Abstract
Introduction
Abnormalities in the elbow range of motion (ROM) can be subtle; therefore, it is important that the examiner can compare findings with reliable reference values, matching the patients’ characteristics. Primarily, we aimed to provide normative values for the elbow ROM in subpopulations based on age, sex, dominance and body mass index (BMI). The secondary objective was to determine intra- and inter-rater reliability.
Methods
aROM (active range of motion) and pROM (passive range of motion) were measured bilaterally in healthy adults using a universal goniometer. The influence of factors affecting the ROM was calculated using Pearson’s correlation coefficient. In two samples of subjects, intra-rater and inter-rater reliability were determined.
Results
The study population (n = 352) consisted of 47.2% male and 52.8% female subjects. For aROM (dominant hand), mean flexion was 146°, extension –2°, pronation 80° and supination 87°. Male subjects had smaller ROM compared to females (p < 0.001). Differences between dominant and nondominant hand were less than one degree. pROMs were 3° to 5° larger than aROMs (p < 0.001). Intra- and inter-rater reliability was good.
Conclusions
Elbow ROM is influenced by age, sex and BMI. In the general population, the ROM of the uninjured side can serve as a reference in case of an injured elbow.
Keywords: elbow, joint mobility, range of motion, normative values, reference values
Introduction
The elbow joint allows us to perform flexion–extension and pronation–supination movement. According to the literature, values for flexion lie between 130° and 154° and extension between –6° and 11°. Pronation varied from 75° to 85° and supination from 80° to 104°.1–6 Daily activities can be performed with an elbow extension restriction of 30° and minimal flexion of 130°, in combination with 50° of pronation and supination;7 more extensive activities such as handling a cell phone require more mobility.8,9 Sports activities also require a greater elbow range of motion (ROM); however, athletes are also prone to reduced elbow ROM, especially overhead throwing athletes. The literature shows that the flexion-extension range is decreased by approximately 14° in asymptomatic baseball pitchers2 and a significant decrease in passive elbow ROM in the first 24 h after throwing.10 Furthermore, overhead throwing athletes often also have a reduced shoulder ROM, which makes them prone for elbow injuries.11,12
Conversely, a restriction in elbow ROM will result in a greater load on the shoulder and wrist, causing injuries to those joints
Measuring the ROM is considered an integral part of physical examination for elbow pathology. Flexion is usually restricted by anterior soft tissues such as the biceps muscle, resulting in an elastic end-feeling. Pronation and supination also have an elastic end-feeling caused by ligaments, the interosseous membrane and forearm muscles.13 Extension, however, has a hard end-feel as a result of the olecranon pushing into the humerus. The end-feeling provides information on the cause of the ROM restriction.
To accurately measure the elbow ROM, the use of the universal goniometer comprises an easy, reliable and commonly used assessment method.3,6,14–18 ROM assessment is important for both acute injuries, chronic injuries and to evaluate the effectiveness of a treatment. Athletes are more prone to acute elbow injuries, mostly fractures (e.g. in gymnasts falling on an extended elbow). In traumatic injuries, elbow extension can be used as a sensitive clinical screening test for traumatic injuries. When the injured athlete has an unrestricted elbow extension, a fracture can be ruled out without an X-ray.19,20 Malunion, long period of immobilization and heterotopic ossifications following a traumatic injury are risk factors for elbow stiffness.
There are also a number of chronic overuse injuries, mostly in overhead athletes, resulting in ROM restrictions.21 For example loose bodies, chondromalacia, valgus extension overload syndrome, osteochondritis dissecans in children and osteoarthritis in elderly can decrease elbow mobility.22 Intra-articular fluid can also restrict motion, positioned in 70° of flexion, the pressure from intra-articular fluid and pain are lowest.23
Apart from initial assessment of the elbow, measurement of the ROM is a key element for evaluating the effectiveness of a treatment for elbow stiffness.
Previous studies have reported ROM measurements based on either small (under 50 subjects) or specific (e.g. athletes, injured or only one sex/dominant hand) study populations.1–6 Soucie et al.1 included a bigger study population but did not account for factors such as body mass index (BMI) and hand dominance, and only reported passive ROM.
To guide clinical decisions, it is important that reliable normative values are available and influencing factors are known. Therefore, the primary objective of the present study was to provide normative values for subpopulations based on age, sex, hand dominance and BMI. Also, correlations between ROM and age and BMI were be determined. Next to normative values for subpopulations, we aimed to provide standard values for passive ROM (pROM) and active ROM (aROM) of the elbow (i.e. flexion, extension, pro- and supination) for the total population.
