degenerative scoliosis OR adult deformity. These were combined with comorbidities OR clinical outcomes OR factors affecting OR parameters affecting. Inclusion criteria: Studies were included if the factors influencing surgical outcomes for degenerative scoliosis were described. Exclusion criteria: Studies excluded were case reports, deformity due to infection/trauma/tumor, case series with less than 10 patients per group, animal, and in vitro and biomechanical studies. The full-text articles that met the criteria were included for the narrative review. Results: Total numbers of citations reviewed were 619. After applying the inclusion criteria, 39 were selected for retrieval of full-text. Out of which, 27 were excluded from the review as they did not meet the inclusion criteria of the present study. Twelve studies were selected and included for final analysis in this study. Leg pain, spinal stenosis, obesity, osteoporosis, and age were found to be the major influencing factors. The factors included in the available classifications, that is, Aebi et al, Simmons et al, Frank Schwab, SRS (Scoliosis Research Society)—Frank Schwab classifications were reviwed and results were tabulated. Conclusion: Classifying ASD patients according to radiological parameters will not address the full spectrum of ASD pathology. The present systematic review revealed the importance of neurological symptoms, spinal stenosis, osteoporosis, obesity, age, and smoking significantly influence the management of ASD. With increasing number of patients being diagnosed and treated with ASD, there has been increasing need to comprehensively classify these patients into clinico-radiological sub groups. There is an urgent need for a comprehensive classification of ASD, which inaddition to radiological factors should include clinical factors as well as comorbid factors.
Degenerative Cervical
P167: Comparative Analysis of Single-Level Total Disc Arthroplasty and Interbody Fusion in the Treatment of Patients With Degenerative Diseases of the Cervical Spine
Vadim Byvaltsev1, Andrei Kalinin1, Marat Aliev1, Ivan Stepanov1, Bakhyt Aglakov1, and Bobur Yussupov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: Total arthroplasty allows not only elimination of neurological manifestations of disco-radicular conflict but also preservation of the physiological volume of movements in the operated segment and prevention of degeneration of adjacent levels. Despite the accumulated extensive experience in the use of anterior cervical discectomy and interbody fusion, data from a comparative analysis of clinical and radiological findings with dynamic fixation are contradictory. The purpose of our study was to conduct a comparative analysis of single-level total disc arthroplasty and interbody fusion in the treatment of patients with degenerative diseases of the cervical spine Materials and Methods: The study included 173 patients with a CV-CVI or CVI-CVII 1-level symptomatic degenerative disease of the cervical spine. Two groups of study were identified: (1) (n = 84) were operated using the total disc arthroplasty (TDR); (2) (n = 89) were operated using interbody fusion (anterior cervical decompression and fusion [ACDF]). Clinical outcomes were analyzed by visual analogue scale (VAS), Neck Disability Index (NDI), MacNab scale, and complications. Instrumental results were investigated using cervical spondylography (cervical lordosis, total volume of movements in the cervical spine) and magnetic resonance imaging (MRI; degeneration of the overlying segment—intervertebral disc [IVD] and facet joints [FJ]). Results: According to intraoperative characteristics (duration of operation, volume of blood loss, activation time, and time of inpatient treatment), the study groups were comparable (P > .05). Preoperative clinical parameters in patients of both groups did not differ significantly (P > .05). In all cases, there was a significant decrease in the intensity of pain in the cervical and upper extremities of the VAS, as well as an improvement in the functional state according to NDI. But at the same time, in the early postoperative period, there was no intergroup difference in the above parameters (P > .05), whereas in the long-term period (median = 38 months), the best clinical outcomes in the TDR group were recorded. Good and excellent results on the MacNab scale were obtained in 34% and 61% of the patients in the TDR group, respectively, 53% and 11% of the patients in ACDF group, respectively (P < .001). Radiological parameters of the study of the cervical lordosis and the total volume of movements in the long-term period in both groups were comparable (P > .05). From clinically significant complications confirmed by MRI of the cervical spine, accelerated degeneration of IVD and FJ of adjacent levels was verified in 2 patients of TDR group (2.4%) and 8 patients in ACDF group (9%)—in all cases repeated decompressive-stabilizing interventions (P < .001). In addition, symptomatic adverse effects were registered in 3 patients (3.6%) in TDR group of the study in the form of heterotopic ossification and in 6 patients (6.7%) in ACDF group of pseudarthrosis—in these cases additional conservative therapy was performed. Conclusion: The use of TDR and ACDF with single-level degenerative diseases of the cervical spine allowed to significantly reduce the preoperative level of pain syndrome and improve the functional state of patients. The advantages of dynamic fixation before rigidity in remote clinical parameters, the frequency of degeneration of adjacent segments and repeated surgical interventions are established.
P168: Radiological Characteristics and Clinical Outcome of Ossification of Posterior Longitudinal Ligament Involving C2 After Posterior Laminoplasty and Instrumented Fusion Surgery
Liang Wang1, Yunpeng Jiang1, Lei Qi1, and Mu Li1
1Qilu Hospital of Shandong University, Jinan, China
Introduction: Studies and reports focused on the ossification of posterior longitudinal ligament (OPLL) involving C2 level are rare. When OPLL involves C2 level, it is still unclear whether there is something different from the common type of OPLL. The retrospective study was conducted to analyze the radiological characteristics and surgical outcome of cervical OPLL involving C2 level. Material and Methods: The records of the patients with OPLL involving C2 level who underwent posterior surgery from July 2006 through October 2015 were retrospectively reviewed. The types, longitudinal and transverse extent, occupation ratio, K-line classification of OPLL, and high-intensity zone (HIZ) of spine cord on magnetic resonance imaging (MRI) were analyzed to evaluate the radiological characteristics. All the cases received posterior open-door laminoplasty and instrumented fusion surgery. The Japanese Orthopedic Association (JOA) score and recovery rate (RR) were used to evaluate neurological function after surgery. Results: Forty-five patients with OPLL involving C2 level were enrolled in the study. Their radiological data were carefully analyzed. The mixed (73.3%) and continuous type (24.5%) were observed. The mean number of involved segments was 5.1. The narrowest spinal canal mostly located in the level of C3-C4 and mean occupying ratio was 65.3%. Thirty-two patients were followed up for at least 2 years and the mean follow-up time was 46.2 months. The mean JOA score was 10.3 preoperatively and 15.2 at the final follow-up and the mean RR was 70.7%. The K-line (+) and (−) subgroups showed similar preoperative JOA score and RR. The HIZ (+) subgroup showed lower preoperative JOA score but equal RR with (−) subgroup. Conclusion: When OPLL involving C2 level, it often presented different radiological characteristics. The posterior open-door laminoplasty and instrumented fusion surgery could achieve favorable clinical outcomes. Further researches and long-term clinical follow-up are needed to better appreciate the OPLL involving C2 level.
P169: Fate of Ossification of Posterior Longitudinal Ligament Following Anterior Fusion Surgery
Chul Gie Hong1, Dong-Ho Lee2, and Woo Dong Nam1
1Kangwon National University Hospital, Chuncheon, Republic of Korea
2Asan Medical Center, Seoul, Republic of Korea
Introduction: Progression of ossification masses is one of the important concerns after surgical treatment of ossification of posterior longitudinal ligament (OPLL) of cervical spine. Since most anterior decompression surgery of OPLL needs vertebral body resection with the complete removal of OPLL masses, progression of undamaged OPLL could not be observed after anterior surgery. The basic concept of vertebral body sliding osteotomy (VBSO) technique is forceful anterior translation of involved vertebral bodies without direct manipulation of OPLL masses. The aim of study is to observe the change of OPLL following VBSO. Material and Methods: Clinical data from 32 patients with cervical myelopathy secondary to OPLL were evaluated retrospectively. All subjects had undergone VBSO at a single center. The immediate postoperative radiograph was considered the reference, and 2 years after surgery, the radiograph was measured. Sagittal reconstructive computed tomography (CT) images were used to measure OPLL thickness. Fusion status was confirmed by complete bridge of trabecular bone between adjacent vertebral bodies on CT image and interspinous motion on dynamic images. Results: Mean OPLL thickness was slightly decreased from 6.27 ± 1.41 mm to 6.07 ± 1.34 mm (P < .01) and no prominent progression (change in thickness > 1 mm) was observed. Ossified masses were classified into 4 types according to the degree of disc space involvement: type 1 (no involvement) in 11 patients; type 2 (involving disc space but not crossing) in 7 patients; type 3 (crossing disc space but not fused) in 11 patients; and type 4 (complete bridging) in 2 patients. Twenty-nine percent patient of type 2 and 70% patient of type 3 OPLL were changed to type 4 (complete bridging) at 2-year follow-up. Conclusion: These observations suggest that the potential cause of postoperative OPLL progression is the repeated minor injury of posterior longitudinal ligament due to increased segmental motion. Therefore, completely eliminating segmental motion through fusion of the anterior column of the vertebral body can drastically reduce the progression of OPLL. Additional long-term studies on the possibility of OPLL mass shrinkage after fusion surgery will be performed following anterior decompression and fusion surgery.
P170: Early Result of EIT Cervical Cage for ACDF
Younus Hanif1, Fakouri Bharam1, and Panos Liantis1
1 Department of Trauma and Orthopaedic, Stoke, UK
Introduction: To evaluate the safety, clinical efficacy, and radiological outcomes of anterior cervical discectomy and fusion (ACDF) using EIT (Emerging Implant Technologies) cages. Material and Methods: We performed a retrospective review of a prospective database of ACDF operations performed by 2 senior surgeons at our institute. Patient who had EIT cage implanted between January 2016 and December 2017 were included in this study. At most recent follow-up, the patients’ condition was evaluated by an independent physician examiner. Neck Disability Index score, EQ5D-5L (EuroQol 5-Dimensions-5 level) Health Assessment and visual analogue scale (VAS) before and after the surgery were measured. Subsidence was defined as ≥3-mm decrease of the segmental height, and cervical kyphosis was defined as progression of ≥5° at 06 months after postoperative follow-up compared with that measured at the immediate postoperative period. Results: A total of 35 patients were included in study. All patient had ACDF performed by using EIT plate. Mean age was 55 years. Most common size of cage used was 6 large (range = 5-7 large). Average Neck Disability Index was improved from 43/60 moderate disability to mild disability 21/60. Average EDQ5D-5L index was improved from 0.52 (12/25) to 0.77 (7/25) and VAS-pain was improved from 8 to 5. Segmental subsidence was observed in 1 (2.8%) patient. Segmental kyphosis was not observed in any case to date. Conclusion: Our short-term follow-up using EIT cages shows excellent fusion rate, improved outcome, and no serious complication. We concluded that this cage provides better fusion, low subsidence, and is technically easy to perform.
P171: The Effects of Clinical Factors and Retro-Odontoid Soft Tissue Thickness on Atlantoaxial Instability in Patients with Rheumatoid Arthritis
Je Il Ryu1, Myung Hoon Han1, Jae Min Kim1, and Jin Hwan Cheong1
1Hanyang University Guri Hospital, Guri, Republic of Korea
Introduction: Rheumatoid arthritis (RA) is an autoimmune disease that often occurs in the atlantoaxial segment of the cervical spine and results in instability that can cause severe pain and neurological symptoms. Thickening of soft tissue posterior to the odontoid process of the atlantoaxial segment is referred to as retro-odontoid soft tissue (ROST) thickness or pseudotumor. The mechanism of ROST thickness is still unknown. Materials and Methods: Among patients diagnosed with RA, those with cervical X-ray and magnetic resonance imaging records were selected for investigation of their clinical symptoms, laboratory findings, radiologic evaluation, and RA medication history. Results: A total of 199 patients were selected and divided into lower and upper median groups according to the ROST thickness value. In RA patients, the median ROST thickness value was 2.3 mm (interquartile range = 1.4-3.4). The median value of the anterior atlanto-dens interval (ADI) was 2.4 mm, with a significant difference being observed between the lower and upper median ROST thickness groups (P = .001). Multivariable linear regression analysis revealed a correlation between Steinbrocker stage and the positivity of rheumatoid factor (RF). For each unit increase in the Steinbrocker stage, the ROST thickness increased by 0.35 mm (β = −0.349; 95% confidence interval [CI] = −0.643 to −0.055; P = .020). For every 1 mm ADI increase, ROST thickness decreased by 0.16 mm (β = −0.163; 95% CI = −0.264 to −0.062; P = .002). Conclusions: This study showed a statistical correlation between ROST thickness and ADI related to biomechanical changes in the dynamic atlantoaxial segment, thereby suggesting the value of a prospective study.
P172: Predictors of an Unpredictable Entity and the Surgical Strategy: To Tackle the Enigma of Cervical Myelopathy
Nandan Marathe1, and Sudhir Srivastava1
1Seth GS Medical College and KEM Hospital, Mumbai, India
Introduction: Compressive degenerative cervical myelopathy (CDCM) is the most common cause of spinal cord dysfunction worldwide. Given that CDCM is a prevalent cause of spinal cord injury, and since surgery is often an appropriate intervention, it would be useful to identify the most important predictors of surgical outcome. Materials and Methods: All patients with CDCM treated surgically at a tertiary care center. Type of study: Retrospective, observational. Inclusion criteria: Operated CDCM cases with minimum 2 years of follow-up. Exclusion criteria: Asymptomatic cases, previous spine surgeries. Factors evaluated: Clinical (modified Japanese Orthopaedic Association [mJOA] score, demographic data, comorbidities, etc), radiological (instability on X-ray, diffusion tensor imaging [DTI], Torg ratio, and neurography). Results: Severity of myelopathy, gender, duration, comorbidity, hand wasting, bladder bowel involvement, MRI (magnetic resonance imaging) changes, and instability on radiographs were predictive of the outcome with a P value <.05. Age, diagnosis, surgical procedure, and Torg ratio were not significantly related to the outcome Conclusion: (1) DTI will be helpful objective prognostic factors for patients in whom surgery is planned. However, a study with larger subject size is required to increase the accuracy of determination of regression coefficient. The cost-benefit ratio still remains a question in Indian scenario. (2) Clinical parameters are better predictors of the outcome as compared with radiological findings. (3) A lower preoperative mJOA score (greater severity), intrinsic hand muscles wasting, longer duration of symptoms, male gender, and diabetes mellitus were associated with a decreased probability of a successful outcome. (4) One of the radiological parameters (instability) was statistically related to the outcome with a P value <.05.
P173: Rigid Cervical Plate Fixation Is Associated With Greater Restoration and Maintenance of Cervical Lordosis Compared With Semi-Rigid Plate Fixation in Anterior Cervical Discectomy and Fusion
Bryce Basques1, Philip Louie1, Michael Nolte1, Jannat Khan1, Coralie Pardo1, Gagan Grewal1, Clayton Maschhoff1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Anterior cervical discectomy and fusion (ACDF) is one of the most common procedures in spine surgery. Both rigid and semi-rigid plates have been used to stabilize the anterior cervical spine after intervertebral graft application. There is a lack of studies comparing the radiographic outcomes between rigid and semi-rigid cervical plate fixation over multiple level ACDF procedures. The purpose of this study was to determine relative differences in radiographic and clinical outcome between rigid cervical plate fixation versus semi-rigid cervical plate fixation in anterior cervical discectomy and fusion. Materials and Methods: A retrospective cohort analysis was conducted of patients who underwent a single-level or multi-level ACDF for cervical radiculopathy or myelopathy. All of the cases were performed by one of two senior spine surgeons in the department. Patients were excluded from analysis if they were younger than 18 years at the time of surgery, had postoperative follow-up less than 1 year, or had an ACDF for cervical spine fracture or infection. Radiographic assessments included the following: C2-C7 lordosis, T1 angle, levels fused, sagittal vertical axis (SVA), fusion mass lordosis, proximal and distal adjacent segment lordosis, adjacent segment degeneration (ASD), and fusion. Patient reported outcomes were obtained in the form of Neck Disability Index (NDI) scores and visual analogue scale (VAS) scores for the neck/arm. Baseline patient characteristics were compared using chi-square analysis and independent-sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare clinical outcomes between procedure groups. Multivariate analyses controlled for differences in baseline patient characteristics. Results: A total of 403 patients met our inclusion criteria; 257 patients underwent semi-rigid plating and 147 patients underwent rigid plating. Regarding demographic variables, there were statistically significantly higher proportions of smokers (P = .001) in the semi-rigid plating group relative to the rigid group (Table 1). Both plating systems successfully restore cervical lordosis with an ACDF, without significant changes in the SVA. Rigid plate fixation was associated with greater change in pre- to postoperative overall lordosis compared with semirigid plating (P = .046). Similarly, rigid plating was associated with greater change in preoperative to postoperative fusion segment lordosis compared to semi-rigid plate fixation (P = .002). Rigid plate fixation also maintained fusion segment lordosis from the immediate postoperative period to final follow-up better than semi-rigid plating (P = .014). There was no significant difference in the rate of radiographic ASD overall (P = .582). Similarly, there were no significant differences between preoperative, postoperative, or change in patient reported outcomes between the 2 groups. The ASD, reoperation rate, fusion rate, and subsidence rate were not significantly different between the 2 groups. Conclusion: Rigid plating group had a superior maintenance in fusion segment lordosis relative to the semi-rigid plating group at final follow-up. However, at final follow-up, all other radiographic and clinical variables, including reoperation rate, fusion rate, and patient-reported outcomes, were similar between the 2 groups. Both plating modalities are acceptable treatments for anterior cervical instrumentation in patients undergoing anterior cervical discectomy and fusion for cervical radiculopathy or myelopathy.
P174: Degenerative Cervical Spondylolisthesis: Does Adjacent Level Surgical Stabilization Result in Progressive Listhesis?
Philip Louie1, Hollis Johanson1, Jacob Emerson1, Jannat Khan1, Bryce Basques1, Michael Nolte1, Zayd Hayani1, Dino Samartzis1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Patients with cervical spondylotic myelopathy (CSM) often present with multilevel disease and may experience spondylolisthesis within or adjacent to the levels of clinical pathology. The progression of an unfused degenerative cervical spondylolisthesis (DCS) segment remains unclear when it is not included within the surgical construct. We sought to evaluate if unfused DCS segments, adjacent to the fusion, develop worsening instability that requires surgery. Materials and Methods: We performed a retrospective cohort study of patients who presented with CSM, had radiographs revealing DCS at one or more levels, and underwent anterior cervical discectomy and fusion (ACDF) or posterior laminectomy and fusion from 2005 to 2013 with a minimum of 6 months of follow-up. Exclusion criteria included previous spine surgery, less than 6 months of follow-up, history of spine trauma, a diagnosis of ossification of the posterior longitudinal ligament (OPLL), rheumatoid arthritis, or currently undergoing hemodialysis; and incomplete set of radiographs (requirement to have preoperative neutral, flexion, and extension imaging, and postoperative lateral and anterior-posterior neutral imaging). All patients showed no evidence of clinical symptoms present at the DCS level and had surgery performed at adjacent levels. Demographic information was collected for all patients that included: age, sex, body mass index, smoking status, and Charleston Comorbidity Index (CCI). Several radiographic parameters were measured preoperatively and at the last follow-up: amount of listhesis, cervical lordosis, sagittal vertebral axis, and T1 slope at the pathologic level. On lateral cervical plain radiographs, the number of millimeters (mm) of anterolisthesis was measured. Spondylolisthesis was deemed present if there was greater than 2 mm of anterolisthesis. Patients were considered to have progressed if mm of spondylolisthesis on follow-up radiography was 0.5 mm or greater than initial listhesis. This value was chosen to adjust for measurement error. Clinically, reoperation status was assessed. Baseline patient characteristics were compared using chi-square analysis and independent-sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare radiographic outcomes. Multivariate analysis was used to find independent risk factors for progression of disease. Results: A total of 23 patients fulfilled inclusion criteria. Average follow-up was 31.5 months (range = 6-76 months). DCS was present at C2-3 in 3 cases (13%), C3-4 9 cases (39.5%), C4-5 7 cases (30.4%), C5-6 2 cases (8.7%), C6-7 no cases (0%), and C7-T1 2 cases (8.7%). The average preoperative slip was 2.7 mm ± 0.5 mm. At final follow-up, 5 (21.7%) demonstrated progression (>0.5 mm) of their slip, 18 (78%) remained stable (within 0.5 mm) or improved. Older age and male sex were associated with progression, but did not increase the risk of reoperation. Two patients (8.7%) with DCS underwent revision surgery, one for symptomatic pseudoarthrosis and one for myeloradiculopathy due to progression of the adjacent DCS. Conclusion: Despite the presence of altered stress at the DCS level with the adjacent surgical intervention, the majority of patients did not experience DCS progression at final follow-up nor require further surgical intervention. Given our findings, surgeons may not need to extend a proposed cervical fusion for CSM to include the adjacent asymptomatic DCS level.
P175: Do Large Increases in Disc Space Height Have Consequences After ACDF?
Jannat Khan1, Islam Elboghdady1, Bryce Basques1, Michael Nolte1, Philip Louie1, Landan Banks1, Steve Heidt1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: During anterior cervical discectomy and fusion (ACDF), distraction of the disc space is used to assist with decompression and graft insertion. In patients with significant preoperative disc space collapse, there may be a large increase in disc space height postoperatively after graft insertion. There are concerns that this acute increase may increase the stresses across the graft-endplate interface and may lead to subsidence or affect other radiographic or clinical outcomes. The aim of the present study was therefore to characterize the difference in preoperative and postoperative disc space height, and to determine the association of an increased change in disc space height with clinical and radiographic outcomes following ACDF. Methods: A retrospective cohort analysis was performed on patients who underwent a single-level ACDF by 1 of 2 senior spine surgeons between 2008 and 2015 for cervical radiculopathy and/or myelopathy, with a minimum of 6 months of clinical and radiographic follow-up. Radiographs were reviewed preoperatively and immediately postoperatively and at final follow-up. Disc height was measured as the anterior vertebral distance (AVD), mid-vertebral distance (MVD), and posterior vertebral distance (PVD) on preoperative and immediate postoperative radiographs. Sagittal parameters were also measured, and included C2-C7 lordosis, T1 angle, fusion segment lordosis, sagittal vertical axis (SVA), proximal and distal adjacent segment lordosis. Visual analogue scale (VAS) neck, VAS arm, and Neck Disability Index (NDI) scores were collected at each postoperative clinical visit. The rates of adjacent segment disease, reoperation, successful fusion, and subsidence (postoperative disc space collapse ≥2 mm) were determined. Multivariate regressions were used to control for baseline patient characteristics. Results: A total of 120 patients met inclusion criteria. Mean follow-up length was 29 months, and mean age was 46.9 years, mean BMI (body mass index) was 28.4 kg/m2, and 45.4% of patients were female (Table 1). On multivariate analysis, increased preoperative to postoperative disc height change in all regions was associated with development of distal adjacent segment disease (Table 2: AVD odds ratio [OR] = 1.89, P = .013; MVD OR = 1.75, P = .043; and PVD OR = 2.07, P = .014), but not proximal adjacent segment disease. Increased change in AVD was associated with a greater change in preoperative to postoperative C2-C7 lordosis, fusion segment lordosis, and proximal segment lordosis. Increased change in AVD was also associated with increased preoperative to final change in lordosis. No other associations were found between preoperative to postoperative difference in AVD, MVD, or PVD, and preoperative, immediate postoperative, or final sagittal parameters. Additionally, no associations were found between preoperative to postoperative disc height change and any clinical outcomes (Table 3). Rates of reoperation, fusion, and subsidence did not vary based on preoperative to postoperative disc height change. Conclusions: This study found that a greater difference in preoperative to postoperative disc space height following ACDF was associated with the development of distal adjacent segment degeneration; however, it was not associated with most radiographic outcomes or any patient-reported outcomes. Large changes in disc space height may not be benign, and further study is needed to characterize the etiology of ASD associated with these changes.
P176: Sagittal Alignment Parameters and Early Radiographic Changes Associated With Adjacent Segment Pathology After Anterior Cervical Discectomy and Fusion
Philip Louie1, Bryce Basques1, Michael Nolte1, Jannat Khan1, Steve Heidt1, Clayton Maschhoff1, Konstantin Tchalukov1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Changes in cervical alignment from pre- to postoperative may alter cervical spine mechanics and increase the rate of early adjacent segment degeneration (ASD). The goal of this study was to further evaluate the relationship between pre- and postoperative cervical spine sagittal alignment, as measured by various radiographic parameters. We also sought to identify early radiographic changes suggestive of ASD given the presence of both radiographic and clinical ASD, and the subsequent need for reoperation following anterior cervical discectomy and fusion (ACDF). Methods: We performed a retrospective cohort analysis with patients undergoing ACDF who developed radiographic signs of ASD (+) (103 patients) were identified and compared with a matched group of ACDF patients without evidence of ASD(−) (132 patients) for a period of at least 1 year. The sagittal parameters measured included change in C2-C7 lordosis, T1 angle, levels fused, sagittal vertical axis (SVA), fusion mass lordosis, proximal, and distal adjacent segment lordosis. Radiographic diagnosis of ASD was determined by the presence of new or enlarged osteophytes, spondylolisthesis, endplate sclerosis, disc space narrowing >30%, and/or increased calcification of the anterior longitudinal ligament (ALL). Patient-reported outcomes were obtained in the form of Neck Disability Index (NDI) scores and visual analogue scales (VAS) scores for the neck and arm. Results: A total of 235 patients met the inclusion criteria. Patients of female sex had significantly lower presentations with radiographic signs of ASD (38.8% vs 61.4%; P = .001) (Table 1). Patients with greater kyphosis throughout the cervical spine at final follow-up had increased odds of developing ASD (odds ratio [OR] 0.97 per degree, P = .040). Patients with greater preoperative kyphosis through the planned fusion segment had increased odds of ASD (OR 0.93 per degree, P = .003). Patients who lost lordosis through the fusion from initial postop to final follow-up had greater odds of developing ASD (OR 0.85 per degree, P < .001) (Table 2). Patients who had greater change in preoperative to postoperative fusion segment lordosis were found to exhibit a greater risk of ASD (OR 1.06 per degree, P = .019). Specifically, patients with 2 or fewer radiographic ASD signs had a reoperation rate of 2.73%, while patients with 3 or greater signs experienced a reoperation rate of 31.25% (P < .001) (Table 3). Clinically, all patients showed improvement in NDI as well as VAS-Neck and VAS-Arm scores from preoperative levels to final follow-up. Reoperation, fusion, and subsidence rates were similar for both groups. Conclusion: Patients with greater preoperative cervical kyphosis and kyphosis through the proposed fusion segment may have greater odds of developing radiographic ASD. Similarly, those who had a greater correction of cervical lordosis postoperatively and those with loss of lordosis at the fusion segment also presented with increased odds of developing radiographic ASD and subsequent clinical symptoms at these levels. Thus, there is a balance between overcorrection and undercorrection of lordosis that warrants further exploration. Among patients who do develop radiographic ASD, there may be a relationship between the severity of radiographic findings and the need for reoperation.
P177: Which Patients With Radiographic Evidence of Adjacent Segment Degeneration Following an Anterior Cervical Discectomy and Fusion Develop Clinical Symptoms at These Adjacent Levels?
Bryce Basques1, Jannat Khan1, Michael Nolte1, Victor Lei1, Jeremy Mormol1, Steve Heidt1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Radiographic evidence of adjacent segment degeneration (ASD) has been well described following anterior cervical discectomy and fusion (ACDF). However, it is unclear, which patients with radiographic changes progress to become symptomatic at these adjacent levels. The aim of the present study was to evaluate patients who developed radiographic evidence of ASD and identify clinical and radiographic characteristics associated with the development of clinical symptoms at those levels following an ACDF. Methods: A retrospective cohort study was performed using consecutive patients who developed radiographic evidence of ASD following a primary ACDF at an academic institution between 2008 and 2015 for cervical radiculopathy and/or myelopathy, with a minimum of 6 months of clinical and radiographic follow-up. Patients were grouped by the presence or absence of clinical evidence of ASD. Preoperative, postoperative, and final radiographs were reviewed. Disc height was measured as the anterior vertebral distance (AVD), mid-vertebral distance (MVD), and posterior vertebral distance (PVD) on preoperative and immediate postoperative radiographs. Sagittal parameters were also measured, and included C2-C7 lordosis, T1 angle, fusion segment lordosis, sagittal vertical axis (SVA), and proximal and distal adjacent segment lordosis. ASD was deemed present if there anterior/radial osteophytes, a decreased in disc space, >3 mm of motion on flexion-extension lateral radiographs, or calcification of the anterior longitudinal ligament. Preoperative and final visual analogue scale (VAS) neck, VAS arm, and Neck Disability Index (NDI) scores were collected. The rates of reoperation, successful fusion, and subsidence (postoperative disc space collapse >2 mm) were determined. Clinical evidence of ASD was deemed present if the patient presented with radicular symptoms in the distribution of the adjacent segment. Radiographic parameters were tested for association with patient-reported outcomes, reoperation, fusion, and subsidence using multivariate linear regression and multivariate logistic regression for continuous and binary outcomes, respectively. Multivariate regressions controlled for potential confounding variables in order to identify independent risk factors for each outcome. The Šidák-Holm method was used to adjust P values in order to correct for multiple statistical comparisons. The threshold for statistical significance was set at P < .05. Results: A total of 75 patients were identified with radiographic evidence of ASD following primary elective ACDF. Of these patients, 32 (42.3%) presented with clinical symptoms at that adjacent level. Average follow-up length was 28 months. Diabetes was diagnosed in significantly more patients who developed clinical evidence of ASD compared with those who did not (odds ratio [OR] 11.17, P = .030). Otherwise, there were no additional significant differences in patient demographics. Similarly, there were no significant differences in the presentation of ASD at the proximal or distal segment between those who presented with clinical ASD and those who did not. On multivariate analysis, patients with clinical ASD presented with a greater amount of lordosis change at the distal adjacent segment (from preoperative to immediate postoperative measurements) compared with those with only radiographic ASD (OR 0.84, P = .037; Table 1). Otherwise, there were no significant differences in the preoperative, immediate postoperative, or final follow-up measurements as well as the change in these parameters between the 2 groups (Tables 2 and 3). Patients with clinically symptomatic ASD presented with significantly worse VAS-neck scores (2.88 ± 2.70 vs 2.08 ± 2.21; P = .036) compared with those who did not have clinical ASD (Table 4). Discussion and Conclusion: The present study found that patients with radiographic and clinical evidence of ASD presented with a greater change in lordosis at the distal adjacent level compared with those who only presented with radiographic evidence of ASD. Care should be taken when assessing the amount of lordosis correction intraoperatively. Future research should attempt to further describe the relationship between patients who develop clinical symptoms at adjacent levels and the associated radiographic features, following an ACDF.
P178: Rigid Plating and Cortico-Cancellous Allograft Are Effective for 3-Level Anterior Cervical Discectomies and Fusion: A Radiographic Study
Jannat Khan1, Philip Louie1, Daniel Bohl1, Ben Mayo1, Kamran Movassaghi2, Bryce Basques1, Michael Nolte1, and Howard An1
1Rush University, Chicago,IL, USA
2University of California, San Francisco–Fresno, Fresno, CA, USA
Introduction: Anterior cervical discectomy and fusion (ACDF) has demonstrated efficacy for treatment of multilevel degenerative cervical conditions, but current data exists in small heterogeneous forms. As such, the purpose of the current study is to detail the radiographic and clinical outcomes of a series of 3-level primary ACDF procedures using a rigid construction with cortico-cancellous allograft at a single institution. Methods: We conducted a retrospective cohort analysis of patients who underwent primary 3-level ACDF surgery from 2008 to 2013 with minimum 1-year follow-up. Exclusion criteria included revision surgeries, infections, anterior/posterior surgeries, and follow-up of less than 12 months. Demographics such as age, sex, body mass index (BMI), and Charleston Comorbidity Index (CCI) were recorded. Patient-reported outcomes (PRO) were assessed using the Neck Disability Index (NDI) and visual analogue scale (VAS) neck and arm survey scores. All radiographs were analyzed to calculate and compare changes in cervical sagittal vertical axis (SVA), segmental height, fusion, and cervical lordosis between preoperative, immediate postoperative, and final follow-up period. Radiographic measurements were compared using Student’s t tests. Bivariate and multivariate analyses were used to identify risk factors for clinical and radiographic outcomes. Results: A total of 98 patients met the inclusion criteria. The average follow-up was 24.3 ± 13.7 months. Mean age at time of surgery was 55.2 ± 6.1 years. Rates of asymptomatic pseudoarthroses and total reoperations were 18% and 4%, respectively. In total, 13 (13.3%) patients were active tobacco smokers, and 12 patients had a diagnosis of diabetes mellitus (12.3%) (Table 1). Results demonstrated immediate improvements in cervical lordosis (5.5°, P < .01) and segmental height (5.0 mm increase, P < .01) with little changes in the cervical SVA (3.2 mm increase, P < .01). Additionally, segmental alignment improved (7.1°, P < .001) from preoperative measurements at final follow-up (Table 2). The segmental height decreased from immediate postoperative period to final follow-up (1.7 mm decrease, P < .01). Older age was protective against radiolucent lines (P < .05) (Table 3). Patient-reported outcomes significantly improved following surgery (P < .01) (Table 4). Current smoking status and diagnosis of diabetes mellitus had no impact on radiographic or clinical outcomes. Risk factors were not identified for the 5 (4%) reoperations. Conclusion: Overall, 3-level ACDF with rigid-plating and cortico-cancellous allograft is an effective procedure for degenerative diseases of the cervical spine without the application of additional adjuncts or combined anterior-posterior cervical surgeries. Significant improvements in cervical lordosis, segmental height, and segmental alignment can be achieved with little change in cervical SVA and a low rate of reoperations over short-term follow-up. Similarly, patient-reported outcomes show significant improvements following 3-level ACDF procedures.
P179: The Association of Preoperative Disc Height With Radiographic and Clinical Outcomes Following Anterior Cervical Discectomy and Fusion
Bryce Basques1, Jannat Khan1, Philip Louie1, Kamran Movassaghi2, Jonathan Markowitz1, Gagan Grewal1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
2University of California, San Francisco–Fresno, Fresno, CA, USA
Introduction: Disc space collapse often occurs later in the natural course of cervical degenerative disc disease. During anterior cervical discectomy and fusion (ACDF), restoration of disc space height and lordosis can assist with decompression and restoration of alignment. However, it is unclear if the amount of preoperative cervical disc space collapse correlates with outcomes following ACDF. The aim of the present study was to characterize preoperative disc space height in a sample of ACDF patients and to determine the association with postoperative clinical and radiographic outcomes following ACDF. Methods: A retrospective cohort analysis was performed on patients who underwent a single-level ACDF between 2008 and 2015 for cervical radiculopathy and/or myelopathy, with more than 6 months of clinical and radiographic follow-up. Radiographs were reviewed preoperatively, immediately postoperatively, and at final follow-up. Preoperative disc height was measured in terms of preoperative anterior vertebral distance (pAVD), mid-vertebral distance (pMVD), and posterior vertebral distance (pPVD). Sagittal parameters were also measured, and included change in C2-C7 lordosis, T1 angle, levels fused, sagittal vertical axis (SVA), fusion mass lordosis, and proximal and distal adjacent segment lordosis. Visual analogue scale (VAS) neck, VAS arm, and Neck Disability Index (NDI) scores were collected at each postoperative clinical visit. The rates of adjacent segment disease (ASD), reoperation, fusion, and subsidence (postoperative disc space collapse ≥2 mm) were determined for the study period. Results: A total of 120 patients who underwent a 1-level ACDF during the study period were included. As expected, increased pAVD was associated with increased preoperative lordosis, SVA, fusion segment lordosis, and proximal lordosis. Increased pAVD was also associated with increased postoperative SVA, T1 angle, and proximal segment lordosis. At final follow-up, pAVD was associated with increased lordosis, SVA, and proximal lordosis. Additionally, pMVD was associated with increased postoperative SVA (P = .025) and final SVA (P = .011). Preoperative PVD was associated with decreased postoperative distal lordosis (P = .037) and increased final SVA (P = .032) (Table 1). Notably, greater pAVD was associated with greater final VAS arm scores (P = .022), greater pMVD was associated with increased final VAS neck (P = .037) and final VAS arm scores (P = .040), and greater pPVD was associated with greater final VAS neck (P = .031) and arm (P = .023) scores. Greater AVD, MVD, and PVD were all associated with a decreased preoperative to postoperative difference in VAS neck (P value range = .034-.04) (Table 2). No associations were found between preoperative disc height and NDI scores, or rates of ASD, reoperations, fusion, or subsidence. Conclusion: Preoperative disc height was found to be associated with radiographic and clinical outcomes on multivariate analysis. Notably, increased anterior, middle, and posterior preoperative disc height were all associated with increased final SVA, among other parameters. Patients with well-maintained preoperative disc heights had greater final VAS neck and arm scores and had less postoperative improvement in VAS neck scores compared with patients with preoperative collapsed discs. These results suggest that patients with preoperative cervical disc space collapse may have superior outcomes compared with patients with maintained cervical disc height, and future studies are needed to further explore these differences.
P180: Sagittal Parameters Poorly Predict Clinical Outcomes Following Anterior Cervical Discectomy and Fusion
Bryce Basques1, Jannat Khan1, Michael Nolte1, Philip Louie1, Kamran Movassaghi2, Jonathan Markowitz1, Victor Lei1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
2University of California, San Francisco–Fresno, Fresno, CA, USA
Introduction: Sagittal radiographic measurements of the spine have received significant attention in recent years, and in the lumbar spine, the relationship between sagittal balance, spinopelvic parameters, and clinical outcomes is well established. However, the relationship between these radiographic measurements and clinical outcomes is less clear. This study characterizes independent associations between cervical spine radiographic parameters and clinical outcomes following anterior cervical discectomy and fusion (ACDF). Methods: A retrospective cohort study was performed using consecutive patients who underwent a single-level ACDF at an academic institution between 2008 and 2015 for cervical radiculopathy and/or myelopathy, with a minimum of 6 months of clinical and radiographic follow-up. Preoperative, postoperative, and final radiographs were reviewed. Disc height was measured as the anterior vertebral distance (AVD), mid-vertebral distance (MVD), and posterior vertebral distance (PVD) on preoperative and immediate postoperative radiographs. Sagittal parameters were also measured, and included C2-C7 lordosis, T1 angle, fusion segment lordosis, sagittal vertical axis (SVA), and proximal and distal adjacent segment lordosis. Preoperative and final visual analogue scale (VAS) neck, VAS arm, and Neck Disability Index (NDI) scores were collected. The rates of reoperation, successful fusion, and subsidence (postoperative disc space collapse >2 mm) were determined. Radiographic parameters were tested for association with patient-reported outcomes, reoperation, fusion, and subsidence using multivariate linear regression and multivariate logistic regression for continuous and binary outcomes, respectively. The Šidák-Holm method was used to adjust P values in order to correct for multiple statistical comparisons. The threshold for statistical significance was set at P < .05. Results: A total of 381 patients met inclusion criteria. Average follow-up length was 28 months, average age was 50.2 years, average body mass index was 28.7 kg/m2, and 49.2% of patients were female. Of these patients, 93.7% achieved successful fusion, 6.6% had graft subsidence, and 4.99% had a reoperation. Preoperative and postoperative radiographic measurements and patient-reported outcomes were collected. Preoperative radiographic measurements poorly predicted clinical outcomes. Increased preoperative lordosis at the adjacent unfused segment proximal to the eventual fusion mass was found to be associated with increased final NDI (corrected P = .018), and increased final proximal lordosis was associated with increased final NDI (corrected P = .049). However, no other radiographic parameters were associated with any patient-reported clinical outcomes. Subsidence rates were increased with greater change in proximal lordosis from preoperative to postoperative (odds ratio [OR] 1.30, corrected P = .007) and from preoperative to final follow-up (OR 1.17, corrected P = .044). Subsidence was negatively associated with increased change in lordosis across the fused segments from preoperative to postoperative (OR 0.88, corrected P = .032) and from preoperative to final follow-up (OR 0.86, corrected P = .017). No other radiographic parameters were associated with subsidence, and no parameters were associated with reoperation or pseudoarthrosis. Conclusion: The present study found that sagittal parameters were poorly predictive of clinical outcomes. Increased preoperative lordosis at the adjacent segment proximal to the fusion mass was associated with worse final NDI scores and was the only preoperative radiographic parameter associated with clinical outcomes. Further research should attempt to identify other preoperative factors or radiographic parameters that are more closely associated with clinical outcomes.
P181: Clinical Outcomes Following Anterior Cervical Discectomy and Fusion for Patients With Central Versus Foraminal Stenosis
Bryce Basques1, Jannat Khan1, Michael Nolte1, Philip Louie1, Jeremy Mormol1, Tarush Khurana1, Landan Banks1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Anterior cervical discectomy and fusion (ACDF) is an effective surgical option for the treatment of cervical stenosis. However, the adequacy of decompression and stabilization for patients with central stenosis versus foraminal stenosis has been debated. Many advocate for the use or addition of a posterior cervical approach to the neural foramen to ensure adequacy of decompression. However, this may be associated with a number of adverse effects, including inadequacy of central or anterior decompression and persistent postoperative neck pain. The aim of this study was to assess the effectiveness of ACDF alone across a number of postoperative clinical outcome measures for patients with central stenosis, foraminal stenosis, or both. Methods: We performed a retrospective cohort analysis of patients who underwent ACDF for cervical radiculopathy or myelopathy between 2008 and 2015 by 1 of 2 senior spine surgeons at our institution. Patients were excluded from analysis if they were younger than 18 years, had a previous operation to the cervical spine, or did not meet a minimum of 6 months follow-up. Preoperative magnetic resonance imaging (MRI) was assessed to determine the location of neural stenosis and compression. Stenosis that occurred medial to the facet or uncovertebral joint in the axial plane was identified as central, whereas stenosis that occurred at, or lateral to, the facet and uncovertebral joints was identified as foraminal. Sagittal measures on plain films were also measured and analyzed, including cervical lordosis, sagittal vertical axis, fusion, and T1 angles. Patient-reported outcome measures included visual analogue scale (VAS) neck, VAS-arm, and Neck Disability Index (NDI). Objective outcome measures included the incidence of adjacent segment disease (ASD), fusion, subsidence, and reoperation rate. Bivariate and multivariate analyses were performed to account for baseline differences in patient factors. Results: In total, 381 patients met our inclusion criteria. Of these, 126 had central stenosis, 96 had foraminal stenosis, and 159 had both. Average length of follow-up was 28.2 (range 6-101) months. The central stenosis-only and foraminal stenosis-only cohorts had a significantly greater percentage of females compared with the cohort with both central and foraminal stenosis (56.35% and 54.74% vs 40.25%, respectively), with no additional baseline differences between groups (Table 1). There were no significant differences in the preoperative or postoperative sagittal parameters (Table 2) as well as in the amount of sagittal plane change from preoperative to postoperative between cohorts on multivariate analysis (Table 3). Each cohort experienced considerable improvements in patient-reported outcome measures; however, there were no significant differences in preoperative or postoperative VAS-neck, VAS-arm, or NDI scores between groups (Table 4). Similarly, there were no significant differences in the incidence of ASD, fusion, subsidence, or reoperation rate between groups (Table 5). Conclusion: Our findings suggest that ACDF offers adequate decompression and stabilization for patients with cervical stenosis, regardless of the location of neural compression as central, foraminal, or a combination of the 2. These data may help to better guide preoperative planning and consideration of surgical approach at the affected level(s).
P182: Surgical Treatment of Degenerative Cervical Spine Disease in Elderly Patients
Takahiro Tanaka1, H. Murata1, M. Sato1, R. Miyazaki1, and T. Yamamoto1
1Yokohama City University, Yokohama, Japan
Introduction: The spinal surgery for elderly patients is increasing with the increasing elderly people in Japan. Worsening of activities of daily living (ADL) due to spinal disease is one of the serious problems in elderly patients who want to live independently. Improvement with surgical treatment is expected to reduce an amount of care. Our surgical indication of cervical spine disease is (1) patient’s request, (2) surgical feasibility, (3) no disturbance of consciousness and dementia (however, it is not the limit when surgery could decrease an amount of care). There is no age restriction. We evaluated the surgical outcome of degenerative cervical spine disease in elderly patients. Material and Methods: We retrospectively reviewed 341 consecutive operative cases between January 2006 and December 2015. Forty-seven patients were 75 years old or older, and 16 of them were 80 years old or older. We analyzed 32 patients who could be followed up for over 1 year. Old patients 80 years of age or older were classified in group A (8 cases), and patients between 75 and 79 years of age were classified in group B (24 cases). The preoperative risk was evaluated by American Society of Anesthesiologists (ASA) physical status classification, and the preoperative and postoperative neurological symptoms were evaluated using Neurosurgical Cervical Spine Scale (NCSS) and odom’s Criteria. We also evaluated the length of hospitalization after surgery. Results: In group A, we treated 2 patients with anterior approach, 5 patients with posterior approach, and 1 patient with combined approach. In group B, we treated 8 patients with anterior approach and 16 patients with posterior approach. Seven patients belonged to ASA class 2, and 1 patient belonged to ASA class 3 about the preoperative risk in Group A. In Group B, 3 patients belonged to ASA class 1, 13 patients ASA class 2, and 8 patients ASA class 3. NCSS was significantly improved after surgery in both groups (group A, 11.1 ± 1.7 → 12.8 ± 1.5 [P = .0015]; group B, 10.5 ± 2.1 → 12.3 ± 1.6 [P < .0001]). In Odom’s Criteria, 7 cases in group A (88%) and 18 cases in group B (75%) could achieve the score of “good” or more. The length of hospitalization after surgery did not show significant difference between groups (group A, 12.5 ± 2.8 days; group B, 11.8 ± 4.3 days) (P = .26). Conclusion: In this study, the surgical treatment for degenerative cervical spine disease can accept for the improvement or maintenance of ADL in elderly patients, even in patients older than 80 years.
P183: The Effect of Uncinate Process Resection on Subsidence Following Anterior Cervical Discectomy and Fusion
Dong Wuk Son1, Geun Sung Song1, Sang Weon Lee1, Soon Ki Sung1, Jun Seok Lee1, and Doo Kyung Son1
1Pusan National University Yangsan Hospital, Yangsan, Republic of Korea
Introduction: Subsidence is a frequent complication of anterior cervical discectomy and fusion. Postoperative segmental micro-motion, thought to be a causative factor of subsidence, has been speculated to increase with uncinate process resection area (UPR). To evaluate the effect of UPR on micro-motion, we designed a method to measure UPR area based on pre- and postoperative computed tomography images and analyzed the relationship between UPR and subsidence as a proxy of micro-motion. Material and Methods: We retrospectively collected clinical and radiological data from January 2011 to June 2016. A total of 38 patients (53 segments) were included. All procedures included bilateral UPR and anterior plate fixation. UPR area was evaluated with reformatted coronal computer tomography images. To reduce level-related bias, we converted UPR area to the proportion of UPR to the preoperative UP area (pUPR). Results: Subsidence occurred in 18 segments (34%) and positively correlated with right-side pUPR, left-side pUPR, and the sum of bilateral pUPR (sum pUPR) (R = .310, 301, 364; P = .024, .029, .007, respectively). Multiple linear regression analysis revealed that subsidence could be estimated with the following formula: subsidence = 1.522 + 2.7 × sum pUPR (R 2 = .133; P = .007). Receiver operating characteristic analysis determined that sum pUPR ≥0.38 could serve as a threshold for significantly increased risk of subsidence (P = .005, area under curve = 0.737, sensitivity = 94%, specificity = 51%. This threshold was confirmed by logistic regression analysis for subsidence (P = .009, odds ratio = 8.471). Conclusion: The UPR measurement method confirmed that UPR was correlated with subsidence. Particularly when the sum of pUPR is ≥38%, the possibility of subsidence increased.
P184: Differences in Cervical Sagittal Alignment Changes in Patients Undergoing Laminoplasty and Anterior Cervical Discectomy and Fusion
Dong Wuk Son1, Geun Sung Song1, Sang Weon Lee1, Jun Seok Lee1, Soon Ki Sung1, and Doo Kyung Son1
1Pusan National University Yangsan Hospital, Yangsan, Republic of Korea
Introduction: Anterior cervical discectomy and fusion (ACDF) and laminoplasty (LP) are the most commonly performed procedures for degenerative cervical spondylosis. Cervical sagittal alignment (CSA) has recently been studied as an important predictor of clinical and radiological outcomes. The data from previous studies are insufficient for analysis using the recently designed CSA parameters, T1 slope (T1s), and T1s minus cervical angle (T1sCA). Material and Methods: We retrospectively collected data from patients who underwent ACDF and LP from January 2013 to May 2016. The CSA parameters included CA, sagittal vertical axis, T1s, and T1sCA. T1sCA values were used to evaluate the preoperative cervical balance (T1sCA >20°: imbalance). Clinical results were evaluated using the Neck Disability Index (NDI) and recovery rate (RR) according to the Japanese Orthopedic Association scoring system. Results: We analyzed the data of 72 patients (ACDF, n = 39; LP, n = 33). Imbalance on ACDF was associated with an increase in CA (balance: preoperative [PRE], 15.64° →follow-up [F/U], 15.74°, P = .953; imbalance: PRE, −1.14°→F/U, 8.045°, P = .008), whereas balance on LP was associated with a significant decrease in CA (balance: PRE, 16.26°→F/U, 11.59°, P = .009; imbalance: PRE, 5.36°→F/U, 2.38°, P = .249). No significant difference was found in the RR, and NDI changes in the ACDF group based on balance, but a significant difference was found in RR in the LP group (balance: 61.65 ± 19.88%, imbalance: 46.90 ± 15.71%, P = .046). Conclusion: We found a significant difference in postoperative alignment in cases of ACDF and LP according to preoperative cervical sagittal balance. The postoperative clinical results of the LP group were more affected by F/U alignment than by the degree of alignment change.
P185: Fusion Pattern in Anterior Cervical Discectomy and Fusion With Polyetheretherketone (PEEK) Cage
Ayush Sharma1, Romit Aggrawal1, Vijay Singh1, Sumit Mathapati1, Priyank Deepak1, Shourab Sinha1, Nilesh Mangale1, Jeet Savle1, and Ajay Jaiswal1
1Dr B. R. Ambedker Central Railway Hospital, Mumbai, Maharashtra, India
Introduction: Interbody fusion in anterior cervical discectomy and fusion (ACDF) with polyetheretherketone (PEEK) cage ACDF is seen by formation of bridging trabecular bone through the cage or by formation of bridging bone anterior or posterior to the cage. Aim of the study was to analyze the pattern of bony formation during fusion and functional recovery in patients who underwent ACDF with PEEK cages filled with chronOS (synthetic β-tricalcium phosphate—Depuy Synthes) Material and Methods: Prospectively collected data of all patients who underwent ACDF with stand along PEEK cages filled with chronOS was analyzed. mJOA (modified Japanese Orthopaedic Association) scoring was used to assess for functional outcomes. Only cases with more than 1-year follow-up were included in the study. Sixty cases were finally included in the study design. Two authors blinded to clinical data did independent assessment for fusion and graft subsidence based on the follow-up X-rays and CT (computed tomography) scan. Graft subsidence was further assessed by comparing the sequential follow-up X-rays. Fusion rate was assessed at 3months, 6 months, and 1-year follow-up based on < 1 mm of motion between spinous process on flexion extension X-rays, by presence of bony trabeculae between bone end plates and by formation of bridging bone anterior or posterior to cage (PEEK) across the end plates. P value less than .05 was considered significant. Results: There was statistically significant difference noted at various time intervals in postoperative MJOA scores at 3 months, 6 months, and 1 year. In 61% of cases fusion was seen by formation of bridging bone anterior or posterior to cage (PEEK) across the end plates. In rest 39, bony fusion was observed through the cage. Six months fusion rate in cases showing fusion by anterior or posterior bony bridge formation was significantly higher than those who fused through the cage (P = .05). Although 1-year fusion rate was comparable among the 2 groups. Among the 47 patients who underwent single-level noninstrumented ACDF, only 2 (4.25%) had psuedoarthrosis. The fusion rate for single-level ACDF in our series was 95.74% at 1 year. Among the 13 patients operated for 2-level noninstrumented ACDF, 3 patients (23.00%) had pseudarthrosis. The fusion rate for 2 levels ACDF in our series is 76.00%. The mean loss of segmental lordosis on follows-up X-ray was 1.88 ± 2.77°. Subsidence and loss of segmental lordosis was more in 2-level ACDF compared with 1-level ACDF. Conclusion: ACDF with PEEK cage results in good functional outcome with statistically significant improvement in postoperative MJOA scores. Fusion by formation of bridging bone anterior or posterior to cage across the end plates is the most common fusion pattern in ACDF with PEEK cage. Fusion pattern of bridging bone anterior or posterior to cage across the end plates also results in early bony fusion of cages compared with fusion pattern of bone formation through the cage.
P186: Neurologic Recovery and Quality of Life Assessment After Anterior Cervical Discectomy and Fusion in a Series of 58 Patients
Gabriele Carrabs1, Giovanni Sessa1, and Ines Di Muccio1
1Neurosurgery, Avellino, Italy
Introduction: Cervical radiculopathy is a disorder of the cervical nerve root with a combination of sensory and motor disturbance. Anterior cervical discectomy and fusion (ACDF) is the gold standard for treatment of cervical radiculopathy not conservatively treatable. The aim of the present study is a retrospective 5-year follow-up evaluation of 2 surgical goals (neurologic recovery and global quality of life) on a series of 58 patients who underwent ACDF. Material and Methods: We operated on 58 patients (26 males and 32 females) with a mean age of 56.7 years (ranging from 26 to 65 years) at our institution. The mean follow-up was 5 years. We evaluated patients with 2 end-points: neurological recovery (motor strength with MRC [Medical Research Council] scale, sensory disturbance) and global quality of life (Quality of Life Scale—QOLS). The evaluation was performed preoperatively at 6 weeks, 3 months, 6 months, 1 year, 2 years, and 5 years. Results: We performed 32 single-level and 26 two-level procedures on 58 patients included in the study. At time of surgery, 70% of patients had a sensory deficit, and recovery of sensory function was seen in 90%of patients within 2 years. An adjacent segment syndrome developed in 15% of patients at 5 years: in this group, we performed a new discectomy and fusion procedure in only 2 patients. Motor disturbance was seen preoperatively in 50% of patients with recovery at 2 years in 95% of cases. The QOLS was 7 to 5 in 80% of patients, 4 in 10% of patients, and 3 to 2 in 5% of patients. Conclusion: In our series, the motor and sensory recovery reach the maximum within 2 years from surgery. The adjacent level syndrome was the primary cause of unsatisfactory general outcome and superseed the real functional recovery after ACDF.
P187: Clinical Outcomes for 1- and 2-Level Anterior Cervical Discectomy and Fusion Utilizing an Integrated Interbody Devices: A Prospective, Nonrandomized Study
Jad Khalil1, Rick Sasso2, Ryan Snowden3, Sheetal Vinayek2, and Lisa Motowski1
1Michigain Orthopedic Institute, Southfield, MI, USA
2Indiana Spine Group, Carmel, IN, USA
3Tennessee Orthopedic Alliance, Nashville, TN, USA
Introduction: Anterior cervical discectomy and fusion (ACDF) is an effective, reliable, and safe treatment modality in the treatment of cervical disc disease. However, there is very little in the literature concerning outcomes data on “stand-alone” devices. This work presents the first prospective, non-randomized trial in patients undergoing 1- and 2-level anterior cervical fusions with an integrated interbody device. Material and Methods: A total of 144 patients underwent an IRB (institutional review board) approved study of 1- and 2-level ACDF with an integrated interbody device. Only patients who had reached a minimum 12 months follow-up were evaluated for a total of 53 patients. We obtained baseline clinical exams, Neck Disability Indices (NDI), visual analogue scale (VAS) scores, and EAT Dysphagia score on all patients at the following time points: preoperative, 6 weeks, 3 months, and 6 months, and 12 months postoperatively. EAT-10 was considered abnormal if greater than 3. Results: All patients underwent 1-and 2-level ACDF procedures. Of the 53 total patients, 41 patients underwent 1-level fusion, and 12 patients underwent 2-level fusion. Average surgical times were 48 minutes and 68 minutes for 1 and 2 levels, respectively. There was no significant blood loss, and average length of stay was less than 24 hours. The average NDI scores were 54 preoperatively and were significantly improved at each following time-point (< P = .001). VAS scores were 72/48/48 for neck/right arm/left arm pain preoperatively, and showed significant improvement at each following time-point (<P = .001). Five patients had abnormal EAT-10 scores preoperatively. At the 6-week postoperative visit, 9 patients had abnormal scores. The mean score was 1.75 and 2.3, respectively. All patients with dysphagia improved, and the highest EAT-10 score at 12 months was 4. The average EAT-10 score improved from 2.3 to 0.295 (P = .001) at 12 months. There were no hardware failures or adverse surgical outcomes. Conclusion: Successful anterior cervical fusion is dependent on many factors. In the age of value-based health care delivery, it is important to mitigate the potential complications of healing. This study is the first to show the successful, prospective outcomes of an integrated interbody device in a cervical spine fusion model. It shows patient-reported outcomes consistent with or better than previously reported results of both ACDF and cervical disc arthroplasty. Patient rates of dysphagia were also consistent with or lower than reports of standard ACDF dysphagia rates.
P188: Were There Relationships Between Ankylosis in the Occipitocervical Junction, Thoracic Kyphosis, and C2 High-Riding Vertebral Artery in Patients With Ankylosing: Analysis of a Cohort of 86 Cervical Fractures Treated Surgically
Nodoka Manabe1, Augusto Covaro2, Yohan Robinson3, and Claes Olerud3
1Inanami Spine and Joint Hospital, and East Maebashi Orthopaedic Hospital, Tokyo, Japan
2Institut Universitari Dexeus Hospital de Igualada, Barcelona, Spain
3 Uppsala University, Uppsala, Sweden
Introduction: The ankylosing spondylitis (AS) affects the axial skeleton and can lead to progressive ankylosis of all spinal segments. Even though commonly observed, the progress of the ankylosis in the upper cervical spine is not well documented. The aim of this study is to describe radiographical features of the relationship between hyper thoracic kyphosis, C2 high-riding vertebral artery (HRVA), and the occipitocervical (OC) junction in AS patients using a novel measure, the X-angle. Materials: Eighty-six surgically treated AS patients in a single institution for a cervical spinal fracture between 2007 and 2014, were followed prospectively using the SWESPINE registry. Patients were divided according to their C0-C1 and C1-C2 facet joint integrity in F group: fused, and NF group: nonfused articulation. All of the patients had a completely ankylosing facet joint between C3 and T1 due to their pathology. Methods: Level of cervical fracture and thoracic kyphosis: T1-T12 and T5-T12 angles were measured. The integrity of the C0-C1-C2 joints was determined by “X-angle”: novel technique by measuring the angle of C0-C1-C2 articulations in the coronal plane of the computed tomography with the objective of describing the integrity and degeneration of the occipitocervical area, and HRVA was classified into HRVA+ and HRVA− groups. Intraobserver and interobserver reliability of X-angle was determined. Results: The most common level of fracture was at C5-6, and occipitocervical ankylosis was not related to the level of fracture. C0-C1 F group had more thoracic kyphosis compared with NF group (P < .01). The patients with HRVA were older than without it and C1-C2 fused joint was related to HRVA. The mean X-angle was 125° in C0-C1 NF group and 136° in F group (P < .01). The intra- and inter-class reliabilities for X-angle measurement were very high (ICC [intraclass correlation coefficient] = 0.95, 0.98). Conclusions: Hyperthoracic kyphosis was highly related with fused OC junctional joint in patients with AS. HRVA was related with C1-2 joint change. The X-angle increased in step with vertical destruction of C0-C1-C2 joints. The X-angle is a reliable way of measuring C0-C1-C2 joint integrity in patients with AS.
P189: Integrated Screws With Cage Spacer System in the Treatment of Cervical Spine Degenerative Disease With Minimum Follow-up of 2 Years
R. S. Chahal1, and Shankar Acharya1
1New Delhi, India
Introduction: Anterior cervical discectomy and fusion (ACDF) is a widely accepted surgical treatment for cervical degenerative disease. Integrated screws with cage spacer system is a relatively new device designed for patients undergoing ACDF with the dual properties of plating and standalone cage. We are reporting our findings in term of clinico-radiological outcomes following the use of such devices in the treatment of cervical spine degenerative diseases. Methods: Retrospectively, we studied 18 patients treated with integrated screws and cage spacer system for cervical degenerative diseases with a minimum follow-up period of 2 years. We compared the preoperative visual analogue SCALE (VAS) pain score both neck and for arm, Neck Disability Index (NDI), overall cervical sagittal alignment (OSA), and segmental sagittal alignment (SSA) with the postoperative data. The final outcome was assessed with Odom’s criteria. Paired Student t test was used for statistical analysis. Results: The mean age of the patient was 46 years (range: 29-63 years) with the mean follow-up period of 28 months (range: 24-47 months). The total operated levels were 19. Out of which 11 were at C5-C6 level. The mean pain VAS score for neck and arm along with NDI improved significantly after surgery at last follow-up. The mean OSA and SSA improved from 8.00 ± 5.00 to 10.61 ± 3.50 and 3.50 ± 3.20 to 8.11 ± 4.65 at last follow-up. X-ray showed 100% fusion rate and majority of the patients had a good outcome. Conclusion: Integrated screws and cage spacer device is a safe and effective alternative for the treatment of cervical degenerative diseases.
P190: Anterior Cervical Corpectomy and Fusion in the Elderly: Complications and Outcomes Using National Database
Murray Echt1, Rafael De la Garza Ramos1, Yaroslav Gelfand1, Michael Longo2, Jonathan Nakhla3, Phillip Cezayirli1, Adam Ammar1, Neil Haranhalli1, Andrew Kobets1, Merritt Kinon1, and Reza Yassari1
1Montefiore Medical Center, Bronx, NY, USA
2Albert Einstein College of Medicine, Bronx, NY, USA
3Brown University, Providence, RI, USA
Introduction: The prevalence of complications after anterior cervical corpectomy in the elderly patient in comparison with other age groups has not been previously studied. The aim of this study is to report 30-day mortality and complication rates after cervical corpectomy using the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), a multicenter prospective database. Material and Methods: The NSQIP database was used to identify 1511 patients who underwent elective cervical corpectomy for spondylosis with or without myelopathy in between 2013 and 2014. Patients were stratified by age into 4 groups—group 1 aged <60 years, group 2 aged 60 to 69 years, group 3 aged 70 to 79 years, and group 4 aged >80 years. Thirty-day outcomes were examined, and included mortality, pneumonia, prolonged ventilation (defined as >48 hours), reintubation, and length of stay. Frequencies were compared between groups via Fisher’s exact test. Results: Overall, there were 918 (60.8%) in group 1, 398 (26.3%) in group 2, 163 (10.8%) in group 3, and 32 (2.1%) in group 4. The maximum age was 90 years. The mortality rate was significantly different between groups—0.1%, 0.3%, 0.6%, and 3.1% for groups 1 to 4, respectively (P = .039). Pneumonia was also higher with increasing age—0.1%, 0.5%, 0.6%, and 3.1% (P = .038). The average length of stay was 2.2 for all patients, 2.0 days for group 1, 2.4 days for group 2, 2.3 days for group 3, and 4.8 days for group 4 (P < .001). The reintubation and prolonged ventilation rates were found to have a trend with increasing age but did not reach significance (P = .088 and P = .087, respectively). Conclusion: We have described the morbidity rates of elderly patients undergoing anterior cervical corpectomy using the largest series reported to date. This demonstrates the significant risk of mortality and pneumonia associated with increasing age (specifically in patients 80 years or older), as well as an increased length of stay. Reintubation and prolonged ventilation were also higher but did not reach statistical significance.
P191: Impact of Anterior Plating Versus Stand-Alone Cage on Rate of Fusion, Subsidence, and Adjacent Segment Disease in Single-Level Corpectomy for Cervical Spondylosis: A Retrospective Review
Murray Echt1, Michael Longo2, Julio Inocencio1, Rafael De la Garza Ramos1, Yaroslav Gelfand1, Jonathan Nakhla3, Phillip Cezayirli1, Adam Ammar1, Neil Haranhalli1, Andrew Kobets1, Merritt Kinon1, Reza Yassari1
1Montefiore Medical Center, Bronx, NY, USA
2Albert Einstein College of Medicine, Bronx, NY, USA
3Brown University, Providence, RI, USA
Introduction: The impact of anterior plating versus stand-alone grafts in anterior cervical discectomy and fusion has been extensively studied; however, the use of a plate in anterior cervical corpectomy and fusion has not been well described. The aim of this study is to report the rate of fusion, subsidence, and adjacent segment disease in single-level cervical corpectomy with or without the use of anterior plating using a single-institution retrospective review. Material and Methods: A chart review was performed for the dates of July 2008 until June 2018. Inclusion criteria was single-level corpectomy performed for spondylosis in patients at least 18 years of age. Exclusion criteria was evidence of trauma, tumor, infection, or circumferential fusion with posterior instrumentation. Patient’s charts and radiographs were reviewed as exempt by the Institutional Review Board for retrospective studies. Fusion was scored in a binary fashion as well as scaled using criteria set by Bridwell et al. Subsidence was calculated by comparing the immediate postoperative lateral X-ray films to those obtained during follow-up visits. Subsidence was considered present if there was at least 3 mm of settling into the end plates. Rate of fusion, subsidence, and adjacent segment disease was compared using Pearson’s χ2 test (P < .05 was considered significant). Results: A total of 65 patients were identified with 38 constructs including anterior plating and 27 as stand-alone cages. Average age was 61.1 years, 55% were males, and average follow-up was 12.7 years. Patient demographics including medical comorbidities and type of graft used, 86% PEEK (polyetheretherketone) and 9% titanium, were similar between the 2 groups. Overall fusion rate was 89.2% with no difference in fusion between plate and stand-alone, 88.9% versus 89.5%, respectively (P = .94). There was no difference in the Bridwell Grading Scale for fusion. The overall subsidence rate was 38.5% with a nonsignificant increase in subsidence for stand-alone cages, 40.7% versus 36.8% (P = .75). The mean amount of subsidence was 3.3 mm versus 2.7 mm for stand-alone versus plate (P = .669). Adjacent segment disease had a nonsignificant increase with the use of anterior plating, 13.2% versus 3.7% (P = .19). Patients had similar outcomes with regard to dysphagia and symptoms as estimated using the mJOA (modified Japanese Orthopaedic Association) score. Despite relatively high rate of subsidence, there was only need for one revision surgery for hardware failure in a patient with a stand-alone construct due to the development of osteomyelitis and epidural abscess in setting of endocarditis. There were only 2 complications including one C5 palsy that improved on follow-up, and one return to the OR for evacuation of a neck hematoma. Conclusion: In this study, we affirmed the null hypothesis that there is no significant radiographic or clinical difference in using an anterior plate versus a stand-alone cage. A stand-alone graft construct may be considered for single-level cervical corpectomy for spondylosis. Larger, prospective trials with long-term follow-up is necessary to draw more definitive conclusions.
P192: Clinical and Radiographic Outcomes of Uncoforaminotomy in Anterior Cervical Discectomy and Fusion
Sung Kyu Kim1 and So Hyun Moon2
1Cheonnam National University Hospital, Gwangju, Republic of Korea
2Chosun University, Gwangju, Republic of Korea
Introduction: Anterior cervical discectomy and fusion (ACDF) is the basic procedure for relief of neck pain and upper extremity radiating pain in cervical spondylosis. However, the controversy continues as to whether uncoforaminotomy is necessary for ACDF. The purpose of this study was to evaluate clinical and radiologic result of uncoforaminotomy in ACDF. Materials and Methods: A retrospective study was performed on 40 patients (males: 11, females: 29, mean age: 57.25 ± 11.86 years) who underwent ACDF for cervical spondylosis from January 2010 to December 2016. There were 20 patients with ACDF alone, and 20 patients with ACDF and unilateral uncoforaminotomy (ACDF-U). Plate and tricortical iliac bone graft were used as fusion material in all patients. The visual analogue scale (VAS) and Odom’s criteria for patient satisfaction were analyzed for clinical outcome. Radiologic assessment included segmental angle, fused segment height on preoperative, postoperative, and last follow-up lateral radiograph. The fusion rates were compared between the 2 groups by computed tomography at 1 year postoperatively. Results: Clinical results showed statistically significant improvement of pain in ACDF-U group at final follow-up in VAS score better than ACDF only group (ACDF only: 2.25 ± 1.07, ACDF-U: 1.73 ± 0.90, P < .05). There was no statistically significant difference in patient satisfaction between 2 groups. In both groups, almost solid fusion was achieved. Fusion rates and the degree of subsidence was no statistically significant difference between the 2 groups. No complications were observed between the 2 groups, except hoarseness was found in ACDF-U group. Conclusions: Uncoforaminotomy in ACDF showed no significant difference in clinical outcome and fusion rate, except for the VAS score at final follow-up. We should pay more attention to the need for uncoforamitomy in ACDF.
P193: Correlation Between Cervical Sagittal Balance and Functional Disability in Postoperative Patients in Anterior Decompression
Gustavo Vera Perez1
1Centro Medico ISSEMYM Ecatepec, Estado de Mexico, Mexico
Introduction: The physiological sagittal alignment of the subaxial segments (c2-c7) and the suboccipital hyperextension (c0-c1-c2) are included within the ability to maintain a horizontal position for walking. It is essential to maintain the functionality during the activities of daily life. These should increase the expenditure of energy needed in the activities of daily life and often develop changes in painful cervical and lumbar alignment to maintain the walking posture, including knee flexion, pelvic retroversion, in addition to cervical hyperlordosis. All this is done to compensate as best as possible the horizontal gaze. Jeon (2017) showed that adult spinal deformities are aimed at the incident of clinical symptoms and the identification of radiographic findings can predict the curvature of progression. A previous study showed that the tilt of t1 was a key factor in the evaluation of the sagittal cervical balance, correlated with c2-7 SVA (sagittal vertical angle). The high inclination of t1 requires an extensive cervical lordosis to preserve the physiological sagittal balance of the cervical spine. Material and Methods: Retrospective, comparative place: medical center ISSEMYM Ecatepec. Subjects/selection: patients after operation of cervical spondylosis by anterior route of 2 or more levels of intervention; time: March 2015 to June 2018; procedures: (1) collection of general data, (2) analysis of records with records of NDI (Neck Disability Index) cervical functions scales and radiographic measurements described postsurgical cervical segmental sagittal cervical balance; statistical method: Pearson correlation, association with relative risk. Results: Sixty-one patients were identified (26 men, 36 women), the mean age was 63.4 years, SD 7.8, the surgical indication for cervical fusion included cervical spondylotic myelopathy (n = 16), cervical stenosis caused by ossification of the posterior longitudinal ligament (n = 37), and degenerative disc disorders (n = 8). Radiographic results and clinical results: suboccipital lordosis with a mean of 42.9° SD 8.4°, subaxial lordosis with a mean of 18.5°, SD 10.5, and range 37.0. SVA c2-c7 with an average of 32.6 mm, SD 13.3, and range 47. The inclination of t1 with an average of 27.7° range 24, SD 7.4°. NDI scale with an average of 43.1% disability, SD 19.2%. The relationships of the cervical radiographic measurements SVA c2-c7, lordosis c0-c2, lordosis c2-c7, tilt t1, were examined in correlation with the results of the functional disability scales. Very good direct correlation between NDI% and SVA c2-c7 (Pearson r = .814, P = .000), good relation NDI% and lordosis c0-c2 (r = .685, P = .000), good inverse relationship NDI% and lordosis c2-c7 (r = −.631, P = .000), moderate inverse correlation NDI% and t1 tilt (Pearson r = −.453, P = .000). Conclusion: There is a correlation between the cervical sagital balance in a significant manner and functional disability in postoperative patients of decompression anterior.
P194: Mild Degenerative Cervical Myelopathy: Two-Year Results of an Ongoing Prospective Observational Cohort
Sasha Rogers1, Bradley Jacobs1, Jacques Bouchard1, Nicolas Dea2, Roger Cho1, Steven Casha1, Stephan DuPlessis1, John Hurlbert3, Peter Lewkonia1, Paul Salo1, Alexandra Soroceanu1, Ganesh Swamy1, Kenneth Thomas1, Fred Nicholls1, and David Cadotte1
1University of Calgary Spine Program, Calgary, Alberta, Canada
2Combined Neurosurgery and Orthopaedic Spine Program, University of British Columbia, Vancouver, British Columbia, Canada
3University of Arizona, Tucson, AZ, USA
Introduction: There is controversy over the optimal treatment paradigm for patients with mild degenerative cervical myelopathy (DCM). Our objective was to evaluate a cohort of patients with a diagnosis of mild cervical myelopathy. We report the degree of impairment in baseline quality of life metrics compared with age-related norms, as well as functional disability and pain. We then report on the rate of surgical intervention and follow-up functional metrics to 2 years. Material and Methods: Patients with mild DCM (modified Japanese Orthopaedic Association [mJOA] 15 to 17) enrolled in the prospective CSORN (Canadian Spine Outcomes Research Network) registry, limited to a single centre (Calgary) were selected. Outcomes including functional status (mJOA), disability (NDI [Neck Disability Index]), pain (arm and neck pain scale), quality of life (SF-12), and health utility (EQ-5D) were evaluated at baseline, 3 months, 1 year, and 2 years for the surgical and nonsurgical cohorts. Results: Fifty patients who were enrolled prospectively over the past 2 years met eligibility criteria. Mean age was 56.2 ± 12.9 years. There were 18 females (36%). The baseline functional status was represented by a mean mJOA score of 16.20 (95%CI 15.93 to 16.47); mean neck and arm pain scores were 5.08 (95% CI 4.20 to 5.95) and 4.8 (95% CI 3.93 to 5.63), respectively. There was significant impairment in all domains of quality of life measures for the SF-12 (mean MCS −0.98 (95%CI −3.45 to 1.49) and PCS −8.06 (95 CI −11.40 to −4.72). The mean preoperative NDI was 31.8 (95%CI 25.79 to 35.97) and EQ-5D index was 0.69 (95% CI 0.57 to 0.69) and health-state VAS was 59.65 (95% CI 54.9 to 64.41). In the nonsurgical cohort (n = 16), at 3 months, there was no significant change noted in arm or neck pain scales compared with baseline, but quality of life measures suggested a reduction in mental health score (P = .005) despite an apparent improvement in physical component (P = .01), while disability measures remained unchanged. At 2 years no significant change was noted in any of the metrics. At 3 months after surgery (n = 34): mean mJOA score was 15.70 (95% CI 14.92 to 16.48). There was a reduction in neck −1.28 (95% CI −2.38 to −0.18) and arm pain −2.03 (95% CI −2.98 to −1.08, P = .01), and this was maintained at 2 years: −0.375 (95%CI −2.8 to 2.05, P = .05) and -2.75 (95% CI −5.11 to 0.387, P = .0008) respectively. While there was a significant improvement in the physical health domain 7.2 (95% CI 2.64 to 11.84, P < .0001) there was a reduction in the mental health component of quality of life −8.2 (95% CI −12.55 to −3.81, P = .006). At 2 years, the improved physical component was maintained, 2.6 (95% CI −4.12 to 9.32, P = .03), and the mental health component returned to baseline levels. The EQ-5D index improved to 0.84 (95%CI −0.11 to 1.80, P = .06), and the VAS by 11.43 (95% CI 3.22 to 19.62, P = .01). Conclusion: Within 3 months of surgery, patients with mild DCM showed benefits from intervention with regard to neck and arm pain, health-related quality of life, and health utility, which remained robust to 2 years. These findings were not noted in the observational arm.
P195: The Relevance of Bone Mineral Density on Cage Subsidence After 1- and 2-Level Stand-Alone Anterior Cervical Discectomy and Fusion
Martin Erhard1, Anna Rienmüller2, Magnus Michaelis1, Judith Bernett1, Bernhard Meyer1, and Yu-Mi ryang1
1Klinikum rechts der Isar, Technical University Munich, Munich, Germany
2Medical University Vienna, Vienna, Austria
Introduction: Anterior cervical discectomy and fusion (ACDF) is an established surgical intervention for cervical degenerative foraminal and spinal stenosis. Although it is a common and highly recognized procedure, cage subsidence remains a frequent problem possibly leading to revision surgery. So far, no clear relationship between bone mineral density (BMD) of the cervical spine and cage subsidence could be established. We therefore aimed to investigate a potential relationship between cage-subsidence and low cervical BMD. Material and Methods: We performed a retrospective analysis based on the preoperative CT (computed tomography) images of 167 patients (males = 88, females = 79) who underwent stand-alone ACDF surgery between January 2010 and December 2016. Mean age was 64 ± 12 years. A total of 81 patients received a 1-level stand-alone ACDF, whereas 86 patients obtained a 2-level surgery. Measurements of attenuation values of all vertebral bodies from C2 to C7 were performed on sagittal reformation using QCT. Cage subsidence ≥3 mm was defined as remarkable and determined on follow-up imaging after a minimum of 18 months (range: 18-31 months). The cutoff value suggested for defining osteoporosis in the cervical spine is <180 mg/mL. Results: A mean overall BMD of 213.44 ± 67.22 mg/mL (range: 64.57-460.34 mg/mL) was found in all patients. Yet, the mean BMD for patients who suffered from cage subsidence was 149.13 ± 38.4 mg/mL, and it deviated significantly from those without subsidence, where a mean BMD of 246 77 ± 53.3 mg/mL was ascertained (P < .001). A binary logistic regression analysis was performed to identify the effects of the cervical BMD on the likelihood of specific cage subsidence. Overall lower cervical BMD significantly increased the risk of cage subsidence (odds ratio [OR] = 0.942; P = .008). Concerning 1-level stand-alone ACDF, it revealed the respective segment’s upper vertebral body (OR = 0.960; P = .018) as the most important factor for cage subsidence, which was not the case for 2-level stand-alone ACDF surgery (OR = 0.979; P = .352) nor the overall cohort (OR = 0.982; P = .098). Conclusion: Our results show a clear relationship between low cervical BMD and cage subsidence in 1- and 2-level ACDF in a short-term follow-up. Calculated mean cervical BMD values in case of cage subsidence appeared below the suggested cutoff value for defining osteoporosis in the cervical spine. We therefore suggest to carefully evaluate possible patients before performing 1- or 2-stage stand-alone ACDF in relation to osteoporosis and BMD.
P196: Morphologic Variations of the Second Cervical Vertebra in Down Syndrome Compared With Age-Matched Peers
Ryan Hofler1, Daniel M Heiferman1, Ayrin Molefe2, Ryan Leduc2, Stephen Johans1, Jordan Rosenblum1, Russ P Nockels1, and G Alexander Jones1
1Loyola University Medical Center, Maywood, IL, USA
2Loyola University Chicago, Maywood, IL, USA
Introduction: This study provides a quantitative analysis of C2 morphology in Down syndrome (DS) patients compared with non-DS peers, relevant to safe placement of instrumentation. Material and Methods: Retrospective chart review identified age-matched patients, with and without DS, who underwent computed tomography scans of the cervical spine. 3D reconstructions with images through the pars, lamina, facet, and transverse foramen of C2 were used to perform measurements of anatomic structures by 2 authors. Pedicle height and width, pars axis length (PAL—distance from the facet to the anterior vertebral body through the pars), pars rostral caudal angle (PRCA—angle of the PAL to the end plate of C2), pars axial angle (angle of PAL line to the median coronal plane), lamina height, length and width, lamina angle (LA—angle of the lamina to the median coronal plane), and transverse foramen posterior distance (TFPD—distance from the posterior wall of the transverse foramen to the tangent of the posterior vertebral body) were measured bilaterally. Patients with and without DS were compared using a mixed effects model accounting for patient height. Results: Eighteen patients with and 20 without DS were included in the analysis. The groups were matched based on age and gender. Median patient height was 147 cm (interquartile range [IQR]: 142-160) in the DS group and 165 cm (IQR: 161-172) in the non-DS group (P < .001). After accounting for variations in height, mean PRCA was greater (50.86° vs 45.54°, P = .004), mean TFPD was less (−1.5 mm vs +1.3 mm, P = .001), and mean lamina width was less (6.2 mm vs 7.7 mm, P = .038) in DS. Conclusion: Patients with DS had a steeper PRCA, more posteriorly positioned transverse foramen, and narrower lamina compared with age- and gender-matched peers. These variations should be considered during surgical planning as they may have implications to safe instrumentation placement.
P197: Transcorporeal Removal of Cervical Segmental Ossification of Posterior Longitudinal Ligament in Old Age
Seyoung Pyo1 ,2, Yongwoo Shim1 ,2, Seonghwa Paeng1 ,2, and Yongtae Jung1 ,2
1Busan Paik Hospital, Busan, Republic of Korea
2Inje University, Gimhae, Republic of Korea
Introduction: Cervical spondylotic myelopathy (CSM) caused by ossification of posterior longitudinal ligament (OPLL) had been treated by directly or indirect decompression surgeries on condition of being involved number of levels or cervical alignment. However, removal of causing pathology that is OPLL have been most crucial in the decision of anterior surgical method. For removal of OPLL, discectomy or corpectomy and then fusion surgery were mandatory in general. We introduced transcorporeal removal without fusion surgery to the segmental OPLL cases. The purpose of this study is to evaluate of clinical and radiological results about this surgical method. Material and Methods: Inclusion criteria were Lhermitte’s sign and hard to use chopsticks in symptomatically, segmental type OPLL without involving disc level and not involved K-line in radiologically, and at least older than 70 years. Nonsymptomatic OPLL, multiple pathologic CSM, continuous type of OPLL, kyphosis, and younger than 70 years were exclusion criteria. From January 2015 to May 2017, 11 males and 4 females were treated by transcorporeal OPLL removal using air drill and/or Sonopet. Any fusion surgery was not combined. Treated levels were 4 cases in 1 level, 9 cases in 2 levels, and 2 cases in 3 levels. For 6 to 12 months follow-up periods, the Modified Japanese Orthopaedic Association (mJOA) score was used to assess the severity of clinical symptoms. The Neck Disability Index (NDI) were also estimated. Radiologically X-ray was used for evaluation of Cobb’s angle of cervical lordotic curvature, and the space available for the spinal cord (SAC) was measured by computed tomography scan. Results: The mean mJOA score improved from 11.8 ± 2.3 points preoperative to 15.4 ± 2.1 points at 12 months postoperative (P < .01). NDI were decreased from 20.14 ± 5.25 preoperative to 12.22 ± 4.83 at last follow-up (P < .005). The mean ratio of SAC of the OPLL level improved from 62.2% (range, 50.4-72.2) to 84.8% (range, 78.6-100; P < .0001). The mean Cobb’s angles were preserved 12.65° (range, 8.98-14.54) preoperative to 12.23° (range, 8.62-13.98) at the last follow-up (P < .05). There was no surgical event such as leakage of cerebrospinal fluid, adverse neurological symptom, or postoperative infection. Conclusion: Although our study had small cases with short-term follow-up periods, the results represent favorable in effectiveness and safety. Then transcorporeal removals of segmental OPLL in CSM can be alternative surgical option in old ages.
P198: Surgical Outcomes of Atlando-Axoidal Instabilities in Rheumatoid Arthritis
Hassen Makhlouf1, Ameur Triki1, Ahmed Jabeur1, Haroun Bouhali1, Bouzid Lanouar1, Abdelhakim Kherfani1, and Mondher Mestiri1
1Kassab Institute, Manouba, Tunisia
Introduction: Due to the delay of diagnosis of rheumatoid arthritis in developing countries such as Tunisia, patients are seen in advanced stages, and therefore, surgical management of its deformities is challenging. The upper cervical spine location is a severe turning point in the medical history of a patient with this polyarticular disease. The treatment of occipitocervical instability aims to restore spinal stability, to prevent spinal cord injuries, and to improve the neurological status. Multiple surgical techniques were described basing on the same principles: decompression and arthrodesis. Materials and Methods: This was a retrospective study of 30 patients operated for unstable upper cervical spine in rheumatoid arthritis and treated in Kassab Institute between March 1985 and December 2014. Data gathering was performed through a clinical and radiological examination prior to surgery, in postoperative and at a minimum of 1-year follow-up. Results: Patients were predominantly female, with an average age of 50.2 years. The instability was anterior in 56.6% of cases, vertical in 10% of cases and combined in 33.3%. C1C2 arthrodesis was performed in 7 cases and occipitocervical arthrodesis in 23 cases. Before surgery, 40% of patients were Ranawat class 1. In follow-up, the class 0 was predominant and found in 47% of cases. Fifty-two percent of patients improved their neurological status, the remaining half were stationary. The average radiological Ranawat index moved from 14.2 mm preoperatively to 13.1 mm at last follow-up. Among the 7 patients with C1C2 fusion, 4 developed a vertical instability. Conclusion: C1C2 arthrodesis does not avoid progression toward vertical instability. The occipitocervical arthrodesis gives better stability, fewer nonunion, and shorter immobilization without significant morbidity. Despite added stiffness, occipitocervical fusion would be a more adequate procedure in our particular population.
P199: Cervical Alignment and Range of Motion After Myoarchitectonic Spinolaminoplasy With Titanium Plate
Seishi Matsui1, Seiji Shigekawa1, and Naoki Shinohara2
1Ehime University, To-on City, Japan
2HITO Hospital, Japan
Introduction: Myoarchitectonic spinolaminoplasy (MSLP), which utilizes a hydroxyapatite (HA) implant as a substitute for the spinous process, is an effective procedure for cervical spondylotic myelopathy (CSM). It can preserve all of the nuchal musculature and prevent the postoperative diminution in lordosis. The HA implant, however, have disadvantages such as lack of plasticity and occasionally difficulty in fixation. The authors have performed MSLP with a titanium plate (Laminolasty Basket: LB) in place of the HA implant. This LB was easily fixed to the laminar flaps with 5-mm or 7-mm length screws and connected to the spinous process by suture. This study aimed to analyze changes in neurological condition, cervical sagittal alignment, and range of motion (ROM) after MSLP with LB. Material and Methods: Fourty-one patients with CSM (25 males and 16 females, with a mean age of 66.6 years) who underwent MSLP with LB in 3 or 4 laminae with at least 2 years follow-up were enrolled. The Neurosurgical Cervical Spine Scale (NCSS: full score, 14 points) was used to evaluate neurological condition. The C2-C7 angle was measured on the lateral radiographs in the neutral and flexion-extension position. The ROM was assessed by the difference in the C2-C7 angle between flexion and extension. Results: The mean NCSS was 9.4 points before surgery and 12.8 points at 2 years after surgery. The improvement rate was 73.9%. In the neutral position, the mean C2-C7 angle was 8.1° before surgery and 10.3° at 2 years after surgery. In the flexion position, it was 10.6° and 5.1° of kyphosis, showing significantly difference of 5.5°, and in the extension position, it was 21.0° and 20.3° before and 2 years after surgery, respectively. The mean ROM at 2 years after surgery was 80.7% of the preoperative value. In 9 patients with preoperative kyphosis >0°, the mean C2-C7 kyphotic angle in the neutral position was 4.0° before surgery and 0.1° at 2 years after surgery, showing significant difference. Conclusion: Neurological improvement rate was 73.9%. The cervical sagittal alignment was slightly increased in lordosis even among patients with kyphosis during follow-up period. The ROM of the cervical spine was mildly decreased due to the restriction of flexion in the neck by this procedure. Compared with previous reports, this study demonstrates that MSLP with LB results in better preservation of the cervical alignment and ROM.
P200: The Relationship Between Gastrointestinal Comorbidities, Clinical Presentation, and Surgical Outcome in Patients With Degenerative Cervical Myelopathy: Analysis of a Global Cohort
Aria Nouri1, So Kato2, Hamed Reihani-Kermani3, Kishan Patel4, Daniel Sciubba5, Jetan Badhiwala6, Jefferson Wilson6, Enrico Tessitore7, Joseph Cheng1, and Michael Fehlings6
1University of Cincinnati, OH, USA
2University of Tokyo, Tokyo, Japan
3Kerman University of Medical Sciences, Kerman, Islamic Republic of Iran
4Yale School of Medicine, New Haven, CT, USA
5Johns Hopkins School of Medicine, Baltimore, MD, USA
6University of Toronto, Toronto, Ontario,Canada
7University of Geneva, Geneva, Switzerland
Introduction: Degenerative cervical myelopathy (DCM) is the most common cause of spinal cord impairment in adults, presenting most frequently in patients 50 years or older. Gastrointestinal comorbidities (GIC) commonly occur in this group, but their relationship with DCM has not been thoroughly investigated. It is the objective of the present study to investigate the difference between patients with or without GICs who are surgically treated for DCM. Material and Methods: A cohort of 757 patients with clinical data and 458 with MRI (magnetic resonance imaging) data from the AOSpine NA and AOSpine International study on DCM were evaluated. GIC were obtained at presentation and included gastric, intestinal, hepatic, and pancreatic conditions. Patients were dichotomized into 2 groups: with GIC and without GIC. Clinical and MRI presentation and baseline neurological and functional status were compared. Neurological and functional outcomes at 2-year follow-up were also compared. Results: GIC were present in 121 patients (16%). These patients were less commonly male (48.76% vs 65.4%, P = .001), were slightly less neurologically impaired based on Nurick grade (3.05 ± 1.10 vs 3.28 ± 1.16, P = .044) but not based on mJOA (modified Japanese Orthopaedic Association; 12.74 ± 2.62 vs 12.48 ± 2.76, P = .33), had a worse general health score (71.27 ± 16.88 vs 75.22 ± 17.08, P = .022), worse neck disability (46.31 ± 20.04 vs 38.23 ± 20.44, P < .001), and a lower prevalence of upper motor neuron signs (hyperreflexia, 70.2% vs 78.9%, P = .037; Babinski’s sign 24.8% vs 37.3%, P = .008). On MRI, GIC patients less commonly exhibited signal intensity changes (T2 hyperintensity, 49.2% vs 75.6%, P < .001; T1 hypointensity, 9.7% vs 21.1%, P = .036) and had a lower number of T2 hyperintensity levels (0.82 ± 0.98 vs 1.3 ± 1.11, P = .001). There was no difference in surgical outcome between the groups. Conclusion: DCM patients with GICs are more likely to be female and have significantly more general health impairment and neck disability. However, these patients have less clinical and MRI features typical of more severe neurological impairment. This constellation of symptoms is considerably different than those typically observed in DCM, and it is therefore plausible that nutritional factors including B12 deficiency, which frequently manifests in elderly patients may contribute to this unique observation.
P201: Complication Rates and Revision Surgery After Anterior Cervical Corpectomy and Fusion Using PEEK Cage
Anna Rienmüller1, Judith Bernett2, Martin Erhard2, Bernhard Meyer2, and Yu-Mi ryang2
1Medical University Vienna, Vienna, Austria
2Klinikum rechts der Isar, Technical University Munich, Munich, Germany
Introduction: Although anterior cervical corpectomy and fusion (ACCF) is a common surgery, this procedure, indications, complication and revision rates, and implants used in ACCF are discussed controversially. So far it is not clear if additional posterior stabilization is necessary or not with regard to revision surgery and cage subsidence. Material and Methods: We performed a retrospective analysis of our prospectively collected database of all patients undergoing one or multilevel ACCF between January 2010 and June 2016. For stability reason, all patients undergoing ACCF had additional ventral plating and in case of more than 2 vertebral level resection received additional dorsal stabilization. We analyzed patient demographics, intra- as well as postoperative complication rates and revision surgeries. Results: We found 153 patients (females = 69, males = 84) with a mean age of 75 ± 15.5 (range 11-87) years at the time of surgery. Indication for surgery was metastasis in 40 cases, spinal canal stenosis in 33, revision of ACDF in 21, trauma in 17, degenerative lesions in 19, primary tumor in 12, and spondylodiscitis in 11 cases. Additional ventral plating in the same intervention was performed in 149 patients, in a secondary attempt dorsal stabilization was performed in 96 patients. No intraoperative implant associated complications, in case of malignant disease blood loss was common and had to be substituted. The postoperative surgical complication rate was 3.9% (1.9% postoperative bleeding 1.3% infections, 0.65% superficial wound infections). A total of 3 patients underwent revision surgery after a mean time of 18 ± 8 months. No significant differences were found in relation to number of segments involved and number of surgeries performed. Conclusion: In relation to our results ACCF seems to be a valuable tool. Intraoperative and postoperative complication rates are low for 1-level and multilevel vertebral body replacements. Although fairly invasive, also after additional dorsal stabilization complication rates and infection rates are fairly low. We therefore conclude the use of ACCF for various above-mentioned pathologies is a safe method with and without additional posterior stabilization.
P202: New Surgical Method of Cervical Fractures in Ankylosing Spondylitis Using a Ventral Plate, Vertebral Body Screws and Cement Augmentation Into Vertebral Bodies
Árpád Viola1
1Péterfy S. Hospital and Accident Centre, Budapest, Hungary
2Semmelweis University, Budapest, Hungary
Introduction: In case of unstable subaxial spinal fracture of the elderly, it is often the patients’ general condition that limits us in performing optimal surgical treatment. We are often forced to make compromises. Ideally, dorsal and ventral stabilization together would be appropriate; however, the surgical tolerance of the patients is limited. We introduce a novel spinal surgical procedure in 18 patients where 1 ventral cervical spine surgery was effective in providing stability for the spinal column. Material and Methods: The new procedure was used in 18 patients over 65 years of age with unstable subaxial cervical spine fractures. No severe neurological deficit was detected at the patients, and their main complaint was the intense local pain in the cervical spine. All 18 patients had ankylosing spondylitis. They suffered their fracture as a result of banal trauma—trip and fall—in 13 cases and traffic accident in 5 cases. The surgery was extended to 2 segments above and 2 below the fracture, 4 segments in total. Following ventral exploration, the plate was placed on the spinal column and bone cement was injected via 10 gauge needles from ventral access into all 4 vertebral bodies from both the left and right side. Using the access point of the needles, the plate was fixed to the spinal column by screws. Results: One patient has died due to cardiac decompensation 10 days after the surgery. In 17 patients, the preoperative pain has decreased by 4.9 units on the 10-unit VAS (visual analogue scale). In 17 patients remained ambulatory after the surgery and can lead a full life. Conclusion: Based on our experience, the above-described surgical procedure is appropriate for the treatment of unstable cervical spine fractures in elderly patients with ankylosing spondylitis and provides sufficient stability for the injured cervical spine; therefore, no dorsal stabilization is necessary. By filling the hollow vertebral body with bone cement, there is no need to use bicortical screws.
P203: Stand Alone Multiple Anterior Cervical Cages
Sherif Elghamry1, Youssry Elhawary1, and Mohamed Khattab1
1Orthopedic and Spine, Cairo, Egypt
Introduction: Anterior cervical discectomy and fusion is common surgical procedure for treatment of cervical spondylotic radiculopathy and/or myelopathy after failure of conservative management. Previous studies of multilevel cervical discectomies and fusions have shown decrease fusion rates with increase number of surgical levels. Fusion rate and sagittal contour is better with anterior plating but complications like increase dysphagia rates, tracheoesophageal lesions, plate malposition, and accelerated adjacent disc degeneration, even when low-profile plates are used. Further to avoid the adverse effect of autograft harvesting techniques allograft can be used. Cages were used to add stability and prevent graft complications. Stand-alone PEEK (polyetheretherketone) cages filled with allograft were used in 3 to 4 levels anterior cervical discectomy and fusion. Aim: To assess the clinical and radiological efficacy of stand-alone multiple level cervical cages in treatment of degenerative cervical disc disease. Materials and Methods: Thirty-three patients (18 males, 15 females), 28 with cervical spondylotic radiculopathy and 5 with cervical spondylotic myelopathy was treated with multiple levels anterior cervical discectomies and fusion using stand-alone PEEK cages filled with allograft. Total numbers of levels114, 18 patient operated for 3 levels ACDF and 15 patients operated for 4 levels. Clinical evaluation using visual analogue scale (VAS), Neck Disability Index (NDI), and patient satisfaction were analyzed. Cervical lordosis, cervical fusion, and complications were assessed. Results: Improvement of the clinical outcome and the radiological parameters were detected.1-3 Conclusion: Three to 4 levels anterior stand-alone PEEK cages filled with allograft is very good option for treatment of degenerative cervical disc disease with low complication rate, good clinical, and radiological outcomes.
Reference
1. Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine. 2007;6:298-303.
2. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008;15:1017-1022.
3. Healy AT, Sundar SJ, Cardenas RJ, et al. Zero-profile hybrid fusion construct versus 2-level plate fixation to treat adjacent-level disease in the cervical spine. J Neurosurg Spine. 2014;21:753-760.
P204: A Systematic Review of Spinal Cord Serum and Cerebrospinal Fluid Biomarkers for Use in Degenerative Cervical Myelopathy
Benjamin Davies1, Max Stewart1, and Mark Kotter1
1University of Cambridge, Cambridge, UK
Introduction: While radiological evidence of compression is the hallmark of degenerative cervical myelopathy (DCM), it is unable to stage or prognosticate. Moreover, asymptomatic spinal cord compression is common, and therefore, new methods of assessing spinal cord function are required. We aimed to (1) evaluate the evidence base for serum and CSF biomarkers of spinal cord damage in diagnosis, prognosis, or predicting response to treatment in DCM and (2) identify serum and CSF biomarkers of spinal cord damage studied in other conditions, which may have relevance to DCM. Material and Methods: A search of MEDLINE and EMBASE was performed. Studies involving DCM patients or biomarkers relevant to spinal cord pathobiology were included. Results: A total of 852 results were screened, of which 83 were included. Nine studies explored 12 biomarkers in DCM. NFH (N = 3), S100b, and NSE (N = 2) received most study. Seventy-four studies explored a further 118 biomarkers in other conditions; S100b (N = 13), NFH (N = 11), and GFAP (N = 10) received most study. Overall, 72 studies used targeted approaches, in which candidate biomarkers were chosen in advance. Eleven used unbiased approaches, in which high-throughput analyses identified candidate biomarkers during the study. Conclusion: The evidence base for use of biomarkers in DCM is limited. While-targeted approaches have identified a number of candidate spinal cord markers, few have shown clinical utility. There is a shift toward investigating panels of multiple markers and unbiased, high-throughput approaches.
P205: Impact of Pre-Surgical Self-Reported Exercise on Post-Surgical Outcomes in Patients With Cervical Pathology
Mark Xu1, Michael Johnson1, and Mohammad Zarrabian1
1University of Manitoba, Winnipeg, Manitoba, Canada
Introduction: There is evidence that preoperative physical fitness affects surgical outcomes, specifically preceding abdominal, cardiovascular, and spine surgery. To our knowledge, there are no articles on self-reported exercise frequency as a predictor of cervical spine surgery outcomes. Our objectives were to quantify self-report of exercise frequency in cervical spine surgery patients, and to elucidate if self-reported exercise prior to surgery confers less pain, improved health state, and/or less disability post-surgery. Material and Methods: We performed a retrospective review of prospectively collected data from the Canadian Spine Outcomes and Research Network (CSORN) database from the time of its inception. Inclusion criteria specified all elective cervical surgery patients over 18 years with degenerative pathology who proceeded to surgery and completed the pre- and postoperative outcomes measure up to 24 months post surgery (n = 460). Outcome measures were visual analogue scales (VAS) for neck and arm pain, Neck Disability Index (NDI), and EuroQOL score at baseline and 3, 12, and 24 months postoperatively. Exercise frequency was self-reported as “none” (n = 212) versus “some” (n = 248). These groups were further categorized into “none due to physical limitations,” “none” (not due to physical limitations), those to exercised “once or less per week” and those who exercised “twice or more per week.” Student’s t tests were used to compare the mean scores of the outcome measures, and analysis of variance for subgroup comparisons, with results considered significant at P < .05. Results: At baseline, 56% of total patients reported exercise prior to surgery, of which 73% reported doing so twice or more per week. Of the 44% reporting no exercise, 74% could not exercise due to physical limitations. Those who reported “some” exercise had more favorable VAS neck and arm pain scores preoperatively (neck: 5.55 vs 6.11, P < .001) (arm: 5.69 vs 6.04, P = .011), but no difference at 3 and 24 months postoperatively. Significantly lower NDI scores and higher EuroQOL Index scores were seen in the exercise group compared with the no exercise group preoperatively (NDI: 39 vs 48, P < .001; EuroQOL: 0.60 vs 0.50 P < .001) as well as at 3, 12, and 24 months postoperatively (NDI: 24 vs 31, P = .007) (EuroQOL: 0.75 vs 0.68, P = .001). Further subgroup analysis demonstrated that compared with the “no exercise due to physical limitation” group, the “twice or more” exercise group showed favorable NDI and EuroQOL scores up to 24 months postoperatively (NDI: 24.32 vs 32.33, P = .001) (EuroQOL: 0.76 vs 0.66, P = .001), whereas the “once or less times per week” group no longer demonstrated any significant difference at 24 months. Conclusion: Self-reported exercise prior to cervical spine surgery does not predict improved long-term neck and arm pain at 2 years postoperatively. However, self-reported exercise does demonstrate less disability and improved health state at baseline and up to 2 years postoperatively and this relationship is dose dependent.
P206: Recode Degenerative Cervical Myelopathy (DCM) Protocol: An International, Multi-Stakeholder, Consensus Process to Define the Research Objectives and Common Data Elements for DCM
Benjamin Davies1, Bizhan Aarabi2, James Harrop3, Michael Fehlings4, Robert Grossman5, Sukhvinder Kalsi-Ryan1, Shekar Kurpad6, Brian Kwon7, Iwan Sadler8, Jefferson Wilson4, Michelle Starkey1, and Lindsay Tetreault1
1University of Cambridge,Cambridge, UK
2University of Maryland, College Park, MD, USA
3Thomas Jefferson University Hospital, Philadelphia, PA, USA
4University of Toronto, Toronto, Ontario, Canada
5Houston Methodist Hospital, Houston, TX, USA
6Medical College of Wisconsin, Wauwatosa, WI, USA
7University of British Columbia, Vancouver, British Columbia, Canada
8Myelopathy.org
Introduction: Degenerative cervical myelopathy (DCM) affects up to 5% of people older than 40 years. Currently few patients make a complete recovery, retaining lifelong disabilities and among the lowest quality of life scores of all chronic diseases. Research inefficiency is present in DCM research, including extensive research duplication and incompatible research synthesis due to varying outcome reporting. Given the significant unmet needs such inefficiencies need to be overcome. These have been addressed in other health fields by defining research priorities and standards for research reporting. Materials and Methods: A multistakeholder, DELPHI consensus process will be conducted online, to inform an eventual face-to-face consensus meeting. Health care professionals, patients, carers, scientists, and industry will be approached to participate. The research priority component will be overseen by the James Lind Alliance, NIHR, UK, and the minimum dataset component in accordance with the Core Outcomes in Effective Trials, University of Liverpool, UK. This project is supported by the AO Spine foundation. Results: Findings will be published and disseminated using a quality improvement strategy, with uptake reviewed at 5 years from publication. The minimum reporting set will be refined by the steering committee to provide an abridged version suitable for DCM clinical surveillance and audit. Conclusions: This project will define the minim reporting set for DCM clinical trials and the research priorities for DCM research. Interested stakeholders can register at myelopathy.org/recodedcm.html.
P207: Long-Segment Posterior Fusion Involving the Cervicothoracic Junction: How Distal and Proximal Extensions Affect Long-Term Outcomes?
Adam D’Sa1, Wataru Ishida1, Arun Chandra1, Joshua Casaos1, Alexander Perdomo-Pantoja1, Seba Ramhmdani1, Ziya Gokaslan2, Nicholas Theodore1, Jean-Paul Wolinsky3, Daniel Sciubba1, Ali Bydon1, Timothy F. Witham1, and Sheng-Fu L. Lo1
1Johns Hopkins University, Baltimore, MD, USA
2Brown University, Providence, RI, USA
3Northwestern University, Chicago, IL, USA
Introduction: Long-segment posterior spinal fusion involving the cervicothoracic junction carries higher complication rates due to its unique anatomy and biomechanical stress as compared with nonjunctional regions. To address this issue, the extension of fusions from C7 to the thoracic spine and/or C3 to C2 is oftentimes performed. However, the impact of the caudal extension in conjunction with the rostral extension on clinical outcomes has not been well characterized in the literature yet. Methods: Retrospective clinical record review from 2010 to 2015, identified 162 patients undergoing long-segment posterior cervical or cervicothoracic fusion (C3-C7, C3-T2, C2-C7, or C2-T2) for degenerative diseases, trauma, or infection with a minimum 1-year follow-up period. They were sub-classified into the 2 groups: fusions ending in the cervical spine (group 1, n = 60) and those ending in the thoracic spine (group 2, n = 102). Rates of pseudarthrosis, adjacent segment disease (ASD), and overall surgical revision were compared as primary outcome measures. Fisher’s exact tests (categorical variables), unpaired t tests (continuous variables), and nominal logistic models (multivariate analyses) were performed to identify factors affecting primary outcome measures. P values < .05 were defined as statistically significant. Results: There were no statistically significant differences in baseline characteristics such as age, BMI (body mass index), and gender. Group 2 had significantly higher estimated blood loss (mL; (275.0 ± 218.4 [group 1] vs 488.0 ± 561.3 [group 2], P < .001) and longer operative time (minutes; 210.7 ± 48.5 vs 290.5 ± 84.8, P < .001) and hospital stay (days; 3.5 ± 2.1 vs 6.1 ± 3.2, P < .001) than those in group 1. Rates of all 3 primary outcomes were comparable between the 2 groups, with the trend of lower incidences of pseudoarthrosis and ASD in Group 2 (overall surgical revision rate: 27.9% vs 20.6%, P = .34; overall pseudarthrosis rate: 9.8 vs 2.9%, P = .08; overall ASD: 11.5% vs 3.9%, P = .10). In multivariate analysis of rates of localized pseudoarthrosis and ASD, C7 to T2 extension (group 1 vs group 2) independently reduced rates of pseudoarthrosis at the most distal level (P = .02) and distal ASDs (P = .04), whereas C3 to C2 extension was independently protective against pseudoarthrosis at the most proximal level (P = .01) and proximal ASDs (P = .03). Conclusion: While the overall rates of the adverse surgical outcomes in long-segment posterior fusions involving the cervicothoracic junction were not affected by C7 to T2 extension with statistical significance, the rates of pseudoarthrosis and ASDs at distal and proximal segments were independently reduced by C7 to T2 and C3 to C2 extension, respectively, with statistical significance. Given these improved long-term outcomes, the judicious selection of the uppermost fusion level and the lowermost fusion level should be weighed against the detrimental short-term outcomes, including higher estimated blood loss as well as longer operative time and hospital stay associated with the caudal extension, in treating this patient population with unique biomechanical considerations.
P208: Detection of Titanium Alloy Cervical Spine Implants by Current Metal Detectors
Sebastian Fras1, and Christian Fras1
1Institute for Spinal Surgery, Broomall, PA, USA
Introduction: Security measures at airports and government buildings typically includes use of walk-through metal detectors, prompting inquiries from many patients prior to spinal instrumentation procedures. The literature suggests previously a significant incidence of detection of orthopedic implants by metal detectors, with recent studies indicating a decrease in this incidence, possibly related to greater refinement of the metal detectors. Prior studies have suggested stainless steel and cobalt chrome implants in scoliosis correction surgery may trigger alerts by metal detectors. This study was undertaken to assess if modern titanium alloy implants used specifically in the cervical spine–triggered alerts in metal detectors currently in actual use in the United States. Materials and Methods: A telephone interview was conducted with patients who had undergone anterior cervical plate fixation within the past 7 years, and inquiring if the patient had gone through a walk-through metal detector at an airport or courthouse within the past 2 years; and, if so, if they had triggered an alert. All patients had titanium alloy anterior cervical plate implants made either by Globus or Medtronic Corporation. The results were then tabulated. Results: Fifty-five consecutive patients who met the above criteria and who had passed through a metal detector were contacted. Of these, 26 had a 1-level construct inserted (plate and 4 screws); 24 had a 2-level construct inserted (plate and 6 screws); and 5 had more than a 2-level construct inserted (plate and greater than 6 screws) inserted. Sixteen had passed through a metal detector once; 39 had passed through a metal detector more than once. None of the patients ever triggered an alert of a walk-though metal detector. There were zero (0/55) patients who reported triggering an activation after they had passed through a metal detector. Conclusions: In previously published studies, the frequency of detection in patients with orthopedic implants in walk-through metal detectors varied based on the nature of the implant, and the age of the study; in the past, total hip replacements triggered alerts more frequently than other implants, with the overall incidence of detection noted to be less frequent in more recent studies than in older studies. In the spine literature, studies have noted alerts to have been triggered in some (but not all) patients with stainless steel and/or cobalt chrome implants for scoliosis correction. In this study focusing on titanium alloy anterior cervical implants, there were no alerts in 55 consecutive patients with recent experiences going through metal detectors in the United States. This information may be used to reassure patients about to undergo anterior cervical spine instrumentation with titanium implants that passing through a metal detector is not expected to trigger an alert, and that medical documentation of the presence of such implants is not needed.
P209: Parameters of Evaluation of Sagittal Cervical Equilibrium in Healthy Patients of the Medical Center ISSEMYM Ecatepec
Iris Sotelo1, Amado González1, Juan Guzmán1, and Gustavo Vera1
1Issemym Ecatepec Medical Center, Estado de México, Mexico
Introduction: It has been demonstrated that the sagittal balance is closely related to the symptoms, the quality of life, and the independence or disability of the patients, so that it becomes increasingly important in the assessment, management, and surgical planning. Its study is so recent that universally accepted parameters do not exist until now, each author proposes what he considers appropriate among them Le Huec in France and Lee and Youn in Korea among others. Below are the most commonly reported and those who have shown some kind of clinical relevance. Objective: There are no established values as standard in the literature for the evaluation parameters of cervical sagittal balance in healthy patients. This study describes cervical sagittal parameters in healthy patients. Material and Methods: Study conducted in a third-level hospital in 150 healthy patients by means of the evaluation of cervical spine radiographs in a lateral projection. The Cobb method was used for the evaluation of the cervical lordosis from C2 to C7, measure of the inclination of T1 (T1 slope), and plumb line of C7 to S1 (SVA [sagital vertical axis] C7-S1), and the angle of O-C2. Statistical analysis of the data was performed to obtain an average of the parameters. Results: Total of 90 patients were women (60%) and 60 men (40%). The average of the SVA values for C1-C7 the average is 33.37 mm, for C2-C7 the average was 20.64 mm. For the Cobb angle C2-C7, the average was 14.2 °. The tilt of T1 the average was of 25.23° and of the angle of O-C2 the average was of 34.83°. Conclusion: There is an important number of measurements and spinocranial parameters, some of which have shown important associations such as the slope of C7 and the magnitude of the cervical lordosis or how the increase of the SVA is related to a decrease in the quality of life.
P210: Comparison of Zero-P Spacer Versus Plate-and-Cage After 1-Level ACDF With Uncinate Process Resection: Three-Year Assessment of Radiographic and Clinical Outcomes
Sung Hyun Noh1 ,2 and Kyung Hyun Kim1 ,2
1Gangnam Severance Hospital, Seoul, Republic of Korea
2Yonsei University College of Medicine, Seoul, Republic of Korea
Objective: When conducting cervical foraminal stenosis with collecting osteophyte or uncovertebral hypertrophy, surgeons perform uncinate process resection (UPR) with anterior cervical discectomy and fusion (ACDF). The purpose of this study is to compare of Zero-profile device (Zero-p) and traditional plate-and-cage implant (Plate-and-Cage) in ACDF with UPR to treat 1-level cervical degenerative disc disease. Methods: We retrospectively surveyed the data from all patients who underwent single-level ACDF with UPR between 2011 and 2015. In total, 80 patients participated in 3 years of follow-up. Among them, a Zero-p (38 patients) and Plate-and-Cage (42 patients) were used in ACDF with UPR. Visual analogue scale (VAS), Neck Disability Index (NDI), and Odom’s criteria were evaluated at preoperation, immediately postoperation, and last follow-up. Moreover, radiographic studies were reviewed retrospectively. The demographics, age, sex, body mass index (BMI), diabetes mellitus (DM), and smoking in the 2 groups were compared. Radiographic parameters of disc height, C2-C7 lordosis, T1 slope, C2-C7 sagittal vertical axis (SVA), center of the sellar turcica/C7 SVA (St-SVA), spinocranial angle (SCA), and fusion rate were estimated on plain radiographs at preoperation, immediately postoperation, and during the follow-up period (median follow-up duration: 37.1 ± 18.2 months). Results: The duration of operation, intraoperative blood loss, and the length of hospitalization were significantly lower in the Zero-p than Plate-and-Cage groups (P < .05). The clinical outcomes such as VAS, NDI, and Odom’s criteria were improved after operation. The fusion rates, C2-C7 lordosis, T1 slope, C2? C7 SVA, St-SVA, and SCA after single-level ACDF were not significantly different between the 2 groups. Subsidence occurred in 11 cases (26%) in the Zero-p group and 20 cases (54%) in the Plate-and-Cage group. Horizontal length of Zero-p implant is longer than that of allobone graft. Fusion occurred in 39 cases (98%) in the Zero-p group, 36 cases (94%) in the Plate-and-Cage group. Conclusions: Subsidence occurred more frequently Zero-p than Plate-and-Cage after ACDF with UPR. Surgeons should be known of these results so that postoperative complication such as subsidence can be avoided.
Degenerative Lumbar
P211: Mismatch Between Rod Bending and Actual Postoperative Lordosis in Lumbar Arthrodesis With Poly Axial Screws
Abdollah Moufid1, Thibault Cloché2, Soufiane Ghailane2, Amine Ounajim3, Tanguy Vendeuvre1, and Olivier Gille2
1 Orthopedic Department, Spine Unit, Poitiers, France
2 Spine Unit, Bordeaux, France
Introduction: The question of rod bending is essential during posterior lumbar fusion. The role of posterior instrumentation during spinal surgery remains to be defined: just maintaining the correction or also helping to get the good angles to fuse the operated segment in a proper curve. Despite an appropriate bending, a mismatch between rod lordosis and lumbar lordosis can occur. There is no study on the link between rod bending and postoperative vertebral lordosis. The purpose of this study was to evaluate parameters that explain the mismatch between lumbar lordosis and rod bending in lumbar surgery using polyaxial screws. Material and Methods: This study was monocentric, descriptive, and analytic. All patients with degenerative lumbar disease who needed posterior L3L5 fusion in a university-affiliated hospital in 2017, were included. Patients with past surgical history of anterior fusion on the levels L3L5, coronal malalignment with a Cobb angle greater than 5°, and the use of dynamic fixation systems were excluded. We measured on a standing profile X-ray: pelvic incidency, lumbar lordosis, lordosis of the instrumented segment, and rod lordosis. We define 3 parameters: the homogeneity of the distance between posterior wall and rod (SD), which reflect how homogeneously the screws are put in depth, the angle between screw and rod: theta Mismatch Angle (thetaMA), the angle between screw and superior endplate: lambda Mismatch Angle (lambdaMA). Univariate and multivariate analysis were conducted to see if there was a link between all those parameters and the mismatch: vertebral lordosis–rod lordosis. Results: Seventy-four patients were included, mean age was 67 years. Eighteen were 360° fusion and 56 were postero-lateral fusions. There was no statistical association between demographic data, pelvic parameters, use of interbody devices, and the mismatch. There was a statistical association between thetaMA, lambdaMA, SD, and the mismatch (P < .0001). A multivariate linear regression model was developed to create a new index: Mismatch Analysis Index. Conclusion: Our study is the first on the link between rod bending and lumbar lordosis. We spotted 3 factors involved in not obtaining on the spine the lordosis we put in the rod in short lumbar fusion with polyaxial screws. Two factors are depending on the way the surgeon positions screws: parallel to the superior vertebral endplate (lambdaMA), and with a homogeneous depth (SD). And the last factor: ThetaMA is depending on the surgical technique (compression on screws, osteotomies, monoaxial screws, use of interbody devices).
P212: Transforaminal Interbody Fusion With Unilateral Pedicle Screw Fixation (UNILIF): 46-Patient Prospective Series
Mario Cahueque1, William Lopez1, and Enrique Azmitia1
1Hospital Centro Medico, Guatemala City, Guatemala
Introduction: The success of lumbar spine fusion depends on good patient selection. Bilateral pedicle instrumentation with transforaminal interbody fusion, now popular, improves fusion rates, eliminates the need for postoperative braces, and allows early mobilization. However, the stress shielding caused by rigid internal fixation is thought to lead osteopenia and degeneration of adjacent segments. Theatre times, intraoperative complications, and costs are increased when pedicle screw fixation is added. The following report is a 46-patient prospective study, with lumbar degenerative disease treated with transforaminal lumbar interbody fusion with unilateral pedicle screw fixation (UNILIF). We analyzed clinical outcomes, fusion rates, and complications. Material and Methods: Prospectively collected clinical and radiological data on patients with degenerative lumbar disease managed by UNILIF. Preoperatively and at 5 years, we recorded ODI (Oswestry Disability Index) and VAS (visual analogue scale). Interbody fusion was analyzed on radiography and on a computed tomography (CT) scan. Results: Mean operation time was 93.5 ± 16.8 minutes, mean blood loss was 130.8 ± 210.9 mL. Average follow-up of 4.8 years (2.8-5.6). ODI and VAS were significantly improved (P < .005). The fusion rate was 96.8% on radiographic analysis and was 95.9% on CT scan analysis. A loosening of the screw was reported, without pain. He was treated with rest and physical therapy, with good evolution. No infections were reported Conclusion: Although it is a small group, but with a long follow-up, the UNILIF technique has been shown to be effective and safe for patients with lumbar degenerative disease.
P213: Spino-Pelvic and Adjacent Segment Alignment After Cantilever Transforaminal Lumbar Interbody Fusion: Radiological Study
Aleksandr Aleinik1, Sergey Mlyavikh1, and Andrey Bokov1
1Privolzhskiy Research Medical University, Nizhniy Novgorod, Russian Federation
Introduction: Spinal fusion remains the most common spinal surgery. The restoration of normal sagittal alignment of the operated and adjacent spinal segments is a key to the successful fusion surgery. Transforaminal lumbar interbody fusion (TLIF) is a widely used spinal fusion technique, but, according to the literature, its ability to correct the sagittal alignment is inferior to other interbody fusion techniques. A special technique—“cantilever” TLIF (cTLIF) was proposed to improve sagittal correction. The aim of this study was to evaluate the impact of mono-segemental or bisegmental cTLIF on spinal and spino-pelvic balance and adjacent spinal segments. Material and Methods: The study included 30 patients (20 females, 10 males; mean age = 57 ± 12.77 years) who underwent 1- or 2-level lumbar fusion using the cTLIF technique. All patients underwent full spine radiography with hip joints before the surgery, after verticalization and 1 year after surgery. The measurements of sagittal parameters at the fused level, adjacent segments, and spinopelvic relations were made. Statistical analysis was performed using Friedman ANOVA (analysis of variance) and Wilcoxon watched pairs test. Results: Segmental lordosis (SL) changed from 4.85 ± 8.021° to 12.58 ± 6.031° after surgery, P < .0001 (the average value of segmental correction was 8.35 ± 6.64° per level). After 1 year, SL decreased to 10.42 ± 5.13°, P = .00092. Lumbar lordosis (LL) increased from 44.97 ± 17.58° to 51.8 ± 11.61°, P = .01, and after 1 year, it slightly increased to 55.6 ± 8.74°, P = .82. Adjacent segment lordosis decreased from 8.77 ± 4.57° to 6.83 ± 3.96° after surgery, P = .015 and was 7.33 ± 3.62°, P = .86 after 1 year. The relation of pelvic incidence (PI) to lumbar lordosis (PI-LL) decreased from 13.1 ± 11.022° to 7.93 ± 5.97°, P = .018 and after 1 year it remained within normal limits (8.15 ± 5.16°, P = .16). There were no significant changes in the pelvic tilt before the surgery 20.9 ± 7.18°, after operation 19.1 ± 8.58°, P = .13 and after 1 year 16.47 ± 8,7°, P = .53. Conclusion: CTLIF allows to achieve correction of segmental lordosis on average 8° per segment. Lumbar lordosis significantly increased and adjacent segment lordosis decreased after surgery. An improvement in the relationship between lumbar lordosis and pelvic incidence was achieved. At 1-year follow up, we reveal significant loss of correction of segmental lordosis, but improvement of spinopelvic relations, lumbar lordosis, and adjacent segment were preserved.
P214: Low Back Pain After Lumbar Discectomy for Disc Herniation: What Can You Tell Your Patient?
Christian Iorio-Morin1, Charles Fisher2, Greg McIntosh3, and Nicolas Dea2
1Université de Sherbrooke, Sherbrooke, Quebec, Canada
2Combined Neurosurgical and Orthopedic Spine Program, Vancouver General Hospital, Vancouver, British Columbia, Canada
3University of British Columbia, Vancouver, British Columbia, Canada
4Canadian Spine Outcomes and Research Network, Toronto, Ontario, Canada
Introduction: Lumbar discectomy is frequently performed to alleviate radicular pain resulting from disc herniation. While this goal is achieved in most patients, improvement in low back pain (LBP) has been reported inconsistently. The goal of this study was to characterize how LBP evolves following discectomy. Material and Methods: We performed a retrospective analysis of the Canadian Spine Outcomes Research Network (CSORN) registry. Patients who underwent surgery for lumbar disc herniation were eligible for inclusion. The primary outcome was a clinically significant reduction in the back pain numerical rating scale (BPNRS) assessed at 12 months. A binary logistic regression was used to model the relationship between the primary outcome and potential predictors. Results: There were 751 patients included in the analysis. The chief complaint was radiculopathy in 79%; 47% underwent a minimally invasive procedure; and 26% underwent fusion. BPNRS improved at 3 months by 43% and this improvement was sustained at all follow-ups. LBP and leg pain improvement were correlated. Clinically significant improvement in BPNRS at 12 months was reported by 57% of patients. Six factors predicted a lack of LBP improvement: the number of operated levels, low education, marriage, not working, low expectations with regard to LBP improvement, and a low BPNRS preoperatively. Conclusion: Clinically significant improvement in LBP is observed in 57% of patients after lumbar discectomy. These data should be used to better counsel patients.
P215: Analysis of Efficiency of Local Application of Bupivocaine With Epinefrine to During Multilevel Decompressive-Stabilizing Interventions on the Lumbosacral Spine
Vadim Byvaltsev1, Andrei Kalinin1, Evgenii Belykh1, Victorya Goloborodko1, Vladislav Borisov1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: Multilevel decompressive-stabilizing interventions on the lumbosacral spine are quite aggressive and require long-term analgesia in the early postoperative period, including narcotic analgesics. To reduce the severity of the pain syndrome in the field of surgical intervention in patients, use of prolonged local anesthesia with bupivacaine and epinephrine before suturing the wound was introduced into the medical process. Materials and Methods. The study included 178 patients who underwent decompressive-stabilizing neurosurgical interventions on 3 vertebral segments for degenerative diseases of the lumbosacral spine, and 2 study groups were identified. The main group (MG, n = 82) included patients who before the suturing of the wound performed a local infiltration anesthesia of paraspinal muscles, subcutaneous fat and skin with a 0.5% bupivacaine solution with epinephrine 1: 200000 with a volume of 30 mL. The clinical comparison group (CCG, n = 96) included patients operated without of a local anesthetic. For the analysis, gender characteristics, constitutional features, technical parameters of the intervention, activation time, and duration of inpatient treatment after surgery, complications were investigated. We also studied: the level of pain syndrome based by VAS (visual analogue scale), which was monitored for the first 10 days after the operation every 24 hours; the need for analgesics for the daily number of injections of nonsteroidal anti-inflammatory drugs; the level of glucose before surgery and during the first 3 days after the operation; and the degree of patient satisfaction with the operation performed on the MacNab scale at discharge. Results. Comparative analysis of intergroup differences by sex, age, and constitutional peculiarities and technical peculiarities of interventions was not revealed (P > .05). At the same time, statistically significant early activation of patients (P = .02) was recorded with a reduction in the duration of inpatient treatment (P = .03) in the MG. When analyzing the severity of the pain syndrome in the field of operative intervention, a statistically significantly lower level was observed in the MG both in the first 72 hours (P = .001) and at the time of discharge (P = .03). In this connection, the patients of the MG had a statistically significant lower total need for the introduction of analgesics for the entire period of hospitalization (P = .003) compared with the CCG. On the subjective satisfaction scale performed by the Macnab operation at discharge, the proportion of good and excellent results was 89% in the MG (n = 73) and 60% (n = 56) in the CCG. The efficacy of the localized use regimen of bupivacaine with epinephrine was confirmed by a statistically significantly lower blood glucose level in the MG as a marker of “surgical stress”. In the MG 1, complication (1.2%) was verified and no side effects of the use of drugs for infiltration anesthesia were registered, 10 complications (10.4%) were registered in the CCG (P < .001). Conclusion. The study showed a high clinical effectiveness of local application of bupivacaine with epinephrine in the reduction of local postoperative pain and early rehabilitation of patients when performing multilevel decompressive-stabilizing interventions on the lumbosacral spine and the absence of side effects associated with the use of drugs.
P216: The Influence of Spondylometric Parameters With the Clinical Outcome of Surgical Treatment of Patients With Degenerative Diseases of the Lumbosacral Junction
Vadim Byvaltsev1, Andrei Kalinin1, Yurii Pestryakov1, and Alena Okoneshnikova1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: The most important in spinal surgery are interventions in the transitional zones of the spine, in particular, the lumbosacral junction. In connection with biomechanical, anatomical, and physiological characteristics, this segment receives the greatest axial load, and in the overwhelming majority of cases, it is subject to degeneration. Complications of surgical interventions in patients with degenerative diseases of the lumbosacral junction are verified up to 57% of cases. The purpose of our study was to evaluate the relationship between the X-ray and neuroimaging parameters of the vertebral segment with the clinical outcome of surgical treatment of patients with degenerative diseases of the lumbosacral junction in order to clarify the indications for dynamic and rigid stabilization. Materials and Methods: The study included 267 patients with degenerative diseases of the lumbosacral junction. Depending on the method of stabilization 2 groups of patients were identified: (1) n = 83—using a dynamic artificial disc prosthesis, (2) n = 184—using interbody fusion and transpedicular fixation. The analysis of remote clinical parameters and biomechanical characteristics before and after the operation was made. Results: In the analysis of clinico-spondylometric parameters a significant nonparametric correlation of the value of the long-term result of surgical treatment with VAS (visual analogue scale) and ODI (Oswestry Disability Index) with X-ray parameters (the height of the interbody spacing, the amplitude of the segmental angle, the angle of the lumbar lordosis, and the degree of linear displacement of the vertebrae) and the results of neuroimaging (the degree of degeneration of IVD [intervertebral disc] by Pfirmann, the degree of degeneration of the FJ [facet joints] by Fujiwara, the degree of degeneration from the apparent diffusion coefficient [ADC]). It has been established that the use of dynamic artificial disc prosthesis, depending on the initial radiographic data, allows to achieve a minimum level of pain syndrome and good functional recovery with an effective preservation of the volume of physiological movements in the operated segment and restoration of the common angle of lumbar lordosis. Conclusion: (1) With objective neuroimaging data (II-IV degree of IVD degeneration) and radiographic parameters (linear displacement of the vertebrae—no more than 4 mm, sagittal volume of movements in the vertebral segment—less than 6°, decrease in the height of the interbody gap no more than 2/3 of the overlying) it is possible to use total arthroplasty. (2) In the detection of neuroimaging parameters (IV-V degree of IVD degeneration) and radiographic data (linear displacement of the vertebrae—more than 4 mm, sagittal volume of movements in vertebral segment— no less than 6°, decrease in the height of the interbody gap more than 2/3 of the overlying) is the implementation of interbody spinal fusion and rigid stabilization.
P217: Interrelation of the Parameters of Tropism and Angulation of Facet Joints With a Clinical Outcome After Rigid and Dynamic Surgical Interventions in Patients With Degenerative Diseases of the Lumbar Spine
Vadim Byvaltsev1, Talgat Kerimbaev1, Andrei Kalinin1, Alena Okoneshnikova1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: At present, a significant number of unsatisfactory clinical postoperative results are associated with the progression of the degenerative process in the operated and adjacent segments due to biomechanical changes. The search for diagnostic and treatment methodic to optimize the outcomes of surgical treatment of patients with degenerative diseases of the lower lumbar spine based on the analysis of the clinical and morphological parameters of the vertebral segments was the purpose of this study. Materials and Methods: The results of surgical treatment of 141 patients with degenerative diseases of the lumbar spine are analyzed. Taking into account, the performed surgical intervention, patients are divided into 3 groups: (1) (n = 48) using artificial disc prosthesis; (2) (n = 42) with the use of interbody fusion, combined transpedicular and transfacet stabilization; (3) (n = 51) using interbody fusion and bilateral transpedicular stabilization. Correlative analysis of remote clinical outcomes (the level of pain syndrome by VAS [visual analogue scale], functional state according by ODI [Oswestry Disability Index], MacNab scale) and preoperative neuroimaging parameters of facet joints (FJ; degree of degenerative changes according to Fujiwara A, magnitude of facet angles, the presence of tropism). Results: A direct significant nonparametric correlation of neuroimaging parameters of facet angles and tropism of FJ with long-term clinical outcomes of surgical treatment according to VAS and ODI was revealed. It was established that good clinical outcomes were achieved with preoperative parameters of FJ in group I— the facet angle <60°, while the presence of tropism had no correlation dependence; in group II—facet angle >60°, in the absence of tropism FJ; in group III—the facet angle >60°, in the presence of tropism FJ. Conclusion: (1) With objective neuroimaging parameters of the facet angle of less than 60°, irrespective of the presence of tropism, it is possible to perform total disc arthroplasty. (2) When identifying parameters neuroimaging facet angle 60° shows the execution of the rigid stabilization of the operated segment, thus in the absence of possible contralateral tropism FJ transfacet fixation, and in the presence tropism advisable to perform bilateral transpedicular stabilization.
P218: Optimization of Surgical Care and Anesthesia in the Treatment of Multilevel Degenerative Diseases of the Lumbar Spine in Patients With Overweight and Obesity
Vadim Byvaltsev1, Andrei Kalinin1, Victorya Goloborodko1, and Evgenii Belykh1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: The provision of surgical care in the treatment of degenerative diseases of the lumbar spine in patients with obesity and obesity is associated with significant risks of anesthesia and the development of perioperative complications. The purpose of our study to conduct a comparative analysis of the clinical efficacy of surgical care and anesthesia in the treatment of multilevel degenerative diseases of the lumbar spine in patients with excessive body weight and obesity. Materials and Methods: The results of surgical treatment of 86 patients were studied, 2 groups were identified. In the study group (SG, n = 37), minimally invasive surgical techniques, paravertebral musculature infiltration with bupivacaine with epinephrine, and multimodal anesthesia with dexmedetomidine were used. The comparison group (CG, n = 49) consisted of patients who used the technique of traditional open transpedicular fixation in combination with the posterior interbody fusion without the above combination of surgical procedures and anesthesia. Observation and clinical evaluations were performed in the early (during hospitalization) and in the distant (on average 36 months) postoperative periods. Results: In SG, there were no changes in hemodynamics and better results were obtained on the speed of recovery of psychomotor functions. The use of local anesthetics significantly reduced the local pain syndrome (P < .05) and the need for analgesics (P = .002). Comparative analysis in the main group revealed significantly better results in indices of the duration of the operation (SG 145 [105; 155] minutes, CG 185 [100; 205] minutes; P = .02), the volume of blood loss (SG 110 [90; 140] mL, CG 510 [390; 640] mL; P < .001), the activation time (SG 1 [1; 2] days, CG 3 [3; 4] days; P = .01), the length of hospitalization (SG 10 [9; 11] days, CG 13 [12; 15] days; P = .03), remote clinical parameters of the pain syndrome level from the visual analogue scale in the lower extremities (SG 3 [1; 4] mm, CG 9 [6; 14] mm; P = .006) and the lumbar spine (SG 6 [4; 9] mm, CG 16 [11; 21] mm; P = .001), functional state according to ODI (SG 8 [6; 10] points, CG 16 [12; 24] points; P = .008), subjective satisfaction with the operation performed on the Macnab scale (P = .01). The number of postoperative complications in SG was 8%, in CG was 18% (P = .006). Conclusion: Analysis of the results of the introduction of a combination of surgical and anesthetic support methods in the treatment of multilevel degenerative diseases of the lumbar spine in patients with overweight and obesity, including minimally invasive surgical techniques, infiltration of paravertebral muscles with bupivacaine and epinephrine, multimodal anesthesia with dexmedetomidine showed its high perioperative safety, low number of complications, as well as better clinical outcomes in the early and late postoperative periods.
P219: Oblique Lumbar Interbody Fusion Using a Stand-Alone Construct for the Treatment of Adjacent-Segment Lumbar Degenerative Disease: Report of 6 Cases and Brief Literature Review
Kai Wang1, Can Zhang1, Fengzeng Jian1, and Hao Wu1
1Xuanwu Hospital of Capital Medical University, Beijing, China
Introduction: Adjacent segment disease (ASD) is common in patients undergone previous lumbar fusion. A typical revision treatment from posterior approach requires management of postoperative scar tissue and previously implanted instrumentation. An oblique lateral interbody fusion (OLIF) approach allows the surgeon to potentially reduce the risk of these hazards. The goal of this study was to determine if stand-alone OLIF is safe and effective in treating adjacent-segment disease. Material and Methods: From December 2016 to December 2017, we collected cases underwent stand-alone OLIF for treating ASD. Visual analogue scale (VAS) of back pain and leg pain and the Oswestry Disability Index (ODI) before surgery and at last postoperative clinic visits were obtained. CT (computed tomography) and MRI (magnetic resonance imaging) before and at last follow-up after surgery was evaluated in all patients. Results: During the study period, 6 cases were successfully treated using stand-alone OLIF. The mean follow-up was 11.5 ± 4.0 months. The back pain VAS improved from 6.5 ± 0.6 to 1.3 ± 1.3 (P < .01), and the leg pain VAS improved from 8.3 ± 2.1 to 0.8 ± 1.0 (P < .01). ODI improved from 32.7 ± 5.2 to 11.2 ± 5.5 (P < .01). Radiographic outcomes also improved significantly. All patients had bridging bone on CT scanning at the last follow-up, indicating solid bony fusion. No major or minor complications were observed. Conclusion: Stand-alone OLIF provides a safe and effective alternative way to treat ASD with reduced blood loss, operation time, and complications.
P220: Reducing the Severity of Pain in the Postoperative Period After Surgery for the Degenerative Process Using High-Frequency Denervation
Konstantin Tiulikov1, Vadim Manukovsky1, and Tahir Tamaev1
1Dzhanelidze Research Institute of Emergency Care, Saint Petersburg, Russian Federation
Introduction: Patient satisfaction with elective spine surgery for degenerative diseases is influenced by whether they achieve clinically significant improvement in pain and disability, are Medicaid recipients or are uninsured, and have worse pain and disability at baseline. The defeat of the intervertebral joints degenerative process at adjacent levels is accompanied by stenosis of the spinal canal, degenerative spondylolisthes, and contribute a significant role in the development of low back pain after surgical treatment. The efficacy of radiofrequency facet nerve ablation or denervation as advanced minimally invasive method of pain syndrome surgery for spondiloarthrosis occurring in degenerative-distrophic spine diseases after operations has been studied. Methods and Materials: The purpose of the study was to assess the effectiveness of radiofrequency facet nerve ablation of adjacent intervertebral joints as advanced minimally invasive surgical technique for alleviating pain after operations about degenerative spine disease. We performed a prospective analysis of 87 patients with low back pain after operations about degenerative spine disease, which were treated at the Dzhanelidze Research Institute of Emergency Care. Among them were 47 men and 40 women. Indications for performing denervation were signs of facet joint arthrosis on MRI (magnetic resonance imaging) and clinical manifestations below or higher the level of surgery. Minimally invasive electrosurgical methods are considered to be safe and effective treatment in carefully selected patients suffering from low back pain after operations about degenerative spine disease, caused by degenerative-distrophic process. No complications were noted. On the next day and at 3-month follow-up, all patients undergoing the procedure demonstrated marked pain syndrome decrease by visual analogue scale, while patients’ satisfaction with the results was higher compared with those therapeutically treated. To assess the statokinetic function of spine, patients were asked to note the time of painless stay in a different condition. To determine the indications for the use of this method performed pharmacological blockade of the facet joints. Thirty patients of control group were treated therapeutically after operation. Results: No complications were noted. In the group of patients, after the radiofrequency facet joints denervation, the regress of acute pain syndrome was noted mostly on the operating table or the day after the manipulation. The positive effect of the procedure increased with time and had a persistent character. Conclusion: The high-frequency denervation of the facet joints is a modern low-traumatic effective method of pain management at spondylarthrosis and can be used in complex treatment of patients after surgery for degenerative disease of spine with stabilization systems. Treatment of postoperative pain requires good multidisciplinary and multiprofessional cooperation. Every care-providing unit where surgery is performed should provide a pain management team structured according to local needs.
P221: Do Clinical Outcomes and Sagittal Parameters Differ Between Transforaminal Lumbar Interbody Fusion and Posterolateral Lumbar Fusion for Degenerative Spondylolisthesis?
Bryce Basques1, Jannat Khan1, Kyle Kunze1, Ian Chen1, Jessica Gosse1, Lindsay Friedman1, Clayton Maschhoff1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: In the debate regarding effective surgical approaches for low-grade degenerative spondylolisthesis, critics of interbody fusion cite issues with possible increased surgical time, implant costs, and nerve retraction that are not counterbalanced by associated increase in clinical outcomes. However, there is minimal conclusive information on potential risks and benefits in literature, and sparse information on comparative effects of these differing techniques on lumbar sagittal parameters postoperatively. This study aims to evaluate clinical outcomes and sagittal parameters in patients who underwent transforaminal lumbar interbody fusion (TLIF) versus posterolateral lumbar fusion (PLF). Materials and Methods: A retrospective cohort study was conducted of consecutive patients undergoing primary elective open posterior lumbar spinal fusion for grade I degenerative spondylolisthesis at one academic institution from 2014 to 2018. Patients excluded from analysis: <18 years at surgery time, ≥ grade II spondylolisthesis, had lumbar fusion to treat isthmic spondylolisthesis, lumbar fracture, tumor, or infection. Patients were separated into 2 groups based on whether they had open TLIF or open PLF. Patient and operative characteristics were compared using chi-square analysis and independent sample t tests for categorical/continuous data. Preoperative/final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt, pelvic incidence (PI), with PI-LL calculated. Additionally, rates of dural tear, postoperative complications, postdischarge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis, along with operative time and postoperative length of stay were recorded. Binary outcome variables were compared between TLIF/PLF with multivariate logistic regression, and continuous outcome variables using multivariate linear regression, using PLF as reference. Multivariate analyses controlled for baseline patient and operative characteristics, with threshold for statistical significance P < .05. Results: A total of 275 patients were included; 240 (87.27%) PLF and 35 (12.72%) TLIF. On bivariate analysis, patients who underwent PLF were older (P < .001), had greater rates of diabetes (P = .040), likelihood of preoperative opiate use (P = .022), and rates of 3 or more levels of fusion (P < .001), but lower ASA (American Society of Anesthesiologists) scores (P = .009). On multivariate linear regression, patients who underwent TLIF had greater change of LL from preoperative to postoperative (P = .003) and longer operative times (P = .001) compared with PLF patients. There were no differences in patient-reported outcomes between groups using VAS back, VAS leg, and ODI; however, patients with TLIF achieved MCID for VAS back (P = .011) and VAS leg (P = .032) at lower rates. There were no differences in complication or reoperation rates. Conclusions: For low-grade degenerative lumbar spondylolisthesis, open transforaminal lumbar interbody fusion patients achieved MCID in VAS at higher rates than open posterolateral lumbar fusion. Placement of interbody device during TLIF was associated with greater change of LL from preoperative to postoperative with longer operative times. These findings suggest that TLIF may be more effective than PLF for providing clinically significant relief of symptoms for low-grade degenerative spondylolisthesis; however, both surgical approaches were effective in maintaining sagittal alignment. Future study is necessary to evaluate if differences in clinical outcomes remain over longer-term follow-up.
P222: Does the Number of Patient-Reported Allergies Affect Clinical Outcomes After Lumbar Spinal Fusion?
Jannat Khan1, Bryce Basques1, Dong Gue Oh1, Zayd Hayani1, Jennifer Hwang1, Konstantin Tchalukov1, Peter Derman1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Accurate documentation of allergies is essential for patient care. However, there have been reported correlations between the number of patient-reported allergies and diagnosis of psychological disorders, such as depression and anxiety, as well as worse health-related quality of life. Additionally, patients with multiple allergies may have limited options for perioperative pain and medical management. The association between the number of allergies, possible psychiatric conditions, and clinical outcomes has not been well characterized in lumbar spinal fusion patients, and a better understanding of these patients is essential in order to optimize outcomes. The purpose of this present study was therefore to explore the potential association between multiple reported allergies and clinical and radiographic outcomes following elective posterior lumbar spinal fusion. Materials and Methods: A retrospective cohort study was conducted of consecutive patients who underwent primary elective posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were under 18 years of age at the time of surgery or underwent surgery for the treatment of lumbar fracture, tumor, or infection. Patient and operative characteristics were collected, and the number of medication allergies was dichotomized at 3 allergies, as this was the 95th percentile for the number of allergies. Chi-square analysis and independent sample t tests were used to compare categorical and continuous data, respectively. Preoperative and final postoperative visual analogue scale (VAS) back pain, VAS leg pain, and Oswestry Disability Index (ODI) were collected. Additionally, the rates of dural tear, postoperative complications, postdischarge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 504 patients met inclusion criteria. There were 472 (93.65%) patients who reported less than 3 allergies, while 32 (6.35%) patients presented with 3 or more allergies. Patients with 3 or more reported allergies were more often older (P = .026), of the female sex (P < .001), and had American Society of Anesthesiologists Physical Status Score (ASA) equal to or greater than 3 (P = .038). On multivariate analysis, patients with more allergies had significantly higher VAS leg scores preoperatively and lower improvement in ODI scores from preoperative to final visit (P = .001). No significant differences were found for postoperative complication (P = .347) or reoperation rates (P = .825). Conclusions: Patients with 3 or more reported allergies have significantly less improvement of ODI scores from preoperative to final assessment. Interestingly, the patients with more reported allergies did not have different rates of psychiatric conditions compared with patients with under 3 reported allergies. These results suggest that there is a lower perceived improvement of disability in patients with more than 3 reported allergies when compared with patients with lower number of allergies. This study underscores the importance of considering the number of allergies as a possible prognostic factor.
P223: Does Obesity Impact Clinical Outcomes and Lumbar Sagittal Alignment After a Posterior Lumbar Spine Fusion?
Jannat Khan1, Bryce Basques1, Zayd Hayani1, Coralie Pardo1, Landan Banks1, Young Soo Hong1, Konstantin Tchalukov1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Obesity is an increasingly common comorbidity in patients undergoing lumbar spinal fusion, and is a well-known risk for increased technical difficulty of surgery, perioperative medical complications, and adverse short-term outcomes. However, information about the effect of obesity on radiographic and clinical outcomes following posterior lumbar fusion is less well understood. The purpose of the present study was therefore to compare obese and nonobese patients and those without diabetes based on clinical patient-reported outcomes, radiographic sagittal parameters, fusion rates, and reoperation rates. Materials and Methods: A retrospective cohort study was conducted of consecutive patients who underwent primary elective open posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were younger than 18 years at the time of surgery or had a fusion to treat a lumbar fracture, tumor, or infection. Patients were classified as obese per Center for Disease Control and Prevention (CDC) guidelines if their body mass index (BMI) was above 30 kg/m2. Other patient and operative characteristics were collected and compared between obese and nonobese groups using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative and final postoperative visual analogue scale (VAS) back/leg pain, and Oswestry Disability Index (ODI), were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and the PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 974 patients were included; 506 (51.95%) patients with BMI < 30 (nonobese) and 468 (48.05%) patients with BMI ≥30 kg/m2 (obese). On bivariate analysis of baseline characteristics, patients with BMI ≥30 kg/m2 were more likely to have diabetes mellitus (P < .001), ASA ≥3 (P < .001), grade 1 spondylolisthesis (P = .012), isthmic spondylolisthesis (P = .045), and neuromonitoring used (P < .001). On multivariate linear regression, assessment of all subjects showed that patients with BMI ≥30 kg/m2 had significantly longer operative times (P < .001) and postoperative length of stay (P < 0) compared with patients with BMI <30; there was no significant difference between other values for radiographic measurements or postoperative length of stay. There was no difference in patient-reported outcomes between groups using VAS back, VAS leg, and ODI. On multivariate logistic regression, there was no difference in postoperative complications and reoperations between groups. Conclusions: Obese patients had significantly more comorbidities, longer operative time, extended postoperative length of stay compared with nonobese patients. However, sagittal parameters, patient-reported outcomes, inpatient complications, and reoperations were similar between the 2 groups. Given these findings, open posterior lumbar fusion can be considered safe and effective in obese patients after thorough consideration of related comorbidities.
P224: Patients Presenting With Isthmic and Degenerative Spondylolisthesis Present with Similar Radiographic and Clinical Outcomes Following Open Lumbar Fusion
Bryce Basques1, Jannat Khan1, Michael Iloanya1, Karishma Kadakia1, Christian Vetter1, Ian Chen1, Sapan Gandhi1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Isthmic and degenerative spondylolisthesis are commonly and effectively treated with posterior lumbar fusion, and while technical and approach-related considerations have received much attention for these 2 pathologies, less attention has been paid to differences in sagittal radiographic parameters for these conditions. Additionally, even less is known about the comparative effects of posterior lumbar fusion on these radiographic parameters. The aim of this study was to evaluate and compare the radiographic and clinical outcomes following an open lumbar fusion between patients with isthmic or degenerative spondylolisthesis. Methods: A retrospective cohort study was conducted, using consecutive patients who underwent elective open posterior-only lumbar fusion for low-grade degenerative or isthmic spondylolisthesis at one academic institution from 2014 to 2018. Patients excluded from analysis: <18 years of age at the time of surgery, had a nonposterior approach, or had fusion for a reason other than degenerative or isthmic spondylolisthesis. Patient and operative characteristics were collected and compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative and final postoperative visual analogue scale (VAS) Back pain, VAS leg pain, Oswestry Disability Index (ODI), were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, postdischarge destination, reoperation, achievement of minimal clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses were controlled for baseline patient and operative characteristics. Results: A total of 337 patients were identified with low-grade isthmic or degenerative lumbar spondylolisthesis (306 isthmic spondylolisthesis, 31 degenerative spondylolisthesis). Patients presenting with isthmic spondylolisthesis were significantly younger than those with degenerative spondylolisthesis (52.5 vs 65.6 years; P < .001) and had a lower ASA score (P = .021). A significantly higher percentage of patients diagnosed with isthmic spondylolisthesis presented with a Meyerding grade 2 spondylolisthesis (38.7 vs 10.1%; P < .001). Significantly more patients with isthmic spondylolisthesis received an interbody compared with degenerative spondylolisthesis patients (74.2 vs 12.8%; P < .001). There were no statistically significant differences between groups in terms of sex, BMI, pain duration, diabetes mellitus, history of psychiatric condition, and preoperative opiate use (P > .05). On multivariate analysis, both groups had similar changes in lumbar lordosis, pelvic tilt, and PI-LL difference from preoperative to final follow-up (P > .05). Patients with isthmic or degenerative spondylolisthesis had similar improvements in VAS back, VAS leg, and ODI from preoperative to final follow-up (P > .05). There was no significant difference between groups in terms of dural tear, postoperative complication, discharge to rehabilitation facility, reoperation, and pseudoarthrosis (P > .05). Conclusions: Patients presenting with isthmic or degenerative spondylolisthesis showed similar improvements in radiographic and patient-reported outcomes following an open posterior lumbar spine fusion. Additionally, the 2 groups of patients experienced similar operative times and postoperative hospital stays as well as rates of dural tears, postoperative complication, discharge to rehabilitation facility, reoperation, and pseudoarthrosis.
P225: Single Versus Multilevel Lumbar Arthrodesis: Demographic Patterns and Clinical Outcomes
Jannat Khan1, Bryce Basques1, Sapan Gandhi1, Christian Vetter1, Karishma Kadakia1, Jennifer Hwang1, Zayd Hayani1, Chaim Kalish1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Patients with multilevel lumbar pathology requiring arthrodesis may pose a therapeutic challenge to the treating surgeon. Surgeons must balance treating patient pathology with perceived morbidity of multilevel arthrodesis. The purpose of this study is to examine the debate of whether increased number of fused levels affects clinical outcome after posterolateral lumbar fusion. Materials and Methods: A retrospective cohort study was conducted of patients who underwent primary elective open posterior lumbar spinal fusion at one academic institution 2011 to 2018. Patients excluded from analysis: <18 years at surgery, underwent fusion to treat a lumbar fracture, tumor, or infection. Patients were divided into 3 groups based on the number of intervertebral levels fused intraoperatively: 1, 2, or 3 or more levels. Patient and operative characteristics were compared using chi-square analysis and analysis of variance for categorical and continuous data. Preoperative and final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), with PI-LL calculated. Rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected, along with operative time, and postoperative length of stay. Binary outcome variables were compared with multivariate logistic regression, and continuous outcome variables using multivariate linear regression, with 1-level fusions as reference. Multivariate analyses controlled for baseline patient and operative characteristics, with threshold for statistical significance at P < .05. Results: A total of 850 patients were reviewed/divided into groups as described above (single-level: 546, 2-level: 254, 3- or more levels: 50). Age was significantly greater for patients among those who underwent 3- or more levels fusion compared with single- and 2-level fusions (P < .01). Single- and 2-level fusions more often included interbody fusion (P < .01) and neuromonitoring use (P < .05) compared with those with 3 or more levels. Three- or more level fusions had significantly small preoperative, postoperative, and final follow-up lumbar lordosis (P < .02 for all cases). PT (pelvic tilt) was significantly greater in the final follow-up for 3-level fusions (P < .02). Two-level fusions had significantly higher preoperative (P < .05) and final follow-up (P < .01) ODI compared with single-level fusions. Change of ODI values between preoperative and final follow-up was significantly less in 3- or more level fusions than the single- and 2- level fusions. All groups had similar improvements in clinical outcomes. Intraoperative dural tear was significantly greater in 2-level fusions (P < .03), and discharge to facility was much more significant in 3-level fusions (P < .01 multilevel fusions had a higher operative time, and longer postoperative stay compared with single-level fusions (P < .01). Conclusions: In the appropriate setting, multilevel lumbar fusion may provide similar improvements in clinical outcomes compared with single-level fusion. Despite concerns of morbidity associated with fusion of several levels, multilevel fusion is not associated with significantly higher complications or reoperation. Increasing number of levels fused to 3 or more levels appears to be a safe and efficacious procedure under the right clinical and radiographic criteria.
P226: Discharge to a Facility Following Posterior Lumbar Fusion: Risk Factors and the Development of a Predictive Scoring System
Bryce Basques1, Philip Louie1, Jannat Khan1, Oscar Chen1, Joseph Michalski1, Kyle Kunze1, Matthew Colman1, Dino Samartzis1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Discharge to acute/intermediate care facility following elective open posterior lumbar fusion is common but disadvantageous. These facilities are more costly to the patient and health care system, and may increase risk of postoperative complications. As bundled-care payments become commonplace, discharge cost to facility may affect inpatient surgical fees’ reimbursement. Preoperative stratification of patients for possible facility discharge may optimize planning and risk factors. The aim of the study was to develop a risk stratification system by identifying risk factors for facility discharge following elective open posterior lumbar fusion. Materials and Methods: Consecutive patients underwent elective open posterior lumbar fusion at one academic institution from 2014 to 2018. Patients excluded from analysis: <18 years at surgery time, underwent fusion treating lumbar fracture/tumor/infection. Preoperative patient characteristics and the patient-reported outcomes (PROs) visual analogue scale (VAS) back pain, VAS leg pain, and Oswestry Disability Index (ODI) were collected/compared between patients discharged to facility (DTF) versus home. Rates of reoperation, pseudoarthrosis, and achievement of minimally clinically important differences (MCIDs) for PROs were collected. Data was compared by independent-sample t tests and multivariate linear regression and categorical data using chi-square tests and multivariate logistic regression. Stepwise multivariate logistic regression was used to determine risk factors for DTF, which sequentially excluded nonsignificant preoperative variables until only P < .05 remained. A nomogram was generated and used to develop a predictive scoring system. Results: Out of 510 patients, 56 (10.98%) were DTF. Average age was 58.9 + 13.43 years, average Body mass index was 31.1 + 6.03. 54.2% of patients were female. On bivariate analysis, patients DTF were older (P < .001), more likely female (P = .014), had greater diabetes rates (P < .001), decreased preoperative opioid use (P = .020), increased grade 1 spondylolisthesis (P = .002), and decreased interbody use (P < .001). Patients DTF had average postoperative length of stay 2 days longer than those discharged home (P < .001). On multivariate linear regression, patients DTF had increased preoperative VAS back (P = .020) and VAS leg (P = .025), final VAS back (P < .001), and final ODI (P < .001). No differences in reoperation, pseudoarthrosis, or achievement of MCID for VAS back, VAS leg, or ODI were found. Backwards stepwise multivariate logistic regression found the following risk factors for DTF: age (P < .001), increased preoperative VAS leg (P = .018), increased number of fusion levels (P = .034), and diabetes (P = .001). A nomogram was created, and points for each factor were as follows: age: +1 per decade, VAS: +1 per 3 VAS points, +0.5 per level fused, and +2 for diabetes. Probability of DTF ranged from <0.1% with 5 total points to >96% with 16 or more total points. Goodness-of fit was confirmed with the Hosmer-Lemeshow test, and the area under the receiver operating characteristic curve indicated a strong predictive model (AUC [area under curve]: 0.855). Conclusions: Multivariate analysis found that age, preoperative VAS leg pain, number of fusion levels, and diabetes were significant independent risk factors for DTF following elective posterior lumbar fusion, and this model was used to develop a point-scoring system for predicting discharge destination. Preoperative stratification of patients may facilitate perioperative planning and decision-making, and future studies should seek to further validate this predictive scoring system.
P227: Do Clinical and Radiographic Outcomes Differ Between Diabetics and Nondiabetics Following Posterior Lumbar Spinal Fusion?
Bryce Basques1, Jannat Khan1, Oscar Chen1, Joseph Michalski1, Zayd Hayani1, Jennifer Hwang1, Chaim Kalish1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Diabetes mellitus (DM) is a common comorbidity in lumbar spinal fusion patients and is a well-characterized risk factor for increased perioperative medical complications and adverse short-term outcomes. However, information about effect of diabetes on radiographic and clinical outcomes following posterior lumbar fusion is less understood. The objective of this study was to compare diabetic patients and those without diabetes based on clinical patient-reported outcomes, radiographic sagittal parameters, fusion rates, and reoperation rates. Materials and Methods: A retrospective cohort study was conducted of consecutive patients who underwent primary elective open posterior lumbar spinal fusion at one academic institution between 2014 and 2018. Patients excluded from analysis: <18 years of age at surgery time, had fusion to treat a lumbar fracture, tumor, or infection. Patients being medically treated for diabetes mellitus were identified and separated from nondiabetic patients. Patient and operative characteristics were compared between diabetic and nondiabetic groups using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative and final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt, pelvic incidence (PI), and PI-LL calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimal clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Operative time, and postoperative length of stay were recorded. Binary outcome variables were compared between diabetic and nondiabetic groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics, threshold for statistical significance set at P < .05. Results: A total of 504 patients were included; 62 (12.30%) diabetic and 442 (87.70%) nondiabetic. On bivariate analysis, diabetics were older (P = .001), had higher body mass index (P < .001) and higher ASA (American Society of Anesthesiologists) values (P < .001), while nondiabetics were more likely to have had a deformity (P = .027) and had an interbody used in their spinal fusion operation (P = .047). On multivariate linear regression, there was no significant difference between radiographic measurements, operative time, or postoperative length of stay. There was no difference in VAS back, VAS leg, and ODI between the 2 groups. On multivariate logistic regression, diabetic patients were found to have a higher rates of postoperative complication (P = .013) and were also more likely to be discharged to a facility following surgery (P = .015). No differences in reoperation, pseudoarthrosis, or achievement of MCID for VAS back, VAS leg, ODI were found. Conclusions: Diabetic patients have a higher likelihood of associated comorbidities and rates of postoperative complications compared with nondiabetics. Notably, diabetic patients had increased rates of discharge to facilities versus discharge home, which is relevant in emerging bundled payment models. However, patients with DM have similar patient-reported and radiographic outcomes along with no difference in reoperations than non-DM patients. This study indicates that diabetic patients should be expectantly managed when indicated for lumbar spinal fusion, however, clinical/radiographic outcomes are similarly as successful as nondiabetic patients.
P228: Following Open Lumbar Spinal Fusion, Patients With High-Grade Central Stenosis Experience Less Clinical Improvement Compared With Patients With Low-Grade Central Stenosis
Jannat Khan1, Bryce Basques1, Chaim Kalish1, Konstantin Tchalukov1, Konstantin Tchalukov1, Lindsay Friedman1, Jennifer Hwang1, Zayd Hayani1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Open lumbar fusion is an effective intervention for leg and back pain from lumbar spinal stenosis, after conservative treatments fail. However, difference of outcomes between patients with moderate to severe central stenosis versus minimal-mild central stenosis is poorly characterized in literature. This study’s aim is to compare radiographic and clinical outcomes of patients who presented with moderate-to-severe central stenosis to minimal-to-mild central stenosis following open lumbar fusion surgery. Material and Methods: A retrospective cohort study was conducted of patients who underwent primary elective open posterior lumbar spinal fusion at one academic institution from 2014 to 2018, excluding: age <18 years at surgery time, previous lumbar fusion, fusion to treat lumbar fracture, tumor, or infection. Central stenosis was graded on axial T2-weighted images: grade 0 (no lumbar stenosis without obliteration of anterior CSF space); grade 1 (mild stenosis with separation of all cauda equina); grade 2 (moderate stenosis with some cauda equina aggregated); and grade 3 (severe stenosis with none of cauda equina separated). Patients were placed into 2 groups based on the lumbar central stenosis severity: “low-grade”: patients with grade 0-1, or “high-grade”: patients with grade 2-3. Patient/operative characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data. Preoperative/final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed measuring lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), with PI-LL calculated. Rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference for VAS back/leg, and ODI, and pseudoarthrosis were collected, with operative time and postoperative stay length. Binary outcome variables were compared with multivariate logistic regression, and continuous outcome variables, using multivariate linear regression, with lower lumbar fusions as the reference. Multivariate analyses controlled for baseline patient and operative characteristics, threshold for statistical significance set at P < .05. Results: A total 504 patients met criteria; 218 in the low-grade and 286 in the high-grade group. Patients with high-grade stenosis were significantly older (P < .001), presenting with ASA (American Society of Anesthesiologists) score ≥3 (P = .017) when compared. They also more commonly had grade 1 spondylolisthesis (P < .001), while patients with low-grade stenosis had more isthmic spondylolisthesis (P < .001). On multivariate analysis, patients with high-grade stenosis achieved greater PT from preoperative to immediate postoperative (P = .026). However, they lost more PT on final follow-up in comparison (P = .037). Additionally, they had worse final ODI (P = .047) experienced lesser improvements in ODI scores from preoperative to final follow-up (P = .011). There was no significant difference in terms of dural tear, postoperative complication, discharge to rehabilitation facility, reoperation, and pseudoarthrosis rates (P > .05). Conclusions: Open lumbar spine fusion can be effective for patients with lumbar central stenosis, but high-grade stenosis had worse final ODI and preoperative to final improvement in ODI compared with low-grade stenosis. Radiographic parameters were similar between groups, along with dural tear rates, postoperative complication, discharge to rehabilitation facility, reoperation, and pseudoarthrosis. These clinical outcome findings can apply to preoperative discussion with patients regarding expectations of surgical intervention for lumbar stenosis.
P229: A Comparative Analysis of Radiological and Clinical Outcomes of Stand-Alone Versus Instrumented Extreme Lateral Lumbar Interbody Fusion
Christian Heng1, Reuben Soh1, and Chang Ming Guo1
1Singapore General Hospital, Singapore
Introduction: Extreme lateral lumbar interbody fusion (XLIF) has been gaining popularity in recent years as a means of treating lumbar spinal degenerative disease via a minimally invasive approach. The principle of XLIF is achieving spinal canal decompression through ligamentotaxis via restoration of disc height. This is achieved through the insertion of interbody cages through a lateral approach to the spine. This can either be a standalone procedure, or the interbody cage can be supplemented with posterior instrumentation to provide additional stability. Material and Methods: We looked at prospectively collected data from our institution’s database on all cases of XLIF performed between 2007 and 2015; patients with other additional surgeries performed were excluded. In total, 95 surgeries were performed, and they were stratified into 2 groups: 34 stand-alone XLIF and 61 XLIF with posterior instrumentation. Patients were followed-up for at least 2 years, and outcomes scores in addition to radiographical parameters were recorded. Results: The demographics of both groups were similar, of note, there was no statistical difference between age or BMI (body mass index). The operation time was significantly shorter in the stand-alone group versus instrumented group (operation time: 101.6 vs 241.9 minutes). The clinical outcome scores in both groups were improved (statistically significant) at 2-year follow-up. There was no statistically significant difference in the improvement of clinical outcomes between the 2 groups. Subgroup analysis showed that in the stand-alone group, higher BMI correlated negatively with improvement in functional scores (Pearson correlation coefficient −0.549; P = .22). There were 8 complications noted in the study group, 3 from the stand-alone group and 5 from the supplementary instrumentation group. Conclusion: Standalone XLIF is not inferior to XLIF with supplementary posterior instrumentation in terms of 2-year outcomes. The advantage of stand-alone XLIF is a shorter operation time. Patient selection is important as high BMI correlates with lesser improvement in outcome scores in the stand-alone group.
P230: Patients With Predominantly Back Pain at the Time of Posterior Lumbar Fusion Experience Similar Clinical Improvement to Patients With Predominantly Leg Pain
Bryce Basques1, Michael Nolte1, Jannat Khan1, Karishma Kadakia1, Jessica Gosse1, Jeremy Mormol1, Peter Derman1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Clinicians frequently assess the degree of back pain versus leg pain during initial presentation in the setting of lumbar spinal pathology to help guide operative management, with lower extremity symptoms being a typical indication for lumbar spine surgery. Patients with predominantly back pain have traditionally been thought to derive less predictable symptomatic relief from lumbar fusion. The goal of this study was to compare postoperative clinical outcomes as well as degree of improvement in clinical outcome measures between patients with predominantly back pain and patients with predominantly leg pain undergoing posterior lumbar fusion. Methods: Consecutive patients who underwent primary elective open posterior lumbar fusion at a single academic institution from January 2014 to January 2018, were identified. Patients were excluded from analysis if they were younger than 18 years at the time of surgery or underwent surgery for the treatment of lumbar fracture, tumor, or infection. Preoperative and final visual analogue scale (VAS) back pain, VAS leg pain, and Oswestry Disability Index (ODI) were obtained. Patients with preoperative VAS back pain greater than VAS leg pain were identified and separated from patients with VAS back pain equal to or greater than VAS leg pain. Patient and operative characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), and pelvic incidence (PI). The PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, and pseudoarthrosis, as well as operative time and postoperative length of stay were recorded. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 665 patients met inclusion criteria. Of these, 485 had VAS leg greater than back scores, and 180 had VAS back greater than leg scores. Patients with back greater than leg pain were younger (56.94 vs 60.44 years, P = .006), and more likely to have a grade 4 spondylolisthesis (1.11% vs 0.00%, P = .020) compared with patients with leg pain greater than back pain (Table 1). There were no additional differences with regard to demographics, baseline spinal pathology, or intraoperative factors. With regard to radiographic measures, there were no differences between the cohorts in preoperative, immediate postoperative, final, or the change in sagittal parameters (Table 2). Furthermore, there were no differences in operative time or postoperative length of stay. As expected, the preoperative mean VAS back (6.04 vs 7.59, P = .001) and VAS leg scores (7.48 vs 4.57, P < .001) were significantly different between the 2 cohorts (Table 3). Patients with preoperative leg pain worse than back pain experienced greater improvements in VAS leg scores postoperatively (−4.30 vs −1.68, P < .001), and greater improvements in ODI score postoperatively (−18.16 vs −12.42, P = .012) compared with those with back worse than leg pain. However, there were no differences in the postoperative VAS leg scores, back scores, or ODI between the 2 cohorts. Finally, there were no differences in the rate of complications, reoperations, or the likelihood of discharge to a facility between the 2 cohorts (Table 4). Discussion and Conclusion: In the present study, posterior lumbar fusion patients who presented with a predominance of back pain had similarly successful postoperative clinical outcomes as patients who presented with a predominance of leg pain. While lower extremity symptoms in the setting of lumbar spinal pathology are an important part of the clinical assessment for surgical management, these results challenge the traditional belief that patients with predominantly back pain are worse surgical candidates. In properly indicated patients, posterior spinal fusion for those with back pain is effective, and clinicians can use this information for perioperative discussions and surgical decision-making.