Our secondary objective was to define intra-rater and inter-rater reliability of goniometric measurement of the elbow ROM and present this in a comprehensible way, aiming to facilitate interpretation of changes observed in the clinic.
Materials and methods
Study design
The present study assessed the ROM using a cross-sectional design. Data were collected from August 2015 to October 2015 and researchers were based in Onze Lieve Vrouwe Gasthuis (OLVG) hospital, Amsterdam, the Netherlands. Ethical approval was waived by the local ethical committee (WO15.069).
Study population
Subjects who were aged 18 years to 79 years and had volunteered to undergo a ROM examination were included. Subjects diagnosed with a disease or previous injury that could potentially affect elbow ROM on either right or left side were excluded. Volunteers were recruited at (pre-informed) public spaces and events, such as sports clubs/events, businesses, schools/universities, family/friends gatherings, supermarkets etc. An effort was made to include a minimum of 25 subjects in each age category as following: 18 years to 29 years, 30 to 39 years, 40 to 49 years, 50 to 59 years, 60 to 69 years and 70 to 79 years.
Data collection
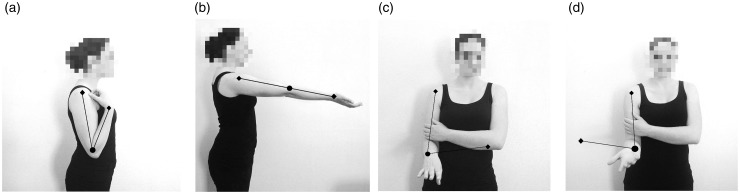
All subjects were examined by a clinician in the orthopaedic department (EZ), trained for elbow ROM measurements using a predefined protocol developed by two human movement scientists (NW, VS), an orthopaedic surgeon (MB) and a physiotherapist. For flexion and extension measurement, the acromion and radial styloid process were used as landmarks for the arms of the goniometer and the lateral epicondyle as the centre of rotation. Flexion was measured with 0° shoulder anteflexion and 0° abduction and a maximally supinated forearm. With the same forearm position and the shoulder in 90° anteflexion and 0° abduction, the extension was measured. In both measurements, the centre of rotation for pronation and supination was the ulnar styloid process and the arms of the goniometer were placed parallel to the humeral midline and dorsal or volar wrist respectively. Both measurements were taken with 90° of elbow flexion and manual fixation of the upper arm to the body. The shoulder and elbow position and landmarks for the goniometer positioning were based on guidelines and recommendations from previous literature.3,24–30 aROM was measured by asking the patient to make the movement as far as they could. pROM was measured with added support by the examiner in the direction of the movement. aROM and pROM were measured in both arms of each subject. Execution of ROM measurements with landmarks are presented in Fig. 1.
Figure 1.
(a) Flexion. (b) Extension. (c) Pronation. (d) Supination.
For each subject age (years), sex (male/female), height (cm), weight (kg) and hand dominance (right/left) were obtained. Subjects were not asked for any personal details and data was stored using anonymous consecutive study numbers.
For intra-rater reliability analysis, the range of motion of both elbows for 20 subjects was measured twice by the primary examiner within a time frame between 1 day to 7 days. To analyze the inter-rater reliability, both elbows of 10 subjects were measured by the primary examiner and a trained orthopaedic surgeon, who was blinded for the first measurement results. The first measurement by the primary examiner of these 30 subjects was also included in the final study. The subsequent 322 subjects were assessed once.
Statistical analysis
All data were collected using Excel 2010 (Microsoft Corp. Redmon, WA, USA) and analyzed using the Statistical Package for Social Science for Windows (SPSS Statistics, version 22; IBM Corp., Armonk, NY, USA). Before conducting the analyses, all data were double-checked by visual inspection and box-plots. p < 0.05 was considered statistically significant.
Normative values based on subgroups
An unpaired samples t-test was used to compare patients’ demographics and to compare ROM measurements between sex, age categories and BMI categories. Differences for dominant and nondominant arm were tested with a paired samples t-test. Subjects were divided in different age groups: 18 years to 29 years, 30 years to 39 years, 40 years to 49 years, 50 years to 59 years, 60 years to 69 years and 70 years to 79 years. BMI was divided into the categories < 18.5 kg/m2 (underweight), 18.5 to 24.9 kg/m2 (normal), 25.0 to 29.9 kg/m2 (overweight) and ≥ 30.0 kg/m2 (obese).31
Pearson’s correlation coefficients were calculated to determine the influence of the continuous parameters BMI and age on the elbow ROM.