P231: Scoliosis is Not Associated With Adverse Clinical Outcomes for Patients Undergoing Limited Posterior Lumbar Spinal Fusion
Bryce Basques1, Jannat Khan1, Chaim Kalish1, Michael Iloanya1, Kyle Kunze1, Steve Heidt1, Dong Gue Oh1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Adult scoliosis is often treated with long posterior fusion constructs for deformity correction, however, recently more attention has been paid to limited fusion for individually symptomatic levels. There is limited data on the outcomes of limited lumbar fusion in patients with scoliosis compared with patients with spondylolisthesis, disc disease, or other lumbar pathology who undergo posterior lumbar fusion. The goal of this study was to compare posterior lumbar fusion patients with and without adult degenerative scoliosis in order to better characterize outcomes for this population. Methods: Retrospective cohort study was conducted of consecutive patients who underwent primary open posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were younger than 18 years at the time of surgery or had a fusion to treat a lumbar fracture, tumor, or infection. Patients with scoliosis were identified and separated, with scoliosis defined as a Cobb angle in the coronal plane of 10° or greater. Preoperative and final postoperative visual analogue scale (VAS) back/leg pain, and Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and the PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference for VAS and ODI, and pseudoarthrosis were collected. Operative time and postoperative length of stay were also recorded. Results: A total of 665 elective open posterior lumbar fusion patients met inclusion criteria, and 68 patients had concomitant scoliosis. Patients in the scoliosis cohort had a lower mean BMI (body mass index; P < .001), and a greater proportion of females (P = .002) compared with those without scoliosis. Patients with scoliosis were less likely to undergo a 1-level fusion (P < .001), more likely to undergo a fusion of 3 or more levels (P < .001), and less likely to have one or more interbody fusions (P = .019). Patients with scoliosis had a lesser degree of lumbar lordosis postoperatively compared with those without scoliosis (P = .025), but there were no other differences in sagittal parameters between the groups. In addition, patients with scoliosis experienced a longer average operative time (P = .049). Clinical outcomes were comparable between patients with and without concomitant scoliosis. No differences were found in the rate of complications or reoperation between the 2 cohorts. Conclusion: The presence of scoliosis in patients undergoing posterior lumbar fusion presents an added challenge for spinal surgeons. Scoliosis patients did have longer fusion constructs and longer operative times; however, our findings suggest that the presence of concomitant spinal scoliosis in patients undergoing posterior lumbar fusion is not associated with adverse clinical outcomes, higher complication rates, or higher reoperation rates when compared with those without scoliosis. Limited posterior lumbar fusion appears to be a safe and effective treatment option for scoliosis patients with isolated pathology that is amenable to surgical intervention. Surgeons may use this information to better counsel their patients and manage expectations when considering surgical intervention.
P232: Are Clinical Outcomes and Lumbar Sagittal Parameters Comparable Between Upper and Lower Lumbar Spine Fusions?
Bryce Basques1, Jannat Khan1, Peter Derman1, Karishma Kadakia1, Alistair Fleming1, Jennifer Hwang1, Ian Chen1, Landan Banks1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: The biomechanics of more caudal segments of the lumbar spine have been previously found to be distinct from those of the more cephalad segments. At upper lumbar levels, due to anatomic considerations, there is concern that the rate of complications may be higher. However, there is poor data on clinical and radiographic outcomes for 1- or 2-level fusions in the upper lumbar spine versus the lower lumbar spine. The aim of this study was therefore to compare clinical and radiographic outcomes between upper and lower lumbar spine fusions. Methods: A retrospective cohort study was conducted of consecutive patients who underwent primary elective open posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were younger than 18 years at the time of surgery, had a procedure that included fusion of an intervertebral level cranial to L1, or had a fusion to treat a lumbar fracture, tumor, or infection. Only 1- or 2-level fusions were included, and patients were separated into 2 groups based on the caudal level of fusion: patients with fusions ending at L2, L3, or L4 (“upper lumbar fusions”) and patients with fusions ending at L5 or S1 (“lower lumbar fusions”). Preoperative and final postoperative visual analogue scale (VAS) back/leg pain, and Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and the PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back/leg and ODI, and pseudoarthrosis were collected. Operative time, and postoperative length of stay were also recorded. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 444 patients were included; 402 (90.54%) patients with lower lumbar fusions and 42 (10.98%) patients with upper lumbar fusions. Upper lumbar fusions were older (P = .043), had greater rates of prior lumbar spine surgery (P < .001) and prior lumbar fusions (P < .001), had increased rates of one level fusions (P = .001), but were less likely to be smokers (P = .043), had decreased rates of 2-level fusions (P = .001), and had decreased rates of interbody use (P < .001). There was no significant difference between 2 groups for radiographic measurements, postoperative length of stay, or patient-reported outcomes. Upper lumbar fusions had greater rates of dural tear; otherwise, there was no difference in reoperation, pseudoarthrosis, or achievement of MCID were found. Discussion and Conclusion: Patient who underwent upper lumbar fusion had higher rates of dural tears when compared with patients undergoing lower lumbar fusions. However, other complications, clinical outcomes, radiographic sagittal parameters, and reoperations were comparable between the 2 groups. These findings indicate that despite being less commonly performed, outcomes after 1- or 2-level posterior upper lumbar fusions are similarly predictable to those in the lower lumbar spine. This information can be used for perioperative discussions, surgical planning, and clinical decision making when considering upper lumbar fusions.
P233: Equivalent Outcomes in Patients Undergoing Open Posterior Lumbar Fusion With and Without a History of Prior Lumbar Laminectomy
Jannat Khan1, Bryce Basques1, Christian Vetter1, Kyle Kunze1, Coralie Pardo1, Oscar Chen1, Jeremy Mormol1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Lumbar laminectomy remains a reliable procedure for recalcitrant spinal stenosis. However, concerns of post laminectomy syndrome and accelerated spondylolisthesis have historically suggested worse outcomes in those undergoing subsequent lumbar fusions. The aim of this study was to compare preoperative characteristics and outcomes following elective open posterior lumbar fusion in those with and without a history of a prior lumbar laminectomy at that level. Methods: Consecutive patients who underwent primary elective open posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were younger than 18 years at the time of surgery, had a procedure that included fusion of an intervertebral level cranial to L1, or had a fusion to treat a lumbar fracture, tumor, or infection. Patients with a history of prior laminectomy at a planned fusion level were identified and separated. Patient and operative characteristics were compared between unilateral and bilateral radiculopathy using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative and final postoperative visual analogue scale (VAS) back/leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and the PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, and achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Operative time and postoperative length of stay were also recorded. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression, with lower lumbar fusions used as the reference. Multivariate analyses controlled for baseline patient and operative characteristics. The threshold for statistical significance was set at P < .05. Results: Total of 444 patients were included in this study, 42 (9.46%) of whom had undergone a prior laminectomy at the fusion level. There were no differences in patient characteristics, and while patients with no prior laminectomy had a higher incidence of grade 1 spondylolisthesis (P = .001), patients with a prior laminectomy were more likely to also have a history of a prior lumbar fusion (P < .001). Postoperatively, patients with a prior laminectomy had a shorter length of stay (P = .026). There were no differences in preoperative or final VAS back/leg, or ODI scores, but patients with no prior laminectomy experienced a greater change between preoperative and final ODI scores (P = .036). There were no differences in radiographic measurements or complication rates between the 2 cohorts. Conclusion: While patients without a history of prior lumbar laminectomy had a higher incidence of grade 1 spondylolisthesis and larger improvement in ODI scores, overall clinical and radiographic outcomes were good in both cohorts. When performing appropriately indicated posterior lumbar fusion procedures, surgeons can expect good outcomes regardless of whether patients have a history of prior laminectomy at that level, although one should be aware of the more complex anatomy when approaching the spine in such a setting.
P234: Duration of Symptoms does not Affect Clinical Outcome After Lumbar Arthrodesis
Jannat Khan1, Sapan Gandhi1, Bryce Basques1, Alistair Fleming1, Clayton Maschhoff1, Cristina Mendoza1, Edward Goldberg1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Nonoperative measures are generally employed and exhausted prior to consideration of surgical intervention for degenerative lumbar spine pathology. As such, patients can often experience symptoms for various lengths of time prior to surgical referral. It is unclear at what point in time surgical intervention may become less efficacious at relieving preoperative symptoms. The purpose of this study is to examine the effect of symptom duration on clinical outcomes after posterolateral lumbar fusion for degenerative and isthmic spondylolisthesis. Methods: Consecutive patients who underwent primary elective open posterior lumbar spinal fusion at a single academic institution between January 2014 and January 2018. Patients were excluded from analysis if they were younger than 18 years at the time of surgery or had a fusion to treat a lumbar fracture, tumor, or infection. Patient and operative data were collected, and duration of symptoms measured in months and was dichotomized at the 50th percentile, which was 24 months. Patient and operative characteristics were compared between symptom duration groups using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Preoperative and final postoperative Visual Analog Scale (VAS) back/leg pain, and Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and the PI-LL difference was calculated. Additionally, the rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Binary outcome variables were compared between groups with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 650 patients were reviewed and separated into 2 groups based on symptom duration (group 1: <2 years of pain, group 2: ≥2 years of pain). A total of 316 patients were included in group 1, while 334 patients were included in group 2. There was a higher proportion of female patients among those who had pain for more than or equal to 2 years compared with patients who had pain for less than 2 years (P = .042). Group 2 had a significantly smaller proportion of patients who underwent single-level fusions, and a higher proportion of patients who required 3 or more level fusions (P = .054 and .015, respectively). Both groups had similar changes in sagittal parameters. Groups 1 and 2 had no significant differences in clinical outcome measures. Group 2 had a lower proportion of any postoperative complication, but similar rates of dural tear, discharge to rehabilitation facility, reoperation, and pseudoarthrosis compared with group 1. Conclusion: Despite differences in symptom duration, patients who have had pain for more than or equal to 2 years appear to show similar improvement after posterolateral lumbar arthrodesis than those who have had pain for less than 2 years. Extended effort of conservative treatments or delay of operative intervention do not appear to negatively affect the eventual outcome of surgery.
P235: Does Increasing Age Affect Clinical and Radiographic Outcomes Following Lumbar Spinal Fusion?
Jannat Khan1, Bryce Basques1, Christian Vetter1, Chaim Kalish1, Alistair Fleming1, Michael Iloanya1, Jessica Gosse1, Howard An1, and Matthew Colman1
1Rush University, Chicago, IL, USA
Introduction: Despite the growing senior population within the United States, there is a lack of consensus regarding the safety and efficacy of performing lumbar spinal fusion for this population. The purpose of our study is to evaluate the clinical and radiographic outcomes in different age cohorts following lumbar spinal fusion. Materials and Methods: A retrospective cohort study was conducted of patients who underwent primary elective open posterior lumbar spinal fusion at one academic institution between 2011 and 2018, excluding: <18 years old at surgery time or with fusion to treat a lumbar fracture, tumor, or infection. Patients were divided into3, roughly equal-numbered, age groups: 18 to 54 years (“young”), 55 to 69 years (“middle-aged”), and ≥70 years (“elderly”). Patient/operative characteristics were compared using χ2 and analysis of variance for categorical and continuous data. Preoperative/final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), and PI-LL calculated difference. Additionally, rates of dural tear, postoperative complications, post-discharge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Operative time, and postoperative stay length were recorded. Binary outcome variables were compared with multivariate logistic regression, and continuous outcome variables were compared using multivariate linear regression, using 1-level fusions as the reference, with reference age 18 to 54 years. Multivariate analyses controlled for baseline patient and operative characteristics, the threshold for statistical significance set at P < .05. Results: A total of 850 patients were included; 330 (38.80%) young, 317 (37.30%) middle-aged, and 203 seniors (23.90%). Senior patients had a greater postoperative PT (P = .043) than young patients but less change in PT from postoperative to final analysis (P = .028), whereas middle-aged patients had larger final PI-LL than young patients (P = .026). Seniors had higher postoperative length of stay compared with younger patients (P < .001). Younger patients had higher final ODI scores compared with middle-aged (P = .002) and senior (P = .009) patients. Seniors had higher rates of discharge to facility (P = .007), overall ASD (P = .004), and proximal ASD (P = .002), while middle-aged patients had higher number of dural tears (P = .022) compared with young patients. Conclusions: Senior patients have significant improvement in patient-reported clinical outcomes, despite having greater comorbidities, longer length of stay, and higher rates of discharge to facility. Thus, senior patients should be similarly considered for lumbar spinal fusion despite greater postoperative PT and higher ASD rates given comparable clinical outcomes, and postoperative complication rates in all age groups.
P236: Addressing Adjacent Segment Disease Following Previous Lumbar Fusion Surgery: Stand-Alone Lateral Lumbar Interbody Fusion Versus Open Laminectomy and Posterolateral Fusion
Philip Louie1, Brittany Haws2, Jannat Khan1, Jonathan Markowitz1, Kamran Movassaghi3, Gregory Lopez1, Howard An1, and Frank Phillips1
1Rush University, Chicago, IL, USA
2University of Rochester, Rochester, NY, USA
3University of California, San Francisco–Fresno, Fresno, CA, USA
Introduction: Adjacent segment disease (ASD) following previous lumbar spine fusion is an ongoing consequence that can lead to severe back pain, radiculopathy, or neurogenic claudication. Multiple surgical fusion techniques can be applied with varying morbidity. Stand-alone lateral lumbar interbody fusion (LLIF) may be an attractive option as it provides a minimally invasive solution to achieve interbody fusion and spinal canal decompression. We performed a retrospective review of the clinical and radiographic outcomes for patients who underwent stand-alone LLIF or open laminectomy and posterolateral instrumented fusion for symptomatic ASD. Methods: We retrospectively reviewed consecutive patients with a prior posterior instrumented fusion who underwent a subsequent stand-alone LLIF or open posterolateral fusion (PLF; 1-3 levels) for ASD between 2010 and 2015. One surgeon performed all LLIF and one surgeon performed all open PLF surgeries. Patient-reported and radiographic outcomes were compared between preoperative and final follow-up using paired t tests. Results: A total of 55 patients (31 LLIF, 24 PLF) met inclusion criteria with a mean follow-up of 22.5 ± 17.2 months and 32.8 ± 21.2 months for the LLIF and PLF patients, respectively. The LLIF group had a significantly higher CCI score (1.8 ± 1.1 vs 1.1 ± 1.3; P = .025) and more male patients (70.8% vs 35.1%; P = .006). Operative times (186.9 ± 72.2 vs 104.4 ± 41.1 minutes; P < .001) and estimated intraoperative blood loss (550.8 ± 715.8 vs 65.2 ± 65.9 mL; P < .001) was significantly higher in the PLF group (Table 1). Patients who underwent a PLF had a greater PI-LL mismatch and less lordosis preoperative, immediately postoperatively, and at final follow-up (P < .001), but the amount of correction was similar. The LLIF was able to achieve greater disc height improvement compared with the PLF patients (preoperative to immediate postoperative 6.7 ± 1.9 vs 0.2 ± 3.2; preoperative to final follow-up 5.0 ± 2.6 vs 1.3 ± 3.0 mm; P < .001; Table 2). Although patients who underwent PLF had significantly greater preoperative Oswestry Disability Index (ODI) scores and pre- and postoperative visual analogue scale leg (VAS-Leg) scores, the amount of improvement from both surgeries were similar. Three PLF patients suffered an intraoperative dural tear, while none experienced this complication in the LLIF group. Conclusion: Traditional open posterior surgical approaches for patients requiring decompression and fusion adjacent to prior instrumented posterior fusion may be associated with higher morbidity and complication rates related to exposure and extension of prior posterior instrumentation as well as challenging decompression in the face of epidural scar tissue. Stand-alone LLIF is a safe and effective approach with substantially less intraoperative morbidity, acceptable complication rates, and similar successful outcomes compared with patients undergoing open laminectomy and posterolateral fusion for symptomatic adjacent segment disease. Summary: Stand-alone lateral lumbar interbody fusion is an effective approach with less intraoperative morbidity compared with open laminectomy and posterolateral fusion for symptomatic adjacent segment disease.
P237: Patients Undergoing 3 Level or Greater Decompression-Only Surgery For Lumbar Spinal Stenosis Have Similar Outcomes to those Undergoing Single-Level Surgery at 2 Years
Michael Nolte1, Philip Louie1, Bryce Basques1, Jannat Khan1, Coralie Pardo1, Christian Vetter1, Steve Heidt1, Edward Goldberg1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: There has been debate on the stability, and thus clinical outcomes, of multilevel lumbar decompression-only surgeries compared with a single-level procedure. However, few studies have directly compared patient outcomes following multilevel versus single-level lumbar decompression. The goal of this study was to compare patient outcomes following a multilevel versus a single-level stability preserving decompression-only surgery for lumbar spinal stenosis. Methods: A retrospective cohort analysis of patients who underwent a primary lumbar laminectomy from 2009 to 2015 for lumbar spinal stenosis was conducted. Patients were excluded from analysis if they had any previous lumbar surgery, an unstable spondylolisthesis, were younger than 18 years at the time of surgery, or had postoperative follow-up less than 3 months. Patients were divided into 3 groups based on the number of decompression levels: single-level, 2-level, or 3 or more levels. Patient-reported outcomes were obtained in the form of Oswestry Disability Index (ODI), visual analogue scale (VAS) back/leg, 12-Item Short Form Mental and Physical Survey (SF-12), and the Veterans Rand 12-Item Health Mental and Physical Survey (VR-12). Baseline patient characteristics were compared using chi-square analysis and independent sample t tests for categorical and continuous data, respectively. Bivariate and multivariate regressions were subsequently used to compare clinical outcomes between procedure groups. Multivariate analyses controlled for differences in baseline patient characteristics. Results: Overall, 212 consecutive patients who fulfilled our inclusion criteria were assessed. Average follow-up was 24.14 months. There were 106 patients who underwent a single-level, 74 patients underwent a 2-level, and 32 patients underwent a 3 or more level laminectomy. The multilevel decompression patients were significantly older (P < .001) Patients undergoing a 3+ level decompression had significantly greater presentations of diabetes diagnosis (P = .001) and a higher number of patients with the American Society of Anesthesiologists Physical Status Score (ASA) greater than or equal to 3 (P < .001). On multivariate analysis, patients who underwent a 2-level decompression presented with significantly lower preoperative VAS-back (P = .043), VAS-leg (P = .007), and ODI (P = .021) scores compared to those who underwent a single-level decompression. Conversely, compared to patients that underwent a single-level decompression, those that underwent a 2-level procedure described significantly higher post-operative VAS-back (P = .014) and VAS-leg (P = .039). Otherwise, there were no significant difference among all pre-operative, post-operative, and the change patient reported outcome scores between patients that underwent a 3+ level decompression group and those that underwent a single-level decompression. Reoperation rates were low and similar between the groups. Conclusion: Patients undergoing decompression of 3 or more levels present with similar postoperative outcomes compared with those who undergo single-level decompression for lumbar spinal stenosis. Despite concerns for instability following multilevel decompression, reoperation rates are low and not significantly different when comparing the number of levels that underwent a stability-preserving lumbar decompression. Under specific clinical and radiographic criteria, multilevel decompression of 3 or more levels appears to be a safe and effective procedure with acceptable outcomes at 2 years after surgery.
P238: Back Pain in Surgically Treated Degenerative Lumbar Spondylolisthesis: What Can We Tell Our Patients?
Michael Bond1, Hangbing Zhou2, Nicolas Dea1, Christopher Bailey3, Raphael Charest-Morin1, Andrew Glennie4, Neil Manson5, Hamilton Hall6, Kenneth Thomas7, Raja Rampersaud6, Greg McIntosh8, and Charles Fisher1
1Combined Neurosurgical and Orthopaedic Spine Program, Vancouver General Hospital, Vancouver, British Columbia, Canada
2Hartford Hospital, Hartford, CT, USA
3Western University, London, Ontario, Canada
4Dalhousie University, Halifax, Nova Scotia, Canada
5Saint John Regional Hospital, St John, New Brunswick, Canada
6University of Toronto, Toronto, Ontario, Canada
7University of Calgary, Calgary, Alberta, Canada
8Canadian Spine Outcomes and Research Network, Toronto, Ontario, Canada
Introduction: Surgery for degenerative lumbar spondylolisthesis (DLS) has traditionally been indicated for patients with neurogenic claudication. Surgery improves patients’ disability and lower extremity symptoms, but less is known about the impact on back pain. This study aims to evaluate changes in back pain after surgery and identify prognostic factors influencing these changes in surgically treated DLS. Methods: Consecutive patients with DLS surgically treated were prospectively enrolled in the Canadian Spine Outcomes Research Network (CSORN) registry. Patients had demographic data, clinical information, disability (ODI [Oswestry Disability Index]), and back pain (NRS [Numerical Rating Scale] back pain) scores collected prospectively at baseline, 3, 12, and 24-month follow-up. Results were compared with baseline using simple summary statistics and factors associated with improved back pain were assessed with multivariate regression (significance was P < .05). Results: A total of 557 patients were identified, all had reached 3-month follow-up, 376 (67.5%) had reached 12-month follow-up, and 141 (25.3%) had reached 24-month follow-up. Mean age at baseline was 66.2 (±9.5), and 58.5% were female. Back pain improved significantly at 3 months, and was maintained at 12, and 24-month follow-up compared with baseline (P < .001). Improvement in NRS-back pain scores at 12 months was on average 3.2 (±2.8) points and clinically significant improvement in back pain was observed in 75% of patients (MCID [minimal clinically important difference] NRS-pain 1.2 points). Factors associated with meeting MCID NRS-Back pain at 12-month follow-up were higher baseline back pain, worse baseline physical function, and symptoms duration of <2 years (P < .05). Conclusion: Back pain improved significantly during follow-up for patients treated surgically for DLS. This research demonstrates that for patients undergoing surgery for DLS, the majority will have improved back pain at 1-year follow-up.
P239: Posterior Lumbar Spinal Decompression Combined With Coflex Interspinous Dynamic Stabilization for Degenerative Lumbar Stenosis: A Minimal 7 Years Follow-up Study
Yong Hai1 and Aixing Pan1
1Beijing Chaoyang Hospital, Capital Medical University of China, BeijingChina
Introduction: This study aimed to evaluate the long-term outcome of posterior lumbar spinal decompression combined with Coflex interspinous dynamic stabilization for lumbar spinal stenosis (LSS). Material and Methods: It was a retrospective study. Thirty patients (12 males and 18 females) with the diagnosis of LSS were treated by Coflex interspinous dynamic stabilization in our clinic from September 2007 to June 2009. Clinical evaluation including visual analogue scale score (VAS) and Oswestry Disability Index (ODI) were performed. Complications, reoperation rate, adjacent segment degeneration (ASD) rate were recorded. Meanwhile, radiographic measurements including intervertebral foraminal height (IFH), intervertebral space height (ISH), lumbar range of motion (ROM) were compared at preoperation, postoperation, and last follow-up. Results: Twenty-five Coflex surgeries, 5 topping-off surgeries (Coflex combined with fusion) were completed successfully. The average follow-up period was 94.6 months (84-108). The operation time, blood loss, and length of hospital stay was 76.5 minutes (60-126), 120.8 minutes (100-180) and 150.7 mL (100-200), 280.1 mL (180-400), 10.8 days (8-14) and 12.5 days (10-16) in Coflex group and hybrid group, respectively. The postoperative VAS score improved significantly in both groups (Back pain: 6.87 ± 1.53 to 2.13 ± 0.78 (P = .000). Leg pain: 7.81 ± 1.49 to 2.08 ± 0.83 [P = .000]). The postoperative ODI evaluation improved significantly in both groups (54.2 ± 16.39 to 8.87 ± 2.86 [P = .000]). In the aspect of imaging study, the IFH increased from 19.41 ± 1.74 (preoperative) mm to 22.14 ± 2.39 mm (postoperative) and returned to 19.52 ± 2.87 mm (last FU). The ISH manifested the same changing trend. The ROM on Coflex level had a slightly drop form 5.70 ± 3.69° to 3.04 ± 2.31°, but the ROM of the adjacent segment were maintained. Three patients (10%) presented ASD, 1 patient had restenosis of the operated segment and 1 patient had degeneration on other segment, 4 of them went through a second surgery. Conclusion: The present retrospective study demonstrated that the Coflex interspinous dynamic stabilization implanted after decompression was long-term effective for LSS with acceptable complication and reoperation rate. Meanwhile, the Coflex device could maintain the IFH, ISH and ROM of operated level, which might prevent the occurrence of ASD.
P240: Impact on Spinal Global Balance by Only Laminectomy in Patients With Lumbar Canal Stenosis
Takahiro Iizuka1, Hironari Debata1, Toyohito Iwami1, Atsuji Kashiro1, and Tetsuro Takai1
1Kouseikai Takai Hospital, Tenri, Japan
Introduction: One of the major concerns on spinal surgery is the spinal balance, which is defined with SVA (sagittal vertical axis), LL (lumbar lordosis), PI (pelvic incidence), PT (pelvic tilt), S1 slope and L1 inclination. Some reports recommend the surgical procedure to correct PI-LL <10°. However, there are little discussions on the degree, which should be corrected. Spinal balance commonly gets worse on SVA and LL by aging. Decrease of LL is considered as one of aging changes. Because loss of disc height in lumbar spine causes loss of LL and restriction of LL with close spinous processes. Avoidance posture of lumbar stenosis is also presented as loss of LL. We performed laminectomy for lumbar central canal stenosis without vertebral deformities. Decompression and resection of spinous process may be one of the keys to correct lumbar spinal balance. Aims: To elucidate the impact of only decompression for LCS on the spinal balance. Material and Methods: Thirty patients (Males: 22, Females: 8, age 72.3 years) who underwent laminectomy for LCS were enrolled in this study. Pre- and postoperative (at 3 months) SVA, LL, PI, PT, S1 slope, and L1 inclination were recorded. Results: Preoperative and postoperative parameters were restored, respectively. SVA: 80.3→53.0 mm, LL: 35.1→40.1, PT: 23.6→19.9, S1 Slope: 29.2→27.2, L1 inclination: 8.6→11.5. Preoperative PI-LL: 16.6 and postoperative PI-LL: 11.5. Conclusion: The loss of global spinal balance may be related to the avoidance posture for neural compression and aging changes in LCS patients. In this study, laminectomy settled loss of spinal global balance shown with SVA and LL change. These results suggest that laminectomy may restore the spinal global balance in the patients with central canal stenosis and that the parameter does not always verify the correction surgery.
P241: Efficacy of Transforaminal Steroid Injection as a Surgery-Sparing Intervention
Daniela Linhares1, Sara Almeida Santos1, Manuel Ribeiro da Silva1, Jorge Lopes1, and Nuno Neves1
1Centro Hospitalar São João, Porto, Portugal
Introduction: The efficacy of a transforaminal steroid injection (TFSI) is still a matter of debate. Few studies are available on long-term effect of TFSI and in their impact in the further need of surgery. This study aims to evaluate and assess the efficacy of TFSI in patients with lumbar and sciatic pain Material and Methods: A retrospective analysis was performed. All patients submitted to a TFSI from 2014 to 2016 were assessed, and included if at least 16 months of follow-up after TFSI were available. Rates of recovery, relapse, and need for further surgery were assessed based in local and central clinical records. Results: Seven-three patients, 40 females (P = .413), mean age 54.84 ± 14.22 years were included in the final assessment, with lumbar and sciatic pain complaints. All had a CT (computed tomography) and/or MRI (magnetic resonance imaging) showing disc herniation and/or stenosis; 10 had root compression signs on MRI, in 9 no root compromise was identified and in 54 the compression was doubtful (P < .001). Thirty-three were submitted to TFSI at L4L5 level, 39 at L5S1 and 4 at 2 levels; 35 procedures on the right side, 35 on the left, and 3 bilateral. In 41 patients, an electromyogram was performed; 27 were normal, 12 had chronic changes, and 2 patients had signs of an acute compression. A total of 46.6% (n = 34) of patients resolved after the procedure. (P = .558); from these 10 (29.4% of those that resolved) had recurrence of pain (P = .016), in a mean time of 4.7 ± 3.5 months. Twenty-two patients (30.1%) were referred to surgery, and 14 were already operated (4 remain on the waiting list, 2 refused, and 2 had medical problems contraindicating the intervention). From these 14 patients, 11 improved after the intervention (P = .033). One of the 10 patients with root compression in the CT/MRI had a normal EMG (electromyography). No significant differences were found among genders in resolution and recurrence of pain. Also, EMG and MRI/CT findings did not predict resolution or recurrence (P = .605 and P = .407). No differences were found in age, comparing patients with and without resolution. Thirteen patients were submitted to a previous intervention. From these, 4 (30.8%) became asymptomatic after the procedure, opposing the 50% of resolution in the group without previous interventions. No significant changes were found in resolution or recurrence rates in patients with previous interventions. When evaluating the overall result of the procedure at 18 months, 24 patients became asymptomatic (32.9%), with the other 67.1% remaining symptomatic (after no direct relieve or relapse), P = .003. Also, only 2 patients with previous spine surgery were asymptomatic (P = .013). Conclusion: TFSI leads to a high success rate, but almost 30% relapsed. Nevertheless, long-term resolution of symptoms is present in a reasonable number of patients, representing almost one third of the individuals who underwent TFSI. In this setting age, gender, MRI/CT, and EMG did not significantly predict resolution of symptoms. This study goes along with previous reports stating that TFSI is effective for treating radicular symptoms as a surgery-sparing intervention. However, literature on post surgery pain is still scarce, and as reported in our setting, its effect is low.
P242: Risk Factors for Radiologic Adjacent Segment Degeneration After Lumbar Fusion: Does Paraspinal Muscle Atrophy Increase the Rate of Adjacent Segment Degeneration?
Jong Yeol Kim1
1Gospel Hospital, Kosin University, Busan, Republic of Korea
Introduction: The purpose of this clinical study was to evaluate the relationship between body mass index (BMI), preoperative adjacent facet joint degeneration, disc degeneration, paraspinal muscle atrophy, and radiologic adjacent segment degeneration (ASD) after lumbar fusion. Material and Methods: A retrospective study was conducted on a consecutive series of 510 patients who underwent posterior lumbar fusion for degenerative lumbar disease between January 2009 and October 2009. A total of 50 patients with ASD after surgery were selected. Another group of 50 matched patients with degenerative lumbar disease without ASD after spinal fusion were selected as the control group. Each patient in the ASD group was matched by age, sex, fusion level, and follow-up period with a control patient. The risk factors considered were higher BMI, preoperative adjacent segment disc, and facet degeneration, paraspinal muscle atrophy, and paraspinal muscle fatty degeneration. The ASD and control groups were compared for demographic distribution and radiographic data to investigate the predictive factors of radiologic adjacent segment degeneration after posterior lumbar fusion by logistic regression. Results: The mean age of the patients with ASD was 60.80 years, which did not differ significantly from that of the control patients in which ASD did not develop (60.82 years, P = .988). The average body mass index (BMI) was 24.86 kg/m2 for the ASD group and 23.70 kg/m2 for the control group (P = .04). The 2 groups did not differ significantly in follow-up duration, sex ratio, body height, body weight, or number of fused segments. A multivariate logistic regression analysis demonstrated that higher BMI (OR [odds ratio]: 1.318, P = .009), preoperative facet degeneration on preoperative CT (computed tomography) examination (OR: 2.151, P = .031), disc degeneration on MRI (magnetic resonance imaging; OR: 2.788, P = .002), and a smaller relative cross-sectional area (CSA) of the paraspinal muscle (OR: 0.079, P = .001) maintained their significance in predicting the development of ASD. Conclusion: The occurrence of radiologic ASD is most likely multifactorial and is related to higher BMI, preexisting facet and disc degeneration on preoperative examination, and a smaller preoperative relative CSA of the paraspinal muscle on preoperative MRI examination.
P243: Surgical Treatment of Lumbar Yuxta Facet Cysts—When Is a Segmental Fusion Necessary? Analysis of 29 Surgical Outcome and Literature Review
Francesco Ciccolo1, David Cancer Castillo1, Augusto Covaro1, Gemma Vila Canet1, Anna Isart Torruella1, Anna Garcia De Frutos1, Maria Teresa Ubierna Garces1, and Enric Caceres Palou1
1ICATME, Hospital Universitari Dexeus, Barcelona, Spain
Introduction: Yuxta facet cysts (YFCS) it is a rare cause of nerve root compression, back pain, and neurogenic claudication. Optimal surgical treatment is not yet clarified. The purpose of this article is to specify whether the surgical excision and nerve root decompression by itself is enough as the sole surgery measure or a further back segmental fusion has required. Material and Methods: A single center retrospective analysis of 29 patients, surgically treated for YFCS. A clinical evaluation was performed trough preoperative and postoperative lumbar radicular visual Analogue scale (VAS) and postoperative Oswestry Disability Index (ODI). The surgical decompression technique was described, and the cases in which a segmental fusion has been necessary were analyzed. Results: Analysis of 29 patients (15 women and 14 men), mean age 61.5 years. Mean follow-up was 3 years (2-6). In 21 cases (75%), affected level was L4-L5, 3 cases in L3-L4, and 5 cases in L5-S1. Radiculopathy was the predominant symptom. Fourteen patients (48.3) showed no slipped vertebra, on the other hand, 14 patients (48.3%) showed Meyerding grade 1 degenerative spondylolisthesis (flexion dynamic lateral X-ray) and 1 case (3.4%) present Meyerding grade 2 degenerative spondylolisthesis. Previously to the surgery 28 of 29 patients were treated conservatively. The failure of conservative treatment has placed the indication for surgery. In 25 cases (86.2%), a removal of the YFCS has been performed with the liberation of the nervous structures; only in 4 cases (13.7%) it was associated with a lumbar fusion. Postoperative lumbar and radicular VAS score improve significantly. Post operative Oswestry Disability Index show a mean rate of 9 point. No statistically significant correlations emerged between sex, age, level, presence of spondylolisthesis, and reoperation rate, when compared with lumbar and radicular VAS. The coexistence of degenerative spondylolisthesis and YFCS shows a high incidence. Conclusion: No many studies analyze the coexistence of YFCS and spondylolisthesis. Improve in leg pain, back pain, and neurogenic claudication may be achieved in most of cases by complete YFCS resection trough unilateral segmentary decompression, without complete artrecthomy. Decompression without fusion (86.2%), has shown good and excellent results in most cases. The rate of reoperations for progression of spondylolisthesis was statistically not significant. No reoperations cases were reported for recurrence of the cyst.
P244: Efficacy of Steroid Epidural Injections in Treating Radicular Type Lower Back Pain
Charaka Dasanayake1
1Teaching Hospital Kandy, Kandy, Sri Lanka
Introduction: Steroid epidural injection (ESI) is a common nonsurgical treatment modality for radicular type of low back pain. Current evidence, including systematic reviews have shown a mixed response in terms of its efficacy. There is still no strong evidence to predict, which patients are more likely to improve with steroid epidural injections. Methodology: We conducted a prospective cohort study on 41 patients (35 females and 6 males) between ages of 29 and 80 years (median 56 years), who had radicular type of low back pain and had no features of significant canal stenosis on MRI. Forty milligrams of methylprednisolone were injected to the epidural space close to the spinal root level most compatible with symptoms. Patients were reassessed after 6 months. Pre and post injection straight leg raising test angles (SLRT) were measured. Quality of life (QOL) was assessed using Oswestry Low Back Pain Disability Questionnaire (ODQ) and Quebec Back Pain Disability Scale (QDS) before and after ESI. Results: ESI significantly improved SLRT (P = .002), and quality of life according to ODQ (P < .001) and QDS (P < .001) questionnaires at 6 months post injection. Improvement of QOL was fairly consistent with improvement of SLRT. Significantly better improvement of SLRT was seen among patients who had higher (near normal) SLRT prior to injection. Older patients showed better improvement of QOL compared with younger patients. Whereas younger patients showed better improvement of SLRT than older patients. Conclusion: ESI is an effective treatment against radicular type of lower back pain. Age and SLRT before injection can be used to predict the likelihood of improvement following ESI in terms of QOL and SLRT.
P245: The Effect of Lumbar Decompression Surgery on Gait in Spondylolisthesis Patients
Ram Haddas1, and Isador Lieberman1
1Texas Back Institute, Plano, TX, USA
Introduction: Lumbar spondylolisthesis is a degenerative disorder typically causing mechanical and neurological symptoms in the back and lower extremities, which can detrimentally affect the patients’ quality of life. Leg pain and gait disturbance are the usual manifestations of spondylolisthesis and are commonly alleviated by decompression with or without stabilization surgery. Gait analysis uniquely allows for the objective functional evaluation pre- and postoperatively. The purpose of this study was to evaluate the effect of surgical intervention in spondylolisthesis patients using gait analysis. Materials and Methods: Thirty-three patients with spondylolisthesis who have been deemed appropriate surgical candidates underwent clinical gait analysis the week before surgery (Pre) and 3 months (Post) after surgery. Fifty reflective markers were incorporated to collect full body 3-dimensional kinematics using 10 cameras. The patients walked at his/her self-selected speed along a 10-m level walkway. Spatiotemporal parameters (ie, gait speed, cadence, single and double support time, and step length) and Gait Deviation Index (GDI) were calculated and analyzed with a repeated measurement ANOVA (analysis of variance) to determine differences between times. Results: Walking speed (Pre: 0.85 ± 0.18 vs Post: 0.94 ± 0.15 m/s; P = .002), cadence (Pre: 95.08 ± 14.96 vs Post: 102.10 ± 10.68 steps/min; P = .011). single support time (Pre: 0.41 ± 0.15 vs Post: 2.06 ± 0.85 seconds; P = .021) and GDI (Pre: 63.37 ± 18.62 vs Post: 70.04 ± 9.28; P = .050) improved after surgical intervention. No significant differences were found at the stride length and time. Patients-reported outcomes, such as VAS low back (Pre: 4.94 ± 2.80 vs Post: 2.42 ± 2.37; P = .001), VAS middle back (Pre: 2.99 ± 2.97 vs Post: 1.12 ± 1.55; P = .001), VAS leg (Pre: 4.77 ± 2.86 vs Post: 1.73 ± 2.16; P = .001), and ODI (Pre: 39.65 ± 15.12 vs Post: 27.61 ± 12.80; P = .001) all improved following surgical intervention. Conclusions: Spondylolisthesis patients can typically present with a claudicatory gait disturbance, manifest as numbness, heaviness, or lower extremity weakness. This study objectively demonstrates and support previous clinical reports that lumbar decompressive surgery helps spondylolisthesis patients improve their gait and overall function. It is beneficial to have objective, quantitative data to describe changes in a subjective clinical finding such as gait. This study not only provides a richer understanding of the gait pathology in spondylolisthesis patients but also uniquely showed that spondylolisthesis patients have altered gait cycle. Spine care providers should use gait analysis as part of their clinical evaluation to better understand the effects of the disease and its treatment on their patients’ gait, function, and ultimately, quality of life.
P246: The Polymethylmethacrylate-Augmented Lumbar Screw Fixation for Lumbar Spondylolisthesis in Osteoporosis Patients: Experiences With 32 Cases
Tuan Pham Anh1
1University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh, Vietnam
Introduction: The pull-out and loosening of pedicle screws are common and serious problems in pedicle screw fixation surgery with osteoporosis patients. Polymethylmethacrylate (PMMA) augmentation of the pedicle screw can significantly increase the stiffness and strength of spinal fusion in osteoporosis patients. The purpose of this study is to evaluate the efficacy and safety of the lumbar spinal fusion surgery with the PMMA-augmented pedicle screw for lumbar spondylolisthesis in osteoporosis patients. Material and Methods: Between November 2015 and November 2017, 32 osteoporosis patients with lumbar spondylolisthesis were operated by the lumbar fusion surgery with the PMMA-augmented pedicle screw. We evaluated the improvement based on the VAS score and the modified MacNab classification. The PMMA leakage and other complications were assessed intraoperatively and postoperatively. The PMMA leakage was evaluated by postoperative multislices CT (computed tomography) scanner. Results: All patients are female. The age ranged from 50 to 79 years (the mean age 64.5 ± 7.8 years). It consisted 25 (78.2%) patients with grade 1 spondylolisthesis and 7 patients (21.8%) with grade 2. No patient died postoperatively. A total of 190 PMMA-agumented pedicle screws were inserted in 95 vertebral bodies. The improvement rate is 81.2% and 81.3% at 3 and 6 months follow-up based on the modified Macnab classification. Three patients had cement leakage and 2 patients had CSF leakage intraoperatively. The perivertebral cement leakage rate was 43.68% inspected by postoperative multislices CT scanner. No patients had complications related with this leakage. The bone fusion rate is 65.6% (21 patients) at 6 months follow-up and no screws loosening happens. Conclusion: The lumbar spinal fusion surgery with the PMMA-augmented pedicle screw for lumbar spondylolisthesis in osteoporosis patients has reasonable outcome and is safe without the significant complication.
P247: Evaluation of Minimally Invasive Lumbar Interbody Fusion in Degenerative Lumbar Disc Disease
Ahmed Ramadan Abdelfattah saber1, Hasan Salheen2, and Gouda Mohamed3
1Fayoum University, Fayoum, Egypt
2Sankt Elisabeth Hospital Gutersloh, Gutersloh, Germany
3Benha Faculty of Medicine, Benha, Egypt
Introduction: The indication for minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) was restricted to the cases of neuroforaminal stenosis this study aims to evaluate the results of MI-TLIF with bilateral pedicle screw fixation, in patients with degenerative spondylolisthesis associated with absolute canal stenosis. Methods: Twenty-five patients with degenerative spondylolisthesis and spinal canal stenosis underwent MI-TLIF from June 2016 to June 2017 with at least 1-year follow-up. In our study, the surgery was performed through a unilateral parasagittal approach at the symptomatic side with bilateral decompression via cross-over technique. Microscopic assisted transforaminal micro-discectomy was done using the microscope and insertion of single interbody cage through the discectomy side done for 10 patients (40%) underwent single-level MI-TLIF, 13 (52%) patients underwent double-level MI-TLIF and 2 patients (8%) underwent triple-level MI-TLIF. Microscopic assisted transforaminal micro-discectomy was done using the microscope and insertion of single interbody cage through the discectomy side. Clinical assessment parameters included Visual Analog Scale (VAS) score and Oswestry Disability Index (ODI), while radiologic assessment done via Bridwell interbody fusion grading system. At the last follow-up, the level of bone fusion was determined in accordance with the Bridwell interbody fusion grading system for classification of fusion results. Results: The VAS scores of back pain and radiating leg pain tended to improve postoperatively for leg pain back pain irrespective of the number of the affected levels. In terms of ODI, the results of functional assessments also irrespective of the number of the affected levels. According to the Bridwell interbody fusion grading system; 18 (72%) cases with grade 1, 5 (20%) cases with grade 2 (8%), and only 2 cases with grade 3 while no case ended by grade 4. There was 1 case with wound dehiscence and another case developed transient motor weakness of the quadriceps postoperatively recovered after 6 weeks conservative therapy, and there was no revision. Conclusions: MI TLIF is applicable and safe in cases of degenerative spondylolisthesis associated with spinal stenosis. The indication for this technique is not only restricted anymore for the cases of neuroforaminal stenosis. Regardless the number of the affected levels this study showed satisfactory clinical and radiological outcomes.
Keywords
multilevel interbody fusion, minimally invasive surgery, transforaminal lumbar interbody fusion
P248: Lumbar Laminectomy in the Outpatient Setting is Associated With Lower 30-Day Complication Rates
Teja Karukonda1, Nickolas Mancini1, Austen Katz1, Mark Cote1, and Isaac Moss1
1University of Connecticut Health Center, Farmington, CT, USA
Introduction: Lumbar laminectomy is being increasingly performed in the outpatient setting, however, few studies have examined the difference in complication rates between performance of this procedure in the inpatient and outpatient settings. The purpose of this retrospective cohort study was to compare the incidence of complications in patients undergoing single-level and 2-level lumbar laminectomy in either the inpatient or outpatient settings. The primary outcome measure was the risk of postoperative complications for both a 1- and 2-level lumbar laminectomy in either the inpatient or outpatient setting. Secondary outcome measures included independent risk factors for a complication following 1- and 2-level lumbar laminectomy. Patient demographics and the proportion of laminectomies performed in the inpatient and outpatient settings annually were also reported. Material and Methods: Patients who underwent single-level and 2-level lumbar laminectomy were identified in the ACS NSQIP (American College of Surgeons National Surgical Quality Improvement Program) database from the years 2006 to 2015 using the Current Procedural Terminology (CPT) codes 63047 and 63048 as the primary procedural code. Independent patient variables were recorded including demographics and preoperative health characteristics. Logistic regression was then carried out on the entire cohort (unadjusted) and matched sample (adjusted) to determine the risk of postoperative complications for both a 1- and 2-level lumbar laminectomy. A multivariate logistic regression model was created in an effort to identify independent risk factors for a complication. Comparisons were made between 2 groups: (1) inpatient and (2) outpatient as determined by billing data. No conflicts of interest were identified. Results: A total of 18 076 1- and 2-level lumbar laminectomy cases were identified with 10 743 (59.4%) inpatient procedures and 7333 (40.6% outpatient procedures. The incidence of any postoperative complication was significantly lower in the outpatient group than in the inpatient group among all cohorts including 1-level lumbar laminectomy (1.9% vs 6.7%), 2-level lumbar laminectomy (3.17% vs 7.38%), as well as in the combined cohort of 1 and 2-level laminectomies (2.47% vs 7.01%). Significant independent risk factors for complications after lumbar laminectomy were identified including BMI (body mass index) >30 kg/m2 (odds ratio [OR] 1.23, 95% confidence interval [CI] 1.02-1.49, P = .027), age ≥55 (OR 1.28, 95% CI 1.01-1.61, P = .041), a functional status of partially dependent (OR 2.36, 95% CI 1.34-4.18, P = .003), COPD (Chronic Obstructive Pulmonary Disease; OR 1.59, 95% CI 1.10-2.29, P = .013), chronic steroid use (OR 3.38, 95% CI 2.39-4.79, P < .001), and ASA class 3 or 4 (OR 1.74, 95% CI 1.43-2.12, P < .001), and operative time >90 minutes (OR 1.86, 95% CI 1.50-2.30, P < .001). A factor that was found to be protective was performance of the procedure in the outpatient setting (OR 0.40, 95% CI 0.32-0.50, P < .001). Conclusion: This study reports a lower overall complication rate in the 30-day postoperative period following single-level and 2-level lumbar laminectomy performed in an outpatient versus inpatient setting. Outpatient lumbar laminectomy is a viable and potentially safer option than inpatient lumbar laminectomy in appropriately selected patients.
P249: Comparative Analysis of the Occurrence Factors for Adjacent Segment Disease—With Patients Followed More Than 10 Years After Lumbar Spinal Fusion
Jaewan Soh1
1Soonchunhyang University Cheonan Hospital, Cheonan, Korea
Introduction: There are many concerns about adjacent segment disease (ASD) after lumbar spinal fusion. There are many studies that the causes of ASD are natural degenerative change or risk factors. Analysis of risk factors for ASD was carried out targeting the patients among more than 10 year-follow-up after lumbar spinal fusion for degenerative lumbar spinal disease. Materials and Methods: From August 1988 to December 2005, 581 patients underwent lumbar spinal fusion of 3 and less segment to treat degenerative lumbar disease. Among them, 163 patients followed more than 10 years were included in this study. Gender, age, residence, clinical result, preoperative diagnosis, fusion method, number of fused segments, whether laminectomy of adjacent segments, preoperative degree of disc degeneration of adjacent segments in MRI (magnetic resonance imaging), whether adjacent segments included L4-5 or L5-S1, and radiological measurements were analyzed. In radiological measurement, preoperative and postoperative lumbar lordotic angle (LLA), correction of LLA, postoperative fusion segment lordotic angle (FSLA), postoperative FSLA per level were estimated. Statistical univariate analysis was performed with the chi-square test and multivariate logistic regression analysis was done by using SPSS 14.0 (P < .05). Results: There were 22 patients with revision surgery due to ASD. Two patients were operated by decompression or discectomy and 20 patients needed additional fusion. In univariate analysis, the frequency of ASD was significantly high in cases that age was more than 65 years (P = .028), number of fused segments was single (P = .008), adjacent segments included L4-5, or L5-S1 (P = .046), FSLA per level was <16 (P = .013). In multivariate logistic regression analysis, the frequency of ASD was significantly high in case that age was more than 65 years (P = .022, OR = 3.857). Conclusions: Of patients followed-up more than 10 years after lumbar spinal fusion, we analyzed risk factors for ASD. In this study, the important risk factor of ASD was age that the patients were more than 65 years old at initial operation. In case of old patients, careful decision should be considered to carry out lumbar spinal fusion.
P250: Multilevel Anterior Lumbar Disc Replacement: Sagittal Balance Correction
Shamil Gizatullin1, Viacheslav Kurnosenko1, Alexander Chistosturov1, and Ilya Dubinin1
1Burdenko Clinical Military Hospital, Moscow, Russian Federation
Introduction: In modern spinal (lumbar) surgery, it is obvious that the preservation or restoration of sagittal balance is vital, as it guarantees long-term treatment outcome. Sagittal balance of the spine is the basis of dynamic balance between the shape of the vertebral column and the mechanisms that support it. Posterior spondylodesis is a widely used method for the treatment of various diseases of the spine. Today, fusion 360° technique is considered as a standard priority in spinal stabilizing surgeries. However, spinal fusion alters the normal biomechanics of the spine, restricts vertebral-motor segments mobility, thereby causing the overload on the adjacent segments. Thus, according to some authors, the posterior spinal fusion can accelerate the degenerative cascade in adjacent spinal segments. On the other hand, in some cases, the complete removal of intervertebral disk using anterior lumbar interbody fusion (ALIF) with prior calculation and restoration of sagittal balance, shows good long-term results, especially with multilevel (2-3 lower-lumbar segment) interventions. Purpose of research was to evaluate the effectiveness, long-term results, and the degree of degenerative changes in adjacent vertebral disk segments in single-and multilevel sagittal balance correction through anterior extraperitoneal access. Material and Methods: A retrospective examination of 40 patients following ALIF operation in multilevel (2-3 levels) sagittal balance correction using rigid lordotic cages from 2014 to 2017 for degenerative-dystrophic lumbar diseases. Of the 40 patients, 14 were females (36%) and 26 males (64%). The mean age was 35 ± 12.3 years. The mean follow-up period was 2 ± 0.8 years. MRI (magnetic resonance imaging) assessment of degenerative changes in adjacent spinal segments and X-rays in the standing position in the anterio-posterior and lateral projections were carried out during the preoperative, postoperative, and during patients’ follow-up visits. All patients included in the study had normal spinal X-rays, heights of adjacent intervertebral discs; none showed signs of instability in the adjacent spinal discs. In all cases, we studied the preoperative, postoperative periods, and assessed the changes in the adjacent intervertebral discs X-rays according to the Schwabb’s classification. Based on the determination of the pelvic-vertebral parameters, we evaluated the condition of the sagittal profile with the use of formulas with reliable sensitivity of 91% to predict preservation of normal sagittal balance within 24 months after surgery: PI – LL – TK ≤ 45°. Patients with postoperative values satisfying the formula were regarded as patients with normal sagittal balance. Statistical data processing was performed using a simple regression analysis and Student t test. If P < .05, the differences were considered statistically reliable. Changes assessment in the adjacent intervertebral discs was evaluated based on the MRI according to the classification of Pfirrmann. Results: After 1-year follow-up, 5 patients (12.5%) had degenerative changes in adjacent intervertebral discs. They all had initial preoperative changes in the intervertebral discs (Pfirrmann 2-5 stage). Sagittal imbalance was identified only in 2 cases. After 2 years of monitoring, the number of patients with degenerative changes in adjacent intervertebral discs and sagittal imbalance did not change. Conclusion: In conclusion, the direct influence of sagittal balance on the quality of life of patients cannot be ignored in modern spinal surgery; however, this notion raises a number of skeptical questions and contradictions. Our study showed that the anterior single and multilevel sagittal balance correction using lordotic (with a given angle of correction) cages allows not only to achieve the formation and preservation of the necessary lumbar lordosis, but also significantly reduces the risk of degenerative changes in the adjacent intervertebral discs.
P251: Bilateral Decompression in Lumbar Spinal Stenosis Through a Unilateral Posterior Endoscopic Approach: Surgical Technique and Results About 723 Cases
Destandau Jean1, and Rué Marjory1
1Endoscopic Spine Center, Bordeaux, France
Introduction: This endoscopic surgical technique has been used by the first author since 1993 for disc prolapses and since 2001 for lumbar spinal stenosis. Moreover, a dynamic rehabilitation program is used to improve postoperative recovery. Surgical technique is described and results of 723 cases are presented as well as long-term results. Material and Methods: The device (Endospine, Karl Storz GmbH, Tuttlingen, Germany) is composed of 3 tubes: one for the endoscope, one for suction canula, and the largest one for classical surgical instruments. Since 2001, this endoscopic technique has been used in spinal stenosis performing a bilateral decompression through a unilateral posterior approach on the left side or on the side of predominant signs. From February 2001 to December 2015, 723 patients have been operated on with this technique. In 87%, surgery was a single level decompression and in 17% there was an associated spondylolisthesis. Prolo’s criteria were used. A key point is to determine how many levels have to be operated. In this study, 629 patients underwent a single-level approach, and all of them had the dynamic rehabilitation program. Results: A total of 542 questionnaires (75%) were returned showing excellent results in 487 cases (90%) and poor in 48 (9%). With an average delay of 2 weeks, 482 patients (89%) returned to a normal life. Sixteen patients (3%) needed a second operation with an average delay of 27 months. The complications observed were dural tear in 50 (6,9%); nerve root lesion in 4 (0,5%); resection of articular process in 28 (4%); wrong level decompression in 2 (0,7%); and 5 compressive hematomas (0,7%); no infection. In answer to the questions on global satisfaction and on the accuracy of the information given before surgery, 98% responded as satisfied and felt the information given to be accurate and 100% were pleased to rise early after the surgery and walk all around. Conclusions: This minimally invasive technique is mainly used in single-level spinal stenosis even with associated spondylolisthesis, but can be also used in several levels of decompression. The good results and the fast resumption of normal activities explain that this endoscopic technique could become an advantage in spinal stenosis, pathology that is increasing with the lifespan extension. The option to treat as less levels as possible looks good as rate of reoperations is quite low.
P252: The Regional Effect of Lumbar Fusion Surgery on Volumetric Bone Mineral Density Measured by Quantitative Computed Tomography in Adjacent Vertebrae: A Longitudinal Cohort Study
Ichiro Okano1, Conor Jones1, Stephan Salzmann1, Courtney Ortiz Miller1, Colleen Rentenberger1, Jennifer Shue1, John Carrino1, Andrew Sama1, Frank Cammisa1, Federico Girardi1, and Alexander Hughes1
1Hospital for Special Surgery, New York, NY, USA
Introduction: Previous studies reported that lumbar spine surgery has a negative effect on bone mineral density (BMD) in the lumbar spine. Dual X-ray absorptiometry (DXA) was generally used for following BMD change in these studies, however, DXA has several limitations for measuring BMD in the vertebrae with morphological changes and metal implants, which are often associated with lumbar spine surgery. Also, it is still unclear if this BMD change is caused by a local mechanical effect or a systemic physiological insult associated with the surgery. In this study, we investigated the change of BMDs in multiple adjacent vertebrae utilizing quantitative computed tomography (QCT). Material and Methods: Institutional ethics board approval was obtained for this study. We reviewed clinical records and images of 297 consecutive patients who underwent posterior lumbar spine surgery between 2014 and 2017, at a single academic institution. Patients who underwent posterior fusion surgery with instrumentation and had both preoperative and secondary postoperative computed tomography of the lumbar spine between 6 and 12 months were included. Volumetric bone mineral density (vBMD) measurements by quantitative computed tomography (QCT) were conducted in L1 to S1 vertebral trabecular bone. The change of vBMD in the vertebrae 1 or 2-level above the upper instrumented vertebra (UIV + 1, UIV + 2) and one level below the lower instrumented vertebra (LIV + 1) were analyzed. Statistical analyses were conducted utilizing paired t test, 1-way/repeated-measures ANOVA (analysis of variance), and Pearson’s correlation test. The statistical significance level was set at P < .05. Results: A total of 91 patients met our inclusion criteria. Mean age (± SD [range]) was 61.9 ± 11.9. A total 55.6% of the patients were female. Median interval between the surgery and the secondary CT was 248 [180-364] days. Volumetric BMD (± SD) in UIV + 1 was 113.1 ± 32.6 mg/cm3 preoperatively and 102.4 ± 32.2 mg/cm3 (percent change: −10.5 ± 12.6%) postoperatively (P < .001). No correlation was observed between percent vBMD change in UIV + 1 and interval between operation and postoperative CT (r = .15, P = .15). This trend of vBMD change was similar regardless of UIV level and number of fused levels. The change of vBMDs in UIV+2 and LIV+1 appeared similar as UIV + 1 (UIV + 2: −11.9 ± 12.3%, P = .19, LIV + 1: −7.2 ± 20.7%, P = .40). Conclusion: Posterior lumbar fusion surgery negatively affected the regional vBMDs measured by QCT in adjacent levels. BMDs in UIV + 1, UIV + 2, and LIV + 1 were equally affected by the surgery. Our finding suggests that the postoperative decrease of regional BMDs in the lumbar spine dominantly occurs in the early postoperative phase (within 6 months) and a systemic effect has a greater role, rather than a regional mechanical one, in this postoperative BMD decline.
P253: Evaluation of Microsurgical Lumbar Disc Surgery in Obese Patients in Lateral Position
Hasan Salheen1, Gouda Mohamed2, and Ahmed Ramadan Abdelfattah saber3
1Sankt Elisabeth hospital Gutersloh, Gutersloh, Germany
2Benha Faculty of Medicine, Benha, Egypt
3Fayoum University, Fayoum, Egypt
Introduction: Generally, operating on obese patients is a challenge, especially if applying microsurgical techniques is considered. Complications of the commonly applied prone position in lumbar disc surgery are reported. This study aimed to evaluate the safety and efficacy of the microsurgical disc surgery in a lateral position in obese patients with lumbar disc herniation (LDH). Patients and Methods: In the time period between July 2013 and January 2017, 132 obese patients (mean BMI [body mass index] 35.5 kg/m2, range 30.1-47.3 ± 3.9) suffering from LDH with unilateral radicular symptoms had undergone microsurgical disc surgery in a lateral position. Patients with bilateral affection were excluded from this study. The surgeon and the assistant have operated seated. The main surgeon operated using magnification loupes. This sample includes 69 males and 63 females. The most operated levels were L4/5 (n = 66) and L5/S1 (n = 44). The clinical and follow-up data were prospectively analyzed. The degree of pain and disability were measured on the basis of the visual analogue scale (VAS) at 1 day before surgery 3 months and 1 year after surgery. The clinical outcome was evaluated according to modified Odom’s criteria. Complications during and after surgery were documented to evaluate the safety of surgery. Results: A total of 132 patients were followed-up for at least 12 months. The VAS scores at 3 months and 1 year postoperatively were significantly reduced (P < .05) compared with preoperative scale. The clinical outcomes according to modified Odom criteria showed that 85.6% of patients had excellent or good outcome, 10.6% fair and 3.8% poor rates. Regarding the complications, dural tears occurred in 4 patients, 1 case was revised because of persistent dural leakage, 2 patients suffered from postoperative permanent neurological deficit. Five patients had wound dehiscence, 3 of them were revised. The complication rate was higher at the beginning of using the technique. Fives cases of recurrence were observed at different intervals during the follow-up. Conclusions: The early efficacy of microsurgical disc surgery in lateral position is relatively good and safe for the selected obese patients with LDH in this study. The increased intrabdominal pressure that occurs in the prone position can be avoided. It also allows the anesthesiologist a better access for intraoperative monitoring of the patient and allows the surgeons to operate while seated. However, a good experience with the disc surgery in prone position is mandatory before starting to operate in the lateral positioning. The limited visualization of the field for the assistant prolongs the learning curve of younger surgeons and can lead to intraoperative difficulties. Cases that need bilateral decompression or cases with extraforaminal LDH are still a limitation for this technique. A better magnification tool should be considered to overcome these disadvantages.
P254: Factors Influencing Stability and Treatment in Grade 1 Degenerative Spondylolisthesis
Nicholas Spina1, Carlijn Schoutens1, Brook Martin1, William Ryan Spiker1, Brandon Lawrence1, and Darrel Brodke1
1University of Utah, Salt Lake City, UT, USA
Introduction: Several studies have recently questioned the optimal treatment for “stable” grade 1 lumbar spondylolisthesis. Yet diagnostic and treatment consensus among spine surgeons does not exist regarding what defines “stability.” Classic parameters have been described based on cadaveric studies, but their translation into clinical practice remains imprecise and unclear. The purpose of this study was to understand how surgeons define “stability” and characterize surgical treatment patterns of stable and unstable grade 1 spondylolisthesis. Materials and Methods: A survey was distributed to LSRS (Lumbar Spinr Research Society) and AOspine North America members through REDCap (Research Electronic Data Capture). Members were queried as to the degree of static translation, dynamic translation, and angular change that would define an unstable lumbar motion segment. The relative importance of several other clinical and radiographic features were ascertained using a 5-point Likert-type Scale. Demographic data included subspecialty, primary practice setting, as well as preferred treatment method for both stable and unstable Grade 1 spondylolisthesis. Results: A total of 226 respondents completed the survey. Seventy-five percent were orthopedic, 25% neurosurgical trained. Fifty-nine surveyed practice in an academic setting, with 41% of respondents practicing in a community, private practice, or VA (Veterans Affairs) setting. Ninety-nine percent of surgeons felt dynamic translation was moderately to extremely influential compared with slightly or not influential at all in defining stability whereas only 54% felt the same with regard to static translation. Sixty-eight percent of surgeons felt facet angulation was moderately to extremely influential, 67% for disc height, 47% for pelvic incidence, 51% severity of back pain, and 42% severity of neurogenic claudication. Sixty percent of surgeons treated stable grade 1 spondylolisthesis with decompression alone versus 40%fusion. All, but 2 respondents treated unstable spondylolisthesis with some type of fusion with 99% utilizing hardware. No clear consensus existed as to the type of decompression or fusion performed. Conclusion: A clear consensus regarding how surgeons define stability does not exist. Dynamic translation appears to be the most influential factor in that definition. Surgeons are divided on whether a fusion should be performed on “stable” grade 1 spondylolisthesis. Whereas a clear consensus exists that fusion is required when “instability” is present.
P255: Is It Possible to Restore a Correct Lumbar Lordosis Only With a Cage?
Andrea Casella1, Fabio Tresoldi1, and Giuseppe Andreoletti1
1Policlinico San Marco, Zingonia, Bergamo, Italy
Introduction: Among the surgical procedures for the correction of the lumbar lordosis, the double approach is frequently performed in spine surgery. However, are we sure it is the correct solution? Is an interbody fusion alone not sufficient to obtain the same results? Aim of our study is to evaluate the degree of lumbar lordosis correction after an interbody fusion, performed by anterior approach. Patients and Methods: During the period between 2014 and 2017, we performed 100 anterior approach surgical procedures with only cage. All patients underwent cervical MRI (magnetic resonance imaging) and pre-, intra-op, and postoperative X-ray. Clinical follow-up was at 1, 3, 6, and 12 months. Results: We had no aseptic mobilization. Only 3% had a local hemorrage and required further surgery; 1% had a retrograde ejaculation. Conclusion: The surgical solution of L5-S1 discopathy with only cage is safe and achievable with an anterior approach interbody fusion. This reduces surgery time (posterior approach) and reduces postoperative rehabilitation time (movement, gait, and daily activities).
P256: L5-S1 Spondylolisthesis Reduction: Only After a Posterior Approach Must the Anterior Interbody Fusion be Performed
Andrea Casella1, Fabio Tresoldi1, and Giuseppe Andreoletti1
1Policlinico San Marco, Zingonia, Bergamo, Italy
Introduction: In the degenerative lumbar diseases, great importance is given to high-level dysplasia spondylolisthesis. When these are diagnosed at L5-S1 level, we believe is best to perform a double approach: posteriorly, reduction of the slip, and stabilization with rods and screws; anteriorly, interbody fusion to correct and obtain an adequate lumbar lordosis. Materials and Methods: During the period between 2014 and 2017, data of 150 patients with high-level dysplasia, who underwent double approach L5-S1 interbody fusion were analyzed. All patients underwent lumbar MRI (magnetic resonance imaging) and pre-op, intra, and postoperative X-ray. Clinical follow-up was at 1, 3, 6, and 12 months. Results: The average degree of lumbar lordosis obtained was 20°. There were no major complications in our population; 2 patients had a superficial wound infection, treated with antibiotics. Conclusions: We believe that a double approach is the best surgical option in high-level dysplasia spondylolisthesis. The posterior approach allows a greater correction of the lumbar lordosis with regard to TLIF (transforaminal lumbar interbody fusion), and the anterior approach permits to implant dedicated cages, which stabilize the correction achieved posteriorly.
P257: Endoscopic Interlaminar Laminectomy as Treatment of Lumbar Canal Stenosis: Surgical Technique Step by Step
Angela Carrascosa Granada1 and Ralf Wagner2
1Madrid, Spain
2Ligamenta Spine Center, Frankfurt am Main, Germany
Introduction: Multiple studies have shown that endoscopic interlaminar laminectomy (EIL) can be performed safely and effectively in the treatment of lumbar spinal stenosis (LSS). Our objective is the detailed description of the accomplishment of the surgical technique, its advantages and disadvantages. Methods: Description of a surgical technique step by step. Results: This surgical procedure is performed under general anesthesia. The patient is positioned in prone decubitus. Under radiographic marking in anteroposterior, the interlaminar space to be intervened is located. An incision of 1 cm by 1 cm of the midline is made and dilator tubes are inserted until the insertion of the endoscope. This consists of a 6 mm working channel through, which you can insert kerrison, dissectors, drill, and the bipolar clamp. The first step is to find the point of attachment of the lower edge of the lamina with the ligamentum flavum. The muscle and blood vessels are coagulated. Once this point is identified, the lower edge of the lamina begins to be drilled with the 3 mm diamond bur hole to locate the yellow ligament. The laminectomy is performed with a kerrison clamp and careful dissection of the yellow ligament and the dura is carried out. Once you have a complete feeling that there are no adhesions to the dura mater, flavectomy is performed. At this point epidural bleeding may appear secondary to the decompression of the dural sac that must be carefully coagulated with the bipolar to avoid losing a clear visualization with the endoscope. Once the laminectomy and flavectomy have been carried out, the foraminotomy should be performed, taking great care not to damage the dura in the lateral recess, since at this point it is particularly common for the dural lesions to be produced by the foraminal stenosis. Once the foraminotomy is performed, it is checked that the general decompression is satisfactory and hemostasis is performed with the bipolar forceps. The endoscope is removed, and a suture is given in muscle fascia and skin. Conclusion: Traditional open laminectomy performed in the treatment of LSS has been associated with excessive muscular dissection, abundant surgical bleeding, hospital admission for several days, and a prolonged recovery time. The EIL is a novel surgical technique that offers a viable, safe, and effective option since, since it is a minimally invasive technique, it can be performed in elderly patients with multiple comorbidities, which allows early mobilization, a 1-day hospital admission and good postsurgical results. It is particularly relevant that age and obesity are not contraindications for this procedure. The main disadvantage when you start the first cases and the learning curve, is that the procedure can be prolonged and if you are performing uniportal endoscopy the disadvantage is that you cannot count on the help of your other hand to facilitate the dissection and resection of structures. This is the reason why the cadaver workshop is crucial for training.
P258: Diagnostic and Surgery for Lumbar Spine Degenerative Disease in Osteoporotic Patients
Shamil Gizatullin1, Viacheslav Kurnosenko1, Ilya Dubinin1, Sergey Bitner1, and Sergey Kazakov2
1Burdenko Clinical Military Hospital, Moscow, Russian Federation
Introduction: Among vertebrogenic pathologies, degenerative-dystrophic diseases are most common in all countries of the world. In this case, the lumbosacral localization is determined in more than 60.0% of patients. This problem is especially acute in patients older than 50 to 55 years. In the same age period, the degenerative changes in the spine are aggravated by the syndrome of mineral and bone disorders, which is no less relevant in the overall structure of musculoskeletal disorders due to its high prevalence and impact on patient disability and significant mortality from complications. The wide spread of the syndrome of mineral and bone disorders as well as the lack of a clear algorithm for surgical treatment in planning operations on the spine in such patients have served as the reasons for this study. Purpose of research was to evaluate the effectiveness of already existing, as well as new, potentially promising methods of surgical correction of degenerative-dystrophic changes of the spine, against the background of systemic osteoporosis. Material and Methods: The study analyzed 60 patients, after corrective operations on the spine using various instrumental stabilizing systems and techniques in the period from 2010 to 2017. Among the patients, 38 were females (63.3%) and 22 males (36.7%). The mean age was 64 ± 7.4 years. The mean follow-up period was 7 ± 2.3 years. All the patients included in the study underwent X-ray examination, CT (computed tomography), MRI (magnetic resonance imaging), a standard study of bone mineral density (densitometry), as well as the study of markers of the mineral and bone metabolism, whose indices make a significant correction in the tactics of planned surgical treatment. Results: Patients were divided into 3 groups of 20 people, depending on the method of surgical correction performed. In group I, T-criterion and bone mineral exchange marker indicators did not go beyond the normal values, as a result of which spine surgery was performed using standard screw stabilization techniques without additional augmentation with bone cement. In group II, indices of mineral density of bone tissue (T criterion >2, but <2.5 SD) and indicators of markers of bone mineral metabolism corresponded to osteopenia. Patients of this group transpedicular stabilization was accompanied by additional augmentation of the screws. In group III, bone mineral density was consistent with osteoporosis. And 100% of patients in this group were women aged 55 to 71 years. Patients of this group used the technique of cortical bone trajectory screw technic, as well as robot-assisted Go-Lif Technic (Mazor Surgical, Israel). The distribution was 10/10. After 7 years of follow-up, 2 patients from group I showed instability of the screws because of osteolytic changes around the screws, which required revision surgery with screws replacement and their additional augmentation. In 5 patients, on the background of progressive osteoporosis, compression fractures of overlying vertebrae of different levels developed, which required surgical correction. Twelve patients (20%) had degenerative changes in adjacent segments. After 7 years of follow-up, signs of instability of systems with additional augmentation of the screws and a cortical bone trajectory were not noted. Conclusion: Planning spine surgery, especially in elder patients, it is necessary to carry out a study of indicators of bone mineral density in the preoperative period and give preference to surgical techniques, which provide additional stability in conditions of a decrease in mineral bone density. Such measures can significantly improve the long-term results of surgical treatment.
P259: In-Hospital Repeat Spine Surgery Following Lumbar Fusion for Degenerative Disease Versus Instability From Fracture, Neoplasm, or Infection
Brook Martin1, Sohail Mirza2, Ian Engler3, William Ryan Spiker1, and Darrel Brodke1
1University of Utah, Salt Lake City, USA
2PEER CLINIC for Back Pain and Spine Surgery, Fairfax, VA, United States
3Tufts University, Boston, MA, USA
Introduction: Repeat surgery following lumbar fusion is an important outcome for patients, surgeons, hospitals, device makers, and payers. Repeat surgeries after a period of 3 to 6 months required for healing an arthrodesis are usually due to disease progression or treatment failure. Repeat surgeries during the initial hospitalization and immediate postoperative period before the arthrodesis has fully healed are usually due to wound problems, neurological issues, or technical device problems. Repeat surgery during the initial hospitalization, thus, is an important quality indicator. Emerging payment models increasingly force hospitals to be accountable for unexpected costs borne during an inpatient stay. We are interested in patient characteristics and technical aspects of the procedure associated with in-hospital repeat surgery. Previous studies have examined repeat surgery rates following hospital discharge, excluding repeat operations occurring during the index admission. However, trends in repeat spine surgery during the index hospitalization have not been reported. We are also interested in trends for repeat surgery for operations performed to treat degenerative disease, where patient and surgical discretion play a greater role in timing of surgery (ie, elective surgery) compared with operations performed to treat instability due to trauma, neoplasm, or infection (ie, nonelective). Therefore, we compared these trends for elective and nonelective lumbar fusion surgeries from 2004 to 2015. Materials and Methods: We used a validated coding algorithm to identify patients undergoing lumbar fusion surgeries from 2004 to 2015 in the National Inpatient Sample (NIS). Leveraging timing and procedure variables reported by participant hospitals, we compared trends for in-hospital repeat surgery rate for elective and nonelective lumbar fusion. We used survey-weighted generalized logistic regression to identify predictors for in-hospital repeat surgery, including patient age, sex, race, insurance, comorbidity, indication for surgery, use of fixation, multilevel fusion, and 360° fusion. We also examined interaction between surgical approach and year of surgery. Results: In 2015, the adjusted in-hospital repeat spine surgery rate for nonelective lumbar fusion was almost 4.3 times higher than elective fusion (15% vs 3.5%). Both rates nearly doubled from 2004 to 2015. Rate for nonelective lumbar fusion increased from 7.9% in 2004 to 13.4% in 2015 (P < .001). Rate for elective lumbar fusion increased from 1.8% in 2004 to 3.2% in 2015 (P < .001). Multilevel fusion and 360° fusion were associated with increased risk of in-hospital repeat surgery in elective lumbar fusion (odds ratio [OR] 1.94; 95% confidence interval [CI] 1.86-2.04; P < .001), but not for nonelective fusion. Repeat surgery risk for elective 360° fusion compared with posterior-only fusion increased 3.6-fold between 2004 (OR 1.75; 95% CI 1.45-2.12; P < .001) and 2015 (OR 6.23; 95% CI 5.45-7.13; P < .001). Cost of admission for patients who had an in-hospital repeat surgery increased by 125% for elective lumbar fusion ($111 792 vs $49 780) and 78% for nonelective lumbar fusion ($102 435 vs $57 379). Conclusion: Rate of in-hospital repeat surgery increased for both elective and nonelective lumbar fusion from 2004 to 2015. Increase in the rate for elective surgery was largely due to greater use of multilevel fusion and 360° fusion. In-hospital repeat surgery substantially increased the cost of admission.
P260: To Fuse or Not to Fuse: A 17-Year Spondylolisthesis Review
Natasha Greene1, Chase Grover1, William Ryan Spiker1, Ashley Neese1, Brandon Lawrence1, Darrel Brodke1, and Nicholas Spina1
1University of Utah, Salt Lake City, UT, USA
Introduction: Several recent publications have questioned lumbar fusion over decompression alone as the gold standard in the treatment of lumbar spondylolisthesis. Proponents of fusion, while being more invasive, argue for a more enduring solution by providing stabilization and limiting recurrent stenosis at the treated level. Conversely, isolated decompressions achieve the same neurologic relief without limiting motion, potentially reducing the rate of adjacent segment disease. Historically, decompressions have exhibited a higher revision rate, often necessitating fusion. However, decompression techniques become continually more sophisticated and potentially less destructive, influencing these outcomes. A clear consensus is currently lacking in the optimal treatment of patients with degenerative lumbar spondylolisthesis. Therefore, this study provides an updated analysis of demographic and revision trends in the surgical decision-making of spondylolisthesis. Materials and Methods: A retrospective, single-center review of all patients undergoing single- and 2-level laminectomies from 2000 to 2017 was performed to identify those who were being treated for spondylolisthesis. Of that cohort, patients were categorized into decompression surgeries with or without the addition of a fusion. Revision surgeries were recorded, and demographic information was obtained, including age, gender, smoking status, BMI (body mass index), and Charlson Comorbidity Index (CCI). Chi-square comparisons and 2-sample t tests were performed to identify trends in the patient cohort according to initial treatment type. Results: A total of 1829 patients underwent a single- or 2-level laminectomy in the study period. Preoperative radiographs were reviewed to identify 612 patients with spondylolisthesis, meeting our inclusion criteria. Two thirds of spondylolisthesis patients underwent a decompression with the addition of a fusion, while the remaining third were treated with a decompression alone. The mean age of fusion patients (60.6) was significantly younger than the mean age of independent decompression patients (69.4; P = .000). No significant trends were recorded between fusion and nonfusion patients in relation to smoking status, BMI, and CCI. Female patients were significantly more likely to be treated with the addition of a fusion over decompression alone than male patients (P = .001). The revision rates for decompression alone and decompression with fusion are 15.53% and 10.67%, respectively (P = .084). Conclusion: Demographically, patients who are treated for spondylolisthesis with a laminectomy and fusion are significantly younger than the population of patients treated with decompression alone. This suggests that age is an important consideration in the invasive nature of a treatment plan. Furthermore, a significant preference for fusion was seen in females compared with a more normal distribution in males. This may indicate a greater likelihood for females to present with unstable spondylolisthesis, a commonly accepted indication for lumbar fusion. A strong trend toward higher revision rates was seen in decompression alone, consistent with historical literature; however, our results may be influenced by the progression of decompression techniques over the study period. Further study is needed to better characterize the factors influencing surgical failures in both fusion and isolated decompression patients.
P261: Lumbar Canal Stenosis Clinico Radiological Analysis: A Prospective Study
Nikhil Jain1, Shankar Acharya1, Mukesh Haritwal1, Kashmiri Lal Kalra1, Rupinder Singh Chahal1, and Manoj Kumar1
1Sir Ganga Ram Hospital, New Delhi, India
Introduction: Although spinal canal narrowing is thought to be the defining feature for clinical diagnosis of lumbar canal stenosis, the degree of spinal canal stenosis necessary to elicit neurologic symptoms is not clear. Several studies have been performed to detect an association between narrow spinal canal and clinical symptoms. Here through our prospective comparative study, we aim to compare the radiological criterion with clinical criterion and assess if they can reliably predict the severity of symptoms clinically in lumbar canal stenosis patients. Material and Methods: We have used the Qualitative Grading (morphological classification system on MRI [magnetic resonance imaging]) system, dural sac cross-sectional area (DSCA) and sedimentation sign on MRI images and compared them with the Self-Paced Walking Ability (Self-Paced Walking Test) and Oswestry Disability Index (ODI) of the patients included in the study. The systems were applied to 85 patients divided into 3 groups: group A: 43 patients with neurogenic claudication, and able to walk less than 30 minutes, group B: 11 patients with neurogenic claudication and able to walk more than 30 minutes, and group C: 31 patients with simple back pain and no signs of neurologic claudication. DSCA has been calculated using SURGIMAP. Results: The mean ODI of patients was 21.19 in group C, 46.50 in group B, and 61.95 in group A. The difference was statistically significant. The mean DSCA was 164.42 mm2 in group C, 49.94 mm2 in group B and 35.07 mm2 in group A. The difference was statistically significant. The sedimentation sign was negative in 96.8% patients of group C, 54.5% patients in group B, and 32.6% patients group A. The difference was statistically significant. Group C had 9.3% patients in morphology grade A3, 51.6% in grade A2, and 38.7% patients in grade A1. Group B had 63.6% patients in grade C, 18.2% patients in grade B, 9.1% in grade A4, and 9.1% in grade A3. Group A had 18.6% patients in grade D, 39.5% in grade C, 27.9% in grade B, 11.6% in grade A4, and 2.3% in grade A3. The mean DSCA of group C was significantly different from group A and group B, but the difference of mean DSCA between group A and group B was not statistically significant. The relationship of ODI to DSCA, ODI to sedimentation sign and ODI to morphologic grading for group C and group A was not statistically significant. The relationship of morphologic grading to DSCA was statistically significant for all 3 groups (A, B, and C). Conclusion: Morphologic grading is a better radiological indicator for assessing the DSCA and the radiological severity does not correlate to ODI. Hence, we conclude that, we cannot reliably assess the severity of clinical symptoms using radiological parameters only, or, maybe ODI is not a very good indicator of clinical severity in lumbar spinal stenosis.
P262: Radiographic and Clinical Outcomes of Posterior Interbody Fusion for High-Grade Spondylolisthesis
Sung Kyu Kim1, and So Hyun Moon2
1Chonnam National University Hospital, Gwangju, Republic of Korea
2Chosun University, Gwangju, Republic of Korea
Introduction: The surgical treatment of high-grade spondylolisthesis has been controversial. However, few reports on the results of reduction and posterior interbody fusion after posterior decompression have been published. The purpose of this study was to evaluate the clinical and radiological outcomes of posterior interbody fusion using pedicle screw fixation after posterior decompression for high-grade spondylolisthesis. Materials and Methods: Thirteen patients with L5-S1 high-grade spondylolisthesis (Meyerding grade III, IV) who underwent reduction and posterior interbody fusion were analyzed with at least 2 years of follow-up. The mean age of the patients (male 2, female 11) was 51 years. Classified by the type of spondylolisthesis, 10 cases were isthmic, 2 cases dysplastic, and 1 case degenerative. A visual analogue scale (VAS), the Oswestry Disability Index (ODI) score, bone union, anterior slippage, and slip angle were used in comparing clinical and radiographic outcomes. Results: All cases showed improvement of preoperative symptoms. The VAS and ODI score improved from a mean of 8.9 points and 36.2 points preoperatively to 2.1 points and 10.2 points, respectively, at last follow-up. The degree of anterior slippage measured by Taillard’s method was improved from a mean of 57.7% before surgery to mean of 14.6% at last follow-up. The slip angle also changed from a mean of 2.4° kyphosis before surgery to a mean of 7.6° lordosis at last follow-up. There were 2 complications: infection and new radiating pain. Conclusions: Reduction and posterior interbody fusion using pedicle screw fixation after posterior decompression was a useful surgical method for high-grade spondylolisthesis that corrected lumbosacral kyphosis, filled the structural space of the anterior column, and achieved fusion of interbody movement.
P263: Union Rate Between Autogenous Iliac Bone Graft and Local Bone Graft in Lumbar Spine Fusion: Evaluation up to 3-Level Fusion
Dong-Gune Chang1, Se-Il Suk1, Jin-Hyok Kim2, Ki-Youl Nam1, Kang-Un Kim1, Jae Hyuk Yang3, Seung-Woo Suh3, Kwang-Sup Song4, Jong-Beom Park5, and Jung-Hee Lee6
1Inje University Sanggye Paik Hospital, Seoul, Republic of Korea
2CM Hospital, Seoul, Republic of Korea
3Korea University Guro-Hospital, Seoul, Republic of Korea
4Chung-Ang University Hospital, Seoul, Republic of Korea
5Uijeongbu St Mary’s Hospital, Uijeongbu, Republic of Korea
6Kyung Hee University Hospital, Seoul, Republic of Korea
Introduction: Solid bone fusion is primary goal of all fusion procedures for lumbar spinal disease. Autologous iliac crest bone graft (ICBG) has been considered the gold standard for fusion methods. However, there were no studies comparing the union rates of ICBG and local bone graft in lumbar fusion up to 3-level. Therefore, this study aimed to compare the radiologic union rate and incidence of perioperative complication rate between ICBG group and local bone group in 1- to 3-level lumbar spine fusion. Materials and Methods: We retrospectively examined 158 consecutive patients who underwent 1- to 3- level lumbar spine fusion surgery due to lumbar spinal stenosis from January 2008 to December 2013. Patients were divided into 2 groups based on the ICBG group (86 patients) and the local bone graft group (72 patients). Circumferential lumbar spine fusion that simultaneous anterior and posterior fusion was performed in all patients. Fusion status of anterior or posterior segments were evaluated by the anteroposterior (AP) and lateral plain radiographies obtained at 24 months postoperatively. If at least either anterior or posterior segment were fused, that segment was regarded as achieved fusion, and was termed “combined segment union.” The definition of over-all union was when the combined segment union was observed in all surgical segments in one patient. Results: For each ICBG group and local bone graft group, 1-level fusion was performed in 33 and 39 patients, 2-level fusion in 32 and 24 patients, and 3-level fusion in 21 and 9 patients. Fusion rate of anterior and posterior segments and union rate of combined segments and over-all patients at postoperative 2 years were not different between ICBG group and the local bone group in 1-level, 2-level, and 3-level surgery. In the ICBG group, there was little difference in over-all fusion rate according to the fusion level (96.9%, 96.9%, and 95.2% for 1-, 2-, 3-level fusion, respectively, and P = .746, .640, .631 in 1-2, 2-3, and 3-1 level, respectively) but in the local bone graft group, the over-all fusion rate tended to decrease gradually as the fusion level increased (100%, 95.8%, and 88.9%) for 1-, 2-, 3-level fusion, respectively) without any statistically significant differences (P = .381, .477, .188 in 1-2, 2-3, and 3-1 level, respectively). Conclusions: Local bone graft showed comparable union rate to autogenous iliac bone graft even in 3-level lumbar fusion surgery. Union rate of 3-level fusion was not inferior to 1- or 2-level fusion in both ICBG and local bone graft. Local bone graft could be regarded as an adequate option for not only 1- or 2-level lumbar fusion but also 3-level surgery.
P264: Modification of Bohlman’S Technique for High-Grade L5-S1 Spondylolisthesis: Report of Two Cases
Javier Matta1, Daniel Macias1, Victor Arrieta1, and Juan Guevara1
1Hospital Militar Central, Bogotá, Colombia
Introduction: Spondylolisthesis is the anterior translation of a vertebra in relation to the caudal one. High-grade spondylolisthesis (HGS) has been described as a translation of more than 50% over the inferior vertebra, and it is argued that even for expert spine surgeons the management of HGS is a challenge because of the significant risk of neurologic deficit, hardware failure, nonunions, and progression of the slippage. Different options for treatment have been published including in situ posterior fusion without instrumentation, posterior instrumentation, circumferential fusion, even vertebral resection; nevertheless, the surgical management is still controversial. In 1982, Bohlman presented a technique that consisted of a trans-sacral fusion following lumbosacral laminectomy, a fibular autograft was passed from posterior to anterior through the body of S1 into the body of L5 without instrumentation, obtaining an anterior and posterolateral fusion with an appropriate decompression in 1-stage surgery. The motivation to modify this technique was the report in some journals of the fracture or resorption of the fibular graft and pseudoarthrosis; in addition, at that time, the spine-pelvic parameters were not taken in account in the management of HGS. We present a modification of Bohlman’s procedure for high-grade L5-S1 spondylolisthesis. Material and Methods: A modification of Bohlman’s technique has been used as a surgical option for HGS of L5-S1 segment. Two patients operated with this procedure has been assessed. Age, Labelle classification, pre- and postoperative low back pain, neurological symptoms, slip %, fusion, and complications were analyzed. Surgical technique: with general anesthesia, in prone position, under multimodal-evoked potentials, and fluoroscopic control, standard midline posterior approach from L5 to S2, subperiosteal dissection until transverse processes, decompression is achieved with bilateral laminectomy of S1 then partial reduction correcting lumbosacral kyphosis is done with bilateral instrumentation of L5 and S1 (this fixation must be done with Schanz pins or pedicle screw with reduction extensions). Two guides are placed 1 cm lateral, between nerve roots of S1 and S2, through S1 toward L5 vertebral. Then, a perforation of 8 mm is made with a cannulated drill, 2 titanium meshes filled with bone graft are positioned to archived a trans-disk fusion of L5-S1. Finally, we add graft to the transverse processes to obtain a circumferential fusion (anterior and posterolateral). LSO was indicated until radiological fusion. Results: Two male patients with HGS were treated with this modified technique, both had low back pain and 1 had right L5 radiculopathy. One had a slip percentage of 60% and the other one of 90%. Labelle classification were type 4 and type 5, respectively. Both patients improved the lumbosacral kyphosis after surgery from 14° to 8° and 35° to 15°. There were no complications during the surgery. After 3 years follow-up, both patients had a tomographic circumferential fusion with no back pain nor radiculopathy. Conclusion: In conclusion, HGS is a disabling degenerative disease, one of the most challenging spine deformities. Therefore, we suggest a modification of Bohlman’s technique for the treatment of HGS of L5-S1.
P265: Clinical Study of Stand-Alone Anterolateral Lumbar Interbody Fusion for Degenerative Spondylolisthesis Based on Sagittal Classification
Yawei Li1, Bing Wang1 and Guohua Lv1
1The Second Xiangya Hospital of Central South University, Changsha, China
Introduction: Lumbar degenerative spondylolisthesis (DS) is a common, acquired condition leading to disabling back and/or leg pain. Although surgery is common to treat patients with severe symptoms, there are no universally-accepted treatment guidelines. In this study, for the first time, stand-alone anterolateral lumbar interbody fusion (ALLIF) for lumbar DS based on a novel sagittal morphology classification was reported. Materials and Methods: A total of 37 patients (females/males: 22/15) with the average age 54.5 ± 8.5 years who underwent stand-alone ALLIF at L4/5 level between January 2014 and October 2016 were enrolled in our study. All patients were assigned to 3 groups according to slipping angle (SA): group A, opened type with SA > 5°; group B, parallel type with −5° ≤ SA ≤ 5°; and Group C, closed type with SA < −5°. The measurement of spinopelvic parameters including lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS) and sagittal vertical axis (SVA), and VAS (visual analogue scale) for low back and leg pain, ODI (Oswestry Disability Index) for functional disability, SF-36 for quality of life were recorded and analyzed. Results: All of them underwent operations successfully and were followed-up for 12 months at least. Thirty-seven patients were divided into 3 groups: group A (16 cases), group B (13 cases), and group C (8 cases). There were significant differences in preoperative PT, SS, and LL among the groups (P < .05), and closed type had the lowest LL and SS of all subtypes (P < .05), but no difference was found in PI and SVA (P > .05). At final follow-up, there were no significant changes in spinopelvic parameters in groups A and B compared with those before surgery (P > .05), while PT in group C decreased, and SS, LL increased postoperatively (P < .05). Back and leg pain VAS and ODI decreased (P < .001), and SF-36 increased postoperatively in each group (P < .001), and closed type had the highest mean back pain VAS, ODI, and SF (Short Form)-36 MCS (mental component summary) scores of all subtypes (P < .05). Conclusions: The novel sagittal morphology classification system represents a simple and reliable method for classifying cases of DS, and stand-alone ALLIF could achieve satisfactory short-term results, especially for closed type DS, could help to restore LL, and obtain a greater degree of improvement in multiple outcome measures following surgical intervention.
P266: Segmental Fusion and Formation of Outer Bone Bridge Following Lateral Lumbar Interbody Fusion in Multilevel Instrumented Spinal Surgery
Yu Moriguchi1, Hiroyasu Fujiwara1, Takenori Oda1, Shinichi Nakagawa1, Takashi Kaito2, and Hiroyuki Tsukazaki2
1National Hospital Organization Osaka Minami Medical Center, Kawachinagano, Japan
2Osaka University, Suita, Japan
Introduction: Lateral lumbar interbody fusion (LLIF) is an alternative to standard posterior approaches for achieving interbody arthrodesis in the spine. However, fusion status including formation of outer bone bridge noted as extra-cage bony connection on epiphyseal rings has not been well studied. In the present study, we investigated the LLIF fusion rate and incidence of outer bone bridge in comparison with posterior lumbar interbody fusion (PLIF) segments in the patients undergoing multilevel instrumented spinal surgery. Material and Methods: In 2013-2016, 30 patients with multilevel spinal canal stenosis and degenerative lumbar scoliosis underwent a 2-staged operation: LLIF for upper levels (a total of 64 segments ranging from L1/2 to L4/5) followed by PLIF for lower levels (32 from L2/3 to L5/S) and posterior instrumentation. Artificial interbody cages, iliac bone grafts, and collagen-based bone expanders were used for bone grafting. Data was collected on patient demographics, cage parameters, side of approach (convex or concave side of scoliosis), and bone metabolism-related factors such as T-score of bone density test, history of smoking, and presence of anabolic treatment for osteoporosis. Radiographic parameters including lumbar lordosis, Cobb angle, disc wedge angle of fusion segment, foraminal height, and disc height were measured preoperatively and postoperatively. A computed tomography (CT) analysis was performed at 6 and 12 months postoperatively to assess intra-cage fusion, formation of outer bone bridge (herein after referred to as extra-cage fusion), and segmental fusion defined as a state where at least 1 of the 2 was confirmed. Of the LLIF parameters measured, factors associated with at least a borderline significance (P < .2) in a univariate regression analysis were included in a multivariate regression analysis. Results: CT examination demonstrated an LLIF fusion rate (intra-cage/extra-cage/segmental) at 6 and 12 months of 67/28/75 and 82/42/88%, versus 81/28/81 and 91/30/91% in PLIF, respectively, although difference between LLIF and PLIF was not statistically significant in any of the 3 fusion rates. In the LLIF segments, both intra- and extra-cage fusion was better achieved on the concave side of scoliosis (63% and 42%) than the convex side (38% and 11%) at 12 months (P = .02). Multivariate analysis of LLIF segments demonstrated that only absence of smoking was positively associated with fusion rate at 12 months (OR [odds ratio], 4.9; 95%CI, 1.1-21.7; P = .04). Conclusion: Fusion rate of LLIF segments was equivalent to that of PLIF, especially when outer bone bridge was taken into consideration. Fusion, whether it is intra- or extra-cage, was better achieved on the concave side of scoliosis, and this can influence the decision on where to place autologous bone when its amount was limited.
P267: Predictive Factors of Favorable Outcome in Posterior Lumbar Decompression in the Mexican Patient
Crisanto Mora1, Amado Gonzalez1, Enrique Guzman1, Gabriel Huerta1, Miguel Fuentes1, Hugo Santos2, Henry Vergara1, and Jeancarlo Arreola1
1ISSEMYM Medical Center, Ecatepec, Mexico
2Unidad de Neurocirugía Cerebral y Vertebral, Madrid, Spain
Introduction: There are few prospective studies that deliver data about the long-term results of the decompressive laminectomy in the degenerative lumbar stenosis (DLS). On the other hand, the predictive factors that influence the long-term results are contradictory and little studied in the literature. The study of these criteria is a key issue to determine the best time to propose surgical treatment. The objective of our study was to evaluate the long-term functional outcome of patients undergoing decompressive laminectomy with a diagnosis of DLS and to determine the predictive factors of a favorable outcome. Material and Methods: A retrospective study with follow-up of 98 patients evaluated during 5 years after a surgical decompression procedure of DLS. The final point was the evaluation of the Beaujon score increased by at least 5 points between the preoperative stage and the follow-up assessment. The logistic regression was performed with a univariate and multivariate analysis to reveal the predictive factors of a favorable long-term outcome (P ≤ .05). Results: The preoperative characteristic of our population (n = 98) was an average age of 67.3 ± 8.8 years, a low comorbidity (average of the Charlson score = 2.8 ± 1.5), and overweight (BMI [body mass index] = 29.4 ± 6.3 kg/m2), and the average of the Beaujon score was 9.3 ± 3.1. Five years after surgery, the average Beaujon score increased to 14.1 ± 4.2. A favorable functional result corresponds to 45.9% of our series. The predictive factor of favorable functional outcome identified in the univariate analysis was the neurological deficit (P ≥ .05) and in the multivariate analysis was low comorbidity (P ≥ .01). Conclusion: Our study shows that surgical treatment of lumbar spinal stenosis improved by 49.5% at 5 years. The only independent predictor of long-term improvement reveals that comorbidity can significantly limit the quality of the expected functional outcome and should be taken into account when choosing the therapeutic orientation. The Beaujon score appears as a useful tool in the preoperative evaluation. The outbreak of a neurological deficit and a Beaujon score below 11 during the natural evolution of degenerative lumbar stenosis is the appropriate threshold to obtain optimal long-term results.
P268: Lumbar Lordosis Correction With EIT Transforaminal Lumbar Interbody Fusion Cage: Retrospective Single Center Data Analysis
Anneli Duits1, and Steven van Gaalen2
1Diakonessenhuis Utrecht, Utrecht, Netherlands
2ACIBADEM International Medical Center, Amsterdam, Netherlands
Introduction: Recently, the importance of a normal sagittal alignment has come into the limelight. Previous literature suggests that restoring optimal lumbar alignment is associated with reduced surgical pain, reduced adjacent segment disease, and reduced revision rates. The Emerging Implant Technologies (EIT) TLIF (transforaminal lumbar interbody fusion) cage is a titanium-vanadium-aluminum cage. The porous structure of this cage is hypothesized to improve outcomes compared with conventional cages. Indeed, this cage showed promising results in the cervical spine with good clinical outcomes, good primary stability and early osseointegration. However, little is known about its ability to correct lumbar lordosis. This study is a retrospective cohort aimed to examine the improvement in monosegmental lordosis after TLIF surgery performed with the EIT TLIF cage. Material and Methods: From January 2014 until May 2018, a total of 61 patients with degenerative lumbar disease underwent 1-level TLIF surgery at L4-5 or L5-S1 and received either an EIT TLIF cage or a T-pal cage. All patients were operated in the same hospital by the same orthopedic surgeon. Patients were divided into 2 groups based on the cage used. The T-pal cage was selected as a control, as this cage has a similar design to the EIT TLIF cage, although it should be noted that the lordotic angle differs. (T-pal 5°, EIT TLIF 8° to 9°) 34 patients received a T-pal cage and 27 patients received an EIT TLIF cage. The preoperative and 4 to 6 weeks postoperative lumbar lordosis (LL) and fused segment lordosis (FSL) were measured on X-ray. Results: Mean age in the T-pal group was 56.4 ± 12.7 years and 56,9 ± 12.2 years in the EIT TLIF group. There was no statistically significant difference between the groups in pelvic incidence, preoperative segmental lordosis or preoperative LL (measured between L4-S1). In the EIT TLIF group, a statistically significant increase in FSL correction was seen compared with the T-pal Group. In the T-pal group, the mean correction of FSL was 0.94 ± 4.80°, in the EIT TLIF group the FSL correction was 4.13 ± 4.58 (P = .0076). In the T-pal group the median correction of LL was 0.00, interquartile range (IQR) 6-30°, in the EIT TLIF group the median LL correction was 1.05 and IQR 6° to 80°. However, this difference was not statistically significant. Subsidence of the cage was seen in 5 patients in both groups. Conclusion: The study shows that both cages promote LL correction. The higher degree of FSL correction of the EIT TLIF cage indicates that the EIT TLIF should be considered when performing TLIF surgery.
P269: The Efficacy of Intraoperative Multimodal Monitoring in Pedicle Subtraction Osteotomies of the Lumbar Spine
Jianning Shao1, Maxwell Lee1, Shreya Louis1, Konrad Knusel2, Bryan Lee3, Dominic Pelle4, Jason Savage3, Joseph Tanenbuam2, Thomas Mroz3, and Michael Steinmetz3
1Cleveland Clinic Lerner College of Medicine, Cleveland, OH, USA
2Case Western Reserve University, Cleveland, OH, USA
3Cleveland Clinic, Cleveland, OH, USA
Introduction: Iatrogenic spine injury remains one of the most dreaded complications of spine deformity surgeries such as pedicle subtraction osteotomy (PSO), the treatment of choice for correction of global sagittal imbalance. As such, intraoperative multimodal monitoring (IOM), which has the potential to provide real-time feedback regarding cord integrity, has become the gold standard in such operations. However, despite the widespread usage of IOM, there is currently no standardization of IOM usage in complex spine surgeries, including lumbar PSOs, and decisions concerning IOM utilization are often driven by surgeon experience and preference. This clinical picture is further complicated by the apparent dependence of IOM efficacy on the spinal levels involved. Indeed, while the benefits of IOM are well established in PSOs of the thoracic spine, its utility in PSOs of the lumbar spine has not been robustly documented. Since PSOs of the lumbar spine are among the most commonly performed spine deformity surgeries, it is imperative to elucidate the efficacy of IOM in PSOs of the lumbar spine. Methods: All patients above the age of 18 years who underwent lumbar PSOs at our institution from 2007 to 2017 were analyzed via retrospective chart review. Patients were categorized into 1 of 2 groups: those who underwent the operation with IOM guidance and those who underwent the operation without IOM guidance. PDQ (Parkinson’s Disease Questionnaire)-39 quality of life (QOL) scores were gathered for each patient and multivariate analysis was preformed to compare the QOL scores between the 2 patient groups. In addition, the proportion of patients who reached minimal clinically important difference (MCID), defined as an increase in PDQ-39 score of 4.72, in the 2 patient groups was also determined, and statistical analysis was preformed to determine whether IOM had a statistically significant impact on achieving MCID. Results: A total of 101 patients were included in the final analysis. Multivariate analysis shows that parameters with a statistically significant impact on achieving MCID included age (odds ratio [OR] = 1.11, P = .001) and female sex (OR = 7.6, P = .005). Importantly, IOM usage was not correlated with a statistically significant increase in QOL scores (P = .230) or achievement of MCID 3 months after surgery (P = .196). Conclusions: In our particular cohort, IOM did not lead to statistically significant improvement in outcomes in patients undergoing PSOs of the lumbar spine (P = .230). However, it is worthwhile to note that while statistical significance was no shown in this particular study, IOM is rapidly becoming the standard of care, and can be considered worthwhile if it prevents even one iatrogenic injury. The existing clinical equipoise, however, indicates future studies in this arena are necessary to achieve systematic guidelines on IOM usage in PSOs of the lumbar spine.
P270: The Safety of Lumbar Spinal Fusion Surgery for Degenerative Spondylolisthesis in Older Patients
Jetan Badhiwala1, Brij Karmur1, Laureen Hachem1, Jamie Wilson1, Christopher Witiw1, Farshad Nassiri1, Michael Fehlings1, and Jefferson Wilson1
1University of Toronto, Toronto, Ontario, Canada
Introduction: Degenerative spondylolisthesis (DS) is often treated with lumbar spinal fusion (LSF). However, because physiological reserves diminish with age, older adults may have a poorer tolerance for extensive surgical procedures requiring prolonged anesthetic time. Treatment decision paradigms in the elderly must therefore factor in the potential added risk of surgical interventions. Using a large administrative health care dataset, we sought to evaluate the impact of advanced age on the safety of LSF for DS. Materials and Methods: Patients who underwent LSF for DS (ICD-9-CM 738.4) were identified from the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) datasets for years 2011 through 2015 using standard CPT (Current Procedural Terminology) codes. Data relating to demographic characteristics, comorbidities, surgical factors, and morbidity and mortality were collected. Propensity score matching (nearest neighbor) was performed in a 1-to-1 ratio with age (<70 years vs ≥70 years) as the treatment indicator and sex, type of fusion procedure, number of levels fused, diabetes, smoking, hypertension, and chronic steroid use as covariates. Outcomes were compared between age <70 years and age ≥70 years groups. Outcomes evaluated were 30-day complications, including wound infection/breakdown, pneumonia, venous thromboembolism (VTE; ie, DVT [deep vein thrombosis], PE [pulmonary embolism]), prolonged intubation or reintubation, urinary tract infection (UTI), cardiac event (myocardial infarction [MI] or cardiac arrest), blood transfusion, sepsis, reoperation and readmission related to the principal operative procedure, and mortality, as well as discharge destination and length of hospital stay (days). Results: The study cohort consisted of 2238 patients, with 1,119 patients aged less than 70 years and 1119 patients 70 years or older. The mean age was 67.0 ± 11.0 years. The 2 age groups were balanced for key covariates including sex, race, diabetes, hypertension, CHF (congestive heart failure), smoking, chronic steroid use, type of fusion, and number of levels. The older age group (≥70 years) had similar length of stay (mean 3.7 days vs 3.5 days) and rates of wound infection (1.6% vs 2.1%), pneumonia (0.9% vs 0.8%), VTE (0.8%vs 1.2), intubation (0.4% vs 0.4%), renal failure (0.3% vs 0.09), cardiac event (0.4% vs 0.2%), blood transfusion (14.4% vs 13.1%), stroke (0.2% vs 0.09%), sepsis (0.6% vs 0.7%), reoperation (2.4% vs 2.7%), readmission (4.3% vs 3.0%), and mortality (0.18% vs 0%) as the younger age group (<70 years). However, UTI’s were more frequent in the older age group (odds ratio [OR] 2.32, 95% confidence interval [CI] 1.23 to 4.38, P < .01). There were also significant differences between the 2 groups with regard to discharge destination—more patients in the ≥70 years group were discharged to a rehabilitation (OR 2.94, 95%CI 2.16-4.01, P < .01) or skilled care (OR 3.66, 95% CI 2.77-4.84, P < .01) facility than in the <70 years group. Conclusions: Perioperative complication rates after spinal fusion for DS are comparable between young and elderly patients. LSF may therefore be performed safely in older adults with DS. When establishing treatment decision paradigms, older age alone should not exclude a patient from undergoing a lumbar fusion operation.
P271: Does Titanium Coating Affect Fusion Ratio of Lumbar Interbody Fusion With PEEK Cage?
Ushio Nosaka1, Kandi Sasaki1, Mizuki Watanabe1, Toshiaki Hitora1, and Tetsutaro Mizuno1
1Seireihamamatsu General Hospital, Hamamatsu Shizuoka, Japan
Introduction: The aim of interbody fusion is the fixation of lined vertebrae. One of a “true” rapid surgery is fast bone ingrowth and fusion of lumbar interbody. On the other hand, many factors (eg, ages, sex, comorbidity alignment, bone quality, surgical technique etc) are related to bone ingrowth and fusion, but there is not so much what we can surgically interfere. From the view of surgical devices, progress of the material is still now advancing and considers affecting bone ingrowth. Now, we are able to use titanium-coated polyetheretherketone (PEEK)cage, which has the characteristic of the elasticity of PEEK and biocompatibility of titanium. The chief aim of this study is to reveal whether the material affect the rapid bone ingrowth of lumbar interbody fusion or not. Material and Methods: This study included 52 cases. All cases are single-level interbody fusion, and performed by oblique lateral lumbar interbody fusion (OLIF). Twenty-six cases were enrolled to PEEK cage group (group P; mean age 63.7 years, males:females 11:15), and 26 cases were assigned to PEEK cage coated by titanium (group T; mean age 69.1 years, males:females 20:6). In all cases, the cage was fulfilled by the autograft of iliac bone and the hydroxyapatite/collagen soaked into the bone marrow. For aftercare, nobody used hard/soft corset. Three months after the surgery, we evaluated the interbody bone fusion by the sagittal and coronal view of computed tomography. Fusion completed or not is defined by means of bone cross-linking between the endplate in the cage. One year after the surgery, instability was checked by X-ray, and over 5° gap by flexion and extension in the lateral view is defined as instability. We evaluated by multivariate analysis the correlation between the fusion rate and the spinal alignment (sagittal vertical axis [SVA], lumbar lordosis [LL], sacral slope [SS]). Results: Bone fusion was confirmed in 12 cases (46%) of group P, and 19 cases (73%) of group T. Group T has significantly higher fusion rate than group P. Multivariate analysis revealed that only no-coated and male are significant risk factors about the delayed bone fusion. After 1-year, there is no significant difference of instability in these groups. These results suggest that materials affect rapid bone union, but finally there are few effects for the instability or fusion. Conclusion: Noncoating PEEK and male is statistic risk factor of delayed bone fusion in the lateral access lumbar interbody fusion. Effect of titanium coating is powerful for early phase lumbar interbody fusion. To use titanium coating cages is ideal surgical device for interbody fusion.
P272: Multilevel Stenosis and Deformity of Spine: When Is Only a Microsurgical Approach Indicated?
Dmitry Dzukaev1, Vladimir Gulyy1, Anton Borzenkov1, and Aleksander Pejker1
1Moscow Spine Center, Moscow, Russian Federation
Introduction: Among a large range of patients with multilevel stenosis and deformity of spine not everyone needs complicated operation with multilevel instrumentation. The aim of the study was to work out an algorithm of preoperative examination of patients with spine deformity and multilevel canal stenosis, which gave an ability to pick up the patients with indications for microsurgical approach. Material and Methods: During the period between 2014 and 2017, our research had collected 152 patients with multilevel lumbar stenosis and spine deformity. Fifty-eight out of 152 patients were operated with minimally invasive approach without instrumentation. The patients of this group (58 persons) were selected according to the following criteria: (1) Acute deterioration took place suddenly in the period from 1 week to 2 to 3 months before entrance to our spinal center against the background of satisfying live quality before. (2) One or 2 nerve roots got a compression, according to the clinical examination. These measurements were approved clinically and radiologically. (3) Patients’ selection for microsurgery was performed with the preoperative examination and MRI (magnetic resonance imaging) assessment algorithm. The research was provided by MR tomography 1.5 T. The protocol included diagonal slices (slice’s thickness 1-3 mm), which had been conducted through each stenosis level. After MRI data had been received, the detail assessment of nerve root condition (its route, diameter, edema signs) and the degree of compressive factors influence was performed. Also, multispiral CT (computed tomography) and functional radiographs data of these patients confirmed stable character of deformity. In all the patients nerve root microsurgery decompression by minimally invasive approach was performed. In each case, instrumentation was not used. Results: The usage of the preoperative examination and MRI assessment algorithm allowed to pick 58 patients with multilevel stenosis that had indications only for microsurgery out of 152 patients with expressed degenerative spine lesion. All the patients of microsurgery group got rid of pain immediately and had persistent effect during all the observation period, which was between 1 and 3.5 years. Conclusion: Correct interpretation of present clinical data, disease development also as the usage of the preoperative examination and MRI assessment algorithm allows to emphasize irritated nerve root, causing low patients live quality, against the background of multilevel stenosis. Establishing of precise lesion localization gives an opportunity for microsurgery, therefore, it rids a patient of aggressive operation, decreases X-ray dose, reduces instrumentation expenses, and lessens postoperative rehabilitation period.
P273: Bladder Recovery Patterns in Complete Cauda Equina Syndrome Patients? A Single Center Study
Karthik Yelamarthy1, Tarush Rustagi1, Rajat Mahajan1, Kalidutta Das1, and Harvinder Chhabra1
1Ohio State University, Columbus, OH, USA
Introduction: Cauda equina syndrome (CES) is associated with etiologies including lumbar disc herniation (LDH) and lumbar canal stenosis (LCS). CES has 2% prevalence among LDH and has variable outcomes even with early surgery. Literature is scant regarding factors influencing bladder outcome prognosis. The aim of our study was to look at the factors contributing to bladder recovery and propose a simplified bladder recovery classification. Overview of Literature: There are only a few reports mentioning the prognostic clinical factors for bladder recovery following CES. There is also dearth of any meaningful bladder recovery status classification that is useful in an office setting by the clinicians. Methods: A single-center retrospective study was conducted (April 2012-2015). CES secondary to LDH or LCS were included. The retrieved data were evaluated for variables including demographics, symptom duration, presenting neurology, bladder symptoms, and timing of surgery. Resultant variable bladder function at the time of discharge and at later follow-up were noted. Minimum 2 years follow-up was taken in the study. A simplified bladder recovery classification is proposed. Statistical analysis was done to study the correlation between patient variables and bladder function outcome. Results: A total of 39 patients were included in the study. Men (79.8%) with average age of 44.4 years secondary to LDH was the most commonly involved group. Perianal sensation (PAS) had statistical correlation with neurological recovery. With absent PAS, there was no recovery in bladder function (100%). Voluntary anal contraction (VAC) was affected in all the patients. Conclusion: Intactness of perianal sensation was the only significant prognostic variable. Decreased or absent voluntary anal contraction was most sensitive for diagnosis of CES. We also proposed a simplified bladder recovery classification for recovery prognosis.
P274: Differential Surgical Treatment of Lumbar Spinal Stenosis in Elderly Patients
Ivan Vasilenko1, Klimov Vladimir1, and Roman Khalepa1
1Federal Neurosurgical Center, Novosibirsk, Russian Federation
Introduction: Lumbar spinal stenosis is the most common cause of spinal surgery in elderly patients. The aims of surgical treatment of older patients with spinal stenosis are elimination of the backpain, leg pain, increase of the walking distance, and improvement in the quality of life. There are 2 surgical options for treatment of lumbar spinal stenosis but indications for decompression alone and decompression with fusion remain controversial. Material and Methods: A total of 107 patients aged 60 to 85 years with symptomatic spinal stenosis underwent bilateral over the top decompression with fusion (N = 52) and bilateral over the top decompression alone (N = 55). Standard scales and questionnaires were used to objectify and standardize the clinical manifestations of the disease: walking distance in meters, visual analogue scale (VAS) back or leg pain, Oswestry Disability Index (ODI), Short Form–36 (SF-36). MRI (magnetic resonance imaging) and computed tomography (CT) were used to determine the parameters of the spinal canal: the cross-sectional area of the dural sac, the cross-sectional size of the spinal canal, the dural sac, the sagittal size of the spinal canal, dural sac, and the interfacet distance. Indication for decompression alone was spinal stenosis without segmental instability (less than 5 points of White-Panjabi criteria). Indication for fusion was spinal stenosis with segmental instability (5 or more points of White-Panjabi criteria). Clinical outcome defined during 24 months after surgery by VAS, ODI and SF-36 questionnaires. Results: After the surgery, the leg pain, back pain (VAS), disability (ODI), and quality of life (SF-36), walking distance were significantly improved (P < .001). According to the CT after the surgery, there was significantly increase in the dimensions of the spinal canal (P < .001). When comparing the results of decompression alone and decompressive-fusion surgery, it was established that the indices of back and leg pain, quality of life in group 1 are somewhat better; however, the statistical significance of this difference was confirmed only for the value of the MH (mental health) component of the SF-36 questionnaire (P = .03). The optimal value of the cross-sectional area of the dural sac obtained as a result of the decompression is 0.8 to 1.6 cm2, which is associated with the improvement in the quality of life according to ODI and SF-36 . Excessive increase of all parameters of the spinal canal leads to a deterioration in the quality of life. In the group of fusion complications were more frequent (21%) than in the group of decompression alone (9%). Conclusion: The use of differential surgical treatment for elderly patients with lumbar spinal stenosis, provides an improvement in the quality of life in 80% of cases. The cross-sectional area of the dural sac is the key parameter for assessing the adequacy of the decompression. Excessive decompression does not improve the quality of life of patients. Instrumental fusion for degenerative spinal stenosis does not improve the outcome of surgery and quality of life, but is associated with an increased risk of complications and should be used only in case of clinically significant instability of the motion segment unit.
P275: Cortical Bone Trajectory Screw Placement Accuracy With a Patient-Matched 3D-Printed Guide in Lumbar Spinal Surgery: A Clinical Study
Matteo Monticelli1, Nicola Marengo1, Marco Ajello1, Paolo Pacca1, Fabio Cofano1, Federica Penner1, Salvatore Petrone1, Francesco Zenga1, and Diego Garbossa1
1AOU Cittá della Salute e della Scienza, University of Turin, Turin, Italy
Introduction: Degenerative spine surgery requires effectiveness while causing less damage to the surrounding tissues especially with posterior approaches. Cortical bone trajectory (CBT) is an attractive technique in terms of both fixation strength and less invasiveness. However, to insert the screw penetrating cortical bone on the ideal trajectory is technically demanding. The use of 3-dimensional (3D) printed patient-matched guides may facilitate the use of this technique. In this technical note and case series the use of a patient-matched 3D targeting guide for a circumferential posterior fixation with CBT screws is described. Material and methods: Eleven patients with mean age of 47 years complaining low back pain with sciatalgic irradiation and with radiological images showing single-level lumbar disc herniations/central stenosis with disc degeneration underwent circumferential fixation surgery after failure of conservative treatments. The MySpine MC (Medacta International SA, Castel San Pietro, CH) technology was used to place CBT screws. A computed tomography (CT)–derived 3D model of the patient vertebra was created after the surgeons planned the best custom CBT screw trajectory. Then, scaffolds that fit exactly the vertebra surface were printed and used during surgery in order to guide the screw through the patient pedicle. An intersomatic arthrodesis with T-PAL (DePuy-Synthes GmbH Oberdorf CH) was also performed. Results: The images of the planned trajectory were superimposed on the axial and sagittal postoperative CT reconstruction confirming the accuracy of the actual trajectory. The mean deviation from the planned pedicle midpoint was 0.91 ± 0.71 mm and 85.2% of the screws were placed within 2° from the planned trajectory. There were 2 grade A (<2 mm) and no grade B or C perforations. The actual entry point was always within 2 mm from the planned. All the patients showed clinical improvement without new neurological deficits and where discharged 2 days after the procedure. Conclusion: This technical note and case series is, to the best of the authors’ knowledge, the first clinical description on the use of patient-matched guided for posterior CBT screw placement. The use of these devices for CBT fixation allows not only a customized planning, but could also improve placement accuracy and decrease the risk of nerve damage. Furthermore, the need of fluoroscopy could potentially be set down to zero.
P276: Comparison of Bone Ongrowth on the Lumbar Interbody Cage Surfaces Between Titanium-Coated PEEK and 3D-Printed Porous Titanium Alloy: In Vivo Analysis Using CT Color Mapping
Takahiro Makino1, Yusuke Sakai1, Shota Takenaka1, Hideki Yoshikawa1, and Takashi Kaito1
1Osaka University, Suita, Japan
Introduction: Polyetheretherketone (PEEK) is one of the most widely used cage materials. However, there has been recently concern that the lack of osteoconductivity and the hydrophobic nature of PEEK have negative impacts on the primary stability of PEEK cages. Thus, titanium-coated PEEK (TCP) or 3D-printed porous titanium alloy (PTA) cages have been developed for promoting osseointegration of implant surfaces. This study was aimed to reveal the differences of bone ongrowth on the surfaces of TCP and PTA cages after posterior lumbar interbody fusion (PLIF) using in vivo computed tomography (CT) color mapping. Material and Methods: Forty-one consecutive patients who underwent single- or 2-level PLIF since March 2015 were included. TCP cages were used in 24 patients until June 2017 (11 men and 13 women; median age, 71.0 years (interquartile range [IQR], 63.5-75.0 years); PTA cages in 17 patients after July 2017 (9 men and 8 women; median age, 68.0 years [IQR, 62.5-75.5 years]). Two cages were inserted in all PLIF segments. The Hounsfield unit (HU) values of instrumented vertebrae in preoperative CT scans were calculated for the assessment of bone quality.1 Bone ongrowth was evaluated on the surface of the frame constituting a lateral wall of each cage (4 surfaces per one cage) by CT color mapping from reconstructed sagittal planes of postoperative CT scans (within 1 week and 6 months postoperatively),2 and then scored (grade 0, without bone ongrowth; grade 1, 1%-33% of surface with bone ongrowth; grade 2, 34%-66%; Grade 3, 67%-100%). The obtained data was compared between the TCP cage group and PTA cage group. Results: In the TCP cage group, 17 patients underwent single-level PLIF and 7 patients underwent 2-level PLIF. In the PTA cage group, 13 patients underwent single-level PLIF and 4 patients underwent 2-level PLIF. Thus, 248 cage frame surfaces were evaluated in the TCP cage group; 168 cage frame surfaces in the PTA cage group. The age, sex distribution, body mass index (median [IQR], 23.4 [21.3-24.9] kg/m2 vs 24.7 [20.1-27.1] kg/m2), and HU values of instrumented vertebrae (median [IQR], 136.9 [117.3-238.8] HU vs 138.7 [126.9-191.9] HU) were not different between the groups. In the TCP cage group, 99 cage frame surfaces were judged as grade 0; 58 surfaces, grade 1; 49 surfaces, grade 2; and 42 surfaces, grade 3. In the PTA cage group, 34 cage frame surfaces were judged as grade 0; 58 surfaces, grade 1; 34 surfaces, grade 2; and 42 surfaces, grade 3. The grades of bone ongrowth were significantly higher in the PTA cage group than the TCP cage group (P < .001). Conclusion: Bone ongrowth was more likely to occur on the surfaces of the PTA cage frames than those of the TCP cage frames 6 months postoperatively. Because the elastic modulus was almost similar between the TCP and PTA cages, the difference of surface microstructure between the cages could affect the osseointegration of implant surfaces.
Reference
1. Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93:1057-1063. doi:10.2106/JBJS.J.00160
2. Makino T, Kaito T, Sakai Y, Takenaka S, Yoshikawa H. Computed tomography color mapping for evaluation of bone ongrowth on the surface of a titanium-coated polyetheretherketone cage in vivo: a pilot study. Medicine (Baltimore). 2018;97:e12379. doi:10.1097/MD.0000000000012379
P277: One-Year Results of a Prospective, Multicenter Study to Assess the Clinical Efficacy of a Trabecular Metal Interbody Instrumented Lumbar Fusion
Ahmed Aoude1, Sultan Aldebeyan1, Thomas Barz1, Rune Hedlund1, Jorg Franke1, Geoffrey Lesage1, Luis A. Galovich1, Patrick Chatellier1, Jan Splawinski1, Gunter Raderschadt1, Albert Yee1, and Peter Jarzem1
1University of Calgary, Calgary, Alberta, Canada
Introduction: Trabecular metal has been used in orthopedics for many years with positive effects demonstrated in total hip arthroplasty. However, its use in spine surgery has not been popularized due to its sharpness and fear of dural tears during the process of implantation. The purpose of this study was to investigate the clinical outcomes for patients treated with a new trabecular metal interbody fusion system with smooth edges. Methods: A multicenter prospective study was conducted across 10 centers in Europe and Canada. All patients included in the study had a diagnosis of lumbar degenerative disc disease with up to grade 1 spondylolisthesis or retrolisthesis at the involved level. The surgical intervention consisted of a transforaminal lumbar interbody fusion (TM Ardis, Zimmer) along with posterior instrumentation. Patients were evaluated postoperatively for minor and major complications. In addition, patient-reported outcomes (PRO) such as back pain, leg pain, Oswestry Disability Index (ODI), and EQ5D were evaluated using questionnaires at 3, 6, and 12 months. Means of PRO at each follow-up were compared with preoperative values using the Student t test and 95% CI. A P value < .05 was considered statistically significant. Results: A total of 77 patients met the inclusion criteria and completed the study. A significant decrease in leg pain was noted at 3, 6, and 12 months postoperatively. Similarly, back pain improved significantly at all follow-ups. ODI results demonstrated a statistically significant decrease (P < .01) in scores at all follow-ups (3, 6 and 12 months). Moreover, a decrease of more than 15 points in the ODI was seen in 68% of patients at the 12 months mark. Similarly, the EQ5D score significantly increased at each follow-up time point (P < .001). Conclusions: Clinical outcomes in our study were favorable up to 12 months for pain, ODI, and EQ5D scores in comparison to preoperative values. In addition, no dural tears were related to implant design. Therefore, this study demonstrates promising clinical results for a new trabecular metal interbody fusion system.
P278: Risk Factors for Developing Recurrent Disc Herniation After Microdiscectomy Within Five Years
Jarnail Bal1, Dina Ridwan1, Gregoris Prezerakos1, Babak Arvin1, Karoyl David1, and Ahmed Ibrahim1
1Queens Hospital, London, UK
Introduction: To identify risk factors for developing disc recurrence following microdiscectomy within 5 years. Methods: Operative records were interrogated from 2010 to 2015. Those patients who had an index operation and revision operation within the 5 years were selected. Age, weight, height, occupation, smoking, level and no of levels operated, and type of index/revision surgery performed were analyzed. Results: A total of 555 patients had a microdiscectomy between 2010 and 2015. Twelve patients had a recurrent disc herniation requiring surgery with 2 patients requiring 2 revisions. The mean age 47, the time from index operation to revision surgery was on average 12 months, the level affected was L4/5 (41%) L5/S1 (41%), L3/4 (18%). Males and females were equally affected and average BMI (body mass index) was 27.2 60% of the patients worked in the construction/building industry. Parameters such as disc height, presence/degree of spondylolisthesis, adjacent modic changes and Cobb angle will be analyzed and compared with a propensity-matched cohort. Conclusions: All patients who had recurrent disc disease requiring surgery presented with recurrent symptoms. They tended to be overweight and have a physically demanding job. Their presentation was usually within 12 months of their index surgery. This information may help in preoperative counselling in this group of patients when discussing risk of recurrence.
P279: The Effect of Surgical Treatment of Degenerative Lumbar Spine Conditions on Mental Health: A Canadian Spine Outcomes and Research Network Study
Duncan Cushnie1 and Kenneth Thomas2
1McMaster University, Hamilton, Ontario, Canada
2University of Calgary, Calgary, Alberta, Canada
Introduction: Lumbar spine disease is associated with considerable morbidity, disability, and decreased quality of life. Surgery for some spine conditions has been shown to reduce pain and disability. Several small studies have shown an associated improvement in mental health after surgery. The aim of this national registry study was to examine the association between spine surgery and improvement in mental health. Material and Methods: The Canadian Spine Outcomes and Research Network (CSORN) registry was poled for all patients who had surgery for chronic lumbar spine disorders. Exclusion included infection, inflammation, tumor, and fracture. Preoperative and 12-month postoperative Short Form (SF)-12 Mental Component Score (MCS) was examined to assess for differences and associations with secondary metrics including Patient Questionaire-9 (PHQ-9), Oswestry Disability Index (ODI), SF-12 Physical Component Score (PCS), and Leg and Back Pain Numeric Rating Scales. Based on previous literature MCS <45 was used as a cutoff sensitive and specific for major depression. Results: A total of 2472 patients met the inclusion criteria and had preoperative and 12-month outcomes of interest. Mean MCS improved from 48.2 (95%CI 47.9-48.4) preoperation to 51.9 (95%CI 51.6-52.2; P < .00001) postoperation, with the improvement significant in every diagnosis separately. Patients meeting the cutoff for depression preoperatively had a 71.5% rate of reaching minimally clinically important difference (MCID) compared with 30.6% in those who did not (P < .001). Overall, there was a 51.2% drop in the proportion meeting the depression cutoff after surgery (P < .001). MCS correlated with PHQ9 (r = −.66; P < .0001). Improvement in MCS correlated with improvement in ODI (r = −.37; P < .0001), PCS (r = 0.15; P < .0001), leg pain (r = −0.19; P < .0001), and back pain (r = −0.23; P < .0001). Conclusion: Patients receiving surgery for chronic lumbar spine conditions demonstrated a significant improvement in overall mental health, consistent with previous reports. This was clinically significant in the majority of cases meeting criteria for preoperative major depression. Postoperatively there was a substantial decrease in the overall proportion of patients with low MCS scores. Improvements in mental health correlated with improvements in disability and pain suggesting that the benefits of surgery for these conditions may extend to include mental as well as physical health.
P280: Cortical Bone Trajectory Prevents Implant Loosening
Hooi Ming Tan1 and Kim Soon Oh1
1Island Hospital Spine Centre, Penang, Malaysia
Introduction: More surgeons have adopted the cortical bone trajectory (CBT) technique while instrumenting the osteoporotic lumbar spine. This technique finds increasing relevance in primary surgery in our ageing population as well as revision procedures. Material and Methods: We studied patients receiving spine surgery from December 2012 till June 2016, when 127 adult women underwent lumbar spine decompression and instrumentation via the cortical bone trajectory technique. The entire series of surgery was performed by a single main surgeon and his assisting spinal team. All were postmenopausal women with ages ranging from 61 to 92 years. All patients had evidence of abnormal bone density with T-score readings of worse than −2.5. Surgery was indicated for lumbar spine stenosis presenting with radiculopathy. The number of levels operated on ranged from 1 to 3. Excluded from our study were patients with acute traumatic lesions, metastatic spine disease, infective spine lesions, and spondylolisthesis greater than grade 1. Thoracic spine involvement was not studied. These patients were chosen for CBT on an alternate basis with classical pedicle screws. Full informed consent was taken before the surgery, with the assumed advantages of both CBT and classical pedicle screws explained and counselled. All patients had bilaminar decompression and at least 1 level of interbody fusion. These patients were then followed up for a minimum of 24 months. Of the 127 cases, 7 were lost to follow-up. A total of 130 patients underwent classical pedicle screws. Five were lost to follow-up. Our monitoring of the incidence of implant loosening was performed with quarterly radiographs in the first year and twice annually in the second, with computed tomography scans at 12 and 24 months. Radiographs were read and interpreted separately by the author and 2 radiologists, with statistical adjustment of interobserver variation. Results: Ten CBT patients suffered screw loosening, 6 of them having it at the sacral level and the remaining, on the cephalad last instrumented vertebra. Twenty-four pedicle instrumented patients had loosening. The chronological incidence of loosening ranged from 3 months to 10 months after surgery. Conclusion: This double-arm study is a continuation of 2 previous audits of ours looking at rates of loosening in cortical bone trajectorized screws. As in previous studies, the CBT method apparently promises a lower rate of loosening.
P281: Factors Associated With Early Cage Subsidence Following Oblique and Lateral Lumbar Interbody Fusion
Tamara Soh1, Arun Kumar Kaliya Perumal1, and Jacob YL Oh1
1Tan Tock Seng Hospital, Singapore
Introduction: Lumbar interbody fusion is widely used for the treatment of degenerative disc disease in the lumbar spine, as well as spondylolisthesis and in deformity correction. Different techniques are utilized, including the conventional PLIF (posterior lumbar interbody fusion), TLIF (transforaminal lumbar interbody fusion), ALIF (anterior lumbar interbody fusion) and LLIF (lateral lumbar interbody fusion). The OLIF (oblique lumbar interbody fusion) is an approach that utilizes the corridor between the anterior vessels (aorta and inferior vena cava) and psoas muscle to access the disc space. The advantages of an OLIF are that the psoas muscle and the lumbosacral plexus are not disrupted. In addition, a large interbody device can be used to optimize interbody fusion in OLIF and LLIF. Our study aims to review the factors associated with early cage subsidence in patients treated with OLIF and LLIF. Material and Methods: A retrospective review of patients who underwent OLIF or LLIF at our institution from 2017 to 2018 was done. Radiographs were evaluated for the following pre- and postoperative parameters: L1-S1 lordosis angle, anterior disc height, posterior disc height, disc angle, and segmental angle. Postoperative radiographs at 1 month, 3 months, and 6 months were evaluated for the presence of cage subsidence. Correlation analysis was done to evaluate the relationship between cage subsidence and age of the patient, length of construct, pre- and postoperative lordosis, cage length, cage height, cage breadth, and cage lordosis. Results: A total of 37 patients underwent OLIF/LLIF at 72 surgical levels. There were 22 female and 15 male patients, with a mean age of 62 years (range: 51.8-72.2). The mean construct length was 4.2 ± 1.5 segments. At 6 months postoperatively, the mean anterior disc height increased from 6.7 ± 3.9 mm to 9.9 ± 2.3 mm (P < .05), mean posterior disc height increased from 3.8 ± 2.4 mm preoperatively to 5.6 ± 2.3 mm (P < .05), while mean disc angle increased from 4.7 ± 4.9° to 7.2 ± 4.2 (P < .05). Global (L1-S1) lordosis increased from 35.7 ± 13.2° preoperatively to 33.8 ± 12.3° postoperatively, however, this did not reach statistical significance. Spearman’s rank correlation coefficient analysis was done for the following variables: age; length of construct; pre- and postoperative lordosis angle, cage length; height; breadth; and lordotic angle. All variables did not reach statistical significance except for the cage length and lordotic angle. The correlation coefficient for cage length was −0.266 (P < .05), and 0.271 for cage lordotic angle (P < .05). Conclusion: Results from our study showed that use of a smaller interbody cage and a higher lordotic angle was associated with early subsidence. However, patient age, length of construct, and cage height or breadth did not appear to affect the rate of early subsidence. While there are substantial advantages associated with OLIF and LLIF, it is pertinent to ensure that the cage length is optimized to avoid early cage subsidence in OLIF/LLIF. In addition, cage lordosis does not appear to be beneficial based on our series as it was also associated with early cage subsidence.
P282: The Impact of Presurgical Self-Reported Exercise Patterns on Postsurgical Outcomes in Thoracolumbar Spine Pathology
Mohammad Zarrabian1, James McCammon1, Mark Xu1, and Michael Johnson1
1University of Manitoba, Winnipeg, Manitoba, Canada
Introduction: There is evidence that preoperative physical fitness affects surgical outcomes. Walking ability prior to decompression surgery can improve outcomes. To our knowledge, there are no articles on self-reported exercise frequency as a predictor of thoracolumbar surgery outcomes. We predict patients who report exercise prior to surgical intervention will demonstrate decreased pain and disability but increased perceived health state following surgery compared with patients who do not exercise. Materials and Methods: We performed a retrospective review of prospectively collected data from the Canadian Spine Outcomes and Research Network (CSORN) national spine registry database from the time of its inception. Inclusion criteria specified all thoracolumbar patients who proceeded to spine surgery and completed the pre- and postoperative outcome measures up to 12 months postsurgery (N = 992). Outcome measures were numeric rating scales for back and leg pain, health state and Oswestry Disability Index (ODI). Exercise frequency was self-reported as “none” (n = 637) versus “some” (n = 355). These groups were further categorized into “none due to physical limitations,” “none” (not due to physical limitations), exercising “once or less per week,” and exercising “twice or more per week.” Student’s t tests were used to compare the mean scores of the outcome measures, and analysis of variance for subgroup comparisons, with results considered significant at P < .05. Results: Those who reported “some” exercise had significantly more favorable back and leg pain scores preoperatively (back: “some” mean [M] = 6.74, standard deviation [SD] = 2.311; “none” M = 7.23, SD = 2.124; P < .001) (leg: “some” M = 6.76, SD = 2.599; “none” M = 7.47, SD = 2.198; P < .001) and at 6 months postoperatively (back: “some” M = 3.30, SD = 2.354; “none” M = 3.68, SD = 2.539; P < .003) (leg: “some” M = 3.11, SD = 2.826; “none” M = 3.58, SD = 3.022; P < .003), but no difference at 1-year postoperatively. Overall, significantly lower ODI scores and higher EuroQOL health state index scores were seen in the “some” exercise group compared with the no exercise group preoperatively and at 3 and 12 months postoperatively (ODI: “some” M = 20.65, SD = 17.32; “none” M = 25.07, SD = 18.97; P < .001) (EuroQOL: “some” M = 73.62, SD = 18.42; “none” M = 68.18, SD = 18.56; P = .003). Compared with the “no exercise due to physical limitation” group, the “twice or more per week” exercise group demonstrated significantly favorable back and leg pain scores at baseline and 6 months postoperatively (back: 3.78 vs 3.16, P < .001) (leg: 3.69 vs 3.11, P = .009), whereas this difference was only seen at baseline and not at 6 months postoperatively when compared with the “once or less per week” exercise group. The “no exercise due to physical limitations” group had significantly higher ODI scores and lower EuroQOL health state index scores at all postoperative time points up to 1 year when compared with the “twice or more per week” group, but not when compared with the “once or less times per week” group. Conclusions: Patients who reported at least “some” exercise had consistently more favorable scores in outcome measures preoperatively and 6 months postsurgery. Beyond 6 months, some presurgical exercise decreases disability and improves health state up to 12 months postthoracolumbar spine surgery. The relationship between exercise, ODI, pain, and health state appear to be dose dependent.
P283: Lumbar Fusion in Elderly Patients—Mortality, Morbidity, and Functional Outcomes
Maheswara Akula1, Jetan Badhiwala2, Ajay Asokan1, Yeswanth Akula3, and Michael Fehlings2
1Basildon, UK
2University of Toronto, Toronto, Ontario, Canada
3Brighton and Sussex Medical School, Brighton, UK
Study Design: Systematic review and meta-analysis. Objective: Lower back pain and sciatica are increasingly common causes of disability in the elderly population, resulting in significant increases in health care costs. With an increasingly elderly population, significant numbers of patients in this group are treated with instrumented posterior lumbar fusion. This review aims to quantify the morbidity and mortality of lumbar fusion in order to aid surgeons, anesthetists, and hospital administrators in planning peri- and postoperative care and resources. Functional outcomes of these procedures were analyzed using validated scoring systems to justify the role of these procedures in this fragile group of the population. Methods: This systematic review of the literature regarding lumbar fusion in elderly population was performed using the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA) for article identification, screening, eligibility, and inclusion. Electronic literature search of Medline/PubMed, Cochrane, EMBASE, and Scopus databases yielded 960 articles. These articles were screened against established criteria for inclusion into this study. Studies presenting the morbidity and mortality outcomes for people above 65 were identified, and further screening done for extractable data as per our inclusion criteria. The Morbidity and mortality data from studies were incorporated into Microsoft Excel, with event rates and confidence intervals analyzed. Functional outcome data published in terms of the Japanese Orthopedic Association (JOA) score, Visual analogue scale (VAS) pain score, and Oswestry disability index (ODI) data extracted and subjected to meta-analysis. Results: Our search strategy identified a total of 960 studies. An additional 28 studies were identified by screening the references of relevant articles. After removal of 540 duplicate publications, the inclusion and exclusion criteria were applied to the titles and abstracts of the 448 articles. This yielded 51 articles that underwent full-text analysis. Twenty-four articles of these were excluded. Twenty-Seven articles were subjected to qualitative and quantitative analysis. Mortality rate was 2.5% (95% CI 0.9 to 6.6%). Mean estimated blood loss was 491.3 mL (95% CI 298.5 to 684.1 mL) and operative duration 195.5 minutes. (95% CI 162.7 to 228.4 minutes). Incidence of systemic complications were as follows: arrhythmia, 4.6%; CHF (congestive heart failure), 3.1%; pneumonia/respiratory distress, 5.4%; delirium, 7.1%; stroke, 2.1%; UTI (urinary tract infection), 5.0%; renal failure, 3.8%; DVT (deep vein thrombosis), 2.2%; PE (pulmonary embolism), 2.7%; ileus, 7.1%; MI (myocardial infarction), 2.7%. SIADH (syndrome of inappropriate antidiuretic hormone secretion) , 1.8%; Spinal procedure–related complications include neurological deficit, 3.6%; proximal junctional kyphosis, 4.0%; pseudoarthrosis, 8.5%; seroma/dehiscence, 3.7%; and wound infection, 4.2%; adjacent segment degeneration, 5.4%; dural tear, 6.7%; hardware failure, 2.8% and; epidural hematoma, 5.0%. Subgroup analysis was done to assess the impact of fusion technique on mortality and morbidity. Functional outcomes: Following the fusion, the mean improvement in VAS is by 3.7 with 95% CI of 3.0 to 4.3. The ODI decreased by 37.1 with 95% CI of 34.3 to 39.9. The JOA score improved by 10.6 with 95% CI of 9.5 to 11.8. Conclusions: A shared decision-making process between health care professionals and patients and family members is essential in offering lumbar arthrodesis to older patients. This study provides essential information to guide surgeons and anesthetists in planning peri- and postoperative care in this challenging demographic, and also this data informs health care policy makers considering the aging population. Quality of life and functional outcomes significantly improved following Lumbar fusions in this group of elderly patients.
P284: Instrumented Posterior Lumbar Fusion, With Only Local Bone Graft: Radiographic Evaluation
Imposti Felix1, Valacco Marcelo1, Servidio Mariano1, and Gonzalez Viescas Juan Manuel1
1Hospital Churruca, Ciudad Autonoma de Buenos Aires, Argentina
Introduction: Iliac crest bone graft is the gold standard in posterior lumbar fusion; nevertheless, the complications at the harvest site are common. Local bone graft is rarely used, because of its reliability as a graft to perform solid fusions. But it is used to avoid morbidity in relation with the donor site. The objective is to examine the viability of local bone graft in instrumented posterior Lumbar fusions with or without anterior support. Material and Methods: Ninety-three patients, underwent instrumented posterior lumbar fusion with (73 patients) or without (20 patients) anterior support due to degenerative lumbar pathology, between January 2014 and December 2016. Evaluation was performed by 3 different spine surgeons, with anteroposteroir and lateral X-ray, 12 months after surgery; looking for solid bone union or indirect signs of pseudoarthrosis (screw loosening) in case of doubts CT (computed tomography) scan was performed. Average follow-up was 30 months. All patients surgery were performed by the same 3 surgeons. In the group with anterior support (73), TLIF (transforaminal lumbar interbody fusion; 64), XLIF (extreme lateral lumbar interbody fusion; 16) and ALIF (anterior lumbar interbody fusion; 2) were used. Results: Three patients were lost in the follow-up, 9 were reoperated due to pseudoarthrosis, 7 whit out anterior support and 2 with TLIF. No signs of nonunion were observed in XLIF and ALIF patients. The bony union rate was 90% at 12 months after surgery. In 18 patients, screw loosening was observed but only in 9 patients no union was identified. Conclusion: The results show that the local bone is a good option for instrumented posterior lumbar fusion, with a union rate of 90%.
P285: Comparative Review Between Minimally Invasive and Traditional Approaches in Spinal Surgical Decompression
Mohammed Khashab1 and Mohamed Elkhalifa1
1King Saud bin Abdul-Aziz University for Health Sciences, Jeddah, Saudi Arabia
Introduction: Minimal invasive spinal surgery (MISS) is still generating controversy. Advocates are promoting that it is a surgical method with lesser tissue damage, lesser blood loss, and comparative outcomes to traditional (open) (Tra) surgical techniques. Material and methods: To compare decompression procedures done in our institute between 2011 and 2013 using (Tra) and MISS. Records of patients (n = 31) who fulfilled the inclusion criteria in the study period were included in this retrospective chart review. A specially designed sheet was used to obtain data from the patients’ medical records, and the patients were interviewed. Results: Eight patients (26%) underwent MISS and 23 (74%) underwent Tra. Twenty-one patients (68%) had 1-level surgeries, 10 (32%) underwent 2-level surgeries. Mean operative time was 161 minutes for the MISS, 185 minutes for the Tra surgeries. Mean blood loss was 63 mL for MISS, 413 mL for the Tra. Hospital stay mean was 3.75 days for the MISS and 5.48 days for the Tra. Mobilization out of bed was on the first day for MISS and the 1.75th day for Tra group. Mean level of pain was 1.71 and 3.45 on day 1 postoperatively for MISS and Tra, respectively. Three surgery related readmissions; 2 were post Tra. One of them was admitted with CSF (cerebrospinal fluid) leak and the other with severe unbearable pain. The third was MISS due to wound dehiscence Conclusions: Apart from the amount of blood lost during the procedure, which was more in the Tra, this study showed no significant difference between MISS and Tra.
P286: Relationship Between Cage Position and Lumbar Lordosis in Transforaminal Lumbar Interbody Fusion
Emiliano Vialle1, Luiz Gustavo Dal Oglio Rocha1, Fabian Catarino Lopez Hinojosa1, Guilherme Zandavalli1, Alfredo Guiroy1, and Luiz Roberto Vialle1
1Hospital Universitario Cajuru, Curitiba, Brazil
Introduction: Interbody fusion is a common procedure performed in the daily life of spine surgeons. Restoring the sagittal balance of the spine is one of the most important factors for a successful fusion and better clinical outcomes for the patients. Adequate position of the cage is critical to achieve better correction of lumbar sagittal parameters. The use of an intersomatic device provides support to load bearing of the anterior column, increases the fusion rate, and also offers indirect foraminal decompression by increasing the disc height. The aim of this study is to determine if anterior transforaminal lumbar interbody fusion (TLIF) cage placement does achieve better radiographic lumbar lordosis correction than those cages that were placed posteriorly. Material and Methods: A retrospective radiographic evaluation of patients treated for degenerative lumbar pathologies with a single level fusion using TLIF and pedicle screw instrumentation. Patients were categorized in 2 groups, those with cages placed in the anterior half of the disc space (TLIF-A) and those with cages placed on the posterior half (TLIF-P). Preoperative (preop) and postoperative (postop) standing lateral X-rays were measured to obtain lumbar lordosis (LL; L1-S1 angle), segmental lordosis (SL; L4-S1 angle), and the cage segmental lordosis (CSL; depending on the level fused). Results: A total of 100 patients underwent single-level TLIF procedure from 2011 to 2018. Fifty-four males and 46 females, mean age was 50.5 years (range 27-76 years). Forty-three cages were considered “anterior” (TLIF-A) and 57 “posterior” (TLIF-P). The average postoperative measures in the TLIF-A group were: lumbar lordosis 50.7, segmental lordosis 34.9, and cage segmental lordosis 21.6. In the TLIF-P group, average postoperative lumbar lordosis was 42.3 (P < .01); segmental lordosis 30.7 (P < .05), and cage segmental lordosis 18.8 (P > .05). Conclusion: Anterior interbody cage positioning provides better radiographic lumbar lordosis as well as segmental lordosis when compared with posterior positioning implants.
P287: Herniated Discs—Open Microsurgical or Endoscopic Approach? What Is Better for the Surgeon and What Is Better for the Patient?
Dmitry Dzukaev1, Andrey Grin2, Aleksander Pejker1, Alan Margiev3, Soslan Torchinov1, and Alla Geht3
1Moscow Spine Center, Moscow, Russian Federation
2N. V. Sklifosovsky Research Institute of Emergency Medicine, Moscow, Russian Federation
3Pirogov Russian National Research Medical University, Moscow, Russian Federation
Introduction: One of the main tasks for the neurosurgeon during the herniated disk surgery is to make the optimal window that will allow the safe decompression of nerve structures. At the same time, it has to minimize the damage to soft tissues, adjacent arches, and the facet joint to prevent segmental instability. So which approach is better to achieve these goals and good long-term effect? According to the literature, the comparison of their results is subjective and based on analysis of the regression time of the pain syndrome, patient’s activation, the return of a complete quality of life, the number of complications, and recurrences of a hernia. We should accept that no matter how much we want to optimize the study, obtaining objective results is difficult, since the patients with the same herniated disk diagnosis, might have anatomical features of the affected segment differ, and sometimes differ significantly. Material and Methods: The originality of our research is that each patient has a real time, both endoscopic using endoscopic trocar and endoscope and microsurgical approaches using the microscope. Forty patients were divided into 2 groups of 20 patients each. Each surgery is conditionally divided into 2 stages. 1 group: Stage 1: Comparative evaluation of visualization of the working window by endoscopic and microsurgical methods: (A) Endoscopic trocar was installed with a maximum diameter (23 mm) with video fixation of the interstitial gap (adjacent arches, facet joints). (B) Removal of the endoscopic trocar, installation of the Caspar retractor. At this stage, the inter-gap interval was visualized through a microscope and a comparison was made with the data obtained through the endoscope. Stage 2: Discectomy: (A) Standard microsurgical discectomy was performed with a neurosurgical microscope with a video fixation of the final anatomical picture of the spinal canal. (B) Removal of the Caspar retractor, reinstallation of the endoscopic trocar, and assessment of the possibility of manipulation in the spinal canal by the endoscopic method. In the second group work of devices was carried out in the reverse order. Results: Advantages of microsurgical decompression using a microscope are: the better visualization of the working window, the control of surgical aggression in the spinal canal, the possibility of changing angles of attack depending on the situation, and the anatomical features of the degenerative changes in the operated segment. Advantages of the endoscopic approach are: smaller cutaneous incision, less trauma to soft tissues. Conclusion: The endoscopic approach is a good choice for lateral sequestered hernias. The microscope provides better visualization of the operating field and safe decompression of the nerve root in case of degenerative changes in the anatomy of the arch and facet joint.
P288: Herniated Discs. Open Microsurgical or Endoscopic Approach? What is Better for the Surgeon and what is Better for the Patient?
Dmitry Dzukaev1, Alan Margiev2, and Andrey Grin3
1Moscow Spine Surgery Center, Moscow, Russian Federation
2Pirogov Russian National Research Medical University, Moscow, Russian Federation
3N. V. Sklifosovsky Research Institute for Emergency Medicine, Moscow, Russian Federation
Introduction: One of the main tasks for the neurosurgeon during the herniated disk surgery is to make the optimal window that will allow the safe decompression of nerve structures. At the same time it has to minimize the damage to soft tissues, adjacent arches, and the facet joint to prevent segmental instability. So which approach is better to achieve these goals and good long-term effect? According to the literature, the comparison of their results is subjective and based on analysis of the regression time of the pain syndrome, patient’s activation, the return of a complete quality of life, the number of complications, and recurrences of a hernia. We should accept that no matter how much we want to optimize the study, obtaining objective results is difficult, since the patients with the same herniated disk diagnosis, might have anatomical features of the affected segment differ, and sometimes differ significantly. Material and Methods: The originality of our research is that each patient has a real-time, both endoscopic using endoscopic trocar and endoscope and microsurgical approaches using the microscope. Fourty patients were divided into 2 groups of 20 patients each. Each surgery is conditionally divided into 2 stages. 1 Group: Stage 1: comparative evaluation of visualization of the working window by endoscopic and microsurgical methods: (a) endoscopic trocar was installed with a maximum diameter (23 mm) with video fixation of the interstitial gap (adjacent arches, facet joints) and (b) removal of the endoscopic trocar, installation of the Caspar retractor. at this stage, the intergap interval was visualized through a microscope and a comparison was made with the data obtained through the endoscope. Stage 2: discectomy: (a) standard microsurgical discectomy was performed with a neurosurgical microscope with a video fixation of the final anatomical picture of the spinal canal. (b) removal of the caspar retractor, reinstallation of the endoscopic trocar, assessment of the possibility of manipulation in the spinal canal by the endoscopic method. In the second group work of devices was carried out in the reverse order. Results: Advantages of microsurgical decompression using a microscope are: the better visualization of the working window, the control of surgical aggression in the spinal canal, the possibility of changing angles of attack depending on the situation, and the anatomical features of the degenerative changes in the operated segment. advantages of the endoscopic approach are: smaller cutaneous incision, less trauma to soft tissues. Conclusion: The endoscopic approach is a good choice for lateral sequestered hernias. the microscope provides better visualization of the operating field and safe decompression of the nerve root in case of degenerative changes in the anatomy of the arch and facet joint.
P289: The Influence of Preoperative Stigmata on MR Imaging on the Outcome of Minimally Invasive Tubular Lumbar Decompression in Patients With Lumbar Stenosis
Christoph Wipplinger1, Rafael L. Sugino1, Sertac Kirnaz1, Franziska A. Schmidt1, Ahmed Abdelsalam1, and Roger Härtl1
1Weill Cornell Medicine, New York, NY, USA
Introduction: Degenerative spinal imaging findings are frequently seen among the common population. Several imaging stigmata for adverse outcome have been described. They include the absence of epidural fat in the affected segment as well as redundancy of nerve roots (RNR). RNR describes nerve roots diverging from each other leading to a coiled or serpentinous appearance due to severe spinal stenosis. While controversially discussed, these findings are described to be associated to more severe symptoms as well as a predictor of poor outcomes after decompression. The goal of this study was to investigate correlations of radiological stigmata, like coiled or serpentinous nerve roots or absent epidural fat with pre- and postoperative pain or functional questionnaires. Material and Methods: The cohort is retrospective. Patients were selected from one institution, operated by a single surgeon, and were all treated by minimally invasive surgical (MIS) tubular lumbar decompression without arthrodesis. We identified 703 patients operated from 2010 to 2018 with lumbar decompression resulting in 57 patients. Patients included had to have preoperative magnetic resonance imaging (MRI) available, full Oswestry Disability Index (ODI), and visual analogue scale (VAS) pre- and postoperatively. Patients with spinal tumors, infections, fractures, or deformities were excluded. The analyzed MRI findings included serpentinous or coiled nerve roots as well as the absence or presence of epidural fat. Preoperative and postoperative VAS for leg and back pain as well as ODI were compared with the above-mentioned MRI findings. Kruskal-Wallis analysis of variance followed by Mann-Whitney U tests were used to determine statistical differences of the nonparametric VAS and ODI scores. P values less than .05 were considered statistically significant; the statistical analyses were performed in SPSS. Results: Preoperative MRI scans of 57 patients were grouped into coiled nerve roots (n = 7), serpentinous (n = 27), both (n = 8), and no RNR (n = 15). We also analyzed the presence (n = 50) and the entire absence (n = 7) of epidural fat in the affected segment. The median follow-up was 77 days (minimum = 15; maximum = 364 days). All groups showed significant improvement from preoperative to postoperative VAS and ODI scores (P < .05). However, there was no statistically significant difference among the radiographic finding groups neither in preoperative nor in postoperative VAS or ODI. Conclusion: The findings among this patient population suggest that the presence of preoperative RNR or the absence of epidural fat do not influence the outcome of MIS tubular lumbar decompression.
P290: Degeneration of the Adjacent Segment in Lumbar Spine Surgery With Stabilization System Transpedicular and PEEK Rods
Luis López1 and Antonio Reyes1
1National Institute of Rehabilitation, Mexico, Mexico
Introduction: Degeneration of the adjacent segment (DAS) that develops in the mobile segments above or below an instrumented segment (14), is the result of a greater biomechanical stress subsequent to rigid lumbar arthrodesis (15), has an incidence of 5.2% to 100% (16). The introduction of polyetheretherketone (PEEK) offers an alternative in the degenerative pathology of the lumbar spine (10) by mimicking the physiological load at adjacent levels. The objective is to determine the frequency of degeneration of the adjacent segment in patients operated with a transpedicular stabilization system and PEEK bars in the treatment of degenerative spondylolisthesis. Material and Methods: Habitual Clinical Practice Trial type study: prospective, descriptive self-controlled, longitudinal, quasi-experimental and open with a minimum follow-up of 2 years of 2 patient groups: the experimental, operated with semirigid system (PEEK bars), and a group control operated with rigid system (titanium) between January 2015 and December 2016. Radiographs (lateral and dynamic) and magnetic resonance imaging before and after surgery (at 12 and 24 months) were compared. Results: Thirty-six patients were included, 23 males and 13 females, average age of 57.3 ± 7.6 years (range 39-70). They were treated with titanium 14 and with PEEK 22. The incidence of global DAA considering was 26/36 (72.2%). The overall DAS rate was 81.8% with PEEK versus 57.1% with titanium (P = .11) for a relative risk of PEEK equal to 1.7 (CI 95% 0.7-3.8]. Conclusion: No significant difference was observed between both groups, although in some of the measurements the experimental group would seem superior to titanium.
Diagnostics
P291: Outcome of Intramedullary Arteriovenous Malformation
Toshitaka Seki1
1Hokkaido University, Sapporo, Japan
Introduction: There are various classification methods for spinal cord arteriovenous malformations, but from the localization of the arteriovenous shunt, we are concerned with (1) spinal epidural arteriovenous fistula, (2) spinal dural arteriovenous fistula, (3) spinal cord marginal part arteriovenous fistula, and (4) in arteriovenous malformations are classified and treated. Intramedullary arteriovenous malformations can cause congestive myelopathy, such as intramedullary hemorrhage or subarachnoid hemorrhage. Despite the development of microsurgical technique and endovascular treatment, it is still a complicated disease to treat. The treatment of intramedullary arteriovenous malformation is the most difficult disease in the spinal vascular disorder. Material and Methods: The subjects were 12 intramedullary arteriovenous malformations treated from 2000 to 2017 in Hokkaido University Hospital. Results: The patients were 6 males and 6 females, and the age was 19 to 48 years (average: 30.8 years, median: 33 years). Seven patients showed severe onset, and 5 patients showed a slow onset. The follow-up period was 15 to 161 months (average: 53.6 months, median: 50.5 months). The shunt sites were 5 patients of cervical cord level, 4 patients of thoracic cord level and 3 patients of conus medullaris. All patients underwent stereotactic therapy (20 Gy/4 fr). Two patients underwent only stereotactic therapy, 9 patients underwent both of direct surgery and stereotactic therapy, and 1 patient underwent both of embolization and stereotactic therapy. There was no patient only direct surgery or embolization. No patients had bleeding during the follow-up period. Conclusion: Stereotactic radiotherapy for intramedullary arteriovenous malformation seems to be a safe treatment option. However, more patients and long-term follow-ups are needed.
P292: A Clinical Manifestation That Challenges the Main Diagnostic Framework Necessitates Radiological Examination Addressing a Wider Spectrum of the Differential Diagnosis: A Case Report
Grigorios Delaportas1 and George Manolarakis2
1Univeristy of Vermont Medical Center, South Burlington, VT, USA
2Sitia’s Health Center, Sitia, Greece
Introduction: Visceral pathology identification as a cause of low back or even sacroiliac joint pain is not always apparent. It is not uncommon that an often painful condition steers the clinical thinking to draw the primary cause from a pool of the most apparent etiologies utilizing a “universal” algorithm that requires a single or a set of laboratory/imaging tests. How can a seemingly insignificant information from the patient’s history affect the choice of proper imaging as well as underline a rare diagnosis of low back pain? Material and Methods: We present the case of a 33-year old female who presented to our spine clinic with left-sided low back pain radiating to her left groin. The patient was referred by her primary doctor who had already ordered plain radiographs, MRI (magnetic resonance imaging), and ultrasound with nonremarkable findings thus ruling out disc herniation affecting the L1 nerve root, inguinal hernia, and pathology of the left ovary. Steroid injection in the left SI (sacroiliac) joint provided no relief of symptoms at all. Given the fact that MRI revealed minor degenerative disc and facet changes, a single-photon emission computed tomography (SPECT)-CT scan of the lumbar spine was ordered in order to assess radiotracer uptake by the discs or facet joints. However, an “odd” symptom reported by the patient herself—pain exacerbation with water consumption— was of paramount importance, as finally proven, for the diagnosis. Results: While awaiting for SPECT-CT scan to be scheduled, a suddenly increased intensity of pain in the left lower abdominal quadrant led the patient to seek treatment at the emergency department (ED). The ED physician ordered an abdominal CT scan with contrast, which revealed a “kink” in the left ureter just inferior to the iliac crest. The patient was immediately admitted to the hospital where a surgeon placed a stent in the patient’s ureter. The patient, as confirmed by phone follow-up, has been pain free since the placement of the stent. Conclusion: In-depth search and meticulous evaluation of all information obtained from the patient’s history, even the most bewildering one, could lead to the selection of the most appropriate imaging test that will address a broad spectrum of the differential diagnosis. As a result, a timely and appropriate treatment initiation will most likely have a powerful impact on the ramifications of the disease.
P293: Clinical Prediction of Recovery Following Whiplash Injury: Minimum Standards for Prognostic Models
Aidin Abedi1, Zorica Buser1, and Jeffrey Wang1
1University of Southern California, Los Angeles, CA, USA
Introduction: Whiplash injury is a common consequence of motor vehicle accidents and results in poor recovery in up to 50% of the victims. Clinical prediction rules (CPRs) are used to identify the patients at risk of chronic whiplash, and in part facilitate the selection of optimal treatment plan. Although several CPRs exist for whiplash, the comprehensive prognostic model for recovery is controversial. This study is part of the Whiplash Evidence Project and aims to summarize and evaluate the quality of existing CPRs, to identify the fundamental prognostic factors of recovery, and to set the minimum standards for appraisal of the prognostic models in whiplash. Material and Methods: PubMed, Medline, Web of Science, Scopus, CINAHL, and Embase databases were searched in May 2017, for studies on development and validation of CPRs in whiplash. Prognostic models were judged based on performance indices, such as R 2 and the area under the curve, using predefined criteria. High-performance models were screened for prognostic factors, which were validated in at least 2 studies, and those factors were recommended as the minimum standards for comprehensiveness of predictors of recovery in whiplash CPRs. Results: A total of 8 validation studies were included in this review. Psychologic and sociodemographic factors were the most common categories of predictors. There was a significant variability in the definition of recovery. The following domains met our criteria for inclusion in the minimum standard: age, pain, number of symptoms, cervical range of motion, disability, coping and post-traumatic distress. Conclusion: Based on our initial findings, 7 prognostic factors were identified as an evidence-based minimum standard for comprehensiveness of the existing CPRs, and can be used for development of future prognostic models. Our next step is to identify the most reliable and valid measures for each domain. Variability in definition and assessment of recovery limits the credibility of our appraisal for the performance of existing CPRs. Therefore, the core measure of whiplash recovery needs to be defined.
P294: Machine Learning Can Identify Delirium Following Orthopedic Surgery Using Medical Notes
Brian Cho1, Varun Arvind1, Deepak Kaji1, Ivan Ye1, Ray Tang1, Andrew Warburton1, Aly Valliani1, Daniel Ranti1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Quality improvement studies have provided surgeons with systematic insight on how to make changes to their practice to improve patient outcomes and avoid complications. However, currently most automated methods to identify patient complications for quality improvement studies rely on prelabeled administrative codes sampling data from fixed electronic medical databases. Medical notes contain a rich supply of medical data, yet the format of unstructured text has precluded these data from use in large retrospective analyses. Therefore, the utilization of free-text from electronic medical records using natural language processing in combination with machine learning can provide an additional tool for patient complication surveillance and identification. The purpose of this study was to develop a machine learning algorithm that can identify postsurgical delirium based on unstructured patient notes. Material and Methods: This was a retrospective analysis of medical notes from the Medical Information Mart for Intensive Care (MIMIC III), a large, single-center database composed of intensive care unit admissions data from 2001 to 2012. A total of 947 patients from the orthopedic service were identified. Patients who experienced delirium were identified using ICD-9 (the International Classification of Diseases, Ninth Revision) code (78009). A total of 15004 notes were analyzed in total from the 947 patients. Of the 15004 notes, 807 notes were from patients positive for delirium, and 14 197 notes were negative for delirium defined by ICD-9 code. Area under the receiver operating characteristic curve (ROC), accuracy, sensitivity, and specificity of the model were evaluated to assess performance of the model. Natural language processing was used to analyze unstructured narrative discharge notes and train a support vector machine algorithm to train a classifier to automatically identify patients with delirium based solely on unstructured discharge notes. The data was randomized with 70% used for training and 30% used for testing. Results: The SVM (support vector machine) algorithm identified delirium notes with a sensitivity and specificity of 70% and 94%, respectively. The overall accuracy was 92.8% with area under receiver operating characteristic curve of 0.82. Conclusion: Combining natural language processing with machine learning is a valid approach for automatic identification of delirium using unstructured text from discharge notes. This method provides a robust survey of surgical encounters and may be used for real-time surveillance of postoperative complication risk and for automated identification of patient complications such as delirium for quality improvement studies.
P295: Machine Learning Can Identify Deep Vein Thrombosis Following Orthopedic Surgery Using Medical Notes
Varun Arvind1, Brian Cho1, Deepak Kaji1, Ray Tang1, Ivan Ye1, Andrew Warburton1, Aly Valliani1, Daniel Ranti1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Quality improvement studies have provided surgeons with systematic insight on how to make changes to their practice to improve patient outcomes and avoid complications. However, currently most automated methods to identify patient complications for quality improvement studies rely on prelabeled administrative codes sampling data from fixed electronic medical databases. Medical notes contain a rich supply of medical data, yet the format of unstructured text has precluded these data from use in large retrospective analyses. Therefore, the utilization of free-text from electronic medical records using natural language processing in combination with machine learning can provide an additional tool for patient complication surveillance and identification. The purpose of this study was to develop a machine learning algorithm that can identify postsurgical deep vein thrombosis (DVT) based on unstructured patient notes. Material and Methods: This was a retrospective analysis of medical notes from the Medical Information Mart for Intensive Care (MIMIC III), a large, single-center database composed of intensive care unit admissions data from 2001 to 2012. A total 947 patients from the orthopedic service were identified. Patients who experienced DVT were identified using ICD (the International Classification of Diseases, Ninth Revision)-9 code (45340). A total of 15004 notes were analyzed in total from the 947 patients. Of the 15004 notes, 227 notes were from patients positive for DVT, and 14777 notes were negative for DVT defined by ICD-9 code. Area under the receiver operating characteristic curve (ROC), accuracy, sensitivity, and specificity of the model were evaluated to assess performance of the model. Natural language processing was used to analyze unstructured narrative discharge notes and train a support vector machine algorithm to train a classifier to automatically identify patients with DVT based solely on unstructured discharge notes. The data was randomized with 70% used for training and 30% used for testing. Results: The SVM algorithm identified DVT notes with a sensitivity and specificity of 62% and 99%, respectively. The overall accuracy was 89.7% with area under receiver operating characteristic curve of 0.80. Conclusion: Combining natural language processing with machine learning is a valid approach for automatic identification of DVT using unstructured text from discharge notes. This method provides a robust survey of surgical encounters and may be used for real-time surveillance of postoperative complication risk and for automated identification of patient complications such as DVT for quality improvement studies.
P296: Vertebral Level Identification
Kathryn Ramshaw1 and Palaniappan Lakshmanan1
1City Hospitals Sunderland, East Boldon, UK
Introduction: Wrong-level surgery in the spine is still not uncommon. Not only do transitional vertebral bodies confirm this, but also the way vertebral bodies are numbered there is no consensus between radiologists and spinal surgeons. Radiologists prefer counting from atlas downward, while spinal surgeons count from lumbosacral junction upward as upper thoracic spine cannot be seen on fluoroscopy during surgery. Aim: The objective of this study is to highlight the differences in vertebral level identification, when starting counting from the top of the cervical spine as opposed to counting from the bottom of the lumbar spine. Materials and Methods: A cohort of 200 consecutive whole-spine magnetic resonance imaging (MRI) scans were analyzed between January 1, 2015, and December 31, 2017. Scans were eliminated if the whole spine was not accessible in one clear image, and if they had a lumbosacral transitional vertebral body. Vertebral bodies were counted from the top down to lesion level, then again from the bottom up to lesion level. In any spines without a lesion the mid-point was selected by the researcher. Results: Out of 200 MRI scans, 66 were eliminated, leaving 134 suitable for counting. A total of 6.7% (9) of these demonstrated variations in vertebral level if counted from the top of the cervical spine down, then from the bottom of the lumbar spine up. The L5/S1 junction should normally be 24/25 vertebra on count. In 6 patients, it was 23/24 and in 3 patients, it was 25/26. Conclusion: Vertebral body identification can be different if counted from the cervical spine down, or from the lumbar spine up in whole spine MRI. Problems may arise if radiologists use different methods of vertebral body counting than surgeons do, in patients with physiological differences that require whole spine MRI. Adopting the approach to count from bottom up, even though counting from top down may be considered as anatomical, is recommended to ensure that we can identify the levels correctly during operations using image intensifier, as the upper thoracic spine cannot be imaged properly.
P297: A Clinical Diagnostic Method Based on Acoustic Analysis of Spine Sounds in Degenerative Disorders of the Lumbar Spinal Column
Vugar Nabiyev1, Selim Ayhan2, Mustafa Arda Ahi3, Hakan Toreyin4, Enis Cetin5, and Emre Acaroglu6
1ARTES Spine Center, Acibadem Ankara Hospital, Ankara, Turkey
2Acibadem Mehmet Ali Aydinlar University, Istanbul, Turkey
3Bilkent University, Ankara, Turkey
4San Diego State University, San Diego, CA, USA
5University of Illinois at Chicago, IL, USA
6Ankara Spine Center, Ankara, Turkey
Introduction: Because of the associated costs and potential unavailability of advanced diagnostic modalities in clinical practice, there is a need for a novel spine health assessment technique that could enable early detection of spinal disorders outside the clinic. Acoustic analysis has been shown to be effective in pathologies of joints. This study aims to investigate spine sounds from a perspective of their use in diagnosing degenerative disease. Material and Methods: Thirteen patients who had magnetic resonance imagings (MRIs) taken because low back pain (LBP) and 17 (non-MRI, non-LBP) volunteers were enrolled. MRIs were graded for disc (DD) and facet joint (FD) degeneration by 2 independent clinicians (c1) and (c2). All enrollees had adverse events (AE) of their lumbar spine captured by an airborne electret BY-M1 omnidirectional microphone with wide bandwidth (18 kHz) and high signal-to-noise-ratio (SNR = 74 dB) and high sensitivity (31 mV/Pa) and recorded using a mobile phone application. Data were analyzed for the probability of a “click” sounding signal (CSP) that is distinct and detectable during active motion of the lumbar spine. Results: Average age was 32.26 ± 7.56 in LBP (5 females, 8 males) versus 31.29 ± 5.28 (9 females, 8 males) in non-LBP groups. Average grades of DD and FD were 2.92 and 1.67 for c1, 2.92 and 1.92 for c2, and 2.92 (range 2-4) and 1.79 (0-3) on average, respectively. The average CSP was 0.71 ± 0.18 in LBP versus 0.21 ± 0.22 in non-LBP groups (P < .0001). CSP was correlated with both DD (0.87) and FD (0.83). The accuracy of the AE-based diagnosis is 90.62 with a 95% CI (confidence interval) is 74.98% to 98.02%. Conclusion: Acoustics analysis of sounds emitted by the lumbar spine in active motion are significantly different in patients with LBP compared with those without LBP. Moreover, the CSP of the AE correlates with facet as well as disc degeneration in LBP patients. These results suggest that acoustic analysis, following larger studies for better calibration through machine learning, may be a useful tool in diagnosing and potentially grading degenerative disease of the spine and may substantially decrease the need for imaging with higher costs.
P298: Intraoperative Neurophysiological Monitoring for Intramedullary Spinal Cord Tumors
Ehab Shiban1, Sebastian Ille1, Arthur Wagner1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Background: Intraoperative neurophysiological monitoring (IONM) has increased patient’s safety and extent of resection in patients with eloquent brain tumors. Despite its comprehensive capability for the resection of intramedullary spinal cord tumors (ISCT), the application during the resection of these tumors is controversially discussed. Patients and Methods: We retrospectively analyzed the resection of ISCTs in 86 consecutive cases. IONM was performed in all cases. The patient’s motor status and the McCormick’s scale were determined preoperatively, directly after surgery and at day 5 and 90 following surgery. Results: IONM was feasible in 74 cases (86%). Gross total resection (GTR) was performed in 76 cases (88%). Postoperatively, patients showed new transient deficits in 13 cases (15%) and new permanent deficits in 13 cases (15%). The mean McCormick’s variance between baseline and 3 months follow-up was −0.07 ± 0.57. IONM’s sensitivity, specificity, positive predictive value, and negative predictive value for the patient’s motor status 5 days postoperatively was 76.2%, 64.2%, 45.7%, 87.2, and 90.0%, 59.4%, 25.7%, 97.4% for the motor outcome at 3 months follow-up. Patients suffered from postoperative complications in 16 cases (18%). Conclusion: IONM shows a high sensitivity and negative predictive but low specificity and positive predictive value particularly for the patients motor status at the long-term follow-up. Hence, our results confirm IONM’s usefulness for the application during the resection of ISCTs.
P299: There are Significant Psychological and Clinical Outcome Differences Between Smokers and Nonsmokers in Patients Undergoing Elective Spine Surgery
Ehab Shiban1, Bernhard Meyer1, Arthur Wagner1, Nicole Lange1, Amm-Kathrin Jörger1, and Youssef Shiban2
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
2Private University of Applied Sciences, Göttingen, Germany
Objectives: Previous results have shown that smoking is a major risk factor for perioperative morbidity and complications in spine surgery. However, the differences in psychological comorbidities and their influence on clinical outcome, between smokers and non-smokers has not been examined so far. Methods: A prospective study of patients undergoing elective spine surgery from 2015 till 2017 was performed. Evaluation for smoking habits, mental comorbidities (ADS-K, STAI-S, STAI-T and ASI-3 scores) and clinical outcome (SF [Short Form]-36, Oswestry Disability Index [ODI] and pain visual analogue scale [VAS]) were done before and 1 year after surgery. Smoking habits were correlated with the mental and physical outcome measurements. Results: A total of 342 patients were included. In all, 202 (59.1%) were female and the mean age was 62 years. A total of 233 (68.1%) and 109 (31.9%) had thoracolumbar and cervical surgery, respectively. There were no differences in baseline characteristics between smokers and non-smokers with regard to clinical outcome. Mental status was worse in smokers. Non-smokers had superior clinical outcome both for cervical cases (ODI: 37.6 vs 42, P = .013; VAS pain: 2.5 vs 4.2, P = .009; PCS [physical component summary]: 40.3 vs 22.1, P = .002) and thoracolumbar cases (ODI: 34.62 vs 49, P = .004; VAS pain: 2.9 vs 4.1, P = .008; PCS: 41.6 vs 24.1, P = .002). Also, non-smokers had better mental status than smokers both in cervical cases (ADS-K: 12.2 vs 19.3, P = .037; ASI-3:17.9 vs 29.7, P = .047; STAI-S: 43.2 vs 49.5, P = .047;STAI-T:40.1 vs 48.4, P = .041) and thoracolumbar cases (ADS-K: 9.4 vs 14.2, P = .053; ASI-3:12.8 vs 22.9, P = .029; STAI-S: 33.6 vs 42.1, P = .039; STAI-T:39.3 vs 45.2, P = .049). Conclusion: Smoking correlates with worse mental and clinical outcome 1 year following surgery for degenerative disc disease.
P300: How to Screen for Psychological Morbidities Before Elective Spine Surgery?
Ehab Shiban1, Youssef Shiban2, Ann-Kathrin Jörger1, Arthur Wagner1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
2Private University of Applied Sciences, Göttingen, Germany
Objectives: Aim of this study was to examine the diagnostic value of standardized questionnaires evaluating for anxiety and depression before elective spine surgery. Methods: From a prospective observational study of 374 patients undergoing elective spine surgery from 2016 till 2017, for degenerative disc disease, patients were randomly selected, and a structured clinical interview for DSM (SKID) as well as a battery of standardized questioners evaluating for mental comorbidities were performed. The presence or absence of psychiatric disorder symptoms was correlated the gold standard SKID. Results: Sixty-seven patients were examined. Fifty-seven percent were females. Mean age was 52 years. A total of 42% of patients were diagnosed with depression in the SKID interview, but only 26% of patients had pathological ADS scores (0.019). Concordant positive results were seen in 14 cases only. Forty-three percent of patients were diagnosed with an anxiety disorder in the SKID interview and 40% of patients had pathological STAI-T and STAI-S scores (P = .068). Concordant positive results were seen in 20 cases. Conclusion: Standardized questionnaires were capable to distinguish for real anxiety but underestimated the rate of depression as detected by the SKID interview, during screening for mental comorbidities before elective spine surgery.
P301: A New Score Predicting Clinical Outcome Following Lumbar Spine Surgery for Degenerative Disc Disease
Ehab Shiban1, Youssef Shiban2, Arthur Wagner1, Nicole Lange1, Ann-Kathrin Jörger1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
2Private University of Applied Sciences, Göttingen, Germany
Objectives: This study was performed to create and validate a scoring system to predict unfavorable outcome following first-time elective lumbar spine surgery for degenerative disc disease. Methods: A prospective cohort study of 175 patients was performed. One hundred patients were assigned to a test group, and 75 patients to a validation group. In the test group, 16 pretreatment factors including age, gender, education level, relationship status, presents of previous psychiatric disorders, the Anxiety Sensitivity Index, State Anxiety Inventory, Trait Anxiety Inventory, Depression Scale, Berliner Social Support Scale, PTSS-10 for PTSD symptoms, SF (Short Form)-36 physical and mental composite scores, visual analogue scale for pain, EuroQOL-5D, and Oswestry Disability Index (ODI) were prospectively analyzed. Unfavorable outcome was defined as less than 15 points improvement of ODI 1 year postoperatively. Results: A multivariate logistic regression analysis identified age (P = .031), trait anxiety (P = .020), depression (P = .022) and SF-36 physical (P = .002) and mental composite scores (P = .004), and ODI (P = .049) as predictors of unfavourable outcome 1 year postoperatively. These factors were included in the score. The total risk score was the sum of the 6 factor scores and ranged from 0 to 12 points. Three prognostic groups were designed. Group A—0 to 3 points for favourable outcome, group B—4 to 5 points for probable unfavourable outcome, and group C—6 to 12 points for unfavourable outcome. In the validation group 100%, 61% and 87% of patients in groups A, B, and C were successfully predicted, respectively (P = .019). Conclusion: Clinical outcome following elective spine surgery for lumbar degenerative disease is influenced by physical and mental factors. This newly developed score appears reproducible as most cases in the validation group were successfully identified. This new score can help identify possible patients with unfavorable outcome. Thereby concomitant psychosomatic treatment may me initiated.
P302: Understanding and Managing IONM Changes During Spinal Deformity Surgery
Stephen Lewis1, Ian Wong1, Fan Jiang1, So Kato1, Hailey Bensky1, Sam Strantzas2, and Laura Holmes2
1Toronto Western Hospital, University of Toronto, Ontario, Canada
2Hospital for Sick Children, University of Toronto,Ontario, Canada
Introduction: Intraoperative multimodality neuromonitoring (IONM) has been established as the standard as an adjunct to spinal deformity surgery. Despite its universal acceptance and use, there remains significant controversy into what constitutes a neuromonitoring change, what significance does that change represent, what actions should be taken in response to the change, and which factors led to the changes. Material and Methods: A retrospective review of prospectively collected neuromonitoring data in preestablished forms on consecutive patients undergoing spinal deformity surgery was performed. In the event of signal change, the neuromonitoring form was completed detailing surgical or systemic causes for the alert, actions taken in response to the alert, and outcome of the signal recovery of the alert. The inclusion criteria included pediatric patients with a minimum of 50° primary coronal deformity for idiopathic or syndromic causes. All patients underwent posterior column osteotomy (PCO) or intraoperative traction with motor-evoked potential (MEP) and somatosensory-evoked potential (SSEP) monitoring. Results: A total of 97 pediatric patients involving 71 females and 26 males with a mean age of 14.9 (11-18) years were included in this study. There were 39 alerts in 27 patients (27.8% overall incidence). Significant differences were noted among the groups with no motor-evoked potential (MEP) changes (n = 70) versus those with MEP changes (n = 27) based on mean number of levels fused (12.8 vs 13.4) and patients who underwent PCOs (25.7% vs 51.9%). IONM alerts were divided into 2 subgroups: cases involving spinal cord perfusion deficits and those occurring as a result of direct trauma to the cord. All perfusion-based changes (n = 23) involved bilateral MEP loss without SSEP loss. Direct trauma (n = 16) resulted in unilateral MEP alerts with 2 cases having SSEP changes as well. All bilateral changes responded to a combination of transfusion, increasing blood pressure, and rod removal. Unilateral changes as a result of direct trauma, mainly during decompressions, resolved with removal of the causative agent and time. At skin closure, the signal recovered to baseline (BL) in 20 patients, between 75% and 100%of BL in 3 patients, between 50% and 75% of BL in 2 patients, and between 25% and 50% of BL in 2 patients. Patients with perfusion-based changes were monitored closely postoperatively for blood pressure and anemia management. There were no new neurological deficits in this series. Conclusion: A high incidence of alerts occurred in our series of cases. Dividing IONM changes into perfusion-based versus direct trauma helped direct treatment to the offending cause, allowing for safe corrections of the deformities. Patients did not need to recover signal to baseline to have a normal neurological examination. Careful monitoring and management helped to maintain spinal cord perfusion in the perioperative period.
P303: Comparison of Machine-Assisted Trunk Muscle Strength Measurement and a Functional Posture Test
Philipp Flößel1, Stefan Zwingenberger1, Alexander Thomas1, Achim Walther1, Heidrun Beck1, Klaus-Dieter Schaser1, and Alexander C. Disch1
1University Center of Orthopaedics and Traumatology, University Hospital Carl Gustav Carus at Technische Universität Dresden, Dresden, Germany
Introduction: Functional trunk muscle stability as a combination of sufficient trunk muscle strength and neuromuscular control is a condition of an active compensation of spinal load. Therefore, trunk muscle strength is often assessed in a machine-assisted and isokinetic manner for sports scientific diagnostics and that is also regarded as gold standard in literature. However, this form of diagnostic is expensive and lacks availability. Aim of this study was the identification of a sufficient easily available field test. Material and Methods: Thirty probands took part in this prospective cross-sectional study (n = 17/13, males/females). The median age was 35.4 (25.6; 48.2) years. The testing phase was divided into 2 parts: First, the biomechanical testing was done with an automatic trunk muscle strength measurement with an IsoMed 2000 dynamometer—both concentric and isokinetic. After warming up with 10 to 20 repetitions, a 1-minute break was given, followed by 10 further repetitions with maximal power. Finally, the Biering Sorensen’s functional extension holding test was performed. Purpose of this test is to keep a body position horizontally as long as possible. The comparison of both methods was made due to the comparison of the maximal relative turning moment (Extmax/kg = Extnorm) with the absolute maximal holding time in seconds (ExtHz). For descriptive statistics the median with 0.25 quartile and 0.75 quartile was used. The significance level was defined as P ≤ .01. For analysis Spearman’s rank correlation coefficient was used. Results: The group of probands reached an absolute maximal holding time ExtHz of 151 seconds (131; 200) and a maximal relative turning moment Extnorm of 3.7 Nm/kg (3,2; 4,3). Spearman’s rank correlation coefficient was R 2 = .46 with P < .01. Regarding the body weight, male probands reached a higher power-load ratio than female (3.9 vs 3.3 Nm/kg). This result was also achieved with the maximal holding time. Male probands reached a median of 158 seconds compared with female with 146 seconds, despite lower body weight. Conclusion: The study shows high significant methodical correlation between the functional and automatical diagnostic method. Gender-related differences can be explained by the power-load-ratio. The higher incidence of lower back pain of women could be caused by less relative extensional power. Further studies are necessary for further investigating those aspects. The functional method offers a highly reproducible testing method, independently adjustable of a dynamometer, already with reference values for healthy people in literature.
Disc Degeneration
P304: Assessment of Lactate Production and Proteoglycans Synthesis by The Intact and Degenerated Intervertebral Disc Cells Under the Influence of Activated Macrophages: In Vitro Study
Liudmila Bardonova1, Evgenii Belykh1, Vadim Byvaltsev1, and Morgan Giers2
1Irkutsk, Russian Federation
2Oregon State University, Corvallis, OR, United States
Introduction: Inflammation is one of the main factors in the development of intervertebral disc (IVD) degeneration. Nevertheless, the cellular mechanisms of the proinflammatory cytokines’ influence on IVD cells remain not fully elucidated. Synthesis of extracellular matrix is an energy-dependent process, which may be affected by the shortage of nutrient supply observed in degenerated IVD. However, the effect of inflammatory mediators on nutrient consumption and metabolic activity of IVD cells is unknown. Using the model of co-cultivation with activated macrophage-like cells, we studied the effects of the inflammatory cytokines on the secretion of glycosaminoglycans (GAG) and production of lactate by the intact and degenerated IVD cells. Material and Methods: Cells obtained from the human annulus fibrosus fibrous ring and the nucleus pulposus (inner core) of intact (ScienCell) and degenerated (Barrow Neurological Institute BioBank) intervertebral discs were used for the experiment. Cells were expanded in monolayer, then trypsinize and resuspend in 1.2% sodium with formation of alginate beads using 102 mM CaCl2. The IVD cells incapsulated in alginate beads (2 × 105 cells/well) were cocultured with or without 60 ng/mL phorbolmyristate acetate-activated macrophage-like THP-1 cells (aTHP-1). Viability, lactate production, glucose consumption and sulfated GAGs (1,9-dimethyl-methylene blue assay) were assessed. The levels of TNF-α, IL-1β, IL-6, IL-8, IL-10, and IL-12p70 were assessed by flow cytometry using microspheres (BD Biosciences, San Jose, CA). Cell morphology in 3D culture was studied using immunocytochemistry: whole beads were fixed and stained with phalloidin for F-actin and DAPI for DNA, and imaged on a laser confocal microscope. All experiments were repeated in triplicate. A main effects ANOVA (analysis of variance) and post hoc Mann-Whitney U tests were performed to compare control and aTHP-1 groups. Results: aTHP cells produced significantly more IL-10, IL-6, IL-1β, and IL-8 (P < .05) compared with control media and nonactivated THP-1 cells. Significant increase of IL-1β, IL-8 levels was observed in all coculture groups compared with controls (P < .05). Proliferative activity (P = .12) and viability (P = .01) of both intact and degenerated annulus fibrosus (AF) and nucleus pulposus (NP) cells significantly decreased in aTHP-1 coculture groups. GAG production was significantly lower in degenerated NP and AF cells when compared with the intact groups, P < .05 for both cell types. Pro-inflammatory cytokines significantly decreased GAG mass/cell in all aTHP-1coculture groups (pANOVA = 0.003). Significant decrease (P < .05) of lactate production was observed in all aTHP-1coculture groups of intact and degenerated NP and AF cells compared with control. The imaging study showed smaller cell size and grouping in clusters in the degenerated IVD cells compared with intact. Conclusion: We revealed that pro-inflammatory cytokines have a direct effect on IVD cells in a 3-dimensional culture, reducing the rate of glycolysis, and level of synthetic activity of both intact and degenerated cells of annulus fibrosus and nucleus pulposus, which is an important factor in the progression of IVD degeneration.
P305: Enhanced Recovery Following Interbody Fusion by Transforaminal Endoscopic Techniques
J. N. Alastair Gibson1, Ralf Wagner2, and Bernd Illerhaus3
1Spire Murrayfield Hospital, Edinburgh, UK
2Ligamenta Spine Centre, Frankfurt, Germany
3Elisabeth-Krankenhaus, Recklinghausen, Germany
Introduction: In the past decade, transforaminal endoscopic spine surgery (TESS) has become increasingly commonly used for disc resection and foraminotomy. The transforaminal approach minimizes damage to the paraspinal muscles and should enhance patient recovery postsurgery. We aimed to evaluate the technical and clinical success of endoscopic disc resection and interbody cage fusion via a transforaminal approach. Materials and Methods: Forty patients (mean age 60 ± 10 years, 75 ± 14 kg, 10 males, 30 females) presenting with stenotic symptoms secondary to single-level disc protrusion and degenerative instability (Grade 1 spondylolisthesis) were admitted for surgery. Patients with significant lateral recess in-growth producing a “trefoil” canal were excluded. Median duration of symptoms was 48 months. Surgery was performed in all patients under general anesthesia in the prone position. Transforaminal discectomy removed prolapsed and central disc back to the end-plates. Titanium (Ti6Al4 V) trabecular cages (EndoLIF Oblique cage, joimax GmbH) were then inserted obliquely without graft. The operated level was stabilized further by a percutaneous pedicle screw/rod construct (Percusys joimax, GmbH or similar). Outcomes were collated with hospital stay and re-admission rates compared to those reported on the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database for patients after posterior lumbar fusion (2005-2010: 1861 and 2011-15: 36,610 patients respectively). Results: Mean surgical time was 128 ± 57minutes and radiation dose area product 1166 ± 552 cGy·cm2. There were no intraoperative complications and median hospital stay was 12 hours (range 4-120) compared with ACS-NSQIP of 2.9 ± 1 days. Two cages were inserted at L2/3, 5 at L3/4, 26 at L4/5 and 7 at L5/S1. Most cages were 30 mm × 11 mm × 12 mm size and mean blood loss was 150 mL. Disc height increased with instrumentation from 7.6 ± 1.9 mm to 10.5 ± 1.6 mm anterior, and from 4.9 ± 1.0 to 9.8 ± 1.7 mm posterior (P < .001). Preoperative ODI decreased from 50 ± 17 to 27 ± 20 at 6 months, back pain VAS (0-10) from 7.3 ± 2.2 to 3.3 ± 2.5 (both P < .001) and pain in the most affected leg from 5.9 ± 3.5 to 3.7 ± 3.0 (P < .01). One readmission for cage displacement at 4 months (2.5%) compared with a rate of 5.4% within 30 days on the ACS-NSQIP. Conclusion: Our results indicate that endoscopic interbody fusion via a transforaminal approach is safe and effective. Mean hospital stay was significantly less than that reported for other fusion methods. Randomized studies are still required to determine whether instrumentation and fusion are required over and above transforaminal endoscopic decompression alone.
P306: Size Does Not Matter: Correlating Disc Size With Disability and Leg Pain
Sohail Nisar1, Peter Loughenbury1, and Robert Dunsmuir1
1Leeds General Infirmary, Leeds, UK
Introduction: The size of the herniated disc is commonly mentioned as a factor when deciding if a patient requires surgical intervention. Various studies have suggested the size of the herniated disc should be considered when deciding between operative or conservative management. However, to our knowledge, there are no published studies correlating the size of the herniated disc with severity of symptoms using visual analogue scale (VAS) or Oswestry Disability Index (ODI) scores. Material and Methods: Data was collected prospectively. Patients were asked to complete VAS and ODI scores on the day of surgery. All patient with primary disc herniation were included. Exclusion criteria included recurrent disc herniation or any other associated spinal pathology, for example, fracture, scoliosis, and infection. T2-weighted MRI (magnetic resonance imaging) scans were reviewed on PACS software by the authors. The axial image showing the largest disc protrusion was used for measurements. The size of the disc and canal were measured. The VAS Leg score and ODI score were correlated with the size of the disc using the Pearson correlation coefficient. Interobserver and Intraobserver reliability was assessed using the interclass correlation coefficient (ICC). Results: Forty patients were included in the study. Ages ranged from 20 to 72 years, with an average age of 42 years. A high degree of interobserver reliability was found. The single measure ICC was 0.85 (95% confidence interval [CI] 0.51-0.96 [F = [9.9] = 12.4, P < .001]). A high degree of intraobserver reliability was observed. The single measure ICC was 0.81 (95% CI 0.42-0.95. [F = [9.9] = 9.8, P = .001]). The Pearson correlation coefficient comparing VAS leg scores with percentage canal occupied by the herniated disc was 0.0004. When comparing ODI scores with percentage of the canal occupied by the herniated disc the Pearson correlation coefficient was −0.02. Conclusion: The results of the statistical analysis show that there is a very low strength of association between the size of the disc and a patient’s symptoms. This study highlights the importance of clinical assessment. Management decisions should not be made on the basis of radiological imaging but rather a clinician must consider a patient’s symptoms and the impact on their life.
P307: Adjacent Level Degeneration and Post-Traumatic Deformity After Thoracolumbar Fractures
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler I Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Introduction: To evaluate thoracolumbar fractures and the complications such as adjacent disc degeneration (ADD) and posttraumatic deformity. Methods: We evaluated 32 patients divided into 2 equal groups, 16 in the case group (removal of the synthesis material), and 16 in the control group (not submitted to removal of the synthesis material), in order to verify if there was difference between the incidence of these complications. Results: There were no statistically significant differences between the groups regarding the progression of the ADD and the post-traumatic deformity, but both progressed during the 2-year follow-up. Conclusion: It was concluded that the removal of the synthesis material was not effective in preventing these complications after surgical fractures of the thoracolumbar spine.
P308: Basal and Cytokine-Stimulated Biomarker Production by Degenerative Lumbar Discs From Microdiscectomy Versus Interbody Fusion Patients
Chaiyapruk Pundee1, Naomi N. Lee1, Jacob S. Kramer1, Aaron M. Stoker1, Christina L. Goldstein1, Don K. Moore1, Theodore J Choma1, and James L. Cook1
1University of Missouri, Columbia, MO, USA
Introduction: Intervertebral disc (IVD) degeneration is implicated in back pain, a leading cause of a spine-related disability. Both local and systemic inflammatory processes have been associated with IVD degeneration, though it is unclear if differences between these processes exist in degenerative IVDs of patients undergoing lumbar microdiscectomy versus lumbar interbody fusion. To the authors’ knowledge, these differences have not previously been investigated. Hence, this study was designed to examine basal and cytokine-stimulated metabolic responses of degenerative lumbar IVD tissues collected from patients undergoing lumbar microdiscectomy or interbody fusion with the hypothesis that tissues from patients undergoing fusion would produce significantly higher levels of degradative enzymes and inflammatory mediators under both basal and cytokine-stimulated conditions when compared with tissues from patients undergoing microdiscectomy. Material and Methods: Tissue Collection and Culture: With institutional review board approval (IRB#2010692) and informed patient consent, degenerative IVDs excised as part of a standard-of-care spinal surgery, which would otherwise be discarded after lumbar microdiscectomy (n = 3) or fusion (n = 4) surgery was obtained from patients (n = 7, mean age 53, 4 females) being treated for symptomatic degenerative lumbar IVD disorders. Tissues composed of degenerative nucleus pulposus (NP) and annulus fibrosus (AF) were collected and explants of combined NP and AF (based on gross assessment) were created with a 6 mm diameter biopsy punch. Two explants per disc were randomly assigned to the 10 ng/mL IL-1β stimulation group (IL) or the untreated basal metabolism group (BASAL). Tissues were cultured for 3 days, after which media were collected for biomarker evaluation. Media Analyses: Media were tested for MMP-1, MMP-2, MMP-3, MMP-7, MMP-8, MMP-9, MMP-13, TIMP-1, TIMP-2, TIMP-3, TIMP-4, GRO-α, MCP-3, PDGF-AA, PDGF-AB/BB, IL-2, IL-4, IL-6, IL-8, MCP-1, MIP-1α, MIP-1β, RANTES, TNF-α, and VEGF using commercially available assays according to the manufacturer’s protocol. Statistical Analysis: Significant differences between groups were determined by t test or rank sum test based on normality of the data using SPSS with significance set at P ≤ .05. Results: In the BASAL group, the production of MMP-8 and TIMP-4 was significantly higher in the IVD tissues from the fusion cohort compared with that from the microdiscectomy group. In response to cytokine stimulation with IL-1β, tissues in the fusion group responded with significantly greater production of TIMP-2, TIMP-4, PDGF-AA, IL-6, IL-8, MIP-1β, and VEGF when compared with the response by the tissues from the microdiscectomy patients. Conclusion: These findings indicate that the basal inflammatory and degradative metabolism of degenerative lumbar IVD tissues collected from lumbar microdiscectomy versus fusion patients was not significantly different, since MMP-8 and TIMP-4 were the only biomarkers significantly different between the 2 patient groups. However, tissues from the lumbar fusion patients do appear to be more sensitive to cytokine stimulation compared with those from the microdiscectomy patients. The biochemical processes underlying, and clinical significance of, this observed difference require further study. A deeper understanding of this phenomenon may provide insight into potential therapies for prevention and treatment of both symptoms and progression of lumbar intervertebral disc degeneration.
P309: Establishment of a Large Cohort: Genetic Machinery of Lumbar Disc Disease
Hai-Qiang Wang1, Ping-Heng Lan2, Zhi-Heng Liu3, Chi-Jiao Ma4, Jun Zhang5, and Dino Samartzis6
1Shaanxi University of Chinese Medicine, Xi’an, China
2Xiang’an Hospital, Xiamen University, Xiamen, China
3Chinese PLA No.451 Hospital, Xi’an, China
4Ankang Hospital of Chinese Traditional Medicine, Ankang, China
5The First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
6Rush University Medical Center, Chicago, IL, USA
Introduction: Despite lumbar disc disease (LDD) affecting the health and welfare of global people greatly; the exact etiologic machinery remains elusive, in particular genetic roles. Accumulating evidence reveals family aggregation and early-onset type of LDD with undefined underlying mechanisms. Consequently, the study aimed for establishing a large cohort and unraveling the genetic roles in LDD. Material and Methods: With the approval of Institutional Ethic Committee and informed consent from patients and healthy participants, we collected peripheral blood, demographic data (including gender, age, body weight, height, diagnosis, treatment, family history of LDD), and clinical diagnostic imaging (if applied) with corresponding linked codes. DNAs from peripheral blood of each cohort member were extracted with quality control. All qualified DNA samples were saved appropriately. Results: In total, we have successfully established the LDD cohort in the past 4 years. The cohort consists of 853 persons with qualified DNA samples, excluding 27 cases with degraded DNA samples. There were 304 medical professionals, medical students (with or without low back pain/LDD family history), and 549 LDD patients. Among the 549 LDD patients, there were 127 patients from 34 pedigrees with LDD (participated family members range: 2-25) and other sporadic LDD patients. As an innovative for DNA collection, we verified, DNAs can be obtained noninvasively from drainage liquid instead of peripheral blood for patients undergoing lumbar surgery. Conclusion: Through years of efforts, we successfully established a large cohort for studying the genetic machinery of LDD. For surgical patients, DNAs can be obtained noninvasively from drainage liquid.
P310: Outcome of Ceramic on Ceramic Disc Arthroplasty in Cervical Spine
Palaniappan Lakshmanan1, Yehya Ghonem1, and Kathryn Ramshaw1
1Sunderland Royal Hospital, Sunderland, UK
Introduction: Cervical disc replacement is one of the promising options for the treatment of pain and disability of disc diseases, the use of an artificial prosthetic disc treatment modality provides pain relief while maintaining the mobility of the vertebral spines, these unprecedented advantages offered an option that can evade the main concerns that accompanies the traditional spinal fusion. The complications and outcomes of this treatment modality need further assessment to establish its short- and long-term validity and effectiveness. Material and Methods: We conducted a retrospective study to assess the outcome of the ceramic on ceramic disc arthroplasty of the cervical spine in terms of subsidence and the revision rates from 2013 to 2017 under a single surgeon. A total of 34 patients went disc replacement surgery using the ceramic on ceramic disc prosthesis. Subsidence rate was calculated as incidence rate, the end point was Subsidence on X-ray review after 6 months. The revision rate was calculated as incidence rate as well where the end point was a revision surgery being indicated at any time whether or not the operation was done. Results: Among the 34 patients, the mean age was 44 years, while the median was 45 years, the youngest patient was 31 years old and the oldest was 57 years old. The subsidence rate was 0.09% (only 3 patients experienced artificial disc subsidence) and revision rate of 0.06% (only 2 patients were indicated for revision of the disc replacement). Conclusion: Ceramic on ceramic arthroplasty of cervical spines can be successful with good clinical outcome and little complications including subsidence and the need for revision even in younger patients where excessive movement is expected.
P311: Disproportion of Vertebral Bodies and Its Impact on Lumbar Disc Herniation
Robin Brugger1, Sven Hoppe1, Christoph Albers1, and Ralph Läubli1
1Bern, Switzerland[
Introduction: The radiographic correlation of disproportional lumbar vertebral bodies and bilateral spondylolysis and degenerative changes of the disc has been described previously.1,2 Nevertheless, its clinical relevance has never been evaluated. The aim of this study was to analyze whether disproportion of vertebral bodies is a risk factor for disc herniation. Materials and Methods: Seventy-two patients (males:34, females: 38; mean age: 49years; range, 16-85 years) who underwent lumbar microdiscectomy due to symptomatic disc herniation between January 2013 and June 2018, could be included. In every patient Magnetic Resonance Images (MRI) of 3 motion segments (1 pathologic and 2 healthy) were analyzed for anteroposterior diameter of the caudal endplate of the upper compared with the cranial endplate of the lower vertebra body. Disproportion of the motion segment was defined as shortening of >10% of the anteroposterior diameter of the cranial endplate of the lower compared with the caudal endplate of the upper vertebral body. Results: In total, n = 216 motion segments were analyzed. The level of disc herniation was L5/S1 in 48.6%, L4/5 in 37.5% and L3/4 and L2/3 in 6.9%, respectively. In total, 26 disproportional motion segments were found (12.04%) (L5/S1: 18.06%; L4/5: 12.5%; L3/4: 5.56%). There was a significant difference between disc herniations in disproportional and normal motion segments (P < .01). Multiregression analysis revealed that disproportion of the motion segment triples the risk for disc herniation compared with normal (odds ratio: 3.04). Conclusion: Disproportion of the motion segment is a risk factor for disc herniation and triples the risk for its occurrence.
Reference
1. Frank DF, Miller JE. Hypoplasia of the lumbar vertebral body simulating spondylolisthesis. Radiology. 1979;133:59-60.
2. Kim SK, LeeSR, MoonWJ, et al. Regional disc change in segmental hypoplasia of the lumbosacral vertebral bodies. J Korean Radiol Soc. 2000;43:25-30.
P312: One-Way Street Disc Degeneration? An Investigation of Hydrogel and Fibroblast Growth Factor 18 (FGF-18) for Intervertebral Disc Regeneration
Sonja Haeckel1, Zhen Li2, Avner Yayon3, Sven Hoppe1, Lorin Benneker1, Mauro Alini1, and Sibylle Grad1
1University of Bern, Bern, Switzerland
2AO Research Institute Davos, Davos, Switzerland
3ProCore Bio Med Ltd, Ness Ziona, Israel
Introduction: The intervertebral disc (IVD), as the biggest avascular organ in the human body, has a low supply of nutrients and oxygen, resulting in a limited self-healing capacity. The healthy nucleus pulposus (NP) is rich in collagen 2 (COL 2) and water binding proteoglycans like Aggrecan (ACAN). During disc degeneration, collagen 1 (COL 1) is increasing in the NP tissue, which leads to a more fibrous and resistant tissue. This degenerative is still a 1-way street, because treatment strategies focusing on biological regeneration of the IVD are still missing. Therefore, we investigated a hyaluronic acid hydrogel (HA: FBG, RegenoGel), and the fibroblast growth factor 18 (FGF-18), which has been subject of clinical studies promoting cell differentiation and proliferation in cartilage tissue (which represents a similar situation as found in the avascular disc tissue).1,2 The aims of the present work were to investigate the regenerative effect of (1) HA: FBG hydrogel, and (2) FGF-18 on human and bovine NP cells in vitro. Material and Methods: Healthy bovine NP cells (n = 4, age 8-12 month) and human mildly degenerated NP cells (n = 4, age 30-55 years, Pfirrmann grade 2-3) were cultured for 14 days in a fibrinogen-hyaluronic acid (Fibrin-HA) hydrogel (RegenoGel, provided by ProCore, Israel). Cells were stimulated by adding FGF-18 (1, 10, and 100 ng/mL) in the culture medium. At day 7 and day 14, gene expression was measured by real-time RT-PCR (reverse transcription polymerase chain reaction); glycosaminoglycan (GAG) content in the gel and medium was evaluated by DMMB assay, and histology was performed by cryosection followed by safranin-o/fast green staining. Results: Aim (1): Both bovine and human NP cells encapsulated in the HA: FBG hydrogel, showed a donor dependent upregulation in gene expression for the anabolic marker Col 2 ([+]: 24× P < .01 in human NP cells) and Aggrecan ([+]: 13×, nonsignificant). Furthermore, an increase of glycosaminoglycans content in hydrogel over the time (P < .001) was detected. Aim (2): No significant difference on addition of FGF-18 were seen. In contrast to the biochemical analysis, histological sample revealed an increase in proteoglycan content in a dose dependent manner, this was more evident in bovine NP cells compared with the human NP cells. Conclusion: Analysis showed that the hydrogel supports cell function in already degenerated human disc cells. By adding FGF-18, we could not see a significant improvement of this effect at the tested experimental conditions. More pronounced matrix synthesis may be observed in longer term studies. The hydrogel might be a promising treatment option and could also be loaded with other drugs, with or without FGF18.
Reference
1. Ellsworth JL, Berry J, Bukowski T, et al. Fibroblast growth factor-18 is a trophic factor for mature chondrocytes and their progenitors. Osteoarthritis Cartilage. 2002;10:308-320.
2. Shapiro IM, Risbud MV. The Intervertebral Disc: Molecular and Structural Studies of the Disc in Health and Disease. Vienna, Austria: Springer-Verlag; 2014.
Epidemiology
P313: Consultation and Surgical Wait Times in Patients With Cervical Spondylotic Myelopathy: A Prospective Canadian Spine Outcomes and Research Network Study
Babak Sharifi1, Charles Fisher1, Raphaële Charest Morin1, Brad Jacobs2, Mike Johnson3, Chris Bailey4, Sean Christie5, Andrew Nataraj7, Neil Manson8, Hamilton Hall9, Ken Thomas2, Raj Rampersaud9, Greg McIntosh10, and Nicolas Dea1
1University of British Columbia, Vancouver, British Columbia, Canada
2University of Calgary, Calgary, Alberta, Canada
3University of Manitoba, Winnipeg, Manitoba, Canada
4University of Western Ontario, London, Ontario, Canada
5Dalhousie University, Halifax, Noa Scotia, Canada
7University of Alberta, Edmonton, Alberta, Canada
8Dalhousie University of Medicine, Saint John, New Brunswick, Canada
9University of Toronto, Toronto, Ontario, Canada
10Canadian Spine Outcomes and Research Network, Markdale, Ontario, Canada
Background: Cervical spondylotic myelopathy (CSM) is the leading cause of spinal cord impairment. Prompt surgical intervention halts clinical deterioration and results in clinical improvement in most patients; however, in a public health care system, wait times to see a spine specialist and eventually access surgical treatment may be substantial. The goals of this study were to assess the consultation wait time (CWT) and the surgical wait time (SWT), as well as to identify predictors of wait time length in this population. Methods: Consecutive patients enrolled in the Canadian Spine Outcomes and Research Network (CSORN) prospective, observational CSM study from March 2015 to July 2017, were included. Predictors of CWT and SWT were assessed using survival analysis. Results were stratified by disease severity based on the mJOA (Modified Japanese Orthopaedic Association). A data splitting technique was used to develop and test the multivariable models looking at potential predictive factors. Results: CSORN query returned 264 CSM patients for CWT (88 females and 176 males). Mean age was 59.4 years. The median CWT was 46 days. There were 31% mild, 35/% moderate, and 33% severe CSM. There was a statistically significant difference in median CWT between moderate and severe groups. There were 207 patients who underwent surgical treatment. Median SWT was 42 days. There was a statistically significant difference between mild/moderate and severe groups. Short symptom duration, less pain, radiologic cord compression, lower BMI (body mass index), and lower PCS (physical component score) scores were predictive of shorter CWT. On the other hand, SWT was mainly affected by pain and symptom duration. Both CWT and SWT were shorter for CSM patients compared with lumbar stenosis patients (P < .001). Conclusion: CSM patients with more severe symptoms had a shorter CWT and SWT. Patients with short symptom duration, less pain and spinal cord compression waited less to see a spine specialist in Canada. Patients with less pain and symptom duration less than a year had shorter SWT.
P314: Epidemiology of Adolescent Idiopathic Scoliosis in Students in the District Public Network Federal
Alessandro Leite1
1Ceilandia Regional Hospital, Brasilia, Brazil
Objective: The objective of this study is to investigate the prevalence of adolescent idiopatic scoliosis in school children aged 10 to 14 years of elementary school in Federal District, Brazil, participating in the Anisio Teixeira de Ceilandia park school in 2016. Methodology and Data Sources: Cross-sectional, observational study with students of both sexes from 10 to 14 years elementary school education in the Federal District, Brazil, from Parque Anisio Teixeira Ceilandia School, in 2016 for evaluation of the presence of scoliosis. With more than 1400 students, it was decided to draw 40% of this total. Participants were those who were randomly assigned to participate in the evaluation and excluded those with pathologies that influenced the genesis of idiopathic scoliosis. The cases that presented scoliosis were conducted for outpatient follow-up. From the information collection, we studied the variables of the practical applicability of the Z score, and calculated the data collected to facilitate the diagnosis of idiopatic scoliosis in the adolescent. Discussion: Adolescent idiopatic scoliosis has as unknow etiology and is defined as a lateral and rotational curve of the spine. There are no prevalence studies in our community. And within the collected sample 204 students were observed, (37.1%) of students with some type of alteration. The Adams test was performed, the plumb line test, the Talhe triangle survey, the asymmetrical height between the shoulders and shoulder blades. Those with some type of alteration in the physical examination were submitted to panoramic radiographs of the spine. An incidence of 2.1% of adolescent idiopatic scoliosis was confirmed in the Federal District. All students diagnosed with adolescent idiopatic scoliosis were referred to the clinic of the Ceilandia regional hospital for follow-up and treatment guidelines. Conclusion: Of the total number of students examined 549, 37.1% were suspected cases, and this total, 2.1% had a diagnosis of scoliosis. There was no predominance between the sexes. And the radiographic diagnosis perfomed in those who had 2 or more associated alterations, justifies the accomplishment of a physical examination well done and the beginning of an education program of research and awareness of health professionals and relatives in the relation to the early detection and treatment of idiopatic scoliosis adolescent.
P315: Racial Disparities in Surgical Outcomes After Spine Surgery: An ACS-NSQIP Analysis
Haley Taylor1, Zachary Sanford1, Justin Turcotte1, Amina Zaidi1, and Chad Patton1
1Anne Arundel Medical Center, Annapolis, MD, USA
Introduction: Racial disparities are a well-documented occurrence in postoperative outcomes relating to spine surgery, with higher comorbidity and postoperative burdens seen in African American (AA) populations. However, presently little to no literature is available on Native American (NA) individuals. In this study, we assess whether race is an independent risk factor for postoperative complications after spine surgery for AA and NA patients. Material and Methods: The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was queried for all spine procedures performed in 2015. Data was subdivided by surgery type, demographics, comorbidities, and 30-day postoperative outcomes, which were then compared between racial groups. Regression was performed holding race as an independent risk factor. Results: A total of 4308 patients were identified in the 2015 ACS-NSQIP database (4106 Caucasian, 522 African American [AA], 175 Native American [NA]). Other races (219 patients) were excluded due to insufficient reporting. AA patients experienced greater lengths of stay in all categories of surgery and longer OR (operating room) times (P < .001) excluding lumbar fusion, which were significantly shorter (P = .035). AA patients had a higher comorbidity burden, specifically for diabetes, hypertension, and smoking (P < .001), while NA also had increased rates of smoking (P < .001). Both AA and NA patients had higher morbidity probabilities (P = .020) excluding lumbar fusion, where NA patients had a lower morbidity probability (P = .048). Compared with Caucasians, AA race was an independent risk factor for longer length of stay (LOS; OR [odd ratio] = 1.541, P < .001) and operation time (OR = 12.212, P = .032) in cervical fusion, DVT (deep vein thrombosis; OR = 3.720, P = .017), longer LOS (OR = .767, P = .009), and shorter operation time (OR = −23.99, P = .016) for lumbar fusion, and superficial surgical site infections (SSIs; OR = 5.22, P = .001), pulmonary embolism (PE; OR = 5.76, P = .048), longer operation time (OR = 1.22, P < .001), longer LOS (OR = 20.94, P < .001) for decompression laminectomy. NA race was an independent risk factor for superficial SSIs following cervical fusion (OR = 14.58, P = .044) and decompression laminectomy (OR = 4.80, P = .021). Conclusion: AA and NA patients undergoing spine surgery have a disproportionate number of comorbidities and greater 30-day complications. AA and NA race independently affected rates of complications, LOS, and operation time.
P316: A Propensity Score-Matched Cohort Study on Traumatic Spinal Cord Injury Comparing Military Personnel Versus Civilians
Julio Furlan1,2, Dilnur Kurban3, and B. Catharine Craven1,2
1University Health Network, Toronto, Ontario, Canada
2University of Toronto, Toronto, Ontario, Canada
3Rick Hansen Institute, Vancouver, British Columbia, Canada
Introduction: Prior studies suggest that war-related spinal cord injury (SCI) may be different from traumatic SCI among civilians, but the literature is lacking comparative studies focused on the possible differences of SCI between the military and civilian subpopulations. Given this, 2 retrospective studies were undertaken to further clarify the potential differences in injury epidemiology, management, and outcomes after SCI between military personnel and civilians. Material and Methods: A retrospective cohort study (n = 1043) and a propensity-score matched cohort study (n = 100) were carried out using data from a Canadian multicenter SCI database. The retrospective cohort study included all individuals who were enrolled in the Rick Hansen Spinal Cord Injury Registry (RHSCIR) with sufficient data from October 2013 to January 2017. In the propensity-score matched cohort study, a group of 50 military personnel with SCI was compared with a group of 50 civilians with SCI who were matched on an 1:1 ratio using the propensity score matching on sex, age at the time of SCI, level and severity of SCI, and mechanism of injury. Results: In the retrospective cohort study, military personnel with SCI (n = 61) were significantly older and predominantly Caucasian men when compared with civilians with SCI (n = 982). However, the study groups were comparable with regard to their level and severity of SCI, mechanisms of injury, frequency of associated bodily injuries, and need for mechanical ventilation after SCI. In the propensity-score matched cohort study, the group of military individuals with SCI (n = 50) was statistically comparable to the group of civilians with SCI (n = 50) with regard to preexisting medical comorbidities, degree of motor impairment at admission, initial treatment for SCI, and clinical and neurological outcomes after SCI. Conclusion: The results of these studies suggest that military SCI group has disproportionally more Caucasian older males at the time of injury compared with civilians with SCI. However, the military and civilian SCI groups had similar outcomes of alike initial treatment when both groups were matched regarding their demographic profile and injury characteristics.
P317: Demographics, Presentation, and Symptoms of Patients With Klippel-Feil Syndrome: Analysis of a Global Patient Reported Registry
Aria Nouri1 ,2, Kishan Patel2, Hardy Evans1, Mohamed Saleh1, Mark Kotter3, Robert Heary4, Enrico Tessitore5, Michael Fehlings6, and Joseph Cheng1
1University of Cincinnati, Cincinnati, OH, USA
2Yale University, New Haven, CT, USA
3University of Cambridge, Cambridge, UK
4Rutgers University, Camden, NJ, USA
5University of Geneva, Geneva, Switzerland
6University of Toronto, Ontario, Canada
Introduction: Klippel-Feil syndrome (KFS) occurs due to failure of vertebral segmentation during development. Minimal research has been done to understand the prevalence of associated symptoms and pain. Here, we report one of the largest collections of KFS patient data. Material and Methods: Data were obtained from the CoRDS registry. Participants with cervical fusions were categorized into type I, II, or III based on the Samartzis criteria. Symptoms and comorbidities were assessed against type and location of fusion. Results: Seventy patients (60 females/14 males/1 unknown) were identified and classified as: type I, n = 21 (28%); type II, n = 15 (20%); and type III, n = 39 (52%). Cervical fusion by level were the following: OC-C1, n = 17 (22.7%); C1-C2, n = 24 (32%); C2-C3, n = 42 (56%); C3-C4, n = 30 (40%); C4-C5, n = 42 (56%); C5-C6, n = 32 (42.7%); C6-C7, n = 25 (33.3%); and C7-T1, n = 13 (17.3%). A total 94.6% of patients-reported current symptoms, and the average age when symptoms began and worsened was 17.5 (±13.4) and 27.6 (±15.3), respectively. Patients reported an average of 12.5 ± 7.1 comorbidities, and 12.2 ± 6.3 general and chronic symptoms. Sprengel deformity was reported in 26.7%. Multilevel fusions (Samartzis II or III) were associated with dizziness (P = .040), limited range in spine motion (P = .022), and Sprengel deformity (P = .036). Patients with cervical fusions: (1) in the upper region were more likely to report missing ribs (P = .018), craniocervical junction (CCJ) abnormalities (P = .022), cervical instability (P = .001), and mirror movements in hand (P = .041); (2) in the middle region were more likely to report osteoarthritis (P = .019), headaches, migraines, and/or head pain (P = .007); (3) in the lower region were more likely to report mirror movements in hand (P = .026), spina bifida occulta (P = .029), and cord tethering (P = .049). Conclusion: KFS is associated with multiple musculoskeletal and neurological problems. Fusions are more prevalent toward the center of the cervical region, and less common at the occipital and thoracic junctions. Associated comorbidities including Sprengel deformity may be more common with multilevel cervical fusions.
P318: Injuries in Contact Rugby at School Level in United Kingdom
Younus Hanif1, Mohammed Shahvaiz Younus2, Siddique Ather3, and Younus Hanif1
1Stoke, UK
2Great Ormond Street Hospital, London, UK
3Guys and St Thomas Hospital London, London, UK
Introduction: The primary aim of our project was to determine the injuries received by nonprofessional rugby players at sixth form colleges in the United Kingdom. Our secondary aim is to identify the areas involved in the injuries and how these injuries can be avoided in the future to make this game safer and enjoyable for all. Material and Methods: In this study, we will look at the main cause of injury, the most common type and site of injury, the position that is most at risk of injury, the mechanism of injury, time taken to recover from such injury, and finally if and how it can be prevented. Series of questions designed to help us collect the necessary information. The data was collected from sixth form students in Cambridge and 3 other counties. (Dorset, Northern Ireland, and Hertfordshire). All colleges were asked to complete a questionnaire about the type of injury mechanism, site, severity of injury, and so on. Results: A total of 44.64% of injuries were secondary to collision. The most common site of injury (30%) was blows to the head. Direct impact was found to be the most common mechanism resulting in injury (71.43%). A total of 50.9% of injuries require hospital treatment. The time taken for a player to recover was varied, as the majority (46.4) took up to a month to recover, 39.3% of players took up to 12 months to recover fully. Out of the 22 players who received a severe injury, the position that was most prone to such injury was the wing, followed by center, second row and props. The level of game did not make a difference to the injury as the results are varied. Thirty-two percent of injuries were during league games, closely followed-up by (27%) cup games, 23% were during friendlies, and finally 14% during training. Conclusion: It was our motive to bring the highly controversial and arguable debate regarding the health and safety of players in the most compelling and appealing sport among the youth. Sport in itself is not harmful but it does have adverse consequences. Just a few amendments and revision of rules and extra precautionary measures in the protection gear can make this sport even more entertaining yet safer for the players.
P319: Influence of Diabetes Mellitus on Patients With Lumbar Spinal Stenosis: A Nationwide Population-Based Study
Sun Kyu Choi1, Dong Ah Shin1, Seong Yi1, Yoon Ha1, Keung Nyun Kim1, Insoo Kim2, and Chang Kyu Lee2
1Yonsei University College of Medicine, Seoul, Republic of Korea
2Keimyung University Dongsan Medical Center, Daegu, Republic of Korea
Introduction: The prevalence of lumbar spinal stenosis (LSS) in patients with diabetes mellitus (DM) is growing. DM is associated with various chronic diseases, resulting in high socioeconomic cost, and negative surgical outcome. Previous studies reporting surgery for LSS patients with DM are relatively small cohort studies limited by sample size. The purpose of this study is to evaluate the relationship between comorbidities, medical cost, and surgical outcome in LSS patients with DM. Material and Methods: Data on the LSS patients (n = 14 298) was collected from the Korean National Health Insurance Service database. After 8 years of follow-up, a “DM group” (n = 3478) and a “non-DM group” (n = 10 820) were compared according to outcome measures. Cox proportional hazard regressions were used to examine the relationship between DM, hypertension (HTN), cardiovascular disease (CVD), chronic kidney disease (CKD), cerebrovascular disease (CbVD), and surgery for LSS. The admission rate and medical cost for LSS patients with DM and the overall survival rate for those who underwent lumbar surgery were also assessed. The authors have no financial disclosures related to this study. Results: The DM group had about 1.35 times higher mortality than the non-DM group. Patients with DM and comorbidities including HTN (hazard ratio [HR], 1.40; 95% confidence interval [CI], 1.25-1.56; P < .001), CVD (HR, 1.53; 95% CI, 1.36-1.73; P < .001), CKD (HR, 3.18; 95 CI, 2.7-3.76; P < .001), and CbVD (HR, 1.69; 95% CI, 1.49-1.91; P < .001) showed an increased risk of mortality. The mean hospitalization time and average medical expenses of the DM group were 34.9 days and USD1590, respectively. Particularly, the mean hospitalization time and average medical cost of DM patients who underwent lumbar surgery were 60.8 days and USD7127, which were 31.3 days longer and USD6207 higher than those of DM patients with conservative treatment for LSS. The survival rate of the DM group with surgery for LSS had a significant tendency for positive prognosis compared with that of the DM group with conservative treatment (P = .046). Conclusion: DM in LSS patients was associated with poor prognosis, most significantly in those with CKD, and increased medical cost in those who underwent surgery. Nevertheless, surgical treatment for LSS in DM patients was related to good prognosis compared with conservative treatment.
P320: The Relationship Between Sarcopenia and Lumbar Spinal Stenosis
Hirokazu Inoue1, Hideaki Watanabe1, Atsushi Kimura1, Ryo Sugawara1, and Katsushi Takeshita1
1Jichi Medical University, Shimotsuke, Japan
Introduction: The symptom of lumbar spinal stenosis includes as leg pain, leg numbness, leg muscle weakness, low back pain, and intermittent claudication. But few articles focus on the relationship between sarcopenia and lumbar spinal stenosis. In this study, we researched the relationship among intermittent claudication, muscle strength, the imaging analysis using CT (computed tomography) for lumbar spinal stenosis. Material and Methods: One hundred one patients (68 males, 33 females, mean age 69.8 years) underwent laminectomy for lumbar spinal stenosis from July 2015 through December 2016. We evaluated intermittent claudication the grip strength, the quadriceps strength, 10 m walk test (time and steps), the area of total muscle, and the multifidis using plain CT imaging at the third lumbar level, Psoas Muscle Index (PMI) before spine surgery. We diagnosis the sarcopenia by grip strength, walking speed, and PMI of L3 multifidis. Results: We diagnosed 4 patients (4%) as sarcopenia. Quadriceps muscle significantly correlated with grip strength (P < .001, r = .707), walking speed (P = .007, r = −.265), 10 m walking test (steps; P < .001, r = −.369), total muscle area at L3 level (P < .001, r = .526), multifidus muscle area (P < .001, r = .399), PMI (P = .009, r = .259). There was no correlation between intermittent claudication and the quadriceps strength. Conclusion: Sarcopenia was 4% in the patients with lumbar spinal stenosis. The more quadriceps strength the patients with lumbar spinal stenosis have, the more grip strength, the faster walking speed, the more area of multifidus muscle, the less steps of 10 m they have. However, their quadriceps strength has no relationship to intermittent claudication.
P321: Spine Surgery Outcomes: A Comparison of Patient Versus Surgeon Expectations From a Canadian Perspective
Ahmed Aoude1, Madison Lena Litowski1, Sultan Aldebeyan1, Raj Rampersaud3, Greg McIntosh4, Charles G. Fisher1, Alex Soroceanu1, and Kenneth Thomas1
1University of Calgary, Calagary, Alberta, Canada
2Toronto Western Hospital, Toronto, Ontario, Canada
3Canadian Spine Society, Markdale, Ontario, Canada
Introduction: Limited data exists comparing surgeon and patient expectations of outcome in spine surgery. Expectation has been shown to be directly linked to patient satisfaction after surgery and is therefore an important topic to investigate. To our knowledge, there is no data that exists in which patient and surgeon postoperative goals have been investigated in the Canadian spinal surgery community. The objective of this study was to elicit whether any differences exist between patient and surgeon expectations after spine surgery and if age plays a role in these differences. Material and Methods: A retrospective study from a prospectively collected database (CSORN) was conducted. To begin, 10 common clinical scenarios where generated and sent to Canadian spine surgeons to determine surgeon expectations for standard spine surgeries. Patients in the CSORN database were then identified with matching symptoms and procedures to those in the scenarios. Patient expectation data were then extracted and compared with surgeon responses. A chi-square analysis was then completed to determine discrepancies between surgeon and patient expectations. Results: A total of 51 Canadian spine surgeon completed the survey on expectation and 876 patients for multiple centers in Canada were identified in the CSORN database to match the clinical scenarios. Our results did demonstrate that patients tended to be more optimistic about the surgery expected outcomes in comparison to the treating surgeon. The majority of patients in all clinical scenarios analyzed in this study anticipated to have improvement in back or neck pain after surgery, which differed with statistical significance from surgeon expectations. Results also highlighted the effect of age on both patients and surgeons’ expectations. In general, all scenarios with younger patients tended to have higher number of positive expectations by the surgeons, which matched patient expectations compared with similar scenarios for older patients. Therefore, discrepancies between patient and surgeon expectations were higher for older patients. Conclusion: In this study, we present data on patient and surgeon expectation for spine surgeries and show that differences do exist. We also show that age plays a role in the agreement between the treating physicians and patients in regard to surgical expectations. Furthermore, this article shows discrepancies exist between our patients’ and our own expectations for common spine procedures. Overly optimistic patients with regard to surgery can lead to high dissatisfaction rate in spine surgery. This can also affect quality of life measures in patients anticipating higher functionality, which may not be obtainable from surgery. The reasons for the discrepancies between surgeon and patient expectations needs to be clarified and may be related to lack of adequate communication and documentation prior to surgery. These results encourage spine surgeons to clarify anticipated benefits of surgery with patients in order to improve patient satisfaction.
P322: Traumatic Spinal Cord Injuries in a North Tanzanian Referral Hospital
Mubashir Alavi Jusabani1, Sakina Mehboob Rashid1, Honest Herman Massawe1, and Marieke Cornelia Johanna Dekker1
1Kilimanjaro Christian Medical Centre, Moshi, United Republic of Tanzania
Introduction: Suffering a traumatic spinal cord injury (TSCI) in a low-income country such as Tanzania, often represents devastating damage to the quality of life for both the injured individual and their dependents. The establishment of the Orthopedic Rehabilitation Unit (ORU) in 2014 at Kilimanjaro Christian Medical Centre (KCMC) in Tanzania signified a major achievement for spinal cord injury (SCI) care in the country. A multidisciplinary team was formed in January 2018, comprising of an orthopedic surgeon, neurologist, occupational therapist, physiotherapist, and nurse, which reviewed every patient admitted to the KCMC Orthopedics and Trauma Ward and ORU. Following the introduction of multidisciplinary ward rounds for TSCI patients at KCMC, our objective was to present the burden of these injuries at our center. Due to the lack of resources and skill set at KCMC only 5 patients underwent spine fixation surgeries and the remaining majority were managed with halotraction (for cervical spine injuries) and bed rest (thoracic and lumbar spine injuries). Material and Methods: Multidisciplinary ward rounds were initiated in January 2018, comprising of the above team who reviewed every patient admitted to the KCMC Orthopedics and Trauma Ward and ORU. The study period was January 2018 to August 2018, and data were collected prospectively on every patient’s gender, age, cause of injury, level of injury, occurrence of secondary complications while in the ward and insurance cover. Results: A total number of 62 TSCI patients were admitted over the study period with a male preponderance of 50 (80.6%). The average age of the patients was 40.4 years with a range of 12 to 74 years. Falling from a tree (n = 25, 40.3%was the most common cause of injury, followed by involvement in motor traffic accidents (n = 18, 29.0%). Cervical SCIs were the most common (n = 34, 54.8%), followed by thoracic level (n = 16, 25.8%) and lumbar level SCIs (n = 12, 19.4%). Complete SCIs occurred in 19 (30.6%) patients and the incidence of secondary complications was 46.8%. The most common complication was pressure scores (27.4%. Only 30.6% of patients had insurance cover. Conclusion: TSCIs in a low-income country like Tanzania place a strain on the already scarce health resources. The average TSCI patient in our study population is a middle-aged male; previously able-bodied and the primary earner in the household, who now faces a drastic change in the quality of life. Review of our hospital’s past medical records has also demonstrated a decrease in the incidence of secondary complications (66.4% to 46.8%) following the introduction of the multidisciplinary ward round. The results of this short-term study highlight the dire need of spine surgery expertise as well as on-going TSCI rehabilitation services in North Tanzania.
P323: The Epidemiology of Low Back Injuries in the National Collegiate Athletic Association Athlete
Andrew Chung1, Jeff Hasselbrock1, Justin Makovicka1, and Anikar Chhabra1
1Mayo Clinic, Phoenix, AZ, USA
Introduction: To date, back injuries in National Collegiate Athletic Association (NCAA) athletes have not been well studied. As such, the purpose of this study was to describe the epidemiology of lower back injuries in NCAA athletes during the 2009-2010 to 2014-2015 academic years utilizing the NCAA Injury Surveillance Program (NCAA-ISP) database. Material and Methods: A convenience sample of NCAA varsity teams from 25 sports was examined to determine the rates and patterns of lower back injuries. Rates and distributions of back injuries were identified within the context of mechanism of injury, injury recurrence, and time lost from sport. Rates of injury were calculated as the number of injuries divided by the total number of athlete-exposures (AEs). AEs were defined as any student participation in 1 NCAA-sanctioned practice or competition with the inherent risk of exposure to potential injury. Injury rate ratios (IRRs) and injury proportion ratios (IPRs) were then calculated to compare the rates within and between sports by event type, season, sex, mechanism, injury recurrence, and time lost from sport. Comparisons between sexes were only made utilizing sports data that had both male and female samples. Results: A national estimate of 37 435 lower back injuries occurred over the 5-year period. The resultant overall rate of injury was 6.01 per 1000 AEs. The rate of back injuries in men was 4.94 per 1000 AEs, while women suffered injuries at a rate of 3.94 per 1000 AEs. In sex-comparable sports, men were 1.25 times more likely to suffer a back injury compared with women. Men’s football (24.6 per 1000 AEs) and women’s indoor track (8.84 per 1000 AEs) were the sports with the highest rates of back injuries. Back injuries were more 1.15 times more likely to occur during competition when compared with practice. Athletes were 1.8 and 3.7 times more likely to sustain a back injury during the preseason than compared with regular season or postseason, respectively. Noncontact was the most common mechanism of injury (38%). Injury recurrence was most common in men’s outdoor track (58.3%) and most back injuries resulted in < 24 hours of time loss from event participation (61.4%). Conclusion: Analysis of this data demonstrates a rate of relatively high rate of lower back injuries (6.010 lower back injuries per 1000 AEs). There was a significantly higher injury rate for men in sex comparable sports, and an overall higher injury rate in competition settings with the majority of injuries occurring via a noncontact mechanism. While the majority of injuries (79%) were new, there was a relatively high recurrence rate (20%). With the high rate of recurrence, reconditioning programs in addition to prevention programs, should be implemented to prevent these injuries. These programs would be particularly helpful in men’s football and women’s indoor track, sports that had the highest rate of lower back injuries.
P324: Determinants of Health as Predictors of a Major Complication After Spinal Fusion for Lumbar Spondylolisthesis
Christina L. Goldstein1, Jinpu Li1, Ryan Knigge1, Emily Leary1, and Theodore J Choma1
1University of MissouriColumbia, MO, USA
Introduction: Various risk factors for complications following spinal fusion for lumbar spondylolisthesis have been examined, though a comprehensive examination of the interplay between several determinants of health and the risk of postoperative major complications in this setting has not been performed. The purpose of this study is to determine those biological, environmental and health service variables related to the occurrence of a major complication after spinal fusion for lumbar spondylolisthesis using a uniform, multistate database approximating a 20% stratified sample of annual discharges from American community hospitals. Material and Methods: Using the 2014 National Inpatient Sample (NIS) dataset, the ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnostic codes for congenital (756.12) and degenerative/acquired (738.4) spondylolisthesis were used to identify admissions for study inclusion. Patient demographics, geographic location, length of stay, discharge destination, insurance, complication, and diagnosis data were extracted. Thirty diagnostic codes for diagnoses specific to a reoperation (eg, incision and drainage of hematoma) were used to code admissions as being associated with an unplanned reoperation. Admissions coded with a postoperative complication, reoperation, or patient death were identified as associated with a major complication and summed. Demographic, socioeconomic, geographic, and health factors for patients were summarized. Complication and reoperation rates were calculated and compared using chi-square or 2-sided t tests. Similarly, rates were compared between whites and non-whites. Demographic, socioeconomic, and geographic effects were examined for their association with major complication, using stepwise multivariate logistic regression analysis with a significance cutoff of .05. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: A total of 23 003 admissions with a mean age of 61.9 years were identified for study inclusion. A total of 61.6% of the admissions were females and 83.2% were white. Almost 1 in 4 (24.1%) admissions was associated with a postoperative complication, the total reoperation rate was 0.66%, and the in-hospital death rate was 0.07%. The total rate of a major complication was 24.4%, with the majority being postoperative complications. Accounting for all other covariates, older females with more chronic conditions and lower median household income, who lived in central countries of metro areas of greater than 1 million population in the West North Central region of the United States and who had a longer length of stay and were discharged somewhere other than home, were more likely to experience a major complication following admission for a lumbar spine fusion. Conclusion: This examination of the effect of a variety of determinants of health on the risk of major complications following lumbar fusion for spondylolisthesis, using the largest all-payer inpatient database in the United States, has identified disparities in outcomes related to demographics, social, physical, and health services determinants of health. These findings support a more in-depth analysis to identify that surgical indications, surgical approach, and patient characteristics would define high-risk patient populations to prevent major complications through alternative treatment strategies or increased resource allocation to optimize care.
P325: Determinants of Health as Predictors of a Major Complication After Lumbar Spine Fusion
Austin Sanders1, Jinpu Li1, Ryan Knigge1, Emily Leary1, Theodore J Choma1, and Christina L. Goldstein1
1University of Missouri, Columbia, MO, USA
Introduction: Complication rates after lumbar spine fusion range from 5.6% to 31.4%. Multiple investigations have examined risk factors for complications following lumbar spine fusion, though none have performed a comprehensive investigation of the association between a variety of determinants of health and the risk of postoperative major complications in this setting. The purpose of this study is to determine those variables related to the occurrence of a major complication after lumbar spine fusion using a uniform, multistate database approximating a 20% stratified sample of annual discharges from American community hospitals. Material and Methods: Using the 2014 National Inpatient Sample (NIS) dataset, ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) procedure codes for lumbar spine fusion were used to identify admissions for study inclusion. Patient demographics, geographic location, length of stay, discharge destination, insurance, complication, and diagnosis data were extracted. Thirty diagnostic codes for diagnoses specific to a reoperation (eg, incision and drainage of hematoma) were used to code admissions as being associated with an unplanned reoperation. Admissions coded with a postoperative complication, reoperation, or patient death were identified as associated with a major complication and summed. Demographic, socioeconomic, geographic, and health factors for patients were summarized. Complication and reoperation rates were calculated and compared using chi-square or 2-sided t tests. Similarly, rates were compared between whites and non-whites. Demographic, socioeconomic, and geographic effects were examined for their association with major complication, using stepwise multivariate logistic regression analysis with a significance cutoff of 0.05. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: A total of 57 248 admissions with a mean age of 57.3 years were identified for study inclusion. A total of 55.3% of the admissions were females and 81.4% were white. More than 1 in 4 (26.2%) admissions was associated with a postoperative complication, the total reoperation rate was 0.99%, and the in-hospital death rate was 0.19%. The total rate of a major complication was 26.6%, with the majority being postoperative complications. Accounting for all other covariates, non-white females with more chronic conditions and lower median household income, who lived in central countries of metro areas of greater than 1 million in population in the West North Central region of the United States and who had a longer length of stay and were discharged somewhere other than home, were more likely to have experienced a major complication following admission for a lumbar spine fusion. Conclusion: This examination of the effect of sociodemographic and perioperative variables on the risk of major complications, including a postoperative complication, unplanned reoperation, or in-hospital death, using the largest all-payer inpatient database in the United States, has identified disparities in outcomes related to social determinants of health, burden of comorbid disease, and postoperative course. These findings support a more in-depth analysis to identify, which surgical indications, fusion procedures, and patient characteristics would better identify high-risk patient populations for which alternative treatment strategies may result in better health outcomes or to increase resource allocation to optimize episode of care for these patients.
P326: Flipped Classroom Is an Effective Educational Method for Spine Deformity Courses
Alpaslan Senkoylu1, Berkay Senkoylu2, Ozlem Coskun3, Irem Budakoglu1, and Emre Acaroglu3
1Gazi University, Ankara, Turkey
2Hacettepe University, Ankara, Turkey
3ARTES Spine Center, Ankara, Turkey
Introduction: The so-called “flipped classroom” model of blended learning, including online prelearning and small group discussions, became popular because it facilitates learning by affording more interaction between teachers and learners. It is in accordance with the constructive theory of learning, which suggests a more effective learning environment by active and voluntary individuals interacting in groups. However, there is no evidence on its effectiveness in spine deformity surgery. Aim of current study is to assess efficiency of flipped classroom on spine deformity education by using outcome measures. Materials and Methods: Subjects: Following an open call, 39 participants applied to a course designed as a flipped classroom for basic pediatric deformity. Thirteen of them (group A) attended to the face-to face (F2F) part and the rest (group B) did not. These 2 groups were compared by their quiz scores. Structure of Course: The online part was 3-week long and every week had specific sessions with online learning material based on predetermined learning outcomes (LO). Following these 3 weeks, a F2F part based only on small group case discussions was executed. Outcome Measures: A quiz with 20 questions, which covers all LO was composed. Twelve of these representing a thorough and even distribution of LO were chosen as a core quiz and was validated on peers who would not attend this course. This quiz was completed by group A before and after the online part as well as following the F2F course. Group B completed the quiz just before and after online part. The baseline quiz scores of the groups were similar (P = .368). Both groups demonstrated significant increases in scores at the end of the pre-learning (P = .014). Group A furthered this improvement at the end of the F2F learning significantly (P = .023) (Table 1). Results: Scores of group A were significantly better than those of group B and also scores within group B significantly improved at the end (Table 1). Conclusion: Flipped classroom is an effective method for such a complex surgical subspecialty. Participants progressed significantly in both parts of the basic pediatric deformity course. These results suggest that a flipped class room model based on a theoretical background of construction theory may be the ideal method in spinal surgery education.
Table 1.
a
| Group A | Group B | |
|---|---|---|
| Before online part | 5.4 (0.0-9.2) | 5.4 (0.0-7.9) |
| After online part | 6.8 (4.2-9.6) | |
| After face-to-face part | 7.9 (6.8-8.9) | 6.8 (5.1-9.3) |
a Median (minimum-maximum).
P327: Risk Factors for 30-Day Unplanned Readmissions After Posterior Lumbar Fusion: A Nationwide Readmissions Database Study
Brian Cho1, Ivan Ye1, Ray Tang1, Andrew Warburton1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1 Mount Sinai Health System, New York, NY, USA
Introduction: Unplanned hospital readmissions in the United States are a significant burden on the continually rising national health care expenditures. With the rise of value-based payment models and hospital penalties for unplanned readmissions, there has been increasing interest in understanding risk factors for readmission following surgery in order to alleviate the associated cost burden and improve quality of care. Posterior lumbar fusion (PLF) is one of the most common procedures in spine surgery, and the rate of PLF being performed annually continues to increase. The objective of this study was to use the Nationwide Readmissions Database (NRD) from the Healthcare Cost and Utilization Project (HCUP) to determine risk factors for 30-day readmission following elective PLF. Material and Methods: A retrospective cohort study was performed using the 2012-2014 NRD. ICD-9 (International Classification of Diseases, Ninth Revision) diagnosis codes and procedure codes were used to identify elective PLF cases. The primary outcome of interest was all-cause 30-day readmission. Baseline patient characteristics included demographics, medical comorbidities, discharge destination, and insurance type. Bivariate analysis was performed to identify covariates associated with 30-day readmission and adjusted with the Bonferroni correction for multiple testing correction. A multivariate regression analysis was then performed with a model that was fitted using significant covariates from the bivariate analysis in order to identify independent risk factors associated with 30-day readmission. Results: A total of 126 913 elective PLF were included in this study. The overall 30-day readmission rate was 6.23% (7915/126913). Of the 35 baseline patient characteristics examined, 29 were covariates and significantly associated with other characteristics in the bivariate analysis for 30-day readmission. In the subsequent multivariate regression analysis, 24 variables were found to be independent predictors of 30-day readmission. The strongest predictors were a diagnosis of metastatic cancer (odds ratio [OR] = 4.70; 95% confidence interval [CI] = 3.82-5.78; P < .001), discharge to a short-term hospital (OR = 2.18; 95% CI = 1.84-2.58; P < .001), age older than 90 years (OR = 1.90; 95% CI = 1.45-2.51; P < .001), discharge to a skilled nursing or intermediate care facility (OR = 1.88; 95% CI = 1.81-1.96; P < .001), and Medicaid insurance (OR = 1.72; 95% CI = 1.59-1.86; P < .001). Conclusion: This study demonstrated a national 30-day unplanned readmission rate of 6% after elective PLF. Age, metastatic cancer, Medicaid insurance, and discharge to a short-term hospital or skilled nursing facility were the strongest independent predictors of 30-day readmission. As the population continues to age and the rate of PLF increases, more studies are needed to develop effective preventive strategies for reducing unplanned readmission following surgery in order to improve patient outcomes and quality of care, as well as reduce health care costs.
P328: Ontario Inter-Professional Spine Assessment and Education Clinics (ISAEC): Patient, Provider, and System Impact of an Integrated Model of Care for the Management of Low Back Pain (LBP)
Raja Rampersaud1 on behalf of ISAEC Evaluation Team
1 Krembil Research Institute, University Health Network, Toronto, Ontario, Canada
Introduction: Inter-Professional Spine Assessment and Education Clinics (ISAEC) uses an interdisciplinary shared-care model to provide upstream secondary and tertiary standardized clinical evaluation, stratified education, and self-management recommendations for low back pain (LBP) patients. ISAEC was designed to integrate care between ongoing patient self-management, primary care, and specialist care including standardized imaging and referral criteria. The objectives of this study are to determine the impact of an evidence-based shared-care model of care (ISAEC) on: (1) patient-reported satisfaction and outcome; (2) primary care provider (PCP) satisfaction and knowledge transfer; (3) surgical referral appropriateness; and (4) utilization of spinal imaging from the perspective of the health care system. Material and Methods: (1) Mixed methods study for patient and provider evaluation (patient reported outcomes measures (Oswestry Disability Index [ODI]/Start Back Chronicity Risk Assessment) as well as process and satisfaction surveys. (2) Institute for Clinical Evaluative Sciences (ICES) administrative data analysis comparing spine imaging test ordering by ISAEC and non-ISAEC physicians and determine the direct cost impact. Results: From November 2012 to February 2016, 4532 patients have been assessed. The mean wait time for secondary assessment was 12 days. The majority of patients (68%) were diagnosed with back-dominant pain. The majority of presentations (68%) were considered complex (eg, positive for psychosocial factors [52.2%]). Patient satisfaction (n = 1922) was 99%, and 95% felt they understood their condition better. For 811 patients enrolled in a longitudinal study, 54% of patients reported a perceived improvement in their symptoms with a mean reduction in ODI score of 10 was observed at 6 months (baseline = 36%/6 months = 26%). At 4 and 12 months into the program, enrolled PCPs (n = 134/220) on average showed a 2-fold increase in their confidence managing LBP (assessment and management, referral for imaging, and specialist consultation). Ninety-seven percent of PCPs reported overall satisfaction with the ISAEC model of care and felt that ISAEC services would be useful to all PCPs. Within the ISAEC network of providers, surgical referral appropriateness was 96% (compared with 20% to 30% prior to ISAEC) and <4% of overall ISAEC patients have gone on to surgical interventions. Average wait-time for surgical assessment was 5.4 weeks, 4.3 weeks, and 2.2 weeks at the metropolitan, urban, and rural centers, respectively, compared with 6 to 18 months prior to formation of the ISAEC network. Compared with non-ISAEC PCPs, the overall annual utilization for all LBP-related diagnostic imaging ordered by ISAEC-PCPs fell 28% in year 1 and an additional 5% in year 2 compared with their non-ISAEC peers. This translated to an annual estimated per physician cost avoidance of $3150 and $4175 in year 1 and 2, respectively, based only on imaging. Conclusion: In single-payer public health care delivery system, a shared-care, stratified education, and self-management model of care for LBP provides significant positive multidimensional impact on patients, providers, and the health care system. Overall, the ISAEC model was able to improve on the quality and appropriateness of care, while reducing cost.
P329: Machine Learning Can Identify Subpopulations of Depression that Pose Greater Risk for Postoperative Complication Following Lumbar Fusion
Andrew Warburton1, Varun Arvind1, Brian Cho1, Jun S. Kim1, and Samuel K. Cho1
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Many postoperative complications have been characterized and correlated in postoperative spinal fusion patients. Mental health has emerged as an important contributing factor to clinical outcomes following spinal fusion; however, little work has been performed to identify populations of patients with psychiatric illness with increased or decreased risk. Machine learning has proven to be a powerful tool to gain insight into layered comorbidities and possible complications. Furthermore, machine learning techniques can cluster patients within populations to find subgroups that are vulnerable to future complications postoperatively. The purpose of this study was to develop a machine learning algorithm that can identify unique patient clusters within depressed postoperative lumbar spinal fusion patients and any complications that were statistically different between the 2 groups. Materials and Methods: This was a retrospective analysis of the National Readmissions Database (NRD), a part of the Healthcare Cost and Utilization Project that provides national readmission rates for insured and uninsured patients. The compiled NRD data for the depressive comorbidity was coded under the following International Classification of Diseases, Ninth Revision (ICD-9) (codes: 29383, 29620, 29621, 29622, 29623, 29624, 29625, 29626, 29630, 29631, 29632, 29633, 29634, 29635, 29636, 3004, and 311). ICD-9 codes for cardiac complications were (410 and 9971). ICD-9 codes for pulmonary complications were (9973, 99731, 99732, 51851, 51852, 51853). ICD-9 codes for thromboembolism complications were (41511, 41513, 41519, 45111, 45119, 4512, 45181, 45340, 45341, 45342). K-means clustering, partitioning around medoids (PAM) clustering, and hierarchical clustering were used and compared against each other to support results. Statistical analysis was performed using an independent 2-group t test. Significance was defined as P < .05 to allow for a 95% confidence interval. Results: A total of 126 913 patients were indented from 2012-2014 NRD datasets as having undergone lumbar spinal fusion (IDC-9: 8107). A total of 20 354 of the patients (16.04%) were coded as depressed. Within the depressed patient population, 2 subgroups emerged from clustering (n1 = 20,227, n2 = 77). The first group had an average age of 60.05. The first group is 71.35% female and the second group is 81.81% female, which proved to be statistically significant (P age = .0197). The second group had an average age of 59.08. Three complications were analyzed: cardiac, pulmonary, and thromboembolism complications. Cardiac and pulmonary complications within the depressed patients was statistically significant between the 2 clusters (P cardiac = .02698, P pulmonary = .2676) whereas thromboembolism complications were not found to be significantly different (P thromb = .36240). Conclusions: Implementing machine learning algorithms to cluster subgroups of depressed postoperative patients is a powerful method for visualizing and predicting future complications. This clustering method provides a valuable tool for surgeons to identify at risk subpopulations within depressed patients that may require further management or consultation to improve outcomes within this at-risk cohort.
P330: The Ponticulus Posticus: Prevalence and Case Report of C1 Lateral Mass Screw in a Patient With This Anomaly
Emanuel Zaragoza1, and Federico Gelosi1
1Austral University Hospital, Pilar, Buenos Aires, Argentina
Introduction: The ponticulus posticus or arcuate foramen is an osseous anomaly of the atlas, specifically on posterior arch, which has to be taken into consideration during placement of lateral mass screw into the atlas to avoid injuring the vertebral artery. Material and Methods: Through a retrospective review of 650 lateral radiographs of the neck was determined the prevalence of ponticulus posticus in our patient population. Also one of the patients with ponticulus was operated with C1-C2 instrumentation due to atlanto-axial osteoarthritis. Results: The prevalence of arcuate foramen was 14.9% in our population. Almost were male gender (70%). The case report was of a 72-year-old woman with chronic neck pain due to atlanto-axial osteoarthritis. She was operated with C1 lateral mass screw taking into consideration the ponticulus posticus. The patient responded well to surgical intervention without complications. Conclusion: The ponticulus posticus is a common anomaly, it is often not recognized. Identification of this anomaly on preoperative lateral radiographs should alert the surgeon to avoid using the ponticulus posticus as a starting point for a lateral mass screw. We recomended to find specifically the lateral mass, below of the posterior arch, as starting point for the C1 screw in patient with ponticulus posticus.
P331: Liver Disease Is a Risk Factor for 30-Day Complications Following Adult Spinal Deformity Surgery
Ray Tang1, Ivan Ye1, Brian Cho1, Samuel White1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Mount Sinai Health System, New York, NY, USA
Introduction: The effect of underlying liver disease on surgical outcomes has been thoroughly studied in various surgical subspecialties. In comparison, however, it has not been as well investigated in spine surgery. Adult spinal deformity (ASD) is becoming increasingly prevalent with an aging population. Corrective surgery for ASD is often complex and requires not only thorough preoperative planning from a technical standpoint, but also in the assessment of the patient’s medical condition in order to minimize complications and associated health care costs. The objective of this study was to identify 30-day perioperative complications that were independently associated with liver disease in patients undergoing elective surgery for ASD. Material and Methods: This was a retrospective cohort study of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2008 to 2014. Adult patients who underwent elective corrective surgery for ASD were identified and divided into 2 groups based on liver disease, which was assessed with the Model of End-stage Liver Disease–Sodium (MELD-Na) score. Liver disease was defined as a MELD-Na score ≥10. Baseline patient characteristics, comorbidities, and operative factors were compared between the 2 groups. Univariate analysis was performed to identify differences in 30-day perioperative complications between the 2 groups. After adjusting for confounding variables, a multivariate regression analysis was performed to determine perioperative complications that were independently associated with liver disease. Results: A total of 2337 patients were included in this study. The rate of liver disease in this cohort was 13.9% (325/2337). The liver disease group had a higher rate of 30-day pulmonary complications (6.3% vs 2.9%), blood transfusion (34.6% vs 23.9%), sepsis (2.2% vs 0.9%), and prolonged length of stay (19.0% vs 8.0%). The liver disease also had a higher rate of any 30-day perioperative complication (45.4% vs 29.4%). The multivariate analysis found that liver disease was independently associated with any 30-day complication (odds ratio [OR] = 1.43; 95% confidence interval [CI] = 1.15-1.77; P = .001), pulmonary complications (OR = 1.78; 95% CI = 1.16-2.74; P = .009), blood transfusion (OR = 1.67; 95% CI = 1.36-2.05; P < .001), and prolonged length of stay (OR = 2.16; 95% CI = 1.64-2.84; P < .001). Conclusion: In this ACS-NSQIP database study, liver disease was found to be an independent risk factor for any 30-day postoperative complication, pulmonary complications, blood transfusion, and prolonged hospitalization following corrective surgery for ASD. Liver function should therefore be considered in the preoperative assessment of patients for ASD surgery in order to identify patients at higher risk for perioperative complications.
P332: Return to Work After Spinal Fracture Surgery: An Analysis of Predictive Factors
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler i Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Objective: To retrospectively evaluate factors that influence the return to work of patients of economically active age submitted to surgery due to spinal fractures. Methods: Patients aged between 18 and 65 years who underwent surgery after spinal fracture from 2012 to 2014 were selected. Through a specific questionnaire and review of the medical records, we identified factors that may have influenced the labor return of these patients. Results: Initially, 114 patients were allocated. After applying the inclusion criteria, 51 patients remained. Age, schooling, time to sit on the bed, and residual pain were the factors that influenced all outcomes. Other variables such as ISS (Injury Severity Score), segment of spine, number of affected vertebrae, associated lesions, and previous employment regimen had no influence. Conclusions: The rate of return to work after being submitted to surgery due to a fracture of the spine is related to age, schooling, residual pain, length of hospital stay, and the time the patient takes to be able to sit alone postoperatively. Physiotherapy positively influences the patient’s self-assessment regarding the ability to perform basic tasks. These variables can be used to identify a possible difficulty in the reallocation of these patients in the labor market.
P333: Determinants of Health as Predictors of a Major Complication After Cervical Spine Fusion
Garrett Mitchell1, Jinpu Li1, Ryan Knigge1, Emily Leary1, Theodore J. Choma1, and Christina L. Goldstein1
1 University of Missouri, Columbia, MO, USA
Introduction: Complication rates following cervical spine fusion have been estimated to range from 11% to 38%. Prior investigators have examined risk factors for complications following cervical spine fusion; however, none have performed a comprehensive investigation of the association between a variety of determinants of health and the occurrence of a major postoperative complication in this setting. The purpose of this study is to determine those associations between demographic, geographic, and health factors with the occurrence of a major complication after cervical spine fusion using a uniform, multistate database approximating a 20% stratified sample of annual discharges from American community hospitals. Materials and Methods: Using the 2014 National Inpatient Sample (NIS) dataset, ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnostic codes for cervical spine fusion were used to identify admissions for study inclusion. Patient demographics, geographic location, length of stay, discharge destination, insurance, complication, and diagnosis data were extracted. Thirty diagnostic codes for diagnoses specific to a reoperation (eg, incision and drainage of hematoma) were used to code admissions as being associated with an unplanned reoperation. Admissions coded with a postoperative complication, reoperation, or patient death were identified as associated with a major complication and summed. Demographic, socioeconomic, geographic, and health factors for patients were summarized. Complication and reoperation rates were calculated and compared using chi-square or 2-sided t tests. Similarly, rates were compared between whites and non-whites. Demographic, socioeconomic, and geographic effects were examined for their association with major complication, using stepwise multivariate logistic regression analysis with a significance cutoff of 0.05. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: A total of 36 623 admissions with a mean age of 56.3 years were identified for study inclusion. A total of 49.6% of the admissions were females and 78.5% were white. Moreover 12.2% of the admissions were associated with a postoperative complication, the total reoperation rate was 0.73%, and the in-hospital death rate was 0.43%. The total rate of a major complication was 12.6%, with the majority being postoperative complications. Accounting for all other covariates, older females with more chronic conditions, living in central counties of metro areas of greater than 1 million people in the West South-Central region of the United States, who had a longer length of stay, and were discharged somewhere other than home were more likely to have experienced a major complication following admission for a cervical spine fusion. Conclusions: This examination of the effect of sociodemographic and perioperative variables on the risk of major complications following cervical spine fusion, including a postoperative complication, unplanned reoperation, or in-hospital death, using the largest all-payer inpatient database in the United States, has identified disparities in outcomes related to biological, physical, and health services determinants of health. These findings support a more in-depth analysis to identify which surgical indications, fusion procedures, and patient characteristics that would define high-risk patient populations who may be better served using alternative treatment strategies or who require increased resource allocation to optimize their episode of care.
P334: Determinants of Health as Predictors of a Major Complication in Inpatients With Spine Trauma
Jason Tegethoff1, Jinpu Li1, Ryan Knigge1, Emily Leary1, Theodore J. Choma1, and Christina L. Goldstein1
1University of Missouri, Columbia, MO, USA
Introduction: Multiple investigations have examined risk factors for complications following spine trauma, though none have examined associations between determinants of health and complications in these patients. The purpose of this study is to determine those biological, environmental, and health service variables related to the occurrence of major complications following admission of patients with spine trauma using a uniform, multistate database approximating a 20% stratified sample of annual discharges from American community hospitals. Materials and Methods: The 2014 National Inpatient Sample (NIS) dataset and ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) diagnostic codes for closed cervical (805.00-805.07, 806.0_) and thoracolumbar/lumbar (805.2, 806.2, 805.4, and 806.4_) fractures with and without a spinal cord injury were used to identify admissions associated with a spine fracture. Demographic, geographic location, length of stay, discharge destination, insurance, complication, and diagnosis data were extracted. Unplanned reoperations following any surgical procedure were coded using 30 diagnostic codes for diagnoses specific to a reoperation following any surgical procedure (eg, incision and drainage of hematoma). Admissions coded with a postoperative complication, reoperation, or patient death were aggregated and coded as being associated with a major complication. Demographic, socioeconomic, geographic, and health factors for patients were summarized. Complication and reoperation rates were calculated and compared using chi-square or 2-sided t tests. Similarly, rates were compared between whites and non-whites. Determinants of health were examined for their association with major complication, using stepwise multivariate logistic regression analysis with a significance cutoff of 0.05. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: A total of 44 177 admissions with a mean age of 62.6 years were identified for study inclusion. A total of 47.0% of the admissions were females and 79.0% were white. Almost 1 in 2 (48.1%) admissions was associated with a complication, the total reoperation rate after all surgical procedures was 0.67%, and the in-hospital death rate was 4.0%. The total rate of a major complications was 42.7%, with the majority being a complication as opposed to reoperation or death. Accounting for all other covariates, older females with more chronic conditions, lower median household income, who lived in central counties of metro areas of greater than 1 million in population in the West North-Central region of the United States, who had a longer length of stay, and were discharged somewhere other than home, were more likely to have experienced a major complication following admission with a comorbid spine fracture. Conclusions: This examination of the effect of determinants of health on the risk of major complications following hospital admission with a comorbid spine fracture, using the largest all-payer inpatient database in the United States, has identified disparities in outcomes related to biological, social, physical, and health services determinants of health. These findings support a more in-depth analysis to identify which fracture, injury, and patient-related variables defining high-risk patient populations, as well as how these variables and determinants of health relate to fracture management. This information will inform decisions regarding resource allocation and treatment to optimize care in patients with spine fractures.
P335: Lumbar Spinal Implant Detection by Current Metal Detectors
Sebastian Fras1 and Christian Fras1
1Institute for Spinal Surgery, Broomall, PA, USA
Introduction: Security measures at airports and government buildings typically includes use of walk-through metal detectors, prompting inquiries from many patients prior to lumbar spinal instrumentation procedures. Previous medical literature suggests a significant incidence of detection of orthopedic implants by metal detectors, with recent studies indicating a decrease in this incidence, possibly related to greater refinement of the metal detectors. Prior studies have suggested that stainless steel and cobalt chrome implants in scoliosis correction surgery may trigger alerts by metal detectors. This study was undertaken to assess if modern titanium alloy implants used specifically in the lumbar spine triggered alerts in metal detectors currently in actual use in the United States. Materials and Methods: A telephone interview was conducted with patients who had undergone lumbar instrumented fusion within the past 7 years, and inquiring if the patient had gone through a walk-through metal detector at an airport or courthouse within the past 2 years; and, if so, if they had triggered an alert. All patients had 1 of 2 types of titanium alloy pedicle screw implants: Medtronic TSRH or Globus BEACON. The results were then tabulated. Results: Fifty consecutive patients who met the above-mentioned criteria and who had passed through a metal detector were contacted. Of these, 20 had 4 pedicle screws inserted; 25 had 6 screws inserted; and 5 had more than 6 screws inserted. Twelve had passed through a metal detector once; 38 had passed through a metal detector more than once. None of the patients ever triggered an alert of a walk-though metal detector. There were 0 (0/50) patients who reported triggering an activation after they had passed through a metal detector. Conclusion: In previously published studies, the frequency of detection in patients with orthopedic implants in walk-through metal detectors varied based on the nature of the implant and the age of the study; in the past, total hip replacements triggered alerts more frequently than other implants, with the overall incidence of detection noted to be less frequent in more recent studies than in older studies. In the spine literature, studies have noted alerts to have been triggered in some (but not all) patients with stainless steel and/or cobalt chrome implants for scoliosis correction. In this study focusing on titanium pedicle screw implants in the lumbar spine, there were no alerts in 50 consecutive patients with recent experiences going through metal detectors in the United States. This information may be used to reassure patients about to undergo lumbar spine instrumentation with titanium implants that passing through a metal detector is not expected to trigger an alert, and that medical documentation of the presence of such implants is not needed.
P336: The Epidemiology of Low Back Injuries in the National Collegiate Athletic Association Football Athlete
Justin Makovicka1, Andrew Chung1, Jeff Hasselbrock1, and Anikar Chhabra1
1Mayo Clinic, Phoenix, AZ, USA
Introduction: There is a paucity of literature on back injuries in National Collegiate Athletic Association (NCAA) football players. Therefore, the purpose of this study was to describe the epidemiology of back injuries in NCAA football players during the 2009/2010-2014/2015 academic years utilizing the NCAA Injury Surveillance Program (NCAA-ISP) database. Material and Methods: A convenience sample of NCAA varsity football teams was utilized to determine the rates and patterns of back injuries. Rates and distributions of back injuries were identified within the context of mechanism of injury, injury recurrence, and time lost from sport. Rates of injury were calculated as the number of injuries divided by the total number of athlete-exposures (AEs). AEs were defined as any student participation in one NCAA-sanctioned practice or competition with the inherent risk of exposure to potential injury. Injury rate ratios (IRRs) were then calculated to compare the rates of injury between season, event type, mechanism, injury recurrence, and time lost from sport. Results: Nationally, there were an estimated 7076 back injuries over the 5-year period, 82% of which were new injuries. These occurred at a rate of 24.42 per 1,000 AEs. Overall, injuries were 2.05 times more likely to occur in competition than in practice. Athletes were 3.10 times more likely to sustain a back injury during the regular season compared with postseason but were 1.57 times as likely to sustain a low back injury during the preseason compared with regular season. Both contact and noncontact were reported equally as the mechanism of injury (38% each) and unspecified low back pain was the most common injury (64%). Outside of low back pain, the most common injury diagnoses were contusions (12%), sacroiliac injuries (8%), and disc injuries (8%). Only 2% of patients required surgery for their injury, and the majority of athletes (60%) returned to play within 24-hours. Conclusion: There was a relatively high rate of lumbar back injuries at the college level (24.42/1000 AEs)—the majority of which were new injuries. About 18% of athletes were reinjured. The highest risk of injury was during regular season competition. Although very few required surgery, careful examination and workup should be conducted to evaluate each injury. Regimented physical therapy and reconditioning programs are recommended to avert reinjury.
P337: The Epidemiology of Low Back Injuries in the National Collegiate Athletic Association Basketball Athlete
Justin Makovicka1, Jeff Hasselbrock1, Andrew Chung1, and Anikar Chhabra1
1Mayo Clinic, Phoenix, AZ, USA
Introduction: There is a paucity of literature on back injuries in National Collegiate Athletic Association (NCAA) basketball players. Therefore, the purpose of this study was to describe the epidemiology of back injuries in NCAA men’s and women’s basketball players during the 2009/2010-2014/2015 academic years utilizing the NCAA Injury Surveillance Program (NCAA-ISP) database. Material and Methods: A convenience sample of NCAA varsity men’s and women’s basketball teams was utilized to determine the rates and patterns of back injuries. Rates and distributions of back injuries were identified within the context of mechanism of injury, injury recurrence, and time lost from sport. Rates of injury were calculated as the number of injuries divided by the total number of athlete-exposures (AEs). AEs were defined as any student-athlete participation in 1 NCAA-sanctioned practice or competition with the inherent risk of exposure to potential injury. Injury rate ratios (IRRs) were then calculated to compare the rates of injury between season, event type, mechanism, injury recurrence, and time lost from sport. Injury proportion ratios (IPRs) were calculated to compare rates between men and women athletes. Results: A national estimate of 1805 and 3391 back injuries occurred in women’s and men’s basketball, respectively. The rate of back injuries in men was 4.89 per 1000 AEs, while women suffered injuries at a rate of 2.71 per 1000 AEs. Men were 1.82 (95% CI [confidence interval] = 1.70-1.91) times more likely to suffer a back injury compared to women. Injuries occurred more often during competition than practice in both sexes (men: 9.59 vs 3.34 per 1000 AEs; women: 3.09 vs 2.58 per 1000 AEs). Women suffered the highest rate of injury during the postseason (6.88 per 1000 AEs), while the highest rate of injury for men was during the preseason (5.39 per 1000 AEs). Conclusion: Back injuries occur at a high rate in NCAA basketball athletes. While men suffer these injuries at a higher rate compared with women, they still frequently occur in women. The yearlong vulnerability of athletes to these injuries is evident by the highest rate of injury in men occurring during the preseason, but during the postseason in women. With this information, teams should implement conditioning and back injury prevention programs that are year-round. These programs can hopefully lead to a decrease in back injuries seen in these athletes.
P338: Difference of Clinical Adjacent Segmental Pathology Among Continents Following Anterior Cervical Discectomy and Fusion: Meta-Analysis of Randomized Controlled Trials
Sung Kyu Kim1 and So Hyun Moon2
1Chonnam National University Hospital, Gwangju, Republic of Korea
2Chosun University, Gwangju, Republic of Korea
Background: Adjacent segment pathology (ASP) is a long-term complication of the cervical fusion procedure. However, no epidemiological data on prevalence of clinical ASP (cASP) with regard to continents has been published. The purpose of this study was to evaluate and compare the cASP after anterior cervical discectomy and fusion (ACDF) among continents. Methods: MEDLINE, EMBASE, and Cochrane Library with manual searching in key journals, reference lists, and the National Technical Information Service were searched from inception to August 2016. Active researchers in the field were contracted to determine the relevant studies. Nineteen studies with total 1829 patients were included in the meta-analysis. We extracted the publication details, sample size, and prevalence of cASP. We considered that the patient’s race depended on the location of a study’s corresponding institution. Results: A total of 11 articles from North America, 5 from Europe, and 3 from Asia met the inclusion criteria. A total number of 1829 patients from 19 studies underwent ACDF, and 124 patients among them had cASP. The prevalence of cASP ranged from 1% to 24%. The mean prevalence of cASP in the North America group was 6.22%, Europe 6.64%, and Asia 7.23%, and there were no statistically significant differences. Conclusions: The current study using the method of meta-analysis revealed that there were no significant differences in cASP following ACDF among the continents.
P339: Surgical Management, Survival Rate, and Recurrance of Metastatic Renal Cell Carcinoma in Vertebral Bodies
Kathryn Ramshaw1, Yehya Ghonem1, Anne-Marie Rowley1, and Palaniappan Lakshmanan1
1City Hospitals Sunderland, East Boldon, Sunderland, UK
Introduction: Metastatic spread of renal cell carcinoma to the spine is common; symptoms include pain and/or neurological deficit. Surgical management offers symptomatic relief using a combination of spinal surgical interventions. The aim of this study is to look at indication for surgery, survival rate, and recurrences of metastatic renal cell carcinoma to vertebral bodies from 2011 to 2017. Materials and Methods: Between July 2011 and November 2017, 23 patients with spinal metastases secondary to renal cell carcinoma were operated on, and data was entered prospectively in to a local database at a district general hospital. Indication for surgery, mortality, and recurrence of metastases were collected on the database. Mortality was calculated and survival data was used to formulate a Kaplan-Meier graph. The graph was used to estimate survival time in patients with symptomatic renal cell carcinoma spinal metastasis following surgical intervention. Results: Results showed that the majority of patients (62%) were indicated for surgery due to pain and instability; 19% of patients were indicated for surgery for neurological deficit alone. Fourteen percent of patients were indicated for surgery for curative purposes. Four percent of patients were indicated for surgery due to pain alone. Postoperative survival time ranges from 55 to 1809 days with an average of 736 days. The Kaplan-Meier survival showed 30-day mortality is nil, steps in the graph demonstrated 80% survivorship after 100 days, with another significant step showing 60% of survivorship after 200 days. Fifty percent of people were alive after 350 days. Forty percent of people survived after approximately 750 days, with 30% of people surviving to 1000 days. Twenty percent of people are still surviving. Most people died due to progression of their metastatic disease, notably brain metastasis. Patients in the particular age group are 50 to 79 years old with an average age of 62 years. Fifty-six percent of patients had progression of their disease causing recurrence in their symptoms and required further surgical intervention. Conclusion: With advances in oncological and surgical management, metastatic renal cell carcinoma to the spine has a high survival rate; however, a limiting factor to this survival rate is a high prevalence of brain metastasis. There are common dips in survival to be vigilant for up to 1000 days. The management of such complex patients can be done in a district general hospital with a variety of surgical management techniques appropriate to individual need.
P340: Metastatic Spinal Cord Compression: Surgical Management in a District General Hospital
Kathryn Ramshaw1, Anne-Marie Rowley1, and Palaniappan Lakshmanan1
1City Hospitals Sunderland, East Boldon, Sunderland, UK
Introduction: Surgical management for spinal metastasis has shown to have better outcomes along with radiotherapy and chemotherapy. Normally, most resources are concentrated in the University Hospital setting for such multidisciplinary management of these complex patients. This study aims to analyze the results of surgical management of metastatic spinal cord compression, in a district general hospital with multidisciplinary team involvement. Materials and Methods: Between October 2010 and August 2018, 120 patients with spinal metastasis had surgical management in a district general hospital. The data was entered prospectively in a local tumor database held at the hospital. Survivorship was plotted on a Kaplan-Meier graph. Results: Fifty of the patients were female and 70 were male, with the average age of patients who had surgery for metastatic spinal cord compression being 65 years. The nature of primary tumor was lung cancer in 24 patients (20%), prostate cancer in 21 patients (18%), renal cancer in 19 patients (16%), and breast cancer in 13 patients (11%). Indication for the surgery included pain (28%); pain combined with instability (23%); instability (17%); paraplegia (14%); and the remaining 13% of patients had surgery for a combination of the aforementioned reasons, with one patient having had a sacral fracture. Five percent of patient reasons for surgery were not entered in to the database. Twenty-five percent (30) of patients had thoracic surgery alone, while 22% (26) had surgery across both the thoracic and lumbar spines. Ten percent (12) of patients had lumbar surgery alone, with 8% (8) having surgery across both lumbar and sacral regions. Three percent (4) of patients had cervical surgery alone, with 8% (10) of people having surgery across both the cervical and thoracic spines. Two percent (2) of patients had sacral surgery alone, with another 2% (2) having surgery across the thoracic, lumbar, and sacral regions. A total of 0.8% (1) of people had occipital surgery. Twenty percent (24) of patients had no operated region documented on the database. Overall cervical spine involvement 8%; thoracic spine involvement is 57%; lumbar spine involvement is 42%; and sacral spine involvement is 4%. Twenty patients had minimally invasive surgical procedures. The Kaplan-Meier graph shows a step to around 75% survival rate at around 100 days and 53% survivorship at around 400 days. Another step is present demonstrating 46% survivorship around 475 days, with a plateau in the graph showing around 43% of patients survive to 800 days. The graph demonstrates 40% of people are still surviving past 1500 days. Conclusion: There is a downward trajectory in survivorship against time after surgery for metastatic spinal cord compression. Once patients reach 800 days postoperation, survivorship plateaus and they continue to live longer. The thoracic spine is most involved in spinal metastasis affecting quality of life and requiring surgical intervention in patients with a range of primary disease cancer. The management of such complex patients can be done in a district general hospital setting provided adequate multidisciplinary team resources are available.
P341: Completeness and Accuracy of Data in Spine Registries: An Independent Audit-Based Study
Ehab Shiban1, Sandro Krieg1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Background: Spine registries are used for quality management and clinical research. Due the importance and implications of both aims, completeness and high quality of data is of paramount importance. However, this remains uncertain, as none of these registries have implemented independent monitoring. Aim of this study was to determine the accuracy and completeness of the German Spine Society Registry. Methods: In a prospective study design audits by a board–certified neurosurgeon were planned and conducted at Deutsche Wirbelsäulengesellschaft (DWG)-certified spine centers with mandatory minimum follow-up data input in the spine registry. For the visit, a 2-week period was defined several months before the initial contact to the centers, in which all patients operated in, were analyzed. Any discrepancy between the patients’ charts and the registry entry was detected and analyzed. A median of 33 items per patient were analyzed. Results: Out of 23 certified spine centers contacted, 17 centers were willing to participate, but 4 were still lacking any data entries. Even in the remaining 13 centers eligible for audits, 83% of entries were finalized only after the audits were announced. Only 84% of surgeries were documented, and on average, 15% of entries were not accurate with a wide variation (range = 3% to 51%) between centers. Conclusion: Both completeness and accuracy of data in the DWG registry were unacceptable for study as well as QM purposes. Unannounced audits might reveal even a more worrisome situation. Thus these data should not be used for the time being, since wrong conclusion will inevitably be drawn. Several aspects for improvement of the situation were identified.
P342: The Impact of Liver Disease on Surgical Outcomes Following Posterior Lumbar Fusion
Ray Tang1, Ivan Ye1, Brian Cho1, Samuel White1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Mount Sinai Health System, New York, NY,- USA
Introduction: Liver disease is a leading cause of morbidity and mortality in the United States. The association between liver disease and poor surgical outcomes has been consistently reported in the literature across multiple surgical subspecialties. Posterior lumbar fusion is a common procedure in spine surgery that is being performed at an increasing rate with an aging population. In this study, the objective was to assess the impact of liver disease on 30-day postoperative complications following elective posterior lumbar fusion using a nationwide surgical outcomes database. Material and Methods: We performed a retrospective cohort analysis of data from the 2011-2014 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). Adult patients who underwent elective posterior lumbar fusion were identified and included in this study. They were divided into 2 groups based on the comorbidity of liver disease, which was defined as a MELD-Na (Model of End-stage Liver Disease–Sodium) score ≥10. Univariate analysis was performed to compare baseline patient characteristics, comorbidities, functional status, and operative variables between the 2 groups. Multivariate regression analysis was then performed while adjusting for patient and operative variables in order to determine 30-day perioperative complications that were independently associated with liver disease. Results: A total of 6916 patients who underwent elective posterior lumbar fusion were identified. Within this cohort, the rate of liver disease was 18.8% (1300/6916). Univariate analysis identified significantly higher rates of cardiac complications (1.2% vs 0.5%), pulmonary complications (2.0% vs 0.6%), renal complications (0.5% v. 0.1%), blood transfusion (22.2% vs 16.0%), sepsis (2.0% vs 0.8%), urinary tract infection (2.9% vs 1.6%), and prolonged length of stay (32.3% vs 21.9%). Multivariate regression analysis found that liver disease was an independent risk factor for 30-day pulmonary complications (odds ratio [OR] = 2.5; 95% confidence interval [CI] = 1.4-4.2; P < .001), renal complications (OR = 10.2; 95% CI = 2.6-39.3; P < .001), blood transfusion (OR = 1.3; 95% CI = 1.3-4.5; P = .005), sepsis (OR = 2.2; 95% CI = 1.3-3.7; P = .003), urinary tract infection (OR = 1.5; 95% CI = 1.0-2.3; P = .005), and prolonged length of stay (OR = 1.5; 95% CI = 1.3-1.7; P < .001). Conclusion: In patients who underwent elective posterior lumbar fusion, liver disease was an independent predictor of several 30-day postoperative complications, including pulmonary complications, renal complications, blood transfusion, sepsis, urinary tract infection, and prolonged hospitalization. Assessment of liver function is therefore an important component of preoperative risk stratification of patients undergoing posterior lumbar fusion.
P343: Risk Factors for 30-Day Readmissions due to Venous Thromboembolism Following Posterior Thoracolumbar Fusion
Ray Tang1, Ivan Ye1, Brian Cho1, Andrew Warburton1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Mount Sinai Health System, New York, NY, USA
Introduction: Postoperative venous thromboembolism (VTE) events, such as deep vein thrombosis and pulmonary embolism, are a major source of morbidity and mortality following spine surgery. Unplanned readmissions due to postoperative VTE represent a significant burden on health care costs across the United States. Posterior thoracolumbar fusion is one of the most common procedures performed in spine surgery. The use of chemical prophylaxis to prevent VTE postoperatively remains controversial due to concerns about the possibility of epidural hematoma formation The objective of this study was to identify independent risk factors for 30-day unplanned readmission due to VTE following elective posterior thoracolumbar fusion using the Nationwide Readmissions Database (NRD). Material and Methods: This was a retrospective cohort analysis of the 2012-2014 NRD by the Healthcare Cost and Utilization Project (HCUP). Patients who underwent elective posterior thoracolumbar fusion were identified based on ICD-9 (Internationl Classification of Diseases, Ninth Revision) diagnosis and procedure codes. Thiry-day readmissions due to VTE were identified using Clinical Classification Software and ICD-9 diagnosis codes on readmission. Bivariate analysis was performed to determine covariates for readmission among baseline patient characteristics, including demographics, comorbidities, and insurance type. A multivariate logistic regression model was then performed to identify independent risk factors that were predictive of 30-day readmission due to VTE while adjusting for covariates. Results: A total of 223 788 cases of elective posterior thoracolumbar fusion were identified in the NRD. The overall any-cause 30-day readmission rate was 6.4% (14 264/223 788) and the readmission rate due to VTE was 0.40% (872/223 788). Bivariate analysis showed that patients who were readmitted due to VTE had a higher incidence of deficiency anemia, rheumatoid arthritis, congestive heart failure, coagulopathy, diabetes mellitus, diabetes with chronic complications, hypertension, hypothyroidism, obesity, pulmonary circulation disorders, renal failure, weekend admission, and insurance type. The multivariate regression model identified 16 independent risk factors for 30-day readmission due to VTE. Among these risk factors, the strongest predictors were pulmonary circulation disorder (odds ratio [OR] = 2.22; 95% confidence interval [CI] = 1.67-2.94; P < .001), Medicaid insurance (OR = 1.93; 95% CI 1.58-2.35; P < .001), weekend admission (OR = 1.87; 95% CI = 1.44-2.43; P < .001), paralysis (OR = 1.55; 95% CI = 1.24-1.94; P < .001), and rheumatoid arthritis (OR = 1.48; 95% CI = 1.25-1.76; P < .001). Conclusion: Comorbidities that were most predictive of unplanned 30-readmission due to VTE following posterior thoracolumbar fusion were pulmonary circulation disorder, paralysis, and rheumatoid arthritis. In addition, Medicaid insurance and weekend admission were also among the strongest predictors of 30-readmission due to VTE. Risk stratification to identify patients at high risk for readmission due to VTE is important in order to develop quality improvement programs aimed at decreasing the incidence of postoperative VTE and associated health care costs, while also improving patient outcomes and quality of life following posterior thoracolumbar fusion.
P344: Determinants of Health as Predictors of a Major Complication for Inpatients With Central Cord Syndrome
Allison Hall1, Jinpu Li1, Ryan Knigge1, Emily Leary1, Theodore J Choma1, Michael G. Fehlings2, and Christina L. Goldstein1
1 University of Missouri, Columbia, MO, USA
2 Toronto Western Hospital, University of Toronto, Toronto, Ontario, Canada
Introduction: Central cord syndrome (CCS) is characterized by upper extremity weakness greater than lower extremity weakness, varying degrees of sensory loss, and less severe sacral level dysfunction. The most common form of incomplete spinal cord injury (SCI), CCS is increasingly being managed with operative intervention, though many patients are still treated non-surgically. Given the morbidity of CCS and often advanced age and medical comorbidities of these patients, post-admission complications in these patients would be expected. However, no comprehensive reviews of risk factors for complications have been performed. The purpose of this study is to examine the relationships between determinants of health and major complication occurrence in inpatients with CCS using a uniform, multistate database approximating a 20% stratified sample of annual discharges from American community hospitals. Materials and Methods: The 2014 National Inpatient Sample (NIS) dataset was and ICD-9-CM (Internationl Classification of Diseases, Ninth Revision, Clinical Modification) diagnostic codes for CCS (952.03 [C1-4] and 952.08 [C5-7]) were used to identify admissions for study inclusion. Demographic, geographic location, length of stay, discharge destination, insurance, complication, and diagnosis data were extracted. Unplanned reoperations following any surgical procedure were coded using 30 diagnostic codes for diagnoses specific to a reoperation (eg, incision and drainage of hematoma). Admissions associated with a postoperative complication, reoperation, or patient death were aggregated and coded as being associated with a major complication. Demographic, socioeconomic, geographic, and health factors for patients were summarized. Complication and reoperation rates were calculated and compared using chi-square or 2-sided t tests. Similarly, rates were compared between whites and non-whites. Determinants of health were examined for their association with major complication, using stepwise multivariate logistic regression analysis with a significance cutoff of 0.05. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: A total of 946 admissions with a mean age of 61.6 years were identified for study inclusion. Overall, 71.6% of the admissions were males and 67.0% were white. More than 1 in 3 (35.0%) admissions was associated with a complication, the total reoperation rate after all surgical procedures was 1.02%, and the in-hospital death rate was 3.1%. The total rate of a major complications was 35.5%, with the majority being a complication as opposed to reoperation or death. Accounting for all other covariates, older patients with more medical comorbidities, who stayed longer in hospital following surgery, and were discharged somewhere other than home were more likely to have experienced a major complication following admission. Conclusions: This examination of the effect of a variety of determinants of health on the risk of major complications in inpatients withCCS, using the largest all-payer inpatient database in the United States, has identified that older patients with a greater number of chronic conditions are at increased risk of experiencing a postoperative complication, unplanned reoperation, or in-hospital death following treatment in a community hospital. These findings support ongoing analyses to determine how the setting, timing, and approach to treatment affect outcomes to inform decision-making in order to optimize management of these at-risk patients.
P345: Determinants of Health as Predictors of a Complication After Posterior Lumbar Fusion at a Single Tertiary Care Spine Center
Shelby Harris1, Jinpu Li1, Emily Leary1, Joshua Karlin1, Theodore J Choma1, and Christina L. Goldstein1
1 University of Missouri, Columbia, MO, USA
Introduction: Complication rates after lumbar spine fusion range from 5.6% to 31.4%. Multiple investigations have examined risk factors for complications following lumbar spine fusion, though none have performed a comprehensive investigation of the association between multiple determinants of health and the risk of postoperative complications in this setting. This study aims to determine those demographic, biological, behavioral, and health determinant variables significantly associated with occurrence of a postoperative complication following lumbar spine fusion for all indications at a single Midwest tertiary care spine center. Material and Methods: After obtaining institutional review board approval, CPT (Current Procedural Teminology) codes for posterior lumbar spinal fusion were used to screen hospital billing data to identify all patients undergoing surgery for any indication between June 1, 2006, and December 31, 2016. Patients ≥18 years of age with at least 1-year follow-up were selected for study inclusion. Electronic medical records were reviewed to extract the following data: age, sex, race, body mass index, ZIP code, insurance status, smoking status, medical comorbidities, ASA (American Society of Anesthesiologists) class, complications, readmission, reoperation, and discharge destination. ZIP codes were used to determine median income. Descriptive statistics were summarized, complication rates calculated, and differences between whites and non-whites examined using 2-sample t tests or chi-square tests as appropriate. Univariate analysis followed by multivariate logistic regression analysis using a significance cutoff of 0.05 was performed to identify variables significantly related to occurrence of a postoperative complication. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: Over the 10-year period, 181 patients with a mean age of 55.8 years (standard deviation [SD] = 14.1) and mean BMI (body mass index) of 33.3 kg/m2 (SD = 7.2) were identified for study inclusion. A total of 59.7% (n = 78) of the subjects were female and 89.0% (n = 161) were white. A total of 30.9% (n = 56) of the patients experienced a postoperative complication. The majority of patients (n = 169, 95.5%) were able to be discharged home postoperatively, though 28.7% (n = 52) experienced a readmission at some point following their index procedure. Multivariate logistic regression analysis performed using complete data from 177 patients showed that diabetes was the only significant predictor of a postoperative complication in our cohort, though complications were also associated with discharge somewhere other than home. On univariate analysis, the odds of a postoperative complication in the presence of diabetes was 1.744 (95% CI [confidence interval] = 0.850-3.58). Conclusion: This comprehensive analysis of preoperative variables as predictors of postoperative complications in adult patients undergoing posterior lumbar fusion has identified that diabetic patients are at 70% greater risk of developing a postoperative complication. This finding supports ongoing investigations into the role preoperative HbA1c optimization and strict postoperative glucose control in the prevention of postoperative complications. This information will inform decisions regarding patient selection and timing of surgical intervention such that surgical outcomes may be optimized and discharge to higher levels of care, with their associated increased direct health care costs, may be avoided following posterior lumbar spine fusion in diabetic patients.
P346: Determinants of Health as Predictors of a Complication After Cervical Spine Fusion at a Single Tertiary Care Spine Center
Jacob Bailey1, Linlin Zhang1, Emily Leary1, Joshua Karlin1, Mark Lambrechts1, Theodore J Choma1, and Christina L. Goldstein1
1 University of Missouri, Columbia, MO, USA
Introduction: Complication rates after cervical spine fusion range from 11% to 38%. Multiple investigations have examined risk factors for complications following cervical spine fusion, though none have performed a comprehensive investigation of the association between multiple determinants of health and the risk of postoperative complications in this setting. This study aims to determine those demographic, biological, behavioral, and health determinant variables significantly associated with occurrence of a postoperative complication following cervical spine fusion of all types and for all indications at a single Midwest tertiary care spine center. Material and Methods: After obtaining institutional review board approval, CPT (Current Procedural Teminology) codes for anterior and posterior cervical spine fusion were used to screen hospital billing data to identify all patients undergoing surgery for any indication between June 1, 2006, and December 31, 2016. Patients ≥18 years of age with at least 1- year follow-up were selected for study inclusion. Electronic medical records were reviewed to extract the following data: age, sex, race, body mass index, ZIP code, insurance status, smoking status, medical comorbidities, ASA (American Society of Anesthesiologists) class, complications, readmission, reoperation, and discharge destination. ZIP codes were used to determine median income. Descriptive statistics were summarized, complication rates calculated, and differences between whites and non-whites examined using 2-sample t tests or chi-square tests as appropriate. Univariate analysis followed by multivariate logistic regression analysis using a significance cutoff of 0.05 was performed to identify variables significantly related to occurrence of a postoperative complication. SPSS and R were used to perform the statistical analysis and a P value of .05 was determined to be statistically significant. Results: Over the 10-year period, 256 patients with a mean age of 50.5 years (standard deviation [SD] = 10.0) and mean BMI (body mass index) of 30.7 kg/m2 (SD = 6.8) were identified for study inclusion. A total of 61.3% (n = 157) of the subjects were female and 92.6% (n = 237) were white. A total of 32.4% (n = 83) of the patients experienced a postoperative complication such as pseudarthrosis (10.2%) and implant loosening (11.3%). The majority of patients (n = 247, 96.5%) were able to be discharged home postoperatively, though 24.6% (n = 63) experienced a readmission at some point following their index procedure. Multivariate logistic regression analysis performed using complete data from 252 patients showed that smoking was the only significant predictor of a postoperative complication in our cohort, though complications were also associated with readmission. On univariate analysis, the odds of a postoperative complication in smokers was 1.877 (95% CI [confidence interval] - 1.077-3.272). Conclusion: This comprehensive analysis of preoperative variables as predictors of postoperative complications in adult patients undergoing cervical spine fusion has identified that smokers are at almost 90% greater risk of developing a postoperative complication than nonsmokers. This finding confirms the importance of preoperative smoking cessation prior to cervical spine fusion and supports further investigations into the efficacy and cost-effectiveness of preoperative smoking cessation. This information may substantiate the need for extra resource allocation by health systems to preoperative smoking cessation programs in order to optimize patients’ surgical outcomes and prevent undesired and costly complications and readmissions.
P347: Epidemiology of Spinal Fractures in a Level-1 Trauma Center in the Netherlands: A 10-Year Review
Lars den Ouden1, Arjen Smits1, Agnita Stadhouder1, Ricardo Feller1, Jaap Deunk1, and Frank Bloemers1
1VU University Medical Center, Amsterdam, Netherlands
Introduction: Spinal fractures may have large socioeconomic consequences. The prevalence and outcomes likely change over the years due to improved traffic safety, increasing population age, and improved medical treatment. This is the first study to address the epidemiology of spinal fractures over a large time period in the Netherlands. Material and Methods: A retrospective epidemiological study was performed. All patients with a cervical, thoracic, or lumbar spine fracture admitted to a level-1 trauma center from 2007 to 2016 were prospective registered and retrospectively analyzed. In addition to patient- and accident-associated injury characteristics, radiological and surgery data were obtained from the hospital’s Electronic Patient File system. Results: Between 2007 and 2016, 1479 patients with a total of 3029 spinal fractures were admitted. 40.8% were female and 59.2% were male, with a mean age of 52.0 years. A total of 4.9% of fractures occurred at a juvenile age (0-18 years) and 63.6% at the age of 19 to 64 years. Most fractures occurred in the thoracic spine, followed by the lumbar and cervical spine. The most common cause of injury was a fall from height, followed by traffic accidents. Spinal cord injury occurred in 8.5% and associated injuries were reported in 73% of the patients. Sixteen percent of the admitted patients were treated operatively. Over time, there was a larger increase in amount of spine fractures in elderly (>65 years) compared with younger people. Conclusion: A considerable amount of spine fractures occur in the age group of 19 to 64 years. Most fractures were located in the thoracic spine. The total amount of spine fractures per year increased over time, especially in the elderly. This study might stimulate development of policy on precautionary actions to prevent spine fractures.
P348: Prevalence, Consequences, and Predictors of Low Back Pain Among Nurses in a Tertiary Care Setting
Sameh Abolfotouh1, Khaled Faraj2, and Gemah Moammer3
1University of Missouri, Columbia, MO, USA
2OrthoCure Medical Center, Dubai, United Arab Emirates
3Grand River Hospital, Kitchener, Ontario, Canada
Introduction: Nursing is a profession with high incidence and prevalence of low back pain (LBP), with its medical and professional consequences. These prevalence rates vary among countries and various measurements have been used to determine LBP. Individual and work-related factors are regarded as causal factors for many back injuries. The aims of study were the following: (1) to estimate the prevalence of LBP using different measures, (2) to determine medical and professional consequences of LBP, and (3) to determine the associated factors and significant predictors of LBP. Material and Methods: A cross-sectional study was conducted among 254 nurses from different departments/wards at Hamad General Hospital (HGH), Doha, Qatar, over 2 months (January and February, 2015). Self-administered modified Nordic questionnaire was used to collect data regarding 5 different measures of LBP, its medical and occupational consequences, and individual/lifestyle and work-related risk factors of LBP. Descriptive and analytic statistical analyses were done using chi-square and multivariate logistic regression techniques. Significance was considered at P < .05. Results: The findings of this study broadly confirm the high levels of back pain innursing, with a 1 year prevalence of LBP of 54.1% for LBP of at least 1 day, % for chronic LBP, % for seeking sick leave seeking LBP, and % for medical treatment seeking LBP. Difficult or impossible activities daily living were reported due to LBP in; climbing stairs (50.7%), walking (42.8%), standing up (39.9%), sleeping (33.3%), getting out of bed (30.4%), and wearing clothes (20.3%). Work stop due to LBP was reported by 76.8% of nurses, with 2.03 ± 3.09 days within the past year. Treament was sought in 58.7% by medical care, and 15.9% by physiotherapy, while seeking rest days and/or sick leave was sought in 50.8% of nurses with LBP. Sports practice (P = .003), office work (P < .001), and exposure to physical stress (P = .002) were the only significant predictors of LBP among nurses, when logistic regression analysis was conducted. Conclusion: The prevalence of LBP among nurses at HGH is high and should be actively addressed; however, it was not a major cause of sick leave.Preventive measures should be taken to reduce the risk of lower back pain, such as arranging proper rest periods, educational programs to teach the proper use of body mechanics, and sports activity programs.
P349: The Epidemiology of Neck Injuries in the National Collegiate Athletic Association Athlete
Andrew Chung1, Justin Makovicka1, Sailesh Tummala1, Jeff Hasselbrock1, Karan Patel1, and Anikar Chhabra1
1Mayo Clinic, Phoenix, AZ, USA
Introduction: To date, neck injuries in National Collegiate Athletic Association (NCAA) athletes have not been well studied. As such, the purpose of this study was to describe the epidemiology of neck injuries in NCAA athletes during the 2009/2010-2014/2015 academic years utilizing the NCAA Injury Surveillance Program (NCAA-ISP) database. Material and Methods: A convenience sample of NCAA varsity teams from 25 sports was examined to determine the rates and patterns of neck injuries. Rates and distributions of injuries were identified within the context of mechanism of injury, injury recurrence, and time lost from sport. Rates of injury were calculated as the number of injuries divided by the total number of athlete-exposures (AEs). AEs were defined as any student participation in 1 NCAA-sanctioned practice or competition with the inherent risk of exposure to potential injury. Injury rate ratios (IRRs) and injury proportion ratios (IPRs) were then calculated to compare the rates within and between sports by event type, season, sex, mechanism, injury recurrence, and time lost from sport. Results: A national estimate of 11 510 neck injuries occurred over the 5-year period. The resultant overall rate of injury was 1.7 per 1000 AEs. Men’s football (25.9 per 1000 AEs) and men’s wrestling (6.3 per 1000 AEs) were the sports with the highest rates of neck injuries. Neck injuries were more likely to occur during competition when compared with practice (risk ratio [RR] = 2.73; 95% confidence interval [CI ] = 2.63-2.83). Athletes were less likely to sustain a neck injury preseason when compared to inseason (RR = 0.74; 95% CI = 0.71-0.77) and more likely to sustain an injury in the preseason when compared with postseason (RR = 1.49; 95% CI = 1.35-1.65). Contact injury (83.2%) was the most common mechanism of injury in all observed sports. In all sports, stingers (48.1%) and cervical strain/contusions (42.2%) were the 2 most common injuries sustained and most neck injuries resulted in <24 hours of time loss from event participation (62.2%). Injury recurrence was most common in men’s football (14.4%). Only 0.3% of all athletes required surgery for their injury. Conclusion: The rate of neck injury in NCAA athletes is relatively low (1.7 neck injuries per 1000 AEs). Contact injuries are the most common mechanism of injury. Neck injuries are most commonly seen in the setting of men’s football. Fortunately, most injuries appear to be transient in nature and of limited clinical significance as only 0.3% patients require surgical intervention as a result of injury.
P350: Cervical Ossification of the Posterior Longitudinal Ligament: A Computed tomography–Based Epidemiological Study of 2917 Patients
Wajeeh Bakhsh1, Ahmed Saleh2, Jillian Gruber1, Paul Rubery1, and Addisu Mesfin1
1University of Rochester Medical Center, Rochester, NY, USA
2Maimonides Medical Center, New York, NY, USA
Introduction: Ossification of the posterior longitudinal ligament (OPLL) is a rare condition with variable symptomology. Due to its low prevalence, epidemiology is poorly understood although characterized as most common in the cervical spine, disproportionately affecting Asians, and age of onset usually 50 to 70 years. This study is the largest of its kind to evaluate and better characterize cervical OPLL among 2917 patients. Methods: Computed tomography (CT) scans of all patients receiving cervical spine CT imaging in a level 1 Emergency Department from January 1, 2014, to December 31, 2014, were reviewed. Reviewers included board-certified orthopedic surgeon, orthopedic surgery fellow, resident, and medical student. Diagnosis and classification of OPLL was made, and demographic data for associated patients was obtained (age, sex, race, ethnicity, BMI [body mass index], and diabetes). US census data was obtained for reference of the sample population. Statistical analysis included t test and chi-square testing, with significance cutoff of P < .05. Results: The sample population closely mirrored US census data with no significant differences. Of 2917 patients reviewed, 74 were diagnosed with OPLL (2.5%). Age distribution between OPLL and non-OPLL cohorts was significantly different (P < .01), with highest prevalence of OPLL in the age-groups of 40 to 49, 50 to 59, 70 to 79, and 80 to 89 years. There was no significant difference between groups in distributions of sex, race, or ethnicity. For OPLL, segmental type is the most common (67.6%), involving on average 3.4 levels. OPLL involvement begins at levels C2-C6 with similar frequency, but ends most commonly at C6 (40.5%) or C7 (36.5%). Among OPLL patients, 18 (24.3%) demonstrated concurrent PP (ponticulus posticus). Discussion: This review of 2917 patients reaffirms previous data, with OPLL prevalence of 2.5%. It suggests an earlier asymptomatic onset of OPLL in ages 40 to 49 years, and it characterizes OPLL with segmental type being most common and the caudal extent typically involving C6-C7 (77%). While this study has some limitations, it better characterizes OPLL and suggests routes for further research.
P351: Spinal Tumor Epidemiology in an Ecuadorian Neurosurgical Reference Center
Jaime Jara1, Andrea Ortiz1, and Laura Bottani2
1Universidad San Francisco de Quito–Hospital Eugenio Espejo, Quito, Ecuador
2Hospital Eugenio Espejo, Quito, Ecuador
Introduction: Epidemiological data from primary spinal tumors, spinal meninges and cauda equina, are scarce in medical literature. The Central Brain Tumor Registry of the United States (CBTRUS) reports a global 3% prevalence of spinal localization out of every primary tumor located in the central nervous system. Ecuador’s statistical data is very limited and there are no published studies involving epidemiology of spinal neoplasia. Material and Methods: A retrospective revision of clinical files from patients admitted to the Department of Neurosurgery of Hospital Eugenio Espejo in Quito, Ecuador, between January 2017 and March 2018, was performed. Search criteria was patients diagnosed and admitted with diagnosis of spinal tumors. Twenty-five patients were included in the study. Results: A wide range in age was found, with ages between 15 and 78 years (mean = 42.2; SD [standard deviation] = 17.3). Male population was 48% and females were 52%. Individuals with motor symptoms were 24 (96%); there were 21 patients (84%) with sensibility impairment; sphincter involvement was present in 10 patients (40%). The time between the onset of the symptoms and the patients seek for medical attention ranged widely between 15 days and 10 years. There were 4 (16%) intramedullary lesions of which 2 reported a histopathology of low-grade astrocytoma and half were hemangioblastoma. Fourteen of the tumors were located extramedullary and intradural, of which 8 (57%) were meningiomas and 6 (43%) where schwannomas. The extradural, extramedullary located tumors were 7 of which only 1 was a primary tumor (sarcoma) the rest corresponded to metastases. The anatomical location of the tumors was primarily lumbar (52%), followed by thoracic (36%). Cervical spine location was found in 12% of the patients. Conclusion: Our study found similar sex distribution than that found in the CBTRUS. Literature provides a classification of spinal tumors according to location in intramedullary, extramedullary intradural, and extramedullary extradural; however, there were no reports in our search that reported epidemiology concerning this classification, which our study does. There is a palpable lack of epidemiologic studies in Latin America and more so in Ecuador. Our center receives cases from all over the country, so a regional tendency can be established despite the low number of cases included. We exhort the need of these types of studies in our region, so we can tackle better not only spinal pathology but also neurosurgical pathology as a whole.
P352: Surgical Disc Herniation on First Trimester of Pregnancy: The First Case Report and Literature Review
Sauri-Barraza José Carlos1, Callejas-Ponce Eduardo1, and Carral Robles-León Eugenio1
1ABC Medical Center, Mexico City, Mexico
Introduction: Spinal disorders, relatively frequent in pregnancy, may induce major functional and structural changes. At worst, fetal development disturbances also could be included as a result. Disc herniation estimated incidence, 1/10 000 on pregnancy, makes it the most frequent spinal disease in such patients. Considering the health of the fetus, surgical approaches are delayed traditionally until delivery comes or to latest months of gestation. This work presents a case report of surgical disc herniation treatment on early stages of pregnancy and a systematic literature review available on this subject. Materials and methods: We reviewed a case involving 34-year-old woman at eigth week of pregnancy suffering lumbar pain attack irradiated to thigh and gluteus of left side, 10/10 according to visual analogous scale of pain (VAS) and 90% according to Oswestry disability index (ODI). Pain was persistent, disabilitating, and walk-limiting. MRI (magnetic resonance imaging): L4-L5 disk bulging with facet hypertrophy molding dural sac; L5-S1 with left posterolateral disc extrusion that reaches and displaces S1 radicular sheath. Pharmacotherapy and caudal blocking both failure to get adequate pain control, therefore a column surgery was disposed. Briefly, after adequate induce of L2-L3 epidural anesthesia, column was approached on affected region and a conventional left L1-S1 hemilaminotomy was made. Surgery also included left yellow ligament resection, radicular release and L5-S1 discectomy. A systematic related literature search in PubMed was performed. Searching keywords were “lumbar disc herniation” and “pregnancy.” All results in English, Spanish, or French were included. No other filters or restrictions were applied. Results: No eventualities were observed during trans-surgical neurophysiologic checkup neither on postsurgical immediate period. L5 and S1 left roots showed conduction improvement what turned out in an excellent analgesic control. Indeed, acetaminophen solely was enough to keep down EVA as low as 1/10. Throughout 2 days of obstetric follow-up after surgery, no premature uterine contractions, fetal cardiac frequency disturbances, or another deviations were observed. Ulterior obstetric checkups showed both normal uterine and fetal development. Obstetric outcome: Kerr cesarean at week 38, normal product weigh (2580 g), Apgar score 9/9, and painless mother. The literature systematic review lead 56 related articles. Mention of early stages pregnancy (first trimester) and lumbar disc herniation surgery were not showed in any of them. Mostly citations discuss surgical treatment until second trimester of gestation. Conclusion: Surgical treatment of disc herniation on first trimester of pregnancy was exposed at first time in this work. We demonstrated that pain relief is possible in these patients by conventional hemilaminotomy and discectomy as early as week 8 of gestation without major fetal-maternal inconveniencies. Certainly, candidates must be select carefully in order to avoid therapeutic failure or miscarriage. Our results open a field where confirmatory and long-term studies are imperative.
P353: Utilization and Outcomes for Spine Surgery in the United States and Canada
Peter Cram1, Bruce E. Landon2, John Matelski3, Vicki Ling4, Anthony V Perruccio5, J. Michael Paterson4, and Raja Rampersaud5
1University of Toronto, Toronto, Ontario, Canada
2Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
3Sinai Health System and University Health Network, Toronto,Canada
4Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
5University Health Network, Arthritis Program, Toronto, Ontario, Canada
Introduction: Spine surgery is common and costly. Researchers and policy makers believe that utilization of spine surgery in the United States is significantly higher than in other industrialized countries. Although within-country variation in spine surgery utilization is well studied, there has been little exploration of variation in spine surgery between countries. Material and Methods: We used population level administrative data from Ontario (years = 2011-2015) and New York (2011-2014) to identify all adults who underwent inpatient spinal decompression or fusion surgery. We compared Ontario and New York with regard to patient demographics and the percentage of hospitals performing spine surgery. We compared rates of decompression and fusion surgery (procedures per-10 000 population per-year) in Ontario and New York for all procedures, emergent procedures alone, and elective procedures and after stratifying by patient age. Results: Patients in Ontario were older than patients in New York for decompression (mean age = 58.8 vs 51.3 years; P < .001) and fusion (58.1 vs 54.9; P < .001). A smaller percentage of hospitals in Ontario performed decompression or fusion compared with New York (decompression = 26.1% in Ontario vs 54.9% in New York: fusion 15.2% vs 56.7%; both P < .001). Overall, utilization of spine surgery in Ontario was 6.6 procedures per 10 000 population per-year and in New York was 18.0 per 10 000 per-year (P < .001). Ontario-New York differences in utilization were small for emergent cases (2.0/10 000 in Ontario vs 2.8 in New York; P < .001), but large for elective cases (4.6 vs 15.2; P < .001). In analyses stratified by surgical subtype, differences in utilization of decompression in New York and Ontario were relatively modest (2.4 vs 3.1; P < .001), while utilization of fusion was approximately 400% higher in New York than Ontario (15.7 vs 3.5; P < .001). Further analysis demonstrated that the New York-Ontario difference in utilization was substantially larger among younger patients and smaller for older patients. For example, utilization of spine procedures in New York was 340% greater than Ontario for patients <50 years of age (11.7 vs 3.4), but only 25% greater in patients aged 80 years and older (10.0 vs 12.6). After adjusting for patient demographics, hospital length of stay (LOS) and surgical urgency, differences in mortality in Ontario and New York were not significant for either decompression or fusion. In adjusted analyses, differences in hospital LOS were slightly greater for decompression in Ontario, but similar for fusion and readmission rates in Ontario were significantly lower than in New York. Conclusion: In conclusion, we found significantly lower utilization of spine surgery in Ontario when compared with New York. The difference in utilization was attributable to less elective fusion surgery, primarily in younger (ie, non-Medicare) patients. These findings can serve inform broader spine surgery policy reforms in both jurisdictions.
P354: Ninety-Day Readmission Following Primary Lumbar Spine Surgery
Nicolas Rubel1, Andrew Chung1, Varun Arvind2, Michael Chang3, and Samuel Cho2
1Mayo Clinic, Phoenix, AZ, USA
2Icahn School of Medicine at Mount Sinai, New York, NY, USA
3Sonoran Spine Center, Phoenix, AZ, USA
Introduction: In the United States, there has been a recent surge in the popularity of bundled-payment models for the reimbursement of surgical services. As this trend continues to grow, the focus is shifting toward longer term patient outcomes in the context of 90-day episodes of care as defined by Centers for Medicare and Medicaid Services (CMS). There is currently limited data available on national 90-day readmission statistics for patients undergoing elective lumbar surgery in the inpatient setting. By utilizing a large readmissions database, we hope to provide evidence that will aid in the development of more cost-effective perioperative care models that emphasize high-quality care in patients undergoing primary lumbar spine surgery. With further implementation of bundled-payment reimbursement models in spine likely, this information will also allow providers to better select and implement care strategies for high-risk patients. Material and Methods: Using the 2014 Nationwide Readmissions Database (NRD), all patients with 18 years of age and older who underwent an elective, inpatient, primary lumbar surgical procedure were included for analysis. Two cohorts were created from this subset of patients: those readmitted to the hospital within 90 days for any reason, and those who were not. Using multivariate logistic regression, we identified independent predictors of 90-day readmission while controlling for a multitude of confounding variables. Finally, a cost analysis was run to quantify the increased cost burden to organizations associated with readmission within the 90-day window of treatment. Results: Utilizing ICD-9 (International Classification of Diseases-Ninth Revision) procedure codes, a total of 169 788 patients who underwent a primary lumbar surgical procedure were identified. A total of 4268 (2.51%) were readmitted within 90 days. There was no difference in comorbidity burden between cohorts as quantified by the Elixhauser Comorbidity Index. Comorbidity predictors of readmission were anemia (odds ratio [OR] = 1.16; 95% confidence interval [CI] = 1.04-1.30; P = .01), uncomplicated diabetes (OR = 1.12; 95% CI = 1.03-1.22; P = .006), and diabetes with chronic complications (OR = 1.57; 95% CI = 1.31-1.90; P < .001). Furthermore, surgical wound disruption (OR = 2.25; 95% CI = 1.36-3.74; P = .002) and acute myocardial infarction (OR = 2.34; 95% CI = 1.49-3.67; P < .001) at time of the index admission increased the odds of 90-day readmission. In terms of payer status, using Medicare as a benchmark, only patients who were self-pay had a higher likelihood of being readmitted (OR = 1.70; 95% CI = 1.25-2.30; P = .001). Procedurally, an anterior approach was associated with increased odds of 90-day readmission (OR = 1.12; 95% CI = 1.04-1.21). Hardware complications were identified as the primary related cause of readmission. Last, readmission within 90 days was associated with a significant cost increase (P < .001). Conclusion: There are clearly identifiable risk factors that increase the odds of hospital readmission within 90 days of primary lumbar spine surgery. An overall 90-day readmission rate of 2.51%, while relatively low, carries significantly increased cost to both the patient and hospital. As surgical reimbursement continues to shift toward bundled-payment models, an understanding and appreciation of these risk factors will be of paramount importance.
P355: Ninety-Day Readmission Following Revision Lumbar Spine Surgery
Nicolas Rubel1, Andrew Chung1, Varun Arvind2, Michael Chang3, and Samuel Cho2
1Mayo Clinic, Phoenix, AZ, USA
2Icahn School of Medicine at Mount Sinai, New York, NY, USA
3Sonoran Spine Center, Phoenix, AZ, USA
Introduction: There is little evidence available to aid in the identification of patients at high risk of hospital readmission within 90 days of elective revision lumbar spine surgery in the inpatient setting. Given the inherent complexity of revision surgeries of the lumbar spine, defining who is at risk of 90-day readmission within this population will allow for overall risk-reduction and cost savings, particularly if reimbursement shifts toward bundled payment models. Material and Methods: The 2014 Nationwide Readmissions Database (NRD) was used to identify all patients greater than 18 years of age who underwent an elective revision surgery of the lumbar spine in the inpatient setting. Patients were separated into 2 cohorts based on whether or not they were readmitted to the hospital within 90 days of their index hospitalization. Independent predictors of 90-day readmission were identified through the use of multivariate logistic regression. Last, total hospital cost within the 90-day window of care was calculated for both cohorts. Results: We identified an estimated 14 378 patients who underwent an elective, revision lumbar surgery in 2014 using ICD-9 (International Classification of Diseases-Ninth Revision) procedure codes. A total of 446 readmissions occurred (3.10%) within 90 days of discharge. There was no difference in comorbidity burden between the cohorts as measured by the Elixhauser Comorbidity Index. The only comorbidity that was found to increase the likelihood of 90-day readmission was diabetes with chronic complications (odds ratio [OR] = 1.86; 95% confidence interval [CI] = 1.17-2.95; P = .008). The following complication that occurred during the index hospitalization were associated with an increased odds of 90-day readmission: deep vein thrombosis (OR = 1.78; 95% CI = 1.23-2.57; P = .002), disruption of the surgical wound (OR = 2.39; 95% CI = 1.08-5.30; P = .03), hematoma/seroma (OR = 2.42; 95% CI = 1.20-4.18; P = .011), and pneumonia (OR = 3.84; 95% CI = 2.21-6.67; P < .001). An anterior surgical approach to the spine was associated with an increased risk of 90-day readmission (OR = 1.40; 95% CI = 1.12-1.75; P = .003). Interestingly, when compared with Medicare, patients with Medicaid (OR = 0.32; 95% CI = 0.17-0.59; P < .001), private insurance (OR = 0.67; 95% CI = 0.52-0.86; P = .002), and “other” pay as defined by the Healthcare Cost and Utilization Project (HCUP) (OR = 0.60; 95% CI = 0.41-0.88; P = .009) all had lower likelihood of 90-day readmission. Age, sex, and disposition status did not affect 90-day odds of readmission. The most common related cause for readmission was hardware complications, and readmission was found to be associated with a significant cost. Conclusion: As a whole, the odds of 90-day readmission for elective, revision lumbar spine surgery is relatively low given the inherent risks involved. Nonetheless, readmissions are costly to both the patient and the health care system. With the likely implementation of bundled payment models in spine, understanding where risk-mitigation strategies can be applied will certainly be of utility.
P356: Radiographic Sagittal Alignment in the Asymptomatic Elderly: What Is Normal for Age?
Brad Segebarth1, Casey Davidson1, Christian Klare1, David McConda1, Matt Chapman1, and Susan Odum1
1OrthoCarolina Spine Center, Charlotte, NC, USA
Introduction: Over the past several years, there has been an increasing awareness of the impact of positive sagittal alignment in the overall health-related quality of life (HRQOL).1-3 However, attempts to restore normal spino-pelvic parameters in the elderly population can introduce challenges with risk factors inherent in this age group and complications such as proximal junctional failure are high.4,5 The purpose of this study is to help define “normal for age” SVA (sagittal vertical axis) in asymptomatic individuals ranging 60 to 80 years in order to create an acceptable target for postop realignment in these patients. Material and Methods: One hundred and thirty-five volunteers were recruited and divided into cohorts for age ranges of 60, 65, 70, 75, and 80 years. Subjects were asked to complete ODI (Oswestry Disability Index) and VR-12 (Veterans Rand 12) questionnaires as well as stand for a full lateral radiograph. The primary outcome measure was the SVA with other measurements including thoracic kyphosis (T4-T12), total lumbar lordosis (L1-S1), lumbar lordosis (LL; L4-S1), pelvic tilt (PT), pelvic incidence (PI), pelvic incidence lumbar lordosis mismatch (PI-LL), sacral slope (SS), and T1 spino pelvic inclination (T1SPi). Exclusion criteria included any history of back pain requiring medical attention within previous 1 year, prior spinal surgery, neuromuscular condition, or compression fracture. Statistical analysis was performed with significance set at (P < .05). Results: The mean SVA for the 60-, 65-, 70-, 75-, and 80-year age groups were 21.55, 18.22, 27.68, 37.3, and 39.04 mm, respectively, which, overall, were not significantly different and were in the normal range of <40 mm (P = .1083).1 We did find significant differences between the age groups in L1-S1 (P = .0056) and SS (P = .0113), with a positive correlation between age group and L1-S1 (P = .0006) and a negative correlation between age group and SS (P = .0061). The mean L1-S1 for the age groups were 57.32°, 52.93°, 53.4°, 48.77°, and 45.39°, respectively, with significant differences between the 60- and 75-year age groups (P = .0382) and the 60- and 75-year age groups (P = .006). The mean SS for the age groups were 39.18°, 32.97°, 34.33°, 32.57°, 32.17°, respectively, with significant differences between the 60 year and 70 year age groups (P = .0354), the 60- and 75-year age groups (P = .0194), and the 60- and 80-year age groups (P = .0384). The ODI and VR-12 scores were not significantly different between the age groups. Conclusion: Asymptomatic elderly individuals maintained a relatively normal SVA; however, full-body radiography may better demonstrate other compensatory mechanism accounting for this.
P357: A Population-Based Study Evaluating Patient Outcomes Following Surgery for Spinal Metastases
Kunal Bhanot1, Jessica Widdifield2, Anjie Huang3, Michael Peterson3, David Shultz4, and Joel Finkelstein2
1University of Toronto, Toronto, Ontario, Canada
2Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada
3Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
4University Health Network, Toronto, Ontario, Canada
Purpose: Metastatic spread of cancer to the vertebral column is of significant clinical and epidemiological concern. Up to one third of all patients with cancer develop metastases to the spine. Bone is the third most common site of metastases after the liver and the lungs, and two thirds of all bone metastases are located in the spine. With advances in spinal metastasis management, including improvements in surgical technique, chemotherapy, and stereotactic radiotherapy (SBRT), we hypothesize that life expectancy has improved over the past decade. The aim of this study is to evaluate the survival of patients who have undergone surgery for spinal metastases in Ontario, a province within Canada, and evaluate risk factors that may be associated with poor survival. A secondary objective is to determine postoperative complication rates, assess differences in outcomes based on mode of radiation therapy, and assess hospital readmissions and repeat spine surgery (eg, vertebroplasty, kyphoplasty). Methods: A population-based, retrospective cohort study of patients who underwent surgical treatment of spinal metastases in Ontario between 2002 and 2015 is underway. Using the Ontario Cancer Registry, the Discharge Abstract Database (DAD), and Ontatio Health Insurance Plan (OHIP) procedure codes, we will identify all patients who had undergone surgery for spinal metastases between 2002 and 2015. After identification of the primary cancer diagnosis for the metastatic lesion, surgical procedures (and dates performed) for decompression/reconstruction surgery of a spin mestastatic lesion will be identified from the DAD. Additionally, we will ascertain the use of SBRT, conventional RT (CRT), chemotherapy, and vertebroplasty or kyphoplasty. The primary outcome of interest is time to death. Secondary outcome measures will include postoperative complication rates (including stroke, myocardial infarction), vertebral fractures, and hospital readmissions and repeat spine surgery (eg, vertebroplasty, kyphoplasty). Statistical Analysis: Descriptive analyses will be used to characterize patients undergoing surgery for spinal metastases. Univariate analysis will be used to compare patient demographics and clinical characteristics at the time of their index surgical admission by radiotherapy (CRT vs SBRT) and chemotherapy (neoadjuvant/adjuvant versus none). In addition to a Kaplan-Meier (KM) survival analysis, a multivariable Cox proportional hazard regression analysis will be performed to identify independent prognostic factors associated with survival. For secondary outcomes, cumulative incidence curves (KM curves taking into account competing risk of death) will estimate the probability of the occurrence of these outcomes (separately) over time. Significance and Conclusions: These results will provide patients, families, and clinicians with objective data to help in the choice of treatment and the understanding of surgical risk and outcome.
Imaging
P358: Demographic Analysis of Pedicle Diameters in a Diverse Population
Joseph Albano1, Jonathon Lentz1, Robert Stockton1, Vincent Depalma1, Michael1 Markowitz1, Gus Katsigiorgis1, and Kanwarpaul Grewal1
1Plainview Hospital, Northwell Health, Plainview, NY, USA
Introduction: A retrospective review of all computed tomography (CT) abdomen and pelvis studies performed over a 2-week period focusing on lumbar pedicle measurements. We sought to determine the difference in pedicle diameter (PD) in the lumbar spine compared between different races, including “Asian,” “Black,” “Other,” and “White.” This data aids in perioperative planning during instrumented spinal fusion. Studies have supported the relationship between PD and maximum pedicle screw diameter. There are also studies analyzing PD within specific populations, but none comparing PD between races. Methods: Coronal cuts of 5060 lumbar spine pedicles were inspected to obtain the transverse outer cortical PD as measured through the isthmus at lumbar segments 1 through 5. Data was collected and categorized based on patient-reported race. We looked at average PD and PD range at each level for each race. The data was analyzed using mixed ANOVA (analysis of variance) to determine significance. Results: The “Asian” cohort consistently had significantly smaller PD at L1-L5 than “Blacks” and “Whites” (P < .001), and “Others” had significantly smaller PD than “Blacks” (P < .001) and “Whites” (P = .032). At L1-2 “Other” group showed the least variability in PD. At L3-5 “Asian” population showed the smallest range, and the “Black” population had the largest variability in PD except at L5. There was significant difference in PD between different races. Conclusions: The Asian population consistently had significantly smaller pedicles in the lumbar spine than the Black or White populations. We recommend the use of preoperative CT for pedicle screw templating as the safest method of pedicle screw instrumentation with the strongest pullout strength because of the wide range of PD in “Black” population and the variability of PD between races.
P359: Inserting C1 Lateral Mass Screw Using the Intersection Between Lateral Mass and Posterior Arch as a Reference: Radiographic Study
Torphong Bunmaprasert1 and Watcharapong Puangkaew1
1Chiang Mai University, Chiang Mai, Thailand
Introduction: C1 lateral mass screw fixation has been used in posterior C1-C2 fixation to stabilize the atlantoaxial joints in various disorders. Proper entry point and trajectory of C1 lateral mass screw insertion is required to prevent massive neurovascular injuries. Prior techniques for screw insertion have been proposed, but all of them requires extensive dissection of C1 lateral mass causing lethal bleeding. Purpose is to determine proper C1 lateral mass screw placement and trajectory by using the intersection between medial border of the posterior arch and the lateral mass as an isolated medial reference. Material and Methods: Seventy 3-dimensional computed tomography reconstruction images were simulated. Virtual placement of C1 lateral mass screws were performed in 4 entry points and 2 trajectory angle parameters. The safety during simulating screw insertion and the screw length were evaluated. Results: C1 lateral mass screws could be placed bilaterally in 3 mm.and 5 mm lateral from the reference point in both 0° and 15° medial screw angulation without cortex violation. The average screw length within the lateral mass in 3 mm and 5 mm lateral from the reference point was 16 mm in 0° medial angulation and 18 mm in 15° medial angulation respectively. Conclusion: C1 lateral mass screw is safely placed in 3 mm and 5 mm lateral from the intersection between medial border of the posterior arch at its junction with the lateral mass beneath the posterior arch. The 15° medial angulation trajectory is recommended because of increasing the screw length and pull-out strength.
P360: Diffusion Weighted Magnetic Resonance Imaging to Differentiate Vertebral Hemangiomas From Spine Metastases
Vadim Byvaltsev1, Serik Akshulakov2, Alexander Kichigin1, Andrei Kalinin1, Evgenii Belykh1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
2 National Center of Neurosurgery, Astana, Kazakhstan
Introduction: The purpose of this study was to identify apparent diffusion coefficient (ADC) values for typical vertebral hemangiomas in the spine and to compare them with spine metastases. Materials and Methods: This was a retrospective single-center study. Diffusion-weighted MRI (magnetic resonance imaging) scans of 57 patients with metastatic tumors were analyzed. ADC values of typical vertebral hemangiomas and spine metastases were recorded. Results: The ADC of hemangiomas (median ADC = 1065 mm2/s, interquartile range = 934-1178 × 1 mm2/s) was significantly higher than the ADC of spine metastases (median ADC = 682 × 10−6 mm2/s, interquartile range = 577-1133 mm2/s; P < .01). An ADC threshold of 868 mm2/s separated hemangiomas from spine metastases with a sensitivity of 81.4% and specificity of 89.6%. Conclusions: ADC values of classical vertebral hemangiomas are significantly higher than spine metastases. The high ADC of vertebral hemangiomas allows them to be distinguished visually and quantitatively from active sites of disease, which show restricted diffusion.
P361: A Novel Method of Thorax Development in Children With Early-Onset Scoliosis
Nikita Khusainov1 and Sergey Vissarionov1
1Saint-Petersburg, Russian Federation
Introduction: Thoracic insufficiency syndrome is one of the biggest issues in children with EOS (early-onset scoliosis). There are a few imaging methods for evaluation of thorax and lungs development in these patients including SAL (space available for the lung) and thoracic index of asymmetry. These methods require computed tomography (CT) or MRI (magnetic resonance imaging) for evaluation and are complex in calculation. Material and Methods: We developed a novel method for evaluation of thorax condition and development based on Th1-Th12 height and the chest width at the level of the Th12 vertebrae measured on a simple AP (anteroposterior) X-ray film. This index does not depend on the scale of the film as it is being calculated in relative manner using the following formula: Th1-Th12 height (cm)/chest width (cm). We measured this index in 50 children aged from 1 year to 11 years without thoracic spine deformity who were examined with an X-ray for lung disease or in process of lumbar spine trauma evaluation for the purpose of getting normal mean value. The same was done in 60 patients of the similar age with multiple congenital spine deformities before and after the surgical treatment to analyze its effect on thorax development. Also CT scan before and after surgery was performed in order to calculate the lung volume in 13 patients. Results: Mean normal value for purposed index in control group was 0.93 ± 0.06 (0.8-1.0) and did not differ significantly between the age groups (P > .05). Mean preoperative value in study group was 0.74 ± 0.13 (0.5-1.0) and also did not differ between the age groups (P > .05). Postoperative mean value did not significantly differ from the preoperative one and was 0.76 ± 0.13 (0.6-1.0). These results were supported by the CT data, which showed no significant changes before and after treatment: 990.6 ± 399 cm3 and 972.8 cm3± 346.1 cm3 (P > .05), respectively. The strength of correlation was statistically significant (P = .01) according to Spearman’s test. Conclusion: Our data supports the thesis that proposed method is highly specific for evaluation of thorax condition and development in children with thoracic spine deformities. We assume that the absence of difference between the children of different age in control group is related to constant increase of both Th1-Th12 height and chest width whereas lower values in study group were related primarily to the decrease of Th1-Th12 height due to the scoliotic and kyphotic deformity.
P362: Predictors of Successful Outcomes of Selective Nerve Root Blocks for Acute Lumbar Disc Herniation
Rishi M. Kanna1, Ajoy P. Shetty1, and Rajasekaran S1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Selective nerve root block (SNRB) is an effective, standard interventional procedure for failed medical management for patients with acute lumbar disc herniation (LDH). However, the factors that would predict successful outcomes in patients undergoing SNRB has not been clearly studied. We performed a prospective, observational cohort study of consecutive patients presenting with radiculopathy due to acute LDH treated with SNRB. Methods: Patients with failed conservative treatment for at-least 3 weeks for acute LDH were treated with SNRB and periodically followed till 1 year. During follow-up, patients who failed to have consistent pain relief or had recurrent pain after SNRB underwent surgery. Various clinical, radiological factors, and radiculogram images (pattern of radiculogram during SNRB was classified into 4 types—“arm,” “arrow,” “linear,” and “splash”) were compared between patients who had consistent pain relief (group A) and those patients whom did not (Group B). Results: During the study period, 91 patients underwent SNRB and formed the study cohort. During the follow-up, 69 patients (group A) had good pain relief maintained till 1 year (69/91,75.8% efficacy). Twenty-two patients, either did not have adequate pain relief (n = 8) or had a temporary period of relief followed by severe pain (n = 14), underwent surgery at a mean of 6.3 weeks after the failed NRB (group B). Univariate analysis showed that patients with sensory symptoms (P = .01), higher mean pre-injection Oswestry Disability Index (ODI) score (P = .02), higher mean postinjection ODI score at 3 weeks (P = .004), white-collared office job (P = .01), and lumbo-sacral transitional segment (P = .00005), and splash pattern of radiculogram (P = .005) were predictive of failed NRB. Other factors including age, sex, duration of symptoms, side of pain, level, presence of back pain, smoking, comorbidities, body mass index, VAS (visual analogue scale) score, previous attacks, SLR (straight leg raise) positivity, and other MRI (magnetic resonance imaging) findings (disc type and position, level of degeneration) were not predictive. Multivariate logistic regression analysis showed that presence of lumbo-sacral transitional segment (P = .0005) was the most significant factor for predicting a failed SNRB. Conclusion: SNRB is an effective technique to provide consistent symptom relief at least till 1 year in patients with acute LDH. The study identified several factors that predicted poor outcomes of SNRB and such patients can be forewarned about need for later surgery. The radiculogram, observed after injecting the dye, was broadly classified into 4 types as “arm,” “arrow,” “linear,” and “splash.” ARM pattern was defined as a thick band of dye around the entire thickness of the nerve root, ARROW pattern was defined by the flow of the dye around the medial aspect of the nerve root and tracks down around the thecal sac, LINEAR pattern denoted as a single streak of dye along the lateral aspect of the nerve root, and the SPLASH pattern—an irregular distribution of the dye around the nerve root.
The radiculogram, observed after injecting the dye, was broadly classified into 4 types as “arm,” “arrow,” “linear,” and “splash.” ARM pattern was defined as a thick band of dye around the entire thickness of the nerve root, ARROW pattern was defined by the flow of the dye around the medial aspect of the nerve root and tracks down around the thecal sac, LINEAR pattern denoted as a single streak of dye along the lateral aspect of the nerve root, and the SPLASH pattern—an irregular distribution of the dye around the nerve root.
P363: Plain Roentgenographic and Computed Tomography Scan–Based Morphometric Analysis of the Craniovertebral Junction in Indian Population
Nandan Marathe1 and Sudhir Srivastava1
1Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India
Introduction: The craniovertebral junction (CVJ)—defined as the occiput, atlas, and axis—is a complex area that houses vital neural and vascular structures while achieving the most mobility of any segment within the spine. Because of the vital structures present in the craniovertebral region, the operating surgeon should have a thorough anatomic knowledge of the dimensions of the CVJ to avoid damage to these structures. The purpose of this narrative review is to provide an up to date overview of CVJ anatomy and morphometric measurements of various parameters in Indian population, as these are subject to racial and ethnic variability, and compare the dimensions with those of other populations. We will also compare dimensions as measured on X-ray and computed tomography (CT) scan. Materials and Methods: The study included 116 subjects who presented to a tertiary care center in the year 2015 and 2016 with history of head trauma thereby requiring X-ray and CT scan. Retrospective analysis of the data was done. Parameters measured included clivus canal angle, dimensions of the foramen magnum, anteroposterior and mediolateral dimensions of dens, height of dens, dens axis angle, atlantodens interval, distance between tip of dens, and McRae lines. Patients younger than 18 years, cervical spine fracture and dislocation, previous surgeries, and rheumatoid arthritis were excluded from the study. Results: Mean Clivus canal angle as measured on X-ray was 150.53° and CT was 150.51°. Mean anteroposterior (AP) diameter of foramen magnum on CT scan was 33.48 mm, distance between anterior and posterior ends of occipital condyles was 16.5 mm and 36.68 mm, respectively. AP diameters of dens on X-ray and CT were 9.58 mm and 9.61 mm, respectively; ML diameter of dens on X-ray and CT were 8.21 mm and 8.18 mm, respectively. Height of dens on X-ray was 14.33 mm and 14.36 mm on CT. Dens axis angle as measured on X-ray and CT is 10.04° and 10.07°, respectively. Anterior atlantodens interval as measured by X-ray and CT was 1.418 mm and 1.464 mm, respectively; posterior atlantodens interval as measured on X-ray and CT was 18.69 mm and 18.73 mm, respectively. Distance between tip of dens and McRae line was 4.67 mm on X-ray and 4.7 mm on CT. Conclusion: These dimensions will be useful to determine what measurements are to be done in preoperative planning and to classify Indian patients as normal or abnormal. There is no significant difference between measurements made on X-ray and CT scan; hence, X-ray is a reliable diagnostic technique for assessing morphometry of CVJ in emergency setting.
P364: Can C7 Slope Be Used as a Substitute for T1 Slope? A Radiographic Analysis
Ivan Ye1, Ray Tang1, Zoe Cheung1, Samuel White1, Jun Kim1, and Samuel Cho1
1 Mount Sinai Health System, New York, NY, USA
Introduction: Sagittal imbalance in the cervical spine is a major cause of neck pain, headache, fatigue, and disability. While parameters such as C2-C7 lordosis and C2-C7 sagittal vertical axis have been extensively studied, they do not fully characterize cervical sagittal balance. T1 is an important new parameter of both cervical as well as global spinal sagittal balance. However, the T1 superior endplate can be difficult to visualize on standard lateral radiographs due to overlying anatomical structures. C7 slope has therefore been proposed as a potential substitute for T1 slope when the T1 superior endplate is not well visualized. The objectives of this study were (1) to assess the correlation between C7 slope and T1 slope on upright lateral cervical spine radiographs, and (2) to evaluate the inter-rater reliability of C7 slope. Material and Methods: Cervical spine radiographs taken between December 2017 and June 2018 at a single institution were reviewed. Only radiographs with visible C7 superior and inferior endplates and T1 superior endplate were included. Radiographs with cervical instrumentation were excluded. Two independent observers measured upper C7 slope, lower C7 slope, and T1 slope. The correlations between upper C7 slope and T1 slope, as well as between lower C7 slope and T1 slope were evaluated. Linear regression analyses were also performed. Inter-rater reliability of C7 slope as assessed. Results: A total of 650 radiographs were reviewed. The superior endplate of C7, inferior endplate of C7, and superior endplate of T1 were visible in 72.9%, 50.2%, and 31.2% of these radiographs, respectively. After applying our exclusion criteria, 152 patients remained and were included in our analysis. The average age was 48.1 years, with 70.4% females. The average upper C7 slope, lower C7 slope, and T1 slope was 23.5 ± 9.1°, 22.9 ± 9.0°, and 27.5 ± 8.7°, respectively. There was a strong correlation between upper C7 slope and T1 slope (r = .91, P < .001), as well as between lower C7 slope and T1 slope (r = .90, P < .001). Linear regression analyses showed that T1 slope could be estimated from C7 slope based on the equation, T1 slope = 0.87 × C7 slope + 7, with an overall model fit of R 2 = .8. There was strong inter-rater reliability for upper (intraclass correlation coefficient [ICC] = 0.95, P < .001) and lower (ICC = 0.96, P < .001) C7 slope. Conclusion: The upper and lower C7 slope are strongly correlated with T1 slope and can be used as a substitute to estimate T1 slope when the superior endplate of T1 is not well visualized.
P365: The Use of Magnetic Resonance Imaging by Spine Surgeons in Management of Spinal Trauma and Spinal Cord Injury Across AO Regions: Results of AOSpine Survey
Saman Shabani1, Ha Son Nguyen2, Mayank Kaushal1, Hesham Soliman1, Bizhan Aarabhi3, Mark Kotter4, Michael Fehlings5, Brian Kwon6, James Harrop7, and Shekar Kurpad1
1Medical College of Wisconsin, Milwaukee, WI, USA
2California Institute of Neuroscience, Thousand Oaks, CA, USA
3University of Maryland, Baltimore, MD, USA
4University of Cambridge, Cambridge, UK
5University of Toronto, Toronto, Ontario, Canada
6University of British Columbia, Vancouver, British Columbia, Canada
7Thomas Jefferson University, Philadelphia, PA, USA
Introduction: AOSpine has been at the forefront of developing and regulating the standard of care in spine trauma and spinal cord injury (SCI). Evaluation and treatment of patients with SCI often involves multiple steps due to their complexity. Radiographic imaging plays an important role in the evaluation of these patients. Although magnetic resonance imaging (MRI) has an integral role in management of these patients, its usage across physicians from different continents has not been assessed. The goal of this AO-funded study was to assess the current trends and limiting factors in accessibility to MRI across spine surgeons in different AO regions. Material and Methods: A survey regarding MRI accessibility was conducted across the 6 global AO regions (Africa, Asia Pacific, Latin America, Middle East, Europe, and North America). Responses were tabulated with frequencies and percentages. Pairwise comparison regarding the distribution of responses between AO regions were performed. Results: A total of 561 surgeons from 6 global AO regions completed the survey (Africa 3%, Asia Pacific 22.1%, Europe 30.8%, Latin America 25.7%, Middle East 9.4%, and North America 8.9%). With regard to the availability of MRI, 31.9% responded that MRI was readily available at all times, 51.3% noted 24-hour availability, which was more difficult during night time, and 8.7% of participants reported not having MRI at their hospital. With regard to the time taken to obtain scans if MRI is readily available, 32.4% responded the imaging would be completed within 1 hour while 39.9% stated the imaging would be completed between 1 and 4 hours. Latin America (18.8%) and Africa (23.5%) noted the lowest proportions while Europe (42.8%) and North America (36%) noted the highest proportions. Latin America responses were significantly different (P < .05) compared with all other AO regions except Africa. Responses from Africa were significantly different (P < .05) compared with all other AO regions except Latin America and Middle East. Finally, when asked about the time taken to obtain scans during a time when MRI is least available, 7% responded the imaging would be completed within 1 hour while 31.4% stated the imaging would be completed between 1 and 4 hours. Similar relationships to other AO regions were observed for both Latin America and Africa. Conclusion: MRI utilization varies across AO regions. Overall, a large determinant is the availability of resources such as radiologists and imaging units per population size. Further study is required to assess differences, if any, in the preference for MRI as an imaging modality in different clinical scenarios among different AO regions. The impact of the use of MRI on clinical outcome is difficult to assess given its limited availability and use.