Intra-rater and inter-rater reliability analysis
The intraclass coefficient (ICC) and 95% confidence intervals (CI) were calculated for each ROM measure using a two-way random effects model where both people effects and measures effects are random. An ICC > 0.75 indicates good reliability.32 In addition to the ICCs, for the contribution of variance caused by subjects (Varsubject), occasion (Varoccasion) or measurement error (Varerror) was determined using variance components analysis, aiming to calculate the SEM and the smallest detectable difference (SDD) in Excel. SEM was calculated using the formula: SEM = √(Varoccasion + Varerror) and was calculated SDD using the formula: SDD = √2 ×1.96 × √(Varoccasion + Varerror).33
Results
Subject demographics
The distribution of age, hand dominance and BMI by sex of the 352 participants is presented in Table 1. An unpaired t-test did not show a statistically significant difference between the demographics of the male and female subjects (p < 0.05).
Table 1.
Subject demographics compared by sex (n=352).
| Male (n = 166, 47.2%) N (%) | Female (n = 186, 52.8%) N (%) | |
|---|---|---|
| Age in years, mean (95% CI) | 49 (45 to 51) | 45 (42 to 47) |
| Age categories (years) | ||
| 18 to 29 | 33 (19.9%) | 57 (30.6%) |
| 30 to 39 | 27 (16.3%) | 25 (13.4%) |
| 40 to 49 | 28 (16.9%) | 29 (15.6%) |
| 50 to 59 | 27 (16.3%) | 25 (13.4%) |
| 60 to 69 | 25 (15.1%) | 25 (13.4%) |
| 70 to 79 | 26 (15.7%) | 25 (13.4%) |
| BMI mean (95% CI) | 24.2 (23.6 to 24.7) | 23.5 (23.0 to 24.1) |
| BMI categories | ||
| < 18.50 | 6 (3.6%) | 8 (4.3%) |
| 18.50 to 24.99 | 105 (63.3%) | 133 (71.5%) |
| 25.00 to 29.99 | 40 (24.1%) | 34 (18.3%) |
| ≥ 30.00 | 15 (9.0%) | 11 (5.9%) |
| Dominance | ||
| Right | 150 (90.4%) | 167 (89.8%) |
| Left | 16 (9.6%) | 19 (10.2%) |
BMI, body mass index; CI, confidence interval.
Normative values for ROM based on subgroups
Table 2 presents average aROM and pROM values for male and female subjects (dominant and nondominant sides separately). An unpaired t-test showed significantly smaller ROM for all measurements for male subjects compared to females (p < 0.01).
Table 2.
Normative values for elbow range of motion (ROM) by sex.
| Movement | ROM in degrees, mean (95% CI) |
|||
|---|---|---|---|---|
| Male (n = 166) |
Female (n = 186) |
|||
| Dominant | Nondominant | Dominant | Nondominant | |
| Active | ||||
| Flexion | 143 (142 to 144) | 143 (142 to 144) | 148 (147 to 149) | 148 (147 to 149) |
| Extension | 0 (0 to 1) | 0 (−1 to 1) | −5 (−6 to −4) | −5 (−6 to −5) |
| Pronation | 78 (77 to 79) | 79 (78 to 80) | 82 (81 to 83) | 83 (82 to 84) |
| Supination | 85 (84 to 86) | 85 (83 to 86) | 88 (87 to 89) | 88 (87 to 89) |
| Passive | ||||
| Flexion | 147 (146 to 148) | 147 (146 to 148) | 153 (152 to 154) | 153 (152 to 154) |
| Extension | −2 (−2 to −1) | −2 (−3 to −1) | −8 (−9 to −7) | −9 (−10 to −8) |
| Pronation | 82 (81 to 83) | 83 (81 to 84) | 86 (85 to 87) | 87 (86 to 88) |
| Supination | 89 (88 to 90) | 88 (87 to 90) | 93 (92 to 94) | 92 (9 to 93) |
CI, confidence interval.
Differences in ROM between the dominant and nondominant sides varied from 0.3° to 0.7° and were statistically significant (p < 0.05) for all movements, except for active flexion. For all movements except pronation, the ROM of the dominant side was slightly larger compared to the nondominant side.
Compared to aROM, pROM was higher in flexion, pronation and supination and more negative in extension, all statistically significant (p < 0.001). Tables 3 and 4 present normative values by age and BMI, with aROM and pROM separately, for the dominant side. Differences between age groups (by sex) were all statistically significant (p < 0.001). For BMI, in females, all measurements between groups were statistically significant (p < 0.001). In males, active and passive flexion and passive pronation showed a statistically significant difference between BMI groups (p < 0.05). Note that the underweight and obese groups are relatively small.