P366: Analysis of Bacterial Adherence of Clinical Relevant Staphylococcus Species on Carbon/PEEK Composite Versus Standard Titanium: Possible Implications in Spinal Instrumentation for Spondylodiscitis
Ehab Shiban1, Ann-Kathrin Jörger1, Andreas Obermeier2, Rainer Burgkart2, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
2Klinik für Orthopädie und Sportorthopädie, Technische Universität München, Munich, Germany
Background: Spinal instrumentation in neurosurgery has giant popularity for the treatment of spondylodiscitis. Thereby most of the implants are made of titanium alloys (Ti), which is associated with artefacts on postoperative imaging. However, for patients with suspected relapse of the infection, these artefacts render these imaging modalities to be useless. Recently, carbon fiber–reinforced polyetheretherketone (CFRP) implants became available for posterior instrumentation with the aim to reduce imaging artifacts by implants. The aim of this study was to compare the bacterial adhesion by numbers on titanium with CFRP, in order to evaluate the material-associated property to facilitate such infections. Methods: A bacterial adhesion assay was conducted with the main surgical site infection bacterial strains—Staphylococcus aureus (ATCC 25923), S epidermidis (ATCC 35984), and methicillin-resistant S aureus (ATCC 43300). Within the adhesion assay, both types of implants polished titanium discs and CFRP discs were incubated in bacterial suspensions (1.3 × 105 colony-forming unit [cfu]/mL) over 24 hours. Then, viable adhered bacteria on implant surfaces were determined quantitatively after sample sonication and plating of supernatants on agar. Colonies were counted for each sample. Moreover, to characterize material surfaces the average roughness (Ra in μm) was measured with a stylus surface profilometer Dektak 8 (Veeco Inc, Plainview, NY). Additionally, contact angles were measured with the sessile drop method using standardized fluids, followed by calculating the surface free energy for each sample type. Results: Incubation in bacterial suspensions resulted in numbers of adhered bacteria on CFRP (methicillin-resistant S aureus [MRSA] = 8.7 × 106 cfu; S aureus = 7.6 × 106 cfu; S epidermidis = 6.4 × 106 cfu), and on Ti controls (MRSA = 3.3 × 106 cfu; S aureus = 3.6 × 106 cfu; S epidermidis = 4.0 × 106 cfu). Each cfu-value per sample is the average of at least 8 samples. There are no significant differences between cfu numbers of adhered bacteria on CRRP and Ti materials. Surface profilometry showed Ra values for titanium at 0.20 ± 0.04 μm and 0.38 ± 0.10 μm for CFRP. Both materials showed a similar hydrophilic wettability by water (contact angels = 83° for Ti and 73 for CFRP). Completely different surface energy values were measured (overall/polar/disperse), for titanium (39.0/38.9/0.1 in mJ/m2) and CFRP (12.4/12.4/∼0 in mJ/m2). Conclusion: Despite CFRP has a roughness double as titanium, there were no significant differences in bacterial adherence of MRSA, S aureus or S epidermidis between CFRP implants and Ti implants. Possibly, because of CFRP’s low surface free energy, the bacterial adhesion could be determined at a comparably low level as for polished titanium. The application of carbon/PEEK (CFRP) in neurosurgical instrumentations is a promising approach to combine the properties of titanium, possibly without increasing infection rates and the benefit of reducing imaging artefacts.
P367: Reduced Radiation Exposure With a New Mobile 3-Dimensional C-Arm
Oliver Strohbach1, Eduardo M. Suero1, Benjamin Els1, Wolfgang Boecker1, Christian Kammerlander1, and Simon Weidert1
1 Ludwig Maximilian University of Munich, Klinikum Grosshadern, Munich, Germany
Introduction: In the past decade, several manufacturers have introduced mobile C-arms with 3-dimensional (3D) capabilities that offer intraoperative visualization quality similar to that of multidetector computed tomography (MDCT), thus improving spinal procedures by allowing implant control or computer navigation on intraoperative datasets. However, radiation exposure to the patient remains a primary concern when using these devices. Recently, a new motorized mobile C-arm with improved CMOS flat-panel detector and Beam Filtration technology (Vision RFD CMOSline, Ziehm, Nurenberg, Germany) was introduced with the aim of further improving image quality while significantly reducing radiation exposure to the patient. We aimed to compare radiation exposure between a standard MDCT scan and 3D scans using both the newly introduced C-arm and its previous generation (Vision RFD3D) in a phantom setting. Material and Methods: We used a polymethyl methacrylate (PMMA) phantom to simulate the torso of an adult human patient in the supine position. The phantom has a cylindrical shape with a diameter of 32 cm and has 5 specific areas for radiation dose measurement at the top, bottom, left, right, and center regions. The phantom was placed on a carbon operating table and carefully centered within the C-arm’s field of view. Using each of the C-arms, 3D scans using 2 different protocols (standard and large patient key [LPK]) were obtained and the radiation dose was measured at the 5 different locations within the phantom using a radiation dosimeter. Then, CT scans with standard protocols were obtained and the dose measured at the same 5 locations. The main outcome measure was the CT dose index with a 100-mm standard pencil dose chamber (CTDI100). We also measured the radiation dose at each of 5 specific locations within the phantom. Results: CTDI100 with the previous-generation C-arm was 44% higher compared with CT using the standard protocol and 26% higher using the LPK protocol. In contrast, the new C-arm had 38% lower CTDI100 using the standard protocol and 40% lower CTDI100 using the LPK protocol compared with CT. With the standard protocol, the new C-arm achieved dose reductions of 37% to 66% at each of the center, top, right, and bottom locations compared with CT. The radiation dose at the left location was the same. With the LPK protocol, the C-arm achieved dose reductions of 31% to 77% at each of the center, top, right, and bottom locations compared with CT. The radiation dose at the left location was 6% higher. Conclusion: The new CMOSline C-arm demonstrated significantly lower radiation dose compared with both the previous-generation C-arm and standard CT scans. This reduced radiation dose, while at the same time achieving an image quality comparable to that of a CT scan, can facilitate intraoperative visualization of complex procedures. It also allows for acquiring 3D scans for navigation or to confirm implant placement with a patient dose equivalent to that of a diagnostic CT scan. Routine use of the device could lead to higher rates of intraoperative detection of complications, reducing the financial burden of postoperative imaging and revision surgery.
P368: Feasibility of Multiparametric Quantitative MRI Techniques to Measure Spinal Cord Injury
Allan Martin1, Muhammad Ali Akbar1, Jetan Badhiwala1, Julien Cohen-Adad2, Jefferson Wilson1, David Mikulis1, Benjamin De Leener2, Adrian Carwley1, Sukhvinder Kalsi-Ryan1, and Michael Fehlings1
1University of Toronto, Toronto, Ontario, Canada
2Polytechnique Montreal, Montreal, Quebec, Canada
Introduction: Conventional magnetic resonance imaging (MRI) only provides limited information about the structure and integrity of the spinal cord. We describe a multiparametric quantitative MRI protocol for microstructural analysis of the spinal cord to determine the precise degree of injury to the spine in the setting of degenerative cervical myelopathy (DCM) as well as traumatic spinal cord injury. Material and Methods: Thirty-five healthy controls and 56 DCM patients have so far been studied. Each patient underwent a battery of clinical assessments including modified Japanese Orthopaedic Association (mJOA), International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), QuickDASH (Quick Disability of the Arm, Shoulder, and Hand), GRASSP-M (Graded Redefined Assessment of Strength, Sensibility and Prehension), and GaitRITE. Each patient had MRI acquisitions using our protocol in a 3-T GE clinical scanner. The multiparametric protocol combines MRI techniques including conventional MRI, diffusion tensor imaging (DTI), magnetization transfer (MT), and T2*-weighted imaging (T2*WI). Image analysis was performed using the Spinal Cord Toolbox (SCT) v.3.0 to calculate spinal cord cross-sectional area (CSA), fractional anisotropy (FA), magnetization transfer ratio (MTR), and T2* weighted white matter to gray matter ratio (T2*WI WM/GM). Results: Study of healthy subjects identifies an alarming rate of asymptomatic spinal cord compression. Significant differences in 10 metrics were identified between 56 DCM and 32 healthy subjects. These 10 measures of tissue injury correlate with disability (mJOA) in a linear regression model (R 2 = .55) and T2*WI WM/GM showed strongest correlation with upper extremity motor and sensory scores (P = 1 × 10−11). Longitudinal study (ongoing) of DCM patients correlates qMRI findings with clinical assessment and suggest mJOA underestimates progression. Conclusion: We have established a reliable, clinically feasible quantitative MRI protocol where the combined methodologies in the protocol can help overcome several individual limitations. This protocol can be used for diagnosis, detection of subclinical tissue injury, and can potentially help with prediction of outcomes in DCM as well as spinal cord injury.
P369: Worldwide Knowledge and Attitude of Spine Surgeons Regarding Radiation Exposure
Asdrubal Falavigna1, Miguel Bertelli Ramos1, Chung Chek Wong2, Giuseppe Barbagallo3, Darrel Brodke4, Abdulaziz Al-Mutair5, Zoher Ghogawala6, and K. Daniel Riew7
1University of Caxias do Sul, Caxias do Sul, Brazil
2Sarawak General Hospital, Kuching, Malaysia
3Policlinico “G. Rodolico” University Hospital, Catania, Italy
4University of Utah, Salt Lake City, UT, USA
5Alrazi Hospital, Ministry of Health/Kuwait Institute for Medical Specialization, Adailiya, Kuwait
6Alan and Jacqueline Stuart Spine Center, Lahey Hospital and Medical Center, Burlington, MA, USA
7The Och Spine Hospital, Columbia University, New York, NY, USA
Introduction: Spine surgery often requires the use of radiation by means of fluoroscopy during surgery, and fluoroscopy-assisted spinal procedures are on the rise worldwide due to the growth in the popularity of minimally invasive techniques and endoscopy. These techniques often require real-time fluoroscopic visualization to perform precise intraoperative localization and minimize instrument and implant malposition, leading to an increase in the exposure of spine surgeons to radiation. Since studies of spine surgeons’ knowledge and attitude regarding radiation exposure are scarce in the literature, this study aims to assess worldwide the spine surgeon’s perceptions and attitudes regarding radiation exposure during spine procedures. Material and Methods: Questionnaire about general information and the surgeon’s perception and attitude regarding radiation exposure during spine surgery. We sent it to worldwide AOSpine members from December 15, 2016, to April 15, 2017. The main variables studied were specialty, years of experience, surgeon’s position during fluoroscopy, and practices to reduce the patient’s and surgeon’s radiation exposure during surgery. Results: The questionnaire was answered by 979 spine surgeons, who were members of AOSpine Latin America (n = 371), European Union (n = 248) Asia Pacific (n = 204), North America (n = 112), and Middle East (n = 44). Most were orthopedic surgeons (64.5%) with ≥10 years of experience (54.9%). A thyroid shield was used by 66.4% and lead glasses by 17.3%. A dosimeter badge was rarely or never used by 67.8% of the participants. Only 36.7% of the surgeons worldwide knew the correct answer for optimum surgeon position during lateral lumbar fluoroscopy, with the highest percentage being among North American spine surgeons (61.6%; P < .001). Pulse-mode fluoroscopy is used with a similar frequency among regions. Conclusion: Independent of the region analyzed, we observed a lack of adequate awareness regarding intraoperative radiation exposure as well as available safety measures. We strongly recommend further education for all spine surgeons using fluoroscopy during surgical procedures.
P370: Segmentation of the Caudal End of the Myelon and the Escaping Fibers Through MRI
Helena Nics1, Georg Grohs1, Gregor Kasprian2, Klaus Friedrich2, Petra Krepler1, Reinhard Windhager1, and Anna Rienmueller1
1 Department of Orthopedics and Trauma Surgery, Vienna, Austria
2 Department of neuroradiology and musculoskeletal radiology, Vienna, Austria
Background: The conus medullaris and its exiting nerve rootlets are able to almost move freely due to the fluid liquor surrounding them. During clinical interventions, we use this to our advantage and change the body position to influence the intraspinal location of those structures. Still preoperational examinations are run in supine position while the surgical position of the patients is a prone position. The aim of this study was to investigate the dimensions of the influence of the position on the location of the intraspinal structures. Methods: Ten healthy probands were undergoing magnetic resonance imaging in supine and prone positions. To examine the change of the location of the intraspinal structures, we measured the angles of the escaping nerve fibers (enclosed between myelon and fiber), the anteroposterior diameter of the spinal cord, the height of the conus medullaris, as well as the anterior and the posterior distance from spinal cord to vertebral body or vertebral arc. Furthermore, the segmentation of the cauda equina plus the number of fibers belonging to the cauda equina was evaluated. The height of the intervertebral discs, the facet joint orientation and the segmental, and the total lumbar lordosis were mechanical parameters to gain knowledge about the surrounding conditions. All the parameters were compared via t tests to work out the significance of the changes between supine and prone position. Other than that, descriptive statistics were used to show the differences, as well as a generalized mixed model to compare the measured angles. Results: There was no significant change in the height of the conus medullaris after changing the position (50% no change, 40% cranially, and 10% caudally). Therefore, the number of fibers belonging to the cauda equina did not generally change. The segmentation of the cauda equina showed that the conus and the cauda move ventrally, when in prone position. This was confirmed by the significant change of the anterior distance to the vertebral body and the posterior distance to the vertebral arc. The anteroposterior diameter did not show a significant change, while the angles of the caudal posterior fibers showed significant differences. The total lordosis changed significantly and also the segmental lordosis has been proven to change significantly at the levels Th12/L1, L1/L2, L3/4, and L4/5. Furthermore, the height of the intervertebral discs changed significantly on levels Th12/L1, L1/L2, and on L4/L5. However, the orientation of the facet joints did not change significantly. Moreover, it was shown that in prone position a significant sagittal sliding is caused. Conclusion: The distance of the spinal cord to the vertebral body and the vertebral arc as well as the angles of the posterior nerve rootlets changed significantly when switching from supine to prone position in all patients. Moreover, sagittal gliding and focal lordosis significantly changed. Further studies are necessary to define if those changes have an influence on pathologies of the spine and patient’s symptoms.
P371: Primary Imaging Modality and Diagnostic Delays in Emergency Spinal Imaging: A Single-Center Prospective Observational Cohort Study
Christof Birkenmaier1, Bernd Wegener1, Volkmar Jansson1, and Carolin Melcher1
1Ludwig Maximilian University of Munich, Munich, Germany
Introduction: The need for emergency spinal imaging (ESI) arises on a regular basis. In most instances, magnetic resonance imaging (MRI) is the imaging modality that is primarily requested. Depending on a number of factors, MRI is not always immediately available to us and in these instances we often resort to computed tomography (CT) as a first line of imaging. In some cases though, additional MRI is necessary after CT in order to ascertain a diagnosis, which in turn creates delays in the diagnostic workup. At present, we have no precise knowledge of the possible consequences or even the absence of such. We therefore decided to prospectively collect and analyze all such events. Material and Methods: Since 2012 and after obtaining ethics board approval, we began to collect data on all cases in which ESI was requested from the radiology department. Among the parameters collected are suspected diagnosis, imaging modality requested, imaging modality available, delay to primary imaging, day of the week and time of the day, whether the primary imaging modality was sufficient to decide on the patient’s treatment, whether secondary imaging was required, delay to secondary imaging, and what the final treatment strategy was. In cases, where a decision for surgery was made, the time from decision to incision was recorded as well as the reason for any delays. Status at discharge was recorded. Results: A total of 131 events of ESI were recorded. There were 19 females and 10 males, aged on average 57 years. MRI was the primary imaging modality requested in 27 cases, CT in 2 cases. MRI was the primary imaging modality obtained in 16 cases, CT in 13 cases. There were 4 situations, where the on-call radiologist felt that a CT would be sufficient to examine the suspected pathology, only 1 of which required an additional MRI after the CT. In 3 cases of primary CT, MRI was additionally required whereas in only 1 case of primary MRI, an additional CT was necessary. In the 4 patients requiring secondary ESI, the total delay was on average 17 hours, ranging from 4 to 29 hours. Secondary imaging was necessary in 3 cases, where primary MRI had been requested and CT had been performed, but also in 1 case, where primary MRI had been requested and performed. The delay from decision to incision was 9.4 hours on average, ranging from 1.3 to 22 hours. The final presentation will provide updated data. Conclusion: In this series, we found that primary MRI (16 instances) was sufficient to ascertain a diagnosis with the exception of 1 case, whereas primary CT (13 instances) required 3 additional MRI to generate a reliable diagnosis. These initial data suggest that except in cases where implant position is the key issue, MRI should be the primary ESI of choice. Additional imaging requires additional time, and in this series, the mean delay from imaging request to decision was 3.4 as opposed to 17 hours, when a single imaging study was sufficient as opposed to when secondary ESI was necessary. An additional 9.4 hours delay from decision to incision has to be added to these numbers.
P372: Modified Position for Global Sagittal Balance Assessment in Imbalance Patient
Danaithep Limskul1, Asadapong Srinawakul1, Aticha Ariyachaipanich1, Weerasak Singhatanadgige1, Worawat Limthongkul1, and Wicharn Yingsakmongkol1
1Chulalongkorn University, Bangkok, Thailand
Introduction: The sagittal vertical axis (SVA) is important in spinal sagittal balance evaluation. Elderly patients with sagittal imbalance were usually assessed by whole-spine standing lateral view. Some patients have standing difficulty maintaining balance while performing radiography. We come up with new positions to facilitate imbalance patient who cannot tolerate stance position, which could be used as a substitute to evaluate global sagittal balance. The objective of this study is to evaluate the correlation of new positions to evaluate sagittal balance assessment from standard method. Material and Methods: Thirty healthy candidates (15 males, 15 females) had their SVA evaluated by whole-spine lateral film in 4 positions: standard standing with hands on the clavicles with elbows touching the trunk (TC), standing with hands hold on to a front stationary within arm reach distance (TS), sitting with hands on the clavicles (IC), and sitting with hands hold on to stationary (IS). The measurement was done and compared with the differences and correlation between each position. Results: The mean SVA of TS group (−0.26 ± 2.52 cm)., compared with TC group (−0.38 ± 1.55 cm) shows no statistically significance (mean difference = 0.12; 95± CI [confidence interval] = 1.72-1.96 cm, P = .89) and has moderate correlation (r = .67). SVA of IC and IS has low correlation with TC and both have increased positive balance. Conclusion: TS position can be used as a substitute when measuring SVA in patients with standing difficulty while performing radiography. Though sitting can be performed with ease, the positions does not correlate well with standard SVA measurement.
P373: Anatomical Variation of C2 Pedicle Using 3-Dimensional Reconstruction Technique: Standardization to the General Population
Luis Miguel Marques1 and Miguel Brito1
1de Egas Moniz Hospital, Lisbon, Portugal
Introduction: Surgical fixation of C2 pedicle has gained popularity, as it is believed to be biomechanically the most stable C2 fixation technique. The main technical limitation is the vertebral artery variability and the true dimension of C2 pedicle. There is controversy in literature in the proportion of pedicle screws that are feasible for surgical fixation, and no published method of measuring it is currently standardized. The authors propose to study the true dimension of C2 pedicle in general population, standardized by a 3-dimentional reconstruction technique using a DICOM software OsiriX, previously published. Material and Methods: It was preformed a retrospective analysis to 49 consecutive CT (computed tomography) scans of cervical spine (98 pedicles) without traumatic, tumor, or malformation pathology. The minimum diameter of each C2 pedicle was calculated using a 2 step 3-dimentional reconstruction technique: first the correction to the true coronal and sagittal plane of C2 vertebrae, and then the interpolation of the orthogonal planes to the true anatomical plane of C2. It was considered a minimum of 4.5 mm for surgical feasible fixation of the pedicle, with 0.5 mm of security margin for each side of the screw. Results: Of the 49 patients, with ages between 24 and 87 years, 32 were female. The average of minimal pedicle diameter was 6198 mm (6.00 in women and 6.57 in men). A total of 84.7% and 78.6% of pedicles were feasible for surgical fixation using 3.5 mm or 4.0 mm screws, respectively, with the minimum 0.5 mm of security margin for each side of the screw. Conclusion: The authors conclude that almost 85% of C2 pedicles are feasible for surgical fixation and that the 3-dimentional reconstruction technique of the C2 pedicle is a fundamental tool in preoperative planning.
Infections
P374: Spondylodiscitis Secondary to Stab Wound
Rafael Sanchez1
1AOSpine, Havana, Cuba
Introduction: Spondylodiscitis is one of the forms of presentation of infectious processes in the rachis. It can be observed in immunocompromised patients or secondary to local interventions such as blockages or procedures of minimal access to the spine. Given the unusual occurrence of spondylodiscitis secondary to sharp trauma, and the presence of early imaging signs capable of showing the spread of the infection from the site of the lesion to the vertebral segment, a case of spondylodiscitis secondary to stab injury is presented. Material and Methods: We report a 48-year-old male patient with previous health history, who suffered a stab wound in the left lumbar region. After trauma, he began to present pain in the lumbar spine and absolute functional impotence. Laboratory and imaging studies are performed. The hematological parameters inclined to the diagnosis of an infectious process in the column and the nuclear magnetic resonance evidenced lumbar spondylodiscitis, as well as the fistulous path of the infection from the skin to the affected segment. Treatment consisted of administration of antibiotics and immobilization with a corset during 6 months. Results: The patient presented improvement of symptoms at 3 weeks, with total pain relief at 1 month. The hematological results gradually improved until reaching normality at 6 months. Conclusion: Spondylodiscitis produced by knife wounding is uncommon condition, but it should be suspected in any patient suffering from this type of injury.
P375: Is Dental Prophylaxis Required Following Spinal Fusion? A Systematic Review and Call for Evidence
Parker Martin1, Rajbir Hundal1, Kathryn Matulich1, Rakesh Patel1, and Ilyas Aleem1
1 University of Michigan Medical School, Ann Arbor, MI, USA
Introduction: Controversy exists regarding the need for antimicrobial prophylaxis prior to dental procedures following spinal fusion. Neither spinal surgeons nor dentists have evidence-based guidelines regarding dental prophylaxis in protecting against hematogenous infection of spinal instrumentation. As the number of spinal fusions increases significantly, the lack of clear guidelines poses a problem as no standard of care has been established for these patients. In this review, we attempt to synthesize a comprehensive summary of the published literature to provide recommendations on the use of antimicrobial prophylaxis before dental procedures in patients with a history of spinal fusion. Material and Methods: We searched PubMed, Web of Science, Cochrane Library, and EMBASE databases from inception to February 2018. Eligible studies included patients with a history of spinal fusion treated with or without antimicrobial prophylaxis in preparation for dental procedures. Two reviewers independently assessed the eligibility of potential studies and extracted data. Outcomes of interest were the indications and efficacy of antimicrobial prophylaxis to protect against infection of spinal prostheses with dental origin. Results: A total of 1909 articles were initially screened. After inclusion and exclusion criteria were applied, one study was found specifically relating to dental prophylaxis and spine surgery. This was an expert survey, which revealed that approximately two-thirds of spine surgeons would not recommend antimicrobial prophylaxis for patients with a history of uncomplicated lumbar fusion. The survey, as well as objective studies and professional organization guidelines on dental prophylaxis in patients with total hip and knee replacements, were reviewed to add context to the controversy. Conclusion: There is a significant paucity of literature regarding dental prophylaxis in spine surgery patients. The continued disagreement revealed by expert surveys is likely due to the lack of research addressing this population in combination with shifting recommendations from professional organizations. Although there has been a recent movement away from recommending antimicrobial prophylaxis before dental work in patients with other forms of orthopedic prostheses, the gap in the literature addressing spine patients represents an important question that requires more targeted and specific research.
P376: Prevention of Surgical Site Infection in Lumbar Interbody Fusion
Kosuke Kuribayashi1
1 Department of Spine Surgery, Ainomiyako Neurosurgical Hospital, Osaka, Japan
Introduction: Although surgical site infection (SSI) is one of the serious complications in spine surgery, it is difficult to identify its cause. Meanwhile, posterior lumbar interbody fusion (PLIF) is useful for degenerative lumbar disease, but PLIF itself is a risk factor for both in posterior approach and using spinal instrumentation. Even after CDC (Centers for Disease Control and Prevention) guideline was extensively adhered, SSI rate in spinal instrumentation was said to be 1% to 2% in many reports. Next, Povidone-iodine (PVP-I) has strong sterilization ability, but organic matter prevents it from this ability. Furthermore, it is said that PVP-I can damage not only bacteria but also normal tissues and it may inhibit wound-healing. However, some say that it can be used safely and prevent SSI in spine surgery. On the other hand, hydrogen peroxide (H2O2) can wash away organic matter from tissue mechanically with gas although its sterilization is very short-acting. I report the important risk factors and preventive measures against SSI in PLIF from my experience. Material and Methods: Between 1997 and 2017, I performed PLIF with cages on 1254 consecutive cases for degenerative lumbar disease. Surgical wound was irrigated with PVP-I following H2O2 and saline just before closing it in every patient. Results: Neither PVP-I nor H2O2 caused neural disturbance. Ten patients (0.80%) developed SSI. Three had uncontrolled diabetes and 3 had previous spine surgery. Eight of 10 infection cases occurred during a particular period on which was disorder of the air conditioning systems of the operating room. Furthermore, there were no infection cases in other spine surgery at the same operation room on this period. If the operating room had been always clean, infection rate in my series would be only 0.16%. Conclusion: First of all, irrigation with a combination of PVP-I and H2O2 before closing wound is very useful for prevention from SSI. PVP-I sterilizes after H2O2 washes away organic matter from tissue. Second, it is essential to keep the operating room clean especially in PLIF. Finally, I would like to cite uncontrolled diabetes and previous spine surgery as the 2 major patient-related risk factors.
P377: The Effect of Intradiscal Vancomycin Powder in Prevention of Postoperative Discitis
Ghazwan Hasan1, Hayder Raheem2, and Luay Al-Naser3
1AlAlamy Hospital of Specialized Surgery, Baghdad, Iraq
2 Al-Mustansiriya Medical College, Baghdad, Iraq
3Baquba Teaching Hospital, Baquba, Iraq
Introduction: Post discectomy discitis although is relatively uncommon (4%) but it is regarded as most disabling causes of failed back surgery. Preoperative antibiotic decreases the risk of postoperative infection, many risk factors for infections are reviewed in the literature like diabetes mellitus, smoking, and increase the time of surgery. Material and Methods: This is a prospective randomized comparative study on 400 patients in which microscopic or open discectomy was planned either due to the failure of conservative treatment or the presence of neurological deficit at the time of presentation. The patients were divided randomly by simple randomization into 2 groups, each group 200 cases, the first group in which a local vancomycin powder was inserted in the disc space after finishing discectomy and in the second group nothing was inserted. The follow-up was done by a third team, which did not know the patients’ group and double blindness was applied. The follow-up was done clinically at 1 week, 2 weeks, 6 weeks, and 3 months, and in any suspicious cases, laboratory and MRI studies were performed. Results: In the second group, there were10 cases (5%) of postoperative discitis, 4 men and 6 women, ranging in age between 24 and 50 years, 3 were diabetics, 7 cases were in L4-L5 disc space, 3 cases in L5-S1. While in the first group (vancomycin group), there were 3 cases 1.5%, 1 male and 2 females, all at the level of L4-L5. Conclusion: We concluded that the intraoperative prophylaxis with vancomycin intradiscally is effective in decreasing the incidence of postoperative discitis
P378: Oral Cavity Infection: An Underestimated Source of Pyogenic Spondylodiscitis?
Alexander Romagna1, Christoph Schwartz1, and Stefan Zausinger2
1Paracelsus Private Medical University, Salzburg, Austria
2Klinikum der Universität München, Munich, Germany
Introduction: The incidence of pyogenic spondylodiscitis is increasing; however, the source of infection often remains obscure. We analyzed predisposing factors, pathogens, and outcome of patients undergoing surgical and/or conservative treatment of spondylodiscitis with focus on the diagnostic workup, including a comprehensive maxillofacial assessment. Material and Methods: The analysis of prognostic factors comprised comorbidities, nicotine-dependence, symptom duration, and oral cavity peculiarities. After a standardized diagnostic workup, a detailed examination of the oral cavity was additionally performed. The outcome analysis included assessment of the patients’ clinical status. Results: Forty-one patients with pyogenic spondylodiscitis were investigated of whom 24% had undergone spinal surgery within 4 weeks prior to the infection. A total of 29% of patients were found to suffer from a concomitant bacterial oral cavity disease, and in 22%, the definite source of infection remained unidentified. Among the 12 patients with oral cavity infections, 10 patients suffered from periodontitis, 8 from root canal pathologies, 6 from periapical lesions, and another 8 patients from caries; in 25% of these patients, typical oral cavity pathogens were found in the intervertebral disc. The prevalence of oral cavity infections was associated with a history of nicotine dependence (P = .003). All other analyzed comorbidities did not differ compared with patients without an oral cavity focus. Conclusion: Oral cavity infections appear to be a frequent source of pyogenic spondylodiscitis, with smoking being its most relevant associated risk factor. In case of an unidentified infection focus, a detailed diagnostic workup, including a mandatory maxillofacial assessment is strongly recommended.
P379: Minimally Invasive Treatment of Tuberculosis of Spine: An Old Disease With a Modern Way of Treatment
Aftab Younus1, Mohammad Hamza Sultan Aftab1, and Abdirashid Aden1
1Helen Joseph Hospital, University of Witwatersrand, Johannesburg, South Africa
Introduction: Tuberculosis is one of the oldest disease known to modern world. Its prevalence is increasing secondary to the high burden of HIV disease within the South African setting. Other factors involved include multidrug resistant tuberculosis and emigration of immigrants from neighboring countries of South Africa. Spinal tuberculosis accounts for 50% of musculoskeletal tuberculosis and most commonly affects the lower thoracic and thoracolumbar spine. This classic disease leads to distraction of the intervertebral disc and the adjacent vertebral body with the patient presenting with kyphotic deformity, gibbous formation, and neurological stigmata. Material and methods: In Helen Joseph Hospital, there were 3497 reported cases of pulmonary tuberculosis during the past 2 years (2015-2016). These included 29 case spinal tuberculosis. Out of these 13 patients presented with neurology and deformity of the lumber spine in addition 10 of these patients were HIV positive as well. All these patients underwent surgery, with 2 patients having precautious posterior spinal fusion, 2 patients having open posterior spinal fusion, 3 having spinal biopsies, 3 open thoracotomies, and 3 underwent thoracoscopic corpectomy and anterior spinal fusion. Result: All patients who underwent surgery were started on antituberculosis drugs. The neurology was graded according to Frankel grading system. Seven patients were classified as Frankel grade B, 1 patient Frankel grade A, and 5 patients were Frankel grade C. They were followed-up (and some continue to follow-up) at 6 monthly intervals for 2 years. All included patients had improved by 1 or 2 Frankel grades following the operation and antituberculosis treatment. The patients who had minimally invasive spine surgery showed early improvement and mobilization compared with the other patients. Conclusion: The outcome of following appropriate treatment of spinal tuberculosis is generally good, with about 85%-95% of patients showing improvement with deformity and neurological deficit. In patients with neurological deficit, good prognostic factors include young age, incomplete paralysis, and performance of good surgical decompression and stabilization. Minimally invasive surgery showed the advantage of early mobilization, less analgesia, early discharge from hospital, and earlier return to work.
P380: Multilevel Spinal Reconstruction in Pediatric Patients With Infectious Spondylitis: Predictors of the Late Postoperative Complications (3 and More Years Follow-up)
Denis Naumov1 and Alexandr Mushkin1
1Research Institute of Phthisiopulmonology, Saint Peterburg, Russian Federation
Introduction: The treatment of infectious spondylitis in pediatric patients is one of most difficult area in spinal surgery. Despite the large number of articles, focused on different surgical technique for pediatric spondylitis management, the data concerning late postoperative complications and their predictors is fully absent. According to this fact, the research goal is to find complications predictors of the multilevel spinal reconstruction in pediatric patients with infectious spinal lesions. Materials and Methods: A total of 197 pediatric patients were operated with 2 and more vertebral motion segments (VMS) reconstruction between 2005 and 2015 due to spine infections: tuberculosis spondylitis (n1 = 114) and pyogenic spondylitis (n2 = 83). Late postoperative complications were presented in 13 patients. Average follow-up period was 5 years and 4 months. Clinical parameters and radiological data were evaluated. SPSS v. 22, ANOVA (analysis of variance) were used for analysis of predictors influence for late complications developed. A P value of less than .05 was considered statistically significant. Results: There were not any complications during early (from 9 to 30 days) or delayed (before 12 months) postoperative period. All 13 complications developed minimum 12 months after initial surgery (median = 2 years 9 months). Four types of complications were found: (1) late recurrence/progression of primary infection (n1 = 4); (2) non-fusion between bone-graft and recipient vertebra (n2 = 5); (3) proximal junctional kyphosis (n3 = 3); and (4) bone-graft resorption (n4 = 1). Thoracic lesions related to deformity progression (P 1 = .039; odds ratio [OR] = 5.250), the lumbar lesions related to pseudoarthrosis (P 2 = .016; OR = 16.000). The reconstruction extent (number of VMS) was not connected with development of postoperative complications (P 3 = 0.476). Anterior fusion material (bone-graft or titanium mesh cage [TMC] with bone graft) was no impact on postoperative complications (P 4 = .694), but the risk of pseudoarthrosis was higher for bone-graft compared with TMC plus bone-graft (OR = 9.333). The disease etiology, patient’s age, and gender were not related to postoperative complications (P 5 = .697; P 6 = .151; and P 7 = .180). Conclusion: The rate of the late postoperative complications after multilevel spinal reconstructions in pediatric patients with infectious spondylitis was 6.1%. The majority of complications appeared few years after initial surgery, connected with the level of reconstruction and anterior fusion material.
P381: Surgical Correction of Angular Thoracic Kyphosis in Pediatric Patients With Infectious Spondylitis: Original Technique and Comparative Analysis
Alexandr Mushkin1 and Denis Naumov1
1Research institute of Phthisiopulmonology, Saint Peterburg, Russian Federation
Introduction: Posterior vertebral column resection (PVCR) is a modern surgical technique for pediatric angular kyphosis correction. Despite high rate of deformity correction, the negative effects of such procedure are intraoperative blood loss (up to 65% of circulating blood volume [CBV]), operation time (from 6 to 8 hours), and neurological complications rate (up to 30%). According to those facts, the alternative surgical technique could potentially reduce negative outcome. Materials and Methods: Study design—case series. Twenty-one children aged from 8 months till 11 years (M ± m = 2 years 7 months ± 1 year 9 months) were operated between 2011 and 2015 on thoracic angular kyphosis M = 53.7° (minimum = 35°, maximum = 80°) caused by spine infectious – pyogenic (n = 5) or tuberculosis (n = 16). All cases included 2 and more VMS (vertebral motion segments) lesion and ineffective conservative treatment. Three different methods for kyphosis’ correction were used during anterior column reconstruction (ACR) followed by posterior instrumentation (PI): (1) manual reclination with anterior fusion (AF) by bone auto-graft; (2) manual reclination with titanium mesh cage (TMC) plus bone auto-graft for AF; and (3) instrumented anterior interbody reclination with TMC plus bone auto-graft for AF. Average follow-up (FU) period was 3 years 6 months ± 1 year 2 months. The groups were comparable. Evaluated parameters were blood loss, operation time, degree of kyphosis correction, loss of correction, and complications rate. Statistical analysis: SPSS v.22, Kolmogorov-Smirnov test, independent t test, and Mann-Whitney U test. A P value less than .05 was considered statistically significant. Results: The evaluated parameters per groups were (1) operation time: 3 hours + 59 minutes ± 0 + 50 minutes, 3 hours + 35 minutes ± 0 + 25 minutes, 3 hours + 0 minute ± 0 + 25 minutes (P 1 = .021, P 2 = .032); (2) blood loss (mL): 224 ± 42, 162 ± 33, 120 ± 24 (P 3 = .001, P 4 = .038); (3) blood loss (%CBV): 28.7 ± 6.1, 17.1 ± 2.5, 12.3 ± 3.7 (P 5 = .001, P 6 = .026); (4) degrees of kyphosis correction: 19.6 ± 11.7°, 21.1 ± 14.3°, 31.6 ± 8.7° (P 7 = .001, P 8 = .362); and (5) loss of correction: 21.5 ± 31.1°, 3.2 ± 1°, 2.9 ± 0.8° (P 9 = .001, P 10 = .635). There were no complications, connected with vertebral resection or kyphosis correction (manual or instrumented). One case of bone auto-graft resorption was detected 3.5 years after surgery in group 1. Conclusion: The anterior spinal column reconstruction through the anterior approach is safe and effective procedure that reduces blood loss and operation time in pediatric patients with angular kyphosis. The instrumented anterior interbody reclination technique produce better intraoperative correction compared with manual one. The use of TMC with bone graft for AF decrease loss of correction at the FU.
P382: Analysis of a 10-Step Protocol to Decrease Postoperative Spinal Wound Infections
Hossein elgafy1, Craig Raberding1, Joan Duggan1, Megan Mooney1, and Kyle Andrews1
1University of Toledo Medical Center, Toledo, OH, USA
Introduction: This post hoc analysis was conducted to define a 10-step protocol that reduced the incidence of surgical site infection in the spine surgery practice of the senior author and evaluate the support for each step based on current literature. Methods: In response to unexplained increased infection rates at our institution following spine surgery, a 10-step protocol was implemented. (1) Preoperative glycemic management based on hemoglobin A1c (HbA1c), (2) skin site preoperative preparation with 2% chlorhexidine gluconate disposable cloths, (3) limit operating room traffic, (4) cut the number of personnel in the room to the minimum required, (5) absolutely no flash sterilization of equipment, (6) double-gloving with frequent changing of outer gloves, (7) local application of vancomycin powder, (8) re-dosing antibiotic every 4 hours for prolonged procedures and extending postoperative coverage to 72 hours for high-risk patients, (9) irrigation of subcutaneous tissue with diluted povidone-iodine solution after deep fascial closure, and (10) use of DuraPrep skin preparation at the end of a case before skin closure. Through an extensive literature review, the current data available for each of the 10 steps was evaluated. Results: Use of vancomycin powder in surgical wounds, routine irrigation of surgical site, and frequent changing of surgical gloves are strongly supported by the literature. Preoperative skin preparation with chlorhexidine wipes is similarly supported. The majority of current literature supports control of hb A1c preoperatively to reduce risk of infection. Limiting the use of flash sterilization is supported, but has not been evaluated in spine-specific surgery. Limiting operating room (OR) traffic and number of personnel in the OR are supported although without level 1 evidence. Prolonged use of antibiotics postoperatively is not supported by the literature. Intraoperative use of DuraPrep prior to skin closure is not yet explored. Conclusions: The 10-step protocol defined herein has significantly helped in decreasing surgical site infection rate. Several of the steps have already been shown in the literature to have significant effect on infection rates. As several measures are required to prevent infection, instituting a standard protocol for all the described steps appears beneficial.
P383: A Simple Risk Score for Predicting Surgical Site Infections in Patients After Lumbar Spine Fusion
Vadim Byvaltsev1, Vladislav Borisov1, Andrei Kalinin1, Evgenii Belykh1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction. Patients after lumbar spine fusion are often at risk for surgical site infections. We sought to define the predictors of surgical site infections and to develop a risk score for predicting those at risk. Materials and Methods. Patients undergoing a lumbar spine fusion were identified from 3 neurosurgical centers. Univariate and multivariate analyses were conducted to identify predictors of surgical site infections. An integer-based scoring system risk score was created proportional to the logistic regression coefficients, grouping patients into categories of similar risk. Results. We identified 3768 patients and 174 (4.6%) patients developed surgical site infections. Predictors included obesity, diabetes mellitus, wound class, smoking, operative time (minutes), and an ASA (American Society of Anesthesiologists) score >2. A risk score was developed by stratifying patients into low (0-5), medium (6-8), and high (8) risk. Conclusion. Patients after lumbar spine fusion are at risk for surgical site infections. Preoperative factors including obesity, diabetes mellitus, wound class, smoking, operative time (minutes), and an ASA score >2 are strong predictors of surgical site infections. Operative time and wound class are important intraoperative predictors. A risk score, based on pre- and intraoperative variables, can be used to identify patients at risk of developing surgical site infections. This may allow for appropriate process measures to be implemented to prevent and lessen the impact of surgical site infections in high-risk population.
P384: A Novel Classification of Postsurgical Infections After Transforaminal Lumbar Interbody Fusion Surgeries: Guide to Management
Rishi M. Kanna1, Renjith K. R.1, Ajoy P. Shetty1, and Rajasekaran S.1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Postoperative infections after transforaminal lumbar interbody fusions (TLIFs) are unique because it can involve different tissue zones (sub-cutaneous, sub-fascial, peri-implant, osseous, and disc). Infections in each of these zones can occur mutually exclusive of the other zone and are unique in clinical presentation, magnetic resonance imaging (MRI) findings, and treatment plan (implant removal or exchange/cage removal/vacuum closure and antibiotic protocol). Thus, a classification of these infections with specific management protocol would help in optimizing the decision making. Methods: A total of 1279 consecutive adult patients (1520 segments) who underwent open TLIF with an average follow-up of 1 year were analyzed. Sixty-two patients (4.8%) had postoperative wound complications, which were classified anatomically into 5 groups; (1) supra-fascial dehiscence, (2) sub-fascial dehiscence, (3) peri-implant pus, (4) vertebral edema, and (5) disc space infection. Clinical, laboratory and radiological findings, and management details were recorded. Results: Eighty-seven percent patients (54/62) presented in the early postoperative period (<30 days). There were 5 in group 1 (8%), 37 in group 2 (60%), 4 in group 3 (6%), 10 in group 4 (16%), and 6 in group 5 (10%).
Supra-fascial dehiscence: (Group 1) All 5 patients presented with delayed healing, aseptic clinical features at a mean 2.3 weeks, and were managed with debridement and suturing without need for antibiotics or further procedure.
Sub-fascial dehiscence: (Group 2) was the most common presentation and presented as wound gaping with discharge (mean = 10.2 days). All patients required formal debridement while 3 patients required vacuum assisted closure. None of them grew any organism.
Peri-implant pus: (Group 3) presented with severe back pain and fever at a mean 22.7 days, with demonstrable pus around the screw site (MRI and intraoperative finding). Screw revision was done in one patient and the remaining were managed by debridement with implant retention. Tissue culture identified organisms in 9 patients. Antibiotics administered for 6 weeks.
Vertebral edema: (Group 4) all presented as increasing back ache at a mean 36.7 days. MRI showed bone marrow edema without any abscess collection in the sub-fascial or discal zones. Implant exchange was performed followed by antibiotics for 4 weeks.
Disc-space infection: Group 5 had severe back pain and fever, with demonstrable pus in the disc space in postoperative MRI. Three presented at a mean 46.33 days (range = 33-58 days), while 2 at 1.5 years. Early infections were treated by cage removal while later presentations had pan-implant removal.
Conclusion: Management of infections and wound complications after TLIF need an individualized approach. While patients in groups 1 and 2 required only debridement and closure, the increasing complexity of presentation in groups 3 to 5 required implant exchange and prolonged antibiotic therapy. MRI was diagnostic in classifying them into different groups, which guided the management. Our new anatomical classification of surgical site infections helps in grading the severity of infection and provides appropriate treatment guidelines.
P385: Advance of Treatment and Prognosis in Pyogenic Spondylodiscitis: Use of Simultaneous PET-MR Imaging
Ikchan Jeon1, Sang Woo Kim1, and Eun Jung Kong1
1Yeungnam University Hospital, Daegu, Republic of Korea
Introduction: As people are aging, spinal infection also rapidly increasing. Spinal infection requires long-term antibiotics and accompanies several complications during the treatment period. There are still no definite guidelines for the use of antibiotics, and existing hematological and radiological methods are insufficient in the judgment of remission. Recently, simultaneous Fluorine-18 fluorodeoxyglucose positron emission tomography/magnetic resonance (PET/MR) imaging shows great potential as a new option in spinal infection. In this study, we present the application of PET/MR imaging to evaluate treatment response and the clinical usefulness in terms of treatment and prognosis. Material and Methods: Retrospective study. From January 2017 to February 2018, 83 patients (53 male and 30 female, mean ages of 63.67 ± 11.61 years) were enrolled among total 95 patients with pyogenic thoraco-lumbar spondylodiscitis without other cause of infectious condition. Twelve patients were excluded due to death (2), follow-up loss (9), and severe other complication (1). The evaluation of treatment response was performed after at least 3 weeks of parenteral antibiotics. We analyzed clinical characteristics related with PET/MR imaging, parenteral antibiotics period, rate of recurrence, and result of bacterial culture. Results: Bacteremia, epidural abscess, and extent of infection were the statistical significant clinical factors related with longer parenteral antibiotics period (P < .05). There were no definite clinical factors, which can explain recurrence (6%, 5/83). However, application of PET/MR imaging was the independent factor decreasing parenteral antibiotics period over 10 days (40.59 ± 17.33 days vs 51.47 ± 18.44 days, P < .05). The incidence of recurrence in the patients with PET/MR imaging was also low even though there was no statistical difference (2.9% [1/34] vs 8.2% [4/49]). Bacterial culture was confirmed at only 40.9% (34/83), and methicillin-sensitive Staphylococcus species was the most common pathogen (35.3%, 12/34). Conclusion: PET/MR imaging is an independent valuable method to evaluate treatment response, which is not affected by other general conditions. We think decrease of parenteral antibiotics period and lower recurrence rate could be achieved by using PET/MR imaging despite negative bacterial culture, extent of infection, and limitation of existing methods.
P386: Unilateral Sacroiliitis: Differentiating Infective and Inflammatory Etiology by Magnetic Resonance Imaging
Rishi M. Kanna1, Aju Bosco1, Ajoy P. Shetty1, and Rajasekaran S1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Unilateral sacroiliitis is an uncommon disease with varied etiology including infection, inflammation, neoplastic destruction, degeneration, and trauma, with the first 2 causes accounting for most patients. The differentiation between infective and inflammatory causes for unilateral sacroiliitis based on magnetic resonance imaging (MRI) alone is often difficult, portending the need for tissue studies. Furthermore, MRI diagnosis of infective sacroiliitis is also unreliable in the delineation between pyogenic and tubercular etiology, which is essential considering the widely varied treatment regimes. Hence, we studied the efficacy of MRI findings in comparison to tissue culture studies and histopathology as the gold standard tests in the diagnosis of unilateral sacroiliitis. Methods: A retrospective analysis of case records of patients who presented with unilateral sacroiliitis and evaluated with 1.5 Tesla MRI, percutaneous Jamshedi needle biopsy for histopathological examination, tissue cultures and DNA PCR (polymerase chain reaction) (GeneXpert) test, was performed. All patients had underwent clinical examination to confirm unilateral sacroiliitis, MRI, and image intensifier–based needle biopsy. Patients with evidence of bilateral sacroiliitis, degenerative sacroiliitis, trauma, and postpartum sacroiliitis were excluded from the study. Based on MRI findings, the patients were divided into 2 groups—infective (group A) and inflammation (group B). The predictive value of MRI findings in diagnosing the appropriate cause for sacroiliitis was evaluated. Results: Thirty-three patients (mean age = 33.4 ± 17.2 years) had MRI evidence of unilateral sacroilitis. All patients had unilateral gluteal pain (100%), with positive Patrick’s test in 91.9%, fever in 43.2%, and constitutional symptoms in 10.8%. MRI showed features of infective sacroiliitis (group A) in 20/33 (60.6 cases), based on subchondral marrow edema along with widening of joint space and peri-articular abscess. Among these 20 patients, 4 had additional features of tuberculosis in MRI (extensive edema, permeative bony destruction, cavitation, and sequestrum formation). In all, 13 of 33 (39.3%) patients had features of inflammation (group B; minimal to moderate subchondral edema and mild to severe subchondral sclerosis with erosions, maintained joint space, without abscess or permeative/lytic bone destruction, and contralateral asymptomatic minimal edema). Tissue culture and histopathological evidence of infection was positive in 13/20 (65%) patients in group A while it was negative in all group B patients. MRI had 100% sensitivity and 59% specificity in diagnosing infective sacroiliitis while it was 100% specific for diagnosing inflammatory sacroiliitis. In 16 patients diagnosed as pyogenic in MRI, 4 patients (25%) had tissue culture or histopathological evidence of tuberculosis. Discussion and Conclusion: Our study showed that MRI has high sensitivity (71%) and 100% specificity in diagnosing inflammatory sacroiliitis while having low specificity but 100% sensitivity for diagnosing infective sacroiliitis. Hence, patients diagnosed as inflammatory sacroiliitis in MRI may not require further tissue studies. We also noted that MRI had less specificity to differentiate pyogenic from tubercular infections. Hence, percutaneous biopsy and tissue analysis are recommended in patients diagnosed in MRI as infective sacro-iliitis for confirmation and further accurate categorization.
P387: Risk Factors for Deep Postoperative Infections Following Transforaminal Lumbar Interbody Fusion
Rishi M. Kanna1, Renjith K. R.1, and Rajasekaran S1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Postoperative spinal wound infections complicating transforaminal lumbar interbody fusions (TLIF) are unique because it can involve multiple tissue planes (suprafascial, submuscular, peri-implant, osseous, and disc space), which need different treatment approaches. The presence of spinal implant and the interbody cage makes treatment more complicated. Recognition of a patient’s preoperative risk factors may allow for strict vigilance and specific interventions, thus reducing the incidence of postsurgical infections. We evaluated the incidence and risk factors for surgical site infections following TLIF in a large consecutive cohort. Material and Methods: The case records of 1279 consecutive patients (n = 1520 levels) who underwent posterior instrumented open TLIF for degenerative or dysplastic conditions between January 2014 and June 2017 was performed. Patients operated for trauma, tumor, or infection were excluded. The electronic medical record was reviewed for patient demographic data, medical comorbidities, primary diagnosis, and operative variables. Infection rates were calculated and multivariate logistic regression analysis was used to determine the effect of various preoperative variables on postoperative infection. Results: The mean age was 54 years (range = 19-65 years), including 879 females and 400 males. The mean follow-up period was 14.3 ± 3.6 months. There were 1179 primary surgeries and 110 revision cases. Postoperative infections were reported in 62 patients (4.8%), which included 42 superficial (67.7%) and 20 deep (32.3%) according to CDC (Centers for Disease Control and Prevention) classification. Eighty-seven percent patients presented in the early postoperative period. Tissue culture isolated organisms in 13 patients (21%), with Staphylococcus aureus being the most common. Multivariate logistic regression identified age >50 years (P < .05, odds ratio [OR] = 4.5), diabetes mellitus (OR = 1.45), BMI (body mass index) >25 kg/m2, multilevel fusions (OR = 1.51), and revision surgeries (OR = .72) were found to have significant association with postoperative infections. Duration of surgery, blood loss, transfusion requirements, use of wound drains, dural tear, and level of surgery were not significantly associated. Conclusion: The incidence of infections in open TLIF surgeries was 4.8% and several risk factors including age >50 years, diabetes mellitus, obesity, revision surgeries, and multilevel fusions had significant association with postoperative infections. Patient counselling and stringent perioperative protocols may need to be excised in such patients to reduce the incidence.
P388: Loss of Kyphotic Deformity After 3- and 5-Year Follow-up in Caries Spine Patients Who Underwent Anterior Decompression and Locally Made Cage With Autologous Bone Graft
Ammar Dogar1, Haseeb Hussain1, Amer Aziz1, Shahzad Javed1, and Rizwan Akram1
1Ghurki Trust Teaching Hospital, Lahore, Pakistan
Background: Spinal deformity and paraplegia/quadriplegia are the most common complications of tuberculosis (TB) of spine. TB of dorsal spine almost always produces kyphosis while cervical and lumbar spine shows reversal of lordosis to begin with followed by kyphosis. Kyphosis continues to increase in adults when patients are treated nonoperatively or by surgical decompression. In children, kyphosis continues to increase even after healing of the tubercular disease. Surgical procedure for these pathologies can be performed through both anterior and posterior approaches but anterior approach has the advantage of better canal clearance and better chances of graft fusion and deformity correction than posterior approach. Objective: The main objective of this study is to find out the immediate kyphosis correction and loss in correction after 3- and 5-year follow-up. Materials and Methodology: A prospective study was conducted in the Department of Orthopaedics and Spine of Ghurki Trust Teaching Hospital, Lahore, from 2003 to 2016. A total of 1049 patients were totally operated during this interval.Out of which 513 patients were operated 5 years back and they were considered in the study. All patients underwent anterior decompression and placement of inter body titanium mesh cage with packed bone graft. Pre- and postoperative lateral view X-rays were taken to check and record the postoperative change in kyphotic angle at immediate postoperative period, after 3 years and after 5 years. Boston brace was applied for at least 6 months. Data was analyzed using SPSS 17.0. Results: There were 513 patients in which 301 (58.67%) males and 212 (41.32%) females. The patients aged between 15 and 30 years were 232 (45.22%), those aged between 31 and 45 years were 115 (21.83%), and between 46 and 60 years there were 166 (32.36%). The mean local kyphosis correction in the immediate postoperative period was 23.1 ± 2.1°. The mean late loss of correction of local kyphosis at 3 years follow-up was 1.7 ± 0.7° and almost similar findings after 5 years follow-up. Conclusion: Anterior decompression along with titanium mesh cage and bone graft in patients suffering from caries spine showed immediate postoperative improvement in kyphotic angle.There is no significant loss of kyphotic angle even after 3- and 5-year follow-up. It is safe and cheap procedure as compared with other instrumentation especially for the poor patients of developing countries.
P389: Body Mass Index and the Risk of Deep Surgical Site Infection Following Posterior Cervical Instrumented Fusion
Christina Cheng1, Amy Cizik2, Armagan Dagal2, Larissa Lewis2, John Lynch2, Carlo Bellabarba2, Richard Bransford2, and Haitao Zhou2
1University Hospitals Cleveland Medical Center, Cleveland, OH, USA
2Harborview Medical Center, Seattle, WA, USA
Introduction: Surgical site infection (SSI) following spine surgery is associated with increased morbidity, reoperation rates, hospital readmissions, and cost. The incidence of SSI following posterior cervical spine surgery is higher than anterior cervical spine surgery, with rates from 4.5% to 18%. It is well documented that increase body mass index (BMI) is associated with increased risk of SSI after spine surgery. There are only a few studies that examine the correlation of BMI and SSI after posterior cervical instrumented fusion (PCIF) using national databases; however, none that compare trauma and non-traumatic patients. The purpose of this study is to determine the odds of developing SSI with increasing BMI after PCIF and to determine the risk of SSI in both trauma and nontraumatic adult patients. Material and Methods: This is a retrospective cohort study using a prospectively collected database of all spine surgeries performed at one academic institution from April 2011 to October 2017. We identified 1406 patients who underwent PCIF for both traumatic injuries and nontraumatic pathologies using International Classification of Diseases 9 and 10 procedural codes. Thirty-day readmission data were obtained. Patient’s demographics, BMI, presence of diabetes, preoperative diagnosis, and surgical procedures performed were identified. Using logistic regression analysis, the risk of SSI associated with every 1-unit increase in BMI was determined. Results: Of the 1406 patients identified, 1143 met our inclusion criteria. Of those patients, 688 had PCIF for traumatic injuries and 454 for nontraumatic pathologies. The incidence of SSI for all patients who underwent PCIF was 3.9%. There was no significant difference in the rate of SSI between our trauma group and nontraumatic group. There was a higher rate of infection in patients who were diabetic and with BMI ≥ 30 kg/m2. The presence of both diabetes and BMI ≥ 30 kg/m2 had an added effect on the risk of developing SSI in all patients who underwent PCIF. Additionally, logistic regression analysis showed that there was a positive difference measure between BMI and SSI. Our results demonstrate that for 1-unit increase in BMI, the odds of having a SSI is 1.048 (95% CI [confidence interval] = 1.007-1.092, P = .023). Conclusion: Our study demonstrates that our rate of SSI after PCIF is within the range of what is cited in the literature. Interestingly, we did not see a statistically significant difference in the rate of infection between our trauma and nontrauma group. Overall, diabetes and elevated BMI is associated with increased risk of SSI in all patients who underwent PCIF with even a higher risk in patient who are both diabetic and obese. Obese patients should be counseled on elevated SSI risk after PCIF and those with diabetes should be medically optimized prior to and after surgery when possible to minimize SSI.
P390: Costotransverse Joint: A Rare Localization for Tubercular Arthritis
Aashish Ghodke1, Ram Chaddha2, Agnivesh Tikoo2, Harshal Bamb1, and Sagar Kelkar1
1Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, Shropshire, UK
2Apollo Hospitals, Navi Mumbai, Maharashtra, India
Introduction: Tubercular arthropathy can affect any joint but the most common form of articular tuberculosis is spondylitis followed by arthtritis of weightbearing joints especially hip and knee. Other frequently reported joints are ankle, sacroiliac, sternoclavicular joint, shoulder, elbow, and wrist. To the best of our knowledge, tuberculosis of the costotransverse joint has only been reported twice in literature. Materials and Methods: A 18-year-old girl who presented with 3 months history of left sided dorsal spinal pain. No constitutional symptoms. Past history or family history not suggestive of TB (tuberculosis). On physical examination, There was no deformity, but only mild tenderness elicited over the transverse process. There was no neurological deficit. MRI (magnetic resonance imaging) was suggestive of enhancing perarticular erosive lesions and marrow oedema in the medial portion of the seventh rib and left posterolateral portion of the vertebral body and lateral portion of the left seventh pedicle with thickening and enhancement of the synovium of the seventh costotransverse joint with enhancing soft tissue elevating the overlying pleura and abutting the descending aorta. CT (computed tomography)-guided biopsy on cytology showed caseous necrosis with epitheloid and langerhans giant cells suggestive of tuberculosis. Results: Patient was treated with anti-tubercular drugs. At 1-year follow-up, patient showed clinical as well as radiological improvement. Conclusion: Tubercular arthritis of the costotransverse joint is extremely rare and can occur as an isolated lesion in the absence of disease elsewhere. Diagnosis of such cases can be prolonged unless a strong suspicion is kept and appropriate diagnostic studies are obtained as early as possible to avoid neurological complications.
P391: Which Parameters Other Than and in Addition to Neurological Status are Relevant on Surgical Decision-Making in Spinal Tuberculosis?
Prashant Adhikari1, Selcen Yuksel2, Selim Ayhan3, Bigyan Bhandari1, Binod Bijukachhe4, and Emre Acaroglu5
1Hospital for Advanced Medicine and Surgery, Kathmandu, Nepal
2Yildirim Beyazit University, Ankara, Turkey
3Acibadem Mehmet Ali Aydinlar University, Istanbul, Turkey
4Grande International Hospital, Kathmandu, Nepal
5Ankara Spine Center, Ankara, Turkey
Introduction: Patients treated for spinal tuberculosis (TB) with chemotherapy alone may have an average increase of 15° in deformity and 3% to 5% of these develop kyphosis greater than 60°. Surgery has been advocated as the standard treatment in these patients, as well as in those with neurological loss. The aim of this study is to analyze the impact of the parameters other than neurological status of the patients on surgical decision-making in spinal TB. Material and Methods: A retrospective analysis of a single-center case series was performed, and a total of 99 patients with spinal TB, managed surgically (S) or nonsurgically (NS) between 2006 and 2016, were analyzed. This patient series was not started for any research purposes and reflects the treatment preferences of the treating physician as well as the patients. Neurological status was set as dependent variable while the visual analogue scale (VAS) score, contiguity of the disease, and sagittal plane deformity were set as independent variables. A stepwise multivariate logistic regression method was used to evaluate the impact of clinical variables on S group. Results: Of the 99 patients (60 female/39 male) with a median age of 27 years; 83 (83.8%) were treated surgically and 16 (16.2%) were managed nonsurgically. The median values for VAS score, number of vertebral involvement, erythrocyte sedimentation rate (ESR), and preoperative kyphotic angles were 9, 2, 56, and 30, respectively. Multivariate logistic regression test results showed that the probability of having a surgical intervention increases by 8.036 and 5.249 times for the patients with deformity and with contiguous disease, respectively (P < .05). Moreover, 1-unit increment on VAS score increases the probability of having a spinal surgery by 1.371 times, as well (P < .05). Conclusion: TB of the spine may result in sagittal plane deformity and most of the patients are suffering from significant amount of back pain because of the disease. In this study based on pure surgeon and patient preferences, the presence of kyphotic deformity, contiguity of the lesion, and pain intensity (in addition to neurology) were shown to be relevant factors while making the decision for a surgical intervention.
P392: Recent Increase in the Rate of Spinal Infections May Be Related to Growing Substance Use Disorder in the State of Washington: Wide Population-Based Analysis of the Comprehensive Hospital Abstract Reporting System Database
Ronan Blecher1, Basem Ishak1, Emre Yilmaz1, Rod Oskouian1, and Jens Chapman1
1Swedish Neuroscience Institute, Seattle, WA, USA
Introduction: Spinal infections (SI) pose major diagnostic and therapeutic challenge in developed countries, resulting in substantial morbidity and mortality. With an estimated incidence of up to 1:20 000, recent clinical experiences suggest that this rate may be rising. The goal of this epidemiological study was to evaluate trends in the incidence of SI and the possible role of substance use disorder as a key associated factor. Material and Methods: To evaluate a possible change in trend in the proportion of SI, we searched the Washington State CHARS (Comprehensive Hospital Abstract Reporting System) data over a period of 15 years. We retrieved ICD-9 and -10 codes (International Classification of Diseases, Ninth and Tenth Revision), searching for all conditions that are regarded as SI (discitis, osteomyelitis, and intraspinal abscess), as well as major known SI-related risk factors. Results: We found that the proportion of SI among discharged patients had increased by more than 60% during the past 6 years, starting at 2012 and increasing steadily thereafter. Analysis of SI-related risk factors within the group of SI revealed that proportion of substance use disorder and malnutrition had undergone the most substantial change, with the former increasing more than 3-fold during the same period. Conclusion: Growing rates of drug abuse, drug dependence, and malnutrition throughout the State of Washington may trigger a substantial increase in the incidence of SI in discharged patients. These findings may provide important insights in planning prevention strategies on a broader level.
P393: Safety and Efficacy of Silver Alloy–Coated Urinary Catheters in Patients With Acute Traumatic Cervical Spinal Cord Injury
Hanbing Zhou1, John Street2, Leanna Ritchie2, Lise Belanger2, and Nikolas Wong2
1Orthopedic Associates of Hartford, Hartford Hospital, Hartford, CT, USA
2Vancouver General Hospital, Vancouver, British Columbia, Canada
Introduction: Patients with acute traumatic cervical spinal cord injury (ATCSCI) have an increased risk of catheter associated urinary tract infection (CAUTI). The safety and efficacy of antiseptic silver alloy–coated silicone urinary catheters (SACC) in CSCI is unknown. This study examined the safety and efficacy of SACC for preventing CAUTI in patients with ATCSCI. Material and Methods: A longitudinal observational study examining all CAUTI incidents in all patients undergoing spine surgery at a single quaternary center from January 2014 to December 2016 inclusive. Prior to July 2015, all patients received a latex indwelling catheter (LIC). After July 2015, SACC was used in all patients with ATCSCI only. Duration of catheterization, microbiology, duration of infection, antibiotic susceptibility, and catheter associated adverse events were recorded prospectively, as was the occurrence of other non-catheter adverse events and length of stay. The safety and efficacy of SACC versus LIC is reported. Results: A total of 3081 patients were studied of whom 302 (9.8%) were ATCSCI. Sixty-three percent of ATCSCI patients were AIS (American Spinal Injury Association Impairment Scale) A or B. The overall rate of CAUTI was 19% (585 of 3081), with 38% (116 of 302) in patients with ATCSCI. Of 178 ATCSCI patients with LIC, 100 (56%) developed a CAUTI compared with of 28 of 124 (23%) with SACC (P < .05). The median time of urethral catheterization was 27 days in the SACC group and 28 days in the LIC group (P = .602). Polymicrobial and gram positive infection was more common in LIC than in SACC groups (P < .05). The median duration of infection was 9 days in the SACC group and 12 days in the LIC group (P = .08). Resistance to trimethoprim (P < .001) and to ciprofloxacin (P < .05) were more common in LIC group. There was no difference in catheter associated adverse events or length of stay between the groups. Conclusion: This study illustrates the safety and efficacy of antiseptic SACC in acute traumatic cervical spinal cord injured patients. The use of SACC reduces the incidence and duration of CAUTI and the incidence of antibiotic resistance. This study provides the preliminary data for a prospective randomized controlled trial in patients with neurogenic bladder.
P394: Spine Surgery Infection: Who Is at Risk?
Hanbing Zhou1 and John Street2
1Orthopedic Associates of Hartford, Hartford Hospital, Hartford, CT, USA
2 Vancouver General Hospital, Vancouver, British Columbia, Canada
Objectives: Surgical site infections (SSI) remain a common problem among surgically treated patients with associated increased rates of morbidity and mortality, hospital LOS (length of stay), and cost. The rate of SSI reported can range from 0.2% to 16.7%, depending on the type of procedures. Numerous studies have attempted to identify the specific risk factors associated with SSI but are often limited to one specific diagnosis or procedure. The purpose of this study is to perform a systematic review of SSI risk factors and more specifically, categorize them into patient, surgical, and disease-related factors. Methods: Systematic review of published literature on SSI risk factors in adult spine surgery was performed. We included studies that reported risk factors for SSI in adult spinal surgery. Excluded are pediatric patient populations, systematic reviews, and meta-analyses. Overall, we identified 71 cohort studies, 1 controlled-cohort study, 1 matched-cohort study, 1 matched-paired cohort study, 12 case-controlled studies (CCS), 6 case series, and 1 cross-sectional study. Results: Patient-associated risk factors: DM (diabetes mellitus; level II), obesity (BMI [body mass index] >35 kg/m2), age, subcutaneous fat thickness, chronic steroid, ASA (American Society of Anesthesiologists) >3, immunosuppression, chronic renal disease, Parkinson’s, current smoker, and socioeconomic status (level III) were associated with SSI. Disease associated risk factors: traumatic injury, deformities, tumors (no difference in primary vs metastatic), preoperative radiation, and revision surgery (level III) were associated with SSI. Surgical associated factors: prolong OR time (level II), ICU (intensive care unit) stay, delay in surgery (trauma), combined anterior/posterior approach, open surgery (vs MIS [minimally invasive surgery]), surgical invasiveness, or levels of instrumentation, lumbosacral junction, number of surgeons, and less surgeon experience (level III) were associated with increased SSI. Furthermore, early tracheostomy, gender, and NSAIDs (nonsteroidal anti-inflammatory drugs; level III) were not associated with SSI. Conclusions: SSIs are associated with many risk factors that can be patient or surgically related. Our review was able to identify important modifiable and nonmodifiable risk factors that can be essential in surgical planning and discussion with patients.
P395: Treatment of Aeromonas hydrophila Infection After Spinal Surgery: A Report of 9 Rare Cases
Yu Jiang1, Weishi Li1, Zhaoqing Guo1, Qiang Qi1, Yan Zeng1, Chuiguo Sun1, Woquan Zhong1, and Zhongqiang Chen1
1Peking University Third Hospital, Beijing, China
Introduction: Aeromonas hydrophila infection is relatively rare in spinal surgery incisions. A hydrophila is a heterotrophic, Gram-negative, rod-shaped bacterium mainly found in areas with a warm climate. A hydrophila was isolated from humans and animals in the 1950s. It can survive in aerobic and anaerobic environments, and can digest materials such as gelatin and hemoglobin. The treatment process of 9 cases with infection of Aeromonas. Material and Methods: From December 2012 to June 2017, 9 cases of A hydrophila infection after spinal surgeries were treated, including 4 males and 5 females. Seven cases received posterior lumbar interbody fusion surgeries, 1 case with adolescent idiopathic scoliosis received spinal corrective surgery, and 1 case with thoracic tumor received posterior decompression surgery. The average age is 54 years. Nine cases of drainage fluid bacterial culture or blood bacterial culture were found A hydrophila. According to the results of laboratory drug sensitivity, we adjusted the types and consumption of intravenous and oral antibiotics. Six cases that we found large amounts of pus in deep incision on MRI (magnetic resonance imaging) received complete debridement. We put the opposing direction of the drainage tubes to flush the spinal surgical incision. We monitored the body temperature, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), procalcitonin (PCT), and blood routine test to assess the treatment of infection. It depends on the results of 3 consecutive days of drainage fluid culture; we decide whether to pull out the flushing tube and drainage tube. Two cases were treated with intravenous and oral sensitive antibiotics, and surgical incision infection was treated without debridement. Results: Nine cases recovered when they received suitable treatment, the body temperature, ESR, CRP, PCT, and blood routine test were normal. Follow-up duration last from 2 to 53 months, an average of 10 months. No infection recurred during final follow-up. Nine cases of wound drainage fluid were cultured A hydrophila. Four cases of blood culture were found A hydrophila. Fever started from the third day to the 12th day after surgery, the average starting time is 5.2 days. The highest body temperature was from 37.9°C to 39.9°C, an average of 39.0°C. The duration of using intravenous antibiotics was from 15 to 82 days, an average of 31.8 days. All cases were found that the most sensitive antibiotic to A hydrophila was ertapenem. Six cases who received debridement reserved the internal fixation. Conclusion: Aeromonas hydrophila infection is relatively rare in spinal surgery incisions. A hydrophila infection of spinal surgery incision results in the rapid onset of hyperthermia (6/9), the higher incidence of bacteremia (4/9). Blood and drainage culture positive rate of A hydrophila is high, and early detection helps use exact intravenous antibiotic therapy. Reasonable use of antibiotic, combined with complete debridement and opposing catheter drainage, can realize effective treatment of A hydrophila infection after spinal surgery.
P396: Tapping Into the Atypical Thread of Centrifugal Tuberculous Vertebral Body Osteomyelitic Compression Fracture Within the Realm of the Ancient Disease
Wendy Lee1, Ying Chyi Chong2, Tiam Siong Tan1, and Chung Chek Wong2
1Sibu Hospital, Sarawak, Malaysia
2Sarawak General Hospital, Kuching, Malaysia
Introduction: Tuberculous spondylitis typically renders characteristic anterior-superior or inferior initiative focus with subligamentous spread to adjacent vertebrae, leading to a relative secondary narrowing of intervertebral disc space as the disc progresses to herniate into the diseased subchondral end-plates. The herniated disc as appeared spared in the earlier phase on magnetic resonance imaging (MRI) induces a “fluffy-void” within the inner nucleus pulposus, being thus analogous to “waffle-like” consistency from the ballooned disc dimension. Less encountered are cases with atypical radiological manifestation taxing diagnosis, namely, isolated neural arch involvement, and panvertebral body destruction with compression fracture. We ventured out to garner features of commonality and pathological aetiology in this latter atypical group. Material and Methods: First, we illustrate a frail 73-year-old female presented with L5 vertebral osteoporotic fracture, preceded by 1-month mechanical instability low back pain and S1 radiculopathy with bilateral L5 and S1 myotomal weakness confining her to bed. Prior trauma was not elicited nor was she immunocompromised. Radiograph exhibited global osteopenia, L5 collapse, and increased L4-L5, L5-S1 disc spaces. MRI demonstrated centrifugal cephalad two third L5 body signal changes (hypointense-T1W, hyperintense-T2W-STIR, hypointense Gad-T1W) breaching anterior-posterior cortices. Second is a 74-year-old immunocompetent male presented in semi-paraplegic state heralded by 7 months of resting, nocturnally accentuated back pain with recurrent falls. The centrifugal panvertebral T3 body collapse—signal changes of which had extended beyond subligamentous plane to involve adjacent vertebra without structural changes, along with heightened T2-T3, T3-4 disc spaces. Results: Percutaneous pedicle screws stabilization was elected for the first patient. Jamshidi trochar advancement into L5 pathological pedicle unanticipatedly drained 40 mL of disgorging pus containing fragmented spicules. A redivac drain enveloped over the guide wire in a retrograde fashion was left in place. Second-stage anterior iliac crest tricortical grafting over the deficient column ensued. Transpedicular anterior debridement and curettage during posterior instrumented surgery for the second patient yielded 10 mL of pus material similar to that of the former case. Acid-fast bacilli stained positive for the first patient. Gene Xpert assay detected Mycobacterium tuberculosis in both patients. Conclusion: Spinal tuberculosis in more developed regions have observed increasing predilection in the elderly population. Both arterial and venous routes of dissemination following a delayed hypersensitivity immune reaction have been conceded. Seeding of granulomatous pre-pus inflammatory reaction with Langerhans’ giant cell, epitheliod cells, and lymphocytes aggregate at vertebral metaphyseal zone, which in adult consists of end-arteries in its horizontal plane—as intraosseous arterial anastomosis involute during adolescence. Granulomatous tissues further proliferate and thrombose these end arteries, resulting in retrograde extravasation and subligamentous spread, engendering typical features involving adjacent vertebrae. Microarteriography in the elderly, however, demonstrated secondary periosteal arteries proliferation and resurgence of metaphyseal-intraosseous anastomosis. This, coupled with vertebral body venous stasis and increased hyperaemia in the osteopenic spine propagate centrifugal destruction of bony trabeculae, and panvertebral body collapse with ongoing axial loading. Vertebral microcirculation and osteopenic attributes distinctive to this population render atypical imaging features, muddling preliminary disease consideration. Tuberculous vertebral osteomyelitis should be borne in mind as differential in the elderly population presented with vertebral osteoporotic fractures notwithstanding the often times distracting comorbidies.
P397: Long-Term Clinical and Radiological Outcome of Conservative and Surgical Treatment in Tuberculosis of Pediatric Spine in North Indian Subcontinent
Mukesh Haritwal1, Shankar Acharya1, Nikhil Jain1, Rupinder Chahal1, and K. L. Kalra1
1 Sir Ganga Ram Hospital New Delhi, India
Introduction: Spine tuberculosis in children results in permanent deformity and disability. Both conservative and surgical methods are effective for treatment. However, kyphosis may progress after both types of treatment methods. The purpose of this study was to evaluate clinical and radiological outcome of both type of treatment methods of spine tuberculosis in children treated at our institute. Materials and Methods: We retrospectively reviewed the prospectively collected data of children treated at our institute from year 2006 to June 2015. The main inclusion criteria were; age <18 years, clinic-radiological or tissue diagnosis of spine tuberculosis, and minimum follow-up of 18 months. Thirty-three patients (19 boys, 14 girls) satisfied the inclusion criteria. Twelve patients (mean age 11.75 ± 4.78 years) received ambulatory chemotherapy and 21 patients (mean age 11.66 ± 3.89 years) received surgical treatment. Average duration of presentation was 5.35 months. At the time of presentation, 48.5% had neurodeficit, 9% bowel and bladder involvement, and 36% deformity. According to regions of spine, 6% (n = 2) had cranio-vertebral junction (CVJ), 6% (n = 2) sub axial cervical spine, 6% (n = 2) cervico-thoracic junction, 54.5% (n = 18) thoracic spine, 24% (n = 8) thoraco-lumbar junction, and 6% (n= 2) lumbar spine disease. On MRI (magnetic resonance imaging), skip lesions were detected in 18% (n = 6) of the cases. Most common lesions were paradiscal and central accounting for 60% (n = 20) and 33% (n = 11) of the cases, respectively. Average numbers of involved vertebrae were 2.3. Average destruction of the vertebral bodies was 1.18. Average duration of chemotherapy was 13.93 months. Two patients were diagnosed as MDR-TB (multidrug-resistant tuberculosis) during the course of the treatment. Surgical approach was posterior in 16 cases, anterior in 2, combined anterior and posterior in 2, and combined anterolateral and posterior in 1 case. Instrumented fusion was performed in all cases. Decompression was performed in 18 cases and all patients were augmented with anterior bone graft. Average duration of follow-up was 28 months (range = 18-115 months). Results: Majority of children presented with complication of spine tuberculosis due to delayed presentation or diagnosis. All children attained healed status at an average of 14 months (range = 12 to 30 months). Except one MDR-TB child (who remained AIS-C [American Spinal Injury Association Impairment Scale, Class C]), all improved to normal neurology (AIS-E). Pain (VAS [visual analogue scale]) was improved rapidly in surgical group as compared with conservative group. In operative group, kyphosis was corrected significantly from mean 40.35 ± 30.7° preoperative to 20.25 ± 25° postoperative. At final follow-up, it remained static in 18 children and increased in 2 patients. Conservative group showed increase in kyphosis from mean 37 ± 18.7° pretreatment to 41.7 ± 16.4° at the final follow-up. Fusion was attained in all children. Out of the 2 MDR-TB children, one underwent 2 revision surgeries and another developed implant exposure at 2 years of follow-up. None of the children developed complications of chemotherapy. Four main indications for surgery were identified; neurodeficit (n = 10), instability (n = 8), deformity (n = 9), and neurological worsening on chemotherapy (n = 6). Conclusion: Emphasis should be on early diagnosis and early institution of chemotherapy to prevent complications of spine tuberculosis. Children presenting without neurodeficit, instability, and deformity can be treated conservatively with acceptable clinical and radiological outcome.
P398: Risk Factors for Surgical Site Infection Following Posterior Thoracolumbar Spinal Surgery with Drain Placement
Jennifer Urquhart1, Parham Rasoulinejad1, Lori Nutt1, Alyssa Fleming1, Linda Kuska1, Kevin Gurr1, Fawaz Siddiqi1, and Christopher Bailey1
1Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Ontario, Canada
2Lawson Health Research Institute, and London Health Sciences Center, London, Ontario, Canada
Introduction: Posterior thoracolumbar surgery with instrumentation followed by placement of a closed-suction drain is associated with a relatively high surgical site infection (SSI) ≥12%. Identifying risk factors for SSI is an important strategy for preventative strategies to reduce the associated morbidities and costs. The purpose of this study was to identify risk factors for SSI after spinal surgery in a homogeneous cohort. This study is an ambispective cohort study and was performed at a single tertiary spine center. Material and Methods: A retrospective analysis was performed on data that was prospectively collected in a prior randomized controlled trial of 552 patients who were randomized to either antibiotic for 24 hours or antibiotic for 72 hours (to ensure 24 hours of postoperative antibiotics post-drain removal, as drains were discontinued by postoperative day 2). For the current study, univariate analysis was performed to investigate the relationship between patient-related and procedure-specific risk factors for developing a SSI. Continuous variables were dichotomized. Clinically important and statistically important variables were included in a stepwise multiple logistic regression model to determine the best combination of predictors of postoperative SSI. Model performance was assessed by receiver operator characteristics (ROC) and area under the curve (AUC). The regression coefficients obtained from the multivariate model were used to estimate the probability of a SSI. Results: There were a total of 80 infections out of 552 procedures (14.5%). Of the total infections, 31 were deep and 49 were superficial infections. On univariate analysis, significant patient risk factors included ASA (American Society of Anesthesiologists) score ≥3, body mass index (BMI) ≥30 kg/m2, prophylactic preoperative vancomycin, duration of surgery ≥280 minutes, preoperative SF12 mental component summary (MCS) score ≤35, blood loss ≥600 mL, and revision procedure. Nonsignificant factors of clinical relevance were diabetes, number of surgical assistants, scrub events, and season. In the stepwise regression model, the odds of a SSI were greater when a patient had a BMI ≥ 30 kg/m2 (odds ratio [OR[ = 2.34, P = .006), prophylactic preoperative vancomycin (OR = 3.00, P = .020), prolonged surgery (OR = 1.96, P = .033), worse preoperative mental functioning (1.87, P = .055), blood loss >600 mL (2.32, P = .048) and a revision procedure (1.86, P = .077). The AUC for the final model was 0.723 ± 0.037, indicating acceptable predictive discrimination. Using the regression coefficients from the final logistic model the odds of developing a SSI decreased by 22% for patients that had preoperative prophylactic cefazolin, decreased by 16% for patients that had a BMI < 30 kg/m2, decreased by 12% for patients that shorter duration surgery < 280 minutes, decreased by 16% for patients who had blood loss < 600 mL, decreased by 11% for patients who had MCS >35 at the preoperative assessment, and decreased by 11% for patients undergoing primary surgery. Conclusion: In this study cohort, obesity, antibiotic type, prolonged surgery, blood loss, revision procedure, and preoperative mental functioning were modifiable risk factors for SSI. This study provides insight into risk at the population level. Development of a preoperative risk calculator that informs risk at the individual level is warranted.
P399: The Role of One-Stage Exchange of Spinal Implants After Implant-Associated Deep Surgical Site Infections
Hans-Heinrich Trouillier1
1Kantonsspital Baselland, Liestal, Switzerland
Introduction: A special algorithm in prevention and therapy was developed and standardized for the increasing number of deep wound infections after instrumented stabilization of the spine. Most of these elder patients with American Society of Anesthesiologists (ASA) classification grade 3 have a special difficult therapeutic situation. Implant-associated infections in spine surgery peak in the first 3 postoperative months. This is different to periprosthetic joint infections after hip and knee surgery. Beside the need for a special algorithm in preoperative preparation of the patient, postoperative diagnostics including sonication of implants we performed a consequent one-stage exchange of the spine instrumentation. Material and Methods: In a prospective, observational 2-center study, patients with implant-associated deep wound infections were included. All patients had a grade III in the ASA physical status classification system. The revision surgery, as one part of the whole therapy concept, was a consequent one-stage exchange of the complete spinal instrumentation. This allows in every case the use of the diagnostic tool of sonication, biopsies supra- and subfascial, and biopsies from the implant site. Results: The one-stage exchange of spinal implants lead to a significant reduction of second look operations. Sixty-eight patients needed surgical revision. Only in one case a second look surgery was necessary. The use of sonication improved the isolation of the right bacteria spectrum in its sensitivity from 60% up to 79% without deterioration of specificity. This reduced significantly duration of hospitalization and the need of intravenous antibiosis. The calming of the inflammatory values is in general much earlier with the possibility of oralization of antibiosis. Conclusion: Independent of the age of the patient, the number of repeated surgical interventions must be minimized, especially in spine surgery with the risk of chronic pain problems like postlaminectomy syndrome is it compellingly necessary. The one-stage exchange of spinal implants is a costly procedure, but a profit for the affected patient.
P400: A Comparison of the Antibacterial Effect of Titanium and Cobalt-Chromium Alloys In Vitro and In Vivo
Kota Watanabe1, Satoshi Fukuzaki2, Atsushi Sugino3, Newton Metcalf1, and Nicholas Benson1
1Keio University, Tokyo, Japan
2Graduate School of Bioresources, Mie University, Tsu, Japan
3Medtronic, Tokyo, Japan
Introduction: Cobalt-chromium alloy (CC) and titanium alloy (Ti) have high corrosion resistance, wear resistance, and fatigue strength. These properties cause them to be used widely for orthopedic implants. Previous studies have looked at the biofilm formation of dental implants and the antibacterial agents of cobalt ions; however, there has not been a study to evaluate the bacterial proliferation difference between common spine implant materials. Material and Methods: The antibacterial effect of CC and Ti were evaluated using cultured mediums and animals. In the in vitro study, pedicle screw heads were soaked in nutrient broth with one of the following bacteria: Methicillin-resistant Staphylococcus aureus (MRSA, IID 1677), MRSE (methicillin-resistant S epidermidis; GTC 13320), S aureus (NBRC 12732), S epidermidis (NBRC 12993), Escherichia coli (NBRC 3972), and Pseudomonas aeruginosa (NBRC 13275). After a 24-hour incubation, the nutrient broth including the bacteria was collected with gentle washing and transferred to nutrient agar plates, and the colony-formation units (CFU) were counted as viable cells. The in vivo study used discs made of CC or Ti that were implanted into subcutaneous layer of BALB/c mice. After skin closure, a 0.05 mL of S aureus suspension (1 × 106 CFU) was directly inoculated on the implanted discs. The mice were sacrificed by excessive anesthesia 12, 24, or 72 hours later. The discs were then removed from the implanted site and the viable cells were counted. A Wilcoxon signed-rank test with a 1% significance threshold was used to determine statistical differences between CC and Ti. Results: The mean number of viable S aureus cultured with CC and Ti screw heads were 3.2 × 102 CFU/mL and 2.3 × 106 CFU/mL, respectively. There was a lower mean number of MRSA cultured with CC screw (6.1 × 102 CFU/mL) as compared with the Ti screw (2.5 × 106 CFU/mL). Similar reductions were obtained for the other bacteria. In the in vivo model, the number of viable S aureus on Ti discs increased for each implantation period while it decreased on CC discs. Significant differences in the mean number of viable S aureus between CC and Ti were observed at all time points (P < .01). Conclusion: These data demonstrate that CC suppressed bacteria proliferation compared with Ti in both in vitro and in vivo studies. Robust clinical studies will be needed to draw clinical conclusions.
P401: Lumbar Spondylolisthesis Associated With Infection
Mohamed Abdel-Wanis1
1Sohag University, Sohag, Egypt
Introduction: A few reports are available in the literature of discitis with spondylolisthesis. The aim of this article is to report 6 patients in whom both lumbar spondylolisthesis and infection coexist at the same level. Materials and Methods: The patients were 4 males and 2 females with a mean age of 56.8 (range = 38-72) years. Levels affected by spondylolisthesis were L2-3 in 1 patient, L4-5 in 3 patients, and L5-S1 in 2 patients. In 2 patients, infection extended to an adjacent level to the lythetic one. Two patients had neurological impairment (Frankel grade D). Five patients received posterior lumbar interbody fusion (PLIF). One patient was treated by laminectomy, evacuation of the epidural abscess, and instrumented posterolateral fusion. Postoperative functional outcome was graded based on the criteria of Kirkaldy-Willis et al. Results: Causative organisms were TB (tuberculosis) in 3 patients, Staphylococcus aureus in 1 patient, Brucella in 1 patient, and bacteriologic testing of intraoperative samples did not find germs in 1 patient. The 2 patients with preoperative neurological deficit had neurological improvement to grade E. Mean follow-up was 36.2 months (range = 18-56 months). Mean preoperative local lordotic angle was 5.7° (range = + 30° to −5°). Postoperative local lordotic angle improved to a mean of 13.2° (range = +3° to −8°). Functional outcome was graded as excellent in 4 patients, good in 1 patient, and fair in 1 patient. Conclusion: The occurrence of spinal infection at spondylolisthetic level might be not a very rare association. MRI (magnetic resonance imaging) signs at level of degenerative spondylolisthesis must be carefully evaluated not to miss infection at that level. Surgical treatment by posterior instrumentation and interbody fusion allows early mobilization with least incidence of complications.
P402: Correlation Between Hemoglobin A1c and Rates of Infection/Wound Complications Following Lumbar Discectomy
Milad Alam1, S. Tim Yoon2, Blake Formanek1, Hans-Joerg Meisel3, Jong-Beom Park4, Darrel Brodke5, Patrick Hsieh1, Jeffrey Wang1, and Zorica Buser1
1University of Southern California, Los Angeles, CA, USA
2Emory Spine Center, Atlanta, GA, USA
3Bergmannstrost Hospital, Halle, Germany
4Uijongbu St. Mary’s Hospital, The Catholic University, Uijongbu, Republic of Korea
5University of Utah, Salt Lake City, UT, USA
Introduction: Intervertebral disc herniation is one of the most common causes of neck and low back pain. Open and minimally invasive discectomies are often used as a procedure of choice for the treatment of disc herniation. Despite lower complication rates, various factors play a significant role in surgical outcomes. Hemoglobin A1c (HbA1c) has been linked to poor postoperative outcomes, in particular infection. The aim of the current study is to examine a correlation between HbA1c and rates of postoperative infection and wound complications in patients undergoing lumbar discectomy procedure. Material and Methods: Data were collected for patients undergoing single-level and multilevel discectomy between January 2007 and December 2016 using commercially available PearlDiver database. The nationwide Humana private insurance database was queried for patients billed with the Current Procedural Terminology (CPT) codes for lumbar discectomy procedure. The index group was then followed for 1 and 3 months postoperatively. Infection and wound complications were collected using the International Classification of Diseases, Ninth and Tenth Revision Diagnostic codes (ICD-9-D and ICD-10-D). Levels of HbA1C were extracted using Logical Observation Identifiers Names and Codes (LOINC). Levels of HbA1c 3 months prior, day of, and 2 months after surgery were considered. Odds ratios and CI (confidence interval) will be used to compare infection rates between different HbA1c groups. Risk factors and demographics will be controlled using logistic regression. Results: A total of 25 531 patients who underwent lumbar discectomy was identified in our cohort. A total of 21 140 patients underwent a single-level and 4391 patients underwent multilevel lumbar discectomy. A total of 11.3% patients had reported HbA1c measurement on their record. Discectomy procedure was the most common for patients with HbA1c values 6% to 7% (38%), followed by <6% (28%). The highest incidence of infection/wound complications at 3months was seen in patients with HbA1c value 8% to 9% at 6.02% (15/249), followed by >9% at 5.88% and HbA1c 7% to 8% at 4.13%. The lowest incidence of infection was seen in patients with HbA1C value 6% to 7% at 3.11% (34/1095) and <6% at 3.59% (29/807). There was a higher incidence of infection/wound within each HbA1C subset at 3-month versus 1-month follow-up. Additionally, male patients had a higher incidence of infection versus female patients. Conclusion: Lumbar discectomy patients with HbA1c values >8% had the highest rate of infection and wound complications. Male patients had a higher incidence of infection/wound complication. HbA1c did not linearly correlate with the incidence of infection/wound. Our preliminary data suggest that clinicians should take into consideration the higher infection rate in patients with A1C higher than 8 by either delaying surgery until A1C can be lowered or considering additional infection prevent measures.
P403: New Alternatives in the Management of Spine Infections: Case Presentation and Literature Review
Fernando Alvarado-Gomez1, Constanza Bedoya1, David Meneses-Quintero1, Jorge Uribe1, Daniel Gaitan Vargas1, Jose Dangond Millan1, Yuli Fuentes-Barreiro1, and Kenny Lopez-Gomez1
1Hospital Universitario Fundacion Santa Fe de Bogota, Bogota, Colombia
Introduction: The incidence of postoperative infection after spinal surgery has been reported between 0.1% and to 6.7%, and it can result in increased morbidity and mortality, the length of hospital stay, increased readmission rate and hospital costs, and postoperative pain. Conventional management of spine infections have included during time surgical drainage, bone graft removal, subatmospheric pressure systems, intravenous antibiotic while maintaining the instrumentation. Bioactive grafts have emerged as a tool for local control of the infection and promotion of bone growth in orthopedic surgery for long bone infection. Bioactive glass has osteogenic properties based on silica additives that lower the pH, diminishing bacterial growth, and it forms a hydroxyapatite, co-activating osteoblasts. Bioceramics are osteinductors of calcium phosphate and silica, which are mixed with antibiotics that are guided by bacterial cultures. These 2 options may play an important role in spine surgery, and it is still limited and underreported. Material and Methods: A review of the literature was performed on the PubMed database using the terms “bioactive glass” OR “Mg5 ceramic” AND “infection” [Mesh] AND “orthopaedic/surgery” [Mesh] OR “spine/surgery” [Mesh]. A total of 59 articles were found that met the inclusion criteria. Additionally, a series of cases are reported in which bioceramics or bioglasses were used to control deep postoperative infection in spine surgery. Follow-up was made with C-reactive protein, ESR (erythrocyte sedimentation rate), and computed tomography (CT) scans to ensure control of infection and progression of bone growth. Results: The search showed 1 article that involved the application of bioglass in 1 patient and none of bioceramics in spine surgery. Thirty-seven of active bioglass in orthopedic surgery (long bones) and 21 with bioceramics. These articles show the utility and efficacy of these tools in controlling the local growth of germs and bone growth rates. In our series, the average age was 55.88 years, 77% were women and 22% men; 44% of procedures were in the thoracic spine, 22% in the thoracolumbar junction, and 33% in the lumbar region. The main spinal pathology for surgery was degenerative disease (33%) 2 due to fracture, 2 tumoral (both primaries), 1 deformity, and 1 infection. Two cases required a second series of surgical drainage. Conclusion: To our knowledge, this is the largest series of application of bioactive grafts in spinal infection. These provide a novel option for the local management of the infection and also help bone formation to promote fusion. Results in orthopedic surgery have shown and adequate at long-term follow-ups. The theoretical basis for its use is well supported, but it needs longer follow-ups and series of cases in spinal surgery. Most of the patients in our series (78%) had adequate evolution with no recurrence of infection and signs of bone growth in CT scans.
P404: Instrumentation for Pyogenic Spinal Infection: A Single-Center Experience With 368 Cases
Ehab Shiban1, Amm-Kathrin Jörger1, Nicole Lange1, Arthur Wagner1, and Insa Janssen1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Aim: To determine the safety and efficacy of surgical debridement with instrumentation in treating pyogenic spinal infection. Material/Methods: Between June 2006 and June 2016, 387 consecutive patients suffering from spondylodiscitis were admitted to our department. Three hundred sixty-eight (95%) underwent surgical debridement and instrumentation, while 19 were treated conservatively. Surgically treated patients were analyzed. Clinical outcome was assessed with neurological and laboratory examinations at 3 months following surgery. Long-term clinical outcome was assessed at a minimum of 12 months following surgery with a telephone interview. Results: The mean age at presentation was 67 years, and 244 patients were male (66%). Distribution of the inflammation was lumbar in 241 (66%), thoracic in 57 (15%), and cervical in 51 (14%) cases. Nineteen patients (5%) had 2 concomitant noncontiguous spondylodiscitis in different segments of the spine. Epidural abscess was found in 74 patients (35%). Three hundred thirty-eight patients (92%) had pain. Neurological deficit was found in 160 patients (43%). In the thoracic and lumbar cases, dorsal instrumentation alone was considered sufficient in 125 cases and additional interbody fusion from dorsal was performed in 89 cases. In 94 cases, 360° instrumentation was performed. In the cervical cases, ventral spondylodesis was performed in 18 cases and ventral plating, dorsal instrumentation alone in 19 cases, and 360° instrumentation in 21 cases. Postoperative intravenous antibiotics were administered for 13.6 ± 8.2 days followed by 3.0 ± 0.9 months of oral antibiotics. Complete healing of the inflammation was achieved in 204 (97%) cases. Only 4 patients had a relapse of the inflammation. Five patients died due to septic shock (2 because of fulminant endocarditis and 3 by multiple organ dysfunction syndrome). One patient died postoperatively due to pulmonary embolism. From the 160 patients with neurological deficit, 44 (46%) had full recovery and 33 (34%) had improved incompletely after surgery. Conclusion: Surgical debridement and instrumentation is relatively safe and a very effective approach to achieve complete healing of spinal inflammation. Thereby, a short period of intravenous antibiotics of 1 to 2 weeks followed by 3 months of oral antibiotics is appropriate in most cases.
P405: Low-Grade Infection in Spinal Instrumentation: Is This the Real Cause of Screw Loosening?
Ehab Shiban1, Insa Janssen1, Ann-Kathrin Jörger1, Nicole Lange1, Arthur Wagner1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Introduction: We investigated the hypothesis that many aseptic screw-loosening revisions in spinal instrumentations are in fact low-grade infections and not due to mechanical screw overload. Methods: A prospective observational study was performed. All patients undergoing spinal instrumentation revision surgery between August 2015 and August 2017 were screened. In the study group, all patients with an indication for revision due to screw loosening on CT (computed tomography) scan were included. In the control group, those needing revision for adjacent disc disease were included. The rate of low-grade infection using a sonification fluid culture was analyzed. Results: A total of 101 revision surgeries after spinal instrumentation were analyzed. Sixty-three (62.4%) were performed because of radiographic signs of screw loosening, and 38 (37.6%) were done because of other reasons, mainly adjacent segment degeneration. In the screw-loosening group, there were significantly more germs cultivated either through the sonication method or the swab method (55.9% vs 42.9%) compared with the control group (35.3% vs 27.3%; P = .001). The most frequent bacterium cultivated in both groups was propionibacterium acnes, and the second most frequent were Staphylococcus spp. Median serum CRP (C-reactive protein) and leucocyte levels before revision surgery were not significantly elevated in both groups, and there was no significance in between groups difference. Conclusion: More than half of symptomatic screw loosening was associated with a low-grade infection. Sonification is recommended in all patients with screw loosening.
P406: Surgical Site Infection Following Spine Surgery: Role of Prevention Care Bundle
Shanmuganathan Rajasekaran1, Rajdeep Singh Bagga1, Ajoy Prasad Shetty1, and Rishi Mugesh Kanna1
1Ganga Hospital, Coimbatore, India
Introduction: Postoperative surgical site infections (SSIs) pose a significant burden on health care, and despite surgical advances and the use of prophylactic antibiotics, continue to be of major concern. Efforts like care bundle to improve safety have been focused on reducing SSI, but literature discussing its effectiveness specific to spine surgery is limited. The purpose of the study was to analyze the effect of care bundle protocol on SSI in our institution. Material and Methods: A retrospective analysis of 6986 consecutive patients who underwent spine surgery in our institute from January 2014 to December 2017 was performed. All patients who received prevention care bundle divided into (1) preoperative bundle-strict glycemic control, chlorhexidine gluconate (CHG) 20% v/v bath, (2) Intraoperative bundle-time specified iv (intravenous) cefuroxime prior to induction, skin preparation with 2.5% v/v CHG, and (3) postoperative bundle-strict protocol for drain use, antibiotic use, and sterile dressing, from January 2017 formed post-implementation group and patients prior to that formed the pre-implementation group. Patient data drawn from weekly and yearly spine audits, HIC (Hospital Infection Committee) software were collected. Infection was categorized as (1) superficial and deep (CDC [Centers for Disease Control and Prevention] criteria classification), (2) early and late (depending on time of onset less or more than 4 weeks), (3) instrumented/uninstrumented, (4) depending on spinal disorders (degenerative, trauma, deformity, tumor), and (5) spine level (cervical, thoracic, lumbar). Preexisting infections formed the exclusion group. Variables were analyzed in pre- and post-implementation group and evaluated using SPSS (16.0) Software. Results: Mean age of patients was 45.3 ± 18.18 years (72 males and 79 females). Reduction rate of SSI in pre-implementation group 2.4% (131/5532) compared with post-implementation group 1.5% (22/1454), which was statistically significant (P = .04).The rate of reduction in early (P = .03) and superficial (P = .049) infection were significantly higher (χ2 test) in post-implementation group, but no significant difference was found in deep and late infection, level and approach of surgery, presence of instrumentation and spinal disorders (P ≥ .05). Among infected cases, 6.54% were cervical, 27.45% thoracic and 66.01% lumbar, 67.32% cases were degenerative, 5.23% tumor, 14.38% trauma, and 13.07% deformities with 71.24% instrumented and 28.76% noninstrumented. There were 94 (61.44%) superficial and 59 (38.56%) deep SSIs of which 127 (83.01%) were early and 26 (16.99%) late infections. Conclusions: Our study revealed that using prevention care bundle significantly reduced SSIs compared with patients who did not receive these interventions, more prominently early and superficial infections.
P407: Drains in Posterior Spinal Fusion Surgery for Scoliosis in Children: Do We Really Need to Use Them to Keep Infection Rates Down?
Jun Liang Derrick Lam1 and Boon Leong Kevin Lim1
1KK Women’s and Children’s Hospital, Singapore, Singapore
Introduction: There is little published evidence on drain usage in pediatric spinal surgery, particularly in scoliosis surgery, and their role in preventing infection. The hypothesis of our study is that the infection rate does not increase when drains are not used in posterior spinal fusion surgery (PSF) for pediatric scoliosis. Materials and Methods: This is a single-center retrospective analysis of all children who had primary PSF for scoliosis over a 9-year period (2008-2016). No drains were used. They had antibiotic prophylaxis for no more than 72 hours postoperatively. They were followed-up for at least 2 years. Primary outcome was infection rate, superficial and deep inclusive. Results: A total of 146 patients were divided into 4 groups: 107 idiopathic, 24 neuromuscular, 5 congenital, and 10 syndromic. The infection rate in the idiopathic group was 0.93% (1/107): a well 22-year-old girl presented with paraspinal abscess 18 months postoperatively. After wound exploration and drainage (cultures: Finegoldia anaerobe), she had removal of implants, recovering well. The infection rate in the syndromic group was 10% (1/10): a 13-year-old boy with Marfan syndrome and a history of ginseng usage was readmitted on postoperative day 8 with a paraspinal fluid collection that was drained with image guidance. Cultures negative. His implants were retained; and he has been well the past 2 years. The neuromuscular and congenital groups had no infection. The overall infection rate was 1.37% (2/146). Our infection rates are generally lower than published studies: idiopathic up to 1.9% (drain) and 2.8% (no drain); for combined infection rates (drain and no drain), neuromuscular up to 13.3%, congenital 6.1%, syndromic 6.9%, and overall 2.6%. Conclusion: Our results suggest drain usage following PSF for scoliosis may not be essential; and our infection rates are generally lower than published studies. Significantly, we have zero infections in the neuromuscular group, which classically has a higher infection rate. In our syndromic group, ginseng, which has been shown to have an effect on hemostasis, could have accounted for higher than average infection rate. Our study’s main limitation is the assumption that the study population is similar in all other respects, particularly with regard to general health, surgical, and perioperative factors including antibiotic prophylaxis and medications.
P408: CT-Guided Biopsy Is Superior to Blood Cultures in Detecting Causative Bacteria in Pyogenic Spinal Infection
Ehab Shiban1, Ann-Kathrin Jörger1, Nicole Lange1, Arthur Wagner1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Background: The Infectious Diseases Society of America recommends in nonseptic cases to withhold antibiotic treatment until a germ has been identified. Thereby, culture from infected tissue remains the gold standard. We aimed to assess the effectiveness of computed tomography–guided biopsy (CT-GB) in detecting the causative bacteria in comparison to blood cultures (BC) in pyogenic spinal infection. Methods: A consecutive cohort of patients suffering from spondylodiscitis between January 2015 and June 2016 were retrospectively analyzed. Results: In 53 cases a CT-GB was performed, and in 28 (52%) cases a bacterium was found. In 71 cases BC were obtained, and in 34 (47%) cases a bacterium was found. In 36 patients, both CT-guided biopsy and BC were obtained. A causative bacterium was identified in 21 (58.3%) and 25 (69.4%) from BC and CT-GB, respectively. Conclusion: Only in half of cases, a causative bacterium is found through CT-GB or BC in patients with spondylodiscitis. Thereby, on direct compression CT-GB was superior to BC in detecting a causative bacterium.
P409: Posterior Instrumentation and Fusion in Thoracolumbar Spinal Tuberculosis as an Effective Technique in a Kenyan National Referral Hospital
Nilesh Mohan1
1Moi Teaching and Referral Hospital, Eldoret, Kenya
Introduction: Tuberculosis of the thoracolumbar spine is common in developing countries. It is a common cause of disability and paraplegia. Surgery is done in patients with cord compression, and this involves use of anterior and/or posterior instrumentation techniques in addition to antituberculous therapy. We compare fusion and complications of using the posterior instrumentation techniques. Materials and Methods: Thirty patients with thoracolumbar tuberculosis who underwent posterior decompression and instrumentation were selected retrospectively. The age distribution, duration of symptoms, Frankel score, immunosuppression status, extraspinal tuberculosis infection, and level of spine involvement were recorded preoperatively. Patients who had been followed-up for a minimum duration of 6 months were included in the study. The disability score at 6 months and 1 year was recorded, and implant complications were recorded. Results: Majority of the patients (75%) were young (20-35 years of age), 78% were immunocompetent, and 40% had Frankel score of A and B. All patients had posterior instrumentation with minimum of 3 level instrumentation, the commonest being the thoracolumbar junction. All patients had antituberculous therapy for 1 year. Fusion rates at 6 months was present in 85% of patients at 1 year. Complications included postoperative infections, paraspinal abscesses, and implant failure, which occurred in 14% of patients. Conclusion: Posterior instrumentation is an effective technique in thoracolumbar spine tuberculosis. It is relatively easier for the spine surgeons to adapt the technique compared with anterior instrumentation with lesser morbidity associated with anterior approaches in regions where surgeons are not well trained. Complication rates are associated with immunosuppression status, severe disability before surgery, and greater than 4 levels of instrumentation.
P410: Intervertebral Disc Penetration by Antibiotics Used Prophylactically in Spinal Surgery: Implications for the Current Standards and Treatment of Disc Infections
Christof Birkenmaier1, Manu N. Capoor2, Jan Lochman3, Andrew McDowell4, Martin Solansky3, Martina Zapletalova3, Todd F. Alamin5, Michael F. Coscia6, Steven R. Garfin7, Jonathan E. Schmitz8, Radim Jancalek3,9, Filip Ruzicka3,9, A. Nick Shamie10, Martin Smrcka3,11, Jeffrey C. Wang12, and Ondrej Slaby3,13
1Ludwig-Maximilian-University Munich, München, Germany
2Rockefeller University, New York, NY, USA
3Masaryk University, Brno, Czech Republic
4Ulster University, Londonderry, UK
5Stanford University Medical Center, Stanford University, Stanford, CA, USA
6OrthoIndy Hospital, Indianapolis, IN, USA
7University of California San Diego, CA, USA
8Vanderbilt University School of Medicine, Nashville, TN, USA
9St. Anne’s University Hospital, Brno, Czech Republic
10University of California, Los Angeles, CA, USA
11University Hospital Brno, Brno, Czech Republic
12University Southern California, Los Angeles, CA, USA
13Central European Institute of Technology (CEITEC), Brno, Czech Republic
Introduction: A high prevalence of Propionibacterium acnes colonization in intervertebral disc material obtained from patients undergoing discectomy or microdiscectomy has led to the suggestion that this prominent human skin and oral commensal may exacerbate the pathology of degenerative disc disease. This hypothesis, in turn, raises the possibility that antibiotics could play a role in treating this debilitating condition. In addition, the existence of low-grade disc infections with P acnes, which is not consistently sensitive to cephalosporins, challenges the current recommendations as to which antibiotic should be used for perioperative prophylaxis in spinals surgery. To date, however, little information about antibiotic penetration into the intervertebral disc is available. Material and Methods: Nucleus pulposus material from 54 microdiscectomy patients who had received prophylactic cefazolin (n = 25), clindamycin (n = 17), or vancomycin (n = 12) was analyzed by means of high-performance liquid chromatography (HPLC), with cefaclor serving as an internal standard, to determine the concentration of antibiotic penetrating into the disc tissue. Results: Intervertebral disc tissues from patients receiving the positively charged antibiotic clindamycin contained a significantly greater percentage of the antibacterial dose than the nucleus material from patients receiving the negatively charged cefazolin (P < .0001) and vancomycin, which has a slight positive charge (P < .0001). Conclusion: Positively charged antibiotics appear more appropriate for future studies investigating potential options for the treatment of low-virulent disc infections with P acnes. The current standards for perioperative antibiotic prophylaxis in spinal surgery probably should be reexamined.
P411: Outcome of Surgical Treatment of Tuberculosis Spine
Md Yousuf Ali1
1Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Introduction: Spinal tuberculosis (TB) accounts for over 40% of all spine infections. This clinical entity is socioeconomic related, occurring more often in developing countries, although an increase in incidence has been documented in developed countries. About 10% of all TB cases present with musculoskeletal involvement and 50% of these involve the spine (Pott’s disease). The thoracic and lumbar spine are most commonly involved (90% of cases). Delay in establishing diagnosis and management cause spinal cord compression and spinal deformity. Material and Methods: This is a prospective study, was performed in different private clinics in Dhaka from July 2006 to July 2018, and included total 102 patients, among them 53 were male and 49 were female, with age ranging from 17 to 70 years. Neurological deficits were graded using the American Spinal Injury Association (ASIA) Impairment Scale of motor and sensory impairment, which ranges from A (no motor or sensory function) to E (normal functioning). Thoracotomy along with anterolateral decompression, autogenous bone graft with case, and fixation by screws and rods were done in 12 cases. Posterior decompression, posterior interbody, and posterolateral fusion by bone graft with or without cage and stabilization by pedicle screws and rods were done in remaining 90 cases. Appropriate anti-TB drugs were given to all patients for 12 to 18 months. Follow-up period was 3 months to 10 years. Results: Infection eradication and spine fusion was achieved in all patients. All patients improved back pain and neurological status except 1 case. There was no progressive kyphotic deformity. Among all patients, revision surgery was done in 2 cases and superficial wound infection were encountered in 5 cases. There was no mortality. Conclusion: Surgical treatment combined with chemotherapy is a safe and effective approach to treat spinal TB infection. Severe cases with large abscesses and extensive vertebral column involvement, aggressive treatment with direct aspiration and debridement, anterior reconstruction and posterior instrumentation can result in a rapid recovery and acceptable rate of complications.
P412: Method to Protect the Neural Elements When Using a Vacuum-Assisted Closure to Manage Deep Postoperative Wound Infections
Tochukwu Ikpeze1 and Addisu Mesfin1
1University of Rochester Medical Center, Rochester, NY, USA
Introduction: The use of vacuum-assisted closure (VAC) devices in the management of surgical site infections following spine surgery has been well documented. However, the use of VAC in the setting of exposed dura and neural elements does not have an established standard of care. Our objective is to describe a technique of protecting the neural elements when using VAC for postoperative deep wound infections. Material and Methods: A single surgeon database from October 2012 to August 2018 was evaluated for patients undergoing VAC to manage deep postoperative wound infections. All patients were managed at a level I trauma center by a fellowship-trained orthopedic spine surgeon. The following patient variables were collected: age, sex, site of surgery, complications, intraoperative culture results, and definite management of the infection. The decision to use a VAC depended on the extent of pus and necrotic muscle below the fascia. After a thorough debridement and irrigation, Adaptic, a non-adherent wound dressing is applied on top of the neural elements (dura, exposed nerves). Following the application of VAC sponges and tubing, the VAC machine suction is turned on at continuous, 125 mm Hg. On return to the OR (operating room) to change the VAC or to perform the definitive closure, the VAC sponges can be easily removed without concern of adhesion to neural elements. After minimal irrigation, the Adaptic can be peeled off the neural elements with a Woodson elevator. Results: A total of 1170 patients underwent surgical intervention over the study period, and 4 patients (0.3%) needed Adaptic coverage of neural elements and VAC treatment of deep postoperative wound infections. Average age was 49 (30-57), with 3 females and 1 male. All deep wound infections were posterior, 2 in the lumbar spine and 2 in the cervicothoracic junction. Initial diagnoses were lumbar spondylolisthesis treated with laminectomy and fusion (1), 2-level lumbar disc herniations/stenosis treated with laminectomy and discectomies (1), metastatic lung cancer with epidural extension at C7 treated with laminectomy and fusion (1), and cervicothoracic spondylodiscitis that underwent prior laminectomy and fusion (1). Cultures grew MSSA (methicillin-resistant Staphylococcus aureus; n = 2 patients), Proteus mirabilis, Escherichia coli, Klebsiella pneumoniae, Bateroides fragilis (n = 1 patient), and coagulase-negative Staph (n = 1 patient). Three of 4 patients underwent multiple debridements and VAC changes prior to closure. Both patients with infections in the cervicothoracic junction needed a trapezius flap due to the dead space present and amount of infected tissue. There were no complications associated with Adaptic coverage of the neural elements. Conclusion: The decision to immediately close versus stage the closure of a deep postoperative spine infection is dependent on the extent of infection and soft tissue involvement. VAC is useful in the setting of a staged wound closure. The use of Adaptic to protect the neural elements along with a VAC can minimize the risk of VAC sponge adhesion to the neural elements and helps protect the neural elements.
P413: Neonatal Cervical Epidural Abscess With Cervical Cord Compression From Maternal Antenatal Pneumonia: A Rare Case Report
Denis Dian Lee1, Abdul Razak Bin Haidzir1, and Zulasri Azan Bin Md Zain1
1Hospital Putrajaya, Putrajaya, Malaysia
Introduction: Prevertebral abscess in neonates is exceedingly rare. Diagnostic difficulty is further compounded by a grossly uncooperative patient and often times sketchy history. Radiological evidence is often times made difficult by hesitance of the radiology unit to provide sedation for neonates. A high index of suspicion is vital. Material and Methods: We report a case of an infant who presented at day 28 of life with fever, rhinorrhea, and sudden onset of upper limb weakness at a district hospital. The infant was diagnosed as right Erb’s palsy on presentation and referred to the orthopedic unit for further assessment and management. On examination, it was discovered that Moro’s reflex was incomplete bilaterally with paucity of movement of bilateral upper limbs. Radiographs ordered at the emergency department ruled out any fractures. On further history-taking, the child was born via uneventful cesarean section due to maternal pregnancy–induced hypertension with birth weight 2.8 kg. Bilateral upper limb was normal at birth. On further probing, the mother revealed a recent antenatal ward admission for pneumonia and was administered intravenous antibiotics for a week. The infant’s blood counts revealed leukocytosis, perceived to be associated with the rhinorrhea by the pediatrics team. An urgent brain and cervical magnetic resonance imaging (MRI) was ordered by the attending orthopedic surgeon and was duly rejected by a tertiary center as the pathological entity was rare. Only the following day was an MRI obtained after much coaxing of the radiology unit. Results: MRI cervical revealed prevertebral fluid collection extending from C1 to C6, which invaded the C5 vertebral body causing epidural intraspinal extension. A diagnosis of a cervical prevetebral abscess and C5 osteomyelitis with epidural extension causing cervical cord compression was made. Due to the anatomical peculiarity of the neonate spine, the patient had to be referred to the National Neurosurgical Unit for surgical decompression. Supportive antibiotic therapy for the isolated Klebsiella pneumoniae thereafter saw complete resolution of neurological deficit. Conclusion: Epidural abscess is a rare entity with less than 90 cases reported in children. This novelty diagnosis is even rarer among neonates. However, a high index of suspicion is vital to avoid unnecessary diagnostic and treatment delays, which can result in undesirable permanent neurological disabilities. Typically, spinal epidural abscess represent a hematogenous spread. In this patient, the source of bacteremia was through the antenatal placenta during an antenatal episode of maternal pneumonia. Our literature review was unable to return previously recorded cases of similar pathophysiology. MRI remains the best modality to visualize the extent of epidural abscess. MRI offers multiplanar soft tissue imaging of the cervical spine and its periphery, and it is a distinct advantage compared with CT (computed tomography) scans. However, when MRI is inconclusive, a myelography should be performed in suspected cases.
P414: 360° Long-Segment Cervico-Dorsal Spinal Fusion for Treatment of Pediatric Cervical Spinal Tuberculosis With Kyphosis Using Dual Plate and Hartshill Frame: A Salvage Technique and Technical Note
Varun Agarwal1
1Rohilkhand Medical College, Bareilly, India
Introduction: There is limited literature on surgical management of pediatric CST (craniosacral therapy) more so involving the junctional areas. We present a case of staged cervico-dorsal junctional TB (tuberculosis) treated with anterior decompression and long-segment C4 to D4 fusion with iliac crest strut graft and dual plates using the standard anterior cervical approach followed by posterior fusion with Hartshill frame. Case Report: A 15-year-old female presented to the OPD (outpatient department) with weakness in all 4 limbs. On examination, there was tenderness lower cervical spine region with grade 3 power in all 4 limbs. X-ray and computed tomography (CT) scan showed marked destruction C6 to T1. MRI (magnetic resonance imaging) showed prevertebral abscess up to D4. Surgical Technique: Stage 1 (Anterior Surgery): Patient was positioned supine head in crutchfield traction. A longitudinal incision was taken along the anterior border of the sternocleidomastoid till as the medial end of the clavicle. Access to D4 was achieved by obliquely placing a retractor and retracting without removing part of clavicle or manubrium. A single-piece iliac crest graft was harvested and placed in the graft bed. Since single long plate able to span C4 to D4 was not available, 2 smaller plates were used innovatively by anchoring one ends of the plates with screws in the upper and lower bodies and the other ends of the plates anchored to the iliac crest graft with 1 screw each to stabilize both the plates and graft. Stage 2 (Posterior Surgery): Patient was positioned prone after GA (general anesthesia). Posterior stabilization was done using Hartshill frame and wires. Patient was allowed ambulation from day 2. Result: Three-month follow-up CT shows no loss of fixation and good fusion. Discussion: Anterior approach to cervico-dorsal junction in itself is difficult and may involve a sternotomy and handling of great vessels, which most surgeons are not comfortable with. Anterior radical curettage and damage to end plates destroy the anterior growth potential. The posterior column continues to grow, and this may lead to severe deformities. Straightforward anterior surgery may land the patient in complex deformity later in life, hence the role for 360° fusion. Combining both anterior and posterior fusion greatly decrease stresses on graft and hence graft- and fixation-related complications and greatly increase stability. But in cases like these involving such long segments more often than not, it is found that ideal length plates are not commercially available. Hence an innovative “out-of-the-box” approach was employed to anchor the graft using dual plates as described above. A second-stage posterior fusion using Hartshill frame and sub laminar wires and outer cortex of posterior spinous process and lamina shingled with osteotome and nibbler and bone used as onlay graft was used to posteriorly fuse the spine and also at the same time restricting the posterior segment growth in the fused segments leading to late kyphotic deformity and anterior construct failure. Conclusion: The 360° fusion decreases the stress on the plate and graft, increases stability, reduce graft- and fixation-related complications, and increases fusion rates.
P415: Application of “Custom-Made” PMMA Corpectomy Spacer in Cervical Spondylodiscitis: A Case Report
Adam Biczo1, Balazs Szollosi1, Zoltan Hoffer1, and Peter Pal Varga1
1National Center for Spinal Disorders, Budapest, Hungary
Introduction: Primary cervical spondylodiscitis are a rare but very severe entity. It is more frequently associated with neurological symptoms than lumbar discitis due to the vicinity of the spinal. Its incidence is growing possibly due to the increasing elderly and immunocompromised patient population. There is some evidence in the literature that cervical spondylodiscitis requires more often a surgical treatment than other localizations. Therefore, the proper multimodal management of the entity can be challenging. Materials and Methods: Case report. Results: A male patient (76 years) with medical history of right-side nephrectomy, ischemic heart disease, azotemia, and lumbar disc herniation was hospitalized to a cardiac unit with suspected acute coronary syndrome (ACS). He had elevated inflammatory markers (CRP [C-reactive protein], ESR [erythrocyte sedimentation rate]). ACS was ruled out but he had a positive blood culture (Escherichia coli) and positive urine culture (Citrobacter sp) and was treated with intravenous (iv) antibiotics. He was discharged to home with normalized inflammatory parameters. Some days after the emission, he developed upper extremity palsy and pain and was hospitalized again. He had greatly increased CRP and ESR. One week after the admission, he developed lower extremity irradiating pain and parapalsy. According to the neurosurgeon’s opinion based on a cervical computed tomography (CT) scan and clinical symptoms, the patient needed no surgical intervention but was transferred to our institution for a second opinion. Acute cervical MRI (magnetic resonance imaging) has shown the signs of spinal infection from CV to CVII. Moreover, 2-level myelopathy was present. A staged ventro-dorsal procedure was planned. From anterior approach, CV-VI and VI-VII discectomy and CVI corpectomy with the use of “custom made” polymethyl methacrylate (PMMA) corpectomy spacer and CV-VII plated fixation was done first. On the next day, a dorsal decompression and CV-ThI lateral mass and transpedicular screw fixation was performed. Based on the intraoperative cultures (Enterobacter cloacae), targeted iv imipenem therapy was admitted for 14 days, which was continued with oral co-trimoxazole therapy for 3 months. Immediately after the surgery, the patient showed mild improvement in the left upper extremity palsy but no change in the paraplegia. After the surgery, CT scan showed optimal screw and PMMA spacer positions. At 3-month follow-up, the patient had normal labor parameters and a significant improvement in all muscle strength. CT showed optimal implant position. Conclusion: Multimodal management of a cervical spondylodiscitis case can be challenging, and mechanical complications after a surgical intervention are frequent because of the compromised local bone quality. This case report represents the use of “custom made” PMMA spacer in a cervical spondylodiscitis case with extensive endplate destructions. The use of PMMA spacer in spinal infections has got several advantages. It can contain and release antibiotics and can be shaped to completely fill out the corpectomy space providing an increased stability. The stability of the construct can be further enhanced by the anchoring the plate or posterior instrumentation into the spacer with screws.
P416: Application of Negative Pressure Wound Therapy in Spinal Infections
Istvan Klemencsics1, Ivan Lambertusz1, Aron Lazary1, Zoltan Hoffer1, and Peter Pal Varga1
1National Center For Spinal Disorders, Budapest, Hungary
Introduction: Surgical site infection (SSI) after extended thoracolumbar spine surgery is a serious complication. Treatment of SSI in these complicated cases is a major challenge for both patients and clinicians too because of prolonged hospitalization and antibiotic therapy and several times performed revision surgeries. Negative pressure wound therapy (NPWT) can offer a comfortable and hygienic help in extensive infected wounds. Aim of our study was to analyze the success of NPWT application among patients who underwent thoracic and/or lumbar spinal surgery from dorsal approach and suffered from poorly healing, ornery deep wound SSI. Material and Methods: All of the patients were treated in a tertiary referral center because of primary spinal infection, degenerative spinal disorders, or deformity. Success of NPWT was defined as no need for further surgical intervention (eg, suture, debridement, and revision) because of SSI after the completion of NPWT. Duration of NPWT (days) and fate of spinal implants (retain, exchange, remove) were also analyzed. Results: The clinical data of 31 patients were analyzed between November 2013 and November 2016 retrospectively. All patients suffered from a severe deep wound SSI after extended thoracic and/or lumbar spinal surgery from dorsal approach. The mean age of study population was 55.7 years (16-84 years). Most of the patients were female (N, female = 21; N, male = 10). The mean duration of NPWT was 24.6 days (6-110 days). Most of the spinal instruments could be preserved (N = 22, 70.9%) with NPWT. Surgical wound was closed after NPWT by plastic surgeon in 3 cases. There was no need for further surgical intervention because of SSI in case of nearly two third of patients (N = 19). NPWT-related complication did not occur in the cohort. There were 3 patients who died during NPWT due to septic conditions. Conclusion: NPWT can offer a hygienic and comfortable wound care in even seemingly hopeless, unmanageable deep wound spinal SSI cases. NPWT can decrease the number of septic revision surgeries or can prevent the propagation of the septic condition. Previously implanted spinal instruments can also be preserved providing the mobilization possibility for the patient. Wound closure after NPWT may require the involvement of a plastic surgeon.
P417: Acute Life-Threatening Complex Craniocervical Infection and Instability Secondary to Chronic Middle Ear Cholesteatoma: A Case Report and Review of Literature
Ali Mohammad1, Olakunle Badmus1, Holger Schlag2, Guiseppe Morassi3, Bronek Maximilian Boszczyk4, and Masood Shafafy1
1Queen’s Medical Center Nottingham University Hospital, Nottingham, UK
2Nuremberg
3Brighton and Sussex University Hospitals NHS Trust, Brighton, UK
4 Benedictus Clinic Tutzing, Tutzing, Germany
Introduction: Cholesteatoma refers to an expanding and destructive abnormal growth of keratinized, desquamated epithelium in the middle ear or mastoid. Cholesteatomas are locally destructive due to the production of proteolytic enzymes by the lesion. We are reporting an extremely uncommon complication of cholesteatoma as a rare cause of craniocervical junction (CCJ) infection and instability. We are also describing our successful management of this rare condition. No similar condition has been reported in the literature that makes it more challenging to manage. Material and Methods: A 75-year-old woman with a medical background of right side cholesteatoma, which was treated surgically 35 years back, presented to our department with history of neck pain, speech problems, and pyrexia. She was tachycardic with paradoxical breathing and GCS (Glasgow Coma Scale) 13/15. Examination revealed motor power deficit on the right upper and lower limbs with purulent and smelly discharge from the right ear. Investigations, imaging (CT [computed tomography]/MRI [magnetic resonance imaging]), and cultures showed a clinical picture osteomyelitis of the CCJ with basilar invagination, brainstem compression, and meningitis secondary to chronic middle ear infection. Results: Dramatic improvement of her motor functions and general condition started to improve after giving intravenous antibiotics with urgent decompression, reduction of basilar invagination by applying halo traction, and drainage of the middle ear abscess. Because of her CNS (central nervous system) infection, we did not perform any definitive surgical decompression or stabilization except for the halo traction. Close follow-up and imaging showed autofusion of the CCJ in good position and no brainstem compression with recovery of all her symptoms. Conclusion: There was no clear or established treatment guidelines to treat basilar invagination secondary to infection of the CCJ. Immediate reduction with urgent surgical stabilization is the standard rule of treatment for symptomatic cases. The management of this complex and rare condition remains a therapeutic challenge, and successful treatment with conservative treatment is not typically possible. However, each case should be managed according to the specific clinical circumstances and alternative treatment options may be possible.
P418: Natural Recovery in Walking Function After Incomplete Spinal Cord Injury: Novel Insight from Group-Based Trajectory Modeling
Blessing Jaja1, Jetan Badhiwala2, Bizhan Aarabi3, Maxwell Boakye4, Robert Grossman5, Fred Geisler6, James Harrop7, Shekar Kurpad8, Ralph Schar2, Michael Fehlings2, and Jefferson Wilson2
1University Health Network, Toronto, Ontario, Canada
2University of Toronto, Toronto, Ontario, Canada
3University of Maryland, Baltimore, MD, USA
4University of Louisville Hospital, Louisville, KY,-USA
5Weill Cornell Medical College, Houston, TX, USA
6Independent Neurosurgeon, Chicago, IL, USA
7Jefferson University, Philadelphia, PA, USA
8Medical School of Wisconsin, Wauwatosa, WI, USA
Introduction: The prognosis of walking function has considerable implication for quality of life after traumatic spinal cord injury (SCI). Consequently, recovery in walking ability and measures to maximize are of extreme value to affected subjects and the health care team who are involved at different paths along the continuum of care. In this study, we investigated subjects with incomplete SCI to test the hypothesis that there are latent longitudinal recovery trajectories in walking function and patient or injury-related factors are associated with recovery trajectories. Material and Methods: Study population consisted of subjects with incomplete SCI (American Spinal Injury Association [ASIA] grade B/D) from the North American Clinical Trials Network (NACTN) multicenter longitudinal studies. Walking ability was assessed according to the SCIM (Spinal Cord Independence Measure) subscale for mobility indoors within 7 days of SCI at 3-, 6-, and 12-month follow-up. Group-based trajectory modeling (GBTM) was used to identify subgroups of subjects who follow distinct homogenous trajectories of recovery in walking ability during the initial 12 months post injury. Multinomial logistics regression was applied for association analysis. Results: Among 337 subjects studied, 4 stable walking recovery trajectories were identified including: poor minimal recovery (30.3%), progressive incomplete (28.4%), progressive complete (22.3%), and full recovery (19.0%). Having ASIA grade C or D injury was associated with belonging to trajectories with better prognosis, compared with grade B injury. Having pneumonia, wound infection or sepsis was negatively associated with belonging to trajectories with better prognosis. In addition, increasing age was negatively associated with belonging to the progressive complete recovery trajectory (OR [odds ratio] = 0.97, 95% CI [confidence interval]: 0.95-0.99, P = .004). Conclusion: This study contributes to a better understanding of the heterogeneity in walking recovery seen among subjects with incomplete SCI. The identified longitudinal trajectories might be suitable endophenotypes for characterizing, and predicting recovery in walking function after incomplete SCI as well as for planning future interventional studies.
P419: Pyogenic Vertebral Osteomyelitis Complicated by Neurological Deficits and Spinal Epidural
Aleksandr Bazarov1, Konstantin Sergeev2, and Vladislav Osintsev2
1GBUZ TO Regional Clinical Hospital #2, Tyumen, Russian Federation
2FGBOU VO Tyumen State Medical University, Tyumen, Russian Federation
Introduction: In recent years, the number of patients with pyogenic vertebral osteomyelitis (PVO) has been rising, recording 0.2 to 2.0 of new incidences per 100 000 persons annually. In the past times, there is a significant increase in the number of people affected by PVO, which also leads to the increased number of cases with PVO complications. The most hazardous complications to PVO are sepsis and spinal epidural abscess (SEA). The frequency of the neurological deficit is up to 22.4% to 75%. Material and Methods: According to the records of the Regional Hospital #2 in Tyumen, 209 PVO patients were treated in the period 2006 to 2016 and retrospectively reviewed. In the past 3 years, the number of PVO cases has increased by 2.3 times. The average diagnosis time is 2.6 months. Neurological deficit has been diagnosed with 37 patients (17.7%) that comprised group I; and patients without neurological deficit make up 172 cases (82.3%) were in the II group. The patients’ average age is 49.1 ± 15.01. The female–male sex ratio is 1:3. The number of patients with HIV is 41 (19.6%). The largest recorded number of patients in the age group of 31 to 40 years: n = 54 (25.8%), and the cases of neurological deficit is more frequent in the age group of 51 to 60 years: n = 12 (5.7%). Results: Within group I, SEA was diagnosed in 24 (64.9%) cases and in 11.5% of all the number of patients with PVO, and Staphylococcus aureus was recorded in 14 patients (58.3%). The severity of the neurological deficit according to the Frankel scale on the patient’s arrival day: A = 6, B = 7, C = 17, D = 5, and E = 2. On the release day: A = 3, B = 2, C = 13, D = 11, and E = 8. Cervical spine was diagnosed in 15 cases (40.6%), thoracic in 16 cases (43.2%), and lumbar in 6 cases (16.2%). The impact of the cervical spine increases the risk of neurological damages (P = .001). The infection by S aureus increases the risk by 3.15 times. Group II had the following damage location: cervical spine was diagnosed in 6 cases (3.5%), thoracic in 53 cases (30.8%), and lumbar in 113 cases (65.7%). Surgery was performed in 35 cases (94.6%) in group I. The treatment included drainage and debridement (42.9%), instrumentation, and fusion (57.1%). The instrumentation was used in 45.7% cases (n = 16): with drainage and debridement 8.6% (n = 3), with fusion 31.4% (n = 11), and laminectomy 5.7% (n = 2). The patients with instrumentation and patients without any did not have statistical differences in the restoration of neurological deficit. Thirteen patients (35.1%) were released without any improvement, 15 patients (40.5%) were released with the registered improvement by 1 grade of the Frankel scale, 6 patients (16.2%) with improvement by 2 grade of the scale, and 1 patient (2.7%) with improvement by 3 grade. Two patients (5.4%) were moved from group B to A due to negative dynamics. In group II, 68 patients (39.5%) were treated nonsurgically and 104 (60.5%) patients were operated on. Relapse was recorded in 8.7% of patients (n = 17). The statistics of lethal cases within the hospital is 3.8% (n = 8); in group I, it is 8.1% (n = 3). Conclusion: In the past 3 years, there has been a significant increase in the number of patients with PVO by 2.3 times. The PVO affection of the cervical spine, as well as infection by S aureus, increase the risks of neurological damage. Active surgical intrusion in the cases of complicated forms of spinal osteomyelitis allows partial or full regress of neurological deficit in 62.8% cases.
P420: Concertina Collapse of Vertebrae During Spinal Tuberculosis Medical and Surgical Management of 3 Cases
Hassen Makhlouf1, Mehdi Meddeb1, Ahmed Jabeur1, Ahmed Mzid1, Bouzid Lanouar1, and Mondher Mestiri1
1Kassab Institute, Manouba, Tunisia
Introduction: Spinal tuberculosis is a frequently encountered extrapulmonary form of the disease. It affects mostly young adults. The upper lumbar and lower thoracic spine are most frequently involved sites. More than one vertebra is typically affected, and the vertebral body is more frequently affected than the posterior arch. In this report, we describe 3 cases of different locations of spinal tuberculosis with collapse of the spinal elements. Cases Presentation: Three patients of spinal tuberculosis were treated at our institute, a man and 2 women. The first patient was 42 years old, and she had persistent back pain (lower thoracic spine) and fever with incomplete neurologic deficit. Magnetic resonance imaging (MRI) found a spondylitis of the T10-T11-T12 levels, a large epidural collection severely compressing the cord, with a collapse of D11 vertebral body. A CT (computed tomography)–guided percutaneous biopsy confirmed the diagnosis of tuberculous spondylitis. The patient had anterior combined posterior surgery: debridement, pedicle screw implantation in D7/D8/D9/L1/L2/L3, laminectomy of D10-D11-D12, D10-D11 and D11-D12 discectomy, corporectomy of D11 vertebral body, and bone grafting in the defect area. She had antituberculous combination therapy, and her symptoms had improved much after the operation. The second patient was 62 years old, she had the same symptoms but in the upper thoracic spine. MRI concluded to a spondylitis of T1, T2, and T3 with total destruction of T2 body and epidural abscess. The anatomopathological examination retained the diagnosis of tuberculosis. She had 1-stage posterior surgery: debridement, posterior fixation from C6 to T5, laminectomy, corporectomy of D2, and bone grafting. The third patient was a 66-year-old man with tuberculous spondylitis of L4-L5 and collapse of the whole vertebral body of L5. He had only a posterior surgical approach with transpedicular screws in L4 and S1, decompression, focal debridement, and interbody fusion. We found that the correction of kyphosis was remarkable without the need of an anterior surgery. Conclusion: Early diagnosis and localizing the site of disease is important for deciding treatment strategies and to prevent permanent neurological disabilities. Medical treatment with a good immobilization is generally effective, but surgical intervention is still necessary in advanced cases. A characteristic sign of tuberculosis is a “concertina collapse” of a vertebrae weakened by the ingrowth of granulation tissue, often resulting in neurological compromise, severe kyphosis, and spinal instability. In this case, a surgical decompression with correction of the kyphosis are the main stays of treatment.
P421: Minimally Invasive Surgery for the Treatment of Thoracolumbar Pyogenic Spondylodiscitis: Indications and Outcomes
Enrico Pola1, Luigi Aurelio Nasto1, Virginia Pambianco1, Valerio Cipolloni1, Luca Piccone1, Francesco Ciro Tamburrelli1, Roberto Cauda1, and Massimo Fantoni1
1Catholic University of the Sacred Heart, Milan, Italy
Introduction: Pyogenic spondylodiscitis (PS) is a nonspecific infection affecting intervertebral discs and adjacent vertebral bodies. Once considered a rare condition in developed countries, the incidence of PS has been alarmingly increasing still representing a challenge for clinicians and orthopedic surgeons. New minimally invasive techniques have been proposed, but the proper indications of these different approaches remain controversial. Aim of this study was to describe the available minimally invasive surgical techniques and to evaluate their proper indications through a review of recent literature. Material and Methods: More than 30 articles of recent scientific literature have been reviewed and analyzed. Studies were searched through PubMed database using the key words: spondylodiscitis, minimally invasive, and surgical treatment. The most interesting and valid techniques and results have been reported. Despite the exclusion of case reports, all the available studies have been conducted on small groups of patients. Indications for each technique have been reported according to a clinical-radiological classification of PS. Results: Six of the most widely used minimally invasive surgical techniques have been described. High success rates have been reported in terms of preventing the progression of spondylodiscitis into more destructive forms, reduction of time and operative hospitalization, faster pain relief, early mobilization, and achievement of microbiological diagnosis. Conclusion: The role of minimally invasive surgery in the treatment of PS is rapidly expanding. Reducing surgery-related morbidity in these frail patients is possible and often necessary. However, while more and more new techniques are being proposed, still few clinical data are available. Clinical comparison studies with open traditional surgery should be encouraged, and more attention should be paid to long-term outcomes. For the present, the indications for minimally invasive procedures should therefore be evaluated on a case by case basis and on clinical and radiological fiundings.
MEDICAL ECONOMICS
P422: A 5-Year Review of Hospital Costs and Reimbursement in the Surgical Management of Degenerative Spondylolisthesis
Keith Lyons1, Christian Klare1, Samuel Kunkel1, Jason Lemire1, Mike Bao1, Adam Pearson1, and William Abdu1
1Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA
Introduction: Surgical management of degenerative spondylolisthesis (DS) with spinal stenosis (SS) remains controversial, as studies reveal that fusion technique may not affect outcomes. Various considerations may drive the decision to which type of fusion to use, including patient, surgeon, and economic factors. This study was designed to characterize different charges, expenses, reimbursement, and hospital margins with noninstrumented fusion in situ (PLF), posterolateral fusion with pedicle screws (PPS), and PPS with interbody device (PLIF). Materials and Methods: A retrospective chart review was performed from 2010 to 2014 based on ICD-9 (International Classification of Diseases, Ninth Revision) diagnoses of DS with SS in patients undergoing single-level fusions. All service and procedural charges (what was billed to insurance), expenses (direct costs incurred by the hospital), hospital reimbursement, and hospital margins were obtained through the financial audit for each surgery and hospital stay. A multivariate linear regression model was used to compare patient demographics, charges, expenses, and so on. A 1-way analysis of variance (ANOVA) with Tukey post hoc analysis was used to analyze different reimbursements and margins based on insurance types. Results: A total of 233 patients met inclusion criteria for the study. There were no significant differences with BMI (body mass index), ASA (American Society of Anesthesiologists) class, length of stay, or gender distribution. Both types of instrumented fusions had longer operating room times and estimated blood loss (P < .001). The overall mean charges and expenses for PLF were significantly less compared with both types of instrumented fusions (P < .0001). The mean total charges to insurance companies for PLF, PPS, and PLIF were $74 650, $93 371, and $102 766, respectively. The mean total expenses for the hospital for PLF, PPS, and PLIF were $13 248, $18 104, and $19 740, respectively. Medicare and private insurance were the most common insurance types; Medicare and private insurance mean reimbursements for PLF were $36 903 and $47 086, for PPS $37 450 and $53 851, and for PLIF $40 171 and $51 640, respectively. Hospital margins for PPS and PLIF in Medicaid patients were negative (−$3702 and −$6456). Hospital margins were largest for both worker’s compensation and private insurance patients in all fusion groups. Hospital margins with Medicare for PLF, PPS, and PLIF were $24 347, $19 205, and $23 046, respectively. Hospital margins for private insurance for PLF, PPS, and PLIF were $37 569, $36 834, and $33 134, respectively. Discussion: As more instrumentation is used, the more it costs both the hospital (expenses) and the insurance company (charges). Hospital margins varied depending on both fusion method and insurance type. While charges, expenses, and reimbursement tend to increase with instrumentation, hospital margins did not correspondingly. This study highlights the importance in better aligning the economic interests of all parties involved (patient, surgeon, hospital, insurance, etc) in order to help control spending and transition to a more cost-effective system.
P423: The Effects of Older Age on the Costs of the Initial Spine Care of Individuals With Acute Spine Trauma
Julio Furlan1,2, Michael Fehlings2,3, and B. Catharine Craven1,2
1Toronto Rehabilitation Institute, University Health Network, Toronto, Ontario, Canada
2University of Toronto, Toronto, Ontario, Canada
3Toronto Western Hospital, University Health Network, Ontario, Canada
Introduction: Aging of the population has prompted an escalation of service utilization and costs in many jurisdictions including North America. Yet, the economic impact of the caring for the elderly with spine trauma remains incompletely understood. This study was undertaken to examine the potential effects of age on the service utilization and costs of the management of patients with acute spine trauma (AST). Material and Methods: This retrospective cohort study included consecutive patients with AST admitted to an acute spine care unit of a quaternary university hospital between February 2002 and September 2007. The study population was grouped into elderly (age of 65 years or older at the time of trauma) and younger individuals. All costing data were converted and updated to US dollars. Results: There were 55 women and 91 men with AST (age range from 16 to 92 years, mean age of 49.9 years) of whom 37 were elderly. Elderly individuals with AST had a significantly longer stay in the acute spine trauma center (10.5 ± 1.3 days vs 22.1 ± 6.2 days, P < .01) and greater total hospital costs than younger individuals with AST (US$19 338 ± 4892 vs US13 775 ± 1344; P = .04). However, elderly people with AST had significantly lower per diem total costs, lower per diem fixed costs, lower per diem direct costs, and lower per diem indirect costs than younger individuals with AST. While elderly people with AST had significantly lower per diem fixed costs than younger individuals with AST (P < .01), there were no significant differences between the groups regarding their per diem variable costs (P = .28). Using multivariate regression analysis, higher total hospital costs were significantly correlated to longer stay in the acute spine trauma center, complete traumatic SCI (spinal cord injury), and need for mechanical ventilation (P < .05). Further multivariate regression analysis revealed a significant interaction between longer hospital stay and need for mechanical ventilation (P < .01); there was no significant interaction between length of hospital stay and severity of AST (P > .14). In another multivariate regression analysis, higher per diem total costs were significantly associated with shorter stay in the acute spine trauma center and lumbosacral AST (P < .05). Further multivariate regression analysis revealed that there was no significant interaction between length of stay and level of AST (P > .39). Finally, elderly people with AST were statistically comparable to their younger counterparts regarding their proportions of the hospital services utilized during admission for management of AST (P = 1.00). The top 10 most costly services utilized during admission were, in the decreasing order, intensive care unit, ward, operating room, pharmacy, respiratory therapy, imaging, laboratory, occupational therapy, emergency department, and social work. Conclusion: Given the escalating demand for surgical and nonsurgical spine treatment in the age of aging population, the results of this study timely underline key aspects the economic impact of the spine care of the elderly. Further investigations are needed to fulfill significant knowledge gaps on the economics of caring for elderly with AST.
P424: Health Economics in Surgical Interventions for Acute Spine Trauma: A Scoping Review
Julio Furlan1,2, Brian Chan2,3, and B. Catharine Craven1,2
1Toronto Rehabilitation Institute, University Health, Toronto, Ontario, Canada
2University of Toronto, Toronto, Ontario, Canada
3Lyndhurst Centre, Toronto Rehabilitation Institute, University Health Network, Toronto, Canada
Introduction: Acute spine trauma (AST) has a relatively low incidence; however, it often results in substantial individual impairments and societal economic burden resulting from the associated disability. Given the key role of neurosurgeons in the decision-making regarding operative management of individuals with AST, we performed a systematic search with scoping synthesis relevant literature to review current knowledge regarding the economic burden of AST. Material and Methods: This systematic review with scoping synthesis original articles reporting cost-effectiveness, cost-utility, cost-benefit, cost-minimization, cost-comparison, and economic analyses related to surgical management of AST, whereby AST is defined as trauma to the spine that may result in spinal cord injury with motor, sensory, and/or autonomic impairment. The initial literature search was carried out using MEDLINE, EMBASE, CINAHL, CCTR, and PubMed. All original articles captured in the literature search published from 1946 to September 27, 2017, were included. Search terms used were the following: (cost analysis, cost effectiveness, cost benefit, economic evaluation or economic impact) AND (spine or spinal cord) AND (surgery or surgical). Results: The literature search captured 5770 titles of which 11 original studies met the inclusion/exclusion criteria. There were 4 cost-utility analyses, 5 cost analyses that compared the cost of intervention with a comparator, and 2 studies examining direct costs without a comparator. There are few potentially cost-saving strategies in the neurosurgical management of individuals with AST including the following: (1) early surgical spinal cord decompression for acute traumatic cervical spinal cord injury (or traumatic thoracolumbar fractures, traumatic cervical fractures); (2) surgical treatment of the elderly with type II odontoid fractures is more costly but more effective than the nonoperative approach among individuals with age at AST between 65 and 84 years; (3) surgical treatment of traumatic thoracolumbar spine fractures is implicated in greater direct costs but lower general practitioner visit costs, private expenditures, and absenteeism costs than nonsurgical management; and (4) removal of pedicle screws from 1 to 2 years after a posterior instrumented fusion for individuals with thoracolumbar burst fractures is more cost-effective than retaining the pedicle screws. Conclusions: This scoping synthesis underscores a number of potentially cost-saving opportunities for neurosurgeons when managing patients with AST. There are significant knowledge gaps regarding the potential economic impact of therapeutic choices for AST that are commonly used by neurosurgeons.
P425: A Cost-Utility Analysis of Dynesys Dynamic Stabilization Versus Instrumented Fusion for the Treatment of Degenerative Lumbar Spine Diseases
Kan Liu1, Wei Sun2, Qiang Lu3, Jiying Chen4, and Jiaguang Tang5
1Beijing University of Chinese Medicine Third Affiliated Hospital, Beijing, China
2Nanyuan Hospital, Beijing, China
3University of Southampton, Southampton, UK
4General Hospital of Chinese People’s Liberation Army, Beijing, China
5First Affiliated Hospital of Chinese PLA General Hospital, Beijing, China
Introduction: Symptomatic chronic low back and leg pain resulting from lumbar spine degenerative disorders is highly prevalent in China, and for some patients, surgery is the final option for improvement. Several techniques for spinal nonfusion have been introduced to reduce the side effects of fusion methods and hasten postoperative recovery. In this study, the authors have evaluated the cost-effectiveness of Dynesys posterior dynamic stabilization system (DY) compared with lumbar fusion techniques in the treatment of single-level degenerative lumbar spinal conditions. Materials And Methods: A total of 221 patients undergoing single-level elective primary surgery for degenerative lumbar pathology were included. Two-year postoperative health outcomes of the visual analogue scale (VAS) for back and leg pain, Oswestry Disability Index (ODI), 36-Item Short Form Health Survey (SF-36), and EuroQol-5 Dimensions (EQ-5D) questionnaires were recorded. Two-year back-related medical resource use, missed work, and health-state values (quality-adjusted life-year [QALY]) were assessed. Cost-effectiveness was determined by the incremental cost per QALY gained. Results: At each follow-up point, both cohorts were associated with significant improvements in VAS scores, ODI, SF-36 scores, and EQ-5D QALY scores, which persisted at the 2-year evaluation. The 2-year total mean cost per patient were significantly lower for Dynesys system ($20 150) compared with fusion techniques ($25 581, $27 862, and $27 314, respectively; P < .001). Using EQ-5D, the mean cumulative 2-year QALYs gained were statistically equivalent between the 4 groups (0.28, 0.27, 0.30, and 0.30 units, respectively; P = .74). Results indicate that patients implanted with the DY system derive lower total costs and more utility, on average, than those treated with fusion. Conclusions: The Dynesys dynamic stabilization system is cost effective compared with instrumented lumbar fusion for treatment of single-level degenerative lumbar disorders. It is not possible to state whether DY or lumbar fusion is more cost-effective after 2 years.
P426: Economic Performance of Oblique Lateral Lumbar Interbody Fusion With a Focus on Hospital Throughput Efficiency
Hamid Abbasi1
1Tristate Brain & Spine Institute, Alexandria, MN, USA
Introduction: Oblique lateral lumbar interbody fusion (OLLIF) is a minimally invasive lumbar surgery. Differences in resource consumption between open spinal surgeries, transforaminal lumbar interbody fusions (TLIF), and OLLIF are not documented. Material and Methods: We monetize quantifiable differences in resource utilization between the 2 procedures. A retrospective review of 124 surgeries was performed (OLLIF = 69, TLIF = 55). Standard conversion factors were used and values reported based on the levels (1-4) addressed at surgery. Results: One-level surgery time (OLLIF 62.9 vs TLIF 134.9 minutes) and surgical expense (OLLIF $5253 vs TLIF $11 264) were reduced in the OLLIF population. Inpatient costs (OLLIF $5712 vs TLIF $9271) and length of stay (LOS) were also reduced (OLLIF 2.6 vs TLIF 4.2 days). Conclusion: Per case, reduced resource consumption suggests lower total hospital costs. Reduced surgical time and LOS can result in greater patient throughput per operating room and patient bed for OLLIF patients in hospitals that have resourced constrained environments.
P427: A Validated Preoperative Score for Predicting 30-Day Readmission After 1- to 2-Level Elective Posterior Lumbar Fusion
Deeptee Jain1, Paramjit Singh2, Mayur Kardile1, and Sigurd Berven1
1New York University Medical Center, New York, NY, USA
2University of California, San Francisco, CA, USA
Background: Posterior lumbar fusion is one of the most commonly performed procedures in the United States. Readmission rates are an important metric of quality of care. The purpose of this study was to develop a model to predict 30-day readmission rates in elective 1- to 2-level posterior lumbar fusion patients. Methods: This was a case-control study. Patients who underwent elective 1- to 2-level posterior lumbar spine fusion in the State Inpatient Database were identified. Data were queried for 30-day readmission, as well as demographic and surgical data. Patients were randomly assigned to either the derivation or validation cohort. A stepwise multivariate analysis was conducted on the derivation cohort to predict 30-day readmission. Next, the readmission after posterior spinal fusion (RAPSF) score was created. Variables with odds ratio (OR) >1.1 and P < .01 on multivariate analysis were included; and the value assigned to each variable was based on the OR and calibrated to 100. Linear regression was performed between readmission rate and RAPSF score to test its accuracy both in the derivation and validation cohorts. Results: There were 92 262 and 90 257 patients in the derivation and validation cohorts. Thirty-day readmission rates were 10.9% and 11.1%, respectively. The RAPSF consisted of (point value in parentheses): age (50-59: 4, 60-69: 4, 70-79:6, >90: 8), gender (female: 3), race (Hispanic: 4, black: 5), insurance (Medicare: 4, Medicaid: 5, other noncommercial: 3), anterior approach (4), cerebrovascular disease (3), chronic pulmonary disease (3), congestive heart failure (4), diabetes without chronic complications (4), diabetes with chronic complication (4), hemiplegia/paraplegia (7), rheumatic disease (3), drug abuse (4), electrolyte disorder (4), osteoporosis (3), depression (3), obesity (4), and morbid obesity (5). Linear regression between readmission rate and RAPSF fit the derivation cohort with an adjusted r 2 of 0.92 and a coefficient of 0.011 (P < .001), and the validation cohort with an adjusted r 2 of 0.94 and a coefficient of 0.011 (P < .001). Conclusion: We developed an easy-to-use tool, the RAPSF, to accurately predict readmission rates in patients undergoing elective 1- to 2-level posterior lumbar fusion. The RAPSF may be useful to empower informed choice regarding the risks of surgery and to guide an evidence-based approach to preoperative optimization and risk adjustment within alternative payment models for elective spine surgery.
P428: Machine Learning For Predictive Modeling of 90-Day Readmission, Major Medical Complication, and Discharge to a Facility in Patients Undergoing Surgery for Adult Spinal Deformity: Logistic Regression Versus Random Forest
Deeptee Jain1, Wesley Durand2, Thomas Peterson3, and Sigurd Berven3
1New York University Medical Center, New York, NY, USA
2Brown University, Providence, RI, USA
3University of California, San Francisco, CA, USA
Background: Surgery for adult spinal deformity has been proven to be effective for treating spine-related disability; however, it is associated with high complication rates and readmission rates. The literature examining predictive models for outcomes after adult spinal deformity surgery is limited. Methods: This was a retrospective case-control study. Patients who underwent posterior spinal fusion for adult spinal deformity, as defined as 3 or more levels fused, were identified in the State Inpatient Database using ICD-9 (International Classification of Diseases, Ninth Revision) codes. Patients who underwent surgery for nonelective indications were excluded. Data were queried for discharge to facility (DTF), 90-day readmission, and 90-day medical complications including death, deep vein thrombosis, pulmonary embolism, respiratory failure, myocardial infarction, and cerebrovascular accident, as well as demographic data, comorbid data, and surgical data. Data were partitioned in training and testing sets. Both stepwise multivariate logistic regression analyses and random forest analyses were performed on the training sets. Models were then applied to the testing sets to generate area under the curve (AUCs). AUCs between logistic regression and random forest were compared using the method by DeLong et al. Results: There were 40 822 patients who met inclusion/exclusion criteria. After patients with missing data were excluded, there were 37 852 patients. The DTF rate was 35.4%. The 90-day readmission rate was 19.0%. The 90-day medical complication rate was 13.0%. For DTF, the logistic regression model AUC was 0.77, compared with 0.75 for the random forest model (P < .01). For 90-day readmission, AUC for the logistic regression model was 0.65, compared with 0.63 for random forest (P < .01). For 90-day medical complications, the AUC for logistic regression was 0.70, compared with 0.69 for random forest (P < .01). Conclusion: This study created the most comprehensive models to date to predict discharge to facility, 90-day readmissions, and 90-day medical complications after undergoing surgery for adult spinal deformity. This information can be used to guide decision making between the surgeon and patient, as well as provide information for structuring value-based payment models.
P429: Impact of Telemedicine Triage on Efficiency and Cost-Effectiveness in Spinal Care
Shari Cui1, Leslie Crossley2, Cara Sedney1, John France1, Sanford Emery1, and Scott Daffner1
1West Virginia University, Morgantown, WV, USA
2West Virginia University Spine Center, Morgantown, WV, USA
Introduction: Patients with nonsurgical spine pathology who are initially seen by a surgeon are often referred to nonoperative providers for ongoing care. This results in patients “wasting a visit” to a surgeon, when they should have been seen by another provider, leading to additional clinic visits, unnecessary health care costs, and wasted time off work. Providers and health systems must optimize efficient patient triage while improving access to appropriate specialists, particularly when serving large populations where geographic or economic factors already challenge access to care. We have previously shown that use of a telemedicine/electronic triage system improves waiting time for appointments as well as both patient and referring provider satisfaction. The purpose of this study was to evaluate the impact of a telemedicine/electronic triage system on quantitative and qualitative measures of cost savings and efficiency. Material and Methods: All new referrals to our spine center from 2011 through 2014 were included. Once referred, an intake nurse contacts patients to collect information regarding history, symptoms, prior treatment, imaging, and test results. The data are recorded within our electronic triage system and placed into a queue to be reviewed by a spine surgeon, who then recommends either referral to a surgical provider, nonoperative spine provider, other provider, and/or requests additional testing. This triage database was mined for data from intake until triage completion. Hospital electronic medical records (EMR) were then reviewed for data on clinic visits, tests ordered, follow-up appointments, and presence of surgical encounters. Variables included time from intake to appointment, rate of referral to surgeons versus nonoperative providers, and additional testing required. Cost savings was estimated by calculating number of “trips saved” (ie, avoidance of unnecessary office visits) and extrapolating the cost of visit and estimated mileage from the patient’s home. Results: A total of 10 832 records (10 271 patients) were triaged by a spine surgeon from 2011 to 2014. Average time from referral to surgeon review was 11 days. After electronic triage, 4446 (43%) patients were offered an appointment with a spine surgeon, 4959 (48%) were directed to a nonsurgical provider, and 6723 (65%) received recommendations for additional testing or treatment. Referral to our in-network nonoperative spine providers generated 3718 ambulatory visits in 2444 patients. This resulted in estimated savings of $793 835 ($649 572 for unnecessary appointment with a surgeon and $144 263 in travel costs), or $325 per patient ($266 for clinic visit, $59 for travel). This excludes those patients who opted for out-of-network/community nonoperative providers, for whom data were unavailable. Among the 4446 patients directed to surgical providers, 3528 arrived within 6 months of their most recent telemedicine review (average appointment time was 44 days after referral). Once seen, 2331 (66%) did not require any further workup (ie, complete imaging, testing, treatment required for surgical assessment at initial visit). Among the 3528 patients, 745 (26%) patients underwent spine surgery within 2 years of the index visit. Conclusion: We found that the use of telemedicine/electronic triage for spine patients resulted in improved access to appropriate care, substantial cost savings, and more efficient use of surgeon time on potentially surgical patients.
P430: Online Ratings of Spinal Deformity Surgeons: Analysis of 634 Surgeons
Giresse Melone1, Cesar Hernandez2, Emmanuel Menga2, Rishi Balkissoon2, Ximing Liu3, Jun Zhang4, and Addisu Mesfin2
1University of Texas Medical Branch, Galveston, TX, USA
2University of Rochester, Rochester, NY, USA
3Wuhan General Hospital of the Chinese People’s Liberation Army, Wuhan, Hubei Province, China
4Zhejiang Provincial People’s Hospital, Hangzhou, Zhejiang Province, China
Introduction: Physician review websites (PRW) continue to be an emerging trend in the United States, across all specialties. Previous literature with smaller sample sizes revealed that most spine surgeons are rated on at least one PRW. To date, the online ratings of spinal deformity surgeons have not been evaluated. The authors aim to evaluate the online ratings of spine deformity surgeons and variables that may affect online ratings. Material and Methods: A review of the 2017 Scoliosis Research Society (SRS) Fellowship directory for active fellows and candidate members yielded 634 active members. Online ratings from “Healthgrades,” “Vitals,” “RateMDs,” “WebMD,” and “Yelp” were all recorded and scaled from 0 to 100. Using SPSS, 1-way analysis of variance was used to compare differences between multiple groups. A t test was used to compare differences between 2 groups. Significance was set at P < .05. Results: Nearly all surgeons, 98.7% were rated on at least one PRW. Surgeons in academic practice had significantly higher ratings than those in private practice (84.3 vs 79.7; P = .00005). Hospital-employed surgeons had significantly higher ratings than those in private practice (85.1 vs 79.7; P = .0001). Surgeons in practice for 0 to 5 years had significantly higher ratings than those practicing for 11 to20 and ≥21 years, respectively (91.8 vs 83.6, P = .001, and 91.8 vs 81.4, P = .001). No significant differences in ratings with regard to sex (83.3 male vs 80.1 female; P = .368), specialty (83 orthopedics vs 85.1 neurosurgery; P = .199), geographic location (P = .917), or fellowship training (84.3 pediatrics vs 82.5 spine; P = .065). Conclusion: Spine deformity surgeons in practice between 0 and 10 years have higher ratings than more experienced surgeons (practice 21+ years). Academic- and hospital-employed SRS surgeons had higher ratings than those in private practice. Nearly all, 98.7%, SRS surgeons were rated on at least one PRW.
P431: Lumbar Total Disc Arthroplasty at Ambulatory Surgery Center: A Safe Alternative to Hospital Admission?
Benjamin Dorenkamp1 and Michael Janssen2
1McLaren Greater Lansing, Lansing, MI, USA
2Center for Spine and Orthopedics, Thornton, CO, USA
Introduction: Modern health care is under constant pressure to improve patient satisfaction and lower cost, while providing the most effective and safe services available. To achieve this, certain surgeries have transferred out of the hospital and into ambulatory surgery centers (ASC). Wohns et al published an article in 2010 showing the difference in cost of a 1-level cervical disc arthroplasty is $11 144.83 in the ASC compared with $68 000 in the hospital setting. They also detailed in their study that they had no transfers to a hospital, no postoperative emergency room (ER) visits, and no late hospitalizations. While there is significant literature regarding anterior and posterior cervical spine surgery and posterior lumbar surgery, there is little to no literature discussing anterior lumbar surgery in the ambulatory setting. We present 50 patients who had a lumbar total disc arthroplasty (lumbar TDA) between 2007 and 2018 with a review of perioperative and immediate postoperative complications. Material and Methods: Fifty consecutive patients who underwent a lumbar TDA at a single ASC were reviewed. Surgery was performed by orthopedic spine surgeons and a general surgeon with significant experience in the anterior retroperitoneal approach to lumbar spine. Surgeries were completed at the ASC and were all transferred from post–anesthesia care unit (PACU) to an attached convalescence care center (CCC), which allows up to 3 days of observation. Patients who had either a 1-level or 2-level lumbar TDA between 2007 and 2018 were included in the retrospective study. Data consisting of demographics, ASA (American Society of Anesthesiologists), length of stay, estimated blood loss (EBL), cell saver volume, transfusion, perioperative, and postoperative complications were recorded. Results: Records of 50 patients were reviewed. The mean age was 40.86 ± 9.45, 48 (96%) patients had a 1-level lumbar TDA, 1 (2%) patient had a 2-level lumbar TDA, 1 (2%) patient had a lumbar TDA at L4/5 and an anterior lumbar interbody fusion at L5/S1. There were 0 mortalities, and 0 patients had perioperative complications. Zero patients received allogenic blood transfusion, 4 (8%) had an autologous transfusion (2 patients receiving approximately 400 mL of autologous blood and 2 patients receiving approximately 200 mL of autologous blood). One (2%) patient had respiratory failure in PACU due to narcotics and was successfully rescued with Narcan. Zero patients were transferred from the ASC or the CCC to the ER or hospital. Fifty (100%) of patients were discharged home in stable condition. Average length of stay was 30 ± 12 hours with a maximum length of stay of 75 hours and a minimum length of stay of 17 hours. Conclusion: This review of 50 patients that had lumbar TDA in an ASC with admission to attached CCC showed that in the hands of an experienced spine and general surgeon, lumbar TDA can be safely performed outside the hospital in the ASC with subsequent recovery in an associated CCC. This review has shown that there is a low rate of complications both perioperatively and postoperatively. This provides a safe and cost-effective alternative to the hospital setting for lumbar TDA.
P432: Virtual Scoliosis Surveillance Clinic: The Alder Hey Experience
Ignatius Liew1, Lisa Andre1, Samir Abdalla1, and Neil Davidson1
1Alder hey Children’s Hospital, Liverpool, UK
Introduction: At Alder Hey Children’s Hospital, surveillance of patients with scoliosis is enhanced by the EOS imaging system. Due to low radiation doses (1/50th of traditional spinal radiographs), we were able to enhance scoliosis surveillance and reduce impact on outpatient setting, making the process more dynamic allowing early identification of patients at risk of curve progression. Patients are virtually followed-up with X-ray radiographs obtained, reviewed, and a decision of outcome/followed-up/surgical intervention. We aim to describe the Alder Hey experience in virtual scoliosis surveillance clinic (VSSC). Material and Methods: All patients reviewed in VSSC from June 2017 to May 2018 were prospectively reviewed. Cobb angle and Risser sign were measured on whole spine EOS radiographs. Patients were stratified based on outcome —discharge, surveillance, bracing, surveillance (on waiting list), and surgical intervention. Results: A total of 450 radiographs were reviewed, which includes 296 patients (68% female) with mean age of 13 years (range = 3-18). Twenty-two patients were identified to require earlier intervention and prioritization during their 4-month surveillance radiographs with an average Cobb angle of 76 with mean increase from 66, and mean of 65 days to surgery from most recent surveillance films (P = .0172). Twenty percent of patients were discharged either from scoliosis service, transitioned to adult sector or through nurse specialist clinic from final radiographs with no curve progression with Risser sign 4 to 5. Sixty percent of patients continued to be under surveillance, of which 18% were on the waiting list for spinal instrumentation and 27% on spinal bracing. Twenty-three percent of patients were brought to a consultant clinic for further evaluation. Conclusion: Virtual scoliosis surveillance is a novel way to monitor patients’ scoliosis progression, during observation, brace treatment, or while on the waiting list. It offers easy access and review allowing changes in management, early review, and prioritization to prevent more extension multilevel surgery, especially in the climate of increasing waiting list.
P433: The Need to Improve Prediction of Responders and Nonresponders in Elective Spine, Hip, and Knee Surgery: A Health-Economic Argument
Raja Rampersaud1, Kala Sundararajan1, Anthony V. Perruccio1, Rajiv Gandhi1, Rod Davey1, Khalid Syed1, Christian Veillette1, and Nizar Mahomed1
1Krembil Research Institute, University Health Network, Toronto, Ontario, Canada
Introduction: Surgeries for joint/spine disorders are among the most frequently performed elective procedures, with growing global annual volumes. Over 1.6 million joint replacement and spinal fusion surgeries were performed in the United States in 2012, and 120 000 were performed in Canada in 2014, with corresponding hospital costs of US$32 billion and CAN$1 billion, respectively. Despite these substantial costs, 20% to 25% of these procedures result in poor patient outcomes. This suggests that approximately US$6.4 billion and CAN$200 million are spent each year on elective joint/spine procedures for people who do not benefit from them. The purpose of this study was to evaluate the 1-year cost-utility of elective joint replacement and spinal decompression with or without fusion with regard to patient-reported surgical outcome. Material and Methods: Incremental cost-utility analysis from the hospital perspective, based on a single-center prospective longitudinal cohort study. Hospital case cost data were obtained for a cohort of 403 elective surgical cases in 2011 to 2012, comprising inpatient spine (n = 48), outpatient spine (n = 39), inpatient hip (n = 150), and inpatient knee (n = 166) procedures. Costs were adjusted to 2016 Canadian dollars. Patients completed the Short Form (SF)-12/36 health status survey before and 1 year after surgery. Clinically important improvement was defined as a 4.6-point improvement in SF-12/36 Physical Component Summary score 1 year post surgery. This criterion was used to categorize patients as “responders” and “nonresponders.” One year incremental cost-utility ratios (ICURs) were calculated for each group as cost per quality-adjusted life year (QALY) gained following surgery. QALYs were determined using SF-6D utility scores before and 1 year after surgery. Results: The cohort was 47% female and had mean age 64 years. Overall, 71% of cases were categorized as responders 1 year after surgery: 62% of spine cases, 85% of hip cases, and 63% of knee cases. In the combined group, mean per procedure hospital cost was $10 937 (SD = $6657) and patients gained 0.12 QALY (SD = 0.14) in the year after surgery, corresponding to $89 464 per QALY gained in the year after surgery. Patients categorized as nonresponders had higher mean case cost: $12 447 versus $10 319 for responders (P = .02). Nonresponders also had substantially smaller QALY gains at 1 year, gaining 0.03 QALY versus 0.13 QALY in responders (P < .01). The resulting 1 year ICURs varied greatly with responder status: $64 015/QALY for responder cases compared with $460 399/QALY for nonresponder cases. Estimates also varied by operative site: responder/nonresponder ICURs were $115 694/$1 574 451 for inpatient spine cases; $23 599/$139 362 for outpatient spine cases; $57 975/$118 068 for hip cases; and $77 761/$1 121 714 for knee cases. Conclusion: Considering the ICUR for all patients, elective joint replacement and spine surgery meet an acceptable threshold for cost-effectiveness. However, the cost-utility estimate for the 29% of patients who do not achieve clinically important change in physical status demonstrates that surgery in this subset of patients is grossly cost-ineffective. This is particularly the case for knee replacement and spinal fusion. These findings provide a strong economic argument for further research in surgical prognostication, and development of real-world predictive analytics tools for joint replacement and spinal surgery.
P434: Length of Stay After Lumbar Spine Surgery in a Private Hospital After Early Mobilization
Kathryn Ramshaw1 and Palaniappan Lakshmanan1
1City Hospitals Sunderland, East Boldon, UK
Introduction: Lumbar fusion is a common operation performed to help relieve symptoms of back and leg pain associated with degenerative disc disease. The aim of this study is to look at length of stay after lumbar spine fusion in a private hospital, following early mobilization. Materials and Methods: Between January 2014 and August 2018, 355 patients had lumbar spine instrumented fusion with decompression at a private hospital. All patients received early mobilization through the accelerated rehabilitation program at the hospital, mobilizing within 3 to 12 hours post operation. Data include 1-level to 3-level surgeries and revision surgeries. Data were prospectively added to a local database held at the hospital with length of stay, readmission, and reason for readmission documented in Datex for each patient. The Charlson Index was used to assess the significance of comorbidities on the data. Readmission was analyzed as any unplanned readmission <31days of discharge. Length of stay was calculated as standard deviation of the mean. Results: Seventy percent (248) of patients stayed for <24 hours; 21% (73) of patients stayed for 24 to 48 hours; 5% (17) of patients stayed for 3 days; 3% (12) of patients stayed for 4 days; 0.5% (2) of patients stayed for 5 and 6 days, respectively; less than 0.3% (1) of patients stayed for 7 days. The average length of stay: 1.47 ± 0.9 days. Three percent (11) of patients had unplanned readmissions within 31 days of discharge. Readmission reasons varied: pain 1.1% (4); wound related 0.8% (3); urinary retention 0.5% (2); generally unwell 0.2% (1); confusion 0.2% (1). One patient required revision surgery within 30 days due to hematoma. The Charlson Index demonstrated that there was no significant difference between comorbidities and length of private hospital stay after lumbar fusion. Conclusion: Length of stay is most commonly <24 hours following lumbar spine fusion, followed by a 24 to 48 hours stay, which is much less common. Comorbidities are not shown to affect length of stay, which can be due to the accelerated rehabilitation program in place in the private hospital, where patients are mobilized on the operative day between 3 and 12 hours post-surgery. The reduced length of stay in the hospital did not result in more late developing postoperative complications or readmission.
P435: Perioperative Adverse Events in Spine, Hip, and Knee Surgery: Impact on Hospital Cost and Length of Stay
Raja Rampersaud1,2, Kala Sundararajan1,2, Anthony V Perruccio1,2, Rajiv Gandhi1,2, Diana Adams1,2, Natasha Briggs1,2, Rod Davey1,2, Michael Fehlings1,2, Stephen Lewis1,2, Rosalie Magtoto1,2, Massicotte Eric1,2, Angela Sarro1,2, Khalid Syed1,2, Nizar Mahomed1,2, and Christian Veillette1,2
1Krembil Research Institute, Toronto, Ontario, Canada
2University Health Network, Toronto, Ontario, Canada
Introduction: Reducing the perioperative adverse event (AE) rate is a key goal for improving quality of care and reducing health system costs. Our objective was to use the OrthoSAVES (Orthopaedic Surgical AdVerse Event Severity) reporting tool to estimate the impact of AEs on hospital case cost and length of stay (LOS) in patients undergoing spine, hip, or knee procedures. Material and Methods: Prospective cohort study of consecutive orthopedic/spine surgeries at an academic hospital (2011-2012). A total of 2654 inpatient cases were included: 693 spine, 956 hip, and 1005 knee procedures. Perioperative AEs were recorded using the OrthoSAVES tool. Patient, admission, and surgery details were collected via chart review. Hospital costs for each admission were obtained from the hospital’s financial department and adjusted to 2017 equivalent values. Propensity score methodology was used to assess the independent impact of AEs on cost and length of stay. Multiple logistic regression stratified by operative site and sex was used to estimate each patient’s propensity of having an AE, considering age, overweight/obesity, comorbidities, diagnosis type, primary versus revision surgery, American Society of Anesthesiologists (ASA) score, and site-specific tertile of operating time. Each AE case was matched to 2 non-AE cases on site, sex, and propensity score. Results: The sample was 55% female and had average age 64; the majority of cases were elective (85%). A total of 785 cases (30%) suffered at least one AE: 33% of spine, 31% of hip, and 26% of knee cases. Eighty-one percent of cases with AEs had a minor event at worst; the most common events reported were postoperative urinary retention (11% of all cases), urinary tract infection (3%), and delirium (2%). The incremental cost and LOS attributable to AEs was $8817 CDN (95% confidence interval [CI] = 5768-11 866) and 4.1 days (95% CI = 3.0-5.1) per admission. This corresponded to a cumulative $6.9 million cost (15% of total cohort cost) and 3200 bed-days (18% of all bed-days) attributable to AEs overall. Estimates varied substantially by site: among spine admissions, AEs accounted for increases of $21 650 in case cost, and 7.7 days in length of stay versus $5829/3.9 days in hip admissions and $2190/1.3 days in knee admissions. AE severity also affected hospital impact, with major AEs accounting for cost/LOS increases of $31 437/10.9 days versus $4030/2.6 days for minor AEs. Cumulatively, major AEs accounted for 9.8% of costs and 8.9% of bed-days; minor AEs accounted for 5.5% of costs but 9.5% of bed-days. The impact of AEs also varied greatly by admission type. Among elective admissions, AEs accounted for $3657 higher cost (95% CI = 1909-5405) and 1.7 days longer LOS (95% CI = 1.0-2.3). In contrast, AEs in nonelective admissions accounted for $30 596 higher cost (95% CI = 16 923-44 269) and 14.2 days longer LOS (95% CI = 9.9-18.4). Conclusion: AEs in orthopedic surgery have a considerable impact on hospital resources, and their impact is significantly larger in spine cases and nonelective cases. Changes in clinical practice to mitigate perioperative AEs may result in significant savings to the health care system, while also improving quality of care and patient outcomes.
P436: Medical Malpractice Litigation in Pediatric Scoliosis: A Comprehensive, Nationwide Analysis for the Past 3 Decades
Assem Sultan1, Linsen Samuel1, Benjamin Yao1, Morad Chughtai1, Jacob Rabin1, Thomas Kuivila1, and Ryan Goodwin1
1Cleveland Clinic, Cleveland, OH, USA
Introduction: Recent trends have demonstrated a steady increase in the number of pediatric patients diagnosed with or undergoing surgical correction for scoliosis. With increased utilization of surgical options, complications may also increase, which may potentially increase the risk for malpractice litigation for the orthopedic surgeons and clinicians. Such litigation imposes both an economic and psychological toll on surgeons and the health care systems. Therefore, understanding the underlying causes and risk factors for litigation may help reduce these litigations, which will also reflect positively on the patients and their families. Previous studies have attempted to investigate causes and outcomes of malpractice litigation in different orthopedic specialties. However, to the best of authors’ knowledge, there has been no study that attempted to investigate causes and outcomes of malpractice litigations in pediatric scoliosis. Therefore, the purposes of this study was to (1) determine the most common reasons of medical malpractice litigation associated with pediatric scoliosis and (2) report on the most likely outcomes of these lawsuits through a comprehensive nationwide analysis of malpractice claims over the past 3 decades in the United States. Methods: The Westlaw legal research database (Thompson Reuters, New York, NY) and the Lexis Advance legal research database (LexisNexis Legal & Professional, New York, NY) were queried for jury verdicts and settlements completed between 1988 and 2018 for cases related to pediatric scoliosis in the United States. Cases were included when (1) plaintiff was diagnosed with scoliosis, (2) aged less than 25 years, and (3) the reason for the lawsuit was the plaintiff’s scoliosis. Cases of adult scoliosis and those with incomplete data were excluded. Causes of the lawsuit, patient characteristics, and demographics, state/outcome of verdict or settlement, and indemnity payments were noted. Results: A total of 72 records (47 females [65%], 24 males [35%]) with a mean age of 14 years (range = 2-25) were included in the final analysis. For all patients, massive neurological injury or paralysis was the leading cause for malpractice litigation (36%), followed by delay in diagnosis or surgery (35%), partial neurological injury (32%), and medical complications (15%). Most lawsuits were filed in the state of New York (23%), followed by Ohio (12.5%) and Illinois (8.3%). The jury ruled in the defense favor 43% of the time, and 30% in plaintiff’s favor. Parties settled in 27%. Therefore, a total of 40 cases (55.5%) resulted in a total payments of $263 529 569 with a mean of $2 778 703 per case ranging between $16 500 and $45 625 000 per case. Conclusion: Neurological complications whether partial or complete were the leading reasons of malpractice litigation in pediatric scoliosis patients. Notably, delay in diagnosis or treatment was the second most common cause for litigation. The single most likely outcome of these lawsuits was a jury verdict in favor of the clinician. However, the majority of cases resulted in some amount of payment, unlike what is currently reported in other orthopedic specialties. The total and mean amounts of indemnity payments were also among the highest reported among all other orthopedic specialties.
P437: History and Economics of Puerto Rico, and Its Implications to the Development and Advancement of Neurosurgery
Allyson Pagán Rodríguez1, Timothy O’Connor2, Asham Khan2, and Jeffrey Mullin2
1Ponce Health Sciences University, Ponce, Puerto Rico
2University at Buffalo, Buffalo, NY, USA
Introduction: The history and economics of neurosurgery in Puerto Rico have been immensely influenced by the political status of the Island since it passed from being a Spanish colony to an American colony, and finally an American Commonwealth, or Free Associated State, on July 25, 1952. Material and Methods: We researched and analyzed the writings of journalists, the personal experiences, and writings of residents, physicians, and other historians, as well as the numerous documents issued by both local and national governmental agencies, in order to shine a light on the most influential economic hardships, and hypothesize the etiology of the dramatic inequities that exist between the neurosurgical services in Puerto Rico, and those in the mainland. Results: Our research demonstrates how this controversial, and constantly confusing, political ideology has resulted in dramatic inequities, which have ultimately affected all aspects of the development and advancement of neurosurgery. Conclusion: Political ideology, nationality, and authority have all great influence on a country’s initial strides and subsequent growth; being critical to both the development and well-being of all governmental agencies, and health status of its population. We conclude that the economic crisis being faced by American citizens in Puerto Rico has been detrimental to stability and advancement of neurosurgery, limiting both the care and education of patients, residents, fellows, and physicians, alike.
P438: Cost-Effectiveness Analysis Comparing Endoscopic Discectomy Versus Open Discectomy for Lumbar Disc Herniation With Sciatica Pain in Brazilian Health System
Vitor Viana Bonan de Aguiar1
1Sarah Network of Rehabilitation Hospitals, Macapá, Brazil
Introduction: In the past few years, minimally invasive spine (MIS) surgery has been developed for several disorders promising shorter hospital stays, smaller surgical scars, minor surgical complications, and earlier return to daily activities. In Brazil, the MIS technique costs higher than the standard open discectomy, but it is unknowing if global costs are also higher too. Global costs of a procedure can include since the first patient visit until complete recovery. The literature demonstrated a slight superior difference of endoscopic surgery in quality of life and surgery complications. Our objective is to compare the cost-effectiveness of MIS and open discectomy to treat lumbar disc herniation under Brazilian health system perspective. Material and Methods: Target population is patients with sciatica pain with clinic-radiologic correlation. A decision tree model started with patients going to standard discectomy or endoscopy discectomy. Surgery complications (such as dural tear, dysesthesia, discitis, and site infection), length of hospital stay, and recurrence rate (incomplete removal, stenosis, or other causes) were considered. Direct costs correspond to surgery cost, anesthesia, image examinations, medical devices, and inpatient costs. All costs were calculated originally in local currency units and then converted to US dollars using the purchase power parity conversion factor (PPP, 2018. Effectiveness was based on quality-adjusted life year (QALY) estimated by the Oswestry Disability index and SF (Short Form)-6D. The model was analyzed from a health care payer perspective based on Brazilian private sector. The incremental cost-effectiveness ratio was the ratio between delta cost (total cost of endoscopy − total cost of open discectomy) per delta effect. Results: The estimated total cost of endoscopy surgery was US$11 600.00 per patient comparing to US$2000.00 of open discectomy. Therefore, the estimated QALY does not have an important difference between them (endoscopy: 0.658 vs open: 0.621). The incremental cost-effectiveness ratio was US$258 000.00 per QALY gained. Sensitivity analyses have shown that the price of endoscopy surgery (mainly the medical devices) was the most influential factor on ICER (incremental cost-effectiveness ratio). In Brazil, endoscopy surgery can cost 10 times the open discectomy. If the price of endoscopic surgery was only 20% more, the endoscopic technical will be cost-saving. Conclusion: Regarding costs and effectiveness, the endoscopic surgery costs higher than open discectomy with a slight gain in quality of life. The endoscopic surgery could be cost-effectiveness if the price reduces until 20% of the current price of open discectomy in our Brazilian settings.
P439: Postoperative Impact of Lumbar Stenosis Surgery: Analysis of the EQ-5D Health Questionnaire
Fernando Alvarado-Gomez1, Luis Carlos Morales Saenz1, Constanza Bedoya1, Andres Rodriguez Munera1, David Meneses-Quintero2, Camilo Velez Escallon1, Kenny Lopez-Gomez1, Yuli Fuentes-Barreiro1, Jorge Uribe1, Jose Dangond Millan1, Gerardo Ardila1
1Hospital Universitario Fundacion Santa Fe de Bogota, Bogota, Colombia
2Instituto de Ortopedia Infantil Roosevelt, Bogota, Colombia
Introduction: Patients with spine stenosis have marked limitations that compromise their quality of life. Because of this, it is awfully important to measure and apply all the possible alternatives that can reach the maximum possible patient improvement. The objective of this article is to define the individual impact of the spine surgery over each one of the 5 dimensions of the EQ-5D questionnaire that determine life quality in patients with lumbar stenosis and thus specify what additional interventions may be carried out in order to improve the global postoperative score and with it the general patient welfare. Material and Methods: A retrospective descriptive design study was carried out of a cross-sectional cohort of patients who underwent lumbar stenosis surgery between the year 2016 and 2018. All the patients included in this study answered the EQ-5D health questionnaire at the presurgical assessment and at the next 6 months. Also, follow-up at 12 months was included but was not an exclusion criterion, because of the absence of data of that time. Scores were obtained according to the premise that level 1 indicates no problem and 5 indicates extreme problems. The total sample size was 58 patients and only 40 of these patients had the postoperative 12-month control score. Results: When the descriptive analysis of the information was carried out, the following points were found: taking the total sample, 41 patients correspond to women, and 17 patients correspond to men, with an average age of 68.5 years. The number of levels intervened is directly proportional to the average age, as well as directly proportional to the time of evolution in months of the disease. In the initial questionnaire, the majority of patients obtained a score of 3 for pain and 2 for mobility and usual activities. In the 6-month control, similar results were obtained except that the variable of usual activities reached a score of 1, which remained in 12-month control. According to the analysis of correspondence, the dimension of pain progressively moved away from the score no. 3, which shows an important pain improvement through the months. Through the χ2 test, the multivariate analysis showed that the dimension most compromised preoperatively was pain; even no person reports of having pain. The majority of patients answered 2 in the second question, which means that this pathology does not usually compromise personal care (P value of 2.0E-06). There was a decrease in the level referred by patients about the mobility dimension and no one reported a level greater than 2 in the control of 12 months, which means a marked improvement in postoperative mobility less than or equal to slight problems in walking about (P value of 4.0E-04). Conclusion: It was determined that in our population, surgical treatment improves the quality of life at 6 months and even more at 12 months (in the patients that could be analyzed), specifically in performing the usual activities and, less noticeable but very important, in the pain and discomfort feeling at long term.
P440: Online Ratings, Spine Deformity Surgeon, Scoliosis Research Society, Physician Review Websites, and Physician Practice
Addisu Mesfin1, Giresse Melone1, Cesar Hernandez1, Rishi Balkissoon1, and Emmanuel Menga1
1University of Texas, Galveston, TX, USA
Introduction: Physician review websites (PRW) continue to be an emerging trend in the United States, across all specialties. Previous literature with smaller sample sizes revealed that most spine surgeons are rated on at least one PRW. To date, the online ratings of spinal deformity surgeons have not been evaluated. Our objective was to evaluate the online ratings of spine deformity surgeons and variables that may affect online ratings. Material and Methods: A review of the 2017 Scoliosis Research Society (SRS) Fellowship directory for active fellows and candidate members yielded 634 active members. Online ratings from “Healthgrades,” “Vitals,” “RateMDs,” “WebMD,” and “Yelp” were all recorded and scaled from 0 to 100. Using SPSS, 1-way analysis of variance was used to compare differences between multiple groups. A t test was used to compare differences between 2 groups. Significance was set at P < .05. Results: Nearly all surgeons, 98.7% were rated on at least one PRW. Surgeons in academic practice had significantly higher ratings than those in private practice (84.3 vs 79.7; P = .00 005). Hospital employed surgeons had significantly higher ratings than those in private practice (85.1 vs 79.7; P = .0001). Surgeons in practice for 0 to 5 years had significantly higher ratings than those practicing for 11 to 20 years and ≥21 years, respectively (91.8 vs 83.6, P = .001, and 91.8 vs 81.4, P = .001). No significant differences in ratings with regard to sex (83.3 male vs 80.1 female; P = .368), specialty (83 orthopedics vs 85.1 neurosurgery; P = .199), geographic location (P = .917), or fellowship training (84.3 pediatrics vs 82.5 spine; P = .065). Conclusion: Spine deformity surgeons in practice between 0 and 10 years have higher ratings than more experienced surgeons (practice 21+ years). Academic- and hospital-employed SRS surgeons had higher ratings than those in private practice. Nearly all, 98.7%, SRS surgeons were rated on at least one PRW.
P441: Drivers of Episode Payments for Non-Cervical Spinal Fusion
Mohamed Macki1, John Syrjamaki2, David Nerenz1, Scott Regenbogen2, and Victor Chang1
1Henry Ford Hospital, Detroit, MI, USA
2University of Michigan, Ann Arbor, MI, USA
Introduction: The objective of this study is to determine the drivers of episode payments among different hospital payment quartiles. Methods: The Michigan Value Collaborative (MVC) maintains a detailed claims-based registry of comprehensive 90-day episodes of care that includes costs and utilization surrounding an admission for non-cervical fusion based on discharge diagnosis-related group (DRG). The hospitals were partitioned into 4 equally sized quartiles with the first quartile of total episode payments referred to as the lowest payment hospitals and the fourth quartile of total episode payments referred to as the highest payment hospitals. Results: Of a total of 10 168 non-cervical spinal fusion operations, the 90-day episode payment averaged $42 879 (range = 37 965-48 868). The difference of $8371 between the highest payment hospitals ($47 124) and lowest payment hospitals ($38 753) reached statistical significance (17.7% difference, P < .0001). Index hospitalizations accounted for the majority of payments: 73.3% in the first quartile of hospitals, 69.1% in the second quartile of hospitals, 63.8% in the third quartile of hospitals, and 62.5% in the fourth quartile of hospitals. Between the highest- and lowest-quartile hospitals, the greatest variation was actually attributable to post-acute care ($7478 vs $3178, P < .0001), followed by professional fees ($7675 vs $5836, P < .0001), readmissions ($2497 vs $1307, P = .018), and index hospitalizations ($29 474 vs $28 432, P = .019). In other words, 51.4% of the total $8371 episode payment difference between the highest- and lowest-quartile hospitals derived from post-acute care followed by 22.0% in professional fees, 14.2% in readmissions, and 12.4% in index hospitalizations. On examining subcomponents of post-acute care payments, the largest difference between the highest- and lowest-quartile hospitals was $2169 for inpatient rehabilitation (P = .004), followed by $1822 for skilled nursing facility (P = .007) and $785 for home health (P = .007). Conclusion: Post-acute care, namely, rehabilitation service, is the primary driver of variations in 90-day bundled payments for non-cervical spinal fusions.
P442: Associated Risk Factors of Malpractice Outcomes Following Spine Surgery
Howard Park1, Richard Hwang1, Amador Bugarin1, Christopher Hamad1, Joshua Proal1, William Sheppard1, Ryan Smith1, Nicholas Bernthal1, Arya Nick Shamie1, and Don Park1
1University of California, Los Angeles, CA, USA
Introduction: Medical malpractice claims involving spine surgery are common. A small number of studies have described characteristics of spine medical malpractice litigation. However, few studies have identified predictors of legal outcomes following spine surgery, and no studies have compared legal outcomes between different types of spine surgery. The purpose of this study is to compare medical malpractice outcomes among different types of spine surgery and identify other predictors of medical malpractice outcomes. Methods: The national medicolegal database Westlaw was queried for medical malpractice verdicts and settlements involving spine surgery from 2012 to 2018 in the United States. Only cases with complaints related to surgery or postoperative complications were included in the study. Patient demographics, clinical and procedural data, reasons for litigation, injuries, and legal outcomes were recorded for each case. Univariate analysis was performed to identify predictors of defendant outcome and higher monetary awards. Results: A total of 199 cases were included from the database search. Cases were categorized based on instrumentation (noninstrumented: 77, instrumented: 111), number of spinal levels (single level: 85, multilevel: 82), and procedure type (decompression only: 67, decompression with fusion: 74, fusion only: 34, other: 16). Of these 199 cases, 145 (73%) resulted in a defendant verdict, 33 (17%) resulted in a plaintiff verdict, and 21 (11%) resulted in a settlement. The median monetary award for plaintiff verdicts and settlements was $1.3 million. The most common reasons for litigation in noninstrumented cases were intraoperative error (43%), failure to obtain informed consent (36%), and improper postoperative management (36%), compared with improper postoperative management (38%), improper hardware placement (37%), and failure to obtain informed consent (26%) for instrumented cases. Cases involving multilevel spine surgery were associated with higher monetary awards (median: $1.88 vs $0.79 million, P = .04) than single-level spine surgery. Median monetary awards and the likelihood of a defendant verdict were similar regardless of instrumentation and procedure type. Cases were less likely to result in a defendant verdict if the patient suffered postoperative cauda equina syndrome (41% vs 77%, P = .001) or other catastrophic injury (paraplegia, quadriplegia, anoxic brain injury, or death) (62% vs 77%, P = .03). Orthopedic surgeons were more likely to successfully defend the malpractice case than neurosurgeons (85% vs 67% defendant, P = .005). Conclusion: Most spine surgery litigation cases are related to intraoperative errors such as improper hardware placement, improper monitoring, and management of postoperative complications. Overall, spine surgeons are likely to successfully defend lawsuits related to spine surgery, and risk factors of unsuccessful defense include multilevel spine surgery, cauda equina syndrome, or other catastrophic injury.
MINIMALLY INVASIVE SPINE SURGERY
P443: Anterior Transforminal Approach for Cervical Radiculopathy
Santosh Kumar Bashyal1
1Kathmandu University, Rupandehi, Nepal
Introduction: Cervical radiculopathy can be treated by anterior endoscopic approach to access its target pathology decompressing spinal nerve roots without fusion. The transforaminal anterior percutaneous endoscopic cervical discectomy (PECD) approach is easy way to transverse process and decompress and remove osteophytes. It preserves spinal motion, stability, and reduces risk of vertebral injury. Material and Methods: A case selected had neck pain radiating toward right arm for 2 months but severe pain from 20 days, neck deformities, head tilted toward right side. Neurological examination showed decreased sensation and weakness over right-sided trapezius, biceps, and triceps muscles. Eaton sign and Spurling sign were positive. Preoperative dynamic X-ray showed degenerative changes, osteophtyes at C3-4, C5-6, CT (computed tomography) intervertebral foraminal stenosis at C3-4 and C5-6 level, and MRI (magnetic resonance imaging) disc protrusion severely compressing spinal cord at C3/4 level. We operated at most significant level as first successful newer approach for cervical radiculopathy with osteophytes removal, decompression, and discectomy by PECD anterolateral (transforaminal approach) under general anesthesia. Results: Blood loss was 100 mL, hospital stay was 3 days, and operative time was 80 minute. There was marked improvement of preoperative VAS (visual analogue scale) score from July 2010 to March 2010. After surgery, drain was fixed for 24 hour to collect some residual fluids and avoid hematomas. There were no significant postoperative events or surgery-related complications. Conclusion: Under percutaneous endoscopic system is easy to visualize proper minute structure, drill, dissect, and lessen the chance of iatrogenic injury, and decrease the risk of vertebral arteries. Anterior transforaminal endoscopic surgical approach can be further developed and trained for treatment of cervical radiculopathy in large population.
P444: Assessment of Efficiency of the Easy Go Spinal Endoscopic Spine System: Is This Easy Go or Not so Easy Go System
Aftab Younus1 and Mohammad Hamza Sultan Aftab1
1Helen Joseph Hospital, University of Witwatersrand, Johannesburg, South Africa
Introduction: With the advent of technology, endoscopic discectomy is becoming popular. The spine surgeons all over the world have started exploring this new technology, although there is a steep learning curve and complication rate will be high in the early case. We assess the efficiency of new Easy Go endoscopic discectomy system by Storz. This system allows you to do discectomy through 20-mm incision. Furthermore, we want to assess the clinical outcome, quality of life, neurological function, and complications. Material and Methods: We describe 25 patients who had lumber disc prolapse at various levels during 2014 to 2016. They were treated conservative for 3 to 6 months. Twenty of these patients had neurology problems and remaining had sciatic problems. All of these patients had endoscopic discectomy by the using Easy Go system. In 2 patients, we had to ignore the procedure and do open discectomy. Result: These patients were followed-up for 1 year. The technique’s problem and other clinical assessments were done. The duration of operation was 2 to 3 hours. The author had difficulty in initial cases. The difficulties and complications that came across with this system is as following: (1) difficult to work through a 19-mm tube; (3) prolonged operation time; (3) frequent fog and blood on the camera, which require frequent cleaning; (4) two patients had other complications, that is, dural tear and nerve damage; (5) One patient developed recurrence of disc prolapse in 6 months time. However, the positive aspects that we found about the system are the following: (1) less bleeding; (2) less painkiller required by the patient; (3) early discharge from the hospital; (4) early return to work. Conclusion: Lumber endoscopic discectomy with the Easy Go system (Storz) is not easy. First of all, working through a small size tubular retractor is difficult and technically demanding. In 2 patients, we had nerve root damage and dural tear. In 2 patients, we had to ignore the procedure because of frequent fog and bleeding in the tubular retractor. There is a steep learning curve. Overall, 72% of our patients were satisfied with the procedure. The complications are more than benefits.
P445: Possibilities of Using Minimally Invasive Dorsal Decompressive Stabilizing Interventions in Patients With Overweight and Obesity
Vadim Byvaltsev1, Talgat Kerimbaev1, Andrei Kalinin1, and Evgenii Belykh1
1Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: Spinal surgery in patients with overweight and obesity is associated with an increased risk of perioperative complications. Minimally invasive transforaminal lumbar interbody fusions (MIS-TLIF) and traditional methods (open TLIF [O-TLIF]) of rigid stabilization are used universally, but the advantages and disadvantages of MIS-TLIF in patients with an elevated body mass index (BMI) remain controversial. The purpose of our study is to evaluate the effectiveness of a new less invasive technology of rigid fixation and the traditional open method of interbody fusion in the surgical treatment of degenerative diseases of the lumbar segments in patients with overweight and obesity. Materials and Methods: The study included 73 patients (49 men and 24 women) with a BMI greater than 25 kg/m2 at the age of 53 (42-65) years. Two study groups were identified: I group MIS-TLIF (n = 32), operated according to the original technique of reconstruction of the spinal canal, interbody fusion, and combined transpedicular stabilization; II group O-TLIF (n = 41), which performed a single-level rigid stabilization from the median approach. The mean follow-up period was 34 months in group I, 40 months in group II. For the comparative analysis, clinical parameters, intraoperative characteristics, specificity of the postoperative period, instrumental data, and the presence of complications were investigated. Results: In comparison with the O-TLIF group, MIS-TLIF showed smaller parameters: the duration of the operation, the amount of blood loss, the time of X-ray radiation, the time of activation, and the duration of inpatient treatment. A comparative analysis of the severity of pain on a visual analogue scale and the functional state of ODI (Oswestry Disability Index) in a catamnesis revealed significantly better results in group I of patients, which is associated with less intraoperative soft tissue damage. The number of postoperative complications in group I was 9% and in group II was17% (P = .01). At the same time, the formation of the interbody block in the long-term postoperative period was noted in 88% of the patients of the group I and in 83% of the group II (P = .15). According to the instrumental data, there was a statistically significant greater muscular atrophy in group O-TLIF (P < .001). Conclusion: The original technique of MIS rigidity stabilization is safe and highly effective in the surgical treatment of degenerative diseases of the lumbar segments in patients with obesity. MIS-TLIF has a number of significant advantages over O-TLIF in the dynamics of clinical parameters and a low number of perioperative complications, which is confirmed by less damage to paravertebral tissues and better functional state in the long-term postoperative period.
P446: Comparative Results Between Open and Minimally Invasive Fusion Surgery in Lumbar Degenerative Disc Disease
Ezequiel Gimenez1, Marcelo Montaño Urna1, and Raul Santivanez2
1Sociedad Argentina de Patología de Columna Vertebral, Buenos Aires, Argentina
2Universidad de Buenos Aires, Buenos Aires, Argentina
Introduction: Lumbar spine fusion is indicated in patients refractory to traditional treatment for degenerative disc disease. The aim of this study was to compare perioperative and postoperative results of conventional open surgery versus minimally invasive surgery (MIS) in posterior 360° lumbar fusion with pedicle screw instrumentation. Material and Methods: A total of 25 patients underwent MIS and 40 underwent open surgery between 2015 and 2017. Perioperative variables and lumbar and radicular pain values were compared using a visual analogue scale (VAS) and Oswestry Disability Index (ODI) until 12 months post-surgery. Results: The MIS cohort presented less blood loss (140 vs 345 mL; P = .001), shorter hospital stay (1.1 vs 2.2 days; P = .001), longer operative time (113 vs 94 minutes; P = .001), and greater X-ray exposure (80 vs 6 seconds; P = .001), compared with the open surgery group. The MIS cohort showed better results in ODI and lumbar VAS scores. No significant differences were observed in radicular VAS. Conclusion: MIS surgery showed advantages over the open surgery technique; however, the learning curve should be improved in order to reduce operative time.
P447: The Treatment of Osteoporotic Thoracolumbar Burst Fractures by Unilateral Percutaneous Kyphoplasty
Peng Yin1, Yong Hai1, and Qingjun Su1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Objective: The objective of this study was to evaluate the clinical effects of unilateral percutaneous kyphoplasty (PKP) on osteoporotic thoracolumbar burst fractures. Methods: From January 2014 to January 2016, 46 patients with osteoporotic thoracolumbar burst fractures treated by PKP were included in our study. The height of posterior wall (HPW), the height of anterior wall (HAW), and kyphotic angle (KA) were measured via X-ray radiographs before surgery, 1 day after surgery, and at final follow-up. Visual analogue scale (VAS) score and the Oswestry Disability Index (ODI) score were evaluated preoperatively, postoperatively, and at final follow-up. Results: All patients were followed-up, and the mean follow-up was 28.8 ± 7.0 months. The preoperative HAW was 20.1 ± 2.3 mm, and the HAW was significantly improved to 22.9 ± 2.4 mm after operation (P < .05), and at the final follow-up, the HAW was 19.9 ± 2.1 mm, which was lower than the postoperative HAW. The HPW was also significantly corrected after surgery (P < .05). There were no significant differences between postoperative HPW and the HPW at the final follow-up (P > .05). The KA was significantly corrected after operation (P < .05), but relapse occurred at the final follow-up, and at the final follow-up, the average of KA was 19.4 ± 1.6°. The VAS and ODI were significantly improved at the final follow-up compared with the preoperative period (P < .05). Cement leakage was found in 8 patients, and adjacent vertebral fracture was found in 2 patients. Conclusions: Our present results showed that unilateral PKP acquired satisfied treatments effect in the management of osteoporotic thoracolumbar burst fractures. Meticulous evaluation of preoperative images and careful repetitious injection of cement are important to prevent the cement leakage.
P448: Anatomical Relation of Vertebral Artery From Lateral Recess for Safe Foraminotomy in Endoscopic Posterior Foraminotomy
Hyeun-Sung Kim1, Ravindra Singh1, Nitin Maruti Adsul2, Seong-Hoon Oh3, Jung Hoon Noh1, Seong-Hoon Oh3, and Il Tae Jang1
1Nanoori Gangnam Hopsital, Seoul, Republic of Korea
2Sir Ganga Ram Hospital, New Delhi, India
3Nanoori Incheon Hospital, Incheon, Republic of Korea
Introduction: Vertebral artery injury when performing posterior cervical foraminotomy is rare but can have fatal consequences for patients. We searched studies for the anatomical relationship between vertebral artery and lateral recess to avoid vertebral artery injury during the surgery. Material and Methods: We measured the distance between vertebral artery and facet joint at C2-3, C3-4, C4-5, C5-6, and C6-7 levels using the cervical MRI (magnetic resonance imaging) of randomly selected 110 patients. First, the distance (A) from inferior margin of vertebral artery to medial border of facet joint was measured and second, the distance (B) from medial margin of vertebral artery to medial border of facet joint was measured. Finally, we calculated the angle (C) of 2 lines (A and B). We analyzed the differences between each levels and difference between right and left using the paired t test. Results: The mean value of right (A) showed a statistically significant difference at C3-4 (10.15, SD: 1.27), C4-5 (11.67, SD: 1.53), C5-6 (12.83, SD: 1.57), and C6-7 (16.41, SD: 1.86) levels. The mean values of left (A), right (B), left (B) had the same aspect with the mean value of right (A). The mean value of right (C) showed statistically significant difference at C3-4 (63.49, SD: 7.02), C4-5 (63.98, SD: 6.44), C5-6 (58.12, SD: 6.58), and C6-7 (52.96, SD: 5.93) levels, and the mean value of left (C) had the same aspect with the mean value of right (C). All data showed that the difference between C5-6 and C6-7 levels was the largest, and the higher level, the closer distance from lateral recess. The mean values of right (A) and left (A) had the statistically significant difference in all level; the left was closer than the right. But the mean values of right (C) and left (C) showed no statistically significant difference in all levels. Conclusion: The distance from the lateral recess to the vertebral artery gets closer as cervical level rises and left than right. When performing the posterior cervical foraminotomy, it is necessary to be more careful at C5-6 level or above, especially left.
P449: Percutaneous Endoscopic Lumbar Discectomy for All Types of Lumbar Disc Herniations Including Severely Difficult and Extremely Difficult Lumbar Disc Herniations Cases
Hyeun-Sung Kim1, Keun Lee1, Paudel Byapak2, Jee Soo Jang3, Seong-Hoon Oh4, and Il Tae Jang5
1Nanoori Juan Hospital, Incheon, Republic of Korea
2Grande International Hospital, Kathmandu, Nepal
3Nanoori Hospital Suwon, Suwon, Republic of Korea
4Nanoori Hospital Incheon, Incheon, Republic of Korea
5Nanoori Hospital Gangnam, Seoul, Republic of Korea
Introduction: Lumbar disc herniation (LDH) is being treated with limited indication by percutaneous full-endoscopic lumbar discectomy. However, microscopic lumbar discectomy (MLD) is still considered as a gold standard. With the advances in spinal endoscopic instruments and surgical techniques, all LDHs have now become operable with percutaneous full-endoscopic lumbar discectomy procedure. We report the results of percutaneous full-endoscopic lumbar discectomy (PELD) for all patients diagnosed with LDH, including severely difficult and extremely difficult LDH cases who visited our clinic with leg pain and lower back pain. Material and Methods: Electronic medical records of 98 consecutive patients (104 levels) who underwent surgery from October 2015 to May 2016, by PELD for different LDHs either by percutaneous endoscopic transforaminal lumbar discectomy (PETLD) or percutaneous endoscopic interlaminar lumbar discectomy (PEILD) approach were reviewed retrospectively. The L5-S1 level was accessed with PEILD approach, and the other levels were accessed with PETLD approach. Outcomes were analyzed utilizing the visual analogue scale (VAS), Oswestry Disability Index (ODI), MacNab Criteria, and endoscopic surgical success grade/score. Results: There were 75 (72.1%) men and 29 (27.9%) women patients with a mean age of 48.12 ± 15.88 years. Follow-up range from a minimum of 10 to 15 months (mean 12.77 ± 1.84 months). Most of the LDHs were located at L4-5 level. There were 76% severely difficult and extremely difficult cases. PETLD was the choice of approach in most of the cases (78 cases, 75%). VAS decreased significantly. ODI improved from preoperative 54.67 ± 7.52 to 24.50 ± 6.45 at last follow-up. A total of 96.1% good to excellent result was obtained as per MacNab criteria and 98.1% of patients were managed with a successful to completely successful grade according to the endoscopic surgical success grading/scoring. Two cases (1.9%) developed transient motor weakness. Conclusion: With more than 96% success (98.1% as per endoscopic success grading/scoring), all kinds of LDHs, including severely difficult and extremely difficult LDHs, are accessible by the PELD (PETLD and PEILD) technique. PELD can now be considered an alternative to microscopic lumbar discectomy (MLD) in the treatment of all kinds of disc herniations with the added benefits of keyhole surgery even for severely difficult and extremely difficult LDH cases.
P450: Early Outcomes of Endoscopic Contralateral Foraminal and Lateral Recess Decompression Via an Interlaminar Approach in Patients With Unilateral Radiculopathy From Unilateral Foraminal Stenosis
Hyeun-Sung Kim1, Paudel Byapak2, Il Tae Jang1, and Seong-Hoon Oh3
1Nanoori Hospital Gangnam, Seoul, Republic of Korea, Republic
2 Grande International Hospital, Kathmandu, Nepal
3Nanoori Hospital Incheon, Incheon, Republic of Korea
Introduction: Percutaneous endoscopic contralateral interlaminar lumbar foraminotomy (PECILF) for lumbar degenerative spinal stenosis is an established procedure. Better preservation of contralateral facet joint compared with that of the approach side has been shown with uniportal bilateral decompression. The aim of this retrospective case series was to analyze the early clinical and radiologic outcomes of stand-alone contralateral foraminotomy and lateral recess decompression using PECILF. Material and Methods: Twenty-six consecutive patients with unilateral lower limb radiculopathy underwent contralateral foraminotomy and lateral recess decompression using PECILF. Their clinical outcomes were evaluated with the visual analogue scale leg pain score, the Oswestry Disability Index, and the MacNab criteria. Completeness of decompression was documented with a postoperative magnetic resonance imaging. Results: Mean age for the study group was 62.9 ± 9.2 years and the male–female ratio was 4:9. A total of 30 levels were decompressed, with 18 patients (60%) undergoing decompression at L4-L5, 9 at L5-S1 (30%), 2 at L3-L4 (6.7%), and 1 at L2-L3 (3.3%). Mean estimated blood loss was 27 ± 15 mL per level. Mean operative duration was 48 ± 12 minutes/level. Visual analogue scale leg score improved from 7.7 ± 1 to 1.8 ± 0.8 (P < .0001). The Oswestry Disability Index improved from 64.4 ± 5.8 to 21 ± 4.5. Mean age for the study group was 62.9 ± 9.2 years and the male–female ratio was 4:9. A total of 30 levels were decompressed, with 18 patients (60%) undergoing decompression at L4-L5, 9 at L5-S1 (30%), 2 at L3-L4 (6.7%), and 1 at L2-L3 (3.3%). Mean estimated blood loss was 27 ± 15 mL per level. Mean operative duration was 48 ± 12 minutes/level. Visual analogue scale leg score improved from 7.7 ± 1 to 1.8 ± 0.8 (P < .0001). The Oswestry Disability Index improved from 64.4 ± 5.8 to 21 ± 4.5. Conclusion: Facet-preserving contralateral foraminotomy and lateral recess decompression with PECILF is effective for treatment of lateral recess and foraminal stenosis. Thorough decompression with acceptable early clinical outcomes and minimal perioperative morbidity can be obtained with the contralateral endoscopic approach.
P451: Cost-Effectiveness Comparison Between Open Microdiscectomy and Endoscopic Discectomy for Lumbar Disc Herniation
Kyung-Chul Choi1
1The Leon Wiltse Memorial Hospital, Anyang, Republic of Korea
Introduction: To assess cost-effectiveness of 4 surgical techniques, which are microdiscectomy (MD), percutaneous endoscopic lumbar discectomy (PELD), percutaneous endoscopic interlaminar discectomy (PEID), and unilateral biportal endoscopic discectomy (UBED) for lumbar disc herniation. Material and Methods: Five hundred sixty-five patients who underwent the 4 surgical techniques between 20 and 60 years were reviewed up to 1 year postoperatively. Health care costs were defined as sum of direct costs, which included National Health Insurance covered and uncovered costs from operation through 1-year follow-up and indirect costs include the costs incurred by work loss. The direct costs can be defined as the sum of primary hospital costs associated with operation and secondary hospital costs associated with postoperative course management and unexpected events after surgery. Incremental cost-effectiveness ratio (ICER) was determined using cost/quality-adjusted life year (QALY). Results: One hundred fifty-seven patients of PELD, 132 of PEID, 140 of UBED, and 136 of MD were enrolled. There were no differences between the groups in baseline demographics. The direct costs of PELD, PEID, UBED, and MD were $3037.9 ± 963.9, $3179.8 ± 566.9, $3,328.3 ± 925.6, and $3,625.8 ± 800.1, respectively (P < .01). The indirect costs of PELD, PEID, UBED, and MD were $574.5 ± 495.9, $587.8 ± 488.3, $647.4 ± 455.6, and $759.7±491.7, respectively (P < .01). One-year QALY gains were 0.208 for PELD, 0.211 for PEID, 0.194 for UBED, and 0.186 for MD. ICER (costs/QALY) was highest in the MD ($30,215.2 ± 22,202.8, P < .01). ICERs of PELD, PEID, and UBED were $22 402.7 ± 17 ±710.4, $23 730.2 ± 28 497.3 and $23 344.6 ± 13 257.8 respectively. Compared with MD, endoscopic discectomy (ED) saved additional net cost of $34 576 per QALY (P < .01). There was no significant difference of ICERs in 3 endoscopic techniques. Conclusion: ED was more cost-effective than MD at 1-year follow-up.
P452: Percutaneous Stabilization of Spinal Fractures: Complication Results of a New Technique
Thomas Weiss1, Stefan Hauck1, and Oliver Gonschorek1
1 Spine Surgery, Murnau, Germany
Introduction: Minimally invasive stabilization techniques (MISS) are gaining importance in the treatment of spinal fractures. The purpose of this investigation was to evaluate the complication rate of this new procedure. Especially the complications of the hardware (screws and rods) will be illustrated. Materials and Methods: In the years 2010 to2014, a total of 670 patients have been stabilized with MISS techniques in spinal fractures. In 118 patients of this collective, we used cement augmentation of the screws in instable osteoporotic fractures. The complications have been divided into intraoperative, postoperative, and implant-related complications. Data collection has been prospective. Especially complications and hardware problems of the new technique has been described. The results have been compared with the complications results in the open procedure technique of the MCS-2 study from the German Society of Trauma surgery (DGU). Results: We found 7 patients with infection and operative revision. In all patients, it was not necessary to remove the implant. In 5 patients, we saw loosening of the set screws. In 2 cases, there was a loss of reduction and gaining kyphosis. It was necessary to indicate an early revision. In one case, it was an incidental finding. In total, the complication rate of intraoperative and postoperative complications is 2.1%. Compared with the study group, the rate in the open procedure is 9.4%. Intraoperative bleeding and conversion to open procedure was not observed. There was no revision necessary because of malpositioning of a pedicle screw. Conclusions: The percutaneous stabilization technique of spinal fractures is a safe procedure. In general, the complication rate is less than in the open techniques. We found implant-related complications such as loosening of the set screws. This should be recognized and improved by the companies.
P453: Sky Is the Limit in Minimally Invasive Surgery! Feasibility and Efficacy of Minimally Invasive Microscopic-Assisted Stand-Alone Transarticular Screw Fixation in the Management of 82 Cases of Mobile Atlantoaxial Instability
Zahirabbas Merchant1, Vishal Kundnani1, Ankit Patel1, Rahul Prakash1, Mihir Upadhyaya1, Neil Kire1, Sanyam Jain1, and Rahul Mehta1
1Bombay Hospital & Medical Research Center, Mumbai, India
Introduction: Transarticular screw fixation is the gold standard for mobile reducible atlantoaxial instability. Minimal invasive advantages reduce the morbidity of standard techniques and have added to the value of technique. Aim and Objective: To evaluate clinico-radiological efficacy of stand-alone MIS-TAS (minimally invasive transarticular screw fixation) without supplemental Gallie fixation in the management of mobile C1-C2 instability. Material and Methods: Prospective study; patients with mobile reducible atlantoaxial instability and >2 years follow-up were included and managed by microscopic-assisted minimal invasive technique and stand-alone TAS fixation using morselized allograft without additional wiring or supplemental fixation. Patient demographics and perioperative parameters (blood loss, surgical time, vehicular accident injury, hospital stay) were noted. Clinical parameters (visual analogue scale [VAS]/Oswestry Disability Index [ODI]), neurology (modified Japanese Orthopaedic Association [mJOA]) and radiological factors (anterior atlanto-dens interval [ADI] and space available for cord [SAC]) were evaluated pre- and postoperatively. Fusion evaluated with dynamic X-rays .Computed tomography (CT) scan was obtained in those who did not show interspinous fusion on X-ray at 1 year to see intra-articular fusion. Statistical analysis done with SPSS-20.0 with Student’s t test and ANOVA (analysis of variance) to assess level of statistical significance (P < .05). Results: Eighty-two consecutive cases (male-female = 3:1, mean age = 36.26 ± 5.78 years) were evaluated. One hundred sixty-three transarticular screws were placed. Mean blood loss was 104.84 ± 21.75 mL (range = 80-350 mL), mean surgical time 120.11 ± 15.82 minutes, hospital stay was mean 3.2 days, and incision size was mean 3.5 cm (2.8-6 cm). Significant improvement was noticed in clinical (mean preoperative/postoperative VAS = 7.2 ± 2.19/3.3 ± 1.12, pre/postoperative ODI = 78.3 ± 4.83/34.05 ± 3.26) and neurological features (mean preoperative/postoperative mJOA = 14.73 ± 2.68/17.5 ± 2.21). Radiological evidence of fusion was noted in 97.5% cases at final follow-up. Seventeen patients did not show interspinous fusion on X-rays, but CT scan but revealed facet fusion in all of them except 2. Inadvertent vertebral artery injury was noticed in 3 cases managed with tamponade in 1 case and screw insertion in 2 cases. No inadvertent OC or C23 fusion noted in our series. Conclusion: MIS microscopic-assisted stand-alone TAS fixation with morselized allograft provides excellent radiological and clinical outcomes with lesser morbidity than conventional TAS. Addition of a supplementary tension band and structural graft are not essential. This provides the opportunity to avoid the complications associated with graft harvesting and wiring.
P454: Can Paravertebral Muscle MRI Assessment Be Used for Determining Potential Recurrent Herniated Disc? A Nested Case-Control Study
Kanthika Wasinpongwanich1,2, Krit Pongpirul2,3,4, Khin Myat Myat Lwin2, and Verapan Kuansongtham2
1Suranaree University of Technology, Nakhon Ratchasima, Thailand
2Bumrungrad International Hospital, Bangkok, Thailand
3Chulalongkorn University, Bangkok, Thailand
4Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
Introduction: Lumbar herniated disc recurrence is not uncommon and might be related to the strength of the paravertebral muscle. This study aims to explore if recurrent herniated disc patients have different paravertebral muscle property. Material and Methods: This case-control study was nested in the Bumrungrad Spine Cohort containing data of 545 patients who underwent full endoscopic discectomy during 2011 to 2016. A patient was considered a case if he/she experience a recurrent herniated disc. An age and gender-matched controls were randomly selected from the non-case group. Paravertebral muscle volume was measured quantitatively by lumbar indentation value (LIV) technique, whereas Goutallier’s classification was used for assessing degeneration. Results: Of 545, 60 cases with recurrent herniated disc and another 60 age-and-gender matched controls were reviewed. The overall mean age of the patients was 47.38 years and 30.83% were female. Mean LIV was 14.59 with no significant difference between case and control (14.93 vs 14.25 mm; P = .5021). Both groups had a similar distribution of Goutallier’s classification (P = .543). Conclusion: Paravertebral muscle volume and degeneration were not associated with the herniated disc recurrence.
P455: Unilateral Tubular Retractor–Guided TLIF Combined With Contralateral Decompression to Spondylolisthesis Having Bilateral Radiculopathy
Seyoung Pyo1, Yongwoo Shim1, Seonghwa Paeng1, and Yongtae Jung1
1Busan Paik Hospital, Inje University, Busan, Republic of Korea
Introduction: The patients of spondylolisthesis having both leg pain even while supine posture had been treated by bilateral direct decompression with PLIF (posterior lumbar interbody fusion) or transforaminal lumbar interbody fusions (TLIF) and posterior stabilization. If indirect decompression with ALIF (anterior lumbar interbody fusion), OLIF (oblique lateral interbody fusion), or DLIF (direct lumbar interbody fusion) was chosen, additional posterior decompression surgery might be necessary. Wide operation field and transabdominal approaches were considerable to time spent, blood loss, and clinical results. Then, we introduced unilateral tubular retractor–guided TLIF combined with contralateral decompression on this pathology. The aim of this study was to evaluate clinical efficacy of this procedure. Material and Methods: From June 2014 to May 2017, 20 patients of degenerative or spondylolytic spondylolisthesis having both leg pain even while lying down were treated by unilateral tubular retractor–guided TLIF and contralateral decompression simultaneously, and posterior stabilization with percutaneous pedicle screws and rods. Fourteen females and the others male, median ages 56, were enrolled. All patients had back pain and both leg pain even while rest with supine posture. And preoperative electrophysiologic studies applied to all treated patients represented suggested evidence of radiculopathy on both legs. Higher grade of Meyerding’s grades such as 3 or more were exclusion criteria. Clinical outcomes were measured by visual analogue scale (VAS) on back and legs pain on time intervals. And functional outcomes were estimated by MacNab and 36-item Short Form (SF-36) scores. Results: Mean VAS scores of back pain was improved 7.6 to 2.3 (P < .05). Mean VAS scores of each leg pain was improved 7.8 to 2.3 on right leg and 7.6 to 2.2 on left leg (P < .05). MacNab criteria were mostly excellent and good and SF-36 was also improved. Electrophysiologic studies after 6 months of surgery represented improving or improved radiculopathy. There was no revision or additional surgery case. Conclusion: Unilateral tubular retractor–guided TLIF combined with contralateral decompression to spondylolisthesis having both leg symptoms even while supine posture was a clinically effective, safe, and time-saving alternative treatment.
P456: Restoration of Vertebral Height After Cement Augmentation
Jesús Payo-Ollero1, Sebastian Cruz-Morande2, Matías Alfonso1, Rafael Llombart-Blanco1, and Carlos Villas1
1Clínica Universidad de Navarra, Pamplona, Spain
2Clínica Arcangel San Miguel, Pamplona, Spain
Introduction: Vertebroplasty and kyphoplasty are minimally invasive techniques applied to the treatment of vertebral fractures. The effect of cementation on the restoration of intraoperative vertebral height is not well established. The aim of the present study was to assess the intraoperative and evolutionary change happened in the vertebral body after cementation. Material and Methods: We performed a prospective study with 36 patients with a total of 67 vertebrae treated. The mean of age, BMI (body mass index), and ASA (American Society of Anesthesiologists) were 74 (range = 50-89) years, 27 (range = 17.4-34.1) kg/m2, 2.8 (2-4), respectively. The change in the dorsal kyphosis, lumbar lordosis, vertebral height, and wedge angle were measured at the time of fracture (standing), intraoperatively prior to cementation and after cementation (prone position), in the first and in the last revision (standing) with X-rays anteroposterior and lateral views. Likewise, it was assessed if these results change depending on Kümmel disease or using different types of cementation (vertebroplasty or radiofrequency kyphoplasty). We used a paired t test or Wilcoxon test to analyze the differences between each point of the study. Results: The average time among onset of the pain and the moment when the surgery took place was 69 (range = 15-180) days, between the surgery and the first revision was 41 (range = 15-55) days, and between the first revision and the last revision was 6 (range = 1-26) months. Of the 67 treated vertebrae, 91.6% were osteoporotic fractures and 8.4% were secondary fractures to multiple myeloma. There were no changes in the dorsal kyphosis or lumbar lordosis in the revisions made with regard to the moment of the vertebral fracture (P > .05). Intraoperatively, when the patient was placed in the prone position, there was a reduction in the vertebral body of +1.6 mm (22.6 mm vs 24.2 mm, 6.7%, P < .05). Furthermore, after cementation, there was an additional reduction in the vertebral collapse of +1.7 mm (25.9 mm vs 24.2 mm, 6.5%, P < .05). Then, a final reduction in the vertebral collapse was +3.3 mm, which were achieved with regard to the preoperative vertebral state (25.9 mm vs 22.6 mm, 12.7%, P < .05).The vertebrae height in vertebrae with Kümmel disease increased in +1.5 mm more than without Kümmel disease when the patient changed the standing position to prone position (P < .05). After cementation, vertebrae with Kümmel disease increased in +2.9 mm and +1.8 mm more than without Kümmel disease in the anterior and middle zone of the vertebral body, respectively (P < .001, P = .042). Radiofrequency kyphoplasty restored the vertebral body height more than vertebroplasty and achieved less collapse of the vertebral body during follow-up (P > .05). Conclusion: Vertebroplasty does not produce a significant change in dorsal kyphosis or lumbar lordosis. Intraoperatively, not only vertebroplasty produces a restoration of the vertebral height, but also the change of patient’s position. The vertebrae with Kümmel disease get greater vertebral height increase than vertebrae without Kümmel disease. In the vertebrae with or without Kümmel disease, the anterior and middle zones of the vertebral body were those that increased more after cementation. After the first postoperative month, there was a progressive slight collapse of the vertebral body.
P457: Transforaminal Percutaneous Endoscopic Lumbar Discectomy for Treatment of Intervertebral Disc Herniation: The Outcomes and Learning Curve in the First 60 Cases
Asrafi Rizki Gatam1, Harmantya Mahadhipta1, and Luthfi Gatam1
1Fatmawati General Hospital, Jakarta Selatan, Indonesia
Introduction: Symptomatic lumbar disc herniation often needs surgical decompression. The management itself has been developed through generation with microdiscectomy as the “gold standard” for surgical decompression. Percutaneous endoscopic lumbar discectomy (PELD) offers the less invasive surgery with many advantages. However, the steep learning curve discourages many surgeons, and this technique remains uncommon. The aim of this study is to share the outcome, complication, surgical technique, and obstacle of transforaminal PELD. Method: This is a nonrandomized prospective study. The inclusion criteria were patients with true herniated nucleus pulposus without any degenerative process who failed for conservative treatment. Visual analogue scale (VAS) for sciatica was compared pre- and post-operatively, and the patients satisfactory result was measured using modified MacNab’s criteria. All patients underwent transforaminal PELD in local sedation anesthesia. Result: The mean age was 31.9 years (range = 14-51), which consist of 27 male (45%) and 33 female (55%). The herniation occurred at L2-3 in 3 patients (5%), L3-4 in 2 patients (3%), L4-L5 in 32 patients (53%), and L5-S1 in 23 patients (38%). The mean sciatica VAS decreased from 5.7 (range = 4-7) to 2.5 after surgery. The first 3 patients had persistent symptoms after endoscopic discectomy and converted to open microdiscectomy. Ten patients had dysesthesia on subsequent exiting root that persist until 3.5 months after surgery, and 1 patient had motoric deficiency that completely recovered in 1-month follow-up. The overall satisfactory result was excellent and good in 56 (94%) patients and fair or poor in 4 (6%) patients. Conclusion: PELD is one of the reliable method in treating lumbar disc herniation. It offers many advantages such as day care procedure, local anesthesia, minimal soft tissue damage, and less possibility for nerve injury. In Indonesia, this is the future in managing lumbar disc herniation.
P458: Open ACDF Versus Full-Endoscopic ACDF for Treatment of Cervical Spondylotic Myelopathy: Retrospective Study
KangTaek Lim1 and Chun-Kun Park1
1Good Doctor Teun Teun Hospital, Anyang, Korea
The purpose of this study is to evaluate the clinical efficacy and safety of endoscopic anterior cervical discectomy and fusion (ACDF) and to discuss its operative strategies. A retrospective review was completed on 42 patients, 27 men, and 15 women with a mean age of 55 years who had ACDF from June 2017 to June 2018. They were divided into 2 subgroups, Group 1: 20 patients who underwent endoscopic ACDF, and Group 2: 22 patients who underwent conventional open ACDF. We reviewed the clinical and radiographic records of these patients. Method: All adult patients who underwent ACDF were diagnosed with cervical spondylotic myelopathy (CSM) and had been under conservative treatment for at least 6 months. Studies were included patients with 1-level segmental CSM caused by anterior compression with calcified disc, OPLL (ossification of the posterior longitudinal ligament), if patients have combined anterior and posterior compression or cervical myelopathy caused by posterior compression were excluded. All patients underwent detailed preoperative neurological examination, cervical spine plain X-rays, CT (computed tomography), and MRI (magnetic resonance imaging). In total, 42consecutive CSM patients undergoing ACDF from June 2017 to June 2018 were assigned into 2 groups. In the group 1 (n = 20), patients underwent endoscopic ACDF, and in group 2, conventional open ACDF (n = 22) were performed in the control group. ACDF in 2 groups was performed by 2 different surgeons. The Japanese Orthopaedic Association (JOA), pain visual analogue scale (VAS), postoperative swallowing discomfort and operation-related complications, and operation time were considered as the clinical outcomes that were performed before surgery and the routine postoperative 1 week, 3 months, and 6 months. Postoperative radiologic outcomes were measured for operated lordosis angle, subsidence, fusion rate at 6 months to compare preoperative radiologic parameter. Results: There was significant improvement in all JOA, VAS scores following surgery in both group. According to JOA at 6 months, 87.2% (group 1) and 86.4% (group 2) of patients reported excellent or good results and improved VAS scores in group 1, preoperative 8.32 ± 0.35, postoperative 6 months 2.16 ± 0.36, and 8.52 ± 0.47 preoperative, 1.83 ± 1.72 postoperative in group 2. The lordosis angle was more physiologic at 6-month follow-up in both groups. Of the 42 cases, there was no segmental instability and subsidence, and the bone fusion rate was 100% in both groups at 6 months. We found an incidence of postoperative swallowing discomfort was 13.8% in group 1, significantly lower compared with 26.5% in group 2 at first and 24 postoperative hours, respectively. One patients (1.7%) in endoscopic ACDF developed a postoperative soft tissue hematoma within the first 24 postoperative hours, which presented with dyspnea, severe difficulty in swallowing. Small pharyngeal perforation was documented in 1 patient in group 1 and was confirmed with endoscopic image during procedure. The operation time was investigated in the 2 groups. The operation time in group 1 and group 2 was 121.4 ± 35.9 and 92.5 ± 19.8 minutes. Significant difference in operation time was observed between the 2 groups (P > .01). There were no statistically significant difference in fusion rates in both groups. At follow-up, fusion rate in group 1 was 91.5%, and in group 2, it was 90.8%. Skin incision in group 1 was 1.7 cm and 4.8 cm in group 2. Conclusion: Endoscopic ACDF yields clinical benefits for CSM patients. The outcomes of follow-up showed that endoscopic ACDF was a viable surgical option for CSM patients as a less invasive technique. The limitation of this study is the relatively short follow-up time.
P459: Evidence on Long-Term Follow-up After Minimally Invasive Fusion of the Sacroiliac Joint With Triangular Titanium Implants
Jacques D. Müller-Broich1, Marcus Rickert1, and Andrea Meurer1
1Orthopedic University Hospital Friedrichsheim, Frankfurt, Germany
Introduction: About 32% of patients who complain for the first time of low back pain are affected by pathological modifications of the sacroiliac joint (SIJ). As standard for a safe diagnostic serves a 50% reduction of pain after controlled local block with anestethics. It has been calculated that pain in SIJ has a point prevalence of 25%. In connection with the clinical use of a new minimally invasive fusion using triangular titanium implants with a porous surface for reduction of rotational movements, we did a systematic analysis of the available literature to therapeutic options and safety of this principle. Materials and Methods: We used 8 publications listed in PubMed (2014-2017) on the minimally invasive fusion of the SIJ (Polly, Dehon, Capobianco, Sachs, Vanalocha, Darr, Dengler), which had clearly defined data for methods and clinical results. With same authors, we included the latest publications with the longest follow-up period. In comparative studies, only data for the trinangular titanium implants were evaluated. Results: Data of 8 studies with 960 patients (age 52years; 70% female) were compiled for the analysis. A total of 47% (39% to 62%) had prior fusions at the lumbar spine. The follow-up time was 3 × 12 months, 3 × 24 months, and 2× up to 5 years. The VAS (visual analogue scale) scores declined to the last follow-up by 63% (53% to 76%), and the ODI (Oswestry Disability Index) scores declined by 48% (44% to 73%). In some studies, positive effects for the improvement of QoL (quality of life) and patient satisfaction were listed. Follow-up/revisions surgery were necessary in very few cases. Discussion: Long-term follow-up examinations after minimally invasive fusion of the SIJ prove the significant improvement of pain and functionality as well as a high stability with triangular titanium implants.
P460: Tubular Retropleural Approach for the Microsurgical Exploration of Thoracic Disc Herniations
Vanessa Hubertus1, Julia Onken1, Ulf Schneider1, Marcus Czabanka1, Peter Vajkoczy1, and Johannes Woitzik1
1Charité University Medicine, Berlin, Germany
Introduction: Thoracic disc herniations are surgically addressed using thoracotomy, costotransversectomy, or dorsal approaches with different but considerable morbidities. We describe a new tubular retractor–assisted retropleural approach to the thoracic spine, which allows for microsurgical exploration of thoracic disc herniations. Material and Methods: The patient was positioned lateral. Following fluoroscopic identification of index level, a 3-cm skin incision was performed approximately 12-cm paramedian. The caudal rib was partially resected using diamond drill. Retropleural dissection and exposure of the ipsilateral head of the lower rib and the neuroforamen was performed using a short apnea and deflation of the ipsilateral lung. Thereafter, using fluoroscopy, a tubular retractor was positioned over disc and neuroforamen. Results: This method was hitherto used in 3 patients. In all cases, the disc herniation could be addressed thoroughly and without complication. Conclusion: This retropleural tubular approach allows for excellent microsurgical exposure to the anterior lateral thoracic spinal canal in a minimally invasive technique.
P461: Comparison of 2 Minimally Invasive Spine Surgical Techniques: Interlaminar and Transforaminal Endoscopic Discectomy
Andre Sebben1, Alynson Larocca Kulcheski1, Xavier Soler i Graells1, Pedro Grein del Santoro1, and Marcel Luiz Benato1
1Hospital do Trabalhador, Curitiba, Brazil
Introduction: Surgical techniques for the treatment of lumbar disc herniation have evolved. Among these, there is the spinal endoscopy. Of the endoscopic techniques, the most common are the transforaminal and the interlaminar. Material and Methods: Thirty-one patients underwent interlaminar technique and 24 transforaminal for the treatment of lumbar disc herniation. They were assessed by VAS (visual analogue scale) and ODI (Oswestry Disability Index) preoperatively, in the first postoperative and sixth month after the procedure. Results: We had 89.1% of good results and 10.9% of complications. Conclusion: We conclude that both endoscopic techniques are safe and effective for the surgical treatment of lumbar disc herniation.
P462: Minimally Invasive Lateral Access Lumbar Interbody Fusion: Preliminary Results
Rajeesh George1, Gamaliel Tan1, Wu Pang Hung1, Joel Lee Zhao Jie1, Low Shiong Wen1, and Ira Sun1
1Ng Teng Fong General Hospital, Singapore, Singapore
Introduction: Lateral access lumbar spinal surgery is a recently adopted surgical technique in Singapore to mitigate the risks associated with anterior and posterior lumbar spinal surgery. There is a paucity of local published literature on the outcomes of these surgeries. Objective: A retrospective review of patients in our institution who underwent lumbar interbody fusion using a minimally invasive lateral retroperitoneal approach for degenerative lumbar spinal stenosis. Methodology: All patients who underwent lateral access lumbar spinal surgery (eXtreme lumbar interbody fusion (XLIF) and oblique lateral interbody fusion (OLIF) for degenerative lumbar spinal conditions from February 2017 to July 2018 were identified and outcomes analyzed. Outcome measures reviewed included operating time, estimated blood loss, length of hospital stay, and presence of complications. Patients with infective or neoplastic lumbar spinal conditions were excluded. Published lateral access spinal surgery results were summarized and compared with current study data. Results: There were a total of 34 patients, 24 of which underwent XLIF and 10 who underwent OLIF. Among the XLIF patients, 9 underwent a single-level surgery, 12 underwent 2-level surgery, and 3 underwent 3-level surgery. Among the OLIF patients, 4 underwent single-level surgery and 6 underwent 2-level surgery. Operation duration averaged 277 minutes, and length of hospital stay averaged 5.1 days. Mean follow-up was 9.3 months. 13 out of 34 patients experienced complications (38.2%), of which 2 were infection-related, 1 was a vessel injury, 2 were implant-related, and 8 had thigh numbness. Discussion: Lateral access lumbar spinal surgery avoids the morbidity of vertebral muscular dissection from the posterior approach and allows for a larger interbody cage to be inserted for fusion. However, it is also associated with a learning curve and a higher incidence of lumbar plexus injuries and pelvic vascular injuries. The rate of complications, although higher than those in the literature, can be attributed to surgeon experience. Another advantage is the shorter hospital stay and improved pain control postoperatively. Transient thigh numbness is common but often resolves. Conclusion: Lateral access spinal surgery is a novel technique with many advantages in treating degenerative lumbar spinal disorders. Our data corroborate and contribute to the existing body of literature discussing outcomes of lateral access surgery. The short-term outcomes were generally favorable, and our institution feels that this technique should be more widely adopted. This study forms the platform for analyzing the future long-term outcomes including patient-reported pain and function scores as well as radiographic parameters and rates of fusion.
P463: Percutaneous Endoscopic Transforaminal Interbody Fusion Through Biportal Access: The Solution for Direct and Indirect Decompression by Percutaneous Endoscopy
Javier Quillo-Olvera1, Javier Quillo-Reséndiz1, Diego Quillo-Olvera1, and Dong-Hwa Heo2
1The Brain and Spine Care, Minimally Invasive Spine Surgery Center, Queretaro, Mexico
2The Leon Wiltse Memorial Hospital, Suwon, Republic of Korea
Introduction: Currently, there is a tendency to be lesser destructive with the tissues adjacent to the spine to achieve the desired result of any surgical treatment. Because that, spine surgery has evolved and together with technological development have allowed the creation of new techniques. Among these techniques, the transforaminal lumbar interbody fusion (TLIF) in patients with low back pain (LBP) and unilateral radicular symptoms due to instability has demonstrated encouraging outcomes. However, the approach is usually iatrogenic with paraspinal muscles, and sometimes preparation of the endplates is not sufficient. We decided to perform a prospective case-control study with a ninth month cohort of 10 patients who underwent a new technique of TLIF, the full-endoscopic biportal unilateral (UBE) TLIF to present our preliminary results. Material and Methods: We included 10 patients who underwent UBE-TLIF during February to May 2018. The patients operated suffered from chronic LBP treated by conservative strategies without improvement at least 8 weeks before, unstable low-grade spondylolisthesis (I or II) with mild or severe degenerative disc disease with foraminal stenosis associated, and unilateral radicular symptoms. We evaluated all patients preoperatively and postoperatively immediately after surgery and at 1, 3, 6, 9, 12, and 24 months by using the visual analogue scale (VAS) for back and leg pain. The Oswestry Disability Index (ODI) was used in the preoperative and in the ninth month along with MacNab criteria for satisfaction. The radiological outcome also was evaluated. Statistical analysis for comparing changes over the time in all the evaluations was done. Results: The 10 patients completed the 9-month assessments. Mean age was 53.24. Among the patients, 6 were female and 4 males. Four L4-L5 and 6 L5-S1 levels were operated. The mean surgical time was 16 825 minutes, and mean intraoperative bleeding was 7018 mL. All the cases were discharged on the next day. No patient required postoperative narcotics for pain control. The scores from both scales (VAS and ODI) decreased from preoperative to postoperative with statistical significance (P < .05), and MacNab criteria resulted in 9 patients referring excellent and one good outcome. Radiological evaluations showed a proper location of the cage into the intervertebral space and an appropriate direct decompression. Conclusion: Despite the small size of the sample, we concluded that percutaneous endoscopic biportal unilateral TLIF is another minimally invasive alternative for patients with low-grade spondylolisthesis with axial and unilateral radicular symptoms associated. All patients showed good short-term clinical results in the cohort at 9 months. We should still wait for the results of 24 months to evaluate the fusion status. However, the direct visualization of the neural elements, excellent preparation of the endplates with direct visualization through the endoscopic portal and minimum postoperative pain are some advantages observed in our study.
P464: Percutaneous Minimally Invasive Pedicle Screw Fixation for Hangman’s Fracture Using Intraoperative 3-Dimensional Fluoroscopy
Guofeng Bao1 and Zhiming Cui1
1The Second Affiliated Hospital of Nantong University, Nantong, China
Introduction: The traditional operation method for Hangman’s fracture is open reduction with cervical 2/3 fusion, but with the help of intraoperative 3-dimensional (3D) image, we can fix the fracture with minimal invasive method. To investigate the accuracy and feasibility of percutaneous axial pedicle screw fixation based on 3D intraoperative fluoroscopy in the treatment of Hangman’s fracture. Material and Methods: From November 2015 to November 2016, 12 patients with Hangman’s fracture underwent percutaneous pedicle screw fixation under O-Arm guidance, 4 of which underwent unilateral pedicle screw fixation. In the same period, 10 patients underwent posterior cervical 2/3 fusion fixation under the guidance of C-Arm. Operation time, radiation dose, blood loss, screw accuracy, and neck pain visual analogue scale (VAS) 6 months after the surgery were recorded. Results: The operative time was 84.2 ± 8.9 minutes and 159.3 ± 30.8 minutes, respectively (P < .05), and the blood loss was 46.9 ± 5.8 mL and 269.0 ± 121.4 mL (P < .01) in 2 groups, respectively. All 60 screws were implanted without screw-related neurovascular injury. The percentage of the screws assessed as level 1 by CT (computed tomography) scan after surgery in both groups was 85% (17/20) and 80% (32/40; P > .05). The neck pain VAS of preoperative, postoperative 10 days, and postoperative 6 months were 5.4 ± 1.4, 2.0 ± 1.1, 0.5 ± 0.4, 5.6 ± 1.5, 3.2 ± 1.8, and 1.2 ± 0.7 (P > .05, P < .05, and P < .01). The intraoperative radiographic doses were 6.1 ± 0.7 mGy and 0.5 ± 0.4 mGy, respectively (P < .01). Conclusion: Combined minimally invasive with 3D intraoperative fluoroscopy techniques applied for the safe and accurate treatment of Hangman fractures with minimal invasive surgical stripping, better control of neck pain, preservation of motion segments, and blood loss compared with the traditional open C2/3 fusion surgery.
P465: Multilevel Percutaneous Pedicle Screw Fixation for Adult Degenerative Lumbar Scoliosis by a Single Surgeon: Preliminary Report
Sang Gu Lee1
1Gachon University Gil Medical Center, Incheon, Republic of Korea
Introduction: Minimally invasive deformity correction and fusion remains an exciting field of spine surgery. Traditional surgical approaches for adult scoliosis are associated with significant blood loss and morbidity, in elderly patients with multiple medical comorbidities. Percutaneous screw fixation in the deformity correction is a promising approach to spinal deformity surgery where deformity correction and fusion can be achieved with less tissue trauma, reduced blood loss, and potentially less complications. Material and Methods: This was a retrospective study of 16 consecutive patients who underwent minimally invasive correction and fusion over 3 or more levels for adult scoliosis under single spine surgeon. Functional outcome data were collected at each visit and at the last follow-up. All radiological measurements were obtained using standardized computer measuring tools. Results: All patients underwent MIS (minimally invasive surgery) without conversion to a traditional open procedure. The mean age of the patients in the study was 65.9 years (range = 55-81 years), with a mean follow-up time of 18.5 months. The preoperative Cobb angle was 13.5 ± 6.5°, which corrected to 3.1 ± 2.9°. All patients maintained correction of their deformity and were noted to have solid arthrodesis on plain radiographs. Lumbar lordosis between L-1 and S-1 improved from a mean of 30.7 ± 13.6° to one of 35.6 ± 12.2°. Sagittal vertical axis improved from 5.6 cm to 4.1 cm. The mean preoperative visual analogue scale and Oswestry Disability Index scores were 7.6 ± 0.9 and 51.1 ± 10.3; postoperatively these were 3.6 ± 1.1 and 29.0 ± 12.3, respectively. In terms of major complications, 2 patients had screw failure due to osteoporosis, 1 patient had transient acute renal injury, and 1 patient had an unlocked set screw. Conclusion: Although percutaneous screw fixations are limited surgery in the adult degenerative lumbar deformity, minimally invasive surgical correction of adult scoliosis results in favorable surgical outcomes similar to traditional surgical approaches. Meticulous surgical technique and careful patient selection are required for good results and to avoid complications. Although further studies are needed, the percutaneous screw fixation for adult degenerative lumbar deformity may be particularly useful in the elderly.
P466: Uniportal Endoscopic Interlaminar Approach as a Treatment of Lumbar Spinal Stenosis
Angela Carrascosa Granada1, Willian Velazquez2, Ralf Wagner3, and Andres Vargas1
1Department of Neurosurgery, Madrid, Spain
2Department of Neurosurgery, Salta, Argentina
3Ligamenta Spine Center, Frankfurt, Germany
Introduction: Degenerative spine disease leading to lumbar spinal stenosis is a major cause of morbidity among the elderly. The spinal surgery used for the decompression of the spinal canal is considered as an effective treatment to improve walking ability. The use of microsurgical techniques has reduced tissue damage and its consequences. In this article, we present a technique for a fully endoscopic bilateral decompression of lumbar spinal stenosis performed through a 10-mm incision using a high-definition uniportal endoscope. Methods: We present our first cases series with 9 patients whom underwent endoscopic decompression. Inclusion criteria were neurogenic claudication, failure of conservative treatment in past 3 months, and evidence of central lumbar stenosis in MR (magnetic resonance). Exclusion criteria were degenerative spondylolisthesis grade II or higher, degenerative scoliosis greater than 30 grades, significant axial back pain, no spinal surgical history, and segmental instability on dynamic radiographs. They were evaluated with VAS (visual analogue scale), ODI (Oswestry Disability Index), and JOA (Japanese Orthopaedic Association Score), in pre- and postsurgical stage at 1, 3, and 6 months of follow-up and spinal cross-sectional area (SCSA) at axial cuts of T2-weighted MR and Walking Claudication Distance (WCD) in presurgical stage and at 6 months. Results: A total 9 patients were enrolled in this study with 1-year of recruitment period. A total of 11 levels were decompressed: 1 L2-L3, 2 L3-L4, and 8 L4-5. The median age of patients were 77 years, and male–female ratio was 1:1.25. The mean of surgical time was 125 minutes and of blood loss of 18 mL. No complications were found. The median of presurgical VAS was 8/10. The median postsurgical VAS at 1 month was 1/10, at 3 months 1/10, and at 6 months was 0/10, with a significant difference (P ≤ .01). The median of presurgical ODI was 49%. The median postsurgical ODI at 1 month was 24%, at 3 months 12%, and at 6 months 6%, with a significant difference (P ≤ .01). The median of presurgical JOA was 7/29. The median postsurgical JOA at 1 month was 22/29, at 3 months 25/29, and at 6 months 27/29, with a significant difference (P = .01). The median of presurgical SCSA was 67 mm2. The median of postsurgical SCSA was 163.7 mm2, with an enlargement of the lumbar canal of 242%, with a significant difference (P ≤ .01). The median of presurgical WCD was 150 m. The median of postsurgical WCD was 3000 meters, with a significant difference (P ≤ .01). Conclusion: The endoscopic interlaminar approach for lumbar spinal stenosis is a safe minimally invasive technique with good clinical results than offers a good decompression of lumbar spinal canal, as well as maintenance and enhancement in time of follow-up in our cases series.
Reference
1. Rosen J, O’Toole JE, Eichholz KM, et al. Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery. 2007;60:503-510.
2. Wen B, Zhang X, Zhang L, Huang P, Zheng G. Percutaneous endoscopic transforaminal lumbar spinal canal decompression for lumbar spinal stenosis. Medicine (Baltimore). 2016;95:e5186.
3. Polikandriotis JA, Hudak EM, Perry MW. Minimally invasive surgery through endoscopic laminotomy and foraminotomy for the treatment of lumbar spinal stenosis. J Orthop. 2013;10:13-16.
4. Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18:61-70.
5. Asgarzadie F, Khoo LT. Minimally invasive operative management for lumbar spinal stenosis: overview of early and long-term outcomes. Orthop Clin N Am. 2007;38:387-399.
6. Cavuşoğlu H, Kaya RA, Türkmenoglu ON, Tuncer C, Colak I, Aydin Y. Midterm outcome after unilateral approach for bilateral decompression of lumbar spinal stenosis: 5-year prospective study. Eur Spine J. 2007;16:2133-2142.
7. Kalbarczyk A, Lukes A, Seiler RW. Surgical treatment of lumbar spinal stenosis in the elderly. Acta Neurochir (Wien). 1998;140:637-641.
8. Szpalski M, Gunzburg R. Lumbar spinal stenosis in the elderly: an overview. Eur Spine J. 2003;12(suppl 2):S170-S175.
9. Yuan S, Zou Y, Li Y, Chen M, Yue Y. A clinically relevant MRI grading system for lumbar central canal stenosis. Clin Imaging. 2016;40:1140-1145.
10. Lin SI, Lin RM, Huang LW. Disability in patients with degenerative lumbar spinal stenosis. Arch Phys Med Rehabil. 2006;87:1250-1256.
11. Lim YS, Mun JU, Seo MS, et al. Dural sac area is a more sensitive parameter for evaluating lumbar spinal stenosis than spinal canal area: a retrospective study. Medicine (Baltimore). 2017;96:e9087.
P467: Low-Cost Minimally Invasive Surgery for Lumbar Spine Bullet Fragment Removal: A Case Report
Felipe Mendes Ferreira1, Geraldo Vitor Cardoso BIcalho1, Marcos Antônio Ferreira Júnior1, Thiago Pereira Andrade1, and Bernardo Pinto Coelho Keuffer Mendonça1
1Hospital João XXIII and Felicio Rocho, Belo Horizonte, Brazil
Introduction: We present a case of civilian gunshot injury to lumbar spine. Patient was admitted at a public hospital where there is no traditional minimally invasive material, so we developed a low-cost minimally invasive approach to bullet fragments removal. Material and Methods: Male patient 31 years, victim of civilian gunshot at lumbar level. The bullet was located at right laminae of L5. Patient presented allodynia and paresthesia at right L5-S1 dermatome plus minor hallux extension paresis. Although without having a classical surgery indication for gunshot spinal cord injury and after formal patient’s consent, we performed a new and low-cost procedure for bullet removal after 3 days of injury. Patient was positioned on ventral decubitus under general anesthesia. After proper antisepsis, we marked a 2 cm point off midline and a 1.5-cm incision was performed. We utilized a K-wire through incision, and under fluoroscopy view, we marked the best trajectory to the bullet location. Syringes of 4 progressive diameter were inserted through the K-wire similar to tubular discectomy. After getting sufficient space, we performed a monopolar dissection exposing the laminae of L5, which was drilled. Under magnification of loupe glasses, we visualized the bullet, which was successfully removed. Results: Patient was kept in antibiotic regimen for 24 hours. In the first postoperative day, patient referred resolution of allodynia and paresthesia. Motor recovery was noted 1 week after surgery and absence of fistula in long-term follow-up. Conclusion: There are few clear indications for bullet spinal injury surgery such as neurological deterioration, infection, and cerebrospinal fluid leakage according to the latest reviews. There are no sufficient articles focusing on minor deficits and minimally invasive approach. We demonstrated technical feasibility of minimally invasive approach with cheap materials (syringes). This technique proved successful and without complications for this specific case. However, we need a large series of patients to indicate it routinely.
P468: Facet Joint Angulation in Minimally Invasive Contralateral Facet-Sparing Decompression for Lumbar Stenosis
Artsiom Klimko1 and Stefan Mindea2
1Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
2Medstar Hospital, Washington, DC, USA
Introduction: Symptomatic lumbar stenosis can often require surgical treatment if other treatment options fail. Ipsilateral lumbar decompression, especially in the mid to upper lumbar spine, may cause iatrogenic instability secondary to aggressive facet disruption or spondylolysis. We present a contralateral facet-sparing decompressive technique for lumbar stenosis that facilitates exceptional lumbar canal and nerve root decompression without the risk of iatrogenic instability, thus obviating the need for spinal fixation/fusion. We provide measurements based on 250 lumbar magnetic resonance imaging (MRI) images demonstrating that a small rostral caudal lumbar facet joint angle (FJA) limits the degree of safe facet joint disruption in surgical decompression. In this setting, the contralateral facet-sparing decompressive technique for lumbar stenosis is an excellent option for adequate decompression and minimal risk for spinal destabilization. Material and Methods: Bilateral FJAs were measured axially, at all 5 lumbar levels on MRI images of 250 patients, age 20 to 84 years. The measurement was taken as the angle between a reference line that bisects the disc center and spinous process, and a line through the anteromedial and posterolateral margins of the superior articular facet. Results: We measured 1992 facet angles from 250 patients, with average values being L1-L2: 26.96 ± 2.30°, L2-L3: 30.45 ± 2.11°, L3-L4: 38.05 ± 2.62°, L4-L5: 47.07 ± 2.31°, and L5-S1: 51.81 ± 2.15°. Furthermore, we found that with age, FJAs for the lower lumbar spine increase (eg, L5-S1 for the 20- to 30-year-old group increased from 50.67° to 53.68° for the 70- to 80-year-old group), while FJAs for the upper lumbar spine decreased (eg, L1-L2 for the 20- to 30-year-old group decreased from 31.85° to 22.83° for the 70- to 80-year-old group). Conclusion: Contralateral facet-sparing lumbar stenosis decompression is an effective surgical strategy for decompression of the lumbar nerve roots and spinal canal without inadvertent destabilization of the spine. A small angulation of the rostral/caudal facet joint can limit the degree of safe facet joint disruption in surgical decompression. Our anatomical analysis of the facet joint as measured from 250 MRI images suggests that for low facet angles (as in mid to upper lumbar spine), ipsilateral decompression can increase the risk for inadvertent lumbar instability. This important surgical complication may be successfully avoided utilizing the contralateral facet-sparing technique described in this report.
P469: Lumbar Endoscopic Percutaneous Discectomy—Clinical Outcome: Prospective Study
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler i Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Objective: Lumbar disc herniation is a common indication for surgical treatment of the spine. Open microdiscectomy is the gold standard. New surgical techniques have emerged, such as spinal endoscopy. We compared and evaluated 2 endoscopic techniques: the transforaminal and the interlaminar. Methods: Fifty-five patients underwent endoscopic technique and were assessed by the VAS (visual analogue scale) and ODI (Oswestry Disability Index) in the preoperative period, and in the first and sixth month after the procedure. Results: We had 89.1% of good results and 10.9% of complications. Conclusion: We conclude that endoscopic techniques are safe and effective for the surgical treatment of lumbar disc herniation.
P470: Evaluation of Endoscopic Lumbar Discectomy in Obese Patients
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler i Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Introduction: Obesity is a public health problem with high morbidity and mortality rates and perioperative complications in relation to the general population. Minimally invasive procedures are promising alternatives to perioperative complications in individuals with elevated body mass index (BMI). Endoscopic lumbar discectomy has been gaining popularity in this regard. However, there are few descriptions in the literature about the endoscopic approach in improving pain and quality of life in obese individuals. Similarly, it is not established whether individuals with high BMI have more complications in this type of surgical approach. Methods: A longitudinal retrospective case-control study was performed with 63 subjects submitted to endoscopic discectomy, divided into 2 groups according to BMI (Group A, BMI ≥ 30 kg/m2 and Group B <30 kg/m2), in order to compare improvement in quality of the Oswestry Disability Index (ODI) and pain improvement by the visual analogue scale (VAS), as well as to observe the incidence of postoperative complications in both groups. Results: There was no difference in postoperative ODI (P = .36) and EVA (P = .54) between groups, nor was there a statistical difference in the incidence of complications between groups (P = .56). Conclusions: Endoscopic discectomy brings similar results in pain and quality of life in obese and nonobese patients without presenting higher rates of complications.
P471: Percutaneous Contralateral Interlaminar Sublaminoplastic Approach
Cheulwoong Park1
1Daejeon Woori Hospital, Daejeon, Republic of Korea
Introduction: Percutaneous contralateral endoscopic interlaminar sublaminoplastic approach for lumbar decompression is a versatile and novel minimally invasive technique in certain specific pathologies at lumbar spine. Using the advantage of freedom to manipulate instruments with biportal endoscopy, we report a novel technique of accessing contralateral traversing and exiting nerve roots at lateral recess and foraminal region, respectively, via single interlaminar window. The purpose of this study was to determine the feasibility and efficacy of percutaneous contralateral endoscopic interlaminar sublaminoplastic surgery for treating lumbar degenerative disease. Material and Methods: We performed percutaneous contralateral endoscopic interlaminar sublaminoplastic surgery between March 2017 and August 2018. These patients were then evaluated retrospectively for their clinical and radiological outcomes. We reviewed the patients with complaints of unilateral radiculopathy with associated neurogenic claudication, patients with a diagnosis of degenerative lumbar spinal stenosis, migrating disc herniation, double root compressive lesion, facetal synovial cysts, or ossified ligamentum flavum or hypertrophied osteophytes. Results: The principle on which it is based is preservation of facet joint especially in upper lumbar levels where an ipsilateral symptomatic side approach can lead to excessive bony removal and facet instability or pars injury in an attempt for complete decompression. In this approach, because the trajectory of approach is oblique and the approach starts with a keyhole in the contralateral spinolaminar junction. By this, we also preserve the facet structure undisturbed on the contralateral side. The approach is extended on the pathologic side by removal of the lamina from underneath, thus a laminoplasty done from inside keeping the outer cortex intact. To begin with, the ligamentum flavum is also kept intact until the bony work is complete. After removal of ligamentum flavum, the lateral dural margin can be clearly identified and nerve root decompression can be completed. The contralateral keyhole can also be extended on to the lamina on lower side so as to reach the traversing nerve root more effectively. The ideal indication for this is an upmigrated extruded disc herniation at upper lumbar spine. This technique has also been effectively applied in treating double root compression involving the traversing and exiting nerve root at the same level at lower lumbar levels. One can reach and decompress the exiting and traversing nerve root without destabilizing the vertebral segment and also percutaneously through an endoscope by going from the contralateral side. This technique applied to asymmetric unilateral compression of the thecal sac at lumbar spine causing unilateral symptoms especially due to compressive pathologies coming from the dorsal elements like facetal synovial cysts or ossified ligamentum flavum or hypertrophied osteophytes arising from the facetal joints. In such cases, the advantage of using this approach is that we can clearly delineate and visualize the dural margin from the pathologic compressive tissue and thus increasing the safety of the procedure. Using instruments from the contralateral side parallel to the pathology becomes relatively easy. The key to this approach is proper planning of the contralateral keyhole or window of approach on preoperative MRI (magnetic resonance imaging) and CT (computed tomography) imaging and thus targeting precisely. Creating enough space by sufficient sublaminar bony resection is also helpful in increasing the mobility of the endoscope and instruments. The approach was initially started with a uniportal endoscopic surgery, but it can be done more effectively by biportal endoscopic approach with the same benefits as uniportal approach. Often using a hybrid approach is also practical where the bony work, and initial dissection is done by the biportal technique and subsequently replaced with uniportal endoscope for effectively decompressing the exiting nerve root. This approach is contraindicated if there is a centrally compressing disc pathology wherein it is difficult to remove from this approach, and more so ever, it is contraindicated as it can cause nerve root injury. Conclusion: Percutaneous contralateral interlaminar sublaminoplastic approach is a safe and effective minimally invasive surgical technique. In view of good clinical and radiological outcomes of patients, this procedure may be considered as a surgical technique worth further evaluation and application.
P472: The Clinical Effect of Treatment of Lumbar Degenerative Disease in Single Incision via MAST QUADRANT Minimally Invasive System
Jianzhong Huo1, Xinghua Ji1, Peng Shang1, and Zhongyi Su1
1Affiliated Shanxi DaYi hospital of Shanxi Medical University, Taiyuan, China
Introduction: To assess the possibility and clinical efficacy of treating the patients with lumbar degenerative disease by pedicle screw fixed and intervertebral fusion via MAST QUADRANT minimally invasive system in single incision. Material and Methods: A series of 60 patients with degenerative lumbar disease from July 2016 to July 2018 were enrolled and treated with pedicle screw fixed and intervertebral fusion surgery in single incision using MAST QUADRANT system (Group A) and open surgery (Group B). All surgeries were performed by the same surgeon team. Operation time, × times, intraoperative blood loss, wound drainage, length of stay, pain score, and Japanese Orthopaedic Association (JOA) were evaluated. Results: Operation time of Group A is shorter than that of Group B, but there is no statistical difference. Whether the amount of intraoperative bleeding or postoperative wound drainage of Group A is less than that of Group B. Group A requires shorter hospital stays than Group B. There is no statistical difference between pain scores and JOA scores. Conclusion: In single posterior median incision, decompression and pedicle screw fixation and intervertebral fusion surgery via MAST QUADRANT system can be successfully performed (Figures 1 and 2). In other words, patients with lumbar degenerative disease will have less pain and shorter hospital stay and fewer hospitalization costs.
Figure 1.

Preoperative film material. (A) AP (anteriorposterior) and lateral X-ray film. (B) Overextension and overflexion X-ray film. (C) CT (computed tomography) scan film. (D): L34 layer scan film shows that there is large disc herniation in left part of the canal. (E) L45 layer scan. There is a large and marginal calcified disc herniation. (F) Lumbar MRI (magnetic resonance imaging) scan film. (G) There is a large disc herniation at the L34 layer. (H) It is a large and marginal calcified disc herniation at the L45 layer.
Figure 2.
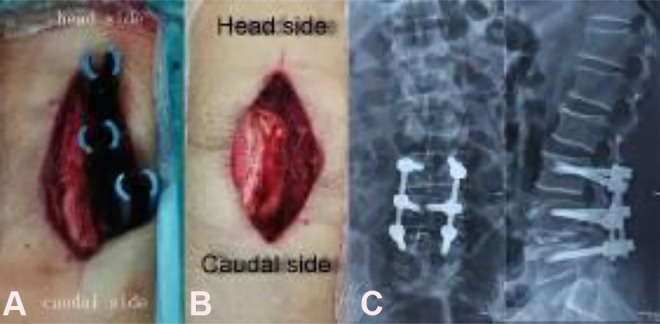
(A) After decompression and intervertebral fusion and pedicle screw fix (the nail tails have been broken) at the left, pedicle screw fix is performed at the right in the same incision. (B) Pedicle screw fix have been performed at both sides. (C) Postoperative X-ray AP film.
P473: Target Punctures Technique for Percutaneous Endoscopic Lumbar Discectomy for Highly Migrated Lumbar Disc Herniation
Xiaofeng Lian1 and Jianguang Xu1
1Shanghai Sixth People’s Hospital, Shanghai, China
Introduction: The traditional transforaminal endoscopic approaches have many limitations in the treatment of highly migrated lumbar disc herniations, such as insufficient exposure, vision limitation, and unreachable disc fragments. Some spinal surgeons suggest that this surgical method is not suitable for the treatment of highly migrated lumbar disc herniation. However, using target punctures technique, the working cannula could be inserted directly toward the disc fragments. So, in this study, we introduce a free-hand target punctures technique in percutaneous endoscopic lumbar discectomy (PELD) for highly migrated lumbar disc herniation. Methods: From June 2016 to June 2017, 32 patients with high-grade migrated lumbar disc herniation that were treated with PELD using free-hand target puncture technique in our hospital were selected, and a retrospective study was demonstrated. Among these 32 patients, there were 19 males, 13 females with an average age of 41.5 years (21-86 years old). All patients were followed-up for 18.4 months averagely (range = 12-26 months). Operative time, hospital stay, visual analogue scale (VAS), Oswestry disability index (ODI), modified MacNab criteria, and surgical complications were evaluated. Results: All 32 patients were successfully operated on and followed-up. Average operative time was 56.5 minutes (range = 32-115 minutes). The hospitalization was 2.6 days (range = 2-4 days). The VAS score decreased significantly from 5.3 ± 1.5 preoperatively to 2.4 ± 1.3 (P < .001) 1 day postoperatively, and to 0.9 ± 1.0 (P < .001) at final follow-up. The ODI score improved significantly from 23.8 ± 3.6 preoperatively to 16.4 ± .2 (P < .001) 1 day postoperatively, and to 3.3 ± 1.2 (P < .001) at final follow-up. According to the modified MacNab criteria, 22 patients (68.8%) showed excellent results, 8 patients (25.0%) were rated as good, 2 patients (6.3%) were fine; and no cases were rated as bad at final follow-up. No nerve root injury or wound infection was shown in this series. Conclusions: The free-hand target punctures technique PELD could be an effective and safe treatment of highly migrated lumbar disc herniation. It expands minimally invasive surgical options for the patients with highly migrated lumbar disc herniation.
P474: Radiographic and Clinical Outcome of Selective Fusion in Isthmic Spondylolisthesis with Multilevel Spondylolysis
Moo Sung Kang1
1Catholic Kwandong University, Incheon, Republic of Korea
Introduction: Spondylolytic spondylolisthesis that is not improved with conservative management is an indication for surgery. Considering the instability, fusion is usually performed. There are little data about treatment of spondylolisthesis with multiple-level spondylolysis. This study is to evaluate the occurrence of new-developed instability in adjacent segment with spondylolysis in the patients who underwent selective 1 segment fusion for spondylolytic spondylolisthesis. Material and Methods: From January 2004 to March 2014, 514 patients underwent fusion in the diagnosis of spondylolytic spondylolisthesis. To evaluate instability preoperative and postoperative anterior translation (%) using Meyerding method were checked in the plain dynamogram. Preoperative and postoperative sagittal rotation (°) was also compared. Clinical outcome was compared with each visual analogue scale (VAS) score of back and legs. Results: In the 514 patients with spondylolytic spondylolisthesis, 62 patients had double-level spondylolysis and 1 had triple-level. Incidence of multiple-level spondylolysis was 12.3%. Forty-nine patients underwent fusion including all spondylolysis level, and 15 patients had selective fusion for the segment with definite instability. After average of 11.7 months follow-up, preoperative and postoperative anterior translation (%) were 8.73 and 8.78, respectively. However, it was not significantly different sagittal rotation (°) showed significant increase from 4.3° to 8.4 (P = .006). Both VAS (visual analogue scale) score of back pain and radiculopathy showed statistically significant improvement (both score, P = .000). Two patients had revision surgery for radiculopathy accompanied by radiographic instability (13.3%). Conclusion: In the patients, selective fusion of spondylolisthesis with double-level spondylolysis can induce increase range of sagittal rotation in the adjacent spondylolytic segment. With strictly narrow indication, selective fusion in patients with double spondylolysis could be one viable option. Preoperative meticulous evaluation for exclusion should be needed to prevent early surgical failure.
P475: Long-Term Results of Endoscopic Lumbar Discectomy by “Destandau’s Technique” in Rural India
Roshan Bhaisare1 and Kisan Patond2
1Raipur Institute of Medical Sciences, Raipur, India
2Mahatma Gandhi Institute of Medical Sciences, Sevagram, India
Introduction: Minimally invasive (MIS) techniques in spine are being used widely. Many techniques are established and many are developing. Endoscopic disc surgery by Destandau’s technique (ENDOSPINE Karl Storz system) is a relatively new technique. Dr Destandau started it in 1993. It is gaining increasing popularity among the spine surgeons, as it is attractive for small skin incision, gentle and excellent tissue dissection, and excellent visualization. Many authors had published results of their studies using Destandau’s technique. In all these studies, the long-term follow-up is not stressed on and was somewhat missing. We conduct a prospective study of endoscopic lumbar discectomy by Destandau’s technique in rural part of India, where advance medical services are in relatively developmental state. The aim of the prospective study was to present long-term results of 10 years following endoscopic lumbar discectomy by Deatandau’s technique. Method: A total of 21 patients were selected, on basis of strict inclusion criteria including patients who underwent endoscopic lumbar discectomy by Destandau’s technique from November 2004 to March 2006. Outcome was assessed by using Prolo’s Anatomic-Functional-Economic Rating System (1986). Patients were followed-up for 10 years from the day of surgery. We had compared results of our study with studies by J. Destandau, Tomaz Lyson, Zenon Marek Jadeszko, Jan Kochanowicz, Janusz Lewko, S. Bhandari, and others. A review of similar studies was done, and results of different studies were compared. Result: Results were excellent in 17 patients (80.95%), good in 3 patients (14.28%), and fair in 1 patient (4.78%), with no poor result. In our study, 19 (90.47%) patients were able to resume their previous works/jobs, only 2 (9.52%) needed to change their jobs to light work. No patient had retired from his previous activity following operation. Conclusion: The initial and long-term results are very good for endoscopic lumbar discectomy by Destandau’s technique. Endoscopic lumbar discectomy by Destandau’s technique in properly selected patients is a safe and MIS technique. The key is selection of patients.
P476: Endoscope-Assisted Anterior Lumbar Interbody Fusion With CT-Guided Image-Navigated Unilateral Cortical Bone Trajectory Screw Fixation in Managing Adjacent Segment Disease in L5/S1: A Technical Note
Vit Kotheeranurak1 and Jin-Sung Kim2
1Queen Savang Vadhana Memorial Hospital, Sriracha, Thailand
2Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
Introduction: Adjacent segment disease (ASD) after spinal fusion can be found as common as up to one fourth of the patients. The mainstay of the treatment of ASD consists of achieving an adequate decompression of neural elements and providing subsequent extension of the fusion if instability is established, typically done through posterior approach via the old scar and incision. We described a novel technique in managing the patient with ASD at the L5/S1 level. Material and Methods: Authors performed an endoscope-assisted anterior lumbar interbody fusion (ALIF) with computed tomography (CT)-guided image-navigated unilateral cortical bone trajectory (CBT) screw fixation to treat L5/S1 intervertebral disc pathology. Results: Patient was successfully treated by a direct endoscopic decompression through the anterior access, interbody fusion using ALIF cage, unilateral CBT instrumentation under CT-guided image navigation. The follow-up CT scan showed solid fusion and the index level. Conclusion: This minimally invasive technique is effective in terms of decompression and fixation. It could be used as an alternative method to treat patient with L5/S1 ASD.
P477: Preliminary Report on 1-Year Follow-up of a Series of Ethanol Gel Chemonucleolysis: Prospective Study
Kajetan Latka1 and Dariusz Latka1
1University Hospital in Opole, Opole, Poland
Introduction: Chemonucleolysis with chymopapain—an enzyme extracted from papaya—became an effective treatment for symptomatic lumbar disc protrusion in 1960s. This procedure, introduced by Lyman Smith, was based on needle intervertebral disc administration of an enzyme that selectively decomposes the mucopolysaccharides of the nucleus pulposus causing the disc to shrink and relieve of symptoms. Its effectiveness, according to some studies (including prospective randomized trial), reached 90%. This method was used until the beginning of the 21st century, when it was suddenly withdrawn from the market. The official reason was high risk of complications—anaphylactic reaction and intervertebral subsidence. Since 2007 the new alternative is available—alcohol gel chemonucleolysis. The idea of its action mechanism is the same as in classic chemonucleolysis but without any potential threats. Although this method has been used for over 9 years, there are still very few studies determining its effectiveness. Material and Methods: The single-center prospective study was conducted from November 2017. Patients with protrusion of the intervertebral disc diagnosed in MRI (magnetic resonance imaging) with symptoms of sciatica and were qualified for the procedure. All of these procedures were commercially funded by patients. Till now there are 30 patients in the observation group with 12-month follow-up. Each patient was evaluated before the procedure (baseline) and at 1, 3, 6, and 12 months after the procedure, using the visual analogue scale (VAS) score for pain and the Core Outcome Measures Index (COMI) questionnaires. Results: The average COMI score before the procedure was 6.86. Twenty-six out of 30 patients had significant reduction of lumbar and radicular pain at 1, 3, and 6 months after the procedure. The average COMI score improvement was 2.86 after 4 to 6 weeks, 1.58 after 2 to 3 months, and 1.92 after 6 months. There was only one case of symptomatic adjacent level disc herniation (also treated with ethanol gel injection). No other complications were reported. Conclusion: Although our study is still at the very early stage and the follow-up is short, ethanol gel chemonucleolysis seems to be safe and effective alternative for classic surgical decompression in symptomatic lumbar spine disc protrusion. The observation group and follow-up in our study continues to enlarge, and we hope that soon we will be able to clearly determine the effectiveness of this method.
P478: Unilateral Instrumentation in MIS-TLIF for Grade I Degenerative Spondylolisthesis
Xiaofeng Lian1, Yiheng Liu2, and Jianguang Xu1
1Shanghai Sixth People’s Hospital, Shanghai, China
2Haikou Orthopedics and Diabetes Hospital, Haikou, China
Introduction: The aim of this study is to compare the clinical and radiographic outcomes of unilateral versus bilateral instrumentation in minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for grade I degenerative spondylolisthesis. Methods: Between January 2014 and June 2016, 63 patients with single-level grade I degenerative spondylolisthesis who were treated with MIS-TLIF were retrospectively analyzed in this study. According to method of pedicle screws fixation, the patients were assigned to unilateral instrumentation group (Group A, n = 29) and bilateral instrumentation group (Group B, n = 34). Both groups were followed-up for an average of 28.8 months (range = 24-54 months). Clinical outcomes were evaluated using the visual analogue scale (VAS), Oswestry Disability Index (ODI), and Japanese Orthopaedic Association (JOA) scores. Radiographic outcomes included percentage of vertebral slippage, focal lordosis, and disc height. The clinical and radiographic outcomes were compared between the 2 groups. Results: The average operative time and blood loss during surgery was significantly less in group A than that in group B (P < .001, both). Clinical outcomes depicting as VAS, ODI, and JOA scores were significantly improved postoperatively in both groups. There was no obvious difference of clinical outcomes between the 2 groups at the same follow-up time point. Spondylolisthesis, disc height, and focal lordosis were significantly improved postoperatively in both groups. Postoperative vertebral slippage and focal lordosis were significantly better in group B than that in group A (P < .01). There was no significant difference of postoperative disc height between the 2 groups (P > .05). Incident rate of surgical complications was similar in 2 groups, but in group B, the complication seemed more severe because of 2 patients with neurological symptoms at contralateral side. Conclusions: MIS-TLIF with unilateral instrumentation provides comparable clinical outcomes as with bilateral instrumentation. Better vertebral slippage and focal lordosis reduction do not necessarily indicate better clinical outcomes.
P479: Differences Between Men and Women in Outcomes of Decompression Alone for Lumbar Spinal Stenosis With Degenerative Spondylolisthesis
Akira Miyauchi1, Shin-ichi Saka1, Yoshifumi Fuse1, and Kobun Takazawa1
1Saka Midorii Hospital,– Hiroshima, Japan
Introduction: Less/minimally invasive decompression alone provides satisfactory surgical outcomes for lumbar spinal stenosis (LSS) with degenerative spondylolisthesis (DS). However, it is unknown whether sex (male/female) affects surgical outcomes. Material and Methods: Patients with ≥10% slip in the neutral position on a standing radiograph were diagnosed with DS. We enrolled 56 patients that had LSS with DS at L4/5 who had undergone microscopic decompression alone. After 3 years of follow-up, we performed a retrospective review. Two patients who required reoperation, 1 man and 1 woman, were excluded, and the study included 17 men and 37 women. Clinical symptoms and standing radiographic findings were evaluated and compared annually in men versus women. We determined the following: Japanese Orthopaedic Association (JOA) score (15 points); visual analogue scale (VAS) for low back pain (B-VAS: 0-10 points, with 10 indicating the most severe pain); VAS for leg symptoms (L-VAS: 0-10 points for pain and 0-10 points for numbness, with 20 indicating the greatest symptom severity); the slipping rate (% slip) at each position (flexion, neutral, and extension); and for mobility, the % slip difference between flexion and extension (▵%slip) and the range of motion (ROM) at L4/5. Results: There were no differences in men versus women in age, symptom duration, and preoperative clinical symptoms. Preoperative % slip at each position was higher in women than in men (P < .01 for each position); however, mobility did not differ between men and women. In men, the JOA score and L-VAS improved 1 year post-surgery (P < .01) but did not change subsequently. B-VAS decreased 1 year and from 1 to 2 years post-surgery (P < .01 and P < .05, respectively). Interestingly, the % slip decreased from 1 to 2 years post-surgery in a neutral position (P < .05); otherwise, the % slip did not change at any position during follow-up. Mobility did not change during follow-up. In women, the JOA score improved 1 year and from 2 to 3 years post-surgery (P < .01 for both). B-VAS decreased 1 year and 1 to 2 years post-surgery (P < .01 for both), and L-VAS decreased each year (P < .01 each year). The % slip at each position increased 1 year post-surgery (P < .01 at all positions) but did not change subsequently. ROM decreased from 2 to 3 years post-surgery (P < .05); otherwise, mobility did not change during follow-up. In men versus women, L-VAS was lower in men until 2 years post-surgery (P < .05 each year); otherwise, the clinical symptoms did not differ between men and women. The ▵% slip was lower in men 1 year post-surgery; otherwise, mobility did not differ between men and women. Conclusion: Decompression alone for LSS with DS causes slip progression more frequently in women than in men until 1 year post surgery; however, no further slip progression and restabilization can be expected after that in both. As a result, clinical symptoms may improve earlier in men than in women, and less/minimally invasive decompression alone ultimately can relieve clinical symptoms to the same extent in men and women.
P480: Changes in the 3D Geometry of the Neuroforamen Induced by Percutaneous Cement Discoplasty
Peter Endre Eltes1, Laszlo Kiss1, Ferenc Bereczki1, Gabor Jakab1, Peter Pal Vagra1, and Aron Lazary1
1 National Center for Spinal Disorders, Budapest, Hungary
Introduction: Minimally invasive procedures are the preferred surgical method in case of elderly patients for symptomatic degenerative disc disease of the lumbar spine because standard surgical treatments are often limited due to severe comorbidities. The percutaneous cement discoplasty (PCD) technique was introduced by our institution to treat dynamic, vertical instability of the symptomatic, severely degenerated lumbar segment. The aim of this study is to measure the changes in 3-dimensional (3D) geometry of the neuroforamen, which might occur during the procedure of injection of bone cement (polymethylmethacrylate [PMMA]) into the vacuum disc space via a posterolaterally positioned Jamshidi needle. Methods: We used pre- and postoperative thin-slice computed tomography (CT) images of patients (n = 10, age: 78.5 ± 6.0 years) who underwent PCD to determine the pre- and postoperative geometries of the neuroforamen using a 3D segmentation procedure. We compared the 3D geometries represented by triangle surface meshes with Reverse Engineering, and Computer-Aided Design (CAD) algorithms, using Mimics Innovation Suite 21 software (Materialise, Leuven, Belgium) Results: We detected a significant increase of the neuroforaminal volumes (2659 ± 1851 mm3) in the PCD-treated segments (P < .05). Furthermore, we found a significant positive correlation between the injected cement volume and the geometrical changes of the neuroforamen (P < .01). Conclusions: In this article, we proved the indirect decompression effect of PCD procedure using an in silico simulation method. The biomechanical effect of the surgical procedure can be directly related to the favorable clinical result.
Acknowledgement
This study was funded by the Hungarian Scientific Research Fund, Grant No. 123884.
P481: Contralateral Sublaminar Endoscopic Approach for Removal of Lumbar Juxtafacet Cysts Using Percutaneous Biportal Endoscopic Surgery: Technical Report and Preliminary Results
Dong Hwa Heo1 and Choon Keun Park1
1The Leon Wiltse Memorial Hospital, Suwon, Republic of Korea
Introduction: Lumbar extradural cystic lesions such as juxtafacet cysts are one of reasons of radicular pain of legs. Microscopic removal of cystic lesions is usually the treatment of choice. Laminotomy and partial facetectomy can induce postoperative back pain and iatrogenic instability. Contralateral sublaminar endoscopic approach may minimize facet violation and visualize dura and cystic lesions during operation. The purpose of this study is to introduce surgical technique of contralateral sublaminar endoscopic removal of lumbar juxtafacet cysts using percutaneous biportal endoscopic approach and present preliminary clinical and radiologic results. Materials and Methods: The authors consecutively treated 11 patients with lumbar juxtafacet cysts using contralateral sublaminar endoscopic approach using percutaneous biportal endoscopic surgery. Postoperative magnetic resonance imaging (MRI) was evaluated on postoperative day 1 for optimal removal of cyst and neural decompression status. Demographic characteristics, histopathologic diagnosis, distribution of operation level, operative time, and surgical complications were investigated. Clinical findings were evaluated in the preoperative and postoperative periods using the visual analogue scale (VAS) for the legs and the Oswestry Disability Index (ODI). Results: A total of 11 lumbar juxtafacet cysts in 11 patients were treated using contralateral sublaminar biportal endoscopic approach. Postoperative MRI (magnetic resonance imaging) depicted complete removal of juxtafacet cyst and optimal neural decompression of the treated segments in all patients. Preoperative VAS and ODI scores improved significantly after surgery: VAS scores from 8.12 ± 0.63 preoperatively to 2.79 ± 1.24 at the last follow-up visit (P < .05) and ODI scores from 45.65 ± 12.97 to 15.41 ± 9.07 (P < .05). Conclusions: The authors can achieve complete removal of lumbar juxtafacet cyst using contralateral sublaminar approach by percutaneous biportal endoscopic surgery. In right of this study, contralateral sublaminar approach using percutaneous biportal endoscopy may be an alternative treatment for symptomatic lumbar juxtafacet cysts. This approach may minimize iatrogenic facet violation and traumatization of posterior muscle and ligamentous structures.
P482: Analysis of Dural Sac Cross-Sectional Area Before and After Percutaneous Laser Disc Decompression
Ricardo P. Saick1, Leonardo F. Bocca1, Franz J. Onishi1, Samuel Salu1, Vinicius M. Benites1, Daniel A. Paz1, Eduardo A. Iunes1, Thiago Salati1, Sérgio Cavalheiro1, Feres Chaddad Neto1, and Ricardo Silva Centeno1
1Universidade Federal de Sao Paulo, São Paulo, Brazil
Introduction: Chronic back pain is widely prevalent in the all populations, especially in older ages. Some longitudinal studies show up to 80% of incidence over life. The etiology of back pain can be challenging and difficult to treat. Changings in biomechanical function of intervertebral discs associated with aging and other factors may deform the lumbar intervertebral discs leading to protrusion. The degenerated disc may be the source of pain (discogenic pain), and it may continue to disc herniation and neural radicular compression and, finally, other articular processes eventually will provide vertebral arthrodesis. Some minimally invasive techniques like percutaneous laser disc decompression (PLDD) were created aiming to reduce the disc volume and subsequently reducing the spinal vertebral canal compression. The disc volume reduction leads to lower pain intensity. Material and Methods: The study seeks to analyze the differences between the spinal vertebral canal cross-sectional areas before and after the PLDD in the level of the worst stenosis. The results intend to provide anatomical basis for the technique. A retrospective longitudinal study was performed using data collected from 15 lumbar PLDD before and after the surgeries. All patients were submitted to 1.5 Tesla magnetic resonance imaging (MRI) before and after the procedure. Cross-sectional area on the level of the treated disc was obtained using Eximius software. The main goal was to measure the difference between the areas using a statistically significant P < .05. Results: There is a mean gain of 14.5% of cross-sectional area including all patients, with a better result among women (increase of 16.8%). The difference was statistically significant, with P < .001. Conclusion: There was a significant decrease in the vertebral canal sectional area. The method is safe and had no immediate complication. Over the outpatient follow-up, 2 patients had secondary pain worsening, one female patient had nucleus pulposus extrusion after a fall and another female patient evolved to discitis. When well indicated, the technique reduces the disc prolapse and can be a bridge to more invasive procedures like discectomy and vertebral fusion.
P483: Contralateral Sublaminar Approach for Lumbar Degenerative Disease Using Percutaneous Biportal Endoscopic Surgery: Clinical and Radiological Results
Dong Hwa Heo1 and Choon Keun Park1
1The Leon Wiltse Memorial Hospital, Suwon, Republic of Korea
Introduction: Recently, percutaneous endoscopic contralateral interlaminar or sublaminar approaches have been attempted for lumbar degenerative disease. Preservation of facet joint was one of the benefits of contralateral approaches. Foraminal lesion and migrated disc herniation were recommended indications of endoscopic contralateral approaches. The authors have treated patients with unilateral radicular pain using biportal endoscopic contralateral sublaminar approaches. The purpose of this study is to analyze the early clinical and radiologic outcomes of percutaneous contralateral sublaminar approaches using biportal endoscopic systems. Materials and Methods: Fifty consecutive patients with unilateral lower limb radiculopathy have underwent percutaneous endoscopic contralateral sublaminar approaches. Fifty patients were treated by biportal approach. We analyzed clinical outcomes using the Oswestry disability Index (ODI) and visual analogue scale (VAS) of leg. Postoperative magnetic resonance imaging (MRI) was investigated for completeness of neural decompression and removal of pathologic lesions. Demographic characteristics, diagnosis, distribution of operation level, operative time, and surgical complications were investigated. Results: Percutaneous endoscopic contralateral sublaminar approaches can precisely demonstrate contralateral traversing root as well as exiting nerve root. Pathologic lesions were also clearly demonstrated and completely removed by contralateral sublaminar approaches. Postoperative MRI depicted complete neural decompression and facet joint preservation. Operation levels were distributed from L1-2 to L5-S1. There were 25 cases of migrated herniated disc, 16 cases of foraminal herniated disc, and 9 cases of foraminal stenosis. Lower extremity radicular pain was relieved after surgery. Preoperative ODI and VAS scores of leg were significantly improved after surgery (P < .05). There was no significant complication related with surgical approaches. Only one patient needed revision surgery for remnant disc materials and instability. Conclusions: Percutaneous endoscopic contralateral sublaminar approaches may be a safe and useful technique for foraminal lesion, upper lumbar lesion, and migrated disc herniation. The author obtained acceptable clinical and radiologic outcomes through endoscopic contralateral sublaminar approaches. In right of this study, contralateral sublaminar approach using percutaneous biportal endoscopy may be an alternative treatment for symptomatic lumbar degenerative disease. This approach may minimize iatrogenic facet violation and traumatization of posterior muscle and ligamentous structures.
P484: Splitting of the Semispinalis Capitis Muscle as a Less Invasive Approach for Atlantoaxial Fusion: A Technical Note
Alexander Spiessberger1, Alexandra Stauffer1, Fabian Baumann2, Serge Marbacher1, Karl F. Kothbauer2, Javier Fandino1, and Bernhard Moriggl3
1Kantonsspital Aarau, Aarau, Switzerland
2LUKS, Lucerne, Switzerland
3Medical University of Innsbruck, Innsbruck, Austria
Introduction: Atlantoxial fusion with screw rod constructs traditionally requires subperiosteal dissection of the C1/C2 muscle attachments, which may lead to postoperative axial neck pain and intraoperative blood loss. We evaluate a potentially less invasive, muscle splitting approach for atlantoaxial fusion in a cadaver model. Material and Methods: A technical feasibility study was performed in a human cadaveric specimen with standard surgical instruments and an operating microscope. Surgically relevant anatomical structures as well as final exposure of the C1, C1/C2, and C2 screw entry points are demonstrated. Results: Following a midline skin incision, blunt mobilization, and downward retraction of the trapezius and splenius capitis muscle is followed by a longitudinal split of the semispinalis capitis muscle. At the lower border of the rectus capitis posterior major and the obliquus capitis inferior muscle the entry points for C1 lateral mass, C1/C2 transarticular and C2 pedicle screw are exposed. Conclusion: Minimal invasive splitting of the semispinalis capitis muscle allows adequate exposure of the screw entry points of C1, C1/C2, and C2 while preserving the intrinsic muscles of the back at the craniocervical junction.
P485: Percutaneous MIS Fixation of Cervical Facetal Dislocation Using Cervical Pedicle Screws and Percutaneous MIS Fixation of Thoracolumbar Fracture: A Technical Note
Varun Agarwal1
1Rohilkhand Medical College, Bareilly, India
Introduction: Microendoscopic techniques are being increasingly used in management of degenerative disorders of the spine. As the experience with these have grown, the use have extended to use not only in lumar and cervical spine degeneration but also minimally invasive fixations. We present a report extending the indication yet further of minimally invasive (MIS) fixations in complex trauma by MIS reduction and fixation of cervical spine dislocation using tubular retractors and cervical pedicle screws and simultaneous percutaneous MIS fixation of thoracolumbar fracture in same patient. Material and Methods: A 45-year-old male presented with a fall of heavy object over the neck and back 10 days back with inability to move B/L lower limb and loss of bowel and bladder function. X-rays and CT (computed tomography) scan revealed compression fracture of L1 vertebra with unifacetal dislocation C6 and C7 vertebra. MRI (magnetic resonance imaging) scan of cervical spine revealed grade 1 spondylolisthesis C6 over C7 with rupture of PLL (posterior longitudinal ligament) and dislocation of right facet joint and dorso limbor spine revealed unstable fracture L1 involving anterior and middle column with retropulsion of posterior fracture fragment causing spinal canal stenosis with compression on the conus medullaris. The MIS technique using tubular retractors (Quadrant, Medtronic, Memphis, TN) was used to reduce the cervical dislocation and simultaneous fixation with cervical pedicle screws to avoid any further damage to the natural stabilizing structures of the cervical spine. Percutaneous MIS fixation of L1 fracture was done simultaneously in the same sitting. Results: There were no intraoperative surgical complications. Neurological recovery started from day 2 itself. The patient was put on hard Philadelphia cervical collar. The patient was discharged on day 14 with neurological recovery at 4/5 and bowel and bladder recovery. Conclusion: MIS techniques can be a viable alternative in complex trauma to the spine in experienced hands, avoiding minimal dissection and damaging natural stabilizing spine structures.
P486: Long-Term Clinical and Radiological Follow-Up After AECD: Case Report
Dong-Hyun Bae1, Ju-Wan Seuk1, Sang-Ho Lee1, and Junseok Bae1
1Wooridul Spine Hospital, Seoul, Republic of Korea
Introduction: Anterior endoscopic cervical discectomy (AECD), using a laser and microforceps for cervical intervertebral disc herniation, has been regarded as an effective treatment modality in selected cases. However, many spine surgeons have worried about the postoperative instability, disc space narrowing, and segmental kyphosis of the cervical spine after discectomy without fusion. Material and Methods: We report 2 cases who underwent AECD at least 19 years ago and present the course of the patients. These cases had cervical intervertebral disc herniation, and they underwent AECD that removed selectively ruptured particle only. Results: In both cases, the symptom was improved after AECD, and the patients were not admitted to the hospital with any problems until now. In the radiological evaluation, it was confirmed that the area where AECD done was stable and disc height was preserved. Furthermore, sagittal alignment and segmental motion of the cervical vertebra were maintained. Conclusion: Good clinical results have been shown over the long term, as seen in the 2 cases mentioned above. Disc height was not significantly different from before surgery, and it turned out that there is no need to worry about adjacent segmental disease after surgery such as anterior cervical discectomy and fusion. Thus, AECD can be considered as a good alternative treatment option that compared with standard ACDF in well-selected cervical intervertebral disc herniation patients.
P487: Full-Endoscopic Decompression for Lumbar Stenosis With Uniportal Bilateral Interlaminar Approach: Preliminary Report
Seyi Chen1
1Chung-Shan Medical University Hospital, Taichung, Province of China
Introduction: The place of endoscopic lumbar discectomy for herniation disc is beyond doubt. For lumbar stenosis, endoscopic decompression method is developing, though decompression or fusion surgery remains the mostly performed operation. Method: Twenty patients with 32 levels of lumbar stenosis were operated with endoscopic decompression. Preoperative and postoperative visual analogue scale (VAS) score, ability of walking, and patient satisfaction were evaluated. All patients were reviewed for at least 12 months. Result: The symptom of claudication and paresthesia were relieved immediately after operation in all patients. Mean preoperative VAS score was 7.8, and became 2.4 postoperatively. No patients need further fusion nor decompression surgery. Conclusion: Endoscopic lumbar decompression for stenosis shows noninferior result than traditional decompression and fusion surgery.
P488: Comparison of Open Decompression and Full-Endoscopic Decompression in the Management of Spinal Stenosis
Asrafi Rizki Gatam1, Harmantya Mahadhipta1, and Luthfi Gatam1
1Fatmawati General Hospital, Jakarta Selatan, Indonesia
Introduction: Until recently, open decompression is still being considered as the gold standard for management of spinal stenosis, but the evolution of minimally invasive spine device has brought new dimension in the management of spinal stenosis management. Full-endoscopic surgery has a lot of advantages in term of minimal soft tissue damage, less bleeding, less hospital stay, and earlier return to work. We tried to compare the result of open decompression and full-endoscopic decompression for management of spinal stenosis case. Methods: This is a prospective cohort study of a single spinal stenosis case without instability consisting of 30 cases of open decompression and 26 cases of full-endoscopic decompression. We evaluate the preoperative and postoperative VAS of leg pain, walking distance, Oswestry Disability Index (ODI) and 36-item Short Form (SF-36) score, intraoperative bleeding, and length of hospital stay. We observe patient until 1 year post operation. Results: The clinical parameter of VAS, ODI, and SF-36 were better in the postoperation compared with preoperation. The ODI, VAS of leg pain, and walking distance was significantly better in both group compared with preoperation with P value of .033, .04, and .035. The main difference between open and full-endoscopic decompression was the level of back pain and amount of bleeding. In the full-endoscopic group, the mean VAS for back pain was 0.7 and the amount of bleeding was very minimal, but in the open decompression, the mean VAS back pain was 3.5 and the amount of bleeding was around 75 mL. Length of hospital stay was shorter in the full-endoscopic group, which is 1.2 days compared with 3.6 days in open decompression (P = .021) Conclusion: Full-endoscopic decompression showed better early result compared with open decompression group, even though long-term study is still needed for further evaluation in clinical result. The use of full-endoscopic technique is very promising in the management of spinal stenosis, and further advancement in the technique should be available in the next future.
P489: Early Results of MIS-TLIF in High-Grade Spondylolisthesis in Adults
Vishal Peshattiwar1 and Pradhyumn Rathi1
1Kokilaben Dhirubhai Ambani Hospital, Mumbai, India
Introduction: High-grade spondylolisthesis (HGS) is characterized by slip of more than 50% or Meyerding grade 3 and above. HGS is characterized by progression due to pelvic remodeling and a more complex surgical management. Aim and Objective: There are very few reports of management of HGS by MIS-TLIF (minimally invasive surgery–transforaminal lumbar interbody fusion). Hence, our study demonstrates early results of MIS-TLIF using tubular retractor system with percutaneous pedicle screw instrumentation for HGS in adults. Method: This is a prospective study of 12 patients with HGS at a single level who underwent MIS-TLIF by a single spine surgeon in a single institute. Inclusion criteria were HGS of more than 50% slip with neurogenic claudication/radiculoptahy confirmed on radiology with symptoms refractory to conservative management. Exclusion criteria included multilevel disease, postlaminectomy lysthesis, traumatic lysthsis, spinal infection, or malignancies. Level of Study: IV. Type of Study: Prospective case series. Results: Mean age was 53 years. Mean BMI (body mass index) was 31 kg/m2. Preoperatively 7 patients had mild and 1 had severe systemic disease. Mean preoperative visual analogue scale (VAS) and Oswestry Disability Index (ODI) scores were 7 and 70.66, respectively. Mean blood loss was 147.5 mL. Lumbosacral kyphosis was corrected from 9.6° (mean) to 2.6° (mean). Mean disc height was corrected from 3.8 mm to 11.8 mm. Partial reduction to grade 1 was achieved in 10 patients and complete reduction in 2 patients. Mean operative time was 3 hours 40 minutes. Mean length of stay was 5.5 days, and none of the patients had any immediate or early postoperative complications like infection, neurodeficit, dural tear, or CSF (cerebrospinal fluid) leak. Mean postoperative VAS and ODI scores on discharge were 1.75 and 29.16, respectively. CT (computed tomography) scan at 6 months confirmed fusion in 10 patients with no violation of pedicle by any screws (Lerch grade 0) Conclusion: Early results of MIS-TLIF in HGS are promising, and it can prove to be a safe and effective treatment modality.
P490: Bowel and Visceral Complications Associated With the Minimally Invasive Anterior to the Psoas Approach for Lumbar Fusion
Tony Tannoury1, Giuseppe Orlando1, Avilash Das2, Rahul Bhale2, Molly Vora2, Kathy Chen2, and Chadi Tannoury1
1Boston Medical Center, Boston, MA, USA
2Boston University, Boston, MA, USA
Introduction: Anterior access to lumbar fusion is desirable and can be applied to a large spectrum of spinal pathologies. However, reported injuries to bowel, abdominal viscera, and ureter can be catastrophic and often lead to underutilization of the anterior lumbar approach even with the assistance of access surgeon. The lateral transpsoas approach (LLIF [lateral lumbar interbody fusion]/XLIF [eXtreme lumbar interbody fusion]) also failed to eliminate such injuries and does not allow safe access to L5-S1, and at times to L4-5 disc. Ureteral injuries and direct bowel injuries have been reported during anterior lumbar interbody fusion (ALIF; 0.17% and 0.25% to 1.6%, respectively)1,2 and XLIF/DLIF (direct lumbar interbody fusion; 0.6% and 0.41%, respectively)3-5 procedures. We report our experience with the anterolateral “anterior to the psoas” (ATP) approach that allows access to the spine from T12 to S1 under direct visualization. This study is the largest investigation into the incidence of bowel and visceral complications associated with the ATP approach. Methods: This is a retrospective review of 909 consecutive patients who underwent ATP lumbar spine fusion between 2008 and 2017. All procedures were done by 2 spine surgeons and without the assistance of access surgeon. The spine was approached from either lateral sides (if no deformity) and from the concave side for coronal deformities. For patients with a unilateral predominant symptomatic mechanical neural compression, the spine was approached from the contralateral side to achieve direct adequate decompression of the stenosed canal, lateral recess, and/or foramen. Variables collected included bowel, visceral, and ureteral injuries identified during the surgery or postoperatively. Results: We identified 909 patients (55.9% females, 44.1% males) who underwent spinal fusion using an ATP approach, and 540 patients (59%) included L5-S1 level. The average age of the cohort was 59 years. Indications for fusion included the following: lumbar spondylolisthesis with stenosis (n = 622), adult spine deformity with stenosis (n = 128), adjacent segment disease (n = 141), trauma (n = 7), pseudoarthrosis (n = 5), metastasis (n = 4), and infection (n = 2). A total of 2373 levels were fused, with a mean of 2.25 levels patient. The exposure was carried anterolaterally along the retroperitoneum and the anterior border the psoas. When exposing L5-S1, the L5 segmental vessels were typically ligated and coagulated at least 5 mm away from the common iliac tributary. Despite there were no intraoperative direct bowel injuries noted, 1 patient (0.11%) experienced a delayed onset (24-48 hours postoperatively) of bowel ischemia due to a superior mesenteric artery syndrome warranting an uncomplicated partial bowel resection. Besides, there were no visceral or direct ureter and bowel injuries encountered. Conclusions: The minimally invasive ATP approach to the spine affords a significantly safer access to the lumbar spine between T12-S1 with no encountered “ureter injuries” and “direct bowel injuries” compared with ALIF (0.17% and 0.25% to 1.6%, respectively)1,2 and XLIF/DLIF (0.6% and 0.41%, respectively).3-5 Ureteral injuries were also encountered in oblique lateral interbody fusion (OLIF; 0.3%).6 We noted 1 case of delayed bowel ischemia secondary to superior mesenteric artery syndrome, following an ATP fusion (0.1%) compared with 0.7% following OLIF6 and 0.17% following XLIF/DLIF.3-5 In our experience, ATP lumbar fusion is a promising and safer alternative to ALIF, LLIF, and OLIF.
Reference
1. Bateman DK, Millhouse PW, Shahi N, et al. Anterior lumbar spine surgery: a systematic review and meta-analysis of associated complications. Spine J. 2015;15:1118-1132.
2. Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg. 1999;91(1 suppl):60-64.
3. Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976). 2013;38:1853-1861.
4. Anand N, Baron EM, Khandehroo B, Kahwaty S. Long-term 2- to 5-year clinical and functional outcomes of minimally invasive surgery for adult scoliosis. Spine (Phila Pa 1976). 2013;38:1566-1575.
5. Hijji FY, Narain AS, Bohl DD, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 2017;17:1412-1419.
6. Woods K, Fonseca A, Miller LE. Two-year outcomes from a single surgeon’s learning curve experience of oblique lateral interbody fusion without intraoperative neuromonitoring. Cureus. 2017;9:e1980.
P491: Full-Endoscopic Lumbar Discectomy: Retrospective Study of 25 Cases
Anderson Alves Dias1, Leonardo Franco Pinheiro Gaia Franco Pinheiro Gaia1, Jorge Mauad Filho1, Rodrigo Bernardi Colombero2, Daniel Almeida Siqueira2, Bruna Luisa Palhares Gomes2, Marina Andrade Donzeli1, Ana Carolina Ribeiro Terra1, and Andréa Licre Pessina Gasparini1
1University Federal of Triangulo Mineiro, Uberaba, Brazil
2University Hospital Mario Palmério, Uberaba, Brazil
Introduction: Open discectomy is a surgical procedure that has been used for many years in the treatment of lumbar disc hernias. Percutaneous methods have been described since the early 1970s. One of these methods, the interlaminar microdiscectomy using a microscope, emerged at the end of the 1970s and gained attention due to its good results and low surgical trauma. Full-endoscopic (FE) and transforaminal (TF) surgeries emerged at the end of the 1990s following the use of endoscopy in posterolateral approach surgeries. Minimally invasive procedures have been used to minimize tissue damage. In several areas, endoscopy is already the standard treatment technique. In spine surgery, 2 techniques have been used more often—FE-TF surgery and FE interlaminar (IL) surgery. The purpose of this study is to retrospectively evaluate the outcomes of patients with symptomatic lumbar disc herniations submitted to full endoscopic (TF or IL) treatment. Material and Methods: Twenty-five consecutive patients, 18 men and 7 women, mean age of 36.2 years, were evaluated at 15, 30, 90, and 180 days after surgery through the Oswestry Disability Index (ODI) questionnaire and the visual analogue scale (VAS) of axial and lower limbs pain. Results: There was a significant improvement in ODI evaluation of patients when comparing the preoperative results with the third and sixth postoperative month (P < .05), as well as the VAS for preoperative axial pain with regard to 15, 30, and 90 days (P < .05) after surgery, and VAS for preoperative pain in the lower limbs with regard to 15, 90, and 180 days postoperatively (P < .05). Conclusion: The FE discectomy is an effective procedure that should be considered as an alternative to conventional discectomy.
Navigation
P492: Robotics in Spine Surgery: The Use of Preoperative Planning to Optimize the Outcome of Spondylolisthesis Reduction
Isador Lieberman1 and Xiaobang Hu1
1Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: Robotic-assisted spine surgery has shown promising initial results by increasing the accuracy of spinal instrumentation. However, few studies have investigated the use of robotic system in the surgical treatment of spondylolisthesis. Material and Methods: Data were retrospectively collected from consecutive patients who underwent lumbar fusion for degenerative L4-L5 spondylolisthesis. The robotic system was used to plan the placement of instrumentation in order to achieve the best reduction. Postoperative surgical and medical complications were reviewed. Radiological outcome was measured by L4-L5 anterior and posterior disc height, L4-L5 slippage, and L4-L5 segmental lordosis. Clinical outcome was measured by the change of back pain, leg pain, and Oswestry Disability Index (ODI) scores. Results: A total of 20 patients were included in this study. The patients’ mean age was 64 years (range = 43-80) and their mean BMI (body mass index) was 29.0 kg/m2 (range =19.8-42.1). Robotic-assisted placement of pedicle screws was carried out according to the preoperative planning in all patients. Postoperatively, 1 patient developed radiculopathy due to misplaced right L4 pedicle screw. All the rest pedicle screws were successfully and accurately implanted. One patient had delayed wound healing due to diabetes. At mean 17-month follow-up, the patients’ mean anterior L4-L5 disc height improved from 7.5 mm to 11.2 mm (P < .001), mean posterior L4-L5 disc height improved from 4.4 mm to 6.5 mm (P < .01), mean L4-L5 slippage improved from 8.1 mm to 4.2 mm (P < .001). The patients’ mean L4-L5 segmental lordosis improved from 18.0° to 22.4°, but the change was not statistically significant (P = .08). On average, the patients’ back pain visual analogue scale (VAS) scores improved 4.5 points (P < .001), leg pain VAS scores improved 5.6 points (P < .001), and ODI scores improved 19.7 points (P < .005). Conclusion: For surgical treatment of adult degenerative spondylolisthesis, the use of robotic system and its preoperative planning platform is associated with satisfactory outcomes.
P493: Robotic-Guided Placement of Cervical Pedicle Screws: Feasibility and Accuracy
Isador Lieberman1 and Xiaobang Hu1
1Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: It has been shown that pedicle screw instrumentation in the cervical spine has superior biomechanical pullout strength and stability. However, due to the complex and variable anatomy of the cervical pedicles and the risk of catastrophic complications, cervical pedicle screw placement is not widely utilized. The purpose of this study is to review and report our experience with robotic-guided cervical pedicle screw placement. Material and Methods: We retrospectively reviewed consecutive patients who underwent cervical pedicle screw fixation with robotic guidance using preoperative and postoperative computed tomography (CT) scans. Screw placement and deviation from the preoperative plan were assessed using the robotic system’s planning software by fusing the preoperative CT (with the planned cervical pedicle screws) to the postoperative CT. This process was carried out by manually aligning the anatomical landmarks on the 2 CTs. Once a satisfactory fusion was achieved, the software’s measurement tool was used manually to compare the planned versus actual screw placements in both axial and sagittal planes at the midpoint of the pedicle in a resolution of 0.1 mm. Medical charts were reviewed for technical issues and intraoperative complications. Results: A total of 21 cervical pedicle screws were reviewed in 4 patients. The patients’ mean age was 59 years and mean BMI (body mass index) was 23 kg/m2. No intraoperative complications that related to the placement of cervical pedicle screws were reported, and robotic guidance was successful in all 21 screws. The number of screws placed were 4 at C2, 2 at C3, 4 at C4, 3 at C5, and 4 at both C6 and C7. Postoperative CT scans showed that there were 4 pedicle screw breaches. However, all the trajectories and screw positions were clinically acceptable. In the axial plane, the left-side screw deviated from the preoperative plan by 1.1 ± 0.7 mm and the right-side screw deviated from the preoperative plan by 1.4 ± 1.3 mm. In the sagittal plane, the left-side screw deviated from the preoperative plan by 1.0 ± 0.9 mm and the right-side screw deviated from the preoperative plan by 1.2 ± 0.7 mm. Conclusion: This study indicates that robotic-guided cervical pedicle screw placement is feasible with clinically acceptable results.
P494: Predictive Accuracy of Surgical Planning Using Robotic Guidance System
Isador Lieberman1 and Xiaobang Hu1
1Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: Navigation and robotic-guided systems are being used much more often to facilitate more efficient and accurate placement of hardware during spinal surgeries. Preoperative surgical planning is a key step in the safe use of these tools. To the best of our knowledge, no studies have investigated the predictive accuracy of surgical planning using robotic guidance system. Material and Methods: Data were prospectively collected from patients who underwent instrumented spine surgery with a single surgeon. The robotic guidance system was used to plan the instrumentation in order to achieve the best possible correction, and then the plans were executed intraoperatively. The patients’ preoperative deformity, planned and postoperative corrections in the coronal and sagittal planes were collected and compared. Results: A total of 10 patients were included in this study. The patients’ mean age was 54 years (range = 13-78) and their mean BMI (body mass index) was 25.6 kg/m2 (range = 20.0-35.9). The patients’ primary diagnoses were scoliosis (5), kyphosis (2), adjacent segment degeneration (2), and spondylolisthesis (1). Preoperatively, the patients’ mean coronal Cobb angle was 24.7 ± 16.8°, and their mean sagittal Cobb Angle was 20.6 ± 16.6°. The planned coronal Cobb angle after correction was 0°, and the planed sagittal Cobb angle after correction was 32.0 ± 13.8°. Instrumentation under robotic guidance was carried out according to the planning in all patients. Postoperatively, the patients’ mean coronal Cobb angle that was achieved was 7.7 ± 3.9°, and their mean sagittal Cobb angle was 27.2 ± 12.4°. The accuracy of planning was 7.7 ± 8.0° for the coronal Cobb angle and 9.8 ± 7.5° for the sagittal Cobb angle. Conclusion: This study indicates that the use of preoperative planning and robotics facilitates the surgical plan with a high degree of accuracy.
P495: Problems of Spinal Pedicle Screw Insertion Using Cone Beam CT and Spinal Navigation System in Hybrid Operating Room
Ryoji Yamasaki1, Kenta Ariga1, and Eiji Wada1
1Osaka Police Hospital, Osaka, Japan
Introduction: The number of institutions using computed tomography (CT)-like image captured by cone beam CT (CBCT) in hybrid operating room for spinal surgery is increasing. It is not well known that the influence of metal artifact is stronger in CBCT than multidetector CT, and the pedicle screws (PS) are seen to be enlarged compared with the actual size and affect the evaluation of PS diameter. The purpose of this study is to investigate the influence of metal artifact to PS in CBCT. Material and Methods: A total of 274 PS (108 cervical PS, 166 thoracic and lumbar PS) inserted using the navigation curve (Brainlab) that is linked with the angiographic imaging apparatus Artis zeego (Siemens) were evaluated. These 2 devices enable automatic registration. Three-dimensional image analysis software Synapse Vincent (Fujifilm) was used to reconstruct the slice arbitrarily in the PS insertion direction, and the PS transverse diameter was measured and compared with the actual size. Results: The actual size of cervical PS was 4.0 ± 0.4 mm, and the measured size was 5.1 ± 0.9 mm in CBCT. The measured size in CBCT was significantly larger (P < .01). The actual size of thoracic and lumbar PS was 6.4 ± 0.7 mm, and the measured size was 8.5 ± 1.4 mm in CBCT, the measured size in CBCT was significantly larger (P < .01). The enlargement ratio was 130.6 ± 20.5% on average, and correlation was found between the actual size of PS and the measured size (P < .001, r = .8192, R 2 = .7186). In the case of cervical spine, 11 PS in CBCT were judged to misplacement (grade 2 = 3, grade 1 = 8), but 5 PS in postoperative multidetector CT were judged to misplacement (grade 2 = 2, grade 1 = 3). A 54.5% of cervical PS measured in CBCT was evaluated as misplacement incorrectly. Conclusion: The size of PS evaluated in CBCT was observed to be significantly larger than the actual size. Although it was not a problem with PS insertion of thoracic and lumbar spine, even a slight misplacement may lead to nerve and vascular injury in cervical spine. The maximum magnification of cervical PS in this study was 198%. We think that the number of inserted PS and the presence or absence of rods and transverse connectors influence metal artifact and the enlargement ratio of PS. Therefore, if the position of inserted PS is checked in CBCT during operation, it should be evaluated before rod connection. It is also useful to confirm the trajectory using 1-mm diameter K-wires. When performing spinal surgery using CBCT in hybrid operating room, the influence on metal artifact should always be considered.
P496: Assessment of Spinal Column Stability for Image-Guidance After Lateral Corpectomy
Jerald Redmond1, Julien Prevost1, Daniel Woods1, and Ripul Panchal2
1Medtronic Spine, Memphis, TN, USA
2American Neurospine Institute PLLC, Plano, TX, USA
Introduction: Lateral corpectomies are well-established procedures that have been used successfully in the treatment of numerous conditions, including infection, deformity, tumor, trauma, and degenerative disease. To reestablish vertebral body stability post resection, cage placement is typically performed, with proper alignment of the cage between the superior and inferior bodies to ensure vertebral column alignment and fusion. Image guidance provides enhanced visualization in spinal surgical procedures, particularly for accuracy of implant placement. However, image guidance with dynamic referencing depends on stability of the anatomy relative to the patient reference frame for accuracy of visuals provided by the system. A cadaveric study was conducted to evaluate stability of the spine following partial and full corpectomy procedures to assess the ability to accurately navigate cage placement post-corpectomy. Material and Methods: Two cadavers were prepped in the right decubitus position per typical clinical setup. Thoracic and lumbar access was performed for 1 cadaver, with lumbar access only for the second. Two fiducials each were placed in the superior and inferior bodies above and below the planned corpectomy levels (Centerpiece Screws; Medtronic PLC, Dublin, Ireland), followed by 3-dimensional (3D) imaging to establish the pre-procedure state of the anatomy (O-arm, Medtronic PLC). For the procedures, a partial corpectomy was performed using osteotomes and rongeurs, with screw hole prep to simulate lateral plating, followed by final extension of the resection to a full corpectomy. Additional 3D imaging was conducted after each procedure (partial and full) to establish the post-procedure state of the anatomy. Image data were postprocessed with Mimics (Materialise, Leuven, Belgium) to segment the fiducials. Three-D models of the fiducials were exported to Geomagic (3D Systems, Rock Hill, SC) to assess displacement of the vertebral bodies and relative shift of fiducials with regard to the pre-procedure state. Results: Displacement between fiducials on the same body showed a maximum of 0.31 mm, representing error of the 3D reconstruction. Displacement between fiducials on different bodies showed a maximum of 1.58 mm. Relative shift of the fiducials after registration showed a maximum of 1.42 mm. The maximum for both displacement and shift were observed between the pre-procedure and post-full corpectomy states. Directionality of the positional shift was generally contraction of the bodies including lateral shift from midline. Conclusion: The results show minimal change in position after both partial and full corpectomies in a cadaveric model, indicating spinal column stability despite significant bone removal. This observed stability is associated with maintenance of facet joints as well as anterior and posterior ligamentous structures, demonstrating capability for procedural accuracy with image guidance.
P497: Pedicle Screws Can Be Safely Placed in the Thoracolumbar Spine With a Novel Navigation and Robotic-Guided System
Deeptee Jain1, Jordan Manning1, Elizabeth Lord1, Themistocles Protopsaltis1, John Bendo1, Charla Fischer1, Aaron Buckland1, and Jeffrey Goldstein1
1New York University Medical Center, New York, NY, USA
Background: There has been a recent interest in robotic-guided navigation systems for pedicle screw placement to ensure accuracy and safety and diminish radiation exposure while improving outcomes. There have been no published studies using a new combined robotics and navigation system (Globus Excelsius GPS system). Prior studies have addressed navigation or robotics but not a system that combines both these elements. Methods: This is a case series of consecutive patients at a single institution from February 2018 to August 2018. All patients who had planned placement of thoracic and lumbar pedicle screws using combined robotics and navigation system were included in the study. Results: A total of 104 patients were included in this study. Three cases were aborted for technical issues. There were 636 pedicle screws, 6 iliac screws, and 1 S2AI screw placed. Eighty-eight patients had screws planned using preoperative CT (computed tomography), 13 using intraoperative fluoroscopy. All screws except for 5 pedicle screws in 2 patients were placed successfully using the robot (99%). Five pedicle screws were placed by converting to a freehand fluoro-guided technique. Eighty-six patients had screws placed using a percutaneous technique, and 15 patients had screws placed using an open technique. Twenty-eight patients had concurrent anterior lumbar interbody fusions (ALIFs), 12 had lateral lumbar interbody fusions (LLIFs), and 58 had TLIFs (transforaminal lumbar interbody fusions). All ALIFs and LLIFs were performed prior to placement of the screws. Four of the 12 LIF patients had screws placed with the patient in the lateral position. No patients had screw-related complications intraoperatively or postoperatively, and no patients returned to the operating room for screw revision. Conclusion: This study demonstrates that the robotics and navigation system is a novel technology that can be utilized to place pedicle screws and pelvic screws safely and has the potential to reduce screw related complications.
P498: Pedicle Screw Accuracy of the Prevailing Methods of Insertion: A Systematic Review and Meta-Regression Analysis of More than 50 000 Screws
Alexander Perdomo-Pantoja1, Wataru Ishida1, Corinna Zygourakis1, Christina Holmes2, Nicholas Theodore1, L.Lo Sheng-Fu1, and Timothy F. Witham1
1Johns Hopkins University, Baltimore, MD, USA
2Florida A&M University–Florida State University, Tallahassee, FL, USA
Introduction: Pedicle screws (PS) are routinely used for stabilization and enhancing fusion in the spine, in a broad diversity of spinal pathologies, and several techniques have been developed to decrease screw misplacement.1 These methods are commonly categorized as freehand (FH) technique, fluoroscopy-assisted (FA), computed tomography–image navigation (CTNav), and more recently, robot-assisted (RA). The purpose of this comprehensive study was to investigate the current status of PS placement accuracy rates among the 4 techniques, focusing on the individual results of these existing modalities and analyzing the features linked with PS misplacement. Materials and Methods: We performed a systematic review, including articles from January 1990 to May 2018, following the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) to study PS insertion accuracy in the spine. The search strategy was designed along with a library clinical informationist at our institution and based on the Peer Review of Electronic Search Strategies (PRESS) guidelines. Once articles were selected, information on demographic data, diagnosis, the accuracy of PS insertion, spinal levels, the method for screw insertion, and breach features were collected. A modification of Gertzbein’s grading scale for pedicle violations was utilized, and breaches were classified as minor (<4 mm) or major (≥4 mm). We conducted a meta-analysis to determine the overall pooled rates of PS accuracy as a primary outcome, stratified by screw placement techniques. Potential factors were examined via meta-regression analyses. Results: Of a total of 5855 references identified in the electronic databases, 78 studies (including 7858 patients, 51 161 pedicle screws, and 3614 cortical pedicle breaches) were included in this study. The overall pooled accuracy rates were 93.1% via the FH, 91.5% via the FA, 95.5% via CTNav, and 90.5% via the RA. CTNav exhibited a higher PS insertion accuracy compared with the FA and the RA (P = .01 and .04, respectively). Percentages of thoracic screws in each study showed a negative correlation with screw accuracy rates (P = .04). The FH technique presented a positive correlation with thoracic pedicle breach compared with CTNav and the RA (P < .01 and .02, respectively). The FA technique displayed a higher patient revision rate than FH and CTNav (P < .01 and .01, respectively); and it also revealed a positive correlation with the number of screws revised in a second surgery, compared with the FH (P = .01). Preoperative diagnosis, patient age, study design, approach, and the number of surgeons did not significantly influence the accuracy rates. Conclusions: Recognizing the limitations of this study, we conclude that currently, CTNav provides higher accuracy and lower revision rates for PS placement over other techniques. CTNav and RA exhibited fewer breaches in the thoracic spine. The FA exhibited higher rates of revision surgery. Given the heterogeneity among reports, further comparative and standardized studies are required to support these findings.
Reference
1. Parker SL, McGirt MJ, Farber SH, et al. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery. 2011;68:170-178. doi:10.1227/NEU.0b013e3181fdfaf4
P499: The Intraoperative Portable CT Scanner–Based Spinal Navigation: A Viable Option for Instrumentation in the Region of Cervicothoracic Junction
Pavel Barsa1, Robert Frohlich1, and Petr Suchomel1
1Regional Hospital of Liberec, Liberec, Czech Republic
Introduction: Innovative intraoperative imaging modalities open new horizons to more precise image acquisition and possibly to better results of spinal navigation. Planning of screw entry points and trajectories in this prospective study had been based on intraoperative imaging obtained by a portable 32-slice computed tomography (CT) scanner. The authors evaluated accuracy and safety of this novel approach in the initial series of 18 instrumented surgeries in anatomically complex segment of cervicothoracic junction. Material and Methods: We report on the single-institution results of assessment of anatomical accuracy of C5-T3 pedicle screw insertion as well as its clinical safety. The evaluation of total radiation dose and of time demands was secondary endpoint of the study. Results: Out of 129 pedicle screws inserted in the segment of C5-T3, only 5 screws (3.9%) did not meet the criteria for correct implant positioning. These screw misplacements had not been complicated by neural, vascular, or visceral injury, and surgeon was not forced to change the position intraoperatively or during the postoperative period. Quality of intraoperative CT imaging sufficient for navigation was obtained at all spinal segments regardless of patient’s habitus, positioning, or comorbidity. A higher radiation exposition of the patient and 27-minute longer operative time are consequences of this technique. Conclusion: The intraoperative portable CT scanner–based spinal navigation is reliable and safe method of pedicle screw insertion in cervicothoracic junction.
P500: Perception of Navigation in Spine Surgery Among Orthopedic Residents
Tamara Soh1, Arun Kumar Kaliya Perumal1, and Jacob Y. L. Oh1
1Tan Tock Seng Hospital, Singapore, Singapore
Introduction: Spinal navigation is a relatively new technology that has revolutionized spine surgery. Its fundamental purpose is to have an interactive 3-dimensional real-time feedback during spine procedures to facilitate appropriate instrumentation. In some institutions, orthopedic residents have the opportunity to participate in navigation-assisted spine surgeries during their training; however, it is not previously studied whether this positively affects their competency to perform spinal instrumentation. Therefore, we conducted a survey among orthopedic residents to study their perception about learning spinal navigation during their residency training and its impact on their competency. Material and Methods: A cross-sectional descriptive survey was formulated to assess the perception of spinal navigation among orthopedic residents who had the opportunity to participate and learn navigation-assisted pedicle screw application during their residency training. Our selected sample represents a unique set of young orthopedic surgeons who start their spine career by learning navigation-assisted spine surgery. The first part of the questionnaire deals with perception of understanding the concepts, level of exposure, instrumentation, confidence about screw placements, intraoperative stress anxiety, and overall satisfaction of the procedure. The second part of the questionnaire was drafted to learn about each resident’s understanding of the entry point and trajectory during freehand pedicle screw insertion. In the final part of our questionnaire, images of the posterior aspect of the lumbosacral and thoracic spine models were provided, and the residents had to identify the most appropriate pedicle screw entry points for right L4, right S1, and left T8 pedicles. This was done to assess each resident’s understanding about the surface anatomy of the entry points. Results: Orthopedic residents (n = 20) who had completed 3 years of training that included at least one spine rotation in our spine were included. The overall resident’s perception regarding their competency to apply pedicle screws on their own using spinal navigation was 3.65 ± 0.81 on a 5-point Likert-type scale. Their perception of understanding the concepts, level of exposure, knowledge of instrumentation, confidence about screw placements, feeling of decreased anxiety, and overall satisfaction of the procedure positively correlates with their competency at the end of their training. Seventeen residents (85%) had assisted for a freehand pedicle screw application. The overall perception regarding their competency to apply pedicle screws on their own using freehand technique was only 2.8 ± 0.77 on a 5-point Likert-type scale. In terms of surface anatomical landmarks, 65% of residents were correct with their entry point for the L4 pedicle and 70% of residents were correct with their entry points for S1 and T8 pedicles. Conclusion: All residents invariably agreed that they understood the concepts, instrumentation, and felt they were competent to apply pedicle screws on their own using navigation by the end of their training. Despite their confidence, 30% to 35% of residents were unable to identify the appropriate surface anatomy for pedicle screw insertion. For training in spine surgery, exposure to a variety of cases that utilize both the navigation-assisted pedicle screw insertion and the freehand technique is ideal.
P501: Navigated Needle Placement for Sacroplasty for Sacral Insufficiency Fractures Is Much Safer Than Standard Needle Placement Methods: A Single-Center Experience
Ehab Shiban1, Nicole Lange1, Ann-Kathrin Jörger1, Arthur Wagner1, and Bernhard Meyer1
1Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Objective: Sacral fractures are an infrequent but often disabling cause of severe low back pain. Needle placement can be controlled by 2-dimensional (2D) fluoroscopy or 3D fluoroscopy–guided navigation. We compare our results of those 2sacroplasty techniques in a group of patients with sacral fractures. Methods: We retrospectively analyzed all patients with sacral insufficiency fractures from January 2012 to February 2018. We analyzed the patients’ clinical characteristics, comorbidities, and outcome. Results: A consecutive cohort of 18 patients (4 male, 14 female) were identified. The mean age was 70 years (range = 48-87 years). Ten procedures were conducted in a standard fashion with 2D fluoroscopy, and 8 procedures were navigated via 3D fluoroscopy. All patients suffered from severe local pain. Fractures were half pathological (9 patients) and traumatic (9 patients). Postoperatively, cement placement and leakage was controlled in every patient via CT (computed tomography) scans. Cement leakage was recorded for 80% in the non-navigation group, compared with 37% in the navigated group (P = .03). None of them were symptomatic. All patients showed significant pain relief at the time of discharge. Surgery time was 1 hour (mean) and did not differ significantly between the groups. Conclusion: The 3D-guided needle placement seems to be much safer than standard needle placement methods, as half as much cement leakage was observed.
P502: Image Outcome of Cement-Augmented Screws Before and After the Era of 3D Navigation
Shiu-Jau Chen1
1Mackay Memorial Hospital, Taipei, Taiwan, Province of China
Introduction: Cement-augmented transpedicle screw is beneficial for pullout prevention in osteoporotic patients. However, cement leakage is a complication and may cause neurological deficits especially when the screws is in inappropriate position. Three-dimensional (3D) navigation was reported to increase the accuracy of screw trajectory. Our study assessed the radiological outcome of cement-augmented transpedicle screw before and after the era of 3D navigation. Material and Method: From January 2013 to December 2017, 64 patients receiving cement-augmented screw insertion for spinal fusion were included in our study. They were divided into 2 groups. Group 1 included 40 patients. They underwent this procedure with the assistance of 2D fluoroscope. Postoperative computed tomography (CT) scan was achieved at 12 months. Group 2 had 24 patients. Their screws were inserted under 3D navigation by Zeego Artis in hybrid operating room (OR) since September 2016. They received cone-beam CT immediately in the OR and 1 year after the operation. The incidence of screw malposition and cement leakage were accessed between 2 groups. The incidence of screw loosening, broken screw, and further fracture was assessed in group 1 patients. Results: Group 1 patients received 201 screws. Forty were located in thoracic spine and 161 were in lumbar spine. Twenty-one screws (10.4%) were graded as malposition. Seven of them belongs to inner or inferior perforation that were at risk for nerve injury. Cement lead was noted in 12 screws (6%). Besides, screw loosening occurred in 27 screws (13%) but no screw pullout happened. There were 2 broken screws and 5 subsequent vertebral fracture, 2 on the adjacent segment and 3 on the screw segment. Group 2 patients received 129 screws. Twenty-two (17%) were located in thoracic spine. There were 12 screws (9%) graded as malposition. All were either lateral (7) or anterior (5) penetration that had low risk of nerve injury. Two cement leaks were noted in group 2 patients. Both were bicortical screw in sacrum. Conclusion: The 3D navigation by cone-beam CT in hybrid OR reduces the possibility of inner and inferior screw penetration that tend to injure the roots. The incidence of cement leak was decreased because the screws were inserted in a deeper position under navigation. For osteoporotic patients who have undergone fusion surgery with cement screws, 3D navigation should be considered to decrease the primary injury by screw malposition and secondary injury by cement leak.
P503: Custome Spine Surgery: Transforaminal Lumbar Interbody Fusion
Alberto P. Contreras1, Fernando Calderon Carrillo1, Erik Hernandez Vasquez1, and Diana Chavez Lizarraga1
1Centro del Cerebro y Columna Vertebral Hospital Mexico, Mexico City, Mexico
The TLIF (transforaminal lumbar interbody fusion) represented in the history of spine surgery a relevant part in the evolution of techniques that not only preserve spinal canal and neurological elements but also a technique that has been the keystone in the minimum invasion of the spine. On the other hand, the use of fluroscopy and now 2D (2-dimensional) navigation was the beginning of what is now the O-arm navigation system, integrating a work station that integrates the images acquired from a fluroscopy arch. The fusion of techniques and the evolution of emerging technology is what has allowed us to define a new term: “Custom Surgery” that not only allows to guide the decompression of neurological elements performing it under navigation in real time but also the placement of customized implants and performing a strictly supervised arthrodesis, with this the result has improved translating into a brief recovery compared with the conventional technique. From January to June 2018 at the Hospital Angeles Mexico of the Angeles Health Services Group, fully navigated lumbar spine surgery was performed on the scheduled patients. Patients were selected from medical appointments, performing radiographic studies that included panoramic vertebral column for measurement of sagittal balance, dynamic studies, simple lumbar spine resonance, and bone densitometry from spine and hip. Inclusion criterion was the diagnosis of degenerative disease of symptomatic lumbar spine that did not improve with conservative treatment based on pain killers, weight control, and column hygiene indications, including physical therapy in the previous 6 months. Patients were also assessed by psychology avoiding additional benefits like laboral inability, and the preoperative valuation was mandatory in those older than 45 years and grading ASA (American Society of Anesthesiologists) I-II/IV. Exclusion criteria were the following: deformative disease greater than 20° in the coronal plane, single-segment L5S1 disease with bifurcation suitable for anterior or anterolateral access, active smoking, BMI (body mass index) greater than 28 kg/m2, and psychiatric and/or psychological disorder. Informed consent was signed for both the procedure and to obtain photographic and video material during the surgery. For 80 patients who were asked to perform the procedure, the following demographic data was revealed: the female gender predominates in 48 patients (60%) and men gender in 32 patients (40%). Active working patients with no distinction of gender. There was no difference in the right/left access side, choosing symptomatic side and, if both sides were affected, the image study was taken as a guide to define access, choosing the most affected for access.Time of surgery was improved from 90 minutes in the first 5 cases to 45 minutes in 1 column-level performed surgery, and when there were 2 levels, the average time was 110 minutes total. In total, there were 128 levels in the 80 patients and all the pedicles were instrumented, navigation from the incision to follow a pedicle trajectory of the screw, finding that there was variation in the measure of the polyaxial screws used in the same level up to 50%, adjusting according to the navigation length and diameter necessary to reach the desired position, achieving symmetry on both sides with the adjustments made, we navigate the placement of the dilator system to use a working port of 20 mm identifying lateral articulation as an access target. The cage was selected according to the measure to reach the contralateral epiphyseal ring in oblique trajectory from the insertion by the Kambin triangle. Bone graft (demineralized bone matrix plus autologous) was placed, which were placed before the cage to achieve the necessary compaction. The length of the bar is measured in the navigation system, and at the end of the procedure, the implant placement confirmation was made. The patient’s radiation exposure time was minimal only during the initial image acquisition, and the surgical team was not exposed to any radiation. Postoperative pain control was with acetaminophen at a dose of 3 g per day with parecoxib 80 mg daily, antibiotic prophylaxis with vancomycin single dose. Moving in and out of bed was recommended at 4 hours after the surgery and they left home with indication of dorsolumbar and lower limb stretching exercises. The emerging technology that uses an image system that can be acquired moments before the surgery in anatomical position according to the selected surgical technique associated with the navigation work station allowed us not to reposition implants when placing them safely and effectively, there was less consumption of pain killers in the immediate and mediate postoperative period, being able to be checked out home in the first 24 hours of the procedure, there was no need to use morphine or modulators as well as postoperative physical therapy, this allows an early reintegration to the social activity and work.
P504: Using Spinal 2D Navigation in Transiliosacral Implant Placement
Julia Vavken1, Harry Gebhard1, and Alexander Mameghani1
1Kantonsspital Baden, Baden, Switzerland
Introduction: Minimal-invasive placement of transiliosacral implants is only safe with intensive intraoperative image guidance. Indications for this procedure are, for example, iliosacral screw osteosynthesis in acute sacral insufficiency fractures in the elderly or sacroiliac joint fusions (SIJ fusion) in refractory painful conditions. Both procedures are well described. Conventional placement is performed with fluoroscopic control in alternating inlet and outlet view to find the optimal entry point, direction, and implant size. High radiation doses are necessary. We report on a case series using standard spinal 2-dimensional (2D) navigation for transiliosacral implant placement. Material and Methods: In 10 patients, a spinal 2D navigation (Kick2D) was mounted to the iliac crest. Image acquisition included both inlet and outlet views and additional lateral view. With the navigated pointer, the intended entry point and direction was found and the skin incision site was identified. After incision, the navigated Jamshidi needle was placed on the entry point and deepened into the sacral alar or body as intended. The desired length was measured with the navigation system using the pointer. A long K-wire was then threaded, and the Jamshidi needle was removed. In Seldinger technique, any thicker K-wire could replace the first one. The implant was finally set with minimal additional fluoroscopic control in conclusion. Intraoperative radiation dose was documented. Routine computed tomography on day 1 showed implant position postoperatively. Results: There was no violation of the anterior or posterior cortex of the sacrum. No vascular injury occurred. The sacral spinal canal was intact in every case. There was 1 L5 palsy in 1 patient with sacral insufficiency fracture, when we additionally performed sacroplasty. No revision surgery was necessary. The radiation dose was lower than in conventional implant placement. Identifying the desired entry point was possible in less time than in conventional technique. Conclusion: Spinal 2D navigation can safely be used for transiliosacral implant placements in nondisplaced sacral insufficiency fractures or in SIJ fusion procedures. The overall accuracy was good. We are convinced that exposure to radiation is reduced for the operating room staff members. Further studies are needed to quantify the amount of dose reduction and time saving.
P505: Portable Combined Robotic/Navigation Platform Without K-Wires: Initial Real-World Clinical Experience in Spinal Instrumentation
Hoon Choi1
1Medical College of Wisconsin, Milwaukee, WI, USA
Introduction: The field of spinal surgery has seen an increase in the use of intraoperative navigation for spinal instrumentation. With correct use, intraoperative navigation has provided the surgeons with more consistency and accuracy of spinal instrumentation. There has been increasing interest in the use of robotics in spinal surgery. Until now, the use of robotics has been limited to an external trajectory guidance system that is: (1) additional to the navigation platform; (2) mounted to the patient and/or the table; and (3) relies on the use of Kirschner wires (K-wires). We present our initial clinical experience with a portable combined robotic/navigation platform without K-wires in a wide range of clinical scenarios involving spinal instrumentation. Material and Methods: Patients were prospectively and consecutively recruited over an 8-month period. Intraoperative imaging of the spinal anatomy with rigidly attached reference arrays was obtained with a portable 3D (3-dimensional) X-ray system (Medtronic O-Arm). Images were uploaded into a newly Food and Drug Administration–approved portable robotic/navigation platform (Globus Excelsius GPS). Screws were planned on the platform via touchscreen interface by the operating surgeon intraoperatively. An electrically operated robotic arm attached to the portable navigation platform was used to guide screw trajectories. A battery-operated drill held by the robotic arm was used to cannulate the cortical and cancellous bone in the preplanned trajectories. Screws were placed by the operating surgeon without the use of K-wires working through the end effector of the robotic arm. Intraoperative imaging was obtained after instrumentation to evaluate accuracy per Gertzbein and Robbins criteria and categorized into groups A to E. Multimodal neuromonitoring was used for all cases. Results: Forty-one surgeries in 41 patients were included in the analysis: 24 (58.5%) for degenerative disease; 8 (19.5%) for adjacent segment degeneration; 7 (17%) for trauma; and 2 (4.9%) for tumor. Open technique was used for 13 patients (31.7%); hybrid technique in 12 (29.3%); and minimally invasive technique in 16 (39%). A total of 212 screws were attempted with the robotic system. A total of 183 screws were fully executed (86%). Reasons for nonexecution include: software failure (n = 14; 6.6%); contamination (n = 8; 3.8%); hardware failure (n = 3; 1.4%); hardware limitation (n = 2; 0.9%); and medical instability (n = 2; 0.9%). A total of 181 screws (98.9%) were in Gertzbein and Robbins Group A (fully within pedicle); 1 screw (0.5%) was in group B (breach <2 mm) (not repositioned); 1 screw (0.5%) was in group C (2 mm < breach < 4 mm) (removed). No neurologic deficit occurred due to the breaches. Conclusion: The new portable robotic navigation system can be used for a variety of degenerative (both new and revision), trauma, and tumor indications with open, hybrid, and minimally invasive techniques. Execution rate improved throughout the initial 8-month period with hardware and software updates. The system demonstrated high, but not perfect, screw accuracy, and therefore, it requires vigilance and confirmatory imaging.