Table 3.
Normative values by age.
| Dominant side ROM (°), mean (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Age category (years) | 18 to 29 | 30 to 39 | 40 to 49 | 50 to 59 | 60 to 69 | 70 to 79 |
| Male (n = 166) | 33 | 27 | 28 | 27 | 25 | 26 |
| Active | ||||||
| Flexion | 146 (144 to 148) | 145 (142 to 147) | 143 (141 to 146) | 143 (141 to 146) | 141 (139 t 143) | 139 (138 to 141) |
| Extension | −1 (−3 to 0) | −1 (−2 to 0) | 0 (−1 to 2) | 0 (−1 to 1) | 1 (−1 to 3) | 2 (1 to 4) |
| Pronation | 81 (79 to 83) | 80 (77 to 83) | 81 (78 to 83) | 79 (77 to 81) | 74 (72 to 76) | 74 (72 to 76) |
| Supination | 89 (88 to 91) | 87 (84 to 90) | 86 (84 to 88) | 85 (83 to 87) | 81 (78 to 84) | 81 (79 to 83) |
| Passive | ||||||
| Flexion | 151 (149 to 153) | 150 (147 to 152) | 147 (145 to 149) | 148 (146 to 150) | 144 (142 to 146) | 142.7 (141 to 144) |
| Extension | −3 (−5 to −2) | −2 (−4 to −1) | −2 (−4 to 1) | −2 (−3 to 0 | 0 (−2 to 1) | 1 (−1 to 2) |
| Pronation | 86 (84 to 87) | 83 (80 to 86) | 85 (82 to 87) | 83 (81 to 85) | 78 (75 to 80) | 77 (75 to 79) |
| Supination | 94 (92 to 96) | 92 (89 to 95) | 91 (89 to 93) | 89 (87 to 91) | 84 (82 to 87) | 83 (81 to 85) |
| Female (n = 186) | 57 | 25 | 29 | 25 | 25 | 25 |
| Active | ||||||
| Flexion | 149 (148 to 151) | 153 (152 to 155) | 149 (147 to 151) | 148 (146 to 149) | 145 (143 to 148) | 142 (140 to 144) |
| Extension | −8 (−10 to −6) | −6 (−8 to −4) | −5 (−7 to −3) | −1 (−3 to 2) | −2 (−4 to −1) | −2 (−4 to −01) |
| Pronation | 83 (82 to 85) | 87 (85 to 89) | 86 (84 to 87) | 80 (77 to 82) | 78 (75 to 81) | 76 (74 to 78) |
| Supination | 92 (90 to 93) | 93 (91 to 95) | 90 (89 to 91) | 87 (85 to 89) | 84 (81 to 86) | 81 (79 to 84) |
| Passive | ||||||
| Flexion | 155 (154 to 157) | 158 (156 to 160) | 154 (152 to 156) | 152 (150 to 154) | 149 (146 to 152) | 145 (143 to 147) |
| Extension | −12 (−14 to −10) | −10 (−12 to −8) | −8 (−11 to −6) | −3 (−6 to 0 | −5 (−7 to −4) | −4 (−6 to −3) |
| Pronation | 89 (88 to 91) | 91 (90 to 93) | 90 (89 to 91) | 84 (80 to 86) | 82 (79 to 85) | 79 (76 to 81) |
| Supination | 96 (96 to 98) | 98 (96 to 101) | 94 (92 to 95) | 91 (89 to 93) | 87 (85 to 89) | 84 (82 to 86) |
CI, confidence interval; ROM, range of motion.
Table 4.
Normative values by body mass index (BMI).
| Dominant side ROM (°), mean (95% CI) | ||||
|---|---|---|---|---|
| BMI category | < 18.50 | 18.50 to 24.99 | 25.00 to 29.99 | ≥ 30.00 |
| Male (n = 166) | 6 | 105 | 40 | 15 |
| Active | ||||
| Flexion | 151 (148 to 155) | 145 (144 to 146) | 140 (139 to 142) | 136 (134 to 138) |
| Extension | −2 (−4 to 1) | 0 (−1 to 1) | 1 (0 to 2) | 0 (−3 to 2) |
| Pronation | 84 (80 to 89) | 78 (77 to 80) | 77 (75 to 79) | 78 (75 to 81) |
| Supination | 90 (85 to 94) | 86 (85 to 87) | 83 (81 to 85) | 82 (80 to 85) |
| Passive | ||||
| Flexion | 155 (152 to 159) | 149 (148 to 150) | 144 (143 to 1456) | 140 (138 to 143) |
| Extension | −3 (−8 to 2) | −2 (−3 to −1) | −1 (−2 to 0) | −2 (−4 to 1) |
| Pronation | 89 (85 to 92) | 82 (81 to 84) | 81 (78 to 83) | 82 (79 to 85) |
| Supination | 95 (89 to 100) | 90 (89 to 91) | 87 (85 to 89) | 86 (83 to 89) |
| Female (n = 186) | 8 | 133 | 34 | 11 |
| Active | ||||
| Flexion | 157 (154 to 159) | 149 (148−150) | 146 (144 to 148) | 138 (135 to 141) |
| Extension | −15 (−17 to −12) | −5 (−6 to −4) | −3 (−6 to −1) | −2 (−5 to 2) |
| Pronation | 86 (82 to 89) | 82 (81 to 84) | 80 (78 to 82) | 78 (75 to 82) |
| Supination | 94 (90 to 97) | 89 (88 to 90) | 8 (84 to 89) | 84 (81 to 88) |
| Passive | ||||
| Flexion | 163 (161 to 166) | 154 (153 to 155) | 150 (148 to 152) | 142 (139 to 145) |
| Extension | −20 (−24 to −17) | −8 (−9 to −7) | −6 (−8 to −2) | −4 (−8 to −1) |
| Pronation | 91 (88 to 95) | 87 (86 to 88) | 84 (81 to 87) | 81 (77 to 85) |
| Supination | 100 (95 to 105) | 93 (92 to 95) | 90 (88 to 92) | 88 (84 to 92) |
CI, confidence interval; ROM, range of motion.
Correlations
Age correlated moderately (r ≥ 0.50) negative with passive pronation (dominant –0.50; nondominant –0.56) and supination (–0.56; –0.50). BMI correlated moderately negative on flexion, both active (–0.57; –0.59) and passive (–0.59; –0.59). Age correlated moderately negative with passive flexion (–0.59; –0.59). All other combinations showed low correlations (r < 0.50), ranging from –0.29 to –0.49 for flexion/pronation/supination and 0.22 to 0.44 for extension. No major differences in correlations were observed between the dominant and nondominant sides.
Intra- and inter-rater reliability
In the subgroup (n = 20) for intra-rater reliability analysis, only the difference in age between the intra-rater subgroup and total group was statistically significant. Intra-rater ICCs for all measurements showed good reliability. SEM and SDD were higher for pronation and supination compared to flexion and extension. Demographics of the subgroup (n = 10) for inter-rater reliability were not statistically significant different compared to the total group. Inter-rater ICCs showed good reliability (>0.75), apart from passive flexion (0.74). The SEM and SDD were slightly higher for pronation and supination compared to flexion and extension. Inter-rater ICCs, SEM and SDD were similar to intra-rater reliability. For both inter-rater and intra-rater reliability, the results from the dominant side were similar to nondominant side. The intra-rater and inter-rater reliability results from the dominant side are presented in Table 5.
Table 5.
Intra- and inter-rater reliability.
| Movement (dominant side) | Intra-rater reliability |
Inter-rater reliability |
||||
|---|---|---|---|---|---|---|
| ICC (95% CI) | SEM | SDD | ICC (95% CI) | SEM | SDD | |
| Active | ||||||
| Flexion | 0.76 (0.47 to 0.90) | 3° | 7° | 0.86 (0.53 to 0.96) | 2° | 5° |
| Extension | 0.92 (0.80 to 0.97) | 2° | 6° | 0.89 (0.63 to 0.97) | 1° | 4° |
| Pronation | 0.90 (0.77 to 0.96) | 3° | 8° | 0.92 (0.47 to 0.98) | 3° | 7° |
| Supination | 0.91 (0.78 to 0.96) | 3° | 8° | 0.87 (0.56 to 0.97) | 3° | 8° |
| Passive | ||||||
| Flexion | 0.74 (0.45 to 0.89) | 3° | 7° | 0.79 (0.33 to 0.94) | 2° | 6° |
| Extension | 0.95 (0.88 to 0.98) | 2° | 5° | 0.85 (0.52 to 0.96) | 2° | 5° |
| Pronation | 0.86 (0.69 to 0.94) | 3° | 9° | 0.91 (0.54 to 0.98) | 3° | 8° |
| Supination | 0.90 (0.75 to 0.96) | 3° | 7° | 0.82 (0.46 to 0.95) | 3° | 9° |
As an example, in dominant side active flexion the SEM was 3°, which means that individual scores had an average measurement error of 3°. SDD in this measurement was 7°, which means that, if the dominant side active elbow flexion for a subject changes by more than 7°, the change is considered as a true change with 95% confidence.