P506: Ventral and Dorsal Fusion as Correction of Craniocervical and Atlantoaxial Instability in Patients With Benign and Malignant Lesions Using O-Arm System
Nikolay Mirchev1 and Behr Robert1
1Klinikum Fulda gAG, Fulda, Germany
Introduction: A prospective analysis of the surgical treatment and results of 129 patients with benign and malignant craniocervical, atlantoaxial, and high cervical lesions operated during 7 years period (2011-2017) at our department was performed. The aim of the analysis was to assess the factors affecting dorsal fusion as correction of craniocervical and atlantoaxial instability. Material and Methods: We analyzed 90 patients with traumatic lesions, 12 patients with inflammatory lesions, 8 patients with degenerative instability, and 19 patients with craniocervical tumors. Results: We performed 132 operations. Because of craniocervical/cervical instability we made posterior screw fixation in all of 129 patients. In order to improve screw placement accuracy, we performed intraoperative O-arm in 112 cases. The operative duration was 2 hours in O-arm operations and 4.30 hours in C-arm operation. The blood loss was 250 mL in O-arm and 550 mL in C-arm procedures. The mean screw length in C1/C2/C3 vertebras was 30 mm in O-arm procedures and 24 mm in C-arm procedures. The most common operative complications were: cerebrospinal fluid leak in 2 cases, postoperative infection in 6 cases, and screw misplacement in 2 cases (in C-arm procedures) without early operative mortality. The 12-month follow-up patients showed good recovery in 88 patients, moderate disablity in 27 patients, severe disablity in 5 patients, vegetative state in 4 patients, and death in 5 patients with malignant lesions. Conclusion: Early correction of craniocervical and high cervical instability facilitated neurological recovery by preserving the existent neurological function. Using O-arm increased operative screw placement accuracy and preserve intraoperative nerve and vertebral artery injury. Recently because of the improvement of neuroimaging techniques, surgical techniques, and neurointensive care, the results of treatment of these lesions are optimal.
P507: Novel Single-Step MIS 3D-Navigated Thoracolumbosacral Pedicle Screw System: Workflow, Accuracy, and Initial Clinical Experience
Franziska Anna Schmidt1, Hervé M. Lekuya2, Sertaç Kirnaz1, R. Nick Hernandez1, Christoph Wipplinger1, Cameron Rawanduzy1, and Roger Härtl1
1Weill Cornell, New York, NY, USA
2Makerere University, Kampala, Uganda
Introduction: Single-step 3D-navigated thoracolumbosacral percutaneous pedicle screw systems were developed for minimally invasive spine surgery. The safety of the system has been previously reported, and we performed this study to report our initial clinical experience with this novel technique. We would like to evaluate a potential improvement of the workflow, the accuracy, and a decrease in surgery time. Material and Methods: The prospective case study was conducted on collected data from patients who underwent posterior pedicle screw fixation between October 2017 and April 2018. Viper Prime system (DePuy Spine, Raynham, MA) was used. Outcome measurements were obtained from intraoperative computed tomography, including sagittal, axial, and coronal reformatted images. The images were evaluated to determine pedicle wall penetration after surgery. We used a previously published grading system to assess the severity of the pedicle wall penetration. Severity was classified as grade 1 (<2 mm), grade 2 (2-4 mm), or grade 3 (<4 mm), and the directions were assessed as medial, cranial, caudal, and lateral. Results: Our study includes 24 patients with a total number of 135 screws. Pedicle wall penetration occurred in 14 screws (10%). Other variables such as sex, age, and number of operated levels did not influence screw placement accuracy. Grade 1 breaches occurred in 4 screws (3%), and grade 2 breaches occurred in 10 screws (7%). Lateral breaches were observed more often than medial breaches. The accuracy rate in our study was 90%. The median time per screw was 2.45 minutes. No revision surgery was needed, and no complications occurred. Conclusion: We conclude that the thoracolumbosacral pedicle system is a safe, accurate, and efficient tool in minimally invasive spine surgery. Our accuracy rate is comparable to that found in the literature. We experienced an improvement in workflow and effectiveness with this 1-step technique.
P508: Learning Curve in Robot-Assisted Percutaneous Pedicle Screw Placement in Thoracolumbar Surgery
Jeremy Kam1, Calvin Gan1, Stefan Dimou1, Mohammed Awad1, Bhadu Kavar1, and Girish Nair1, Andrew Morokoff1
1Royal Melbourne Hospital, Melbourne, Victoria, Australia
Introduction: Percutaneous pedicle screws have multiple advantages over open freehand screws. However, they depend on intraoperative imaging (eg, fluoroscopy, navigation) and requires increased surgeon training and skill, with the learning curve overcome for operative time and complications when case numbers reach aproximately 20 to 30. Robot-assisted pedicle screw placement is advantageous compared with navigation or fluoroscopy by reducing the 6 degrees of motion in a 3D (3-dimensional) space for Jamshidi needle placement to only 2 degrees of motion. As it is relatively new technology, there remains a small amount of literature regarding the Renaissance (Mazor Robotics Ltd, Caesarea, Israel) robot in terms of its accuracy and advantages. We aimed to evaluate the learning curve if any of this new technology over the course of our initial experience. To our knowledge, this is the first study to look at the learning curve of robot-guided thoracolumbar percutaneous pedicle screw placement with comprehensive objective postoperative computed tomography (CT) scoring, time per screw and fluoroscopy time. Material and Methods: We included the first 80 consecutive patients undergoing robot-assisted spinal surgery for several indications, mostly thoracolumbar degenerative disc disease at a single institution. Data was collected for pedicle screw placement accuracy using the Gertzbein-Robbins classification, screw placement time, fluoroscopy time, and revision rate. Patient demographic and relevant data such as surgical indication, number of spinal levels undergoing surgery, and complications were also collected. Patients were divided equally into 4 subgroups by their chronological date of surgery to evaluate how learning curve affected screw outcomes. Results: A total of 80 patients were included of which 73 (91%) had complete data and postoperative CT imaging to assess hardware placement. Participant mean age (SD) was 66.6 (11.1) years and 63.0% were female. There were no significant differences between the time groups for comorbidities, number of levels operated, indication, or approach. A total of 352 thoracolumbar percutaneous pedicle screws were placed for 73 patients. The rate of clinically acceptable screw (<2 mm deviation) placement was high and did not change between groups (96.6%, 95.4%, 95.6%, 90.7%, Groups 1 to 4, respectively, P = .314) over time. Median time per screw was 7.0 minutes and did not vary over time (6.5, 7.0, 6.0, and 6.0 minutes, groups 1 to 4, respectively, P = .605). Median fluoroscopy time per screw was 3.0 seconds and slightly increased to 4.0 seconds in the third quarter but was statistically significant (2.0, 3.0, 4.0, and 3.0 seconds, groups 1 to 4, respectively, P = .021*). Intraoperative revision occurred in only 1 of 352 (0.3%) screws. There were no screw-related complications. Conclusion: Our study includes a comprehensive analysis of learning curve associated with the adoption of robot-assisted pedicle screw placement as a new surgical technique. We evaluated multiple outcomes such as screw accuracy, screw placement time, and complication rate, and found that robot-assisted screws were associated with high overall accuracy, low placement and fluoroscopy times, and low complication rates but no significant differences from initial experience to practicing experience after approximately 1 year indicating robot-assisted pedicle screw placement has very little to almost no learning curve.
P509: O-Arm Navigated Screw Placement for 360° Fusion: Retrospective Analysis
Orlin Pavlov1 and Nikolay Mirchev1
1Klinikum Fulda, Fulda, Germany
Introduction: The screw placement with O-arm has a reported accuracy of 99%. The crucial meaning of the perfect placement of the screws can be illustrated in 360° stabilization of the spine. The position of the screws is going to play an important role, when choosing an extended cage with a variable angle. Nevertheless, the necessity to eliminate a revision surgery because of a suboptimal positioning of the screws has to be emphasized. Most of these patients have multiple comorbidities and are considered as high-risk patients. Methods: In our study, we reviewed 25 patients operated between 2013 and 2018, who underwent a 360° fixation. This is a single-centre, multisurgeon, retrospective analysis. Eight patients underwent surgery because of tumor (primary or metastatic), 5 patients because of infection, 8 patients because of trauma, and 4 patients because of degenerative spine. In our study, 5 patients were operated on the cervical spine, 4 on the cervicothoracic junction, 11 on the thoracic spine, and 5 on the lumbar spine. In our series, all 25 patients underwent a dorsal spondylodesis with O-arm. Twenty patients underwent 3 or more levels of dorsal spondylodesis and and only 5 underwent a bisegmental stabilization. In 14 patients, the ventral fusion was performed via a ventral approach and in 11 via a dorsal approach. Results: The usage of O-arm improved the screws placement and recording to literature reviews, it has a reported accuracy of 99%. In surgeries, where a multilevel dorsal spondylodesis is required, the usage of O-arm navigation system leads to shorter operating time, thus less blood. One of the 25 patients underwent a revision surgery because of extended epidural hematoma with extension of the dorsal spondylodesis and thus prolonged hospital stay. Intraoperatively, 1 screw had to be revised. Conclusions: The optimal placement of the screws is a decisive factor for the placement of ventral expandable cages. The shorter operating time and lesser blood loss is of crucial meaning for multiple comorbidities.
P510: Navigation for Pedicle Screw Placement in Trauma Patients: Only for Peripheral Zones?
Martin F. Hoffmann1 and Christian Fisahn1
1Berufsgenossenschaftliches Universitätsklinikum Bergmannsheil, Bochum, Germany
Introduction: Thoracic and lumbar spine instabilities are routinely treated by initial posterior instrumentation. Pedicle screw placement is fundamental for these procedures. Misplaced pedicle screws may result in severe complications. Although navigation systems may support pedicle screw placement and may reduce radiation exposure for patients and OR (operating room) personnel, fluoroscopy is generally utilized for pedicle screw placement in trauma patients. The purpose of our study was to examine utilization and effects of navigation for pedicle screw placement and the need for revision. Materials and Methods: Between 2015 and June 2018, 502 trauma patients were treated by 4 fellowship-trained orthopedic surgeons utilizing 3168 pedicle screws in the thoracic and lumbar spine in a level I trauma center. A passive navigation system (Curve, Brainlab, Germany) was available and utilized at the surgeons’ discretion. Pedicle screw placement was routinely controlled by postoperative CT (computed tomography) scans. Groups were retrospectively analyzed regarding demographic factors, vertebral level of screw placement, and accuracy of screw placement. Results: In our study, 2567 pedicle screws (81%) were inserted by standard procedure. Navigation was utilized in 19%. Mean patient age was 63 years (range = 15-91 years). BMI (body mass index) averaged 27.7 kg/m2 (range = 15.2-48.4 kg/m2). No differences were observed between the groups regarding demographics. Number of screws inserted per patient was greater in the standard group (6.46 vs 5.59, P = .012). Surprisingly, there was no difference in screw misplacement for standard procedure or navigation (P = .576; 0.8% and 0.7%, respectively). Analysis of screw location showed a typical distribution with the majority placed in the lower thoracic and upper lumbar spine. Comparison of navigation and standard procedure screw location revealed an opposing trend. While the majority of standard screws were placed in the thoracolumbar junction, navigation was utilized in the upper thoracic region and lower lumbar spine. Conclusion: In our study, screw misplacement was low compared with the current literature (1% navigation, 2.3% standard procedure). Surprisingly, there was no reduction of screw misplacement by navigation. Analyzing screw locations revealed that navigation was utilized in anatomically more challenging zones with reduced fluoroscopic quality, while surgeons tended to the quicker standard procedure in their thoracolumbar “safe zone.” This treatment algorithm reduced screw misplacement to less than 1% in the overall study population and shows the importance of navigation as an additional tool.
Nonoperative Clinical Treatments
P511: Three-Dimensional Transverse Plane Evaluation of Immediate Chêneau-in-Brace Biomechanical Efficacy for Patients With Adolescent Idiopathic Scoliosis: A Detorsion Investigation
Haidara Almansour1, Wojciech Pepke1, and Michael Akbar1
1Heidelberg University Hospital, Heidelberg, Germany
Introduction: Transverse plane pattern comprising apical axial rotation (AVR), the intervertebral axial rotation (IAR), and the torsion index (Ti) are being increasingly studied due to their significance at predicting the progression of curves in the setting of mild adolescent idiopathic scoliosis (AIS). This study aims at quantifying the immediate in-brace correction of transverse plane parameters. Material and Methods: Spines of 45 patients with AIS undergoing Chêneau brace treatment were reconstructed using biplanar stereoradiography in a standing position. AVR, IAR at junctions, and Ti (the mean of the 2 sum of IAR from lower junction to the apex, then from the apex to the upper junction) were calculated. Subsequently, a detorsion index was computed to quantify the immediate in-brace correction on scoliotic curves. Mean values of each parameter were compared between thoracic, thoracolumbar, and lumbar curves. Shapiro-Wilk test was used for normality testing. Paired t test was utilized to delineate the pre- to in-brace changes. Results: Descriptively, thoracic (n = 19), thoracolumbar (n = 10), and lumbar (n = 14) curves were analyzed. As expected, a significant correction of Cobb angle for all curves was observed (all P < .01) with a pre- to in-brace correction of 14° for the thoracic, 15° for thoracolumbar, and 10° for the lumbar curves. Without the brace, mean Ti for the thoracic, thoracolumbar, and lumbar curves was, respectively, 15 ± 12°, 13 ± 7°, and 8 ± 5°. Mean AVR was 8 ± 5°, 13 ± 9°, and 9 ± 5°. With the brace, mean Ti for the aforementioned curves was 14 ± 8°, 8 ± 6° and 9 ± 4°. Mean AVR was 7 ± 4°, 9 ± 6°, and 10 ± 5°. A significant correction of AVR was noted in thoracolumbar curves (P = .04). Similarly, a significant correction of IAR (“detorsion index” = pre brace − in brace/pre brace) was found at 40% in thoracolumbar curves (P = .03). No significant differences were found for the correction (in terms of AVR, IAR, and detorsion) in thoracic or lumbar curves.1 Conclusion: Coronal correction of AIS curves is insufficient to describe the efficacy of bracing. In this retrospective 3-dimensional (3D) analysis of transverse plane parameters, we were able to demonstrate that despite Chêneau bracing success in coronal correction, it differed in its immediate transverse correction between thoracic, lumbar, and thoracolumbar curves. Our results elucidate the efficacy of Chêneau 3D corrective forces on thoracolumbar curves and variability of its corrective forces on thoracic and lumbar curves. To our knowledge, this is the first study that addresses this issue in a population of AIS patients undergoing Chêneau bracing. Despite the small sample size, our results should enhance the brace maker’s understanding of Chêneau correction and pave the way for prospective studies with a larger sample size and a follow-up until skeletal maturity to predict curve progression under bracing treatment.
Reference
1. Steib JP, Dumas R, Mitton D, Skalli W. Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine (Phila Pa 1976). 2004;29:193-199.
P512: Results of Nonsurgical Treatment of Ostoporotic Thoracic Fracture
Robert Weglowski1, Piotr Piech2, and Tomasz Gieroba2
1University of Physical Education, Biala Podlaska, Poland
2Medcical University of Lublin, Lublin, Poland
Introduction: With age, especially in women undergoing menopause, bone density decreases causing the increase in the risk of osteoporotic fractures. The aim of the study is to assess the angular angulation of low-energy thoracic vertebral fracture and its effect on increasing thoracic kyphosis. In addition, the progression of pain and subjective feelings of the patient were assessed in the early and distant follow-up period after the fracture. Material and Methods: The study involved 51 women in postmenopausal period, aged 55 to 80 years (mean = 69.0 years), with an osteoporotic fracture of 1 thoracic vertebra. In the computed tomography, the degree of angular bending of the vertebral body, segmental curvature, and additionally the angle of thoracic spine kyphosis contained between the Th4 and the Th12 bodies were evaluated. Pain complaints were assessed using the visual analogue scale (VAS) after 1 month and 12 months after fracture. In the same period, subjective assessment of patients was carried out using Oswestry Low Back Pain Distress Questionnaire and the Roland-Morris Disability Questionnaire. Results: The measurements showed a vertebral body angle on average 11.8 ± 3.7°, the segmental angle was on average 16.9 ± 5.1°, and the angle of kyphosis between Th4 and Th12 on average 31.2 ± 7.9°. A statistically significant relationship was found between the values of the degree of vertebral body angle and the size of the segmental angle and the angle of thoracic kyphosis. The correlation between the level of fracture and the vertebral body angle was not proven. In the distant period, a significant reduction in pain was demonstrated, as well as an improvement in the subjective assessment of the patient. Conclusions: The fracture of a single vertebrae does not cause a significant kyphotic bending of the thoracic spine. Surgical treatment of such fractures should be considered in the early period, mainly as an analgesic treatment. In the distant period after the fracture, the pain is significantly reduced.
P513: A Canadian Experience With Halo Vest Treatment for Cervical Spine Trauma, Risk Factors, and Complications
Ahmed Aoude1, Sultan Aldebeyan1, David Ben Isreal1, Benjamin Beland1, and Steven Casha1
1University of Calgary, Calagary, Alberta, Canada
Introduction: Halo vest for treatment of cervical spine problems can help avoid surgery for the appropriate patients. However, the literature is unclear about the complication rate and risk factors associated with halo vest treatment. Here we present our experience for halo vest treatment at our institution. Material and Methods: We conduct a retrospective analysis of prospectively collected data for all patients treated with halo vest as definitive treatment at our institution between January 2000 and 2018. All complications were analyzed and documented as patient characteristics that can account for high risk of complication such as past medical history, age, gender, and fracture type. A logistic regression was used to identify risk factors and Student’s t test was used to compare means. Results: This section presents preliminary results to finalize. A total of 750 patients were identified in our database. Among them, 347 were males and 403 females with average age of 63 years (range = 18-91). The average complication rate was 19% and 16% were minor and 3% were major. The majority of minor complication were pin site infection and pin loosening in approximately 50% of minor complications. Failure of halo treatment requiring surgical intervention was seen in approximately 10% of reviewed cases. Different risk factors were analyzed with logistic regression and will be presented at the conference. Age and comorbidities were analyzed. Conclusion: Here we present results for halo vest treatment used as definitive management at our institution. At our institution, we have biweekly follow-ups for patients with halo vest and show that complication rates can be lower than shown in the literature, 19% in our study with the majority being minor complications. Therefore, although no definite conclusion can be made, our results shows that halo vest can be used routinely with low complication rates if adequate follow-up is maintained.
P514: Functional Neurorehabilitation Using the Hybrid Assistive Limb: Are Patients Still Benefiting at the 1-Year Follow-Up?
Emre Yilmaz1, Angeli Mayadev1, Cameron Schmidt1, Kim Kobata1, Ziadee Cambier1, Daniel Norvell1, Alexander von Glinski1, Christian Fisahn1, Rod Oskouian1, and Jens Chapman1
1Swedish Neuroscience Institute, Seattle, WA, USA
Introduction: The hybrid assistive limb (HAL, Cyberdyne, Japan) facilitates voluntary, user-driven ambulation through a neurologically controlled system based on bioelectrical signals derived from the user. This allows for the repeated execution of physiologically faithful gait patterns, crucial to recovery in cases of neurologic motor deficit. In this series, we present the first 9 patients in the United States to undergo HAL neurorehabilitation training. Material and Methods: A case series of 9 patients participating in a single-center prospective, interventional pilot study, who were suffering neurologic motor deficits secondary to spinal cord infarct/injury, multiple sclerosis, surgical resection of a petroclival meningioma, and stroke. Patients were included if they had achieved a stable nonprogressive state in their motor neurologic deficit. The patients underwent 60 sessions of body weight-supported treadmill training (BWSTT) in the HAL over the course of 12 weeks. Measures of functional ambulation (10-m walk test) were performed out of the HAL before and after each session, and at the 12-week, 6-month, and 12-month follow-up. Timed Up and Go (TUG) test was performed each week. Treadmill data (time, distance) while in HAL was recorded at each session. Measures of endurance (6-minute walk test), risk of fall (TUG test), balance impairment (Berg Balance Scale), and improvements in walking performance (Walking Index for Spinal Cord Injury II score [WISCI II]) were measured at baseline, 12-week, 6-month, and 12-month follow-up. Eight out of 9 patients were available for 12-month follow-up. Results: All patients underwent 60 sessions of BWSTT in the HAL suit over the course of 12 weeks. Eight out of 9 patients achieved markedly increased treadmill paces. All patients improved their functional scores, increased the distance in the 6-minute walk test, and decreased TUG times at 12-month follow-up. In the 10-m walk test, all patients achieved a clinically significant decrease in time and steps, and showed improvements in the required assistance level to perform the test. Conclusion: These data show that HAL training is both feasible and effective in the neurorehabilitation of patients. This study showed that patients still benefit from HAL training in terms of improved functional mobility at the 1-year follow-up. Further studies are needed to analyze the long-term benefits for patients.
P515: Is Corticosteroid Application Necessary in Selective Root Blocks?
Carlos Mariano Nirino1 and Carlos Eduardo Nemirovsky1
1Corporación Medica of General San Martin, Buenos Aires, Argentina
Introduction: The aim of this article is to describe the results obtained in 496 patients, who underwent a selective root block because of radiculopathies, lumbosciatica, or chronic low back pain caused by herniated discs, stenosis of the foramen, and/or lateral recess. All of them performed when there was not a good response to medical treatment with nonsteroidal analgesics (NSAIDs) and rehabilitation. All the procedures were performed between February 2016 and August 2018 in our Department of Orthopedics and Traumatology in Corporación Medica of General San Martin in Buenos Aires, Argentina. All the patients were treated by the same spinal team. We have used the same technique in all patients. In 302 patients, we infiltrated a mixture of corticosteroid and local anesthetics and in the rest only anesthetics. This depended mainly on which surgeon performed the procedure and not on the type of pathology of the patient. In both cases, there was a great decrease of pain immediately without depending on the application of corticosteroids or not. The results were very good since 96% of the patients remitted their pain partially or totally with a follow-up at 7 days, at 1 month, and at 6 months. Materials and Methods: A total of 496 patients were evaluated, 161 men and 335 women, who underwent a selective block root according to established protocols. Sixty-one percent of them received a mixture of anesthetics and corticosteroids and the remaining 39% only anesthetics. Patients who had previous spinal surgeries and those who had to be infiltrated in more than 2 lumbosacral levels were excluded from this study. All patients were studied with X-ray and MRI (magnetic resonance imaging). Surgical Technique: Placement of a needle following the desired foraminal pathway controlled under an image intensifier in the anteroposterior and lateral plane in the operating room and infiltration of a mixture of anesthetics and corticosteroids in 61% of the cases and anesthetics in the rest only. Results: In almost all cases, patients had partial or complete remission of their symptoms. In 23%, more than 2 selective root blocks were performed to remit their symptomatology. Only 4% required surgical treatment after having performed more than 6 blocks without success. We did not have any difference between patients who were applied a corticoid and those who underwent the procedure only with local anesthetics. None had post infiltration complications. All patients returned to their normal duties after a few days. Conclusions: After an exhaustive study of each of our patients, we concluded that when we make a selective root block, there is no difference between the injection of a corticoid or not because it is not an inflammatory process of the nerve root but a mechanical process by the compression of it or of the spinal canal. The patients did not present complications and the great majority remitted their symptoms.
P516: Educational Manuals for Low Back Pain and Neck Pain
Ana Clara Alves Cutlac1, Fabiano Araújo Faria1, Sheila Aparecida da Silva1, Anderson Alves Dias1, Jorge Mauad Filho1, Leonardo Franco Pinheiro Gaia Franco Pinheiro Gaia1, and Andréa Licre Pessina Gasparini1
1Federal University of Triangulo Mineiro, Uberaba, Brazil
Introduction: According to the Ministry Health, 70% to 85% of the population will suffer from disabling spinal pain throughout life. Low back pain is the leading cause of absenteeism at work and one of the common reasons for premature retirement. Neck pain, on the other hand, is the second leading cause of consultations in primary health services. The mechanical imbalance of the spine’s structures acts as a harmful factor on the former, often due to influences of incorrect postural and functional attitudes and muscular imbalance. Therefore, the study aims to compare whether self-care manuals developed were effective for pain relief and functional improvement of individuals with nonspecific low back and neck pain in relation to treatment with the same exercise performed in the face-to-face method. Material and Methods: This is a randomized, quantitative, interventional clinical trial involving 11 male and female volunteers with mean age of 51 (±3) years, randomly allocated in a manual group (GM) and a face-to-face group (GP). The application interval of the method was 4 weeks. Results: The GP was present twice a week for intervention, and the GM was advised to perform the exercises, also twice a week, at home, and these volunteers received telephone calls to follow the use of the manual. Both groups were evaluated at the beginning and at the end of the fourth week. Conclusion: Both groups showed clinical relevance, from moderate to severe, of great applicability to the variables cervical and lumbar mobility and pain, which highlights the option of using the self-care manual as a circumstantial support strategy for a patient awaiting care.
Keywords
self-care, low back pain, neck pain, health education
P517: Preliminary Study of the Analysis of Postural Balance in Adolescents With Idiopathic Scoliosis Under the Influence of Virtual Reality
Fernanda Campos1, Lais Lorena Silva1, Luciane Fernanda Rodrigues Martinho Fernandes1, Luciana Aparecida Pascucci Sande de Sousa1, Anderson Alves Dias1, Jorge Mauad Filho1, Leonardo Franco Pinheiro Gaia1, and Andréa Licre Pessina Gasparini1
1Federal University of Triangulo Mineiro, Uberaba, Brazil
Introduction: Postural changes consist of modifications in flexibility, muscular strength, and balance. Thus, body balance is an automatic and unconscious process that enables the individual to withstand the influences of destabilizing gravity and to move freely in the environment. Therefore, the objective of the study was to evaluate whether physiotherapeutic intervention with the use of virtual reality as exercise strategies, promoted changes in the postural balance of adolescents diagnosed with idiopathic scoliosis. Material and Methods: Two volunteers with clinical diagnosis of idiopathic scoliosis were screened at the Maria da Glória Ambulatory, at the Clinical Hospital of the Federal University of Triângulo Mineiro. Volunteer 1, 20 years old, menarche for 5 years, 1.59 cm, and 59 kg (body mass index [BMI] = 23.3 kg/m2) presented with a thoracolumbar scoliotic curve with gibbosity on the right. Volunteer 2, 18 years, menarche for 6 years, 1.61 cm and 50 kg (BMI = 19.3 kg/m2), presented with thoracic scoliotic curve with right gibbosis. Both were evaluated before and after physiotherapeutic intervention with the Balance Error Scoring System and Electronic Balancing Test used to evaluate static postural balance. The study started after the volunteers signed the Free and Informed Consent Term. Results: After 12 weeks of using virtual reality as an intervention method, it was verified that the static balance increased in both tests. The Electronic Balancing Test connected to the Motion Pro 1.0 software showed that the oscillation frequency was decreased in all positions, bipodal, unipodal, eyes open and closed receiving prominence for the unipodal position, with eyes open in both volunteers. Conclusion: Virtual reality, as a physiotherapeutic intervention strategy, offers conditions of stimulation and acquisition of postural balance, being of great importance in cases of idiopathic scoliosis due to the maintenance of upright posture with less postural oscillations and consequently less biomechanical stress.
P518: The Efficacy and Persistence of Selective Nerve Root Block Under Fluoroscopic Guidance for Cervical Radiculopathy
So Hyun Moon1 and Sung Kyu Kim2
1Chosun University, Gwangju, Republic of Korea
2Chonnam National University Hospital, Hwasun, Republic of Korea
Introduction: Cervical selective nerve root block (SNRB) may be considered as alternative treatment when patients suffering from painful cervical radiculopathy have not benefited from conservative therapy. The aim of current study is to evaluate the demographic factors affecting the efficacy of cervical selective nerve root block. Material and Methods: We present result of retrospective 1-year follow-up study of 72 patients with radiculopathy due to cervical disc disease and spondylosis. Patients with myelopathy, gross motor weakness, or any other pathology were excluded. Cervical nerve root blocks were administered every 2 weeks, up to 3 times. The clinical outcomes, including visual analogue scale (VAS) scores, Neck Disability Index (NDI), and patient satisfaction, were assessed before the procedure with those at 1, 3, 6 months, and last follow-up after the procedure. Results: At follow-up, the clinical outcomes showed no significant differences between old age (age ≥60 years) and young age group (age <60 years). Also, there were no significant differences between male and female group. However, acute group (symptom duration ≤3 months) and disc herniation group showed statistically better than chronic group (symptom duration >3 months) and cervical spondylosis group on the clinical outcomes (P < .05). Conclusion: Among multiple demographic factors, the symptom duration and etiology was most significant variable affecting the effect of cervical selective nerve root block.
P519: Safety of Tranexamic Acid Use in Pediatric Patients Undergoing Spinal Fusion Surgery
Sariah Khormaee1, Abhinaba Chatterjee2, Matthew Geiselmann3, and Hooman Kamel2
1Hospital for Special Surgery, New York, NY, USA
2Weill Cornell Medicine, New York, NY, USA
3NYIT College of Osteopathic Medicine, Long Island, NY, USA
Introduction: Pediatric spinal fusion may be associated with significant intraoperative blood loss resulting in postoperative morbidity from transfusion, hypoperfusion, and coagulopathy. One emerging strategy to decrease intraoperative blood loss has been utilization of the antifibrinolytic agent tranexamic acid (TXA). Although widely used in arthroplasty and cardiac surgery, the use of TXA in pediatric spine surgery has been more slowly adopted in part due to safety concerns. To explore these concerns, we examined the perioperative morbidity of TXA use in a large national database. Materials and Methods: This retrospective cohort study included pediatric patients (age 18 years or younger) who were undergoing primary or revision spinal fusion from the Premier Perspective database (Premier, Charlotte, NC) with discharge from January 2013 to December 2015. ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes were used to identify patients who underwent primary or revision spinal fusion and to track postoperative outcomes including transfusions, thrombotic events, seizures, and renal dysfunction. In addition, present on admission indicators were used to ensure that these outcomes were not present prior to the admission for spine surgery. Statistical analysis was performed using Stata v14.2. Results: Of the 2633 pediatric patients who underwent spine fusion in our cohort, 96.2% underwent a primary fusion and 3.84% underwent a revision fusion. The average age in the cohort was 14.1 ± 3.0 years, 64.5% were female, and 66.1% were white. The most common reason for spinal fusion was a diagnosis of adolescent idiopathic scoliosis (AIS) present in 54.7% patients, followed by traumatic injuries requiring fusion (12.8%). On the day of surgery, 15.3% of all pediatric spine fusion patients received TXA. Patients receiving TXA did not have a difference in mean age (14.1 years [95% confidence interval [CI] = 14.0-14.3] vs 14.1y [95% CI = 13.9-14.3]) or mean Charlson Comorbidity Index (0.16 [95% CI = 0.02-0.20] vs 0.17 [95% CI = 0.15-0.18]). However, patients receiving TXA more frequently had a primary diagnosis of AIS compared with those not receiving TXA (74.1% vs 54.5%, P < .001). In contrast, patients receiving TXA were less likely to have a primary diagnosis of trauma compared with those not receiving TXA (0.8% vs 15.0%, P < .001). Overall, 19.2% of patients received a transfusion. Administration of TXA was not associated with a lower odds ratio (OR) of transfusion (OR = 1.2, 95% CI = 0.94-1.58). In this cohort, the only patients with new-onset seizures (5 patients, 0.19% incidence) and pulmonary embolism (4 patients, 0.15% incidence) did not receive TXA. The incidence of deep vein thrombosis was 0.19% (5 patients), but this was not significantly different for patients receiving TXA (0.25% TXA vs 0.18% no TXA, P = .769). There were no patients with new-onset perioperative embolic strokes. Finally, the incidence of a new kidney failure diagnosis was 0.53% (14 patients), which was again not significantly different depending on TXA exposure (0.25% TXA vs 0.58% no TXA, P = .396). Conclusions: In this large cohort of pediatric patients undergoing spinal fusion, there was no increase in seizure, thrombotic (pulmonary embolism/deep vein thrombosis/stroke), or acute renal failure events associated with the use of TXA.
P520: Safety of Tranexamic Acid Use in Adult Spinal Fusion Surgery Patients
Sariah Khormaee1, Abhinaba Chatterjee2, and Hooman Kamel2
1Hospital for Special Surgery, New York, NY, USA
2Weill Cornell Medicine, New York, NY, USA
Introduction: Tranexamic acid (TXA) remains infrequently administered during spine surgery, despite its common use in arthroplasty and cardiac surgery. One potential cause of this may be lingering safety concerns, specifically associated with thromboembolic events and seizures. To explore these concerns, we examined the perioperative morbidity of TXA use during spine fusion in a large national database. Materials and Methods: Adult patients 18 years or older were included in this retrospective cohort study if they had undergone primary or revision posterior spinal fusion as ascertained from International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedural coding within the Premier Perspective database (Premier, Charlotte, NC) from January 2013 to December 2015. This is a nationwide administrative billing database that includes information about inpatient surgical admissions and concomitant drug administration from participating hospitals. ICD-9-CM diagnosis and procedure codes were used to track postoperative outcomes, including transfusions, thrombotic events, and seizures. These diagnoses were separated into new onset and chronic by a present on admission indicator. Statistical analysis was performed using Stata v14.2. Results: There were 182 564 adult patients who underwent spine fusion in our cohort, with 96.6% receiving a primary fusion and 4.38% receiving a revision fusion. The average age in the cohort was 57.8 ± 13.3 years, 52.8% were female, and 80.4% were white. On the day of spine fusion surgery, 3009 (1.65%) received TXA. The patient population that received TXA had different demographic characteristics, compared with who that did not receive TXA. Patients receiving TXA were older (average age 60.6 ± 14.3 years vs 57.8 ± 13.3 years, P < .01) and less likely white (80.7 vs 86.4%, P < .001) compared with those that did not receive TXA. In addition, patients receiving TXA were also more likely to have a primary diagnosis of deformity or scoliosis associated with their fusion surgery (11.2 vs 1.3%, P < .002) and a higher burden of comorbidities (average Charlson Comorbidity Index 0.62 [95% confidence interval [CI] = 0.59-0.65] vs 0.58 [95% CI = 0.57-0.58]). There were 112 patients (0.06%) who had new-onset seizures during an admission for spine fusion surgery. Patients who received TXA during their spine fusion surgery had a higher incidence of new-onset seizures (0.2% TXA vs 0.06% no TXA, P = .01). The overall incidence of new-onset pulmonary embolism during an admission for spine fusion surgery was 0.22%. Those patients given TXA had a higher incidence of pulmonary embolism compared those not receiving TXA (0.40% TXA vs 0.22% no TXA, P = .036). TXA was not associated with increased risk of new-onset deep vein thrombosis (0.33 vs 0.27%, P = .50) or stroke (0.23 vs 0.12%, P = .10). Conclusions: Emerging interest surrounds the use of TXA for decreasing intraoperative blood loss during spine fusion surgery. However, concerns remain regarding its safety profile, particularly for rare events that have high morbidity, like new-onset seizures and thrombotic events. In this large database, we did not find an increased deep vein thrombosis or stroke incidence associated with TXA use but did find that patients who received TXA had an increased incidence of new-onset seizures and pulmonary embolisms in the perioperative period.
P521: Physiotherapy in Nonoperative Management of Degenerative Cervical Myelopathy: A Patient Perspective
Benjamin Davies1, Abdul Badran1, and Mark Kotter1
1University of Cambridge, Cambridge, UK
Introduction: The role of physiotherapy in conservative management of degenerative cervical myelopathy (DCM) is controversial. New international guidelines suggest that it may have a role in the management of mild DCM. To determine patient experience of physiotherapy in nonoperative management of DCM. Material and Methods: An online survey was designed using SurveyMonkey and advertised to patients through a DCM charity (Myelopathy.org), social media (Facebook and Twitter), and Google AdWords. Duplicate responses were limited by respondent IP addresses and identifiable data points. Data was compared using summary statistics. Results: A total of 1075 DCM patients (71% female) completed the survey. Respondents aged 55 (±27.8) years and 55% had suffered from DCM for >3 years. There was global representation but 87% were either from the United Kingdom or the United States, and 92% were Caucasian. Around half of respondents (49%) had received physiotherapy at some point. Of those that had received surgery (38%), only 51% had tried physiotherapy with only 23% having found it subjectively helpful; similar to the proportion in those who had not received surgery (22%). Conclusion: Few patients undergo physiotherapy as part of nonoperative management and fewer still perceive it of benefit. Objective measures of DCM are the same between groups who have and have not undergone physiotherapy.
P522: Evaluation of the Efficiency of Halo Vest Immobilization in Cervical Spine Pathologies
Shankar Acharya1
1Sir Gangaram Hospital, New Delhi, India
Background: Upper cervical spine pathologies like infection and trauma can heal with conservative treatments such as halo vest (HV) immobilization without surgery. The most rigid of these, HV, remains the most frequently used treatment in many centers despite its relatively high frequency of orthosis-related complications. We conducted this study to investigate the clinical outcome, effectiveness, patient satisfaction, and associated complications of HV. Materials and Methods: From January 2009 to January 2017, we treated 23 patients for upper cervical spinal pathologies with HV. For analysis, we divided high cervical pathologies into traumatic fractures and infections. We evaluated the clinical outcome, complication rate, and patient satisfaction. Results: The healing rate for upper cervical fracture using HV was 93.75% (17 patients out of 19 as 3 patients were lost to follow-up and 1 died). Survivorship of the device was 89.47% (17/19 patients completed an intended period of halo immobilization). We observed a 30% failure rate and 10.52% noncompliance rate. The most common complications were ring dislocation (1/19), sixth nerve palsy (1/19), and cervical kyphosis (1/19). Conclusion: The HV produced frequent complications and low patient satisfaction but excellent healing rate. The decision to use HV requires a clarification to the patient of probable complications and constant observation to avoid such complications and unsatisfactory outcomes.
Keywords
halo vest, cervical infection, cervical trauma, complication
P523: Comparison of Corticosteroid Efficacy in Patients With Extruded Disc Hernia Undergoing Transforaminal Root Block
Thiago Maia1, Charbel Junior1, Igor Cardoso1, and Jose Lucas Junior1
1Hospital Santa Casa de Vitória, Vitória, Brazil
Introduction: Among the main causes of low back pain, we highlight the intervertebral disc herniation. As an alternative to surgical treatment, doctors have been using epidural blockade as a minimally invasive technique. The aim of the present study is to compare different corticosteroids (betamethasone, dexamethasone, and triamcinolone) by evaluating the improvement of pain, functionality, and quality of life. Materials and Methods: The initial sample consisted of 60 patients older than 18 years, diagnosed with foraminal extrusive lumbar disc herniation through magnetic resonance imaging, refractory to conservative treatment, and in whom vertebral instability criteria were not observed. All patients responded to visual analogue scale (VAS), Oswestry, Roland-Morris, and 36-item Short Form (SF-36), preblock, 1, 6, and 12 months prior. In the 12-month period, 11 patients failed to follow up due to clinical worsening and need for surgery or new root blockade. Five of these were in the dexamethasone group, 4 in the betamethasone group, and 2 in the triamcinolone group. Results: We obtained the following results referring to the 3 groups: VAS: preblockade: mean 8 to 9, median (M) of 8 to 9, standard deviation (σ) of 1.3 to 1.7; 1 month: mean 5 to 7, M = 6 to 7 and σ = 2.4 to 3.5; 6 months: mean 6, M = 5 to 7, σ = 2.5 to 3.4; 12 months: mean 6, M = 4 to 7, σ = 2.9 to 3.1. Oswestry: preblockade: mean 23 to 28, M = 24-29, σ = 6.9-9.4; 1 month: mean 16 to 22, M = 19 to 25, σ = 9.8 to 14; 6 months: mean 17 to 21, M = 17 to 28, σ = 8.8 to 12.9; 12 months: mean 15 to 20, M = 17 to 24, σ = 11.2 to 12.0; Roland Morris: preblockade: mean 18 to 19, M = 19 and σ = 2.2 to 2.9; 1 month: mean 11 to 16, M = 13 to 17, σ = 4.9 to 8.1; 6 months: mean 13, M = 15 to 17, σ = 7.1 to 8.5; 12 months: mean 11 to 14, M = 14 to 17, σ = 7.4 to 8.9; SF-36: physical health: preblockade: mean 32.3 to 38.5, M = 25.9 to 36.3, σ = 10.8 to 16.7; 1 month: mean 40.4 to 58.7, M = 33.5 to 56.3, σ = 16.7 to 28.1; 6 months: mean 45.8 to 51.5, M = 37.8 to 45.8, σ = 23.6 to 31.4; 12 months: mean 50.1 to 58.1, M = 43.2 to 47.2, σ = 24.5 to 31.0; mental health: preblockade: mean 52.2 to 62.0, M = 46.9 to 64.3, σ = 16.1 to 20.7; 1 month: mean 52.2 to 62.0, M = 46.9 to 64.3, σ = 16.1 to 20.7; 6 months: mean 62.8 to 64.4, M = 57.7 to 61.2, σ = 21.5 to 27.5; 12 months: mean 57.0 to 62.9, M = 53.0 to 55.5, σ = 23.9 to 31.2. Conclusion: The drug should be selected in an individualized way, taking into account its composition, cost, and availability.
Novel Technologies
P524: VITOM Microdiscectomy Assessment and Clinical Outcome
Aftab younus1, Mohammad Hamza Sultan Aftab1, and Abdirashid Aden1
1Helen Joseph Hospital, University of Witwatersrand, Johannesburg, South Africa
Introduction: Lumber disc herniation is a common problem for backache and sciatica. Traditionally, discectomy was done either by open method or by microscope. The problem with microscope is that it is bulky instrument, occupy a large space in theater and costly. The advent of new technology has led to development of VITOM (video-assisted telescopic microscope). This study was done to evaluate and clinical outcome of discectomy with the help of VITOM exoscope. Material and Methods: We have 30 patients from June 2015 to June 2016. All have either pain in the leg or having subtle neurology. All these patients under went microdiscectomy with VITOM and tubular retractor. A 2-cm incision was given, and tubular retractor and discectomy was done. Average duration of surgery was 68 minutes. The blood loss was 120 mL. All patients were discharged in 1 to 3 days. No patient has dural tear, nerve root damage, or recurrence of the disc. These patients were fallow-up for 6 months to 1 year. Result: Ninety percent of patients were satisfied with the procedure. The complication was minimal with this procedure. The advantage of this procedure was following, that is, patient require less analgesia, less postoperative pain, less muscle damage, easy handling of the equipment, good for teaching for the registrar and students in theater. One patient had dural tear, and no other complication was found with this procedure. Conclusion: VITOM micro-exoscopic discectomy is a good procedure. It is a safe and effective procedure for discectomy. It has great advantage that patients had less pain, therefore, they require less analgesia and early return to work. There was very little complication with this procedure.
P525: Fibular Allograft as a Salvage Option in Revision Pedicle Screw Fixation
Hossein Elgafy1, Nathaniel Lempert1, Jacob Stirton1, and Peter Zak1
1University of Toledo Medical Center, Toledo, OH, USA
Introduction: In the setting of revision spine surgery for pseudoarthrosis, a variable amount of pedicle bone loss may be present. This is a result of screw loosening and subsequent screw track widening. Often the bone quality may be poor secondary to aging, malnutrition, previous infection, and smoking. In these difficult cases, multiple techniques have been utilized to enhance the construct strength. Current options for revision pedicle screw fixation include cement-augmented screw fixation and custom-made large diameter screws. The purpose of this study was to present the authors’ experience using fibular allograft in the setting of bone loss with loose pedicle screw revision. Methods: In patients with extensive screw track dilation, fibular allograft was obtained and cut into small, longitudinal strips—approximately 3 mm in thickness. The length of each fibular allograft strut was trimmed to coincide with the length of the former screw, allowing for overhang. Allograft strut was inserted into the screw track along the wall. The screw was then advanced between the allograft, and after full insertion of the screw, the fibular allografts were then trimmed. Results: This technique was successfully used in 10 consecutive patients during revision lumbar spine surgeries for pseudoarthrosis. All patients had loose pedicle screws with significant bone loss around the screw tracks. Excellent purchase was achieved in all patients. Computed tomography scan at the last follow-up showed incorporation of the fibular allograft and sound fusion in all patients except one. Conclusions: Fibular allograft is a viable option in the setting of revision pedicle screw fixation and has several advantages when compared with currently available methods. It avoids the complications associated with cement-augmented pedicle screws. In addition, it can be used impromptu, when other options are not immediately available. This technique can be employed without specialized instrumentation at significant cost savings when compared with custom-made screws. Finally, this technique allows for biologic fixation at the screw-bone interface.
P526: Application of the Rothman Index to Predict Emergency Department Visits Within 30 Days of Elective Posterior Lumbar Surgery
Robert Nicholson1, Nicholas Homsy1, Alireza Nazemi2, Caleb Behrend1, and Jonathan Carmouche1
1Virginia Tech Carilion School of Medicine and Research Institute, Roanoke, VA, USA
2Stony Brook University, Stony Brook, NY, USA
Introduction: The Rothman Index (RI) is a metric used in hospital systems throughout the United States. It synthesizes results from vital signs, laboratory tests, and other values to generate a single numeric value, ranging from −91 to 100, describing patient health. The RI has been studied in elective spine surgery, hip fracture fixation, and other surgical populations to identify patients at risk for unplanned readmission, increased mortality, and admission to the surgical intensive care unit. With each study proposing alternative cutoffs, we sought to determine the ability of each of the published RI thresholds to predict visits to the emergency department (ED) within 30 days of elective spine surgery. Material and Methods: We conducted a retrospective review of 258 patient records from September 30, 2015, to September 6, 2016, at a large tertiary care center. Each patient received posterior lumbar decompression with or without fusion. Four RI values were recorded in the electronic medical record: initial RI, minimum RI, maximum RI, and final RI. The single-value cutoffs analyzed were <65 and <35 for lowest RI score, and <85, <70, and <55 for final RI score. Odds of visiting the ED within 30 days of surgery for each proposed RI cutoff was determined by logistic regression after controlling for surgery duration as recorded in minutes. Variability in RI was determined as the difference between the maximum and minimum RI values. Results: Within the sample (N = 258), 49.8% of patients experienced a decrease in RI before discharge and 8.5% visited the ED within 30 days of surgery. The average decrease from initial RI to final RI was 4.80 for patients who visited the ED and 0.39 for patients who did not visit the ED (P = .08). At discharge, 44.5% of patients had a RI <70, corresponding to high risk of readmission, but did not experience increased odds of visiting the ED (odds ratio [OR] = 0.78, P = .58, 95% confidence interval [CI] = 0.32-1.89). Lowest RI <65 and final RI <85 did not predict whether a patient would visit the ED after surgery (OR = 0.62, P = .37, 95% CI = 0.21-1.78 for lowest RI and OR = 0.50, P = .30, 95% CI = 0.13-1.87 for final RI). Similarly, lowest RI <35 and final RI <55 were not associated with ED visits within 30 days of surgery (OR = 0.83, P = .81, 95% CI = 0.18-3.78 for lowest RI and OR = 1.06, P = .94, 95% CI = 0.23-4.91 for final RI). Finally, we did not observe an association between increased variability in RI score and visiting the ED (OR = 0.99, P = .96, 95% CI = 0.96-1.03). Conclusion: The RI is a promising tool that may help predict adverse outcomes; however, it is currently unknown how the metric should be examined. We do not find that any of the currently proposed cutoffs are able to predict ED visits within 30 days of elective spine surgery. The significance of the RI for the prediction of ED visits and other outcomes is unclear at this time and may vary among institutions.
P527: Thoracic Pedicle Screws—Its Not Difficult! Learning Curve of Thoracic Pedicle Screws Placement and Perforation Parameters Over a Period of 735 Thoracic (T1-T10) Pedicle Screws in Nondeformity Group!!
Zahirabbas Merchant1, Vishal Kundnani1, Rahul Prakash1, Ankit Patel1, Mihir Upadhyaya1, Neil Kire1, and Sanyam Jain1
1Bombay Hospital & Medical Research Center, Mumbai, Maharashtra, India
Introduction: Understanding surgical learning curve and intraoperative problems in thoracic pedicle screws (TPS) insertion may help design education programs/workshops and reduce learning curve and implant-related complications. Aim: Evaluate learning curve of TPS placement over large series of TPS with evolution of perforation incidence and grade in typical thoracic (T1-T10) vertebrae in nondeformity spine Material and Methods: Prospective, cohort study, single surgeon, single center. Postoperative computed tomography (CT) scan of consecutive 92 cases (2012-2017) of typical thoracic vertebrae (T1-T10 vertebrae) pedicle screw instrumentation (n = 735 screws). Perforation incidence, location, and grade using Gertzbein criteria were assessed (3 independent observers) on immediate postoperative CT scan. Grade (1/2/3), level (high/low thoracic and medial/lateral/inferior/superior), type (critical vs noncritical), and clinical implication of perforation were noted. Ninety-two cases divided into 4 equal quartiles (23/group q1, q2, q3, q4)to understand evolution of perforation indices, comparison of perforation indices done over time with each group serving control for prior. Learning curve was assessed using logarithmic curve-fit regression analysis and ANOVA (analysis of variance) test (P < .05). Results: A total of 735 typical TPS (T1 = 52, T2 = 54, T3 = 72, T4 = 82, T5 = 96, T6 = 79, T7 = 82, T8 = 68, T9 = 79, T10 = 71) (q1, n = 180; q2, n = 174; q3, n = 193; q4, n = 188) were studied in 92 patients (53 maleM, 39 female) (infection = 56, trauma = 15, tumor = 11, degenerative = 10). Seventy-two screws classified as perforated = 9.79% (medial-25; lateral-42; superior-2; inferior-3).T4-maximum perforation (n = 14) q1 = 5, q2 = 3, q3 = 3, q4 = 3. High-thoracic (T1-T6) screws higher perforation (55/72, 76.38%) compared with lower levels (T7-T10 = 17/72). Grade 2 = 46 perforation (63.89%), Grade 1 = 22 perforation, and Grade 3 = 4. Critical perforation = 4 patients; neurodeficit in 2 patients required revision. Temporal decrease in perforation rate (q1 = 13.89%, q2 = 9.77%, q3 = 8.31%, q4 = 7.44%) with significant correlation (P = .023) between q1 and q2. Significant lesser medial perforation noted between first 2 quartiles for medial perforation rate with no difference in sequential quartiles (q1 = 5.00%, q2 = 3.44%, q3 = 3.10%, q4 = 2.66%).Similar trends observed for lateral perforation rate, statistical significance not obtained (q1 = 6.66%, q2 = 5.74%, q3 = 5.26%, q4 = 4.78%). Asymptote status achieved after first quartile (23 cases-180 screws) with no statistically significant improvement further. Conclusion: (1) Learning curve with reducing perforation rates can be mastered within first 23 cases and TPS perforation reduces over time—medial perforation, severity, and grade of perforation. (2) Workshop/mentorship programs can be designed to achieve asymptote status and reduce pedicle perforation and complications even before performing the first case.
P528: The HALO Digital Goniometer and VALD HumanTrak System: Validation of Novel Goniometric Devices for the Assessment of the Cervical Spine
Ashley Wilson-Smith1, Saimurooban Muralidaran1, and Monish Maharaj1
1The University New South Wales, Sydney, New South Wales, Australia
Introduction: The universal goniometer (UG) has long been a mainstay in the assessment of range of motion (ROM) in both clinical and research settings.1 The advent of the HALO (model HG1, HALO Medical Devices, Australia) digital goniometer, a novel tool that utilizes a laser guidance system, and the VALD HumanTrak inertial sensor system, present exciting new avenues for research and potential applications for ROM assessment in pathological cohorts. The objective of the present study is to assess the concurrent validity, intra-rater reliability and inter-rater reliability of the HALO and VALD systems for cervical spine, hip, knee, and ankle ROMs. The preliminary findings for 25 cervical spine ROMs are presented here and will soon be completed in full for a cohort of 50 (power 95%, α 5%). It is hoped that following validation, future studies assessing change in ROM in pathological cohorts using these devices will take place. Material and Methods: Twenty-five subjects (ie, those older than 18 years with no history of joint surgery) were recruited and assessed sequentially with the UG, HALO, and VALD devices, by 2 independent researchers (ARWS, SM). The data points of interest for the cervical spine were: cervical flexion (CF), extension (CE), lateral flexion (CLF), and rotation (CR). Both assessors have 3 years of clinical experience and were working off a standardized procedure for measuring ROM that has been outlined by the American Academy of Orthopedic Surgeons (AAOS). All subjects were asked to perform 3 trials of each ROM for all devices, after having performed a “practice” motion to confirm that the movement was being performed correctly and as an effort to curb any learning effect. The VALD system required a number of modifications; primarily, all subjects had to be standing in front of an integrated camera (Microsoft Kinect) to be motion-tracked. Traditionally, a supine position is assumed for assessment of lower limb ROMs, as in the case of the UG and HALO. Each subject was equipped with bracelet sensors on each wrist and ankle, in order to enhance the system’s accuracy. The system was calibrated prior to each subject being assessed, and they were positioned in a set “target zone” for each measurement. Data analysis was carried out using IBM SPSS Statistics 25. Results: The preliminary findings present a good case for the application of the HALO digital goniometer as a substitute for the UG, with excellent intra- and inter-rater agreement and reliability. Intra-assessor agreement values comparing HALO to the UG were 0.856, 0.857, 0.897, and 0.824 for cervical flexion, extension, lateral flexion, and rotation, respectively. Inter-rater reliability values for the same ROMs were 0.684, 0.703, 0.656, and 0.532. In comparison, the HumanTrak system illustrated poor agreement with the UG, with intra-rater values at 0.221, 0.070, and 0.331 (CR was not assessable using this system). Inter-rater values were highly agreeable, at 0.896, 0.913, and 0.882. Conclusion: The primary findings are encouraging for the HALO but not so for the HumanTrak system. With an increased sample size, it is hoped that the improved outcomes for both devices will be elucidated.
Reference
1. de Koning, van den Heuvel SP, Staal JB, Smits-Engelsman BC, Hendriks EJ. Clinimetric evaluation of active range of motion measures in patients with non-specific neck pain: a systematic review. Eur Spine J. 2008;17:905-921.
P529: Cervical-Thoracic Congenital Scoliosis Associated With Sprengel Disease: Does the “One-Narcosis” Correction Could Be Effective or Could Be VEPTR Nonoptimal Option?
Aleksandr Mushkin1 and Igor Komolkin1
1St. Petersburg Research Institute of Phthisiopulmonology, St. Petersburg, Russian Federation
Introduction: Klippel-Feil-Sprengel (KFS) syndrome includes a combination of congenital cervical/upper thoracic (C/uTh) scoliosis, high scapula position, and sometimes absence of upper rib(s). The treatment strategy for such deformity’s simultaneous correction in early aged patients is not clear. Material and Methods: Three patients ranging in age from 1 year 4 months till 5 years 1 month underwent simultaneous surgery on C/uTh scoliosis and high scapula position. In all cases, scapula located on the concave side of scoliosis at suboccipital zone (C1-C2 level). Thoracic insufficieny syndrome was present in all cases, 2 cases were associated with hypoplasia or absence of 2 or 3 upper ribs. The follow-up period floated from 6 months till 2 years. Results: Space available for lung (SAL) on the concave side was 76% (68%; 87%) when compared with convex one. Cervical-thoracic scoliosis was 50.6° in average (48°; 52°) before surgery. Simultaneous surgical scoliosis correction and scapulae lowering were done in all cases. Depending on the type of abnormality, scapula inferior dislocation was associated with “rib-to-rib” VEPTR and spine instrumentation (2 cases); 1 surgery included scapulae inferior dislocation with ribs block resection, wedge spinal osteotomy provided with ultrasound bone scalpel, and posterior instrumentation (PI). Two-stage surgeries were done in VEPTR. The scapula inferior dislocation was effective in all cases. The SAL asymmetry was improved till 87% in average postoperative scoliosis was 28° (24°; 32°) with deformity correction from 16° till 28°; the best effect is reached in case with ribs block resection and spinal osteotomy. No postoperative complications were registered. Conclusion: Treatment strategy in cases of combined congenital C/uTh scoliosis and Sprengel disease (KFS syndrome) have to be individualized: scapula inferior dislocation could be effectively applied simultaneously with spinal surgery despite early age of patients;VEPTR instrumentation could not be effective in cases of hypoplasia or aplasia of upper ribs; upper thoracic spine wedge osteotomy and PI in combination with ribs block resection is most effective surgery for such patients. Study Limitation: Small clinical group due to the rarity of combined abnormality and short follow-up period.
P530: Novel Treatment Technique for Extensive Cervical Ossification of the Posterior Longitudinal Ligament With Kyphotic Deformity Using Posterior Thick Pedicle Screw System Fixation With Laminectomy and Foraminal Decompression
Yuehui Zhang1, Jia Song1, Jing Zhang1, and Jiang Shao1
1Xin Hua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
Introduction: The optimal surgical strategy for extensive cervical ossification of the posterior longitudinal ligament (OPLL) with kyphotic deformity remains controversial. Various complications are associated with anterior decompressive surgery, with poor clinical outcomes due to incomplete decompression in posterior surgery. Moreover, combining the 2 approaches leads to extensive surgical trauma and high cost. This study aimed to present a novel technique in which the K-line is changed from negative to positive in patients with extensive cervical OPLL and kyphotic deformity, using only posterior thick pedicle screw system fixation. Methods: Between 2011 and 2017, 12 consecutive patients with extensive cervical OPLL and kyphotic deformity underwent posterior cervical pedicle screw system fixation with laminectomy and foraminal decompression. The pedicle screw diameter was 4.0 or 4.35 mm and the rod diameter was 5.0 mm. After insertion of the posterior cervical pedicle screw system, laminectomy and foraminal decompression were performed; a prebent rod was then installed to convert the cervical K-line from negative to positive, with excellent bony purchase using the pedicle screw system. Radiographic parameters including extent of OPLL, maximum canal occupying ratio (%), and C2-7 angle was analyzed. Accuracy of pedicle screw placement was assessed on postoperative computed tomography and evaluated using the following definitions: type I, screw threads completely within the bone; type II, less than half the diameter of the screw violates the surrounding cortex; and type III, clear violation of transverse foramen or spinal canal. The Japanese Orthopaedic Association (JOA) score and visual analogue scale (VAS) score were analyzed. Quality of life was assessed using the Neck Disability Index (NDI). The demographic data and complications were recorded. Results: The 12 patients included 8 males and 4 females, mean age 62.5 years, with a mean follow-up of 31 months. The mean extent of OPLL was 4.2 vertebral body levels, and posterior fusion was performed on a mean 5.2 segments. The average C2-C7 angle and maximum canal-occupying ratio improved from 9.20 to −11.42° and from 78.3% to 35.5% at follow-up, respectively. Among 108 pedicle screws, 97.3% were deemed “safe” (type I or II) and 84.2% (91/108) of the remaining screws were rated as being ideal (type I); 3 screws (2.7%) were identified as unacceptable (Type III). Preoperative JOA, VAS, and NDI scores were significantly improved (8.4-13.6, 8.1-2, and 17.4-9.8, respectively) at the last follow-up. No specific complications related to this technique were identified. Conclusion: Single posterior surgery with thick pedicle screw system may be effective and safe for patients with extensive cervical OPLL and kyphotic deformity (K-line negative). Further studies with more cases are required to evaluate long-term efficacy and safety.
P531: A Novel Detoured Unilateral Temporary Stainless Steel Bar for Pedicle Subtraction Osteotomy Procedure: A Technical Note
Wendy Lee1 and Chung Chek Wong2
1Sibu Hospital, Sibu, Malaysia
2Sarawak General Hospital, Kuching, Malaysia
Introduction: Variants of pedicle subtraction osteotomy technique have been described in the literature. The pedicles have long been the conduits through which earlier predecessors employed to reach the anterior column of the spine from the posterior approach. From the perspectives of spinal osteotomies,1 Thomasen2 in 1985 introduced lumbar transpedicular intravertebral body wedge osteotomy, addressing surgical correction of fixed sagittal imbalance in ankylosing spondylitis. A decade prior, Heinig developed the eggshell technique3,4 encompassing procedures from transpedicular decompression and posterior fusion to more complex procedures, including transpedicular vertebrectomy and strut-grafting or pedicle subtraction (closing wedge) osteotomy with posterolateral fusion for trauma, deformity, infection, and tumor. Evolution through time and experience in our practice led to the innovation of this novel temporary stainless steel bar in an effort to refine the seemingly minute but surgical pearls nonetheless across these variations of technique. Material and Methods: A 5.5-mm diameter stainless steel rod was tailored to a unique contour distinct from the conventional unilateral temporary rod in that it detours not only the central but also paracentral fields of surgical work at the intended pathological and/or deformed vertebrae, as far lateral to just beyond the transverse process (lumbar) and costotransverse process (thoracic), in essence to provide more leeway for all surgical maneuvers pertinent to the variants of pedicle subtraction osteotomy techniques. This physical rod diversion, away from the vertebra where the osteotomy and/or transpedicular decompression takes place—analogous to that of an outer frame a flip-open window pane—connects back to the original routes at each cephalad and caudal poles—retains the fundamentally inherent stabilization required for the temporary rod to be held down to the adjacent pedicle screws construct. The horizontally diverted frames at both poles were also concavely curved to enhance smoother transition and assimilation onto the subperiosteally dissected paraspinal soft tissues. Results: The rod contour allows undertakings of surgical work by 2 surgeons simultaneously, obviating contralateral rod switching. Both are afforded ipsilateral less restrictive views into the lateral as well as anterior spinal columns. Greater diagonal angular margin provides convenience of surgical instruments access to the posterior vertebral body and ventral epidural complex—the merit of which is invaluable to achieve most generous decompression and release in tackling foci of epidural compression be it from infective, tumor, trauma, or deformity perspectives. Course of exiting nerve root and importantly that of the cephalad traversing root can be traced to avoid inadvertent injury. In the event that a thoracic root has to be ligated, the inherently limited access zone would not be impeded as would be in the case of conventional rod. The opted stainless steel material prevents potential deformation thus averting compromise to temporary stability and vertebral translation. Conclusion: Cumulative time saved on these ostensibly minutiae of the procedure aid in condensing overall operative time. In a similar vein, inevitable blood loss owing to both the technique itself as well as the underlying pathological process can be abbreviated. Versatility of this novel bar translates into ease of existing spinal instruments incorporation thus adaptability across institutions.
Acknowledgment
The authors would like to thank Mr Edwin Key for his contribution to this novel innovation.
Reference
1. Lazennec JY, Saillant G, Saidi K, et al. Surgery of the deformities in ankylosing spondylitis: our experience of lumbar osteotomies in 31 patients. Eur Spine J. 1997;6:222-232.
2. Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;(194):142-152.
3. Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): a retrospective review of 59 patients. Spine (Phila Pa 1976). 2002;27:2338-2345.
4. Heinig CA. Eggshell procedure. In: Luque ER, ed. Segmental Spinal Instrumentation. Thorofare, NJ: Slack; 1984:221-230.
P532: Effect of Forced-Air Warming Blanket Position in Elective Lumbar Spine Surgery: Intraoperative Body Temperature and Postoperative Complications
Morenikeji Buraimoh1, Alysa Nash1, Bailey Howard2, Farooq Usmani1, Jael Camacho1, Eugene Koh1, Kelley Banagan1, Daniel Gelb1, and Steven Ludwig1
1University of Maryland Medical Center, Baltimore, MD, USA
2University of Maryland, Baltimore, MD, USA
Introduction: Perioperative hypothermia is defined as a core temperature below 36°C, and it may occur during surgery for a number of reasons. In the setting of low operating temperature, anesthesia interferes with the body’s natural thermoregulatory processes. Perioperative hypothermia is linked to multiple postoperative complications, including increased surgical bleeding, surgical site infection, myocardial events, and increased length of hospital stay. Active warming via forced-air warming blankets, such as Bair Hugger, is an effective method for combating intraoperative hypothermia. However, there are no guidelines for its proper positioning. We aimed to determine the effects of Bair Hugger positioning during elective lumbar spine surgery on intraoperative body temperature and perioperative complications. Material and Methods: Patients undergoing elective lumbar spine surgery were enrolled. They were excluded if: they had a history of arterial or venous thromboembolic disease, known heritable hypercoagulable state, active infection at the surgical site, intravascular clotting disorder, active malignancy, or were recipient of intraoperative blood products. Patient were randomized into 2 groups: group 1—upper body Bair Hugger placed on top of upper back and arms or group 2—lower body Bair Hugger secured under the torso and legs. Our primary outcomes were average intraoperative body temperature, hypothermic integral, postoperative medical complications, and postoperative infection. Secondary outcomes included operative blood loss and length of stay. For continuous variables, an independent t test was used to determine differences between groups. For categorical variables, Fisher’s exact test was used to determine associations between the 2 groups. For nonparametric distribution, Kruskal-Wallis test was used. Results: Thirty-eight patients and 36 patients were included for analysis in groups 1 and 2, respectively. There was a higher prevalence of coronary artery disease in group 1 (21.1% vs 2.8%, P = .03). There were no statistically significant differences between groups in terms of levels of surgery, procedure types, operative time (P = .87), or estimated operative blood loss (P = .33). Average body temperature was 35.7°C in group 1 and 35.8°C in group 2 (P = .27). Incidence of critical hypothermia (T < 35°C) was 18.4% and 11.1% in groups 1 and 2, respectively (P = .52), whereas incidence of mild hypothermia (T: 35°C to 36°C) was 34.2% and 30.56% in groups 1 and 2, respectively (P = .81). Pooled data from both groups compared operative blood loss in patients with hypothermia versus normothermia (<36°C vs ≥36°C), showing an increased likelihood of having EBL (estimated blood loss) greater than 300 cm3 (P = .049) for normothermic patients. Separately, pooled analysis comparing average body temperature and incidence infection demonstrated a relationship between mild hypothermia and infection (P = .03) but not critical hypothermia (P = 1.0). Conclusion: The use of standard upper body Bair Hugger positioning may be associated with higher postoperative infection rates when compared with lower body under patient setup. There is also a statistically significant relationship between mild hypothermia and infection, as well as normothermia and increased blood loss. Given the prospective randomized study design evaluating Bair Hugger position in patients undergoing lumbar spine surgery, we recommend the use of lower body Bair Huffer position to reduce risk of postoperative infection.
P533: Titanium Nano-Coated PEEK Cages: A Safe Implant in Spinal Fusions
Annette Kienle1 and Karel Willems2
1SpineServ Gmbh, Ulm, Germany
2Az Delta Roeselare, Roeselare, Belgium
Introduction: Posterior lumbar interbody fusion (PLIF) using cages in conjunction with pedicle screw fixation is considered the gold standard for surgical treatment of degenerative lumbar spine disorders due to its biomechanical stability and high fusion rate. The goal of PLIF surgery is to achieve successful fusion and to improve functional outcomes while limiting a patient’s morbidity. The development of material and techniques evolved from simple wiring to the combination of transforaminal interbody fusion with polyetheretherketone (PEEK) cages and pedicle screw fixation with polyaxial screws. Titanium (Ti) cages are considered the gold standard, but the more elastic PEEK cage seems to result in better clinical and radiological outcome. PEEK is an inert material that does not promote bony ingrowth. Several types of coating have been used to combine the mechanical characteristics of PEEK with a bioactive layer in both an animal sheep model as in a clinical study. Impaction of the Ti nano-coated cage is safe and creates less debris than Ti plasma-sprayed cages. Material and Methods: The experimental setup was designed to mimic cage impaction into the intervertebral disc space using polyurethane (PU) foam blocks as vertebral body substitutes. The cage surface was inspected before and after impaction, and their weight was measured. Impaction resulted in abrasion at the tip of the ridges on the implant surface. Results: The mean weight loss was 0.39 mg for the uncoated cages, 0.57 mg for the CaP nano-coated cages, and 0.75 mg for the Ti nanocoated cages. These differences were statistically significant. In conclusion, differences between the 3 cage types were found concerning the amount of abrasion. However, all 3 cages lost less weight than a comparative Ti plasma spray–coated cage, which showed a mean weight loss of 2.02 mg. Conclusion: The amount of wear during impaction of the Ti nano-coated cage is 075 mg and acceptable for the FDA (Food and Drug Administration) guidance document.
P534: Using Machine Learning on Medical Text Can Identify Acute Kidney Injury Following Orthopedic Surgery
Jun Kim1, Varun Arvind1, Aly Valliani1, Brian Cho1, Daniel Ranti1, Zoe Cheung1, Ivan Ye1, Ray Tang1, Deepak Kaji1, Zoe Cheung1, and Samuel Cho1
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Quality improvement studies have provided surgeons with systematic insight on how to make changes to their practice to improve patient outcomes and avoid complications. However, currently most automated methods to identify patient complications for quality improvement studies rely on prelabeled administrative codes sampling data from fixed electronic medical databases. Medical notes contain a rich supply of medical data, yet the format of unstructured text has precluded these data from use in large retrospective analyses. Therefore, the utilization of free text from electronic medical records using natural language processing in combination with machine learning can provide an additional tool for patient complication surveillance and identification. The purpose of this study was to develop a machine learning algorithm that can identify postsurgical acute kidney injury (AKI) based on unstructured patient notes. Materials and Methods: This was a retrospective analysis of medical notes from the Medical Information Mart for Intensive Care (MIMIC III), a large, single-center database composed of intensive care unit admissions data from 2001 to 2012. A total of 947 patients from the orthopedic service were identified. Patients who experienced AKI were identified using International Classification of Diseases, Ninth Revision (ICD-9) code (5849). A total of 15 004 notes were analyzed in total from the 947 patients. Of the 15 004 notes, 5591 notes were from patients positive for AKI and 9413 notes were negative for AKI defined by ICD-9 code. Area under the receiver operating characteristic curve (ROC), accuracy, sensitivity, and specificity of the model were evaluated to assess performance of the model. Natural language processing was used to analyze unstructured narrative discharge notes and train a support vector machine algorithm to train a classifier to automatically identify patients with AKI based solely on unstructured discharge notes. The data was randomized with 70% used for training and 30% used for testing. Results: The SVM (support vector machine) algorithm identified AKI notes with a sensitivity and specificity of 79% and 78%, respectively. The overall accuracy was 78.1% with area under ROC of 0.78. Conclusions: Combining natural language processing with machine learning is a valid approach for automatic identification of AKI using unstructured text from discharge notes. This method provides a robust survey of surgical encounters and may be used for real-time surveillance of postoperative complication risk and for automated identification of patient complications such as AKI for quality improvement studies.
P535: Machine Learning Can Identify Postoperative Complications Following Anterior Spinal Fusion Using Medical Notes
Varun Arvind1, Brian Cho1, Daniel Ranti1, Deepak Kaji1, Ivan Ye1, Ray Tang1, Zoe Cheung2, Andrew Warburton1, Aly Valliani1, Jun Kim2, and Samuel Cho2
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
2Mount Sinai Hospital, New York, NY, USA
Introduction: Quality improvement studies have provided surgeons with systematic insight on how to make changes to their practice to improve patient outcomes and avoid complications. However, currently most automated methods to identify patient complications for quality improvement studies rely on prelabeled administrative codes sampling data from fixed electronic medical databases. Medical notes contain a rich supply of medical data, yet the format of unstructured text has precluded these data from use in large retrospective analyses. Therefore, the utilization of free text from electronic medical records using natural language processing in combination with machine learning can provide an additional tool for patient complication surveillance and identification. The purpose of this study was to develop a machine learning algorithm that can identify patients with common spine surgery complications based on unstructured patient notes. Material and Methods: This was a retrospective analysis of medical notes from the Medical Information Mart for Intensive Care (MIMIC III), a large, single-center database comproed of intensive care unit admissions data from 2001 to 2012. Spinal surgery complications include pseudoarthrosis, spinal cord injury, retrograde ejaculation, cardiac, respiratory, vascular, CNS (central nervous system), hematoma formation, hemorrhage, infection, and CSF (cerebrospinal fluid) leak complications as identified by International Classification of Diseases, Ninth Revision (ICD-9) codes. Natural language processing was used to analyze unstructured narrative notes including physician, consult, discharge, radiology, nursing, pharmacy, and social work notes. The notes were preprocessed using natural language processing methods and an autocorrect function was performed. A support vector machine (SVM) algorithm was used to train a classifier to automatically identify patients with complicated anterior spinal fusion based solely on the notes. The data were randomized with 70% used for training and 30% used for testing. Area under the receiver operating characteristic curve (ROC) were evaluated to assess performance of the model. Results: A total of 288 patients from the orthopedic service were identified as undergoing anterior spinal fusion (ICD-9: 8104 and 8106), with 133 patients experiencing spinal surgery complication (46%). Sixty-four percent of patients were male with 83% of cases being emergent and 15% elective. Sixty-three percent of patients were Medicare insured, 27% privately insured, 9% insured through Medicaid, and the rest insured through government insurance or self-pay. The SVM algorithm identified anterior spinal fusion notes with an area under ROC of 0.65. Conclusion: Combining natural language processing with machine learning is a valid approach for automatic identification of complications following anterior spinal fusion using unstructured text from discharge notes. This method provides a robust survey of surgical encounters and describes a method that may be used for real-time surveillance of postoperative complication risk and for automated identification of patient complications for quality improvement studies.
P536: Monoaxial Pedicle Screws for Reduction and Ring Fixation of Instable C1 Fractures
Renate Krassnig1, Rainer Gumpert1, Gloria Maria Hohenberger1, Nikolas Eibinger1, and Paul Puchwein1
1University Hospital of Orthopedic Surgery and Traumatology, Graz, Austria
Introduction: Ring fixation of C1 can be performed using pedicle screws and a rod in case of unstable Jefferson or lateral mass fractures of C1. Material and Methods: In a case series of 3 patients, we stabilized C1 fractures surgically using a modified technique of C1 ring fixation by using monoaxial instead of polyaxial screws. Functional outcome and pain was recorded postoperatively. Results: In this very small case series, we observed good results concerning pain and functional outcome. All fractures were bony healed within 13 weeks. In 1 case, a screw penetrated the spinal canal and had to be repositioned. A mild irritation of C2 nerve root occurred in 2 cases postoperatively. Conclusion: C1 ring fusion with monoaxial screws provides a good ability to reduce the fracture indirectly by the screws and the rod itself.
P537: Telemedicine From Neurosurgery Department Patients’ Perspective: Is There a Place for Telerehabilitation in Postoperative Spine Management?
Uladzislau Ulasavets1, Ewelina Grzywna2, Jaroslaw Polak2, Pawel Adamkiewicz3, Katarzyna Jasinska1, Irena Roterman-Konieczna4, and Marek Moskala2
1Jagiellonian University Medical College, Kraków, Poland
2Department of Neurosurgery and Neurotraumatology, Kraków, Poland
3Polskie Centrum Rehabilitacji Funkcjonalnej Votum, Kraków, Poland
4Department of Bioinformatics and Telemedicine, Kraków, Poland
Introduction: The number of patients undergoing neurosurgical procedures increases, wherefore the burdened patients need professional, holistic approach, which is not always available particular in low-income countries. The aim of our study is to assess patients willingness to use a free telerehabilitation (TR) device at neurosurgery department. Material and Methods: The process of potential TR implementation was analyzed, and a 91-item questionnaire was created. Past medical history, current neurological status, disability level, and patients attitude to TR were investigated. Individual and comparative analyses were performed. Results: A total of 100 patients aged 54 ± 19.00 years hospitalized in the neurosurgery department were included into the study (41% males and 59% females). Fifty-one of them lived in urban and 49 in rural area. Forty-four patients suffered from degenerative spine disease. More than the half of the patients (61%) received rehabilitation during life and 88% believed that there is difficulty to admittance rehabilitation; and 26% mentioned high cost of attending rehabilitation. According to patients experience, the accessibility of institutional rehabilitation is not well or bad (34% and 26%). Participants held positive view of potential-free TR interventions (44% to 80%). However, while 90% owned mobile phones, less people had smart phones or computers (42%0vs 65%). Conclusion: According to our survey, patients believe that continuous monitoring of the treatment process through a mobile system, foreseen by specialist can lead to better outcomes. Our data suggests that degenerative spine disease patients group are potential good candidates to start TR. We believe TR can help introduce the innovation service in the e-health field and expand the paradigm of better care.
P538: “Skipping” Posterior Hemivertebra Resection With Short Fusion for Congenital Scoliokyphosis Due to 2 Nonadjacent Fully Segmented Hemivertebras: The Preliminary Results of 7 Patients With More Than 3-Year Follow-Up
Shengru Wang1 and Jianguo Zhang1
1Peking Union Medical College Hospital, Beijing, China
Introduction: Posterior hemivertebra resection with short segmental fusion has been proven to be an ideal procedure for congenital scoliokyphosis due to a single fully segmented hemivetebra. However, the early treatment of the complex congenital spinal deformities due to nonadjacent fully segmented hemivertebras has not been well studied. Traditionally, long fusion or fusionless technique may be chosen. In this study, we chose separate posterior hemivertebra resection with short segmental fusion for selected patients with this kind of deformities. This study was conducted to evaluate the results of separate posterior hemivertebra resection with short segmental fusion for the treatment of complex congenital spinal deformities due to nonadjacent fully segmented hemivertebras. Materials and Methods: Seven patients (3 male, 4 female) averaged 4.7 (3-9) years with congenital scoliokyphosis due to 2 nonadjacent fully segmented hemivertebras were enrolled. The location of the upper hemivertebra of each patient was T7/8, T12, L2/3, T6/7, T12/L1, T10/11, T12/L1 and that of the lower one was T11/12, L3, L4/5, L2, L4/5, L3, and L5. All of them were treated with “skipping” posterior hemivertebra resection with short segmental fusion. Radiographic measurements were taken to evaluate the results of correction. The patients’ charts were reviewed. Results: All patients were followed at least for 3 years. The averaged fused segments were 2.4 for each patient and 1.2 for each hemivertebra. The segmental scoliosis was 42.6 before surgery, 3.1 post surgery, and 5.1 at the latest the follow-up. And the segmental kyphosis (difference to normal segmental alignment) improved from 14.6 to 5.4. The correction of the compensatory cranial and caudal curve was 86.1% and 83.4%. Trunk shift improved from 22.7 mm to 5.7 mm. No complications occurred. Conclusion: Separate posterior hemivertebra resection with short segmental fusion could provide satisfied correction with limited fusion. It could help avoid long fusion or fusionless technique, thus mobile segments could be saved. It may be an ideal procedure for the early treatment of congenital scoliokyphosis due to nonadjacent fully segmented hemivertebras before the long, severe, and rigid deformities occurred.
P539: Design of a Novel Cephalic Traction System for the Treatment of Early-Onset Severe Scoliosis
Fernando Alvarado-Gómez1, David Meneses-Quintero1, Wilmer Godoy-Carrero1, Carlos Montero1, Alejandro Mejía-Rojas1, Laura Montoya-Sánchez1, and Alexander Tristancho-Baró1
1Instituto de Ortopedia Infantil Roosevelt, Bogota, Colombia
Introduction: Severe early-onset scoliosis is known for the complications on pulmonary insufficiency, neurologic compromise, and major difficulty on its management due to curve severity, in most cases, Cobb angle greater than 100°. Treatment of this condition is challenging, as to why many authors have advocated the use of halo-gravity traction to allow gradual curve correction prior to surgery, not only to reduce the burden and perioperative complications but also to monitor neurologic function in the awake patient as traction force is increased, reducing the risk of permanent neurological damage. Even though cephalic traction provides adequate corrective forces for severe deformities, it requires extended periods of bed rest and detriment of patients’ quality of life. Given these conditions, we evaluated the need to create a novel, easy-to-use cephalic traction system that would allow the patients to receive the adequate halo-traction therapy without majorly decreasing their life quality and preventing their prostration. Materials and Methods: The traditional halo-traction system consists of attaching a ring to the patient’s skull using screws and weights that, due to gravity, eject a force in the opposite direction. It has the problem that it is not easily adjustable to patient’s allocation, daily activities, and the required force to support his body weight. It also has problems related with force. Although there is an effective method available using counter weight, our goal was to evaluate how viable it is to change the way this force is being applied in order to improve the treatment’s outcomes and its impact on patient’s overall health. Results: An automatized system was developed, and it has the ability to measure and control the traction force instantaneously. This system is adapted to a metallic tripoidal structure able to resist a maximum of 50 kg of force. The traction force is mechanically driven by a pulley system that can be used either manually or authomatically. It is easily adaptable to all inpatient scenarios such as the beds, therapy bicycles, and restroom lavatories, and it may be adjustable to every outpatient scenario as well. It is powered by a rechargable batteries system that ensures the application of the traction 24 hours a day. Conclusion: A novel cephalic traction system was designed and manufactured with a combination of a motor and manual system, giving the possibility of being easily operated either manually or automatically by all health professionals, reducing mistakes on weight upgrade, and decreasing overall health complications. Further tests are needed in healthy volunteers to proof its safety, so it may be implemented on patients with early-onset severe scoliosis requiring halo-traction therapy prior to surgical correction of the spine deformity.
P540: MiHem Approach to Intradural Pathologies: A Cost-Effective Minimal Access Technique
Amit Thapa1
1Kathmandu Medical College Teaching Hospital, Kathmandu, Nepal
Introduction and Objective: Classically wide laminectomy is used to access intradural spinal pathologies (ISP); however, it puts the spine to risk of lordosis as well increases cost of treatment due to need of implants to counter its occurrence. We have introduced, standardized, and analyzed the technique of MiHem (microscopic hemilaminectomy) technique to safely excise ISP through small exposures and present our experiences here. Materials and Methods: We retrospectively studied the patients with cervical spine ISP undergoing MiHem approach during the past 6 years at KMCTH (Kathmandu Medical College Teaching Hospital). Endpoints studied were feasibility, time taken, extent of tumor excision, postoperative CSF (cerebrospinal fluid) leak, wound infection, change in Cobbs’s angle, neurological deficits, and cost of surgery. Results: Of the total 300 patients operated for spinal conditions, 37 patients underwent MiHem approach, of which 13 were on cervical spine. Age of patients ranged from 28 to 65 years (mean = 47.5 years). Three patients had neurofibroma, 3 ependymoma, 2 schwannoma, 2 astrocytoma, 1 syrinx, 1 GBM (glioblastoma multiforme), and 1 underwent for DREZtomy. MiHem provided adequate exposure, did not add any intraoperative complications, and took an average 1.5 hours. With no requirement of instrumentation, cost of surgery was average $400 and patients could be mobilized on second postoperative day. Average follow-up of 3 years did not show any postoperative scoliosis or kyphotic deformity in spine even in those 50% patients who had been operated at junctional areas or at apex of cervical lordotic curve. Conclusion: MiHem techniques provided good exposure and good postoperative outcomes. As it avoided the need of fixating instrumentations, it is a cost-effective technique in developing countries.
Keywords
intradural spine tumors, minimal invasive, hemilaminectomy
P541: Remote Patient Monitoring: A Systematic Review
Asdrubal Falavigna1, Frederico Arriaga Criscuoli de Farias1, Carolina Matté Dagostini1, and Yan Assunção Bicca1
1University of Caxias do Sul, Caxias do Sul, Brazil
Introduction: Remote monitoring or telemonitoring is an innovative strategy to improve the management and care of patients by early detection of disease decompensation, allowing early interventions and a reduction of mortality and hospitalizations. Available tools consist of intelligent sensors, wearable or handheld devices, telephone, cell phones connected to the Internet, and implanted monitoring devices. Research on telemonitoring has been conducted over the past 15 years. This study aims to perform a systematic review of the publications on telemonitoring for patients with clinical and surgical pathologies. Material and Methods: MEDLINE was searched for clinical studies, clinical trials, comparative studies, and case reports on telemonitoring. Search terms were “telemonitoring OR ihealth OR remote monitoring.” The time frame was from January 1, 2000, to February 1, 2018. Exclusion criteria were case reports with less than 5 cases, surveys, articles in any language other than English, and articles not related to direct telemonitoring of patients. The variables assessed were (1) country of first author’s institution, (2) year of publication, (3) topic or disease, (4) objective of study, (5) mean follow-up time, (6) number of patients in telemonitoring, (7) primary outcome, (8) use of teleconsultation, (9) use of tele-education, (10) presence of a control group, (11) effectiveness of telemonitoring, (12) telemonitoring strategy, and (13) level of evidence. Results: A total of 947 publications were identified but 272 articles were included in the study. The United States was the country with the largest number of publications (38.2%), followed by Italy (11.0%), and the United Kingdom (10.0%). There was a significant increase of publications in recent years, with 43% of articles published between 2015 and 2018. The majority of articles performed the monitoring in clinical pathologies like cardiovascular (47.8%) and endocrine (18.3%) diseases. Postoperative monitoring represented only 2.5% of the sample. The mean follow-up time was ≤6 months in 43.0% of the sample. Studies with ≤50 patients in the telemonitoring group represented 36.0% of the sample, while 23.5% had more than 200 patients. Tele-education was observed in 17.6% of publications and teleconsultation was described in 24.6%. A control group was present in 74.8% of the studies. A positive outcome was perceived in 77.7% of the sample. The most common telemonitoring strategy was the use of wireless devices and/or smartphones (75.7%), followed by implantable devices (15.1%) and telephone call monitoring (9.2%). Analysis of the publications regarding the Oxford Centre for Evidence-Based Medicine Levels of Evidence (LOE) revealed that 18.7% of publications were LOE 1, 73.5% were LOE 2, 6.2% were LOE 3, and 1.5% were LOE 4. LOE 1 studies increased in recent years, providing better evidence on telemonitoring. Conclusion: This review has shown telemonitoring to be more effective than usual care alone. It also shows a growing interest in telemonitoring and its medical applications. Telemonitoring is still to be consistently evaluated in the universe of postoperative care and surgical pathologies.
P542: PMMA Discoplasty for the Stabilization of “Vacuum Discs” in Osteoporotic Patients: An Implant Survival Analysis
Christof Birkenmaier1, Bernd Wegener1, and Carolin Melcher1
1Ludwig-Maximilian-University Munich, Munich, Germany
Introduction: Old and comorbid patients with osteoporosis have a high risk of cage subsidence, nonunion, and construct failure with reconstructive spinal surgery. This is due to poor biology, poor bone quality, and biomechanical challenges (very stiff implants vs very weak bone). Filling an instable (vacuum) disc space with malleable polymethyl methacrylate (PMMA) will lead to a larger contact area and a more homogenous load transfer in comparison to traditional cage fusion techniques. With osteoporosis and poor biologic potential, this might lead to lower rates of subsidence, loosening, and construct failure—even though such a technique does not attempt to generate an intersomatic fusion. This case series examines the survival rates of lumbar and thoracolumbar PMMA discoplasties. So far, only few clinical experiences with PMMA discoplasty have been published.1,2 Material and Methods: Thirty patients (19 female, mean age = 76 years, age range = 56-85 years) requiring lumbar or thoracolumbar reconstruction and with osteoporosis (primary and secondary) received PMMA discoplasty—combined with other procedures as required—after informed consent. Twenty were revision surgeries after previous surgeries (some cage pseudarthroses), and 35 procedures were performed overall (3 repeat discoplasty in 2 patients). Disc spaces treated: 2.1 average (range = 1-8). Upper instrumented vertebra (UIV): T5-T9 (7 cases), T10-L1 (4 cases), and below L1 (16 cases). Instrumentation to the pelvis in 11 cases. Overall, 63 disc spaces were augmented. In 7 cases, additional TLIF (transforaminal lumbar interbody fusion) were performed. Eight cases received posterior fusion with additional BMP. Results: The mean follow-up was 2.3 years (minimum 0.1, maximum 5.4). All patients derived considerable clinicial benefit from the procedures overall. Only 1 of the 72 PMMA discoplasties has so far been explanted, equating to a 98% survival rate. There were 2 cases of PJK (proximal junctional kyphosis) and PJF (proximal junctional failure) each in long constructs and 1 case of DJF (distal junctional failure) at L5-S1, but none of these occurred at the level of a discoplasty. In 2 patients, 3 radiologically loosened PMMA discoplasties were re-augmented. In 13 cases, there were complications: 1 seroma, 1 wound dehiscence, 2 superficial surgical site infections (SSIs), 2 deep SSIs, 4 dural tears, 1 L5 neuralgia, 1 adjacent sacral fracture and cage subsidence/screw loosening, 1 cranial adjacent vertebral fracture, 1 prolonged delirium, and 3 radiolucent seams around PMMA discoplasties. Conclusion: Our complications with these old and comorbid osteoporotic patients and in the context of mostly revision surgery are within the expected range. However, the survival rate of 98% with PMMA discoplasty clearly exceeds our results with cage fusion techniques in such patients. This may warrant further investigation.
Reference
1. Sola C, Willhuber GC, Kido G, et al. Percutaneous cement discoplasty for the treatment of advanced degenerative disk disease in elderly patients [published online March 23, 2018]. Eur Spine J. doi:10.1007/s00586-018-5547-7
2. Varga PP, Jakab G, Bors IB, Lazary A, Szoverfi Z. Experiences with PMMA cement as a stand-alone intervertebral spacer. Percutaneous cement discoplasty in the case of vacuum phenomenon within lumbar intervertebral discs [in German]. Orthopade. 2015;44:124-131.
P543: Dosimetric Impact of Standard Titanium Alloy Versus Radiolucent Carbon FiberReinforced PEEK Spinal Instrumentations in Proton Therapy for Spine Tumors
Yu-Mi Ryang1, Birgit Müller2, Bernhard Meyer2, Anna Rienmüller3, and Stephanie E. Combs2
1Helios Klinikum Berlin-Buch, Berlin, Germany
2Klinikum Rechts der Isar, Technical University Munich, Munich, Germany
3University Hospital Vienna, Vienna, Austria
Introduction: New radiolucent carbon fiber-reinforced polyetheretherketone [PEEK] (CFP) pedicle screw systems promise to reduce dosimetric uncertainties in radiotherapy (RT) compared with titanium alloy (Ti) implants. We investigated relative stopping powers (SP) on dosimetric quality for intensity-modulated proton therapy (IMPT) comparing both systems. Material and Methods: The retrospective planning study was based on computed tomography (CT) scans of 10 patients (5 Ti/5 CFP) who received spinal instrumentations for metastatic spine disease and postoperative treatment with proton RT. CFP pedicle screw rod systems (Icotec, Altstätten, Switzerland) composed of partly Ti-coated CFP screws with Ti tulips and Ti rods. To simulate uncertainties in the assigned Hounsfield units (HU) of Ti, corresponding regions were delineated in all CT scans and assigned varying SPs. For each patient, 1 IMPT plan of 3 fields was optimized onto the planning CT with a SP of 3.2 (prescribed dose to planning target volume [PTV]: 30 Gy to 3 Gy). These plans were recalculated with reduced (SP = 3.0) and increased SP (SP = 3.4). Dose distributions were analyzed by PTV coverage, homogeneity, and several dose volume histogram (DVH) values. Additionally, CT artifacts were contoured and resulting volumes evaluated. Results: Volumes of CT artifacts and metal components were smaller in CTs of CFP compared with Ti systems (mean volumes of VCFP(artifacts) = 5.9 ± 1.2 cm3 vs VTi(artifacts) = 18.7 ± 7.4 cm3 and VCFP(metal) = 10.1 ± 0.2 cm3 vs VTi(metal) = 24.4 ± 5.4 cm3. The impact of varying SPs on DVH criteria was larger for Ti. For a SP of 3.4, the average minimum dose received by 1 cm3 decreased by ▵Dmin(PTV) = 5.9 ± 2.9% for Ti and ▵Dmin(PTV) = 1.5 ± 0.5% for CFP. Recalculated doses resulted in more heterogeneous target coverage and more pronounced deviation from the original dose for Ti. The mean standard deviations inside the PTV increased, for example, by ▵σTi(PTV) = 7.8 ± 4.2% and ▵σCFP(PTV) = 2.4 ± 0.9% for SP = 3.0. Conclusion: Dosimetric uncertainties given by inaccurate HU assignment and its conversion to SP are reduced by CFP compared with Ti implants. However, due to the remaining metal components, some uncertainties in dose distributions still remain. Generally, decreasing the fraction of metal does not only improve dosimetric accuracy but is also considered to be beneficial for RT planning through more accurate contouring.
P544: Comparative Cohort Study of Non-Navigated Versus Navigated Percutaneous Pedicle Screw Implantation Using Intraoperative 3D Fluoroscopy
Edward Fomekong1, Julien Pierrard1, and Christian Raftopoulos1
1Cliniques Universitaires Saint-Luc, Woluwe-Saint-Lambert, Belgium
Introduction: The major limitation of computer-based 3-dimensional (3D) fluoroscopy is the increased radiation exposure of patients and the operating room (OR) staff. Adjunction of spine navigation to intraoperative 3D fluoroscopy (io3DF) can likely overcome this shortcoming while increasing the pedicle screw accuracy rate. Thus, we compared data from a cohort of patients undergoing lumbar percutaneous pedicle screw (PPS) placement utilizing io3DF alone or in combination with spine navigation. Materials and Methods: This cohort study consisted of 168 patients who underwent PPS implantation between 2009 and 2016. The primary endpoint was to compare pedicle screw accuracy between the 2 groups. The secondary endpoints were to compare the radiation exposure of patients and OR staff, duration of surgery, and postoperative complications. Results: A total of 438 screws were placed without navigation guidance (group 1) and 276 with spine navigation (group 2). The mean patient age in both groups was 58.6 ± 14.1 years. The final pedicle accuracy rate was 97.9% in group 1 and 99.6% in group 2. The average radiation dose per patient was significantly larger in group 1 (571.9 mGy m2) than in group 2 (365.6 mGy m2) (P = .000088). Surgery duration and complication rate were not significantly different between the 2 groups (P > .05). Conclusion: The io3D fluoroscopy with spine navigation minimizes the radiation exposure of patients and the OR team and provided an excellent PPS accuracy rate with no permanent complications compared with io3DF alone. The setup is recommended, especially for patients with a complex degenerative spine.
P545: A Novel Cost-Effective Training and Assessment Simulator for Spine Surgery
Arash J. Sayari1, Philip Louie1, Jannat Khan1, Howard An1, and Gregory Lopez1
1Rush University Medical Center, Chicago, IL, USA
Introduction: The approach to surgical training has undergone vast changes over the past several decades, especially given the increasing complexity of spine surgery techniques. While other surgical fields have demonstrated success surgical simulation, spine surgery simulation current includes synthetic bone activities, cadaver laboratories, and virtual reality simulators that are costly and often unaffordable for residency programs or are not replicable. Here, we introduce a novel simulator for spine surgery that is feasible, easily reproducible at any institution, and applicable to clinical settings. Materials and Methods: Using items easily found at a local hardware store, a surgical simulator was created to test and assist the surgical trainee aiming to learn and perfect his or her skills in fundamental techniques related to spine surgery. The simulator was built using wood dowels, foam blocks, various thin pliable materials, and surgical instruments. Thirty-six orthopedic surgery trainees with varying experience were tested with the simulator, which included (1) the use of a hand-held burr in minimally invasive surgery (MIS) and open fashion, (2) the use of a Kerrison Rongeur in MIS and open fashion, (3) triangulating with a gear shift awl at designated start points toward specified endpoints, and (4) peg transfer activity with a pituitary Rongeur down a long wider tube to simulate lateral access surgery. Results: Of the 36 trainees, 31 included those without any formal spine surgery experience. When compared with the 5 trainees with more than 10 hours of dedicated spine surgery experience, the novice trainees performed inferiorly across all tasks. The novice trainees were significantly slower than fellows in the MIS burr (P = .03), MIS Kerrison (P = .015), and lateral access (P = .015) tasks. On average, the novice trainees also demonstrated more errors per task when compared with those with experience in spine surgery. Conclusions: This study demonstrates the construct validity of a cost-effective novel surgical simulator for training the fundamentals of spine surgery, objectively demonstrating the higher level performance by senior trainees when compared with those without experience in spine surgery. The results of this study encourage the application of this simulator as a training tool for resident education.
P546: Tracked C-Arm: A Logical Alternative to Plain Films for Intraoperative Evaluation of Spinal Alignment
Shahram Amiri1, Ganesh Swamy2, W. Bradly Jacobs3, Fred Nicholls3, and Kenneth C. Thomas3
1Simon Fraser University, Vancouver, British Columbia, Canada
2University of Calgary, Calgary, Alberta, Canada
3Foothills Medical Centre, Calgary, Alberta, Canada
Introduction: Successful clinical outcomes of spinal deformity surgery have been linked to achieving global spinal and spino-pelvic alignment, thus tasking surgeons with spinal alignment goals intraoperatively. Failing to achieve these goals in multisegmental spinal fusion, or postoperative malalignment, increases the risk of reoperation 10-fold. Despite the importance of global alignment of the spine, intraoperative evaluation of spinal alignment remains challenging. Plain radiographs are not fit for iterative use due to significant added OR (operating room) time and radiation exposure, combined with difficulties in interpreting the long-cassette image due to uneven exposures. A novel tracked C-arm system equipped with motion tracking and image processing software can take image inputs from any mobile C-arm for the purpose of highly accurate quantitative intraoperative alignment evaluations. The goal of this study was to evaluate the efficacy of the tracked C-arm during spinal deformity correction surgery. Material and Methods: The tracked C-arm system is a mobile stand that consists of an infrared camera for tracking the position of a standard mobile C-arm. This allows multiple C-arm–acquired images to be attached together forming an calibrated expansive view of the anatomy without the need for image overlaps. The system can then provide accurate alignment assessment on both anatomical planes. Accordingly, it obviates many of the above-described limitations of plain films and mobile fluoroscopy alone. The functionality of the system for evaluation of the coronal and sagittal alignment of the spine was tested in 5 multisegmental spinal fusion surgeries. The surgical procedures varied from a 2-level lumbar fusion to primary and revision extensive thoracolumbar instrumentations. The total time for setting up the system, image acquisition, and assessment were recorded along with the corresponding radiation exposure. These were compared with values available for conventional long plain films. The accuracy of the composite images was evaluated by overlaying full-length postoperative radiographs and comparing the coordinates the instrumented segments, assuming that fused segments stay rigid after surgery. Results: In total, there were 16 evaluations conducted during 5 procedures. The full-length radiographic evaluations based on the tracked C-arm were 5 to 6 times faster compared with equivalent conventional plain imaging (2.6 vs 15 minutes). Short lateral plane evaluations were at least 6 times faster than the equivalent short films (2.5 vs 15 minutes). Short coronal plane evaluations were on average 46× faster compared with conventional plain film-based evaluation. The calculated radiation dose exposure was 72% to 95% less compared with equivalent intraoperative plain films. The composite views were accurate for depicting the shape of the fused segment in both planes with 2-mm discrepancies in comparison to postoperative X-rays. Conclusion: A tracked C-arm system allows for intraoperative evaluation of spinal alignment at a fraction of the time and radiation exposure when compared with long plain films. This technology is a logical and potentially widely accessible solution for ensuring accurate execution of the surgical plan in spinal deformity correction.
P547: Sternal Cementoplasty in Multiple Myeloma: A Case Report and Literature Review
Sauri-Barraza José Carlos1, Callejas-Ponce Eduardo1, and Martínez-Berlanga Paulina1
1ABC Medical Center, Mexico City, Mexico
Introduction: Vertebral and sternal lesions/fractures are entities that may trigger severe chronic pain, seriously respiratory and mobility compromise and reduction on quality of life of patients. Traditionally, open surgery for fixation and stabilization of the lesion has been used for treatment of these pathologies. A novel and promising technique, cementoplasty, has emerged as an alternative treatment for fast and safe assistance in these patients. This article presents a case analysis of a patient treated with this procedure and a systematic literature review available on this subject. Materials and Methods: We reviewed a case involving a 62-year-old male patient with severe pain, 10/10 according to visual analogue scale of pain (VAS), especially on dorsal-lumbar spine and sternal region, with ventilatory involvement, important mobility limitation, and impact on quality of life. X-ray: lytic lesions in multiple bones. Computed tomography (CT): T5, T8, T10, and T11 fractures, wedge collapse. MRI (magnetic resonance imaging): No spinal or radicular involvement, multiple lesions in T1, T2, T5, T8, T9, T10, and L1, vertebral collapse with bone edema. Biopsy: plasma cells myeloma infiltration with kappa chains restriction. Sternal cementoplasty and vertebroplasty of affected bones were performed following manufacturer’s suggested techniques (Stabilit Vertebral Augmentation System; Merit Medical, South Jordan, UT). For each procedure, 1 mL of resin (polymethylacrylate) was used. VAS values for dorsal, lumbar, and sternal regions was assessed, and the Oswestry Disability Index (ODI) was determined. Several measurements were obtained before and after surgery with follow-up at 2 years (days 10 and 45, and months 3, 6, 12, and 24 post surgery). A systematic search in PubMed was performed (including MEDLINE and EMBASE databases). MeSH and EMTREE were used for searching keywords: “cement,” cementoplasty,” “kyphoplasty,” “sternal/sternum,” “vertebroplasty,” and their combinations. All results were included (since year 1946). No filters or language restrictions were applied. Results: Surgeries were performed without complications, with no bleeding and with surgical times of 25 minutes or less. A large decrease in pain (VAS = 2/10) was observed on very short term (24 hours after surgery). VAS values for sternal pain were maintained at 2/10 throughout the follow-up. Similarly, dorsal and lumbar pains were maintained between 2 and 3/10 in the same period of time. ODI percentage decreased until 20% at day 45 and remained with minimal fluctuations until month 24. Systematic review lead 52 related citations. All of them were case reports without long-term follow-up. Most of them were associated with cardiothoracic surgery closures procedures or other events. Ten percent of citations were related to malignancy, including 2% with multiple myeloma. Conclusion: Long-term outcome of cementoplasty procedure applied for treatment of medically intractable spinal and sternal pain was evaluated for the first time on this work. This technique has been showed an excellent choice for fast control of chronic pain. Furthermore, it is not time consuming, is simple, and is minimally invasive. Our results demonstrate the enormous potential of cementoplasty in selected patients but also encourage to carry out new studies in this regard.
P548: A New Spine Guide for Pedicle Screw Placement: A Comparison to Freehand Technique
Ahmed Aoude1
1University of Calgary, Calagary, Canada
Introduction: Pedicle screws have been used for posterior spinal fixation since the freehand technique was first reported in 1959. Multiple methods have since been developed to facilitate more accurate screw placement, such as navigation and robotics. Although these techniques have been reported as safer, they also increase radiation exposure and operative time. Pedicle screws remain technically demanding to place. Aberrant screws can lead to serious neurovascular complications, including radicular pain, sensory loss, damage to great vessels, and damage to the pleural cavity. We propose that a new minimally invasive surgery (MIS) Spine Guide can improve pedicle placement screw accuracy and compare it with freehand technique. Material and Methods: We conducted a cadaveric study to assess the accuracy of a new spine guide to improve pedicle screw accuracy. A total of 42 screws were placed in 4 cadavers, with 21 screws being placed with standard freehand fluoroscopy technique and 21 screws with the new spine guide with a single anteroposterior (AP) fluoroscopy image. A computed tomography (CT) scan prior to placement of screws was taken for all cadavers, and another scan was completed after screw placement to assess screw placement accuracy. Screw pedicle breach was then measured on CT scan and classified with a 2-mm increment (A: within pedicle, B: 0-2-mm breach, C: 2-4-mm breach, D: more than 6-mm breach). Results: The study showed that 21 screws placed with the guide 12 were A, 7 were B, 1 was C, and 1 was a D. In contrast, 12 were A, 3 were B, 4 were C, and 4 were D for the freehand technique. The average breach was statistically significantly smaller for the guide compared with freehand technique (P = .047). The average breach for all screws with the guide was 0.28 mm, while the average breach for the freehand technique was 2.76 mm. When defining an unsafe breach as anything more than 2 mm, then only 2 screws were unsafe with the guide compared with 6 with the freehand technique. Conclusion: In this study, we present data on a new pedicle screw guide that was shown to be safer than conventional freehand technique. This guide allows for decreased radiation exposure to the surgeon and the patient and allows for more precision in pedicle screw insertion and is intended for MIS techniques. Future studies will provide data on the tool being used in real human subjects.
P549: Initial Clinical Experience With a Novel Method for Herniated Disc Repair
Scott Blumenthal1
1Texas Back Institute, Plano, TX, USA
Introduction: Microdiscectomy for lumbar disc herniation is focused on resection of disc material impinging on a segmental nerve root. Despite significant symptomatic relief following this procedure, reherniation rates of 3% to 18% are a source of recurrent pain and repeat surgery. Aggressive disc material removal has been associated with a reduced reherniation rate but associated with an accelerated disc height loss (as high as 26%) leading to disc degeneration and long-term back pain. The preservation of disc material has been associated with a decrease in recurrent back and leg pain, and may, as a result, delay or eliminate the need for more invasive spinal procedures such as instrumented spinal fusion. The purpose of this study was to conduct pilot evaluation on the clinical applicability of a novel suture-based closure device for the repair of the defect following lumbar microdiscectomy. Material and Methods: Twenty patients undergoing limited microdiscectomy were offered suture-based closure of the annulus fibrosus. An intraoperative assessment of annular tissue quality was made following the index decompression. If the defect was deemed repairable, a suture-based closure was attempted using the AnchorKnot Tissue Approximation Kit. The suture was composed of nonabsorbable polyethylene and introduced with a single-use delivery device. Patient records were reviewed 2 weeks postoperatively for reherniation symptoms and other complications. Results: Defect closure was attempted in 11 of 20 patients. Successful closure was accomplished in 9 of the 11 attempted cases. Reasons for which closure was not possible/not attempted included insufficient competency of the tissue, or inaccessibility of the tissue margins. No acute complications, including reherniation, were observed in the 2 weeks following each procedure. Conclusion: Satisfactory closure of the annular defect was achieved in 9 of 11 attempted cases. An intraoperative focus on preserving the margins of the annular defect is an important element of the technique to enable subsequent repair. Further study is required to assess the broader applicability of annular closure in herniated disc repair and the potential impact on the rates of recurrence or revision surgery.
P550: Initial Canadian Evaluation of a Novel System for Lumbar Herniated Disc Repair
Albert Yee1, Cari Whyne1, David Yen2, and Ali Faqeeh2
1Sunnybrook Health Sciences Center, Toronto, Ontario, Canada
2Kingston General Hospital, Kingston, Ontario, Canada
Introduction: Lumbar microdiscectomy involves the resection of nerve compressive intervertebral disc material in order to alleviate nerve root pressure for patients suffering from intractable radicular leg pain with or without motor and/or sensory deficit. Despite significant symptomatic nerve pain relief following this procedure, recurrent disc herniation is reported in up to 18% of patients and is a significant source of recurrent pain and repeat surgery.1 Herniated disc repair of annulus fibrosus defects has been proposed as a means of reducing the recurrence rate. Our translational bench to clinic research group previously validated ex vivo and in vivo preclinical (animal) performance of a 2-0 nonabsorbable polyethylene suture-based implant designed specifically for this purpose.2 In this study, we report initial clinical feasibility assessment of the technology on patients from a Canadian perspective. Material and Methods: Procedures were completed at 2 Canadian surgical centers from January 29, 2016 (KGH [Kingston General Hospital]), and March 27, 2017 (Sunnybrook), until May 16, 2018. All posterior lumbar microdiscectomy patients were preoperatively screened using magnetic resonance imaging (MRI) to assess potential suitability (minimum disc height, accessible defect location) for annular fibrosus defect repair. Eligible patients were offered the opportunity to receive the suture repair or not based on clinical considerations including patient and MRI factors. Intraoperatively, repair was attempted using the AnchorKnot Tissue Repair Kit if the annulus fibrosis tissue defect appeared competent and accessible for functional repair. Repair was considered successful is the defect margins could be approximated, and the implant could be knotted in place. Routine postsurgical follow-up was completed at 6 weeks to assess for reherniation symptoms or other complications. Results: Twenty-eight patients were considered for herniated disc repair. Implant delivery was attempted in 18 patients and was successful in 15 (83%). Repair was not attempted for 10 patients based on intraoperative assessment of the defect. Reasons for not attempting or failing to complete a repair included; narrow disc height, annular detachment from the endplate (rim tear), inaccessible defect margins, and friable/incompetent tissue at the defect margin. There were no adverse events or reherniations reported. Successful repair was achieved in the majority (83%) of patients who had annular defects that appeared preoperatively “repairable.” Anatomic, tissue, and defect characteristics appear to be key considerations during intraoperative assessment of potential reparability. The delivery device and knotting accessories were compatible through mini-open surgical access. The average time to deploy the implant was approximately 5 minutes (range = 3-15 minutes). Conclusion: Our initial Canadian experience suggests that this herniated disc repair strategy, currently available worldwide, is feasible when applied to appropriate patients based on preoperative imaging as well as intraoperative disc tissue evaluation. We recognize that a comprehensive evaluation will require ongoing planned clinical follow-up to assess disc reherniation rates (from an imaging as well as clinically relevant patient perspective with regard to recurrent radicular leg symptoms). Herniated disc repair was practically achieved in 53% of the patients who would have been considered eligible from a patient and MRI imaging perspective preoperatively. Further study is planned to investigate the impact of this technology on reherniation and/or surgical revision rates.
P551: Augmented Reality–Assisted Pedicle Screw Placement in a Cadaveric Model
Camilo A. Molina1, Nicholas Theodore1, A. Karim Ahmed1, Erick Westbroek1, Yigal Mirovsky2, Ran Harel3, Emanuele Orru1, Majid Khan1, Timothy Witham1, and Daniel M. Sciubba1
1Johns Hopkins University, Baltimore, MD, USA
2Assaf Harofeh Medical Center, Zefirin, Israel
3Sheba Medical Center, Tel Aviv, Israel
Introduction: Augmented reality (AR) is a novel technology that has the potential to increase the technical feasibility, accuracy, and safety of conventional manual and robotic computer–navigated pedicle insertion methods. Visual data is directly projected to the operator’s retina and overlaid onto the surgical field, thereby removing the requirement to shift attention to a remote display. The objective of this study was to assess the comparative accuracy of AR-assisted pedicle screw insertion in comparison to conventional pedicle screw insertion methods. Material and Methods: Five cadaveric male torsos were instrumented bilaterally from T6 to L5 for a total of 120 inserted pedicle screws. Postprocedural computed tomography (CT) scans were obtained and screw accuracy graded using the Gertzbein (GS) and Heary grading schemes (HGS) by 2 independent neuroradiologists. Noninferiority statistical analysis was performed versus freehand (FH), manual computer–navigated (MN), and robot-assisted computer-navigated (RN) literature reported insertion accuracies. User experience analysis was conducted via a User Experience Questionnaire (UEQ) filled out by operators post procedure. Results: Overall screw placement accuracy was 96.7% and 94.6% when employing HGS and GS grading, respectively. Insertion accuracy was noninferior to MN pedicle insertion when compared with both GS and HGS scores. When compared with RN insertion, accuracy was found to be noninferior when employing the GS score, but superior when employing the HGS score. Last, accuracy results were found to be superior to FH insertion when employing both HGS and GS scores. Accuracy results were not found to be inferior in any comparison. User experience analysis yielded “excellent” usability classification. Conclusion: AR-assisted pedicle screw insertion is a technically feasible and accurate insertion method.
Pain
P552: The Relationship Between Pain and Patient Activation in Individuals Undergoing Spine Surgery: A Prospective Study
Isador Lieberman1 and Xiaobang Hu1
1Texas Back Institute, Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: Patient activation is defined as an individual’s propensity to engage in adaptive health and rehabilitation behaviors. It is a potentially important factor contributing to the variations in postsurgical outcome. However, little is known about the factors that affect activation in patients with spine disorders. The purpose of this study is to prospectively evaluate the relationship between pain and patient activation in a series of individuals undergoing spine surgery. Material and Methods: Adult patients who were scheduled to have spine surgery with 2 surgeons were consented and prospectively enrolled in the study. Preoperatively, the visual analogue scale (VAS) was used to assess the patients’ back pain and leg pain levels. The Patient Activation Measure (PAM) was used to assess the patients’ activation level (higher score = higher level = better activation). The patients were classified into 2 groups based on their PAM scores: low activation (levels 1-3) and high activation (level 4). The patients’ demographics and preoperative diagnosis were also recorded. Results: A total of 56 patients were enrolled in the study. The patients’ mean age was 61 years (range = 20-83) and 39 patients (69.6%) were female. The patients’ primary diagnoses were scoliosis, stenosis, and spondylolisthesis. The patients’ mean back pain was 6.7 points, and their mean leg pain was 4.6 points. Patients with low activation had significantly higher back pain scores (7.7 vs 6.1 points, P < .02). Meanwhile, there is no correlation between patient activation level and leg pain scores (4.1 vs 4.9 points, P > .05). Conclusion: There is a negative correlation between back pain and patient activation in individuals undergoing spine surgery. Further study is underway to examine if optimizing the activation level in these patients can improve their surgical outcome.
P553: Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures Via Unilateral Versus Bilateral Approach: A Meta-Analysis
Peng Yin1 and Yong Hai1
1Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Introduction: Percutaneous kyphoplasty (PKP) has been recognized as an efficient way to relieve pain for patients with osteoporotic vertebral compression fractures (OVCFs), and PKP for OVCFs could be divided into unilateral and bilateral approaches. Until now, there is still no consensus about the optimal approach. The objective of the research was to compare the efficacy of lateral and bilateral PKP approaches for OVCFs. Methods: A comprehensive literature search was performed from the PubMed, Cochrane Library, and EMBASE between January 2008 and May 2017. The clinical efficacy of the 2 approaches was evaluated by comparing perioperative outcomes (operation time, the volume of injected cement, X-ray exposure times, and mean radiation dose), clinical outcomes (kyphotic angle reduction, restoration rate, visual analogue scale [VAS], Oswestry Disability Index [ODI], and 36-item Short Form [SF-36]), and operation-related complications (cement leakage and adjacent vertebral fracture). Data was analyzed using Review Manger 5.3. Results: A total of 791 patients from 10 studies were included in our meta-analysis. The pooled results showed significant differences in operation time (weighted mean difference [WMD] = −19.67, 95% confidence interval [CI] = −25.20 to −14.14; P < .001); volume of injected cement (WMD = −2.03, 95% CI = −2.63 to −1.42; P < .001); mean radiation dose in patients (WMD = −1.06, 95% CI = −1.23 to −0.90; P < .001); and the rate of cement leakage (WMD = 0.58 95% CI = 0.38 to 0.90; P = .01) between these 2 approaches. However, the pooled results revealed no significant differences in X-ray exposure times, kyphotic angle reduction, restoration rate, VAS, ODI, SF-36, and adjacent vertebral fracture. Conclusion: Our study presented that patients with OVCFs could obtained similar satisfactory clinical results via both unilateral and bilateral PKP approaches. Considering less operation time, less cement volume, lower mean radiation dose of patients, a lower rate of cement leakage, and less surgery-related costs, we suggest that a unilateral PKP approach is advantageous.
P554: Reliability of the Fortin Finger Test
Andres Enrique Cobar Bustamante1, Mario Cahueque2, and Mercedes Taracena3
1Spine Surgery, Guatemala City, Guatemala
2Spine Surgery Hospital Centro Medico, Guatemala City, Guatemala
3Fisioactiva, Guatemala City, Guatemala
Introduction: Since Fortin JD described this test in 1997, this has been a useful tool in the clinical setting to enable orthopedic surgeons to determine the origin of lower back pain and help as a diagnostic tool. Since this was published, to our knowledge, no other studies have been published to determine its reliability. We analyzed 40 consecutive patients and injected them in the outpatient setting to evaluate pain relief. Material and Methods: We analyzed 40 consecutive patients with lower back pain and a positive Fortin finger test to determine the correlation between the presence of Fortin finger and sacroiliac pain. When patients had a positive Fortin finger test, we proceeded to inject betamethasone and lidocaine in thumbs with medial to posterior superior iliac spine, at the level of the second sacral spinous process. EVA was measured before and after the injection, a reduction corresponding to a minimum of 75% in EVA was considered positive for sacroiliac pain. Results: Of the 40 patients who participated, 26 were female, 14 were male, mean age of 41.5 (22-52), previous EVA mean score of 8, after injection 33 patients had improved to at least 75% (EVA 2), 5 patients had improved 50% to 75% (EVA 5), and 2 patients had no improvement for more than 1 week. Conclusion: Simple and reliable test are useful in the clinical setting. Fortin finger can be a reliable test to determine if pain is originated at the sacroiliac joint. These findings help reinforce the clinical diagnosis, but a complete physical examination should be always made.
P555: Predictors of Opioid Use Among Patients Undergoing Spine Surgeries
Andrew Broda1, Zachary Sanford1, Haley Taylor1, Amina Zaidi1, Justin Turcotte1, and Chad Patton1
1Anne Arendel Medical Center, Annapolis, MD, USA
Background: Postoperative pain management in spine surgery represents a subject of continuing study based on evolving evidence-based prescribing guidelines. Little is known about risk factors associated with inpatient opioid utilization and prescription pain control needs at discharge. We identify risk factors for inpatient opioid utilization and the relationship between inpatient opioid use and discharge prescription volume. Materials and Methods: A retrospective review of patients undergoing elective spine surgery between January 2014 and May 2018 at a single institution was performed. Patients were subdivided by procedure type into lumbar decompression (LD), lumbar decompression with fusion (LDF), and cervical decompression with/without fusion (CDF). Opioid utilization was normalized into daily morphine milligram equivalents (MME). Multiple regression analysis of age, body mass index (BMI), American Society of Anesthesiologists (ASA), and HCC scores as potential risk factors for opioid utilization while controlling for procedure type was performed. Results: A total of 2281 elective spine surgery patients were identified (1251/54.8% LD, 384/16.8% LDF, 648/28.4% CDF). A total of 54.1% were male with mean age, BMI, and ASA 57.9 years, 30.3 kg/m2, 0.82, respectively. Average HCC score, inpatient daily MME, and discharge MME were 2.4, 44.4, and 496.5. Significant differences were appreciated between procedure types by sex, ASA, and HCC scores (P < .001). Multiple regression models identified lower age (β = −.36, P < .001) and higher ASA (β = 10.1, P < .001) as predictive of increased inpatient daily MME (R 2 = .308). Lower age (β = −4.62, P < .001) and higher ASA (β = 72.1, P < .001) were also predictive of increased discharge MME (R 2 = .097). LDF patients utilized the greatest inpatient and discharge MME, followed by CDF then LD. Significant positive correlations were found between inpatient and discharge MME when inpatient MME is subdivided into quartiles (r = .99 LL, .98 LLF, .96 CLF). Conclusion: Younger patients with higher ASA scores correlate with greater inpatient MME, while younger patients with higher ASA score correlate with greater discharge MME. Prescription volume at time of discharge appears to reflect inpatient opioid consumption. Further study is needed to evaluate total postoperative utilization.
P556: Baseline Opioid Use Prior to Posterior Lumbar Fusion Is Associated With Adverse Preoperative and Postoperative Patient Outcomes
Jannat Khan1, Bryce Basques1, Michael Nolte1, Jessica Gosse1, Christian Vetter1, Karishma Kadakia1, Kevin Alter1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Opioids are prescribed for patients with lumbar spine pathology, and perioperative pain management for those undergoing posterior lumbar fusion is challenging. Also, preoperative opioid use may be associated with adverse clinical effects, including depressed physiological status and physical activity. Many advocate for weaning opioids before surgery, for which the benefit is unclear. These concerns have caused an increased interest in perioperative opioid usage in spine surgery and decreased likelihood of unwanted consequences like refractory pain, abuse, dependence, and overdose. This study aims to analyze the effect of preoperative opioid usage on posterior lumbar fusion patients on both clinical outcomes and symptomatology surrounding the surgery. Materials and Methods: A retrospective cohort study was conducted of patients undergoing primary elective open posterior lumbar spinal fusion at one academic institution between 2014 and 2018. Patients excluded from analysis: <18 years of age during surgery, underwent fusion to treat a lumbar fracture, tumor, or infection. Patients on chronic oral opioid medication at surgery time were identified/separated. Patient and operative characteristics were collected/compared between patients taking and not taking preoperative opioids using chi-square analysis and independent sample t tests for categorical/continuous data. Preoperative and final postoperative visual analogue scale (VAS) back pain, VAS leg pain, Oswestry Disability Index (ODI), along with rates of dural tear, postoperative complications, postdischarge destination, reoperation, achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected. Binary outcome variables were compared with multivariate logistic regression, and continuous outcome variables using multivariate linear regression. Multivariate analyses controlled for baseline patient and operative characteristics. Results: A total of 495 patients met inclusion criteria: 151 had preoperative opioid use and 344 did not. Patients with preoperative opioid use had a younger mean age (57.06 vs 61.51 years, P = .005), higher mean BMI (body mass index; 31.50 vs 30.97, P = .012), and higher percentage of current smokers (19.87% vs 8.72%, P < .001). With perioperative factors, patients who reported preoperative opioid use were more likely to have undergone prior lumbar spine surgery (33.46% vs 20.06%, P = .012), prior lumbar fusion (10.6% vs 4.07%, P = .005), and one or more interbody fusions (37.75% vs 22.09%, P < .001), with no differences in the operative time or postoperative stay length. Patients with preoperative opioid use reported worse preoperative VAS back scores (7.94 vs 6.30, P = .002), postoperative VAS back scores (4.86 vs 3.95, P = .013), and postoperative ODI scores (37.01 vs 27.34, P = .009) versus patients without preoperative opioid use. There were no differences in the rate of postoperative complications and the rate of reoperation between the 2 cohorts. Conclusions: Management of symptoms surrounding surgery time is challenging for patients undergoing posterior spinal fusion, especially for those on preoperative opioids. The present study suggests that preoperative opioid usage may be associated with adverse patient-reported outcome measures, both preoperatively and postoperatively. Specifically, patients with preoperative opioid use reported worse preoperative VAS back scores, postoperative VAS back scores, and postoperative ODI scores. However, there were no differences in rate of postoperative complications or reoperations. These findings highlight the importance of further research into perioperative management of opioids for lumbar spinal fusions.
P557: Patients With Isolated Back Pain at the Time of Posterior Lumbar Fusion Experience Similar Clinical Improvement to Patients With Leg Pain With or Without Back Pain
Jannat Khan1, Bryce Basques1, Young Soo Hong1, Jessica Gosse1, Oscar Chen1, Landan Banks1, Ahish Chitneni1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: A common indication for lumbar spine surgery is lower extremity symptoms refractory to conservative management; however, patients often have back pain without lower extremity pain. Literature lacks consensus regarding indications of surgical interventions for treatment of patients presenting with back pain only. The concern is patients with isolated back pain have less predictable clinical outcomes than those with leg pain. The purpose of our study was to evaluate clinical and radiographic outcomes after posterior lumbar spine fusion between patients with isolated back pain versus leg pain with or without back pain. Materials and Methods: A retrospective cohort study was conducted of patients who underwent primary elective open posterior lumbar spinal fusion at one academic institution between 2014 and 2018. Patients excluded from analysis: <18 years at surgery time, underwent fusion of an intervertebral level cranial to L1, or to treat lumbar fracture, tumor, or infection. Patients were separated into 2 groups: patients with only back pain, and patients with leg pain with or without back pain. Patient and operative characteristics were compared between the 2 groups using chi-square analysis and independent sample t tests for categorical and continuous data. Preoperative and final postoperative visual analogue scale (VAS) back pain, VAS leg pain, and Oswestry Disability Index (ODI) were collected. Preoperative, immediate postoperative, and final radiographs were assessed to measure lumbar lordosis (LL), pelvic tilt, pelvic incidence (PI), with PI-LL calculated. Postoperative complications measures, postdischarge destination, reoperation, and achievement of minimally clinically important difference (MCID) for VAS back, VAS leg, and ODI, and pseudoarthrosis were collected, with operative time and postoperative length of stay recorded. Binary outcome variables were compared with multivariate logistic regression, and continuous outcome variables using multivariate linear regression, with lower lumbar fusions as reference. Multivariate analyses controlled for baseline patient and operative characteristics, with threshold for statistical significance at P < .05. Results: A total of 665 patients were included; 55 patients with isolated back pain and 610 (23.70%) with leg pain with/without back pain. On bivariate analysis, patients with isolated back pain were younger (P = .001), had lower BMI (P = .004), longer pain duration (P = .046), greater rates of deformity (P < .001), and higher likelihood of 3 or more level fusion, but lower rates of prior lumbar spine surgery and lower likelihood of interbody use (P = .041). On multivariate linear regression, there was no significant difference between 2 groups for radiographic measurements, postoperative length of stay, or VAS back, VAS leg, and ODI, other than significantly higher VAS leg score for patients with leg pain plus/minus back pain. Additionally, no difference in dural tears, complications, and discharge to facility, reoperation, pseudoarthrosis, or achievement of MCID for VAS back, VAS leg, or ODI was found. Conclusions: Patients with isolated back pain were younger with longer duration of symptoms compared with other group. However, complications, clinical outcomes, radiographic parameters, and re-operations were comparable between the two. These findings indicate that lumbar fusions are considered a viable intervention for patients with isolated back pain that are surgery-indicated. This information can be used for perioperative discussions, surgical planning, and clinical decision-making.
P558: Persistent or Newly Developed Buttock and/or Leg Pain After Lumbar Degenerative Spine Surgery
Masahiko Akiyama1
1 Teishinkai Hospital, Sapporo, Japan
Introduction: Persistent or newly developed buttock and/or leg pain is not rare and known as failed back surgery syndrome. Failed back surgery syndrome, which includes multiple etiologies such as restenosis, foraminal stenosis, and peripheral entrapment, is real pain for both patients and spine surgeons. This retrospective study analyzes etiologies of persistent or newly developed buttock and/or leg pain after lumbar degenerative spine surgery. Materials and Methods: A total of 182 consecutive lumbar degenerative surgeries were included in this study. Results: Persistent or newly developed buttock and/or leg pain occurred in 39 cases. Etiologies of pain were foraminal or different level spinal stenosis in 13 cases, further peripheral dysfunction in 25 cases, and vascular claudication in 1 case. Further peripheral dysfuction included cluneal nerve entrapment in 2 cases, piriformis or gluteal muscle dysfunction in 16 cases, iliosacral joint dysfunction in 3 cases, tarsal tunnel syndrome in 3 cases, and common peroneal nerve entrapment in 1 case. Conclusions: Persistent or newly developed pain occurred about 20% after lumbar degenerative spine surgery and 2/3 of etiologies were further peripheral dysfunction. Spine surgeons should be aware of these peripheral dysfunctions such as piriformis, gluteal dysfunctions, and peripheral nerve entrapment to reduce “unknown” cause of failed back surgery syndrome.
P559: Using Plasma Cytokine Levels to Characterize Inflammation and Perioperative Pain in Adolescent Patients Undergoing Spinal Fusion Surgery: A Pilot Study
Jun Jie Liao1, Ljiljana Nikolajev1, Shajenth Premachandran2, Sheila Bote1, Alisson R. Teles1, Jean A. Ouellet1, and Catherine Ferland1
1Shriners Hospitals for Children–Canada, Montreal, Quebec, Canada
2McGill University, Montreal, Quebec, Canada
Introduction: Increased release of plasma inflammatory mediators in the postoperative period has been reported in patients undergoing different invasive surgeries. In adolescent idiopathic scoliosis patients, an elevation of plasma interleukin-6 (IL-6) has been observed following elective spinal fusion surgery. It was also known that adolescent idiopathic scoliosis (AIS) patients experience acute and chronic postsurgical pain after surgery. Nonetheless, the relationship between inflammatory response and perioperative pain remains unexplored. The objectives of the study were to evaluate if plasma IL-6 and C-reactive protein (CRP) levels can be used to characterize systemic inflammation following fusion surgery. It is hypothesized that higher plasma IL-6 is associated with greater perioperative inflammation and pain severity. Material and Methods: Twenty-one AIS patients scheduled for elective posterior spinal fusion were recruited in this longitudinal study. Patients self-reported their pain intensity using a Numerical Rating Scale (NRS) from 0 to 10 before surgery, on the day of surgery, postoperative day 1 (POD1), postoperative day 2 (POD2), and 6 weeks after surgery. Venous blood samples were collected at each time point. Plasma IL-6 levels were quantified using human cytokine magnetic 30-plex assay and plasma CRP levels with enzyme-linked immunosorbent assay. Linear mixed models were used to assess the relationship between pain ratings and cytokine levels during the perioperative period. Results: Mean age of patients was 15.74 ± 1.962 and majority were female (84.6%). Preoperative IL-6 and CRP levels showed great variations (IL-6 range = 0.32-10.04 pg/mL; CRP range = 0.03-13.22 ug/mL). A total of 47.6% of patients reported pain before surgery. Mean IL-6 levels at baseline were higher in patients reporting pain than those without pain (5.3910 vs 1.8444 pg/mL, P = .002). Baseline CRP levels are similar in the 2 groups. Plasma IL-6 concentrations peaked on POD1 at 129.21 ± 69.33 pg/mL and plasma CRP levels peaked on POD2 at 313.17 ± 614.45 ug/mL (mean ± SD). Both IL-6 and CRP levels returned to baseline level at 6-week follow-up. There was a significant effect of time on pain level (P < .0001), with highest pain levels on POD1 and POD2 and a significant reduction in pain at 6week follow-up. No effect of IL-6 cytokine levels on pain severity was observed (P = .524). There was no significant effect of gender, surgical duration, blood loss, or weight in IL-6 levels during follow-up (P > .05). A total of 28.6% of patients reported pain at 6 weeks. Variation of IL-6 during the perioperative period was not associated with pain 6 weeks after surgery (interaction group versus time P > .05). Conclusion: AIS patients experience acute inflammatory response after surgery, characterized by increased plasma CRP concentrations. IL-6 level at baseline can be used as a quantitative marker for preoperative pain. However, the concentrations of inflammatory mediators in the postoperative period were not associated with postoperative pain severity in the pilot study.
P560: Mortality Rate and Health Gain After Sacroplasty Following Sacral Insufficiency Fracture
Kathryn Ramshaw1, Yehya Ghonem1, and Palaniappan Lakshmanan1
1City Hospitals Sunderland, East Boldon,United Kingdom
Introduction: Sacral insufficiency fracture is a debilitating injury that can cause acute pain as a result of minimal trauma. The sacroplasty procedure is designed to relieve symptoms. However, cement augmentation in the sacrum can be challenging because of increased cement leakage and poor visualization of sacrum on fluoroscopic images. The objective of this study is to establish mortality rate and health gain after sacroplasty following sacral insufficiency fracture. Material and Methods: Between November 2013 and July 2018, a cohort of 20 patients met the inclusion criteria, with 4 deceased therefore 16 contacted, with 13 available for participation. This retrospective study was completed using questionnaire EQ-5D, with the questionnaire completed both pre- and post-sacroplasty. The cohort was also asked if knowing the results now, would they have gone ahead with the procedure. Results were analyzed with a health gain of ≥0 noted as a positive health gain, and results ≤0 noted as a negative health gain. Results between −0.2 and +0.2 were deemed to not show a vast impact in relation to health, economy, and patient care. Results: The results showed health gains relating to EQ-5D as follows: mobility health gain 1.4; pain/discomfort health gain 1.5; self-care health gain 1.2; anxiety/depression health gain 1.1; usual activities health gain 0.8. Although 20% of patients did report a worsening of their usual activities, no patients reported their mobility worsened after the procedure, with 80% reporting an immediate improvement in mobility. Ninety-two percent of patients said they would have gone ahead with the procedure knowing their outcome now. Mortality rate in sacroplasty patients is 20%, with 10% of deaths in the first year. Zero percent of those deaths were related to sacroplasty complications. Conclusion: Sacroplasty is demonstrated to have a positive health gain after sacral insufficiency fracture. The procedure has the biggest impact on mobility and pain. Sacroplasty is a safe procedure; evidenced by the fact that mortality rate is low, with no procedure-related deaths.
P561: Percutaneous Vertebroplasty in the Management of Compression Vertebral Body Fractures
Uladzislau Ulasavets1, Rafal Morga2, Ewelina Grzywna2, Jaroslaw Polak2, Borys Kwinta2, Artur Jurczyszyn3, Katarzyna Jasinska1, and Krzysztof Stachura2
1Jagiellonian University Medical College, Kraków, Poland
2Kraków, Poland
3Kraków, Poland
Introduction: This study was designed to investigate the role of vertebroplasty in the pain management of patients with multiple myeloma (MM) and patients with osteoporotic vertebral compression fractures. Material and Methods: Data on management and outcomes for patients with compression vertebral body fractures were collected retrospectively. Past medical history and operating protocols were investigated. The study group was divided into 2 subgroups according to the past history: MM group and osteoporotic fracture group. Age, gender, comorbidities, and neurological status were investigated. Primary endpoints were technically successful procedures, and pain relief was measured by the visual analogue pain scores (VAS). Results: A total of 109 patients with compression vertebral body fractures of thoracic and/or lumbar spine have been enrolled. MM fractures were presented more often comparing with osteoporotic fractures (72 vs 37). BMI (body mass index) did not differ significantly between the groups (26.77 ± 3.52 vs 25.39 ± 6.45). Mean preoperative VAS for MM group was 5.1 ± 3.13 and VAS 5.6 ± 2.61 for osteoporotic patients accordingly. Performed procedures were technically successful in both groups. Vertebroplasty has resulted in pain relief in both groups (P < .0001) with greater effect in MM patients (P = .0068. No major complication occurred. Patients who suffered from MM had statistically higher mRS (modified Rankin score) at discharge comparing to osteoporotic fracture group (1 vs 0, P = .02). Conclusion: The use of percutaneous vertebroplasty is effective as the pain management method in both analyzed groups of patients but especially in patients with vertebral involvement of MM.
P562: Spinal Cord Stimulation: First Experiences With 16 Contacts Leads Implantation
Maxime Raket1, Lynn Schroeder1, and Frank Hertel1
1Centre Hospitalier de Luxembourg, Luxembourg, Luxembourg
Introduction: Spinal cord stimulation (SCS) has become a standard procedure in the treatment of chronic pain, for example, failed back surgery syndrome (FBSS) or neuropathic pain, respectively. Whereas the “sweet spots” for FBSS treatment seems to be different from that for the treatment of pain in the lower and especially in the upper extremities, it remains difficult to cover the different areas in the spinal cord by the contacts of only 1 electrode. The combination of 8, 16, or even more contacts seems to be necessary. Furthermore, SCS implantations are being performed more and more under general anesthesia, making it even more necessary to have different options for postoperative programming. Material and Methods: We report our first experiences with implantation and programming of 2 electrodes with 16 contacts under general anesthesia for a patient with FBSS. Results: The implantation does not require any special surgical technique. The patients benefit from several programs alternating between conventional stimulation and burst. As a result, the patient reports a significant pain reduction. The programming possibilities offered by the steering of the current in each contacts independently seem to be useful to cover all painful areas. Conclusion: We report our experiences with the implantation under general anesthesia of two 16 contacts leads. We emphasize about surgical technical aspects, IPG (implantable pulse generator) programming and short-term follow-up. This case open the reflection regarding the “sweets spots” and the possibility to implant SCS under general anesthesia.
P563: Acute Postoperative Opioid Trajectories and Long-Term Outcomes in Pediatric Patients After Surgery
Mandy Li1, Don Daniel Ocay1, Alisson Teles1, Pablo Ingelmo1, Jean Ouellet1, Gabrielle Pagé2, and Catherine E. Ferland4
1 Faculty of Medicine, McGill University, Montreal, Quebec, Canada
2Université de Montréal, Montreal, Quebec, Canada
Introduction: The days following surgery is a critical period where the use of opioids predicts long-term outcomes in adults. It is currently unknown as to whether opioid consumption throughout the acute postoperative period is associated with long-term outcomes in pediatric patients. The aims of this study were to characterize opioid trajectories in the acute postoperative period, identify predictors of opioid trajectory membership, and determine associations between opioid trajectories and long-term patient outcomes. Material and Methods: Medication use, pain, and mental health status were assessed at baseline in adolescents with idiopathic scoliosis who were scheduled for spinal fusion surgery. Cumulative 6-hour opioid consumption was recorded for up to 5 days after spinal surgery. At 6 weeks and 6 months after surgery, medication use, pain, and physical function were evaluated. Growth mixture modeling was used to identify opioid trajectories. Results: One hundred and six patients were included in the study. Mean cumulative opioid consumption in the acute postoperative period was 13.23 ± 5.20 mg/kg. The model with the best fit contained 5 acute postoperative opioid trajectories and a quadratic term (Akaike information criterion [AIC] = 6703.26, Bayesian information criterion [BIC] = 6767.19). Opioid trajectories differed in the total amount of opioids consumed and the rate of opioid intake over the acute postoperative period. Intraoperative epimorphine dose predicted the opioid trajectory membership (P = .0498). Opioid trajectory groups were significantly associated with pain at 6 weeks (P = .0103) and 6 months (P = .0457) after surgery. Conclusion: Intraoperative epimorphine dose predicts the opioid consumption in the acute postoperative period. Opioid consumption during this period is associated with long-term pain. Understanding the acute postoperative period and its association with baseline predictors and long-term patient outcomes will allow for personalized perioperative care.
P564: Reasoning-Based Therapeutic Approach in Chronic Neck Pain: A Pragmatic Study
Sibi Daniel Joseph1
1MGM’s Institute of Physiotherapy, Aurangabad, Maharashtra, India
Introduction: Clinical reasoning–based models for assessment and a biopsychosocial approach for treatment is necessarily not a routine practice in India for chronic neck pain patients. Cultural differences in pain perception have also been well documented. Aims: To assess the feasibility and applicability of existing evidence based paradigms of clinical reasoning–based evaluation and management in patients with chronic neck pain. To develop reasoning-based treatment approach for patients with chronic neck pain relevant to India. Study Design: Observational cohort with a pragmatic component. Materials and Methods: Each patient with chronic neck pain visiting OPD (outpatient department) was evaluated in detail with the evaluation protocol prepared earlier, and the findings were documented. After initial assessment, the therapist came up with physiotherapy-based functional diagnosis to identify the tissue causing discomfort based on a clinical reasoning model. The patients were then categorized under the following groups based on their findings and diagnosis: neck pain with radicular findings, neck pain without radicular findings, and cervicogenic headache. After categorizing the tissues into the respective groups of dysfunction, the appropriate treatment techniques based on the latest evidence was applied to treat patients in their respective subgroups of chronic neck pain. An a priori algorithm was developed after doing a systematic review to standardize the management techniques based on the current evidence. Patients were followed upto a period of 3 months. Data Analysis: Kaplan-Meier survival curve and random effects model. Results: The survival curve found that in group 3, the event occurs faster compared with the other 2 groups. Day of observation, number of episodes, and chronicity of pain are the factors that were significantly affecting the visual analogue score (VAS) score. Day of observation, BMI (body mass index), and number of episodes were the factors that were significantly affecting the Neck Disability Index (NDI) scores. For VAS score to decrease by 3 cm, it will take approximately 75 days. On an average, it will take atleast 59 days to achieve the minimum detectable change for the NDI score, which is 10%. Conclusion: A focussed evaluation and management plan based on clinical reasoning shows improvement in chronic neck pain by a reduction of 3 in the VAS score and has lasting benefits, and the program is acceptable to patients. Hence, this is a feasible and applicable program for women in India. A new clinical algorithm showing the dosage of treatment recommendation was also developed based on the outcome measures used. A new clinical algorithm showing the dosage of treatment recommendation was developed based on outcome measures used.
P565: Evaluation of Functional Limitation in Patients With Lumbar Stenosis
Fernando Alvarado-Gomez1, Luis Carlos Morales Saenz1, Andres Rodriguez Munera1, Constanza Bedoya1, David Meneses-Quintero1, Camilo Velez Escallon1, Kenny Lopez-Gomez1, Yuli Fuentes-Barreiro1, Jorge Uribe1, Jose Dangond Millan1, and Gerardo Ardila1
1Hospital Universitario Fundacion Santa Fe de Bogota, Bogota, Colombia
Introduction: The objective of surgical management of lumbar canal stenosis is to improve the patient’s quality of life in terms of mobility and functionality. This process is chosen once the nonsurgical options have been exhausted (pharmacological therapy, physical therapy, and invasive therapy). In the evaluation of the patient with low back pain, it is important to measure its functional repercussion; imaging studies and laboratory tests do not give the patient’s specific situation regarding terms of pain and functionality, or the changes that occur after being taken to a surgical procedure. The assessment scales are other complementary tests that, although less used, provide information about the intensity of pain and its impact on daily life activities. Material and Methods: A retrospective descriptive study of a cross-sectional cohort of patients who underwent decompression and/or fixation of lumbar canal stenosis was performed by the Orthopedics and Traumatology Department. All the patients included in this study answered the Oswestry questionnaire in at least 2 different moments: presurgical assessment and control at 6 and/or 12 months. A sample of 79 patients was obtained, excluding those who did not have presurgical assessment or any of the postoperative controls. Results: When the descriptive analysis of the information was carried out, the following points were found: taking the total sample, 53 (67%) patients correspond to women and 26 (33%) patients correspond to men, with an average age of 68.8 years. There is a relationship between the gender and the body mass index, while there is no relationship between the number of levels operated and the body mass index. On the other hand, there is a directly proportional relationship between the number of intervention levels and the average age. The Q test (Tukey HSD [honestly significant difference]/Kramer) and post hoc ANOVA (analysis of variance) test showed a highly significant improvement in the control score at 6 months compared with the initial evaluation (P = 1.29E-13) and between the initial assessment with the 12 months later (P = 2, 65E-11). However, there is no significant difference between the 6-month control score compared with the 12 months assessment (P = .1802). Conclusion: We observed an improvement in the scores of the Oswestry questionnaires and therefore terms of functionality in patients with degenerative disease of the lumbar spine who underwent decompression and fixation surgery. The Oswestry scale of functionality gives us a concrete vision of the evolution of patients in terms of functionality, allowing us to assess how effective the surgical technique was and the impact it had on the quality of life of patients.
P566: Pain Sensitivity and Modulation in Patients With Spinal Stenosis Selected for Lumbar Fusion
Alisson R. Teles1, Jean A. Ouellet1, Michael H. Weber1, Carlo Santaguida1, Peter Jarzem1, Rudy Reindl1, Guillaume Léonard2, and Catherine E. Ferland1
1McGill University, Montreal, Quebec, Canada
2Université de Sherbrooke, Sherbrooke, Quebec, Canada
Introduction: Pain is a complex phenomenon influenced by facilitatory and inhibitory processes. Central sensitization and inefficient endogenous pain inhibition have been associated with several chronic painful conditions. Growing evidence has suggested that the measurement of pain processing and modulation may help clinicians predict treatment success. The goal of this study was to evaluate pain sensitivity and modulation in a selected sample of patients with focal lumbar spinal degenerative pathology. Material and Methods: Eighteen patients with single- or 2-level spinal stenosis and instability presenting with chronic low back pain and neurogenic claudication were included in the surgical group (SG). Exclusion criteria were previous spine surgery, systemic disease or other chronic pain conditions, diagnosis of anxiety disorder, or receiving work compensation. A sex and age-matched control group of healthy volunteers (CG, N = 18), was used for comparisons. Participants were evaluated with a standard quantitative sensory testing (QST) and validated questionnaires (NRS [Numerical Rating Scale] of pain, pain catastrophizing scale, state-trait anxiety inventory, and Oswestry Disability Index). A total of 7 QST parameters were evaluated, including pain pressure threshold at a non-painful control site (PPT forearm) and at the most painful site at the back (PPT back), heat pain threshold (HPT), heat tolerance threshold (HTT), cold pressor test (CPT), temporal summation of pain (TSP), and conditioned pain modulation (CPM). Statistical analyses were conducted with SPSS using Student’s t test and Fisher’s exact test for group comparisons and Pearson correlation test. Results: Mean age was 56.1 (14.5) years in the SG and 57.8 (12.9) years in the CG (P = .719), and the male:female ratio was 10:8 on both groups. The mean pain during the first heat task was 55.5 (25.1) in the SG versus 41.5 (16.2) in the CG (P = .055). After the conditioning stimulus, mean pain was 45.9 (24.5) in the SG and 27.7 (16.4) in the CG (P = .013). The mean pain reduction after the conditioning stimulus was 9.6 (21.0, P = .069) in the SG and 13.7 (13.7, P = .001) in the CG. An increase in pain ratings during the first heat task (TSP) was observed in 77% of SG. In addition, 38.9% of SG did not present any inhibition after the conditioning stimulus (16.7% CG, P = .137). There was a positive correlation between pain catastrophizing and pain ratings during the cold pressor task (r = .483, P = .042). Mental component of SF-12 (12-item Short Form Survey) correlated negatively with pain pressure threshold ratio (r = −.512, P = .039): the more sensitive was the back, the lower was the mental health. Conclusion: Patients with chronic low back pain and neurogenic claudication selected for lumbar decompression and fusion present higher pain sensitivity and less efficient conditioned pain modulation in comparison with healthy individuals. Follow-up results of the SG will evaluate the predictive value of individual’s pain processing and modulation on surgical outcomes of spine fusion.
P567: Why Do Some Patients Develop Chronic Pain After Surgery for Adolescent Idiopathic Scoliosis? A Longitudinal Study Exploring the Role of Neuroplastic Changes in Pain Processing
Alisson R. Teles1, Neil Saran1, Sheila Bote1, Jean A. Ouellet1, and Catherine E. Ferland1
1McGill University, Montreal, Quebec, Canada
Introduction: Chronic pain after surgery for adolescent idiopathic scoliosis (AIS) remains poorly understood. In this exploratory study, we investigated the role of neuroplastic changes in pain sensitivity and modulation on long-term self-reported pain outcomes. Material and Methods: A total of 45 adolescents with idiopathic scoliosis were included in this longitudinal study. Patients were evaluated in 5 time-points (1 week before surgery, 5 days, 6 weeks, 6 months, and 1 year after surgery) with quantitative sensory testing (QST) and validated questionnaires (NRS [Numerical Rating Scale] of pain, SRS30, pain catastrophizing scale [PCS]). A total of 6 QST parameters were assessed: pain pressure threshold at a non-painful control site (PPT forearm) and at the back (PPT back), heat pain threshold (HPT), cold pressor test (CPT), temporal summation of pain (TSP), and conditioned pain modulation (CPM). The SRS30 pain domain at 1year was used to identify high and low pain levels (cutoff = 3.5). Linear mixed-effects models were used to assess changes over time in QST variables between groups (low-level × high-level pain), with a random intercept used to control for the repeated measures for each individual with a time point and over time. Models were adjusted for sex. Initially, we looked for the presence of a significant interaction between time and group. In models with significant interaction, the groups were compared in each time point using the Tukey pairwise multiple comparisons. If no significant interaction was observed, the interaction term was removed and the main effect of time and group was tested in order to verify significant changes over time adjusting for group or a significant difference between groups after adjusting for time. Results: A significant interaction between time and group was identified for HPT (P = .030). In the low-pain group, a significant increase in HPT (less heat pain sensitivity) was observed at 1 year in comparison with the other time points (F = 10.92, P < .0001); no significant difference was observed in the high-pain group (F = 1.77, P = .145). After controlling for PCS, the interaction time of X group remained statistically significant. No significant interaction between time and group was observed in the remaining 5 QST parameters (P > .05: PPT forearm, PPT back, CPM, CPT, TSP). A significant main effect of time was observed in PPT forearm (P = .021), PPT back (P < .0001), CPT (P = .022), and CPM (P = .015), meaning that a significant change over time was detected in those parameters after adjusting for groups. Conclusion: Significant neuroplastic changes in pain sensitivity and modulation were observed in this longitudinal study. A significant increase in HPT from 6 months to 1 year was identified in the low pain level but not in the high pain level group, suggesting the potential contribution of neuroplastic changes in pain sensitivity on postsurgical pain outcomes.
P568: Mycroendoscopic Neurolysis Due Sacral Hiatus for Chronic Lumbar Back Pain
Alberto P. Contreras1, Fernando Calderon Carrillo1, Erik Hernandez Vasquez1, and Diana Chavez Lizarraga1
1 Centro del Cerebro y Columna Vertebral Hospital Mexico, Mexico City, Mexico
Introduction: Neurolysis access to the sacral hiatus through a flexible microendoscope for the treatment of chronic low back pain is presented. Lumbosacral degenerative disease has several spectrums of pain. One of the most common techniques for treatment is epidural injection, followed by blockage of dorsal branch of the ventral root, either with medication or with thermal damage. However, the treatment for axial variant pain and spinal claudication associate to degenerative disease, remains a challenge due to the recessive symptoms, which show within a few months after the procedure, leading the patients to the need of having a new intervention and increase drugs consumption, such as pain killers and opiates that directly affects their quality of life. Materials and Methods: From January to July 2018, we perform numerous procedures of flexible micr -endoscope of lumbar spine through sacral hiatus access, associate due degenerative disease of the spine at the Centro del Cerebro y de la Columna Vertebral at Hospital Ángeles de México. The patients were selected in the outpatient clinic, including X-rays studies of panoramic spine for sagittal balance measurement, dynamic studies, simple lumbar spine MRI (magnetic resonance imaging), bone densitometry in spine and hip. Inclusion criteria: integrate diagnosis of lumbar degenerative disease symptomatic, that did not show any improvement with conservative treatment and/or be in treatment of chronic pain, as well, with no improvement. We use the visual analogue scale (VAS) and the Oswestry Disability Index (ODI) for evaluations. Exclusion criteria: psychological score of STarT greater than 3 overall of 6, psychological and/or psychiatric disorder. Informed consent was signed both for the procedure and obtaining photographic and video material during surgery. Results: Demographic data were revealed of 30 patients, who were candidates to have the procedure: female gender predominates in 25 patients (83%) and 5 patients masculine (17%) and 95% of them are nonactive in workplace. The cranial access level were mostly at L2, most commonly L4. Procedure time was of 25 minutes. Symptoms evaluated were: lumbalgia, radiculopathy, and claudication with VAS and ODI. Patient’s position is prone with flexion of the lower extremities. The approach is performed under local anesthesia and radiological planning with 2D (2-dimensional) fluoroscope, placing at hiatus level in lateral projection, introducing a port work, then endoscope to the junction of L5-S1, to posterior navigation of higher levels and control right/left always ventral to the dural sac. Mechanical neurolosis is performed with microendoscope movement from right to left and vice versa, adding a mix of anesthetic plus steroid, followed by a hyaluronic acid gel. Patient leaves ambulatory room 3 hours after the procedure was performed, to be monitored from home. Evaluations are made every 3 hours, weekly, and monthly subsequently with VAS, ODI scale, and pain killers consuptions. Lumbar pain control and claudication to initial VAS 8 to 1 is proportional to 3 hours; it was maintained monthly for 6 months. The control of the radiculopatia achieved in 50% of the patients was 90% returning in 4 patients in whom we replanned the treatment. The ODI scale improve form 68% to 20% overall. Conclusions: This technique of access to the spine has allowed control of pain, improving quality of life, reducing the consumptions of pain killers, and opiates in selected patients that due to morbidity show a high-risk procedure, that was performed under local anesthesia, allowing quick recovery on daily basis activities, having 6 months control, we need more follow time to evaluate the real length of this result.
P569: Spino-Pelvic Parameters Influencing the Sacroiliac Joint Dysfunction
Dmitry Ptashnikov1, Ivan Volkov1, Olga Lapaeva1, and Sergey Masevnin1
1Russian Scientific Research Institute of Traumatology and Orthopedics named after R.R. Vreden, St. Petersburg, Russian Federation
Introduction: Structure of low back pain syndrome comprised 30% sacroiliac joint dysfunction. The etiology and pathogenesis continue to be studied and discussed. The objective of the study was to evaluate the relationship between spino-pelvic alignment and the frequency of development sacroiliac joint dysfunction among the patients with degenerative disc disease. Material and Methods: This prospective nonrandomized study evaluated 197 patients with low back pain syndrome. All patients had intensive pain syndrome—pain level 4 or more using Numerical Rating Scale (NRS)-11. Exclusion criteria were surgical treatment with a pelvic fixation in the anamnesis, obvious indications for surgical intervention cause of compression of nerve structures, pseudoarthrosis instability of spine, spinal deformity with disturbance of the sagittal or frontal balance. Sacroiliac joint dysfunction was determined after positive one-time test block under X-ray navigation, if the pain syndrome was reduced by 50% using NRS-11 scale within 15 minutes after the injection. Sacroiliac joint dysfunction was verified through test nerve block in the main group (79 patients). Another 118 patients with low back pain with another reason of pain were in the control group. We compared X-ray and clinical parameters in 2 groups. Results: Sacroiliac joint dysfunction was more often diagnosed in patients after surgical treatment (P = .05) with spinal fusion. The mean values of spino-pelvic parameters (pelvic incidence [PI], pelvic tilt [PT], sacral slope [SS], and lumbar lordosis [LL]) was not significant differences, but PI-LL, PT/PI, and SS/PI were revealed. The PI-LL and PT/PI values determined as significant in the main group were used for further analysis. Binary logistic regression showed that the greatest risk factor for the development of sacroiliac joint dysfunction was identified for the PT/PI. Conclusion: Patients with retroversion of the pelvis, which is expressed by PT/PI have higher risks of sacroiliac joint dysfunction.
Spine Biologics
P570: Postoperative rhBMP-2–Induced Neuroinflammation at the Lumbar Nerve Root Is Reduced With Systemic Diclofenac
Glen Liau1, Liu Jiani Sherry1, Lam Wing Moon Raymond1, and Wong Hee-Kit1
1National University Health System, Singapore, Singapore
Introduction: Recombinant human bone morphogenetic protein 2 (rhBMP-2) is used clinically to augment spinal fusion. This increases the rate of fusion, avoids donor site morbidity, and reduces the need of allograft. However, complications of postoperative new onset of lower limb radiculitis in up to 11.4% of patients have been reported. The known dose-dependent inflammatory effect of rhBMP-2 extends locally to the adjacent nerve roots to cause such a complication. We hypothesize that administration of systemic NSAIDs (nonsteroidal anti-inflammatory drugs) will reduce the local undesirable neuroinflammatory effects. Hence, this study aims to explore an in vivo rat model, the dose and effectiveness of systemic administration of anti-inflammatory agents in reducing neuroinflammation caused by rhBMP-2. Material and Methods: Eighteen rats were randomized into 3 groups as follows: Group 1 (HD), using high-dose diclofenac as postoperative treatment. Group 2 (LD): treated with low-dose diclofenac. Group 3 (control group) treated with saline injection. An absorbable collagen sponge (ACS) containing rhBMP-2 was surgically wrapped around the L5 nerve root. All rats were administered the respective treatment doses for a week before being sacrificed. We performed quantitative, qualitative, and behavioral analyses: volume of seroma, histology, reverse transcription polymerase chain reaction (RT-PCR; biomarkers: MMP12, MAPK6, GFAP, CD68, IL1-β), immunohistochemical staining (IHC) with DAB stain, and Hargreaves behavioral tests. Results were analyzed with SPSS version 23.0. Results: Seroma Formation: There was a dose-dependent relationship with the use of diclofenac; HD: 0.19 ± 0.22 mL (SD = 0.22), LD: 0.21 ± 0.24mL (0.24); Saline: 0.29 ± 0.34 mL (0.34). Histology and IHC: There was an observable decrease in density of inflammatory cells and disruption of nerve architecture (Figure 1) with increasing doses of diclofenac. RT-PCR: There were quantifiable decreasing trends across multiple markers with increased doses of diclofenac, with that of MMP-12 being statistically significant (P = .02). MMP12: 4.7/23.6/202.4 (HD/LD/Saline); MAPK6: 0.52/2.04/3.36; GFAP: 2.16/5.68/4.51. Upregulation of MMP-12 matched with the pattern of myelin loss in low-dose diclofenac and saline group. No appreciable trend was found in the other biomarkers. Hargreaves Test: There is a reduction in thermal withdrawal latency, with it being lowest in saline group (65%), followed by LD (72%) and HD group (92%). Diclofenac treatment inhibited the development of thermal hyperalgesia of rats in a dose-dependent manner, with a statistically significant difference between HD and Saline groups at day 5, when compared with preoperative baseline (P < .05). Our results suggest that systemic diclofenac is effective in reducing local neuroinflammation caused by rhBMP-2. Conclusion: Our study shows that systemic diclofenac reduces local neuroinflammation caused by rhBMP-2. This has clinical significance in the prevention and management of rhBMP2-induced radiculitis postoperatively.
P571: Novel Zoledronate-Loaded Carriers for Controlled and Local Delivery for the Treatment of Spinal Metastases
Elie Akoury1, Ahmed Alshammasi1, Pouyan Ahangar1, Bardia Barimani1, Michael H. Weber1, and Derek H. Rosenzweig1
1McGill University, Montreal, Quebec, Canada
Introduction: Approximately 80% of primary breast, lung, and prostate cancers metastasize to the spine. Current nonsurgical therapies of these bone metastases focus on chemotherapy and bone preservation, with zoledronate (Zol) being one of the most commonly used drugs. Zol is usually systemically delivered to patients, and it can cause multiple adverse effects. Interestingly, our group has investigated the potential of local delivery of Zol to the site of bone metastasis and has shown reduced tumor-induced osteolysis compared with systemically treated xenograft animals. Over the past decades, researchers have been adopting new methods for delivering anticancer drugs directly to tumor site. We have experience working with silica nanoparticles, which were proven to carry and release many types of drugs and molecules while remaining biologically inert. Alternatively, we and others have been also examining the feasibility of low-cost 3-dimensional (3D)-printed nanoporous scaffolds for drug delivery, which could potentially be applied directly at the tumor resection site as a bone substitute. Our aim is to develop controlled release carriers that locally deliver Zol in a patient-specific manner for the treatment of bone metastases. Materials and Methods: Testing drug release from carriers: fluorescent Zol was incubated with mesoporous silica nanoparticles. Aliquots of drug-containing supernatant were collected daily over a sustained period of time, and fluorescent drug was measured using a plate reader. Alternatively, we have also been testing LAY-FOMM nanoporous 3D printable material, for releasing Zol under the same conditions. Statistical analysis was preformed using 1-way or 2-way ANOVA (analysis of variance) and Tukey post hoc tests at a 95% confidence level. Results: Nanoparticles and 3D printed LAY-FOMM scaffolds take up and release Zol over time. In ongoing experiments, Zol-loaded nanoparticles and Zol-loaded LAY-FOMM scaffolds are being tested to assess cellular proliferation, migration, and 3D invasion on primary cells from patients with bone metastases. Future work will apply both Zol-release approaches to a xenograft bone metastasis animal model for further validation. Conclusions: Nanoparticles or 3D-printed constructs releasing drugs could constitute a promising therapeutic to locally combat metastatic spine tumors while potentially reducing the side effects associated with systemic delivery. Nanoparticles can be integrated into commercial bone cements to develop a bioactive bone graft following bone tumor resection to deliver localized drug-facilitating bone stability and healing while preventing tumor recurrence. Likewise, 3D-printed scaffolds can be made to perfectly fit defect and can be loaded with chemotherapeutics or other bioactive substances to block cancer recurrence and promote bone repair.
P572: A Comparative Study of Adjacent Segment Degeneration Following Discectomy and Instrumented Fusion in Lumbar Spine
Aditya Narula1
1Kempegowda Institute of Medical Sciences, Bengaluru, Karnataka, India
Introduction: Adjacent segment degeneration (ASD) following lumbar spine fusion and lumbar discectomy remains a widely known problem, but due to insufficient knowledge regarding the factors that contribute to its occurrence, it is difficult to diagnose considering the fact that it has variable presentation in terms of the symptoms it produces, the time frame for its occurance, and radiological changes. Another of the challenges is to distinguish it from the more common age-related degenerative process. Background: This is a retrospective study from 2012 to 2017 from Kempegowda Institute of Medical Sciences (KIMS), Bengaluru.To find out the incidence of ASD and prevalance of ASD among people undergoing discectomy and interbody fusion (IF) of lumbar spine in Kims Hospital, Bengaluru. The finding of our study can be used for better patient advice, patient selection, and taking adequate precautions with regard to surgical techniques and postoperative protocol. Methodology: In our study, we included all patients who underwent IF and those who underwent discectomy in lumbar region with a minimum 2-year period of follow-up. We have taken into consideration the associated comorbidities of the patient, any complications post surgery, occupational changes that have been made, and the adjacent segment degeneration has been graded by modified Pfirrmann’s grading on MRI (magnetic resonance imaging) with the clinical outcome correlated with VAS (visual analogue scale) and Oswestry scoring system. Results: In our study, ASD occurs both in single-level discectomy and post IF and is marginally more in post single-level discectomy without fusion. In both groups, cephalic segment is more affected as compared with the caudad segment. There is a significant relationship between radiological degeneration and the clinical ASD. It has been seen that there is a significant relation between degeneration and chronic smokers both radiologically and clinically.Since there is only marginally difference, we hold on to our hypothesis that the role of natural degeneration is more compared with the role of IF causing ASD.
P573: Allogeneic Stem Cells in Cervical and Lumbar Spinal Fusions: A Systematic Review
Patrick Hsieh1, Ki Chang1, Zorica Buser1, Andrea Skelly2, Hans-Joerg Meisel3, Jong-Beom Park4, Jim Youssef5, Darrel Brodke6, Jeffrey Wang1, and S. Tim Yoon7
1University of Southern California, Los Angeles, CA, USA
2Aggregate Analytics Inc, Fircrest, WA, USA
3Bergmannstrost Hospital, Halle, Germany
4Uijongbu St. Mary’s Hospital, The Catholic University of Korea, Uijongbu, Republic of Korea
5Spine Colorado, Durango, CO, USA
6University of Utah, Salt Lake City, UT, USA
7Emory Spine Center, Atlanta, GA, USA
Introduction: Spinal fusions are commonly performed for treatment of symptomatic degenerative spine disease, spinal deformities, spine trauma, and spine tumors. While iliac crest autograft (ICBG) is considered the gold standard for graft material in spine fusions, complications from harvesting ICBG and concerns about the quality and quantity of ICBG in elderly patients have limited its routine use in spine fusions today. Allogenic stems cell (ASC) has been considered a potential alternative to ICBG since it is thought to possess similar osteogenic and osteoinductive properties to achieve spine fusions. In this study, we systematically review the literature for the effectiveness and safety of allogeneic stem cells as graft extenders in spine fusion. Material and Methods: A systematic search of PubMed/MEDLINE, EMBASE, and ClinicalTrials.gov databases was conducted for literature published through April 13, 2018, comparing allogenic cell sources for intervertebral disc fusion in the lumbar or cervical spine to other methods of fusion and well-designed prospective case series of ≥20 patients if no comparative studies were identified. Studies were independently assessed for risk of bias and methodological quality. Primary outcome analyzed was fusion rate and complication rate. Unpaired t tests were used to calculate mean differences and corresponding confidence intervals. Results: For lumbar fusion, 5 studies met the inclusion criteria with 1 retrospective cohort comparing allogeneic multipotent adult progenitor cells versus rhBMP-2 and 4 cases series with the use of ASC in lumbar fusions. The retrospective cohort study of anterior lumbar interbody fusion with allogenic multipotent adult progenitor cells versus anterior lumbar interbody fusion rhBMP-2 found no difference in ODI (Owestry Disability Index) or in VAS (visual analogue scale) pain at 12 months and fusions rate were similar at 90% versus 92% but complication trended higher in the rhBMP-2 group. Across the case series of allogeneic cell products, there was a total of 158 patients included in the analysis and fusion occurred in ≥90% by 12 to 14 months. For the cervical fusions, 5 studies met the inclusion criteria with 1 retrospective cohort comparing Osteocel with allograft and 4 case series using various ASC products. In the retrospective cohort study, the overall fusion rates were lower in the ASC group compared with the allograft controls (88% vs 95%), but statistical significance was not achieved. Across the case series, criteria/definitions of fusion varied and fusion frequency varied across time frames and intervention products but fusion rate ranged from 89% to 94% at 12 months in 2 studies and was 87% at 2 years for another study. In addition, adverse effects and complication rates were poorly reported across the case series. Conclusion: Evidence for the efficacy and safety of allogenic cell sources for lumbar and cervical arthrodesis was very low, primarily due to the high risk of bias and lack of precision of included studies, most of which were case series. Given the significant cost of ASC allografts can have significant economic impact in health care expenditure, high-quality comparative studies are needed to evaluate efficacy and safety of ASC in cervical and lumbar spine fusions.
Surgical Complications
P574: Preoperative Nutritional Status and Postoperative Surgical Site Complications in Adult Spinal Deformity Surgeries
Isador Lieberman1 and Xiaobang Hu1
1Texas Health Presbyterian Hospital, Plano, TX, USA
Introduction: A malnourished state is associated with decreased immune response and can impair wound healing and prolong inflammation. The purpose of this study is to investigate the relationship between preoperative nutritional status and the outcome of adult spinal deformity (ASD) surgeries. Material and Methods: Data was retrospectively collected from all patients who underwent ASD surgeries by a single surgeon between 2010 and 2016. Patients with preoperative albumin level less than 3.5 g/dL were considered as malnourished. The patients’ demographics, surgeries performed, postoperative surgical site complications, and related readmissions were reviewed. The relationship between preoperative serum albumin level and postoperative surgical site complications was studied. Results: A total of 364 patients were included in this study, and 71.2% were female. The patients’ mean age was 60 years (range = 19-84 years) and their mean body mass index (BMI) was 27.6 kg/m2 (range = 15.4-51.7 kg/m2). The average operated levels were 7. Forty-six patients (12.6%) were found to have low preoperative albumin level. The patients’ age, gender, BMI, and levels operated were not different between the groups. The patients who were malnourished had significantly higher incidence of postoperative deep wound infections (15.2% vs 4.1%, P < .005). There is no statistical difference for the incidence of superficial wound infections (0% vs 1.3%, P = .45). For those patients who were readmitted because of wound infections, the malnourished patients had significantly longer length of hospital stay (15.1 vs 8.0 days, P < .05). Meanwhile, the incidence of postoperative wound seroma was not different between the groups (2.2% vs 0.9%, P = .46). Conclusion: A total of 12.6% of adult patients undergoing spinal deformity surgery were found to be malnourished. Poor preoperative nutritional status is associated with a 3-fold increase in postoperative deep or superficial wound infections. Further study is underway to investigate if optimizing preoperative nutritional status can improve clinical outcome.
P575: Investigation of Complication Rates and Peak Timing Post Spinal Fusion
Michael Akbar1, Christine Wantia1, Stefan Hemmer1, Haidara Almansour1, and Wojciech Pepke1
1Heidelberg University Hospital, Heidelberg, Germany
Introduction: Postoperative complications and their rates are well-documented in the literature. However, there are only a few studies that refer to their peak timing after index surgery. The aim of this study was to quantify the peak timing of complications post spinal fusion. Material and Methods: In this single-center, retrospective study, 1344 patients who underwent posterior or anterior/posterior spinal fusion from 2010 to 2015 were included. The minimum follow-up time was 2 years. Patient data was analyzed according to the necessity and the reason of the revision. In relation to the postoperative period, a stratification (<3 months, 3-6 months, 6-12 months, >12 months, and >24 months) was performed to quantify postoperative complications. Results: Of the total study population (n = 1344), 279 (20.8%) patients underwent revision surgery. Almost half of the complications occurred within the first 3 months after surgery (49% of all complications n = 139). Deep wound infection (n = 96, 91.4% of all wound infections) was revealed to be the most common complication in the first 3 months, followed by adjacent segment disease (ASD) (n = 22, 50% of all follow-up adjacent segment diseases) and implant loosening (n = 18, 52.9% of all implant loosening). It is of note that both ASD and implant dislocations had a relatively low and equal distribution over the time frame of 3 to 6, 6 to 12, and 12 to 24 months postoperatively. Adjacent segment disease: period 3 to 6 months, n = 6 (13.6% of all adjacent segment diseases); period 6 to 12 months, n = 7 (15.9% of all adjacent segment diseases); and period 12 to 24 months, n = 6 (13.6% of all adjacent segment diseases). Implant loosening: period 3 to 6 and 6 to 12 months, each n = 4 (11.8% of all implant loosenings), period 12 to 24 months, n = 6 (17.6% of all implant loosenings). In terms of construct failure (rod or screw breakage), most of rod or screw breakage occurred within the second postoperative year: period 13 to 24 months, n = 6 (37.5% of all material failures). Conclusion: Predominantly, most complications of any kind (deep wound infection, ASD, implant dislocation, and construct failure) occurred within the first 3 months after surgery. These findings are consistent with the recently published literature on complications of adult spinal deformity. The secondary peak time of complications relates to construct failure, which occurred more frequently in the second postoperative year. It is to be discussed whether the increased rate of construct failure in the period 12 to 24 months postoperatively is due to pseudoarthrosis, rod fatigue, or both.
P576: Screw-Related Complications After Instrumentation of the Osteoporotic Spine: A Systematic Literature Review With Meta-Analysis
Elke Rometsch1, Maarten Spruit2, Jack E. Zigler3, Venugopal K. Menon4, Jean Ouellet5, Christian Mazel6, Roger Hartl7, Kathrin Espinoza1, and Frank Kandziora8
1AO Foundation, AO Clinical Investigation and Documentation (AOCID), Dübendorf, Switzerland
2St Maartenskliniek Nijmegen, Nijmegen, Netherlands
3Texas Back Institute, Plano, TX, USA
4Sparsh Super Speciality Hospital, Bengaluru, Karnataka, India
5McGill University Health Center, Montreal, Quebec, Canada
6Institut Mutualiste Montsouris, Paris, France
7New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY, USA
8Center for Spine Surgery and Neurotraumatology, Frankfurt am Main, Germany
Introduction: Osteoporosis is common in elderly patients, who frequently suffer from spinal fractures or degenerative diseases, and often require surgical treatment with spinal instrumentation. Diminished bone quality impairs primary screw purchase, which may lead to loosening and its sequelae, in the worst case revision surgery. Information about the incidence of spinal instrumentation–related complications in osteoporotic patients is currently limited to individual reports. The aim of this work was to find information about the incidence of screw loosening and other local complications in osteoporotic spines by means of a systematic literature search and to quantify the results in a meta-analysis. Methods: Publications on spinal instrumentation of osteoporotic patients reporting screw-related complications were identified in 3 databases (PubMed, Web of Science, and Cochrane). Data on screw loosening and other local complications were collected. Pooled risks of experiencing such complications were estimated with random effects models. Risk of bias in the individual studies was assessed with an adapted McHarm Scale. Results: From 1831 initial matches, 32 were eligible and 19 reported screw loosening rates. Studies were heterogeneous concerning procedures performed and risk of bias. In a third of analyzed parameters, I2 amounted to ≥75%, which indicates high heterogeneity. Screw loosening incidences were variable with a pooled risk of 22.5% (95% confidence interval [CI] = 10.8% to 36.6%) in reports on nonaugmented screws and 2.2% (95% CI = 0.0% to 7.2%) in reports on augmented screws. In contrast to this finding, the incidences of other parameters were similar in reports on augmented and nonaugmented screws. For instance, the pooled risk of reoperations was 5.3% (95% CI = 1.5% to 10.6%) for nonaugmented screws and 3.9% (95% CI = 0.0% to 12.4%) for augmented screws. The pooled risk for further vertebral fractures was 8.4% (95% CI = 3.3% to 15.0%) for nonaugmented screws and 6.5% (95% CI = 0.4% to 17.1%) for augmented screws. Conclusions: The findings of this meta-analysis and comparison with the existing literature suggest that screw loosening incidences may be considerably higher in osteoporotic spines than in patients with normal BMD (bone mineral density). Screw augmentation may reduce loosening rates; however, this needs to be confirmed through further comparative prospective clinical studies. Our analysis was hampered by the low quality of complication reporting; therefore, we recommend that standardized reporting of pre-specified complications should be enforced by publishers.
P577: Multimodal Intraoperative Spinal Neuromonitoring for High-Risk Cervical and Cervicothoracic Spinal Disorders
Go Yoshida1, Hiroki Ushirozako1, and Yukihiro Matsuyama1
1Hamamatsu University, Hamamatsu, Japan
Introduction: Intraoperative spinal neuromonitoring (IONM) may have a role in identifying and preventing neural damage for cervical and cervicothoracic high-risk spinal surgery. We aim to analyze the incidence of neurological deterioration and details of IONM alert and to clarify how to prevent neural damage in case of IONM alert. Material and Methods: We analyzed 278 consecutive patients who underwent surgery for high-risk cervical and cervicothoracic spinal disorders using multimodal IONM, including transcranial motor-evoked potentials (Tc-MEPs), somatosensory-evoked potentials (SEPs), and continuous MEP from 2010 to 2016. High-risk cervical and cervicothoracic surgeries were consisted of multiple pathologies include 79 extramedullary spinal cord tumor (EMSCT), 63 intramedullary SCT (IMSCT), 62 ossification of posterior longitudinal ligament (OPLL), 21 cervical deformity, 19 severe cervical spondylotic myelopathy, 11 rheumatoid arthritis (RA), 7 cervical trauma, and 16 other pathologies. We set a 70% and 50% reduction of amplitude as an alarm point of Tc-MEPs and SEPs, respectively. Results: Totally, true positive (TP), false positive (FP), true negative (TN), false negative (FN), and rescue cases of IONM were 18, 26,210, 2, and 22, respectively. Neurological deficit rate of EMSCT, IMSCT, OPLL, deformity, CSM, and RA were 1.3%, 12.7%, 11.3%, 4.8%, and 5.3%, respectively. Main IONM alert and intervention were tumor resection and resting with steroid injection in SCT, posterior decompression and dekyphosis in OPLL, and correction maneuver and release in deformity. However, individual interventions were diverse in each case. Conclusion: This study indicates totally 14.4% possible neural damage of high-risk cervical and cervicothoracic spine surgery and 55% rescue cases by multimodality IONM. Although neurological deficit rates of OPLL and IMSCT were relatively high, appropriate intervention immediately after IONM alert may rescue neural damage even in high-risk cervical and cervicothoracic spinal disorders.
P578: Complications After Spinal Surgery in the First 3 Years of Independent Spine Practice in a Government Trauma Hospital in Nepal: Lessons Learned
Gaurav Dhakal1, Ganesh Gurung1, and Santosh Poudel1
1National Trauma Center, Kathmandu, Nepal
Introduction: Complications following spinal surgery are detrimental to both the patient and the hospital. In a resource-constrained government hospital, managing complications pose a larger challenge. The aim of this study was to determine the postoperative inpatient major complications following first 3 years of independent spine practice in a recently set up spine unit at a government trauma hospital in Nepal. Material and Methods: A retrospective review of spine surgeries performed by a fellowship-trained spine surgeon in a government trauma hospital at Kathmandu, Nepal, from July 2015 to July 2018 was done. Patient demographics, comorbidities, surgical indications, level, instrumentation utilized, neurology, and postsurgery in-hospital complications were extracted from record files and statistically analyzed. Results: A total of 269 spine surgeries were performed, out of which 231 were instrumented surgeries. Mean age was 39.3 years and 64.7% (174) were male patients. Only 16% (43) patients were from Kathmandu. A total of 64.3% (173) patients were operated for spine injuries, 15.2% (41) for stenosis and disc pathology, 8.6% (23) for listhesis, 6.7% (18) for infectious pathology, and 5.2% (14) for tumors. In all, 19.7% (53) had cervical spine surgery, 80.3% (216) dorsal and lumbar spine surgery. Major comorbidities were smoking, diabetes, and hypertension. Postoperative complications prior to discharge were implant revision in 0.74% (2) patients, deep wound infection in 0.74% (2) patients, hematoma necessitating evacuation in 1.1% (3), dural tear in 1.1% (3), deep vein thrombosis in 1.1% (3), urinary tract infection in 1.5% (4), pulmonary complication in 1.9% (6), and anaphylaxis in one patient. No mortality occurred during hospital stay. Conclusion: In a resource and geographically constrained region, where long-term follow-up of patients is a problem, the inpatient post-surgical complications remain the major source of data to develop complication prevention strategies and reduce patient morbidity.
P579: Indirect Decompression Failure After Lateral Lumbar Interbody Fusion—Reported Failures and Predictive Factors: Systematic Review
Sertac Kirnaz1, Rodrigo Navarro-Ramirez1, Jiaao Gu1, Christoph Wipplinger1, Ibrahim Hussain1, Joshua Adjei1, Eliana Kim1, Franziska Schmidt1, and Roger Härtl1
1Weill Cornell Medicine, New York, NY, USA
Introduction: Lateral lumbar interbody fusion (LLIF) achieves indirect neural decompression by restoring disc and foraminal height. In patients with lumbar stenosis undergoing lateral surgery, it is not always clear when indirect decompression is sufficient in order to achieve symptom resolution. Indirect decompression failure (IDF), defined as “postoperative persistent symptoms of nerve compression with or without a second direct decompression surgery to reach adequate symptom resolution,” is not widely reported. This information, however, is critical to better understand the indications, the potential, and the limitations of indirect decompression. The purpose of this study was to systematically review the current literature on IDF after LLIF. Material and Methods: A literature search was performed on PubMed. We included randomized controlled trials (RCTs) and prospective, retrospective, case-control studies, and case reports. Information on sample size, demographics, procedure, number and location of involved levels, follow-up time, and complications were extracted. Results: After applying the exclusion criteria, we included 9 of the 268 screened articles that reported failure. A total of 632 patients were screened in these articles and detailed information was provided. Most of the LLIF surgeries involved “one level” (46.8%). The most commonly treated level was L4-5 (46.7%), followed by L3-4 (31.4%). Average follow-up time was 21 months. Overall reported incidence of IDF was 9%. Conclusion: Failures of decompression via LLIF are inconsistently reported and the incidence is approximately 9%. IDF failure in LLIF may be underreported or misinterpreted as a complication. We propose to include the term “IDF” as described in this article to differentiate them from complications for future studies. A better understanding of why IDF occurs will allow surgeons to better plan surgical intervention and will avoid revision surgery.
P580: Low Incidence of Dysphagia and Early Recovery After Anterior Cervical Discectomy and Fusion Using Stand-Alone 3-Dimensional-Printed Porous Titanium Cage in Single- or 2-Level Cervical Disc Disease
Kyeong-Sik Ryu1, Jin-Sung Kim1, Myung-Soo Song1, Ho-Jung Chung1, and Jung-Woo Hur1
1Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul,Republic of Korea
Introduction: Anterior plating system yielded higher fusion rate and improved alignment after anterior cervical discectomy and fusion (ACDF) surgery but is associated with higher rates of postoperative dysphagia. With the advancement of technology, zero-profile fixation and 3-dimensional (3D)-printed stand-alone cages have been suggested to decrease the incidence of postoperative dysphagia. The purpose of this study is to evaluate the safety and efficacy of stand-alone 3D-printed porous titanium cage (3D-PTC) compared with that of anterior cervical plate and cage in patients undergoing 1- or 2-level ACDF. Material and Methods: Eighty-one patients with single- or 2-level cervical disc disease (CDD) underwent ACDF surgery using an anterior plate and cage or 3D-PTC implant between December 2016 and December 2017. All patients complete at least 12-month postoperative follow-up survey. The clinical outcomes were evaluated using the visual analogue scale (VAS) scores for neck and arm pain, Neck Disability Index (NDI) scores, and recovery of postoperative dysphagia. The radiologic results were evaluated with serial plain film and 3D-CT (computed tomography) to assess fusion status and device-related complications. Results: Forty-two patients received an anterior plate and cage and 38 received the 3D-PTC implant. There were no statistical differences in patient demographics and intraoperative details between the 2 groups. The VAS and NDI scores significantly improved compared with preoperative values in both groups. Fusion rates were found to be similar between the 2 groups. Evaluation of postoperative radiographs revealed significantly more swelling of the prevertebral space (21.7 ± 0.8 mm) after implantation of an anterior plate compared with a stand-alone 3D-PTC implant (14.5 ± 0.9 mm, P < .001). This difference remained significant until 3-month follow-up (P = .035). The incidence of dysphagia in the 3D-PTC group was lower (P = .027) compared with that in the plate with cage group, and the symptom duration was much shorter (P < .01). Both groups had no adverse events associated with the implant except 3 cases of cage subsidence without neurologic deterioration observed in 3D-PTC group. Conclusions: ACDF surgery using stand-alone 3D-PTC seems safe and efficacious and lead to similar clinical and radiographic outcomes compared with anterior plating. The rate of postoperative dysphagia and its recovery was much superior with 3D-PTC compared with anterior plate and cage.
P581: Limitations of National Surgical Quality Improvement Program in Evaluation of Risk for Patients Undergoing Emergent Surgery for Spine Metastases
Hanbing Zhou1 and John Street2
1Orthopedic Associates of Hartford, Hartford Hospital, Hartford, CT, USA
2Vancouver General Hospital, Vancouver, British Columbia, Canada
Objectives: Life expectancy and treatment options for metastatic spine disease continue to evolve. Prospective identification of complications is essential for risk stratification and treatment planning. National Surgical Quality Improvement Program (NSQIP) is currently popular though its accuracy, validity, and applicability to metastatic spine patients is unknown. To examine acute care complications of surgery for spine metastases comparing Spine AdVerse Events Severity system (SAVES) and NSQIP. Assess NSQIP online tool predictive ability for adverse events in metastatic disease of the spine. Methods: All patients at our institution undergoing emergent surgery for spine metastases from 2012 to 2016 were identified. Adverse events were examined from both databases. Complication prevalence and relative risk was compared between NSQIP and SAVES. NSQIP prediction tool was tested using primary and secondary tumor characteristics, hospital-stay characteristics, surgical invasiveness, patient demographics, and patient comorbidities. Comparative analysis of 2 prospectively collected databases. Evaluation of the American College of Surgeons (ACS)/NSQIP online adverse events predictor tool. Results: A total of 188 patients had complete data in both databases. Overall complication rates were 28% in NSQIP and 74.9% in SAVES. AEs more reliably identified using SAVES included wound complications (5.6 more; P < .05), delirium (2.8 more; P < .001), neuropathic pain (3.2 more; P < .001), urinary tract infection (1.4; P < .05), pressure sore (2.9; P < .001), and intraoperative AEs (2.3; P < .05). Six AEs more frequently identified by SAVES affected length of stay (P < .05). Risk factors such as tumor characteristics and severity of deficit more reliably correlated to adverse events collected through SAVES. Reoperation, in-hospital mortality, and 30-day readmission rates were identical for both databases. Current ACS NSQIP online tool had low predictive ability (c-index <0.6) for major complications. Conclusions: SAVES was superior to NSQIP in identifying important medical and surgical complications in patients undergoing emergent surgery for metastatic disease of the spine. Current ACS NSQIP online tool has low predictive ability for major complications.
P582: Surgical Management of Myelomeningocele-Related Spinal Deformities
Olga M. Sergeenko1, Sergey O. Ryabykh1, and Dmitry M. Savin1
1Ilizarov Center, Kurgan, Russian Federation
Introduction: We present a retrospective cohort study. The aims of our study were to evaluate optimal timing and type of surgical treatment of myelomeningocele-related spinal deformities and to provide long-term follow-up of surgical treatment. Material and Methods: We reviewed and presented clinical pictures, treatment strategies, and results of 30 patients with myelomeningocele-related spinal deformities, treated at the Ilizarov Center (Kurgan, Russia) from 2010 to 2018. Results: Average age was 7.0 years. Average preoperative neurological status according to a modified Japanese Orthopaedic Association (mJOA) Scale was 7.6 points (JOA Scale, Benzel’s modification). Average functional status was 48.9 points according to a Functional Independent Measure (FIM) . Eleven patients had lordoscoliosis (lordosis 71.8°, scoliosis 62.9° average Cobb angles), 15 patients had kyphoscoliosis (kyphosis 72.5°, scoliosis 34.4° average Cobb angles), and 4 patients had pathologic kyphosis only (89.8° average Cobb angles). Average duration of surgery was 215.8 minutes. Average total blood loss was 188.5 mL. Average angle of kyphosis correction was 61°, scoliosis correction 25°, and lordosis correction 25° (Cobb angles). Average duration of hospitalization was 15.9 days. Average follow-up was 24.8 months. Total number of complications was 21. Reoperations were needed in 10 cases. Neurological status, according to the mJOA scale improved 0.6 points in average. Functional status, according to the FIM, increased 6.6 points in average. Conclusion: Early surgical correction of myelomeningocele-related spinal deformities improves body balance and quality of life. A dual growing rod technique is safe and effective in cases of moderate neuromuscular spinal deformities in early age. Kyphectomy is a challenging procedure with high complication rates, especially skin problems, but in cases of heavy rigid kyphosis it has no alternatives.
P583: Machine Learning Can Identify Sepsis Following Orthopedic Surgery Using Electronic Medical Records
Varun Arvind1, Brian Cho1, Deepak Kaji1, Ivan Ye1, Ray Tang1, Andrew Warburton1, Aly Valliani1, Daniel Ranti1, Zoe Cheung1, Jun Kim1, and Samuel Cho1
1Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Quality improvement studies have provided surgeons with systematic insight on how to make changes to their practice to improve patient outcomes and avoid complications. However, currently, most automated methods to identify patient complications for quality improvement studies rely on prelabeled administrative codes sampling data from fixed electronic medical databases. Medical notes contain a rich supply of medical data, yet the format of unstructured text has precluded these data from use in large retrospective analyses. Therefore, the utilization of free-text from electronic medical records using natural-language processing in combination with machine learning can provide an additional tool for patient complication surveillance and identification. The purpose of this study was to develop a machine-learning algorithm that can identify postsurgical sepsis based on unstructured patient notes. Material and Methods: This was a retrospective analysis of medical notes from the Medical Information Mart for Intensive Care (MIMIC III), a large, single-center database comprised of intensive care unit admissions data from 2001 to 2012. A total of 947 patients from the orthopedic service were identified. Patients who experienced sepsis were identified using the International Classification of Diseases-Ninth Revision (ICD-9) code (99592). A total of 15 004 notes were analyzed in total from the 947 patients. Of the 15 004 notes, 3547 notes were from patients positive for sepsis and 11 457 notes were negative for sepsis defined by ICD-9 code. Area under the receiver operating characteristic (ROC) curve, accuracy, sensitivity, and specificity of the model were evaluated to assess performance of the model. Natural language processing was used to analyze unstructured narrative discharge notes and train a support vector machine (SVM) algorithm to train a classifier to automatically identify patients with sepsis based solely on unstructured discharge notes. The data was randomized with 70% used for training and 30% used for testing. Results: The SVM algorithm identified sepsis notes with a sensitivity and specificity of 79% and 85%, respectively. The overall accuracy was 83.3% with area under the ROC curve of 0.82. Conclusion: Combining natural language processing with machine learning is a valid approach for automatic identification of sepsis using unstructured text from discharge notes. This method provides a robust survey of surgical encounters and may be used for real-time surveillance of postoperative complication risk and for automated identification of patient complications such as sepsis for quality improvement studies.
P584: Iatrogenic Injuries of Vertebral Arteries During Operations on the Cervical Spine
Aleksey V. Evsyukov1 and Vladimir S. Klimov1
1Federal Center of Neurosurgery, Novosibirsk, Russian Federation
Introduction: Vertebral artery injury (VAI) is a rare but serious complication of cervical spine surgery, with the potential to cause catastrophic bleeding, permanent neurologic impairment, and even death. Iatrogenic VAI occurs from 0.1% to 8.2%. Material and Methods: The retrospective analysis of 513 patients operated on the cervical spine. Of these, 313 with degenerative diseases, 128 injuries, 57 patients with tumours, anomalies, and 15 patients with systemic diseases between March 2013 and September 2018. A total of 323 of them were males (63%) and 190 women (37%). Age was 42.3/37 years (25-44) and ranged from 3 to 75 years. Localization: craniocervical junction 87 (17%), subaxial level 426 (83%). Patients were evaluated on the basis of condition-specific functional status using the American Spinal Injury Association (ASIA) scale (2003), visual analogue scale (VAS), and Owestry Disability Index (ODI). X-ray examination, computed tomography (CT), and magnetic resonance imaging (MRI) of the cervical spine were performed before treatment and after surgery and after 12 months. If there was damage to the vertebral artery, CT angiography and Doppler ultrasound of brachiocephalic artery (BCA) were performed. Follow-up was 48 months. Results: A total of 358 patients underwent operation anterior approach, intraoperative injury of the vertebral artery was observed in 2 patients (0.5%). In all, 155 patients underwent rear access operation. During performing posterior approach, intraoperative injury of the vertebral artery was observed in 7 (4.5%) patients. Overall, 170 patients were implanted 426 screws malposition of the screw with a clinical manifestation of VAI was noted in 2 cases (0.4%). According to classification of Cothren et al, damage to the vertebral artery met grade II and grade IV. The surgery time—225.3/145 (180; 260) varied from 65 to 320 minutes. Blood loss in anterior approach—160/50 (100; 200) varied from 50 to 500 mL, and in posterior approach—360/100 (200; 500) it varied from 100 to 2000 mL. In case of damage to the vertebral artery, blood loss amounted to an average of 2100 ± 500 mL. The average length of hospital stay was 16.2/14 (10.8; 20), and varied from 7 to 31 days. Compared with preoperative baseline ASIA, VAS, and ODI for these patients, there were no observed changes after surgery. Conclusion: Iatrogenic damage to the vertebral artery are rare surgical complication and occur in 0.5% to 4.5% cases. Clinically significant injuries requiring audit intervention are 0.4%.
P585: Delayed Extubation Following Posterior Thoracolumbar Fusion at a Tertiary Academic Institution: Risk Factors and Complications
Samuel White1, Ivan Ye1, Zoe Cheung1, Rachel Bronheim1, Oscar Carrillo1, Jun Kim1, Jonathan Gal1, John Caridi1, and Samuel Cho1
1Mount Sinai Health System, New York, NY, USA
Introduction: Multilevel posterior thoracolumbar fusion (PTLF) often involves prolonged operative time as well as anesthesia time, which have been correlated with a wide array of complications. The physiological stress of surgery in the prone position has been associated with large fluid shifts that cause airway edema, making subsequent extubation more difficult and potentially even dangerous. However, prolonged intubation itself is associated with complications, including infection, sepsis, dysphagia, glottis stenosis, and mortality. The objective of this study was to identify risk factors and complications associated with delayed extubation following PTLF at a single tertiary care institution. Material and Methods: A retrospective cohort study of PTLF cases performed between January 2010 and November 2016 at a single institution was performed. Emergent cases were excluded. Patients were divided into 2 groups based on intubation status on leaving the operating room—delayed extubation versus nondelayed extubation. Univariate analyses were performed to compare baseline characteristics and postoperative complications between the 2 groups. Multivariate regression analysis was then performed to determine patient- and surgery-related characteristics that were independent predictors of delayed extubation. A second multivariate regression analysis was then performed to identify postoperative complications that were independently associated with delayed extubation. Results: A total of 466 patients were included in this study, of which 76.6% were extubated in the operating room and 23.4% were extubated after leaving the operating room. The delayed extubation group had a significantly higher proportion of patients with an ASA (American Society of Anesthesiologists) classification ≥3. The delayed extubation group also had a greater proportion of patients who underwent a long fusion and 3-column osteotomy with longer operative time. Compared with the non-delayed extubation group, the delayed extubation group had higher EBL (estimated blood loss), higher volume of crystalloid administration and colloid administration, higher volume of blood and fresh frozen plasma transfusion, and higher volume of Cell Saver transfusion. Anesthesia attending handoff occurred more often in the delayed extubation group. Independent risk factors for delayed extubation were long fusion (odds ratio [OR] = 2.32; 95% confidence interval [CI] = 1.17-4.58; P = .02), extended operative time (OR = 3.89; 95% CI = 1.38-10.95; P = .01), high volume of crystalloid administration (OR = 5.95; 95% CI = 2.34-15.11; P < .01), high volume of blood transfusion (OR = 3.41; 95% CI = 1.67-6.98; P < .01), high volume of fresh frozen plasma transfusion (OR = 5.59; 95% CI = 1.79-17.35; P < .01), and anesthesia attending handoff (OR = 3.50; 95% = 1.75-6.97; P < .01). Delayed extubation was a predictor of higher overall cost of care (OR = 3.68, 95% CI = 1.48-9.13; P < .01). Conclusion: Independent risk factors for delayed extubation following PTLF were long fusion, extended operative time, high volume of crystalloid administration, high volume of blood transfusion, high volume of fresh frozen plasma transfusion, and anesthesia attending handoff. Delayed extubation was associated with a higher overall cost of care. Therefore, while attempts should be made to extubate in the operating room if deemed safe in order to reduce health care costs, delayed extubation was not found to be associated with any 30-day postoperative complications.
P586: The Effect of Perioperative Adverse Events on Long-Term Patient-Reported Outcomes After Lumbar Spine Surgery
Oliver Ayling1, Tamir Ailon1, Nicolas Dea1, and Charles Fisher1
1Vancouver General Hospital, Vancouver, British Columbia, Canada
Introduction: Perioperative adverse events (AEs) lead to patient disappointment, resource utilization, and increased health care costs. There is a paucity of data on how AEs affect long-term patient-reported outcomes (PROs). The purpose of this study is to examine perioperative AEs and their long-term impact on PROs after lumbar spine surgery. Material and Methods: A total of 3556 consecutive patients undergoing elective spine surgery for degenerative lumbar spine disorders enrolled in the Canadian Spine Outcomes and Research Network (CSORN) prospective database were analyzed. Major and minor AEs were defined using the validated Spine AdVerse Events Severity system (SAVES), defined as grades 3 to 6 and 1 to 2, respectively. Perioperative AEs were analyzed for lumbar disc disease, degenerative spondylolisthesis, spinal stenosis, and lumbar deformity. Outcomes at 3 and 12 months postoperatively on the Owestry Disability Index (ODI), visual analogue scale (VAS) leg and back pain, Short Form-12 Health Survey (SF-12), EQ5D were assessed using univariate and multivariable analyses. Results: AEs occurred in 767 (21.6%) patients, 85 (2.4%) suffered major AEs, and 682 (19.2%) experienced minor AEs. All PROs were equivalent at baseline and all postoperative PROs were significantly better than baseline on ANOVA (analysis of variance; P < .001). Patients with major AEs had significantly worse postoperative ODI scores and did not reach minimum clinically important differences at 1 year (baseline: no AE: 47.5 ± 15.5, major: 48.2 ± 14.8, vs 1 year: no AE 25.5 ± 19.5, major: 37.3 ± 19.3; P < .001). On VAS leg and back, EQ5D, and SF-12 PCS (physical component summary), the 1 year PROs were significantly different between the major AE group and the no AE group (P < .01) but these differences were small and unlikely clinically relevant (VAS leg: baseline: no AE: 7.3 ± 1.9, major: 7.0 ± 2.5, vs 1 year: no AE: 3.2 ± 2.9, major: 3.9 ± 3.1), VAS back (baseline: no AE: 6.9 ± 2.2, major: 7.5 ± 1.9, vs 1 year: no AE: 3.3 ± 2.6, major: 4.3 ± 2.6), EQ5D (baseline: no AE: 0.5 ± 0.2, major: 0.49 ± 0.2, vs 1 year: no AE: 0.75 ± 0.2, major: 0.66 ± 0.2), and SF-12 PCS (baseline: no AE: 32.6 ± 8.2, major: 30.4 ± 7.9, vs 1 year: no AE: 43.6 ± 9.6, major: 37.7 ± 8.5). SF-12 MCS (mental component summary) scores were not significantly different between the major and no AE cohorts at 1 year (baseline: no AE 48.1 ± 8.5, major: 48.2 ± 9.5, vs 1 year: no AE: 51.8 ± 7.43, major: 50.5 ± 9.0). At 1 year post-operatively patients who faced a major AE had significantly lower rates of satisfaction (no AE: 83.5%, major: 71.6%, minor: 82.8%, P < .01). Conclusion: Major AEs during hospital admission after elective lumbar spine surgery lead to significantly worse long-term functional outcomes and lower rates of patient satisfaction. This information highlights the need to implement strategies aimed at reducing in-hospital adverse events.
P587: National Adverse Event Profile After Lumbar Spine Surgery and Comparison of Complication Rates Between Hospitals: A Canadian Spine Outcomes and Research Network Registry Study
Oliver Ayling1, Tamir Ailon1, Nicolas Dea1, and Charles Fisher1
1Vancouver General Hospital, Vancouver, British Columbia, Canada
Introduction: Most of the previous work investigating the rates of adverse events (AEs) in spine surgery have been retrospective, with data collection from administrative databases, and often from single centers. To date, there have been no reports utilizing a rigorous and prospective analysis to capture AEs in spine surgery on a national level or compare the rates of AEs between each center. Material and Methods: The incidence and severity of AEs after spinal surgery was captured using the Spine AdVerse Events Severity system (SAVES), version 2, in 14 spine centers from the Canadian Spine Outcomes and Research Network (CSORN) prospective registry. Data on consecutive patients undergoing elective spine surgery for degenerative conditions were collected prospectively and included demographic variables as well as medical and surgical AEs during hospital admission. Minor and major AEs were defined by SAVES grades 1 to 2 and 3 to 6, respectively. Results: A total of 3556 patients were enrolled in this cohort. As defined by SAVES, there were 85 (2.4%) patients with major AEs and 682 (19.2%) with minor AEs. There were no mortalities. There were 25 patients with major intraoperative AEs and 262 with minor intraoperative AEs. Post-operatively there were 61 patients with major AEs with a total of 80 major AEs and 84 minor AEs. Of the 487 patients with minor AEs post-operatively there were 698 total AEs. The rate of AEs varied by each hospital site. Of the 11 sites with more than 10 patients enrolled in the registry (3 sites had 10 or fewer patients enrolled), the average enrollment was 321 patients (range = 47-1237) per site. The rate of major AEs was consistent between sites (mean: 2.9% ± 2.4%, range = 0% to 9.1%). However, the rate of minor AEs varied widely between sites from 7.9% to 2.5% with a mean of 18.8% ± 9.7% (site A: 25.5%, B: 13.8%, C: 21.3%, D: 11.5%, E: 7.9%, F: 9.1%, G: 18.7%, H: 14.5%, I: 20%, J: 21.7%, and K: 42.5%). Conclusion: On a national level, major AEs after lumbar spine surgery occur and are reported at similar rates between different hospital sites. In contrast, the rate of minor AEs varies widely between sites, which is likely due to the manner in which AEs are collected. This work highlights the need to rigorously collect accurate AE rates in order to establish the true complexity of elective lumbar spine surgery.
P588: Machine Learning can Identify Subpopulations of Psychogenic Disorders That Pose Greater Risk for Postoperative Complication Following Lumbar Fusion
Andrew Warburton1, Varun Arvind1, Brian Cho1, Jun S. Kim1, and Samuel K. Cho1
1 Icahn School of Medicine at Mount Sinai, New York, NY, USA
Introduction: Many postoperative complications have been characterized and correlated in postoperative spinal fusion patients. Mental health has emerged as an important contributing factor to clinical outcomes following spinal fusion; however, little work has been performed to identify populations of patients with psychiatric illness with increased or decreased risk. Machine learning has proven to be a powerful tool to gain insight into layered comorbidities and possible complications. Furthermore, machine-learning techniques can cluster patients within populations to find subgroups that are vulnerable to future complications post-operatively. The purpose of this study was to develop a machine-learning algorithm that can identify unique patient clusters within psychogenic disorders of postoperative lumbar spinal fusion patients and any complications that were statistically different between the 2 groups. Materials and Methods: This was a retrospective analysis of the National Readmissions Dataset (NRD), a part of the Healthcare Cost and Utilization project that provides national readmission rates for insured and uninsured patients. The compiled NRD data for the psychogenic disorders comorbidity was coded under the following International Classification of Diseases, Ninth Revision (ICD-9) codes: 3060, 3061, 3062, 3063, 3064, 30650, 30652, 30653, 30659, 3066, 3067, 3068, and 3069. ICD-9 codes for cardiac complications were 410 and 9971. ICD-9 codes for pulmonary complications were 9973, 99731, 99732, 51851, 51852, and 51853. ICD-9 codes for thromboembolism complications were 41511, 41513, 41519, 45111, 45119, 4512, 45181, 45340, 45341, and 45342). K-means clustering, partitioning around medoids (PAM) clustering, and hierarchical clustering were used and compared against each other to support results. Statistical analysis was performed using an independent 2-group t test. Significance was defined as P < .05 to allow for a 95% confidence interval. Results: A total of 126 913 patients were indented from 2012-2014 NRD datasets as having undergone lumbar spinal fusion (ICD-9: 8107). A total of 3847 of the patients (3.03%) coded as psychogenic. Within the psychogenic patient population, 2 subgroups emerged from clustering (n1 = 3822, n2 = 25). The first group had an average age of 58.66 years. The first group is 67.45% female and the second group is 72% female with an average age of 55.24 years. Three complications were analyzed: cardiac, pulmonary, and thromboembolism complications. Thromboembolism and pulmonary complications within the psychogenic patients were statistically significant between the 2 clusters (P thromb = .00 466, P pulmonary = .04548) whereas cardiac complications were not found to be significantly different (P cardiac = .16 819). Conclusions: Implementing machine-learning algorithms to cluster subgroups of psychogenic postoperative patients is a powerful method for visualizing and predicting future complications. This clustering method provides a valuable tool for surgeons to identify at risk subpopulations within psychogenic patients that may require further management or consultation to improve outcomes within this at-risk cohort.
P589: Albumin Level and Preoperative White Cell Count Are Significant Independent Predictors of Mortality in Surgery for Metastatic Spine Disease
Yaroslav Gelfand1, Rafael De La Garza-Ramos1, Michael Longo1, Jonathan Nakhla2, Murray Echt1, and Merritt Kinon1
1Montefiore Medical Center, New York, NY, USA
2Rhode Island Hospital of Brown University, Providence, RI, USA
Introduction: It is well-documented that patients with severe hypoalbuminemia (albumin <2.5 g/dL) have significantly higher rate of surgical mortality than patients with normal albumin (>3.5 g/dL) or mild hypoalbuminemia (2.5-3.5 g/dL). Patient selection for operative intervention in oncologic spine surgery is crucial to maximize the benefit of the surgical intervention. In this study, we attempted to stratify risk of surgical outcomes for metastatic oncologic spine surgery based on preoperative albumin levels as well as examine other predictors of morbidity and mortality. Material and Methods: Patients who underwent surgery for metastatic spine disease were identified in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2006 to 2016. Three groups were established as follows: patients with normal albumin (>3.5 g/dL), mild hypoalbuminemia (2.6-3.4 g/dL), and severe hypoalbuminemia (≤2.5 g/dL). A multivariate analysis was used to assess the association between various levels of hypoalbuminemia and mortality within 30 days of surgical intervention. Results: A total of 904 patients who underwent surgery for metastatic spinal disease and had preoperative albumin levels available were identified; 73.1% had normal albumin (>3.5 g/dL), 22.1% had mild hypoalbuminemia, and 4.8% had severe hypoalbuminemia. Patients with severe hypoalbuminemia were significantly more likely to be male, have chronic lung disease, have congestive heart failure, be dependent on others for activities of daily living, and undergo emergency surgery. The crude 30-day mortality rate was 7.6% for patients with normal albumin, 16.0% for patients with mild hypoalbuminemia, and 44.2% for patients with severe hypoalbuminemia. After controlling for history of chronic lung disease, dependent functional status, and emergency procedures, patients with mild hypoalbuminemia (odds ratio [OR] = 1.91; 95% confidence interval [CI] = 1.14-3.19; P = .014) and severe hypoalbuminemia (OR = 7.20; 95% CI = 3.42-15.1; P < .001) were significantly more likely to experience mortality within 30 days compared with patients with preoperative albumin above 3.5 g/dL. In addition, patients with a preoperative white blood cell (WBC) count >12 × 109 cells/L were about twice as likely to have 30-day mortality (OR = 2.17; 95% CI = 1.34-3.5; P = .002). Conclusion: In this study, albumin level and WBC count were found to be independent predictors of 30-day mortality in patients operated for metastatic spinal disease. Patients with mild hypoalbuminemia had almost twice the mortality risk compared with controls and patients with severe hypoalbuminemia had a 7-fold increased risk. These findings need to be validated by future studies, but may prove useful for preoperative risk stratification and surgical decision-making.
P590: Spine Surgery in Octogenarians: Quality Improvement and Review of 282 Patients
Pal Randhawa1 and Peter Witt2
1University of C, Edmond, USA
2University of Colorado Dencer, Aurora, CO, USA
Introduction: Given the aging of the population in developed countries, spine surgeons have recently been more likely to encounter elderly patients in need of treatment. This review investigated whether surgery for elderly patients aged 80 years or older would likely be reasonable. We retrospectively reviewed 282 patients over the age of 80 for a variety of factors and compared this to a separate population of patients aged 79 years and younger, which served as a control group. Materials and methods: We gathered a total of 6988 surgical case records, of these 282 patients more than 80 years of age were separated into an “octogenarian” cohort for retrospective analysis. Presurgery factors and postsurgery complications were all coded as yes/no values and tested using either chi-square or Fisher’s exact tests depending on the cell sizes. Operative time was compared both non-parametrically using Wilcoxon rank sum and categorically using a 4-level variable. Length of stay (LOS) was similarly compared using Wilcoxon and a binary flag indicating a “long” LOS ≥5 days. Surgery types were also compared across groups using a chi-square test. We performed all comparisons on both the overall cohort as well as strata defined by surgery type (5 groups) and operative time (4 groups listed above) to further explore the octogenarian effect within strata. Logistic regression models were run predicting overall complications, 30-day mortality and long (≥5 days) LOS using inpatient class, history of cardiac arrhythmias, obesity, and osteoporosis as independent variables. We used PROC LOGISTIC in SAS 9.4 using forward selection with a threshold for inclusion of 0.05. Results: Preoperative factors differed strongly between the octogenarian and control groups. CHF (congestive heart failure; 1.4% to 5%), cardiac arrhythmias (5.3% to 15.6%), and osteoporosis (6.6% to 18.1%) were all more common among octogenarians while obesity (10.4% to 4.6%) was more common among the controls. In the logistic regression analysis, the preoperative presence of cardiac arrhythmias and osteoporosis were highly significant in predicting overall complications, 30-day mortality, and long LOS. Obesity was significant in predicting overall complications and 30-day mortality, and inpatient class was significant in predicting overall complications. Conclusions: Being an octogenarian in itself was not significant in predicting overall complications, 30-day mortality, and long LOS. The gathered preoperative factors of congestive heart failure, cardiac arrhythmias, osteoporosis, and obesity are associated with higher adverse outcomes in patients undergoing spine surgery while age itself was not. Objectives:
Examine the rate of complication and adverse effects in our octogenarian population.
Add to sparse literature regarding outcomes of octogenarians undergoing spine surgery.
Provide data to clinicians regarding outcome to help weigh risk and benefits of surgery in this population.
Keywords
octogenarians, spine surgery, surgical complications
P591: The Cost Effectiveness of an Intensive Care Unit Outreach Program on Adverse Events After Spine Surgery
Tom Inglis1, Daniel Banaszek2, Lise Belanger1, Tamir Ailon1, Nicolas Dea1, Marcel Dvorak1, Charles Fisher1, Brian Kwon1, Raphaele Charest-Morin1, Scott Paquette1, and John Street1
1University of British Columbia, Vancouver, British Columbia, Canada
2Vancouver General Hospital, Vancouver, British Columbia, Canada
Introduction: The Spinal Surgery AdVerse Events System (SAVES) was developed in 2008 with the intention of assessing the frequency and impact of postoperative adverse events (AEs) following spinal surgery. Over the study period, this system identified a number of “minor” AEs (grades 1 and 2) occurring frequently; electrolyte imbalance, medication-related issues, postoperative ileus, and nausea. In daily practice, these may often be dismissed as trivial. However, growing evidence shows the accumulation of minor AEs may have a larger than anticipated consequence. In 2012, an intensive care unit (ICU) outreach program was developed where high-dependency postoperative spine patients were reviewed daily by an intensive care physician. The purpose of this study was to examine the efficacy and cost-effectiveness of the introduction an ICU outreach program on AEs in postoperative high-dependency spine patients. Material and Methods: Study Design: Prospective cohort study. Subjects: All surgical patients admitted to a quaternary spine center for the outlined study periods. Outcome Measures: Data were prospectively collected during the 4-year period before (2008-2012) and after (2012-2016) the introduction of the ICU outreach program. The frequency of postoperative AEs was recorded during each period, as identified by the SAVES framework. Previous research has determined the cost of AE’s, which was applied to the data set. Results: Over the study period, the mean number of patients admitted per year was 984 (912-1090). The introduction of the ICU outreach team lead to a dramatic decrease in the number of AEs reported during the posoperative period. The percentage of patients with electrolyte imbalance decreased by 35% from 46% to 30%. Medication-related events decreased by 70% from 40% to 12%, ileus/constipation 46% from 26% to 14%, nausea by 64% from 22% to 8%, cardiac complications by 55% from 18% to 8%, pulmonary by 65% from 17% to 6%, and delirium/psychiatric by 62.5% from 12% to 4.5% (P < .05). Previous work has established the mean cost of a grade 1 AE is $6370 and grade 2 AE is $21 500. Before the introduction of the ICU outreach program, the top 2 AEs were electrolyte imbalance and medication related. Introduction of the program prevented 285 cases of medication-related AE with total cost savings of $2 895 884 and 157 cases of electrolyte imbalance for total cost savings of $1,5 . Conclusion: The introduction of an ICU outreach program to review postoperative high-dependency spine patients reduces the incidence of minor AEs, which in turn can lead to substantial health care cost savings.
P592: Minor Psoas Hematoma After Oblique Lumbar Interbody Fusion
Tomohiro Murakami1, Takahisa Kaneko2, Hitoshi Hayase1, Hiroshi Nakagawa3, and Koji Saito3
1Hokkaido Ohno Memorial Hospital, Sapporo, Japan
2Kushiro Kojinkai Memorial Hospital, Kushiro, Japan
Introduction: Oblique lumbar interbody fusion (OLIF) is a minimally invasive spinal fusion procedure using a retro-peritoneal approach without splitting the psoas major muscle. Less blood loss but higher complication rate after OLIF than after posterior (P)/transforaminal (T)LIF have been reported. A small psoas hematoma without symptoms was found incidentally on the postoperative computed tomography (CT). The purpose of this study was to analyze the incidence and features of psoas hematoma after OLIF. Material and Methods: There were 55 patients treated with OLIF between January 2017 and July 2018. Of these patients with postoperative small hematoma in the psoas major muscle were examined retrospectively. The psoas hematomas were diagnosed by lumbar CT within 1 week after operation. The operated level was 2 cases at T12-L1, and 4 at L1-2, 8 at L2-3, 13 at L3-4, and 15 at L4-5. There were 11 cases of single fusion segments, 7 of 2 segments, 2 of 3 segments, and 3 of 4 segments. Results: Twenty-three patients with psoas hematoma aged from 58 to 87 years (mean = 73 years) consisted of 7 men and 16 women. All hematomas were small, less than 2 cm. There were 16 hematomas in the left psoas muscle, 5 in the right, and 2 in both. Eight of 23 patients had antiplatetet or anticoagulant drugs. The left psoas hematomas tended to be caudally in the operated disc or vertebral level, and the right psoas hematomas were in the operated disc level. These hematomas had no symptom and were observed conservatively. Conclusion: The incidence of the minor psoas hematoma was 41.8%. These small hematomas need no treatment; however, careful observations are needed after beginning intake of antiplatelet or anticoagulant drugs. To prevent the psoas hematoma, gentle techniques are needed when dissection and retraction of psoas muscle or expansion of the disc space and discectomy.
P593: Incidence and Risk Factors of Symptomatic Epidural Hematoma Following Posterior Cervical Spine Surgery
Tian Xia1
1Peking University Third Hospital, Beijing, China
Objectives: To explore the risk factors of symptomatic epidural hematoma following posterior spine surgery, and to provide basis and interventions for clinical prevention of symptomatic epidural hematomas. Methods: Retrospective review was made on the clinical data of 19 patients with symptomatic epidural hematoma, and pick patients without hematoma randomly through the same period as control group, collect gender, age, body mass index, ossification of the posterior ligament, trauma, hypertension, diabetes, vascular atherosclerotic diseases, antiplatelet or anticoagulate treatment, platelet count, prothrombin time, activated partial thromboplastin time, international normalized ratio, segments, instrumental fixation, laminectomy, intraspinal hemostasis material, duration of surgery, estimated blood loss, and postoperative nonsteroidal anti-inflammatory drug, a total of 20 factors that might affect the occurrence of symptomatic epidural hematoma. T test and chi-square test were used to univariable test. Multifactor logistic regression analysis was used to investigate the correlation with symptomatic epidural hematoma; furthermore, its causes were explored. Results: Among 3859 patients, 19 cases suffered symptomatic epidural hematoma. The median time from the end of index surgery to symptomatic was 120 minutes (range = 30 minutes to 15 days). Two cases first presented with numbness, other 17 cases presented paralysis, finally, all cases suffered paralysis before hematoma evacuation. Seven cases were radiologically diagnosed by MR (magnetic resonance), the other 12 cases were diagnosed through symptom. All 19 patients received emergent hematoma evacuation. Frankel grade were B in 4 cases, C in 13 cases, and D in 2 cases. All patients recovered at least one grade after evacuation. Multifactor logistic regression revealed segments and OPLL are the risk factors for postoperative symptomatic epidural hematoma (P < .05). Conclusions: Segments and OPLL are the risk factors for postoperative symptomatic epidural hematoma. For patients with these risk factors, neurological functions should be under strict surveillance, and drains must be prevented from being obstructed.
P594: Perioperative Outcomes Among Different Fusion Approaches for Single-Level Lumbar Spondylosis
Raj Gala1, Elbert Mets2, Taylor Ottesen2, Jory Kahan2, Arya Varthi2, and Jonathan Grauer2
1Emory University, Atlanta, GA, USA
2Yale University, New Haven, CT, USA
Introduction: Low back pain from lumbar spondylosis affects a large proportion of the population. The operative treatment options for this condition remain controversial. Arthrodesis can be performed through posterolateral spinal fusion (PSF), transforaminal lumbar interbody fusion (TLIF), anterior lumbar interbody fusion (ALIF), or combined anterior-posterior fusion (AP fusion). These approaches have previously been shown to have comparable long-term outcomes in this population, but potential differences in perioperative complications have not been well characterized. The goal of the current study was to determine if there were differences in perioperative morbidity for different fusion techniques utilized for single-level lumbar spondylosis. Material and Methods: Patients with a diagnosis of lumbar spondylosis who underwent a single-level lumbar fusion surgery were identified in the 2010 to 2016 American College of Surgeons National Quality Improvement Program (ACS-NSQIP) database. Patients were identified using specific International Classification of Diseases (ICD) codes for degenerative lumbar disease. The NSQIP database tracks perioperative outcomes for 30 days after surgery. The patients were separated into groups based on their procedure (PSF, TLIF, ALIF, or AP fusion). Propensity-matched groups, accounting for age, BMI (body mass index), diabetes, ASA class, and sex, were created for each procedure. Adverse outcome rates were then compared using Fisher’s exact and Pearson’s chi-square tests. Results: In total, 4247 patients with single-level lumbar spondylosis were identified. Of these, PSF was performed for 628, TLIF for 1352, ALIF for 1561, and AP fusion for 706. The multivariate analysis showed small differences in demographics among the 4 groups, which were controlled for by propensity matching. With the propensity-matched groups, there were no differences among the groups in 30-day rates of individual adverse events or aggregated any adverse events, serious adverse events, or minor adverse events. In addition, there were no differences in infection rates and readmissions within 30 days. Conclusion: Debate continues regarding the optimal surgical procedure for lumbar spondylosis. The current study demonstrated that there were no differences in 30-day perioperative outcomes for the different surgical approaches evaluated for single-level fusion for lumbar spondylosis. These findings suggest that patient/surgeon preference and long-term outcome studies are better used to recommend one surgical approach over another.
P595: Posterior Cervical Laminectomy and Fusion Has Significantly Higher Rate of Overall Complications and Serious Adverse Events Compared With Cervical Corpectomy
Yaroslav Gelfand1, Jonathan Nakhla2, Rafael De La Garza-Ramos1, Murray Echt1, Michael Longo1, Merritt Kinon1, and Reza Yassari1
1Montefiore Medical Center, New York, NY, USA
2Rhode Island Hospital of Brown University, Providence, RI, USA
Introduction: Some cases of cervical stenosis yield themselves to either anterior or posterior approach for cervical intervention. Choosing an approach with less morbidity and shorter hospital stay would be beneficial in those cases. While it is well known that anterior cervical discectomy and fusion is a procedure with minimal morbidity and mortality we compared a more extensive anterior approach, cervical corpectomy to posterior laminectomy and fusion. Material and Methods: We identified patients who underwent elective cervical corpectomy (any number of levels, group1) or posterior cervical laminectomy and fusion (group 2) in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from 2006 to 2016. We excluded patients who had diagnoses of metastatic cancer, infection, or fractures. We also excluded patients who underwent a circumferential fusion (corpectomy with posterior fusion). Preoperative laboratory values, demographic details, and comorbidities were reviewed. A multivariate regression analysis was used to compare complications and serious adverse events between those 2 groups of patients. Complications included infection, wound disruption, pneumonia, pulmonary embolism (PE), reintubation, stroke, myocardial infarction (MI), any renal complication, urinart tract infection (UTI), deep vein thrombosis (DVT), cardiac arrest, and sepsis. Serious adverse events, as defined in prior literature were PE, stroke, MI, cardiac arrest, reintubation, or on ventilation for more than 48 hours, Sepsis or septic shock, acute renal failure, return to operating room, or death. Results: A total of 8702 patients who underwent elective corpectomy or posterior cervical laminectomy and fusion, without the diagnoses of metastatic disease, abscess, or fracture, were identified. Patients in the posterior cervical laminectomy and fusion group were more likely to be male and on average sicker than the patients in the corpectomy group. The rate of overall complications/severe adverse events was 3.6%/3.5% and 8.4%/6.6% in corpectomy group and posterior fusion group, respectively (P < .001). The patients in the posterior cervical laminectomy and fusion group were much more likely to suffer a complication in general (odds ratio [OR] = 1.8; 95% confidence interval [CI] = 1.5-2.3; P < .001) or a sever adverse event (OR = 1.4; 95% CI = 1.1-1.7; P = .001) compared with the patients in the corpectomy group adjusted for age, gender, and all the comorbidities. The length of stay also differed significantly between the 2 groups: 2.2 days for corpectomy group and 4.1 days for the posterior approach group (P < .001). Conclusion: Although further prospective studies are warranted, if there is an equal opportunity for decompression and symptom relief with both approaches, anterior corpectomy for cervical stenosis patients may be a less morbid operation with shorter length of stay.
P596: Perioperative Complication Rates of Spine Surgeries in an Ultra-Aged Cohort: A Single-Center Retrospective Review of 133 Patients Aged 80 Years or Older
Arun Chandra1, Wataru Ishida1, Adam D’Sa1, Joshua Casaos1, Alexander Perdomo-Pantoja1, Seba Ramhmdani1, Nicholas Theodore1, Ziya Gokaslan2, Jean-Paul Wolinsky3, Daniel Sciubba1, Ali Bydon1, Timothy F. Witham1, and Sheng-fu L. Lo1
1Johns Hopkins University, Baltimore, MD, USA
2Brown University, Providence, RI, USA
3Northwestern University, Chicago, IL, USA
Introduction: Spinal disorders such as metastatic spinal tumors, degenerative spine disease, trauma, and deformity are becoming increasingly more prevalent due to population aging, recent advancement in diagnostic modalities and treatment for cancers, and more accessible medical care. Hence, the demand for spinal surgery in the elderly is dramatically increasing. Spinal surgery in the elderly population can be especially challenging for spine surgeons due to higher risks of complications and need for meticulous perioperative management. While there is abundant clinical evidence regarding spine surgeries in patients aged 65 years or older, the literature specifically focusing on ultra-aged populations such as those aged 80 years or older is exceedingly sparse. Thus, the objective of this study was to summarize overall clinical outcomes of this high-risk cohort and understand factors associated with perioperative complications. Methods: Medical records of patients aged 80 years or older undergoing spinal procedures from 2010 to 2015 in a single-center were retrospectively reviewed, which included 133 patients. Baseline characteristics such as age, sex, preoperative diagnoses, and comorbidities as well as operative data including estimated blood loss, operative time, and 30-day perioperative medical (cardiac complications, respiratory complications, deep vein thrombosis, and urinary tract infection) and surgical complications (postoperative hematoma, screw breach, surgical site infection, vessel/nerve damage) (30D-MSC) were collected. Next, 133 patients were divided into the following 2 groups: 16 patients with 30D-MSC (group 1, 12.0%) and 117 patients without (group 2, 88.0%) and then statistically analyzed. P values <.05 were deemed statistically significant. Results: With regard to baseline characteristics, statistically significant intergroup differences were noted in the average age (81.2 ± 1.8 [group 1] vs 84.2 ± 3.0 [group 2], P < .0001), the average operative time (566.6 ± 312.0 vs 284.0 ± 222.5 minutes, P < .0001), and indications for operations (neoplastic pathologies: 25.0% vs 6.8%, P = .04). On the contrary, variables such as sex, estimated blood loss, the location of the operations (cervical vs thoracic vs lumbosacral), surgical approaches (anterior vs posterior vs combined), and spinal fusion procedures (with vs without) were not correlated with 30D-MSC with statistical significance. In multivariate analysis, longer operative time (P < .0001) and younger age (P < .001) were independently associated with increased 30D-MSC. Conclusions: Spine surgery in patients aged 80 years or older resulted in an acceptable perioperative complication rate of 12.0%; however, younger patients and longer operative time were associated with 30D-MSC, while acknowledging the retrospective, non-randomized nature of our study. The paradoxical increase in 30D-MSC in younger populations, other potentially influential factors on 30D-MSC as well as long-term outcomes such as reoperations and functional status need to be further investigated in future prospective studies as well as retrospective studies to better address the safety feature and cost-effectiveness of spine surgeries in this high-risk cohort and facilitate judicious patient selection.
P597: Palacos for Ventral Fusion as a Part of 360° Stabilization
Orlin Pavlov1 and Nikolay Mirchev1
1Klinikum Fulda, Fulda, Germany
Introduction: We reviewed 8 patients, who underwent a 360° spine surgery, in which Palacos cement was used together or all alone for ventral stabilization as a part of the circumferential stabilisation. Palacos is widely used for more than 50 years as a part of the spine surgeries. It is proven to enhance fusion rate and diminish revision rates. It is the golden standard in permanent fixation of the implants. Its role in 360° stabilizations is yet to be investigated. Materials and Methods: In our series, we reviewed 8 patients, who underwent a 360° stabilization of the spine and Palacos was used as a supportive material or alone for the ventral stabilization. This is a single-center, multi-surgeon retrospective review. The patients were operated between 2013 and 2018. In this series, there were 3 patients with tumors (primary or metastatic disease), 3 trauma patients, one with infection and one with degenerative spine. One of the patient was diagnosed with osteoporosis and one patient underwent a hysterectomy in younger age. Palacos was applied in ventral (3 patients) or dorsal (5 patients) approach for additional stabilization of the expanding cage in 7 patients and in one patient was used alone after partial resection of the vertebral body. Results: There were no patients who underwent a revision surgery. Fusion was achieved in all cases in a time period of 6 months. The application of Palacos did not affect the hospital stay. The usage of Palacos did not cause any Palacos-related complications, including pulmonary cement embolism. The usage of Palacos did not change the postoperative pain, measured on the visual analog scale. Conclusion: Palacos is safe for use in ventral stabilization as a part of circumferential spinal stabilization. In our series, there were no Palacos-associated complications. Fusion was achieved in all patients.
P598: Risk Factors Associated With Development of Urinary Retention Following Posterior Lumbar Spinal Fusion
Jeremy Mormol1, Bryce Basques1, Kevin Alter1, Jannat Khan1, Philip Louie1, Edward Goldberg1, Matthew Colman1, and Howard An1
1Rush University, Chicago, IL, USA
Introduction: Postoperative urinary retention (POUR) is common following lumbar spinal fusion procedures. While POUR can be troublesome for patients, it may also be an early symptom of postoperative epidural hematoma and can prompt initiation of an extensive, costly workup in POUR patients. Currently available research has identified conflicting risk factors for POUR, and the majority of these are nonmodifiable and are therefore not useful for prevention of this complication. In order to address this gap in the literature, the present study aims to further investigate several demographic, intraoperative, and postoperative characteristics associated with increased occurrence of POUR. Materials and Methods: A retrospective cohort study was performed using consecutive patients who underwent posterior lumbar laminectomy and fusion at an academic institution between 2011 and 2018. Basic patient demographic and comorbidity information, including presence of benign prostate hyperplasia (BPH) and usage of tamsulosin, was collected, along with operative characteristics such as number of levels fused during surgery, use of reversal agents neostigmine and sugammadex, operative time, and occurrence of intraoperative dural tear. Patients with a history of urologic problems other than BPH or prior history of POUR were excluded. Additionally, postoperative characteristics including urinary tract infection (UTI), prolonged retention of foley catheter (removal on postoperative day 2 or later), and narcotic pain medicine intake (converted to morphine equivalents) were collected. The standard protocol for all lumbar fusion patients at the institution is to document the first 3 postvoid residuals (PVRs) using a bladder scan, with POUR necessitating straight catheterization defined as a PVR greater than 400 mL. Patient, operative, and postoperative variables were tested for association using a multivariate regression model created in backwards stepwise fashion, where variables with the highest P value were sequentially removed until only those with P values <.200 remained in the model. Multivariate regressions controlled for potential confounding variables in order to identify independent risk factors for each outcome. The threshold for statistical significance was set at P < .05. Results: A total of 814 patients were included in this study. Average age was 58 years, average BMI (body mass index) was 30.89 kg/m2, and 52.95% of patients were female. Out of the total cohort, 138 (16.9%) had urinary retention requiring at least one straight catheterization. In the final multivariate model, prior diagnosis of BPH (odds ratio [OR] = 3.19; P = .001), American Society of Anesthesiologists (ASA) class 3 or greater (OR = 1.65; P = .027) were the best preoperative predictors of POUR, while prior history of lumbar spine surgery (OR = 0.57; P = .029) was associated with decreased rates of POUR. Use of neuromuscular blockade reversal agents (P = .026), intraoperative dural tear (P = .045) and postoperative UTI (P = .007) were additionally associated with POUR. Conclusion: In a series of 814 posterior lumbar fusion patients, BPH, ASA 3 or greater, use of neuromuscular blockade reversal agents, intraoperative dural tears, and postoperative UTI were independent predictors of POUR. Several of these identified risk factors, such as the usage of reversal agents, are potentially modifiable and provide attractive targets for limiting the occurrence of this common but impactful complication following lumbar fusion.
P599: Thecal Transection and Intracanal Fusion With Structural Allograft for Refractory Charcot Spinal Arthropathy
Cara Sedney1, Scott Daffner2, and John France2
1West Virginia University, Morgantown, WV, USA
Introduction: Charcot spinal arthropathy (CSA) as a result of impaired proprioceptive sensation is most often seen as a late sequel of spinal cord injury and presents a complex problem for surgical management and reconstruction. Despite the use of multiple strategies, such as circumferential debridement and reconstruction, multiple rod constructs, fusion to the pelvis and use of bone biologics to enhance fusion, nonunion and hardware failure can occur. The purpose of this study is to report a technique for thecal transection and spinal canal fusion as an option for refractory CSA. Methods: Three patients underwent thecal transection and canal fusion due to recurrent CSA. All patients had previously undergone circumferential fusion with extension across all mobile segments below the Charcot joint, but suffered recurrence of the destructive process and failure of fusion. After hardware placement, the thecal sac was exposed at the level of the charcot joint. Nerve roots were identified and ligated along the length of the planned transection. The thecal sac was then circumferentially dissected, ligated, and transected. Once the proximal and distal transection is complete along the area of planned fusion surface, the closed proximal end is pushed further up the canal beneath intact lamina, and the closed distal end is pushed distally. Anterior debridement is then completed. A structural allograft can then be placed within the spinal canal, extending 1 to 2 levels proximal and distal under intact posterior elements. The graft is then secured in compression. Results: Three patients with thoracic paraplegia who had developed recurrent lumbar CSA after previous reconstruction attempts underwent the above technique. On transection of the thecal sac, no cerebrospinal fluid was encountered in these patients due to fibrotic changes within the thecal sac; furthermore, no identifiable neural tissue was been encountered in these patients during transection. Two patients had mesh cages placed for anterior column support and one patient had a structural feloral allograft milled to provide both anterior column and intracanal support. One patient developed a subsequent thoracic CSA above the prior fixation 7 years later and had this technique repeated at that level. All patients had solid fusion at final follow-up. Conclusion: Treatment of refractory CSA with transection of the thecal sac and intracanal structural allograft is a reasonable option in patients with preexisting complete spinal cord injury without salvageable neurologic function who have failed prior reconstructive techniques. The improved visualization for anterior debridement as well as ample surface for bony fusion and the rigid span across the segment provided by the structural allograft contribute to successful fusion.
P600: Removal of Intradural Broken Needle in Thoracolumbar Spine: A Case Report
Felix Imposti1, Mariano Servidio1, Juan Manuel Gonzalez Viescas1, Laura Barutta1, and Marcelo Valacco1
1Churruca Hospital, Buenos Aires, Argentina
Introduction: Decreased needle gauge has decreased the incidence of postdural puncture headache but may make correct placement more difficult. Several cases of deformation and fracture of narrow gauge spinal needles have been reported. However, the literature is sparse about intradural localization. In this article, we report the diagnosis and subsequent removal of a fractured 27-gauge needle in T12-L1 intradural localization, 6 months after caesarean. Material and Methods: A 36-year-old woman who had undergone caesarean 6 months previously visited the hospital as an outpatient. Her symptoms were predominantly low back and radicular pain in right side, over the leg. The study X-ray, MRI (magnetic resonance imaging) and CT (computed tomography) scans revealed a strong metal artefact to be a needle fragment in T12-L1. Results: Surgical removal, under general anesthesia, revealed a severely bent 3 to 4 cm distal tip of a 27-gauge pencil point needle without the inner stylet. It was inserted at the T12-L1 intervertebral disc, through the dura. The dura was closed with 6.0 nylon and blood patch was used. No complications were reported. After that, the patient recovered well and left the hospital after 1 week. Conclusion: Previous report have described how spinal needles may deform or broken, during intradural anesthesia. However, there is no one about broken needle in intradural spine localization.
Trauma—Cervical
P601: Outcomes of Halo Immobilization for Cervical Spine Fractures
Robert Molinari1, Stacy Isidro1, Tochukwu Ikpeze1, and Addisu Mesfin1
1University of Rochester, Rochester, NY, USA
Introduction: To evaluate complications and outcomes of halo immobilization in patients with cervical spine fractures treated at a level I trauma center. Material and Methods: A retrospective evaluation of consecutive patients treated at a single institution with halo immobilization from August 2000 to February 2016 was performed. Demographic information (age, gender, and race), mechanism of injury, level of spine fracture, length of halo immobilization, complications associated with halo immobilization, and length of patient follow-up were collected. Inclusion criteria included halo immobilization of cervical spine fractures. Halos placed for post-surgical immobilization and for noncervical spine fractures were excluded. Results: A total of 189 patients treated with halos were identified. Of these 189 patients, 121 (64%) received halos for the management of cervical spine fractures and were included in the study. A total of 49.6% were males and 50.4% were females. The average age was 50.8 years (range = 1-89 years). A total of 81.9% were Caucasian, 13.8% were Hispanic/Latino, 3.2% were African-American, and 1.1% were Asian. A total of 10.7% sustained C1 fractures, 71.1% C2 fractures, and 18.2% sub-axial spine (C3-C7) fractures. Mechanism of injury included: 58.7% motor vehicle collisions and 41.3% were from falls. The average length of halo immobilization was 10 weeks (range = 0.29-16 weeks). The average length of follow-up was 10.9 months (range = 0.07-111). At latest follow-up, 73.6% had healed fractures with good alignment, minimal pain, and return to normal activities. There was a 9.1% mortality rate (18.2% died within 90 days of injury and 81.8% died within 1 year of injury). The mortality group had an average age of 68.4 years (range = 19-85). Mechanisms for halo-related deaths included cardiac, respiratory, and renal complications. A total of 17.4% of patients failed halo immobilization and were treated surgically. Overall, 39.7% of patients had minor perioperative complications or longer term complications such pin-site infections (9.1%), loose pins (3.3%), neck pain (18.2%), and decreased range of motion (4.9%). Conclusion: The use of halo immobilization for cervical spine fractures resulted in clinical success in 74.4% of patients. Loss of fracture reduction and surgical management occurred in 17.4% of patients who were initially treated with a halo. Early mortality rates are high in the elderly population. Lesser complications of halo use also remain moderately high and mostly include loosening of infected pins, neck pain, or decreased range of motion. Complication rates in geriatric patients averaged 25.5% and lower than previously reported in the literature.
P602: Realignment of Traumatic Subaxial Cervical Spondylolisthesis: Closed Reduction Followed by Anterior Cervical Discectomy and Fusion Gives the Highest Chance of Recovery
Pasquale Donnarumma1, Vincenzo Bozzini1, Arturo Berardi1, Savino Iodice1, Paola Salis1, and Gaetano Rizzi1
1Ospedali Riuniti di Foggia, Foggia, Italy
Introduction: Traumatic subaxial cervical spondylolisthesis is a severe form of fracture with dislocation of one vertebral body typically occurring after high kinetic energy trauma. Options of treatment include closed or open reduction, anterior, posterior, or combined arthrodesis. The aim of the study is to describe our 10 years experience of closed reduction using cervical traction followed by ACDF (anterior cervical discectomy and fusion) within 12 hours from injury. Material and Methods: We conducted a retrospective cohort study including consecutive patients affected by traumatic cervical spondyloptosis, operated by one main surgeon from January 2008 to December 2017. Participants were selected after surgical record review. The minimum follow-up is 1 year. Results: A total of 24 patients were included in the study. Cervical traction was applied within 1 to 5 hours from the diagnosis. A satisfactory realignment was achieved in all cases; the minimum wedge enough to obtain reduction was 12 kg, the maximum 26 kg (mean = 18 kg). Surgery consisting of anterior microdiscectomy and fusion with interbody cage and plating was performed 6 to 12 hours after traction positioning. Most patients presented with spinal cord injury: 8 were Frankel A (33%), 3 Frankel B (13%), 6 Frankel C (25%), 3 Frankel D (13%), and 4 Frankel E (17%). No neurologic deterioration was observed after the treatment. In 11 cases (45%), neurological symptoms improved 1 year after the trauma. Two patients (8%) died for complication related to spinal cord transition or organs damage. Conclusion: Early reduction gives the best chance of recovery for patients affected by traumatic subaxial cervical spondylolisthesis. Cervical traction is more often successful and safer than manipulation under anesthesia and surgical manipulation using a posterior approach. Once a satisfactory realignment was achieved the fracture can be successfully stabilized with anterior surgery alone.
P603: Odontoid Fractures Management With Aspen Collar in Elderly Patients
Yehya Ghonem1, Kathryn Ramshaw1, and Palaniappan Lakshmanan1
1Sunderland Royal Hospital, Sunderland, UK
Introduction: The cervical spine is the most commonly injured part of the spinal column. Among the cervical spines, the most common sites of injury are around the second cervical vertebra (C2, odontoid, or axis). Odontoid fractures in elderly are different from younger patients as showed by Lakshmanan et al in 2017 particularly in that arthritis involving the atlantoaxial joint plays part in the occurrence of these fractures, hence we aimed to assess the results of managing them conservatively. Material and Methods: We conducted a review to assess the survival rate and non-union rate among patient of odontoid fractures treated only by Aspen collar from 2013 to 2017 presented to our hospital. Thirty-five patients presented with variable types of odontoid fractures and managed solely by Aspen collar. The mean age of patients at the time of the fracture was 82 years and the median was 85 years. Survival rate were calculated using Kaplan-Meier survival curves. Non-union was calculated as incidence rate using standard percentage calculation. Results: The primary endpoint for the non-union was the failure of achieving any evidence of bone union after 6 months. We found that the adjusted non-union rate for those patients was 20%. While the primary endpoint for survival was a death from all causes. We found that the estimated survival probabilities for those patients after first, second, and third year were S (1) = 0.7, S (2) = 0.65, and S (3) = 0.35, respectively. None of the deaths was attributed to the fracture itself or its’ complications. Conclusion: Conservative management of odontoid fractures in elderly can be successful with good clinical outcome and little complications including neurological deficit even in the presence of residual instability.
P604: Do Not Neglect This Time!! Clinicoradiological Results in Surgical Management of Neglected Cervical Fracture Dislocation of Subaxial Spine—A Case Series
Zahirabbas Merchant1, Vishal Kundnani1, Rahul Prakash1, Ankit Patel1, Mihir Upadhyaya1, Rahul Mehta1, Neil Kire1, and Sanyam Jain1
1Bombay Hospital & Medical Research Center, Mumbai, Maharashtra, India
Introduction: Neglected cervical dislocations are difficult to manage as compared with fresh cervical dislocations. However, there is no consensus on guidelines for management and the ideal approach for these cases. Aims: To assess the utility of closed reduction with traction in neglected bilateral cervical facet dislocations and to validate the efficacy of posterior reduction with or without fusion along with anterior surgery for managing these patients with delayed presentations Material and Methods: Retrospective study with prospective data collection. Five patients presenting with neglected (>3 weeks) fracture dislocation of sub axial cervical spine managed surgically formed the study cohort. Demographic data like age, gender, mode of injury, duration of injury to time of presentation, and clinico-radiological variables like pain scores—VAS (visual analogue scale), neurology—Nurricks grade, facet dislocation or fracture, localised kyphosis angle, and myelomalacic changes in cord were evaluated and noted. Data was analyzed using the Student’s paired T test. All the 5 patients were manged by preoperative traction/posterior surgery for reduction followed by definitive anterior surgery. Results: Five cases (male/female = 5, mean age = 45 years), with bilateral facet dislocations (C45 = 1, C5-6 = 4) with >50% translation were included in the study. Mean duration of delay between injury to definitive management was of 8 weeks. One patient had preoperative C5 deficit with Nurrick grade 2 myelopathy and rest of them had no neurological deficit (n = 4). Two of our patients could be managed with closed reduction with skull traction, while 3 required open reduction with posterior release and partial facetectomy. All 5 underwent anterior surgery for definitive fusion after reduction in same sitting. Significant improvement in pain scores (pre/post = 7/2 with P ≤ .05) and local kyphosis (mean pre/post = 15.2 ± 6.2 with P ≤ .05) was achieved. Neurology improved with absence of any myelopathic signs and symptoms at final follow-up for all the patients. Conclusion: There is role for skull traction even in neglected cases of bilateral facet dislocations of subaxial cervical spine provided no autofusion is seen on radiological imaging. If reducible, then anterior fusion alone will suffice; whereas if its irreducible by traction then open posterior release and reduction with or without instrumentation followed by definitive anterior surgery yields satisfactory outcomes.
P605: Chronic Whiplash Injury: Deficient Inhibitory Endogenous Pain Modulation and Poor Quality of Life Correlate With Periaqueductal Gray Matter and Anterior Cingulate Cortex Biomarkers of Neuroexcitation and Neuroinflammation
Andres Barriga1, Luis-Maria Romero1, Diego Serrano1, Julian Taylor1, Jose Florensa1, Gerardo Avila1, Iriana Galan1, Antonio García-Peris1, and Julio Gomez-Soriano2
1Hospital Nacional Paraplejicos, Toledo, Spain
2University Castilla-La Mancha, Toledo, Spain
Introduction: Inhibitory endogenous pain modulation (EPM), mediated in part both by the periaqueductal gray (PAG) and anterior cingulate cortex (ACC), is deficient in chronic pain pathologies. ACCmetabolite levels, measured using magnetic resonance spectroscopy (MRS), are reliable biomarkers of chronic affective central pain. This study examined predictive correlations between ACC and PAG metabolite levels with deficient EPM, pain with specific descriptors and sensory changes, and health-related quality of life (QoL) during chronic whiplash injury (WHI). Material and Methods: Healthy subjects (n = 15), and participants with chronic WHI (Grade II-III), without (n = 5; WHI-noP) or with pain (n = 15; WHI-P), were screened with the Douleur Neuropathique 4 tool (DN4). EPM was assessed with C6 tonic heat pain stimuli with a conditioned pain modulation (CPM) protocol. MRS quantified ACC and PAG metabolite levels. Results: WHI-P participants were characterized with high pain intensity and interference, and lower QoL scores, compared with WHI-noP.Although inhibitory CPM of the 30° tonic pain intensity was identified in the healthy non-injured (−45 ± 16%; P < .001) and WHI-noP groups (−36 ± 8%; P < .001), inhibitory EPM was not detected in the WHI-P group (−25 ± 15%; P = .06).Stepwise multiple regression revealed that PAG glutamate/myo-inositolmetabolite ratio and total Cr levels predicted loss of EPM in the WHI-P group (R 2 = .48, α = .99; R 2 = .7, α = .99, respectively), while ACC glutamate/myo-inositol and myo-inositollevels alone predicted detection of chronic pain (DN4, R 2 = .54; α = .80) and poor QoL (R 2 = 0.55; α = .82). ACC myo-inositol also predicted pronociceptive EPM (R 2 = .44; α = .67), but at lower statistical power. Conclusion: Quantification of PAG and ACC metabolites related to neuroexcitation and neuroinflammation predict pathophysiological central chronic pain mechanisms related to EPM, while ACC biomarkers highlight the biopsychosocial impact of pain.
P606: Treatment Outcome of Axis Fracture
Shigeharu Fukao1
1Kyoto Okamoto Memorial Hospital, Kuse-gun, Japan
Introduction: Odontoid fracture has been recommended for conservative treatment for type 3 (fracture extending C2 body), surgical treatment for type 2 with severe instability. Recent axis body fractures frequently occur in elderly people with osteoporosis, so conservative treatments for type 3 are concerned with pseudoarthrosis and malunion. In this article, we report the outcome of the treatment of axis fractures and examined the points to be noted in the elderly. Material and Methods: Seventeen cases of traumatic axis fractures transported to our hospital during the period from April 2011 to March 2018, 2 cases of the traumatic spondylolisthesis of the axis (Hangman’s fracture), 12 cases of the odontoid fracture, 1 cases of the lateral mass fracture, and 2 cases of the vertebral body burst fracture. Eleven patients with odontoid fracture, excluding one who was transported in the state of cardiopulmonary arrest and died, were classified as odontoid fracture group (6 males, 5 females, average age = 74.1 years). Fracture type was type 2; 8 cases, type 3; 3 cases. The treatment method and its results were examined. In addition, 5 cases where 3 cases of odontoid fracture type 3 and 2 cases of vertebral body burst fracture were combined was treated as a vertebral body fracture group (2 males, 3 females, average age = 65.6 years), and the treatment method and its results were examined. Results: In 11 patients with odontoid fractures, 7 cases of type 2 fracture and 2 cases of type 3 fracture underwent anterior odontoid screw fixation. Two patients after surgery died within 3 months due to merging cerebral contusion and cholangiocarcinoma. In 6 of 7 patients observed after 3 months or more, cervical pain was improved in the early postoperative period and 6 cases confirmed bone fusion in CT (computed tomography). One case with pseudoarthrosis improved cervical pain. Among 2 cases of odontoid fracture with external cervical immobilization conservatively, one case of type 2 fracture was a pseudoarthrosis, and one case of type 3 fracture bone fusion in 3 months. The injuries of 5 vertebral body fracture group were 3 cases of falls and 2 cases of traffic accidents. Two cases achived bone fusion in 3 months following anterior screw fixation. Of the 3 cases of conservative treatment, 2 patients achived bone fusion at 3 months, but one case prolonged bone fusion and malunion. Conclusion: Since the fractures of the axis vertebral bodies of the elderly are often cases of vulnerable fractures based on osteoporosis, it is necessary to take into consideration the early fixation procedure when conservative treatment is not sufficiently successful.
P607: C1-C2 Traumatic Fractures Treatment and Clinico-Radiological Outcome in a Consecutive Series of 94 Patients
Edoardo Cipolleschi1, Giovanni Barbagli1, Giulio Carlo Wembagher1, Andrea Boschi1, and Stefano Romoli1
1Azienda Ospedaliero-Universitaria Careggi, Firenze, Italy
Introduction: The cranio-cervical junction (CVJ) is a complicated anatomical district, characterized by a wide range of movement. This feature makes the CVJ more incline to be a target during a traumatic event, as the junction is the site of more than 30% of all posttraumatic vertebral fractures. Many classifications and treatment algorithm have been designed in the past years in order to standardize the clinical approach to C1-C2 traumatic pathology; nonetheless, there are no enough evidence in the current literature to establish widely accepted guidelines. Our study is designed to analyze the clinical outcome following a conservative or surgical treatment in patient suffered by a C1-C2 traumatic fracture. Material and Methods: We retrospectively evaluated 94 patients treated to our institution in 2 years (2015-2016), encompassing 28 cases treated by surgery and 66 by an orthosis. We focused our analysis in a specific cohort of patients, the elderly ones, meaning only patients older than 70 years. Among patients with a C1 body traumatic fracture, we did stratify patients according to Gehweiler classification, to Dickman classification for the transverse ligament fractures associated to the C1 bony ones, according to Anderson-D’Alonzo modified by Grauer for the dens fractures, to Levine and Edwards for the hangman fractures, and to Benzel for C2 vertebral body fractures. We administrated the Neck Disability Index (NDI) questionnaire for the clinical outcome evaluation and investigated the rate of fusion as well as the impact of this feature on the outcome. The acquired data have been tested with SPSS IBM) v 25 statistical tool and refined by the Student’s t test, Pearson’s chi-square test, and the Fisher’s exact test. Results: Even our results show the same evidence reported in the literature, we should focus on 3 pivotal points: (1) the best clinical outcome in patient suffered by a type-2, type-3 dens fracture treated by surgery, according to the NDI; (2) the worst outcome in patient with a C1-C2 non fused fracture treated by an orthosis, compared with patients with the same but fused fracture; and (3) the statistical independence to the rate of fusion of the surgically treated patients, in the 6-months and 1-year outcome. Conclusion: Our observations led us to the superiority of surgical treatment in elderly patients affected by a type-2 fracture of the dens, when those patients are eligible for surgery, and to the evidenced that the non-fusion in patient treated conservatively represent an extremely negative prognostic factor. In conclusion, we may assume that an elderly patient eligible for surgery, suffering from a C1-C2 fracture, should be treated as the rest of the population, not allowing the advanced age to be an inhibiting factor in the choice of proper treatment.
P608: Upper Cervical Injury: Our Early Experience in National Trauma Centre of Nepal
Nilam Khadka1
1National Academy of Medical Sciences, Kathmandu, Nepal
Introduction: Upper cervical spine injuries account for about 24% of acute cervical fractures and dislocations of the cervical spine. With the inception of neurosurgical services in National Trauma Centre in mid-September of 2015, we have seen and treated more than 2 dozen upper cervical spine injuries. We had a great learning curve from C1-C2 wiring/occipitocervical fixation to anterior odontoid screw fixation. Therefore, we want to share or experiences. Materials and Methods: This is an ongoing prospective case series study being conducted in National Trauma Centre from October, 2015. American Spinal injury Association (ASIA) scale was used to measure the disability of these patients. Results: The number of patients with upper cervical injuries has reached 25 and is increasing in our Centre. Interestingly, almost every third patient (33%) of cervical injury is a case of upper cervical injury. Almost all the patients were from outside the Kathmandu valley and majority of them were in their 30s and had a fall as the cause of injury. There are 4 cases of C1 fractures; 11 cases with dens fracture; 11 cases with C2 body fracture; and 3 cases with hangman’s fracture. At least 5 patients had polytrauma along with cervical injuries. Surgeries were performed in 11 patients, one of them had subaxial cervical spine injury, too. Halo vest placement was performed in 7 patients, 2 of them was post surgery. Seven patients were treated conservatively with rigid cervical collar. Conclusion: The surgical decisions for these patients and outcome will be discussed. We had a great learning experience to deal with upper cervical injuries in the past 3 years.
Keywords
upper cervical injury, ASIA scale, occipito cervical fixation.
P609: Occipitocervical Dissociations: Report of 6 Cases and Review of the Literature
Vicente Ballesteros1, Javier Lecaros1, José Laso1, Marcos Gimbernat1, Alejandro Urzúa1, and José Fleiderman1
1Hospital del Trabajador, Santiago, Chile
Introduction: Occipitocervical dissociations (OCD) are high energy lessions, representing 1% of all cervical spine injuries, and are responsible for 30% of deaths related to cervical injuries. Due to the most effective rescue systems, their frequency is increasing, so it is mandatory to know the occipitocervical anatomy and suspect the lesion for an early diagnosis and proper management. Patients who survive a OCD have an 80% risk of neurological deficit, representing a major therapeutic challenge. Our purpose is to describe the clinical characteristics, the diagnostic process, the treatment and the evolution of patients with OCD, and to make a review of the available literature regarding this type of injury. Material and Methods: We reviewed the case series with occipitocervical dissociation treated in our institution. The data extracted consists of the type of injury, associated neurological injury, associated spinal injuries, radiological parameters, treatment, complications, and imaging evolution. In addition, in July 2018 a review was conducted of the literature in PubMed and EMBASE using the terms “atlantooccipital,” “dislocation,” “atlantooccipital dissociation,” and “craniocervical dislocation.” Results: A total of 3 men and 3 women presented OCD in our center. According to the Traynelis classification, 4 cases corresponded to type 1, one to type 2, and one to type 3. One patient had quadriplegia restored at the time of the accident, and one patient had sixth nerve palsy. Of the total number of patients, only 4 underwent occipitocervical fusion surgery. Perioperative complications were vertebral artery injury during instrumentation and one reoperation due to malreduction. Conclusion: OCD is a highly complex lesion that is frequently associated with neurological injuries and complications due to the surgical technique. Therefore, surgical treatment must be analyzed and defined individually.
P610: Percutaneous Screws Fixation in Occipitocervical Junction Fractures Supported With Computed Tomography–Guided Navigaton System: Five Years’ Experience, Department of Neurosurgery Copernicus Hospital in Gdansk
Wojciech Kloc1, Stanislaw Adamski2, Rafal Pankowski3, Marek Roclawski3, Marek Derenda2, Patryk Kurlandt2, Jakub Wisniewski2, and Katarzyna Aleksandrowicz2
1University of Warmia and Mazury, Olsztyn, Poland
2Copernicus Medical Centre, Gdansk, Poland
3Medical University, Gdansk, Poland
Introduction: With improvement in computed tomography (CT) navigation systems, a new ways of surgery with percutaneous screws placement were introduced. Longston described percutaneous screw fixation in cervical spine performed in human cadaver specimen in 2006. Then Sugimoto reported in 2010 surgery performed with 3D (3-dimensional) fluoroscopy and Yoshida in 2012 reported the same surgery performed with CT-guided navigation system. First series of 6 patients was prescribed by Buchholz in 2015. Also Hauck and Weiss reported series of 32 patient treated percutaneusely between 2007 and 2012 on Global Spine Congresses and World Spine Congress. Material and Methods: Between December 2013 and September 2018, we performed in our department 12 percutaneous surgeries. Percutaneous transarticular C1 C2 stabilization (2) for Gehlweier IIIb fracture, percutaneous stabilization of traumatic spondylolisthesis (6) via fracture sight, percutaneous occipitocervical fusion (3) for complex C1 C2 fractures, and percutaneous reconstruction of Atlas fracture. All surgeries were performed with CT-guided S7 navigation system. Results: All patients were discharged 3 to 5 days after surgery and controlled radiologically and clinically 1 month and 6 months posoperatively. Dynamic X-rays were performed 1 and 6 months postoperatively and confirmed stable and valid constructs. Patients returned to normal daily activity and improved clinically in pain and function. Conclusion: Percutaneous CT-guided systems seem to be a good option to achieve desirable effect in cervical surgery. A perfect knowledge about occipitocervical anatomy is mandatory. Surgeon has to be experienced in open surgeries, posterior instrumentation of cervical spine, and instrumentation under navigation systems.
P611: Treatment of Irreducible Odontoid Fracture Combined With Atlantoaxial Dislocation With Cable-Dragged Reduction and Cantilever Beam Internal Fixation
Qian Chen1
1Affiliated Hospital of North Sichuan Medical College, Nanchong, China
Introduction: Retrospective case study of surgical outcome for 10 odontoid fracture complicated with atlantoaxial dislocation patients treated with a technique called cable-dragged reduction/cantilever beam internal fixation. Surgery was performed by a senior attending surgeon. Material and Methods: Ten patients, aged 52.6 ± 11.3 years, 8 men and 2 women, with odontoid fracture combined with atlantoaxial dislocation that failed to be reduced after 10 to 14 days in traction, underwent posterior cable-dragged reduction/cantilever beam internal fixation surgery. Frankel classification of neural function before surgery was the following: Frankel B, 1 patient; Frankel C, 3 patients; Frankel D, 2 patients; and Frankel E, 4 patients. Plain radiographs, computed tomographic 3-dimensional reconstructive images and magnetic resonance images of the cervical spine were obtained at 3, 6, and 12 months after surgery, and each year thereafter. No patient was lost to follow-up, and the follow-up time ranged from 6 months to 2 years. Rate of reduction and C1∼3 fusion, as well as improvement of neural function, were recorded and analyzed. Results: The average follow-up period was 11.2 months. Radiographic evaluation of the group at follow-up showed 8 complete and 2 partial reductions, and satisfactory decompression and C1∼3 fusion in all cases. Neural function at the end of the follow-up was Frankel C in 1 patient and Frankel E in 9 patients. Conclusion: Posterior cable-dragged reduction/cantilever-beam internal fixation was an optimal salvage maneuver to conventional surgical methods such as anterior screw fixation and C1-C2 screw-rod system. The operative difficulty and incidence of nerve and vascular injury were reduced. Its major disadvantage is the exposure and screw-setting at C3, which is left intact in traditional surgery, and it is suitable only for patients with intact C1 posterior arches.
P612: Traumatic Anterior Atlantoaxial Subluxation (Type II) Associated With Type 3 Odontoid Fracture and Unilateral Locked Facets: A Case Report
Nitesh Gahlot1
1All India Institute of Medical Sciences (AIIMS), Jodhpur, Rajasthan, India
Introduction: Odontoid fracture associated with an atlantoaxial subluxation is a rare injury. Although type 3 odontoid fracture by itself has good healing rates, the associated subluxation of atlas over axis causes instability, which can have dire consequences for the patient. Here, we report a type 3 odontoid fracture with anterior atlantoaxial rotatory subluxation with unilateral locked facets. Material and Methods: This patient is a 47-year-old male who sustained injury to neck after falling from tree. He presented to our outpatient department with the complaints of severe neck pain radiating from the occipital region of neck to the supraclavicular region. The patient was otherwise neurologically normal with no deficit or pain in the upper limbs or weakness. He was given a cervical collar and was further investigated with radiographs, computed tomography (CT) scan and magnetic resonance imaging (MRI). Radiographs showed anterior subluxation at the atlantoaxial joint along with an odontoid fracture. CT scans confirmed the subluxation with the added diagnosis of c2 body fracture. There was locking of the left facets of c1 and c2 vertebrae with instability on lateral flexion extension views. MRI showed arching of the spinal cord over posterior aspect of the odontoid process, but there were no signal changes or compression. Based on imaging, diagnosis of atlantoaxial rotatory subluxation (Fielding type II) with C2 body fracture (Anderson and D’Alonzo type III) was made. Surgical stabilization was decided due to impending spinal cord compression, instability seen on the radiographs, and rotatory subluxation of c1 over c2. Posterior midline approach was used to facilitate reduction of the facet joint. Partial reduction was achieved intraoperatively by partially removing the superior articular facet of c2. Fixation was done by lateral mass screws in the c1 vertebra and laminar screws in c2 (as pedicle were fractured). Postoperative course was uneventful with improvement in pain and no neurological deficit. The patient was kept on cervical hard collar for 3 months. Two year postoperative radiographs show stable fixation and union of fracture. Results and Discussion: Combination of atantoaxial dislocation associated with axis vertebral body fracture is a rare injury pattern. Review of literature provides few cases, most of them having Fielding’s type IV C1-C2 subluxation associated with Anderson D’Alonzo type II/III fracture in C2 vertebra. We found no case with such injury pattern (C1C2 rotatory subluxation Fielding type II with C2 body fracture, Anderson and D’Alonzo type III) along with locking of facet joints of C1-C2. We decided for posterior surgical approach to directly reduce the facet joints and fix the C1 C2 articulation. Conclusion: This is a rare and important injury pattern, not previously reported in the literature. Detailed preoperative planning is important for atlantoaxial injuries to identify these injuries and administer appropriate treatment.
P613: Operative Management of Gunshot Wound to the Cervical Spine With Bullet Simulating C2-C3 Polyetheretherketone: Does It Confer Stability?
Alberto Daza1, David Solano1, William Riveros1, Javier Saavedra2, and Leonardo Laverde2
1Hospital Universitario Mayor, Bogota DC, Colombia
2Hospital Universitario de la Samaritana, Bogotá DC, Colombia
Introduction: The increasing prevalence and devastating socioeconomic consequence of spine injury remain a concern in modern medicine, specially, in developing countries. Patients presenting with gunshot wounds (GSWs) to the cervical spine are difficult to assess because of concomitant injuries as brain injury and poor quality of spine imaging due to artifacts. There is few evidence with the use of magnetic resonance imaging (MRI) in GSWs to the spine, however, MRI seems to be safety and useful to complete evaluation of spinal injury in case X-ray and computed tomography (CT) be insufficient. Surgery for patients with GSWs to the cervical spine remains controversial, however, the presence of neurologic symptoms, cerebrospinal fluid (CSF) leakage, or signs of instability are clear indications for operative treatment. Decompression and fusion are the main goals of surgical treatment. In our case, the bullet simulated a C2-C3 polyetheretherketone (PEEK) generating controversy about the stability of this construct and the real need of surgery. Purpose of the Study: The aim of this article is to describe and share the operative management in an unusual case of gunshot wound to the cervical spine and provide information regarding to the best surgical treatment supported by literature review. Materials and Methods: A 24-year-old male with past medical history positive for interauricular communication surgical repair and ileostomy due to bowel obstruction. The civilian presented gunshot wound with entrance hole at right malar region without exit hole. The initial management followed the standard trauma care. At neurological examination, the patient presented with upper right extremity paresia 4/5. Head-CT was performed without relevant findings. Cervical spine CT revealed the presence of bullet fragments located in intervertebral disc C2-C3 with fracture of upper C3 endplate and C2 posterior wall fracture. Arteriography ruled-out vascular injury. There were doubts about performing MRI due to potential risks as fragments migration, fragments heating, decline on neurologic function, and instability progression. Results: Despite the risks, cervical spine MRI was performed without complications. It confirmed the presence of fragments and extruded disc into spinal canal causing dural sac compression. The patient underwent decompression, resection of splinters and extruded disc, and fusion using PEEK cage with superior and inferior screws in midline to stabilize the vertebral body while preventing expulsion of the implant. Postoperative X-ray and TAC imaging showed a construct stability. The patient was followed-up for 18 months with improve in motor function and early return to work. Conclusions: Penetrating spinal injury is often associated with significant morbidity. Performing MRI to complete evaluation seems to be safety despite the potential risks. The optimal management of these patients has not been determined; however, spinal instability and neurological deficit are clear indications of operative treatment to improve rehabilitation and minimize socioeconomic impact.
P614: Frequency of Subaxial Cervical Spine Injuries in Germany According to the AOSpine Classification System
Philipp Schleicher1, Matti Scholz1, Frank Kandziora1, Andreas Badke2, Martin Bäumlein3, Florian Brakopp4, Hartmut Ekkerlein5, Thies Fischer6, Harry Gebhard7 ,8, Rene Hartensuer6, Miguel Pishnamaz9, Max Reinhold10, Götz Schäfer11, Gregor Schmeiser12, Thomas Weiss13, and Volker Zimmermann5
1BG Unfallklinik Frankfurt, Frankfurt, Germany
2BGU Tübingen, Tübingen, Germany
3Universitätsklinikum Gießen und Marburg, Marburg, Germany
4BG Klinikum Bergmannstrost, Halle, Germany
5Klinikum Traunstein, Traunstein, Germany
6Universitätsklinikum Münster, Münster. Germany
7Kantonsspital Aarau, Aarau, Switzerland
8Kantonsspital Baden, Baden, Switzerland
9Universitätsklinikum Aachen, Aachen, Germany
10Südstadt-Klinikum, Rostock. Germany
11Klinikum Ingolstadt, Ingolstadt, Germany
12Schön Klinik Hamburg-Eilbek, Hamburg, Germany
13BG Unfallklinik Murnau, Murnau, Germany
Introduction: The AOSpine classification system for injuries of the subaxial cervical spine allows for grading the injury severity according to morphologic and clinical-neurologic criteria. In contrast to the former AO Magerl classification, facet injuries and the neurologic status are classified separately using a designated coding. Up-to-date, epidemiologic data concerning the AOSpine classification are lacking. Aim of the study was to gather information about the frequency of the different injury subgroups, their segmental distribution, and a possible correlation to the severity of neurologic lesions. Materials and Methods: Multicentric retrospective analysis. The participating hospitals’ medical records were screened for subaxial cervical spine injuries according to ICD-10 (International Classification of Diseases, 10th Revision) codes. Imaging studies were reviewed and the injuries were classified according to AOSpine subaxial cervical spine injury classification. Neurologic status and therapeutic regimen were recorded. Results: From 2013 to 2017, 1186 cases were identified in the 10 participating hospitals. Of these, 854 could be classified completely according to AOSpine. The average age was 55 years (range = 6-95 years). Gender ratio male:female was approximately 3:1. About 45% of the injuries were Type A and B, respectively; 10% were Type C. Most frequent subgroups were A0 (27%), A1 (10%), B2 (24%), and B3 (20%). Concerning vertebral level, most injuries occurred at C6 (33%) and C7 (29%). Facet joint injuries were present in 40%. Most frequently type F2 (13.5%) and locked injuries (type F4; 12.5%). Floating lateral mass injuries were rarely seen (3.5%). F2 and F4 injuries frequently showed signs of radicular injury (20%), in F4-type injuries additional 30% had a (in)complete spinal cord injury. F3 injuries had a lower rate of radicular injury (13%) but an intermediate rate of SCI (13%). Fifty-five percent of the patients were treated operatively. Treatment regimen varied according to subgroups between 14% (A0) and over 80% (B2, B3, and C). F1-injuries were operated in 30%, F2/F3 in 60%, and F4 in 90%. Conclusion: For the first time, these data provide an overview about the frequency of different types of subaxial cervical spine injuries according to the AOSpine classification as well as the applied treatment regimen.
P615: C1-C2 Epidural Hematoma Related to Type II Odontoid Fracture: Presentation of a Case of an Infrequent Association
Angela Maria Carrascosa Granada1, Andres Camilo Vargas Jimenez1, Fernando Rascon1, and Willian Velasquez2
1Hospital Clinico San Carlos, Madrid, Spain
2Salta, Argentina
Introduction: Cervical spine trauma is an important cause of disability in adult population, particularly odontoid fractures result, in younger adults, from high energy trauma such as traffic accidents and in elderly due to falling from standing height. Biomechanics of trauma represent an important factor in developing an odontoid fracture, hyperextension of cervical spine results in ligamentous injuries as well as dens fracture due to the kynetics of forces applied to cervical spine. We present a case of an elderly patient, falling from standing height, who was identified a type II odontoid fracture, associated with an epidural hematoma, resulting in right hemiparesis, during his emergency room observation, being necessary urgent decompression and further spinal stabilization. Materials and Methods: We present a case of an elderly patient who suffered cervical trauma due to a fall of its own height, during his stay in the emergency room presents neurological deficit given by right hemiparesis, with a head computed tomography within normality. An urgent cervical spine computed tomography was performed identifying a type II odontoid fracture associated with an epidural hematoma on levels C1-C2. The patient underwent urgent decompression with transoral odontoidectomy and epidural hematoma drainage, as well as a Halo Jacket placement. A week later, the patient underwent occipito-cervical fusion due to spinal instability secondary to odontoid fracture. Results: The patient presented during a 12 hours observation period in the emergency room a neurological deterioration given by hemiparesis due to the presence of epidural hematoma and type II odontoid fracture. Due to its acute deficit, it was necessary to accomplish an urgent decompression achieved with a transoral odontoidectomy and epidural hematoma drainage. However, we identify that the presence of epidural hematoma in association with a odontoid fracture is not a common presentation of cervical spine trauma. Furthermore, as the patient had a hemodynamic and neurological stability it was considered an occipito-cervical fusion in a second surgical time in order to stabilize cervical spine after odontoidectomy. Conclusion: Despite of observation period during his stay in the emergency room, we considered important the time of progression of the neurological deficit (epidural hematoma causing hemiparesis), which is crucial at the time of prognosis and surgical outcome. However, we find remarkable the infrequent association of epidural hematoma and type II odontoid fracture, being even more frequently associated entities such as retroclival hematomas, characteristic of pediatric population. The basis of treatment in this patient was directed to spinal cord decompression, accomplished by transoral odontoidectomy, epidural hematoma drainage, and Halo Jacket placement, with occipito-cervical fusion in a second surgery time.
P616: Motion-Preserving Open Reduction With Internal Fixation of C1 Ring for the Treatment of Isolated C1 Burst Fractures
Luis Miguel Marques1, Miguel Brito1, Ding Zhang1, Ana Isabel Luis1, and José Cabral1
1Egas Moniz Hospital, Lisbon, Portugal
Introduction: Controversy surrounds the ideal treatment for isolated C1 burst fractures. The classical treatment used to be external immobilization, with surgery reserved for cases with transverse atlantal ligament disruption (Dickman type I) or as rescue therapy for failed conservative management. Until recently, operative treatment invariably involved some combination of fusion (initially C0-subaxial and lately C1-C2), sacrificing craniovertebral junction range of motion (ROM). Over the past decade, an innovative technique of internal osteosynthesis of C1 ring has emerged as a motion-preserving surgical alternative. We aimed to assess the safety, efficacy, and clinical results of this new technique for the treatment of isolated C1 burst fractures in our institution. Material and Methods: Retrospective review of isolated C1 burst fractures treated with open reduction and internal fixation of C1 ring (C1-ORIF) technique, via posterior bilateral C1 lateral mass screws interconnected with a transverse rod, after gentle compression to achieve reduction. Clinical and radiographic evaluations were preformed. Results: Three patients were treated with this technique (all male, age = 22-53 years). No complications were reported. Mean follow-up was 17.2 months (range = 10.8-28 months). Clinical outcome: mean VAS (visual analogue scale) = 1.66 (0, 2, and 3), mean NDI (Neck Disability Index) = 1.46% (0, 2.2, and 2.2). No significant cervical rotational or flexion/extension ROM limitation was noted. No translational instability on flexion/extension radiographs was seen (ADI [atlantodental interval] <3 mm). CT (computed tomography) scan documented fracture consolidation, with adequate and maintained reduction. Conclusion: Mirroring current literature, our limited but successful experience with posterior C1-ORIF technique for the treatment of isolated C1 burst fractures revealed it to be a safe and effective procedure with good clinical results.
P617: The Effect of Surgical Intervention on Neurologic Recovery in Cervical Injured Patients With Central Cord Syndrome
Yadong Zhang1, Yadong Zhang1, and Yadong Zhang1
1Shanghai Fengxian Central Hospital, Shanghai, China
Introduction: To review the experience of managing central cord syndrome (CCS) surgically, we retrospectively reviewed 71 patients with CCS managed surgically from October 2015 to April 2017. Material and Methods: Deteriorating neurological status with evidence of radiological compression and spinal instability were absolute indications for surgery. In surgical patients, causes of injury were classified. The American Spinal Injury Association (ASIA) motor and sensory scores (AMS) were recorded at the time of admission (aAMS), 3 days postoperatively (3dAMS), 1 month postoperatively (1mAMS), and at final follow-up (fAMS). A paired t test was performed to compare the admission to 3-day postoperative ASIA scores, admission to1-month postoperative ASIA scores, and admission to final follow-up ASIA scores. Surgery was successful in all 71 patients without reinjuring the spinal cord, infection, and other perioperative complications. Results: As for motor scale scores in this study, the ASIA motor scores at 3dAMS, 1mAMS, and fAMS significantly improved over preoperative ones. ASIA sensory scores at fAMS were significantly better than 3dAMS and 1mAMS scores. The ASIA motor and sensory scores at 1mAMS showed no significant improvements compared with the 3dAMS. Conclusion: Our results suggested that early surgery was beneficial for gain of neurological recovery in patients with CCS, spinal cord compression, and spinal instability.
Trauma—Other
P618: Spontaneous Spinal Epidural Hematoma due to Clopidogrel: A Case Study and Review of Literature
Aashish Ghodke1, Ram Chaddha2, Agnivesh Tikoo2, Harshal Bamb3, and Sagar Kelkar1
1Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, Shropshire, UK
2Apollo Hospitals, Navi Mumbai, Maharashtra, India
Introduction: Cases of spinal epidural hematoma without trauma or other mechanical insult are defined as spontaneous spinal epidural hematoma (SSEH). SSEH is an uncommon neurological emergency, which can present with the features ranging from simple back pain with radiculopathy to complete paraplegia or quadriplegia depending on the site and severity of the compression. SSEH associated with antiplatelet drugs is rarely seen and there are less than 10 cases of clopidogrel-induced SSEH being reported in the literature. We report a case of clopidogrel-induced SSEH and discuss what literature has to say on anticoagulant-induced SSEH. Case Presentation: We report a case of SSEH in a 76-year-old hypertensive female who was on clopidogrel post angioplasty done 1 year ago and presented with sudden-onset paraplegia preceded by severe back bain. MRI (magnetic resonance imaging) was done, which revealed a space occupying lesion at D9-D10 level, suggestive of an epidural hematoma. Emergent decompressive laminectomy was done within 8 hours of the presentation with excellent clinical outcome. Results and Discussion: The patient underwent emergency decompressive laminectomy from D9 to D11 level and evacuation of an extradural space occupying lesion, which was later histologically proven to be a hematoma. After surgery, there was a significant sensory recovery, 1 week after surgery, her weakness improved with muscle power of hip, and knee flexors was 3/5, and 1 month postoperatively, she could walk without any assistance. Conclusion: SSEH is a rare neurosurgical emergency and with the growing trend of antiplatelet prescriptions for prophylactic use, clinicians should be aware of this serious complication especially when other risk factors like uncontrolled hypertension are present. Correct diagnosis and urgent decompressive surgery with evacuation of the hematoma is imperative for successful recovery if severe neurological deterioration is present.
P619: Post-Traumatic Charcot Spinal Arthropathy at the Cervicothoracic Junction
Nilesh Mohan1 and Ufuk Aydinli2
1Moi Teaching and Referral Hospital, Eldoret, Kenya
2Medicabil Hospital, Bursa, Turkey
Introduction: Charcot spine arthropathy (post-traumatic neuroarthropathy of the spine) has been reported to be a very late and rare complication of spinal cord injury. Charcot of the cervicothoracic and upper thoracic region rarely is reported in the literature. Charcot spine arthropathy rarely occurs above the level of instrumentation. Charcot spinal arthropathy is a cause of progressive deformity and may present as late as 30 years after the original spinal cord injury. This is more common in paraplegic patients who are actively ambulating. Materials and Methods: A 56-year-old patient with complete paraplegia for approximately 20 years after spinal cord injury presented with severe kyphous deformity and instability of thoracolumbar spine. His sensory level to deep pain was at thoracic (D4). He kept developing new neuroarthropathies at different segments within a span of 5 to 6 months after every decompression and fusion with anterior cage and posterior instrumentation done. A total of 3 surgeries had been done in span of 2 years, initially thoracic, then lumbar and finally cervicothoracic junction. Conclusion: We present this case because of the challenges in surgery for instrumentation of new Charcot spinal arthropathy. Reports of neuroarthropathy developing above the level of spinal cord injury and at the cervicothoracic junction are rare. The treating surgeon should be cognizant of the possibility of developing secondary levels of neuroarthropathy above and below a previously successful fusion.
P620: Outcome in Treatment of Polytrauma Patients: A Single Institution’s 6-Year Experience
Uladzislau Ulasavets1, Ewelina Grzywna1, Jaroslaw Polak1, Katarzyna Jasinska1, and Marek Moskala1
1Jagiellonian University Medical College, Kraków, Poland
Introduction: The aim of our work is to analyze the results of treatment in polytrauma patients who required neurosurgical procedures. Material and Methods: Data on management and outcomes for patients with multiple trauma were collected retrospectively from years 2013 to 2018. The study group was divided into 2 subgroups according to the age (<50 vs >50 years), appearance of head trauma, and combination of head and spine trauma. Age, gender, comorbidities, neurological status, other injuries, and rehabilitation after surgical intervention were investigated. Results: We analyzed 93 patients with a diagnosis of polytrauma with mean age of 47.8 ± 18.35 years. Age >50 years increases the risk of prolonged hospitalization, including transfer to another hospital (odds ratio [OR] = 7.72; 95% confidence interval [CI] = 2.02-29.47), while the chance of being discharged home was higher for patients <50 years old (OR = 5.14; 95% CI = 1.99-13.28). Intensive care unit (ICU) stay increases 6.25 times the risk of long hospital stay (OR = 6.25; 95% CI = 2.21-18.2) and they were 4.96 times more often discharge to rehabilitation center (OR = 4.96; 95% CI = 1.65-14.86). Being male increases the risk at ICU treatment and prolonged hospitalization in rehabilitation facility (OR = 4.14; 95% CI = 1.26-13.59, OR = 4.20; 95% CI = 1.49-11.86, and OR = 6.22; 95% CI = 1.3-29.6). Patients with diagnosed spinal cord compression stayed longer at the hospital (8 vs 23.5 days, P = .001), had increased risk of ICU stay and the necessity of rehabilitation (OR = 7.51; 95% CI = 2.68-21.05, OR = 23.79; 95% CI = 5.92-95.65), and worse outcome in mRS (modified Rankin Scale) (l vs 4, P < . 001). Patients with head trauma presented with lower GCS (Glasgow Coma Scale; 13.3 vs 14.435, P = .025) and spent more days in hospital and ICU (25 vs 8, P = .0016 and 19.9 vs 8.09, P = .015). Conclusion: Results of treatment in multiple trauma patients remains unsatisfactory. The risk factors of prolonged hospitalization include older age, male gender, head trauma, and spinal cord compression according to our study.
P621: Spinal and Head Sports-Related Injury in the Pediatric Patient
Olimdzhan Iskhakov1, Olga Yanushkina1, and Medetbek Abakirov1
1Clinical and Research Institute of Urgent Pediatric Surgery and Traumatology, Moscow, Russian Federation
Introduction: Spinal and head sports-related injury in the pediatric patient sometimes accompanied by severe consequences. Material and Methods: The aim was to analyze the number and character of sports-related injuries in all patients with traumas admitted to the Clinical and Research Institute of Urgent Pediatric Surgery and Traumatology in Moscow, within 2013 to 2015. Totally, 1489 patients had sports injuries what made up 8.1% of 17 610 patients admitted with an acute trauma for the past 3 years. Musculoskeletal injuries were marked in 1129 (75.8%) of 1489 cases; spine injuries—in 93 (6.3%) patients: of them complicated spinal cord injury was revealed in 12 (0.9%) cases. Head injuries were revealed in 287 (19.3%) cases. Results: The distribution of head injuries (HIs) and spinal cord injuries (SCI) cases (299 patients) for each type of sports was as follows: football—78 cases (26.1%), combat sports—60 cases (20.1%), boxing—14 cases (4.7%), horse riding—13 cases (4.3%); gymnastics and acrobatics—11 cases (3.7%); figure skating—16 cases (5.4%); athletics—11 cases (3.7%), hockey—23 cases (7.7%); for winter sports (skiing, skating)—5 cases (1.7%); swimming—9 cases (3.0%); sports games except football—29 cases (9.7%); bicycle—7 cases (2.3%); and other sports—23 cases (7.7 0%). Sports-related neurotrauma was most frequent in children of school age, rarely—in kids of under school age. Age distribution of patients with sports brain injury was the following: ages 0 to 3 years—1 patient (0.3%); ages 4 to 7 years—29 patients (10.0%), ages 8 to 11 years—90 patiets (30.1%); ages 12 to 15 years—128 cases (42.8%), and ages 16 to 17 years—51 cases (17.1%). Mean age was 12.59 ± 3.1 in children with sports injury and 9.41 ± 5.1 in all children with an acute trauma on admission. Mild HI (84%) prevailed in all neurotrauma cases. Surgical operations were performed in 799 (54%) of 1489 patients with sports injury. Of them: operations on the musculoskeletal system were performed in 710 cases (88.8%), debridement of soft tissues wounds—in 50 (6.3%) cases, surgery for craniofacial fractures were necessary in 9 (1.1%) patients, and for abdominal and thoracic traumas—in 9 (1.1%) cases. Twenty-one patients (2.7%) underwent surgery for head injuries, including reposition, removal of intracranial hematomas, and decompressive craniectomy. Stabilization and spinal decompression were performed in 10 patients; 2 small kids revealed SCI by SCIWORA—without any CT (computed tomography) or MRI (magnetic resonance imaging) signs of spinal injury, which did not require any operation. Conclusion: Sports-related injuries in children made up 8.1% of all types of trauma with a musculoskeletal trauma prevailing. Neurotrauma made up 20%, while spine and spinal cord injury 1%. The predominating type of brain injury was concussion (84%). The most frequent types of sports-related injuries were football (26.1%) and combat sports (20.1%). Children aged 12 to 15 years are mostly prone to sports-related injuries. Mean age of children with sports injury was 12.59 ± 3.1, which was evidently higher than the age of all children with an acute trauma (9.41 ± 5.1) on admission.
P622: Robotic-Assisted Fixation for Hyperextension Thoracolumbar Vertebral Fractures in the Ankylosed Spine
Alexandra Satanovsky1, Yehichel Gelman, Hananel Shaar Yeshuv, Leon Kaplan, and Josh Schroeder
1Hadassah Medical Center, Jerusalem, Israel
Introduction: Patients with ankylosed spine have a higher rate of unstable thoracolumbar vertebral fractures that can lead to grave neurological complications. In recent years, several studies have indicated percutaneous fixation (PF) for traumatic thoracolumbar fractures is advantageous in aspects of infection rate, blood loss, and hospitalization time, but the data regarding extension type injuries is lacking. Robotic-assisted navigation registers each vertebra separately, in the ankylosed spine a modification needed to be applied as there are no disk space in the spine. In this study, we present the results for PF in extension type thoracolumbar fractures in the ankylosed spine. Materials and Methods: All patients with traumatic vertebral fractures, who underwent fixation at a level one trauma center between 2014 and 2018 were enrolled. Retrospective data of demographics (age, sex, and comorbidities), mechanism of injury, AO classification, level of injury, level and method of fixation, laboratory results (hemoglobin and hematocrite before and after surgery), requirement of blood products, length of hospital stay, discharge destination, change in Cobb angle, and complications were collected. Results: During the study period, 4 patients underwent fixation for extension type fractures. The average age was 75 years, all had ankylosed spine. The fractures were sustained from low-energy trauma (house falls). The fractures were between T11 and L1. All patients underwent robotic-assisted PF with cement augmented screws. Average level of fixation was 4.3 (range = 3-5), time of surgery 2:25 hours. All screws were properly placed. There were no surgical-related complications. Patients were discharged from the hospital to their home or rehabilitation facilities. Conclusion: We have found that robotic-assisted PF for extension type traumatic thoracolumbar fractures is safe and possible even in elderly patients with ankylosed spine.
P623: Associated Spinal Trauma in a Central London Level 1 Major Trauma Centre
Michail Kaminaris1, Simon Weil1, Jessica Gillchrist1, and Darren Lui1
1St Georges University Hospital, NHS Foundation Trust, London, UK
Introduction: There is a high incidence of concomitant injuries in the Major Trauma Centre (MTC) patients with spinal trauma. Understanding of the epidemiology of spinal injuries is important in guiding resource planning. In the modern era of emergency medicine protocols, MTC patients receive a whole-body computed tomography (CT) scan to assess potential injuries. We aim to assess the incidence of (a) spinal injuries in MTC patients with concomitant visceral, cardiothoracic, head injury (HI), or maxillofacial trauma; (b) the association of spinal injuries with orthopedic trauma subdivided by pelvic, lower, or upper extremity fractures; and (c) the risk of multilevel spinal injury according the type of fracture. Material and Methods: Retrospective analysis of the Trauma Audit Research Network (TARN) data from January 1, 2016, to December 31, 2016. The region of the spinal injuries and additional injuries were determined from the CT scan. Comparison of demographics, spinal injury, fracture type, mechanism of injury, and Injury Severity Score (ISS) were also undertaken. Results: A total of 377 patients identified with traumatic spinal injuries from a total of 2433 MTC patients (15.5%). Only 24% of patient sustained an isolated regional spine injury. The remainder (76%) had a concomitant injury. Concomitant Injuries: Cardiothoracic (45.8%), HI (25.7%), orthopedic trauma (44.2%), visceral injury (9.8%), and maxillofacial (12.4%). Isolated cervical spine fractures—16.9% versus 11.4% with concomitant injury, isolated thoracic spine fractures—5.5% versus 24.4% with concomitant injury, and isolated lumbar spine fractures—4.7% versus 22% with concomitant injury. Incidence of cervico + thoraco + lumbar injuries (1.8%), cervical and thoracic (10.8%), cervical and lumbar (2.6%), thoracic and lumbar (9.5%). Of 376 patients, 186 with ISS >15. Conclusion: Our figures show that fractures in all spinal regions are rare but the chances of 2 adjacent regions is approximately 10%. Our data also show that there is high incidence of concomitant injuries with spinal fractures. These results show higher rates of concomitant injuries than previous epidemiological studies.
P624: Percutaneous Lumbopelvic Fixation in Lumbosacral Trauma
Jaime Cancino1, Oscar Bravo1, Guillermo Izquierdo1, Felipe Novoa1, and Manuel Valencia1
1Mutual De Seguridad, Santiago, Chile
Introduction: Sacral fractures that result in spinopelvic dissociation are unstable injuries, associated with neurologic and soft tissues injuries. Percutaneous lumbopelvic fixation, through minimally invasive approach, has obtained good results in recent studies, with less bleeding, less operative time, and lower wound complication rate than open approach. The aim of this study is to show our experience in high-energy trauma patients with spinopelvic dissociations, treated with percutaneous lumbopelvic fixation. Materials and Methods: Retrospective study of patients admitted with spinopelvic dissociation, in 2 Chilean trauma centers. Every patient underwent percutaneous lumbopelvic fixation by the same surgical team. Demographic characteristics, injury mechanism, associated injuries, surgical time, blood loss, and follow-up complications were analyzed. StataSE12.0 was used for statistical analysis. Results: Ten patients who underwent percutaneous lumbopelvic fixation, after pelvic ring fixation, were included. Most patients were men (80%), mean age 39-year-old (range = 17-55). All of them, with high energy mechanism of injury: fall from height (50%) and pedestrian-motor vehicle accidents (30%). Sixty percent of patients required a bilateral fixation. Operative time averaged 1 hour 40 minutes (range = 75-210 minutes) and blood loss averaged 100 mL (range = 75-200 mL). One iliac screw was registered in wrong position, which was corrected during the same surgery. Four iliac screws were registered as prominent, non-symptomatic, which corresponded to the 3 first patients of the series. In 3 patients, instrumentation was removed, one of them because developed L5-S1 stenosis at 1 year of follow-up, which required decompression and L4-S1 fixation. Discussion: In polytraumatized patients, percutaneous lumbopelvic fixation is a good alternative that allow early mobilization of patients. Less surgical timing and bleeding, associated to clinical results comparable to open surgery, makes this technique a useful tool in these patients.
P625: Complex Fractures of the Sacrum With Spinopelvic Dissociation Treated Surgically With Ileolumbar Fixation
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler i Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Introduction: To analyze a series of cases of complex fractures of the sacrum with spinopelvic dissociation, surgically treated with lumbar ileus fixation. Methods: Retrospective analysis of medical records, cases operated using the Schildhauer technique for fixation, and followed up for at least 12 months. Functional results were assessed using the visual analogue pain scale (VAS) and the Oswestry 2.0 Index. Results: Six cases were analyzed, 4 of which evolved with moderate disability, 1 with minimal disability, and 1 with severe disability. Three cases that presented neurological deficits obtained significant improvement. Conclusion: The Schilhauer technique is efficient for fixation of complex fractures of the sacrum with spinopelvic dissociation. The patients evolved with good functional results. Early loading has been shown to be safe with the use of this treatment.
P626: Epidemiology of Polytrauma Spinal Cord Injury Patients: A Descriptive Study
Elvia Janike Rodriguez Cordoba1, Gustavo Casas Martinez1, Jose Gustavo Rodriguez Garnica2, and Omar Munoz Morales3
1Dr. Victorio De La Fuente Narvaez, Mexico City. Mexico
2Hospital Dr. Victorio De La Fuente Narvaez, Mexico City, Micronesia, Federated States
3Instituto Mexicano Del Seguro Social, Mexico City, Mexico
Introduction: Acute injuries of spinal cord are among the most common causes of severe disability and death after trauma. The purpose of this study was to describe the epidemiology of polytrauma spinal cord injury patients in main Trauma Center, Traumatology Hospital Dr. Victorio De La Fuente Narvaez, Mexican Social Security Institute. Material and Methods: We reviewed medical records of 38 patients with polytrauma spinal cord injury of cervical, thoracic, and lumbar spine admitted to intensive care unit (ICU), from January 2016 to July 2018, the scoring systems used were American Spinal Injury Association (ASIA), Glasgow Coma Scale (GCS), Injury Severity Score (ISS), Revised Trauma Score (RTS), Trauma Score–Injury Severity Score (TRISS). Variables included age, sex, etiology, place, season, weekday, concomitant injuries, comorbidities, lenght of ICU stay, level and severity of injury, surgical management, time of surgery, and bleeding. Results: Thirty-eight patients were admitted into this study. Thirty-three patients (84.1%) were male. The average age was 40.2 ± 16.9 years. The most common spine level injury was cervical (44.7%) being more frequent C6, followed by thoracic spine (31.6%). Among 38 patients with abnormal finding on neurological examination, 21 (55.3%) had complete spinal cord injury (class a of ASIA), B (13.2%), C (23.7%), and ASIA D (3%). By etiology, falls from height (44.7%) and traffic accidents (42.1%) were the most frecuent, followed by gunshot wound (13.2%) and fall of height (5.3%). Ethylic intoxication was found in (10.5%) patients. Overall, 86.8% (33) and 13.2% (5) of total trauma cases were blunt and penetrating, respectively. Most common asociated fractures were in upper extremities 31.6% (12), lower extremities 23.7% (9). One hundered percent had associated injuries, and 2 patients died (5.3%). Public road was the most common location for polytrauma spine cord injury 21 (55.3%), work 9 (23.7%), and home 8 (21.1%). Most accidents ocurred during spring 16 (42.1%). Wednesday and Saturday had the highest incidence of spine cord injuries, both 18.4% (6). The length of ICU stay ranged between 2 and 24 days (mean = 8.92 days). In total, 32 (84.2%) patients underwent surgical stabilization. The mean surgery time was 157 minutes (range = 10-500 minutes). Mean of ISS, RTS scores were 42.8 and 6.38, respectively. Conclusion: Most patients with polytrauma spinal cord injury were aged 18 to 36 years. A male predominance was observed and falls from height was the main cause of injury. Prevention of falls and motor vehicle accidents are important public health concerns.
P627: The Incidence of Timely Application of Mechanical Deep Vein Thrombosis Prophylaxis in Spine Trauma Patients
Jacob Hoffmann1, Matthew Hnatow1, James Showery1, Adam Park1, and Shah Dodwad1
1McGovern Medical School, Houston, TX, USA
Introduction: Patients with traumatic injuries to the spinal column have increased risk for deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT and PE contribute to the morbidity and mortality of these patients, particularly in the setting of poly-trauma. Several interventions have been devised to reduce the risk of these conditions by disrupting Virchow’s triad. It is standard practice to use 2 modalities of prophylactic anticoagulation in trauma patients. Namely, mechanical DVT prophylaxis with thromboembolic-deterrent (TED) hose, pneumatic sequential compression device (SCD) sleeves, and chemical anticoagulation with subcutaneously administered heparin or enoxaparin. Due to the risk of epidural hematoma and subsequent spinal cord compression, chemical anticoagulation is contraindicated in the setting of trauma to the spinal column. Thus, the early application of mechanical DVT prophylaxis is imperative as it is the only mode of prophylaxis in this at-risk population. This study aims to identify barriers to early application of mechanical DVT prophylaxis at a level one trauma center as well as identify and characterize thromboembolic events in patients sustaining spine trauma. Methods: Medical records of 132 patients seen by the orthopedic spine trauma service between June 1, 2017, and December 1, 2017, at Memorial Hermann - Texas Medical Center (MHH-TMC) were retrospectively reviewed. The presence of mechanical DVT prophylaxis devices was documented at the time of the consult being seen by the orthopedic spine trauma team and again at 24 hours after the consult was initiated. This information, as well as patient location at the time of consult and at 24 hours, activation of the general surgery trauma team and any subsequent diagnosis of DVT or PE was recorded and analyzed. Results: At the time of initial consult, only 9% of patients had TED hose in place whereas 14% of patients had SCDs in place and functioning properly. At 24 hours after initial evaluation, 48% of these patients had TED hose in place while 75% of patients had SCDs in place and functioning. The general surgery trauma team was consulted to evaluate 63% of patients in this series. None of the patients in this series were diagnosed with DVT. Two patients were diagnosed with PE at the second and third day mark after initial consult. Of note, both patients had mechanical DVT prophylaxis in place at 24 hours and pharmacologic DVT prophylaxis was not held due to spine trauma. Conclusion: Early application of appropriate mechanical DVT prophylaxis is critically important in preventing venous thomboembolic events. Less than half of all patients seen by the orthopedic spine consult team had documented mechanical DVT prophylaxis in place at the time of initial evaluation and only 75% of patients had SCDs in place at 24 hours after initial spine consult. Two patients were diagnosed with PE. These findings identify an area for potential improvement in the implementation of DVT/PE prophylaxis protocols at a level one trauma center.
P628: Multiple Fractures of the Ankylosed Spine in the Span of 14 Years: A Case Report
Tomi Kunej1 and Igor Movrin1
1Maribor University Medical Centre, Maribor, Slovenia
Introduction: We present a case of a 47-year-old male with 3 noncontiguous spine fractures in advanced ankylosing spondylitis (AS) in the course of 14 years. Materials and Methods: A 33-year-old patient with known AS presented to our department in December 2004 after a fall from 1.5 m, with a C6-C7 type C unstable fracture. On admission, signs of mild spinal cord injury (SCI) with mild senso-motor deficits (ASIA [American Spinal Injury Association] D) in the right upper extremity were noted. Emergency surgery was performed with anterior approach for reduction and fixation of a single spinal level with plate and screws. A week postoperatively dislocation of the fracture was seen and revision surgery was performed, with anterior plating and posterior fixation as a 2-stage procedure. The fracture healed uneventfully, and the neurological deficits improved completely. In January 2016, at the age of 45 years, the patient presented with persisting back pain without neurological deficits a couple of weeks after being hit on the back with a wooden plank. Imaging showed a TH 4-5 type B3 unstable fracture. This fracture was treated with a semi-MIS (minimally invasive surgery) posterior fixation—proximally open, since there was need to link the previous construct with the new one and distally percutaneously with pedicular screws. Postoperatively no special issues were noted, and the fracture healed uneventfully. Regular follow-ups were performed, which showed fracture union with no secondary dislocation or implant failure. In November 2017, the patient presented again to the emergency department (ED) with back pain, which started suddenly with no obvious trauma. Computed tomography (CT) scan showed an undislocated TH 8-9 type B3 fracture. Primarily the patient was treated conservatively, with regular clinical and X-ray follow-ups, which showed no secondary dislocation. In April 2018, the patient fell from standing height and presented to our ED. CT imaging showed dislocation of the previously described fracture. An identical surgery was performed with proximally open lengthening of the screw-rod construct and distally with percutaneous pedicular screws. Postoperatively again no fracture dislocation or hardware failure was seen, and the patient continued with all preoperative activities. Results: The patient suffered 3 unrelated spinal fractures in a setting of AS, with a decreasing severity of the trauma in each case. In the first case symptoms of mild SCI were noted, which disappeared post-operatively. The second and third time there were no symptoms of SCI, probably related to the smaller dislocation of the fractured vertebrae. The postoperative course was uneventful in the thoracic fractures, but the implant dislocation in the first case was probably related to the insufficient length of the plate, which spanned only one level. After revision surgery with longer anterior plates combined with a posterior screw-rod construct, the first fracture healed without complications. Conclusion: Multiple level spinal fractures in patients with AS are quite common and present a challenge for spinal surgeons, although it is uncommon for such fractures to occur in such a long time frame. We believe that further studies are needed to determine the feasibility of longer fixations as a preventative measure in such cases.
Trauma—Thoracolumbar
P629: Neurological Improvement After Early Versus Late Surgical Decompression for Traumatic Thoracolumbar Fractures: A Comparative Study
Ali Al-Hilli1, Wameedh Alsamak2, Sabah Nori2, and Zaid Khaleel2
1University of Baghdad, Baghdad, Iraq
2Medical City, Ghazi Hariri Hospital for Specialized Surgery, Baghdad, Iraq
Introduction: Background: Thoracolumbar spine fractures can result in significant disability and neurological deficit. Surgical treatment may minimize complications, controversies exist regarding the timing of surgery. Objectives: To evaluate the neurological improvement in patients with traumatic thoracolumbar fracture with neurological deficit, after early versus late surgical decompression. Material and Methods: A prospective cohort study was conducted in 25 patients with thoracolumbar fracture, met our inclusion criteria underwent surgical decompression and stabilization in Baghdad Medical City Complex and Neuroscience Hospital of Baghdad from August 2014 till December 2016, all patients evaluated according to the American Spinal Injury Association (ASIA) Impairment Scale (AIS) on admission and at (6) month of follow-up. Twelve patients underwent early surgical decompression (≤72 hours) and 13 patients underwent late surgical decompression mean time from injury to surgery was 12.5 ± 7.7 (range = 4-28) days. Results: A total of 12 patients underwent early surgery, 13 patients underwent late surgery, overall AIS improvement of early group were (66.6%), and late group were (76.9%), The change in AIS from preoperative to postoperative assessment was statically significant in patients who underwent early (P = .016) and late surgery (P = .032). All patients with partial neurological impairments had an improvement at least one grade (except for one early patient who remained in ASIA-B). All patients (6) with complete neurological impairments show no improvement. Both groups show improvement in AIS and the difference in the neurological improvement between the 2 groups were statically non-significant (P = .073). Conclusion: Significant improvement gained in patients with thoracolumbar fractures with partial neurological deficit in both early and late surgically decompressed patients. No significant difference in the rate of neurological improvement between early and late groups. Surgical decompression and fusion did not result in neurological recovery after complete neurological impairment in patients with thoracolumbar spine fractures.
P630: A Case of Traumatic Coronal Spondyloptosis: Review of Literature and Appropriate Operative Management
Anand Kaul1, Rafeed Al Drous1, and Bong-soo Kim1
1Temple University Hospital, Philadelphia, PA, USA
Introduction: Traumatic coronal spondyloptosis (TCS) is defined as greater than 100% subluxation of vertebral body over another in the coronal plane. It represents a rare type of spinal fracture dislocation generally secondary to high energy impact and it has a common association with injury to intraabdominal or thoracic organs, which often complicates management. There are currently no standardized guidelines for the management of this severe traumatic injury. Methods: We present a case of thoracolumbar (TL) junction TCS, discussing the surgical technique used for reduction, deformity correction, stabilization and fusion, and reviewing the techniques used for reduction of similar reported cases. Results: Our presented case with TLTCS was expertly managed with manual caudal reduction and the use of hand held clamps. The patient was positioned prone on gel rolls with pelvic corset applied in anticipation of intraoperative augmentation of traction. The patient was given ample muscle relaxant perioperatively. Pedicle screws were placed 3 levels above and below TL junction and fixated with temporary rods. Complete reduction was achieved with manual caudal reduction and drilling of intervening right T12-L1 facet joint. Following reduction, the installation of permanent rods and cross links with decortication of bone was performed to enhance posterolateral fusion. Conclusions: Our patient had ASIA (American Spinal Injury Association) A spinal cord injury preoperatively, thus we were able to utilize muscle relaxant medication to help facilitate reduction of deformity. In patients with residual neurological function, however, neuromonitoring is required, which limits the use of muscle relaxant and increases the difficulty of vertebral body distraction. Secondarily, reduction can be completed with the use of distraction instrumentation. If reduction requires high magnitude of distraction, a vertebrectomy of the dropped vertebra will shorten the spine and can facilitate reduction more safely. Understanding the variety of surgical options in operative management of TCS is critical in the correction of this debilitating and unstable injury.
P631: Correlation of PROMIS Physical Function and Pain Interference CAT Instruments With Oswestry Disability Index and Neck Disability Index in Spine Trauma Patients
David Bernstein1, Taylor D’Amore1, and Addisu Mesfin1
1 University of Rochester, Rochester, NY, USA
Introduction: The Oswestry Disability Index (ODI) and Neck Disability Index (NDI) were not intended for patients with spine trauma or spinal cord injury but are routinely used for such purposes. To date, the Patient-Reported Outcome Measurement Information System (PROMIS) has not been studied in the spine trauma population. We aimed to identify correlation between legacy outcome questionnaires (ODI, NDI) with PROMIS physical function (PF), pain interference (PI), and depression. Materials and Methods: A cohort of 63 spine trauma patients were identified at a level 1 trauma center between January 1, 2015, and December 31, 2017, through billing codes. The patient-reported questionnaire outcomes from 384 encounters were used for analysis. Fifty-seven patients underwent surgical intervention and 6 patients had a halo vest applied. The ODI was administered for thoracic/lumbar/sacral trauma patients while the NDI was administered for cervical spine trauma patients. Normality of distributions was assessed with Shapiro-Wilk test. PROMIS scores were not normally distributed in our cohort; therefore, the nonparametric Spearman rho (ρ) correlation was performed between ODI and NDI with PROMIS PF, PI, and depression scores. Coefficients of determination were reported for bivariate regression models. Results: PROMIS PF was moderately (ρ = −0.6254, R 2 = .266) and poorly (ρ = −0.259, R 2 = .501) correlated with the ODI and NDI, respectively. PROMIS PI was highly (ρ = 0.7345, R 2 = .537) and moderately (ρ = 0.6912, R 2 = .556) correlated with ODI and NDI, respectively. PROMIS depression was moderately (ρ = 0.528, R 2 = .182) and highly (ρ = 0.7234, R 2 = .378) correlated with OWI and NDI, respectively (Table 1). Conclusion: PROMIS PI is most highly correlated with legacy patient outcome questionnaires in patients with injuries to the spinal axis. While PROMIS PF shows moderate correlation with the ODI, a negligible correlation was found with the NDI. PROMIS tools allow for more effective data collection across multiple domains and, moving forward, may be better poised to monitor changes in function, pain, and depression compared with traditional outcome measures such as the ODI and NDI.
Table 1.
Correlation Between Legacy Patient-Reported Outcome Questionnaires (Oswestry Disability Index and Neck Disability Index) and Patient-Reported Outcome Measurement Information System (PROMIS) Physical Function, Pain Interference, and Depression Domains.
| PROMIS Domain | Spearman ρ | R 2 |
|---|---|---|
| Oswestry Disability Index | ||
| Physical function | −0.6254 | 0.266 |
| Pain interference | 0.7345 | 0.537 |
| Depression | 0.5280 | 0.182 |
| Neck Disability Index | ||
| Physical function | −0.259 | 0.501 |
| Pain interference | 0.6912 | 0.556 |
| Depression | 0.7234 | 0.378 |
P632: Classification and Management of AO Type C Thoraco-Lumbar Fracture Dislocations Without Neurological Deficit
Rishi M. Kanna1, Ajoy P. Shetty1, and Rajasekaran S1
1Ganga Hospital, Coimbatore, Tamil Nadu, India
Introduction: Thoracic and thoraco-lumbar fracture dislocations (TLFD; AO Type C injuries) result from high velocity injuries and frequently result in complete neurological deficit. Very rarely, such patients present with intact neurology and are documented only as case reports. We reviewed thoraco-lumbar AO type C injuries with minimal or no neurological deficit and present a novel classification of these injuries and their management. Methods: Case records of all patients with TLFD (AO type C) treated between 2012 and 2016 were reviewed to select patients with intact neurology, and documented for demographics, clinical and radiological data, and management. Based on coronal and sagittal reformatted CT (computed tomography) imaging, the injuries were classified as follows: lateral translation (LT, n = 9), sagittal translation (ST, n = 10), combined translation—antero (n = 14), and combined translation—retro (n = 3; Figure 1). The injuries were managed by stepwise meticulous unilateral exposure and temporary fixation, spinal decompression, gradual reduction of rods to screw heads and posterior long segment fixation. Perioperative complications, fracture healing, and functional outcomes at 1 year were assessed. Results: Thirty-six patients with thoraco-lumbar type C injury without paraplegia formed the study group. The mean age was 33.2 ± 13.1 years. Imaging and intraoperative observation showed that the integrity or injury of facet joints and posterior ligamentous complex (PLC) determined the different injury types. In LT, the facets were subluxated but PLC was intact, in ST, the facets were distracted but intact, and the PLC was disrupted. In combined—antero type, the facets were subluxated or unilateral facet fractures present but PLC was intact while in combined—retro type, the facets were subluxated posteriorly and the PLC was intact. While uniplanar translation (LT and ST) patients had intact neurology, biplanar translation had incomplete neurological deficits (n = 16). Post-surgery, all patients had complete reduction of the dislocation and the mean anteroposterior translation of 8.3 ± 3.4 mm was corrected to 1.7 ± 1.3 mm while mean lateral translation of 4.7 ± 4.8 mm was corrected to 0.7 ± 0.8. At the final follow-up, there were no implant failures or loss of reduction. Conclusion: TLFD without gross neurological deficit is very rare. The injuries are versatile and could be classified into 4 types based on the direction of translation. The integrity of the facet joints and PLC determined the pattern of the different injuries. Patients with biplanar translation sustained deficits and a meticulous surgical technique ensures safe reduction and good functional outcomes.
Figure 1.
Figure shows the classification of TLFD (thoraco-lumbar fracture dislocations) into 4 types (sagittal and coronal computed tomography [CT] of 4 representative patients given as A, B, C, and D). (A) Lateral translation as seen in coronal CT; (B) sagittal translation as seen in sagittal CT; (C) combined translation—antero, translated in both planes but anteriorly; and (D) combined translation—retro, translated in both planes but posteriorly.
P633: Outcome of Early Surgical Intervention in Spinal Trauma Patients: An Overview of 109 Spinal Trauma Patients
Ammar Dogar1, Rizwan Akram1, Amer Aziz1, Shahzad Javed1, and Haseeb Hussain1
1Surgery Ghurki Trust Teaching Hospital, Lahore, Pakistan
Introduction: The prognosis for spinal cord injuries varies depending on the severity of the injury. There is always hope of recovering some function with spinal cord injuries. The completeness and location of the injury will determine the prognosis. The sooner treatments are implemented to strengthen muscles below the level of the spinal cord injury, the better the prognosis. The first year of recovery is the hardest as the patient is just beginning to adjust to his or her condition. The use of physical and occupational therapy during this time is the key to recovery. The extent of the function fully returning is typically seen in the first 2 years after the initial injury. Objective: To determine the neurological outcome of patients who presented early with those whose presented late. Materials and Methodology: It was a descriptive case series done in the Department of Orthopedics and Spine between January 2014 and Decemeber 2016. A total of 109 patients who presented to ER (emergency room) or OPD (outpatient department) with spinal trauma were included. Those patients who were operated elsewhere or having trauma of more than 10 days or those who were managed conservatively were excluded. After admission, history, examination and investigations, and surgical intervention were done on same day. Every patient were followed regularly for 2 years to assess the neurology. The data was analyzed using SPSS 17.00 Version. Results: There were 109 total patients who presented with spine trauma. Seventy-four (67.9%) were male and 35 (32.1%) were females. Male to female ratio was 2.11:1. Of the 109 total patients who presented 78 (71%) were below 40 years of age and 41 (28.5%) patients were older than 40 years. Seventeen (15.6%) had trauma to the cervical spine, 34 (31.2%) to the thoracic spine, 3 (2.8%) to the thoracolumbar spine, and 55 (50.5%) to the lumbar spine. Seventy-nine (72.5%) patients had a fall from height. Twenty-six (23.9%) were involved in road traffic accidents. One (.9%) had assault and 3 (2.8%) had sports injuries . At the time of presentation out of 109 patients, 97 (89%) had their neurology involved while 12 (11%) had intact neurology. Eighteen (16.5%) presented within the first 24 hours while 91 (83.5%) presented after 24 hours. All the patients were operated on the same day of admission. Among the 18 patient who presented with in 24 hours,17 patients having full recovery with in 12.66 ± 1.2 months .While the late presenters only 15 patients get fully recovered after 2 year follow-up while 42 patients having partial neurology recovery and 24 having just sensory improvement and 28 having no improvement after two year follow-up. Conclusion: Spinal trauma is an emergency and having high morbidity and mortality rate. Early presentation and surgical intervention in spinal trauma patients having good neurological outcome as compared with delayed presentation and surgery.
P634: Review of Surgically Managed Dorsal and Lumbar Spine Trauma: Are We Achieving a Favorable Outcome in Nepal Despite the Odds
Gaurav Dhakal1, Ganesh Gurung1, and Santosh Poudel1
1National Trauma Center, Kathmandu, Nepal
Introduction: Outcome of spine injury treated in resource-constrained regions may not be the same as in developed nations. The aim of the present study was to study the epidemiological characteristics, delay, complications, and outcome of surgically treated dorsal and lumbar trauma. Material and Methods: Retrospective study of dorsal and lumbar spine injury patients treated between December 2015 and August 2017. Patients were segregated into 4 groups based on the timing of surgery: 0 to 2 days, 3 to 7 days, 8 to 30 days, and more than 31 days. Only one operating room twice a week was allotted to spine surgery and spine had to compete with orthopedic and surgical trauma for admission and surgery. Results: Ninety-one patients (male 61) with mean age 33 years were operated for dorsal and lumbar spine injuries. Eighty-four percent sustained a fall and 86.8% were from the periphery. Though 69.2% presented within 2 days, only 4.4% were operated within 2 days. Majority of the delay was due to unavailability of the operating room followed by financial constraints. Twenty-seven patients had complete deficit, 32 incomplete deficit, and 32 normal neurology. Four patients operated within 2 days improved their neurology, 7 incomplete deficit patients in 3 to 7 days group improved, 6 in 8 to 30 days group improved, whereas no patient in more than 31 days group improved. Overall 53.1% of incomplete deficit patients improved if operated within 30 days. No neurological improvement was seen in the 27 complete deficit patients. Wound infection, pulmonary contusion, and deep vein thrombosis were seen in 3 patients. Conclusion: As expected 95.6% of our patients were treated more than 3 days after injury and 60% more than a week later, which may not be acceptable in advanced countries. Despite the delay, 53.1% had an improvement in neurology when operated within 30 days. In resource-constrained regions, surgery still holds the key to improved neurological function and quicker rehabilitation, despite the delay.
P635: Repositioning Options With Percutanous Dorsal Instrumentation in Burst Fractures of the Thoracolumbar Junction
Thomas Weiss1, Oliver Gonschorek1, and Stefan Hauck1
1Berufsgenossenschaftliche Unfallklinik Murnau, Murnau, Germany
Introduction: The purpose of this examination was to evaluate percutaneous systems in reducing a relevant post-traumatic kyphosis in spinal burst fractures. Clinical advantages of percutanous techniques are evident in literature, disadvantage can be a minor result in reducing the fracture kyphosis. With new techniques and especially monoaxial percutaneous screws better results seem to be possible. Material and Methods: Seventy patients with burst fractures (AO-Type Magerl A3.1-A3.3) of the thoracolumbar spine have been treated in a special percutaneous reduction technique in BGU Murnau between June 2009 and March 2011. The post-traumatic and postoperative kyphosis has been measured in CT (computed tomography) scans in a monosegmental and bisegmental angle. Two different percutaneous fixation systems were compared in the reduction possibility. Statistics has been analyzed with Student t test. Results: We found a highly significantly difference between pre- and postoperative kyphosis angles. Between the 2 percutaneous systems we found no differences in reduction. In 39 cases, a additional reconstruction of the anterior column was necessary because of the ventral defect. In comparison with MCS 2 study of the German DGU, we found no difference in postoperative kyphosis angles (3°). Conclusion: A significant reduction of post-traumatic kyphosis in thoracolumbar burst fractures is with percutaneous techniques possible. The prerequisition are percutaneous monoaxial screws and tools and a special percutaneous technique as described.
P636: An Algorithm for Treatment of Multiple Vertebral Fractures
Giulio Carlo Wembagher1, Giovanni Barbagli1, Gianmarco Marchese1, Luigi Pansini1, and Stefano Romoli1
1 Chirurgia della Colonna, AOU Careggi, Florence, Italy
Introduction: Vertebral fractures are one of the most important consequences of osteoporosis and trauma injuries, due to the particular anatomy and biomechanics of the entire spinal segment. This kind of disease is very important in medical care for their both economic and social impact. In medical literature, the incidence of vertebral fractures is variable, amounting to about 700:100 000 (90% due to osteoporosis, 10% trauma injuries) and approximately 10% of patients present a multiple vertebral fracture, defined as the involvement of >2 or more vertebraes. Surgical options of these type of fractures are various and there is no unanimous consent about how to treat them; according to AO Foundation guidelines, it is well-known that type A3-A4-B1-B2 fractures, without severe anterior column damage, can be treated surgically with a short segment arthrodesis (one level above and one below). But what if we are dealing with a B3-C fracture or it is involving the thoraco-lumbar junction? In the past 9 years, surgeon’s choice in our institute was led by an “in house” flowchart developed for contiguous MVF (morphometric vertebral fracture) , taking into consideration both the type of the fracture (as defined by AO trauma classification) and the involvement of the thoraco-lumbar junction. Material and Methods: In this study, we retrospectively analyzed the patients undergoing surgery in the context of MVF: 124 out of a total of 1276 patients with thoraco-lumbar vertebral fracture (average age = 63.7 years, range = 17-78 years) in our operating room from 2009 to 2018. Short segment fixation was performed to A3-A4-B1-B2 fracture with no involvement of thoracolumbar junsction (TLJ), otherwise long fixation was performed as well for B3-C fracture (at least 2 levels above and below) no matter of TLJ involvement. Results: In our series, we had 1 case of fistula (treated with lumbar drainage), 1 case of screw malposition with neurological deficit that led to revision surgery, 4 cases of infections of soft tissues, and 5 cases of screws pull-out (3 with long fixation and 2 with short fixation) about 7 months later that led to an reoperation. Conclusion: AO guidelines suggest the use of short segment arthrodesis in case of A3-A4-B1-B2 fracture with no involvement of TLJ; we totally agree with these indications but they lack in case of most damaged fracture (B3-C) and in case of involvement of the junction decision is left to the single-surgeon experience. Our flowchart shows a clear indications about the choice between short- or long-segment arthrodesis, with good clinical outcomes.
P637: Outcome After Extreme Lateral Transpsoas Approach: Corpectomies Versus Interbody Fusion
Emre Yilmaz1, Ishak Basem1, Tamir Tawfik1, Amir Abdul-Jabbar1, Ronen Blecher1, Tom O’Lynnger1, Fernando Alonso1, Alexander von Glinski1, Rod Oskouian1, and Jens Chapman1
1Swedish Neuroscience Institute, Swedish Medical Center, Seattle, WA, USA
Introduction: The lateral transpsoas approach (LTPA) approach has gained popularity in thoraco-lumbar spine surgery procedures. Advantages include the preservation of posterior ligamentous elements, low blood loss, complete disc removal, and positioning of a large interbody implant increasing disc height and therefore achieving indirect decompression. However, there is a lack of data regarding motor and sensory complications that arise when a corpectomy is performed through the extreme lateral interbody fusion (XLIF) approach. Material and Method: Patients between 2006 and 2016, who underwent a corpectomy through an XLIF approach at a single institution were analyzed. Demographics, neurological outcome, and complications were recorded. All patients had a minimum follow-up of 6-months. Univariate analysis was performed to compare demographics, surgical characteristics, complications, and outcome scores. To compare categorical variables, the chi-square test was used. For continuous outcomes, simple linear regression was used. Statistical significance was set at P < .05. Results: A total of 166 patients were included. The mean age was 66.0 ± 10.4 years. The gender ratio was equal with 50.0% male and 50.0% female patients. The patients were divided into 2 groups; LTPA without corpectomy (n = 112) versus LTPA with corpectomy (n = 54). The groups were similar with regard to BMI (body mass index), gender, and cormorbidities. Patients without corpectomy showed a significantly lower rate of postoperative infections compared with patients with corpectomy (3.6% vs 22.2%; P < .000). A higher percentage of postoperative complications was found in patients with corpectomy (31.5% vs 13.4%; P = .006). The rate of neurologic complications at the 6-month follow-up (24.1% vs 31.5%; P = .313) and the reoperation rate (9.8% vs 7.4%; P = .741) did not show any significant difference. Conclusion: Patients who underwent a LTPA corpectomy might have a higher risk to suffer from postoperative complications. The results at the 6-month follow-up did not significantly differ between the groups. Lateral lumbar corpectomies may be performed safely with the use of intraoperative monitoring. Further research is needed to support these findings.
P638: Thoracolumbar Injury Classification and Severity Score For All? Time to Classify and Clarify
Sarah Barkley1, and James Tomlinson1
1Northern General Hospital, Sheffield, UK
Introduction: Several classifications systems have been developed to help guide clinical management of spinal fractures. The Thoracolumbar Injury Classification and Severity Score (TLICS) has already shown good reliability, reproducibility, and safety between spinal surgeons. There are no published studies on its use among nonspinal orthopedic surgeons, who often see thoracolumbar injuries in their clinical practice. Methods: Twenty-five patients with thoracolumbar spinal injuries were anonymized and their imaging shown to 10 nonspinal orthopedic surgeons. Powerpoint slides of all relevant imaging on each patient were distributed to participating surgeons; with neurological examination findings also included. Imaging was anonymized. Raters were asked to score the injuries using the TLICS classification. Three spinal surgeons also scored the injuries to provide a control group. The interobserver reliability was calculated using Fleiss kappa (κ), and analyzed against the Landis and Koch criteria. Patient treatment suggested by TLICS was also compared with actual treatment to assess its safety in nonexpert hands. Results: Scoring <4 had moderate reliability and score >4 good reliability. (κ scores = 0.53 and 0.75). The interobserver reliability for score = 4 was poor (0.02). There was very good agreement between the nonspinal and spinal surgeons regarding patients scoring <4 or >4 (87% and 75%, respectively), but poor agreement for patients scoring 4 (25%). Ten patients were managed operatively with 9/10 scored ≥4 (88% accuracy). Fifteen patients were managed non-operatively, with 14/15 scored ≤4 (92% accuracy). Conclusion: This is the first study of TLICS use as a triage tool by nonspinal surgeons. It suggests that TLICS is reliable, accurate, and safe in the hands of nonspinal surgeons. Feedback from study participants was that TLICS gave a structured approach to assess these injuries that was useful in their clinical practice.
P639: Posterior Minimally Invasive Surgery for Thoracolumbar Trauma: Los Angeles, Chile
Oscar Gonzalez Guerra1, Patricio Campos Carrasco1, Ramon Segovia1, Luis Medina1, Tatiana Saavedra1, Gustavo Canessa1, Boris Fuentealba1, Nicolas Costa Trucco1, and Marco Guevara1
1Neurosurgery Unit Complejo Asistencial Víctor Ríos Ruíz, Los Angeles, Chile
Introduction: Fractures of the thoracolumbar spine, and specifically of the thoracolumbar junction, are the most frequent injuries of the spine. Since 2016, we have done regularly minimally invasive surgery (MIS) for patients with thoracolumbar fractures in our center. The aim of this study is to compare open surgery versus less invasive techniques such as the mini-open or MIS selecting relevant clinical variables to determine if it is at least as effective and safe. For this, we did a retrospective analysis and literature review. Material and Methods: A descriptive and observational study was conducted on 50 patients aged 15 years or older who suffered fractures of the thoracic and/or lumbar segments who received some type of surgical treatment via posterior, whether traditional open surgery, mini-open or percutaneous, attended in the Neurosurgery Service of the Complejo Asistencial Víctor Ríos Ruiz of Los Ángeles, Chile, between January 2016 and June 2018. Data was collected from electronic records. All CT (computed tomography) scans were categorized under AOSpine Classification. Statistical analysis was performed using Microsoft Excel 2007 and Stata 12. Results: There were fifty cases in all, with mean age 49 years, and 56% were men. The most frequent mechanisms of injury were falls from height followed by traffic accidents, and the most frequent AO type fractures were A4, A3, and C in the thoracolumbar segments. The duration of the hospitalization, the number of postoperative days, the levels operated on, the number of screws used for surgery, the average surgical time, the fall of the postoperative hematocrit, and the time of return to normal activity were bigger in the open surgery group. In relation to postsurgical complications, these were only and exclusively observed in this group, as well as the need for reintervention. Regarding the radiological outcomes, there were no significant differences between both groups, considering the postsurgery angulation and the reduction of the vertebral body height. Conclusion: This is an initial experience, with few cases in MIS techniques, with limitations and bias related to retrospective analysis, but very valuable in terms to get the critical number in the learning curve for MIS surgery and adding options for surgical treatment for this condition in public institutions in our country. We confirm with this study that MIS techniques are at least safe and effective than open techniques presenting advantages by involving less soft tissue damage using smaller incisions and muscular dilators or transmuscular approaches.
P640: Double Balloon Vertebral Kyphoplasty: Early Results of a 10-Year Single-Centre Experience Analysis and Extended Indications in Thoraco-Lumbar Fractures Treatment
Maxime Raket1, Frank Hertel1, and Lynn Schroeder1
1Centre Hospitalier de Luxembourg, Luxembourg
Introduction: Vertebral fractures are a serious issue for public health and the management may involve highly invasive procedure especially regarding the elderly people and the ageing population. There are 2 distinguished entities of thoracic and lumbar fractures: compression fractures due to osteoporosis and traumatic fractures. The osteoporotic compression fractures, according to the expert, are the best indications for balloon kyphoplasty. Loose of height more than 70% and split/burst fractures (A1.2/A1.3/B according Magerl classification) are contraindications for traditional balloon kyphoplasty. Materials and Methods: We present some examples regarding our experience through more than 180 procedures of kyphoplasty mostly done with double balloon kyphoplasty (eg, 4 balloons). This is a single-center descriptive analysis. Results: Kyphoplasty is a mini-invasive technique that provides a quick and significant pain relief. Furthermore, we believe that 4 balloons kyphoplasty allowed the surgeon to perform cementing of complex osteoporotic and traumatic fractures with or without complementary instrumentation in order to provide a better pain relief or a better stability. We describe some techniques (one-side balloon technique to maintain remodelling while cementing, combined posterior approach with instrumentation, kissing cement placement, overlapping cortical fragment repositioning, posterior wall stabilization, etc) through several examples. Also the problem of catheter placement is partially solved by the double balloon system particularly regarding the problem of endplate perforation and posterior wall involvement. In this aim, the surgery planning is crucial to obtain a good remodelling and the intraoperative tomography may be a useful tool in complicated fractures. Double balloon kyphoplasty provides safe way to ensure a good remodelling of those complicated fractures (eg, vertebra plana, split, and burst fractures). Conclusion: We discuss controversial aspect such as adjacent level disease and PMMA (polymethyl methacrylate) long-term effect and stability. To conclude, we believe that this new technique brings more opportunities in the surgical management of vertebral fractures and improves the outcome through the technique, its inherent mini-invasive character and immediate pain relief. Further research and statistical analysis will be performed with this regard.
P641: Review of Mccormack Classification for Thoracolumbar Segment Fractures
Marcel Luiz Benato1, Pedro Grein del Santoro1, Alynson Larocca Kulcheski1, Andre Sebben1, and Xavier Soler i Graells1
1Hospital do Trabalhador, Curitiba, Brazil
Introduction: The aim of this study was to evaluate the success and complications rates of thoracolumbar fractures with a score equal or superior to 7 according to the load sharing classification (McCormack), surgically treated with short posterior fixation at 3 points. Methods: We evaluated 40 patients with thoracolumbar fractures and score by the load sharing classification ≥7, treated exclusively by surgery by short posterior fixation. We assessed epidemiological data, increased kyphosis, loss of vertebral body height, and complications at 2-year follow-up. Results: Although there was a statistically significant increase in kyphosis and a decrease in vertebral height, there was no clinical repercussion. Conclusion: Thus, we conclude that the McCormack classification is not a fundamental predictor for indication of anterior approach complementary to the short posterior fixation.
P642: Clinical and Radiological Evaluation of Vertebral Augmentation With Bone Cement Through Vertebroplasty and Kyphoplasty
Joel Sánchez García1, Ana Marisol González Silva1, and Agustín Caldera Duarte1
1 Private Practice Hospital Angeles del Pedregal, México City, Mexico
Introduction: Fractures in elderly people are associated with bone fragility. Osteoporosis is a skeletal disease characterized by reduced bone mass and loss of bone strength. Nevertheless in osteopenia only the bone density is low. In the past years, the bone cement is indicated for the treatment of pathological vertebral compression fractures using vertebroplasty or kyphoplasty procedures. Vertebral compression fractures may result from osteoporosis, benign lesions, and malignant lesions. The indications for vertebroplasty and kyphoplasty are evolving, and can be used for painful osteoporotic vertebral fractures stabilization, secondary vertebral collapse by trauma, and spinal metastases. This study was designed to determine the frequency that exists in patients with osteoporosis and osteopenia who presented fracture in thoracic and lumbar levels, as well as the radiological characteristics (vertebral body height) before and after performing vertebroplasty and kyphoplasty simultaneously, and placing bone cement. We use the visual analogue pain scale (VAS) to described the clinical evolution. Material and Methods: From 2007 to 2018, we studied 25 patients with pain compression fractures (diagnosed by imaging studies) in addition to osteoporosis and osteopenia, who also had a diagnosis measured by bone densitometry. Fifty-two percent of the 25 patients were female and 48% male. The average was 67.2 years. We performed vertebroplasty and kyphoplasty to the patients and bone cement was applied (StabiliT Vertebral Augmentation System by DFine). During the surgical procedure, we performed bone biopsy to discard any malignancy association. Before and after the procedure, spine radiographs were clinically evaluated, depending on each case. The changes in vertebral body height were measured (anterior, mean, and posterior with kyphosis angle) using a digital system RdiAnt DICOM Viewer. Also, we reviewed the medical records to obtain demographics and clinical parameters of pain relief, using a VAS (VAS, from 0 to 10). Results: According to the affected level, we find that 44% of cases corresponds to thoracic fracture, 28% to lumbar fracture, and 28% presented fracture at both levels. The results about bone densitometry showed that 72% of the patients were diagnosed with osteoporosis in spine and, in 28%, osteopenia was presented. This show significantly association (P < .001) between osteoporosis cases and fractures. After 6 months, the VAS results decreased significantly (P < .001) from preoperative to immediate postoperative and late postoperative evaluations. In average, the vertebral body heights significantly increased. In anterior vertebral body height increased to 3.6 mm, 4.2 mm in mean, and 2.2 mm in posterior vertebral body height. In average, the kyphosis angle significantly decreased 2.6 grades (P < .05) according to preoperatively to immediate postoperatively and late postoperatively evaluations. The bone biopsy results showed that 12% of the patients were diagnosed with multiple myeloma. Conclusion: Osteoporosis and osteopenia on spine are both a determining risk factor to suffer of spine fractures. After the bone fracture, the application of bone cement and the combination of kyphoplasty and vertebroplasty techniques improve the height of the vertebral bodies. This results in the immediately ameliorate of the symptoms and in the decrease of pain.
P643: Thirty-Year Follow-up of Nonoperative and Operative Management of Thoracolumbar Burst Fractures
Andrew Yongkun Liu1, James Brodell Jr1, Kiah Mayo1, and Addisu Mesfin1
1University of Rochester Medical Center, Rochester, NY, USA
Introduction: Burst fractures are common spinal injuries involving axial loading with flexion; they are most common at the thoracolumbar junction, a fulcrum of increased motion. Treatment costs for these fractures approach $17 billion per year. In the absence of neurologic injury, controversy remains over the role of operative management, and prior studies have reached heterogeneous conclusions. Most of these studies have evaluated medium-term follow-up of fewer than 20 years. Patient-Reported Outcomes Measurement Information System (PROMIS) is a validated, adaptive, group of questionnaires that assess clinical outcomes. They are designed to be relevant across all conditions for the assessment of symptoms and function. Our objective is to describe a 30-year follow-up of patients with thoracolumbar burst fractures treated at our institution. Material and Methods: All patients treated for thoracolumbar burst fractures at a single institution from 1987 through 1989 were reviewed. Operative treatment included posterior spinal fusion, while nonoperative treatment comprised body casting or bracing. A standardized phone script was utilized to recruit patients with current contact information and a medical encounter within the past 5 years. Enrolled patients completed the Oswestry Disability Index (ODI) questionnaire along with PROMIS Pain Interference and Physical Function instruments. New radiographs of the lumbar and thoracic spine were also obtained, and kyphosis was measured through Cobb angles. Descriptive statistics were performed for all measures. Results: Out of 93 subjects, 12 patients (7 nonoperative, 5 operative) have been enrolled thus far. No patients had neurologic deficits from their injury. The nonoperative group returned lower ODI scores compared with the operative group (median 0 vs 28, mean 10.7 vs 23.6). A similar trend was seen with PROMIS pain interference scores (median 38.7 vs 60.4, mean 48.6 vs 56.68). The standard error between groups was similar. No association was found between age and ODI or PROMIS scores. The PROMIS physical function score was approximately the same between both groups (47.6 vs 43.7 median; 46.9 vs 45.4 mean). Post-traumatic kyphosis did not substantially differ between patients managed operatively or nonoperatively (range = 1° to 13°). Conclusion: To the best of our knowledge, this is the first study assessing thoracolumbar burst fractures at 30-year follow-up. Our results suggest patients treated operatively may have higher global disability and functional impairment than patients treated non-operatively.
P644: Simply Minimal Invasive Method for Treatment of Thoracolumbar Junction Fractures Type B2 and a Associated with Kyphotic Spinal Deformity
Rafal Zaluski1 and Wiktor Urbanski2
1Medical University of Wroclaw, Wroclaw, Poland
Introduction: Fractures of thoracolumbar junction presents complex problems, particularly when associated with significant kyphosis. According to current literature in order to obtain good clinical result of the treatment, reduction of kyphosis and the restoration of proper sagittal spinal alignment is crucial. The objective of this article is to present minimal invasive technique of management of fractures located within thoracolumbar junction associated with kyphosis. Material and Methods: Thirty-eight consecutive patients who underwent surgical management of type A and B2 fractures located at the thoracolumbar junction fractures of T11-12, L1-2 were included into the study. This was a single-surgeon series of patients who had percutaneous kyphoplasty using stents and cement at fractured vertebra with additional percutaneous pedicular screw fixation. The fixation construct involves pedicle screws inserted 2 segments above and 1 segment below of fractured vertebra. Twenty-one elder patients with poor bone quality had polymethyl methacrylate (PMMA) cement to fill up the fractured vertebral body during kyphoplasty and screws were additionally augmented with PMMA. In 17 younger patients with good bone quality no screws augmentation was done. In this group during kyphoplasty in 11 cases mineral cement (hydroxyapatite with calcium sulfate) was used and in 6 cases PMMA with hydroxyapatite. Fixations without screw augmentation were removed routinely in 2 years follow-up. The restoration of kyphosis was assessed comparing preoperative and postoperative imaging, wedging of involved vertebra as well as kyphosis measured at adjacent to fractures segments. Length of operations, intraoperative blood loss, and complications were analyzed. Results: The authors observed mean postoperative kyphosis improvement of 9.9°, and the results were not statistically significant with P value of .06. The average reduction of kyphosis after operation was more pronounced by 10.3, with P = .0018. Average length of surgery was 1.5 hours with mean blood loss of 200 mL. No blood transfusion were necessary in this series. No major complications were reported, one patient had superficial wound infection. Thirty-eight percent of patients had bone cement leakage, however, all of them asymptomatic. Conclusion: Presented technique of management of thoracolumbar junction fractures with associated kyphosis seemed to be efficient and safe. Moreover, it provides improvement of sagittal spinal alignment.