CI, confidence interval; ICC, intraclass coefficient; SDD, smallest detectable difference.
Discussion
In the present study, normative values for the elbow range of motion derived from a population of 352 healthy volunteers are presented. For male subjects, all ROM measurements were statistically significant lower compared to females. Higher age correlated moderately with lower ROM for passive flexion, pronation and supination. A higher BMI correlated with a lower ROM for active and passive flexion. Differences between the dominant and nondominant sides (< 1°) were too small to be clinically relevant. Therefore, in a general population, the examiner is able to decide whether the measured ROM is abnormal or not, by comparing the injured side with the uninjured side. This of course is combined with the information on the intra-rater reliability and patient specific characteristics such as (overhead throwing) sport activities. If abnormality arises bilaterally, the normative values for specific subgroups (provided in Tables 3 and 4) and correlations (in text) can be used to make an estimation of the expected ROM. Exact estimation of the ROM with all affecting factors incorporated such as sex, age and BMI is not possible as a result of the small numbers of subjects in certain groups (eg. underweight elderly).
The present study is not without limitations. A possible source of error might be unjustified inclusion of subjects who did not report factors that may influence the elbow ROM despite our written and oral inquiries. Given the large study population, we expect the influence of this potential source of error to be small. Furthermore, we did not ask for (professional) sports activities, therefore it is not possible to draw conclusions on the influence of sports on the elbow ROM.
We have chosen to exclude subjects under 18 years and therefore we could not draw conclusions for the paediatric population. A study by Golden et al.34 reported the mean elbow ROM in 300 healthy children supplemented with age- and sex related changes.
In the previous literature, two studies investigated differences between the ROM of the dominant and nondominant sides. One study showed statistically significant differences, with the mean difference varying from 1.7° to 2.6°4 and another study showed nonsignificant differences.35 Similar to the present study, in both studies, the differences were too small to be considered clinically relevant. However, in overhead throwing athletes, the flexion–extension range may be greatly (approximately 14°) decreased,2 being even more distinct up to 24 h after throwing.10 A study on the effect of obesity on active flexion showed no significant differences compared to subjects with an healthy BMI (20 kg/m2 to 25 kg/m2),36 in contrast to the present study. Nevertheless, significant negative correlations for BMI on elbow range of motion (flexion/extension) were found in obese children (right r = –0.54; left r = –0.43).37
For measuring elbow ROM, the universal goniometer is considered to be the most easy to use and clinically available tool.5,6,38–40 Studies published in the past show a good intra-rater and inter-rater reliability of goniometric elbow measurements for all measurements in both injured and healthy volunteers, with ICC ranging from 0.70 to 0.99.3,6,14,16,18 However, a study by Armstrong et al.15 showed lower inter-rater and intra-rater reliability in injured subjects for flexion and extension (0.45 to 0.99). In handball players, lower intra-rater reliability for flexion and extension was observed (0.49 to 0.93).3 One small study concerning inter-rater reliability in healthy subjects showed disappointing results for flexion and extension (ICC = 0.53).17 Because the ICC uses variance between the ROM measurements of subjects to calculate reliability, a large variation between subjects will lead to a higher ICC. This could possibly draw a misleading conclusion of good reliability. Therefore, in the present study, we decided to provide the statistical measures SEM and SDD. These measures provide more meaningful information for repeated measures within subjects, which is relevant for clinical practice.33,41 One study reported results in degrees for intra-rater reliability (mean within 1.2°) and inter-rater reliability (mean within 1.6°).4 Another study presented intra-rater SDDs of 7.8° for active flexion and 6.3° for active extension and inter-rater SDDs of 8.2° for flexion and 6.3° for extension.26 Intra-rater SEM was reported in one study with results from 1.4° to 1.6° for flexion and 1.0° to 1.2° for extension.3 No previous studies were found that reported SEM or SDD values for pronation and supination.
In our reliability analysis, both intra-rater and inter-rater ICCs for all measurements showed good reliability, ranging from 0.74 to 0.95. Reliability analysis for the dominant and nondominant sides was not statistically significant different; therefore, we reported the dominant side only. Relative low ICCs were found for flexion as a result of the small variation of flexion ROM amongst subjects. Our results corresponded with studies measuring non-injured subjects.3,6,16–18 Intra-rater SEM values ranged from 2° to 3° and SDD values ranged from 5° to 9°. Of these measures, passive pronation was the least reliable, with a SEM of 3° and SDD of 9°. Accordingly, in this example, an individual score had an average measurement error of 3° and, for a repetitive measurement, the difference must be minimum of 9° to be considered as a true change with 95% confidence. Inter-rater SEM ranged from 1° to 3° and SDD from 4° to 9° and this applies to measurements between different examiners.