P645: Transdiscal Pedicle Subtraction Osteotomy for the Treatment of Upper Thoracic Fractures
So Kato1, Mohammed Obeidat1, David Perlmutter1, and Stephen Lewis1
1Toronto Western Hospital, University of Toronto, Ontario, Canada
Introduction: Fractures in the upper thoracic spine present a challenge for surgical treatment. The thoracic spine is unique in that the narrowed spinal canal and the limited perfusion combine to exacerbate any trauma to the area. The goals of surgery are to stabilize the fracture and correct any local deformities in order to decompress the spinal cord. Surgical approach tends to vary based on institution and location of the fracture. Anterior approach offers direct access to the vertebral body without compromising the spinal cord but is complicated by anatomical structures in the operative field. The posterolateral approach avoids the anatomical issues of the anterior approach, but is associated with increased operative time and blood loss. While these approaches decompress the spinal cord, the posterior approach offers certain advantages in correcting and preventing progression of deformity. The primary goal of treating fractures with associated spinal cord compression is to decompress the spinal canal and stabilize the column. This includes correction of sagittal deformities, which have the potential to progress and later cause neurological deficits. Pedicle subtraction osteotomies (PSO) have become the choice method for the correction of fixed sagittal imbalance, owing most notably to the elimination of an anterior or combined method, which reduces procedural complexity and patient morbidity. Material and Methods: The radiographs and clinical charts were reviewed of a 49-year-old female and a 72-year-old male who underwent transdiscal PSO to treat upper thoracic fractures, performed by one surgeon at a single institution. A transdiscal osteotomy with resection of the distal pedicle and proximal body, the intervening disc space and the distal body of the proximal vertebra was performed. Reduction was achieved through a central hook rod construct. Results: Both patients presented with an upper thoracic fracture and underwent a segmental instrumented fusion with decompression and transdiscal PSO. At follow-up, both patients were doing well with no complaints or neurological issues. Conclusion: A transdiscal pedicle subtraction osteotomy provides canal decompression and reduction of the deformity in cases of thoracic trauma without the need for anterior interbody structural support.
P646: Assessment of Traumatic Dural Tears Associated With Thoracolumbar Burst Fractures and Its Relationship With AOSpine Injury Classification System
Guillermo Ricciardi1, Ignacio Garfinkel1, Gabriel Carrioli1, and Daniel Ricciardi1
1Centro Médico Integral Fitz Roy and Hospital General de Agudos Dr. Teodoro Álvarez, Buenos Aires, Argentina
Introduction: Thoracolumbar fractures can associate injuries of the dural sac with trapping of the cauda equine between bone fragments. The preoperative assessment of traumatic dural tears associated to thoracolumbar burst fractures allows the spine surgeon include in the surgical plan the duraplasty (microsurgery instruments, magnifying glasses, microscope, patches, or dural adhesives). The aim is to perform a retrospective analysis of the clinical-radiographic variables, the Thoracolumbar AOSpine Injury Classification System and associated dural tears in a series of burst fractures treated in our trauma center. Material and Methods: Retrospective study of a series of thoracolumbar fractures (T12-L5) with posterior wall involvement (A3-A4) treated surgically in our institution during the period between January 2012 and December 2017. Results: N = 46 patients. Sixteen cases with associated dural sac injury. The variables percentage of vertebral canal occupation, interpedicular distance, retropulsed fragment angle, and associated neurological deficit showed statistically significant differences according to the comparison depending on the presence or absence of dural injury (P = .046, P = .007, P = .046, and P = .004, respectively). Type C fractures presented in 80% (8 of 10) an associated dural tear compared with the rest of the types, this difference being statistically significant in the comparison (P = .001). The lamina fracture was diagnosed in 75% (12 of 16 patients) of the patients with dural injury; however, in our series we did not obtain statistically significant differences (P = .065). Three of 9 (19%) type B fractures had a dural tear (P = .919). Conclusion: We suggest that traumatic dural sac tears could be considered in the planning of thoracolumbar fractures in cases of voluminous fragments of the posterior wall with acute angle, severe occupation of the vertebral canal, elevated interpedicular distance, neurological symptoms, and evidence of displacement/dislocation (type C). We consider this study as a stimulus and a basis for the future development of research projects with a higher level of evidence to establish the relationship of risk of dural injury and the variables of the AOSpine classification system.
P647: Does Cement Leakage of PMMA-Augmented Pedicle Screws Lead to Clinically Relevant Complications? Experience From 96 Trauma Patients
Nick Fettke1, Eduardo M. Suero1, Wolfgang Boecker1, Christian Kammerlander1, and Simon Weidert1
1Ludwig Maximilian University of Munich, Klinikum Grosshadern, Munich, Germany
Introduction: Pedicle screw instrumentation is a standard technique for the treatment of spinal disorders such as instabilities or deformities. Previous studies have shown a high loosening and pull-out rate of pedicle screws, particularly in osteoporotic vertebrae. Cement augmentation of the pedicle screws has been proposed as a way to improve the screw-bone interface and prevent loosening. Biomechanical studies have demonstrated the stability advantages of the cement-augmented construct. However, previous authors have reported cement leakage in up to 94% of patients undergoing cement-augmented pedicle screw placement. While in most cases no adverse effects of cement leakage have been noted, leakage could lead to serious complications such as pulmonary cement embolism. In the current study, we aimed to retrospectively review our series of patients who received cement-augmented pedicle screw fixation for vertebral fractures using polymethylmethacrylate (PMMA) cement and determine the cement leakage rate and the rate of serious complications. Material and Methods: A total of 96 patients who were operated for various types of vertebral fractures and treated with cement-augment pedicle screw instrumentation were included in this study. We reviewed the patients’ medical records to extract demographic, clinical, and surgical information. In addition, we evaluated the intraoperative fluoroscopic images and the postoperative computed tomography (CT) scans to assess the rate of cement leakage. Results: There were 37 male patients (38%) and 59 female patients (62%), with a mean BMI (body mass index) of 27.1 kg/m2 (SD = 23.5 kg/m2). According to the American Society of Anesthesiologists (ASA) Physical Status Classification System, 15 patients (16%) were classified as ASA II; 67 patients (70%) as ASA III; 11 patients (12%) as ASA IV; and 1 patient (2%) as ASA V. There were 38 cases (40%) of thoracic instrumentation, 52 cases (54% of lumbar instrumentation), and 6 cases (6.2%) of thoracolumbar instrumentation. The majority of patients (n = 61, 63%) were instrumented at 2 spinal levels, with 25 patients (26%) having been instrumented at 4 levels. Six of the procedures were performed with the help of computer navigation. The average operation time was 118 minutes (SD = 56 minutes) and the average radiation time was 6 minutes (SD = 16 minutes). A total of 78 patients had intraoperative images available for review at the time of this analysis. Cement leakage was detected in 22 of those patients (28%). On examination of the available postoperative CT scans, 40 out of 41 patients (98%) had visual evidence of cement leakage. In total, 2 patients (2%) died within 14 days of the procedure. One case of asymptomatic cement embolism was recorded. Conclusion: We have reviewed a series of 96 patients who underwent cement-augmented pedicle screw placement for various types of vertebral fractures. We found a very high rate of cement leakage, comparable to previous reports, but without clinically relevant complications. Intraoperative imaging assessment was not an effective tool for identifying cement leakage. Further research is underway to identify risk factors of leakage and potential complications.
P648: Weekend Versus Weekday Admission in Spinal Cord Injury and Its Effect on Timing of Surgical Intervention
Rafael De la Garza Ramos1, Yaroslav Gelfand1, Murray Echt1, Michael Longo1, Merrit Kinon1, and Reza Yassari1
1Montefiore Medical Center, New York, NY, USA
Introduction: Cancer and spine surgery are known risk factors for venous thromboembolism (VTE). Patient with spinal tumors are at higher risk for these events compared with patients with other spinal disorders. The purpose of this study is to investigate the effect of timing of initiation of chemoprophylaxis on the incidence of VTE after surgery for metastatic tumors of the spine. Methods: A retrospective review of our institutional neurosurgical spine database for the years 2012 through 2018 was performed. Patients who underwent surgery for metastatic tumors were identified. The development of VTE—deep vein thrombosis (DVT) and/or pulmonary embolism (PE)—within 30 days was examined, as well as the occurrence of epidural hematoma. The incidence of VTE was compared between patients receiving “early” (within postoperative days 1-3) and “delayed” chemoprophylaxis (on or after postoperative day 4). Results: A total of 65 consecutive patients were identified (mean age 57, 62% male). The overall rate of VTE was 16.9%—all of whom had DVTs with a 3.1% rate of nonfatal PE (2 patients also developed PE). From the overall cohort, 36/65 (56%) received chemoprophylaxis in addition to mechanical prophylaxis—22 in the early group (61.1%) and 14 in the delayed group (38.9%). The risk of VTE was 9.1% in the early group and 35.7% in the delayed group (26.6% absolute risk reduction; P = .049); there were no cases of epidural hematoma. On multivariate analysis, delayed chemoprophylaxis was found to significantly increase the odds of VTE development (OR [odds ratio] 6.43; 95% CI [confidence interval] 1.01-41.2; P = .049). Conclusion: The findings of this study suggest that administration of chemoprophylaxis between days 1 and 3 after surgery for metastatic tumors of the spine may significantly reduce the risk of postoperative thromboembolic events.
P649: Smartphone Application as a Tool for the Measurement of Kyphosis in Thoracolumbar Fractures
José Laso1, Javier Lecaros1, Horacio Jimenez1, Marcos Gimbernat1, Ignacio Cirillo1, and Vicente Ballesteros1
1Hospital del Trabajador, Santiago, Chile
Introduction: The measurement of spinal sagittal alignment deviation allows one to calculate the severity of the vertebral damage secondary to a traumatic injury of the spine. Several methods have been described to quantify these angulations, the most used being Cobb. In the past, this method was difficult to quantify due to the need to use a conveyor to measure, but currently there are new digital images and software that more easily allow direct measurement of angulations. Presently, the use of smartphone applications as a measuring tool is growing; however, we do not know its accuracy compared with computational software in the context of trauma. Our purpose is to analyze the reliability of the measurement of angles in thoracolumbar fractures of the Compass application (for iPhone) and the digital software Xero Viewer 8.1.1 (Agfa). Material and Methods: Six surgeons reviewed 50 preoperative computed tomography (CT) scans of the spine in digital format. The scans were of patients treated at the Hospital del Trabajador between January 2013 and July 2018, with A3 and A4 thoracolumbar fractures of the AOSpine classification. Kyphosis measurement was applied by each surgeon twice independently, one with the digital software and another with the Compass application. The vertebral angle, segmental kyphosis, and local kyphosis were measured. The intraclass correlation coefficient (ICC) was used to assess the reliability between the tools. Results: The ICCs between both tools were 0.935 for the vertebral angle, 0.956 for the segmental kyphosis, and 0.851 for the local kyphosis. We found both tools extremely reliable for all the measurements. Conclusion: Overall, the smartphone application is a useful tool for the measurement of kyphosis in thoracolumbar fractures, equivalent in reliability to digital software.
P650: Ligamentotaxis in Thoracolumbar Fractures: Satisfactory Reduction According to Temporality
Javier Lecaros1, Horacio Jimenez1, Marcos Gimbernat1, Ignacio Cirillo1, José Fleiderman1, and Jorge Garrido1
1Hospital del Trabajador, Santiago, Chile
Introduction: Thoracolumbar burst fractures are characterized by a fragment in retropulsion into the spinal canal, which can generate neurological deficit. Surgical candidates are cases with an unstable pattern, progressive kyphosis, or neurological deficit. These fractures are controversial because surgical management varies according to the approach and decompression technique, which is usually achieved through a posterior approach. There is a lack of information in the literature regarding the relationship between temporality of the fracture and the effectiveness of this technique. Our purpose is to identify the association between indirect reduction and decompression obtained by ligamentotaxis and time of evolution of fracture. Material and Methods: We reviewed the thoracolumbar burst fracture cases operated in our center between 2012 and 2018, through a posterior approach using ligamentotaxis technique. We excluded patients with incomplete clinical records as well as patients operated on outside of our center. The data extracted was age, gender, AOSpine classification, presurgical interval days, instrumented levels, kyphosis correction, and canal occupation. The temporality of the fracture at the time of surgery was determined to perform an adequate decompression by ligamentotaxis. Results: We reviewed the thoracolumbar burst fracture cases operated in our center between 2012 and 2018, through a posterior approach using ligamentotaxis technique. We excluded patients with incomplete clinical records as well as patients operated on outside of our center. The data extracted was age, gender, AOSpine classification, presurgical interval days, instrumented levels, kyphosis correction, and canal occupation. The temporality of the fracture at the time of surgery was determined to perform an adequate decompression by ligamentotaxis. Conclusion: The ligamentotaxis technique is effective before 2 days of time evolution of fracture; nevertheless, in cases of more than 1 week from the accident, it loses capacity of reduction.
P651: Factors of Neurological Preservation in Fracture-Dislocation of the Thoracic and Lumbar Spine
Javier Lecaros1, Tomás Bustos1, Marcos Gimbernat1, Ignacio Cirillo1, Vicente Ballesteros1, and Alejandro Urzúa1
1Hospital del Trabajador, Santiago, Chile
Introduction: Fracture-dislocations of the thoracic and lumbar spine have been described based on their epidemiology and morphology, but there is lack of literature detailing those patients without neurological involvement. Our purpose is to identify common characteristics of thoracic and lumbar spinal dislocations without neurological involvement. Material and Methods: We reviewed the medical records and imaging of patients with spinal dislocation without neurological involvement treated in our center between 2008 and 2018. The data extracted was age, gender, presurgical interval, level of injury, number of instrumented levels, and presence of listhesis among others. Results: A total of 22 patients, 20 men and 2 women, with an average age of 45 years were identified. The thoracic spine was the most frequently affected with 72.7%, and the most commonly affected level was T4-T5 with 7 cases. In the total number of patients, median laterolisthesis was 9% (range: 0% to 29%) and antero/retrolisthesis was 9.5% (range: 0% to 70%). Most of the cases presented fracture of the posterior elements (laminae, pedicles, facets). Regarding surgical management, an average of 4-level fusion was made. Two patients needed a revision surgery (septic loosening and repositioning of screws) and another did not require surgery because of medical reasons. Conclusion: From our series of 22 cases with fracture-dislocation of the spine, we hypothesize that high thoracic fractures, translation less than 10% in any plane, and the presence of posterior arch fracture are common factors of neurological preservation.
P652: Appropriate Management of Vertebral Fragility Fractures: Development of a Treatment Pathway Based on the BenchMarket Medical Vertebral Compression Fracture Registry
Sigurd Berven1, Neal Shonnard2, Douglas Beall3, and Paul Anderson4
1University of California San Francisco, CA, USA
2Rainier Orthopedic Institute, Puyallup, WA, USA
3Oklahoma Spine Hospital, Edmond, OK, USA
4University of Wisconsin, Madison, WU, USA
Introduction: The management of vertebral compression fractures is characterized by significant variability regionally and globally. An evidence-based approach to the appropriate management of VCFs is not well-established. The BenchMarket Medical Vertebral Compression Fracture Registry (BMM VCF Registry) is designed to provide outcomes evidence on the topic of cement augmentation for VCFs for Medicare’s coverage with evidence development decision. The purpose of this article is to present a pathway for the appropriate use of vertebral augmentation based on the findings of the registry. Material and Methods: Prospective observational data including the patient characteristics, diagnosis, process of care, and patient-reported outcomes (PROs) for pain and function were collected from each treated patient. PROs were collected at baseline, 1 month, 3 months, and 6 months following the cement-augmented procedure. Primary outcomes were pain as measured by the Numeric Pain Rating Scale (NRS) and function as measured by the Rolland Morris Disability Questionnaire (RMDQ). Patient characteristics were also tracked as well as secondary outcomes including steroid use, diagnosis, cement leakage, new neurologic deficits, adverse events, readmissions, new VCF, and death. Results: The BMM VCF Registry delivered validated outcome data to support Noridian’s coverage with evidence development decision. A total of 1096 patients were included in the prospective registry. Registry outcomes confirmed post-market evidence of significant pain relief with mean pain decreases ranging from 6.1 to 7.3 on the NRS and function improvements ranging from 11.7 to 12.2 on the RMDQ scale for cement-augmented patients. Conclusion: Cement augmentation treatments of patients with acute painful VCFs reliably results in significant benefit regarding pain decrease and functional improvement for this vulnerable, elderly population. The study results support a treatment pathway involving cement augmentation in the management of elderly patients with symptomatic acute VCFs.
P653: Short-Term Clinical and Radiological Outcome of Balloon Kyphoplasty for Vertebral Compression Fractures: A Retrospective Analysis With 1-Year Follow-up
Shankar Acharya1
1Sir Gangaram Hospital, New Delhi, India
Background: Balloon kyphoplasty is a minimally invasive technique to alleviate the intractable pain caused by vertebral compression fractures and dramatically improves the quality of life in early postoperative period. This study is to analyze the clinical and radiological results of the balloon Kyphoplasty at 1 year for vertebral compression fractures. Material and Methods: This is a single-center retrospective consecutive case series with 1-year follow-up. We reviewed 99 patients (110 fractures) who underwent kyphoplasty from January 2013 to February 2015, and followed-up clinical and radiological records of 92 patients (102 fractures; mean age 67.09 years [range 44-91 years]). All patients underwent standing anteroposterior and lateral radiographs preoperatively, postoperatively, and at 1-year follow-up. Preoperative and postoperative visual analogue scores and Oswestry Disability Indexes were compared in 78 of these patients with at least 1-year follow-up. Cobb’s angle, vertebral heights, and height indices were analyzed in preoperative, postoperative, and 1-year follow-up radiographs. Results: Preoperative visual analogue scores and Oswestry Disability Indexes were improved significantly after kyphoplasty and maintained or further improved at 1-year follow-up. In 92.1% of the fractures, vertebral body height was restored in at least one of the measurements at anterior, middle, or posterior part of vertebral body. Mean kyphotic angle correction was 6.6° and 4.2° in postoperative and 1- year follow-up radiographs, respectively. Asymptomatic cement extravasation was observed in 12.74% of the fractures. New fractures were diagnosed in 7.8% of the patients, 37.5% of them were adjacent level fractures. Conclusion: Balloon kyphoplasty significantly improves quality of life in the early postoperative period and shows sustained benefits up to 1-year.
P654: Surgical Timing in Traumatic Thoracic Spinal Cord Injury: A Meta-Analysis
E. Martin1, P. C. de Witt Hamer1, J. van Oortmerssen1, N. A. Van der Gaag2, F. C. Oner3, W. P. Vandertop1, and Paula Valerie ter Wengel4
1Amsterdam UMC, VUMC, Amsterdam, Netherlands
2Leiden University Medical Center, The Hague, Netherlands
3University Medical Center Utrecht, Utrecht, Netherlands
4Slotervaart Hospital, Amsterdam, Netherlands
Introduction: The optimal timing of surgical decompression in thoracic and thoracolumbar traumatic spinal cord injury (tSCI), as well as its impact on neurological recovery, is still subject of debate. In cervical tSCI, early surgery improves neurological recovery in particular in complete tSCI patients. This study addresses neurological improvement after early and late surgery thoracic and thoracolumbar spinal cord injury. Material and Methods: A systematic search retrieved 14 publications of observational studies reporting outcome measurements after surgery in 1075 patients with thoracic and thoracolumbar tSCI from PubMed and Embase databases. The MOOSE guidelines were followed. Surgery was considered early within 24 hours, and late thereafter. An improvement of at least 2 grades on the ASIA (American Spinal Injury Association) scale was considered clinically meaningful. Improvement rates were summarized using individual patient data in a Bayesian random effects model and compared for those with early and late surgery. A subanalysis on complete and incomplete tSCI was also performed. Results: Seven studies investigated the effect of early surgery on neurological recovery. Five studies in patients with complete and incomplete tSCI found a beneficial effect of surgery performed within 24 hours. One study in 721 patients with incomplete tSCI found a significant benefit of early surgery, while another study in 33 complete tSCI patients did not observe a significant benefit on neurological recovery. Eleven studies contained outcome measures of 946 patients, which were suitable for quantitative synthesis. We did not observe a significant benefit of early surgery over late surgery. Conclusion: The results from this study indicate that early surgery within 24 hours might influence neurological recovery.
P655: Cement Augmentation of Compression Fractures Is Safe in the Very Elderly
Murillo Adrados1, Paul Bagi1, Courtney Toombs1, Anoop Galivanche1, Jonathan Grauer1, and Arya Varthi1
1Yale New Haven Hospital, New Haven, CT, USA
Introduction: The risk for a vertebral compression fracture is high for all geriatric patients and increases as patients get older. Cement augmentation has a proven benefit in limiting pain and expediting functional recovery after a fragility vertebral fracture. Although the very elderly (age ≥80) are at the greatest risk for sustaining a vertebral compression fracture, their perioperative risk profile after cement augmentation is not well defined. Materials and methods: The NSQIP (National Surgical Quality Improvement Program) database was queried for all patients over 60 years of age undergoing a single-level kyphoplasty or vertebroplasty between 2015 and 2016. Patients were stratified into 4 categories based on age, from 60 to 69 years, from 70 to 79 years, from 80 to 89 years, and 90 years and above. Demographics, comorbidities, procedure type, and postoperative complications were compared between each group using χ2 analysis. A multivariate odds ratio was performed to compare each group for all adverse events, serious adverse events and minor adverse events, return to the operative room, readmission, and mortality while controlling for sex, BMI, functional status, ASA classification, and procedure type. Results: A total of 1050 patients were included. There were 290 patients between 60 to 69 years of age, 383 between 70 and 79 327 between 80 and 89, and 50 patients were 90 years of age or older. Age groups did not significantly differ in their sex distribution, functional status prior to injury, or procedure type. Patients were significantly different in their BMI (body mass index) range, with younger patients trending toward higher rates of obesity, American Society of Anesthesiologists (ASA) classification, with patients in the older age groups with higher rates of ASA 3 or above. Patient age groups were not statistically different in terms of any adverse event, return to operating room, readmission, or death. Conclusions: The risk for adverse events after cement augmentation of vertebral fracture is not significantly different for patients more than 80 years of age. Cement augmentation has a reasonable adverse event profile in the very elderly.
P656: Functional Clinical Outcome of Patients With Traumatic Thoracolumbar Burst Fractures After Posterior-Anterior and Solitary Posterior Stabilization
Stefan Zwingenberger1, Nathalie Buck1, Alexander Thomas1, Philipp Flößel1, Rene Grass1, Klaus-Dieter Schaser1, and Alexander C. Disch1
1University Hospital Carl Gustav Carus at Technische Universität Dresden, Dresden, Germany
Introduction: Severe destruction of thoracolumbar vertebral body fractures has in unstable situations a high risk of kyphotic deformity, which secondary can cause spinal cord compression or sagittal dysbalance. If the type of surgery influences patients’ functional outcome is yet not clear. Material and Methods: Thirty patients have been included. Eighteen patients were operated in a posterior-anterior manner (male/female = 15/3) performing both operations on separate days but during a single in-patient stay. Twelve patients were only stabilized from posterior (male/female, 5/7). The average age was 50 ± 14 years for patients with posterior-anterior operation and 54 ± 18 for patients with single dorsal stabilization. Included were mono-segmental type-A3 and -A4-fractures or type-B-injuries of Th 11 to L 2. The follow-up-period was 4.1 ± 1.9 years for posterior-anterior and 3.1 ± 1.5 years for posterior stabilization (range: 2-8 years). The body height was 178 ± 8 cm for patients with posterior-anterior and 170 ± 6 cm for patients with posterior stabilization, weight was 78 ± 11 kg posterior-anterior and 73 ± 15 kg for patients with posterior stabilization. Trunk muscle strength was assessed isokinetically and concentrically with IsoMed 2000 dynamometer. HRQOL was determined by the EQ-5D questionnaire and limitations in daily routine by the Oswestry Low Back Pain Disability Questionnaire (ODQ). For descriptive statistics mean values and standard deviation were used. Statistical significance between the 2 groups was determined by Student’s t test. Results: The ratio of maximal extensional power and body weight was 2.7 ± 1.5 N/kg for patients after posterior-anterior and 2.7 ± 1.4 N/kg for patients after posterior stabilization (P = .9842). EQ-5D Index (sum model) showed a tendency to lower live quality in patients operated from posterior-anterior (85 ± 15) compared with patients operated from posterior (92 ± 11, P = .2245). There were equal constellations regarding the EQ-5D’s results with 79 ± 19 in the posterior-anterior and 84 ± 14 in the posterior group (P = .4163). Both groups had only a few limitations in daily routine (Oswestry Disability Index [ODI]) with 7 ± 8% in the posterior-anterior and 9 ± 9% in the posterior group (P = .5047). Conclusion: Patients with traumatic thoracolumbar burst fractures operated in a posterior-anterior manner or only from posterior presented a comparable mid-term outcome. Since an approach only from posterior is less invasive compared with a posterior-anterior operation, thoracolumbar fractures with indication for stabilization should initially be stabilized only from posterior. Only in case of missing osseous consolidation, destruction of the intervertebral disc or secondary kyphosis an additional ventral fusion should be done.
P657: Anterior Versus Posterior Approach in the Management of Traumatic Thoracolumbar Burst Fractures: Systematic Review and Meta-Analysis
Terence Tan1, Joost Rutges2, Travis Marion3, Joseph Mathew4, Mark Fitzgerald4, and Jin Tee1
1Alfred Hospital, Melbourne, Victoria, Australia
2Erasmus MC, Rotterdam, Netherlands
3Big Thunder Orthopaedic Associates, Thunder Bay, Ontario, Canada
4 National Trauma Research Institute, Melbourne, Victoria, Australia
Introduction: Uncertainties remain regarding the optimal surgical approach (anterior versus posterior) in the treatment of traumatic thoracolumbar burst fractures. The aim of this systematic review and meta-analysis is to compare the surgical, radiological, and functional outcomes between anterior and posterior approaches in patients who have sustained a traumatic thoracolumbar burst fracture. In this review, the authors included only “pure” burst fractures without concomitant posterior osteoligamentous, distraction, rotational, or translational injuries. Material and Methods: A systematic review adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was performed. The authors reviewed comparative studies evaluating anterior versus posterior approaches in terms of clinical, surgical, radiographic, and functional patient outcomes. Qualitative analysis was performed. Where suitable, meta-analysis was performed to compute pooled estimates of the differences between anterior and posterior approaches. Results: A total of 6 studies (3 observational, 1 prospective nonrandomized trial, 2 randomized controlled trials) were included. There were no cases of neurological decline postoperatively regardless of approach. Meta-analysis demonstrates a longer duration (mean difference [MD] 81.68, 95% confidence interval [CI] 39.20-123.16, P < .001) and increased estimated blood loss (MD 426.27, 95% CI 119.84-732.70, P = .006) for the anterior as compared with the posterior approach. No difference between approaches was found with regard to length of hospital stay, late postoperative kyphotic angle, construct failure rate, instrumentation revision rate, rate of return to work, and total hospital charges. Conclusion: Considering the similarities in neurological, radiological, and functional outcomes between the anterior and posterior approaches, the longer duration and estimated blood loss in the anterior approach should be a point of consideration when selecting the surgical approach undertaken. To advance current evidence, future studies should compare the anterior and posterior approaches in non-intact patients with traumatic thoracolumbar burst fractures.
P658: Prospective Comparison of Clinical and Radiographic Outcomes of the Treatment of Thoracolumbar A3 and A4 (Ao) Burst Fractures Without Neurology: Open Versus Percutaneous Pedicle-Screw Instrumentation Versus Percutaneous Vertebral Augmentation With Cranio-Caudal Expandable Implant SpineJack
Marek Roclawski1, Rafal Pankowski1, Wojciech Kloc2, Stanislaw Adamski3, Sergiusz Bielocerkowski1, Adam Augustyniak1, and Marcin Ceynowa1
1Medical University of Gdansk, Gdansk, Poland
2University of Warmia and Mazury, Gdansk, Poland
Introduction: Despite an abundant literature there is still lack of agreement due to the management of thoracolumbar burst fractures (TLBF). A number of operative techniques have been described with the absence of consensus that is more advantageous. The objective of this study was to compare the results of 3 different methods of operative treatment of TLBF: open pedicle screw instrumentation (OPSI), percutaneous pedicle screw instrumentation (PPSI), and percutaneous vertebral augmentation with Cranio-Caudal Expandable Implant SpineJack (PVASJ). Material and Methods: A total of 646 patients with thoracolumbar fractures were treated between 2014 and 2017, in 2 departments: orthopedics and neurosurgery of our centre. After exclusion of patients who did not match the inclusion criteria, a total of 154 patients who underwent: OPSI (n = 51), PPSI (n = 59), or PVASJ (n = 44) for the treatment of TLBF left for further analysis. Evaluations were performed before the surgery, immediately after surgery, 6 to 8 weeks postoperative and at the final follow-up (minimum 1-year postoperatively). For clinical evaluation, the intraoperative blood loss, operation time, radiation dose, postoperative hospital stays, the length of postoperative scar, and perioperative complications were analyzed. For the patient’s pain, functional evaluation and quality of life: visual analogue scale (VAS), Oswestry Disability Index (ODI), and Short Form (SF)-36 were evaluated. For radiologic parameters: regional kyphosis, vertebral wedge angle, and vertebral body height compression/reconstruction were evaluated. For statistical analysis Statistica version 16.0 was used. Results: There were significant differences between OPSI and both PPSI and PVASJ in perioperative outcomes and complications in favor of PPSI and PVASJ and with the best results for the last group. Postoperative VAS, ODI, and SF-36 outcomes improved in all groups, and there was a significant difference in favor of PPSI and PVASJ groups 6 to 8 weeks after the surgery and nonsignificant at the time of follow-up. The radiographic outcome significantly improved in each group immediately after the surgery and decreased significantly more for OPSI and PPSI than for PVASJ after 8 weeks and at the final follow-up. Conclusion: Although all 3 groups showed favorable outcomes at the final follow-up, both minimally invasive but especially PVASJ provided earlier and better pain relief, better functional improvement, and less perioperative complications. PVASJ also provided a stronger support for the anterior and middle column of the fractured vertebral body and prevented kyphotic deformity better than both pedicle screw instrumentations.
Tumor
P659: Minimally Invasive Local Treatment of Metastatic Spine Disease: Experience and Results
Sergey Lyulin1, Pavel Balaev1, and Sergey Alexeev1
1Ilizarov Center of Orthopaedics, Kurgan, Russian Federation
Introduction: There is no definite understanding in tactics and results of local treatment of spine metastasis. The evaluation of the effectiveness of minimally invasive surgical treatment of metastatic spine disease was the main purpose of this study. Material and Methods: The analysis of surgical treatment of 48 patients with metastatic spine disease was performed. The main indications for surgery were the presence of an unstable fracture, spinal cord compression, severe pain syndrome, an expecting survival period of 8 month or more. All patients underwent minimally invasive spine stabilization with transpedicular systems followed by endoscopic spinal cord decompression, vertebrectomy with implant defect replacement. Surgeries were done in one session consequentially. During the thoracoscopic session, we used 2 systems of visualization, 2-dimensional (D) and 3D, to compare the difference. The special form filled by surgeon after the surgery to estimate the quality of visualization and decompression after using 2D and 3D. Radiography, CT (computed tomography), MRI (magnetic resonance imaging), pathomorphological studies, VAS (visual analogue scale), Tokuhashi, Karnovsky, Short Form (SF)-36, Frankel scales, and comparable evaluation of 2D versus 3D imagination were used for evaluation. Results: Patients were monitored after discharge from the hospital at 1, 3, 6, and 12 months, followed by a recommendation for annual treatment. There was a decrease in the severity of pain in all patients, partial (60%) or complete (40%) regression of neurological deficit. We found out the difference between 2D and 3D visualization in favor of 3D in quality of decompression and complete removal tumor tissues. According to SF-36, we found out the increase of quality of life in almost all patients (96%) after the treatment. We found out the increase of life expectancy after the local treatment according to our preoperative (Tokuhashi index) prognosis. Conclusion: Minimally invasive local treatment of metastatic spine disease decreases neurological complications, pain syndrome and increase quality of life, and life expectancy. Three dimensional visualization is in favor for quality of decompression and tumor removal.
P660: Telangiectatic Osteosarcoma of the Cervical Spine: A Rare Tumor Presenting as Cervical Spine Dislocation
Sajeev Suraj1 and Krishnakumar R1
1Lakeshore Hospital and Research Centre, Kochi, India
Introduction: Telangiectatic osteosarcoma is one of the 8 subtypes of osteosarcoma. It is characterized by multiple, aneurysmally dilated, blood-filled cavities with high-grade, sacromatous cells in the peripheral rim, and septae. Fifteen cases have been described in the spine and only 3 cases have been described in the cervical spine. We present a case of telangiectatic osteosarcoma of the cervical spine presenting with dislocation causing dense myelopathy. Material and Methods: This is a case report pertaining to a 6-year-old girl with a history of unsteady gait and recurrent falls over a period of 6 months. She developed severe neck pain, dense paraplegia, and sphincter paralysis. Complete upper motor neuron type of motor paralysis (Frenkel grade A paraplegia) was noted in the chest and abdominal wall and bilateral lower limbs. Computed tomography (CT) imaging of the cervical spine showed destruction and collapse of the C7 body with grade 3 C7-T1 spondylolisthesis and an expansive lytic lesion of the posterior elements. MRI (magnetic resonance imaging) with contrast showed an expansile lytic lesion of the C7 spinous process, bilateral laminae, left transverse process, and left pedicle with heterogeneous enhancement. The tumor was not invading any surrounding neurovascular structures. Severe canal stenosis and cord edema was noted from C6-T1. Effacement of bilateral neural foraminae at C6-C7 and C7-T1 was noted. A CT-guided biopsy of the lesion yielded only blood. A 2-stage piece meal spondylectomy of C7 vertebra was performed. The tumor was first approached posteriorly and the tumor was found to be approximately 6 × 5 × 4 cm with no posterior cortical breaches. Curettage was carried out along with all posterior elements. Despite lack of preoperative embolization, there was very little hemorrhage intraoperatively. Bilateral facetectomies of C6-C7 and C7-T1 were completed. Posterior stabilization was achieved with C4-C5 lateral mass screws and T2-T3 pedicle screws with rod instrumentation. The tumor was then approached anteriorly and decompression of the cord was achieved by corpectomies of C7 and T1 followed by stabilization with a nonvascularized fibular strut graft and plating. The tumor was predominantly posterior and little tissue was obtained anteriorly. Postoperative X-ray and CT demonstrated excellent reduction, alignment, and decompression. She developed no complications and was supported with a hard cervical collar for 6 weeks. She was given chemotherapy with the IAP triplet regimen of doxorubicin, cisplatin, and ifosfamide in 6 cycles and radiation to the cervical spine. Results: Patient tolerated the treatment well. Histopathological examination was consistent with telangiectatic osteosarcoma, with MDM2 positivity, and CDK 4 nuclear positivity. At 1-year post operation, she had improved to Frenkel grade C with grade 3 power of bilateral knee extensors and ankle dorsiflexors. Bone scan showed no metastases or recurrence of disease. Conclusion: The current case study shows a 6-year-old girl with a telangiectatic osteosarcoma of the C7 vertebra with Frenkel grade A paraplegia treated successfully at 1 year with staged piece meal spondylectomy and C6-T1 anterior and posterior fusion and adjuvant chemoradiation.
P661: Is Anterior Column Support Needed Following Transpedicular Decompression for Metastatic or Infectious Epidural Compression
Eric Emanski1, Avionna Baldwin1, Addisu Mesfin1, and Robert Molinari1
1University of Rochester, Rochester, NY, USA
Introduction: When combined with longer posterior instrumentation, transpedicular partial corpectomy without anterior structural grafting may be an appropriate treatment option for patients with spinal osteomyelitis or metastatic disease. This limited procedure does not involve the placement of an anterior structural graft through a posterior approach and may result in lower patient perioperative morbidity and complication rates. Material and Methods: During the period of 2010 to 2017, 34 consecutive patients with osteomyelitis or metastatic tumor were treated by the same surgeon (RWM) with transpedicular partial corpectomy decompression and longer posterior spinal fusion (PSF) without anterior structural grafting. All patients had multiple medical comorbidities. A retrospective chart review was performed. The ASIA (American Spinal Injury Association) Impairment score was calculated for all patients both preoperatively and postoperatively. Operative times, blood loss, length of hospital stay, major, and minor complications were recorded for all patients. Results: There were 24 male and 10 female patients with an average age of 66 years (range 46-83). Fourteen of the patients had osteomyelitis and 20 had metastatic tumor of the spinal column. The patients had an average of 2.5 major comorbidities (range 1-7). Mean operative time was 149.8 minutes (range 60-275 minutes). Average number of levels instrumented was 4.9, range of 2 to 8. Estimated blood loss (EBL) for the procedures averaged 786.8 mL (range 200-2500 mL). Hospital stay length prior discharge home or a rehabilitation facility averaged 18.2 days (range 3-61 days). Fifteen of the 34 patients were discharged to a rehabilitation facility where they spent an average of 7.5 days. ASIA impairment scores were noted to improve or remained constant in all patients. Medical follow-up of the patients averaged 437.2 days (range 13-2080) and mean radiographic follow averaged 324.3 days (range 0-1360). The 30-day hospital readmission rate was 8.8% (3/34), 2 patients were readmitted for wound issues, and 1 was readmitted for a clinical trial for their cancer. Five patients died postoperatively from medical complications of their disease. Major medical complications occurred in 9 of the 34 patients (26.5%) and there was postoperative procedure related major complications in 7 of 34 patients (20.6%). Five of 34 patients (14.7%) required a return to the operating room for procedure-related complication. Three patients had infection requiring wound I&D (incision and drainage) and 2 patients required revision of loosened posterior instrumentation. There were no cases of catastrophic instrumentation failure. Conclusion: Transpedicular partial corpectomy decompression and longer PSF without anterior structural grafting demonstrates low operative times, EBL, and instrumentation complications with improved or stable postoperative neurologic function. Morbidity remain high in this critically ill subset of patients. This limited procedure should be considered as a treatment option for debilitated patients with spinal disease and neurologic impairment.
P662: Intradural Extramedullary Tumor of Spinal Cord
Pashupati Chaudhary1, Rosan Kalawar1, Bishnu Pokharel1, and Pricha Upadhaya1
1B. P. Koirala Institute of Health Sciences, Dharan, Nepal
Introduction: Intradural or primary spinal cord tumors (neoplasms) are uncommon lesions and fortunately affect only a minority of the population. However, when lesions grow, they result in compression of the spinal cord, which can cause limb dysfunction, motor and sensation loss, and, possibly, lead to death. The most common presenting symptoms include weakness, back pain and radicular pain. Aim and Objective: To evaluate and management of intradural intramedullary spinal cord tumors presented to the Department of Orthopaedics, BPKIHS, Dharan. Material and Methods: This is a retrospective interventional study done over a period of 4 years from March 2010 to April 2014. A total of 5 patients with intradural extramedullary tumor were operated. The patients’ age ranged from 20 to 50 years, and the mean follow-up was 12 weeks. All patients improved neurologically and functionally after surgery. Results: The study comprised 5 patients with intradural extramedullary tumor of the spina cord. The age incidence in this series ranted from 20 to 50 years. Four patients were male and 1 was female. Three tumors were in the lumbar region, and 2 tumors were in the dorsal region. Conclusion: Patients with intramedullary extramedullary spinal cord tumors (ie, ependymomas, astrocytomas) typically present with back pain referred from the level of the lesion, sensory changes, or worsening function. Optimal treatment options depend on the patient’s clinical symptoms and neurologic finding. However, cures have been reported only after complete surgical resection. Intradural or primary spinal cord tumors (neoplasm) are uncommon lesions and fortunately affect only a minority of the population. Patients with neurologic symptoms and confirmatory findings from imaging studies benefit most from surgical excision, with the surgical goal of total gross resection of the lesion.
P663: A 10-Year, Single-Center Evaluation of Outcomes of Vertebrectomy for Malignancy
Sophia Roser1, Richard Ferch1, Monish Maharaj1, Michael Taylor1, and Mitchell Hansen1
1John Hunter Hospital, Newcastle, UK
Introduction: The consequences of metastatic epidural spinal cord compression are devastating with implications for patient survival, quality of life, and cost to the health care system. Circumferential decompression of the neural elements in vertebral malignancy has been demonstrated to provide superior outcomes compared with radiotherapy but the means by which this should occur is less clear. There are several indications to perform vertebrectomy including acute or impending spinal cord compression, instability, or pain. However, there is often a reluctance to perform aggressive interventions on patients with metastatic cancer, with concern about their ability to tolerate the procedure and the futility of performing cost-intensive procedures on patients with reduced life expectancies. To gain a better understanding of the outcomes and overall survival of patients undergoing vertebrectomy, we performed a retrospective review of all patients who underwent a vertebrectomy for metastatic disease at our unit between 2006 and 2016. Materials and Methods: Medical records were reviewed and the following data were extracted: demographics; primary malignancy; presenting symptoms; preoperative chemo- or radiotherapy; Spinal Instability Neoplastic Score; preoperative and postoperative neurological function; operative approach; operative time; blood loss; need for transfusion; complications; overall survival; discharge destination; delayed neurological deterioration, and construct failure. Results: A total of 141 vertebrectomies were performed on 137 patients over the 10-year period. Forty-two patients were alive at the time of review with a mean survival of 464 days. Four patients died during their admission. Twenty-nine patients were nonambulatory on presentation. Of these 18 (62%), regained ambulatory function in the postoperative period. Five patients suffered a neurological deterioration following surgery, with 4 of these losing their ambulatory function. Overall, 96.5% of patients either had a preservation or improvement of their neurological function postoperatively. The complication rate was 34% with the most common complication being wound infection or dehiscence requiring revision. Mean operative time was 240 minutes and mean blood loss was 1.5 L. Eight patients had preoperative embolization and had a higher mean blood loss of 2.5 L. The average length of stay was 13 days, and 26 patients required admission to the intensive care unit. Our data were also analyzed by age, ambulatory status, and malignancy type. Assessing our cohort by age, we demonstrated no significant difference with regard to complications or inpatient mortality in patients over 65 or over 70 years. Similarly, there was no difference between neurological outcomes or overall survival. We also assessed the cohort based on postoperative neurological outcomes. We demonstrated that patients who are nonambulatory have higher complication rates and significantly lower overall survival. Conclusion: Vertebrectomy is an aggressive and cost-intensive procedure, but we have demonstrated a satisfactory complication rate and an overall survival that is longer than what is frequently cited in this cohort. We failed to demonstrate a difference with regard to complication rates, neurological function, or survival in the older patient cohort as has been previously reported in the literature. We confirmed the devastating implications of becoming nonambulatory, with significantly higher postoperative complication rates and lower overall survival.
P664: Clinico-Radiological Outcome of Denosumab Therapy in Axial Giant Cell Tumor’s (Campanacci Grades 2 and 3)
Rohan Gala1, Saumyajit Basu1, and Amitava Biswas1
1Park Clinic, Kolkata, India
Introduction: Axial giant cell tumors are particularly challenging to treat especially when they are either inoperable, or their complete resection is difficult due to the proximity of vital structures. Denosumab has been quite useful downstaging all those cases that were deemed inoperable or those with disease requiring morbid surgery by not only halting their further extension but also causing shrinkage of the tumor and also by providing a scaffold for the surgeon (ossification or sclerotic rim) Hereby presenting 3 cases managed with denosumab therapy prior to surgery. Material and Methods: The first case was a 16-year-old girl diagnosed of a large sacral giant cell tumor (GCT; Grade II), presented with bilateral S1 radiculopathy. The second case was a 38-year-old female who was diagnosed with odontoid GCT (Grade II) extending into the C1/C2 joint with early signs of myelopathy. The last case was a 37-year-old male who was diagnosed of dorsal GCT involving (D6 Grade III), presented with spastic paraparesis. Each of them received a monthly injection of denosumab for a minimum of 6 months and underwent radiological investigations initially prior to commencement of therapy and at 6 months of therapy. Results: All patients experienced a significant decrease in pain with improvement in VAS (visual analogue scale) scale and concomitant improvement in function to some extent at 6 months of denosumab therapy. Radiological improvement was also evident, not only halting the growth of the lesion but also causing peripheral calcification/ossification and sclerosis and definitive downstaging the tumor in one patient. Conclusion: Denosumab therapy in axial GCTs that are either large or at challenging anatomical locations is beneficial to halt or reduce the extensiveness of the tumor probably making unresectable tumors resectable. They probably also aid in reducing the morbidity of those surgeries, which already pose an increased risk due to the proximity of important neurovascular structures.
P665: Spinal Osteoid Osteoma: An Unusual Cause of Secondary Scoliosis
Aashish Ghodke1, Ram Chaddha2, Agnivesh Tikoo2, Harshal Bamb3, and Sagar Kelkar1
1Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry, Shropshire, UK
2Apollo Hospitals, Navi Mumbai, India
Introduction: Osteoid osteoma of the spine is a rare entity. It requires a high degree of suspicion to diagnose it clinically. A spine surgeon should be well aware of the fact that it can lead to secondary scoliosis, which can be the presenting complaint and hence can be misdiagnosed. A thorough clinical and radiological examination including computed tomography (CT) scan as well as magnetic resonance imaging (MRI) is essential to diagnose it. A meticulous surgical excision can relieve the patient of his pain and also will correct the secondary deformity. Case Report: We report a case of a 33-year-old man with thoracic deformity that was diagnosed with scoliosis and was being treated for the same at various hospitals. He was given an orthosis and analgesics for pain relief at all the centers and was also advised correction of the deformity if pain does not settle. He did not get any relief from the pain and was in constant discomfort. He then consulted us and we thoroughly examined him and did a CT scan along with an MRI. CT was suggestive of D9 thoracic osteoid osteoma. Surgical removal of the lesion resection was done and an intraoperative frozen pathology indicated features of osteoid osteoma. Immediately after the surgery patient was free of his discomforting pain, and on 3 months follow-up X-ray his deformity also got corrected. Results: Three months after the surgery, patient showed marked improvement of scoliosis deformity and complete relief of thoracic pain. Conclusion: Although spine osteoid osteoma is clinically rare, it shall not be overlooked when patients present with scoliosis first. Radiological examinations including CT and MRI shall be undertaken carefully as reference when making diagnosis. Surgical resection of the lesion could well improve scoliosis and relieve the pain.
P666: A Case Report of a Metastatic Gastrointestinal Stromal Tumor to the Vertebra
Yu Tung Lo1, David Siu Kei Mak1, and Colum Patrick Nolan1
1National Neuroscience Institute, Singapore, Singapore
Introduction: We report a case of a 63-year-old Chinese female with metastatic gastrointestinal stromal tumor to the vertebra who presented with a 1-week history of left leg weakness requiring assistance in ambulation. She was diagnosed with jejunal gastrointestinal stromal tumor (GIST) 5 years prior with subsequent disease progression to the liver, mesenteric lymph nodes, pelvis, and bladder. She underwent treatment with tyrosine kinase inhibitors (imatinib, sunitinib, regorafenib, and dasatinib). Physical examination on presentation revealed inability to lift left lower limb against gravity as well as sensory level at T10. Anal tone was preserved. A CT of thorax, abdomen, and pelvis obtained 1 month prior already revealed a T9 lytic lesion. Subsequent MRI whole spine revealed T9 enhancing lesion causing pathological fracture, with prominent extraosseous soft tissue component with cord compression causing cord edema at the T9 level, with adjacent dural enhancement spanning T8 to T10. T1-hypointense, T2-isointense, and STIR-hyperintense lesions were also noted at the L5 vertebral body and L1 spinous process, also suggestive of metastasis. Material and Methods: She underwent T9 decompressive laminectomy, tumor excision, and T7 to T11 instrumentation, followed by adjuvant radiotherapy to the spine and chemotherapy. The L1 and L5 vertebral metastatic lesions were managed conservatively. Results: Intraoperatively, the tumor appeared greyish, soft, friable, and vascular, with extradural component seen anterior to the cord. It also involved the left pedicle, which was excised. Tissue samples biopsied during surgery revealed lamellar bone fragments associated with nests and cords of epithelioid cells with moderate anisonucleosis and fair amounts of cytoplasm with gland-like spaces in some areas. Background myxoid features were noted. The tumor cells stained strongly positive for DOG-1 and weaker positivity for CD117. The stains were negative for S100 protein, HMB45, desmin, CD31, ERG, Cam5.2, and AE1/3. Features were consistent with a metastatic GIST. Following her surgery, she achieved a near-complete neurological recovery and was able to achieve independent ambulation without aid. She subsequently underwent inpatient rehabilitation and commenced on postoperative palliative radiotherapy of 30 Gy over 10 fractions to the spine. Conclusion: Metastatic GIST to the vertebra was rarely reported in the literature. Only one other case of surgically treated vertebral metastasis was reported in the literature, who similarly made an excellent neurological recovery. In the presence of unstable vertebral disease, surgical excision, and instrumented fusion confers a favorable neurological outcome.
P667: Neurological Outcomes After Surgical Treatment of Primary Intramedullary Spinal Cord Tumors in Pregnancy
Vadim Byvaltsev1, Serik Akshulakov2, Talgat Kerimbaev1, and Ivan Stepanov1
1Irkutsk State Medical University, Irkutsk, Russian Federation
2National Center of Neurosurgery, Astana, Kazakhstan
Introduction: Primary intramedullary spinal cord tumors (IMSCTs) can lead to severe neurological complications and even death. Pregnant women often complain of discomfort of the lower limbs, which is usually caused by sciatica. The purpose of our study was to evaluate the recent neurological outcomes after surgical treatment of IMSCTs in pregnant patients. Materials and Methods: We retrospectively reviewed 14 pregnant patients who underwent surgical treatment for IMSCT between 2004 and 2018. Patient’s age, histological origin and grade, tumor location, tumor extension, preoperative neurological state, initial presenting symptom, and extend of tumor resection were analyzed to evaluate predictive factors that affect postoperative functional outcome. Results: The neurological states at last follow-up were improved in 11 patients (78.5%), unchanged in 2 (14.3%), and aggravated in 6 (7.2%). In all patients, the functional outcomes were good in 12 patients (85.8%), fair in 1 (7.1%), and poor in 1 (7.1%). Preoperative good neurological state was the strongest positive predictor of good functional outcome (P < .05). In tumor location, functional outcomes of thoracic tumors were poor than those in cervical and conus medullaris region (P = .044). High-grade tumor shows poor outcome compare with low-grade tumor (P = .028). Conclusion: The most reliable predicting factor of outcome after surgical treatment of IMSCTs in pregnant patients was the preoperative neurological state. In addition, IMSCTs in thoracic region and high-grade tumor showed relatively bad outcome and had a risk of postoperative morbidity.
P668: Hypervascular Metastatic Spine Tumors Are Not Angiographically Associated With the Artery of Adamkiewicz or Other Radiculomedullary Arteries
Erick Westbroek1, A. Karim Ahmed1, Zach Pennington1, Matthew Goodwin1, Yuanxuan Xia1, Philippe Gailloud1, and Daniel Sciubba1
1Johns Hopkins University, Baltimore, MD, USA
Background: Preoperative endovascular embolization of hypervascular metastatic spine tumors can reduce intraoperative blood loss. One frequent objection to embolizing these tumors is the concern for associated large arteries feeding the spinal cord, such as the artery of Adamkiewicz. This study aimed to elucidate a relationship between spinal levels affected by hypervascular spine metastases and associated radiculomedullary arteries. Methods: Retrospective review of 46 patients undergoing preoperative endovascular embolization of hypervascular metastatic spine tumors. A total 484 spinal levels were evaluated by diagnostic spinal angiography during embolization procedures. Each spinal level was categorized based on presence or absence of tumor and radiculomedullary artery. Results: No statistically significant associations were found. Relative risk of affected spinal levels having an associated radiculomedullary artery was 1.10 (95% confidence interval [CI] 0.66-1.85). Attributable risk was 0.01 (−0.01 to 0.02). Chi-squared statistic was 0.13, with P value of .71. Subgroup analysis in renal cell patients was also statistically insignificant, with a relative risk of 0.97 (95% CI 0.43-2.16), χ2 statistic 0.01, P = .94. Conclusions: In this study, no association was found between spinal levels affected by hypervascular metastatic spine tumors and radiculomedullary arteries feeding the spinal cord by diagnostic spinal angiography. Thus, while iatrogenic spinal cord stroke is a feared complication of any spinal embolization procedure, no additional risk is attributable to hypervascular metastases.
P669: Atypical Hemangiomas of the Spine Are Angiographically Associated With Radiculomedullary Arteries
Erick Westbroek1, A. Karim Ahmed1, Zach Pennington1, Matthew Goodwin1, Yuanxuan Xia1, Philippe Gailloud1, and Daniel Sciubba1
1 Johns Hopkins University, Baltimore, MD, USA
Background: Preoperative endovascular embolization of atypical hemangiomas of the spine can reduce intraoperative blood loss. One frequent concern raised about embolizing these masses is a possible association with large arteries feeding the spinal cord, such as the artery of Adamkiewicz. This study aimed to elucidate a relationship between spinal levels affected by atypical spinal hemangiomas and associated radiculomedullary arteries. Methods: Retrospective review of 8 patients undergoing preoperative endovascular embolization of atypical spinal hemangiomas. Fifty-four spinal levels were evaluated by diagnostic spinal angiography during embolization procedures. Each spinal level was categorized based on presence or absence of tumor and radiculomedullary artery. Results: Five of 15 (33.3%) of affected levels had an associated radiculomedullary artery. Four of 39 (10.2%) unaffected levels had an associated cord feeding artery. Relative risk of affected spinal levels having an associated radiculomedullary artery was 3.25 (95% CI [confidence interval] 1.01-10.49). Attributable risk was 0.23 (0.07-0.51). Chi-squared statistic was 4.15, with P value of .04. Conclusions: In this study, spinal levels affected by atypical hemangiomas requiring surgery were associated with radiculomedullary arteries feeding the spinal cord by diagnostic spinal angiography. When performing preoperative embolizations, great care must be taken to identify and preserve arteries supplying the spinal cord.
P670: The Surgical Treatment of Cervical Spinal Tumors
Tao Fan1, Guosong Shang2, Cong Liang1, and YinQian Wang1
1Sanbo Brain Hospital Capital Medical University, Beijing, China
2Linfen People’s Hospital Shanxi Medical University, Linfen, China
Introduction: Surgical treatment strategy for cervical spinal tumors such as extramedullary tumors, intramedullary tumors, and intra-extra spinal tumors. Materials and Methods: From March 2008 to March 2016, we operated on 335 cases of cervical spinal tumors (male/female = 1:1, average age: 40.5 years), among which extramedullary tumors are 117 cases, intramedullary tumors are 130 cases, and intra-extra spinal tumors are 88 cases. Multiple surgical approaches such as hemilaminectomy approach, laminectomy, laminotomy, and paramedian approach were used to resection of different types of cervical tumors. The cervical stability was evaluated before and after resection of the cervical spinal tumors. Results: All begin extramedullary tumors could be totally removed without any complications and severe neurologic dysfunction. Such intramedullary tumors as ependymoma, angioblastoma, and cavernoma could be totally removed without postoperative radiotherapy. We performed subtotal or partial remove on intramedullary astrocytomas according to intraoperative frozen biopsy and intraoperative monitoring of spinal cord-evoked potentials. Laminectomy and duraplasty for decompression were performed at the same time. Postoperative radiotherapy and/or chemotherapy were suggested and tailored to each patient. Surgical related mortality in our cervical intramedullary tumor group is 2.3% (3/130). Approximately 28.2% of the patients need spine instruments to keep the cervical stability. Conclusions: The prognosis of cervical spinal tumor is strictly correlated with the pathologic character of the tumor, preoperative neurologic function of the patient, and resection extend of the tumor. Cervical stability should be evaluated before and after resection of the tumor and spine instruments is important to correct spine deformity combined with spinal tumors.
P671: Imaging-Based Outcomes for Cervical and Sacral Metastases Treated With Stereotactic Body Radiotherapy
Sten Myrehaug1, Liang Zeng1, Hany Soliman1, Chia-Lin Tseng1, Mark Ruschin1, Young Lee1, and Arjun Sahgal1
1University of Toronto, Toronto, Ontario, Canada
Introduction: Vertebral bodies are a common site of metastatic spread. The unique anatomy and biomechanics of the cervical spine and sacrum affect outcomes following stereotactic body radiation therapy (SBRT). Current data for spine SBRT are not specific for these locations. Material and Methods: Retrospective review of prospective spine SBRT database revealed 52 patients with 93 spinal segments treated in the cervical spine or sacrum. All patients were followed clinically and with full spine MRI (magnetic resonance imaging) at 2- to 3-month intervals. Results: Fifty-six targets were treated in the cervical spine and 37 within the sacrum. Median follow-up was 14.4 and 19.5 months, respectively. Median total dose/fraction was 24Gy/2 for both sites. Local control at 1 and 2 years were 94.5% and 92.7% in the cervical cohort and 86.5% and 78.7% in the sacral cohort. Median overall survival was 16.3 and 28.5 months, respectively. Two cases of sacral vertebral body compression fracture, 1 brachial plexopathy, and 1 lumbar-sacral plexopathy were observed. Conclusion: High rates of local control are seen for targets treated in both the cervical spine and sacrum. Given the vertebral body compression fracture seen in the sacral cohort, strategies specific to the sacrum require further refinement.
P672: Analysis of the Results of a Full 1-Stage Segmental Resection From the Posterior Transpedicular Approach With 360° Stabilization in the Treatment of Patients With Spinal Tumors
Y. Kenzhegulov1, Zh. Tuigynov1, Y. Urunbaev1, V. Aleinikov1, T. Kerimbayev1, and V. Byvaltsev2
1National Center of Neurosurgery, Astana, Kazakhstan
2Irkutsk State Medical University, Irkutsk, Russian Federation
Introduction: Analyze the results of complete 1-stage segmental resection from the posterior transpedicular approach with 360° stabilization in the treatment of patients with tumors of the spinal cord. Materials and Methods: We conducted a retrospective analysis of the history of the disease and the observation of 69 patients with primary malignant and benign aggressive and secondary (metastatic) tumors operated according to the proposed method of surgical treatment. Evaluation of neurological disorders was carried out according to the Frenkel/American Spinal Injury Association (ASIA) scale, the Karnovsky’s quality of life assessment, and the evaluation of the Enneking WF tumor distribution, Tomita K. Observation period from 6 months to 60 months, an average of 27 months. Results: Analysis of the results of surgical treatment of 69 patients (47 women, 22 men) showed that the first 6 months of observation, improvement in the quality of life on the Karnovsky scale was noted in 86.9%—60 patients. During the early follow-up period (6 months), 59 patients showed improvement in neurological status, of which 3 (4.3%) patients had complete neurologic recovery from group A to D, 22 (31%) patients who switched from group B to group C, and 34 (49.3%) patients who switched from group C to group D, according to the Frenkel/ASIA scale. There were 10 patients (14.5%) without changing the neurological status. Repeated operations were associated with complications and repeated growth of the tumor. Two cases are associated with complications in the form of kyphotic deformation (1% to 1.4%) of the thoracic spine and inflammation of the postoperative wound (1% to 1.4%). Repeated operations associated with repeated tumor growth were noted in 3 (4.3%) patients. The total number of deaths during follow-up was 15 (21.7%) patients. Thirteen (18.8%) patients died because of metastases that were not directly related to the operation itself for 5 months to 2.5 years. Two (2.9%) patients died of thromboembolic complications (PE [pulmonary embolism], stroke by ischemic type). Conclusion: Our experience shows the importance of total removal of the entire segment of the spine along with the tumor. The method of total spondylectomy allows ensuring resection of the tumor radically, with a low percentage of relapses, preservation of the function of the spinal cord, and improvement patient’s quality of life. In cases with metastatic tumors, the type of primary tumor and the ASIA score were significant prognostic factors for survival.
P673: The Surgical Management of Giant-Invasive Spinal Schwannomas: Experience Over 15 Years From a Single Tertiary Spinal Referral Centre
Jamie R. F. Wilson1, Pratipal Kalsi1, Fan Jiang1, Jessica P. Bauer1, Anick Nater1, Nardin Samuel1, Francois Mathieu1, Suganth Suppiah1, Jetan H. Badhiwala1, Gelareh Zadeh1, Eric M. Massicotte1, and Michael Fehlings1
1Toronto Western Hospital, Toronto, Ontario Canada
Introduction: Spinal schwannomas are the most common primary spinal tumor. These lesions are usually benign, slow growing, and become symptomatic when compression of the neural elements occurs. A rare, poorly understood subtype of these lesions, referred to as “giant invasive” schwannomas (GIS), are characterized by bony erosion and invasion through myofascial planes, and pose distinct surgical challenges. Given the rarity of GIS and the lack of evidence-based management approaches, we sought to report the presentation, treatment approaches, and outcomes in a series from a large, tertiary spine oncology referral center. Material and Methods: An analysis of a prospectively collected series of patients with a histopathological diagnosis of spinal schwannoma was performed from 2003 to 2018 at a single tertiary spinal referral center. Electronic records, imaging studies, operative notes, and follow-up data were examined to compare the clinical features between patients with GIS and those with non-GIS using χ2 and univariable logistic regression. Results: A total of 82 patients underwent surgical resection of a spinal schwannoma. Based on imaging criteria, 15 patients were judged to have “giant invasive” schwannomas (type IV or V on the Sridhar scale). The majority of patients presented with back or radicular pain, but the GIS group had a higher rate of urinary dysfunction compared with the noninvasive group (odds ratio [OR] = 4.29 [95% CI (confidence interval): 1.14-16.20]; P = .023). The mean largest diameter of tumor at presentation in the GIS group was 5.87 [±1.4] cm. The likelihood of achieving a subtotal excision was similar in the GIS group (OR = 0.99 [0.19-5.13]; P = .99), but the GIS group had a significantly higher rate of instrumented fixation compared with the noninvasive group (n = 13; 87% vs n = 17; 34%, P ≤ .0001). Only one patient in the GIS group (7%) required a second operation within 30 days (for CSF [cerebrospinal fluid] leak), compared with 0 patients in the noninvasive group. There was no radiological recurrence in the GIS group (mean follow up: 53.8 [±11.6] months), compared with a recurrence rate of 9% (n = 6) in the noninvasive group (mean follow up: 42.3 [±8.7] months). Two patients required revision surgery after radiological recurrence in the noninvasive group at 3 years and 8 years after index surgery. Conclusion: Giant invasive spinal schwannomas are a rare clinical entity, which have a higher rate of urinary dysfunction at presentation. These lesions can be successfully managed with microsurgical resection, which mandates instrumented reconstruction in most cases.
P674: Spinal Instability Neoplastic Score Is Reliable and Predicts Spinal Adverse Events
Aidin Abedi1, Jeffrey Wang1, and Zorica Buser1
1University of Southern California, Los Angeles, CA, USA
Introduction: Spinal metastasis is a common presentation of advanced cancer. Stability is a major factor in the decision-making process for patients with metastatic spinal tumors, and in combination with patient-specific medical factors, is the key determinant of the need for surgery. The Spinal Neoplastic Severity Score (SINS) is 1 of the 4 fundamental assessments in the NOMS (neurologic, oncologic, mechanical, and systemic) framework, which is a dynamic scheme for multidisciplinary decision-making in spinal metastasis. This systematic review evaluates the evidence on measurement properties of SINS and its predictive value in patients with primary and metastatic spinal neoplasms. Material and Methods: A systematic literature review was performed using PubMed, CINAHL, Medline, Scopus, Web of Science, and Embase databases in May 2017 to identify the studies on reliability, validity, and predictive value of the SINS in primary and metastatic spinal tumors. The primary end point for predictive studies was defined as occurrence of any relevant spinal adverse event, such as vertebral compression fracture, instability, and need for surgical treatment. The COSMIN Risk of Bias checklist was used for critical appraisal of the quality of the included studies, and a modified GRADE approach was used for appraisal of the overall quality of evidence (QoE). Studies on measurement properties were summarized qualitatively. Predictive studies were pooled and meta-analysis was performed using the generic inverse variance method with a random effects model. Results: After screening for the eligibility criteria, 22 articles were included in the final review. The total SINS score had sufficient intraobserver and interobserver reliability in multiple studies (QoE, high, and moderate, respectively). The ternary SINS categorical score showed insufficient reliability. However, the binary scoring version proved to be promising. Four studies were included in the meta-analysis, resulting in a total of 535 patients. The patient population consisted of a variety of primary and secondary tumors, reflecting the high generalizability of the results of this meta-analysis. High SINS score was significantly associated with spinal adverse events (OR [odds ratio] = 5.48, 95% CI [confidence interval]: 3.26-9.21, P < .00001). Conclusion: Our initial findings confirm the reliability of the overall SINS score, and its predictive value for spinal adverse events in patients with primary or metastatic spinal neoplasms. The binary categorization of SINS improves the reliability of this measure and seems to be more practical than the ternary method. Further evidence is needed to confirm the merit of SINS as a stand-alone measure for surgical decision-making by the spine surgeons. However, current evidence permits to conclude that SINS can help the oncologists determine which patients need referrals to spine surgeons. Cost-effectiveness of this approach and the concordance of the recommendations based on SINS with spine surgeons’ treatment plan should be investigated in future studies.
P675: Intraoperative Neuromonitoring: Is There a Role in Metastatic Spine Tumor Surgery?
Naresh Kumar1, G. Vijayaraghavan1, Nivetha Ravikumar1, Yan Ding1, May Lin Yin1, Ravish Patel1, Nandika Naresh2, Hwee Weng Dennis Hey1, Leok-Lim Lau1, and Gabriel Liu1
1National University Hospital, Singapore, Singapore
2Newcastle University, Newcastle upon Tyne, UK
Introduction: Multimodal intraoperative neuromonitoring (IONM) is considered as standard of care in spinal deformity surgeries. However, limited data exist about its role in metastatic spine tumor surgery (MSTS). We aim to report our experience with multimodal IONM in MSTS. Methods: A total of 135 patients from 2010 to 2017, who underwent MSTS with IONM at our institute were studied retrospectively. After excluding 7 with no baseline signals, 128 patients were analyzed. The data collected composed of demographics, preoperative and postoperative ASIA grades and neurological status, indications for surgery, and type of surgical approach. Multimodal IONM included somatosensory-evoked potentials (SSEP), transcranial electric motor evoked potentials (tcMEP), and free running electromyography (EMG). The 128 patients included 61 males and 67 females with mean age of 61 years. A total of 116 underwent posterior procedures; 9 anterior and 3 both. The frequency of preoperative the American Spinal Injury Association (ASIA) Grades were A = 0, B = 0, C = 10, D = 44, and E = 74 patients. In total, 54 underwent MSTS for neurological deficit, 66 for instability pain, and 8 for intractable pain. Of 128 patients, 13 (10.2%) had significant IONM alerts, representing true positives; 114 true negatives, 1 false negative, and no false positives. Among the 13 true positives, 4 (30%) underwent minimally invasive technique and 9 (70%) open procedures. Eight (69.2%) patients had posterior approach. Seven (53.84%) true positive alerts were during decompression, which resolved to baseline on completion of decompression; while 5 (38.46%) were during instrumentation, which recovered to baseline after adjusting/downsizing the instrumentation; and 1 (8.3%) during lateral approach, which reversed after changing the plane of dissection. Of the 7 patients without baseline, 5 were ASIA-A, 2 were ASIA-C. The sensitivity, specificity, positive, and negative predictive values were 99.1%, 100%, 100%, and 92.9%, respectively. Conclusions: Multimodal IONM in MSTS helped in preventing postoperative neurological deficit in 9.4% of patients. The high sensitivity and specificity of multimodal IONM in detecting intraoperative neurological events, envisage its use in ASIA-grade D/E patients requiring instrumented decompression.
P676: Symptomatic Construct Failure After Metastatic Spine Tumor Surgery
Naresh Kumar1, Ravish Patel1, Dhiraj Sonawane1, Anshuja Charvi Wadhwa2, Aditya Singla1, Helena Milavec1, John Nathaniel Ruiz1, Hwee Weng Dennis Hey1, and Hee Kit Wong1
1National University Hospital, Singapore, Singapore
2Khoo Teck Puat Hospital, Singapore, Singapore
Introduction: There is paucity of literature evidence on the incidence and risk factors of symptomatic construct failures (SCF) following metastatic spine tumor surgery (MSTS). It is also unknown whether all SCF result in revision surgery. We aimed to evaluate the incidence and presentation of SCF after MSTS, as well as to identify the associated risk factors. We also intended to categorize SCF based on the treatment modalities by which these patients were managed. Methods: A total of 246 who underwent MSTS between 2005 and 2015 were evaluated retrospectively after applying exclusion criteria. Demographic data, perioperative, and postoperative clinical and radiological features were included. Radiological criteria for failures were defined. Early SCF included patients presenting within 3 months from index surgery, while late SCF included patients presenting after 3 months. Results: A total of 14 failures (5.7%) were recorded in 246 patients and 10 patients underwent revision (4.1%). The median survival of the whole cohort was 13.4 months (range: 1-127 months). The mean age was 58.8 years (range: 21-87 years) and 48.4% were female. The median time to failure was 5 months (range: 1-60 months). Three groups of SCF were the following: (a) Where primary implant was revised—5 (35.7%) patients, (b) peri-construct progression of disease requiring extension—5 (35.7%) patients, and (c) the ones that did not have revision—4 (28.5%) patients. Four (28.5%) patients presented as early failures, while 10 (71.5%) patients presented late. SCF commonly occurred at implant-bone interface (9/14) and these patients had Spinal Instability Neoplastic Score (SINS) >7. Thirteen (92.8%) patients developing failure had fixation spanning junctional regions. Multivariate competing risk regression showed preoperative Eastern Cooperative Oncology Group (ECOG) score as a significant risk factor for implant failure (adjusted sub [HR (hazard ratio)] 7.0, 95% CI (confidence interval) 1.63-30.07, P < .0009). Conclusions: The incidence of SCF (5.7%) was low in patients undergoing MSTS. Preoperatively ambulant patients had 7 times higher risk of failure than the nonambulant patients. Lower preoperative ECOG, preoperative SINS >7, and fixations spanning junctional regions were associated with SCF. Majority of construct failures occurred at implant-bone interface.
P677: The Clinical Utility of the Spinal Instability Neoplastic Score System in Spinal Epidural Metastases: A Retrospective Study
Ayoub Dakson1, Erika Leck1, David Brandman1, and Sean Christie1
1Dalhousie University, Halifax, Canada
Introduction: Metastatic destruction of integral spinal elements increases the risk of instability, pain, and neurologic deficits. The Spinal Instability Neoplastic Score (SINS) is used to assess mechanical instability due to spinal epidural metastasis based on radiographic and clinical factors. This study aims to assess the relationship between the SINS and prognosis, the degree of epidural spinal cord compression (ESCC) and neurologic status as well as describe the natural history of spinal metastases and instability as defined by SINS. Materials and methods: We allocated 285 patients with spinal metastatic disease using an oncology database. Survival and disease data were extracted through a retrospective review. SINS was calculated using CT (computed tomography) imaging. The degree of ESCC was assessed based on MRI (magnetic resonance imaging). Results: The study population was subdivided into stable (35%), potentially unstable (52%), and unstable (13%) groups. The overall incidence of metastatic spinal deformity was 9%. Surgical interventions were performed in 21% of patients, including decompression and instrumented fusion (70%), decompression alone (17%), percutaneous vertebral augmentation (9%), and instrumented vertebral augmentation (5%). The use of spinal instrumentation was significantly associated with unstable SINS (P = .005). Grade 3 ESCC was also significantly associated with unstable SINS (P < .001). Kaplan-Meier analysis revealed that SINS is independent of survival post spinal metastasis (P = .98). In the radiotherapy-alone group, a significant proportion of patients with potentially unstable SINS (30%) progressed into unstable SINS category at an average 364 ± 244 days (P < .001). Multivariate analysis demonstrated that unstable SINS category predicts grade 2 or 3 ESCC (P < .05). Conclusion: SINS is associated with different patterns of surgical interventions in the treatment of metastatic spinal disease, with more instrumented cases bearing unstable SINS. While SINS is separate from the prognosis, it predicts the degree of ESCC and is important in surveillance tool of progressive instability in patients treated with radiotherapy alone.
P678: Idiopathic Spinal Intradural Arachnoid Cysts: A Case Series
Pratipal Kalsi1, Jamie Wilson1, Eric Massicotte1, and Michael Fehlings1
1University of Toronto, Toronto, Ontario, Canada
Introduction: Idiopathic spinal intradural arachnoid cysts (SIAC) are benign cerebrospinal fluid filled sacs lined by arachnoid membrane. They are rare and of uncertain etiology and if symptomatic need to be treated. The main differential is a spinal cord hernia and when the diagnosis is uncertain this must be excluded. We describe a series of 8 symptomatic SIAC, including demographic features, symptoms and signs, radiological diagnosis, and the treatment options and outcomes. Materials and Methods: Retrospective analysis of patients with SIAC that were surgically managed at the Toronto Western Hospital between May 2005 and May 2018. Results: Eight patients, male–female 6:2, age range 44 to 73 years, median age 59 years. All patients presented with thoracic myelopathy and gait disturbance. None of the patients had sphincter disturbance. Mean duration of symptoms prior to surgery was 5.4 years. Average postoperative follow-up was 1.6 years. All patients had magnetic resonance imaging (MRI) of the spine and a computed tomography (CT) myelogram to exclude a spinal cord hernia. All patients had posterior thoracic decompression with excision or marsupialization of the cyst. One patient had a loculated cyst extending to the cervical region and subsequently had a cervicothoracic skip laminectomy, breakdown of cyst wall, and insertion of a cystoperitoneal shunt. All cases used intraoperative neurophysiological monitoring and ultrasound to assess cord decompression and cerebrospinal fluid (CSF) flow. All patients had MRI between 3 months to 1-year postsurgery and all arachnoid cysts except one had completely been excised. Clinically patients had either remained the same or improved from baseline. Conclusions: SIAC are rare entities. Symptomatic arachnoid cysts should be treated surgically. Complete excision of the cyst is the primary goal. If not possible, the cyst should be marsupialized and adhesions broken. Diversion of the cyst fluid in cases where adhesions are found may be an option but may not be successful. Spinal cord hernia must be excluded before an arachnoid cyst is treated, either by CT myelogram or CSF-flow MRI studies.
P679: Hemangiopericytoma of the Thoracic Spine: A Rare Localization
Saul Solorio Pineda1, Carlos Alberto Tevera Ovando1, Milton Inocencio Ruiz Flores1, Raul Huato Reyes1, Jorge Ortega Espino1, Leonardo Alvarez Vazquez1, Miguel Angel Vaca Ruiz1, Antonio Sosa Najera1, and Cesar Adan Almendarez Sanchez1
1Centro Medico Lic. Adolfo Lopez Mateos, Toluca de Lerdo, Mexico
Introduction: Hemangiopericytomas (HPC) were first described by Stout and Murray in 1942. HPC is derived from the pericytes of Zimmerman, which are pericapillary mesenchymal cells with contractileability. Hemangiopericytoma is a rare tumor of central nervous system that has the potential to escape from the central nervous system (CNS) and metastasize widely. The most common sites for extraneural metastasis are bone, liver, lung, and the abdominal cavity. Brain is the most common location for these tumors and spinal occurrence is a rare event. Our search of the literature showed that 140 cases of HPC in the spine had been reported, and 64 cases were extradural. HPCs correspond histologically to the World Health Organization (WHO) grade II, with anaplastic HPCs corresponding to WHO grade III. Classified spinal hemangiopericytomas in 3 types and 5 subtypes type I is extradural tumor (IA intracanal, IB extracanal), type II is intradural type (IIA extramedullary, IIB intramedullary), and type III is intradural tumor with extension into extradural and paravertebral area. Materials and Methods: A 33-year-old woman started 6 months earlier with dorsolumbar pain, intermittent, pulsatile type intensity 6/10 on pain scale, increased intensity when doing home activities, improved with the intake of analgesics type NSAIDs (nonsteroidal anti-inflammatory drugs). At his admission, he presents an increase in pain intensity. Paresthesias in the pelvic limbs, symmetrical dorsolateral predominance, decreased pelvic limbs muscle strength and inability to walk, confined to a wheelchair, without achieving evacuations, and with difficulty in urination. Neurological exploration hypotonia and hypertrophy of pelvic limbs, paraparesis of lower extremities. Patellar and right achillea hyperreflexia, hypoesthesia of T9 toward caudal, hypotonia of anal sphincter, and diminished anal reflex. Magnetic resonance of the thoracic spine shows a heterogeneous lesion that enhances the administration of contrast at the level of vertebral body T8 with intra-/extrarachial and extradural component, extension toward the right thoracic cavity. Posterior thoracic approach, transpedicular arthrodesis level T6.T7-T9.T10, bilateral laminectomy of T7 and T8, tumor resection of intracanal component, medullary decompression, and subtotal resection of intrathoracic portion by transpedicular route without intraoperative complications. Results: Clinical evolution showing immediate improvement of paraparesis, histopathological diagnosis of hemangiopericytoma staining with H&E (hematoxylin and eosin). Proper tomographic control placement of transpedicular screws, without residual hematoma, no intrathoracic complications. He remained under neurological surveillance, without presenting clinical deterioration and his discharge was sent to an oncological center for radiotherapy-based management, during 2 years of clinical follow-up he found no tumor progression. Conclusions: Surgical excision is the most common treatment for CNS HPC. The benefit of radiotherapy after surgery is well established, with a significant increase in the recurrence-free interval (75 months as opposed to 34 months) and longer survival times (92 months as opposed to 62 months). Regardless of the subtype, surgical excision and radiotherapy seem to be the treatment of choice for hemangiopericytoma in the spine. We decided to present this case because of its rarity in our environment and to be clear about the management options for this disease.
P680: Clinical Outcomes of Pathologic Vertebral Fractures in Patients With Multiple Myeloma: Comparison of Reconstruction Surgery with Adjuvant Radiotherapy and Radiotherapy Alone
Hyung-Youl Park1, Young-Hoon Kim1, Kee-Yong Ha1, Sang-Il Kim1, and Jun-Hyung Cho1
1Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
Introduction: Multiple myeloma (MM) is a hematologic malignancy that most commonly causes pathologic vertebral fractures in the spine column. However, the roles of reconstruction surgery on vertebral fractures with instability remain unclear. The purpose of this study is to compare the clinical outcomes of reconstruction surgery with adjuvant radiotherapy (RT) and RT alone in patients with pathologic vertebral fractures of MM. Material and Methods: Among the 116 patients with vertebral fractures in MM were that treated by RT at our hospitals from 2008 to 2014, 28 patients underwent reconstructive surgery followed by RT (group II). Among the patients who were treated by RT alone, 28 patients whose age, performance status (Eastern Cooperative Oncology Group, ECOG) and pathologic conditions of the spine (Spine Instability Neoplastic Score, SINS) matched those of group II were assigned in group I. Clinical outcomes including the duration of maintenance of independent ambulation, neurologic outcomes, visual analogue score (VAS) for back pain were assessed. Results: Median duration of independent ambulation was longer in group II (median, 51.6 months; 95% confidence interval [CI] 43.0-60.2) than in group I (median, 28.0 months; 95% CI 13.4-42.6) (Log rank test; P = .015). Improvement rate of neurological status (group I; 21.4%, group II; 60.7% P = .024) and VAS (group I; 5.0 ± 2.2, group II; 2.7 ± 2.1, P = .000) were higher in the group II. However, median survival period and treatment-related complications were not significantly different between the groups. Conclusion: In spinal MM with pathologic fractures, reconstructive surgery may provide an advantage in preserving independent ambulation and neurological function even though it is not associated with median survival.
P681: Prognostic Significance of Tokuhashi Scale in the Treatment of Metastatic Spine Lesions
Vladimir S. Klimov1, Murodzhon Kosimshoev1, and Murodzhon Kosimshoev1
1Federal Center of Neurosurgery, Novosibirsk, Russian Federation
Introduction: Assessing the prognosis before treatment for metastatic spine tumor is extremely important in the choice of surgical therapy. Material and Methods: The retrospective analysis of 90 patients with metastatic lesions of the spine, operated in spinal surgery Department of the Federal Center of Neurosurgery Novosibirsk in the period from March 2013 to February 2018, 41 of them were men (45.6%) and 49 women (54.4%). The median age was 59 ± 20 years. Patients were evaluated on the basis of condition-specific functional status using the Karnovsky scale, the Tokuhashi scale (2005), and the Tomita classification (2001). Radiography, CT (computed tomography), MRI (magnetic resonance imaging) of the spine were taken. The average time of observation was 3.5 years. Prevailed metastasises low-grade adenocarcinoma without primary focus 28.9%, breast cancer 26.7%, and kidney cancer 17.8%. Static methods: The Kaplan-Meier method, Schoenfeld, and Cox proportional risk models. Results: Patients were divided into 3 groups according to the life expectancy on the Tokuhashi scale. Group 1 (n = 14, 15.6%) patients who life expectancy, which was more than 12 months. According to Tomita (T) classification of the degree of spinal injury, T1, T2, T3 in this group were not observed, T4 was observed in 1 patient, T5 in 4, T6 in 1, and T7 in 8 patients. Group 2 (n = 37, 41.1%) patients who life expectancy, which ranged from 6 to 12 months. According to Tomita (T) classification of the degree of spinal injury, T1, T2 in this group were not observed, T3 was observed in 1 patient T4 in 1, T5 in 7, T6 in 17, and T7 in 11 patients. Group 3 (n = 39, 43.3%) patients’ life expectancy was less than 6 months. According to Tomita (T) classification of the degree of spinal injury, T1, T2, and T3 were not observed in this group, T4 was observed in 4 and T5 in 6, T6 in 12, and T7 in 17 patients. The volume of interventions: resection of a tumor of 18 patients, 5 en-block; palliative surgery in47 patients; biopsy in 25 patients. For a group with a life prognosis of more than a year, the probability to survive 1 year is 93%; for a group with a prognosis of 6 to 12 months, the probability to live up to 6 months is 78%, and survive 12% to 47%; for a group of 3, the probability to live up to 6 months is 46%, and more than a year 18% of patients survived. Significant influence on the survival term was provided by the group on a scale of Tokuhashi (P = .0056); chemotherapy after surgery (P = .0148); and scores on the Karnovsky scale (P = .0464). There is no reliable statistical relationship between the type of surgery and life expectancy of patients. Conclusion: The prognostic significance of the Tokuhashi scale in patients with metastatic spinal lesions ranged from 46% to 93% (P = .0056).
P682: Clinical Significance of Preoperative Embolization for Non-Hypervascular Metastatic Spine Tumors
Hyung-Youl Park1, Young-Hoon Kim1, Kee-Yong Ha1, Sang-Il Kim1, and Jun-Hyung Cho1
1Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
Introduction: The efficacy of preoperative embolization for hypervascular metastatic spine disease (MSD) such as renal cell and thyroid cancers has been reported. However, the debate on the efficacy of preoperative embolization for non-hypervascular MSD still remains unsettled. The purpose of this study is to determine whether preoperative embolization for non-hypervascular MSD decreases perioperative blood loss. Material and Methods: A total of 79 patients (36 cases of preoperative embolization and 43 cases of non-embolization) who underwent surgery for metastatic spine lesions were included. Representative hypervascular tumors such as renal cell and thyroid cancers were excluded. Intraoperative and perioperative estimated blood losses (EBL), total number of transfusions, and calibrated EBL were recorded in the embolization and non-embolization groups. The differences in EBL were also compared along with the type of surgery. In addition, the incidence of Adamkiewicz artery and complications of embolization were assessed. Results: The average age of 50 males and 29 females was 57.6 ± 13.5 years. Lung (30), hepatocellular (14), gastrointestinal (9), and others (26) were the primary cancers. The demographic data were not significantly different between the embolization and the non-embolization groups. There were no significant differences in intraoperative EBL, perioperative EBL, total transfusion, and calibrated EBL between 2 groups. However, intraoperative EBL and total transfusion in patients with preoperative embolization were significantly lower than in non-embolization in the corpectomy group (1645.5 vs 892.6 mL, P = .017, for intraoperative EBL and 6.1 vs 3.9, P = .018, for number of transfusion). In addition, the presence of Adamkiewicz artery at the index level was noted in 2 patients. Disruption of this major feeder artery resulted in significant changes in intraoperative neuromonitoring. Conclusion: Preoperative embolization for non-hypervascular MSD did not reduce perioperative blood loss. However, the embolization significantly reduced intraoperative bleeding and total transfusion in corpectomy group. Moreover, the procedure provided insights into the anatomy of tumor and spinal cord vasculature.
P683: Delay in Patients With Spinal Metastases is Associated With Reduced Patient Outcome and Survival
Floris van Tol1, David Choi2, H. M. Verkooijen3, F. C. Oner1, and J. J. Verlaan1
1University Medical Center, Utrecht, Netherlands
2The National Hospital for Neurology and Neurosurgery, London, UK
3University Medical Center, Utrecht, Netherlands
Introduction: Approximately 10% of all oncological patients develop symptomatic spinal metastases. Early symptoms caused by spinal metastases are difficult to distinguish from nonspecific causes of back pain, potentially leading to a delay in the diagnosis and/or treatment. The primary aim of this study was to assess the relationship between delayed presentation and postoperative patient outcome and survival in patients surgically treated for symptomatic spinal metastases. Materials and Methods: All patients receiving surgical treatment for symptomatic spinal metastases at our tertiary care center between March 2009 and January 2018 were included. Delay was defined as requiring emergency (nonelective) surgery. Patients were divided into an elective group and a nonelective group. Postoperative patient outcome and survival were compared between the 2 groups. Results: In total, 215 elective patients and 102 nonelective patients were included. Patient age, gender, tumor histology, and the number of affected levels did not differ significantly between the 2 groups. The mean EQ-5D scores and Karnofsky Performance Status (KPS) scores at baseline were 0.49 and 75.7 in the elective group and 0.28 and 64.6 in the nonelective group. Between baseline and 3 months postoperatively, EQ-5D and KPS scores increased by 0.16 and 5.1 in elective and 0.20 and 4.8 in nonelective patients (P = .012 P = .032). Absolute KPS and EQ-5D scores at 3 months were 0.66 and 75.7 in elective and 0.47 and 64.6 in nonelective patients (P < .001, P < .001). Between 3 months and 6 months postoperatively, EQ-5D and KPS scores increased by 0.01 and 2.8 in elective and 0.20 and 8.7 in nonelective patients (P = .569, P = .916). Absolute KPS and EQ-5D scores at 6 months were 0.70 and 80.2 in elective and 0.61 and 70.7 in nonelective patients (P = .201, P < .001). Median survival was 24 months in elective patients and 14 months in nonelective patients. Conclusion: Nonelective surgery, a common result of delayed presentation, is associated with lower EQ-5D and KPS scores postoperatively and a decrease in patient survival. The negative effects of delayed treatment may be partially negated by optimization of referral patterns for patients with spinal metastases.
P684: Consideration of Oncological History Among Dutch Health Care Providers in Patients With Spinal Metastases
Floris van Tol1, F. C. Oner1, and J.J. Verlaan1
1University Medical Center, Utrecht, Netherlands
Introduction: Spinal metastases occur in approximately 20% of all oncological patients. Early symptoms may not be very specific for spinal metastatic disease. To differentiate between different causes of back pain, health care providers usually consider other factors, such as the patient’s oncological history. This study investigates the effect of previous malignancy on different forms of delay in patients with spinal metastases. Materials and Methods: Data on all patients surgically treated for spinal metastases within our tertiary facility between the period of March 2009 until June 2017, were prospectively collected. Referral patterns were divided into 4 categories: patient delay (onset complaints until first medical consultation), diagnosis delay (first medical consultation until diagnosis), referral delay (diagnosis until referral to definitive caregiver), and treatment delay (referral definitive caregiver until treatment). Patients’ medical records were screened for any previous malignancies. Results: In total, 273 patients were included into this study. In patients with and without a previous malignancy, median patient-delay was 14 days versus 23 days, diagnosis delay was 14 versus 35 days, referral delay 10 versus 4 days, and treatment-delay 11 versus 5 days, respectively. In the general practitioner’s office, the median time until referral was 19 days for both patients with and without a known previous malignancy. Conclusion: A previous malignancy is correlated with less patient and diagnosis delay, however, is associated with more referral and treatment delay. General practitioners do not appear to consider a previous malignancy when referring patients with new-onset back pain. For identification of spinal metastases, consideration of the patient’s oncological history is recommended.
P685: Complications After Total or Extended Sacrectomy in a Series of Cases
Mauro Costa Morais Tavares Junior1, Michael Minsu Shu1, Douglas Kenji Narazaki2, William Gemio Jacobsen Teixeira2, Cesar Salge Ghilardi2, Alexandre Fogaça Cristante1, and Tarcisio Eloy Pessoa de Barros Filho1
1University of Sao Paulo, Sao Paulo, Brazil
2Cancer Institute of Sao Paulo, Sao Paulo, Brazil
Introduction: Sacral tumors are rare and may be malignant or benign. The term total sacrectomy refers to resection and attachment of the dural sac below bilateral S1, and it may be extended to resection at L5, L4, and iliac if necessary. At present, what is recommended for these tumors is usually a block sacrectomy. However, such procedures are complex7 and may result in several complications. The aim of the present study was to survey the various complications of total or extended sacrectomy in a specialized service in spinal tumor surgeries. Material and Methods: Descriptive analytical study of medical records of a series of 8 cases operated between 2010 and 2018, in a tertiary service specializing in spinal tumor surgeries. Results: Of the 8 cases operated, 6 were men and 2 women with a mean age of 38.9 years. The oncologic diagnoses were chordoma (2), chondrosarcoma (2), peripheral nerve sarcoma (1), malignant fibrohistiocytoma (1), giant cell tumor (1), and Ewing’s sarcoma (1). Regarding the extent of the sacrectomy: total + L5 (5 cases), total + L4 (2), total + L5 + partial iliac (1). In almost all cases, graft (vascularized: 1, tissue bank: 5) was used, except in 2 cases in which patients died. The mean length of hospital stay was 33 days. Of the 8 cases, 4 had postoperative infection requiring surgery. Perioperative complications include the following: hemodynamic instability with vasoactive drug necessity in the immediate postoperative period (2), occlusion of the left external iliac artery (1), immediate postoperative death due to acute myocardial infarction (1), death in the intraoperative due to hemodynamic instability (1). Conclusion: Total or extended sacrectomy is a complex procedure with high morbidity and mortality even in specialized services in the treatment of spinal tumors.
P686: Results of Surgical Treatment of Patients With Metastases of the Cervical Spine Without Histological Verification
Alexander Tatarincev1, Dmitrii Ptashnikov1, Shamil Magomedov1, and Nikita Zaborovskii1
1R. R. Vreden Russian Research Institute of Traumatology and Orthopedics, Saint-Petersburg, Russian Federation
Introduction: Metastatic lesions of the cervical vertebrae are often accompanied by pathological fractures. Fractures lead to instability of the cervical segments, with progressive development of neurological disorders. Surgical treatment on the background of progressive neurological disorders aims to establish a histological diagnosis (with unclear primary focus), decompression of the spinal cord, reducing the volume of the tumor in the body, and stabilization of the spine. Important, in our view, is to “catch” the patient is in a saved state for a surgical treatment that gives the chance to receive a full therapy. The purpose of our research is to evaluate effect of surgical treatment of the patients with neurological deficits due the metastatic lesion of the cervical spine without the histological verification of the tumor. Material and Methods: This retrospective study evaluated 120 patients with cervical spine metastasis and progressive tetraparesis without verification of the primary tumor. All patients were selected using the scale Spinal Neoplastic Severity Score (SINS) and the scale American Spinal Injury Association (ASIA). Surgery was performed by ablastic removal of the tumor in cases of the solitary metastasis. Patients with data about the multiple lessons was treated by decompression of the neural structures and stabilization of the spine. Preoperative and follow-up radiographic, health-related quality of life (HRQoL) parameters (VAS [visual analogue scale], ODI [Oswestry Disability Index], SF [Short Form]-36), and Kaplan-Meier index of survival Kaplan-Meier were evaluated. Results: The selection of patients for surgery was carried out on the basis of data obtained on a scale instability SINS (8 to 10 points—28%, 11 to 15 points—47%, 16 to 18 points—25%), ASIA scale (category B 9%, C 28% D 63%). If solitary metastases were diagnosed, the aim of surgery was total resection of tumor. In the presence of multiple lesions, decompressive-stabilizing operation were performed. An overwhelming number of fractures, on receipt of the pathology report due to metastases of breast cancer of 56%, lung cancer 15%, and stomach 8%. Evaluation of treatment results was evaluated by such indicators as regression of neurological disorders, stability, and relief of pain. Good results were recognized, the treatment results in which the regression of neurological deficits occurred in the clinic of the Institute in the future, the patient received full courses of therapy. Obtained in 54%. Admitted satisfactory results in which there was not a complete regression of neurological deficit due to unsatisfactory laboratory results not received full courses of therapy—32%. Poor performance persisted tetraparesis14%. Conclusion: Surgical treatment is effective for patients with tetraparesis developing in the background of metastatic lesions of the cervical spine and the impossibility of quick verification of the primary tumor in connection with the presence and deepening of neurological deficit.
P687: Open Kyphoplasty for Pathologic Vertebral Compression Fractures
Stefano Telera1, Francesco Crispo1, Laura Raus1, Riccardo Boccaletti1, and Nicola Gorgoglione2
1IRCCS Istituto Nazionale Tumori Regina Elena, Rome, Italy
2University of Messina, Messina, Italy
Introduction: Symptomatic metastatic spine disease (MSD), due to solid or hematological tumors is a challenging pathology involving 3% to 15% of patients with bone metastases. Different surgical options are available and must be tailored to the general and neurologic conditions of the patients. An open balloon Kyphoplasty (BKP), refers to a unilateral or bilateral decompressive hemilaminectomy, associated with a percutaneous kyphoplasty and in some cases to short posterior stabilization (Spinal Neoplastic Severity Score (SINS) score ≥13). It could be a valuable option to relieve an anterolateral epidural compression or whenever the posterior vertebral wall was violated, to expand the indications of palliative surgery in patients otherwise poor candidates for more aggressive surgical procedures and to rapidly deal with possible cement leakages in the spinal canal. Material and Methods: Between 2005 and 2018, 55 cancer patients underwent open BKP for symptomatic MSDs. Postoperative leakages and pulmonary embolism were carefully evaluated with neuroimaging. KPS (Karnofsky Performance Status), VAS (visual analogue scale) and Dennis Pain Score were calculated preoperatively, postoperatively, and at the last follow-up. Results: Median Tokuhashi and SINS scores were respectively 10 and 10. Kyphoplasty was performed in 38 cases with silicone VK100, in 17 patients with polymethylmethacrylate (PMMA). The mean volume of filling material (silicone or PMMA) inserted in each vertebra was 3.6 (range 2-8 cc). Complications included 8 leakages (14.5%), 1 new motor deficit, and 1 asymptomatic pulmonary embolism. Two other patients presented a postoperative hematoma, which required surgical evacuation, both of them had a motor deficit of the lower legs (1 transient, 1 permanent). Mean hospital stay was 7 days. A significant improvement was observed in KPS, VAS, and Dennis Pain Score (P < .0001). Median follow-up was 15.5 months. The overall survival was 22 months (CI [confidence interval] 95% 8-35), significantly longer in hematologic diseases compared with solid tumors (33 vs 13 months, P ≤ .025). In no cases except one, a progression of spinal instability was observed at the radiologic and clinical follow-up. Conclusion: In this series, open BKP proved to be a safe and effective palliative treatment of symptomatic MSDs in carefully selected oncologic patients with an intermediate-low Tokuhashi score, not otherwise surgical candidates. It allowed to decompress lateral epidural compressions, to significantly reduce intractable pain and mechanical instability, consenting an earlier start of adjuvant therapies.
P688: Recurrent Aneurysmal Bone Cyst (Solid Variant) of the Dorsal Spine Treated With Computed Tomography-Guided Direct Injection and Posterior Resection
Haytham Khira1, Amr Nassef1, Shady Mashhour1, and Mostafa Abdelhammid1
1Center for Implantation and Preservation of Musculoskeletal Tissues, Cairo, Egypt
Introduction: Solid aneurysmal bone cyst (S-ABC) is a variant of aneurysmal bone cyst (ABC), an uncommon benign bone tumor. The challenges involved in treating aneurysmal bone cysts are well known in the surgical community. These include hemorrhage, damage to adjacent structures, and recurrence, especially if resection is incomplete. Recurrence rates for ABC after surgery have been reported from 12% to 71%. Some of the lowest rates of recurrence in the spine have been reported where en bloc resection has been possible. Other nonsurgical options described have included arterial embolization, injection of sclerosing agents (such as ethanol or polidocanol), and radiotherapy. These have all had variable results with relatively high recurrence rates. We treated a recurrent case of aneurysmal bone cyst with neurological involvement by direct injection of sclerosing agent followed by posterior excision. Material and Methods: We report a case of D11 located ABC concerning a 30-year-old female treated surgically twice by incomplete intralesional resection.1 month after the second procedure a paraperesis led to diagnose a local recurrence treated by computed tomography (CT)-guided injection of N-Butyl-2Cyanoacrylate lipidol (3:1) using 16 G spinal needle through bilateral costovertebral approach, which followed by posterior surgical excision of the posterior mass with its epidural extension. Results: The paraparesis was resolved during the hospital stay. With a period of 24-months follow-up, imaging studies revealed progressive sclerosis of the vertebral body cystic spaces with no local recurrence. Conclusion: A recurrent case of S-ABC of D11 has been successfully treated with a combination of CT-guided sclerotherapy of the body followed by posterior surgical excision of the posterior mass.
P689: Retrospective Case Study of Occipitocervical Fusion in Patients With Tumors at the Occipitocervical Junction and Upper Cervical Spine
Tarush Rustagi1, Hazem Mashaly1, David Kline1, and Ehud Mendel1
1Ohio State University, Columbus, OH, USA
Introduction: The spine is the most common site of skeletal metastatic cancer and metastases to the cervical spine may occur in as many as 25% of all metastatic spinal tumors. Cranio-cervical instability may manifest as disabling pain, cranial nerve dysfunction, paralysis, or even sudden death. Stabilization and fusion are required to prevent the aforementioned complications. Nonoperative treatment modalities are ineffective in providing stability to the unstable cervical spine and cannot correct deformities caused by tumor destruction of the supporting elements. Surgical treatment is indicated for mechanical instability, neural compression, and the presence of a radio-resistant tumor. Occipitocervical fusion and instrumentation is a technically challenging procedure that can be accomplished successfully with careful attention to local anatomy and working knowledge of the various fixation options. Published literature on the topic is limited, with conflicting opinions. The purpose of this study was to present our experience of diagnosis, presentation, and surgical management of metastatic tumors of the upper cervical spine. To our knowledge, it is a largest series till date. Material and Methods: Study was conducted at Ohio State University, James Cancer Center from 2007 to 2016. Retrospective study was done. The inclusion criteria were consecutive cases (between age >18 years) of occipitocervical fusion following metastasis to upper cervical spine. All other causes and revision surgeries were excluded. Demographic, surgical, and clinical data were collected through chart review. Clinical data included pain scores (presurgery and postsurgery) based in Numeric rating score, Frankel scale. The preoperative and postoperative images were used to evaluate extent of disease, and translation/angulation of C2. Anteroposterior thecal sac diameter was measure preoperative and postoperative based on axial T2-weighted MRI (magnetic resonance imaging). Descriptive statistics will be generated for all variables of interest. Continuous responses will be expressed using means, medians, standard deviations, and other appropriate measures of spread. Categorical responses will be expressed using frequencies and percentages. Results: Thirty-one patients included 17 females and 14 males. The mean age at the time of surgery was 56.4 (range 24-82) years. All patients presented with mechanical pain with average numeric rating scale (NRS) of 8.27 (5-10). No patient had any neurological deficit from the cervical disease (Frankel E). Average SINS (Spinal Neoplastic Severity Score) score was 10, with majority 23 patients lying in the intermediate category (7-12) and the remaining in marked instability group (13-18). Out of 31 cases, 5 cases had average C2 angulation of 5.4° (4-17°) and subluxation was seen in 12 cases (average 5.5 mm). Breast metastasis was most common in 9 cases followed by renal in 5 cases and melanoma in 4. Three cases each had metastasis from lung and colon, 2 had multiple myeloma and 1 each had metastasis from bladder and esophagus. Most cases had occiput to C4 fusion (25), 5 had extension to C5, and tone to C6. All cases had an occipital plate and lateral mass screws. Average blood loss was 386.3 mL (75-1300 cc) and time was 210.5 minutes. The average length of stay was 6.96 days (4-15). Single vertebra was involved in most cases 26, 2 in 3 cases and 3 in 1 case. Axis was most commonly involved in 24 cases with most common being the body involvement (21) followed by pedicle/pars involvement (12 cases). Atlas was involved in 9 cases (mostly unilateral lateral mass involved in 8 cases and arch involved in 3 cases. Occiput was involved in 3 cases. There was no neurological complication. Three patients needed a repeat debridement for wound infection. The NRS reduced from 8.27 (5-10) to 1 (0-3). The average survival (months postsurgery) was 16.61 months (5 days-50 months). Conclusion: Occipitocervical fusion gives good clinical outcomes in patients with metastasis to upper cervical spine. The surgery offers a good palliative treatment to patients with severe neck pain. Most patients complain was debilitating neck pain. C2 body is the most common site of metastasis.
P690: A Retrospective Analysis of the Clinical Utility of the Tokuhashi Scoring System, and Its Impact on the Surgical Management of Spinal Metastatic Disease
Erika Leck1, Ayoub Dakson1, David Brandman1, and Sean Christie1
1Dalhousie University, Halifax, Nova Scotia, Canada
Introduction: The evaluation of patients presenting with spinal metastatic disease is often challenging due to the diversity of disease and variety of factors at play. The Tokuhashi scale intends to facilitate this process by incorporating patient and disease-specific characteristics to assess prognosis and guide intervention. We conducted this study to investigate its clinical utility in surgical-decision making in patients with spinal metastasis, and to compare it with other commonly used scoring systems. Material and Methods: A database was created of patients diagnosed with spinal metastatic disease between January 2010 and 2015. A total of 285 patients with spinal epidural metastases were identified, and a retrospective chart review was conducted to capture their baseline characteristics, along with components related to multiple scoring systems, including the Tokuhashi Scoring System (TSS), Tomita Scoring System, and Modified Bauer Scoring System. Patients were also scored for metastatic epidural spinal cord compression (MESCC) and the Spinal Instability Neoplastic Score (SINS), and thus, stratified into stable, potentially unstable, and unstable categories. Univariate and Kaplan-Meier statistical analysis was performed to compare the different scoring systems and their association with survival curves postspinal met diagnosis. TSS and SINS were then compared with explore clinical utility of TSS and its ability to predict instability. Results: Based on the Tokuhashi scale, there was 69.1% in the nonoperative/radiation group (group 1), 23.2% in the palliative/excisional surgical group (group 2), and 7.7% in the surgical group (group 3). Using Kaplan-Meier estimate, survival time was significantly different across the 3 groups with means 232.8 ± 30.8, 352.3 ± 49.2 and 568.3 ± 206.1 days, respectively. A significantly higher proportion of patients (84.6%) were treated nonsurgically in group 1, compared with 45.5% in group 3 (χ2 = 19.5, P < .001). However, there was no correlation between the type of surgical interventions (ie, instrumented decompression, decompression alone, percutaneous vertebral augmentation, and instrumented vertebral augmentation) and the Tokuhashi score, nor was there any correlation between TSS and the SINS score of degree of metastatic epidural spinal cord compression. Conclusion: This review illustrates the utility of the Tokuhashi scale in predicting survival, and demonstrates that TSS is associated with 3 distinct survival groups. However, it was found to underestimate prognosis in those with a predicted survival of <6 months, and alone cannot be used as a sole treatment guidance strategy. It does not address the new role of emerging different surgical strategies for the treatment of spinal metastasis including surgical interventions and recent advances in targeted molecular pharmacology and lacks information concerning spinal instability, all of which are important factors in making treatment decisions. TSS was also found to be independent of both spinal instability and degree of metastatic epidural spinal cord compression. This calls for a scoring system that combines prognostic data as well as information related to spinal instability in order to better guide surgical treatment of spinal metastases.
P691: Back to Bayesian: A Strategy to Enhance Prognostication of Metastatic Spine Disease
Markian Pahuta1, Joel Werier1, Eugene Wai1, and Doug Coyle1
1Henry Ford Health System, Detroit, MI, USA
Introduction: Clinicians must consider prognosis when offering treatment to patients with spine metastases. Although several prognostic indices have been developed and validated for this purpose, they may not be applicable in the current era of targeted systemic therapies. Even before the introduction of targeted therapies, these prognostic indices should not have been directly used for individual patient decision-making without contextualizing with other sources of data. By contextualizing, we mean that estimates of prognosis should not be based on these scores alone: prognosis should be estimated from multiple data points. Contextualization requires the use of Bayesian statistics—a form of statistics that may be unfamiliar to many readers. In this article, we show readers how to correctly apply prognostic scores to individual patients using Bayesian statistics. Through Bayesian analysis, we explore the impact of new targeted therapies on prognostic estimates obtained using the Tokuhashi score. Methods: We provide a worked calculation for the probability a patient surviving to 6 months using dichotomous prognostication. We then demonstrate how to calculate a patient’s expected survival using continuous prognostication. We perform continuous prognostication using our freely available web-based calculator. Results: When the predicted prognosis from the Tokuhashi score is contextualized with data on contemporary systemic treatments, patients previously deemed nonsurgical candidates may be eligible for surgery. Conclusions: Bayesian prognostication generates intuitive results and allows multiple data points to be synthesized transparently. These techniques can extend the usefulness of existing prognostic scores in the era of targeted systemic therapies.
P692: A Critical Evaluation of Prognostic Contraindications for Surgery in Metastatic Epidural Spinal Cord Compression
Markian Pahuta1, Joel Werier1, Eugene Wai1, and Doug Coyle1
1 Henry Ford Health System, Detroit, MI, USA
Introduction: Surgery followed by radiotherapy (S+RT) for metastatic epidural spinal cord compression (MESCC) is effective for maintaining and improving patients’ physical function and health-related quality-of-life (HRQoL). However, it is generally felt that benefit from surgical intervention requires that patients survive longer than the time needed to recover and rehabilitate from surgery. A commonly used threshold is that patients should have an expected survival of at least 3 to 6 months to be surgical candidates. Patients with poor prognosis are offered radiotherapy alone (RT). Treatment decisions are particularly challenging for MESCC patients with poor prognosis. For patients with short survival, recovery from S+RT and complications will affect a greater fraction of remaining life. Therefore, clinicians are concerned that these patients may not derive net benefit after recovering from surgery and/or experiencing a major complication from S+RT. The objective of this article is to determine whether MESCC patients with poor prognosis can benefit from S+RT. We formally incorporate uncertainty using economic decision analytic methods through a sensitivity analysis of Markov simulation using data from a randomized controlled trial comparing S+RT and RT-alone for MESCC, and a general population utility evaluation study for spinal metastasis. Methods: Markov simulation was used to determine the incremental quality-of-life-years (▵QALYs) gained/lost by patients with poor prognosis undergoing S+RT versus those undergoing RT alone from the societal perspective. Poor prognosis was defined as median survival ≤3 months because 3 months is the lower limit for which patients are generally considered to be S+RT candidates. The model was populated using the results of a randomized controlled trial and general population utility valuation study for MESCC. Since S+RT has greater disutility than RT, we model the “surgical penalty.” The surgical penalty is the average incremental disutility of S+RT versus RT on an average day measured in number of dysfunctions. A uniform distribution on the interval 0 to 4 inclusive was placed on the surgical penalty (quantified by the number of dysfunctions). Results: Mean ▵QALYs were 0.447 and 0.470 for baseline nonambulatory and ambulatory patients, respectively. With increasing surgical penalty (quantified by number of dysfunctions), the frequency of simulation replications with ▵QALYs >0 decreased. The probability of S+RT not being beneficial in terms of HRQoL (▵QALYs ≤0) was greater than 10% if the surgical penalty was greater than 2 dysfunctions for nonambulatory patients, and greater than 3 dysfunctions for ambulatory patients. Conclusions: This is the first study to critically explore survival indications for MESCC treatment. We have demonstrated that MESCC patients with poor prognosis can derive HRQoL benefit for S+RT. Given the inaccuracy of prognostication for MESCC and the treatment advances, blanket survival indications/contraindications to surgery should be avoided.
P693: Collagenous Fibroma (Dermoplastic Fibroblastoma) in Spine: A Case Report
Javier Guerra Garza1, Axel García Villaseñor1, Carla García Ramos1, and Alejandro Reyes Sánchez1
1National Institute of Rehabilitation, Mexico City, Mexico
Study design: Case report. Objective: To present a case of a man 58 years old with diagnosis of collagenous fibroma in the cervical spine and literature review. Background: “Dermoplastic fibroblastomas,” first described by Evans in 1995, and later renamed by Nielsen et al as “collagenous fibroma,” are benign fibroblastic tumors that rise in subcutaneous tissue or skeletal muscle at a variety of anatomical sites. Classically present as nontender, firm, slow-growing masses. The tumors are grossly circumscribed, with spindle to stellate fibroblasts disperse in a fibromyxoid or fibrous matrix with low mitotic activity. The disease can occur at any age with a mean of 50 years and are more frequent in men than women. The anatomic distribution is wide, being the head, neck, back, shoulders, arms, limbs, and dorsal foot the most common. Symptoms are related with local compression. Metastasis or recurrence following surgical resection are not reported. Thus, surgical resection is the treatment of choice. Fewer than 130 cases have been reported in the literature. In this article, we present a case of a man 58 years old with diagnosis of collagenous fibroma in the cervical spine and its surgical resolution. To our knowledge, there are not previous reports of this tumor in this location.
P694: New Posterior Column Reconstruction Using Titanium Lamina Mesh After Total En Bloc Spondylectomy of Spinal Tumor
So Hyun Moon1 and Sung Kyu Kim2
1Chosun University, Gwangju, Republic of Korea
2Chonnam National University Hospital, Gwangju, Republic of Korea
Introduction: There have been few reports about posterior column reconstruction to reinforce the stability by maintenance of the posterior structure and provision of the posterior fusion bed, and to protect the neural structures such as the spinal cord. The purpose of the study was to investigate the usefulness of titanium lamina mesh for posterior column reconstruction after total en bloc spondylectomy in patients with spinal tumor and evaluate the radiographic outcomes of this method. Material and Methods: Eight patients who underwent total en bloc spondylectomy with posterior column reconstruction using titanium lamina mesh and bone graft to treat a spinal tumor were included in this study. The mean age at the time of surgery was 50.6 years (range, 16.5-70.9 years) and the mean follow-up duration was 50.2 months (range, 28.1-68.7 months). The pathological lesions were located from the T2 to L1 vertebrae. There were 4 patients in each primary and metastatic tumor group. For the posterior column reconstruction, titanium lamina mesh was used and bone graft was applied over the lamina mesh. Radiographic evaluation was used to investigate the displacement of lamina mesh and union of the grafted bone above lamina mesh. Results: At the postoperative 6-month follow-up, a bony bridge on the titanium mesh between upper and lower adjacent lamina was observed in all cases, except for one with infection. On the last follow-up, there was no collapse or displacement of titanium lamina mesh, and there was no instability or malalignment of the spinal column. Conclusions: Posterior column reconstruction using titanium lamina mesh during total en bloc spondylectomy for spinal tumor was a useful surgical option that provided new lamina reconstruction for stability of spinal column and protection of the neural elements.
P695: Sacrococcygeal Chordoma: A 14-Year Follow-up of 22 Cases Treated Surgically
Ashok Bajracharya1
1Capital Hospital and Bir Hospital, Kathmandu, Nepal
Introduction: This is an ongoing prospective study of 22 cases of sacrococcygeal chordoma treated by same surgeon, in single stage surgery at same center, which is a government hospital by name of Bir Hospital in Kathmandu surgically. The first surgery was performed in 1996 and last one was performed for recurrence in 2016. Material and Methods: Of 22 patients, 14 were males, and 8 females. Age ranged from 40 to 78 years. Besides clinical examination, all went through radiological evaluation by plain X-ray, CT (computed tomography) scan, MRI (magnetic resonance imaging), and Ba Enema in 2 cases. Four open and 18 needle biopsies were performed to confirm the diagnosis. Operative procedure to excise the tumor with side margin were carried out by posterior approach in 12 cases, by combined posterior and anterior approach without instrumentation in 9 cases, by combined posterior and anterior approach with spinopelvic reconstruction in one case. Operative procedures were long, ranging from 7 to 18 hours. Results: All patients presented with local pain. Eighteen complained of increasing mass over buttock, 19 patients complained of increasing constipation, and sciatica by 2 patients. On examination, tumor mass was prominent posteriorly in 13 cases and anteriorly in 9 cases. None had neurological deficit. Cephalad most extension of tumor was noted at S1 level, while majority were at S4 level. Follow-up ranged from 6 to 16 years mean being 8 years. postoperatively all had satisfactory outcome. Immediate postoperative complications like CSF (cerebrospinal fluid) leak, stool incontinence were not seen. Late complications included lost sexual function in 12 males, local recurrence in 4 patients, neural defect in 5 cases, pelvic instability in one. Three patients had died, 1 from metastasis and 2 from unrelated medical condition. Disease status at final follow-up was 10 alive without evidence of disease, 4 alive with evidence of disease, 2 dead from other causes, 1 dead from disease, and 5 cases were lost to final follow- up. Conclusion: Since chemo and radio therapy has no role in treatment of Sacrococcygeal chordoma. Wide surgical resection is the mainstay of treatment at the cost of some neurological impairment in some cases. Prolonged anesthesia and massive surgery exposes patient to potential hazards. Prevention of local and systemic recurrence is a challenge.
P696: Surgical Management of Aggressive Hemangiomas of the Spine
Bowen Qui1, Adan Omar1, and Addisu Mesfin1
1University of Rochester Medical Center, Rochester, NY, USA
Introduction: Aggressive hemangiomas (AHG) are rare primary spine tumors representing 1% of spinal hemangiomas. Reports on surgical management of AHGs are limited to case series due to its rare nature. The objective of this study is to report the clinical presentation and surgical management of symptomatic aggressive hemangiomas. Material and Methods: Using a pathology database, patients with AHGs undergoing spine surgery at a tertiary referral cancer center from August 2005 to February 2018 were identified. Demographic information, clinical presentation, surgical data, estimated blood loss (EBL), surgical complications, and outcomes were collected. Results: Ten patients were identified; 4 females and 6 males with an average age of 49.9 (31-73) years. The primary clinical presentation was neurological changes and pain. Eight patients were ASIA (American Spinal Injury Association) D on presentation. Out of 10, 8 lesions were in the thoracic spine and 2 in the lumbar spine. Four underwent spinal fusion with transpedicular decompression (2) or corpectomy (2) and 6 underwent laminectomy only. Concurrent vertebroplasty was used in 2 patients at the AGH site. Three orthopedic spine surgeons and 3 neurosurgeons performed the procedures. Average EBL was 890 mL (200-1100). Surgical complications included the following: 1 deep wound infection, 1 implant failure requiring revision, 1 DVT (deep vein thrombosis), and 1 revision due to stenosis. There were no recurrences following surgical intervention. Conclusion: Aggressive hemangiomas are rare tumors of the spine. In the setting of neurological changes and pain, surgical intervention can lead to successful resolution of the tumor with low rates of recurrence.
P697: Low-Dose Zoledronate for the Treatment of Bone Metastasis Secondary to Lung Cancer
Elie Akoury1, Rodrigo Navarro-Ramirez1, Ana Sofia Ramirez Garcia Luna1, Antone Nour1, Pouyan Ahangar1, Michael Weber1, and Derek H Rosenzweig1
1Research Institute of the McGill University Health Centre, Montreal, Quebec, Canada
Introduction: Lung cancer is the leading cause of death from cancer worldwide. Most patients present with metastatic disease at the time of diagnosis and up to 65% of them develop bone metastases. Bone metastases are not only the most common cause of cancer-related bone pain, but they also lead to additional complications like pathological fracture and spine compressions. Current treatment for lung bone metastases includes chemotherapeutic regimens, excisional surgery, and bisphosphonates (BPs), which reduce bone resorption by inhibiting osteoclastic cell activity. Zolendronate (Zol), a high potency of third-generation BP, has shown clinical benefits in patients with metastatic bone disease, such as relief from lung cancer-related bone pain and a reduction in the frequency of skeletal events associated with lung cancers. However, the high therapeutic systemic doses cause several complications ranging from flu-like symptoms and anemia to osteonecrosis of the jaw and renal toxicity. To overcome these debilitating side effects, we aimed at testing low doses of Zol in vitro on patient-derived cells. Materials and Methods: Human lung adenocarcinoma cells from the ATCC (American Type Culture Collection) and lung cancer cells isolated from spine metastases of 3 patients were cultured and treated with either vehicle or 1, 3, or 10 μM of Zol for 7 days in low serum (1% FBS [fetal bovine serum]) conditions. Effects of Zol on proliferation was assessed using Vybrant MTT and alamarblue assays. Additionally, migration and 3D invasion was also carried out using Falcon cell culture inserts and Cultrex 3D spheroid cell invasion kits, respectively. Statistical analysis was preformed using 1-way or 2-way ANOVA and Tukey post hoc tests at a 95% confidence level. Results: The human lung adenocarcinoma cell line and the 3-lung cancer-induced bone metastasis cells showed a significant dose dependent decrease in cell proliferation following 7 day-Zol treatment. Using the same low-dose and longer time course for treatment, we demonstrate that low Zol concentrations also significantly inhibits tumor cell migration and 3D spheroid growth/invasion. Conclusions: Our data shed new light on the use of low Zol doses for longer duration as a new therapeutic regimen that will not only be sufficient to exhibit antitumor effects, but could also prevent unwanted side effects following systemic drug treatment. These attributes could consequently lead to better quality of life and surgical outcomes in patients with bone metastasis.
P698: Delayed Manifestation of Sacral Clear Cell Meningioma: Two Cases
Hassen Makhlouf1, Ahmed Mzid1, Ameur Triki1, Bouzid Lanouar1, Leyla Abid2, Faten Farah2, and Mondher Mestiri1
1Kassab Institute, Manouba, Tunisia
Introduction: Clear cell meningioma is a rare subtype characterized by its inordinately aggressive clinical course despite its benign appearance. The tumor shows proclivity for the cerebellopontine angle and cauda equine region. Recurrence and metastasis have been commonly reported. We report 2 cases of clear cell meningioma (of the sacrum revealed after a removal of the primary tumor). Materials and Methods: First case: a 26-year-old man presented with low back pain related to a lytic lesion of the sacrum. He had a history of an intradural extramedullary meningioma of the cervical spine removed when he was 9-year-old. Computed tomography (CT) scan revealed a sacral osteolytic lesion with anterior and lateral extension. Open biopsy revealed a clear cell meningioma. That was the same pattern of the tumor removed 17 years before. Second case: a 62-year-old man presenting a lumbar and sacro-iliac pain over the past 3 months. He had a history of cerebral meningioma operated 12 years ago. Exploration by CT and magnetic resonance imaging (MRI) highlight an expansive process taking all the sacrum and invading the right sacro-iliac. Biopsy revealed clear cell meningioma with identical appearance to the tumor removed 12 years ago. Results: The 2 patients were handled conservatively by palliative radiotherapy. They have showed significant improvement in pain and walking with a decline of 2 years for the first case and 6 months for the second. Conclusion: Clear cell meningioma is an aggressive tumor with a high risk of metastases through cerebrospinal fluid. A close follow-up with spinal MRI should be performed to detect metastasis earlier.
P699: Timing of Prophylactic Anticoagulation and Its Effect on Thromboembolic Events After Surgery for Metastatic Tumors of the Spine
Rafael De la Garza Ramos1, Michael Longo1, Yaroslav Gelfand1, Murray Echt1, Merrit Kinon1, and Reza Yassari1
1Montefiore Medical Center, New York, NY, USA
Introduction: Cancer and spine surgery are known risk factors for venous thromboembolism (VTE). Patient with spinal tumors are at higher risk for these events compared with patients with other spinal disorders. The purpose of this study is to investigate the effect of timing of initiation of chemoprophylaxis on the incidence of VTE after surgery for metastatic tumors of the spine. Methods: A retrospective review of our institutional neurosurgical spine database for the years 2012 through 2018 was performed. Patients who underwent surgery for metastatic tumors were identified. The development of VTE, deep vein thrombosis (DVT), and/or pulmonary embolism (PE) within 30 days was examined, as well as the occurrence of epidural hematoma. The incidence of VTE was compared between patients receiving “early” (within postoperative days 1-3) and “delayed” chemoprophylaxis (on or after postoperative day 4). Results: A total of 65 consecutive patients were identified (mean age 57, 62% male). The overall rate of VTE was 16.9% —all of whom had DVTs with a 3.1% rate of nonfatal PE (2 patients also developed PE). From the overall cohort, 36/65 (56%) received chemoprophylaxis in addition to mechanical prophylaxis, 22 in the early group (61.1%) and 14 in the delayed group (38.9%). The risk of VTE was 9.1% in the early group and 35.7% in the delayed group (26.6% absolute risk reduction; P = .049); there was one case of epidural hematoma (1.5%). On multivariate analysis, delayed chemoprophylaxis was found to significantly increase the odds of VTE development (OR [odds ratio] 6.43; 95% CI [confidence interval] 1.01-41.2; P = .049). Conclusion: The findings of this study suggest that administration of chemoprophylaxis between days 1 to3 after surgery for metastatic tumors of the spine may significantly reduce the risk of postoperative thromboembolic events.
P700: Spine Giant Cell Tumor Severe Evolution After a Misdiagnosis of Aneurismal Bone Cyst
Hassen Makhlouf1, Mehdi Meddeb1, Ahmed Mzid1, Saber Bouhdiba1, Leyla Abid2, Faten Farah2, and Mondher Mestiri1
1Kassab Institute, Manouba, Tunisia
Introduction: Tumors affecting the spinal column include primary and metastatic tumors. Primary tumors comprise less than 11% of all primary musculoskeletal tumors, and only 4.2% of all spine tumors. The rarity of primary tumors, and the diversity of clinical behavior of these tumors, underlies the absence of clear guidelines for managing these important spinal pathologies. The lack of knowledge of the right diagnosis may lead to severe damage. We report a case where the diagnosis of a benign tumor was wrongly made. Case Presentation: A 26-year-old woman with unremarkable medical history presented with the chief complaint of persistent low back pain for 3 months. On physical examination, there was moderate tenderness in the upper lumbar spine without neurologic deficit. Radiograph showed a “ballooned” osteolytic lesion on the right side of the L1 vertebra. Computed tomography (CT) scan showed lytic expansile and eccentric lesion involving the L1 vertebral body and right pedicle. Magnetic resonance imaging (MRI) found that the lesion had inhomogeneous signals, low signal intensity in T1and multichambered high signal intensity in T2. Multiple fluid–fluid levels could also be seen giving a bubbly appearance. There was also extension of the lesion into the spinal canal. The patient had a CT-guided percutaneous biopsy that confirmed the diagnosis of aneurysmal bone cyst. She had a spinal brace and corticosteroid and calcitonin infiltration into the lesion through a CT-guided approach, with a partial improvement. Two months later, she had a second infiltration but developed an incomplete neurologic deficit. MRI found that the lesion had increased with a complete bone destruction of L1 vertebra and spinal cord compression. She had surgical resection of L1 vertebra with anterior interbody fusion cage and posterior fixation. The histopathological report confirmed the diagnosis of aneurysmal bone cyst. One year later, the patient was admitted with low back pain, local recurrence, and lung metastasis. The pathological reexamination suspected the diagnosis of giant cell tumor colonized by aneurismal bone cyst, and the patient was treated with Zoledronic acid. Three months later, the patient had paraplegia, vesicosphincteric disorders, and scattered multiple pulmonary nodules. The patient had revision surgery. She had also a surgical lung biopsy that confirmed the diagnosis of giant cell tumor. She was put on denosumab. She got well for 2 years and then had 3 recurrences requiring surgical treatment. The patient died from decubitus complications. Conclusion: Giant cell tumor is typically a benign, locally aggressive lesion but 1% to 9% of benign giant cell tumors metastasize to the lung. Aneurysmal bone cysts and giant cell tumors of the spine are important primary tumors that may be considered in the differential diagnosis of a lytic lesion involving the vertebral body or posterior elements of a patient in the first through third decades. The radiographic and histologic features of these tumors may appear similar. However, the biological behavior and clinical course of these tumors differ significantly and an effective approach to treatment is distinct in these conditions. In cases where the diagnosis is uncertain, open biopsy is most appropriate.
P701: Surgical Treatment of Spinal Metastasis: Is Fusion Necessary After Decompression and Instrumentation?
Alvaro Silva1, Oscar Bravo1, Macarena Santorcuato1, Carlos Thibaut1, Manuel Valencia1, Ratko Yurac1, Juan Jose Zamorano1, Felipe Novoa1, Bernardo Merello1, Rodrigo Varela1, and Bartolomé Marré1
1Clinica Alemana of Santiago, Santiago, Chile
Introduction: Surgical treatment goals for spinal metastasis are mainly focused on preserving and hopefully improving quality of life for these patients. This is mainly achieved with pain relief and neural decompression and/or tumor debulking in order to make other treatment modalities safer for the neural elements. The potential morbidity of the planned procedure must always be balanced against the life expectancy or prognosis in every patient. There is growing literature supporting that minimally invasive surgery (MIS) can help us achieve adequate neural decompression and spinal stabilization, with lower surgery-related complications and faster postoperative recovery times when compared with open surgery. This way, a broader spectrum of patients with spinal metastasis can benefit from surgical treatment, as those with lower life expectancy can also be considered. Spinal instrumentation without fusion seems feasible in this population, mainly because of their limited survival and individual tumor growth biology, but there is limited evidence in this regard. Our aim is to determine implant failure in patients with spinal metastasis treated with MIS stabilization (with or without decompression) but without fusion. Material and Methods: This is a retrospective case series of patients operated between January 2007 and June 2018, in 2 private centers in Santiago, Chile. Medical records as well as preoperative and postoperative imaging were reviewed to obtain demographics (age, gender), primary tumor characteristics, location of metastatic disease, SINS (Spinal Instability Neoplastic Score) and Tomita scores, perioperative complications and particularly implant failure during the postoperative period. No statistical analysis was performed due to the descriptive nature of our study. Results: A total of 27 patients (18 men) were identified during the study period with an average age of 64.3 years and a mean follow-up of 621.59 days. All patients had an identified primary tumor, with lung cancer being the most frequent (40.7%), while the thoracic spine was the most common location (51.9%). Median SINS and Tomita scores were 10 and 6 points, respectively. The most frequent MSCC was grade A (67%) with type A1b being the most frequent (6/27). Mechanical pain was the main surgical indication (92.6%). MIS stabilization was combined with cement augmentation in 4 patients and with decompression in 9 patients. Radiotherapy was performed in 81.5% of the patients, starting, on average, 30.8 days after surgery (5-256 days). There were 3 intraoperative complications (dural tears) and 2 postoperative complications (epidural hematomas, both required surgical decompression). No implant failure was identified, and spontaneous facet joint fusion was observed in 29.6% of the patients. Ambulation was preserved in 92.6% of the patients, with significant pain relief. Conclusion: MIS decompression and stabilization without fusion is a feasible alternative for patients with spinal metastasis. We observed no implant failure, both in short- and medium-term follow-up. This treatment modality reduces the delay between surgery and adjuvant therapies and is associated with a lower perioperative complication rate. We consider it is a safe and effective way to treat these patients, even those previously.
P702: Idiopathic Hypertrophic Spinal Pachymeningitis: A Rare Disorder
César Adán Almendárez Sánchez1, Raul Huato Reyes2, Saul Solorio Pineda2, Milton Inocencio Ruiz Flores2, Carlos Alberto Tevera Ovando2, and Jorge Ortega Espino2
1Centro Médico “Lic. Adolfo López Mateos,” Instituto de Salud del Estado de México, Toluca, Mexico
2
Introduction: Idiopathic hypertrophic spinal pachymeningitis (IHSP) is an infrequent condition that produces diffuse or localized thickening of the dura mater due to inflammatory fibrosis, which may evolve to the compression of the spinal cord with unknown etiology. Material and Methods: A 66-year-old woman presented by paraesthesia in lower extremities associated with progressive decreased muscle strength of 6 months of evolution, causing difficulty walking. There was no history of trauma or some other antecedent of importance for the current condition. On physical examination, we found spastic paraparesis in pelvic members with increased muscle stretch reflexes and paraesthesia from T10 to caudal. No alteration in upper limbs was found. MRI (magnetic resonance imaging) of the spine showed a long intradural extramedullary lesion of low T2 signal intensity in the thoracic region. The study with gadolinium showed homogeneous enhancement and thickening of the dura mater, extending from T2 to T10 with greater compression in T5 observed by tractography. Results: We performed decompressive T5-T6 laminectomy and durotomy with T4-T7 posterior arthrodesis with transpedicular screws and biopsy of the lesion. Pathologic examination revealed fibrosis and chronic inflammation compatible with IHSP. The patient showed improvement of neurological symptoms with decompressive surgery and steroid therapy. Conclusion: Although IHSP is a rare disease, the clinical, radiologic, and pathologic findings are characteristics. Despite this, the IHSP remains an underdiagnosed condition that must be taken into consideration, due to decompressive surgery such as laminectomy may be helpful as well as postoperative steroid therapy.
P703: Is Anterior Column Support Needed Following Transpedicular Decompression for Metastatic Epidural Compression?
Eric Emanski1, Avionna Baldwin2, Robert Molinari2, and Addisu Mesfin2
1University of Rochester Medical Center Rochester, NY, USA
Introduction: Patients with metastatic epidural compression often present with neurological deficits and need prompt decompression and stabilization. A transpedicular decompression (TPD) can provide sufficient debulking of the epidural disease that is often situated ventral to the dura. Our objective is to evaluate the outcomes and complications rates following TPD for metastatic epidural compression. Material and Methods: Patients with metastatic spine disease undergoing TPD with posterior segmental instrumentation at a level I trauma center were identified. All patients had symptomatic metastatic epidural disease. The study period was March 2011 to August 2017. Patients were operated on by 2 orthopedic spine surgeons. Demographic information, surgical data (estimated blood loss [EBL], length of surgery, level of TPD, levels instrumented, tumor histology, post-operative complications) were recorded. Results: Thirty-six patients undergoing TPD without anterior column support were identified. There were 12 females, 24 males, average age of 67.2 (46-87). TPD was performed in 26 thoracic lesions, 9 lumbar lesions, and 1 cervical/thoracic lesion. Average of 5.24 levels (2-10) were instrumented and in 5 cases (13.9%) MIS (minimally invasive surgery) screws with open TPD was performed. Average EBL was 725.6 mL, surgical length was 198.1 minutes and average hospital stay was 11.7 days. Common histology included lung (n = 9), prostate (n = 6), breast (n = 5), multiple myeloma (n = 3), renal cell (n = 3), and melanoma (n = 2). Surgical complications included 3 surgical site infections (8.3%), there were no (0%) revisions needed for implant failure. At latest follow-up 12 (33%) were alive, average length of survival was 12.5 months (0.5-70 months). Conclusion: Patients with symptomatic metastatic epidural disease may need debulking of the lesion, often ventral to the thecal sac, in order to preserve neurological function. Although in selected cases there may be a role for anterior column support, we have demonstrated that posterior segmental instrumentation only along with TPD can be performed without a risk of instrumentation failure or need for revision surgery.
P704: Surgery for Spinal Metastases in Patients Surviving Less Than 3 Months: Is It Worthwhile?
Anne Versteeg1, Nicolas Dea2, Arjun Sahgal3, Laurence Rhines4, Daniel Sciubba5, James Schuster6, Michael Weber7, Aron Lazary8, Stefano Boriani9, Chetan Bettegowda5, Michael Fehlings10, Michelle Clarke11, Paul Arnold12, Ziya Gokaslan13, and Charles Fisher2
1University Medical Center Utrecht, Utrecht, Netherlands
2University of British Columbia and Vancouver General Hospital, Vancouver, British Columbia, Canada
3Sunnybrook Odette Cancer Centre and University of Toronto, Toronto, Ontario, Canada
4The University of Texas MD Anderson Cancer Center, Houston, TX, United States
5Johns Hopkins University, Baltimore, MD, USA
6Hospital of the University of Pennsylvania, Philadelphia, PA, USA
7McGill University and Montreal General Hospital, Montreal, Quebec, Canada
8National Center for Spinal Disorders and Buda Health Center, Budapest, Hungary
9IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
10University of Toronto and Toronto Western Hospital, Toronto, Ontario, Canada
11Mayo Clinic, Rochester, NY, USA
12The University of Kansas Hospital, Kansas, KS, USA
13Brown University and Rhode Island Hospital and The Miriam Hospital, Providence, RI, USA
Introduction: Historically, a life expectancy of at least 3 months is considered necessary for patients to be considered for surgical treatment of spinal metastases. The purpose of this study was to compare health-related quality of life (HRQOL) outcomes in patients surviving ≤3 months after surgical treatment for spinal metastases to patients surviving >3 months. Materials and Methods: Patients who underwent surgical treatment for spinal metastases between August 2013 and May 2017, were identified from an international prospective observational cohort study. Demographic, histologic, treatment, adverse event, survival, and HRQOL data were collected. HRQOL was evaluated using the numerical rating scale (NRS) pain score, EQ-5D-3 L, and the Spine Oncology Study Group Outcomes Questionnaire (SOSGOQ2.0) at 6, 12, and 26 weeks postsurgery. Results: A total of 219 patients were identified; 37 patients died within the first 3 months after surgery and 182 patients survived more than 3 months. Of the patients surviving <3 months, 16 died within the first 6 weeks postsurgery. Patients surviving ≤3 months after surgery presented more often with lung cancer (P < .001), a higher grade of epidural spinal cord compression (P = .002), lower baseline ASIA (American Spinal Injury Association) scores (P < .001), and lower baseline HRQOL scores as compared with patients surviving >3 months. At 6 weeks postsurgery, patients surviving ≤3 months experienced a 1.4-point decrease (P = .445) in NRS pain scores compared with a 2.6-point decrease (P < .001) in patients who survived >3 months. Nonsignificant improvements in HRQOL at 6 weeks postsurgery were observed in patients who survived ≤ 3 months, while significant improvements were observed in patients who survived >3 months. Conclusion: The effect of surgical treatment for spinal metastases on HRQOL in patients surviving ≤3 months is not as profound as the effect observed in patients surviving >3 months. Yet, the small number of patients surviving <3 months should be taken into account when interpreting the results.
P705: Differential Surgical Treatment of Craniovertebral Tumors
Roman Khalepa1, Klimov Vladimir1, Vladislav Kelmakov1, and Murodzhon Kosimshoev1
1Federal Neurosurgical Center, Novosibirsk, Russian Federation
Introduction: The craniovertebral junction is a funnel composed of the clivus and foramen magnum and the upper 2 cervical vertebrae that acts as a biomechanical unit. Neoplasms that arise within the craniovertebral junction comprise osseous tumors, extensions from the soft tissue that surround the region and neoplasms of nervous system structures. There are posterior, lateral, anterior approaches to the craniovertebral area for the removal of these tumors. The use of these approaches should be differentiate depending on the location of the tumor and its relationships to the spinal cord and blood vessels. Material and Methods: From 2013 till 2018, 45 patients (16 males and 29 females) were provided surgical treatment. Average age was 52 years. Assessment of the neurological status was performed by the ASIA scale (American Spinal Injury Association) and functional status was performed by McCormick scale. MRI (magnetic resonance imaging), CT (computed tomography) angiography were performed to determine the size, location of tumors, and their relationships to the spinal cord and vertebral arteries. To determine the instability, the SINS (Spinal Instability Neoplastic Score) scale was used. Surgery: far lateral approach used for ventral and ventrolateral extramedullary tumors or vertebral tumors 21 (47%), transoral approach used in case of ventral vertebral tumor—1 (2%), median posterior approach with lateral extension used in cases of intramedullary and extramedullary dorsolateral tumors—23 (51%). Results: Clinical outcomes were estimated according to McCormic and ASIA scales. Average McCormic before surgery 1.8 ± 0.6, after surgery 1.7 ± 0.8, and in 1.5 year 1.6 ± 0.8. ASIA before surgery E 13; D 26; and C 4; after surgery E 12; D 29; C 3; and B 1, and in 1.5 year E 13, D 31; C 1; and B 0. Gross total resection 40 (28 extramedullary tumors, 8 vertebra tumors, 4 intramedullary), and subtotal 5 (4 vertebra tumor, 1 extramedullary). Histology: ependymoma 1; cavernous angioma 2; hemangioblastoma 1; schwannoma 11; meningioma 12; neurofibroma 6; chondrosarcoma 1; plasmacytoma 5; metastasis of adenocarcinoma 4; chordoma 1; and osteoma 1. Complications: infection of the surgical site 1 case; pseudomeningocele 3; and neurological deterioration 1. Follow up 1.5 years. Three patients died: 1 neurofibroma (concomitant pathology, myocardial infarction) in 6 months after surgery; 1 chondrosarcoma, continued growing (refusal to reoperation) in 12 months after surgery; and 1 metastasis of adenocarcinoma (progression of the underlying disease) in 6 months after surgery. Conclusion: The differentiated application of various surgical approaches ensures the achievement of good functional results.
P706: Upper Cervical Corpectomy: Outcomes and Complications
Addisu Mesfin1, Wajeeh Bakhsh1, and Emmanuel Menga1
1University of Rochester Medical Center, Rochester, NY, USA
Introduction: Cervical corpectomies are often performed to treat cervical spondylotic myelopathy (CSM), cervical spine trauma, infection, and tumors. Cervical corpectomy of C3 and/or C4 is uncommon and reported sparsely in the literature. Due to the anatomy of the upper cervical spine, there are unique complications to this region as well as increased risks of dysphagia. The objective was to describe our tertiary referral center’s outcomes and complications following upper cervical corpectomy. Materials and Methods: Using a surgical database maintained by the first author, all patients undergoing anterior cervical spine procedures from November 2012 to November 2017 at a level I trauma center and regional cancer center were identified. Patients undergoing C3 and/or C4 corpectomies with a follow-up of greater than 30 days were enrolled. Demographic information (age, sex, race/ethnicity), diagnoses, ASIA (American Spinal Injury Association) grade, surgical data (levels fused, estimated blood loss (EBL), posterior stabilization, length of hospital stay, discharge status) as well as complications (intraoperative and postoperative) were collected. Results: A total of 162 patients undergoing anterior cervical procedures over the 5-year study period were identified. Nine of 162 (5.6%) underwent upper cervical corpectomies. Four out of 9 (44%) had C3 corpectomy, 1 out of 9 had a C3 and C4 corpectomies (11%), and 3 out of 9 (33%) had a C4 corpectomy and 1 out of 9 had a C4 and C5 corpectomies (11%). Average age was 55.3 years (16-75), 5 males and 4 females with 7 Caucasians and 2 African-Americans. Diagnoses were the following: 3 tumors (endometrial, prostate, lymphoma), 2 fractures, 2 CSM, 1 central cord syndrome and 1 osteomyelitis. Five of 9 procedures were performed on an emergent manner due to neurological deficits or instability. ASIA grade was the following: E (5), D (3), and B (1). An average of 3.4 levels were fused with an average EBL of 216.7 mL (25 mL-800 mL). Six of the 9 (66.7%) had either a staged or same day posterior cervical fusion/instrumentation. Average hospital stay was 6.8 days and 4 of 9 patients were discharged to rehabilitation. There were no intraoperative complications. Three patients had the following postoperative complications: Patient 1: C3 corpectomy (fibula strut graft dislodgement, dysphagia requiring temporary PEG tube); Patient 2: C3 corpectomy (PE [pulmonary embolism], anterior cervical hematoma requiring evacuation arising from anticoagulation); Patient 3: C3 corpectomy (temporary marginal mandibular branch of facial nerve neuropraxia manifesting as ipsilateral lip drooping). Two of the 3 patients with tumors passed away at latest follow-up (average 16.5 months post-operative). C3 corpectomy had a significantly higher rate of complications compared with the other approaches (P = .01). Conclusion: In this series, upper cervical corpectomy was commonly performed in patients with tumors, fractures, and CSM. Six of 9 patients had no intraoperative or postoperative complications. A significantly higher rate of complications (P = .01) was noted in patients undergoing C3 corpectomy.
P707: Multidisciplinary Management of Benign Aggressive Vertebral Hemangiomas in a Hybrid Operating Room: A Case-Series
Marco Corniola1, Claudio Schonauer2, Gianmarco Bernava3, Paolo Machi3, Hasan Yilmaz3, Karl Schaller1, and Enrico Tessitore1
1Geneva University Hospitals, Geneva, Switzerland
2Santa Maria delle Grazie Hospital, Naples, Italy
3Geneva University Hospitals, Geneva, Switzerland
Introduction: Vertebral hemangiomas account for 2% to 3% of all spinal tumors. The majority are asymptomatic and incidentally identified on radiographic studies. Approximately 1% become symptomatic and may present with pain and/or neurologic deficits. Our aim was to report the multidisciplinary treatment of symptomatic aggressive hemangiomas in a hybrid operating room. Material and Methods: Aggressive hemangiomas treated with a combination of presurgical embolization, surgical decompression and intraoperative sodium tetradecyl sulfate (Trombovar) administration were retrieved. Clinical and radiological data were retrospectively analyzed. This study was approved by the local ethics committee (IRB approval 2018-01108). Results: Six patients were included, with a mean age of 53 years. Three patients presented with a chronic, progressive myelopathy, 2 patients presented with a rapidly progressing myelopathy requiring urgent decompression and 1 patient presented with isolated dorsal pain without associated deficit. Five patients had subtotal resections, and 1 patient had an “en bloc,” complete resection of the lesion. Five patients had blood losses inferior to 500 mL. The mean follow-up length was of 9 months: 1 patient developed postoperative upper segmental kyphotization, 1 patient developed anemia, 1 patient developed atrial fibrillation and one patient developed postoperative seroma. Patients with subtotal resection had no evidence of radiological progression of the remaining lesion up to date. Conclusion: The combined multidisciplinary approach of aggressive thoracic VH, including the intraoperative sclerotization of the tumor is a safe and effective procedure when performed in a dedicated hybrid room.
P708: Advance of Cancer Treatment Change the Surgical Strategy for Vertebral Metastasis
Toshiaki Hitora1, Kanji Sasaki1, Mizuki Watanabe1, Ushio Nosaka1, Tetsutaro Mizuno1, and Keiji Ishii1
1Seirei Hamamatsu General Hospital Spine Center, Hamamatsu, Japan
Introduction: Including molecular target treatments, the advance of cancer treatments is widely spreading, and these therapies change life prognoses radically. Accordingly, quality of life (QOL) is moreover important and mortgage of keeping motion of extremity and/or pain free is also preferred. Aims of surgical treatments for metastatic spinal tumors are mainly to improve intolerable pains and to avoid spinal cord injury. However, for life time aspect, there is much space to discuss whether surgical treatments are better or not. From 2013, we accepted the patients with vertebral metastasis and underwent surgical treatment. The purpose of this study is to investigate the efficacy for symptomatic metastatic spinal tumor (life prognosis, pain scale, paralysis and complications) and reveal the value of surgical treatment. Materials and Methods: Sixty-two cases of vertebral metastasis (males 32 and females 30; mean age: 65 years old) had surgical treatment from 2013 to 2017. We adapted the surgeries for the patients with spinal cord injury or with highly possibility of spinal cord injury and/or the patients with severe pains. Average follow-up period was 14 months (1-60 month). Primary lesions were 15 cases: lung, 10 cases: breast, 8 cases: prostate, 5 cases: rectal cancer, 4 cases: thyroid and liver, 3 cases: pancreatic and uterus, 2 cases: bladder and lymphoma, and each one case: others and unknown origin. Operative time, amount of bleeding, complications, and prognosis were investigated. Preoperative and postoperative pain and paralysis were evaluated by numerical rating scale (NRS) and Frankel classification. As the life prognosis predictive factor, Tokuhashi’s score in each case was evaluated and compared with actual prognosis. Results: Operative time was 144 (51-288) minutes. Total amount of surgical bleeding was 614 (5-2255) mL. All the cases had posterior (to vertebral) decompression and/or fusion. And we did not do total en bloc spondylectomy. There was no fatal case caused by perioperative complications. Thirty-nine cases were died at the time of investigation and the mean period in these cases was 9.7 (1-33) months. The mean preoperative NRS was significantly improved (pre 6.8 to post 2.5). Fifty-eight cases (94%) showed improvement in NRS. Preoperative Frankel’s classification was follows; A 4 cases, B 4 cases, C 9 cases, D 13 cases, and E 32 cases. Frankel A 4 cases were not improved, but B: only one case (75% improved), C, D, and E were1, 7, 15, and 35 cases. There were no cases of functional deterioration at surgical periods. There were 40 cases of less than 9 points in Tokuhashi’s score, which were usually regarded to poor prognosis. Of these, 9 cases survived at the time of investigation. Furthermore, 19 of these 40 fatal cases survive more than 9 months. Conclusions: In present study, surgical treatments could improve QOL especially in pain. No fatal complications occurred. But the patients with Frankel A were not improved. Half of the patients survived longer than expected by Tokuhashi’s classification. These results suggest that we must adapt the surgical strategies with the advance of the cancer treatments and we should do decompression and fusion before complete paralysis.
P709: Minimally Invasive Spine Surgery and Total 3D Navigation for Extra- and Intradural Extramedullary Spinal Tumors
Sertac Kirnaz1, Franziska Schmidt1, Christoph Wipplinger1, and Roger Härtl1
1Weill Cornell Medicine, New York, NY, USA
Introduction: The resection of extradural and intradural extramedullary spinal tumors using minimally invasive spinal surgery (MISS) techniques has been shown to be safe and effective. Compared with traditional open surgery, MISS techniques may reduce complications and morbidity in appropriately selected patients. Using a portable intraoperative CT (computed tomography; iCT) scanner combined with state-of-the-art total 3D computer navigation offers more precise navigation in MISS, favors reduction of radiation exposure for the surgical staff and enhances efficient and reproducible workflows. In this study, we described our experiences on MISS approach for the removal of extradural and intradural extramedullary spinal tumors using 3D total navigation. Material and Methods: We demonstrate the step-by-step surgical technique for microsurgical resection of extradural and intradural extramedullary spinal tumors via utilization of a portable intraoperative CT for stereotactic localization and 3D navigation-guided planning of incision, screw implantation, and placement of tubular retractors. Results: We provided outcomes of 15 patients (10 lumbar, 3 thoracolumbar, 2 thoracic) who underwent surgery between May 2015 and December 2017. Twelve patients had an intradural extramedullary tumor, 9 had schwannomas, 2 had meningiomas, and 1 had myxopapillary ependymoma; 3 patients had an extradural intraforaminal schwannoma. Mean age of patients was 54.9 years and average follow-up time was 5.8 months. No intraoperative or postoperative complications were observed. Conclusion: Using navigation for spinal procedures trough tubular retractors optimizes pathology localization and implant placement. Both extradural and intradural extramedullary tumors can be safely and effectively removed by minimally invasive techniques using 3D total navigation.
P710: Surgical Management of a Spinal Intradural Arachnoid Cyst With Cyst-to-Peritoneal Shunt: Case Report and Review of the Literature
Pedro Coutinho1, Michael Paci2, Andrew Fanous2, and Glen Manzano2
1Yale University, New Haven, CT, USA
2University of Miami, Miami, FL, USA
Introduction: Spinal intradural arachnoid cysts are rare entities, which consist of cerebrospinal fluid (CSF)-filled sacs lined by arachnoid membranes, and may be either idiopathic or acquired. Primary arachnoid cysts are defined as those not associated with trauma or inflammatory insults. Secondary arachnoid cysts result of inflammatory reactions related to trauma, subarachnoid hemorrhage, meningitis, intradural surgery, or instillation of substances into the subarachnoid space. Patients diagnosed as having intradural arachnoid cysts of the spine can be managed either conservatively or surgically, depending on their clinical presentation. For those who require surgical intervention, the gold standard for treatment is laminectomy or laminotomy at the affected site followed by cyst excision or fenestration. Material and Methods: We provide a thorough review of the literature regarding diagnosis and treatment of spinal arachnoid cysts. We further present a case report of a patient who required surgical treatment but refused to undergo extensive multilevel laminectomies. That is the first time a cyst-to-peritoneal shunt is reported as a primary treatment for this entity. Results: A 28-year-old female presented with stabbing pain in the right lumbar paraspinal region along with intermittent right posterior thigh burning pain. She had persistent right anterior thigh numbness and tingling, as well as stabbing pain radiating to the shin and ankle. There was progressive right quadriceps weakness and urinary urgency. A thoracic MRI (magnetic resonance imaging) was performed showing an intradural multilevel arachnoid cyst causing cord compression. Surgical treatment was indicated, however, the patient refused undergo multilevel laminectomies. She was primary treated with a cyst-to-peritoneal shunt with complete postoperative neurological recovery. Conclusion: Patients diagnosed with spinal arachnoid cyst and overt spinal cord compression should be considered for surgery. Complete neurosurgical resection remains the treatment of choice for symptomatic patients. However, primary cystoperitoneal shunting should be part of the spine surgeons’ armamentarium, particularly in cases where multilevel laminectomies need to be avoided.
P711: C3 Cervical Spine Osteoblastoma Complicated With Secondary Aneurysmal Bone Cyst in an Adolescent Patient: Case Report
Nitesh Gahlot1 and Divesh Jalan1
1All India Institute of Medical Sciences (AIIMS), Jodhpur, India
Introduction: We report here a rare combination of aggressive osteoblastoma with secondary aneurysmal bone cyst masquerading as neck pain, arising from cervical C4 vertebra in a 19-year-old male. Material and Methods: The patient was a 19-year-old male presented to us with complaints of neck pain since past 7 months, gradual in onset, dull aching, and progressively increasing in severity. A diffuse, nonfluctuant, slightly tender swelling was noted on posterior aspect of neck deep to the posterior neck muscles. Neck movements were restricted due to pain. Neurology was normal, with no radiation symptoms or deficit. Detailed radiology was done (CT [computed tomography] and MRI [magnetic resonance imaging]), suspected tumor was seen arising from the posterior elements of C4 vertebra involving the left facet. After preoperative planning, tumor was removed en bloc posteriorly and intralesional anteriorly. Lateral mass screws and fusion was done from C3 to C5 for stability. Histopathology confirmed the radiological diagnosis. Postoperatively patient recovered well, sitting and walking with collar was started on second postoperative day. No recurrence has been seen on 1 year follow-up. Results/Discussion: Osteoblastomas originating in the cervical spine have been reported by many authors. But osteoblastoma associated with secondary aneurysmal bone cyst is rare diagnosis and only a few care reports exist in literature. Our case is also unique due to the benign clinical presentation with no neurological symptoms, making it an important differential while treating young patients with long standing refractory neck pain. Complete removal of tumor was attained via posterior approach, followed by spinal fusion as tumor had eroded into the lateral mass of C3 and C2 vertebrae. Conclusion: Being a rare disease, cervical osteoblastoma with secondary aneurysmal cyst should be kept in differential, while treating a case of neck pain in adolescent age patient and prompt and planned surgery is essential.
P712: Benefits of Structural Femoral Shaft Allografts for Anterior Spinal Column Reconstruction After ThXII Metastatic Spinal Lesion
Andras Bank1, Peter Endre Eltes1, Magor Zoltan Gyorgy1, Zoltan Hoffer1, and Peter Pal Vagra1
1National Center for Spinal Disorders, Budapest, Hungary
Introduction: Total en bloc spondylectomy is a challenging surgical technique for primary and metastatic spinal lesions that requires a significant experience in spine surgery. The anterior column can be reconstructed using a variety of implants: structural femoral shaft allograft, polymethyl methacrylate block, mesh cage, and expandable cages from different materials (polyether ether ketone, carbon fiber reinforced polymer, titanium alloy). Currently, however, the choice of the implants is still a matter of debate, due to the lack of comparative studies related to the benefits of the different implants and reconstruction methods from surgical, economical, and biomechanical perspective. We present the first case from a prospective investigation in which we will compare different reconstructions options. Materials and methods: We present a case report with 6-month follow-up. We performed computer aided preoperative planning based on the preoperative CT scan. We defined the 3-dimensional (3D) geometry of the affected vertebra and the neighboring vertebras using segmentation algorithm and we performed distance, volume, and surface measurements on the geometries. Results: A female patient (48 years) presented with intermittent costal, back, and low back pain. Her medical history revealed left side ductal carcinoma (Gr, II. Her2+), which was treated surgically and oncologically (chemotherapy, radiotherapy) 7 years earlier. The oncological follow-up showed no recurrence; however, her current imaging studies (PET/CT, MRI) describe a solitary bone lesion in the ThXII vertebra of mixed (lytic/blastic) characteristics affecting the vertebral body and the right pedicle. The vertebral body is not collapsed and is in normal radiological alignment. Spinal Instability Neoplastic Score (SINS) of the lesion was 10. Based on the 3D geometries of the segment, we decided to perform a ThXII total en bloc spondylectomy with ThX-LII stabilization. The anterior column reconstruction was performed with a structural femoral shaft allograft. The size and the shape of the grat was also determined from the 3D in silico model. Autologous bone from resected ribs and articular processes were packed into the middle of the femoral shafts prior to its implantation. The surgery was performed successfully as planned, and the patient showed no neurological deficits after surgery. The postoperative, 3 months follow-up and 6 months follow-up standing X-ray and CT scan images showed no sign for subsidence, implant failure, or kyphotic deformity. Conclusion: We used 3D virtual geometry and computer-aided planning to develop the optimal surgical technique, which was performed successfully. We plan to carry out Finite Element Analysis (FEA) studies based on the preoperative and postoperative CT scans, to measure the fusion rate, and the mechanical stability of the reconstruction methods. This case is part of a prospective study comparing these measures between several reconstruction methods with the aim to test the benefits of different technologies/implants.
P713: Early Postoperative Neurologic Changes in Pediatric Patients With Malignant Spinal Tumors
Denis Malamashin1, Margarita Belogurova2, Svetlana Kuklina1, and Aleksandr Mushkin1
1Saint-Petersburg Research Institute of Phthisiopulmonology, St-Petersburg, Russian Federation
2Saint-Petersburg Cities Oncological center, St-Petersburg, Russian Federation
Introduction: Malignant spinal tumors in pediatric patients are rare and frequently diagnosed due to severe back pain or neurological disorders. The aim is to study the changes in patients’ neurological status during early postoperative after decompressive and reconstructive surgery in pediatric patients with malignant spinal tumors. The follow-up period was limited by 30 days because it most important for improvement after mechanic decompressive procedure in contrast with ischemic myelopathy. Material and Methods: Thirty-two patients (18 girls, 14 boys) aged from 1 year 6 months till 17 years (8.5 years in average) underwent spinal surgery (spine reconstruction) due to malignant spinal tumors. The causes for surgery were non-Hodgkin and Hodgkin lymphomas (7 and 2 patients corresponding), Ewing sarcoma (10), other form of sarcoma (6), PNET (4), malignant histiocytosis, extrarenal rhabdoid tumor, and myxopapillary ependymoma (1 case for every). All cases surgery was a stage of complex therapy; the indication for surgery were neurological or orthopedic complications of spinal tumors. Neurological symptoms studied by Frankel scale before surgery and 30 day after operation (this period is most effective for changes after disappears of mechanical compression for spinal cord). Results: Twenty-one patients (67.7%) had motor dysfunction before surgery, including 10 (31%) with severe complication according Frankel scale (types A-C): types A 1, type B 1, type C 8, and type D 11. Only 11 patients had no neurological disorders (11 patients). Thirty days after surgery nobody had neurological deterioration. The positive changes registered in 14, including types A and B 1 case for every type, type C and D 6 cases for every type. It was not improvement in 2 patients who had severe complications (types B and C) and in 5 with initial type D. All patient who has positive dynamic can improved neurological status only for 1 step by Frankel scale. Conclusion: Pediatric patient with malignant spinal tumors complicated by neurological disorders had a high chance to improve their conditions after surgery. The spinal cord decompression and spinal reconstruction significantly improve general patient’s condition. However, within 30 days after surgery improvement of motor functions is noted only on 1 level of Frenkel scale despite the level of initial disorders.
P714: Tethered Cord Syndrome in Adult: Experience of 12 Cases and Review of Literature
Soichiro Takamiya1, Toshitaka Seki1, Kazutoshi Hida2, and Kiyohiro Houkin1
1Hokkaido University Hospital, Sapporo, Japan
2Sapporo Azabu Neurosurgical Hospital, Sapporo, Japan
Introduction: Tethered cord syndrome (TCS) commonly discovered in childhood with various neurological symptoms and is usually associated with spinal dysraphism. TCS in adult is a relatively rare condition, although it seems more frequent than once thought, and it sometimes leads to a delay in diagnosis and treatment. Therefore, it is important for us to recognize clinical features of adult TCS to diagnose and treat in their early stage. We report on 12 adult cases with TCS and summarize them and case series reported previously. Material and Methods: We retrospectively reviewed adult patients (more than 18 years old) with TCS who had been diagnosed and undergone untethering at Hokkaido University Hospital from January 1996 to August 2018. Results: This study includes 12 adult patients with TSC. The average age at diagnosis was 37.8 years (from 22 to 62 years). The frequent symptoms were urinary complains (91.7%), sensory disturbance (83.3%), and weakness of leg (58.3%). Low back pain was less than other previous studies. Pain and sensory disturbance improved postoperatively in 75% and 70%, in contrast urinary problems never improved at all. The improvement of symptoms was not always associated with duration of the symptoms in this study. Conclusion: Low back pain and sensory disturbance in adult TCS patients tended to improve by untethering in this study. However, it was difficult to improve urinary dysfunction. Early surgery is recommended to prevent irreversible neurological deficits, yet some symptoms sometimes improve even if their duration are long.
P715: Surgical Treatment of Spinal Litic Lesions in Patients Affected by Malignant Hematologic Diseases
Stefano Telera1, Laura Raus1, Francesco Crispo1, Francesco Pisani1, Svitlana Gumenyuk1, Daniela Renzi1, Francesca Palombi1, Melina Castiglione1, Atelda Romano1, and Riccardo Boccaletti1
1IRCCS Istituto Nazionale Tumori Regina Elena, Rome, Italy
Introduction: Medical treatment of patients affected by malignant hematologic diseases has allowed in the last 20 years, striking results in terms of overall survival. Nevertheless, these patients often present a decrease of quality of life (QoL) due either to direct spinal involvement by the tumor, or to damages to the vertebral column induced by prolonged pharmacologic therapies, chemotherapy and radiotherapy. The role of neurosurgeons in the multidisciplinary management of these conditions has been progressively increased due to availability of new instrumentations and materials for complex spinal instrumentation, and the option to combine traditional surgical decompressive techniques of the spinal cord and spinal roots with minimally invasive approaches, as vertebro- or kyphoplasty or percutaneous fixation. The different surgical options currently available must be wisely tailored to the general and neurologic conditions of the patient. Material and Methods: The results of spinal surgery in 146 patients affected by multiple myeloma, plasmacytoma and lymphoma, operated at “Regina Elena” Institute, between 2005 and 2017, have been analyzed. Karnofsky (KPS), visual analogue scale (VAS), and Dennis Pain Score were calculated preoperatively and postoperatively and at the last follow-up. Neuroradiological investigations were reviewed. Results: Overall 107 kyphoplasty-vertebroplasty (22 open procedures combined with laminectomy), 19 open biopsy and laminectomy, 12 laminectomy and posterior stabilization, and 8 somatectomy have been performed. Follow-up was available for 129 patients (12-68 months). A significant improvement was observed in KPS, VAS, and Dennis Pain Score in 92% of cases right after surgery. Mean hospital stay was 7 days. The effect of surgery on pain control (combined with other treatments) and on prevention of neurologic dysfunction was maintained over the FU period: 79% of patients without localized pain; 21% still taking medication at the last interview. Major complications included 4 patients who suffered for postoperative hematomas. One postoperative death occurred. The overall survival was 38 months. Three cases of instrumentation failures occurred, during the FU period, which required reoperation. Conclusion: Symptomatic metastatic spine disease (MSD), related to hematological tumors is a challenging pathology involving up to 15% of patients with such bone lesions and require prompt recognition. The role of early surgery for treatment of patients with spinal lesions due to hematologic diseases appear absolutely relevant allowing to (1) confirm histologic diagnosis and/or tumor staging, particularly in controversial cases, (2) an effective and tailored treatment with a reduced morbidity and mortality, even in patients with multiple vertebral localization, (3) to prevent dismal neurological consequences due to vertebral collapse and spinal cord compression, (4) to maintain a good QoL in long survivors and (5) to allow a rapid access to adjuvant therapies particularly radiotherapy, since these are very radiosensitive tumors.
P716: Can SpineSage be Used as a Tool Predicting Complications in En Bloc Spinal Resections for Primary Tumors?
Marcin Czyz1, Muaaz Tahir1, Simon Hughes1, Petr Rehouzek1, and Mel Grainger2
1The Royal Orthopaedic Hospital NHS Trust, Birmingham, UK
2 University Hospitals of Birmingham NHS Foundation Trust, Birmingham, UK
Introduction: SpineSage is an online tool that provides estimated risk of postoperative complications based on the patient’s comorbidities and invasiveness of the proposed spine procedure. To our knowledge this model has not been externally validated in patients who undergo invasive en bloc resections of the spinal column. This study aims to validate the use of SpineSage in en bloc resections for primary spinal neoplasms. Material and Methods: We performed a retrospective review of operative, anesthetic, and medical notes of consecutive patients who underwent en bloc spinal resections at a single institution between 2007 and 2014. Patient demographics and comorbidities were noted along with any major or minor complications occurring in the immediate postoperative period. Surgical Invasiveness Index (SII) and predicted rate of complication were retrospectively calculated by a blinded assessor using the SpineSage criteria. The validity of SpineSage as a predictive model (ie, its ability to discriminate well between those participants who did and did not have a complication) was measured as the area under the ROC (Receiver operating characteristics) curve (AUC [area under the curve]). The interrater agreement statistic (κ) was calculated. Results: Thirty patients met the inclusion criteria, median age 40 years (21 males, 9 females), of whom 5 were excluded due to missing data. Indications for surgery were as follows: chondrosarcoma (n = 13), chordoma (n = 6), Ewing’s sarcoma (n = 3), osteosarcoma (n = 1), osteoblastoma (n = 1), and chondroma (n = 1). Sixteen patients experienced at one or more postoperative complications (24 minor and 1 major complications in total). The AUC value was 0.80 (P = .015), (confidence interval [CI] 0.62-0.98), where a value 1 would indicate perfect discrimination. The weighted Kappa reached 0.82 (95% CI 0.71-0.93). Conclusion: Our results indicate that SpineSage can reliably predict complications following en bloc resections for primary neoplasms of the spine. This simple characterized by very high interrater agreement tool may help clinicians provide more accurate prognostic information to patients in the preoperative stage. These results, however, require further validation in larger cohorts.
P717: Complications in En Bloc Resections of Primary Tumors in the Thoracic Spine: Systematic Review
James Holton1, Marcin Czyz1, Okezika Uhiara1, Petr Rehouzek1, Simon Hughes1, Alistair Stirling1, Morgan Jones1, and Mel Grainger2
1The Royal Orthopaedic Hospital NHS Trust, Birmingham, UK
2University Hospitals of Birmingham NHS Foundation Trust, Birmingham, UK
Introduction: En bloc spondylectomy remains a relatively infrequent procedure usually undertaken for primary spinal tumors and occasionally truly isolated metastases with curative intent, ideally performed in highly specialized spinal centers. For a surgeon counseling a patient and his family for a potentially life changing procedure, it would be useful to have available information specific to the anatomical level of the planned operation, which is not currently available. Our objective is to systematically review the literature of en bloc resections of primary malignancy of the thoracic spine focusing on the surgical techniques, complication, and associated morbidity and mortality. Material and Methods: A systematic review of the literature was conducted using the PubMed, Cochrane Library database, and Medline OVID database with suitable articles being assessed with the PRISMA checklist 2009. Articles with less than 5 patients or focusing solely on cervical, lumbar, and sacral pathology were excluded. Results: Review of the literature revealed 7 small retrospective studies containing 54 patients. Mean-reported age of the subjects was 40 years. The minimum follow-up period was 10 months. Disease recurrence occurred in 13% (7/54). Mortality occurred in 6 patients (11%, 6/54). Of the reported deaths, 4 patients had marginal resection and 2 were intralesional highlighting the importance of clear margins. Only 4 studies reported complications specific to en bloc resection of the thoracic spine at 68.2%. Conclusion: En bloc resection of the thoracic spine is an infrequent but complex procedure with high associated morbidity. Surgery should be focused at designated units with surgical and anesthetic teams who frequently manage these patients alongside the required postsurgical rehabilitation services. There is a need for larger studies with clear reporting of complications relative to the specific spinal level of disease to quantify risk and associated morbidity from en bloc resection.