Conclusions
Elbow ROM measurement was conducted on 352 healthy subjects and was found to be influenced by sex, age and BMI. For all movements, males have a significantly smaller range of motion. Also, a higher age correlates with a smaller passive pronation–supination range of motion and a higher BMI with less flexion. Differences between the the dominant and nondominant sides were too small to be clinically relevant; therefore, in the general population, the ROM of the opposite side could serve as a reference for the injured side.
Acknowledgements
We would like to thank our colleague Paul Hoogervorst for performing the measurements for the inter-rater reliability.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: We have read and understood SAGE policy on declaration of interests and declare that we have no competing interests.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Ethical Approval was given by the Medical Ethical Committee of the OLVG on the 18th of September, 2015 in Amsterdam, the Netherlands. Assigned study number: WO15.069.
Level of Evidence
Level II: study of diagnostic test
References
- 1.Soucie JM, Wang C, Forsyth A, et al. Range of motion measurements: reference values and a database for comparison studies. Haemophilia 2011; 17: 500–507. [DOI] [PubMed] [Google Scholar]
- 2.Wright RW, Steger-May K, Wasserlauf BL, O'Neal ME, Weinberg BW, Paletta GA. Elbow range of motion in professional baseball pitchers. Am J Sports Med 2006; 34: 190–193. [DOI] [PubMed] [Google Scholar]
- 3.Fieseler G, Molitor T, Irlenbusch L, et al. Intrarater reliability of goniometry and hand-held dynamometry for shoulder and elbow examinations in female team handball athletes and asymptomatic volunteers. Arch Orthop Trauma Surg 2015; 135: 1719–1726. [DOI] [PubMed] [Google Scholar]
- 4.Gunal I, Kose N, Erdogan O, Gokturk E, Seber S. Normal range of motion of the joints of the upper extremity in male subjects, with special reference to side. J Bone Joint Surg Am 1996; 78: 1401–1404. [DOI] [PubMed] [Google Scholar]
- 5.Karagiannopoulos C, Sitler M, Michlovitz S. Reliability of 2 functional goniometric methods for measuring forearm pronation and supination active range of motion. J Orthop Sports Phys Ther 2003; 33: 523–531. [DOI] [PubMed] [Google Scholar]
- 6.Chapleau J, Canet F, Petit Y, Laflamme GY, Rouleau DM. Validity of goniometric elbow measurements: comparative study with a radiographic method. Clin Orthop Relat Res 2011; 469: 3134–3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am 1981; 63: 872–877. [PubMed] [Google Scholar]
- 8.Sardelli M, Tashjian RZ, MacWilliams BA. Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am 2011; 93: 471–477. [DOI] [PubMed] [Google Scholar]
- 9.Raiss P, Rettig O, Wolf S, Loew M, Kasten P. [Range of motion of shoulder and elbow in activities of daily life in 3D motion analysis]. Z Orthop Unfall 2007; 145: 493–498. [DOI] [PubMed] [Google Scholar]
- 10.Reinold MM, Wilk KE, Macrina LC, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med 2008; 36: 523–527. [DOI] [PubMed] [Google Scholar]
- 11.Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med 2014; 42: 2075–2081. [DOI] [PubMed] [Google Scholar]
- 12.Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med 2011; 39: 1997–2006. [DOI] [PubMed] [Google Scholar]
- 13.Spinner M, Kaplan EB. The quadrate ligament of the elbow – its relationship to the stability of the proximal radio-ulnar joint. Acta Orthop Scand 1970; 41: 632–647. [DOI] [PubMed] [Google Scholar]
- 14.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther 1983; 63: 1611–1615. [DOI] [PubMed] [Google Scholar]
- 15.Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg 1998; 7: 573–580. [DOI] [PubMed] [Google Scholar]
- 16.Gajdosik RL. Comparison and reliability of three goniometric methods for measuring forearm supination and pronation. Percept Mot Skills 2001; 93: 353–355. [DOI] [PubMed] [Google Scholar]
- 17.Petherick M, Rheault W, Kimble S, Lechner C, Senear V. Concurrent validity and intertester reliability of universal and fluid-based goniometers for active elbow range of motion. Phys Ther 1988; 68: 966–969. [DOI] [PubMed] [Google Scholar]
- 18.Blonna D, Zarkadas PC, Fitzsimmons JS, O'Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg 2012; 21: 29–35. [DOI] [PubMed] [Google Scholar]
- 19.Docherty MA, Schwab RA, Ma OJ. Can elbow extension be used as a test of clinically significant injury? South Med J 2002; 95: 539–541. [PubMed] [Google Scholar]
- 20.Lennon RI, Riyat MS, Hilliam R, Anathkrishnan G, Alderson G. Can a normal range of elbow movement predict a normal elbow x ray? Emerg Med J 2007; 24: 86–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med 1986; 5: 621–636. [PubMed] [Google Scholar]
- 22.King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res 1969; 67: 116–123. [PubMed] [Google Scholar]
- 23.Morrey BF. Applied anatomy and biomechanics of the elbow joint. Instr Course Lect 1986; 35: 59–68. [PubMed] [Google Scholar]
- 24.Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry, Philadelphia, PA: F.A. Davis, 2009. [Google Scholar]
- 25.Shaaban H, Pereira C, Williams R, Lees VC. The effect of elbow position on the range of supination and pronation of the forearm. J Hand Surg Eur 2008; 33: 3–8. [DOI] [PubMed] [Google Scholar]
- 26.Cleffken B, van BG, van MH, Brink P, Olde DS. Test-retest reproducibility of elbow goniometric measurements in a rigid double-blinded protocol: intervals for distinguishing between measurement error and clinical change. J Shoulder Elbow Surg 2007; 16: 788–794. [DOI] [PubMed] [Google Scholar]
- 27.Philippou A, Maridaki M, Bogdanis GC. Angle-specific impairment of elbow flexors strength after isometric exercise at long muscle length. J Sports Sci 2003; 21: 859–865. [DOI] [PubMed] [Google Scholar]
- 28.Stokdijk M, Biegstraaten M, Ormel W, de Boer YA, Veeger HE, Rozing PM. Determining the optimal flexion-extension axis of the elbow in vivo – a study of interobserver and intraobserver reliability. J Biomech 2000; 33: 1139–1145. [DOI] [PubMed] [Google Scholar]
- 29.Fish DR, Wingate L. Sources of goniometric error at the elbow. Phys Ther 1985; 65: 1666–1670. [DOI] [PubMed] [Google Scholar]
- 30.Shiba R, Sorbie C, Siu DW, Bryant JT, Cooke TD, Wevers HW. Geometry of the humeroulnar joint. J Orthop Res 1988; 6: 897–906. [DOI] [PubMed] [Google Scholar]
- 31.Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452. [PubMed] [Google Scholar]
- 32.Portney LG, Watkins MP. Foundations of clinical research: applications to practise, Upper Saddle River, NJ: Prentice-Hall, 2000. [Google Scholar]
- 33.Roebroek ME, Harlaar J, Lankhorst GJ. The application of generalization theory to reliability assesment: an illustration using isometric force measurements. Phys Ther 1993; 73: 386–395. [DOI] [PubMed] [Google Scholar]
- 34.Golden DW, Jhee JT, Gilpin SP, Sawyer JR. Elbow range of motion and clinical carrying angle in a healthy pediatric population. J Pediatr Orthop B 2007; 16: 144–149. [DOI] [PubMed] [Google Scholar]
- 35.Macedo LG, Magee DJ. Differences in range of motion between dominant and nondominant sides of upper and lower extremities. J Manipulative Physiol Ther 2008; 31: 577–582. [DOI] [PubMed] [Google Scholar]
- 36.Park W, Ramachandran J, Weisman P, Jung ES. Obesity effect on male active joint range of motion. Ergonomic 2010; 53: 102–108. [DOI] [PubMed] [Google Scholar]
- 37.Golden DW, Wojcicki JM, Jhee JT, Gilpin SL, Sawyer JR, Heyman MB. Body mass index and elbow range of motion in a healthy pediatric population: a possible mechanism of overweight in children. J Pediatr Gastroenterol Nutr 2008; 46: 196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gajdosik RL, Bohannon RW. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys Ther 1987; 67: 1867–1872. [DOI] [PubMed] [Google Scholar]
- 39.Hawi N, Liodakis E, Musolli D, et al. Range of motion assessment of the shoulder and elbow joints using a motion sensing input device: a pilot study. Technol Health Care 2014; 22: 289–295. [DOI] [PubMed] [Google Scholar]
- 40.van de Pol RJ, van TE, Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother 2010; 56: 7–17. [DOI] [PubMed] [Google Scholar]
- 41.Scholtes VA, Terwee CB, Poolman RW. What makes a measurement instrument valid and reliable? Injury 2011; 42: 236–240. [DOI] [PubMed] [Google Scholar]